From the Journals
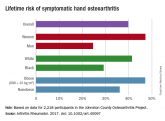
Lifetime risk of hand OA comes close to 40%
Risk approaches 50% for women and the obese, according to data from the Johnston County Osteoarthritis Project.

EULAR has updated its 2007 guidelines for the management of hand osteoarthritis. I find the recommendations helpful, and I have no disagreements.
The authors performed a systematic literature review that was more complete than the original guidelines. In addition, the methodology in developing the guidelines was updated utilizing the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) system to guide the expert opinion. The manuscript presents recommendations that are carefully supported in the text. To understand guidelines, one really needs to read the text.
They have developed a set of overarching principles that precede the recommendations. These principles address the goals of therapy, patient education, comorbidities, decision-making involving the patient, and the common need for the multidisciplinary approach.The update lists a set of research questions, similar to the 2007 recommendations.
The authors group their therapeutic recommendations according to nonpharmacologic, pharmacologic, and surgical approaches, as well as about the need for follow-up. The three nonpharmacologic recommendations include education and training, exercise and muscle strengthening, and the use of orthoses. The pharmacologic approach includes topical therapy as a first-line, oral NSAIDs and analgesics, chondroitin sulfate, and intra-articular injections. There is a negative recommendation for the use of biologics. The surgical recommendation is directed at the relief of pain. The last recommendation emphasizes the need for follow-up and individual care.
The differences between the recommendations include the removal of acetaminophen as a first-line therapy. Indeed, it seems to be barely recommended at all. In addition, there is an emphasis on topical therapy, particularly NSAIDs. The authors are equivocal on the recommendations for intra-articular therapy. Paraffin and local heat are no longer included. The recommendation against biologic therapy is new. They included agents used for rheumatoid arthritis, such as methotrexate, in this negative recommendation.
These new recommendations are an update of guidelines that are over 10 years old. They are practical and helpful. Unfortunately, more research is needed as the present day therapy is often inadequate.
Roy D. Altman, MD, is professor emeritus of medicine in the division of rheumatology and immunology at the University of California, Los Angeles. He is a consultant to Ferring, Flexion, GlaxoSmithKline, Novartis, Olatec, Pfizer, and Sorrento Therapeutics.
FROM ANNALS OF THE RHEUMATIC DISEASES
Updated EULAR recommendations on the management of hand osteoarthritis include five overarching principles as well as two new recommendations that reflect new research in the field.
The task force, led by Margreet Kloppenburg, MD, PhD, of the department of rheumatology at Leiden (the Netherlands) University Medical Center, noted that a decade had passed since the first recommendations were published in 2007.
“It was timely to update the recommendations, as many new studies had emerged during this period. In light of this new evidence, many of the 2007 recommendations were modified and new recommendations were added,” wrote Dr. Kloppenburg and her colleagues. The recommendations were published online in Annals of the Rheumatic Diseases.
They noted that the recommendations were targeted to all health professionals across primary and secondary care but also aimed to inform patients about their disease to “support shared decision making.”
In line with other EULAR sets of management recommendations, the update included five overarching principles that cover treatment goals, information and education for patients, individualization of treatment, shared decision making between clinicians and patients, and the need to take into consideration a multidisciplinary and multimodal (pharmacologic and nonpharmacologic) treatment approach.
The authors noted that for a long time hand OA was a “forgotten disease” and this was reflected by the paucity of clinical trials in the area. As a direct consequence, previous recommendations were based on expert opinion rather than evidence.
However, new data allowed the task force to recommend not to treat patients with hand OA with conventional synthetic or biologic disease-modifying antirheumatic drugs (DMARDs). The recommendation achieved the strongest level of evidence and a high level of agreement from the 19-member expert panel, which included 2 patient research partners. The authors said the recommendation was based on newer studies that demonstrated a lack of efficacy of csDMARDs and bDMARDs.
The authors also advised adapting the long-term follow-up of patients with hand OA to individual needs, although they noted this was based on expert opinion alone and that in the absence of a disease-modifying treatment, the goal of follow-up differs from that of many other rheumatic diseases. Individual needs will dictate the degree of follow-up required, based on the severity of symptoms, presence of erosive disease, reevaluation of the use of pharmacologic therapy, and a patient’s wishes and expectations. They also noted that “for most patients, standard radiographic follow-up is not useful at this moment” and that “follow-up does not necessarily have to be performed by a rheumatologist.
“Follow-up will likely increase adherence to nonpharmacological therapies like exercise or orthoses, and provides an opportunity for reevaluation of treatment,” they wrote.
The recommendations advise offering education and training in ergonomic principles and exercises to patients to improve function and muscle strength, as well as considering the use of orthoses in some patients.
Treatment recommendations suggested preferring topical treatments over systemic treatments and that oral analgesics, particularly NSAIDs, should be considered for a limited duration. The authors advised that chondroitin sulfate may be used in patients for pain relief and improvement in functioning and that intra-articular glucocorticoids should not generally be used but may be considered in patients with painful interphalangeal joints. Surgery should be considered for patients with structural abnormalities when other treatment modalities have not been sufficiently effective in relieving pain.
The recommendations were funded by EULAR. Several of the authors reported receiving consultancy fees and/or honoraria as well as research funding from industry.
SOURCE: Kloppenburg M et al. Ann Rheum Dis. 2018 Aug 28. doi: 10.1136/annrheumdis-2018-213826.
Risk approaches 50% for women and the obese, according to data from the Johnston County Osteoarthritis Project.
