User login
Medicare Outlines Anticipated Funding Changes Under Affordable Care Act
The Centers for Medicare & Medicaid Services (CMS) recently released a few Fact Sheets on how they anticipate funding changes on a few of their programs that were implemented (or sustained) under the Affordable Care Act. As a background, CMS pays most acute-care hospitals by prospectively determining payment based on a patient’s diagnosis and the severity of illness within that diagnosis (e.g. “MS-DRG”). These payment amounts are updated annually after evaluating several factors, including the costs associated with the delivery of care.
One of the most major changes described in the Fact Sheet that will affect hospitalists is how CMS will review inpatient stays based on the number of nights in the hospital. CMS has proposed that any patient who stays in the hospital for two or more “midnights” should be appropriate for payment under Medicare Part A. For those who stay in the hospital for only one (or zero) midnights, payment under Medicare Part A will only be appropriate if:
- There is sufficient documentation at the time of admission that the anticipated length of stay is two or more nights; and.
- Further documentation that circumstances changed, and the hospital stay ended prematurely because of those changes.
Overall for hospitalists, this should substantially simplify the admitting process, whereby most inpatients being admitted with the anticipation of two or more nights should qualify for an inpatient stay. This also reduces the administrative burden of correcting the “inpatient” versus “observation” designation, which keeps many hospital staffs entirely too busy. This change also should relieve a significant burden from the patients and their families, who if kept in observation for a period of time, may have to pay substantially out of pocket to make up for the difference between the cost of the stay and the reimbursement from CMS for observation status. So this is one of the moves that CMS is making to simplify (and not complicate) an already too-complicated payment system. This should go into effect October 2013 and will be a sigh of much relief from many of us.
A few other anticipated changes that will affect hospitalists include:
Payments for Unfunded Care
Another major change that will go into affect October 2013 is the amount of monies received by hospitals that care for unfunded patients. These payments historically have been made to “Disproportionate Share Hospitals” (DSH), which are hospitals that care for a higher percentage of unfunded patients. Under the Affordable Care Act, only 25% of these payments will be distributed to DSH hospitals; the remaining 75% will be reduced based on the number of uninsured in the U.S., then redistributed to DSH hospitals based on their portion of uninsured care delivered.
Most DSH hospitals should expect a decrease in DSH payments, the amount of which will depend on their share of unfunded patients.
Any reduction in the “bottom line” to the hospital can affect hospitalists, especially those who are directly employed by the hospital.
Hospital-Acquired Conditions
CMS has long had the Hospital-Acquired Condition (HAC) program in effect, which has the ability to reduce the amount of payment for inpatients who acquire a HAC during their hospital stay. Starting in October 2014, CMS will impose additional financial penalties for hospitals with high HAC rates.
Specifically, those hospitals in the highest 25th percentile of HAC rates will be penalized 1% of their overall CMS payments. Another proposed change is that the following be included in the HAC reduction plan (two “domains” of measures):
- Domain No. 1: Six of the AHRQ Patient Safety Indicators (PSIs), including pressure ulcers, foreign bodies left in after surgery, iatrogenic pneumothorax, postoperative physiologic or metabolic derangements, postoperative VTE, and accidental puncture/laceration.
- Domain No. 2: Central-line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTIs).
The domains will be weighted equally, and an average score will determine the total score. There will be some methodology for risk adjustment, and hospitals will be given a review and comment period to validate their own scores.
Most hospitalists have at least indirect control over many of these HACs,and all need to pay very close attention to their hospital’s rates of these now and in the future.
Readmissions
As we all know, the Hospital Readmission Reduction program went into effect October 2012; it placed 1% of CMS payments at risk. This will increase to 2% of payments as of October 2013. CMS will continue to use AMI, CHF, and pneumonia as the three conditions under which the readmissions are measured but will put in some methodology to account for planned readmissions.
In addition, in October 2014, they plan to add readmission rates for COPD and for hip/knee arthroplasty.
Hospitalists will continue to need to progress their transitions of care programs, at least for these five patients conditions but more likely (and more effectively) for all hospital discharges.
Quality Measures
Currently more than 99% of acute-care hospitals participate in the pay-for-reporting quality program through CMS, the results of which have been displayed on the Hospital Compare website (www.hospitalcompare.hhs.gov) for years. The program started in 2004 with 10 quality metrics and now includes 57 metrics. These include process and outcome measures for AMI, CHF, and pneumonia, as well as process measures for surgical care, HACs, and patient-satisfaction surveys, among others.
This program will continue to expand over time, including hospital-acquired MRSA and Clostridium difficile rates. The few hospitals not participating will have their CMS annual payments reduced by 2%.
EHR Incentives
CMS is evaluating ways to reduce the burden of reporting by aligning EHR incentives with the Inpatient Quality Reporting program.
Summary
After an open commentary period, the Final Rule will be published Aug. 1, and will become effective for discharges on or after Oct. 1. Although CMS will continue to expand the total number of measures that need to be reported, and the penalties for non-reporting or low performance will continue to escalate, CMS is at least attempting to reduce the overall burden of reporting by combining measures and programs over time and using EHRs to facilitate the bulk of reporting over time.
The global message to hospitalists is: Continue to focus on reducing the burden of HACs, enhance throughput, and carefully and thoughtfully transition patients to the next provider after their hospital discharge. All in all, although at times this can feel overwhelming, these changes represent the right direction to move for high-quality and safe patient care.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
The Centers for Medicare & Medicaid Services (CMS) recently released a few Fact Sheets on how they anticipate funding changes on a few of their programs that were implemented (or sustained) under the Affordable Care Act. As a background, CMS pays most acute-care hospitals by prospectively determining payment based on a patient’s diagnosis and the severity of illness within that diagnosis (e.g. “MS-DRG”). These payment amounts are updated annually after evaluating several factors, including the costs associated with the delivery of care.
One of the most major changes described in the Fact Sheet that will affect hospitalists is how CMS will review inpatient stays based on the number of nights in the hospital. CMS has proposed that any patient who stays in the hospital for two or more “midnights” should be appropriate for payment under Medicare Part A. For those who stay in the hospital for only one (or zero) midnights, payment under Medicare Part A will only be appropriate if:
- There is sufficient documentation at the time of admission that the anticipated length of stay is two or more nights; and.
- Further documentation that circumstances changed, and the hospital stay ended prematurely because of those changes.
Overall for hospitalists, this should substantially simplify the admitting process, whereby most inpatients being admitted with the anticipation of two or more nights should qualify for an inpatient stay. This also reduces the administrative burden of correcting the “inpatient” versus “observation” designation, which keeps many hospital staffs entirely too busy. This change also should relieve a significant burden from the patients and their families, who if kept in observation for a period of time, may have to pay substantially out of pocket to make up for the difference between the cost of the stay and the reimbursement from CMS for observation status. So this is one of the moves that CMS is making to simplify (and not complicate) an already too-complicated payment system. This should go into effect October 2013 and will be a sigh of much relief from many of us.
A few other anticipated changes that will affect hospitalists include:
Payments for Unfunded Care
Another major change that will go into affect October 2013 is the amount of monies received by hospitals that care for unfunded patients. These payments historically have been made to “Disproportionate Share Hospitals” (DSH), which are hospitals that care for a higher percentage of unfunded patients. Under the Affordable Care Act, only 25% of these payments will be distributed to DSH hospitals; the remaining 75% will be reduced based on the number of uninsured in the U.S., then redistributed to DSH hospitals based on their portion of uninsured care delivered.
Most DSH hospitals should expect a decrease in DSH payments, the amount of which will depend on their share of unfunded patients.
Any reduction in the “bottom line” to the hospital can affect hospitalists, especially those who are directly employed by the hospital.
Hospital-Acquired Conditions
CMS has long had the Hospital-Acquired Condition (HAC) program in effect, which has the ability to reduce the amount of payment for inpatients who acquire a HAC during their hospital stay. Starting in October 2014, CMS will impose additional financial penalties for hospitals with high HAC rates.
Specifically, those hospitals in the highest 25th percentile of HAC rates will be penalized 1% of their overall CMS payments. Another proposed change is that the following be included in the HAC reduction plan (two “domains” of measures):
- Domain No. 1: Six of the AHRQ Patient Safety Indicators (PSIs), including pressure ulcers, foreign bodies left in after surgery, iatrogenic pneumothorax, postoperative physiologic or metabolic derangements, postoperative VTE, and accidental puncture/laceration.
- Domain No. 2: Central-line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTIs).
The domains will be weighted equally, and an average score will determine the total score. There will be some methodology for risk adjustment, and hospitals will be given a review and comment period to validate their own scores.
Most hospitalists have at least indirect control over many of these HACs,and all need to pay very close attention to their hospital’s rates of these now and in the future.
Readmissions
As we all know, the Hospital Readmission Reduction program went into effect October 2012; it placed 1% of CMS payments at risk. This will increase to 2% of payments as of October 2013. CMS will continue to use AMI, CHF, and pneumonia as the three conditions under which the readmissions are measured but will put in some methodology to account for planned readmissions.
In addition, in October 2014, they plan to add readmission rates for COPD and for hip/knee arthroplasty.
Hospitalists will continue to need to progress their transitions of care programs, at least for these five patients conditions but more likely (and more effectively) for all hospital discharges.
Quality Measures
Currently more than 99% of acute-care hospitals participate in the pay-for-reporting quality program through CMS, the results of which have been displayed on the Hospital Compare website (www.hospitalcompare.hhs.gov) for years. The program started in 2004 with 10 quality metrics and now includes 57 metrics. These include process and outcome measures for AMI, CHF, and pneumonia, as well as process measures for surgical care, HACs, and patient-satisfaction surveys, among others.
This program will continue to expand over time, including hospital-acquired MRSA and Clostridium difficile rates. The few hospitals not participating will have their CMS annual payments reduced by 2%.
EHR Incentives
CMS is evaluating ways to reduce the burden of reporting by aligning EHR incentives with the Inpatient Quality Reporting program.
Summary
After an open commentary period, the Final Rule will be published Aug. 1, and will become effective for discharges on or after Oct. 1. Although CMS will continue to expand the total number of measures that need to be reported, and the penalties for non-reporting or low performance will continue to escalate, CMS is at least attempting to reduce the overall burden of reporting by combining measures and programs over time and using EHRs to facilitate the bulk of reporting over time.
The global message to hospitalists is: Continue to focus on reducing the burden of HACs, enhance throughput, and carefully and thoughtfully transition patients to the next provider after their hospital discharge. All in all, although at times this can feel overwhelming, these changes represent the right direction to move for high-quality and safe patient care.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
The Centers for Medicare & Medicaid Services (CMS) recently released a few Fact Sheets on how they anticipate funding changes on a few of their programs that were implemented (or sustained) under the Affordable Care Act. As a background, CMS pays most acute-care hospitals by prospectively determining payment based on a patient’s diagnosis and the severity of illness within that diagnosis (e.g. “MS-DRG”). These payment amounts are updated annually after evaluating several factors, including the costs associated with the delivery of care.
One of the most major changes described in the Fact Sheet that will affect hospitalists is how CMS will review inpatient stays based on the number of nights in the hospital. CMS has proposed that any patient who stays in the hospital for two or more “midnights” should be appropriate for payment under Medicare Part A. For those who stay in the hospital for only one (or zero) midnights, payment under Medicare Part A will only be appropriate if:
- There is sufficient documentation at the time of admission that the anticipated length of stay is two or more nights; and.
- Further documentation that circumstances changed, and the hospital stay ended prematurely because of those changes.
Overall for hospitalists, this should substantially simplify the admitting process, whereby most inpatients being admitted with the anticipation of two or more nights should qualify for an inpatient stay. This also reduces the administrative burden of correcting the “inpatient” versus “observation” designation, which keeps many hospital staffs entirely too busy. This change also should relieve a significant burden from the patients and their families, who if kept in observation for a period of time, may have to pay substantially out of pocket to make up for the difference between the cost of the stay and the reimbursement from CMS for observation status. So this is one of the moves that CMS is making to simplify (and not complicate) an already too-complicated payment system. This should go into effect October 2013 and will be a sigh of much relief from many of us.
A few other anticipated changes that will affect hospitalists include:
Payments for Unfunded Care
Another major change that will go into affect October 2013 is the amount of monies received by hospitals that care for unfunded patients. These payments historically have been made to “Disproportionate Share Hospitals” (DSH), which are hospitals that care for a higher percentage of unfunded patients. Under the Affordable Care Act, only 25% of these payments will be distributed to DSH hospitals; the remaining 75% will be reduced based on the number of uninsured in the U.S., then redistributed to DSH hospitals based on their portion of uninsured care delivered.
Most DSH hospitals should expect a decrease in DSH payments, the amount of which will depend on their share of unfunded patients.
Any reduction in the “bottom line” to the hospital can affect hospitalists, especially those who are directly employed by the hospital.
Hospital-Acquired Conditions
CMS has long had the Hospital-Acquired Condition (HAC) program in effect, which has the ability to reduce the amount of payment for inpatients who acquire a HAC during their hospital stay. Starting in October 2014, CMS will impose additional financial penalties for hospitals with high HAC rates.
Specifically, those hospitals in the highest 25th percentile of HAC rates will be penalized 1% of their overall CMS payments. Another proposed change is that the following be included in the HAC reduction plan (two “domains” of measures):
- Domain No. 1: Six of the AHRQ Patient Safety Indicators (PSIs), including pressure ulcers, foreign bodies left in after surgery, iatrogenic pneumothorax, postoperative physiologic or metabolic derangements, postoperative VTE, and accidental puncture/laceration.
- Domain No. 2: Central-line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTIs).
The domains will be weighted equally, and an average score will determine the total score. There will be some methodology for risk adjustment, and hospitals will be given a review and comment period to validate their own scores.
Most hospitalists have at least indirect control over many of these HACs,and all need to pay very close attention to their hospital’s rates of these now and in the future.
Readmissions
As we all know, the Hospital Readmission Reduction program went into effect October 2012; it placed 1% of CMS payments at risk. This will increase to 2% of payments as of October 2013. CMS will continue to use AMI, CHF, and pneumonia as the three conditions under which the readmissions are measured but will put in some methodology to account for planned readmissions.
In addition, in October 2014, they plan to add readmission rates for COPD and for hip/knee arthroplasty.
Hospitalists will continue to need to progress their transitions of care programs, at least for these five patients conditions but more likely (and more effectively) for all hospital discharges.
Quality Measures
Currently more than 99% of acute-care hospitals participate in the pay-for-reporting quality program through CMS, the results of which have been displayed on the Hospital Compare website (www.hospitalcompare.hhs.gov) for years. The program started in 2004 with 10 quality metrics and now includes 57 metrics. These include process and outcome measures for AMI, CHF, and pneumonia, as well as process measures for surgical care, HACs, and patient-satisfaction surveys, among others.
This program will continue to expand over time, including hospital-acquired MRSA and Clostridium difficile rates. The few hospitals not participating will have their CMS annual payments reduced by 2%.
EHR Incentives
CMS is evaluating ways to reduce the burden of reporting by aligning EHR incentives with the Inpatient Quality Reporting program.
Summary
After an open commentary period, the Final Rule will be published Aug. 1, and will become effective for discharges on or after Oct. 1. Although CMS will continue to expand the total number of measures that need to be reported, and the penalties for non-reporting or low performance will continue to escalate, CMS is at least attempting to reduce the overall burden of reporting by combining measures and programs over time and using EHRs to facilitate the bulk of reporting over time.
The global message to hospitalists is: Continue to focus on reducing the burden of HACs, enhance throughput, and carefully and thoughtfully transition patients to the next provider after their hospital discharge. All in all, although at times this can feel overwhelming, these changes represent the right direction to move for high-quality and safe patient care.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
Should Skyrocketing Health Care Costs Concern Hospitalists?
Median hospitalist compensation has grown steadily over the past decade, but physicians aren’t immune to the sting of accelerated premiums, copays, and contributions imposed by health insurers.
According to the Hay Group’s 2011 Physician Compensation Survey, the number of physicians who contributing to health insurance premiums increased to 68% in 2011 from 58% in 2010. The survey showed only 9% of physicians did not pay anything for medical coverage, down from 19% in 2010.
Moreover, the expected physician contribution was between 1% and 25% of the premium.
Dan Fuller, president and cofounder of Alpharetta, Ga.-based IN Compass Health, has noticed an uptick in candidates’ interest in their health-care benefits. “Especially for physicians who have families, health benefits have become one of the top issues in recruiting,” the SHM Practice Analysis Committee (PAC) member says.
Christopher Frost, MD, FHM, medical director of hospital medicine at the Hospital Corporation of America in Nashville, Tenn., reports that he is seeing an upward trend in employees’ contributions to premiums and out-of-pocket costs. He’s also observed colleagues becoming more selective when choosing their own health-care plans and how they use those plans.
Gretchen Henkel is a freelance writer in California.
Median hospitalist compensation has grown steadily over the past decade, but physicians aren’t immune to the sting of accelerated premiums, copays, and contributions imposed by health insurers.
According to the Hay Group’s 2011 Physician Compensation Survey, the number of physicians who contributing to health insurance premiums increased to 68% in 2011 from 58% in 2010. The survey showed only 9% of physicians did not pay anything for medical coverage, down from 19% in 2010.
Moreover, the expected physician contribution was between 1% and 25% of the premium.
Dan Fuller, president and cofounder of Alpharetta, Ga.-based IN Compass Health, has noticed an uptick in candidates’ interest in their health-care benefits. “Especially for physicians who have families, health benefits have become one of the top issues in recruiting,” the SHM Practice Analysis Committee (PAC) member says.
Christopher Frost, MD, FHM, medical director of hospital medicine at the Hospital Corporation of America in Nashville, Tenn., reports that he is seeing an upward trend in employees’ contributions to premiums and out-of-pocket costs. He’s also observed colleagues becoming more selective when choosing their own health-care plans and how they use those plans.
Gretchen Henkel is a freelance writer in California.
Median hospitalist compensation has grown steadily over the past decade, but physicians aren’t immune to the sting of accelerated premiums, copays, and contributions imposed by health insurers.
According to the Hay Group’s 2011 Physician Compensation Survey, the number of physicians who contributing to health insurance premiums increased to 68% in 2011 from 58% in 2010. The survey showed only 9% of physicians did not pay anything for medical coverage, down from 19% in 2010.
Moreover, the expected physician contribution was between 1% and 25% of the premium.
Dan Fuller, president and cofounder of Alpharetta, Ga.-based IN Compass Health, has noticed an uptick in candidates’ interest in their health-care benefits. “Especially for physicians who have families, health benefits have become one of the top issues in recruiting,” the SHM Practice Analysis Committee (PAC) member says.
Christopher Frost, MD, FHM, medical director of hospital medicine at the Hospital Corporation of America in Nashville, Tenn., reports that he is seeing an upward trend in employees’ contributions to premiums and out-of-pocket costs. He’s also observed colleagues becoming more selective when choosing their own health-care plans and how they use those plans.
Gretchen Henkel is a freelance writer in California.
Advanced-Practice Providers Have More to Offer Hospital Medicine Groups
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
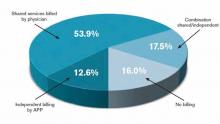
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Effective Clinical Documentation Can Influence Medicare Reimbursement
Back in the 1980s, I would go by medical records every day or two and find, on the front of the charts of my recently discharged patients, a form listing the diagnoses the hospital was billing to Medicare. Before the hospital could submit a patient’s bill, the attending physician was required to review the form and, by signing it, indicate agreement.
The requirement for this signature by the physician went away a long time ago and in my memory is one of the very few examples of reducing a doctor’s paperwork.
For my first few months in practice, I regularly would seek out the people who completed the form and explain they had misunderstood the patient’s clinical situation. “The main issue was a urinary tract infection,” I would say, “but you listed diabetes as the principal diagnosis.”
I don’t ever remember them changing anything based on my feedback. Instead, they explained to me that, for billing purposes, it was legitimate to list diabetes as the principal diagnosis because it had the additional benefit of resulting in a higher payment to the hospital than having “urinary tract infection” listed first.
Such was my introduction to the world of documentation and coding for hospital billing purposes and how it can sometimes differ significantly from the way a doctor sees the clinical picture. Things have evolved a lot since then, but the way doctors document medical conditions still has a huge influence on hospital reimbursement.
Hospital CDI Programs
About 80% of hospitals have formal clinical documentation improvement (CDI) programs to help ensure all clinical conditions are captured and described in the medical record in ways that are valuable for billing and other recordkeeping purposes. These programs might lead to you receive queries about your documentation. For example, you might be asked to clarify whether your patient’s pneumonia might be on the basis of aspiration.
Within SHM’s Code-H program, Dr. Richard Pinson, a former ED physician who now works with Houston-based HCQ Consulting, has a good presentation explaining these documentation issues. In it, he makes the point that, in addition to influencing how hospitals are paid, the way various conditions are documented also influences quality ratings.
Novel Approach
The most common approach to engaging hospitalists in CDI initiatives is to have them attend a presentation on the topic, then put in place documentation specialists who generate queries asking the doctor to clarify diagnoses when it might influence payment, severity of illness determination, etc. Dr. Kenji Asakura, a Seattle hospitalist, and Erik Ordal, MBA, have a company called ClinIntell that analyzes each hospitalist (or other specialty) group’s historical patient mix and trains them on the documentation issues that they see most often. The idea of this focused approach is to make “documentation queries” unnecessary, or at least much less necessary. The benefits of this approach are many, including reducing or eliminating the risk of “leading queries”—that is, queries that seem to encourage the doctor to document a diagnosis because it is an advantage to the hospital rather than a well-considered medical opinion. Leading queries can be regarded as fraudulent and can get a lot of people in trouble.
I asked Kenji and Erik if they could provide me with a list of common documentation issues that most hospitalists need to know more about. Table 1 is what they came up with. I hope it helps you and your practice.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at john.nelson@nelsonflores.com.
Back in the 1980s, I would go by medical records every day or two and find, on the front of the charts of my recently discharged patients, a form listing the diagnoses the hospital was billing to Medicare. Before the hospital could submit a patient’s bill, the attending physician was required to review the form and, by signing it, indicate agreement.
The requirement for this signature by the physician went away a long time ago and in my memory is one of the very few examples of reducing a doctor’s paperwork.
For my first few months in practice, I regularly would seek out the people who completed the form and explain they had misunderstood the patient’s clinical situation. “The main issue was a urinary tract infection,” I would say, “but you listed diabetes as the principal diagnosis.”
I don’t ever remember them changing anything based on my feedback. Instead, they explained to me that, for billing purposes, it was legitimate to list diabetes as the principal diagnosis because it had the additional benefit of resulting in a higher payment to the hospital than having “urinary tract infection” listed first.
Such was my introduction to the world of documentation and coding for hospital billing purposes and how it can sometimes differ significantly from the way a doctor sees the clinical picture. Things have evolved a lot since then, but the way doctors document medical conditions still has a huge influence on hospital reimbursement.
Hospital CDI Programs
About 80% of hospitals have formal clinical documentation improvement (CDI) programs to help ensure all clinical conditions are captured and described in the medical record in ways that are valuable for billing and other recordkeeping purposes. These programs might lead to you receive queries about your documentation. For example, you might be asked to clarify whether your patient’s pneumonia might be on the basis of aspiration.
Within SHM’s Code-H program, Dr. Richard Pinson, a former ED physician who now works with Houston-based HCQ Consulting, has a good presentation explaining these documentation issues. In it, he makes the point that, in addition to influencing how hospitals are paid, the way various conditions are documented also influences quality ratings.
Novel Approach
The most common approach to engaging hospitalists in CDI initiatives is to have them attend a presentation on the topic, then put in place documentation specialists who generate queries asking the doctor to clarify diagnoses when it might influence payment, severity of illness determination, etc. Dr. Kenji Asakura, a Seattle hospitalist, and Erik Ordal, MBA, have a company called ClinIntell that analyzes each hospitalist (or other specialty) group’s historical patient mix and trains them on the documentation issues that they see most often. The idea of this focused approach is to make “documentation queries” unnecessary, or at least much less necessary. The benefits of this approach are many, including reducing or eliminating the risk of “leading queries”—that is, queries that seem to encourage the doctor to document a diagnosis because it is an advantage to the hospital rather than a well-considered medical opinion. Leading queries can be regarded as fraudulent and can get a lot of people in trouble.
I asked Kenji and Erik if they could provide me with a list of common documentation issues that most hospitalists need to know more about. Table 1 is what they came up with. I hope it helps you and your practice.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at john.nelson@nelsonflores.com.
Back in the 1980s, I would go by medical records every day or two and find, on the front of the charts of my recently discharged patients, a form listing the diagnoses the hospital was billing to Medicare. Before the hospital could submit a patient’s bill, the attending physician was required to review the form and, by signing it, indicate agreement.
The requirement for this signature by the physician went away a long time ago and in my memory is one of the very few examples of reducing a doctor’s paperwork.
For my first few months in practice, I regularly would seek out the people who completed the form and explain they had misunderstood the patient’s clinical situation. “The main issue was a urinary tract infection,” I would say, “but you listed diabetes as the principal diagnosis.”
I don’t ever remember them changing anything based on my feedback. Instead, they explained to me that, for billing purposes, it was legitimate to list diabetes as the principal diagnosis because it had the additional benefit of resulting in a higher payment to the hospital than having “urinary tract infection” listed first.
Such was my introduction to the world of documentation and coding for hospital billing purposes and how it can sometimes differ significantly from the way a doctor sees the clinical picture. Things have evolved a lot since then, but the way doctors document medical conditions still has a huge influence on hospital reimbursement.
Hospital CDI Programs
About 80% of hospitals have formal clinical documentation improvement (CDI) programs to help ensure all clinical conditions are captured and described in the medical record in ways that are valuable for billing and other recordkeeping purposes. These programs might lead to you receive queries about your documentation. For example, you might be asked to clarify whether your patient’s pneumonia might be on the basis of aspiration.
Within SHM’s Code-H program, Dr. Richard Pinson, a former ED physician who now works with Houston-based HCQ Consulting, has a good presentation explaining these documentation issues. In it, he makes the point that, in addition to influencing how hospitals are paid, the way various conditions are documented also influences quality ratings.
Novel Approach
The most common approach to engaging hospitalists in CDI initiatives is to have them attend a presentation on the topic, then put in place documentation specialists who generate queries asking the doctor to clarify diagnoses when it might influence payment, severity of illness determination, etc. Dr. Kenji Asakura, a Seattle hospitalist, and Erik Ordal, MBA, have a company called ClinIntell that analyzes each hospitalist (or other specialty) group’s historical patient mix and trains them on the documentation issues that they see most often. The idea of this focused approach is to make “documentation queries” unnecessary, or at least much less necessary. The benefits of this approach are many, including reducing or eliminating the risk of “leading queries”—that is, queries that seem to encourage the doctor to document a diagnosis because it is an advantage to the hospital rather than a well-considered medical opinion. Leading queries can be regarded as fraudulent and can get a lot of people in trouble.
I asked Kenji and Erik if they could provide me with a list of common documentation issues that most hospitalists need to know more about. Table 1 is what they came up with. I hope it helps you and your practice.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at john.nelson@nelsonflores.com.
'Systems,' Not 'Points,' Is Correct Terminology for ROS Statements
The “Billing and Coding Bandwagon” article in the May 2011 issue of The Hospitalist (p. 26) recently was brought to my attention and I have some concerns that the following statement gives a false impression of acceptable documentation: “When I first started working, I couldn’t believe that I could get audited and fined just because I didn’t add ‘10-point’ or ‘12-point’ to my note of ‘review of systems: negative,’” says hospitalist Amaka Nweke, MD, assistant director with Hospitalists Management Group (HMG) at Kenosha Medical Center in Kenosha, Wis. “I had a lot of frustration, because I had to repackage and re-present my notes in a manner that makes sense to Medicare but makes no sense to physicians.”
In fact, that would still not be considered acceptable documentation for services that require a complete review of systems (99222, 99223, 99219, 99220, 99235, and 99236). The documentation guidelines clearly state: “A complete ROS [review of systems] inquires about the system(s) directly related to the problem(s) identified in the HPI plus all additional body systems.” At least 10 organ systems must be reviewed. Those systems with positive or pertinent negative responses must be individually documented. For the remaining systems, a notation indicating all other systems are negative is permissible. In the absence of such a notation, at least 10 systems must be individually documented.
What Medicare is saying is the provider must have inquired about all 14 systems, not just 10 or 12. The term “point” means nothing in an ROS statement. “Systems” is the correct terminology, not “points.”
I am afraid the article is misleading and could be providing inappropriate documentation advice to hospitalists dealing with CMS and AMA guidelines.
The “Billing and Coding Bandwagon” article in the May 2011 issue of The Hospitalist (p. 26) recently was brought to my attention and I have some concerns that the following statement gives a false impression of acceptable documentation: “When I first started working, I couldn’t believe that I could get audited and fined just because I didn’t add ‘10-point’ or ‘12-point’ to my note of ‘review of systems: negative,’” says hospitalist Amaka Nweke, MD, assistant director with Hospitalists Management Group (HMG) at Kenosha Medical Center in Kenosha, Wis. “I had a lot of frustration, because I had to repackage and re-present my notes in a manner that makes sense to Medicare but makes no sense to physicians.”
In fact, that would still not be considered acceptable documentation for services that require a complete review of systems (99222, 99223, 99219, 99220, 99235, and 99236). The documentation guidelines clearly state: “A complete ROS [review of systems] inquires about the system(s) directly related to the problem(s) identified in the HPI plus all additional body systems.” At least 10 organ systems must be reviewed. Those systems with positive or pertinent negative responses must be individually documented. For the remaining systems, a notation indicating all other systems are negative is permissible. In the absence of such a notation, at least 10 systems must be individually documented.
What Medicare is saying is the provider must have inquired about all 14 systems, not just 10 or 12. The term “point” means nothing in an ROS statement. “Systems” is the correct terminology, not “points.”
I am afraid the article is misleading and could be providing inappropriate documentation advice to hospitalists dealing with CMS and AMA guidelines.
The “Billing and Coding Bandwagon” article in the May 2011 issue of The Hospitalist (p. 26) recently was brought to my attention and I have some concerns that the following statement gives a false impression of acceptable documentation: “When I first started working, I couldn’t believe that I could get audited and fined just because I didn’t add ‘10-point’ or ‘12-point’ to my note of ‘review of systems: negative,’” says hospitalist Amaka Nweke, MD, assistant director with Hospitalists Management Group (HMG) at Kenosha Medical Center in Kenosha, Wis. “I had a lot of frustration, because I had to repackage and re-present my notes in a manner that makes sense to Medicare but makes no sense to physicians.”
In fact, that would still not be considered acceptable documentation for services that require a complete review of systems (99222, 99223, 99219, 99220, 99235, and 99236). The documentation guidelines clearly state: “A complete ROS [review of systems] inquires about the system(s) directly related to the problem(s) identified in the HPI plus all additional body systems.” At least 10 organ systems must be reviewed. Those systems with positive or pertinent negative responses must be individually documented. For the remaining systems, a notation indicating all other systems are negative is permissible. In the absence of such a notation, at least 10 systems must be individually documented.
What Medicare is saying is the provider must have inquired about all 14 systems, not just 10 or 12. The term “point” means nothing in an ROS statement. “Systems” is the correct terminology, not “points.”
I am afraid the article is misleading and could be providing inappropriate documentation advice to hospitalists dealing with CMS and AMA guidelines.
Coordinated Approach May Help in Caring for Hospitals’ Neediest Patients
To my way of thinking, a person’s diagnosis or pathophysiology is not as strong a predictor of needing inpatient hospital care as it might have been 10 or 20 years ago. Rather than the clinical diagnosis (e.g. pneumonia), it seems to me that frailty or social complexity often are the principal determinants of which patients are admitted to a hospital for medical conditions.
Some of these patients are admitted frequently but appear to realize little or no benefit from hospitalization. These patients typically have little or no social support, and they often have either significant mental health disorders or substance abuse, or both. Much has been written about these patients, and I recommend an article by Dr. Atul Gawande in the Jan. 24, 2011, issue of The New Yorker titled “The Hot Spotters: Can We Lower Medical Costs by Giving the Neediest Patients Better Care?”
The Agency for Healthcare Research and Quality’s “Statistical Brief 354” on how health-care expenditures are allocated across the population reported that 1% of the population accounted for more than 22% of health-care spending in 2008. One in 5 of those were in that category again in 2009. Some of these patients would benefit from care plans.
The Role of Care Plans
It seems that there may be few effective inpatient interventions that will benefit these patients. After all, they have chronic issues that require ongoing relationships with outpatient providers, something that many of these patients lack. But for some (most?) of these patients, it seems clear that frequent hospitalizations don’t help and sometimes just perpetuate or worsen the patient’s dependence on the hospital at a high financial cost to society—and significant frustration and burnout on the part of hospital caregivers, including hospitalists.
For most hospitals, this problem is significant enough to require some sort of coordinated approach to the care of the dozens of types of patients in this category. Implementing whatever plan of care seems appropriate to the caregivers during each admission is frustrating, ensures lots of variation in care, and makes it easier for manipulative patients to abuse the hospital resources and personnel.
A better approach is to follow the same plan of care from one hospital visit to the next. You already knew that. But developing a care plan to follow during each ED visit and admission is time-consuming and often fraught with uncertainty about where boundaries should be set. So if you’re like me, you might just try to guide the patient to discharge this time and hope that whoever sees the patient on the next admission will take the initiative to develop the care plan. The result is that few such plans are developed.
Your Hospital Needs a Care Plan
Relying on individual doctors or nurses to take the initiative to develop care plans will almost always mean few plans are developed, they will vary in their effectiveness, and other providers may not be aware a plan exists. This was the case at the hospital where I practice until I heard Dr. Rick Hilger, MD, SFHM, a hospitalist at Regions Hospital in Minneapolis, present on this topic at HM12 in San Diego.
Dr. Hilger led a multidisciplinary team to develop care plans (they call them “restriction care plans”) and found that they dramatically reduced the rate of hospital admissions and ED visits for these patients. Hearing about this experience served as a kick in the pants for me, so I did much the same thing at “my” hospital. We have now developed plans for more than 20 patients and found that they visit our ED and are admitted less often. And, anecdotally at least, hospitalists and other hospital staff find that the care plans reduce, at least a little, the stress of caring for these patients.
Unanswered Questions
Although it seems clear that care plans reduce visits to the hospital that develops them, I suspect that some of these patients aren’t consuming any fewer health-care resources. They may just seek care from a different hospital.
My home state of Washington is working to develop individual patient care plans available to all hospitals in the state. A system called the Emergency Department Information Exchange (EDIE) has been adopted by nearly all the hospitals in the state. It allows them to share information on ED visits and such things as care plans with one another. For example, through EDIE, each hospital could see the opiate dosing schedule and admission criteria agreed to by patient and primary-care physician.
So it seems that care plans and the technology to share them can make it more difficult for patients to harm themselves by visiting many hospitals to get excessive opiate prescriptions, for example. This should benefit the patient and lower ED and hospital expenditures for these patients. But we don’t know what portion of costs simply is shifted to other settings, so there is no easy way to know the net effect on health-care costs.
An important unanswered question is whether these care plans improve patient well-being. It seems clear they do in some cases, but it is hard to know whether some patients may be worse off because of the plan.
Conclusion
I think nearly every hospital would benefit from a care plan committee composed of at least one hospitalist, ED physician, a nursing representative, and potentially other disciplines (see “Care Plan Attributes,” above). Our committee includes our inpatient psychiatrist, a really valuable contributor.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
To my way of thinking, a person’s diagnosis or pathophysiology is not as strong a predictor of needing inpatient hospital care as it might have been 10 or 20 years ago. Rather than the clinical diagnosis (e.g. pneumonia), it seems to me that frailty or social complexity often are the principal determinants of which patients are admitted to a hospital for medical conditions.
Some of these patients are admitted frequently but appear to realize little or no benefit from hospitalization. These patients typically have little or no social support, and they often have either significant mental health disorders or substance abuse, or both. Much has been written about these patients, and I recommend an article by Dr. Atul Gawande in the Jan. 24, 2011, issue of The New Yorker titled “The Hot Spotters: Can We Lower Medical Costs by Giving the Neediest Patients Better Care?”
The Agency for Healthcare Research and Quality’s “Statistical Brief 354” on how health-care expenditures are allocated across the population reported that 1% of the population accounted for more than 22% of health-care spending in 2008. One in 5 of those were in that category again in 2009. Some of these patients would benefit from care plans.
The Role of Care Plans
It seems that there may be few effective inpatient interventions that will benefit these patients. After all, they have chronic issues that require ongoing relationships with outpatient providers, something that many of these patients lack. But for some (most?) of these patients, it seems clear that frequent hospitalizations don’t help and sometimes just perpetuate or worsen the patient’s dependence on the hospital at a high financial cost to society—and significant frustration and burnout on the part of hospital caregivers, including hospitalists.
For most hospitals, this problem is significant enough to require some sort of coordinated approach to the care of the dozens of types of patients in this category. Implementing whatever plan of care seems appropriate to the caregivers during each admission is frustrating, ensures lots of variation in care, and makes it easier for manipulative patients to abuse the hospital resources and personnel.
A better approach is to follow the same plan of care from one hospital visit to the next. You already knew that. But developing a care plan to follow during each ED visit and admission is time-consuming and often fraught with uncertainty about where boundaries should be set. So if you’re like me, you might just try to guide the patient to discharge this time and hope that whoever sees the patient on the next admission will take the initiative to develop the care plan. The result is that few such plans are developed.
Your Hospital Needs a Care Plan
Relying on individual doctors or nurses to take the initiative to develop care plans will almost always mean few plans are developed, they will vary in their effectiveness, and other providers may not be aware a plan exists. This was the case at the hospital where I practice until I heard Dr. Rick Hilger, MD, SFHM, a hospitalist at Regions Hospital in Minneapolis, present on this topic at HM12 in San Diego.
Dr. Hilger led a multidisciplinary team to develop care plans (they call them “restriction care plans”) and found that they dramatically reduced the rate of hospital admissions and ED visits for these patients. Hearing about this experience served as a kick in the pants for me, so I did much the same thing at “my” hospital. We have now developed plans for more than 20 patients and found that they visit our ED and are admitted less often. And, anecdotally at least, hospitalists and other hospital staff find that the care plans reduce, at least a little, the stress of caring for these patients.
Unanswered Questions
Although it seems clear that care plans reduce visits to the hospital that develops them, I suspect that some of these patients aren’t consuming any fewer health-care resources. They may just seek care from a different hospital.
My home state of Washington is working to develop individual patient care plans available to all hospitals in the state. A system called the Emergency Department Information Exchange (EDIE) has been adopted by nearly all the hospitals in the state. It allows them to share information on ED visits and such things as care plans with one another. For example, through EDIE, each hospital could see the opiate dosing schedule and admission criteria agreed to by patient and primary-care physician.
So it seems that care plans and the technology to share them can make it more difficult for patients to harm themselves by visiting many hospitals to get excessive opiate prescriptions, for example. This should benefit the patient and lower ED and hospital expenditures for these patients. But we don’t know what portion of costs simply is shifted to other settings, so there is no easy way to know the net effect on health-care costs.
An important unanswered question is whether these care plans improve patient well-being. It seems clear they do in some cases, but it is hard to know whether some patients may be worse off because of the plan.
Conclusion
I think nearly every hospital would benefit from a care plan committee composed of at least one hospitalist, ED physician, a nursing representative, and potentially other disciplines (see “Care Plan Attributes,” above). Our committee includes our inpatient psychiatrist, a really valuable contributor.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
To my way of thinking, a person’s diagnosis or pathophysiology is not as strong a predictor of needing inpatient hospital care as it might have been 10 or 20 years ago. Rather than the clinical diagnosis (e.g. pneumonia), it seems to me that frailty or social complexity often are the principal determinants of which patients are admitted to a hospital for medical conditions.
Some of these patients are admitted frequently but appear to realize little or no benefit from hospitalization. These patients typically have little or no social support, and they often have either significant mental health disorders or substance abuse, or both. Much has been written about these patients, and I recommend an article by Dr. Atul Gawande in the Jan. 24, 2011, issue of The New Yorker titled “The Hot Spotters: Can We Lower Medical Costs by Giving the Neediest Patients Better Care?”
The Agency for Healthcare Research and Quality’s “Statistical Brief 354” on how health-care expenditures are allocated across the population reported that 1% of the population accounted for more than 22% of health-care spending in 2008. One in 5 of those were in that category again in 2009. Some of these patients would benefit from care plans.
The Role of Care Plans
It seems that there may be few effective inpatient interventions that will benefit these patients. After all, they have chronic issues that require ongoing relationships with outpatient providers, something that many of these patients lack. But for some (most?) of these patients, it seems clear that frequent hospitalizations don’t help and sometimes just perpetuate or worsen the patient’s dependence on the hospital at a high financial cost to society—and significant frustration and burnout on the part of hospital caregivers, including hospitalists.
For most hospitals, this problem is significant enough to require some sort of coordinated approach to the care of the dozens of types of patients in this category. Implementing whatever plan of care seems appropriate to the caregivers during each admission is frustrating, ensures lots of variation in care, and makes it easier for manipulative patients to abuse the hospital resources and personnel.
A better approach is to follow the same plan of care from one hospital visit to the next. You already knew that. But developing a care plan to follow during each ED visit and admission is time-consuming and often fraught with uncertainty about where boundaries should be set. So if you’re like me, you might just try to guide the patient to discharge this time and hope that whoever sees the patient on the next admission will take the initiative to develop the care plan. The result is that few such plans are developed.
Your Hospital Needs a Care Plan
Relying on individual doctors or nurses to take the initiative to develop care plans will almost always mean few plans are developed, they will vary in their effectiveness, and other providers may not be aware a plan exists. This was the case at the hospital where I practice until I heard Dr. Rick Hilger, MD, SFHM, a hospitalist at Regions Hospital in Minneapolis, present on this topic at HM12 in San Diego.
Dr. Hilger led a multidisciplinary team to develop care plans (they call them “restriction care plans”) and found that they dramatically reduced the rate of hospital admissions and ED visits for these patients. Hearing about this experience served as a kick in the pants for me, so I did much the same thing at “my” hospital. We have now developed plans for more than 20 patients and found that they visit our ED and are admitted less often. And, anecdotally at least, hospitalists and other hospital staff find that the care plans reduce, at least a little, the stress of caring for these patients.
Unanswered Questions
Although it seems clear that care plans reduce visits to the hospital that develops them, I suspect that some of these patients aren’t consuming any fewer health-care resources. They may just seek care from a different hospital.
My home state of Washington is working to develop individual patient care plans available to all hospitals in the state. A system called the Emergency Department Information Exchange (EDIE) has been adopted by nearly all the hospitals in the state. It allows them to share information on ED visits and such things as care plans with one another. For example, through EDIE, each hospital could see the opiate dosing schedule and admission criteria agreed to by patient and primary-care physician.
So it seems that care plans and the technology to share them can make it more difficult for patients to harm themselves by visiting many hospitals to get excessive opiate prescriptions, for example. This should benefit the patient and lower ED and hospital expenditures for these patients. But we don’t know what portion of costs simply is shifted to other settings, so there is no easy way to know the net effect on health-care costs.
An important unanswered question is whether these care plans improve patient well-being. It seems clear they do in some cases, but it is hard to know whether some patients may be worse off because of the plan.
Conclusion
I think nearly every hospital would benefit from a care plan committee composed of at least one hospitalist, ED physician, a nursing representative, and potentially other disciplines (see “Care Plan Attributes,” above). Our committee includes our inpatient psychiatrist, a really valuable contributor.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Documentation, CMS-Approved Language Key to Getting Paid for Hospitalist Teaching Services
When hospitalists work in academic centers, medical and surgical services are furnished, in part, by a resident within the scope of the hospitalists’ training program. A resident is “an individual who participates in an approved graduate medical education (GME) program or a physician who is not in an approved GME program but who is authorized to practice only in a hospital setting.”1 Resident services are covered by Centers for Medicare & Medicaid Services (CMS) and paid by the Fiscal Intermediary through direct GME and Indirect Medical Education (IME) payments. These services are not billed or paid using the Medicare Physician Fee Schedule. The teaching physician is responsible for supervising the resident’s health-care delivery but is not paid for the resident’s work. The teaching physician is paid for their personal and medically necessary service in providing patient care. The teaching physician has the option to perform the entire service, or perform the self-determined critical or key portion(s) of the service.
Comprehensive Service
Teaching physicians independently see the patient and perform all required elements to support the visit level (e.g. 99233: subsequent hospital care, per day, which requires at least two of the following three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making).2 The teaching physician writes a note independent of a resident encounter with the patient or documentation. The teaching physician note “stands alone” and does not rely on the resident’s documentation. If the resident saw the patient and documented the encounter, the teaching physician might choose to “link to” the resident note in lieu of personally documenting the entire service. The linking statement must demonstrate teaching physician involvement in the patient encounter and participation in patient management. Use of CMS-approved statements is best to meet these requirements. Statement examples include:3
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of these statements meets the minimum requirements for billing. However, teaching physicians should offer more information in support of other clinical, quality, and regulatory initiatives and mandates, better exemplified in the last example. The reported visit level will be supported by the combined documentation (teaching physician and resident).
The teaching physician submits a claim in their name and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99223-GC). This alerts the Medicare contractor that services were provided under teaching physician rules. Requests for documentation should include a response with medical record entries from the teaching physician and resident.
Critical/Key Portion
“Supervised” service: The resident and teaching physician can round together; they can see the patient at the same time. The teaching physician observes the resident’s performance during the patient encounter, or personally performs self-determined elements of patient care. The resident documents their patient care. The attending must still note their presence in the medical record, performance of the critical or key portions of the service, and involvement in patient management. CMS-accepted statements include:3
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Although these statements demonstrate acceptable billing language, they lack patient-specific details that support the teaching physician’s personal contribution to patient care and the quality of their expertise. The teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99232-GC).
“Shared” service: The resident sees the patient unaccompanied and documents the corresponding care provided. The teaching physician sees the patient at a different time but performs only the critical or key portions of the service. The case is subsequently discussed with the resident. The teaching physician must document their presence and performance of the critical or key portions of the service, along with any patient management. Using CMS-quoted statements ensures regulatory compliance:3
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Once again, the teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99233-GC).
EHR Considerations
When seeing patients independent of one another, the timing of the teaching physician and resident encounters does not impact billing. However, the time that the resident encounter is documented in the medical record can significantly impact the payment when reviewed by external auditors. When the resident note is dated and timed later than the teaching physician’s entry, the teaching physician cannot consider the resident’s note for visit-level selection. The teaching physician should not “link to” a resident note that is viewed as “not having been written” prior to the teaching physician note. This would not fulfill the requirements represented in the CMS-approved language “I reviewed the resident’s note and agree.”
Electronic health record (EHR) systems sometimes hinder compliance. If the resident completes the note but does not “finalize” or “close” the encounter until after the teaching physician documents their own note, it can falsely appear that the resident note did not exist at the time the teaching physician created their entry. Because an auditor can only view the finalized entries, the timing of each entry might be erroneously represented. Proper training and closing of encounters can diminish these issues.
Additionally, scribing the attestation is not permitted. Residents cannot document the teaching physician attestation on behalf of the physician under any circumstance. CMS rules require the teaching physician to document their presence, participation, and management of the patient. In an EHR, the teaching physician must document this entry under his/her own log-in and password, which is not to be shared with anyone.
Students
CMS defines student as “an individual who participates in an accredited educational program [e.g. a medical school] that is not an approved GME program.”1 A student is not regarded as a “physician in training,” and the service is not eligible for reimbursement consideration under the teaching physician rules.
Per CMS guidelines, students can document services in the medical record, but the teaching physician may only refer to the student’s systems review and past/family/social history entries. The teaching physician must verify and redocument the history of present illness. A student’s physical exam findings or medical decision-making are not suitable for tethering, and the teaching physician must personally perform and redocument the physical exam and medical decision-making. The visit level reflects only the teaching physician’s personally performed and documented service.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents. CMS website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed Jan. 8, 2013.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100. CMS website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2013.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2. CMS website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Jan. 8, 2013.
When hospitalists work in academic centers, medical and surgical services are furnished, in part, by a resident within the scope of the hospitalists’ training program. A resident is “an individual who participates in an approved graduate medical education (GME) program or a physician who is not in an approved GME program but who is authorized to practice only in a hospital setting.”1 Resident services are covered by Centers for Medicare & Medicaid Services (CMS) and paid by the Fiscal Intermediary through direct GME and Indirect Medical Education (IME) payments. These services are not billed or paid using the Medicare Physician Fee Schedule. The teaching physician is responsible for supervising the resident’s health-care delivery but is not paid for the resident’s work. The teaching physician is paid for their personal and medically necessary service in providing patient care. The teaching physician has the option to perform the entire service, or perform the self-determined critical or key portion(s) of the service.
Comprehensive Service
Teaching physicians independently see the patient and perform all required elements to support the visit level (e.g. 99233: subsequent hospital care, per day, which requires at least two of the following three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making).2 The teaching physician writes a note independent of a resident encounter with the patient or documentation. The teaching physician note “stands alone” and does not rely on the resident’s documentation. If the resident saw the patient and documented the encounter, the teaching physician might choose to “link to” the resident note in lieu of personally documenting the entire service. The linking statement must demonstrate teaching physician involvement in the patient encounter and participation in patient management. Use of CMS-approved statements is best to meet these requirements. Statement examples include:3
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of these statements meets the minimum requirements for billing. However, teaching physicians should offer more information in support of other clinical, quality, and regulatory initiatives and mandates, better exemplified in the last example. The reported visit level will be supported by the combined documentation (teaching physician and resident).
The teaching physician submits a claim in their name and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99223-GC). This alerts the Medicare contractor that services were provided under teaching physician rules. Requests for documentation should include a response with medical record entries from the teaching physician and resident.
Critical/Key Portion
“Supervised” service: The resident and teaching physician can round together; they can see the patient at the same time. The teaching physician observes the resident’s performance during the patient encounter, or personally performs self-determined elements of patient care. The resident documents their patient care. The attending must still note their presence in the medical record, performance of the critical or key portions of the service, and involvement in patient management. CMS-accepted statements include:3
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Although these statements demonstrate acceptable billing language, they lack patient-specific details that support the teaching physician’s personal contribution to patient care and the quality of their expertise. The teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99232-GC).
“Shared” service: The resident sees the patient unaccompanied and documents the corresponding care provided. The teaching physician sees the patient at a different time but performs only the critical or key portions of the service. The case is subsequently discussed with the resident. The teaching physician must document their presence and performance of the critical or key portions of the service, along with any patient management. Using CMS-quoted statements ensures regulatory compliance:3
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Once again, the teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99233-GC).
EHR Considerations
When seeing patients independent of one another, the timing of the teaching physician and resident encounters does not impact billing. However, the time that the resident encounter is documented in the medical record can significantly impact the payment when reviewed by external auditors. When the resident note is dated and timed later than the teaching physician’s entry, the teaching physician cannot consider the resident’s note for visit-level selection. The teaching physician should not “link to” a resident note that is viewed as “not having been written” prior to the teaching physician note. This would not fulfill the requirements represented in the CMS-approved language “I reviewed the resident’s note and agree.”
Electronic health record (EHR) systems sometimes hinder compliance. If the resident completes the note but does not “finalize” or “close” the encounter until after the teaching physician documents their own note, it can falsely appear that the resident note did not exist at the time the teaching physician created their entry. Because an auditor can only view the finalized entries, the timing of each entry might be erroneously represented. Proper training and closing of encounters can diminish these issues.
Additionally, scribing the attestation is not permitted. Residents cannot document the teaching physician attestation on behalf of the physician under any circumstance. CMS rules require the teaching physician to document their presence, participation, and management of the patient. In an EHR, the teaching physician must document this entry under his/her own log-in and password, which is not to be shared with anyone.
Students
CMS defines student as “an individual who participates in an accredited educational program [e.g. a medical school] that is not an approved GME program.”1 A student is not regarded as a “physician in training,” and the service is not eligible for reimbursement consideration under the teaching physician rules.
Per CMS guidelines, students can document services in the medical record, but the teaching physician may only refer to the student’s systems review and past/family/social history entries. The teaching physician must verify and redocument the history of present illness. A student’s physical exam findings or medical decision-making are not suitable for tethering, and the teaching physician must personally perform and redocument the physical exam and medical decision-making. The visit level reflects only the teaching physician’s personally performed and documented service.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents. CMS website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed Jan. 8, 2013.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100. CMS website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2013.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2. CMS website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Jan. 8, 2013.
When hospitalists work in academic centers, medical and surgical services are furnished, in part, by a resident within the scope of the hospitalists’ training program. A resident is “an individual who participates in an approved graduate medical education (GME) program or a physician who is not in an approved GME program but who is authorized to practice only in a hospital setting.”1 Resident services are covered by Centers for Medicare & Medicaid Services (CMS) and paid by the Fiscal Intermediary through direct GME and Indirect Medical Education (IME) payments. These services are not billed or paid using the Medicare Physician Fee Schedule. The teaching physician is responsible for supervising the resident’s health-care delivery but is not paid for the resident’s work. The teaching physician is paid for their personal and medically necessary service in providing patient care. The teaching physician has the option to perform the entire service, or perform the self-determined critical or key portion(s) of the service.
Comprehensive Service
Teaching physicians independently see the patient and perform all required elements to support the visit level (e.g. 99233: subsequent hospital care, per day, which requires at least two of the following three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making).2 The teaching physician writes a note independent of a resident encounter with the patient or documentation. The teaching physician note “stands alone” and does not rely on the resident’s documentation. If the resident saw the patient and documented the encounter, the teaching physician might choose to “link to” the resident note in lieu of personally documenting the entire service. The linking statement must demonstrate teaching physician involvement in the patient encounter and participation in patient management. Use of CMS-approved statements is best to meet these requirements. Statement examples include:3
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of these statements meets the minimum requirements for billing. However, teaching physicians should offer more information in support of other clinical, quality, and regulatory initiatives and mandates, better exemplified in the last example. The reported visit level will be supported by the combined documentation (teaching physician and resident).
The teaching physician submits a claim in their name and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99223-GC). This alerts the Medicare contractor that services were provided under teaching physician rules. Requests for documentation should include a response with medical record entries from the teaching physician and resident.
Critical/Key Portion
“Supervised” service: The resident and teaching physician can round together; they can see the patient at the same time. The teaching physician observes the resident’s performance during the patient encounter, or personally performs self-determined elements of patient care. The resident documents their patient care. The attending must still note their presence in the medical record, performance of the critical or key portions of the service, and involvement in patient management. CMS-accepted statements include:3
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Although these statements demonstrate acceptable billing language, they lack patient-specific details that support the teaching physician’s personal contribution to patient care and the quality of their expertise. The teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99232-GC).
“Shared” service: The resident sees the patient unaccompanied and documents the corresponding care provided. The teaching physician sees the patient at a different time but performs only the critical or key portions of the service. The case is subsequently discussed with the resident. The teaching physician must document their presence and performance of the critical or key portions of the service, along with any patient management. Using CMS-quoted statements ensures regulatory compliance:3
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Once again, the teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99233-GC).
EHR Considerations
When seeing patients independent of one another, the timing of the teaching physician and resident encounters does not impact billing. However, the time that the resident encounter is documented in the medical record can significantly impact the payment when reviewed by external auditors. When the resident note is dated and timed later than the teaching physician’s entry, the teaching physician cannot consider the resident’s note for visit-level selection. The teaching physician should not “link to” a resident note that is viewed as “not having been written” prior to the teaching physician note. This would not fulfill the requirements represented in the CMS-approved language “I reviewed the resident’s note and agree.”
Electronic health record (EHR) systems sometimes hinder compliance. If the resident completes the note but does not “finalize” or “close” the encounter until after the teaching physician documents their own note, it can falsely appear that the resident note did not exist at the time the teaching physician created their entry. Because an auditor can only view the finalized entries, the timing of each entry might be erroneously represented. Proper training and closing of encounters can diminish these issues.
Additionally, scribing the attestation is not permitted. Residents cannot document the teaching physician attestation on behalf of the physician under any circumstance. CMS rules require the teaching physician to document their presence, participation, and management of the patient. In an EHR, the teaching physician must document this entry under his/her own log-in and password, which is not to be shared with anyone.
Students
CMS defines student as “an individual who participates in an accredited educational program [e.g. a medical school] that is not an approved GME program.”1 A student is not regarded as a “physician in training,” and the service is not eligible for reimbursement consideration under the teaching physician rules.
Per CMS guidelines, students can document services in the medical record, but the teaching physician may only refer to the student’s systems review and past/family/social history entries. The teaching physician must verify and redocument the history of present illness. A student’s physical exam findings or medical decision-making are not suitable for tethering, and the teaching physician must personally perform and redocument the physical exam and medical decision-making. The visit level reflects only the teaching physician’s personally performed and documented service.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents. CMS website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed Jan. 8, 2013.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100. CMS website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2013.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2. CMS website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Jan. 8, 2013.
Bill Seeks to Enhance Patient Access to Post-Hospital Benefit
New national legislation proposed in March would change Medicare billing rules to allow patients to more easily access Medicare’s institutional skilled nursing care benefit following a hospital discharge. Currently, patients can get the benefit only after a qualifying three-day hospital stay. If they don’t qualify, they often have to pay out of pocket for the subsequent skilled nursing facility placement.
The Improving Access to Medicare Coverage Act, introduced by Reps. Joe Courtney (D-Conn.) and Tom Latham (R-Iowa) and Sen. Sherrod Brown (D-Ohio), would allow the time patients spend inside the hospital on “observation status” to count toward their required three-day hospital stay. It also would establish a 90-day appeal period for those who have been denied this benefit.
SHM is one of a dozen endorsing organizations, joining the American Medical Association, American Medical Directors Association, and AARP. For more information, check out this month’s “Policy Corner”.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
New national legislation proposed in March would change Medicare billing rules to allow patients to more easily access Medicare’s institutional skilled nursing care benefit following a hospital discharge. Currently, patients can get the benefit only after a qualifying three-day hospital stay. If they don’t qualify, they often have to pay out of pocket for the subsequent skilled nursing facility placement.
The Improving Access to Medicare Coverage Act, introduced by Reps. Joe Courtney (D-Conn.) and Tom Latham (R-Iowa) and Sen. Sherrod Brown (D-Ohio), would allow the time patients spend inside the hospital on “observation status” to count toward their required three-day hospital stay. It also would establish a 90-day appeal period for those who have been denied this benefit.
SHM is one of a dozen endorsing organizations, joining the American Medical Association, American Medical Directors Association, and AARP. For more information, check out this month’s “Policy Corner”.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
New national legislation proposed in March would change Medicare billing rules to allow patients to more easily access Medicare’s institutional skilled nursing care benefit following a hospital discharge. Currently, patients can get the benefit only after a qualifying three-day hospital stay. If they don’t qualify, they often have to pay out of pocket for the subsequent skilled nursing facility placement.
The Improving Access to Medicare Coverage Act, introduced by Reps. Joe Courtney (D-Conn.) and Tom Latham (R-Iowa) and Sen. Sherrod Brown (D-Ohio), would allow the time patients spend inside the hospital on “observation status” to count toward their required three-day hospital stay. It also would establish a 90-day appeal period for those who have been denied this benefit.
SHM is one of a dozen endorsing organizations, joining the American Medical Association, American Medical Directors Association, and AARP. For more information, check out this month’s “Policy Corner”.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
SHM Tallies Ratio of Hospital Respondents' Observation Admissions to Inpatient Admission Encounters
SHM added a new item to its 2012 State of Hospital Medicine report: the ratio of respondents’ observation admissions to inpatient admission encounters. This metric was added because observation encounters have been increasing, with financial effects on hospitals and patients. SHM survey respondents reported a 20% observation rate for both adult and pediatric practice groups (see Figure 1).
Under observation status, services that used to be billed as inpatient status (e.g. chest pain evaluation, treatment of asthma exacerbation) must be billed by the hospital at much lower outpatient rates. Some hospitals have responded to this financial pressure by creating observation units or making other operational adjustments. One recent analysis suggested that nationwide adoption of such efforts could save billions of dollars.1
Becoming lean enough to do short work in short time, though, does not address all of the observation-related issues facing hospitals. When the Centers for Medicare & Medicaid Services’ (CMS) Recovery Audit Contractors (RACs) determine retrospectively that an inpatient admission should have been an observation encounter, the hospital’s payment is not downgraded but forfeited.2 This development has prompted hospitals to preemptively opt for observation status for certain patients. Case managers and providers increasingly are spending time reviewing inpatient versus observation status throughout a patient’s stay. Many hospitals have turned to third-party contractors to help review observation status.
Observation status has financial implications for patients as well. In the past year, USA Today, The Wall Street Journal, and CNN Money all have reported on patients hit with unexpected out-of-pocket expenses related to observation care.3,4,5 A common theme: Medicare patient hospitalized with an acute fracture, managed nonoperatively but requiring rehabilitation prior to returning home. These patients found out too late that observation, a status they were often unaware of, did not qualify for CMS’ three-day inpatient requirement to cover rehabilitation costs. Some patients were charged exorbitant prices for noncovered “outpatient” services, such as providing their routine medications.
Advocacy groups have joined the fray on patients’ behalf, and legal challenges have ensued. AARP and others are educating patients about observation status—and their right to challenge it. The Center for Medicare Advocacy (www.kslaw.com/Library/publication/HH111411_Bagnall.pdf) has filed a lawsuit against the U.S. Department of Health and Human Services on behalf of patients hit with uncovered rehabilitation costs, and the American Hospital Association has teamed with several hospitals to sue over funds forfeited in RAC audits (www.aha.org/content/12/121101-aha-hhs-medicare-com.pdf). Both houses of Congress have legislation (H.R. 1543 and S. 818) seeking to count observation days toward the Medicare three-day rule. For its part, CMS has promised to review observation status and, hopefully, clarify the rules.
Hospitalists, meanwhile, are gearing up for more observation care. The 2012 State of Hospital Medicine report shows that 37% of adult groups and 28% of pediatric groups reported having primary responsibility for observation or short-stay units. My own hospital runs both a clinical decision unit in the ED and a short-stay unit staffed by our hospitalist group. As SHM tracks observation status in future surveys, HM groups will be able to follow this phenomenon among their colleagues and benchmark their own rates of observation encounters.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
References
- Feng Z, Wright DB, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251-1259.
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323.
- Gengler A. The painful new trend in Medicare. CNN Money website. Available at: http://money.cnn.com/2012/08/07/pf/medicare-rehab-costs.moneymag/index.htm. Accessed March 6, 2013.
- Jaffe S. Patients held for observation can face steep drug bills. USA Today website. Available at: http://usatoday30.usatoday.com/money/industries/health/drugs/story/2012-04-30/drugs-can-be-expensive-in-observation-care/54646378/1. Accessed March 6, 2013.
- Landro L. Filling a gap between ERs and inpatient rooms. The Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052970204349404578101060863887052.html. Accessed March 6, 2013.
SHM added a new item to its 2012 State of Hospital Medicine report: the ratio of respondents’ observation admissions to inpatient admission encounters. This metric was added because observation encounters have been increasing, with financial effects on hospitals and patients. SHM survey respondents reported a 20% observation rate for both adult and pediatric practice groups (see Figure 1).
Under observation status, services that used to be billed as inpatient status (e.g. chest pain evaluation, treatment of asthma exacerbation) must be billed by the hospital at much lower outpatient rates. Some hospitals have responded to this financial pressure by creating observation units or making other operational adjustments. One recent analysis suggested that nationwide adoption of such efforts could save billions of dollars.1
Becoming lean enough to do short work in short time, though, does not address all of the observation-related issues facing hospitals. When the Centers for Medicare & Medicaid Services’ (CMS) Recovery Audit Contractors (RACs) determine retrospectively that an inpatient admission should have been an observation encounter, the hospital’s payment is not downgraded but forfeited.2 This development has prompted hospitals to preemptively opt for observation status for certain patients. Case managers and providers increasingly are spending time reviewing inpatient versus observation status throughout a patient’s stay. Many hospitals have turned to third-party contractors to help review observation status.
Observation status has financial implications for patients as well. In the past year, USA Today, The Wall Street Journal, and CNN Money all have reported on patients hit with unexpected out-of-pocket expenses related to observation care.3,4,5 A common theme: Medicare patient hospitalized with an acute fracture, managed nonoperatively but requiring rehabilitation prior to returning home. These patients found out too late that observation, a status they were often unaware of, did not qualify for CMS’ three-day inpatient requirement to cover rehabilitation costs. Some patients were charged exorbitant prices for noncovered “outpatient” services, such as providing their routine medications.
Advocacy groups have joined the fray on patients’ behalf, and legal challenges have ensued. AARP and others are educating patients about observation status—and their right to challenge it. The Center for Medicare Advocacy (www.kslaw.com/Library/publication/HH111411_Bagnall.pdf) has filed a lawsuit against the U.S. Department of Health and Human Services on behalf of patients hit with uncovered rehabilitation costs, and the American Hospital Association has teamed with several hospitals to sue over funds forfeited in RAC audits (www.aha.org/content/12/121101-aha-hhs-medicare-com.pdf). Both houses of Congress have legislation (H.R. 1543 and S. 818) seeking to count observation days toward the Medicare three-day rule. For its part, CMS has promised to review observation status and, hopefully, clarify the rules.
Hospitalists, meanwhile, are gearing up for more observation care. The 2012 State of Hospital Medicine report shows that 37% of adult groups and 28% of pediatric groups reported having primary responsibility for observation or short-stay units. My own hospital runs both a clinical decision unit in the ED and a short-stay unit staffed by our hospitalist group. As SHM tracks observation status in future surveys, HM groups will be able to follow this phenomenon among their colleagues and benchmark their own rates of observation encounters.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
References
- Feng Z, Wright DB, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251-1259.
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323.
- Gengler A. The painful new trend in Medicare. CNN Money website. Available at: http://money.cnn.com/2012/08/07/pf/medicare-rehab-costs.moneymag/index.htm. Accessed March 6, 2013.
- Jaffe S. Patients held for observation can face steep drug bills. USA Today website. Available at: http://usatoday30.usatoday.com/money/industries/health/drugs/story/2012-04-30/drugs-can-be-expensive-in-observation-care/54646378/1. Accessed March 6, 2013.
- Landro L. Filling a gap between ERs and inpatient rooms. The Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052970204349404578101060863887052.html. Accessed March 6, 2013.
SHM added a new item to its 2012 State of Hospital Medicine report: the ratio of respondents’ observation admissions to inpatient admission encounters. This metric was added because observation encounters have been increasing, with financial effects on hospitals and patients. SHM survey respondents reported a 20% observation rate for both adult and pediatric practice groups (see Figure 1).
Under observation status, services that used to be billed as inpatient status (e.g. chest pain evaluation, treatment of asthma exacerbation) must be billed by the hospital at much lower outpatient rates. Some hospitals have responded to this financial pressure by creating observation units or making other operational adjustments. One recent analysis suggested that nationwide adoption of such efforts could save billions of dollars.1
Becoming lean enough to do short work in short time, though, does not address all of the observation-related issues facing hospitals. When the Centers for Medicare & Medicaid Services’ (CMS) Recovery Audit Contractors (RACs) determine retrospectively that an inpatient admission should have been an observation encounter, the hospital’s payment is not downgraded but forfeited.2 This development has prompted hospitals to preemptively opt for observation status for certain patients. Case managers and providers increasingly are spending time reviewing inpatient versus observation status throughout a patient’s stay. Many hospitals have turned to third-party contractors to help review observation status.
Observation status has financial implications for patients as well. In the past year, USA Today, The Wall Street Journal, and CNN Money all have reported on patients hit with unexpected out-of-pocket expenses related to observation care.3,4,5 A common theme: Medicare patient hospitalized with an acute fracture, managed nonoperatively but requiring rehabilitation prior to returning home. These patients found out too late that observation, a status they were often unaware of, did not qualify for CMS’ three-day inpatient requirement to cover rehabilitation costs. Some patients were charged exorbitant prices for noncovered “outpatient” services, such as providing their routine medications.
Advocacy groups have joined the fray on patients’ behalf, and legal challenges have ensued. AARP and others are educating patients about observation status—and their right to challenge it. The Center for Medicare Advocacy (www.kslaw.com/Library/publication/HH111411_Bagnall.pdf) has filed a lawsuit against the U.S. Department of Health and Human Services on behalf of patients hit with uncovered rehabilitation costs, and the American Hospital Association has teamed with several hospitals to sue over funds forfeited in RAC audits (www.aha.org/content/12/121101-aha-hhs-medicare-com.pdf). Both houses of Congress have legislation (H.R. 1543 and S. 818) seeking to count observation days toward the Medicare three-day rule. For its part, CMS has promised to review observation status and, hopefully, clarify the rules.
Hospitalists, meanwhile, are gearing up for more observation care. The 2012 State of Hospital Medicine report shows that 37% of adult groups and 28% of pediatric groups reported having primary responsibility for observation or short-stay units. My own hospital runs both a clinical decision unit in the ED and a short-stay unit staffed by our hospitalist group. As SHM tracks observation status in future surveys, HM groups will be able to follow this phenomenon among their colleagues and benchmark their own rates of observation encounters.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
References
- Feng Z, Wright DB, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251-1259.
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323.
- Gengler A. The painful new trend in Medicare. CNN Money website. Available at: http://money.cnn.com/2012/08/07/pf/medicare-rehab-costs.moneymag/index.htm. Accessed March 6, 2013.
- Jaffe S. Patients held for observation can face steep drug bills. USA Today website. Available at: http://usatoday30.usatoday.com/money/industries/health/drugs/story/2012-04-30/drugs-can-be-expensive-in-observation-care/54646378/1. Accessed March 6, 2013.
- Landro L. Filling a gap between ERs and inpatient rooms. The Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052970204349404578101060863887052.html. Accessed March 6, 2013.
Affordable Care Act (ACA) Provision Carries Pay Raise for Some Hospitalists
For those who remain unaware, hospitalists who care for Medicaid patients will be getting a raise in 2013 and 2014. The reason is that the Affordable Care Act (ACA) requires Medicaid rates for specified primary-care services to be equal to those of Medicare rates during those two years, with the federal government paying the difference. Hospitalists generally meet the requirements and, therefore, will see this pay increase for their applicable Medicaid billing. For some context of the scope of this change, on average, Medicaid pays physicians at 66% of the national Medicare rates, although there is significant variation among the states.
To qualify, a physician must have a specialty designation of family medicine, internal medicine, or pediatrics, then further attest to board certification in one of those specialties or related subspecialties. Alternatively, the physician must have a 60% claims history for the specified evaluation and management (E&M) codes.
Multiple parties who have heard reports about state plans for Medicaid parity recently have contacted SHM; the plans, they report, intentionally would exclude hospitalists from the promised increase. There are variations on the explanation for the exclusion and where the idea is coming from, but the inquiries follow this general theme: “Since the definition of eligible physicians remains a grey area, states are developing alternative plans with a more narrow interpretation of the qualifying factors for the increase. These plans are only including physicians who practice in the community setting (i.e. not the hospital setting).”
This is demonstrably wrong. Even if states are having these discussions, such a plan is not going to come to fruition. The final rule for Medicaid parity, which essentially has the effect of law, is very clear: It does not allow for differing eligibility or alternate state plans.
The Centers for Medicare & Medicaid Services (CMS) specifically stated in the final rule that the increase is not limited to office-based primary-care services, but it will also include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services. In other words, a hospitalist who attests eligibility for their respective state Medicaid agency and bills 99231-3, 99221-3, 99238-9, etc., will receive the increased payment for these codes.
In response to an SHM inquiry for further clarification, CMS officials have stated, “The regulation requires that qualified physicians billing eligible codes receive higher payment. States do not have the latitude to exclude physicians simply because they practice in hospitals.”
It is possible that some confusion might be arising due to the recent controversies around the upcoming Medicaid expansion, which would extend Medicaid eligibility to individuals who earn up to 138% of the federal poverty line. Some states have chosen to opt out of this expansion and have publicly fought its implementation. The Medicaid parity provision is parallel to, but independent of, Medicaid expansion. Even if a state opts out of the expansion, the Medicaid payment increase for primary-care services should remain unaffected.
This isn’t to say that the Medicaid parity provision is a certainty. With the eyes of Congress turned toward budget cuts and austerity, the funds allocated for this temporary increase could easily be targeted. Regardless, any change in eligibility would require a rule change at the federal level, which is unlikely.
Many states have already devoted much time and effort on plans to implement the provision, and the plans were due to be submitted to CMS on March 31. It is pretty late in the game to consider changes. Barring an unlikely rule change or total elimination of funding, it is clear that hospitalists are eligible for the payment bump and should remain so.
Josh Boswell is SHM’s senior manager of government relations.
For those who remain unaware, hospitalists who care for Medicaid patients will be getting a raise in 2013 and 2014. The reason is that the Affordable Care Act (ACA) requires Medicaid rates for specified primary-care services to be equal to those of Medicare rates during those two years, with the federal government paying the difference. Hospitalists generally meet the requirements and, therefore, will see this pay increase for their applicable Medicaid billing. For some context of the scope of this change, on average, Medicaid pays physicians at 66% of the national Medicare rates, although there is significant variation among the states.
To qualify, a physician must have a specialty designation of family medicine, internal medicine, or pediatrics, then further attest to board certification in one of those specialties or related subspecialties. Alternatively, the physician must have a 60% claims history for the specified evaluation and management (E&M) codes.
Multiple parties who have heard reports about state plans for Medicaid parity recently have contacted SHM; the plans, they report, intentionally would exclude hospitalists from the promised increase. There are variations on the explanation for the exclusion and where the idea is coming from, but the inquiries follow this general theme: “Since the definition of eligible physicians remains a grey area, states are developing alternative plans with a more narrow interpretation of the qualifying factors for the increase. These plans are only including physicians who practice in the community setting (i.e. not the hospital setting).”
This is demonstrably wrong. Even if states are having these discussions, such a plan is not going to come to fruition. The final rule for Medicaid parity, which essentially has the effect of law, is very clear: It does not allow for differing eligibility or alternate state plans.
The Centers for Medicare & Medicaid Services (CMS) specifically stated in the final rule that the increase is not limited to office-based primary-care services, but it will also include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services. In other words, a hospitalist who attests eligibility for their respective state Medicaid agency and bills 99231-3, 99221-3, 99238-9, etc., will receive the increased payment for these codes.
In response to an SHM inquiry for further clarification, CMS officials have stated, “The regulation requires that qualified physicians billing eligible codes receive higher payment. States do not have the latitude to exclude physicians simply because they practice in hospitals.”
It is possible that some confusion might be arising due to the recent controversies around the upcoming Medicaid expansion, which would extend Medicaid eligibility to individuals who earn up to 138% of the federal poverty line. Some states have chosen to opt out of this expansion and have publicly fought its implementation. The Medicaid parity provision is parallel to, but independent of, Medicaid expansion. Even if a state opts out of the expansion, the Medicaid payment increase for primary-care services should remain unaffected.
This isn’t to say that the Medicaid parity provision is a certainty. With the eyes of Congress turned toward budget cuts and austerity, the funds allocated for this temporary increase could easily be targeted. Regardless, any change in eligibility would require a rule change at the federal level, which is unlikely.
Many states have already devoted much time and effort on plans to implement the provision, and the plans were due to be submitted to CMS on March 31. It is pretty late in the game to consider changes. Barring an unlikely rule change or total elimination of funding, it is clear that hospitalists are eligible for the payment bump and should remain so.
Josh Boswell is SHM’s senior manager of government relations.
For those who remain unaware, hospitalists who care for Medicaid patients will be getting a raise in 2013 and 2014. The reason is that the Affordable Care Act (ACA) requires Medicaid rates for specified primary-care services to be equal to those of Medicare rates during those two years, with the federal government paying the difference. Hospitalists generally meet the requirements and, therefore, will see this pay increase for their applicable Medicaid billing. For some context of the scope of this change, on average, Medicaid pays physicians at 66% of the national Medicare rates, although there is significant variation among the states.
To qualify, a physician must have a specialty designation of family medicine, internal medicine, or pediatrics, then further attest to board certification in one of those specialties or related subspecialties. Alternatively, the physician must have a 60% claims history for the specified evaluation and management (E&M) codes.
Multiple parties who have heard reports about state plans for Medicaid parity recently have contacted SHM; the plans, they report, intentionally would exclude hospitalists from the promised increase. There are variations on the explanation for the exclusion and where the idea is coming from, but the inquiries follow this general theme: “Since the definition of eligible physicians remains a grey area, states are developing alternative plans with a more narrow interpretation of the qualifying factors for the increase. These plans are only including physicians who practice in the community setting (i.e. not the hospital setting).”
This is demonstrably wrong. Even if states are having these discussions, such a plan is not going to come to fruition. The final rule for Medicaid parity, which essentially has the effect of law, is very clear: It does not allow for differing eligibility or alternate state plans.
The Centers for Medicare & Medicaid Services (CMS) specifically stated in the final rule that the increase is not limited to office-based primary-care services, but it will also include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services. In other words, a hospitalist who attests eligibility for their respective state Medicaid agency and bills 99231-3, 99221-3, 99238-9, etc., will receive the increased payment for these codes.
In response to an SHM inquiry for further clarification, CMS officials have stated, “The regulation requires that qualified physicians billing eligible codes receive higher payment. States do not have the latitude to exclude physicians simply because they practice in hospitals.”
It is possible that some confusion might be arising due to the recent controversies around the upcoming Medicaid expansion, which would extend Medicaid eligibility to individuals who earn up to 138% of the federal poverty line. Some states have chosen to opt out of this expansion and have publicly fought its implementation. The Medicaid parity provision is parallel to, but independent of, Medicaid expansion. Even if a state opts out of the expansion, the Medicaid payment increase for primary-care services should remain unaffected.
This isn’t to say that the Medicaid parity provision is a certainty. With the eyes of Congress turned toward budget cuts and austerity, the funds allocated for this temporary increase could easily be targeted. Regardless, any change in eligibility would require a rule change at the federal level, which is unlikely.
Many states have already devoted much time and effort on plans to implement the provision, and the plans were due to be submitted to CMS on March 31. It is pretty late in the game to consider changes. Barring an unlikely rule change or total elimination of funding, it is clear that hospitalists are eligible for the payment bump and should remain so.
Josh Boswell is SHM’s senior manager of government relations.