User login
Monitoring Acne Patients on Oral Therapy: Survey of the Editorial Board
To improve patient care and outcomes, leading dermatologists from the Cutis and Dermatology News Editorial Boards answered 5 questions on monitoring acne patients on oral therapy. Here’s what we found.
Do you check potassium levels for patients taking spironolactone for acne?
Half of dermatologists surveyed never check potassium levels for patients taking spironolactone for acne. For those who do check levels, 8% do it at baseline only, 8% at baseline and every 6 months, 23% at baseline and yearly, and 13% at baseline and for dosing changes.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Although some dermatologists are still checking for potassium levels in patients taking spironolactone for acne, there is a clear trend toward foregoing laboratory monitoring. This change was likely spurred by a retrospective study of healthy young women taking spironolactone for acne that found a hyperkalemia rate of 0.72%, which is practically equivalent to the 0.76% baseline rate of hyperkalemia in this age group. Furthermore, since repeat testing in 6 of 13 patients showed normal values, the original potassium measurements may have been erroneous. Based on this study, routine potassium monitoring is likely unnecessary for healthy young women taking spironolactone for acne (Plovanich et al). In another retrospective study of women aged 18 to 65 years taking spironolactone for acne, women aged 46 to 65 years had a significantly higher rate of hyperkalemia with spironolactone compared with women aged 18 to 45 years (2/12 women [16.7%] vs 1/112 women [<1%]; P=.0245). Based on this study, potassium monitoring may be indicated for women older than 45 years taking spironolactone for acne (Thiede et al).
Next page: Cholesterol levels
Do you monitor cholesterol levels in patients taking isotretinoin?
Almost two-thirds of dermatologists indicated that they monitor all cholesterol levels in patients taking isotretinoin, including low-density lipoprotein, high-density lipoprotein, very low-density lipoprotein, and triglycerides, but almost one-third monitor triglycerides only. Five percent do not monitor cholesterol levels.
Do you routinely monitor cholesterol levels in patients taking isotretinoin?
More than 80% of dermatologists surveyed routinely monitor cholesterol levels in patients taking isotretinoin, with almost half (45%) at baseline and every 2 to 3 months. Eight percent check levels at baseline only, 28% at baseline and monthly, and 3% at baseline and end of therapy. Eighteen percent indicated they do not routinely monitor cholesterol levels.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
In this survey, dermatologists most often check cholesterol levels at baseline and then every 2 to 3 months, with most monitoring all cholesterol types. Elevations in cholesterol are by far the most common laboratory abnormality seen with isotretinoin therapy. In a retrospective study of 515 patients undergoing isotretinoin treatment of acne, mild to moderate triglyceride elevations were seen in 23.5% of patients (Hansen et al). At least in part, these elevations are likely due to the fact the levels were not drawn during fasting. Keep in mind that triglyceride-induced pancreatitis due to isotretinoin is remarkably rare, so monthly screening for triglycerides is likely not warranted. It is reasonable to monitor triglyceride levels during isotretinoin dose adjustments and for patients whose values are trending upward.
Next page: Monitoring CBC
Do you routinely monitor complete blood cell count (CBC) in patients taking isotretinoin?
More than half (55%) of dermatologists surveyed routinely monitor complete blood cell (CBC) counts in patients taking isotretinoin, while 45% do not. Of those who do monitor CBC, 13% do so at baseline only, 26% at baseline and monthly, 13% at baseline only and every 2 to 3 months, and only 3% at baseline and end of therapy.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Slightly more than half of dermatologists in this survey are obtaining CBC for their patients taking isotretinoin for acne and many of those are performing the test at baseline and monthly. Multiple studies as well as American Academy of Dermatology guidelines have substantiated that routine CBC monitoring is unwarranted in healthy patients, as abnormal values usually resolve or remain stable with therapy (American Academy of Dermatology, Isotretinoin: Recommendations). Therefore, it is worthwhile to consider foregoing CBC testing or obtaining just a baseline CBC in healthy patients being treated with isotretinoin.
Next page: Pregnancy testing
Which pregnancy test do you perform on female patients taking isotretinoin?
More than 40% of dermatologists surveyed use the urine β-human chorionic gonadotropin (hCG) pregnancy test for female patients taking isotretinoin, while 30% use the serum B-hCG test; 28% indicated that they use both tests.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
The iPLEDGE program was implemented in 2006 to avoid fetal exposure to isotretinoin and requires pregnancy testing (urine or serum) for females of childbearing potential taking isotretinoin. In a study of pregnancy-related adverse events associated with isotretinoin reported to the US Food and Drug Administration, 6740 total pregnancies were reported from 1997 to 2017. The rate peaked with 768 pregnancies in 2006 and then decreased. Because several hundred pregnancies in women taking isotretinoin have been reported yearly in the last 10 years, there is a clear need to have better systems in place and patient education to prevent fetal exposure to isotretinoin.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
I see lab monitoring as an opportunity to engage patients and families in co-directing their care (ie, practice patient- and family-centered care). Some families and patients like frequent monitoring and some want as few blood draws as possible. I do my best to make sure the decision includes components of the patients’ preferences, medical evidence and my best clinical judgement.—Craig Burkhart, MD, MS, MPH (Chapel Hill, North Caroline)
Being familiar with and following the standard of care guidelines for the individual oral therapies used in the treatment of acne is very important. However, it is equally as important to assure the individual patient (medical history, physical examination, social history, etc) is taken into consideration to determine if additional monitoring is required.—Fran E. Cook-Bolden, MD (New York, New York)
The trend seems to be towards less routine monitoring other than pregnancy. Baseline tests may pick out the occasional patient with comorbidities that would preclude or delay treatment, but the majority of patients may not need the repetitive and costly testing that we have done in the past.—Richard Glogau, MD (San Francisco, California)
I have loosened my lab monitoring with isotretinoin over the past few years. If a patient has normal lipid values, comprehensive panel and complete blood cell count for the first 3 months of tests, I skip labs until the end of therapy.—Lawrence J. Green, MD (Washington, DC)
Interestingly, we focus quite a bit of attention on the risk of pregnancy with isotretinoin, and often don't focus enough on the risk with spironolactone. In our practice, we are careful to warn the patients on spironolactone about pregnancy prevention.—Stephen Stone, MD (Springfield, Illinois)
About This Survey
The survey was fielded electronically to Cutis and Dermatology News Editorial Board Members within the United States from May 5, 2019, to June 23, 2019. A total of 40 usable responses were received.
American Academy of Dermatology. Isotretinoin: recommendations. https://www.aad.org/practicecenter/quality/clinical-guidelines/acne/isotretinoin. Accessed August 20, 2019.
Hansen TJ, Lucking S, Miller JJ, et al. Standardized laboratory monitoring with use of isotretinoin in acne. J Am Acad Dermatol. 2016;75:323-328.
Plovanich M, Weng QY, Mostaghimi A. Low usefulness of potassium monitoring among healthy young women taking spironolactone for acne. JAMA Dermatol. 2015;151:941-944.
Thiede RM, Rastogi S, Nardone B, et al. Hyperkalemia in women with acne exposed to oral spironolactone: a retrospective study from the RADAR (Research on Adverse Drug Events and Reports) program. Int J Womens Dermatol. 2019;5:155-157.
Tkachenko E, Singer S, Sharma P, et al. US Food and Drug Administration reports of pregnancy and pregnancy-related adverse events associated with isotretinoin [published online July 17, 2019]. JAMA Dermatol. doi:10.1001/jamadermatol.2019.1388.
To improve patient care and outcomes, leading dermatologists from the Cutis and Dermatology News Editorial Boards answered 5 questions on monitoring acne patients on oral therapy. Here’s what we found.
Do you check potassium levels for patients taking spironolactone for acne?
Half of dermatologists surveyed never check potassium levels for patients taking spironolactone for acne. For those who do check levels, 8% do it at baseline only, 8% at baseline and every 6 months, 23% at baseline and yearly, and 13% at baseline and for dosing changes.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Although some dermatologists are still checking for potassium levels in patients taking spironolactone for acne, there is a clear trend toward foregoing laboratory monitoring. This change was likely spurred by a retrospective study of healthy young women taking spironolactone for acne that found a hyperkalemia rate of 0.72%, which is practically equivalent to the 0.76% baseline rate of hyperkalemia in this age group. Furthermore, since repeat testing in 6 of 13 patients showed normal values, the original potassium measurements may have been erroneous. Based on this study, routine potassium monitoring is likely unnecessary for healthy young women taking spironolactone for acne (Plovanich et al). In another retrospective study of women aged 18 to 65 years taking spironolactone for acne, women aged 46 to 65 years had a significantly higher rate of hyperkalemia with spironolactone compared with women aged 18 to 45 years (2/12 women [16.7%] vs 1/112 women [<1%]; P=.0245). Based on this study, potassium monitoring may be indicated for women older than 45 years taking spironolactone for acne (Thiede et al).
Next page: Cholesterol levels
Do you monitor cholesterol levels in patients taking isotretinoin?
Almost two-thirds of dermatologists indicated that they monitor all cholesterol levels in patients taking isotretinoin, including low-density lipoprotein, high-density lipoprotein, very low-density lipoprotein, and triglycerides, but almost one-third monitor triglycerides only. Five percent do not monitor cholesterol levels.
Do you routinely monitor cholesterol levels in patients taking isotretinoin?
More than 80% of dermatologists surveyed routinely monitor cholesterol levels in patients taking isotretinoin, with almost half (45%) at baseline and every 2 to 3 months. Eight percent check levels at baseline only, 28% at baseline and monthly, and 3% at baseline and end of therapy. Eighteen percent indicated they do not routinely monitor cholesterol levels.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
In this survey, dermatologists most often check cholesterol levels at baseline and then every 2 to 3 months, with most monitoring all cholesterol types. Elevations in cholesterol are by far the most common laboratory abnormality seen with isotretinoin therapy. In a retrospective study of 515 patients undergoing isotretinoin treatment of acne, mild to moderate triglyceride elevations were seen in 23.5% of patients (Hansen et al). At least in part, these elevations are likely due to the fact the levels were not drawn during fasting. Keep in mind that triglyceride-induced pancreatitis due to isotretinoin is remarkably rare, so monthly screening for triglycerides is likely not warranted. It is reasonable to monitor triglyceride levels during isotretinoin dose adjustments and for patients whose values are trending upward.
Next page: Monitoring CBC
Do you routinely monitor complete blood cell count (CBC) in patients taking isotretinoin?
More than half (55%) of dermatologists surveyed routinely monitor complete blood cell (CBC) counts in patients taking isotretinoin, while 45% do not. Of those who do monitor CBC, 13% do so at baseline only, 26% at baseline and monthly, 13% at baseline only and every 2 to 3 months, and only 3% at baseline and end of therapy.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Slightly more than half of dermatologists in this survey are obtaining CBC for their patients taking isotretinoin for acne and many of those are performing the test at baseline and monthly. Multiple studies as well as American Academy of Dermatology guidelines have substantiated that routine CBC monitoring is unwarranted in healthy patients, as abnormal values usually resolve or remain stable with therapy (American Academy of Dermatology, Isotretinoin: Recommendations). Therefore, it is worthwhile to consider foregoing CBC testing or obtaining just a baseline CBC in healthy patients being treated with isotretinoin.
Next page: Pregnancy testing
Which pregnancy test do you perform on female patients taking isotretinoin?
More than 40% of dermatologists surveyed use the urine β-human chorionic gonadotropin (hCG) pregnancy test for female patients taking isotretinoin, while 30% use the serum B-hCG test; 28% indicated that they use both tests.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
The iPLEDGE program was implemented in 2006 to avoid fetal exposure to isotretinoin and requires pregnancy testing (urine or serum) for females of childbearing potential taking isotretinoin. In a study of pregnancy-related adverse events associated with isotretinoin reported to the US Food and Drug Administration, 6740 total pregnancies were reported from 1997 to 2017. The rate peaked with 768 pregnancies in 2006 and then decreased. Because several hundred pregnancies in women taking isotretinoin have been reported yearly in the last 10 years, there is a clear need to have better systems in place and patient education to prevent fetal exposure to isotretinoin.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
I see lab monitoring as an opportunity to engage patients and families in co-directing their care (ie, practice patient- and family-centered care). Some families and patients like frequent monitoring and some want as few blood draws as possible. I do my best to make sure the decision includes components of the patients’ preferences, medical evidence and my best clinical judgement.—Craig Burkhart, MD, MS, MPH (Chapel Hill, North Caroline)
Being familiar with and following the standard of care guidelines for the individual oral therapies used in the treatment of acne is very important. However, it is equally as important to assure the individual patient (medical history, physical examination, social history, etc) is taken into consideration to determine if additional monitoring is required.—Fran E. Cook-Bolden, MD (New York, New York)
The trend seems to be towards less routine monitoring other than pregnancy. Baseline tests may pick out the occasional patient with comorbidities that would preclude or delay treatment, but the majority of patients may not need the repetitive and costly testing that we have done in the past.—Richard Glogau, MD (San Francisco, California)
I have loosened my lab monitoring with isotretinoin over the past few years. If a patient has normal lipid values, comprehensive panel and complete blood cell count for the first 3 months of tests, I skip labs until the end of therapy.—Lawrence J. Green, MD (Washington, DC)
Interestingly, we focus quite a bit of attention on the risk of pregnancy with isotretinoin, and often don't focus enough on the risk with spironolactone. In our practice, we are careful to warn the patients on spironolactone about pregnancy prevention.—Stephen Stone, MD (Springfield, Illinois)
About This Survey
The survey was fielded electronically to Cutis and Dermatology News Editorial Board Members within the United States from May 5, 2019, to June 23, 2019. A total of 40 usable responses were received.
To improve patient care and outcomes, leading dermatologists from the Cutis and Dermatology News Editorial Boards answered 5 questions on monitoring acne patients on oral therapy. Here’s what we found.
Do you check potassium levels for patients taking spironolactone for acne?
Half of dermatologists surveyed never check potassium levels for patients taking spironolactone for acne. For those who do check levels, 8% do it at baseline only, 8% at baseline and every 6 months, 23% at baseline and yearly, and 13% at baseline and for dosing changes.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Although some dermatologists are still checking for potassium levels in patients taking spironolactone for acne, there is a clear trend toward foregoing laboratory monitoring. This change was likely spurred by a retrospective study of healthy young women taking spironolactone for acne that found a hyperkalemia rate of 0.72%, which is practically equivalent to the 0.76% baseline rate of hyperkalemia in this age group. Furthermore, since repeat testing in 6 of 13 patients showed normal values, the original potassium measurements may have been erroneous. Based on this study, routine potassium monitoring is likely unnecessary for healthy young women taking spironolactone for acne (Plovanich et al). In another retrospective study of women aged 18 to 65 years taking spironolactone for acne, women aged 46 to 65 years had a significantly higher rate of hyperkalemia with spironolactone compared with women aged 18 to 45 years (2/12 women [16.7%] vs 1/112 women [<1%]; P=.0245). Based on this study, potassium monitoring may be indicated for women older than 45 years taking spironolactone for acne (Thiede et al).
Next page: Cholesterol levels
Do you monitor cholesterol levels in patients taking isotretinoin?
Almost two-thirds of dermatologists indicated that they monitor all cholesterol levels in patients taking isotretinoin, including low-density lipoprotein, high-density lipoprotein, very low-density lipoprotein, and triglycerides, but almost one-third monitor triglycerides only. Five percent do not monitor cholesterol levels.
Do you routinely monitor cholesterol levels in patients taking isotretinoin?
More than 80% of dermatologists surveyed routinely monitor cholesterol levels in patients taking isotretinoin, with almost half (45%) at baseline and every 2 to 3 months. Eight percent check levels at baseline only, 28% at baseline and monthly, and 3% at baseline and end of therapy. Eighteen percent indicated they do not routinely monitor cholesterol levels.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
In this survey, dermatologists most often check cholesterol levels at baseline and then every 2 to 3 months, with most monitoring all cholesterol types. Elevations in cholesterol are by far the most common laboratory abnormality seen with isotretinoin therapy. In a retrospective study of 515 patients undergoing isotretinoin treatment of acne, mild to moderate triglyceride elevations were seen in 23.5% of patients (Hansen et al). At least in part, these elevations are likely due to the fact the levels were not drawn during fasting. Keep in mind that triglyceride-induced pancreatitis due to isotretinoin is remarkably rare, so monthly screening for triglycerides is likely not warranted. It is reasonable to monitor triglyceride levels during isotretinoin dose adjustments and for patients whose values are trending upward.
Next page: Monitoring CBC
Do you routinely monitor complete blood cell count (CBC) in patients taking isotretinoin?
More than half (55%) of dermatologists surveyed routinely monitor complete blood cell (CBC) counts in patients taking isotretinoin, while 45% do not. Of those who do monitor CBC, 13% do so at baseline only, 26% at baseline and monthly, 13% at baseline only and every 2 to 3 months, and only 3% at baseline and end of therapy.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Slightly more than half of dermatologists in this survey are obtaining CBC for their patients taking isotretinoin for acne and many of those are performing the test at baseline and monthly. Multiple studies as well as American Academy of Dermatology guidelines have substantiated that routine CBC monitoring is unwarranted in healthy patients, as abnormal values usually resolve or remain stable with therapy (American Academy of Dermatology, Isotretinoin: Recommendations). Therefore, it is worthwhile to consider foregoing CBC testing or obtaining just a baseline CBC in healthy patients being treated with isotretinoin.
Next page: Pregnancy testing
Which pregnancy test do you perform on female patients taking isotretinoin?
More than 40% of dermatologists surveyed use the urine β-human chorionic gonadotropin (hCG) pregnancy test for female patients taking isotretinoin, while 30% use the serum B-hCG test; 28% indicated that they use both tests.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
The iPLEDGE program was implemented in 2006 to avoid fetal exposure to isotretinoin and requires pregnancy testing (urine or serum) for females of childbearing potential taking isotretinoin. In a study of pregnancy-related adverse events associated with isotretinoin reported to the US Food and Drug Administration, 6740 total pregnancies were reported from 1997 to 2017. The rate peaked with 768 pregnancies in 2006 and then decreased. Because several hundred pregnancies in women taking isotretinoin have been reported yearly in the last 10 years, there is a clear need to have better systems in place and patient education to prevent fetal exposure to isotretinoin.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
I see lab monitoring as an opportunity to engage patients and families in co-directing their care (ie, practice patient- and family-centered care). Some families and patients like frequent monitoring and some want as few blood draws as possible. I do my best to make sure the decision includes components of the patients’ preferences, medical evidence and my best clinical judgement.—Craig Burkhart, MD, MS, MPH (Chapel Hill, North Caroline)
Being familiar with and following the standard of care guidelines for the individual oral therapies used in the treatment of acne is very important. However, it is equally as important to assure the individual patient (medical history, physical examination, social history, etc) is taken into consideration to determine if additional monitoring is required.—Fran E. Cook-Bolden, MD (New York, New York)
The trend seems to be towards less routine monitoring other than pregnancy. Baseline tests may pick out the occasional patient with comorbidities that would preclude or delay treatment, but the majority of patients may not need the repetitive and costly testing that we have done in the past.—Richard Glogau, MD (San Francisco, California)
I have loosened my lab monitoring with isotretinoin over the past few years. If a patient has normal lipid values, comprehensive panel and complete blood cell count for the first 3 months of tests, I skip labs until the end of therapy.—Lawrence J. Green, MD (Washington, DC)
Interestingly, we focus quite a bit of attention on the risk of pregnancy with isotretinoin, and often don't focus enough on the risk with spironolactone. In our practice, we are careful to warn the patients on spironolactone about pregnancy prevention.—Stephen Stone, MD (Springfield, Illinois)
About This Survey
The survey was fielded electronically to Cutis and Dermatology News Editorial Board Members within the United States from May 5, 2019, to June 23, 2019. A total of 40 usable responses were received.
American Academy of Dermatology. Isotretinoin: recommendations. https://www.aad.org/practicecenter/quality/clinical-guidelines/acne/isotretinoin. Accessed August 20, 2019.
Hansen TJ, Lucking S, Miller JJ, et al. Standardized laboratory monitoring with use of isotretinoin in acne. J Am Acad Dermatol. 2016;75:323-328.
Plovanich M, Weng QY, Mostaghimi A. Low usefulness of potassium monitoring among healthy young women taking spironolactone for acne. JAMA Dermatol. 2015;151:941-944.
Thiede RM, Rastogi S, Nardone B, et al. Hyperkalemia in women with acne exposed to oral spironolactone: a retrospective study from the RADAR (Research on Adverse Drug Events and Reports) program. Int J Womens Dermatol. 2019;5:155-157.
Tkachenko E, Singer S, Sharma P, et al. US Food and Drug Administration reports of pregnancy and pregnancy-related adverse events associated with isotretinoin [published online July 17, 2019]. JAMA Dermatol. doi:10.1001/jamadermatol.2019.1388.
American Academy of Dermatology. Isotretinoin: recommendations. https://www.aad.org/practicecenter/quality/clinical-guidelines/acne/isotretinoin. Accessed August 20, 2019.
Hansen TJ, Lucking S, Miller JJ, et al. Standardized laboratory monitoring with use of isotretinoin in acne. J Am Acad Dermatol. 2016;75:323-328.
Plovanich M, Weng QY, Mostaghimi A. Low usefulness of potassium monitoring among healthy young women taking spironolactone for acne. JAMA Dermatol. 2015;151:941-944.
Thiede RM, Rastogi S, Nardone B, et al. Hyperkalemia in women with acne exposed to oral spironolactone: a retrospective study from the RADAR (Research on Adverse Drug Events and Reports) program. Int J Womens Dermatol. 2019;5:155-157.
Tkachenko E, Singer S, Sharma P, et al. US Food and Drug Administration reports of pregnancy and pregnancy-related adverse events associated with isotretinoin [published online July 17, 2019]. JAMA Dermatol. doi:10.1001/jamadermatol.2019.1388.
Infographic: Hyperhidrosis Survey Results
Hyperhidrosis: Survey of the Cutis Editorial Board
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on hyperhidrosis. Here’s what we found.
In which areas do patients report hyperhidrosis most frequently?
Nearly 70% of dermatologists see patients with hyperhidrosis of the axillae, followed by the palms and soles (27%). Only 4% of dermatologists indicated that they see hyperhidrosis all over the body.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Hyperhidrosis affects up to 5% of the US population and may remarkably affect quality of life. Primary hyperhidrosis accounts for 93% of cases. Before puberty, hyperhidrosis affects the palms and soles in up to 90% of patients. In adults, the axillae are most commonly affected (51%), followed by plantar (30%), palmar (24%), and facial (10%) areas (Strutton et al).
Next page: Topical treatment
Approximately what percentage of patients are satisfied with topical treatments for hyperhidrosis?
The majority of dermatologists (88%) reported that less than half of their patients are satisfied with topical treatments for hyperhidrosis. Only 12% indicated that 51% to 70% of their patients were satisfied, and none of the respondents indicated that >70% were satisfied.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
There is clearly a need for safe and effective treatments for hyperhidrosis. Treatment of hyperhidrosis should include lifestyle and behavioral modifications. It is helpful to try to avoid hot crowded rooms when feasible, as well as stress, tight clothing, occlusive shoes, alcohol, and spicy foods. Patients should be instructed on proper use of medications, as well as the need to continue therapy for maintenance. Patients should be encouraged to follow up for alternative treatment options in cases of therapy failure.
Next page: Botulinum toxin
On average, how long do the effects of botulinum toxin last in your axillary hyperhidrosis patients?
The effects of botulinum toxin last at least 4 months and up to 6 months in most patients, according to 58% of dermatologists surveyed. Thirty percent reported 2 to 4 months, and 13% reported more than 6 months.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
OnabotulinumtoxinA is approved by the US Food and Drug Administration for severe primary axillary hyperhidrosis. Injections are ideally placed at the dermal-subcutaneous junction, with 1 unit placed every 1 to 2 cm. Dosing is 50 to 100 U per axilla with higher dosing required for the palms and soles (off label). Reported efficacy for axillary hyperhidrosis is 82% to 87%; however, 50% of patients with plantar hyperhidrosis are dissatisfied with the treatment. Sweat reduction is most apparent after 2 weeks and typically persists 6 to 8 months in clinical trials (Botox package insert).
Next page: Systemic anticholinergics
When prescribing systemic anticholinergics for hyperhidrosis, what side effect is most common among your patients?
More than three-quarters of dermatologists (81%) reported that dry mouth is the most common side effect of systemic anticholinergics. Dry eyes is the second most common side effect (15%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Systemic anticholinergics are commonly used off label for the treatment of hyperhidrosis. Adverse effects include dry mouth, blurred vision, dry eyes, orthostatic hypotension, gastrointestinal, urinary retention, tachycardia, and drowsiness. Unfortunately, these side effects cause one-third of patients to discontinue treatment (Bajaj and Langtry). A slow escalation of the dose may increase tolerability and reduce these side effects. These anticholinergics should not be taken with other medications with anticholinergic activity to avoid exacerbating these side effects.
Next page: Surgical treatment
What percentage of patients require surgery for treatment of hyperhidrosis after topical, injectable, systemic options and devices have failed?
According to 62% of dermatologists, 10% or less of patients require surgery for treatment of hyperhidrosis after other therapies have failed. Almost one-third indicated that none of their patients require surgical treatment. None of the dermatologists surveyed reported that more than 60% of patients need surgery.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Surgery is an option to treat hyperhidrosis when conservative methods have failed. Surgical therapies include curettage, liposuction, and excision. A last resort is considered sympathectomy. Endoscopic thoracic sympathectomy is employed for palmar, facial, and axillary hyperhidrosis, while endoscopic lumbar sympathectomy is indicated for plantar hyperhidrosis.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
Patients with focal idiopathic hyperhidrosis of the axillae as well as palms/soles report that this condition interferes with the quality of life in major ways, from social interactions to professional interactions. They often don't even know they have a problem and internalize that they must be overly anxious about things. I have patients that buy 3 of the same shirts and change a few times a day, costing a great deal of money (plus cleaning bills for 3 shirts as well) and costing a great deal of wasted time when they could be doing something more productive. It's great that not only botulinum toxins can be helpful for the underarms but also even less-invasive topical anticholinergics (easy to use, no discomfort, predictable, and helping make treatment for axillary hyperhidrosis much more on the radar).—Joel L. Cohen, MD (Denver, Colorado)
More and more patients are presenting to request relief from hyperhidrosis, and increasingly in nontraditional areas (ie, areas other than the axilla and forehead). These include the palms and scalp most commonly, and then the breast, chest, and back. Patients with hyperhidrosis of the feet often present requesting help for their malodorous or smelly feet and shoes.—Fran E. Cook-Bolden, MD (New York, New York)
I have found that systemic hyperhidrosis has usually been responsive to oral glycopyrrolate. But localized hyperhidrosis is more difficult to treat. Glycopyrronium has made life so much easier for my axillary hyperhidrosis patients. Now I am waiting for some game changer for palms and soles.—Lawrence J. Green, MD (Washington, DC)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from March 11, 2019, to April 8, 2019. A total of 26 usable responses were received.
Bajaj V, Langtry JA. Use of oral glycopyrronium bromide in hyperhidrosis. Br J Dermatol. 2007;157:118-121.
Botox [package insert]. Madison, NJ: Allergan, Inc; 2018.
Strutton DR, Kowalski JW, Glaser DA, et al. US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: Results from a national survey. J Am Acad Dermatol. 2004;51:241-248.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on hyperhidrosis. Here’s what we found.
In which areas do patients report hyperhidrosis most frequently?
Nearly 70% of dermatologists see patients with hyperhidrosis of the axillae, followed by the palms and soles (27%). Only 4% of dermatologists indicated that they see hyperhidrosis all over the body.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Hyperhidrosis affects up to 5% of the US population and may remarkably affect quality of life. Primary hyperhidrosis accounts for 93% of cases. Before puberty, hyperhidrosis affects the palms and soles in up to 90% of patients. In adults, the axillae are most commonly affected (51%), followed by plantar (30%), palmar (24%), and facial (10%) areas (Strutton et al).
Next page: Topical treatment
Approximately what percentage of patients are satisfied with topical treatments for hyperhidrosis?
The majority of dermatologists (88%) reported that less than half of their patients are satisfied with topical treatments for hyperhidrosis. Only 12% indicated that 51% to 70% of their patients were satisfied, and none of the respondents indicated that >70% were satisfied.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
There is clearly a need for safe and effective treatments for hyperhidrosis. Treatment of hyperhidrosis should include lifestyle and behavioral modifications. It is helpful to try to avoid hot crowded rooms when feasible, as well as stress, tight clothing, occlusive shoes, alcohol, and spicy foods. Patients should be instructed on proper use of medications, as well as the need to continue therapy for maintenance. Patients should be encouraged to follow up for alternative treatment options in cases of therapy failure.
Next page: Botulinum toxin
On average, how long do the effects of botulinum toxin last in your axillary hyperhidrosis patients?
The effects of botulinum toxin last at least 4 months and up to 6 months in most patients, according to 58% of dermatologists surveyed. Thirty percent reported 2 to 4 months, and 13% reported more than 6 months.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
OnabotulinumtoxinA is approved by the US Food and Drug Administration for severe primary axillary hyperhidrosis. Injections are ideally placed at the dermal-subcutaneous junction, with 1 unit placed every 1 to 2 cm. Dosing is 50 to 100 U per axilla with higher dosing required for the palms and soles (off label). Reported efficacy for axillary hyperhidrosis is 82% to 87%; however, 50% of patients with plantar hyperhidrosis are dissatisfied with the treatment. Sweat reduction is most apparent after 2 weeks and typically persists 6 to 8 months in clinical trials (Botox package insert).
Next page: Systemic anticholinergics
When prescribing systemic anticholinergics for hyperhidrosis, what side effect is most common among your patients?
More than three-quarters of dermatologists (81%) reported that dry mouth is the most common side effect of systemic anticholinergics. Dry eyes is the second most common side effect (15%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Systemic anticholinergics are commonly used off label for the treatment of hyperhidrosis. Adverse effects include dry mouth, blurred vision, dry eyes, orthostatic hypotension, gastrointestinal, urinary retention, tachycardia, and drowsiness. Unfortunately, these side effects cause one-third of patients to discontinue treatment (Bajaj and Langtry). A slow escalation of the dose may increase tolerability and reduce these side effects. These anticholinergics should not be taken with other medications with anticholinergic activity to avoid exacerbating these side effects.
Next page: Surgical treatment
What percentage of patients require surgery for treatment of hyperhidrosis after topical, injectable, systemic options and devices have failed?
According to 62% of dermatologists, 10% or less of patients require surgery for treatment of hyperhidrosis after other therapies have failed. Almost one-third indicated that none of their patients require surgical treatment. None of the dermatologists surveyed reported that more than 60% of patients need surgery.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Surgery is an option to treat hyperhidrosis when conservative methods have failed. Surgical therapies include curettage, liposuction, and excision. A last resort is considered sympathectomy. Endoscopic thoracic sympathectomy is employed for palmar, facial, and axillary hyperhidrosis, while endoscopic lumbar sympathectomy is indicated for plantar hyperhidrosis.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
Patients with focal idiopathic hyperhidrosis of the axillae as well as palms/soles report that this condition interferes with the quality of life in major ways, from social interactions to professional interactions. They often don't even know they have a problem and internalize that they must be overly anxious about things. I have patients that buy 3 of the same shirts and change a few times a day, costing a great deal of money (plus cleaning bills for 3 shirts as well) and costing a great deal of wasted time when they could be doing something more productive. It's great that not only botulinum toxins can be helpful for the underarms but also even less-invasive topical anticholinergics (easy to use, no discomfort, predictable, and helping make treatment for axillary hyperhidrosis much more on the radar).—Joel L. Cohen, MD (Denver, Colorado)
More and more patients are presenting to request relief from hyperhidrosis, and increasingly in nontraditional areas (ie, areas other than the axilla and forehead). These include the palms and scalp most commonly, and then the breast, chest, and back. Patients with hyperhidrosis of the feet often present requesting help for their malodorous or smelly feet and shoes.—Fran E. Cook-Bolden, MD (New York, New York)
I have found that systemic hyperhidrosis has usually been responsive to oral glycopyrrolate. But localized hyperhidrosis is more difficult to treat. Glycopyrronium has made life so much easier for my axillary hyperhidrosis patients. Now I am waiting for some game changer for palms and soles.—Lawrence J. Green, MD (Washington, DC)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from March 11, 2019, to April 8, 2019. A total of 26 usable responses were received.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on hyperhidrosis. Here’s what we found.
In which areas do patients report hyperhidrosis most frequently?
Nearly 70% of dermatologists see patients with hyperhidrosis of the axillae, followed by the palms and soles (27%). Only 4% of dermatologists indicated that they see hyperhidrosis all over the body.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Hyperhidrosis affects up to 5% of the US population and may remarkably affect quality of life. Primary hyperhidrosis accounts for 93% of cases. Before puberty, hyperhidrosis affects the palms and soles in up to 90% of patients. In adults, the axillae are most commonly affected (51%), followed by plantar (30%), palmar (24%), and facial (10%) areas (Strutton et al).
Next page: Topical treatment
Approximately what percentage of patients are satisfied with topical treatments for hyperhidrosis?
The majority of dermatologists (88%) reported that less than half of their patients are satisfied with topical treatments for hyperhidrosis. Only 12% indicated that 51% to 70% of their patients were satisfied, and none of the respondents indicated that >70% were satisfied.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
There is clearly a need for safe and effective treatments for hyperhidrosis. Treatment of hyperhidrosis should include lifestyle and behavioral modifications. It is helpful to try to avoid hot crowded rooms when feasible, as well as stress, tight clothing, occlusive shoes, alcohol, and spicy foods. Patients should be instructed on proper use of medications, as well as the need to continue therapy for maintenance. Patients should be encouraged to follow up for alternative treatment options in cases of therapy failure.
Next page: Botulinum toxin
On average, how long do the effects of botulinum toxin last in your axillary hyperhidrosis patients?
The effects of botulinum toxin last at least 4 months and up to 6 months in most patients, according to 58% of dermatologists surveyed. Thirty percent reported 2 to 4 months, and 13% reported more than 6 months.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
OnabotulinumtoxinA is approved by the US Food and Drug Administration for severe primary axillary hyperhidrosis. Injections are ideally placed at the dermal-subcutaneous junction, with 1 unit placed every 1 to 2 cm. Dosing is 50 to 100 U per axilla with higher dosing required for the palms and soles (off label). Reported efficacy for axillary hyperhidrosis is 82% to 87%; however, 50% of patients with plantar hyperhidrosis are dissatisfied with the treatment. Sweat reduction is most apparent after 2 weeks and typically persists 6 to 8 months in clinical trials (Botox package insert).
Next page: Systemic anticholinergics
When prescribing systemic anticholinergics for hyperhidrosis, what side effect is most common among your patients?
More than three-quarters of dermatologists (81%) reported that dry mouth is the most common side effect of systemic anticholinergics. Dry eyes is the second most common side effect (15%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Systemic anticholinergics are commonly used off label for the treatment of hyperhidrosis. Adverse effects include dry mouth, blurred vision, dry eyes, orthostatic hypotension, gastrointestinal, urinary retention, tachycardia, and drowsiness. Unfortunately, these side effects cause one-third of patients to discontinue treatment (Bajaj and Langtry). A slow escalation of the dose may increase tolerability and reduce these side effects. These anticholinergics should not be taken with other medications with anticholinergic activity to avoid exacerbating these side effects.
Next page: Surgical treatment
What percentage of patients require surgery for treatment of hyperhidrosis after topical, injectable, systemic options and devices have failed?
According to 62% of dermatologists, 10% or less of patients require surgery for treatment of hyperhidrosis after other therapies have failed. Almost one-third indicated that none of their patients require surgical treatment. None of the dermatologists surveyed reported that more than 60% of patients need surgery.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Surgery is an option to treat hyperhidrosis when conservative methods have failed. Surgical therapies include curettage, liposuction, and excision. A last resort is considered sympathectomy. Endoscopic thoracic sympathectomy is employed for palmar, facial, and axillary hyperhidrosis, while endoscopic lumbar sympathectomy is indicated for plantar hyperhidrosis.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
Patients with focal idiopathic hyperhidrosis of the axillae as well as palms/soles report that this condition interferes with the quality of life in major ways, from social interactions to professional interactions. They often don't even know they have a problem and internalize that they must be overly anxious about things. I have patients that buy 3 of the same shirts and change a few times a day, costing a great deal of money (plus cleaning bills for 3 shirts as well) and costing a great deal of wasted time when they could be doing something more productive. It's great that not only botulinum toxins can be helpful for the underarms but also even less-invasive topical anticholinergics (easy to use, no discomfort, predictable, and helping make treatment for axillary hyperhidrosis much more on the radar).—Joel L. Cohen, MD (Denver, Colorado)
More and more patients are presenting to request relief from hyperhidrosis, and increasingly in nontraditional areas (ie, areas other than the axilla and forehead). These include the palms and scalp most commonly, and then the breast, chest, and back. Patients with hyperhidrosis of the feet often present requesting help for their malodorous or smelly feet and shoes.—Fran E. Cook-Bolden, MD (New York, New York)
I have found that systemic hyperhidrosis has usually been responsive to oral glycopyrrolate. But localized hyperhidrosis is more difficult to treat. Glycopyrronium has made life so much easier for my axillary hyperhidrosis patients. Now I am waiting for some game changer for palms and soles.—Lawrence J. Green, MD (Washington, DC)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from March 11, 2019, to April 8, 2019. A total of 26 usable responses were received.
Bajaj V, Langtry JA. Use of oral glycopyrronium bromide in hyperhidrosis. Br J Dermatol. 2007;157:118-121.
Botox [package insert]. Madison, NJ: Allergan, Inc; 2018.
Strutton DR, Kowalski JW, Glaser DA, et al. US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: Results from a national survey. J Am Acad Dermatol. 2004;51:241-248.
Bajaj V, Langtry JA. Use of oral glycopyrronium bromide in hyperhidrosis. Br J Dermatol. 2007;157:118-121.
Botox [package insert]. Madison, NJ: Allergan, Inc; 2018.
Strutton DR, Kowalski JW, Glaser DA, et al. US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: Results from a national survey. J Am Acad Dermatol. 2004;51:241-248.
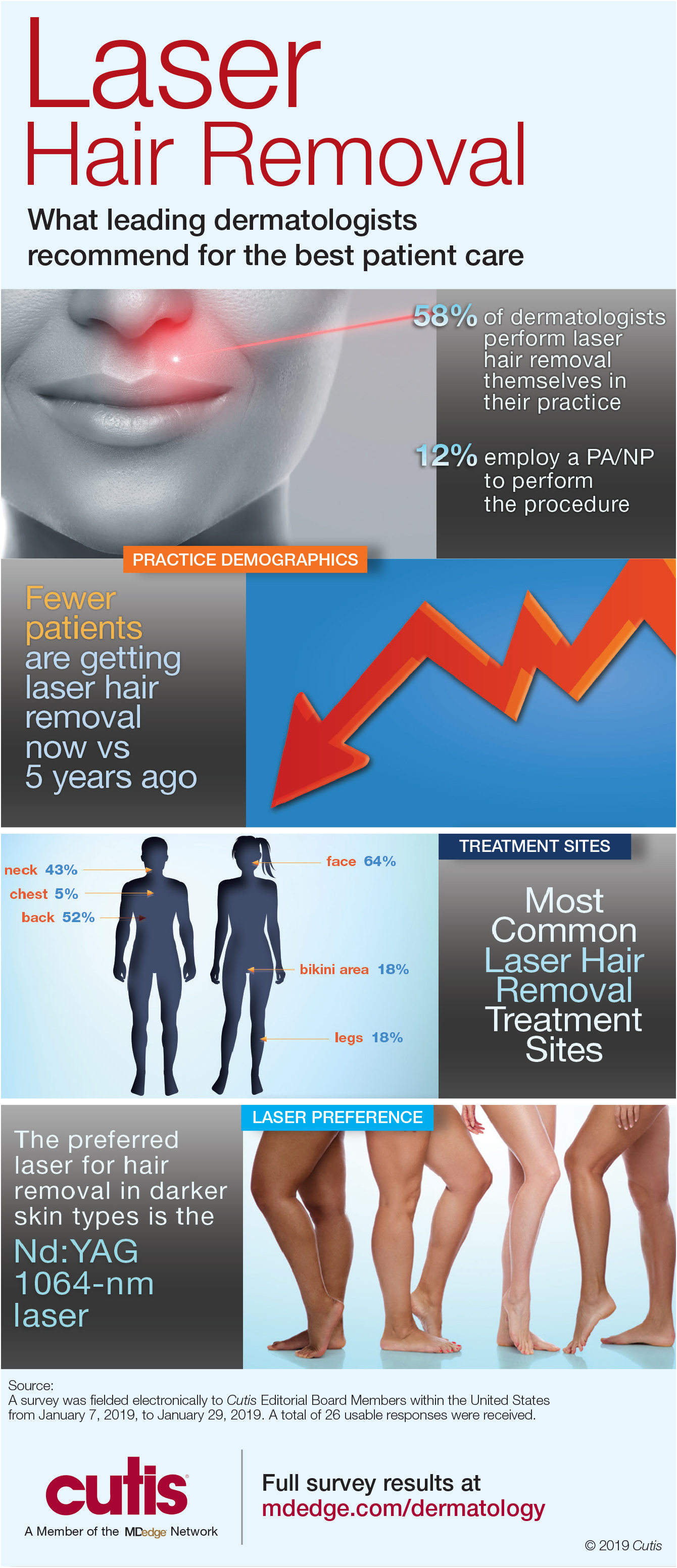
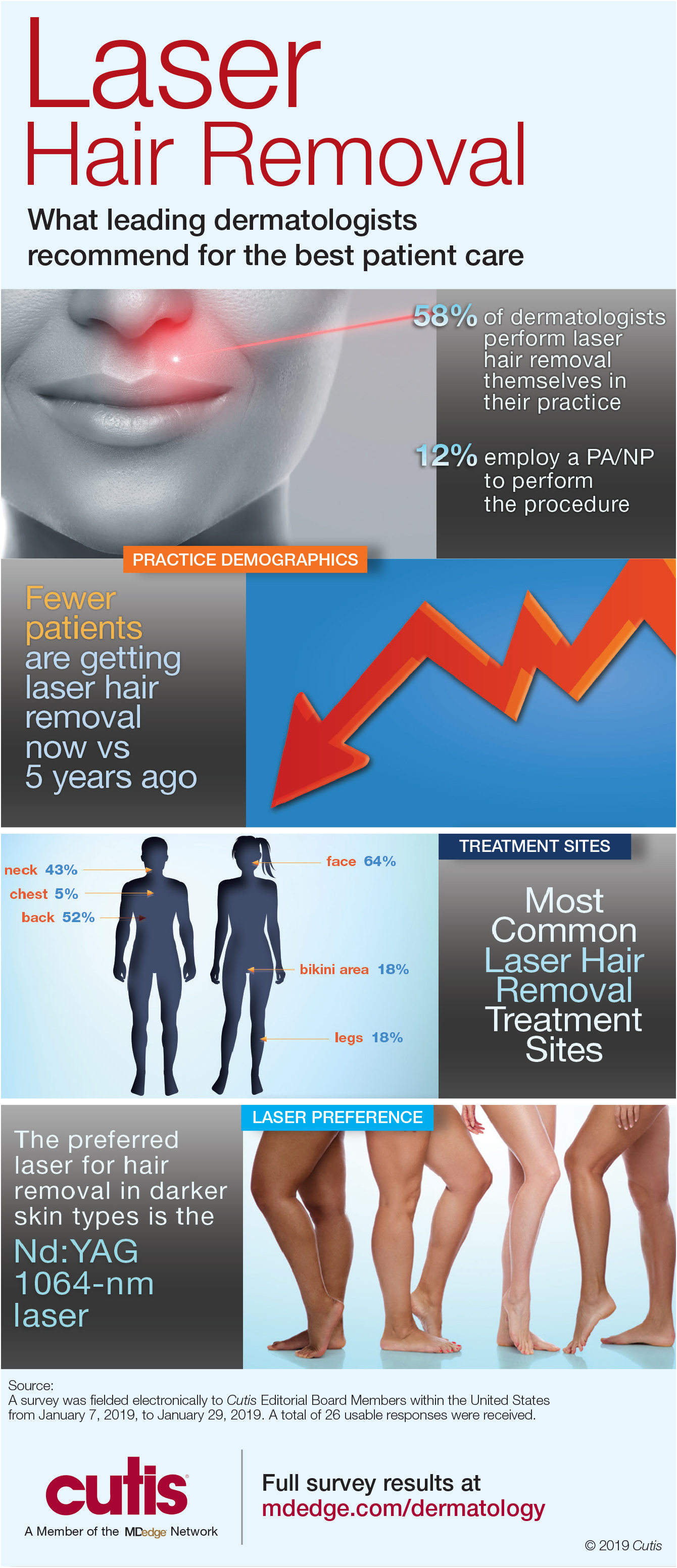
Infographic: Laser Hair Removal
Dermatologists are best equipped to treat patients who are interested in removing unwanted hair safely and effectively. Unfortunately, many patients often undergo laser hair removal treatments at spas by practitioners with limited training. Dermatologists must encourage patients to seek treatment from a board-certified dermatologist.
Full survey results and commentary from Dr. Shari Lipner are available at bit.ly/2tzNbSg.
Dermatologists are best equipped to treat patients who are interested in removing unwanted hair safely and effectively. Unfortunately, many patients often undergo laser hair removal treatments at spas by practitioners with limited training. Dermatologists must encourage patients to seek treatment from a board-certified dermatologist.
Full survey results and commentary from Dr. Shari Lipner are available at bit.ly/2tzNbSg.
Dermatologists are best equipped to treat patients who are interested in removing unwanted hair safely and effectively. Unfortunately, many patients often undergo laser hair removal treatments at spas by practitioners with limited training. Dermatologists must encourage patients to seek treatment from a board-certified dermatologist.
Full survey results and commentary from Dr. Shari Lipner are available at bit.ly/2tzNbSg.
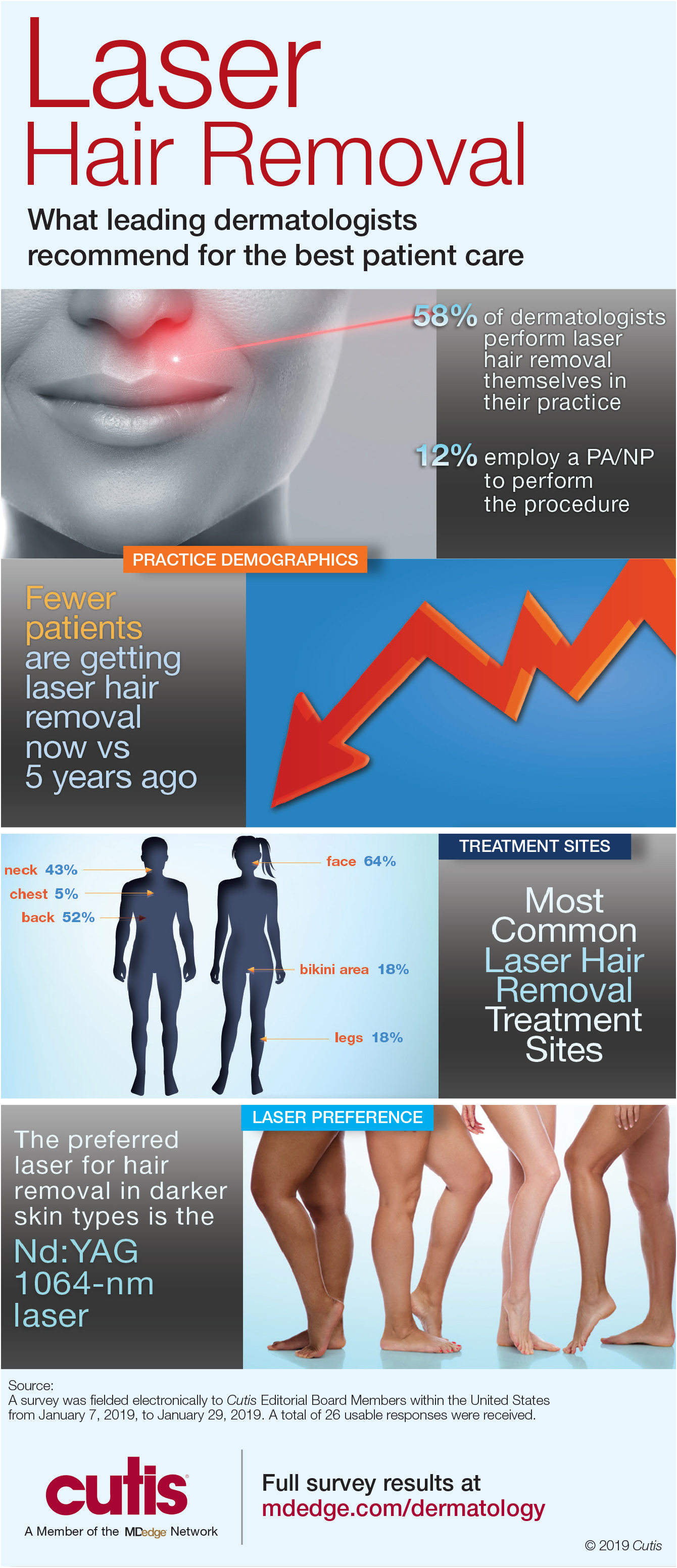
Laser Hair Removal: Survey of the Cutis Editorial Board
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on laser hair removal. Here’s what we found.
Do you perform laser hair removal in your practice?

More than half (58%) of dermatologists perform laser hair removal, while 12% have a PA/NP or aesthetician who performs this procedure on patients. Almost one-third (31%) of respondents do not perform laser hair removal.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Lasers are an important part of dermatology residency training and not a formal part of any other residency program. Therefore, dermatologists are best equipped to treat patients who are interested in removing unwanted hair safely and effectively. Dermatologists should advocate use of both a mask and a vacuum when performing these procedures to protect patients, themselves, residents, and staff from the resulting plume.
Next page: Incidence of treatment
Has the number of patients getting laser hair removal changed over the last 5 years?
Fewer patients are getting laser hair removal now vs 5 years ago, according to half of dermatologists; 42% reported that roughly the same number of patients are getting it done. Only 8% reported that more patients are getting laser hair removal.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Unfortunately, many patients often undergo hair laser treatments at spas by practitioners with limited laser training with sometimes adverse effects, including burns and scars. Therefore, we have a duty to educate our patients about laser safety and encourage them to seek treatment from a board-certified dermatologist.
Next page: Treatment areas
What area do you treat most often in women?
What area do you treat most often in men?
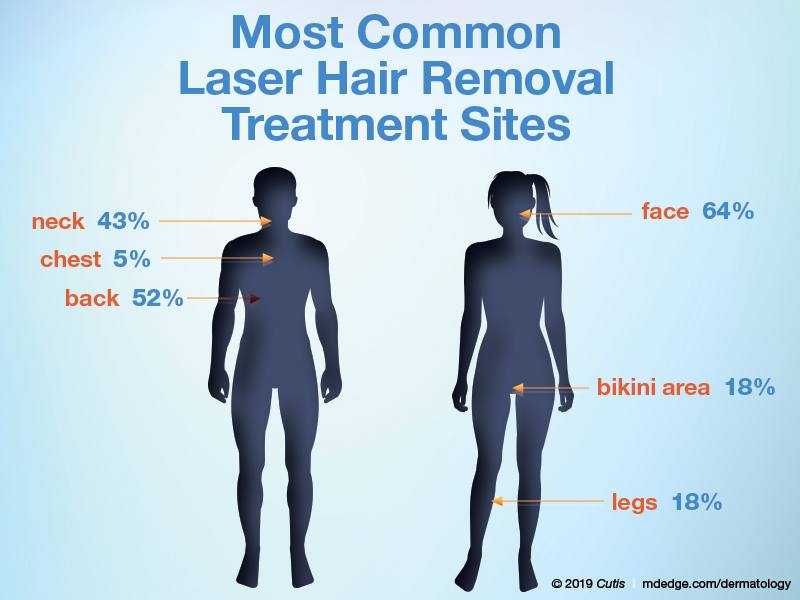
The majority of dermatologists (64%) treat the face most often in women, followed by the bikini area and legs (18% each). In men, half (52%) of dermatologists treat the back most often in men, followed by the neck (43%) and chest (5%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Before undergoing laser hair procedures, patients should be counseled that multiple treatments are often necessary, with the goal being reduction in hair density. Some hairs may still remain even after sufficient treatments. Some patients may be more comfortable with a topical numbing agent.
Next page: Lasers for darker skin types
What laser or device do you prefer to use for darker skin types?

Most dermatologists (79%) prefer to use the Nd:YAG 1064-nm laser for laser hair removal in darker skin types; 11% each prefer intense pulsed light or the alexandrite 755-nm laser.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
The alexandrite 755-nm laser can be used safely in lighter skin types, while the Nd:YAG 1064-nm laser is preferred for darker skin types. It is also highly recommended to perform test spots in darker-skinned individuals.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
Laser hair removal appears to be a safe and effective adjunctive therapy for adolescent hidradenitis patients. This has greatly increased the amount of laser hair removal treatments I perform as a pediatric dermatologist over the past 5 years.—Craig Burkhart, MD, MS, MPH (Chapel Hill, North Carolina)
Curbing unrealistic expectations is essential. It isn't magic. You won't have silky smooth, hairless skin after 1 treatment, or 2, or maybe ever. Discoloration, dyspigmentation, and scarring are possible. Making all of that clear in advance—in writing—will preempt 95% of postoperative complaints and angry phone calls.—Joseph Eastern, MD (Belleville, New Jersey)
In some states, laser hair removal is performed in medical spas without any dermatologist supervision. The lasers used in laser hair removal can be very harmful if used by nonphysicians who are not supervised.—Lawrence J. Green, MD (Washington, DC)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from January 7, 2019, to January 29, 2019. A total of 26 usable responses were received.
Georgesen C, Lipner SR. Surgical smoke: risk assessment and mitigation strategies. J Am Acad Dermatol. 2018;79:746-755.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on laser hair removal. Here’s what we found.
Do you perform laser hair removal in your practice?

More than half (58%) of dermatologists perform laser hair removal, while 12% have a PA/NP or aesthetician who performs this procedure on patients. Almost one-third (31%) of respondents do not perform laser hair removal.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Lasers are an important part of dermatology residency training and not a formal part of any other residency program. Therefore, dermatologists are best equipped to treat patients who are interested in removing unwanted hair safely and effectively. Dermatologists should advocate use of both a mask and a vacuum when performing these procedures to protect patients, themselves, residents, and staff from the resulting plume.
Next page: Incidence of treatment
Has the number of patients getting laser hair removal changed over the last 5 years?
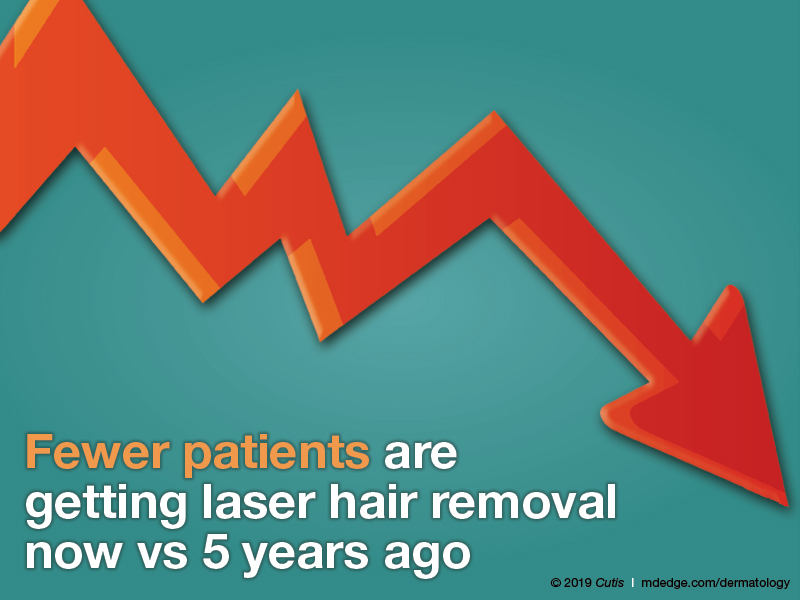
Fewer patients are getting laser hair removal now vs 5 years ago, according to half of dermatologists; 42% reported that roughly the same number of patients are getting it done. Only 8% reported that more patients are getting laser hair removal.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Unfortunately, many patients often undergo hair laser treatments at spas by practitioners with limited laser training with sometimes adverse effects, including burns and scars. Therefore, we have a duty to educate our patients about laser safety and encourage them to seek treatment from a board-certified dermatologist.
Next page: Treatment areas
What area do you treat most often in women?
What area do you treat most often in men?
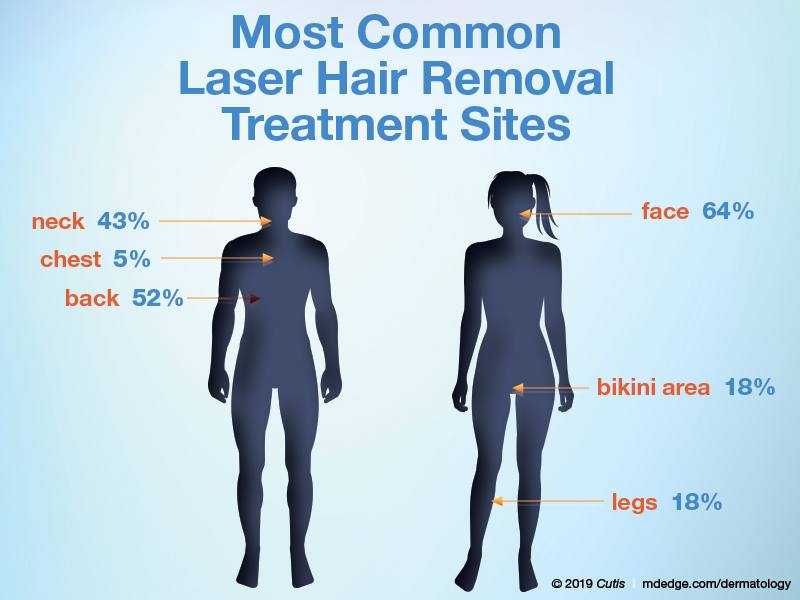
The majority of dermatologists (64%) treat the face most often in women, followed by the bikini area and legs (18% each). In men, half (52%) of dermatologists treat the back most often in men, followed by the neck (43%) and chest (5%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Before undergoing laser hair procedures, patients should be counseled that multiple treatments are often necessary, with the goal being reduction in hair density. Some hairs may still remain even after sufficient treatments. Some patients may be more comfortable with a topical numbing agent.
Next page: Lasers for darker skin types
What laser or device do you prefer to use for darker skin types?

Most dermatologists (79%) prefer to use the Nd:YAG 1064-nm laser for laser hair removal in darker skin types; 11% each prefer intense pulsed light or the alexandrite 755-nm laser.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
The alexandrite 755-nm laser can be used safely in lighter skin types, while the Nd:YAG 1064-nm laser is preferred for darker skin types. It is also highly recommended to perform test spots in darker-skinned individuals.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
Laser hair removal appears to be a safe and effective adjunctive therapy for adolescent hidradenitis patients. This has greatly increased the amount of laser hair removal treatments I perform as a pediatric dermatologist over the past 5 years.—Craig Burkhart, MD, MS, MPH (Chapel Hill, North Carolina)
Curbing unrealistic expectations is essential. It isn't magic. You won't have silky smooth, hairless skin after 1 treatment, or 2, or maybe ever. Discoloration, dyspigmentation, and scarring are possible. Making all of that clear in advance—in writing—will preempt 95% of postoperative complaints and angry phone calls.—Joseph Eastern, MD (Belleville, New Jersey)
In some states, laser hair removal is performed in medical spas without any dermatologist supervision. The lasers used in laser hair removal can be very harmful if used by nonphysicians who are not supervised.—Lawrence J. Green, MD (Washington, DC)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from January 7, 2019, to January 29, 2019. A total of 26 usable responses were received.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on laser hair removal. Here’s what we found.
Do you perform laser hair removal in your practice?

More than half (58%) of dermatologists perform laser hair removal, while 12% have a PA/NP or aesthetician who performs this procedure on patients. Almost one-third (31%) of respondents do not perform laser hair removal.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Lasers are an important part of dermatology residency training and not a formal part of any other residency program. Therefore, dermatologists are best equipped to treat patients who are interested in removing unwanted hair safely and effectively. Dermatologists should advocate use of both a mask and a vacuum when performing these procedures to protect patients, themselves, residents, and staff from the resulting plume.
Next page: Incidence of treatment
Has the number of patients getting laser hair removal changed over the last 5 years?
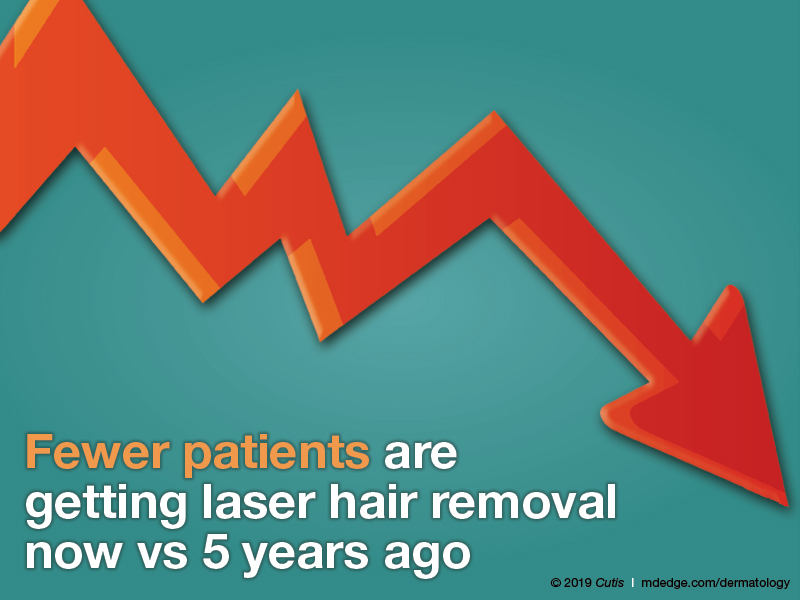
Fewer patients are getting laser hair removal now vs 5 years ago, according to half of dermatologists; 42% reported that roughly the same number of patients are getting it done. Only 8% reported that more patients are getting laser hair removal.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Unfortunately, many patients often undergo hair laser treatments at spas by practitioners with limited laser training with sometimes adverse effects, including burns and scars. Therefore, we have a duty to educate our patients about laser safety and encourage them to seek treatment from a board-certified dermatologist.
Next page: Treatment areas
What area do you treat most often in women?
What area do you treat most often in men?
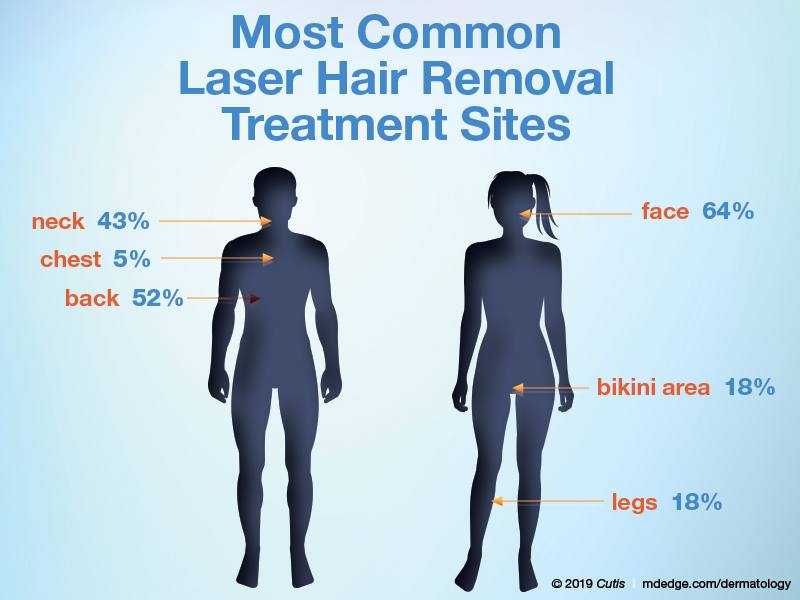
The majority of dermatologists (64%) treat the face most often in women, followed by the bikini area and legs (18% each). In men, half (52%) of dermatologists treat the back most often in men, followed by the neck (43%) and chest (5%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Before undergoing laser hair procedures, patients should be counseled that multiple treatments are often necessary, with the goal being reduction in hair density. Some hairs may still remain even after sufficient treatments. Some patients may be more comfortable with a topical numbing agent.
Next page: Lasers for darker skin types
What laser or device do you prefer to use for darker skin types?

Most dermatologists (79%) prefer to use the Nd:YAG 1064-nm laser for laser hair removal in darker skin types; 11% each prefer intense pulsed light or the alexandrite 755-nm laser.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
The alexandrite 755-nm laser can be used safely in lighter skin types, while the Nd:YAG 1064-nm laser is preferred for darker skin types. It is also highly recommended to perform test spots in darker-skinned individuals.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
Laser hair removal appears to be a safe and effective adjunctive therapy for adolescent hidradenitis patients. This has greatly increased the amount of laser hair removal treatments I perform as a pediatric dermatologist over the past 5 years.—Craig Burkhart, MD, MS, MPH (Chapel Hill, North Carolina)
Curbing unrealistic expectations is essential. It isn't magic. You won't have silky smooth, hairless skin after 1 treatment, or 2, or maybe ever. Discoloration, dyspigmentation, and scarring are possible. Making all of that clear in advance—in writing—will preempt 95% of postoperative complaints and angry phone calls.—Joseph Eastern, MD (Belleville, New Jersey)
In some states, laser hair removal is performed in medical spas without any dermatologist supervision. The lasers used in laser hair removal can be very harmful if used by nonphysicians who are not supervised.—Lawrence J. Green, MD (Washington, DC)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from January 7, 2019, to January 29, 2019. A total of 26 usable responses were received.
Georgesen C, Lipner SR. Surgical smoke: risk assessment and mitigation strategies. J Am Acad Dermatol. 2018;79:746-755.
Georgesen C, Lipner SR. Surgical smoke: risk assessment and mitigation strategies. J Am Acad Dermatol. 2018;79:746-755.
Nail Care: Survey of the Cutis Editorial Board
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on nail care. Here’s what we found.
Do you routinely perform diagnostic testing before treating for onychomycosis?
Ninety-five percent of dermatologists perform diagnostic testing before treating onychomycosis. Of them, nearly two-thirds only test before treating with systemic antifungals, while one-third test before starting systemic or topical antifungals.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
A laboratory diagnosis of onychomycosis is an absolute necessity before treating for onychomycosis, and the vast majority of our board members are testing routinely. Diagnosis should ideally be performed before initiating both oral and topical therapy. Failure to do so may lead to incorrect treatment with progression of disease and missed diagnoses of malignancy (Lipner and Scher, 2016; Lipner and Scher, 2016).
Next page: Nail fungus
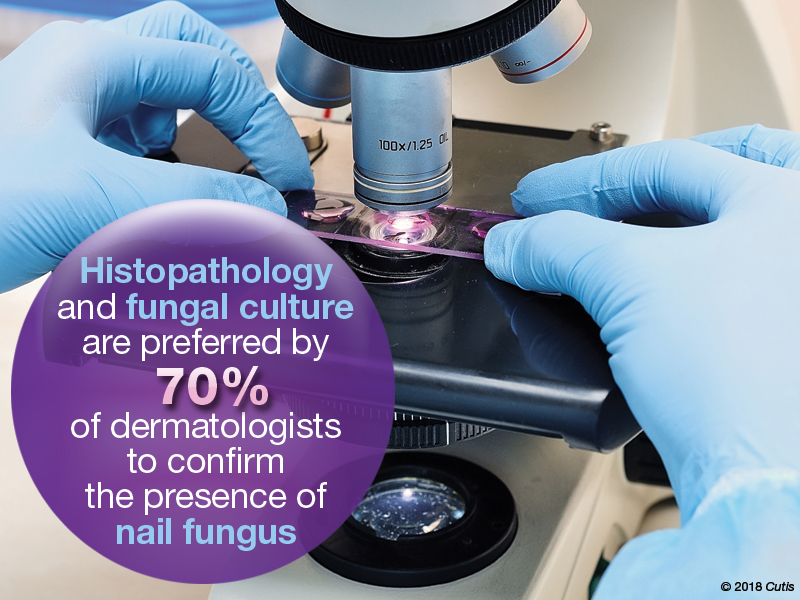
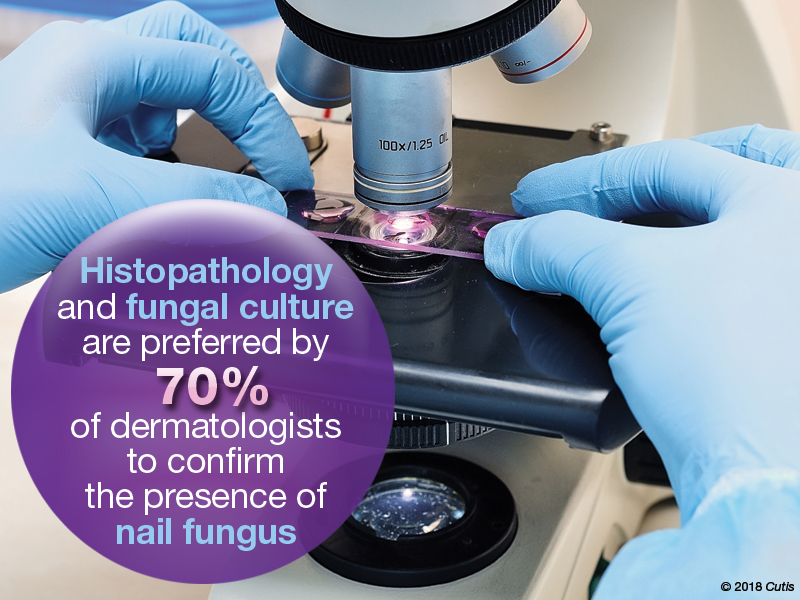
What diagnostic tests do you use to confirm the presence of a nail fungus?
More than 70% of respondents use histopathology or fungal culture to confirm the presence of a nail fungus. Direct microscopy is used by 38% and only 5% use polymerase chain reaction.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Options for diagnosis are potassium hydroxide preparation with microscopy, fungal culture, or nail plate clipping with histopathology. Polymerase chain reaction is another option that is available and covered by many insurance plans. Many of our board members use histopathology and fungal culture more often than other methods. Histopathology is advantageous for its high sensitivity and capacity to detect other nail diseases, such as nail psoriasis. A disadvantage is that the identity and viability of the infecting organism cannot be determined. While fungal culture can detect both identity and viability, the organism may take several weeks to grow and there is a high false-negative rate (Lipner and Scher, 2018 [Part 1]).
Next page: Laboratory monitoring with terbinafine
Almost half (48%) of dermatologists monitor laboratory test results in onychomycosis patients taking terbinafine at both baseline and during therapy. Twenty-three percent monitor at baseline only; 14% at baseline and after therapy; 5% at baseline, during therapy, and after therapy; and 10% don’t monitor at all.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Almost half of board members perform laboratory monitoring for patients taking terbinafine, which was reasonable prior to any published data on blood count and liver function tests in patients taking this drug. However, a new study on this topic should make us reconsider our practices. This study analyzed the rate of laboratory test abnormalities in 4985 patients taking terbinafine or griseofulvin for dermatophyte infections. Elevated alanine aminotransferase, aspartate aminotransferase, anemia, lymphopenia, and neutropenia were uncommon and similar to the baseline rates. Therefore, routine interval laboratory monitoring may be unnecessary in healthy patients taking oral terbinafine for onychomycosis (Stolmeier et al).
Next page: Biotin recommendations
Do you routinely recommend biotin to your patients?
Approximately half (52%) of dermatologists do not recommend biotin to their patients. However, 29% do recommend it for hair and nail disorders.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Biotin is an essential cofactor for mammalian carboxylase enzymes that are involved in important metabolic pathways in humans. Biotin supplementation is likely unnecessary for most individuals, as biotin intake is likely sufficient in a Western diet. There are limited data on biotin supplementation to treat dermatologic conditions, especially in patients with normal biotin levels. In addition, a recent warning issued by the US Food and Drug Administration reported that consumption of biotin may interfere with laboratory tests. Therefore, biotin should not be routinely recommended to patients without sufficient evidence that it would benefit their condition (Lipner, 2018).
Next page: Medication for onychomycosis
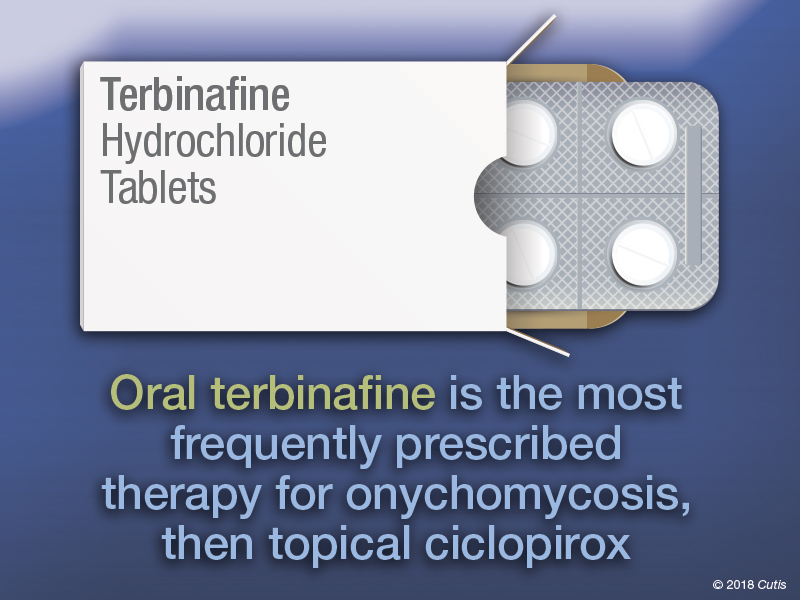
Which medication(s) do you prescribe most often for onychomycosis?
The top medications prescribed by dermatologists for onychomycosis were oral terbinafine (62%) and topical ciclopirox (52%), followed by oral fluconazole (29%), topical efinaconazole (24%), oral itraconazole (14%), and topical tavaborole (5%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Oral terbinafine is most frequently prescribed by our board, likely because it has the best efficacy, dosing regimen, and minimal potential for systemic side effects or drug-drug interactions. Efficacy with ciclopirox lacquer is quite low and the medication is difficult to apply. For toenail onychomycosis, application is daily with weekly clipping and removal and monthly debridement. Patients who are not candidates for terbinafine would likely benefit more from oral itraconazole, oral fluconazole (off label), efinaconazole, or tavaborole (Lipner and Scher, 2018 [Part II]).
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As with care in general in dermatology, the care and treatment of healthy nails and especially diseased nails is multifaceted and is optimized by using combination therapy. The combination of an oral antifungal and a topical that treats the local area and also provides protection and a healthy environment for nail growth and repair is ideal.—Fran E. Cook-Bolden, MD (New York, New York)
It’s important to culture for fungus before starting treatment. It seems many cultures turn out to be nondermatophytes, and terbinafine is not the best treatment.—Lawrence J. Green, MD (Washington, DC)
Nails do care. Diagnoses should be confirmed.—Richard K. Scher, MD (New York, New York)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from October 22, 2018, to November 14, 2018. A total of 21 usable responses were received.
- Lipner SR. Rethinking biotin therapy for hair, nail, and skin disorders. J Am Acad Dermatol. 2018;78:1236-1238.
- Lipner SR, Scher RK. Confirmatory testing for onychomycosis. JAMA Dermatol. 2016 Jul 1;152:847.
- Lipner SR, Scher RK. Onychomycosis–a small step for quality of care. Curr Med Res Opin. 2016;32:865-867.
- Lipner SR, Scher RK. Part I: onychomycosis: clinical overview and diagnosis [published online June 27, 2018]. J Am Acad Dermatol. pii:S0190-9622(18)32188-1.
- Lipner SR, Scher RK. Part II: onychomycosis: treatment and prevention of recurrence [published online June 27, 2018]. J Am Acad Dermatol. pii: S0190-9622(18)32187-X.)
- Stolmeier DA, Stratman HB, McIntee TJ, et al. Utility of laboratory test result monitoring in patients taking oral terbinafine or griseofulvin for dermatophyte infections [published online October 17, 2018]. JAMA Dermatol. doi:10.1001/jamadermatol.2018.3578.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on nail care. Here’s what we found.
Do you routinely perform diagnostic testing before treating for onychomycosis?
Ninety-five percent of dermatologists perform diagnostic testing before treating onychomycosis. Of them, nearly two-thirds only test before treating with systemic antifungals, while one-third test before starting systemic or topical antifungals.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
A laboratory diagnosis of onychomycosis is an absolute necessity before treating for onychomycosis, and the vast majority of our board members are testing routinely. Diagnosis should ideally be performed before initiating both oral and topical therapy. Failure to do so may lead to incorrect treatment with progression of disease and missed diagnoses of malignancy (Lipner and Scher, 2016; Lipner and Scher, 2016).
Next page: Nail fungus
What diagnostic tests do you use to confirm the presence of a nail fungus?
More than 70% of respondents use histopathology or fungal culture to confirm the presence of a nail fungus. Direct microscopy is used by 38% and only 5% use polymerase chain reaction.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Options for diagnosis are potassium hydroxide preparation with microscopy, fungal culture, or nail plate clipping with histopathology. Polymerase chain reaction is another option that is available and covered by many insurance plans. Many of our board members use histopathology and fungal culture more often than other methods. Histopathology is advantageous for its high sensitivity and capacity to detect other nail diseases, such as nail psoriasis. A disadvantage is that the identity and viability of the infecting organism cannot be determined. While fungal culture can detect both identity and viability, the organism may take several weeks to grow and there is a high false-negative rate (Lipner and Scher, 2018 [Part 1]).
Next page: Laboratory monitoring with terbinafine
Almost half (48%) of dermatologists monitor laboratory test results in onychomycosis patients taking terbinafine at both baseline and during therapy. Twenty-three percent monitor at baseline only; 14% at baseline and after therapy; 5% at baseline, during therapy, and after therapy; and 10% don’t monitor at all.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Almost half of board members perform laboratory monitoring for patients taking terbinafine, which was reasonable prior to any published data on blood count and liver function tests in patients taking this drug. However, a new study on this topic should make us reconsider our practices. This study analyzed the rate of laboratory test abnormalities in 4985 patients taking terbinafine or griseofulvin for dermatophyte infections. Elevated alanine aminotransferase, aspartate aminotransferase, anemia, lymphopenia, and neutropenia were uncommon and similar to the baseline rates. Therefore, routine interval laboratory monitoring may be unnecessary in healthy patients taking oral terbinafine for onychomycosis (Stolmeier et al).
Next page: Biotin recommendations
Do you routinely recommend biotin to your patients?
Approximately half (52%) of dermatologists do not recommend biotin to their patients. However, 29% do recommend it for hair and nail disorders.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Biotin is an essential cofactor for mammalian carboxylase enzymes that are involved in important metabolic pathways in humans. Biotin supplementation is likely unnecessary for most individuals, as biotin intake is likely sufficient in a Western diet. There are limited data on biotin supplementation to treat dermatologic conditions, especially in patients with normal biotin levels. In addition, a recent warning issued by the US Food and Drug Administration reported that consumption of biotin may interfere with laboratory tests. Therefore, biotin should not be routinely recommended to patients without sufficient evidence that it would benefit their condition (Lipner, 2018).
Next page: Medication for onychomycosis
Which medication(s) do you prescribe most often for onychomycosis?
The top medications prescribed by dermatologists for onychomycosis were oral terbinafine (62%) and topical ciclopirox (52%), followed by oral fluconazole (29%), topical efinaconazole (24%), oral itraconazole (14%), and topical tavaborole (5%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Oral terbinafine is most frequently prescribed by our board, likely because it has the best efficacy, dosing regimen, and minimal potential for systemic side effects or drug-drug interactions. Efficacy with ciclopirox lacquer is quite low and the medication is difficult to apply. For toenail onychomycosis, application is daily with weekly clipping and removal and monthly debridement. Patients who are not candidates for terbinafine would likely benefit more from oral itraconazole, oral fluconazole (off label), efinaconazole, or tavaborole (Lipner and Scher, 2018 [Part II]).
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As with care in general in dermatology, the care and treatment of healthy nails and especially diseased nails is multifaceted and is optimized by using combination therapy. The combination of an oral antifungal and a topical that treats the local area and also provides protection and a healthy environment for nail growth and repair is ideal.—Fran E. Cook-Bolden, MD (New York, New York)
It’s important to culture for fungus before starting treatment. It seems many cultures turn out to be nondermatophytes, and terbinafine is not the best treatment.—Lawrence J. Green, MD (Washington, DC)
Nails do care. Diagnoses should be confirmed.—Richard K. Scher, MD (New York, New York)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from October 22, 2018, to November 14, 2018. A total of 21 usable responses were received.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on nail care. Here’s what we found.
Do you routinely perform diagnostic testing before treating for onychomycosis?
Ninety-five percent of dermatologists perform diagnostic testing before treating onychomycosis. Of them, nearly two-thirds only test before treating with systemic antifungals, while one-third test before starting systemic or topical antifungals.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
A laboratory diagnosis of onychomycosis is an absolute necessity before treating for onychomycosis, and the vast majority of our board members are testing routinely. Diagnosis should ideally be performed before initiating both oral and topical therapy. Failure to do so may lead to incorrect treatment with progression of disease and missed diagnoses of malignancy (Lipner and Scher, 2016; Lipner and Scher, 2016).
Next page: Nail fungus
What diagnostic tests do you use to confirm the presence of a nail fungus?
More than 70% of respondents use histopathology or fungal culture to confirm the presence of a nail fungus. Direct microscopy is used by 38% and only 5% use polymerase chain reaction.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Options for diagnosis are potassium hydroxide preparation with microscopy, fungal culture, or nail plate clipping with histopathology. Polymerase chain reaction is another option that is available and covered by many insurance plans. Many of our board members use histopathology and fungal culture more often than other methods. Histopathology is advantageous for its high sensitivity and capacity to detect other nail diseases, such as nail psoriasis. A disadvantage is that the identity and viability of the infecting organism cannot be determined. While fungal culture can detect both identity and viability, the organism may take several weeks to grow and there is a high false-negative rate (Lipner and Scher, 2018 [Part 1]).
Next page: Laboratory monitoring with terbinafine
Almost half (48%) of dermatologists monitor laboratory test results in onychomycosis patients taking terbinafine at both baseline and during therapy. Twenty-three percent monitor at baseline only; 14% at baseline and after therapy; 5% at baseline, during therapy, and after therapy; and 10% don’t monitor at all.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Almost half of board members perform laboratory monitoring for patients taking terbinafine, which was reasonable prior to any published data on blood count and liver function tests in patients taking this drug. However, a new study on this topic should make us reconsider our practices. This study analyzed the rate of laboratory test abnormalities in 4985 patients taking terbinafine or griseofulvin for dermatophyte infections. Elevated alanine aminotransferase, aspartate aminotransferase, anemia, lymphopenia, and neutropenia were uncommon and similar to the baseline rates. Therefore, routine interval laboratory monitoring may be unnecessary in healthy patients taking oral terbinafine for onychomycosis (Stolmeier et al).
Next page: Biotin recommendations
Do you routinely recommend biotin to your patients?
Approximately half (52%) of dermatologists do not recommend biotin to their patients. However, 29% do recommend it for hair and nail disorders.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Biotin is an essential cofactor for mammalian carboxylase enzymes that are involved in important metabolic pathways in humans. Biotin supplementation is likely unnecessary for most individuals, as biotin intake is likely sufficient in a Western diet. There are limited data on biotin supplementation to treat dermatologic conditions, especially in patients with normal biotin levels. In addition, a recent warning issued by the US Food and Drug Administration reported that consumption of biotin may interfere with laboratory tests. Therefore, biotin should not be routinely recommended to patients without sufficient evidence that it would benefit their condition (Lipner, 2018).
Next page: Medication for onychomycosis
Which medication(s) do you prescribe most often for onychomycosis?
The top medications prescribed by dermatologists for onychomycosis were oral terbinafine (62%) and topical ciclopirox (52%), followed by oral fluconazole (29%), topical efinaconazole (24%), oral itraconazole (14%), and topical tavaborole (5%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Oral terbinafine is most frequently prescribed by our board, likely because it has the best efficacy, dosing regimen, and minimal potential for systemic side effects or drug-drug interactions. Efficacy with ciclopirox lacquer is quite low and the medication is difficult to apply. For toenail onychomycosis, application is daily with weekly clipping and removal and monthly debridement. Patients who are not candidates for terbinafine would likely benefit more from oral itraconazole, oral fluconazole (off label), efinaconazole, or tavaborole (Lipner and Scher, 2018 [Part II]).
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As with care in general in dermatology, the care and treatment of healthy nails and especially diseased nails is multifaceted and is optimized by using combination therapy. The combination of an oral antifungal and a topical that treats the local area and also provides protection and a healthy environment for nail growth and repair is ideal.—Fran E. Cook-Bolden, MD (New York, New York)
It’s important to culture for fungus before starting treatment. It seems many cultures turn out to be nondermatophytes, and terbinafine is not the best treatment.—Lawrence J. Green, MD (Washington, DC)
Nails do care. Diagnoses should be confirmed.—Richard K. Scher, MD (New York, New York)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from October 22, 2018, to November 14, 2018. A total of 21 usable responses were received.
- Lipner SR. Rethinking biotin therapy for hair, nail, and skin disorders. J Am Acad Dermatol. 2018;78:1236-1238.
- Lipner SR, Scher RK. Confirmatory testing for onychomycosis. JAMA Dermatol. 2016 Jul 1;152:847.
- Lipner SR, Scher RK. Onychomycosis–a small step for quality of care. Curr Med Res Opin. 2016;32:865-867.
- Lipner SR, Scher RK. Part I: onychomycosis: clinical overview and diagnosis [published online June 27, 2018]. J Am Acad Dermatol. pii:S0190-9622(18)32188-1.
- Lipner SR, Scher RK. Part II: onychomycosis: treatment and prevention of recurrence [published online June 27, 2018]. J Am Acad Dermatol. pii: S0190-9622(18)32187-X.)
- Stolmeier DA, Stratman HB, McIntee TJ, et al. Utility of laboratory test result monitoring in patients taking oral terbinafine or griseofulvin for dermatophyte infections [published online October 17, 2018]. JAMA Dermatol. doi:10.1001/jamadermatol.2018.3578.
- Lipner SR. Rethinking biotin therapy for hair, nail, and skin disorders. J Am Acad Dermatol. 2018;78:1236-1238.
- Lipner SR, Scher RK. Confirmatory testing for onychomycosis. JAMA Dermatol. 2016 Jul 1;152:847.
- Lipner SR, Scher RK. Onychomycosis–a small step for quality of care. Curr Med Res Opin. 2016;32:865-867.
- Lipner SR, Scher RK. Part I: onychomycosis: clinical overview and diagnosis [published online June 27, 2018]. J Am Acad Dermatol. pii:S0190-9622(18)32188-1.
- Lipner SR, Scher RK. Part II: onychomycosis: treatment and prevention of recurrence [published online June 27, 2018]. J Am Acad Dermatol. pii: S0190-9622(18)32187-X.)
- Stolmeier DA, Stratman HB, McIntee TJ, et al. Utility of laboratory test result monitoring in patients taking oral terbinafine or griseofulvin for dermatophyte infections [published online October 17, 2018]. JAMA Dermatol. doi:10.1001/jamadermatol.2018.3578.
Pediatric Skin Care: Survey of the Cutis Editorial Board
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on pediatric skin care. Here’s what we found.
Do you recommend sunscreen in babies younger than 6 months?
More than half (64%) of dermatologists we surveyed do not recommend using sunscreens in babies younger than 6 months; they should stay out of the sun. They recommended sun-protective clothing, hats, and sunglasses in this age group.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Babies younger than 6 months are still developing barrier functionality and have a higher surface area to body weight ratio compared to older children and adults. There is decreased UV light barrier protection and increased risk for systemic drug absorption. Therefore, it is best to avoid sunscreen in babies younger than 6 months. Instead, I recommend avoiding sunlight during peak hours, keeping babies in the shade, and dressing them in sun-protective clothing and hats.
Next page: Bathing and eczema
What advice do you give parents/guardians on bathing for babies with eczema?
Two-thirds of dermatologists (68%) indicated that moisturizers should be applied after bathing babies with eczema. More than half (64%) suggested using fragrance-free cleansers. Results varied on the frequency of bathing; 32% said bathe once daily for short periods with warm water, and 41% suggested to reduce bathing to a few nights a week.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Dry skin is a characteristic feature of atopic dermatitis. We now know that skin barrier dysfunction, such as filaggrin deficiency, contributes to the pathophysiology in some patients. In addition, a paucity of stratum corneum and intercellular lipids increases transepidermal water loss. Therefore, emollients containing humectants to augment stratum corneum hydration and occludents to reduce evaporation are extremely helpful in maintenance treatment of atopic dermatitis.
Next page: Nonsteroidal agents
Do you prescribe nonsteroidal agents for children younger than 2 years?
Almost two-thirds (64%) of dermatologists do prescribe nonsteroidal agents for children younger than 2 years.
If yes, which nonsteroidal agents do you prescribe for children?
Of those dermatologists who indicated that they do prescribe nonsteroidal agents for children younger than 2 years, almost half (45%) prescribe pimecrolimus, while 36% prescribe crisaborole or tacrolimus.
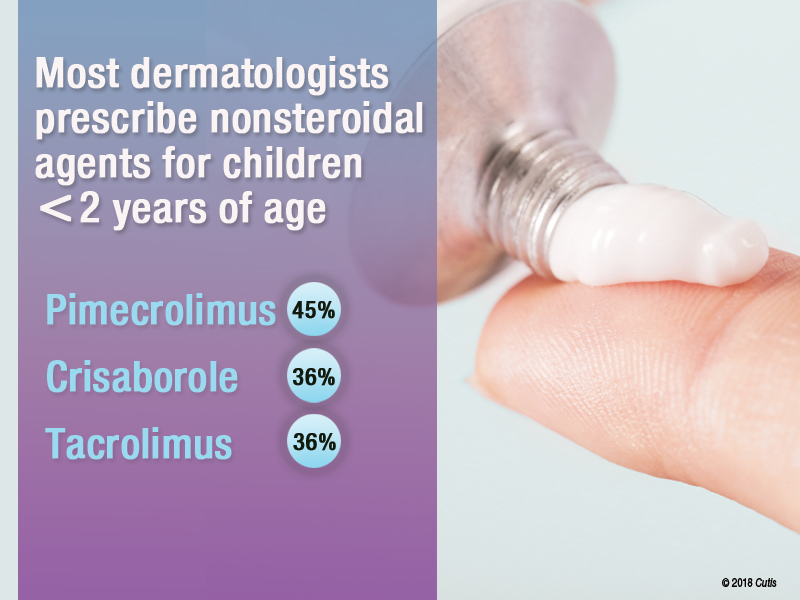
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
We have limited options for US Food and Drug Administration (FDA)–approved therapies for atopic dermatitis in children younger than 2 years. The risks of adverse effects also are higher in younger children compared to older children and adults, particularly hypothalamic-pituitary-adrenal suppression with corticosteroids. Pimecrolimus was the most common nonsteroidal prescribed in this group. It should be noted that pimecrolimus is not FDA approved for use in children younger than 2 years; however, 2 phase 3 studies were conducted with 436 infants aged 3 months to 23 months and they demonstrated safety and efficacy.
Next page: Procedures in adolescents
Which procedures do you perform on adolescents?
Forty-one percent of dermatologists surveyed indicated that they do not perform procedures on adolescents. Of those that do, 32% use laser hair removal or chemical peels in adolescents, while only 23% each use light therapy for acne or onabotulinumtoxinA for hyperhidrosis. Pulsed dye laser use was reported in only 18% of dermatologists.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
The results of this survey are a reflection of the relatively recent trends in dermatology training. Now that there is board certification in pediatric dermatology, many dermatologists now refer to pediatric dermatologists for children who need or want procedures.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
Keep the regimen as simple as possible and make sure your skin care advice is culturally relevant.—Craig Burkhart, MD (Chapel Hill, North Carolina)
Please, avoid direct sun exposure as much as possible by wearing protective garments and finding shades in the outside.—Jisun Cha, MD (New Brunswick, New Jersey)
Good habits start early. Teach children how to care for their skin and they will carry that practice with them over the course of their lifetime, and hopefully pass it on.—James Q. Del Rosso, DO (Las Vegas, Nevada)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from September 13, 2018, to October 4, 2018. A total of 22 usable responses were received.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on pediatric skin care. Here’s what we found.
Do you recommend sunscreen in babies younger than 6 months?
More than half (64%) of dermatologists we surveyed do not recommend using sunscreens in babies younger than 6 months; they should stay out of the sun. They recommended sun-protective clothing, hats, and sunglasses in this age group.
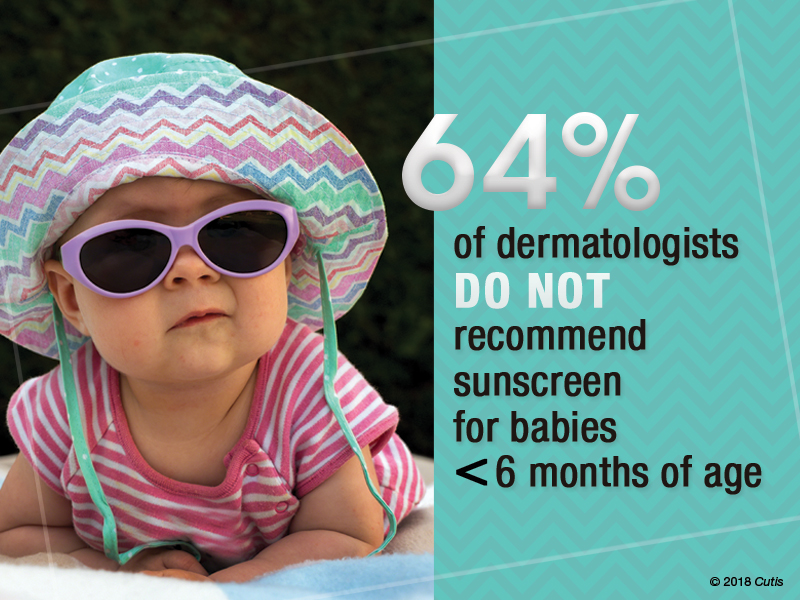
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Babies younger than 6 months are still developing barrier functionality and have a higher surface area to body weight ratio compared to older children and adults. There is decreased UV light barrier protection and increased risk for systemic drug absorption. Therefore, it is best to avoid sunscreen in babies younger than 6 months. Instead, I recommend avoiding sunlight during peak hours, keeping babies in the shade, and dressing them in sun-protective clothing and hats.
Next page: Bathing and eczema
What advice do you give parents/guardians on bathing for babies with eczema?
Two-thirds of dermatologists (68%) indicated that moisturizers should be applied after bathing babies with eczema. More than half (64%) suggested using fragrance-free cleansers. Results varied on the frequency of bathing; 32% said bathe once daily for short periods with warm water, and 41% suggested to reduce bathing to a few nights a week.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Dry skin is a characteristic feature of atopic dermatitis. We now know that skin barrier dysfunction, such as filaggrin deficiency, contributes to the pathophysiology in some patients. In addition, a paucity of stratum corneum and intercellular lipids increases transepidermal water loss. Therefore, emollients containing humectants to augment stratum corneum hydration and occludents to reduce evaporation are extremely helpful in maintenance treatment of atopic dermatitis.
Next page: Nonsteroidal agents
Do you prescribe nonsteroidal agents for children younger than 2 years?
Almost two-thirds (64%) of dermatologists do prescribe nonsteroidal agents for children younger than 2 years.
If yes, which nonsteroidal agents do you prescribe for children?
Of those dermatologists who indicated that they do prescribe nonsteroidal agents for children younger than 2 years, almost half (45%) prescribe pimecrolimus, while 36% prescribe crisaborole or tacrolimus.
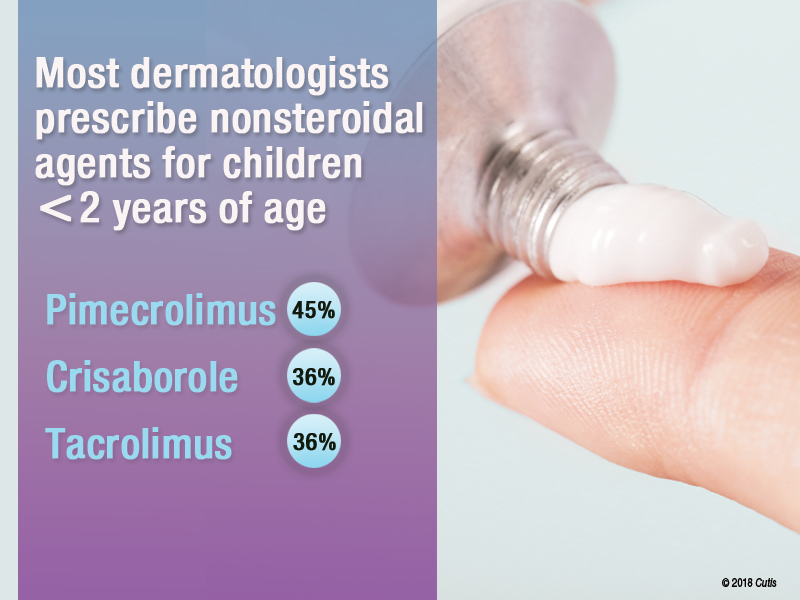
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
We have limited options for US Food and Drug Administration (FDA)–approved therapies for atopic dermatitis in children younger than 2 years. The risks of adverse effects also are higher in younger children compared to older children and adults, particularly hypothalamic-pituitary-adrenal suppression with corticosteroids. Pimecrolimus was the most common nonsteroidal prescribed in this group. It should be noted that pimecrolimus is not FDA approved for use in children younger than 2 years; however, 2 phase 3 studies were conducted with 436 infants aged 3 months to 23 months and they demonstrated safety and efficacy.
Next page: Procedures in adolescents
Which procedures do you perform on adolescents?
Forty-one percent of dermatologists surveyed indicated that they do not perform procedures on adolescents. Of those that do, 32% use laser hair removal or chemical peels in adolescents, while only 23% each use light therapy for acne or onabotulinumtoxinA for hyperhidrosis. Pulsed dye laser use was reported in only 18% of dermatologists.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
The results of this survey are a reflection of the relatively recent trends in dermatology training. Now that there is board certification in pediatric dermatology, many dermatologists now refer to pediatric dermatologists for children who need or want procedures.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
Keep the regimen as simple as possible and make sure your skin care advice is culturally relevant.—Craig Burkhart, MD (Chapel Hill, North Carolina)
Please, avoid direct sun exposure as much as possible by wearing protective garments and finding shades in the outside.—Jisun Cha, MD (New Brunswick, New Jersey)
Good habits start early. Teach children how to care for their skin and they will carry that practice with them over the course of their lifetime, and hopefully pass it on.—James Q. Del Rosso, DO (Las Vegas, Nevada)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from September 13, 2018, to October 4, 2018. A total of 22 usable responses were received.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on pediatric skin care. Here’s what we found.
Do you recommend sunscreen in babies younger than 6 months?
More than half (64%) of dermatologists we surveyed do not recommend using sunscreens in babies younger than 6 months; they should stay out of the sun. They recommended sun-protective clothing, hats, and sunglasses in this age group.
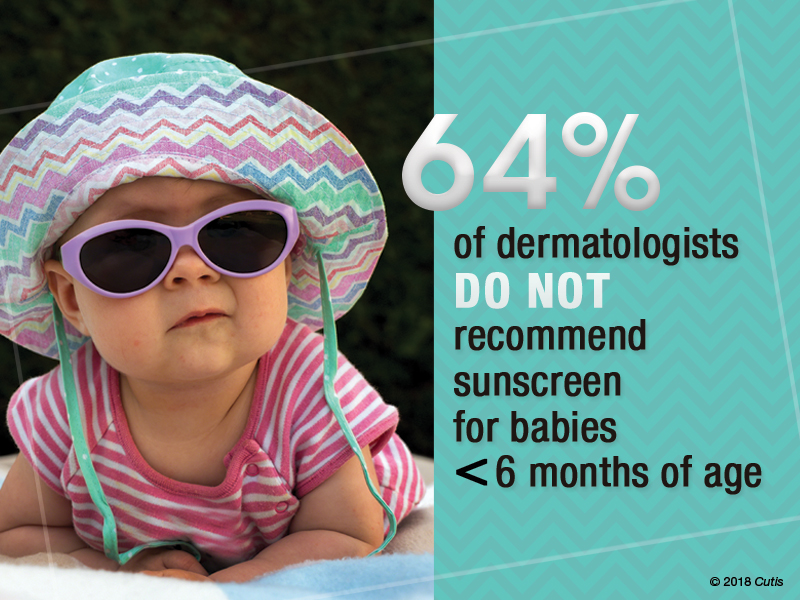
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Babies younger than 6 months are still developing barrier functionality and have a higher surface area to body weight ratio compared to older children and adults. There is decreased UV light barrier protection and increased risk for systemic drug absorption. Therefore, it is best to avoid sunscreen in babies younger than 6 months. Instead, I recommend avoiding sunlight during peak hours, keeping babies in the shade, and dressing them in sun-protective clothing and hats.
Next page: Bathing and eczema
What advice do you give parents/guardians on bathing for babies with eczema?
Two-thirds of dermatologists (68%) indicated that moisturizers should be applied after bathing babies with eczema. More than half (64%) suggested using fragrance-free cleansers. Results varied on the frequency of bathing; 32% said bathe once daily for short periods with warm water, and 41% suggested to reduce bathing to a few nights a week.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Dry skin is a characteristic feature of atopic dermatitis. We now know that skin barrier dysfunction, such as filaggrin deficiency, contributes to the pathophysiology in some patients. In addition, a paucity of stratum corneum and intercellular lipids increases transepidermal water loss. Therefore, emollients containing humectants to augment stratum corneum hydration and occludents to reduce evaporation are extremely helpful in maintenance treatment of atopic dermatitis.
Next page: Nonsteroidal agents
Do you prescribe nonsteroidal agents for children younger than 2 years?
Almost two-thirds (64%) of dermatologists do prescribe nonsteroidal agents for children younger than 2 years.
If yes, which nonsteroidal agents do you prescribe for children?
Of those dermatologists who indicated that they do prescribe nonsteroidal agents for children younger than 2 years, almost half (45%) prescribe pimecrolimus, while 36% prescribe crisaborole or tacrolimus.
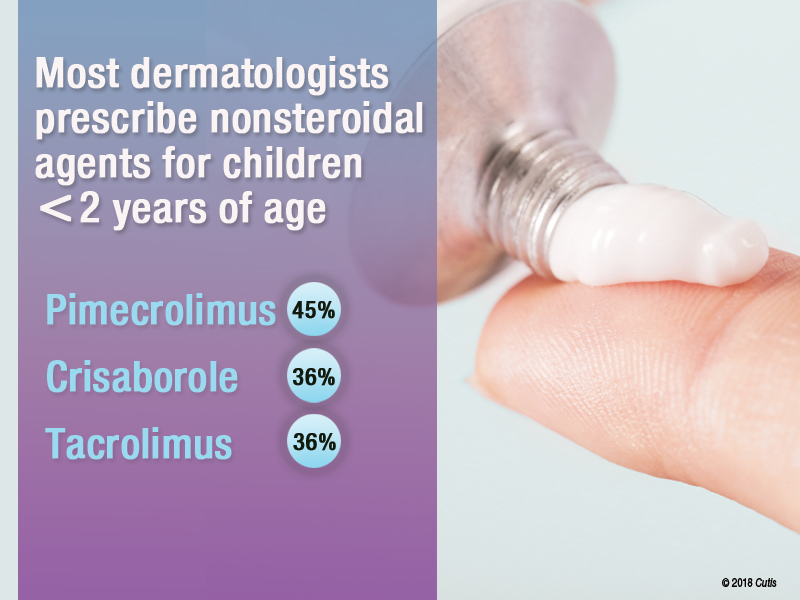
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
We have limited options for US Food and Drug Administration (FDA)–approved therapies for atopic dermatitis in children younger than 2 years. The risks of adverse effects also are higher in younger children compared to older children and adults, particularly hypothalamic-pituitary-adrenal suppression with corticosteroids. Pimecrolimus was the most common nonsteroidal prescribed in this group. It should be noted that pimecrolimus is not FDA approved for use in children younger than 2 years; however, 2 phase 3 studies were conducted with 436 infants aged 3 months to 23 months and they demonstrated safety and efficacy.
Next page: Procedures in adolescents
Which procedures do you perform on adolescents?
Forty-one percent of dermatologists surveyed indicated that they do not perform procedures on adolescents. Of those that do, 32% use laser hair removal or chemical peels in adolescents, while only 23% each use light therapy for acne or onabotulinumtoxinA for hyperhidrosis. Pulsed dye laser use was reported in only 18% of dermatologists.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
The results of this survey are a reflection of the relatively recent trends in dermatology training. Now that there is board certification in pediatric dermatology, many dermatologists now refer to pediatric dermatologists for children who need or want procedures.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
Keep the regimen as simple as possible and make sure your skin care advice is culturally relevant.—Craig Burkhart, MD (Chapel Hill, North Carolina)
Please, avoid direct sun exposure as much as possible by wearing protective garments and finding shades in the outside.—Jisun Cha, MD (New Brunswick, New Jersey)
Good habits start early. Teach children how to care for their skin and they will carry that practice with them over the course of their lifetime, and hopefully pass it on.—James Q. Del Rosso, DO (Las Vegas, Nevada)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from September 13, 2018, to October 4, 2018. A total of 22 usable responses were received.
Sunscreens: Survey of the Cutis Editorial Board
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on sunscreens. Here’s what we found.
What sun protection factor (SPF) do you recommend for the majority of your patients?

Fifty percent of dermatologists we surveyed recommend SPF 30. SPF 50 was recommended by 26%, SPF 50+ by 21%, and SPF 15 by only 2%.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Half of our Editorial Board recommends sunscreen with SPF 30, with many recommending SPF 50 or higher. This trend toward sunscreens with higher SPF is consistent with a survey-based study with 97% of dermatologists stating they were comfortable recommending sunscreens with an SPF of 50 or higher and 83.3% stating that they believe that high SPF sunscreens provide an additional margin of safety (Farberg et al). These trends are supported by a randomized, double-blind, split-face clinical trial in which participants applied either SPF 50+ or SPF 100+ sunscreen after exposure to natural sunlight. The results showed that SPF 100+ sunscreen was remarkably more effective in protecting against sunburn than SPF 50+ sunscreen in actual use conditions (Williams et al).
Next page: Spray sunscreens
Which patient populations do you feel may benefit from spray sunscreens?
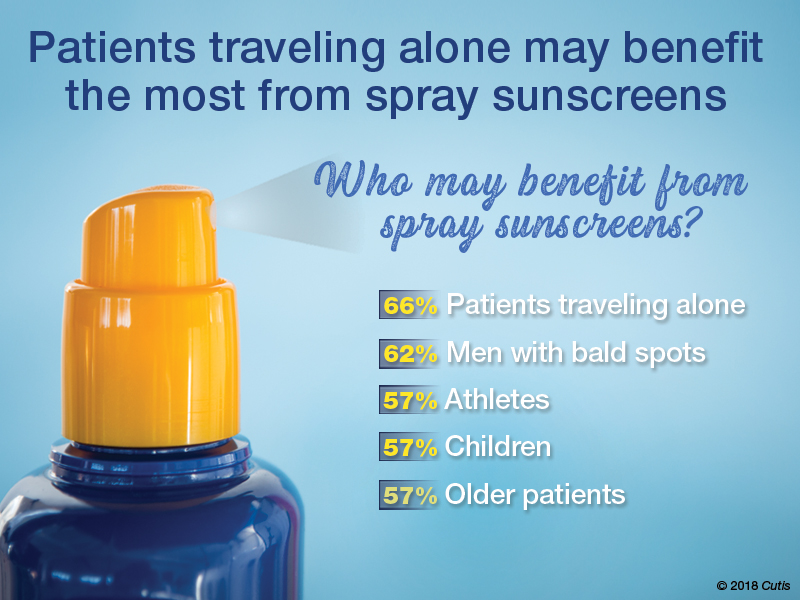
Two-thirds of dermatologists indicated that spray sunscreens may benefit patients traveling alone. Men with bald spots also may benefit (62%), as well as athletes, children, and older patients (57% each).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
As dermatologists, we tell our patients that the best sunscreens are ones that are used consistently. Spray sunscreens are likely as effective as lotions (Ou-Yang et al). There has been a clear trend in consumer purchasing of spray sunscreens from 2011 to 2016 (Teplitz et al). Spray sunscreens may benefit those traveling alone, particularly for hard-to-reach areas.
Next page: Supplemental vitamin D
In patients who apply sunscreen regularly, do you recommend supplemental vitamin D3?

More than half (53%) of dermatologists recommend supplemental vitamin D3.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Because use of photoprotection results in decreased vitamin D levels in most individuals, it is good practice to recommend vitamin D supplementation in patients who are applying sunscreen regularly (Bogaczewicz et al).
Next page: Sunscreen compliance
What is the most often heard reason(s) for not using sunscreen in your patients?
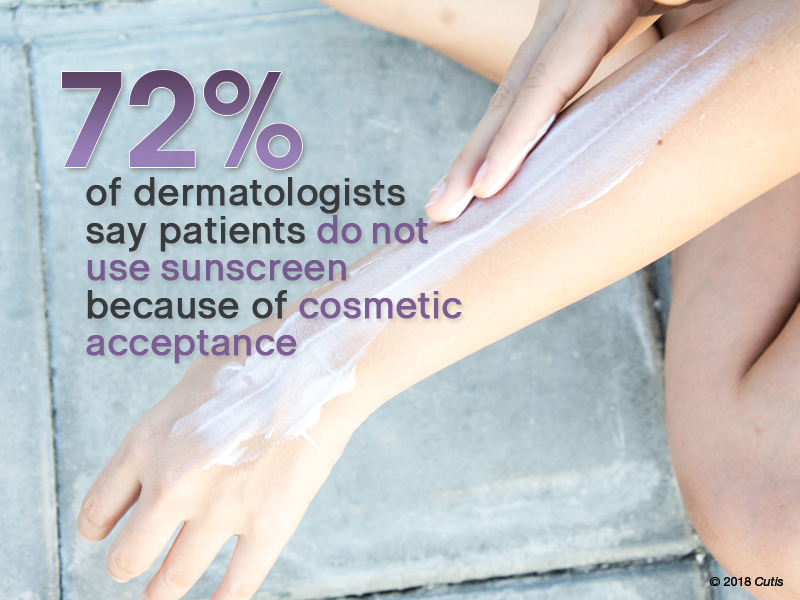
Nearly three-quarters (72%) of dermatologists reported that patients do not use sunscreen because of cosmetic acceptance. Almost one-third (31%) said their patients prefer “natural” products. Price was a factor for 26%. Fewer dermatologists indicated risk of environmental damage (14%), allergy (12%), cancer induction (5%), and hormonal alteration (5%) were reasons patients are not compliant.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Cosmetic acceptance is paramount for patient compliance for sunscreen application. These results from our Editorial Board echo a study on sunscreen product performance and other determinants of consumer preferences, which cited “cosmetic elegance” as an important factor in choosing sunscreens (Xu et al). Dermatologists must stress to patients to find a sunscreen that they find acceptable in terms of vehicle and price to increase compliance.
Next page: Sunscreens in pregnant women
What sunscreens do you recommend to pregnant women and children?

Most dermatologists (86%) recommend physical blockers “chemical-free” only sunscreens to pregnant women and children.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
While absorption of sunscreen by human embryos is likely negligible, because there is limited data on sunscreen effects in embryos and children, it is reasonable to recommend physical blockers for pregnant women and children.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As a dermatologist married to a pediatrician, I try to get my kids to embrace sun-protection strategies. For the little ones it’s hard, but as they have gotten older and been exposed to more derm journals sitting around with pretty graphic pictures, they seem to get on board, even when away at summer camp on their own. If only our patients knew what our kids do.—Joel L. Cohen, MD (Denver, Colorado)
The most important factor in getting patient compliance with sunscreen usage is “cosmetic acceptance.” If they or their children or their spouse don’t like the feel, they won’t use it.—Vincent A. DeLeo, MD (Los Angeles, California)
Not using photoprotection with sunscreen is like crossing a busy road without looking both ways first.—James Q. Del Rosso, DO (Las Vegas, Nevada)
I do not recommend spray sunscreens. At least half of the spray seems to go in the air rather than on the skin. And people often do not rub the spray into their skin well enough. Lotions are better!—Lawrence J. Green, MD (Washington, DC)
The most important factor in sunscreen is not SPF; educate patients on the important role vehicle and sweating play in the length of sun protection.—Orit Markowitz, MD (New York, New York)
Reapplying sunscreen in the appropriate amount is key to blocking the danger rays of the sun.—Vineet Mishra, MD (San Antonio, Texas)
A good sunscreen is the one you put on properly. Regardless of the formulation, make sure you apply the sunscreen evenly to all exposed skin and reapply according to directions on the container. Remember, a regular white T-shirt has minimal SPF 4-5. Either wear sun-protective clothing or wear sunscreen underneath!—Larisa Ravitskiy, MD (Gahanna, Ohio)
Sun protection and sunscreen application go hand-in-hand. We can still enjoy the outdoors without getting excessive UV exposure.—Anthony M. Rossi, MD (New York, New York)
Sunscreens are only part of sun protection. Make sure to reapply them regularly, try to avoid direct sun between about 10 AM and 2 PM if possible, and wear a hat with a wide brim (not a baseball cap, which, after all, is designed for catching baseballs, not sun protection).—Robert I. Rudolph, MD (Wyomissing, Pennsylvania)
Sunscreens keep you younger looking longer!—Richard K. Scher, MD (New York, New York)
The dentist says only floss the teeth you want to keep. I tell patients to only sun block the skin they want to keep.—Daniel M. Siegel, MD, MS (Brooklyn, New York)
The best sunscreen is the one that is used! If it's too greasy or drying, smells bad or stings, it won't be used. Stick to the one YOU like, but at least SPF 30 or better.—Stephen P. Stone, MD, (Springfield, Illinois)
Sunscreen can be a meaningful part of your sun-protection regimen used in conjunction with sun-protective clothing, sun safe behaviors, and a diet rich in natural antioxidants.—Michelle Tarbox, MD (Lubbock, Texas)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from August 2, 2018, to September 2, 2018. A total of 42 usable responses were received.
Bogaczewicz J, Karczmarewicz E, Pludowski P, et al. Requirement for vitamin D supplementation in patients using photoprotection: variations in vitamin D levels and bone formation markers. Int J Dermatol. 2016;55:e176-e183.
Farberg AS, Glazer AM, Rigel AC, et al. Dermatologists’ perceptions, recommendations, and use of sunscreen. JAMA Dermatol. 2017;153:99-101.
Ou-Yang H, Stanfield J, Cole C, et al. High-SPF sunscreens (SPF ≥ 70) may provide ultraviolet protection above minimal recommended levels by adequately compensating for lower sunscreen user application amounts. J Am Acad Dermatol. 2012;67:1220-1227.
Teplitz RW, Glazer AM, Svoboda RM, et al. Trends in US sunscreen formulations: impact of increasing spray usage. J Am Acad Dermatol. 2018;78:187-189.
Williams JD, Maitra P, Atillasoy E, et al. SPF 100+ sunscreen is more protective against sunburn than SPF 50+ in actual use: Results of a randomized, double-blind, split-face, natural sunlight exposure clinical trial. J Am Acad Dermatol. 2018;78:902.e2-910.e2.
Xu S, Kwa M, Agarwal A, et al. Sunscreen product performance and other determinants of consumer preferences. JAMA Dermatol. 2016;152:920-927.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on sunscreens. Here’s what we found.
What sun protection factor (SPF) do you recommend for the majority of your patients?

Fifty percent of dermatologists we surveyed recommend SPF 30. SPF 50 was recommended by 26%, SPF 50+ by 21%, and SPF 15 by only 2%.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Half of our Editorial Board recommends sunscreen with SPF 30, with many recommending SPF 50 or higher. This trend toward sunscreens with higher SPF is consistent with a survey-based study with 97% of dermatologists stating they were comfortable recommending sunscreens with an SPF of 50 or higher and 83.3% stating that they believe that high SPF sunscreens provide an additional margin of safety (Farberg et al). These trends are supported by a randomized, double-blind, split-face clinical trial in which participants applied either SPF 50+ or SPF 100+ sunscreen after exposure to natural sunlight. The results showed that SPF 100+ sunscreen was remarkably more effective in protecting against sunburn than SPF 50+ sunscreen in actual use conditions (Williams et al).
Next page: Spray sunscreens
Which patient populations do you feel may benefit from spray sunscreens?
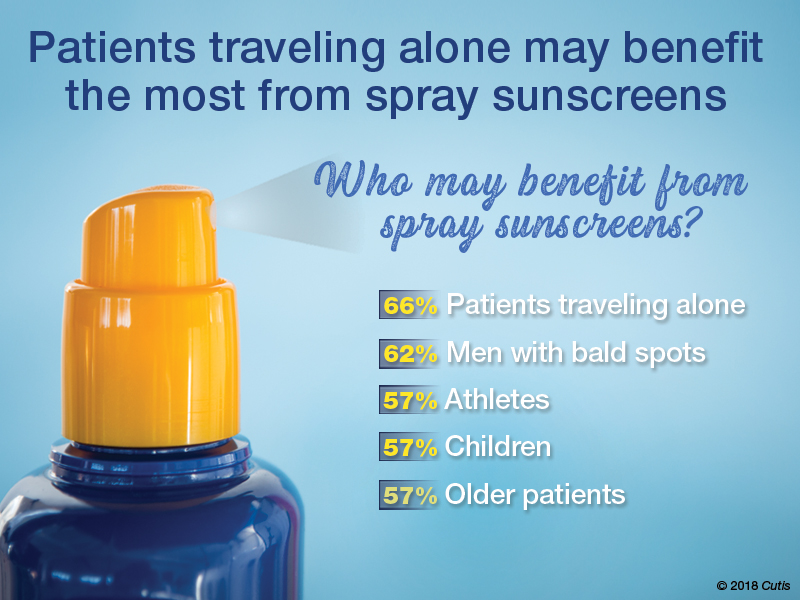
Two-thirds of dermatologists indicated that spray sunscreens may benefit patients traveling alone. Men with bald spots also may benefit (62%), as well as athletes, children, and older patients (57% each).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
As dermatologists, we tell our patients that the best sunscreens are ones that are used consistently. Spray sunscreens are likely as effective as lotions (Ou-Yang et al). There has been a clear trend in consumer purchasing of spray sunscreens from 2011 to 2016 (Teplitz et al). Spray sunscreens may benefit those traveling alone, particularly for hard-to-reach areas.
Next page: Supplemental vitamin D
In patients who apply sunscreen regularly, do you recommend supplemental vitamin D3?

More than half (53%) of dermatologists recommend supplemental vitamin D3.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Because use of photoprotection results in decreased vitamin D levels in most individuals, it is good practice to recommend vitamin D supplementation in patients who are applying sunscreen regularly (Bogaczewicz et al).
Next page: Sunscreen compliance
What is the most often heard reason(s) for not using sunscreen in your patients?
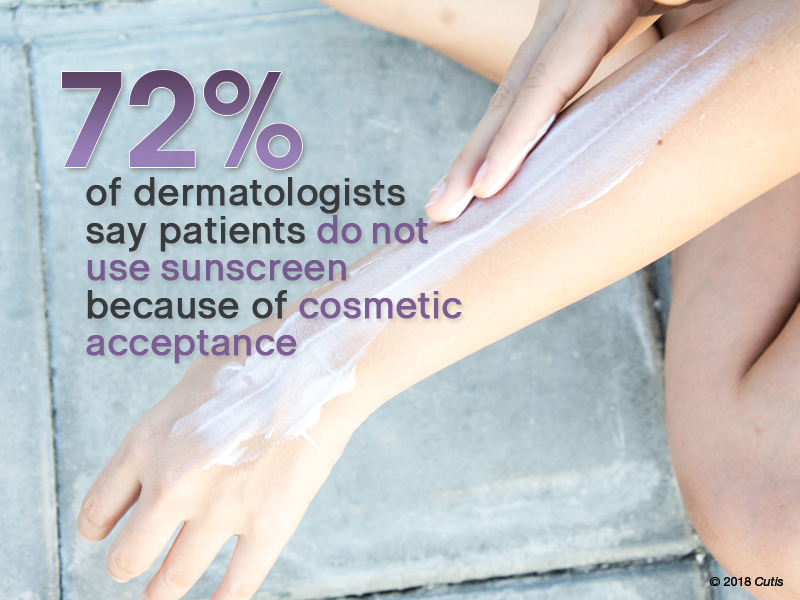
Nearly three-quarters (72%) of dermatologists reported that patients do not use sunscreen because of cosmetic acceptance. Almost one-third (31%) said their patients prefer “natural” products. Price was a factor for 26%. Fewer dermatologists indicated risk of environmental damage (14%), allergy (12%), cancer induction (5%), and hormonal alteration (5%) were reasons patients are not compliant.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Cosmetic acceptance is paramount for patient compliance for sunscreen application. These results from our Editorial Board echo a study on sunscreen product performance and other determinants of consumer preferences, which cited “cosmetic elegance” as an important factor in choosing sunscreens (Xu et al). Dermatologists must stress to patients to find a sunscreen that they find acceptable in terms of vehicle and price to increase compliance.
Next page: Sunscreens in pregnant women
What sunscreens do you recommend to pregnant women and children?

Most dermatologists (86%) recommend physical blockers “chemical-free” only sunscreens to pregnant women and children.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
While absorption of sunscreen by human embryos is likely negligible, because there is limited data on sunscreen effects in embryos and children, it is reasonable to recommend physical blockers for pregnant women and children.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As a dermatologist married to a pediatrician, I try to get my kids to embrace sun-protection strategies. For the little ones it’s hard, but as they have gotten older and been exposed to more derm journals sitting around with pretty graphic pictures, they seem to get on board, even when away at summer camp on their own. If only our patients knew what our kids do.—Joel L. Cohen, MD (Denver, Colorado)
The most important factor in getting patient compliance with sunscreen usage is “cosmetic acceptance.” If they or their children or their spouse don’t like the feel, they won’t use it.—Vincent A. DeLeo, MD (Los Angeles, California)
Not using photoprotection with sunscreen is like crossing a busy road without looking both ways first.—James Q. Del Rosso, DO (Las Vegas, Nevada)
I do not recommend spray sunscreens. At least half of the spray seems to go in the air rather than on the skin. And people often do not rub the spray into their skin well enough. Lotions are better!—Lawrence J. Green, MD (Washington, DC)
The most important factor in sunscreen is not SPF; educate patients on the important role vehicle and sweating play in the length of sun protection.—Orit Markowitz, MD (New York, New York)
Reapplying sunscreen in the appropriate amount is key to blocking the danger rays of the sun.—Vineet Mishra, MD (San Antonio, Texas)
A good sunscreen is the one you put on properly. Regardless of the formulation, make sure you apply the sunscreen evenly to all exposed skin and reapply according to directions on the container. Remember, a regular white T-shirt has minimal SPF 4-5. Either wear sun-protective clothing or wear sunscreen underneath!—Larisa Ravitskiy, MD (Gahanna, Ohio)
Sun protection and sunscreen application go hand-in-hand. We can still enjoy the outdoors without getting excessive UV exposure.—Anthony M. Rossi, MD (New York, New York)
Sunscreens are only part of sun protection. Make sure to reapply them regularly, try to avoid direct sun between about 10 AM and 2 PM if possible, and wear a hat with a wide brim (not a baseball cap, which, after all, is designed for catching baseballs, not sun protection).—Robert I. Rudolph, MD (Wyomissing, Pennsylvania)
Sunscreens keep you younger looking longer!—Richard K. Scher, MD (New York, New York)
The dentist says only floss the teeth you want to keep. I tell patients to only sun block the skin they want to keep.—Daniel M. Siegel, MD, MS (Brooklyn, New York)
The best sunscreen is the one that is used! If it's too greasy or drying, smells bad or stings, it won't be used. Stick to the one YOU like, but at least SPF 30 or better.—Stephen P. Stone, MD, (Springfield, Illinois)
Sunscreen can be a meaningful part of your sun-protection regimen used in conjunction with sun-protective clothing, sun safe behaviors, and a diet rich in natural antioxidants.—Michelle Tarbox, MD (Lubbock, Texas)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from August 2, 2018, to September 2, 2018. A total of 42 usable responses were received.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on sunscreens. Here’s what we found.
What sun protection factor (SPF) do you recommend for the majority of your patients?

Fifty percent of dermatologists we surveyed recommend SPF 30. SPF 50 was recommended by 26%, SPF 50+ by 21%, and SPF 15 by only 2%.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Half of our Editorial Board recommends sunscreen with SPF 30, with many recommending SPF 50 or higher. This trend toward sunscreens with higher SPF is consistent with a survey-based study with 97% of dermatologists stating they were comfortable recommending sunscreens with an SPF of 50 or higher and 83.3% stating that they believe that high SPF sunscreens provide an additional margin of safety (Farberg et al). These trends are supported by a randomized, double-blind, split-face clinical trial in which participants applied either SPF 50+ or SPF 100+ sunscreen after exposure to natural sunlight. The results showed that SPF 100+ sunscreen was remarkably more effective in protecting against sunburn than SPF 50+ sunscreen in actual use conditions (Williams et al).
Next page: Spray sunscreens
Which patient populations do you feel may benefit from spray sunscreens?
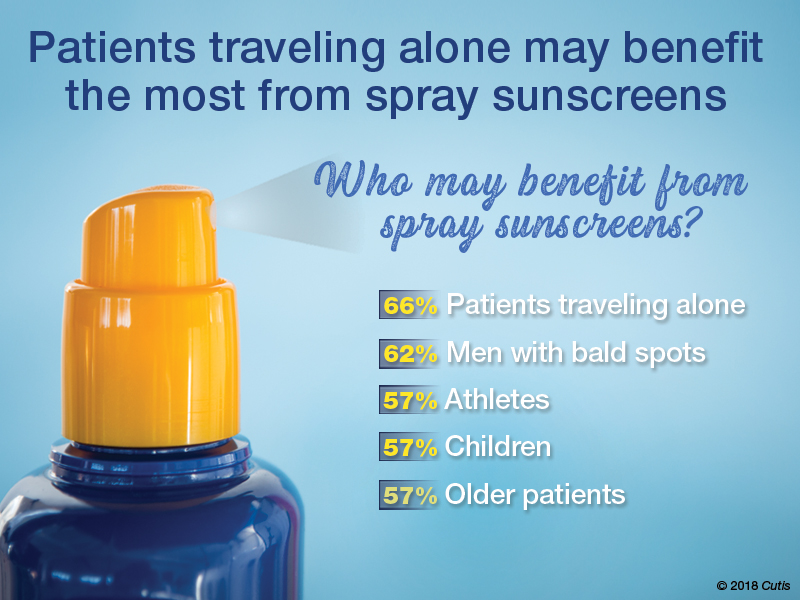
Two-thirds of dermatologists indicated that spray sunscreens may benefit patients traveling alone. Men with bald spots also may benefit (62%), as well as athletes, children, and older patients (57% each).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
As dermatologists, we tell our patients that the best sunscreens are ones that are used consistently. Spray sunscreens are likely as effective as lotions (Ou-Yang et al). There has been a clear trend in consumer purchasing of spray sunscreens from 2011 to 2016 (Teplitz et al). Spray sunscreens may benefit those traveling alone, particularly for hard-to-reach areas.
Next page: Supplemental vitamin D
In patients who apply sunscreen regularly, do you recommend supplemental vitamin D3?

More than half (53%) of dermatologists recommend supplemental vitamin D3.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Because use of photoprotection results in decreased vitamin D levels in most individuals, it is good practice to recommend vitamin D supplementation in patients who are applying sunscreen regularly (Bogaczewicz et al).
Next page: Sunscreen compliance
What is the most often heard reason(s) for not using sunscreen in your patients?
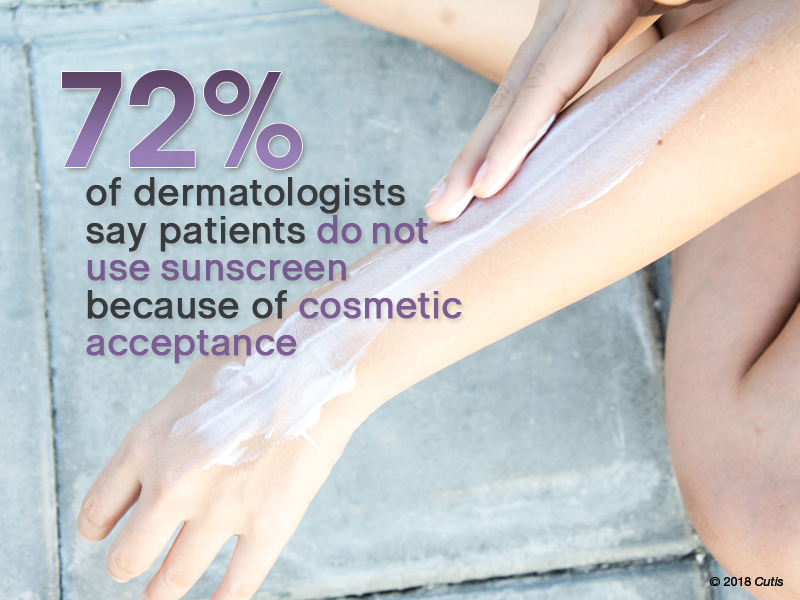
Nearly three-quarters (72%) of dermatologists reported that patients do not use sunscreen because of cosmetic acceptance. Almost one-third (31%) said their patients prefer “natural” products. Price was a factor for 26%. Fewer dermatologists indicated risk of environmental damage (14%), allergy (12%), cancer induction (5%), and hormonal alteration (5%) were reasons patients are not compliant.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Cosmetic acceptance is paramount for patient compliance for sunscreen application. These results from our Editorial Board echo a study on sunscreen product performance and other determinants of consumer preferences, which cited “cosmetic elegance” as an important factor in choosing sunscreens (Xu et al). Dermatologists must stress to patients to find a sunscreen that they find acceptable in terms of vehicle and price to increase compliance.
Next page: Sunscreens in pregnant women
What sunscreens do you recommend to pregnant women and children?

Most dermatologists (86%) recommend physical blockers “chemical-free” only sunscreens to pregnant women and children.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
While absorption of sunscreen by human embryos is likely negligible, because there is limited data on sunscreen effects in embryos and children, it is reasonable to recommend physical blockers for pregnant women and children.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As a dermatologist married to a pediatrician, I try to get my kids to embrace sun-protection strategies. For the little ones it’s hard, but as they have gotten older and been exposed to more derm journals sitting around with pretty graphic pictures, they seem to get on board, even when away at summer camp on their own. If only our patients knew what our kids do.—Joel L. Cohen, MD (Denver, Colorado)
The most important factor in getting patient compliance with sunscreen usage is “cosmetic acceptance.” If they or their children or their spouse don’t like the feel, they won’t use it.—Vincent A. DeLeo, MD (Los Angeles, California)
Not using photoprotection with sunscreen is like crossing a busy road without looking both ways first.—James Q. Del Rosso, DO (Las Vegas, Nevada)
I do not recommend spray sunscreens. At least half of the spray seems to go in the air rather than on the skin. And people often do not rub the spray into their skin well enough. Lotions are better!—Lawrence J. Green, MD (Washington, DC)
The most important factor in sunscreen is not SPF; educate patients on the important role vehicle and sweating play in the length of sun protection.—Orit Markowitz, MD (New York, New York)
Reapplying sunscreen in the appropriate amount is key to blocking the danger rays of the sun.—Vineet Mishra, MD (San Antonio, Texas)
A good sunscreen is the one you put on properly. Regardless of the formulation, make sure you apply the sunscreen evenly to all exposed skin and reapply according to directions on the container. Remember, a regular white T-shirt has minimal SPF 4-5. Either wear sun-protective clothing or wear sunscreen underneath!—Larisa Ravitskiy, MD (Gahanna, Ohio)
Sun protection and sunscreen application go hand-in-hand. We can still enjoy the outdoors without getting excessive UV exposure.—Anthony M. Rossi, MD (New York, New York)
Sunscreens are only part of sun protection. Make sure to reapply them regularly, try to avoid direct sun between about 10 AM and 2 PM if possible, and wear a hat with a wide brim (not a baseball cap, which, after all, is designed for catching baseballs, not sun protection).—Robert I. Rudolph, MD (Wyomissing, Pennsylvania)
Sunscreens keep you younger looking longer!—Richard K. Scher, MD (New York, New York)
The dentist says only floss the teeth you want to keep. I tell patients to only sun block the skin they want to keep.—Daniel M. Siegel, MD, MS (Brooklyn, New York)
The best sunscreen is the one that is used! If it's too greasy or drying, smells bad or stings, it won't be used. Stick to the one YOU like, but at least SPF 30 or better.—Stephen P. Stone, MD, (Springfield, Illinois)
Sunscreen can be a meaningful part of your sun-protection regimen used in conjunction with sun-protective clothing, sun safe behaviors, and a diet rich in natural antioxidants.—Michelle Tarbox, MD (Lubbock, Texas)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from August 2, 2018, to September 2, 2018. A total of 42 usable responses were received.
Bogaczewicz J, Karczmarewicz E, Pludowski P, et al. Requirement for vitamin D supplementation in patients using photoprotection: variations in vitamin D levels and bone formation markers. Int J Dermatol. 2016;55:e176-e183.
Farberg AS, Glazer AM, Rigel AC, et al. Dermatologists’ perceptions, recommendations, and use of sunscreen. JAMA Dermatol. 2017;153:99-101.
Ou-Yang H, Stanfield J, Cole C, et al. High-SPF sunscreens (SPF ≥ 70) may provide ultraviolet protection above minimal recommended levels by adequately compensating for lower sunscreen user application amounts. J Am Acad Dermatol. 2012;67:1220-1227.
Teplitz RW, Glazer AM, Svoboda RM, et al. Trends in US sunscreen formulations: impact of increasing spray usage. J Am Acad Dermatol. 2018;78:187-189.
Williams JD, Maitra P, Atillasoy E, et al. SPF 100+ sunscreen is more protective against sunburn than SPF 50+ in actual use: Results of a randomized, double-blind, split-face, natural sunlight exposure clinical trial. J Am Acad Dermatol. 2018;78:902.e2-910.e2.
Xu S, Kwa M, Agarwal A, et al. Sunscreen product performance and other determinants of consumer preferences. JAMA Dermatol. 2016;152:920-927.
Bogaczewicz J, Karczmarewicz E, Pludowski P, et al. Requirement for vitamin D supplementation in patients using photoprotection: variations in vitamin D levels and bone formation markers. Int J Dermatol. 2016;55:e176-e183.
Farberg AS, Glazer AM, Rigel AC, et al. Dermatologists’ perceptions, recommendations, and use of sunscreen. JAMA Dermatol. 2017;153:99-101.
Ou-Yang H, Stanfield J, Cole C, et al. High-SPF sunscreens (SPF ≥ 70) may provide ultraviolet protection above minimal recommended levels by adequately compensating for lower sunscreen user application amounts. J Am Acad Dermatol. 2012;67:1220-1227.
Teplitz RW, Glazer AM, Svoboda RM, et al. Trends in US sunscreen formulations: impact of increasing spray usage. J Am Acad Dermatol. 2018;78:187-189.
Williams JD, Maitra P, Atillasoy E, et al. SPF 100+ sunscreen is more protective against sunburn than SPF 50+ in actual use: Results of a randomized, double-blind, split-face, natural sunlight exposure clinical trial. J Am Acad Dermatol. 2018;78:902.e2-910.e2.
Xu S, Kwa M, Agarwal A, et al. Sunscreen product performance and other determinants of consumer preferences. JAMA Dermatol. 2016;152:920-927.
Cosmetic Corner: Dermatologists Weigh in on Bar Soaps
To improve patient care and outcomes, leading dermatologists offered their recommendations on bar soaps. Consideration must be given to:
- Avène Cold Cream Ultra-Rich Cleansing Bar
Pierre Fabre Dermo-Cosmetique USA
“This gentle cleansing bar is not only hypoallergenic, soap free, and lanolin free, it also has Avène’s soothing Thermal Spring Water, plus white beeswax and a noncomedogenic, pharmaceutical-grade paraffin oil to protect the skin.”—Jeannette Graf, MD, Great Neck, New York
- Hydrating Cleanser Bar
CeraVe
Recommended by Shari Lipner, MD, PhD, New York, New York
- Vanicream Cleansing Bar
Pharmaceutical Specialties, Inc
“This is a great option for patients with eczema or dry, sensitive skin.”—Gary Goldenberg, MD, New York, New York
Cutis invites readers to send us their recommendations. Lip plumpers, shaving lotions for men, and night creams will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to the Editorial Office.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on bar soaps. Consideration must be given to:
- Avène Cold Cream Ultra-Rich Cleansing Bar
Pierre Fabre Dermo-Cosmetique USA
“This gentle cleansing bar is not only hypoallergenic, soap free, and lanolin free, it also has Avène’s soothing Thermal Spring Water, plus white beeswax and a noncomedogenic, pharmaceutical-grade paraffin oil to protect the skin.”—Jeannette Graf, MD, Great Neck, New York
- Hydrating Cleanser Bar
CeraVe
Recommended by Shari Lipner, MD, PhD, New York, New York
- Vanicream Cleansing Bar
Pharmaceutical Specialties, Inc
“This is a great option for patients with eczema or dry, sensitive skin.”—Gary Goldenberg, MD, New York, New York
Cutis invites readers to send us their recommendations. Lip plumpers, shaving lotions for men, and night creams will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to the Editorial Office.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on bar soaps. Consideration must be given to:
- Avène Cold Cream Ultra-Rich Cleansing Bar
Pierre Fabre Dermo-Cosmetique USA
“This gentle cleansing bar is not only hypoallergenic, soap free, and lanolin free, it also has Avène’s soothing Thermal Spring Water, plus white beeswax and a noncomedogenic, pharmaceutical-grade paraffin oil to protect the skin.”—Jeannette Graf, MD, Great Neck, New York
- Hydrating Cleanser Bar
CeraVe
Recommended by Shari Lipner, MD, PhD, New York, New York
- Vanicream Cleansing Bar
Pharmaceutical Specialties, Inc
“This is a great option for patients with eczema or dry, sensitive skin.”—Gary Goldenberg, MD, New York, New York
Cutis invites readers to send us their recommendations. Lip plumpers, shaving lotions for men, and night creams will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to the Editorial Office.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Cosmetic Corner: Dermatologists Weigh in on Pigment Correctors
To improve patient care and outcomes, leading dermatologists offered their recommendations on pigment correctors. Consideration must be given to:
- dEp Patch Full Face Mask
Activaderm, Inc
“This product uses microcurrent to push vitamin C into the skin. Vitamin C, a known antioxidant that usually has a difficult time passing through the stratum corneum, corrects pigmentary abnormalities. The product also comes with a botanical pigment corrector.”—Gary Goldenberg, MD, New York, New York
- De-Spot Skin Brightening Corrector
Peter Thomas Roth Labs LLC
“This product is a useful over-the-counter adjunct to prescription-strength hydroquinone, with niacinamide as one of the active ingredients.”—Shari Lipner, MD, PhD, New York, New York
- Glytone Dark Spot Corrector
Pierre Fabre Laboratories
“With 2% hydroquinone, glycolic acid, and kojic acid, you have a highly effective combination of ingredients that work synergistically to lighten areas of skin discoloration.”—Jeannette Graf, MD, Great Neck, New York
Cutis invites readers to send us their recommendations. Bar soap, lip plumper, and night cream will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to the Editorial Office.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on pigment correctors. Consideration must be given to:
- dEp Patch Full Face Mask
Activaderm, Inc
“This product uses microcurrent to push vitamin C into the skin. Vitamin C, a known antioxidant that usually has a difficult time passing through the stratum corneum, corrects pigmentary abnormalities. The product also comes with a botanical pigment corrector.”—Gary Goldenberg, MD, New York, New York
- De-Spot Skin Brightening Corrector
Peter Thomas Roth Labs LLC
“This product is a useful over-the-counter adjunct to prescription-strength hydroquinone, with niacinamide as one of the active ingredients.”—Shari Lipner, MD, PhD, New York, New York
- Glytone Dark Spot Corrector
Pierre Fabre Laboratories
“With 2% hydroquinone, glycolic acid, and kojic acid, you have a highly effective combination of ingredients that work synergistically to lighten areas of skin discoloration.”—Jeannette Graf, MD, Great Neck, New York
Cutis invites readers to send us their recommendations. Bar soap, lip plumper, and night cream will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to the Editorial Office.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on pigment correctors. Consideration must be given to:
- dEp Patch Full Face Mask
Activaderm, Inc
“This product uses microcurrent to push vitamin C into the skin. Vitamin C, a known antioxidant that usually has a difficult time passing through the stratum corneum, corrects pigmentary abnormalities. The product also comes with a botanical pigment corrector.”—Gary Goldenberg, MD, New York, New York
- De-Spot Skin Brightening Corrector
Peter Thomas Roth Labs LLC
“This product is a useful over-the-counter adjunct to prescription-strength hydroquinone, with niacinamide as one of the active ingredients.”—Shari Lipner, MD, PhD, New York, New York
- Glytone Dark Spot Corrector
Pierre Fabre Laboratories
“With 2% hydroquinone, glycolic acid, and kojic acid, you have a highly effective combination of ingredients that work synergistically to lighten areas of skin discoloration.”—Jeannette Graf, MD, Great Neck, New York
Cutis invites readers to send us their recommendations. Bar soap, lip plumper, and night cream will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to the Editorial Office.
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc. and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc. endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.



