User login
Stent-retriever Therapy Improves the Rate of Functional Independence for Acute Ischemic Patients
NEW YORK (Reuters Health) - Stent-retriever therapy for the treatment of acute ischemic stroke improves the rate of functional independence at 90 days, according to a systematic
review and meta-analysis.
Stent retrievers are deployed in an occluded vessel, temporarily expanded into the body of a thrombus, and then retracted along with the thrombus.
Dr. Mark J. Eisenberg, from Jewish General Hospital/McGill University, Montreal, Quebec, Canada, and colleagues compared stent retrievers with intravenous recombinant tissue plasminogen activator (rtPA) versus rtPA alone for the treatment of acute ischemic stroke in their systematic review and meta-analysis of five randomized controlled trials (RCTs) with a total of 1,287 patients.
In all five trials, patients randomized to stent-retriever therapy had significantly better functional independence (a modified Rankin Scale (mRS) score of 0-2) at 90 days than did patients randomized to rtPA alone.
Stent-retriever therapy also doubled the likelihood of a one-unit improvement in mRS score at 90 days, according to the January 25 JAMA Neurology online report.
In pooled analyses, there were no significant differences between treatment groups in all-cause mortality, intracranial hemorrhage, or parenchymal hematoma rates at 90 days.
The number needed to treat to achieve an mRS score of 0 to 2 at 90 days was six.
"Given the totality of the evidence regarding the benefits and risks of stent retrievers, our results suggest that the use of these devices in patients with acute ischemic stroke is warranted," the researchers conclude.
Dr. Raphael A. Carandang, from the University of Massachusetts Medical School, Worcester, who wrote an editorial related to this report, told Reuters Health by email, "The data from these five RCTs (as the meta-analysis confirms) provides level 1 class A evidence that in the properly selected patients, stent retriever treatment is superior to the current standard of care with intravenous rtPA and would endorse that it should be considered in all acute ischemic stroke patients that are eligible for it. As with any therapy, proper patient selection is needed, but I do think it changes the landscape of acute stroke treatment going forward. I think that systems of care should be organized in stroke centers around this new therapy."
"The current technology for acute stroke care has reached the point where effective interventional therapies are clearly and unequivocally beneficial in the properly selected patients, but the key takeaway is still that the patients need to be selected properly, and the biggest factor continues to be time to recanalization, which means that all practitioners and systems of care need to focus on getting patients to treatment sooner than ever before," Dr. Carandang concluded.
Dr. Woong Yoon, from Chonnam National University Hospital, Gwangju, Korea, recently found no improvement in outcomes with stent-retriever therapy for patients with acute anterior circulation stroke (http://bit.ly/1OT7M5I). He told Reuters Health by email, "Not all patients with acute ischemic stroke can benefit from this new treatment. Patients with acute stroke due to occlusions of intracranial large vessels such as internal carotid artery, middle cerebral artery, or basilar artery and who presented within six-eight hours of stroke onset can benefit from thrombectomy with stent retrievers."
"We should realize that we are facing the moment of change in the paradigm for acute stroke treatment," Dr. Yoon concluded."Further refinement in the patient selection for stent retrieverthrombectomy is needed in the near future."
Dr. Mayank Goyal, from the University of Calgary, Alberta, Canada, coauthored two of the studies included in the current review. He told Reuters Health by email," There are several additional data coming out on this issue in the near future, which will in fact be more powerful than what is mentioned in this study."
Dr. Goyal said, "However, the key issues going into the future are: how should those patients who were not included in the current trials be treated; how should we as a collective evaluate new devices/technologies; and how do societies/countries who cannot afford stent retrievers implement endovascular stroke treatment."
Dr. Eisenberg was unavailable for comment.
The authors reported no funding. Three coauthors reported disclosures.
NEW YORK (Reuters Health) - Stent-retriever therapy for the treatment of acute ischemic stroke improves the rate of functional independence at 90 days, according to a systematic
review and meta-analysis.
Stent retrievers are deployed in an occluded vessel, temporarily expanded into the body of a thrombus, and then retracted along with the thrombus.
Dr. Mark J. Eisenberg, from Jewish General Hospital/McGill University, Montreal, Quebec, Canada, and colleagues compared stent retrievers with intravenous recombinant tissue plasminogen activator (rtPA) versus rtPA alone for the treatment of acute ischemic stroke in their systematic review and meta-analysis of five randomized controlled trials (RCTs) with a total of 1,287 patients.
In all five trials, patients randomized to stent-retriever therapy had significantly better functional independence (a modified Rankin Scale (mRS) score of 0-2) at 90 days than did patients randomized to rtPA alone.
Stent-retriever therapy also doubled the likelihood of a one-unit improvement in mRS score at 90 days, according to the January 25 JAMA Neurology online report.
In pooled analyses, there were no significant differences between treatment groups in all-cause mortality, intracranial hemorrhage, or parenchymal hematoma rates at 90 days.
The number needed to treat to achieve an mRS score of 0 to 2 at 90 days was six.
"Given the totality of the evidence regarding the benefits and risks of stent retrievers, our results suggest that the use of these devices in patients with acute ischemic stroke is warranted," the researchers conclude.
Dr. Raphael A. Carandang, from the University of Massachusetts Medical School, Worcester, who wrote an editorial related to this report, told Reuters Health by email, "The data from these five RCTs (as the meta-analysis confirms) provides level 1 class A evidence that in the properly selected patients, stent retriever treatment is superior to the current standard of care with intravenous rtPA and would endorse that it should be considered in all acute ischemic stroke patients that are eligible for it. As with any therapy, proper patient selection is needed, but I do think it changes the landscape of acute stroke treatment going forward. I think that systems of care should be organized in stroke centers around this new therapy."
"The current technology for acute stroke care has reached the point where effective interventional therapies are clearly and unequivocally beneficial in the properly selected patients, but the key takeaway is still that the patients need to be selected properly, and the biggest factor continues to be time to recanalization, which means that all practitioners and systems of care need to focus on getting patients to treatment sooner than ever before," Dr. Carandang concluded.
Dr. Woong Yoon, from Chonnam National University Hospital, Gwangju, Korea, recently found no improvement in outcomes with stent-retriever therapy for patients with acute anterior circulation stroke (http://bit.ly/1OT7M5I). He told Reuters Health by email, "Not all patients with acute ischemic stroke can benefit from this new treatment. Patients with acute stroke due to occlusions of intracranial large vessels such as internal carotid artery, middle cerebral artery, or basilar artery and who presented within six-eight hours of stroke onset can benefit from thrombectomy with stent retrievers."
"We should realize that we are facing the moment of change in the paradigm for acute stroke treatment," Dr. Yoon concluded."Further refinement in the patient selection for stent retrieverthrombectomy is needed in the near future."
Dr. Mayank Goyal, from the University of Calgary, Alberta, Canada, coauthored two of the studies included in the current review. He told Reuters Health by email," There are several additional data coming out on this issue in the near future, which will in fact be more powerful than what is mentioned in this study."
Dr. Goyal said, "However, the key issues going into the future are: how should those patients who were not included in the current trials be treated; how should we as a collective evaluate new devices/technologies; and how do societies/countries who cannot afford stent retrievers implement endovascular stroke treatment."
Dr. Eisenberg was unavailable for comment.
The authors reported no funding. Three coauthors reported disclosures.
NEW YORK (Reuters Health) - Stent-retriever therapy for the treatment of acute ischemic stroke improves the rate of functional independence at 90 days, according to a systematic
review and meta-analysis.
Stent retrievers are deployed in an occluded vessel, temporarily expanded into the body of a thrombus, and then retracted along with the thrombus.
Dr. Mark J. Eisenberg, from Jewish General Hospital/McGill University, Montreal, Quebec, Canada, and colleagues compared stent retrievers with intravenous recombinant tissue plasminogen activator (rtPA) versus rtPA alone for the treatment of acute ischemic stroke in their systematic review and meta-analysis of five randomized controlled trials (RCTs) with a total of 1,287 patients.
In all five trials, patients randomized to stent-retriever therapy had significantly better functional independence (a modified Rankin Scale (mRS) score of 0-2) at 90 days than did patients randomized to rtPA alone.
Stent-retriever therapy also doubled the likelihood of a one-unit improvement in mRS score at 90 days, according to the January 25 JAMA Neurology online report.
In pooled analyses, there were no significant differences between treatment groups in all-cause mortality, intracranial hemorrhage, or parenchymal hematoma rates at 90 days.
The number needed to treat to achieve an mRS score of 0 to 2 at 90 days was six.
"Given the totality of the evidence regarding the benefits and risks of stent retrievers, our results suggest that the use of these devices in patients with acute ischemic stroke is warranted," the researchers conclude.
Dr. Raphael A. Carandang, from the University of Massachusetts Medical School, Worcester, who wrote an editorial related to this report, told Reuters Health by email, "The data from these five RCTs (as the meta-analysis confirms) provides level 1 class A evidence that in the properly selected patients, stent retriever treatment is superior to the current standard of care with intravenous rtPA and would endorse that it should be considered in all acute ischemic stroke patients that are eligible for it. As with any therapy, proper patient selection is needed, but I do think it changes the landscape of acute stroke treatment going forward. I think that systems of care should be organized in stroke centers around this new therapy."
"The current technology for acute stroke care has reached the point where effective interventional therapies are clearly and unequivocally beneficial in the properly selected patients, but the key takeaway is still that the patients need to be selected properly, and the biggest factor continues to be time to recanalization, which means that all practitioners and systems of care need to focus on getting patients to treatment sooner than ever before," Dr. Carandang concluded.
Dr. Woong Yoon, from Chonnam National University Hospital, Gwangju, Korea, recently found no improvement in outcomes with stent-retriever therapy for patients with acute anterior circulation stroke (http://bit.ly/1OT7M5I). He told Reuters Health by email, "Not all patients with acute ischemic stroke can benefit from this new treatment. Patients with acute stroke due to occlusions of intracranial large vessels such as internal carotid artery, middle cerebral artery, or basilar artery and who presented within six-eight hours of stroke onset can benefit from thrombectomy with stent retrievers."
"We should realize that we are facing the moment of change in the paradigm for acute stroke treatment," Dr. Yoon concluded."Further refinement in the patient selection for stent retrieverthrombectomy is needed in the near future."
Dr. Mayank Goyal, from the University of Calgary, Alberta, Canada, coauthored two of the studies included in the current review. He told Reuters Health by email," There are several additional data coming out on this issue in the near future, which will in fact be more powerful than what is mentioned in this study."
Dr. Goyal said, "However, the key issues going into the future are: how should those patients who were not included in the current trials be treated; how should we as a collective evaluate new devices/technologies; and how do societies/countries who cannot afford stent retrievers implement endovascular stroke treatment."
Dr. Eisenberg was unavailable for comment.
The authors reported no funding. Three coauthors reported disclosures.
99% of Medical-Device Monitoring Alerts Not Actionable
Nearly all medical-device monitoring alerts on regular hospital units were found not to be actionable, according to a study by pediatrician and researcher Chris Bonafide, MD, MSCE, at Children’s Hospital of Philadelphia, based on reviewing hours of video from patient rooms.1
Reference
- Bonafide CP, Lin R, Zander M, et al. Association between exposure to nonactionable physiologic monitor alarms and response time in a children’s hospital. J Hosp Med. 2015; 10(6):345–351.
Nearly all medical-device monitoring alerts on regular hospital units were found not to be actionable, according to a study by pediatrician and researcher Chris Bonafide, MD, MSCE, at Children’s Hospital of Philadelphia, based on reviewing hours of video from patient rooms.1
Reference
- Bonafide CP, Lin R, Zander M, et al. Association between exposure to nonactionable physiologic monitor alarms and response time in a children’s hospital. J Hosp Med. 2015; 10(6):345–351.
Nearly all medical-device monitoring alerts on regular hospital units were found not to be actionable, according to a study by pediatrician and researcher Chris Bonafide, MD, MSCE, at Children’s Hospital of Philadelphia, based on reviewing hours of video from patient rooms.1
Reference
- Bonafide CP, Lin R, Zander M, et al. Association between exposure to nonactionable physiologic monitor alarms and response time in a children’s hospital. J Hosp Med. 2015; 10(6):345–351.
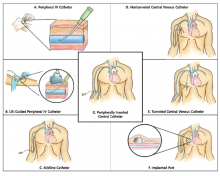
Guide Helps Hospitalists Choose Most Appropriate Catheter for Patients
The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC) is a new resource designed to help clinicians select the safest and most appropriate peripherally inserted central catheter (PICC) for individual patients.
“How do you decide which catheter is best for your patient? Until now there wasn’t a guide bringing together all of the best available evidence,” says the guide’s lead author Vineet Chopra, MD, MSc, FHM, a hospitalist and assistant professor of medicine at the University of Michigan in Ann Arbor.
“These are among the most commonly performed procedures on any hospitalized patient, and yet, the least studied,” he adds. “We as hospitalists are the physicians who order most of these devices, especially PICCs.”
The guide includes algorithms and color-coded pocket cards to help physicians determine which PICC to choose. The cards can be freely downloaded and printed from the Improve PICC website at the University of Michigan.
The project to develop the guide brought together 15 leading international experts on catheters and their infections and complications, including the authors of existing guidelines, to brainstorm more than 600 clinical scenarios and best evidence-based practice for catheter use using the Rand/UCLA Appropriateness Method. “We also had a patient on the panel, which was important to the clinicians because this patient had actually used many of the devices being discussed,” Dr. Chopra explains.
The guidelines “have the potential to change the game for hospitalists,” Dr. Chopra adds. “There has never before been guidance on using IV devices in hospitalized medical patients, despite the fact that we use these devices every day. Now, for the first time, we not only have guidance but also a tool to benchmark the quality of care provided by doctors when it comes to venous access.”
The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC) is a new resource designed to help clinicians select the safest and most appropriate peripherally inserted central catheter (PICC) for individual patients.
“How do you decide which catheter is best for your patient? Until now there wasn’t a guide bringing together all of the best available evidence,” says the guide’s lead author Vineet Chopra, MD, MSc, FHM, a hospitalist and assistant professor of medicine at the University of Michigan in Ann Arbor.
“These are among the most commonly performed procedures on any hospitalized patient, and yet, the least studied,” he adds. “We as hospitalists are the physicians who order most of these devices, especially PICCs.”
The guide includes algorithms and color-coded pocket cards to help physicians determine which PICC to choose. The cards can be freely downloaded and printed from the Improve PICC website at the University of Michigan.
The project to develop the guide brought together 15 leading international experts on catheters and their infections and complications, including the authors of existing guidelines, to brainstorm more than 600 clinical scenarios and best evidence-based practice for catheter use using the Rand/UCLA Appropriateness Method. “We also had a patient on the panel, which was important to the clinicians because this patient had actually used many of the devices being discussed,” Dr. Chopra explains.
The guidelines “have the potential to change the game for hospitalists,” Dr. Chopra adds. “There has never before been guidance on using IV devices in hospitalized medical patients, despite the fact that we use these devices every day. Now, for the first time, we not only have guidance but also a tool to benchmark the quality of care provided by doctors when it comes to venous access.”
The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC) is a new resource designed to help clinicians select the safest and most appropriate peripherally inserted central catheter (PICC) for individual patients.
“How do you decide which catheter is best for your patient? Until now there wasn’t a guide bringing together all of the best available evidence,” says the guide’s lead author Vineet Chopra, MD, MSc, FHM, a hospitalist and assistant professor of medicine at the University of Michigan in Ann Arbor.
“These are among the most commonly performed procedures on any hospitalized patient, and yet, the least studied,” he adds. “We as hospitalists are the physicians who order most of these devices, especially PICCs.”
The guide includes algorithms and color-coded pocket cards to help physicians determine which PICC to choose. The cards can be freely downloaded and printed from the Improve PICC website at the University of Michigan.
The project to develop the guide brought together 15 leading international experts on catheters and their infections and complications, including the authors of existing guidelines, to brainstorm more than 600 clinical scenarios and best evidence-based practice for catheter use using the Rand/UCLA Appropriateness Method. “We also had a patient on the panel, which was important to the clinicians because this patient had actually used many of the devices being discussed,” Dr. Chopra explains.
The guidelines “have the potential to change the game for hospitalists,” Dr. Chopra adds. “There has never before been guidance on using IV devices in hospitalized medical patients, despite the fact that we use these devices every day. Now, for the first time, we not only have guidance but also a tool to benchmark the quality of care provided by doctors when it comes to venous access.”
Institute of Medicine Report Examines Medical Misdiagnoses
Authors of the IOM’s “Improving Diagnosis in Health Care” report cite problems in communication and limitations in electronic health records behind inaccurate and delayed diagnoses, concluding that the problem of diagnostic errors generally has not been adequately studied.1
“This problem is significant and serious. Yet we don’t know for sure how often it occurs, how serious it is, or how much it costs,” said the IOM committee’s chair, John Ball, MD, of the American College of Physicians, in a prepared statement. The report concludes there is no easy fix for the problem of diagnostic errors, which are a leading cause of adverse events in hospitals and of malpractice lawsuits for hospitalists, but calls for a major reassessment of the diagnostic process.2
Hospitalist Mangla Gulati, MD, FACP, SFHM, assistant chief medical officer at the University of Maryland Medical Center in Baltimore, says hospitalists would be remiss if they failed to take a closer look at the IOM report. “Diagnostic error is something we haven’t much talked about in medicine,” Dr. Gulati says. “Part of the goal of this report is to actually include the patient in those conversations.” Patients who are rehospitalized, she says, may have been given an incorrect initial diagnosis that was never rectified, or there may have been a failure to communicate important information.
“How many tests do we order where results come back after a patient leaves the hospital?” asks Kedar Mate, MD, senior vice president at the Institute for Healthcare Improvement and a hospitalist at Weill Cornell Medicine in New York City. “How many in-hospital diagnoses are made without all of the available information from outside providers?”
One simple intervention hospitalists could do immediately, he says, is to start tracking all important tests ordered for patients on a board in the medical team’s meeting room, only removing them from the board when results have been checked and communicated to the patient and outpatient provider.
References
- National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press. 2015.
- Saber Tehrani AS, Lee HW, Mathews SC, et al. 25-year summary of U.S. malpractice claims for diagnostic errors 1986–2010: An analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013 Aug; 22(8):672–680.
Authors of the IOM’s “Improving Diagnosis in Health Care” report cite problems in communication and limitations in electronic health records behind inaccurate and delayed diagnoses, concluding that the problem of diagnostic errors generally has not been adequately studied.1
“This problem is significant and serious. Yet we don’t know for sure how often it occurs, how serious it is, or how much it costs,” said the IOM committee’s chair, John Ball, MD, of the American College of Physicians, in a prepared statement. The report concludes there is no easy fix for the problem of diagnostic errors, which are a leading cause of adverse events in hospitals and of malpractice lawsuits for hospitalists, but calls for a major reassessment of the diagnostic process.2
Hospitalist Mangla Gulati, MD, FACP, SFHM, assistant chief medical officer at the University of Maryland Medical Center in Baltimore, says hospitalists would be remiss if they failed to take a closer look at the IOM report. “Diagnostic error is something we haven’t much talked about in medicine,” Dr. Gulati says. “Part of the goal of this report is to actually include the patient in those conversations.” Patients who are rehospitalized, she says, may have been given an incorrect initial diagnosis that was never rectified, or there may have been a failure to communicate important information.
“How many tests do we order where results come back after a patient leaves the hospital?” asks Kedar Mate, MD, senior vice president at the Institute for Healthcare Improvement and a hospitalist at Weill Cornell Medicine in New York City. “How many in-hospital diagnoses are made without all of the available information from outside providers?”
One simple intervention hospitalists could do immediately, he says, is to start tracking all important tests ordered for patients on a board in the medical team’s meeting room, only removing them from the board when results have been checked and communicated to the patient and outpatient provider.
References
- National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press. 2015.
- Saber Tehrani AS, Lee HW, Mathews SC, et al. 25-year summary of U.S. malpractice claims for diagnostic errors 1986–2010: An analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013 Aug; 22(8):672–680.
Authors of the IOM’s “Improving Diagnosis in Health Care” report cite problems in communication and limitations in electronic health records behind inaccurate and delayed diagnoses, concluding that the problem of diagnostic errors generally has not been adequately studied.1
“This problem is significant and serious. Yet we don’t know for sure how often it occurs, how serious it is, or how much it costs,” said the IOM committee’s chair, John Ball, MD, of the American College of Physicians, in a prepared statement. The report concludes there is no easy fix for the problem of diagnostic errors, which are a leading cause of adverse events in hospitals and of malpractice lawsuits for hospitalists, but calls for a major reassessment of the diagnostic process.2
Hospitalist Mangla Gulati, MD, FACP, SFHM, assistant chief medical officer at the University of Maryland Medical Center in Baltimore, says hospitalists would be remiss if they failed to take a closer look at the IOM report. “Diagnostic error is something we haven’t much talked about in medicine,” Dr. Gulati says. “Part of the goal of this report is to actually include the patient in those conversations.” Patients who are rehospitalized, she says, may have been given an incorrect initial diagnosis that was never rectified, or there may have been a failure to communicate important information.
“How many tests do we order where results come back after a patient leaves the hospital?” asks Kedar Mate, MD, senior vice president at the Institute for Healthcare Improvement and a hospitalist at Weill Cornell Medicine in New York City. “How many in-hospital diagnoses are made without all of the available information from outside providers?”
One simple intervention hospitalists could do immediately, he says, is to start tracking all important tests ordered for patients on a board in the medical team’s meeting room, only removing them from the board when results have been checked and communicated to the patient and outpatient provider.
References
- National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press. 2015.
- Saber Tehrani AS, Lee HW, Mathews SC, et al. 25-year summary of U.S. malpractice claims for diagnostic errors 1986–2010: An analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013 Aug; 22(8):672–680.
Quality Improvement Initiative Targets Sepsis
A quality improvement (QI) initiative at University Hospital in Salt Lake City aims to save lives and cut hospital costs by reducing inpatient sepsis mortality.
Program co-leaders, hospitalists Devin Horton, MD, and Kencee Graves, MD, of University Hospital, launched the initiative as a pilot program last October. They began by surveying hospital house staff and nurses on their ability to recognize and define six different sepsis syndromes from clinical vignettes. A total of 136 surveyed residents recognized the correct condition only 56% of the time, and 280 surveyed nurses only did so 17% of the time. The hospitalists determined that better education about sepsis was crucial.
“We developed a robust teaching program for nurses and residents using Septris, an online educational game from Stanford University,” Dr. Horton says. The team also developed technology that can recognize worsening vital signs in a patient and automatically trigger an alert to a charge nurse or rapid response team.
The team’s Modified Early Warning System (MEWS) for recognizing sepsis is similar to the Early Warning and Response System (EWRS) system used at the University of Pennsylvania Health System and the University of California San Diego, and draws on other hospitals’ sepsis systems. Dr. Horton says one difference in their system is the involvement of nursing aides who take vital signs, enter them real-time into electronic health records (EHR), and receive prompts from abnormal vital signs to retake all vitals and confirm abnormal results. It also incorporates EHR decision support tools, including links to pre-populated medical order panels, such as for the ordering of tests for lactate and blood cultures.
“Severe sepsis is often quoted as the number one cause of mortality among hospitalized patients, with a rate up to 10 times that of acute myocardial infarction,” Dr. Horton explains. “The one treatment that consistently decreases mortality is timely administration of antibiotics. But, in order for a patient to be given timely antibiotics, the nurse or resident must first recognize that the patient has sepsis.”
“This is one of the biggest and most far-reaching improvement initiatives that has been done at our institution,” says Robert Pendleton, MD, chief quality officer at University Hospital. Dr. Horton says he predicts the program will “save 50 lives and $1 million per year.”
For more information, contact him at: devin.horton@hsc.utah.edu.
A quality improvement (QI) initiative at University Hospital in Salt Lake City aims to save lives and cut hospital costs by reducing inpatient sepsis mortality.
Program co-leaders, hospitalists Devin Horton, MD, and Kencee Graves, MD, of University Hospital, launched the initiative as a pilot program last October. They began by surveying hospital house staff and nurses on their ability to recognize and define six different sepsis syndromes from clinical vignettes. A total of 136 surveyed residents recognized the correct condition only 56% of the time, and 280 surveyed nurses only did so 17% of the time. The hospitalists determined that better education about sepsis was crucial.
“We developed a robust teaching program for nurses and residents using Septris, an online educational game from Stanford University,” Dr. Horton says. The team also developed technology that can recognize worsening vital signs in a patient and automatically trigger an alert to a charge nurse or rapid response team.
The team’s Modified Early Warning System (MEWS) for recognizing sepsis is similar to the Early Warning and Response System (EWRS) system used at the University of Pennsylvania Health System and the University of California San Diego, and draws on other hospitals’ sepsis systems. Dr. Horton says one difference in their system is the involvement of nursing aides who take vital signs, enter them real-time into electronic health records (EHR), and receive prompts from abnormal vital signs to retake all vitals and confirm abnormal results. It also incorporates EHR decision support tools, including links to pre-populated medical order panels, such as for the ordering of tests for lactate and blood cultures.
“Severe sepsis is often quoted as the number one cause of mortality among hospitalized patients, with a rate up to 10 times that of acute myocardial infarction,” Dr. Horton explains. “The one treatment that consistently decreases mortality is timely administration of antibiotics. But, in order for a patient to be given timely antibiotics, the nurse or resident must first recognize that the patient has sepsis.”
“This is one of the biggest and most far-reaching improvement initiatives that has been done at our institution,” says Robert Pendleton, MD, chief quality officer at University Hospital. Dr. Horton says he predicts the program will “save 50 lives and $1 million per year.”
For more information, contact him at: devin.horton@hsc.utah.edu.
A quality improvement (QI) initiative at University Hospital in Salt Lake City aims to save lives and cut hospital costs by reducing inpatient sepsis mortality.
Program co-leaders, hospitalists Devin Horton, MD, and Kencee Graves, MD, of University Hospital, launched the initiative as a pilot program last October. They began by surveying hospital house staff and nurses on their ability to recognize and define six different sepsis syndromes from clinical vignettes. A total of 136 surveyed residents recognized the correct condition only 56% of the time, and 280 surveyed nurses only did so 17% of the time. The hospitalists determined that better education about sepsis was crucial.
“We developed a robust teaching program for nurses and residents using Septris, an online educational game from Stanford University,” Dr. Horton says. The team also developed technology that can recognize worsening vital signs in a patient and automatically trigger an alert to a charge nurse or rapid response team.
The team’s Modified Early Warning System (MEWS) for recognizing sepsis is similar to the Early Warning and Response System (EWRS) system used at the University of Pennsylvania Health System and the University of California San Diego, and draws on other hospitals’ sepsis systems. Dr. Horton says one difference in their system is the involvement of nursing aides who take vital signs, enter them real-time into electronic health records (EHR), and receive prompts from abnormal vital signs to retake all vitals and confirm abnormal results. It also incorporates EHR decision support tools, including links to pre-populated medical order panels, such as for the ordering of tests for lactate and blood cultures.
“Severe sepsis is often quoted as the number one cause of mortality among hospitalized patients, with a rate up to 10 times that of acute myocardial infarction,” Dr. Horton explains. “The one treatment that consistently decreases mortality is timely administration of antibiotics. But, in order for a patient to be given timely antibiotics, the nurse or resident must first recognize that the patient has sepsis.”
“This is one of the biggest and most far-reaching improvement initiatives that has been done at our institution,” says Robert Pendleton, MD, chief quality officer at University Hospital. Dr. Horton says he predicts the program will “save 50 lives and $1 million per year.”
For more information, contact him at: devin.horton@hsc.utah.edu.
Policy Changes Hospitalists May See in 2016
The year 2015 brought the repeal of the sustainable growth rate (SGR) and new rules for advanced care planning reimbursement. It saw hospitalists take the lead on improving the two-midnight rule and respond to a global infectious disease scare.
The Hospitalist caught up with Dr. Greeno, chief strategy officer at North Hollywood, Calif.-based IPC Healthcare, to ask him about what he sees for the year ahead in policy.
Question: What are the biggest changes in store for 2016 that stand to impact hospitalists?
Answer: Much of it is just a magnification of the things that most hospitalists are already feeling or sensing. Clearly, there is a very solid movement toward alternative payment methodologies. BPCI (the Bundled Payments for Care Improvement initiative) has been embraced by hospitalists and other physicians all over the country at a scale that has surprised everybody.
There is also more consolidation in the healthcare industry as a whole. Hospital organizations are getting bigger, and we’re seeing consolidation of hospitalist groups. We will see cross-integration in the healthcare system that occurs at a rapid pace: hospitals buying physician groups, health systems and providers starting health plans, health plans acquiring hospital systems. In the not-too-distant future, we are all going to be in the population health business. This is a complete realignment of the healthcare system, and we haven’t seen the half of it yet. We have to be prepared to do it all, or a very big piece of it. The good news is, we are an absolute necessity for success in the future.
Q: It’s a presidential election year. How much weight should physicians put on claims made by candidates?
A: I encourage people to be politically engaged, but I don’t think the majority of what’s happening in healthcare is being driven by politics. It’s being driven by dispassionate economic forces that aren’t going to go away, no matter who is president. We have to figure out how to care for our population more cost-effectively. The ACA (Affordable Care Act) has driven a lot of the political environment in D.C. since its passage, including a big divide between the two parties, but it’s about three things: insurance reform, expanded access, and, particularly, delivery system reform. That’s the part we really care about and can influence the most, I think. Both parties feel like the delivery system needs to be reformed. I don’t think the election will have a major impact on hospitalists and what we do.
The ACA created an environment where things moved faster, created the (CMS) Innovation Center that drives alternative payment methodologies. It created a burning platform for things that already needed to happen.
Q: Is there anything new for meaningful use/EHR in 2016?
A: There are implications of meaningful use for hospitalists. Last year was the first that meaningful use penalties for physician groups came into effect. The way it was written, there was an exception to meaningful use requirements for hospital-based physicians, but a majority of SHM’s membership does not qualify for exemption and are subject to penalties. It’s not small: $2,500 to $5,000 per doctor. The Public Policy Committee at SHM has been working in Washington the last couple of years. We were able to get a one-year exemption, and now they’ve given us a second year, but we can only do five years according to law, and we have to apply every year. We have applied to CMS for a specialty code for hospitalists, and if that gets approved, it will be used to identify who is a hospitalist and who is not. If we submit under that code, then we’re not subject to penalty.

–Dr. Greeno
Q: What is the future of the two-midnight rule?
A: The committee and SHM took that on several years ago at my urging because it didn’t seem like other specialties were leading that issue. It doesn’t affect hospitalists in terms of how we’re paid, but it does affect the patients we care for. I think we’ll have a better solution in the coming years.
Q: What should hospitalists be thinking about heading into 2016?
A: They should be starting to prepare for a world where they no longer get paid with fee-for-service. Hospitalists are in the post-acute setting, where a lot of the action takes place, and it’s the high-cost action. My lesson is to embrace the changes; don’t fight it. As a hospitalist, your job is going to be different a year from now. We might as well get ready for the change, because there’s going to be a lot of change in the system.
Kelly April Tyrrell is a freelance writer in Madison, Wis.
The year 2015 brought the repeal of the sustainable growth rate (SGR) and new rules for advanced care planning reimbursement. It saw hospitalists take the lead on improving the two-midnight rule and respond to a global infectious disease scare.
The Hospitalist caught up with Dr. Greeno, chief strategy officer at North Hollywood, Calif.-based IPC Healthcare, to ask him about what he sees for the year ahead in policy.
Question: What are the biggest changes in store for 2016 that stand to impact hospitalists?
Answer: Much of it is just a magnification of the things that most hospitalists are already feeling or sensing. Clearly, there is a very solid movement toward alternative payment methodologies. BPCI (the Bundled Payments for Care Improvement initiative) has been embraced by hospitalists and other physicians all over the country at a scale that has surprised everybody.
There is also more consolidation in the healthcare industry as a whole. Hospital organizations are getting bigger, and we’re seeing consolidation of hospitalist groups. We will see cross-integration in the healthcare system that occurs at a rapid pace: hospitals buying physician groups, health systems and providers starting health plans, health plans acquiring hospital systems. In the not-too-distant future, we are all going to be in the population health business. This is a complete realignment of the healthcare system, and we haven’t seen the half of it yet. We have to be prepared to do it all, or a very big piece of it. The good news is, we are an absolute necessity for success in the future.
Q: It’s a presidential election year. How much weight should physicians put on claims made by candidates?
A: I encourage people to be politically engaged, but I don’t think the majority of what’s happening in healthcare is being driven by politics. It’s being driven by dispassionate economic forces that aren’t going to go away, no matter who is president. We have to figure out how to care for our population more cost-effectively. The ACA (Affordable Care Act) has driven a lot of the political environment in D.C. since its passage, including a big divide between the two parties, but it’s about three things: insurance reform, expanded access, and, particularly, delivery system reform. That’s the part we really care about and can influence the most, I think. Both parties feel like the delivery system needs to be reformed. I don’t think the election will have a major impact on hospitalists and what we do.
The ACA created an environment where things moved faster, created the (CMS) Innovation Center that drives alternative payment methodologies. It created a burning platform for things that already needed to happen.
Q: Is there anything new for meaningful use/EHR in 2016?
A: There are implications of meaningful use for hospitalists. Last year was the first that meaningful use penalties for physician groups came into effect. The way it was written, there was an exception to meaningful use requirements for hospital-based physicians, but a majority of SHM’s membership does not qualify for exemption and are subject to penalties. It’s not small: $2,500 to $5,000 per doctor. The Public Policy Committee at SHM has been working in Washington the last couple of years. We were able to get a one-year exemption, and now they’ve given us a second year, but we can only do five years according to law, and we have to apply every year. We have applied to CMS for a specialty code for hospitalists, and if that gets approved, it will be used to identify who is a hospitalist and who is not. If we submit under that code, then we’re not subject to penalty.

–Dr. Greeno
Q: What is the future of the two-midnight rule?
A: The committee and SHM took that on several years ago at my urging because it didn’t seem like other specialties were leading that issue. It doesn’t affect hospitalists in terms of how we’re paid, but it does affect the patients we care for. I think we’ll have a better solution in the coming years.
Q: What should hospitalists be thinking about heading into 2016?
A: They should be starting to prepare for a world where they no longer get paid with fee-for-service. Hospitalists are in the post-acute setting, where a lot of the action takes place, and it’s the high-cost action. My lesson is to embrace the changes; don’t fight it. As a hospitalist, your job is going to be different a year from now. We might as well get ready for the change, because there’s going to be a lot of change in the system.
Kelly April Tyrrell is a freelance writer in Madison, Wis.
The year 2015 brought the repeal of the sustainable growth rate (SGR) and new rules for advanced care planning reimbursement. It saw hospitalists take the lead on improving the two-midnight rule and respond to a global infectious disease scare.
The Hospitalist caught up with Dr. Greeno, chief strategy officer at North Hollywood, Calif.-based IPC Healthcare, to ask him about what he sees for the year ahead in policy.
Question: What are the biggest changes in store for 2016 that stand to impact hospitalists?
Answer: Much of it is just a magnification of the things that most hospitalists are already feeling or sensing. Clearly, there is a very solid movement toward alternative payment methodologies. BPCI (the Bundled Payments for Care Improvement initiative) has been embraced by hospitalists and other physicians all over the country at a scale that has surprised everybody.
There is also more consolidation in the healthcare industry as a whole. Hospital organizations are getting bigger, and we’re seeing consolidation of hospitalist groups. We will see cross-integration in the healthcare system that occurs at a rapid pace: hospitals buying physician groups, health systems and providers starting health plans, health plans acquiring hospital systems. In the not-too-distant future, we are all going to be in the population health business. This is a complete realignment of the healthcare system, and we haven’t seen the half of it yet. We have to be prepared to do it all, or a very big piece of it. The good news is, we are an absolute necessity for success in the future.
Q: It’s a presidential election year. How much weight should physicians put on claims made by candidates?
A: I encourage people to be politically engaged, but I don’t think the majority of what’s happening in healthcare is being driven by politics. It’s being driven by dispassionate economic forces that aren’t going to go away, no matter who is president. We have to figure out how to care for our population more cost-effectively. The ACA (Affordable Care Act) has driven a lot of the political environment in D.C. since its passage, including a big divide between the two parties, but it’s about three things: insurance reform, expanded access, and, particularly, delivery system reform. That’s the part we really care about and can influence the most, I think. Both parties feel like the delivery system needs to be reformed. I don’t think the election will have a major impact on hospitalists and what we do.
The ACA created an environment where things moved faster, created the (CMS) Innovation Center that drives alternative payment methodologies. It created a burning platform for things that already needed to happen.
Q: Is there anything new for meaningful use/EHR in 2016?
A: There are implications of meaningful use for hospitalists. Last year was the first that meaningful use penalties for physician groups came into effect. The way it was written, there was an exception to meaningful use requirements for hospital-based physicians, but a majority of SHM’s membership does not qualify for exemption and are subject to penalties. It’s not small: $2,500 to $5,000 per doctor. The Public Policy Committee at SHM has been working in Washington the last couple of years. We were able to get a one-year exemption, and now they’ve given us a second year, but we can only do five years according to law, and we have to apply every year. We have applied to CMS for a specialty code for hospitalists, and if that gets approved, it will be used to identify who is a hospitalist and who is not. If we submit under that code, then we’re not subject to penalty.

–Dr. Greeno
Q: What is the future of the two-midnight rule?
A: The committee and SHM took that on several years ago at my urging because it didn’t seem like other specialties were leading that issue. It doesn’t affect hospitalists in terms of how we’re paid, but it does affect the patients we care for. I think we’ll have a better solution in the coming years.
Q: What should hospitalists be thinking about heading into 2016?
A: They should be starting to prepare for a world where they no longer get paid with fee-for-service. Hospitalists are in the post-acute setting, where a lot of the action takes place, and it’s the high-cost action. My lesson is to embrace the changes; don’t fight it. As a hospitalist, your job is going to be different a year from now. We might as well get ready for the change, because there’s going to be a lot of change in the system.
Kelly April Tyrrell is a freelance writer in Madison, Wis.
Hospitals Save Estimated $67 Million by Tracking Energy Consumption
Estimated savings in energy costs posted by hospitals participating in the American Hospital Association’s affiliated American Society for Healthcare Engineering (ASHE) Energy to Care Program. Twenty participating hospitals received Energy to Care awards from ASHE in July for reducing their energy consumption by 10% or more. ASHE’s free program includes a benchmarking dashboard hospitals can use to track their own energy consumption, thereby saving energy and reducing costs.
Larry Beresford is a freelance writer in Alameda, Calif.
Estimated savings in energy costs posted by hospitals participating in the American Hospital Association’s affiliated American Society for Healthcare Engineering (ASHE) Energy to Care Program. Twenty participating hospitals received Energy to Care awards from ASHE in July for reducing their energy consumption by 10% or more. ASHE’s free program includes a benchmarking dashboard hospitals can use to track their own energy consumption, thereby saving energy and reducing costs.
Larry Beresford is a freelance writer in Alameda, Calif.
Estimated savings in energy costs posted by hospitals participating in the American Hospital Association’s affiliated American Society for Healthcare Engineering (ASHE) Energy to Care Program. Twenty participating hospitals received Energy to Care awards from ASHE in July for reducing their energy consumption by 10% or more. ASHE’s free program includes a benchmarking dashboard hospitals can use to track their own energy consumption, thereby saving energy and reducing costs.
Larry Beresford is a freelance writer in Alameda, Calif.
How to Develop a Comprehensive Pediatric Palliative Care Program
For Ami Doshi, MD, FAAP, a hospitalist at Rady Children’s Hospital San Diego, the path to establishing a comprehensive pediatric palliative care program began with her realization during medical training that doctors didn’t always adequately address the suffering of young patients with advanced disease and their families. Then, in a hospice rotation, she saw that the palliative approach could offer a better way.
During a pediatric hospital medicine fellowship at the University of California at San Diego, Dr. Doshi conducted an educational needs assessment and then created a palliative care curriculum for residents. Rady administrators supported her attending the Palliative Care Leadership Center training at UC San Francisco, with a team from Rady and Harvard Medical School’s program in Palliative Care Education and Practice.
After five years of development, the program Dr. Doshi helped to launch at Rady has grown into a division of palliative medicine, with a medical director, an inpatient consultation service, a palliative home care program coordinated by a health navigator, and a variety of models in the outpatient clinics.
“The goal is to be seamless and to treat patients across the continuum of care,” says Dr. Doshi, who is now board certified in hospice and palliative. Although she is based in the division of hospital medicine, she leads sit-down rounds with the full palliative care team and bioethics consultants every other week.
“Finding time for this work is always a challenge,” she says, adding that administrative support for physicians’ protected time is growing and that the program is ramping up its data collection to document outcomes resulting from palliative care.
For more information on the program, email her at adoshi@rchsd.org.
Larry Beresford is a freelance writer in Alameda, Calif.
For Ami Doshi, MD, FAAP, a hospitalist at Rady Children’s Hospital San Diego, the path to establishing a comprehensive pediatric palliative care program began with her realization during medical training that doctors didn’t always adequately address the suffering of young patients with advanced disease and their families. Then, in a hospice rotation, she saw that the palliative approach could offer a better way.
During a pediatric hospital medicine fellowship at the University of California at San Diego, Dr. Doshi conducted an educational needs assessment and then created a palliative care curriculum for residents. Rady administrators supported her attending the Palliative Care Leadership Center training at UC San Francisco, with a team from Rady and Harvard Medical School’s program in Palliative Care Education and Practice.
After five years of development, the program Dr. Doshi helped to launch at Rady has grown into a division of palliative medicine, with a medical director, an inpatient consultation service, a palliative home care program coordinated by a health navigator, and a variety of models in the outpatient clinics.
“The goal is to be seamless and to treat patients across the continuum of care,” says Dr. Doshi, who is now board certified in hospice and palliative. Although she is based in the division of hospital medicine, she leads sit-down rounds with the full palliative care team and bioethics consultants every other week.
“Finding time for this work is always a challenge,” she says, adding that administrative support for physicians’ protected time is growing and that the program is ramping up its data collection to document outcomes resulting from palliative care.
For more information on the program, email her at adoshi@rchsd.org.
Larry Beresford is a freelance writer in Alameda, Calif.
For Ami Doshi, MD, FAAP, a hospitalist at Rady Children’s Hospital San Diego, the path to establishing a comprehensive pediatric palliative care program began with her realization during medical training that doctors didn’t always adequately address the suffering of young patients with advanced disease and their families. Then, in a hospice rotation, she saw that the palliative approach could offer a better way.
During a pediatric hospital medicine fellowship at the University of California at San Diego, Dr. Doshi conducted an educational needs assessment and then created a palliative care curriculum for residents. Rady administrators supported her attending the Palliative Care Leadership Center training at UC San Francisco, with a team from Rady and Harvard Medical School’s program in Palliative Care Education and Practice.
After five years of development, the program Dr. Doshi helped to launch at Rady has grown into a division of palliative medicine, with a medical director, an inpatient consultation service, a palliative home care program coordinated by a health navigator, and a variety of models in the outpatient clinics.
“The goal is to be seamless and to treat patients across the continuum of care,” says Dr. Doshi, who is now board certified in hospice and palliative. Although she is based in the division of hospital medicine, she leads sit-down rounds with the full palliative care team and bioethics consultants every other week.
“Finding time for this work is always a challenge,” she says, adding that administrative support for physicians’ protected time is growing and that the program is ramping up its data collection to document outcomes resulting from palliative care.
For more information on the program, email her at adoshi@rchsd.org.
Larry Beresford is a freelance writer in Alameda, Calif.
Consumer Reports Rates Hospitals on Infection Control, Prevention
Consumer Reports included for the first time in its national hospital quality ratings a ranking of how well 3,000 hospitals are controlling common deadly infections such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile.
The How Your Hospital Can Make You Sick report is based on information provided to the CDC between October 2013 and September 2014. The CDC found that 105 hospitals distinguished themselves by earning high ratings against both infections. Nine hospitals received top ratings for having no infections from MRSA, C. diff, or other measured infections, although none of the country’s highest-profile hospitals are on that list. Only 6% of hospitals scored well against both infections in the new ratings. The CDC estimates that 648,000 people develop infections during their hospital stay, with 75,000 dying from them; many of the deaths can be traced back to widespread, inappropriate use of antibiotics.
“High rates for MRSA and C. diff can be a red flag that a hospital isn’t following the best practices in preventing infections and prescribing antibiotics,” notes Doris Peter, PhD, director of Consumer Reports’ Health Ratings Center, in a prepared statement. “The data show that it is possible to keep infection rates down and in some cases avoid them altogether.”
Among Consumer Reports’ recommendations for hospitals:
- Consistently follow established protocols for managing superbug infections;
- Accurately track how many infections patients get; and
- Promptly report outbreaks to patients and health authorities.
Reference
- Consumer Reports. America’s antibiotic crisis: how your hospital can make you sick. July 29, 2015. Accessed September 12, 2015.
Consumer Reports included for the first time in its national hospital quality ratings a ranking of how well 3,000 hospitals are controlling common deadly infections such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile.
The How Your Hospital Can Make You Sick report is based on information provided to the CDC between October 2013 and September 2014. The CDC found that 105 hospitals distinguished themselves by earning high ratings against both infections. Nine hospitals received top ratings for having no infections from MRSA, C. diff, or other measured infections, although none of the country’s highest-profile hospitals are on that list. Only 6% of hospitals scored well against both infections in the new ratings. The CDC estimates that 648,000 people develop infections during their hospital stay, with 75,000 dying from them; many of the deaths can be traced back to widespread, inappropriate use of antibiotics.
“High rates for MRSA and C. diff can be a red flag that a hospital isn’t following the best practices in preventing infections and prescribing antibiotics,” notes Doris Peter, PhD, director of Consumer Reports’ Health Ratings Center, in a prepared statement. “The data show that it is possible to keep infection rates down and in some cases avoid them altogether.”
Among Consumer Reports’ recommendations for hospitals:
- Consistently follow established protocols for managing superbug infections;
- Accurately track how many infections patients get; and
- Promptly report outbreaks to patients and health authorities.
Reference
- Consumer Reports. America’s antibiotic crisis: how your hospital can make you sick. July 29, 2015. Accessed September 12, 2015.
Consumer Reports included for the first time in its national hospital quality ratings a ranking of how well 3,000 hospitals are controlling common deadly infections such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile.
The How Your Hospital Can Make You Sick report is based on information provided to the CDC between October 2013 and September 2014. The CDC found that 105 hospitals distinguished themselves by earning high ratings against both infections. Nine hospitals received top ratings for having no infections from MRSA, C. diff, or other measured infections, although none of the country’s highest-profile hospitals are on that list. Only 6% of hospitals scored well against both infections in the new ratings. The CDC estimates that 648,000 people develop infections during their hospital stay, with 75,000 dying from them; many of the deaths can be traced back to widespread, inappropriate use of antibiotics.
“High rates for MRSA and C. diff can be a red flag that a hospital isn’t following the best practices in preventing infections and prescribing antibiotics,” notes Doris Peter, PhD, director of Consumer Reports’ Health Ratings Center, in a prepared statement. “The data show that it is possible to keep infection rates down and in some cases avoid them altogether.”
Among Consumer Reports’ recommendations for hospitals:
- Consistently follow established protocols for managing superbug infections;
- Accurately track how many infections patients get; and
- Promptly report outbreaks to patients and health authorities.
Reference
- Consumer Reports. America’s antibiotic crisis: how your hospital can make you sick. July 29, 2015. Accessed September 12, 2015.
Joint Commission Offers Resource to Prevent Hospital Falls
The Joint Commission’s Center for Transforming Healthcare has released its Targeted Solutions Tool for preventing hospital inpatient falls and falls with injuries. This step-by-step, online resource helps hospitals measure their fall rates and identify barriers to fall prevention and the specific contributing factors that lead to falls. A systematic approach enables the organization to assess each patient’s risk for falling and then implement specific targeted solutions to address the contributing factors, which will vary from one organization to the next.
Hospital falls total between 700,000 and one million per year, according to the Agency for Healthcare Research and Quality; since 2008, the Centers for Medicare and Medicaid Services has not paid hospitals for the costs of extra care related to falls.
The Joint Commission calculates, based on average baseline and improvement figures from its Preventing Falls with Injury Project, that a typical 200-bed hospital could reduce its number of patients injured by falls annually from 117 to 45. Key elements of a program achieving that kind of success include consistent messaging focused on operational and cultural change, staff engagement, and an “all hands on deck” approach that involves hospitalists and other physicians in helping to prevent falls by hospitalized patients.
The Joint Commission’s Center for Transforming Healthcare has released its Targeted Solutions Tool for preventing hospital inpatient falls and falls with injuries. This step-by-step, online resource helps hospitals measure their fall rates and identify barriers to fall prevention and the specific contributing factors that lead to falls. A systematic approach enables the organization to assess each patient’s risk for falling and then implement specific targeted solutions to address the contributing factors, which will vary from one organization to the next.
Hospital falls total between 700,000 and one million per year, according to the Agency for Healthcare Research and Quality; since 2008, the Centers for Medicare and Medicaid Services has not paid hospitals for the costs of extra care related to falls.
The Joint Commission calculates, based on average baseline and improvement figures from its Preventing Falls with Injury Project, that a typical 200-bed hospital could reduce its number of patients injured by falls annually from 117 to 45. Key elements of a program achieving that kind of success include consistent messaging focused on operational and cultural change, staff engagement, and an “all hands on deck” approach that involves hospitalists and other physicians in helping to prevent falls by hospitalized patients.
The Joint Commission’s Center for Transforming Healthcare has released its Targeted Solutions Tool for preventing hospital inpatient falls and falls with injuries. This step-by-step, online resource helps hospitals measure their fall rates and identify barriers to fall prevention and the specific contributing factors that lead to falls. A systematic approach enables the organization to assess each patient’s risk for falling and then implement specific targeted solutions to address the contributing factors, which will vary from one organization to the next.
Hospital falls total between 700,000 and one million per year, according to the Agency for Healthcare Research and Quality; since 2008, the Centers for Medicare and Medicaid Services has not paid hospitals for the costs of extra care related to falls.
The Joint Commission calculates, based on average baseline and improvement figures from its Preventing Falls with Injury Project, that a typical 200-bed hospital could reduce its number of patients injured by falls annually from 117 to 45. Key elements of a program achieving that kind of success include consistent messaging focused on operational and cultural change, staff engagement, and an “all hands on deck” approach that involves hospitalists and other physicians in helping to prevent falls by hospitalized patients.