User login
Optimal gestational age for cell-free DNA sampling in obese women
cfDNA screening failures occur in 1% to 12% of samples, a rate that has an inverse relationship to gestational age. Recent studies have shown an increased risk for screening failures among obese women. To determine the optimal gestational age for cfDNA testing among obese women, Mary C. Livergood, MD, and colleagues at the Mercy Hospital in St. Louis, Missouri, performed a retrospective cohort study of those undergoing cfDNA testing at one center from 2011 through 2016. Study results recently were published online in the American Journal of Obstetrics and Gynecology.1
Details of the study
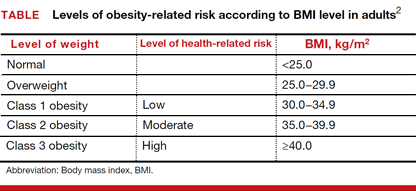
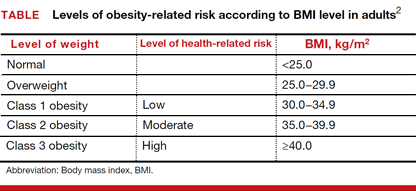
Adjusted odds ratios (aORs) with 95% confidence interval (CI) for a cfDNA screening failure (referred to as a “no call” in the study) were determined for each body mass index (BMI) weight class (TABLE). Each BMI weight class also was compared with the aOR of normal-weight women (BMI <25.0 kg/m2). The predicted probability of a no call was determined for each week of gestational age for normal weight and obese women and the results were compared.1
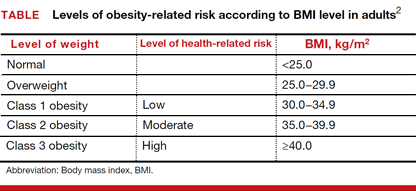
Among the 2,385 patients meeting inclusion criteria, 4.4% (n = 105) received a no call. Compared with normal weight women, the aOR of no call increased as weight increased from overweight (aOR, 2.31 [95% CI, 1.21–4.42]) to obesity class III (aOR, 8.55 [95% CI, 4.16–17.56]).1
At 21 weeks’ gestation, a cut-point was identified for obesity class II/III women (ie, there was no longer a significant difference in the probability of no call when compared with normal-weight women). From 8 to 16 weeks’ gestation, there was a 4.5% reduction in the probability of a no call for obesity class II/III women (aOR, 14.9; 95% CI, 8.95–20.78 and aOR, 10.4; 95% CI, 7.20–13.61; Ptrend<.01).1
Although the authors conclude that a cut-point of 21 weeks’ gestation allowed for optimal sampling of cfDNA in obese women, they also acknowledge that this cut-point limits a woman’s reproductive choices. However, they say that delaying cfDNA testing in obese women is a reasonable strategy to reduce the probability of screening failure.1
- Livergood MC, Lechien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? [published online ahead of print January 28, 2017]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2017.01.011.
- Health risks of obesity. MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000348.htm. Updated February 7, 2017. Accessed March 10, 2017.
cfDNA screening failures occur in 1% to 12% of samples, a rate that has an inverse relationship to gestational age. Recent studies have shown an increased risk for screening failures among obese women. To determine the optimal gestational age for cfDNA testing among obese women, Mary C. Livergood, MD, and colleagues at the Mercy Hospital in St. Louis, Missouri, performed a retrospective cohort study of those undergoing cfDNA testing at one center from 2011 through 2016. Study results recently were published online in the American Journal of Obstetrics and Gynecology.1
Details of the study
Adjusted odds ratios (aORs) with 95% confidence interval (CI) for a cfDNA screening failure (referred to as a “no call” in the study) were determined for each body mass index (BMI) weight class (TABLE). Each BMI weight class also was compared with the aOR of normal-weight women (BMI <25.0 kg/m2). The predicted probability of a no call was determined for each week of gestational age for normal weight and obese women and the results were compared.1
Among the 2,385 patients meeting inclusion criteria, 4.4% (n = 105) received a no call. Compared with normal weight women, the aOR of no call increased as weight increased from overweight (aOR, 2.31 [95% CI, 1.21–4.42]) to obesity class III (aOR, 8.55 [95% CI, 4.16–17.56]).1
At 21 weeks’ gestation, a cut-point was identified for obesity class II/III women (ie, there was no longer a significant difference in the probability of no call when compared with normal-weight women). From 8 to 16 weeks’ gestation, there was a 4.5% reduction in the probability of a no call for obesity class II/III women (aOR, 14.9; 95% CI, 8.95–20.78 and aOR, 10.4; 95% CI, 7.20–13.61; Ptrend<.01).1
Although the authors conclude that a cut-point of 21 weeks’ gestation allowed for optimal sampling of cfDNA in obese women, they also acknowledge that this cut-point limits a woman’s reproductive choices. However, they say that delaying cfDNA testing in obese women is a reasonable strategy to reduce the probability of screening failure.1
cfDNA screening failures occur in 1% to 12% of samples, a rate that has an inverse relationship to gestational age. Recent studies have shown an increased risk for screening failures among obese women. To determine the optimal gestational age for cfDNA testing among obese women, Mary C. Livergood, MD, and colleagues at the Mercy Hospital in St. Louis, Missouri, performed a retrospective cohort study of those undergoing cfDNA testing at one center from 2011 through 2016. Study results recently were published online in the American Journal of Obstetrics and Gynecology.1
Details of the study
Adjusted odds ratios (aORs) with 95% confidence interval (CI) for a cfDNA screening failure (referred to as a “no call” in the study) were determined for each body mass index (BMI) weight class (TABLE). Each BMI weight class also was compared with the aOR of normal-weight women (BMI <25.0 kg/m2). The predicted probability of a no call was determined for each week of gestational age for normal weight and obese women and the results were compared.1
Among the 2,385 patients meeting inclusion criteria, 4.4% (n = 105) received a no call. Compared with normal weight women, the aOR of no call increased as weight increased from overweight (aOR, 2.31 [95% CI, 1.21–4.42]) to obesity class III (aOR, 8.55 [95% CI, 4.16–17.56]).1
At 21 weeks’ gestation, a cut-point was identified for obesity class II/III women (ie, there was no longer a significant difference in the probability of no call when compared with normal-weight women). From 8 to 16 weeks’ gestation, there was a 4.5% reduction in the probability of a no call for obesity class II/III women (aOR, 14.9; 95% CI, 8.95–20.78 and aOR, 10.4; 95% CI, 7.20–13.61; Ptrend<.01).1
Although the authors conclude that a cut-point of 21 weeks’ gestation allowed for optimal sampling of cfDNA in obese women, they also acknowledge that this cut-point limits a woman’s reproductive choices. However, they say that delaying cfDNA testing in obese women is a reasonable strategy to reduce the probability of screening failure.1
- Livergood MC, Lechien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? [published online ahead of print January 28, 2017]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2017.01.011.
- Health risks of obesity. MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000348.htm. Updated February 7, 2017. Accessed March 10, 2017.
- Livergood MC, Lechien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? [published online ahead of print January 28, 2017]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2017.01.011.
- Health risks of obesity. MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000348.htm. Updated February 7, 2017. Accessed March 10, 2017.
Risk-reducing salpingectomy at benign hysterectomy: Have surgeons embraced this practice?
According to its January 2015 Committee Opinion, the American College of Obstetricians and Gynecologists supported the following recommendations and conclusions regarding salpingectomy for ovarian cancer prevention1:
- The surgeon and patient should discuss the potential benefits of the removal of the fallopian tubes during a hysterectomy in women at population risk of ovarian cancer who are not having an oophorectomy.
- When counseling women about laparoscopic sterilization methods, clinicians can communicate that bilateral salpingectomy can be considered a method that provides effective contraception.
- Prophylactic salpingectomy may offer clinicians the opportunity to prevent ovarian cancer in their patients.
- Randomized controlled trials are needed to support the validity of this approach to reduce the incidence of ovarian cancer.
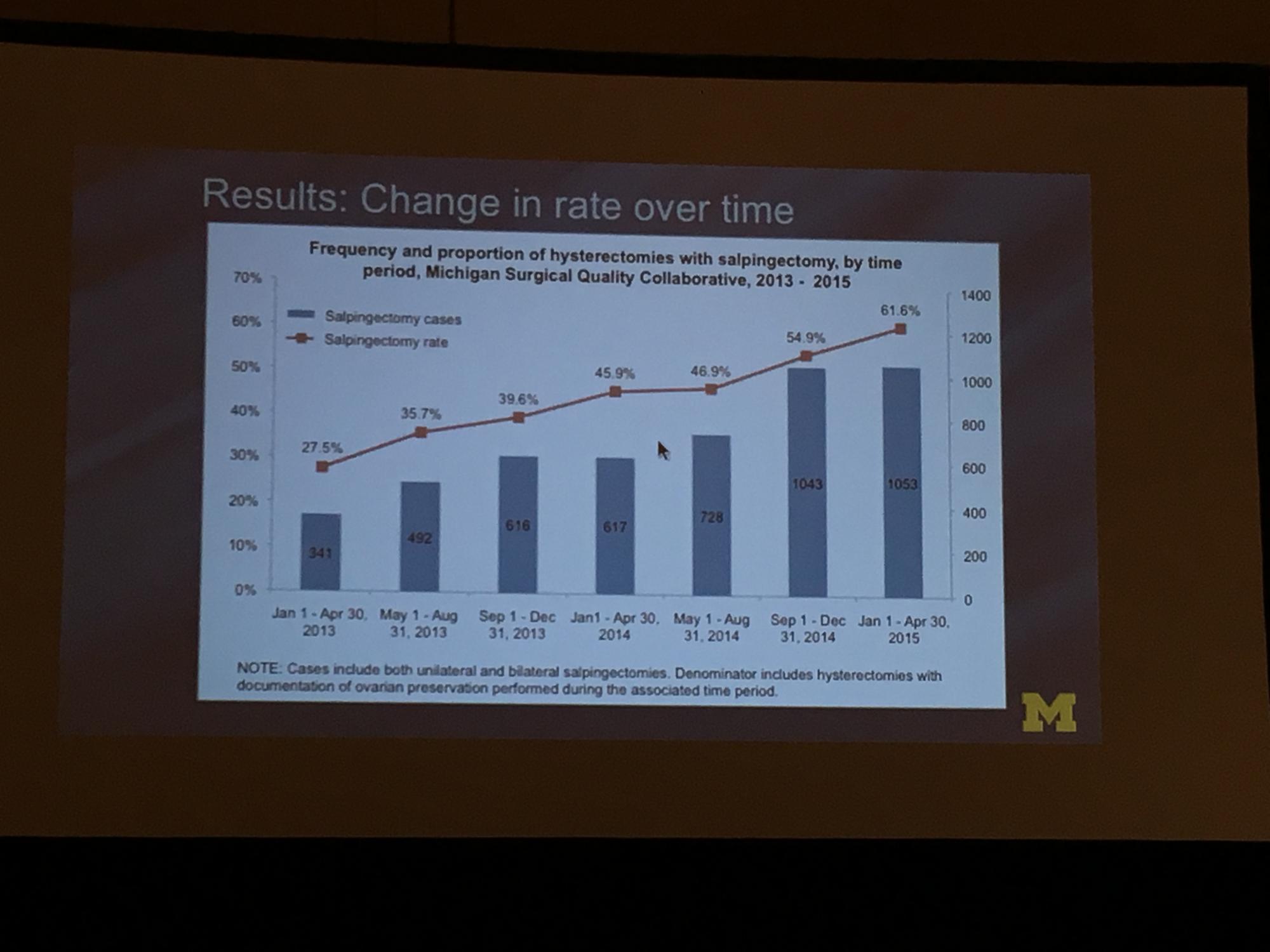
To determine the change in rate of salpingectomy performed at benign hysterectomy at Michigan hospitals, Sara Till, MD, MPH, and colleagues from the University of Michigan Health System performed a retrospective cross-sectioned study of data from the Michigan Surgical Quality Collaborative. They examined hysterectomies performed for all surgical routes between January 2013 and April 2015. Exclusion criteria included malignancy and obstetric indication. The primary objective was to measure salpingectomy at the time of hysterectomy with ovarian preservation. Measures studied included demographics; comorbidities; perioperative and postoperative results; and hospital/surgeon-related data; including surgeon volume, hospital type (ie, teaching), and hospital size.2
During the study period (January 1, 2013, to April 30, 2015), 18,642 hysterectomies were performed for benign indications, of which 55.7% (n = 10,382) were ovarian conserving. Among patients who underwent ovarian conserving hysterectomy, 44.9% (n = 4,668) had salpingectomy, with rates increasing steadily from 26.4% to 61.1% across the study period (P<.001). Salpingectomy was more likely with a laparoscopic approach (odds ratio [OR], 2.93; 95% confidence interval [CI], 2.69–3.20) and among women aged <60 years (OR, 2.60; 95% CI, 1.42–1.98), but did not vary with surgeon volume. After adjustments for age, body mass index, and surgical approach using a mixed model, the researchers found substantial variation in rates of salpingectomy across hospital sites, ranging from 3.7% to 88.3%. Variation in adjusted salpingectomy rates was not associated with academic affiliation or hospital size.2
Dr. Till and colleagues concluded that there was a substantial rise in risk-reducing salpingectomy from January 1, 2013, to April 30, 2015, and that there is substantial variation in the practice of salpingectomy, which is not accounted for by patient, surgeon, or hospital characteristics.2
- American College of Obstetricians and Gynecologists, Committee on Gynecologic Practice. Salpingectomy for ovarian cancer prevention. Committee Opinion No. 620 [published correction appears in: Obstet Gynecol. 2016;127(2):405]. Obstet Gynecol. 2015;125(1):279–281.
- Till SR, Edwards MG, Kobernik EK, Kamdar NS, As-Sanie S, Morgan DM. Implementation rate of risk-reducing salpingectomy at time of benign hysterectomy. Poster presented at: AAGL Global Congress of Minimally Invasive Gynecology; November 16, 2016; Orlando, Florida. J Minim Invasiv Gynecol. 2016;23(7 suppl):S1.
According to its January 2015 Committee Opinion, the American College of Obstetricians and Gynecologists supported the following recommendations and conclusions regarding salpingectomy for ovarian cancer prevention1:
- The surgeon and patient should discuss the potential benefits of the removal of the fallopian tubes during a hysterectomy in women at population risk of ovarian cancer who are not having an oophorectomy.
- When counseling women about laparoscopic sterilization methods, clinicians can communicate that bilateral salpingectomy can be considered a method that provides effective contraception.
- Prophylactic salpingectomy may offer clinicians the opportunity to prevent ovarian cancer in their patients.
- Randomized controlled trials are needed to support the validity of this approach to reduce the incidence of ovarian cancer.
To determine the change in rate of salpingectomy performed at benign hysterectomy at Michigan hospitals, Sara Till, MD, MPH, and colleagues from the University of Michigan Health System performed a retrospective cross-sectioned study of data from the Michigan Surgical Quality Collaborative. They examined hysterectomies performed for all surgical routes between January 2013 and April 2015. Exclusion criteria included malignancy and obstetric indication. The primary objective was to measure salpingectomy at the time of hysterectomy with ovarian preservation. Measures studied included demographics; comorbidities; perioperative and postoperative results; and hospital/surgeon-related data; including surgeon volume, hospital type (ie, teaching), and hospital size.2
During the study period (January 1, 2013, to April 30, 2015), 18,642 hysterectomies were performed for benign indications, of which 55.7% (n = 10,382) were ovarian conserving. Among patients who underwent ovarian conserving hysterectomy, 44.9% (n = 4,668) had salpingectomy, with rates increasing steadily from 26.4% to 61.1% across the study period (P<.001). Salpingectomy was more likely with a laparoscopic approach (odds ratio [OR], 2.93; 95% confidence interval [CI], 2.69–3.20) and among women aged <60 years (OR, 2.60; 95% CI, 1.42–1.98), but did not vary with surgeon volume. After adjustments for age, body mass index, and surgical approach using a mixed model, the researchers found substantial variation in rates of salpingectomy across hospital sites, ranging from 3.7% to 88.3%. Variation in adjusted salpingectomy rates was not associated with academic affiliation or hospital size.2
Dr. Till and colleagues concluded that there was a substantial rise in risk-reducing salpingectomy from January 1, 2013, to April 30, 2015, and that there is substantial variation in the practice of salpingectomy, which is not accounted for by patient, surgeon, or hospital characteristics.2
According to its January 2015 Committee Opinion, the American College of Obstetricians and Gynecologists supported the following recommendations and conclusions regarding salpingectomy for ovarian cancer prevention1:
- The surgeon and patient should discuss the potential benefits of the removal of the fallopian tubes during a hysterectomy in women at population risk of ovarian cancer who are not having an oophorectomy.
- When counseling women about laparoscopic sterilization methods, clinicians can communicate that bilateral salpingectomy can be considered a method that provides effective contraception.
- Prophylactic salpingectomy may offer clinicians the opportunity to prevent ovarian cancer in their patients.
- Randomized controlled trials are needed to support the validity of this approach to reduce the incidence of ovarian cancer.
To determine the change in rate of salpingectomy performed at benign hysterectomy at Michigan hospitals, Sara Till, MD, MPH, and colleagues from the University of Michigan Health System performed a retrospective cross-sectioned study of data from the Michigan Surgical Quality Collaborative. They examined hysterectomies performed for all surgical routes between January 2013 and April 2015. Exclusion criteria included malignancy and obstetric indication. The primary objective was to measure salpingectomy at the time of hysterectomy with ovarian preservation. Measures studied included demographics; comorbidities; perioperative and postoperative results; and hospital/surgeon-related data; including surgeon volume, hospital type (ie, teaching), and hospital size.2
During the study period (January 1, 2013, to April 30, 2015), 18,642 hysterectomies were performed for benign indications, of which 55.7% (n = 10,382) were ovarian conserving. Among patients who underwent ovarian conserving hysterectomy, 44.9% (n = 4,668) had salpingectomy, with rates increasing steadily from 26.4% to 61.1% across the study period (P<.001). Salpingectomy was more likely with a laparoscopic approach (odds ratio [OR], 2.93; 95% confidence interval [CI], 2.69–3.20) and among women aged <60 years (OR, 2.60; 95% CI, 1.42–1.98), but did not vary with surgeon volume. After adjustments for age, body mass index, and surgical approach using a mixed model, the researchers found substantial variation in rates of salpingectomy across hospital sites, ranging from 3.7% to 88.3%. Variation in adjusted salpingectomy rates was not associated with academic affiliation or hospital size.2
Dr. Till and colleagues concluded that there was a substantial rise in risk-reducing salpingectomy from January 1, 2013, to April 30, 2015, and that there is substantial variation in the practice of salpingectomy, which is not accounted for by patient, surgeon, or hospital characteristics.2
- American College of Obstetricians and Gynecologists, Committee on Gynecologic Practice. Salpingectomy for ovarian cancer prevention. Committee Opinion No. 620 [published correction appears in: Obstet Gynecol. 2016;127(2):405]. Obstet Gynecol. 2015;125(1):279–281.
- Till SR, Edwards MG, Kobernik EK, Kamdar NS, As-Sanie S, Morgan DM. Implementation rate of risk-reducing salpingectomy at time of benign hysterectomy. Poster presented at: AAGL Global Congress of Minimally Invasive Gynecology; November 16, 2016; Orlando, Florida. J Minim Invasiv Gynecol. 2016;23(7 suppl):S1.
- American College of Obstetricians and Gynecologists, Committee on Gynecologic Practice. Salpingectomy for ovarian cancer prevention. Committee Opinion No. 620 [published correction appears in: Obstet Gynecol. 2016;127(2):405]. Obstet Gynecol. 2015;125(1):279–281.
- Till SR, Edwards MG, Kobernik EK, Kamdar NS, As-Sanie S, Morgan DM. Implementation rate of risk-reducing salpingectomy at time of benign hysterectomy. Poster presented at: AAGL Global Congress of Minimally Invasive Gynecology; November 16, 2016; Orlando, Florida. J Minim Invasiv Gynecol. 2016;23(7 suppl):S1.
Newly available tissue containment system brings back power morcellation to advanced MIG surgeons
In the 11 studies that have examined the incidence of leiomyosarcoma (LMS) since the 2014 communications by the US Food and Drug Administration (FDA),1 Dr. Matthew Siedhoff and colleagues found that the cumulative LMS incidence in 318,006 women was 0.0017%, or approximately 1 in 600. This is according to data Dr. Seidhoff presented November 16, 2016, at the 45th annual AAGL Global Congress on MIGS.2 This reported risk is smaller than the 1 in 350 cited by the FDA in its 2014 notice.1 Dr. Seidhoff concluded that, particularly in women aged younger than 50 years, minimally invasive hysterectomy remains a safe option for the informed patient to consider.
Regardless of the incidence of unsuspected LMS found in the studies published since 2014, what have been the practice changes among gynecologic surgeons as a result of the FDA’s 2014 actions? Kerac N. Falk, MD, explored this question with his colleagues at the Icahn School of Medicine in New York, New York. He presented these findings to AAGL congress attendees on November 16 in Orlando, Florida.3 Notably, of 197 responders to a survey sent to members of the Society of Gynecologic Oncologists, 12.5% reported decreasing their use of power morcellation. A full 38.8% reported discontinuing altogether the use of a power morcellator.
One in 5 (20%) of gyn oncologists previously using power morcellation reported switching to laparotomy. Importantly, the drive for the switch was “driven by media, patient request, and the FDA rather than physician choice,” Falk said.
What if physicians, and patients, have another choice?
Here at the AAGL meeting, Olympus announced the FDA clearance, marketing, and initial training on its contained tissue extraction system—the PneumoLiner containment device and its accompanying laparoscopic PK Morcellator (FIGURE).

Both tools, FDA cleared in April and October 2016, respectively, provide low-risk, appropriate women with “an improved safety device,” said Jubilee Brown, MD, AAGL representative on power morcellation to the FDA and Associate Director of Gynecologic Oncology at the Levine Cancer Institute of the Carolinas HealthCare System in Charlotte, North Carolina.
“We have found at our institution that we have had to do more opens and minilaps on patients without the option for power morcellation, and this new device offers a way for us not to have to do that. Minimally invasive surgery stays truly minimally invasive surgery,” said Dr. Brown.
“Although I have a handful of patients who have chosen open surgery over minimally invasive surgery when MIS was appropriate, by and large most patients prefer the minimally invasive approach to surgery—especially when they learn that they have reduced risk for complications, blood loss, and pain; will be back to normal life faster; and will have less cosmetic incisions,” said Dr. Brown. “We all have tried workarounds, but for low-risk, appropriate patients under FDA guidelines, this new device by Olympus brings us back to minimally invasive options, and that is a good thing.”
How does the Olympus containment system work?
The PneumoLiner is the first containment device to receive FDA market clearance that is designed for use with certain laparoscopic morcellators to isolate uterine tissue that is not suspected to contain cancer.4
The containment bag and morcellator are not indicated for use in women with tissue that is known or suspected to contain malignancy; and should not be used for removal of uterine tissue containing suspected fibroids in patients who are peri- or post-menopausal, or candidates for en bloc tissue removal vaginally or via mini-laparotomy.4
When insufflated, the PneumoLiner bag allows for space and surgeon visibility throughout the power morcellation procedure while maintaining a barrier to the escape of fluids, cells, and tissue fragments. The bag creates a barrier between the targeted tissue and nontargeted abdominal contents, minimizing the risk of inadvertent damage to adjacent structures, says Olympus.4 See this video, which demonstrates the procedure.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Filtration, immersion, and stress testing were conducted to demonstrate the PneumoLiner as impermeable to human cells, that it maintains its integrity following morcellation, and that its mechanical strength withholds forces in excess of those demonstrated during actual use.5 To support FDA 510 clearance of the PK Morcellator, Olympus performed additional testing with both devices used together, demonstrating compatibility.4
Surgeon training on new device use is rigid, comprehensive, and not to be overlooked
“This is one of the rare times in my career when, right out of the gate, we have a very rigid and comprehensive way of educating and training physicians on the proper utilization of a new technology (avoiding the cart-before-the-horse phenomenon, in which a clinician is given the tools without the proper education),” said AAGL immediate past president Arnold Advincula, MD, “and it is important to underscore that.” Dr. Advincula is the Levine Family Professor, Vice-Chair of Women’s Health, and Chief of Gynecology at Sloane Women’s Hospital, Columbia University Medical Center/New York-Presbyterian Hospital, New York, New York.
Training plans
Instead of its sales force, Olympus is having surgeons train other surgeons. Clinical Education Specialists, a small, select group of individuals within the company, also will be able to train. The required training follows a rigid protocol that was validated and submitted to the FDA as part of the approval process, said Jerilyn Hitchings, Director of Procedure Marketing at Olympus. After training up to 40 surgeons in the past 3 weeks, Olympus expects to train another 100 at AAGL.
“We have strict criteria for training, including that they are advanced laparoscopists,” fulfilling a minimum number of surgeries within a 90-day period, said Hitchings.
The 1-hour training requires surgeons to perform a 4-step protocol and demonstrate unaided proficiency at training conclusion. Olympus will not sell its product to a facility until an advanced surgeon has been trained there, according to Hitchings. And many physicians are approaching their institutions inquiring about training now, she reports.
Applications for training will be submitted to the Olympus Professional Education Team for approval. “We want this to go well. We know that there are many physicians who are hoping that this becomes a good reality, and we want to make sure that it is done properly. The training process adheres to that agenda.”
Having the technology is step 1
OBG Management Board of Editors member Dr. Advincula struck an optimistic tone in his June 2016 Guest Editorial for the journal,6 indicating his belief that the “tissue morcellation pendulum,” which has swung toward non−minimally invasive approaches since 2014, can change direction. At the Olympus containment system official introduction event at AAGL, he expressed the same optimism:
“We now have technology that has the promise of being able to deliver to women a safe way to undergo tissue extraction, to undergo a minimally invasive surgical procedure. …When you combine innovation and education together, you ultimately are going to advance MIS worldwide. With all the things going on around the world today, I think it is important that women be able to have a choice, an autonomous choice with her physician. Having the technology that allows physicians to extract tissue safely, to give women the option of undergoing a minimally invasive surgery, is critically important. I look forward to seeing how we can continue to advance surgery. Partnership with clinicians and with industry, such as Olympus, is going to be key to the success of how we advance women’s health care in general.”
What do AAGL attendees have to say about it?
“It’s a good thing for the minimally invasive market,” said John B. Gebhart, MD, MS, vaginal hysterectomy representative at the star-studded Operating with the Stars event on Thursday, November 17, and Professor of Obstetrics and Gynecology at the Mayo Clinic in Rochester, Minnesota.
May Thomassee, MD, who practices in Lafayette, Louisiana, said that, for the past 3 years, she has been performing extracorporeal morcellation at her institution. “I think the new containment bag and morcellator devices that are attempting to be safer are a very good thing; however, my concern of introducing this new technology, such as bags, is that it may increase the cost within our health care system. We have had great success, and patients feel that they have options when we offer them—after informed consent and appropriate preoperative workup—an abdominal, vaginal, or extracorporeal morcellation approach.”
As a developer and proponent of the Extracorporeal Tissue Extraction (ExCITE) technique, Mireille Truong, MD, who demonstrated the ExCITE surgical approach with Dr. Advincula as part of the Research and Science Plenary here at AAGL, said, “I think the PneumoLiner is a great example of creativity and innovation. It’s good that we now have an FDA-approved device to offer and counsel patients as one of many options.” She added that, overall, the morcellation controversy has been “a positive experience. We have learned better as a community about how to approach new technology.”
- US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. April 17, 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm. Updated November 24, 2014. Accessed November 17, 2016.
- Siedhoff MT, Doll KM, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation versus abdominal hysterectomy for presumed uterine leiomyomata: an updated decision analysis. J Minim Invasiv Gynecol. 2016;23(7):S4-S5.
- Mandelberger AH, Mathews S, Chuang L. Practice changes in power morcellation among gynecologic-oncologists since 2014. J Minim Invasiv Gynecol. 2016;23(7):S3.
Olympus introduces first-of-its-kind contained tissue extraction system, restoring healthcare option for gynecologists and women [press release]. November 16, 2016. Olympus website. http://www.olympusamerica.com/corporate/corp_presscenter_headline.asp?pressNo=2079. Accessed November 16, 2016.
- FDA allows marketing of first-of-kind tissue containment system for use with certain laparoscopic power morcellators in select patients. FDA website. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm494650.htm. Updated April 7, 2016. Accessed November 16, 2016.
- Advincula AP. Tissue extraction: can the pendulum change direction? OBG Manag. 2016;28(6):8, 10, 12.
In the 11 studies that have examined the incidence of leiomyosarcoma (LMS) since the 2014 communications by the US Food and Drug Administration (FDA),1 Dr. Matthew Siedhoff and colleagues found that the cumulative LMS incidence in 318,006 women was 0.0017%, or approximately 1 in 600. This is according to data Dr. Seidhoff presented November 16, 2016, at the 45th annual AAGL Global Congress on MIGS.2 This reported risk is smaller than the 1 in 350 cited by the FDA in its 2014 notice.1 Dr. Seidhoff concluded that, particularly in women aged younger than 50 years, minimally invasive hysterectomy remains a safe option for the informed patient to consider.
Regardless of the incidence of unsuspected LMS found in the studies published since 2014, what have been the practice changes among gynecologic surgeons as a result of the FDA’s 2014 actions? Kerac N. Falk, MD, explored this question with his colleagues at the Icahn School of Medicine in New York, New York. He presented these findings to AAGL congress attendees on November 16 in Orlando, Florida.3 Notably, of 197 responders to a survey sent to members of the Society of Gynecologic Oncologists, 12.5% reported decreasing their use of power morcellation. A full 38.8% reported discontinuing altogether the use of a power morcellator.
One in 5 (20%) of gyn oncologists previously using power morcellation reported switching to laparotomy. Importantly, the drive for the switch was “driven by media, patient request, and the FDA rather than physician choice,” Falk said.
What if physicians, and patients, have another choice?
Here at the AAGL meeting, Olympus announced the FDA clearance, marketing, and initial training on its contained tissue extraction system—the PneumoLiner containment device and its accompanying laparoscopic PK Morcellator (FIGURE).

Both tools, FDA cleared in April and October 2016, respectively, provide low-risk, appropriate women with “an improved safety device,” said Jubilee Brown, MD, AAGL representative on power morcellation to the FDA and Associate Director of Gynecologic Oncology at the Levine Cancer Institute of the Carolinas HealthCare System in Charlotte, North Carolina.
“We have found at our institution that we have had to do more opens and minilaps on patients without the option for power morcellation, and this new device offers a way for us not to have to do that. Minimally invasive surgery stays truly minimally invasive surgery,” said Dr. Brown.
“Although I have a handful of patients who have chosen open surgery over minimally invasive surgery when MIS was appropriate, by and large most patients prefer the minimally invasive approach to surgery—especially when they learn that they have reduced risk for complications, blood loss, and pain; will be back to normal life faster; and will have less cosmetic incisions,” said Dr. Brown. “We all have tried workarounds, but for low-risk, appropriate patients under FDA guidelines, this new device by Olympus brings us back to minimally invasive options, and that is a good thing.”
How does the Olympus containment system work?
The PneumoLiner is the first containment device to receive FDA market clearance that is designed for use with certain laparoscopic morcellators to isolate uterine tissue that is not suspected to contain cancer.4
The containment bag and morcellator are not indicated for use in women with tissue that is known or suspected to contain malignancy; and should not be used for removal of uterine tissue containing suspected fibroids in patients who are peri- or post-menopausal, or candidates for en bloc tissue removal vaginally or via mini-laparotomy.4
When insufflated, the PneumoLiner bag allows for space and surgeon visibility throughout the power morcellation procedure while maintaining a barrier to the escape of fluids, cells, and tissue fragments. The bag creates a barrier between the targeted tissue and nontargeted abdominal contents, minimizing the risk of inadvertent damage to adjacent structures, says Olympus.4 See this video, which demonstrates the procedure.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Filtration, immersion, and stress testing were conducted to demonstrate the PneumoLiner as impermeable to human cells, that it maintains its integrity following morcellation, and that its mechanical strength withholds forces in excess of those demonstrated during actual use.5 To support FDA 510 clearance of the PK Morcellator, Olympus performed additional testing with both devices used together, demonstrating compatibility.4
Surgeon training on new device use is rigid, comprehensive, and not to be overlooked
“This is one of the rare times in my career when, right out of the gate, we have a very rigid and comprehensive way of educating and training physicians on the proper utilization of a new technology (avoiding the cart-before-the-horse phenomenon, in which a clinician is given the tools without the proper education),” said AAGL immediate past president Arnold Advincula, MD, “and it is important to underscore that.” Dr. Advincula is the Levine Family Professor, Vice-Chair of Women’s Health, and Chief of Gynecology at Sloane Women’s Hospital, Columbia University Medical Center/New York-Presbyterian Hospital, New York, New York.
Training plans
Instead of its sales force, Olympus is having surgeons train other surgeons. Clinical Education Specialists, a small, select group of individuals within the company, also will be able to train. The required training follows a rigid protocol that was validated and submitted to the FDA as part of the approval process, said Jerilyn Hitchings, Director of Procedure Marketing at Olympus. After training up to 40 surgeons in the past 3 weeks, Olympus expects to train another 100 at AAGL.
“We have strict criteria for training, including that they are advanced laparoscopists,” fulfilling a minimum number of surgeries within a 90-day period, said Hitchings.
The 1-hour training requires surgeons to perform a 4-step protocol and demonstrate unaided proficiency at training conclusion. Olympus will not sell its product to a facility until an advanced surgeon has been trained there, according to Hitchings. And many physicians are approaching their institutions inquiring about training now, she reports.
Applications for training will be submitted to the Olympus Professional Education Team for approval. “We want this to go well. We know that there are many physicians who are hoping that this becomes a good reality, and we want to make sure that it is done properly. The training process adheres to that agenda.”
Having the technology is step 1
OBG Management Board of Editors member Dr. Advincula struck an optimistic tone in his June 2016 Guest Editorial for the journal,6 indicating his belief that the “tissue morcellation pendulum,” which has swung toward non−minimally invasive approaches since 2014, can change direction. At the Olympus containment system official introduction event at AAGL, he expressed the same optimism:
“We now have technology that has the promise of being able to deliver to women a safe way to undergo tissue extraction, to undergo a minimally invasive surgical procedure. …When you combine innovation and education together, you ultimately are going to advance MIS worldwide. With all the things going on around the world today, I think it is important that women be able to have a choice, an autonomous choice with her physician. Having the technology that allows physicians to extract tissue safely, to give women the option of undergoing a minimally invasive surgery, is critically important. I look forward to seeing how we can continue to advance surgery. Partnership with clinicians and with industry, such as Olympus, is going to be key to the success of how we advance women’s health care in general.”
What do AAGL attendees have to say about it?
“It’s a good thing for the minimally invasive market,” said John B. Gebhart, MD, MS, vaginal hysterectomy representative at the star-studded Operating with the Stars event on Thursday, November 17, and Professor of Obstetrics and Gynecology at the Mayo Clinic in Rochester, Minnesota.
May Thomassee, MD, who practices in Lafayette, Louisiana, said that, for the past 3 years, she has been performing extracorporeal morcellation at her institution. “I think the new containment bag and morcellator devices that are attempting to be safer are a very good thing; however, my concern of introducing this new technology, such as bags, is that it may increase the cost within our health care system. We have had great success, and patients feel that they have options when we offer them—after informed consent and appropriate preoperative workup—an abdominal, vaginal, or extracorporeal morcellation approach.”
As a developer and proponent of the Extracorporeal Tissue Extraction (ExCITE) technique, Mireille Truong, MD, who demonstrated the ExCITE surgical approach with Dr. Advincula as part of the Research and Science Plenary here at AAGL, said, “I think the PneumoLiner is a great example of creativity and innovation. It’s good that we now have an FDA-approved device to offer and counsel patients as one of many options.” She added that, overall, the morcellation controversy has been “a positive experience. We have learned better as a community about how to approach new technology.”
In the 11 studies that have examined the incidence of leiomyosarcoma (LMS) since the 2014 communications by the US Food and Drug Administration (FDA),1 Dr. Matthew Siedhoff and colleagues found that the cumulative LMS incidence in 318,006 women was 0.0017%, or approximately 1 in 600. This is according to data Dr. Seidhoff presented November 16, 2016, at the 45th annual AAGL Global Congress on MIGS.2 This reported risk is smaller than the 1 in 350 cited by the FDA in its 2014 notice.1 Dr. Seidhoff concluded that, particularly in women aged younger than 50 years, minimally invasive hysterectomy remains a safe option for the informed patient to consider.
Regardless of the incidence of unsuspected LMS found in the studies published since 2014, what have been the practice changes among gynecologic surgeons as a result of the FDA’s 2014 actions? Kerac N. Falk, MD, explored this question with his colleagues at the Icahn School of Medicine in New York, New York. He presented these findings to AAGL congress attendees on November 16 in Orlando, Florida.3 Notably, of 197 responders to a survey sent to members of the Society of Gynecologic Oncologists, 12.5% reported decreasing their use of power morcellation. A full 38.8% reported discontinuing altogether the use of a power morcellator.
One in 5 (20%) of gyn oncologists previously using power morcellation reported switching to laparotomy. Importantly, the drive for the switch was “driven by media, patient request, and the FDA rather than physician choice,” Falk said.
What if physicians, and patients, have another choice?
Here at the AAGL meeting, Olympus announced the FDA clearance, marketing, and initial training on its contained tissue extraction system—the PneumoLiner containment device and its accompanying laparoscopic PK Morcellator (FIGURE).

Both tools, FDA cleared in April and October 2016, respectively, provide low-risk, appropriate women with “an improved safety device,” said Jubilee Brown, MD, AAGL representative on power morcellation to the FDA and Associate Director of Gynecologic Oncology at the Levine Cancer Institute of the Carolinas HealthCare System in Charlotte, North Carolina.
“We have found at our institution that we have had to do more opens and minilaps on patients without the option for power morcellation, and this new device offers a way for us not to have to do that. Minimally invasive surgery stays truly minimally invasive surgery,” said Dr. Brown.
“Although I have a handful of patients who have chosen open surgery over minimally invasive surgery when MIS was appropriate, by and large most patients prefer the minimally invasive approach to surgery—especially when they learn that they have reduced risk for complications, blood loss, and pain; will be back to normal life faster; and will have less cosmetic incisions,” said Dr. Brown. “We all have tried workarounds, but for low-risk, appropriate patients under FDA guidelines, this new device by Olympus brings us back to minimally invasive options, and that is a good thing.”
How does the Olympus containment system work?
The PneumoLiner is the first containment device to receive FDA market clearance that is designed for use with certain laparoscopic morcellators to isolate uterine tissue that is not suspected to contain cancer.4
The containment bag and morcellator are not indicated for use in women with tissue that is known or suspected to contain malignancy; and should not be used for removal of uterine tissue containing suspected fibroids in patients who are peri- or post-menopausal, or candidates for en bloc tissue removal vaginally or via mini-laparotomy.4
When insufflated, the PneumoLiner bag allows for space and surgeon visibility throughout the power morcellation procedure while maintaining a barrier to the escape of fluids, cells, and tissue fragments. The bag creates a barrier between the targeted tissue and nontargeted abdominal contents, minimizing the risk of inadvertent damage to adjacent structures, says Olympus.4 See this video, which demonstrates the procedure.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Filtration, immersion, and stress testing were conducted to demonstrate the PneumoLiner as impermeable to human cells, that it maintains its integrity following morcellation, and that its mechanical strength withholds forces in excess of those demonstrated during actual use.5 To support FDA 510 clearance of the PK Morcellator, Olympus performed additional testing with both devices used together, demonstrating compatibility.4
Surgeon training on new device use is rigid, comprehensive, and not to be overlooked
“This is one of the rare times in my career when, right out of the gate, we have a very rigid and comprehensive way of educating and training physicians on the proper utilization of a new technology (avoiding the cart-before-the-horse phenomenon, in which a clinician is given the tools without the proper education),” said AAGL immediate past president Arnold Advincula, MD, “and it is important to underscore that.” Dr. Advincula is the Levine Family Professor, Vice-Chair of Women’s Health, and Chief of Gynecology at Sloane Women’s Hospital, Columbia University Medical Center/New York-Presbyterian Hospital, New York, New York.
Training plans
Instead of its sales force, Olympus is having surgeons train other surgeons. Clinical Education Specialists, a small, select group of individuals within the company, also will be able to train. The required training follows a rigid protocol that was validated and submitted to the FDA as part of the approval process, said Jerilyn Hitchings, Director of Procedure Marketing at Olympus. After training up to 40 surgeons in the past 3 weeks, Olympus expects to train another 100 at AAGL.
“We have strict criteria for training, including that they are advanced laparoscopists,” fulfilling a minimum number of surgeries within a 90-day period, said Hitchings.
The 1-hour training requires surgeons to perform a 4-step protocol and demonstrate unaided proficiency at training conclusion. Olympus will not sell its product to a facility until an advanced surgeon has been trained there, according to Hitchings. And many physicians are approaching their institutions inquiring about training now, she reports.
Applications for training will be submitted to the Olympus Professional Education Team for approval. “We want this to go well. We know that there are many physicians who are hoping that this becomes a good reality, and we want to make sure that it is done properly. The training process adheres to that agenda.”
Having the technology is step 1
OBG Management Board of Editors member Dr. Advincula struck an optimistic tone in his June 2016 Guest Editorial for the journal,6 indicating his belief that the “tissue morcellation pendulum,” which has swung toward non−minimally invasive approaches since 2014, can change direction. At the Olympus containment system official introduction event at AAGL, he expressed the same optimism:
“We now have technology that has the promise of being able to deliver to women a safe way to undergo tissue extraction, to undergo a minimally invasive surgical procedure. …When you combine innovation and education together, you ultimately are going to advance MIS worldwide. With all the things going on around the world today, I think it is important that women be able to have a choice, an autonomous choice with her physician. Having the technology that allows physicians to extract tissue safely, to give women the option of undergoing a minimally invasive surgery, is critically important. I look forward to seeing how we can continue to advance surgery. Partnership with clinicians and with industry, such as Olympus, is going to be key to the success of how we advance women’s health care in general.”
What do AAGL attendees have to say about it?
“It’s a good thing for the minimally invasive market,” said John B. Gebhart, MD, MS, vaginal hysterectomy representative at the star-studded Operating with the Stars event on Thursday, November 17, and Professor of Obstetrics and Gynecology at the Mayo Clinic in Rochester, Minnesota.
May Thomassee, MD, who practices in Lafayette, Louisiana, said that, for the past 3 years, she has been performing extracorporeal morcellation at her institution. “I think the new containment bag and morcellator devices that are attempting to be safer are a very good thing; however, my concern of introducing this new technology, such as bags, is that it may increase the cost within our health care system. We have had great success, and patients feel that they have options when we offer them—after informed consent and appropriate preoperative workup—an abdominal, vaginal, or extracorporeal morcellation approach.”
As a developer and proponent of the Extracorporeal Tissue Extraction (ExCITE) technique, Mireille Truong, MD, who demonstrated the ExCITE surgical approach with Dr. Advincula as part of the Research and Science Plenary here at AAGL, said, “I think the PneumoLiner is a great example of creativity and innovation. It’s good that we now have an FDA-approved device to offer and counsel patients as one of many options.” She added that, overall, the morcellation controversy has been “a positive experience. We have learned better as a community about how to approach new technology.”
- US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. April 17, 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm. Updated November 24, 2014. Accessed November 17, 2016.
- Siedhoff MT, Doll KM, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation versus abdominal hysterectomy for presumed uterine leiomyomata: an updated decision analysis. J Minim Invasiv Gynecol. 2016;23(7):S4-S5.
- Mandelberger AH, Mathews S, Chuang L. Practice changes in power morcellation among gynecologic-oncologists since 2014. J Minim Invasiv Gynecol. 2016;23(7):S3.
Olympus introduces first-of-its-kind contained tissue extraction system, restoring healthcare option for gynecologists and women [press release]. November 16, 2016. Olympus website. http://www.olympusamerica.com/corporate/corp_presscenter_headline.asp?pressNo=2079. Accessed November 16, 2016.
- FDA allows marketing of first-of-kind tissue containment system for use with certain laparoscopic power morcellators in select patients. FDA website. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm494650.htm. Updated April 7, 2016. Accessed November 16, 2016.
- Advincula AP. Tissue extraction: can the pendulum change direction? OBG Manag. 2016;28(6):8, 10, 12.
- US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. April 17, 2014. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm. Updated November 24, 2014. Accessed November 17, 2016.
- Siedhoff MT, Doll KM, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation versus abdominal hysterectomy for presumed uterine leiomyomata: an updated decision analysis. J Minim Invasiv Gynecol. 2016;23(7):S4-S5.
- Mandelberger AH, Mathews S, Chuang L. Practice changes in power morcellation among gynecologic-oncologists since 2014. J Minim Invasiv Gynecol. 2016;23(7):S3.
Olympus introduces first-of-its-kind contained tissue extraction system, restoring healthcare option for gynecologists and women [press release]. November 16, 2016. Olympus website. http://www.olympusamerica.com/corporate/corp_presscenter_headline.asp?pressNo=2079. Accessed November 16, 2016.
- FDA allows marketing of first-of-kind tissue containment system for use with certain laparoscopic power morcellators in select patients. FDA website. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm494650.htm. Updated April 7, 2016. Accessed November 16, 2016.
- Advincula AP. Tissue extraction: can the pendulum change direction? OBG Manag. 2016;28(6):8, 10, 12.
MIGS for infertility: Surgery can address QoL and pathology concerns that ART can’t, remind expert surgeons at AAGL 2016
Although patients have more assisted reproductive techniques (ART) available in recent years, management of infertility through minimally invasive surgical avenues can confront quality of life (QoL) and pathology concerns with birth rates equal to those with ART. This was a main takeaway in a packed ballroom in Orlando, Florida, at the 45th Global Congress of the AAGL. In this session, G. David Adamson, MD, brought together 3 top minimally invasive gynecologic surgeons to discuss clinical decisions in the overall and specific surgical management of: endometriomas and endometriosis, including deeply infiltrating disease; pelvic adhesions; distal tubal injury/occlusion; and proximal tubal occlusion by hysteroscopy.
Tommaso Falcone, MD, maintained that many patients (up to 85%) have pain with endometriomas, and addressing QoL for these women, with surgery versus managing their infertility only with in vitro fertilization (IVF), is an important consideration. Dr. Adamson noted that, “although there are no RCT data to guide management of endometriomas, we do have reasonable data to counsel patients on surgery versus IVF, with clinical considerations including patient age, presence of pain, and size of the endometrioma.”
Antonio Gargiulo, MD, advised attendees that when counseling patients on the role of laparoscopy in adhesiolysis to consider (1) that adhesions interfere with gamete and embryo transplant, (2) retrospective data from a small study show a positive effect of adhesiolysis in infertility, and (3) that the effect is dependent on the ASRM Adhesion Score. Regarding laparoscopy for distal tubal inclusion, he noted that case selection is important, as surgery can restore anatomic integrity but not functional integrity. In addition, he pointed out that neosalpingectomy before IVF should be considered in young women with mild hydrosalpinges when male factor infertility is present.
For proximal tubal occlusion, Dr. Gargiulo noted that hysteroscopy catheterization has diagnostic and therapeutic value, with contraindications including infection, inflammation, male factor infertility, and prior tubal surgery.
“Surgeons must offer and understand ART alternatives so that they can offer patient-centered choices,” said Dr. Gargiulo.
Finally, when does Dr. Leila Adamyan of the Federal State Institution Research Center for Obstetrics, Gynecology, and Perinatology of the V.I. Kulakov Russian Federation perform myomectomy before IVF? In the presence of:
- submucosal myoma
- myoma greater than 4 cm in size
- multiple myoma.
When sarcoma is suspected, she advises the use of endobags.
Although patients have more assisted reproductive techniques (ART) available in recent years, management of infertility through minimally invasive surgical avenues can confront quality of life (QoL) and pathology concerns with birth rates equal to those with ART. This was a main takeaway in a packed ballroom in Orlando, Florida, at the 45th Global Congress of the AAGL. In this session, G. David Adamson, MD, brought together 3 top minimally invasive gynecologic surgeons to discuss clinical decisions in the overall and specific surgical management of: endometriomas and endometriosis, including deeply infiltrating disease; pelvic adhesions; distal tubal injury/occlusion; and proximal tubal occlusion by hysteroscopy.
Tommaso Falcone, MD, maintained that many patients (up to 85%) have pain with endometriomas, and addressing QoL for these women, with surgery versus managing their infertility only with in vitro fertilization (IVF), is an important consideration. Dr. Adamson noted that, “although there are no RCT data to guide management of endometriomas, we do have reasonable data to counsel patients on surgery versus IVF, with clinical considerations including patient age, presence of pain, and size of the endometrioma.”
Antonio Gargiulo, MD, advised attendees that when counseling patients on the role of laparoscopy in adhesiolysis to consider (1) that adhesions interfere with gamete and embryo transplant, (2) retrospective data from a small study show a positive effect of adhesiolysis in infertility, and (3) that the effect is dependent on the ASRM Adhesion Score. Regarding laparoscopy for distal tubal inclusion, he noted that case selection is important, as surgery can restore anatomic integrity but not functional integrity. In addition, he pointed out that neosalpingectomy before IVF should be considered in young women with mild hydrosalpinges when male factor infertility is present.
For proximal tubal occlusion, Dr. Gargiulo noted that hysteroscopy catheterization has diagnostic and therapeutic value, with contraindications including infection, inflammation, male factor infertility, and prior tubal surgery.
“Surgeons must offer and understand ART alternatives so that they can offer patient-centered choices,” said Dr. Gargiulo.
Finally, when does Dr. Leila Adamyan of the Federal State Institution Research Center for Obstetrics, Gynecology, and Perinatology of the V.I. Kulakov Russian Federation perform myomectomy before IVF? In the presence of:
- submucosal myoma
- myoma greater than 4 cm in size
- multiple myoma.
When sarcoma is suspected, she advises the use of endobags.
Although patients have more assisted reproductive techniques (ART) available in recent years, management of infertility through minimally invasive surgical avenues can confront quality of life (QoL) and pathology concerns with birth rates equal to those with ART. This was a main takeaway in a packed ballroom in Orlando, Florida, at the 45th Global Congress of the AAGL. In this session, G. David Adamson, MD, brought together 3 top minimally invasive gynecologic surgeons to discuss clinical decisions in the overall and specific surgical management of: endometriomas and endometriosis, including deeply infiltrating disease; pelvic adhesions; distal tubal injury/occlusion; and proximal tubal occlusion by hysteroscopy.
Tommaso Falcone, MD, maintained that many patients (up to 85%) have pain with endometriomas, and addressing QoL for these women, with surgery versus managing their infertility only with in vitro fertilization (IVF), is an important consideration. Dr. Adamson noted that, “although there are no RCT data to guide management of endometriomas, we do have reasonable data to counsel patients on surgery versus IVF, with clinical considerations including patient age, presence of pain, and size of the endometrioma.”
Antonio Gargiulo, MD, advised attendees that when counseling patients on the role of laparoscopy in adhesiolysis to consider (1) that adhesions interfere with gamete and embryo transplant, (2) retrospective data from a small study show a positive effect of adhesiolysis in infertility, and (3) that the effect is dependent on the ASRM Adhesion Score. Regarding laparoscopy for distal tubal inclusion, he noted that case selection is important, as surgery can restore anatomic integrity but not functional integrity. In addition, he pointed out that neosalpingectomy before IVF should be considered in young women with mild hydrosalpinges when male factor infertility is present.
For proximal tubal occlusion, Dr. Gargiulo noted that hysteroscopy catheterization has diagnostic and therapeutic value, with contraindications including infection, inflammation, male factor infertility, and prior tubal surgery.
“Surgeons must offer and understand ART alternatives so that they can offer patient-centered choices,” said Dr. Gargiulo.
Finally, when does Dr. Leila Adamyan of the Federal State Institution Research Center for Obstetrics, Gynecology, and Perinatology of the V.I. Kulakov Russian Federation perform myomectomy before IVF? In the presence of:
- submucosal myoma
- myoma greater than 4 cm in size
- multiple myoma.
When sarcoma is suspected, she advises the use of endobags.
NAMS 2016 hormone therapy position statement
JoAnn Pinkerton, MD, Professor of Obstetrics and Gynecology at the University of Virginia, Executive Director of the North American Menopause Society (NAMS), and OBG Management Board of Editors Member, revealed the 2016 NAMS position statement on hormone therapy (HT) in Orlando, Florida, on Thursday, October 6, at the NAMS 2016 Annual Scientific Meeting.
The process of consensus among the more than 20 menopause experts who authored the 2016 statement was at times a challenge, indicated Pinkerton, given the variance in views on the significance of published clinical trial findings since the Society’s 20121 HT position statement. Over a 9-month period, the experts developed guidelines for clinicians, using levels of evidence to identify strength of the recommendations.
The clearest benefit for HT to treat hot flashes and prevent bone loss was found for women aged younger than 60 years and within 10 years of menopause onset.
According to the 2016 statement presented at NAMS:
Level I US Food and Drug Administration (FDA)-approved indications for HT include:
- as first-line therapy for women with vasomotor symptoms (VMS) of menopause without contraindications
- possible first-line therapy for prevention of bone loss and fracture in postmenopausal women at elevated risk for fracture (primarily for women aged younger than 60 years and within 10 years of menopause onset)
- low-dose vaginal estrogen as first-line treatment for women with isolated genitourinary symptoms caused by menopause (genitourinary syndrome of menopause [GSM]/vulvovaginal atrophy).
Level II FDA-approved indications for HT include:
- at least until age 52 (the median age of menopause onset) for women with early onset menopause (women with hypogonadism, primary ovarian insufficiency, or premature surgical menopause) and no HT contraindications.
Other level II indications, with observational data indicating benefit over risk, for HT include:
- at least until the median age of menopause for women with early onset menopause
- consideration among women with a family history of breast cancer, although family history is one risk among many for breast cancer that should be assessed
- benefit/risk consideration for women with a BRCA gene mutation who have undergone risk-reducing oophorectomy
- consideration of systemic use until the median age of menopause—after appropriate counseling and in the absence of HT contraindications, with longer duration of HT use individualized.
Level III indications for HT include:
- individualized decisions on use after the age of 60. (The position statement authors did not find that the current Beers criteria recommendation to routinely discontinue HT at age 65 was supported by data.)
The 2016 bottom line on HT
Overall, HT has clear benefits for the treatment of VMS and bone loss prevention, according to the presented position statement. These benefits are most favorable among women aged younger than 60 years who are within 10 years of menopause onset and have no contraindications to HT use. Women older than age 60 who initiate HT beyond 10 years of menopause onset appear to have a less favorable benefit-risk ratio because of elevated risks of coronary heart disease, stroke, venous thromboembolism, and dementia.
The risks of HT vary among women depending on the HT type, duration of use, administration route, timing of treatment initiation, and whether a progestogen is needed. (With longer HT use, estrogen therapy is more favorable than estrogen-progestin therapy.) Therefore, HT should be individualized and reevaluated periodically to maximize the benefits as well as minimize the risks of use, according to the position statement.
Nonhormonal therapies for menopausal symptoms
The Society released its position on nonhormonal management of menopause-associated VMS in 2015.2 Based on examination of 340 original research articles and 105 systematic reviews, clinical and research experts categorized therapies as recommended, recommended with caution, and not recommended at this time.
Recommended non-HT to reduce VMS include:
- cognitive-behavioral therapy
- clinical hypnosis
- low-dose salt of paroxetine (FDA approved for menopausal VMS management)
- other SSRIs/SNRIs
- gabapentinoids
- clonidine.
Recommended-with-caution non-HT for VMS include:
- weight loss
- stress reduction (mindfulness based)
- S-equol derivatives of soy isoflavones
- stellate ganglion block.
Not recommended non-HT for VMS due to negative, insufficient, or inconclusive data include:
- cooling techniques
- avoidance of triggers
- exercise
- yoga
- paced respiration
- relaxation
- over-the-counter supplements and herbs
- acupuncture
- calibration of neural oscillations
- chiropractic interventions.
Note that the NAMS 2016 Hormone Therapy Position Statement was presented at the 2016 Annual Scientific Meeting of the North American Menopause Society, but the statement is not yet published.
- North American Menopause Society. The 2012 hormone therapy position statement of: The North American Menopause Society. Menopause. 2012;19(3):257−271.
- Nonhormonal management of menopause-associated vasomotor symptoms: 2015 position statement of The North American Menopause Society. Menopause. 2015;(11):1155−1172.
JoAnn Pinkerton, MD, Professor of Obstetrics and Gynecology at the University of Virginia, Executive Director of the North American Menopause Society (NAMS), and OBG Management Board of Editors Member, revealed the 2016 NAMS position statement on hormone therapy (HT) in Orlando, Florida, on Thursday, October 6, at the NAMS 2016 Annual Scientific Meeting.
The process of consensus among the more than 20 menopause experts who authored the 2016 statement was at times a challenge, indicated Pinkerton, given the variance in views on the significance of published clinical trial findings since the Society’s 20121 HT position statement. Over a 9-month period, the experts developed guidelines for clinicians, using levels of evidence to identify strength of the recommendations.
The clearest benefit for HT to treat hot flashes and prevent bone loss was found for women aged younger than 60 years and within 10 years of menopause onset.
According to the 2016 statement presented at NAMS:
Level I US Food and Drug Administration (FDA)-approved indications for HT include:
- as first-line therapy for women with vasomotor symptoms (VMS) of menopause without contraindications
- possible first-line therapy for prevention of bone loss and fracture in postmenopausal women at elevated risk for fracture (primarily for women aged younger than 60 years and within 10 years of menopause onset)
- low-dose vaginal estrogen as first-line treatment for women with isolated genitourinary symptoms caused by menopause (genitourinary syndrome of menopause [GSM]/vulvovaginal atrophy).
Level II FDA-approved indications for HT include:
- at least until age 52 (the median age of menopause onset) for women with early onset menopause (women with hypogonadism, primary ovarian insufficiency, or premature surgical menopause) and no HT contraindications.
Other level II indications, with observational data indicating benefit over risk, for HT include:
- at least until the median age of menopause for women with early onset menopause
- consideration among women with a family history of breast cancer, although family history is one risk among many for breast cancer that should be assessed
- benefit/risk consideration for women with a BRCA gene mutation who have undergone risk-reducing oophorectomy
- consideration of systemic use until the median age of menopause—after appropriate counseling and in the absence of HT contraindications, with longer duration of HT use individualized.
Level III indications for HT include:
- individualized decisions on use after the age of 60. (The position statement authors did not find that the current Beers criteria recommendation to routinely discontinue HT at age 65 was supported by data.)
The 2016 bottom line on HT
Overall, HT has clear benefits for the treatment of VMS and bone loss prevention, according to the presented position statement. These benefits are most favorable among women aged younger than 60 years who are within 10 years of menopause onset and have no contraindications to HT use. Women older than age 60 who initiate HT beyond 10 years of menopause onset appear to have a less favorable benefit-risk ratio because of elevated risks of coronary heart disease, stroke, venous thromboembolism, and dementia.
The risks of HT vary among women depending on the HT type, duration of use, administration route, timing of treatment initiation, and whether a progestogen is needed. (With longer HT use, estrogen therapy is more favorable than estrogen-progestin therapy.) Therefore, HT should be individualized and reevaluated periodically to maximize the benefits as well as minimize the risks of use, according to the position statement.
Nonhormonal therapies for menopausal symptoms
The Society released its position on nonhormonal management of menopause-associated VMS in 2015.2 Based on examination of 340 original research articles and 105 systematic reviews, clinical and research experts categorized therapies as recommended, recommended with caution, and not recommended at this time.
Recommended non-HT to reduce VMS include:
- cognitive-behavioral therapy
- clinical hypnosis
- low-dose salt of paroxetine (FDA approved for menopausal VMS management)
- other SSRIs/SNRIs
- gabapentinoids
- clonidine.
Recommended-with-caution non-HT for VMS include:
- weight loss
- stress reduction (mindfulness based)
- S-equol derivatives of soy isoflavones
- stellate ganglion block.
Not recommended non-HT for VMS due to negative, insufficient, or inconclusive data include:
- cooling techniques
- avoidance of triggers
- exercise
- yoga
- paced respiration
- relaxation
- over-the-counter supplements and herbs
- acupuncture
- calibration of neural oscillations
- chiropractic interventions.
Note that the NAMS 2016 Hormone Therapy Position Statement was presented at the 2016 Annual Scientific Meeting of the North American Menopause Society, but the statement is not yet published.
JoAnn Pinkerton, MD, Professor of Obstetrics and Gynecology at the University of Virginia, Executive Director of the North American Menopause Society (NAMS), and OBG Management Board of Editors Member, revealed the 2016 NAMS position statement on hormone therapy (HT) in Orlando, Florida, on Thursday, October 6, at the NAMS 2016 Annual Scientific Meeting.
The process of consensus among the more than 20 menopause experts who authored the 2016 statement was at times a challenge, indicated Pinkerton, given the variance in views on the significance of published clinical trial findings since the Society’s 20121 HT position statement. Over a 9-month period, the experts developed guidelines for clinicians, using levels of evidence to identify strength of the recommendations.
The clearest benefit for HT to treat hot flashes and prevent bone loss was found for women aged younger than 60 years and within 10 years of menopause onset.
According to the 2016 statement presented at NAMS:
Level I US Food and Drug Administration (FDA)-approved indications for HT include:
- as first-line therapy for women with vasomotor symptoms (VMS) of menopause without contraindications
- possible first-line therapy for prevention of bone loss and fracture in postmenopausal women at elevated risk for fracture (primarily for women aged younger than 60 years and within 10 years of menopause onset)
- low-dose vaginal estrogen as first-line treatment for women with isolated genitourinary symptoms caused by menopause (genitourinary syndrome of menopause [GSM]/vulvovaginal atrophy).
Level II FDA-approved indications for HT include:
- at least until age 52 (the median age of menopause onset) for women with early onset menopause (women with hypogonadism, primary ovarian insufficiency, or premature surgical menopause) and no HT contraindications.
Other level II indications, with observational data indicating benefit over risk, for HT include:
- at least until the median age of menopause for women with early onset menopause
- consideration among women with a family history of breast cancer, although family history is one risk among many for breast cancer that should be assessed
- benefit/risk consideration for women with a BRCA gene mutation who have undergone risk-reducing oophorectomy
- consideration of systemic use until the median age of menopause—after appropriate counseling and in the absence of HT contraindications, with longer duration of HT use individualized.
Level III indications for HT include:
- individualized decisions on use after the age of 60. (The position statement authors did not find that the current Beers criteria recommendation to routinely discontinue HT at age 65 was supported by data.)
The 2016 bottom line on HT
Overall, HT has clear benefits for the treatment of VMS and bone loss prevention, according to the presented position statement. These benefits are most favorable among women aged younger than 60 years who are within 10 years of menopause onset and have no contraindications to HT use. Women older than age 60 who initiate HT beyond 10 years of menopause onset appear to have a less favorable benefit-risk ratio because of elevated risks of coronary heart disease, stroke, venous thromboembolism, and dementia.
The risks of HT vary among women depending on the HT type, duration of use, administration route, timing of treatment initiation, and whether a progestogen is needed. (With longer HT use, estrogen therapy is more favorable than estrogen-progestin therapy.) Therefore, HT should be individualized and reevaluated periodically to maximize the benefits as well as minimize the risks of use, according to the position statement.
Nonhormonal therapies for menopausal symptoms
The Society released its position on nonhormonal management of menopause-associated VMS in 2015.2 Based on examination of 340 original research articles and 105 systematic reviews, clinical and research experts categorized therapies as recommended, recommended with caution, and not recommended at this time.
Recommended non-HT to reduce VMS include:
- cognitive-behavioral therapy
- clinical hypnosis
- low-dose salt of paroxetine (FDA approved for menopausal VMS management)
- other SSRIs/SNRIs
- gabapentinoids
- clonidine.
Recommended-with-caution non-HT for VMS include:
- weight loss
- stress reduction (mindfulness based)
- S-equol derivatives of soy isoflavones
- stellate ganglion block.
Not recommended non-HT for VMS due to negative, insufficient, or inconclusive data include:
- cooling techniques
- avoidance of triggers
- exercise
- yoga
- paced respiration
- relaxation
- over-the-counter supplements and herbs
- acupuncture
- calibration of neural oscillations
- chiropractic interventions.
Note that the NAMS 2016 Hormone Therapy Position Statement was presented at the 2016 Annual Scientific Meeting of the North American Menopause Society, but the statement is not yet published.
- North American Menopause Society. The 2012 hormone therapy position statement of: The North American Menopause Society. Menopause. 2012;19(3):257−271.
- Nonhormonal management of menopause-associated vasomotor symptoms: 2015 position statement of The North American Menopause Society. Menopause. 2015;(11):1155−1172.
- North American Menopause Society. The 2012 hormone therapy position statement of: The North American Menopause Society. Menopause. 2012;19(3):257−271.
- Nonhormonal management of menopause-associated vasomotor symptoms: 2015 position statement of The North American Menopause Society. Menopause. 2015;(11):1155−1172.
Elective induction of labor at 39 (vs 41) weeks: Caveats and considerations
Tasked with tackling the literature on the subject and debating the question of whether or not it is best to electively induce labor in women with low-risk pregnancies at 39 weeks (vs at 41 weeks after expectant management), Errol Norwitz, MD, PhD, Chairman of the Department of Obstetrics and Gynecology and Professor at Tufts University School of Medicine in Boston, Massachusetts, and Charles Lockwood, MD, Senior Vice President at the University of South Florida (USF) and Dean of the USF Health Morsani College of Medicine in Tampa came to the same conclusion: Elective induction of labor (eIOL) at 39 weeks is superior to expectant management when it comes to fetal outcomes.
In addition, they both agreed that complication rates to the mother (ie, number of cesarean deliveries [CDs]) would not be increased, and possibly even reduced, with eIOL at 39 weeks versus 41 weeks. Dr. Norwitz postulated that, with IOL there is no increase in CD rate in multiparous women and nulliparous women with a favorable cervical exam but that there likely could be an increase in the CD rate for nulliparous women with an unfavorable cervical exam.
The finding that eIOL at 39 weeks is better than at 41 weeks for the infant is likely due to a bigger baby size past 39 weeks (with more traumatic deliveries) and higher rates of postmaturity complications, said Dr. Lockwood. And for the mother, eIOL at 39 weeks can reduce risks—of preeclampsia, abruption, sepsis, and others—the presenters pointed out.
Arriving at their conclusions: The dataDr. Norwitz explained the challenge before them in this unusual “debate.” “In ObGyn we all read the same literature but we often come away with very different takes as to what the implications are and how we incorporate this into our management algorithms. Instead of taking a pro/con approach, with one assigned to ‘yes’ and the other assigned to ‘no,’ and selectively picking out the literature to support our positions, what we did was we each went away, read the literature, synthesized it, and tried to answer this question for ourselves.”
Dr. Norwitz, who is widely published and known for his research on the causes and prevention of preeclampsia and preterm labor, examined and presented the published literature for benefit and harms to the fetus and mother in continuing pregnancy past 39 weeks.
Dr. Lockwood also examined the literature, including a large population cohort of about 1.27 million women that examined CD rates, perinatal mortality, and neonatal and maternal outcomes of eIOL at 39 weeks versus expectant management.1 He presented, however, that the best evidence to compare the question at hand would be a randomized clinical trial comparing specifically eIOL at 39 weeks versus expectant management, with IOL at 41 weeks. To be powered to detect a difference in perinatal and maternal mortality, this trial would need to include 2.2 to 12.6 million women, he maintained. “When empirical evidence doesn’t exist, the only alternative is some kind of other modeling,” he said. Therefore, he and a team of researchers conducted a Monte Carlo microsimulation modeling decision analysis, taking into account “all outcomes and all preferences that we possibly could cull from the literature.”
Which women actually could benefit from eIOL at 39 weeks?Women with high-risk pregnancies were not included in this debate or considered. Dr. Norwitz clearly defined his case patient at the outset as a 22-year-old G1 at 39 0/7 weeks who has had an uncomplicated pregnancy but is now complaining of decreased fetal movement and tells you that she is worried because her sister lost her baby at 40 weeks to stillbirth. She specifically asks, “Doctor, why can’t you induce my labor now?”
What counseling a patient about the risks/benefits of eIOL at 39 weeks would requireTwo fundamentals would need to be ensured. The first: precise gestational dating. Dr. Norwitz pointed out that menstrual history can be inaccurate, especially in women with irregular cycles, who are taking hormonal contraception, or who have intermenstrual bleeding. “Early dating ultrasound is the best way to date pregnancies and probably should be done routinely,” although it is not currently standard of care in the United States, he said.
The second fundamental: a true induction of labor process, not one that involves “stopping at 5 PM,” said Dr. Lockwood.
“Although Dr. Lockwood’s 5-PM statement was made tongue-in-cheek,” said Dr. Norwitz after the debate, “he certainly was implying that a genuine effort should be made to effect a vaginal delivery—that is, giving the most effective cervical ripening agents, allowing enough time to pass, and defining clearly the criteria for failed IOL. You shouldn’t just throw the towel in at 5 PM because you want to go home.”
Cost implicationsElectively inducing labor in all women with low-risk pregnancies at 39 weeks is a strategy with unknown cost implications, and the cost difference between this strategy and expectant management up to 41 weeks is not known.
“We need to be sure that we understand the cost implications of these strategies, which of course would need to be balanced against the potential perinatal and maternal morbidity and fetal death,” said Dr. Lockwood.
The meaning of “elective”Dr. Norwitz also made the point postdebate that the American College of Obstetricians and Gynecologists (ACOG) does not support elective IOL prior to 39 weeks’ gestation. “The key term here is ‘elective,’" he said, "which refers to a delivery without a clear medical or obstetric indication. ACOG does support delivery prior to 39 weeks’ gestation, there just needs to be an appropriate indication.”
1. Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers J, Norman JE. Outcomes of elective induction of labour compared with expectant management: population based study. BMJ. 2012;344:e2838.
Tasked with tackling the literature on the subject and debating the question of whether or not it is best to electively induce labor in women with low-risk pregnancies at 39 weeks (vs at 41 weeks after expectant management), Errol Norwitz, MD, PhD, Chairman of the Department of Obstetrics and Gynecology and Professor at Tufts University School of Medicine in Boston, Massachusetts, and Charles Lockwood, MD, Senior Vice President at the University of South Florida (USF) and Dean of the USF Health Morsani College of Medicine in Tampa came to the same conclusion: Elective induction of labor (eIOL) at 39 weeks is superior to expectant management when it comes to fetal outcomes.
In addition, they both agreed that complication rates to the mother (ie, number of cesarean deliveries [CDs]) would not be increased, and possibly even reduced, with eIOL at 39 weeks versus 41 weeks. Dr. Norwitz postulated that, with IOL there is no increase in CD rate in multiparous women and nulliparous women with a favorable cervical exam but that there likely could be an increase in the CD rate for nulliparous women with an unfavorable cervical exam.
The finding that eIOL at 39 weeks is better than at 41 weeks for the infant is likely due to a bigger baby size past 39 weeks (with more traumatic deliveries) and higher rates of postmaturity complications, said Dr. Lockwood. And for the mother, eIOL at 39 weeks can reduce risks—of preeclampsia, abruption, sepsis, and others—the presenters pointed out.
Arriving at their conclusions: The dataDr. Norwitz explained the challenge before them in this unusual “debate.” “In ObGyn we all read the same literature but we often come away with very different takes as to what the implications are and how we incorporate this into our management algorithms. Instead of taking a pro/con approach, with one assigned to ‘yes’ and the other assigned to ‘no,’ and selectively picking out the literature to support our positions, what we did was we each went away, read the literature, synthesized it, and tried to answer this question for ourselves.”
Dr. Norwitz, who is widely published and known for his research on the causes and prevention of preeclampsia and preterm labor, examined and presented the published literature for benefit and harms to the fetus and mother in continuing pregnancy past 39 weeks.
Dr. Lockwood also examined the literature, including a large population cohort of about 1.27 million women that examined CD rates, perinatal mortality, and neonatal and maternal outcomes of eIOL at 39 weeks versus expectant management.1 He presented, however, that the best evidence to compare the question at hand would be a randomized clinical trial comparing specifically eIOL at 39 weeks versus expectant management, with IOL at 41 weeks. To be powered to detect a difference in perinatal and maternal mortality, this trial would need to include 2.2 to 12.6 million women, he maintained. “When empirical evidence doesn’t exist, the only alternative is some kind of other modeling,” he said. Therefore, he and a team of researchers conducted a Monte Carlo microsimulation modeling decision analysis, taking into account “all outcomes and all preferences that we possibly could cull from the literature.”
Which women actually could benefit from eIOL at 39 weeks?Women with high-risk pregnancies were not included in this debate or considered. Dr. Norwitz clearly defined his case patient at the outset as a 22-year-old G1 at 39 0/7 weeks who has had an uncomplicated pregnancy but is now complaining of decreased fetal movement and tells you that she is worried because her sister lost her baby at 40 weeks to stillbirth. She specifically asks, “Doctor, why can’t you induce my labor now?”
What counseling a patient about the risks/benefits of eIOL at 39 weeks would requireTwo fundamentals would need to be ensured. The first: precise gestational dating. Dr. Norwitz pointed out that menstrual history can be inaccurate, especially in women with irregular cycles, who are taking hormonal contraception, or who have intermenstrual bleeding. “Early dating ultrasound is the best way to date pregnancies and probably should be done routinely,” although it is not currently standard of care in the United States, he said.
The second fundamental: a true induction of labor process, not one that involves “stopping at 5 PM,” said Dr. Lockwood.
“Although Dr. Lockwood’s 5-PM statement was made tongue-in-cheek,” said Dr. Norwitz after the debate, “he certainly was implying that a genuine effort should be made to effect a vaginal delivery—that is, giving the most effective cervical ripening agents, allowing enough time to pass, and defining clearly the criteria for failed IOL. You shouldn’t just throw the towel in at 5 PM because you want to go home.”
Cost implicationsElectively inducing labor in all women with low-risk pregnancies at 39 weeks is a strategy with unknown cost implications, and the cost difference between this strategy and expectant management up to 41 weeks is not known.
“We need to be sure that we understand the cost implications of these strategies, which of course would need to be balanced against the potential perinatal and maternal morbidity and fetal death,” said Dr. Lockwood.
The meaning of “elective”Dr. Norwitz also made the point postdebate that the American College of Obstetricians and Gynecologists (ACOG) does not support elective IOL prior to 39 weeks’ gestation. “The key term here is ‘elective,’" he said, "which refers to a delivery without a clear medical or obstetric indication. ACOG does support delivery prior to 39 weeks’ gestation, there just needs to be an appropriate indication.”
Tasked with tackling the literature on the subject and debating the question of whether or not it is best to electively induce labor in women with low-risk pregnancies at 39 weeks (vs at 41 weeks after expectant management), Errol Norwitz, MD, PhD, Chairman of the Department of Obstetrics and Gynecology and Professor at Tufts University School of Medicine in Boston, Massachusetts, and Charles Lockwood, MD, Senior Vice President at the University of South Florida (USF) and Dean of the USF Health Morsani College of Medicine in Tampa came to the same conclusion: Elective induction of labor (eIOL) at 39 weeks is superior to expectant management when it comes to fetal outcomes.
In addition, they both agreed that complication rates to the mother (ie, number of cesarean deliveries [CDs]) would not be increased, and possibly even reduced, with eIOL at 39 weeks versus 41 weeks. Dr. Norwitz postulated that, with IOL there is no increase in CD rate in multiparous women and nulliparous women with a favorable cervical exam but that there likely could be an increase in the CD rate for nulliparous women with an unfavorable cervical exam.
The finding that eIOL at 39 weeks is better than at 41 weeks for the infant is likely due to a bigger baby size past 39 weeks (with more traumatic deliveries) and higher rates of postmaturity complications, said Dr. Lockwood. And for the mother, eIOL at 39 weeks can reduce risks—of preeclampsia, abruption, sepsis, and others—the presenters pointed out.
Arriving at their conclusions: The dataDr. Norwitz explained the challenge before them in this unusual “debate.” “In ObGyn we all read the same literature but we often come away with very different takes as to what the implications are and how we incorporate this into our management algorithms. Instead of taking a pro/con approach, with one assigned to ‘yes’ and the other assigned to ‘no,’ and selectively picking out the literature to support our positions, what we did was we each went away, read the literature, synthesized it, and tried to answer this question for ourselves.”
Dr. Norwitz, who is widely published and known for his research on the causes and prevention of preeclampsia and preterm labor, examined and presented the published literature for benefit and harms to the fetus and mother in continuing pregnancy past 39 weeks.
Dr. Lockwood also examined the literature, including a large population cohort of about 1.27 million women that examined CD rates, perinatal mortality, and neonatal and maternal outcomes of eIOL at 39 weeks versus expectant management.1 He presented, however, that the best evidence to compare the question at hand would be a randomized clinical trial comparing specifically eIOL at 39 weeks versus expectant management, with IOL at 41 weeks. To be powered to detect a difference in perinatal and maternal mortality, this trial would need to include 2.2 to 12.6 million women, he maintained. “When empirical evidence doesn’t exist, the only alternative is some kind of other modeling,” he said. Therefore, he and a team of researchers conducted a Monte Carlo microsimulation modeling decision analysis, taking into account “all outcomes and all preferences that we possibly could cull from the literature.”
Which women actually could benefit from eIOL at 39 weeks?Women with high-risk pregnancies were not included in this debate or considered. Dr. Norwitz clearly defined his case patient at the outset as a 22-year-old G1 at 39 0/7 weeks who has had an uncomplicated pregnancy but is now complaining of decreased fetal movement and tells you that she is worried because her sister lost her baby at 40 weeks to stillbirth. She specifically asks, “Doctor, why can’t you induce my labor now?”
What counseling a patient about the risks/benefits of eIOL at 39 weeks would requireTwo fundamentals would need to be ensured. The first: precise gestational dating. Dr. Norwitz pointed out that menstrual history can be inaccurate, especially in women with irregular cycles, who are taking hormonal contraception, or who have intermenstrual bleeding. “Early dating ultrasound is the best way to date pregnancies and probably should be done routinely,” although it is not currently standard of care in the United States, he said.
The second fundamental: a true induction of labor process, not one that involves “stopping at 5 PM,” said Dr. Lockwood.
“Although Dr. Lockwood’s 5-PM statement was made tongue-in-cheek,” said Dr. Norwitz after the debate, “he certainly was implying that a genuine effort should be made to effect a vaginal delivery—that is, giving the most effective cervical ripening agents, allowing enough time to pass, and defining clearly the criteria for failed IOL. You shouldn’t just throw the towel in at 5 PM because you want to go home.”
Cost implicationsElectively inducing labor in all women with low-risk pregnancies at 39 weeks is a strategy with unknown cost implications, and the cost difference between this strategy and expectant management up to 41 weeks is not known.
“We need to be sure that we understand the cost implications of these strategies, which of course would need to be balanced against the potential perinatal and maternal morbidity and fetal death,” said Dr. Lockwood.
The meaning of “elective”Dr. Norwitz also made the point postdebate that the American College of Obstetricians and Gynecologists (ACOG) does not support elective IOL prior to 39 weeks’ gestation. “The key term here is ‘elective,’" he said, "which refers to a delivery without a clear medical or obstetric indication. ACOG does support delivery prior to 39 weeks’ gestation, there just needs to be an appropriate indication.”
1. Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers J, Norman JE. Outcomes of elective induction of labour compared with expectant management: population based study. BMJ. 2012;344:e2838.
1. Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers J, Norman JE. Outcomes of elective induction of labour compared with expectant management: population based study. BMJ. 2012;344:e2838.
Do patients have a gender preference for their ObGyn?
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients’ gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting May 14−17, in Washington, DC.
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. “I was trying to decide if Obstetrics and Gynecology was the right field for me,” he said. “I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results.” After medical school Dr. Tobler pursued this current meta-analysis to address the conflicting results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association’s medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health’s database), Scopus (Elsevier’s abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically-identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.
“We were surprised by the numbers,” comments Dr. Tobler. “The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin.”
“We considered analyzing for age,” he said, “but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers—the Middle East and Africa. But in fact results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference.”
Updated May 20, 2016.
Reference
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider.Accessed May 18, 2016.
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients’ gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting May 14−17, in Washington, DC.
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. “I was trying to decide if Obstetrics and Gynecology was the right field for me,” he said. “I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results.” After medical school Dr. Tobler pursued this current meta-analysis to address the conflicting results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association’s medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health’s database), Scopus (Elsevier’s abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically-identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.
“We were surprised by the numbers,” comments Dr. Tobler. “The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin.”
“We considered analyzing for age,” he said, “but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers—the Middle East and Africa. But in fact results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference.”
Updated May 20, 2016.
Although multiple surveys have been published regarding patient gender preference when choosing an ObGyn, overall results have not been analyzed. To address this literature gap, Kyle J. Tobler, MD, and colleagues at the Womack Army Medical Center in Fort Bragg, North Carolina, and Uniformed Services University of the Health Sciences in Bethesda, Maryland, searched multiple sources to provide a conglomerate analysis of patients’ gender preference when choosing an ObGyn. An abstract describing their study was published in Obstetrics & Gynecology in May 2016 and presented at the American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting May 14−17, in Washington, DC.
A personal impetus for studying gender preference
The impetus for this project truly was initiated for Dr. Tobler when he was a 4th-year medical student. “I was trying to decide if Obstetrics and Gynecology was the right field for me,” he said. “I was discouraged by many people around me, who told me that men in ObGyn would not have a place, as female patients only wanted female ObGyns. And with the residency match at 60% to 70% women for ObGyn, it did seem that men would not have a place. Thus, I began searching the literature to verify if the question for gender preference for their ObGyn provider had been evaluated previously, and I found mixed results.” After medical school Dr. Tobler pursued this current meta-analysis to address the conflicting results.
Details of the study
Dr. Tobler and his colleagues explored PubMed, Embase, PsycINFO (American Psychological Association’s medical literature database), Cumulative Index to Nursing and Allied Health Literature (EBSCO Health’s database), Scopus (Elsevier’s abstract and citation database of peer-reviewed literature), and references of relevant articles. Included were 4,822 electronically-identified citations of English-language studies, including surveys administered to patients that specifically asked for gender preference of their ObGyn provider.
The researchers found that 23 studies met their inclusion criteria, comprising 14,736 patients. Overall, 8.3% (95% confidence interval [CI], 0.08-0.09) of ObGyn patients reported a preference for a male provider, 50.2% (95% CI, 0.49-0.51) preferred a female provider, and 41.3% (95% CI, 0.40-0.42) reported no gender preference when choosing an ObGyn.
What about US patients?
A subanalysis of studies (n = 9,861) conducted in the United States from 1999 to 2008 (with the last search undertaken in April 2015) showed that 8.4% (95% CI, 0.08-0.09) preferred a male ObGyn, 53.2% (95% CI, 0.52-0.54) preferred a female ObGyn, and 38.5% (95% CI, 0.38-0.39) had no gender preference.
“We were surprised by the numbers,” comments Dr. Tobler. “The general trend demonstrated a mix between no preference or a preference for female providers, but not by a large margin.”
“We considered analyzing for age,” he said, “but most of the studies gave a mean or median age value and were widely distributed. We were able, however, to break our analysis down into regions where one would expect a very strong preference for female providers—the Middle East and Africa. But in fact results were not much different than for Western countries. Our results for this subanalysis of Middle Eastern countries and Nigeria (n = 1,951) demonstrated that 8.7% of women (95% CI, 4.1-13.3) preferred a male provider, 51.2% (95% CI, 17.2-85.1) preferred a female provider, and 46.9% (95% CI, 9.3-84.5) had no gender preference.”
Updated May 20, 2016.
Reference
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider.Accessed May 18, 2016.
Reference
- Tobler KJ, Wu J, Khafagy AM, et al. Gender preference of the obstetrician gynecologist provider: a systematic review and meta-analysis. Obstet Gynecol. 2016;127(5)(suppl):43S. http://journals.lww.com/greenjournal/page/results.aspx?txtkeywords=Gender+preference+of+the+obstetrician+gynecologist+provider.Accessed May 18, 2016.
On-site reporting from the Society of Gynecologic Surgeons 2016 annual meeting
4/13/16. DAY 4 AT SGS
A jam-packed day of sessions, posters, awards, and clinical updates
Our last educational day was kicked off by a fascinating lecture by Dr. Amy Park on the “Genetic Determinants of Pelvic Organ Prolapse in Women of European American Descent: The Women’s Health Initiative.” Dr. Park and her colleagues found that there is evidence of phenotypic and genotypic heterogeneity in patients with pelvic organ prolapse, and there were 4 genetic loci identified that correlated with prolapse. Any uterine prolapse was associated with a genome-wide significant intergenic variant on chromosome 13, cystocele was associated with LOXL2, and all prolapse was associated with BMP.
Surmounting surgical site infection
Dr. Sarah Andiman then gave a lecture on the effects of a perioperative bundle and offered timely feedback for surgical site infection (SSI) prevention in hysterectomy. We all know that wound infections are a major morbidity associated with surgery, and Dr. Andiman’s group at Yale found that, by implementing this prevention program, the surgical site infection decreased 52.8%. Another suggestion from the audience was to have all patients use chlorhexidine wipes the night before and morning of a surgery to decrease wound infection. Similarly, Dr. Ali Bazzi gave a lecture on “Chlorhexidine-Alcohol Compared with Povidone-Iodine for Surgical-Site Antisepsis after Abdominal Hysterectomy.” The chlorhexidine was associated with 30% lower odds of SSI compared with povidone-iodine, even though this group had several medical comorbidities and risk factors known for SSIs.
Oral poster presenters make several interesting points
Dr. Christopher Ripperda from UT Southwestern Medical Center in Dallas, Texas, found that medical comorbidities and the presence of detrusor overactivity and PVR are predictors of early postoperative voiding dysfunction following a midurethral sling placement. Dr. Nabila Noor then described a fabulous surgical alternative to the use of morcellation to remove the uterus after a supracervical hysterectomy. She described the technique for performing a posterior colpotomy and stated that patients who had a surgery performed at her institution using this technique did not experience increased postoperative pain or longer postoperative stay.
Dr. Jennifer Thompson then shed some light on a very important question related to the Sunshine Act: Are physicians including all of their disclosures when they submit articles to a conference? When the physicians who submitted an abstract to the Society of Gynecologic Surgeons (SGS) in 2015 were searched on the Centers for Medicare and Medicaid Services (CMS) website, 62% of them had incomplete disclosures, with a total of nondisclosed CMS transactions equaling $1.3 million. We can do better!
Status update: The FPRN and passing of the torch
Congratulations to Dr. Kristin Jacobs, the new Fellows’ Pelvic Research Network (FPRN) Chair! The morning session ended with an innovative video from Dr. Janet Li and colleagues on the “Use of Suprapubic Carter-Thomason Needle to Assist in Cystoscopic Excision of Intravesical Foreign Object.”
The winner of the Distinguished Surgeon Award was given to Dr. Javier Magrina, and the SGS gavel was passed on to Dr. Vivian Sung! Congratulations!
Dr. Stephanie Pickett kicked off the eighth scientific session with a study entitled, “Comparing Methods of NSAID Delivery for Postoperative Pain.” When she and her colleagues compared IV toradol to IV ibuprofen for postoperative pain control after urogynecologic surgery, they found that patients experienced similar rates of pain control and satisfaction regardless of the type of analgesia.
Why are patients being readmitted after gynecologic oncology surgery?
The answer to this question is important as readmission rates are being considered for physician and hospital reimbursement. Dr. MaryAnn Wilbur and colleagues looked at the rates of unplanned 30-day readmission in gyn oncology patients. The patients who were readmitted had the following characteristics: ovarian cancer, creation of ostomy, Charleston score >5, language barrier, and positive discharge screen. Gastrointestinal disturbance and SSI were the most common reasons for readmission, and the total readmission-related costs for these patients was about $4.5 million.
Considering tissue extraction, surgical complications, and cognitive impairment
We then had 3 fabulous oral poster presentations. Dr. Emily Von Bargen and colleagues presented a study entitled, “Prevalence of Occult Pre-malignant or Malignant Pathology at the time of Uterine Morcellation for Benign Disease.” They performed a multicenter retrospective cohort study and found that 1.2% of women had a premalignant or malignant uterine pathology after surgery, with a prevalence of 0.66% of occult malignancy. She was unable to identify risk factors for those patients who had a premalignant or malignant pathology. Overall she found a low prevalence of premalignant or malignant uterine pathology when uterine morcellation was performed for benign disease.
Dr. Alix Leader-Cramer from Northwestern University pointed out “risk factors for a 30-day perioperative complications for total vaginal hysterectomy,” including chronic steroid use, higher ASA classification, current smoking status, diabetes, and lower preoperative serum albumin and sodium levels. Adnexectomy and resident participation were also associated with increased perioperative complications. About 9.5% of patients had a perioperative complication in the study population studied.
Finally, Dr. Elisa Trowbridge pointed out in her talk, on “Cognitive Impairment among Elderly Urogynecologic Patients,” that cognitive impairment is very prevalent among such women aged older than 75 years, and the Mini-Cog is a feasible screening tool.
What a way to end an AMAZING conference!
The conference ended with a fabulous video presentation by Dr. Andrea Benton, entitled “Surgical Approaches to the Management of Bladder and Ureteral Endometriosis.” Overall, the themes of this year’s SGS conference were to:
- emphasize the importance of performing a vaginal hysterectomy when feasible
- continue to strive to balance innovation with experimentation
- ensure that patients are being operated on by surgeons who are competent and frequently performing the indicated procedure.
Thank you to everyone who shared their research to educate the attendees at the conference! I can’t wait until next year!
4/12/16. DAY 3 AT SGS
Vaginal hysterectomy, fecal incontinence, transgender surgery amid tackled topics in Palm Springs
I could get used to sipping my coffee with the sunny background here in Palm Springs! It was a beautiful morning to learn.
We started the day with breakfast and a fabulous lecture on the inferior gluteal neurovascular anatomy in female cadavers, and an insightful lecture by Dr. Bhumy Dave, who brought up concerns about tracking for obstetrics and gynecology residency programs. She specifically highlighted the need for more experience with vaginal hysterectomies for residents who are going to be in a subspecialty that performs vaginal surgery. As the number of hysterectomies, specifically vaginal hysterectomies, declines every year, we need to make sure we are adequately training the physicians who will be performing this procedure in the future. One solution is to have residents join a track their 4th year of residency, after their future career path has been established. Another possible solution would be to increase use of a simulation model for vaginal hysterectomy, as described by Dr. Douglas Miyazaki.
Indigo carmine replacement? A recent issue in gynecologic surgery resulted when there was a national shortage of indigo carmine, which is commonly used to identify UO efflux at the time of cystoscopy. Dr. Katie Propst provided a solution: In the setting of planned cystoscopy, she found that preoperative phenazopyridine is an acceptable alternative and its use led to similar UO identification as with indigo carmine without an increase in complications.
Who should have a vaginal hysterectomy? Dr. Jennifer Schmitt from the Mayo Clinic gave another wonderful lecture describing a decision-tree algorithm for determining the ideal route of hysterectomy. According to a retrospective review of patients at their institution, vaginal hysterectomy was associated with lower infection rates, operative times, and costs.
The highlight of the morning was a very insightful Presidential Address by Dr. Andrew Walter! Not only is a he a very entertaining speaker but he also shed some light on 2 challenges that we currently face in the field. He eloquently stated that, “every woman who is a candidate for a vaginal hysterectomy should be able to get one and have it performed competently, and every woman who needs surgery should have one performed by someone who performs enough surgeries every year to competently perform the surgery.” He frequently alluded to the wise Dr. Mayo, who stated, “The best interest of the patient is the only interest to be considered…” Let’s never forget this as physicians!
Do you find removing the adnexa challenging when performing vaginal surgery? Check out the amazing idea from the Cleveland Clinic shown in video presentation 05! They clearly demonstrate using a single-site gel port or surgical glove placed in the vaginal incision to perform laparoscopy through the vagina. What a novel idea to avoid any abdominal incisions when there is a difficult vaginal adnexal surgery!
After the morning break, we watched a master vaginal surgeon perform a sacral colpopexy through the vaginal route. For details on this method, please reference video presentation 06.
An increase in health care costs is a huge problem in this country. Dr. Mary Van Meter suggested that one area in which we can improve is in the operating room (OR), specifically through decreasing the number of instruments sterilized. She found that only approximately 20% of the instruments on the operating field were actually used by the OR physician. It costs about $3 per instrument on the tray at Vanderbilt University, she said. When you think of the few number of instruments actually used, if we work to limit the number of instruments on the trays, we could cut significant costs. As reimbursement is getting increasingly linked to cost reduction, we all should be thinking about innovative ways to cut costs.
The oral posters were all excellent!
Dr. Ann Peters showed that, at a high-volume tertiary-care center, multimodal preoperative testing failed to definitively identify leiomyosarcoma (LMS), and the factors associated with increased LMS risk included older age, menopause, and presence of fibroids with concurrent pelvic, uterine, or adnexal mass.
Dr. Kevin Kremer found that preoperative antibiotics were used in 23% of cases in which they were not indicated, and the increased use rate was associated with entrance into the abdomen during surgery, the individual surgeon, and time under anesthesia.
Dr. Jessica Heft then stated that the incontinence rate after midurethral sling revision for vaginal exposure or pain was significantly higher with a partial as opposed to complete mesh excision.
Fecal incontinence treatment options
Dr. Peter Rosenblatt tackled the issue of “Innovation or experimentation: Where do we draw the line?” in the TeLinde lecture. He started by describing a condition for which he feels we do not have an acceptable amount of treatment options for patients: fecal incontinence. He described how he observed that the puborectalis muscle, not the external anal sphincter, was critical for fecal continence. He then devised a surgery that created a sling that would act as a synthetic puborectalis muscle. He had amazing success until one patient had a serious complication. Should you abandon a successful, innovative surgery due to one very severe complication, was the question. Where do we draw the line? I don’t have an answer…but I do know that we all need to thank our puborectalis muscle for our daily fecal continence!
This is not a new issue in medicine, explained Dr. Rosenblatt. From the beginning of medicine, there has been a balance between innovation and experimentation. So, what is innovation? It is when someone improves upon a device or process. In medicine, is it innovation or just variation? We frequently use medications and devices “off label,” and these techniques often improve our surgeries and outcomes for our patients. Innovation comes about through careful planning, a necessity created by an emergency, advances in technology, and through evolution of a procedure. Who are the innovators? YOU are! We are the ones who understand the unmet needs and the potential opportunities for improving medicine. Let’s all work together to innovate NOT experiment and make medicine better so our patients have the best care possible!
“New Frontiers in Gynecologic Surgery: Transgender Surgery and Functional Clitoroplasty after Female Genital Mutilation”
The final talk for the day was by the groundbreaking Dr. Marci Bowers, whose lecture started by reminding everyone that there is a difference between gender identity and gender expression. Once a person knows his or her gender identity they use gender expression to express this to the world, she pointed out. Dr. Bowers is a true innovator and is performing gender reassignment surgeries as well as female genital mutilation corrective surgeries. She has perfected a one-stage vaginoplasty, and she showed a video of the procedure, which results in a 90% chance of orgasm. She also noted that she is able to restore clitoral function in 100% of the cases of genital mutilation, and she performs these procedures free of charge.
She reminded us that all ObGyns need to be trained in treating transgender patients, and given the high rate of suicide among adolescent transgender individuals, we all need to work together to provide a supportive medical environment to help these patients. What a fascinating end to the day!
Some relaxation, and entertainment, amid the sun and outdoors
We then had the afternoon to compete in a golf tournament, explore the area on mountain bikes, or lounge by the pool. Regardless of the daytime activities, we all came back together for the great lip-synch competition! All 4 teams gave an impressive performance, but the team from Brown University went home with the win! Such an entertaining event! (Thanks to incoming SGS President Vivian Sung @wih_sung for the pic!)
4/11/16. DAY 2 AT SGS
Experts talk surgical innovations, complementary therapies, value-based payment, and much more at SGS day 2
Wake up and learn! The second day of the 42nd Annual Scientific Meeting of the Society of Gynecologic Surgeons began with a review of research posters at the Poster Session as the sun rose over the Palm Springs mountains. We then moved indoors for the scientific sessions.
In the first lecture, "Reasons for Unplanned 30-Day Readmission After Hysterectomy for Benign Disease," Dr. Courtney Penn and colleagues reiterated that the postsurgical readmission rate is higher for patients undergoing abdominal hysterectomy compared with those who have a laparoscopic or vaginal hysterectomy. Similarly, Dr. Jennifer Schmitt and colleagues suggested that in a patient with a relative contraindication for vaginal hysterectomy, when this procedure is performed by an experienced surgeon there may not be increased complications. However, keep in mind that the study described—"A Comparison of Vaginal and Robotic Hysterectomy for Commonly Cited Relative Contraindications to Vaginal Hysterectomy"—was performed at the Mayo Clinic by expert, highly trained surgeons, and this fact may limit the generalizability of the study. As one audience member eloquently stated, it is important to remember that: "Just because it is feasible does not mean it is the correct procedure."
That yoga or barre class may be doing more good than you think! Lunge, bridge, and cat-into-cow movements may provide a greater degree of pelvic floor muscle unit recruitment than traditional Kegel exercises, according to a presentation by Dr. Bruce Crawford on Kegels versus specialized movement.
Perhaps those exercises should be recommended for surgeons as well. As Dr. Ruchira Singh pointed out, surgeons experience a high amount of musculoskeletal strain when performing vaginal procedures while sitting, regardless of the type of chair used during surgery. Dr. Singh and colleagues’ study, "Effect of Different Chairs on Work-Related Musculoskeletal Discomfort During Vaginal Surgery," found that while the round stool with a backrest and the Capisco chair were more comfortable, they did not eliminate the high risk for musculoskeletal strain, particularly in the head and neck.
Dr. Ann Peters and colleagues, from Magee-Womens Hospital of the University of Pittsburgh Medical Center, gave a fabulous video presentation on "Anatomic and Vascular Considerations in Laparoscopic Uterine Artery Ligation During Hysterectomy."
Need a novel treatment for interstitial cystitis/bladder pain syndrome? Consider mindfulness-based stress reduction. A randomized controlled study performed by Dr. Gregg Kanter and colleagues describes how this technique may help patients and could be considered a first-line therapy.
What is value-based payment and this new trend in reimbursement? And how does it apply to vaginal hysterectomy? Dr. Tina Groat addressed these issues in her keynote lecture. According to the American Congress of Obstetricians and Gynecologists, “Evidence demonstrates that, in general, vaginal hysterectomy is associated with better outcomes and fewer complications than laparoscopic or abdominal hysterectomy.” This is in opposition to what is actually being performed clinically. Dr. Groat explained that United Healthcare decided to incentivize physicians by requiring a prior authorization for all hysterectomies for benign disease. There is both a quality and cost benefit to performing a vaginal hysterectomy. Most insurance companies are moving away from a “fee for service” structure to performance-based payment. Change is always scary and, while I think the overall goal of moving toward the best care for our patients is a positive, this approach may create new challenges for the medical field. What do you think? Is performance-based payment beneficial? Or does it limit physicians and potentially force them to perform a procedure they do not feel as comfortable performing? Will this result in physicians rejecting certain patient populations? [Note from OBG MANAGEMENT: Let Dr. Collins know your thoughts through social media, or email OBG MANAGEMENT with a Letter to the Editor (rbarbieri@frontlinemedcom.com).]
The debate on the best route for hysterectomy continues: According to Dr. Carolyn Swenson and colleagues in their presentation, "Comparison of Robotic and Other Minimally Invasive Routes of Hysterectomy for Benign Indications," while there may be lower complications associated with robotic hysterectomy, the cost of performing a robotic hysterectomy is significantly higher than the cost of laparoscopic or vaginal hysterectomy, thus limiting its utility.
How can we teach a rare surgical procedure to learners? We channel our inner Martha Stewart and make a model out of a beef tongue and chicken. For about $8 a challenging and rare surgery can be taught to residents and medical students, according to the video presentation by Dr. Jana Illston and colleagues, titled "Modified Beef Tongue Model for Fourth-Degree Laceration Repair Simulation."
After the Day 2 lunch break, there was a rousing debate surrounding "Surgeons as Innovators—What Is the Patient Expecting?" Where do we draw the line between using an older more proven therapy as opposed to trying an innovative technology that may actually offer a potential benefit? Dr. Dennis Miller made a good point regarding innovation and pharmaceutical and device companies: If we ignore industry, we lose the ability to help with innovation and shape the future of medical treatments. Perhaps we should use the golden rule: If we would perform the surgery or use the device on ourselves, then we should perform it on our patient. Patients have a greater burden now, because there are more treatment options that they must choose among. Our job as physicians is to educate our patients and to guide them to innovative and evidence-based treatments.
Highlights from the afternoon oral poster session included a presentation by Dr. Caryn Russman that noted the high risk for recurrent urinary tract infection (UTI) after a mid-urethral sling procedure, which seems to be related to specific preoperative risk factors (such as a history of recurrent UTI). Dr. Tanya Hoke suggested that residents and attending physicians have inaccurate estimates of uterine weight, and an educational program may be necessary to improve these estimates. Finally, a study from Massachusetts General Hospital showed that a shorter stay in the hospital, ideally same-day surgery, resulted in a lower complication risk, lower number of emergency department visits, and a decreased readmission rate for patients undergoing urogynecology procedures.
The following recommendations were then suggested regarding vaginal hysterectomy:
- Preoperative prep with 4% chlorhexidine or povidine iodine
- Intracervical vasopressin injection to decrease blood loss
- Use of a pedicle-sealing device for pedicle ligation
- Vertical cuff closure is preferred to maximize vaginal length
Another important point made was that a prior cesarean delivery is not a contraindication to performing a vaginal hysterectomy.
Recommendations regarding recurrent UTI were also made, which include the recommendation for preoperative use of antibiotics to decrease the rate of UTI, with no benefit for a longer course of antibiotics.
News from the Fellows’ Pelvic Research Network
So much exciting research currently is ongoing with the FPRN! New project ideas include comparison of trimethoprim with methenamie for treatment of recurrent UTI; comparison of laparoscopic/robotic sacrocolpopexy with vaginal USLS for management of apical prolapse; a survey study examining surgeon preferences for timing of midurethral sling placement when performed at the time of pelvic organ prolapse (POP) repair; an assessment of the effect of a midurethal sling on overactive bladder in surgical repair in POP; and a study evaluating female pelvic reconstructive surgery in the setting of human immunodeficiency virus infection. It is so great to see the fellows working together to provide groundbreaking research!
Fun with stats
Learning statistics at the end of the day is never easy, but Dr. Matthew Barber did a fabulous job explaining this often-confusing topic. He reminded attendees that the key to learning statistics is repetition. One new recommendation he offered to enhance understanding is to use common language instead of numbers for P values. For example, instead of saying P <.001, use “is superior,” and instead of saying P = .3, use “seems not superior” or “inconclusive.”
A night to remember
The night ended with a wonderful awards ceremony and the president’s reception. Overall, day 2 was a very educational—and fun—day!
4/10/16. DAY 1 AT SGS
Postgrad courses address pain management and social media education
Mastering pelvic pain
With the beautiful Palm Springs, California, backdrop of mountains and palm trees, the 2016 meeting of the Society of Gynecologic Surgeons kicked off with 4 postgraduate courses. At the “Mastering Pelvic Pain: Strategies and Techniques for a Multimodal Approach” course, directed by Dr. Cara King, Dr. Matt Siedhoff explained the key components of the history and physical examination: Keep in mind that this generally is a multifactorial issue and may require a multidisciplinary approach, he told attendees. It is also important to make sure that the patient is fully prepared to combat the chronic pelvic pain (CPP) symptoms by focusing on the fundamentals, he said, including smoking, diet, exercise, weight loss, sleep, and relationship stress.
How is your posture? It turns out that something as simple as altering your posture can significantly affect pelvic floor control. Carol Sobeck, PT, demonstrated this importance with a simple group exercise that proved how the ability to contract the pelvic floor changes significantly with posture. Get to know your pelvic floor physical therapist—they are critical in helping with the treatment of CPP.
But what to do when physical therapy fails? Dr. Jennifer Gunter shed some light on this very difficult medical situation. One suggestion, she said, is to consider the possibility of a local presentation of a systemic issue and screen for the following: fibromyalgia, Ehlers-Danlos syndrome, statin use, and diabetes mellitus. Other treatment ideas include trigger point injections and onabotulinumtoxin A (Botox) therapy. A trigger point is a hypercontracted focus of muscle. To treat a trigger point, a needle must mechanically disrupt the trigger point to reduce the pelvic pain, and injection of local anesthetic is only used to help with postprocedure discomfort. Botox in my pelvis, you ask? Yes! The goal is to block presynaptic release of acetylcholine, which is very effective at reducing muscle spasm.
Tackling endometriosis. Dr. King then described surgical techniques for endometriosis. She recommended that, for mild disease not in close proximity to vital structures, ablation is likely equivalent to excision. For deeply infiltrating endometriosis, or lesions in close proximity to vital structures, excision is more beneficial. Excision is always beneficial for pathologic diagnosis, she said. And she offered this tip for bladder endometriosis: place a stitch in the nodule to allow for counter traction. Here is another tip, for ovarian cystectomy: inject vasopressin (20 U in 60 mL) to help dissect the plane between the ovary and cyst wall, and consider presacral neurectomy for midline pain.
Dr. Frank Tu then explained that we should not think of it as the “terrible triad: endometriosis, irritable bowel syndrome, and interstitial cystsis,” but rather as a system out of balance. Both peripheral and central mechanisms are involved in the generation and maintenance of cross-organ sensitization, he pointed out, which may explain why patients receive multiple diagnoses that describe a myriad of complaints due to a lack of overall homeostasis.
While Dr. Alaa Abd-Elsayed described innovative nerve blocks for CPP, he emphasized that no one specific treatment will result in a complete resolution of symptoms.
Vaginal mesh placement and pain. Dr. Mario Castellanos gave a fabulous lecture describing the pain issues that surround vaginal mesh placement. Interestingly, he noted that many patients had pelvic pain prior to placement of vaginal mesh, and that pain likely only will worsen with mesh placement. Mesh may cause pain by causing inflammation, visceral injury, muscle injury, and nerve injury. While there are guidelines for where mesh should be placed for bladder slings (TVT and TOT) and for prolapse repair, studies show, he pointed out, that the mesh placement often disrupts several muscle groups and may directly injure a nerve.
Alternatives to the typical diagnoses for CPP. The morning ended with a lecture by Dr. Suzie As-Sanie, in which she reminded everyone to start with “gold standard” therapy but, if those fail, consider alternative diagnoses or a central pain disorder. She also suggested cognitive behavioral therapy for treatment of CPP. For patients who cannot afford cognitive behavioral therapy, there is a free online source at fibroguide.med.umich.edu. Other alternative treatment options include exercise, patient education, instruction on sleep hygiene, and neurostimulatory therapies.
Overall, all the speakers this morning agreed that CPP is rarely treated with one modality, and it is best treated with a multidisciplinary approach.
Let’s get social!
The afternoon was spent learning about ways to use social networking sites to educate our patients, in another postgraduate course on “Making Media Social,” presented by the SGS Social Media Committee. Given that a recent survey demonstrated that 74.1% of women have some type of social networking account, it can be a very useful source for medical information for patients. If you have any questions about what is appropriate on social media, check out ACOG committee opinion 622.
Here are some tips that I learned:
Facebook:
- Keep your private Facebook page private and create a separate professional Facebook page
- Adjust your login setting so only administrators can post on your professional page
- Adjust settings so your professional profile cannot be “tagged”
- If a patient contacts your personal page, direct them to your professional page
- Do not give medical advice since Facebook is not digitally encrypted
Twitter:
- “Short bursts of inconsequential information”
- Follow societies, medical centers, and medical journals
LinkedIn:
- It provides a great way to find jobs, people, and business opportunities that are recommended by someone in your contact group
- It is specifically there to help you grow your business and show people who you are and where you have come from
Doximity:
Before we get to tips, first, what is it? Well, Doximity is basically a “LinkedIn” for physicians. It is “a way to find relevant specialists for patients; a rolodex; an email and text service; and a virtual lounge.” It is currently transforming from social network into a ‘platform.’ Now more than 1,000 hospitals and health systems are part of Doximity. Tips:
- There is a secure message option, which is HIPAA compliant
- Provides a way for residents and fellows to understand possible future places of employment
- It is a great way to find someone to refer patients to in an unfamiliar location
Vimeo:
- A benefit over YouTube is the lack of advertisements
- Check out the SGS video archives!
- You also can set privacy settings and embedding stats
Fifty-nine percent of US adults have looked online for health information in the past year. Therefore, it is important for physicians to get good information out for people to see!
A relaxing day’s end
The night ended with a beautiful poolside reception! I can’t wait to see what day 2 will bring!
4/13/16. DAY 4 AT SGS
A jam-packed day of sessions, posters, awards, and clinical updates
Our last educational day was kicked off by a fascinating lecture by Dr. Amy Park on the “Genetic Determinants of Pelvic Organ Prolapse in Women of European American Descent: The Women’s Health Initiative.” Dr. Park and her colleagues found that there is evidence of phenotypic and genotypic heterogeneity in patients with pelvic organ prolapse, and there were 4 genetic loci identified that correlated with prolapse. Any uterine prolapse was associated with a genome-wide significant intergenic variant on chromosome 13, cystocele was associated with LOXL2, and all prolapse was associated with BMP.
Surmounting surgical site infection
Dr. Sarah Andiman then gave a lecture on the effects of a perioperative bundle and offered timely feedback for surgical site infection (SSI) prevention in hysterectomy. We all know that wound infections are a major morbidity associated with surgery, and Dr. Andiman’s group at Yale found that, by implementing this prevention program, the surgical site infection decreased 52.8%. Another suggestion from the audience was to have all patients use chlorhexidine wipes the night before and morning of a surgery to decrease wound infection. Similarly, Dr. Ali Bazzi gave a lecture on “Chlorhexidine-Alcohol Compared with Povidone-Iodine for Surgical-Site Antisepsis after Abdominal Hysterectomy.” The chlorhexidine was associated with 30% lower odds of SSI compared with povidone-iodine, even though this group had several medical comorbidities and risk factors known for SSIs.
Oral poster presenters make several interesting points
Dr. Christopher Ripperda from UT Southwestern Medical Center in Dallas, Texas, found that medical comorbidities and the presence of detrusor overactivity and PVR are predictors of early postoperative voiding dysfunction following a midurethral sling placement. Dr. Nabila Noor then described a fabulous surgical alternative to the use of morcellation to remove the uterus after a supracervical hysterectomy. She described the technique for performing a posterior colpotomy and stated that patients who had a surgery performed at her institution using this technique did not experience increased postoperative pain or longer postoperative stay.
Dr. Jennifer Thompson then shed some light on a very important question related to the Sunshine Act: Are physicians including all of their disclosures when they submit articles to a conference? When the physicians who submitted an abstract to the Society of Gynecologic Surgeons (SGS) in 2015 were searched on the Centers for Medicare and Medicaid Services (CMS) website, 62% of them had incomplete disclosures, with a total of nondisclosed CMS transactions equaling $1.3 million. We can do better!
Status update: The FPRN and passing of the torch
Congratulations to Dr. Kristin Jacobs, the new Fellows’ Pelvic Research Network (FPRN) Chair! The morning session ended with an innovative video from Dr. Janet Li and colleagues on the “Use of Suprapubic Carter-Thomason Needle to Assist in Cystoscopic Excision of Intravesical Foreign Object.”
The winner of the Distinguished Surgeon Award was given to Dr. Javier Magrina, and the SGS gavel was passed on to Dr. Vivian Sung! Congratulations!
Dr. Stephanie Pickett kicked off the eighth scientific session with a study entitled, “Comparing Methods of NSAID Delivery for Postoperative Pain.” When she and her colleagues compared IV toradol to IV ibuprofen for postoperative pain control after urogynecologic surgery, they found that patients experienced similar rates of pain control and satisfaction regardless of the type of analgesia.
Why are patients being readmitted after gynecologic oncology surgery?
The answer to this question is important as readmission rates are being considered for physician and hospital reimbursement. Dr. MaryAnn Wilbur and colleagues looked at the rates of unplanned 30-day readmission in gyn oncology patients. The patients who were readmitted had the following characteristics: ovarian cancer, creation of ostomy, Charleston score >5, language barrier, and positive discharge screen. Gastrointestinal disturbance and SSI were the most common reasons for readmission, and the total readmission-related costs for these patients was about $4.5 million.
Considering tissue extraction, surgical complications, and cognitive impairment
We then had 3 fabulous oral poster presentations. Dr. Emily Von Bargen and colleagues presented a study entitled, “Prevalence of Occult Pre-malignant or Malignant Pathology at the time of Uterine Morcellation for Benign Disease.” They performed a multicenter retrospective cohort study and found that 1.2% of women had a premalignant or malignant uterine pathology after surgery, with a prevalence of 0.66% of occult malignancy. She was unable to identify risk factors for those patients who had a premalignant or malignant pathology. Overall she found a low prevalence of premalignant or malignant uterine pathology when uterine morcellation was performed for benign disease.
Dr. Alix Leader-Cramer from Northwestern University pointed out “risk factors for a 30-day perioperative complications for total vaginal hysterectomy,” including chronic steroid use, higher ASA classification, current smoking status, diabetes, and lower preoperative serum albumin and sodium levels. Adnexectomy and resident participation were also associated with increased perioperative complications. About 9.5% of patients had a perioperative complication in the study population studied.
Finally, Dr. Elisa Trowbridge pointed out in her talk, on “Cognitive Impairment among Elderly Urogynecologic Patients,” that cognitive impairment is very prevalent among such women aged older than 75 years, and the Mini-Cog is a feasible screening tool.
What a way to end an AMAZING conference!
The conference ended with a fabulous video presentation by Dr. Andrea Benton, entitled “Surgical Approaches to the Management of Bladder and Ureteral Endometriosis.” Overall, the themes of this year’s SGS conference were to:
- emphasize the importance of performing a vaginal hysterectomy when feasible
- continue to strive to balance innovation with experimentation
- ensure that patients are being operated on by surgeons who are competent and frequently performing the indicated procedure.
Thank you to everyone who shared their research to educate the attendees at the conference! I can’t wait until next year!
4/12/16. DAY 3 AT SGS
Vaginal hysterectomy, fecal incontinence, transgender surgery amid tackled topics in Palm Springs
I could get used to sipping my coffee with the sunny background here in Palm Springs! It was a beautiful morning to learn.
We started the day with breakfast and a fabulous lecture on the inferior gluteal neurovascular anatomy in female cadavers, and an insightful lecture by Dr. Bhumy Dave, who brought up concerns about tracking for obstetrics and gynecology residency programs. She specifically highlighted the need for more experience with vaginal hysterectomies for residents who are going to be in a subspecialty that performs vaginal surgery. As the number of hysterectomies, specifically vaginal hysterectomies, declines every year, we need to make sure we are adequately training the physicians who will be performing this procedure in the future. One solution is to have residents join a track their 4th year of residency, after their future career path has been established. Another possible solution would be to increase use of a simulation model for vaginal hysterectomy, as described by Dr. Douglas Miyazaki.
Indigo carmine replacement? A recent issue in gynecologic surgery resulted when there was a national shortage of indigo carmine, which is commonly used to identify UO efflux at the time of cystoscopy. Dr. Katie Propst provided a solution: In the setting of planned cystoscopy, she found that preoperative phenazopyridine is an acceptable alternative and its use led to similar UO identification as with indigo carmine without an increase in complications.
Who should have a vaginal hysterectomy? Dr. Jennifer Schmitt from the Mayo Clinic gave another wonderful lecture describing a decision-tree algorithm for determining the ideal route of hysterectomy. According to a retrospective review of patients at their institution, vaginal hysterectomy was associated with lower infection rates, operative times, and costs.
The highlight of the morning was a very insightful Presidential Address by Dr. Andrew Walter! Not only is a he a very entertaining speaker but he also shed some light on 2 challenges that we currently face in the field. He eloquently stated that, “every woman who is a candidate for a vaginal hysterectomy should be able to get one and have it performed competently, and every woman who needs surgery should have one performed by someone who performs enough surgeries every year to competently perform the surgery.” He frequently alluded to the wise Dr. Mayo, who stated, “The best interest of the patient is the only interest to be considered…” Let’s never forget this as physicians!
Do you find removing the adnexa challenging when performing vaginal surgery? Check out the amazing idea from the Cleveland Clinic shown in video presentation 05! They clearly demonstrate using a single-site gel port or surgical glove placed in the vaginal incision to perform laparoscopy through the vagina. What a novel idea to avoid any abdominal incisions when there is a difficult vaginal adnexal surgery!
After the morning break, we watched a master vaginal surgeon perform a sacral colpopexy through the vaginal route. For details on this method, please reference video presentation 06.
An increase in health care costs is a huge problem in this country. Dr. Mary Van Meter suggested that one area in which we can improve is in the operating room (OR), specifically through decreasing the number of instruments sterilized. She found that only approximately 20% of the instruments on the operating field were actually used by the OR physician. It costs about $3 per instrument on the tray at Vanderbilt University, she said. When you think of the few number of instruments actually used, if we work to limit the number of instruments on the trays, we could cut significant costs. As reimbursement is getting increasingly linked to cost reduction, we all should be thinking about innovative ways to cut costs.
The oral posters were all excellent!
Dr. Ann Peters showed that, at a high-volume tertiary-care center, multimodal preoperative testing failed to definitively identify leiomyosarcoma (LMS), and the factors associated with increased LMS risk included older age, menopause, and presence of fibroids with concurrent pelvic, uterine, or adnexal mass.
Dr. Kevin Kremer found that preoperative antibiotics were used in 23% of cases in which they were not indicated, and the increased use rate was associated with entrance into the abdomen during surgery, the individual surgeon, and time under anesthesia.
Dr. Jessica Heft then stated that the incontinence rate after midurethral sling revision for vaginal exposure or pain was significantly higher with a partial as opposed to complete mesh excision.
Fecal incontinence treatment options
Dr. Peter Rosenblatt tackled the issue of “Innovation or experimentation: Where do we draw the line?” in the TeLinde lecture. He started by describing a condition for which he feels we do not have an acceptable amount of treatment options for patients: fecal incontinence. He described how he observed that the puborectalis muscle, not the external anal sphincter, was critical for fecal continence. He then devised a surgery that created a sling that would act as a synthetic puborectalis muscle. He had amazing success until one patient had a serious complication. Should you abandon a successful, innovative surgery due to one very severe complication, was the question. Where do we draw the line? I don’t have an answer…but I do know that we all need to thank our puborectalis muscle for our daily fecal continence!
This is not a new issue in medicine, explained Dr. Rosenblatt. From the beginning of medicine, there has been a balance between innovation and experimentation. So, what is innovation? It is when someone improves upon a device or process. In medicine, is it innovation or just variation? We frequently use medications and devices “off label,” and these techniques often improve our surgeries and outcomes for our patients. Innovation comes about through careful planning, a necessity created by an emergency, advances in technology, and through evolution of a procedure. Who are the innovators? YOU are! We are the ones who understand the unmet needs and the potential opportunities for improving medicine. Let’s all work together to innovate NOT experiment and make medicine better so our patients have the best care possible!
“New Frontiers in Gynecologic Surgery: Transgender Surgery and Functional Clitoroplasty after Female Genital Mutilation”
The final talk for the day was by the groundbreaking Dr. Marci Bowers, whose lecture started by reminding everyone that there is a difference between gender identity and gender expression. Once a person knows his or her gender identity they use gender expression to express this to the world, she pointed out. Dr. Bowers is a true innovator and is performing gender reassignment surgeries as well as female genital mutilation corrective surgeries. She has perfected a one-stage vaginoplasty, and she showed a video of the procedure, which results in a 90% chance of orgasm. She also noted that she is able to restore clitoral function in 100% of the cases of genital mutilation, and she performs these procedures free of charge.
She reminded us that all ObGyns need to be trained in treating transgender patients, and given the high rate of suicide among adolescent transgender individuals, we all need to work together to provide a supportive medical environment to help these patients. What a fascinating end to the day!
Some relaxation, and entertainment, amid the sun and outdoors
We then had the afternoon to compete in a golf tournament, explore the area on mountain bikes, or lounge by the pool. Regardless of the daytime activities, we all came back together for the great lip-synch competition! All 4 teams gave an impressive performance, but the team from Brown University went home with the win! Such an entertaining event! (Thanks to incoming SGS President Vivian Sung @wih_sung for the pic!)
4/11/16. DAY 2 AT SGS
Experts talk surgical innovations, complementary therapies, value-based payment, and much more at SGS day 2
Wake up and learn! The second day of the 42nd Annual Scientific Meeting of the Society of Gynecologic Surgeons began with a review of research posters at the Poster Session as the sun rose over the Palm Springs mountains. We then moved indoors for the scientific sessions.
In the first lecture, "Reasons for Unplanned 30-Day Readmission After Hysterectomy for Benign Disease," Dr. Courtney Penn and colleagues reiterated that the postsurgical readmission rate is higher for patients undergoing abdominal hysterectomy compared with those who have a laparoscopic or vaginal hysterectomy. Similarly, Dr. Jennifer Schmitt and colleagues suggested that in a patient with a relative contraindication for vaginal hysterectomy, when this procedure is performed by an experienced surgeon there may not be increased complications. However, keep in mind that the study described—"A Comparison of Vaginal and Robotic Hysterectomy for Commonly Cited Relative Contraindications to Vaginal Hysterectomy"—was performed at the Mayo Clinic by expert, highly trained surgeons, and this fact may limit the generalizability of the study. As one audience member eloquently stated, it is important to remember that: "Just because it is feasible does not mean it is the correct procedure."
That yoga or barre class may be doing more good than you think! Lunge, bridge, and cat-into-cow movements may provide a greater degree of pelvic floor muscle unit recruitment than traditional Kegel exercises, according to a presentation by Dr. Bruce Crawford on Kegels versus specialized movement.
Perhaps those exercises should be recommended for surgeons as well. As Dr. Ruchira Singh pointed out, surgeons experience a high amount of musculoskeletal strain when performing vaginal procedures while sitting, regardless of the type of chair used during surgery. Dr. Singh and colleagues’ study, "Effect of Different Chairs on Work-Related Musculoskeletal Discomfort During Vaginal Surgery," found that while the round stool with a backrest and the Capisco chair were more comfortable, they did not eliminate the high risk for musculoskeletal strain, particularly in the head and neck.
Dr. Ann Peters and colleagues, from Magee-Womens Hospital of the University of Pittsburgh Medical Center, gave a fabulous video presentation on "Anatomic and Vascular Considerations in Laparoscopic Uterine Artery Ligation During Hysterectomy."
Need a novel treatment for interstitial cystitis/bladder pain syndrome? Consider mindfulness-based stress reduction. A randomized controlled study performed by Dr. Gregg Kanter and colleagues describes how this technique may help patients and could be considered a first-line therapy.
What is value-based payment and this new trend in reimbursement? And how does it apply to vaginal hysterectomy? Dr. Tina Groat addressed these issues in her keynote lecture. According to the American Congress of Obstetricians and Gynecologists, “Evidence demonstrates that, in general, vaginal hysterectomy is associated with better outcomes and fewer complications than laparoscopic or abdominal hysterectomy.” This is in opposition to what is actually being performed clinically. Dr. Groat explained that United Healthcare decided to incentivize physicians by requiring a prior authorization for all hysterectomies for benign disease. There is both a quality and cost benefit to performing a vaginal hysterectomy. Most insurance companies are moving away from a “fee for service” structure to performance-based payment. Change is always scary and, while I think the overall goal of moving toward the best care for our patients is a positive, this approach may create new challenges for the medical field. What do you think? Is performance-based payment beneficial? Or does it limit physicians and potentially force them to perform a procedure they do not feel as comfortable performing? Will this result in physicians rejecting certain patient populations? [Note from OBG MANAGEMENT: Let Dr. Collins know your thoughts through social media, or email OBG MANAGEMENT with a Letter to the Editor (rbarbieri@frontlinemedcom.com).]
The debate on the best route for hysterectomy continues: According to Dr. Carolyn Swenson and colleagues in their presentation, "Comparison of Robotic and Other Minimally Invasive Routes of Hysterectomy for Benign Indications," while there may be lower complications associated with robotic hysterectomy, the cost of performing a robotic hysterectomy is significantly higher than the cost of laparoscopic or vaginal hysterectomy, thus limiting its utility.
How can we teach a rare surgical procedure to learners? We channel our inner Martha Stewart and make a model out of a beef tongue and chicken. For about $8 a challenging and rare surgery can be taught to residents and medical students, according to the video presentation by Dr. Jana Illston and colleagues, titled "Modified Beef Tongue Model for Fourth-Degree Laceration Repair Simulation."
After the Day 2 lunch break, there was a rousing debate surrounding "Surgeons as Innovators—What Is the Patient Expecting?" Where do we draw the line between using an older more proven therapy as opposed to trying an innovative technology that may actually offer a potential benefit? Dr. Dennis Miller made a good point regarding innovation and pharmaceutical and device companies: If we ignore industry, we lose the ability to help with innovation and shape the future of medical treatments. Perhaps we should use the golden rule: If we would perform the surgery or use the device on ourselves, then we should perform it on our patient. Patients have a greater burden now, because there are more treatment options that they must choose among. Our job as physicians is to educate our patients and to guide them to innovative and evidence-based treatments.
Highlights from the afternoon oral poster session included a presentation by Dr. Caryn Russman that noted the high risk for recurrent urinary tract infection (UTI) after a mid-urethral sling procedure, which seems to be related to specific preoperative risk factors (such as a history of recurrent UTI). Dr. Tanya Hoke suggested that residents and attending physicians have inaccurate estimates of uterine weight, and an educational program may be necessary to improve these estimates. Finally, a study from Massachusetts General Hospital showed that a shorter stay in the hospital, ideally same-day surgery, resulted in a lower complication risk, lower number of emergency department visits, and a decreased readmission rate for patients undergoing urogynecology procedures.
The following recommendations were then suggested regarding vaginal hysterectomy:
- Preoperative prep with 4% chlorhexidine or povidine iodine
- Intracervical vasopressin injection to decrease blood loss
- Use of a pedicle-sealing device for pedicle ligation
- Vertical cuff closure is preferred to maximize vaginal length
Another important point made was that a prior cesarean delivery is not a contraindication to performing a vaginal hysterectomy.
Recommendations regarding recurrent UTI were also made, which include the recommendation for preoperative use of antibiotics to decrease the rate of UTI, with no benefit for a longer course of antibiotics.
News from the Fellows’ Pelvic Research Network
So much exciting research currently is ongoing with the FPRN! New project ideas include comparison of trimethoprim with methenamie for treatment of recurrent UTI; comparison of laparoscopic/robotic sacrocolpopexy with vaginal USLS for management of apical prolapse; a survey study examining surgeon preferences for timing of midurethral sling placement when performed at the time of pelvic organ prolapse (POP) repair; an assessment of the effect of a midurethal sling on overactive bladder in surgical repair in POP; and a study evaluating female pelvic reconstructive surgery in the setting of human immunodeficiency virus infection. It is so great to see the fellows working together to provide groundbreaking research!
Fun with stats
Learning statistics at the end of the day is never easy, but Dr. Matthew Barber did a fabulous job explaining this often-confusing topic. He reminded attendees that the key to learning statistics is repetition. One new recommendation he offered to enhance understanding is to use common language instead of numbers for P values. For example, instead of saying P <.001, use “is superior,” and instead of saying P = .3, use “seems not superior” or “inconclusive.”
A night to remember
The night ended with a wonderful awards ceremony and the president’s reception. Overall, day 2 was a very educational—and fun—day!
4/10/16. DAY 1 AT SGS
Postgrad courses address pain management and social media education
Mastering pelvic pain
With the beautiful Palm Springs, California, backdrop of mountains and palm trees, the 2016 meeting of the Society of Gynecologic Surgeons kicked off with 4 postgraduate courses. At the “Mastering Pelvic Pain: Strategies and Techniques for a Multimodal Approach” course, directed by Dr. Cara King, Dr. Matt Siedhoff explained the key components of the history and physical examination: Keep in mind that this generally is a multifactorial issue and may require a multidisciplinary approach, he told attendees. It is also important to make sure that the patient is fully prepared to combat the chronic pelvic pain (CPP) symptoms by focusing on the fundamentals, he said, including smoking, diet, exercise, weight loss, sleep, and relationship stress.
How is your posture? It turns out that something as simple as altering your posture can significantly affect pelvic floor control. Carol Sobeck, PT, demonstrated this importance with a simple group exercise that proved how the ability to contract the pelvic floor changes significantly with posture. Get to know your pelvic floor physical therapist—they are critical in helping with the treatment of CPP.
But what to do when physical therapy fails? Dr. Jennifer Gunter shed some light on this very difficult medical situation. One suggestion, she said, is to consider the possibility of a local presentation of a systemic issue and screen for the following: fibromyalgia, Ehlers-Danlos syndrome, statin use, and diabetes mellitus. Other treatment ideas include trigger point injections and onabotulinumtoxin A (Botox) therapy. A trigger point is a hypercontracted focus of muscle. To treat a trigger point, a needle must mechanically disrupt the trigger point to reduce the pelvic pain, and injection of local anesthetic is only used to help with postprocedure discomfort. Botox in my pelvis, you ask? Yes! The goal is to block presynaptic release of acetylcholine, which is very effective at reducing muscle spasm.
Tackling endometriosis. Dr. King then described surgical techniques for endometriosis. She recommended that, for mild disease not in close proximity to vital structures, ablation is likely equivalent to excision. For deeply infiltrating endometriosis, or lesions in close proximity to vital structures, excision is more beneficial. Excision is always beneficial for pathologic diagnosis, she said. And she offered this tip for bladder endometriosis: place a stitch in the nodule to allow for counter traction. Here is another tip, for ovarian cystectomy: inject vasopressin (20 U in 60 mL) to help dissect the plane between the ovary and cyst wall, and consider presacral neurectomy for midline pain.
Dr. Frank Tu then explained that we should not think of it as the “terrible triad: endometriosis, irritable bowel syndrome, and interstitial cystsis,” but rather as a system out of balance. Both peripheral and central mechanisms are involved in the generation and maintenance of cross-organ sensitization, he pointed out, which may explain why patients receive multiple diagnoses that describe a myriad of complaints due to a lack of overall homeostasis.
While Dr. Alaa Abd-Elsayed described innovative nerve blocks for CPP, he emphasized that no one specific treatment will result in a complete resolution of symptoms.
Vaginal mesh placement and pain. Dr. Mario Castellanos gave a fabulous lecture describing the pain issues that surround vaginal mesh placement. Interestingly, he noted that many patients had pelvic pain prior to placement of vaginal mesh, and that pain likely only will worsen with mesh placement. Mesh may cause pain by causing inflammation, visceral injury, muscle injury, and nerve injury. While there are guidelines for where mesh should be placed for bladder slings (TVT and TOT) and for prolapse repair, studies show, he pointed out, that the mesh placement often disrupts several muscle groups and may directly injure a nerve.
Alternatives to the typical diagnoses for CPP. The morning ended with a lecture by Dr. Suzie As-Sanie, in which she reminded everyone to start with “gold standard” therapy but, if those fail, consider alternative diagnoses or a central pain disorder. She also suggested cognitive behavioral therapy for treatment of CPP. For patients who cannot afford cognitive behavioral therapy, there is a free online source at fibroguide.med.umich.edu. Other alternative treatment options include exercise, patient education, instruction on sleep hygiene, and neurostimulatory therapies.
Overall, all the speakers this morning agreed that CPP is rarely treated with one modality, and it is best treated with a multidisciplinary approach.
Let’s get social!
The afternoon was spent learning about ways to use social networking sites to educate our patients, in another postgraduate course on “Making Media Social,” presented by the SGS Social Media Committee. Given that a recent survey demonstrated that 74.1% of women have some type of social networking account, it can be a very useful source for medical information for patients. If you have any questions about what is appropriate on social media, check out ACOG committee opinion 622.
Here are some tips that I learned:
Facebook:
- Keep your private Facebook page private and create a separate professional Facebook page
- Adjust your login setting so only administrators can post on your professional page
- Adjust settings so your professional profile cannot be “tagged”
- If a patient contacts your personal page, direct them to your professional page
- Do not give medical advice since Facebook is not digitally encrypted
Twitter:
- “Short bursts of inconsequential information”
- Follow societies, medical centers, and medical journals
LinkedIn:
- It provides a great way to find jobs, people, and business opportunities that are recommended by someone in your contact group
- It is specifically there to help you grow your business and show people who you are and where you have come from
Doximity:
Before we get to tips, first, what is it? Well, Doximity is basically a “LinkedIn” for physicians. It is “a way to find relevant specialists for patients; a rolodex; an email and text service; and a virtual lounge.” It is currently transforming from social network into a ‘platform.’ Now more than 1,000 hospitals and health systems are part of Doximity. Tips:
- There is a secure message option, which is HIPAA compliant
- Provides a way for residents and fellows to understand possible future places of employment
- It is a great way to find someone to refer patients to in an unfamiliar location
Vimeo:
- A benefit over YouTube is the lack of advertisements
- Check out the SGS video archives!
- You also can set privacy settings and embedding stats
Fifty-nine percent of US adults have looked online for health information in the past year. Therefore, it is important for physicians to get good information out for people to see!
A relaxing day’s end
The night ended with a beautiful poolside reception! I can’t wait to see what day 2 will bring!
4/13/16. DAY 4 AT SGS
A jam-packed day of sessions, posters, awards, and clinical updates
Our last educational day was kicked off by a fascinating lecture by Dr. Amy Park on the “Genetic Determinants of Pelvic Organ Prolapse in Women of European American Descent: The Women’s Health Initiative.” Dr. Park and her colleagues found that there is evidence of phenotypic and genotypic heterogeneity in patients with pelvic organ prolapse, and there were 4 genetic loci identified that correlated with prolapse. Any uterine prolapse was associated with a genome-wide significant intergenic variant on chromosome 13, cystocele was associated with LOXL2, and all prolapse was associated with BMP.
Surmounting surgical site infection
Dr. Sarah Andiman then gave a lecture on the effects of a perioperative bundle and offered timely feedback for surgical site infection (SSI) prevention in hysterectomy. We all know that wound infections are a major morbidity associated with surgery, and Dr. Andiman’s group at Yale found that, by implementing this prevention program, the surgical site infection decreased 52.8%. Another suggestion from the audience was to have all patients use chlorhexidine wipes the night before and morning of a surgery to decrease wound infection. Similarly, Dr. Ali Bazzi gave a lecture on “Chlorhexidine-Alcohol Compared with Povidone-Iodine for Surgical-Site Antisepsis after Abdominal Hysterectomy.” The chlorhexidine was associated with 30% lower odds of SSI compared with povidone-iodine, even though this group had several medical comorbidities and risk factors known for SSIs.
Oral poster presenters make several interesting points
Dr. Christopher Ripperda from UT Southwestern Medical Center in Dallas, Texas, found that medical comorbidities and the presence of detrusor overactivity and PVR are predictors of early postoperative voiding dysfunction following a midurethral sling placement. Dr. Nabila Noor then described a fabulous surgical alternative to the use of morcellation to remove the uterus after a supracervical hysterectomy. She described the technique for performing a posterior colpotomy and stated that patients who had a surgery performed at her institution using this technique did not experience increased postoperative pain or longer postoperative stay.
Dr. Jennifer Thompson then shed some light on a very important question related to the Sunshine Act: Are physicians including all of their disclosures when they submit articles to a conference? When the physicians who submitted an abstract to the Society of Gynecologic Surgeons (SGS) in 2015 were searched on the Centers for Medicare and Medicaid Services (CMS) website, 62% of them had incomplete disclosures, with a total of nondisclosed CMS transactions equaling $1.3 million. We can do better!
Status update: The FPRN and passing of the torch
Congratulations to Dr. Kristin Jacobs, the new Fellows’ Pelvic Research Network (FPRN) Chair! The morning session ended with an innovative video from Dr. Janet Li and colleagues on the “Use of Suprapubic Carter-Thomason Needle to Assist in Cystoscopic Excision of Intravesical Foreign Object.”
The winner of the Distinguished Surgeon Award was given to Dr. Javier Magrina, and the SGS gavel was passed on to Dr. Vivian Sung! Congratulations!
Dr. Stephanie Pickett kicked off the eighth scientific session with a study entitled, “Comparing Methods of NSAID Delivery for Postoperative Pain.” When she and her colleagues compared IV toradol to IV ibuprofen for postoperative pain control after urogynecologic surgery, they found that patients experienced similar rates of pain control and satisfaction regardless of the type of analgesia.
Why are patients being readmitted after gynecologic oncology surgery?
The answer to this question is important as readmission rates are being considered for physician and hospital reimbursement. Dr. MaryAnn Wilbur and colleagues looked at the rates of unplanned 30-day readmission in gyn oncology patients. The patients who were readmitted had the following characteristics: ovarian cancer, creation of ostomy, Charleston score >5, language barrier, and positive discharge screen. Gastrointestinal disturbance and SSI were the most common reasons for readmission, and the total readmission-related costs for these patients was about $4.5 million.
Considering tissue extraction, surgical complications, and cognitive impairment
We then had 3 fabulous oral poster presentations. Dr. Emily Von Bargen and colleagues presented a study entitled, “Prevalence of Occult Pre-malignant or Malignant Pathology at the time of Uterine Morcellation for Benign Disease.” They performed a multicenter retrospective cohort study and found that 1.2% of women had a premalignant or malignant uterine pathology after surgery, with a prevalence of 0.66% of occult malignancy. She was unable to identify risk factors for those patients who had a premalignant or malignant pathology. Overall she found a low prevalence of premalignant or malignant uterine pathology when uterine morcellation was performed for benign disease.
Dr. Alix Leader-Cramer from Northwestern University pointed out “risk factors for a 30-day perioperative complications for total vaginal hysterectomy,” including chronic steroid use, higher ASA classification, current smoking status, diabetes, and lower preoperative serum albumin and sodium levels. Adnexectomy and resident participation were also associated with increased perioperative complications. About 9.5% of patients had a perioperative complication in the study population studied.
Finally, Dr. Elisa Trowbridge pointed out in her talk, on “Cognitive Impairment among Elderly Urogynecologic Patients,” that cognitive impairment is very prevalent among such women aged older than 75 years, and the Mini-Cog is a feasible screening tool.
What a way to end an AMAZING conference!
The conference ended with a fabulous video presentation by Dr. Andrea Benton, entitled “Surgical Approaches to the Management of Bladder and Ureteral Endometriosis.” Overall, the themes of this year’s SGS conference were to:
- emphasize the importance of performing a vaginal hysterectomy when feasible
- continue to strive to balance innovation with experimentation
- ensure that patients are being operated on by surgeons who are competent and frequently performing the indicated procedure.
Thank you to everyone who shared their research to educate the attendees at the conference! I can’t wait until next year!
4/12/16. DAY 3 AT SGS
Vaginal hysterectomy, fecal incontinence, transgender surgery amid tackled topics in Palm Springs
I could get used to sipping my coffee with the sunny background here in Palm Springs! It was a beautiful morning to learn.
We started the day with breakfast and a fabulous lecture on the inferior gluteal neurovascular anatomy in female cadavers, and an insightful lecture by Dr. Bhumy Dave, who brought up concerns about tracking for obstetrics and gynecology residency programs. She specifically highlighted the need for more experience with vaginal hysterectomies for residents who are going to be in a subspecialty that performs vaginal surgery. As the number of hysterectomies, specifically vaginal hysterectomies, declines every year, we need to make sure we are adequately training the physicians who will be performing this procedure in the future. One solution is to have residents join a track their 4th year of residency, after their future career path has been established. Another possible solution would be to increase use of a simulation model for vaginal hysterectomy, as described by Dr. Douglas Miyazaki.
Indigo carmine replacement? A recent issue in gynecologic surgery resulted when there was a national shortage of indigo carmine, which is commonly used to identify UO efflux at the time of cystoscopy. Dr. Katie Propst provided a solution: In the setting of planned cystoscopy, she found that preoperative phenazopyridine is an acceptable alternative and its use led to similar UO identification as with indigo carmine without an increase in complications.
Who should have a vaginal hysterectomy? Dr. Jennifer Schmitt from the Mayo Clinic gave another wonderful lecture describing a decision-tree algorithm for determining the ideal route of hysterectomy. According to a retrospective review of patients at their institution, vaginal hysterectomy was associated with lower infection rates, operative times, and costs.
The highlight of the morning was a very insightful Presidential Address by Dr. Andrew Walter! Not only is a he a very entertaining speaker but he also shed some light on 2 challenges that we currently face in the field. He eloquently stated that, “every woman who is a candidate for a vaginal hysterectomy should be able to get one and have it performed competently, and every woman who needs surgery should have one performed by someone who performs enough surgeries every year to competently perform the surgery.” He frequently alluded to the wise Dr. Mayo, who stated, “The best interest of the patient is the only interest to be considered…” Let’s never forget this as physicians!
Do you find removing the adnexa challenging when performing vaginal surgery? Check out the amazing idea from the Cleveland Clinic shown in video presentation 05! They clearly demonstrate using a single-site gel port or surgical glove placed in the vaginal incision to perform laparoscopy through the vagina. What a novel idea to avoid any abdominal incisions when there is a difficult vaginal adnexal surgery!
After the morning break, we watched a master vaginal surgeon perform a sacral colpopexy through the vaginal route. For details on this method, please reference video presentation 06.
An increase in health care costs is a huge problem in this country. Dr. Mary Van Meter suggested that one area in which we can improve is in the operating room (OR), specifically through decreasing the number of instruments sterilized. She found that only approximately 20% of the instruments on the operating field were actually used by the OR physician. It costs about $3 per instrument on the tray at Vanderbilt University, she said. When you think of the few number of instruments actually used, if we work to limit the number of instruments on the trays, we could cut significant costs. As reimbursement is getting increasingly linked to cost reduction, we all should be thinking about innovative ways to cut costs.
The oral posters were all excellent!
Dr. Ann Peters showed that, at a high-volume tertiary-care center, multimodal preoperative testing failed to definitively identify leiomyosarcoma (LMS), and the factors associated with increased LMS risk included older age, menopause, and presence of fibroids with concurrent pelvic, uterine, or adnexal mass.
Dr. Kevin Kremer found that preoperative antibiotics were used in 23% of cases in which they were not indicated, and the increased use rate was associated with entrance into the abdomen during surgery, the individual surgeon, and time under anesthesia.
Dr. Jessica Heft then stated that the incontinence rate after midurethral sling revision for vaginal exposure or pain was significantly higher with a partial as opposed to complete mesh excision.
Fecal incontinence treatment options
Dr. Peter Rosenblatt tackled the issue of “Innovation or experimentation: Where do we draw the line?” in the TeLinde lecture. He started by describing a condition for which he feels we do not have an acceptable amount of treatment options for patients: fecal incontinence. He described how he observed that the puborectalis muscle, not the external anal sphincter, was critical for fecal continence. He then devised a surgery that created a sling that would act as a synthetic puborectalis muscle. He had amazing success until one patient had a serious complication. Should you abandon a successful, innovative surgery due to one very severe complication, was the question. Where do we draw the line? I don’t have an answer…but I do know that we all need to thank our puborectalis muscle for our daily fecal continence!
This is not a new issue in medicine, explained Dr. Rosenblatt. From the beginning of medicine, there has been a balance between innovation and experimentation. So, what is innovation? It is when someone improves upon a device or process. In medicine, is it innovation or just variation? We frequently use medications and devices “off label,” and these techniques often improve our surgeries and outcomes for our patients. Innovation comes about through careful planning, a necessity created by an emergency, advances in technology, and through evolution of a procedure. Who are the innovators? YOU are! We are the ones who understand the unmet needs and the potential opportunities for improving medicine. Let’s all work together to innovate NOT experiment and make medicine better so our patients have the best care possible!
“New Frontiers in Gynecologic Surgery: Transgender Surgery and Functional Clitoroplasty after Female Genital Mutilation”
The final talk for the day was by the groundbreaking Dr. Marci Bowers, whose lecture started by reminding everyone that there is a difference between gender identity and gender expression. Once a person knows his or her gender identity they use gender expression to express this to the world, she pointed out. Dr. Bowers is a true innovator and is performing gender reassignment surgeries as well as female genital mutilation corrective surgeries. She has perfected a one-stage vaginoplasty, and she showed a video of the procedure, which results in a 90% chance of orgasm. She also noted that she is able to restore clitoral function in 100% of the cases of genital mutilation, and she performs these procedures free of charge.
She reminded us that all ObGyns need to be trained in treating transgender patients, and given the high rate of suicide among adolescent transgender individuals, we all need to work together to provide a supportive medical environment to help these patients. What a fascinating end to the day!
Some relaxation, and entertainment, amid the sun and outdoors
We then had the afternoon to compete in a golf tournament, explore the area on mountain bikes, or lounge by the pool. Regardless of the daytime activities, we all came back together for the great lip-synch competition! All 4 teams gave an impressive performance, but the team from Brown University went home with the win! Such an entertaining event! (Thanks to incoming SGS President Vivian Sung @wih_sung for the pic!)
4/11/16. DAY 2 AT SGS
Experts talk surgical innovations, complementary therapies, value-based payment, and much more at SGS day 2
Wake up and learn! The second day of the 42nd Annual Scientific Meeting of the Society of Gynecologic Surgeons began with a review of research posters at the Poster Session as the sun rose over the Palm Springs mountains. We then moved indoors for the scientific sessions.
In the first lecture, "Reasons for Unplanned 30-Day Readmission After Hysterectomy for Benign Disease," Dr. Courtney Penn and colleagues reiterated that the postsurgical readmission rate is higher for patients undergoing abdominal hysterectomy compared with those who have a laparoscopic or vaginal hysterectomy. Similarly, Dr. Jennifer Schmitt and colleagues suggested that in a patient with a relative contraindication for vaginal hysterectomy, when this procedure is performed by an experienced surgeon there may not be increased complications. However, keep in mind that the study described—"A Comparison of Vaginal and Robotic Hysterectomy for Commonly Cited Relative Contraindications to Vaginal Hysterectomy"—was performed at the Mayo Clinic by expert, highly trained surgeons, and this fact may limit the generalizability of the study. As one audience member eloquently stated, it is important to remember that: "Just because it is feasible does not mean it is the correct procedure."
That yoga or barre class may be doing more good than you think! Lunge, bridge, and cat-into-cow movements may provide a greater degree of pelvic floor muscle unit recruitment than traditional Kegel exercises, according to a presentation by Dr. Bruce Crawford on Kegels versus specialized movement.
Perhaps those exercises should be recommended for surgeons as well. As Dr. Ruchira Singh pointed out, surgeons experience a high amount of musculoskeletal strain when performing vaginal procedures while sitting, regardless of the type of chair used during surgery. Dr. Singh and colleagues’ study, "Effect of Different Chairs on Work-Related Musculoskeletal Discomfort During Vaginal Surgery," found that while the round stool with a backrest and the Capisco chair were more comfortable, they did not eliminate the high risk for musculoskeletal strain, particularly in the head and neck.
Dr. Ann Peters and colleagues, from Magee-Womens Hospital of the University of Pittsburgh Medical Center, gave a fabulous video presentation on "Anatomic and Vascular Considerations in Laparoscopic Uterine Artery Ligation During Hysterectomy."
Need a novel treatment for interstitial cystitis/bladder pain syndrome? Consider mindfulness-based stress reduction. A randomized controlled study performed by Dr. Gregg Kanter and colleagues describes how this technique may help patients and could be considered a first-line therapy.
What is value-based payment and this new trend in reimbursement? And how does it apply to vaginal hysterectomy? Dr. Tina Groat addressed these issues in her keynote lecture. According to the American Congress of Obstetricians and Gynecologists, “Evidence demonstrates that, in general, vaginal hysterectomy is associated with better outcomes and fewer complications than laparoscopic or abdominal hysterectomy.” This is in opposition to what is actually being performed clinically. Dr. Groat explained that United Healthcare decided to incentivize physicians by requiring a prior authorization for all hysterectomies for benign disease. There is both a quality and cost benefit to performing a vaginal hysterectomy. Most insurance companies are moving away from a “fee for service” structure to performance-based payment. Change is always scary and, while I think the overall goal of moving toward the best care for our patients is a positive, this approach may create new challenges for the medical field. What do you think? Is performance-based payment beneficial? Or does it limit physicians and potentially force them to perform a procedure they do not feel as comfortable performing? Will this result in physicians rejecting certain patient populations? [Note from OBG MANAGEMENT: Let Dr. Collins know your thoughts through social media, or email OBG MANAGEMENT with a Letter to the Editor (rbarbieri@frontlinemedcom.com).]
The debate on the best route for hysterectomy continues: According to Dr. Carolyn Swenson and colleagues in their presentation, "Comparison of Robotic and Other Minimally Invasive Routes of Hysterectomy for Benign Indications," while there may be lower complications associated with robotic hysterectomy, the cost of performing a robotic hysterectomy is significantly higher than the cost of laparoscopic or vaginal hysterectomy, thus limiting its utility.
How can we teach a rare surgical procedure to learners? We channel our inner Martha Stewart and make a model out of a beef tongue and chicken. For about $8 a challenging and rare surgery can be taught to residents and medical students, according to the video presentation by Dr. Jana Illston and colleagues, titled "Modified Beef Tongue Model for Fourth-Degree Laceration Repair Simulation."
After the Day 2 lunch break, there was a rousing debate surrounding "Surgeons as Innovators—What Is the Patient Expecting?" Where do we draw the line between using an older more proven therapy as opposed to trying an innovative technology that may actually offer a potential benefit? Dr. Dennis Miller made a good point regarding innovation and pharmaceutical and device companies: If we ignore industry, we lose the ability to help with innovation and shape the future of medical treatments. Perhaps we should use the golden rule: If we would perform the surgery or use the device on ourselves, then we should perform it on our patient. Patients have a greater burden now, because there are more treatment options that they must choose among. Our job as physicians is to educate our patients and to guide them to innovative and evidence-based treatments.
Highlights from the afternoon oral poster session included a presentation by Dr. Caryn Russman that noted the high risk for recurrent urinary tract infection (UTI) after a mid-urethral sling procedure, which seems to be related to specific preoperative risk factors (such as a history of recurrent UTI). Dr. Tanya Hoke suggested that residents and attending physicians have inaccurate estimates of uterine weight, and an educational program may be necessary to improve these estimates. Finally, a study from Massachusetts General Hospital showed that a shorter stay in the hospital, ideally same-day surgery, resulted in a lower complication risk, lower number of emergency department visits, and a decreased readmission rate for patients undergoing urogynecology procedures.
The following recommendations were then suggested regarding vaginal hysterectomy:
- Preoperative prep with 4% chlorhexidine or povidine iodine
- Intracervical vasopressin injection to decrease blood loss
- Use of a pedicle-sealing device for pedicle ligation
- Vertical cuff closure is preferred to maximize vaginal length
Another important point made was that a prior cesarean delivery is not a contraindication to performing a vaginal hysterectomy.
Recommendations regarding recurrent UTI were also made, which include the recommendation for preoperative use of antibiotics to decrease the rate of UTI, with no benefit for a longer course of antibiotics.
News from the Fellows’ Pelvic Research Network
So much exciting research currently is ongoing with the FPRN! New project ideas include comparison of trimethoprim with methenamie for treatment of recurrent UTI; comparison of laparoscopic/robotic sacrocolpopexy with vaginal USLS for management of apical prolapse; a survey study examining surgeon preferences for timing of midurethral sling placement when performed at the time of pelvic organ prolapse (POP) repair; an assessment of the effect of a midurethal sling on overactive bladder in surgical repair in POP; and a study evaluating female pelvic reconstructive surgery in the setting of human immunodeficiency virus infection. It is so great to see the fellows working together to provide groundbreaking research!
Fun with stats
Learning statistics at the end of the day is never easy, but Dr. Matthew Barber did a fabulous job explaining this often-confusing topic. He reminded attendees that the key to learning statistics is repetition. One new recommendation he offered to enhance understanding is to use common language instead of numbers for P values. For example, instead of saying P <.001, use “is superior,” and instead of saying P = .3, use “seems not superior” or “inconclusive.”
A night to remember
The night ended with a wonderful awards ceremony and the president’s reception. Overall, day 2 was a very educational—and fun—day!
4/10/16. DAY 1 AT SGS
Postgrad courses address pain management and social media education
Mastering pelvic pain
With the beautiful Palm Springs, California, backdrop of mountains and palm trees, the 2016 meeting of the Society of Gynecologic Surgeons kicked off with 4 postgraduate courses. At the “Mastering Pelvic Pain: Strategies and Techniques for a Multimodal Approach” course, directed by Dr. Cara King, Dr. Matt Siedhoff explained the key components of the history and physical examination: Keep in mind that this generally is a multifactorial issue and may require a multidisciplinary approach, he told attendees. It is also important to make sure that the patient is fully prepared to combat the chronic pelvic pain (CPP) symptoms by focusing on the fundamentals, he said, including smoking, diet, exercise, weight loss, sleep, and relationship stress.
How is your posture? It turns out that something as simple as altering your posture can significantly affect pelvic floor control. Carol Sobeck, PT, demonstrated this importance with a simple group exercise that proved how the ability to contract the pelvic floor changes significantly with posture. Get to know your pelvic floor physical therapist—they are critical in helping with the treatment of CPP.
But what to do when physical therapy fails? Dr. Jennifer Gunter shed some light on this very difficult medical situation. One suggestion, she said, is to consider the possibility of a local presentation of a systemic issue and screen for the following: fibromyalgia, Ehlers-Danlos syndrome, statin use, and diabetes mellitus. Other treatment ideas include trigger point injections and onabotulinumtoxin A (Botox) therapy. A trigger point is a hypercontracted focus of muscle. To treat a trigger point, a needle must mechanically disrupt the trigger point to reduce the pelvic pain, and injection of local anesthetic is only used to help with postprocedure discomfort. Botox in my pelvis, you ask? Yes! The goal is to block presynaptic release of acetylcholine, which is very effective at reducing muscle spasm.
Tackling endometriosis. Dr. King then described surgical techniques for endometriosis. She recommended that, for mild disease not in close proximity to vital structures, ablation is likely equivalent to excision. For deeply infiltrating endometriosis, or lesions in close proximity to vital structures, excision is more beneficial. Excision is always beneficial for pathologic diagnosis, she said. And she offered this tip for bladder endometriosis: place a stitch in the nodule to allow for counter traction. Here is another tip, for ovarian cystectomy: inject vasopressin (20 U in 60 mL) to help dissect the plane between the ovary and cyst wall, and consider presacral neurectomy for midline pain.
Dr. Frank Tu then explained that we should not think of it as the “terrible triad: endometriosis, irritable bowel syndrome, and interstitial cystsis,” but rather as a system out of balance. Both peripheral and central mechanisms are involved in the generation and maintenance of cross-organ sensitization, he pointed out, which may explain why patients receive multiple diagnoses that describe a myriad of complaints due to a lack of overall homeostasis.
While Dr. Alaa Abd-Elsayed described innovative nerve blocks for CPP, he emphasized that no one specific treatment will result in a complete resolution of symptoms.
Vaginal mesh placement and pain. Dr. Mario Castellanos gave a fabulous lecture describing the pain issues that surround vaginal mesh placement. Interestingly, he noted that many patients had pelvic pain prior to placement of vaginal mesh, and that pain likely only will worsen with mesh placement. Mesh may cause pain by causing inflammation, visceral injury, muscle injury, and nerve injury. While there are guidelines for where mesh should be placed for bladder slings (TVT and TOT) and for prolapse repair, studies show, he pointed out, that the mesh placement often disrupts several muscle groups and may directly injure a nerve.
Alternatives to the typical diagnoses for CPP. The morning ended with a lecture by Dr. Suzie As-Sanie, in which she reminded everyone to start with “gold standard” therapy but, if those fail, consider alternative diagnoses or a central pain disorder. She also suggested cognitive behavioral therapy for treatment of CPP. For patients who cannot afford cognitive behavioral therapy, there is a free online source at fibroguide.med.umich.edu. Other alternative treatment options include exercise, patient education, instruction on sleep hygiene, and neurostimulatory therapies.
Overall, all the speakers this morning agreed that CPP is rarely treated with one modality, and it is best treated with a multidisciplinary approach.
Let’s get social!
The afternoon was spent learning about ways to use social networking sites to educate our patients, in another postgraduate course on “Making Media Social,” presented by the SGS Social Media Committee. Given that a recent survey demonstrated that 74.1% of women have some type of social networking account, it can be a very useful source for medical information for patients. If you have any questions about what is appropriate on social media, check out ACOG committee opinion 622.
Here are some tips that I learned:
Facebook:
- Keep your private Facebook page private and create a separate professional Facebook page
- Adjust your login setting so only administrators can post on your professional page
- Adjust settings so your professional profile cannot be “tagged”
- If a patient contacts your personal page, direct them to your professional page
- Do not give medical advice since Facebook is not digitally encrypted
Twitter:
- “Short bursts of inconsequential information”
- Follow societies, medical centers, and medical journals
LinkedIn:
- It provides a great way to find jobs, people, and business opportunities that are recommended by someone in your contact group
- It is specifically there to help you grow your business and show people who you are and where you have come from
Doximity:
Before we get to tips, first, what is it? Well, Doximity is basically a “LinkedIn” for physicians. It is “a way to find relevant specialists for patients; a rolodex; an email and text service; and a virtual lounge.” It is currently transforming from social network into a ‘platform.’ Now more than 1,000 hospitals and health systems are part of Doximity. Tips:
- There is a secure message option, which is HIPAA compliant
- Provides a way for residents and fellows to understand possible future places of employment
- It is a great way to find someone to refer patients to in an unfamiliar location
Vimeo:
- A benefit over YouTube is the lack of advertisements
- Check out the SGS video archives!
- You also can set privacy settings and embedding stats
Fifty-nine percent of US adults have looked online for health information in the past year. Therefore, it is important for physicians to get good information out for people to see!
A relaxing day’s end
The night ended with a beautiful poolside reception! I can’t wait to see what day 2 will bring!