User login
Opiate-prescribing standard decreases opiate use in hospitalized patients
Clinical question: Can an opiate-prescribing standard that favors oral and subcutaneous over intravenous administration reduce exposure to intravenous opiates for hospitalized adults?
Background: IV opiates, while effective for analgesia, may have a higher addictive potential because of the rapid and intermittent rises of peak concentrations. Subcutaneous and/or oral administration is a proven method of opioid delivery with similar bioavailability and efficacy of intravenous administration with more favorable pharmacokinetics.
Study design: Intervention-based quality improvement project.
Setting: Adult general medicine inpatient unit in an urban academic center.
Synopsis: Clinical leadership of the study unit collaborated to create an opiate-prescribing standard recommending oral over parenteral opioids and subcutaneous over IV if parental administration was required. The standard was promoted and reinforced with prescriber and nurse education, and prescribers were able to order intravenous opiates per usual protocol.
After a 6-month preintervention control period of 4,500 patient-days, the 3-month intervention period included 2,459 patient-days and led to a 84% decrease in IV opiate doses (0.06 vs. 0.39; P less than .001) and a 55% decrease in parenteral doses (0.18 vs. 0.39; P less than .001). Surprisingly there was a 23% decrease in overall doses of opiates (0.73 vs. 0.95; P = .02). Pain scores were similar between the two groups during hospital days 1-3 and improved in the intervention group between days 4 and 5.
This study was limited by a narrow focus, unblinded participants, and nursing-reported pain scores. While promising, more information is needed before establishing conclusions on a broader scale.
Bottom line: Establishing and promoting an opioid prescribing standard on a single unit led to a decrease in intravenous, parenteral, and overall opiates prescribed with similar or improved pain scores.
Citation: Ackerman AL et al. Association of an opioid standard of practice intervention with intravenous opioid exposure in hospitalized patients. JAMA Intern Med. 2018 Jun 1;178(6):759-63.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Can an opiate-prescribing standard that favors oral and subcutaneous over intravenous administration reduce exposure to intravenous opiates for hospitalized adults?
Background: IV opiates, while effective for analgesia, may have a higher addictive potential because of the rapid and intermittent rises of peak concentrations. Subcutaneous and/or oral administration is a proven method of opioid delivery with similar bioavailability and efficacy of intravenous administration with more favorable pharmacokinetics.
Study design: Intervention-based quality improvement project.
Setting: Adult general medicine inpatient unit in an urban academic center.
Synopsis: Clinical leadership of the study unit collaborated to create an opiate-prescribing standard recommending oral over parenteral opioids and subcutaneous over IV if parental administration was required. The standard was promoted and reinforced with prescriber and nurse education, and prescribers were able to order intravenous opiates per usual protocol.
After a 6-month preintervention control period of 4,500 patient-days, the 3-month intervention period included 2,459 patient-days and led to a 84% decrease in IV opiate doses (0.06 vs. 0.39; P less than .001) and a 55% decrease in parenteral doses (0.18 vs. 0.39; P less than .001). Surprisingly there was a 23% decrease in overall doses of opiates (0.73 vs. 0.95; P = .02). Pain scores were similar between the two groups during hospital days 1-3 and improved in the intervention group between days 4 and 5.
This study was limited by a narrow focus, unblinded participants, and nursing-reported pain scores. While promising, more information is needed before establishing conclusions on a broader scale.
Bottom line: Establishing and promoting an opioid prescribing standard on a single unit led to a decrease in intravenous, parenteral, and overall opiates prescribed with similar or improved pain scores.
Citation: Ackerman AL et al. Association of an opioid standard of practice intervention with intravenous opioid exposure in hospitalized patients. JAMA Intern Med. 2018 Jun 1;178(6):759-63.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Can an opiate-prescribing standard that favors oral and subcutaneous over intravenous administration reduce exposure to intravenous opiates for hospitalized adults?
Background: IV opiates, while effective for analgesia, may have a higher addictive potential because of the rapid and intermittent rises of peak concentrations. Subcutaneous and/or oral administration is a proven method of opioid delivery with similar bioavailability and efficacy of intravenous administration with more favorable pharmacokinetics.
Study design: Intervention-based quality improvement project.
Setting: Adult general medicine inpatient unit in an urban academic center.
Synopsis: Clinical leadership of the study unit collaborated to create an opiate-prescribing standard recommending oral over parenteral opioids and subcutaneous over IV if parental administration was required. The standard was promoted and reinforced with prescriber and nurse education, and prescribers were able to order intravenous opiates per usual protocol.
After a 6-month preintervention control period of 4,500 patient-days, the 3-month intervention period included 2,459 patient-days and led to a 84% decrease in IV opiate doses (0.06 vs. 0.39; P less than .001) and a 55% decrease in parenteral doses (0.18 vs. 0.39; P less than .001). Surprisingly there was a 23% decrease in overall doses of opiates (0.73 vs. 0.95; P = .02). Pain scores were similar between the two groups during hospital days 1-3 and improved in the intervention group between days 4 and 5.
This study was limited by a narrow focus, unblinded participants, and nursing-reported pain scores. While promising, more information is needed before establishing conclusions on a broader scale.
Bottom line: Establishing and promoting an opioid prescribing standard on a single unit led to a decrease in intravenous, parenteral, and overall opiates prescribed with similar or improved pain scores.
Citation: Ackerman AL et al. Association of an opioid standard of practice intervention with intravenous opioid exposure in hospitalized patients. JAMA Intern Med. 2018 Jun 1;178(6):759-63.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Focus on patient experience to cut readmission rates
Incorporate patient-reported quality measures
Hospitalists have focused much attention on reducing 30-day readmission rates, at a time when 15-20% of health care dollars spent on those readmissions is considered potentially preventable.
But until very recently, no study has explored patient perceptions of the likelihood of readmission during index admission. Now, that’s changed.
“Our objective was to examine associations between patient perceptions of care during index hospital admission and 30-day readmission,” says Jocelyn Carter, MD, of Massachusetts General Hospital, Boston, and lead author of November 2017 study in BMJ Quality & Safety.
Enrolled in the study were 846 patients at two inpatient adult medicine units at Massachusetts General, Boston; 201 (23.8%) of these patients were readmitted within 30 days. In multivariable models adjusting for baseline differences, respondents who reported being “very satisfied” with the care received during the index hospitalization were less likely to be readmitted; participants reporting that doctors “always listened to them carefully” also were less likely to be readmitted.
“These findings are important since they suggest that engaging patients in an assessment of communication quality, unmet needs, concerns, and overall experience during admission may help to identify issues that might not be captured in standard postdischarge surveys when the appropriate time for quality improvement interventions has passed,” Dr. Carter said. “Incorporating patient-reported measures during index hospitalizations may improve readmission rates and help predict which patients are more likely to be readmitted.”
Reference
Carter J et al. The association between patient experience factors and likelihood of 30-day readmission: A prospective cohort study. BMJ Qual Saf. 16 Nov 2017. Accessed Feb 2, 2018.
Incorporate patient-reported quality measures
Incorporate patient-reported quality measures
Hospitalists have focused much attention on reducing 30-day readmission rates, at a time when 15-20% of health care dollars spent on those readmissions is considered potentially preventable.
But until very recently, no study has explored patient perceptions of the likelihood of readmission during index admission. Now, that’s changed.
“Our objective was to examine associations between patient perceptions of care during index hospital admission and 30-day readmission,” says Jocelyn Carter, MD, of Massachusetts General Hospital, Boston, and lead author of November 2017 study in BMJ Quality & Safety.
Enrolled in the study were 846 patients at two inpatient adult medicine units at Massachusetts General, Boston; 201 (23.8%) of these patients were readmitted within 30 days. In multivariable models adjusting for baseline differences, respondents who reported being “very satisfied” with the care received during the index hospitalization were less likely to be readmitted; participants reporting that doctors “always listened to them carefully” also were less likely to be readmitted.
“These findings are important since they suggest that engaging patients in an assessment of communication quality, unmet needs, concerns, and overall experience during admission may help to identify issues that might not be captured in standard postdischarge surveys when the appropriate time for quality improvement interventions has passed,” Dr. Carter said. “Incorporating patient-reported measures during index hospitalizations may improve readmission rates and help predict which patients are more likely to be readmitted.”
Reference
Carter J et al. The association between patient experience factors and likelihood of 30-day readmission: A prospective cohort study. BMJ Qual Saf. 16 Nov 2017. Accessed Feb 2, 2018.
Hospitalists have focused much attention on reducing 30-day readmission rates, at a time when 15-20% of health care dollars spent on those readmissions is considered potentially preventable.
But until very recently, no study has explored patient perceptions of the likelihood of readmission during index admission. Now, that’s changed.
“Our objective was to examine associations between patient perceptions of care during index hospital admission and 30-day readmission,” says Jocelyn Carter, MD, of Massachusetts General Hospital, Boston, and lead author of November 2017 study in BMJ Quality & Safety.
Enrolled in the study were 846 patients at two inpatient adult medicine units at Massachusetts General, Boston; 201 (23.8%) of these patients were readmitted within 30 days. In multivariable models adjusting for baseline differences, respondents who reported being “very satisfied” with the care received during the index hospitalization were less likely to be readmitted; participants reporting that doctors “always listened to them carefully” also were less likely to be readmitted.
“These findings are important since they suggest that engaging patients in an assessment of communication quality, unmet needs, concerns, and overall experience during admission may help to identify issues that might not be captured in standard postdischarge surveys when the appropriate time for quality improvement interventions has passed,” Dr. Carter said. “Incorporating patient-reported measures during index hospitalizations may improve readmission rates and help predict which patients are more likely to be readmitted.”
Reference
Carter J et al. The association between patient experience factors and likelihood of 30-day readmission: A prospective cohort study. BMJ Qual Saf. 16 Nov 2017. Accessed Feb 2, 2018.
Launching a surgical comanagement project
Improving quality, patient satisfaction
When hospital medicine and surgical departments (usually orthopedics or neurosurgery) have joined in comanagement programs, improvements in quality metrics and patient satisfaction have often resulted.
At the Level 1 regional trauma center in which he works, Charles L. Kast, MD, and his colleagues wanted to try a comanagement agreement between hospital medicine and trauma surgery.
“The surgical team identified a need within their own department, which was to improve patient mortality and satisfaction in the inpatient setting,” said Dr. Kast, who is based at North Shore University Hospital, Manhasset, N.Y. “Their leadership sought out our hospital medicine leadership team, who then worked together to synthesize their metrics. We were able to identify other quality indicators, such as readmission rates and hospital-acquired conditions, which we felt could also benefit from our services in order to help them improve.”
Five hospitalists became members of the comanagement team. A single hospitalist rotated for 2 weeks at a time, during which they were relieved of routine hospital medicine rounding responsibilities. The hospitalist attended daily interdisciplinary rounds with the trauma surgery team, during which he/she identified patients that could benefit from hospital medicine comanagement: Patients who were over age 65 years, had multiple chronic medical conditions, or were on high-risk medications were preferentially selected. Approximately 10 patients were seen daily.
The comanagement program was well received by trauma surgeons, who talked about improved patient communication and a fostered sense of collegiality. Preliminary quality and patient satisfaction metrics were also positive.
A top takeaway is that the benefits of surgical comanagement can be demonstrated in “atypical” collaborations, depending on the needs of the department and the hospital’s vision.
“The gains in improved patient quality metrics are only half of the story,” Dr. Kast said. “Collaborating in surgical comanagement improves the satisfaction of the hospitalists and surgeons involved and can lead to future quality improvement projects or original research, both of which we are currently pursuing.”
Reference
Kast C et al. The successful development of a hospital medicine-trauma surgery co-management program [abstract]. J Hosp Med. 2017;12(suppl 2). Accessed Feb. 2, 2018.
Improving quality, patient satisfaction
Improving quality, patient satisfaction
When hospital medicine and surgical departments (usually orthopedics or neurosurgery) have joined in comanagement programs, improvements in quality metrics and patient satisfaction have often resulted.
At the Level 1 regional trauma center in which he works, Charles L. Kast, MD, and his colleagues wanted to try a comanagement agreement between hospital medicine and trauma surgery.
“The surgical team identified a need within their own department, which was to improve patient mortality and satisfaction in the inpatient setting,” said Dr. Kast, who is based at North Shore University Hospital, Manhasset, N.Y. “Their leadership sought out our hospital medicine leadership team, who then worked together to synthesize their metrics. We were able to identify other quality indicators, such as readmission rates and hospital-acquired conditions, which we felt could also benefit from our services in order to help them improve.”
Five hospitalists became members of the comanagement team. A single hospitalist rotated for 2 weeks at a time, during which they were relieved of routine hospital medicine rounding responsibilities. The hospitalist attended daily interdisciplinary rounds with the trauma surgery team, during which he/she identified patients that could benefit from hospital medicine comanagement: Patients who were over age 65 years, had multiple chronic medical conditions, or were on high-risk medications were preferentially selected. Approximately 10 patients were seen daily.
The comanagement program was well received by trauma surgeons, who talked about improved patient communication and a fostered sense of collegiality. Preliminary quality and patient satisfaction metrics were also positive.
A top takeaway is that the benefits of surgical comanagement can be demonstrated in “atypical” collaborations, depending on the needs of the department and the hospital’s vision.
“The gains in improved patient quality metrics are only half of the story,” Dr. Kast said. “Collaborating in surgical comanagement improves the satisfaction of the hospitalists and surgeons involved and can lead to future quality improvement projects or original research, both of which we are currently pursuing.”
Reference
Kast C et al. The successful development of a hospital medicine-trauma surgery co-management program [abstract]. J Hosp Med. 2017;12(suppl 2). Accessed Feb. 2, 2018.
When hospital medicine and surgical departments (usually orthopedics or neurosurgery) have joined in comanagement programs, improvements in quality metrics and patient satisfaction have often resulted.
At the Level 1 regional trauma center in which he works, Charles L. Kast, MD, and his colleagues wanted to try a comanagement agreement between hospital medicine and trauma surgery.
“The surgical team identified a need within their own department, which was to improve patient mortality and satisfaction in the inpatient setting,” said Dr. Kast, who is based at North Shore University Hospital, Manhasset, N.Y. “Their leadership sought out our hospital medicine leadership team, who then worked together to synthesize their metrics. We were able to identify other quality indicators, such as readmission rates and hospital-acquired conditions, which we felt could also benefit from our services in order to help them improve.”
Five hospitalists became members of the comanagement team. A single hospitalist rotated for 2 weeks at a time, during which they were relieved of routine hospital medicine rounding responsibilities. The hospitalist attended daily interdisciplinary rounds with the trauma surgery team, during which he/she identified patients that could benefit from hospital medicine comanagement: Patients who were over age 65 years, had multiple chronic medical conditions, or were on high-risk medications were preferentially selected. Approximately 10 patients were seen daily.
The comanagement program was well received by trauma surgeons, who talked about improved patient communication and a fostered sense of collegiality. Preliminary quality and patient satisfaction metrics were also positive.
A top takeaway is that the benefits of surgical comanagement can be demonstrated in “atypical” collaborations, depending on the needs of the department and the hospital’s vision.
“The gains in improved patient quality metrics are only half of the story,” Dr. Kast said. “Collaborating in surgical comanagement improves the satisfaction of the hospitalists and surgeons involved and can lead to future quality improvement projects or original research, both of which we are currently pursuing.”
Reference
Kast C et al. The successful development of a hospital medicine-trauma surgery co-management program [abstract]. J Hosp Med. 2017;12(suppl 2). Accessed Feb. 2, 2018.
Paradigm shifts in palliative care
Better engagement with patients essential
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
Better engagement with patients essential
Better engagement with patients essential
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
Hospital-level care coordination strategies and the patient experience
Clinical question: Does patient experience correlate with specific hospital care coordination and transition strategies, and if so, which strategies most strongly correlate with higher patient experience scores?
Background: Patient experience is an increasingly important measure in value-based payment programs. However, progress has been slow in improving patient experience, and little empirical data exist regarding which strategies are effective. Care transitions are critical times during a hospitalization, with many hospitals already implementing measures to improve the discharge process and prevent readmission of patients. It is not known whether those measures also influence patient experience scores, and if they do improve scores, which measures are most effective at doing so.
Study design: An analytic observational survey design.
Setting: Hospitals eligible for the Hospital Readmissions Reduction Program (HRRP) between June 2013 and December 2014.
Synopsis: A survey was developed and given to chief medical officers at 1,600 hospitals between June 2013 and December 2014; the survey assessed care coordination strategies employed by these institutions. 992 hospitals (62% response rate) were subsequently categorized as “low-strategy,” “mid-strategy,” or “high-strategy” hospitals. Patient satisfaction scores from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey in 2014 were correlated to the number of strategies and the specific strategies each hospital employed. In general, the higher-strategy hospitals had significantly higher HCAHPS survey scores than did low-strategy hospitals (+2.23 points; P less than .001). Specifically, creating and sharing a discharge summary prior to discharge (+1.43 points; P less than .001), using a discharge planner (+1.71 points; P less than .001), and calling patients 48 hours post discharge (+1.64 points; P less than .001) all resulted in overall higher hospital ratings by patients.
One limitation of this study is that no causal inference can be made between the specific strategies associated with higher HCAHPS scores and care coordination strategies.
Bottom line: Hospital-led care transition strategies with direct patient interactions led to higher patient satisfaction scores.
Citation: Figueroa JF et al. Hospital-level care coordination strategies associated with better patient experience. BMJ Qual Saf. 2018 Apr 4. doi: 10.1136/bmjqs-2017-007597.
Dr. Tsien is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: Does patient experience correlate with specific hospital care coordination and transition strategies, and if so, which strategies most strongly correlate with higher patient experience scores?
Background: Patient experience is an increasingly important measure in value-based payment programs. However, progress has been slow in improving patient experience, and little empirical data exist regarding which strategies are effective. Care transitions are critical times during a hospitalization, with many hospitals already implementing measures to improve the discharge process and prevent readmission of patients. It is not known whether those measures also influence patient experience scores, and if they do improve scores, which measures are most effective at doing so.
Study design: An analytic observational survey design.
Setting: Hospitals eligible for the Hospital Readmissions Reduction Program (HRRP) between June 2013 and December 2014.
Synopsis: A survey was developed and given to chief medical officers at 1,600 hospitals between June 2013 and December 2014; the survey assessed care coordination strategies employed by these institutions. 992 hospitals (62% response rate) were subsequently categorized as “low-strategy,” “mid-strategy,” or “high-strategy” hospitals. Patient satisfaction scores from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey in 2014 were correlated to the number of strategies and the specific strategies each hospital employed. In general, the higher-strategy hospitals had significantly higher HCAHPS survey scores than did low-strategy hospitals (+2.23 points; P less than .001). Specifically, creating and sharing a discharge summary prior to discharge (+1.43 points; P less than .001), using a discharge planner (+1.71 points; P less than .001), and calling patients 48 hours post discharge (+1.64 points; P less than .001) all resulted in overall higher hospital ratings by patients.
One limitation of this study is that no causal inference can be made between the specific strategies associated with higher HCAHPS scores and care coordination strategies.
Bottom line: Hospital-led care transition strategies with direct patient interactions led to higher patient satisfaction scores.
Citation: Figueroa JF et al. Hospital-level care coordination strategies associated with better patient experience. BMJ Qual Saf. 2018 Apr 4. doi: 10.1136/bmjqs-2017-007597.
Dr. Tsien is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: Does patient experience correlate with specific hospital care coordination and transition strategies, and if so, which strategies most strongly correlate with higher patient experience scores?
Background: Patient experience is an increasingly important measure in value-based payment programs. However, progress has been slow in improving patient experience, and little empirical data exist regarding which strategies are effective. Care transitions are critical times during a hospitalization, with many hospitals already implementing measures to improve the discharge process and prevent readmission of patients. It is not known whether those measures also influence patient experience scores, and if they do improve scores, which measures are most effective at doing so.
Study design: An analytic observational survey design.
Setting: Hospitals eligible for the Hospital Readmissions Reduction Program (HRRP) between June 2013 and December 2014.
Synopsis: A survey was developed and given to chief medical officers at 1,600 hospitals between June 2013 and December 2014; the survey assessed care coordination strategies employed by these institutions. 992 hospitals (62% response rate) were subsequently categorized as “low-strategy,” “mid-strategy,” or “high-strategy” hospitals. Patient satisfaction scores from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey in 2014 were correlated to the number of strategies and the specific strategies each hospital employed. In general, the higher-strategy hospitals had significantly higher HCAHPS survey scores than did low-strategy hospitals (+2.23 points; P less than .001). Specifically, creating and sharing a discharge summary prior to discharge (+1.43 points; P less than .001), using a discharge planner (+1.71 points; P less than .001), and calling patients 48 hours post discharge (+1.64 points; P less than .001) all resulted in overall higher hospital ratings by patients.
One limitation of this study is that no causal inference can be made between the specific strategies associated with higher HCAHPS scores and care coordination strategies.
Bottom line: Hospital-led care transition strategies with direct patient interactions led to higher patient satisfaction scores.
Citation: Figueroa JF et al. Hospital-level care coordination strategies associated with better patient experience. BMJ Qual Saf. 2018 Apr 4. doi: 10.1136/bmjqs-2017-007597.
Dr. Tsien is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Does nurse-physician rounding matter?
Advancing the Quadruple Aim
Inadequate and fragmented communication between physicians and nurses can lead to unwelcome events for the hospitalized patient and clinicians. Missing orders, medication errors, patient misidentification, and lack of physician awareness of significant changes in patient status are just some examples of how deficits in formal communication can affect health outcomes during acute stays.
A 2000 Institute of Medicine report showed that bad systems, not bad people, account for the majority of errors and injuries caused by complexity, professional fragmentation, and barriers in communication. Their recommendation was to train physicians, nurses, and other professionals in teamwork.1,2 However, as Milisa Manojlovich, PhD, RN, found, there are significant differences in how physicians and nurses perceive collaboration and communication.3
Nurse-physician rounding was historically standard for patient care during hospitalization. When physicians split time between inpatient and outpatient care, nurses had to maximize their time to collaborate and communicate with physicians whenever the physicians left their outpatient offices to come and round on their patients. Today most inpatient care is delivered by hospitalists on a 24-hour basis. This continuous availability of physicians reduces the perceived need to have joint rounds.
However, health care teams in acute care facilities now face higher and sicker patient volumes, different productivity models and demands, new compliance standards, changing work flows, and increased complexity of treatment and management of patients. This has led to gaps in timely communication and partnership.4-6 Erosion of the traditional nurse-physician relationships affects the quality of patient care, the patient’s experience, and patient safety.8-10 Poor communication among health care team members is one of the most common causes of patient care errors.4 Poor nurse-physician communication can also lead to medical errors, poor outcomes caused by lack of coordination within the treatment team, increased use of unnecessary resources with inefficiency, and increases in the complexity of communication among team members, and time wastage.5,7,11 All these lead to poor work flows and directly affect patient safety.7
At Lee Health System in Lee County, Fla., we saw an opportunity in this changing health care environment to promote nurse-physician rounding. We created a structured, standardized process for morning rounding and engaged unit clerks, nursing leadership, and hospitalist service line leaders. We envisioned improvement of the patient experience, nurse-physician relationship, quality of care, the discharge planning process, and efficiency, as well as decreasing length of stay, improving communication, and bringing the patient and the treatment team closer, as demonstrated by Bradley Monash, MD, et al.12
Some data suggest that patient-centered bedside rounds on hospitalized patients have no effect on patient perceptions or their satisfaction with care.13 However, we felt that collaboration among a multidisciplinary team would help us achieve better outcomes. For example, our patients would perceive the care team (MD-RN) as a cohesive unit, and in turn gain trust in the members of the treatment team, as found by Nathalie McIntosh, PhD, et al and by Jason Ramirez, MD.7,16 Our vision was to empower nurses to be advocates for patients and their family members as they navigated their acute care admission. Nurses could also support physicians by communicating the physicians’ care plans to families and patients. After rounding with the physician, the nurse would be part of the decision-making process and care planning.17
Every rounding session had discharge planning and hospital stay expectations that were shared with the patient and nurse, who could then partner with case managers and social workers, which would streamline and reduce length of stay.14 We hoped rounding would also decrease the number of nurse pages to clarify or question orders. This would, in turn, improve daily work flow for the physicians and the nursing team with improvements in employee satisfaction scores.15 A study also has demonstrated a reduction in readmission rates from nurse-physician rounding.19
A disconnect in communication and trust between physicians and the nursing staff was reflected in low patient experience scores and perceived quality of care received during in-hospital stay. Gwendolyn Lancaster, EdD, MSN, RN, CCRN, et al, as well as a Joint Commission report, demonstrated how a lack of communication and poor team dynamics can translate to poor patient experience and be a major cause for sentinel events.6,20 Artificial, forced hierarchies and role perception among health care team members led to frustration, hostility, and distrust, which compromises quality and patient safety.1
One of our biggest challenges when we started this project was explaining the “Why” to the hospitalist group and nursing staff. Physicians were used to being the dominant partner in the team. Partnering with and engaging nurses in shared decision making and care planning was a seismic shift in culture and work flow within the care team. Early gains helped skeptical team members begin to understand the value in nurse-physician rounding. Near universal adoption of the rounding process at Lee Health has caused improvements in the working relationship and trust among the health care professionals. We have seen improvements in utilization management, as well as appropriateness and timeliness of resource use, because of better communication and understanding of care plans by nursing and physicians. Collaboration with specialists and alignment in care planning are other gains. Hospitalists and nurses are both very satisfied with the decrease in the number of pages during the day, and this has lowered stressors on health care teams.
How we did it
Nurse-physician rounding is a proven method to improve collaboration, communication, and relationships among health care team members in acute care facilities. In the complex health care challenges faced today, this improved work flow for taking care of patients can help advance the Quadruple Aim of high quality, low cost, improved patient experience, physician, and staff satisfaction.21
Lee Health System includes four facilities in Lee County, with a total of 1,216 licensed adult acute care beds. The pilot project was started in 2014.
Initially the vice president of nursing and the hospitalist medical director met to create an education plan for nurses and physicians. We chose one adult medicine unit to pilot the project because there already existed a closely knit nursing and hospitalist team. In our facility there is no strict geographical rounding; each hospitalist carries between three and six patients in the unit. As a first step, a nurse floor assignment sheet was faxed in the morning to the hospitalist office with the direct phone numbers of the nurses. The unit clerk, using physician assignments in the EHR, teamed up the physician and nurses for rounding. Once the physician arrived at the unit, he or she checked in with the unit clerk, who alerted nurses that the hospitalist was available on the floor to commence rounding. If the primary nurse was unavailable because of other duties or breaks, the charge nurse rounded with the physician.
Once in the room with the patient, the duo introduced themselves as members of the treatment team and acknowledged the patient’s needs. During the visit, care plans and treatment were reviewed, the patient’s questions were answered, a physical exam was completed, and lab and imaging results were discussed; the nurse also helped raise questions he or she had received from family members so answers could be communicated to the family later. Patients appreciated knowing that their physicians and nurses were working together as a team for their safety and recovery. During the visit, care was taken to focus specially on the course of hospitalization and discharge planning.
We tracked the rounding with a manual paper process maintained by the charge nurse. Our initial rounding rates were 30%-40%, and we continued to promote this initiative to the team, and eventually the importance and value of these rounds caught on with both nurses and physicians, and now our current average rounding rate is 90%. We then decided to scale this to all units in the hospital.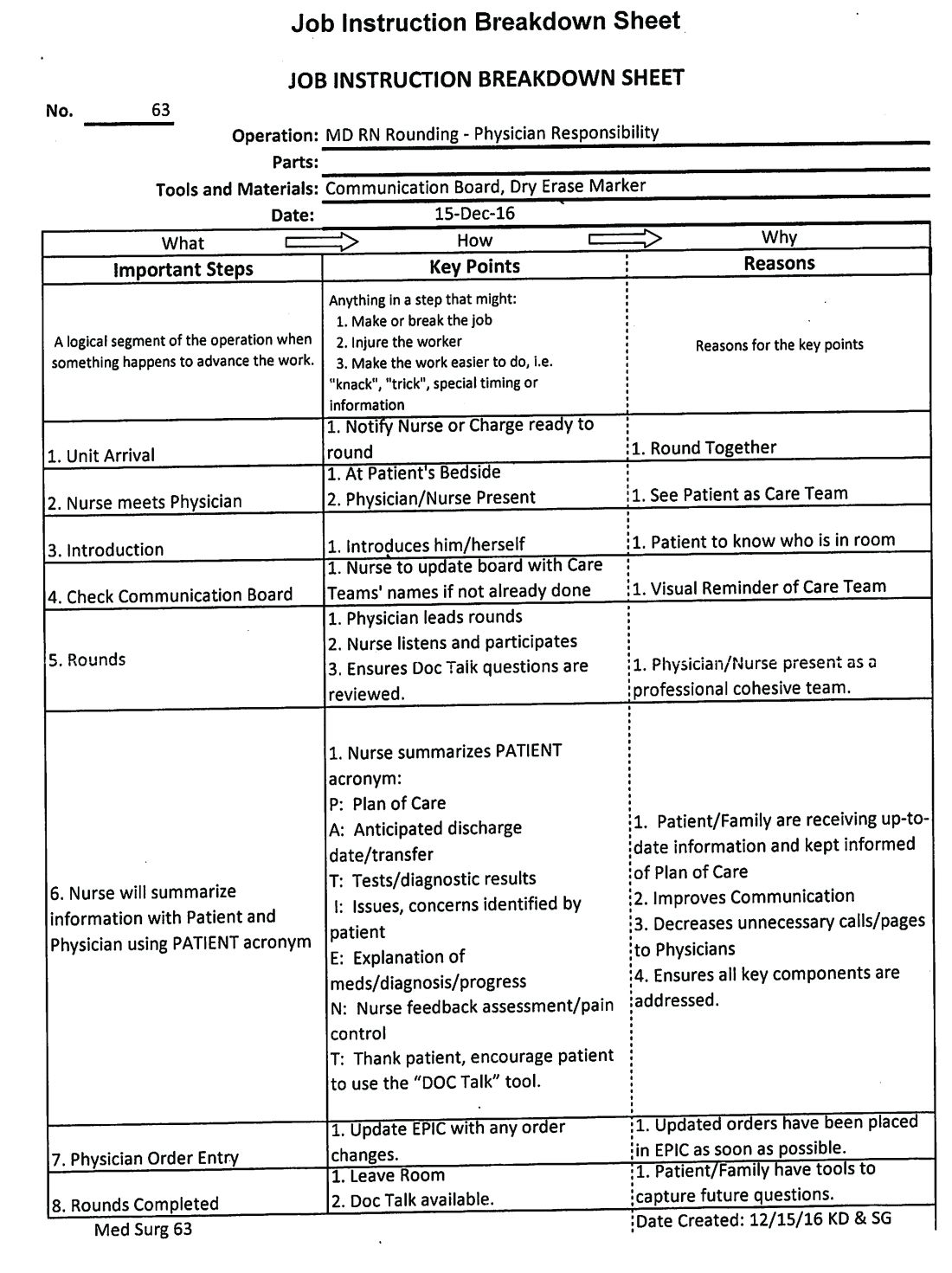
This process was repeated at other hospitals in the system once a standardized work flow was created (See Image 1). This initiative was next presented to the health system board of directors, who agreed that nurse-physician rounding should be the standard of care across our health system. Through partnership and collaboration with the IT department, we developed a tool to track nurse-physician rounding through our EHR system, which gave accountability to both physicians and nurses.
In conclusion, improved communication by timely nurse-physician rounding can lead to better outcomes for patients and also reduce costs and improve patient and staff experience, advancing the Quadruple Aim. Moving forward to build and sustain this work flow, we plan to continue nurse-physician collaboration across the health system consistently and for all areas of acute care operations.
Explaining the “Why,” sharing data on the benefits of the model, and reinforcing documentation of the rounding in our EHR are some steps we have put into action at leadership and staff meetings to sustain the activity. We are soliciting feedback, as well as monitoring and identifying any unaddressed barriers during rounding. Addition of this process measure to our quality improvement bonus opportunity also has helped to sustain performance from our teams.
Dr. Laufer is system medical director of hospital medicine and transitional care at Lee Health in Ft. Myers, Fla. Dr. Prasad is chief medical officer of Lee Physician Group, Ft. Myers, Fla.
References
1. Leape LL et al. Five years after to err is human: What we have learned? JAMA. 2005;293(19):2384-90.
2. Sutcliffe KM et al. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-94.
3. Manojlovich M. Reframing communication with physicians as sensemaking. J Nurs Care Qual. 2013 Oct-Dec;28(4):295-303.
4. Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals. Crit Care Nurse. 2009 Dec;29(6):58-69.
5. Asthon J et al. Qualitative evaluation of regular morning meeting aimed at improving interdisciplinary communication and patient outcomes. Int J Nurs Pract. 2005 Oct;11(5):206-13.
6. Lancaster G et al. Interdisciplinary Communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275-84.
7. McIntosh N et al. Impact of provider coordination on nurse and physician perception of patient care quality. J Nurs Care Qual. 2014 Jul-Sep;29(3):269-79.
8. Jo M et al. An organizational assessment of disruptive clinical behavior. J Nurs Care Qual. 2013 Apr-Jun;28(2):110-21.
9. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, 2010.
10. O’Connor P et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016 Jun;28(3):339-45.
11. Manojlovich M. Nurse/Physician communication through a sense making lens. Med Care. 2010 Nov;48(11):941-6.
12. Monash B et al. Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. J Hosp Med. 2017 Mar;12(3):143-9.
13. O’Leary KJ et al. Effect of patient-centered bedside rounds on hospitalized patients decision control, activation and satisfaction with care. BMJ Qual Saf. 2016 Dec;25(12):921-8.
14. Dutton RP et al. Daily multidisciplinary rounds shorten length of stay for trauma patients. J Trauma. 2003 Nov;55(5):913-9.
15. Manojlovich M et al. Healthy work environments, nurse-physician communication, and patients’ outcomes. Am J Crit Care. 2007 Nov;16(6):536-43.
16. Ramirez J et al. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. 2016 Feb;109(2):112-5.
17. Sollami A et al. Nurse-Physician collaboration: A meta-analytical investigation of survey scores. J Interprof Care. 2015 May;29(3):223-9.
18. House S et al. Nurses and physicians perceptions of nurse-physician collaboration. J Nurs Adm. 2017 Mar;47(3):165-71.
19. Townsend-Gervis M et al. Interdisciplinary rounds and structured communications reduce re-admissions and improve some patients’ outcomes. West J Nurs Res. 2014 Aug;36(7):917-28.
20. The Joint Commission. Sentinel Events. http://www.jointcommission.org/sentinel_event.aspx. Accessed Oct 2017.
21. Bodenheimer T et al. From Triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6.
Advancing the Quadruple Aim
Advancing the Quadruple Aim
Inadequate and fragmented communication between physicians and nurses can lead to unwelcome events for the hospitalized patient and clinicians. Missing orders, medication errors, patient misidentification, and lack of physician awareness of significant changes in patient status are just some examples of how deficits in formal communication can affect health outcomes during acute stays.
A 2000 Institute of Medicine report showed that bad systems, not bad people, account for the majority of errors and injuries caused by complexity, professional fragmentation, and barriers in communication. Their recommendation was to train physicians, nurses, and other professionals in teamwork.1,2 However, as Milisa Manojlovich, PhD, RN, found, there are significant differences in how physicians and nurses perceive collaboration and communication.3
Nurse-physician rounding was historically standard for patient care during hospitalization. When physicians split time between inpatient and outpatient care, nurses had to maximize their time to collaborate and communicate with physicians whenever the physicians left their outpatient offices to come and round on their patients. Today most inpatient care is delivered by hospitalists on a 24-hour basis. This continuous availability of physicians reduces the perceived need to have joint rounds.
However, health care teams in acute care facilities now face higher and sicker patient volumes, different productivity models and demands, new compliance standards, changing work flows, and increased complexity of treatment and management of patients. This has led to gaps in timely communication and partnership.4-6 Erosion of the traditional nurse-physician relationships affects the quality of patient care, the patient’s experience, and patient safety.8-10 Poor communication among health care team members is one of the most common causes of patient care errors.4 Poor nurse-physician communication can also lead to medical errors, poor outcomes caused by lack of coordination within the treatment team, increased use of unnecessary resources with inefficiency, and increases in the complexity of communication among team members, and time wastage.5,7,11 All these lead to poor work flows and directly affect patient safety.7
At Lee Health System in Lee County, Fla., we saw an opportunity in this changing health care environment to promote nurse-physician rounding. We created a structured, standardized process for morning rounding and engaged unit clerks, nursing leadership, and hospitalist service line leaders. We envisioned improvement of the patient experience, nurse-physician relationship, quality of care, the discharge planning process, and efficiency, as well as decreasing length of stay, improving communication, and bringing the patient and the treatment team closer, as demonstrated by Bradley Monash, MD, et al.12
Some data suggest that patient-centered bedside rounds on hospitalized patients have no effect on patient perceptions or their satisfaction with care.13 However, we felt that collaboration among a multidisciplinary team would help us achieve better outcomes. For example, our patients would perceive the care team (MD-RN) as a cohesive unit, and in turn gain trust in the members of the treatment team, as found by Nathalie McIntosh, PhD, et al and by Jason Ramirez, MD.7,16 Our vision was to empower nurses to be advocates for patients and their family members as they navigated their acute care admission. Nurses could also support physicians by communicating the physicians’ care plans to families and patients. After rounding with the physician, the nurse would be part of the decision-making process and care planning.17
Every rounding session had discharge planning and hospital stay expectations that were shared with the patient and nurse, who could then partner with case managers and social workers, which would streamline and reduce length of stay.14 We hoped rounding would also decrease the number of nurse pages to clarify or question orders. This would, in turn, improve daily work flow for the physicians and the nursing team with improvements in employee satisfaction scores.15 A study also has demonstrated a reduction in readmission rates from nurse-physician rounding.19
A disconnect in communication and trust between physicians and the nursing staff was reflected in low patient experience scores and perceived quality of care received during in-hospital stay. Gwendolyn Lancaster, EdD, MSN, RN, CCRN, et al, as well as a Joint Commission report, demonstrated how a lack of communication and poor team dynamics can translate to poor patient experience and be a major cause for sentinel events.6,20 Artificial, forced hierarchies and role perception among health care team members led to frustration, hostility, and distrust, which compromises quality and patient safety.1
One of our biggest challenges when we started this project was explaining the “Why” to the hospitalist group and nursing staff. Physicians were used to being the dominant partner in the team. Partnering with and engaging nurses in shared decision making and care planning was a seismic shift in culture and work flow within the care team. Early gains helped skeptical team members begin to understand the value in nurse-physician rounding. Near universal adoption of the rounding process at Lee Health has caused improvements in the working relationship and trust among the health care professionals. We have seen improvements in utilization management, as well as appropriateness and timeliness of resource use, because of better communication and understanding of care plans by nursing and physicians. Collaboration with specialists and alignment in care planning are other gains. Hospitalists and nurses are both very satisfied with the decrease in the number of pages during the day, and this has lowered stressors on health care teams.
How we did it
Nurse-physician rounding is a proven method to improve collaboration, communication, and relationships among health care team members in acute care facilities. In the complex health care challenges faced today, this improved work flow for taking care of patients can help advance the Quadruple Aim of high quality, low cost, improved patient experience, physician, and staff satisfaction.21
Lee Health System includes four facilities in Lee County, with a total of 1,216 licensed adult acute care beds. The pilot project was started in 2014.
Initially the vice president of nursing and the hospitalist medical director met to create an education plan for nurses and physicians. We chose one adult medicine unit to pilot the project because there already existed a closely knit nursing and hospitalist team. In our facility there is no strict geographical rounding; each hospitalist carries between three and six patients in the unit. As a first step, a nurse floor assignment sheet was faxed in the morning to the hospitalist office with the direct phone numbers of the nurses. The unit clerk, using physician assignments in the EHR, teamed up the physician and nurses for rounding. Once the physician arrived at the unit, he or she checked in with the unit clerk, who alerted nurses that the hospitalist was available on the floor to commence rounding. If the primary nurse was unavailable because of other duties or breaks, the charge nurse rounded with the physician.
Once in the room with the patient, the duo introduced themselves as members of the treatment team and acknowledged the patient’s needs. During the visit, care plans and treatment were reviewed, the patient’s questions were answered, a physical exam was completed, and lab and imaging results were discussed; the nurse also helped raise questions he or she had received from family members so answers could be communicated to the family later. Patients appreciated knowing that their physicians and nurses were working together as a team for their safety and recovery. During the visit, care was taken to focus specially on the course of hospitalization and discharge planning.
We tracked the rounding with a manual paper process maintained by the charge nurse. Our initial rounding rates were 30%-40%, and we continued to promote this initiative to the team, and eventually the importance and value of these rounds caught on with both nurses and physicians, and now our current average rounding rate is 90%. We then decided to scale this to all units in the hospital.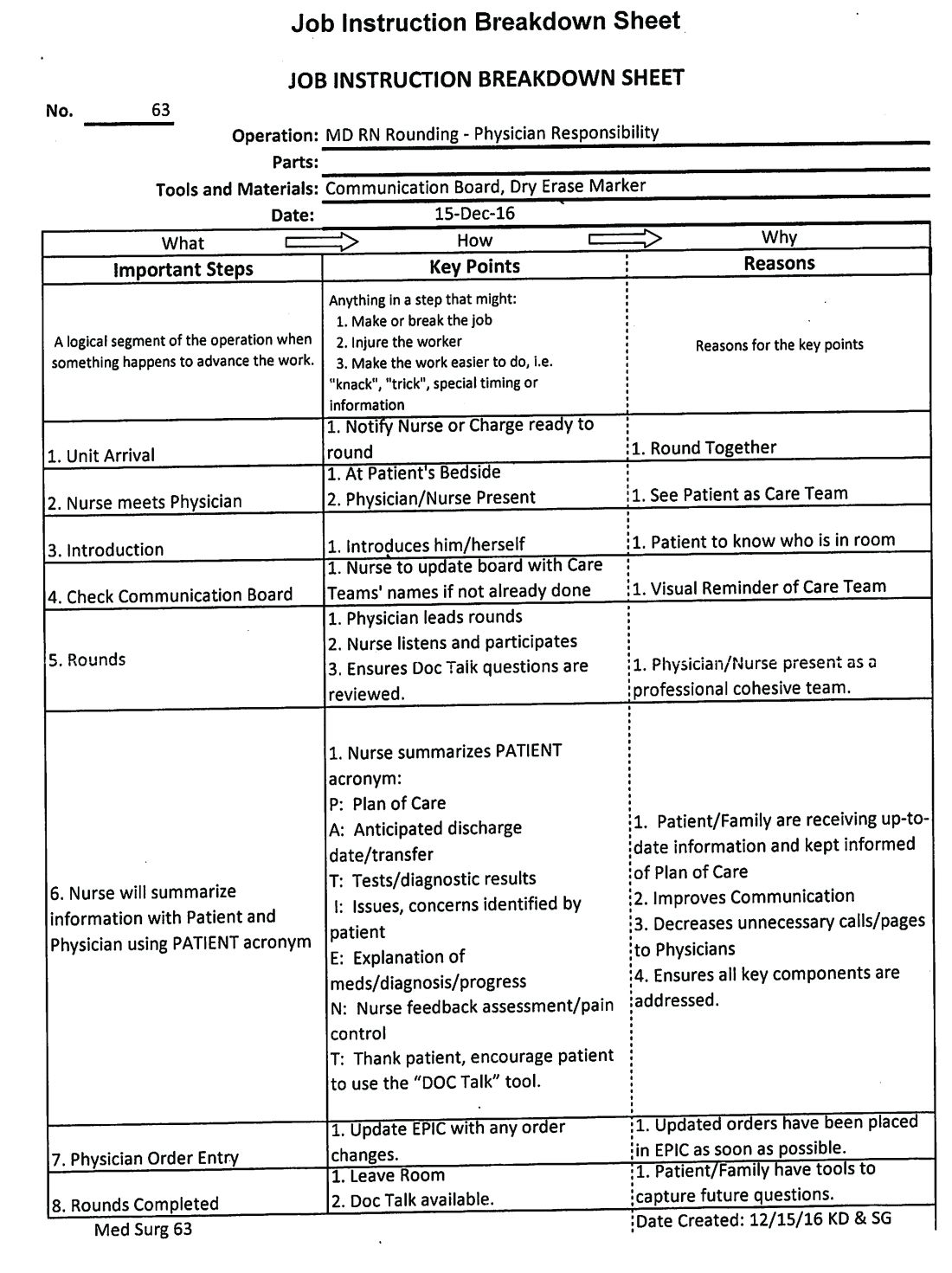
This process was repeated at other hospitals in the system once a standardized work flow was created (See Image 1). This initiative was next presented to the health system board of directors, who agreed that nurse-physician rounding should be the standard of care across our health system. Through partnership and collaboration with the IT department, we developed a tool to track nurse-physician rounding through our EHR system, which gave accountability to both physicians and nurses.
In conclusion, improved communication by timely nurse-physician rounding can lead to better outcomes for patients and also reduce costs and improve patient and staff experience, advancing the Quadruple Aim. Moving forward to build and sustain this work flow, we plan to continue nurse-physician collaboration across the health system consistently and for all areas of acute care operations.
Explaining the “Why,” sharing data on the benefits of the model, and reinforcing documentation of the rounding in our EHR are some steps we have put into action at leadership and staff meetings to sustain the activity. We are soliciting feedback, as well as monitoring and identifying any unaddressed barriers during rounding. Addition of this process measure to our quality improvement bonus opportunity also has helped to sustain performance from our teams.
Dr. Laufer is system medical director of hospital medicine and transitional care at Lee Health in Ft. Myers, Fla. Dr. Prasad is chief medical officer of Lee Physician Group, Ft. Myers, Fla.
References
1. Leape LL et al. Five years after to err is human: What we have learned? JAMA. 2005;293(19):2384-90.
2. Sutcliffe KM et al. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-94.
3. Manojlovich M. Reframing communication with physicians as sensemaking. J Nurs Care Qual. 2013 Oct-Dec;28(4):295-303.
4. Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals. Crit Care Nurse. 2009 Dec;29(6):58-69.
5. Asthon J et al. Qualitative evaluation of regular morning meeting aimed at improving interdisciplinary communication and patient outcomes. Int J Nurs Pract. 2005 Oct;11(5):206-13.
6. Lancaster G et al. Interdisciplinary Communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275-84.
7. McIntosh N et al. Impact of provider coordination on nurse and physician perception of patient care quality. J Nurs Care Qual. 2014 Jul-Sep;29(3):269-79.
8. Jo M et al. An organizational assessment of disruptive clinical behavior. J Nurs Care Qual. 2013 Apr-Jun;28(2):110-21.
9. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, 2010.
10. O’Connor P et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016 Jun;28(3):339-45.
11. Manojlovich M. Nurse/Physician communication through a sense making lens. Med Care. 2010 Nov;48(11):941-6.
12. Monash B et al. Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. J Hosp Med. 2017 Mar;12(3):143-9.
13. O’Leary KJ et al. Effect of patient-centered bedside rounds on hospitalized patients decision control, activation and satisfaction with care. BMJ Qual Saf. 2016 Dec;25(12):921-8.
14. Dutton RP et al. Daily multidisciplinary rounds shorten length of stay for trauma patients. J Trauma. 2003 Nov;55(5):913-9.
15. Manojlovich M et al. Healthy work environments, nurse-physician communication, and patients’ outcomes. Am J Crit Care. 2007 Nov;16(6):536-43.
16. Ramirez J et al. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. 2016 Feb;109(2):112-5.
17. Sollami A et al. Nurse-Physician collaboration: A meta-analytical investigation of survey scores. J Interprof Care. 2015 May;29(3):223-9.
18. House S et al. Nurses and physicians perceptions of nurse-physician collaboration. J Nurs Adm. 2017 Mar;47(3):165-71.
19. Townsend-Gervis M et al. Interdisciplinary rounds and structured communications reduce re-admissions and improve some patients’ outcomes. West J Nurs Res. 2014 Aug;36(7):917-28.
20. The Joint Commission. Sentinel Events. http://www.jointcommission.org/sentinel_event.aspx. Accessed Oct 2017.
21. Bodenheimer T et al. From Triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6.
Inadequate and fragmented communication between physicians and nurses can lead to unwelcome events for the hospitalized patient and clinicians. Missing orders, medication errors, patient misidentification, and lack of physician awareness of significant changes in patient status are just some examples of how deficits in formal communication can affect health outcomes during acute stays.
A 2000 Institute of Medicine report showed that bad systems, not bad people, account for the majority of errors and injuries caused by complexity, professional fragmentation, and barriers in communication. Their recommendation was to train physicians, nurses, and other professionals in teamwork.1,2 However, as Milisa Manojlovich, PhD, RN, found, there are significant differences in how physicians and nurses perceive collaboration and communication.3
Nurse-physician rounding was historically standard for patient care during hospitalization. When physicians split time between inpatient and outpatient care, nurses had to maximize their time to collaborate and communicate with physicians whenever the physicians left their outpatient offices to come and round on their patients. Today most inpatient care is delivered by hospitalists on a 24-hour basis. This continuous availability of physicians reduces the perceived need to have joint rounds.
However, health care teams in acute care facilities now face higher and sicker patient volumes, different productivity models and demands, new compliance standards, changing work flows, and increased complexity of treatment and management of patients. This has led to gaps in timely communication and partnership.4-6 Erosion of the traditional nurse-physician relationships affects the quality of patient care, the patient’s experience, and patient safety.8-10 Poor communication among health care team members is one of the most common causes of patient care errors.4 Poor nurse-physician communication can also lead to medical errors, poor outcomes caused by lack of coordination within the treatment team, increased use of unnecessary resources with inefficiency, and increases in the complexity of communication among team members, and time wastage.5,7,11 All these lead to poor work flows and directly affect patient safety.7
At Lee Health System in Lee County, Fla., we saw an opportunity in this changing health care environment to promote nurse-physician rounding. We created a structured, standardized process for morning rounding and engaged unit clerks, nursing leadership, and hospitalist service line leaders. We envisioned improvement of the patient experience, nurse-physician relationship, quality of care, the discharge planning process, and efficiency, as well as decreasing length of stay, improving communication, and bringing the patient and the treatment team closer, as demonstrated by Bradley Monash, MD, et al.12
Some data suggest that patient-centered bedside rounds on hospitalized patients have no effect on patient perceptions or their satisfaction with care.13 However, we felt that collaboration among a multidisciplinary team would help us achieve better outcomes. For example, our patients would perceive the care team (MD-RN) as a cohesive unit, and in turn gain trust in the members of the treatment team, as found by Nathalie McIntosh, PhD, et al and by Jason Ramirez, MD.7,16 Our vision was to empower nurses to be advocates for patients and their family members as they navigated their acute care admission. Nurses could also support physicians by communicating the physicians’ care plans to families and patients. After rounding with the physician, the nurse would be part of the decision-making process and care planning.17
Every rounding session had discharge planning and hospital stay expectations that were shared with the patient and nurse, who could then partner with case managers and social workers, which would streamline and reduce length of stay.14 We hoped rounding would also decrease the number of nurse pages to clarify or question orders. This would, in turn, improve daily work flow for the physicians and the nursing team with improvements in employee satisfaction scores.15 A study also has demonstrated a reduction in readmission rates from nurse-physician rounding.19
A disconnect in communication and trust between physicians and the nursing staff was reflected in low patient experience scores and perceived quality of care received during in-hospital stay. Gwendolyn Lancaster, EdD, MSN, RN, CCRN, et al, as well as a Joint Commission report, demonstrated how a lack of communication and poor team dynamics can translate to poor patient experience and be a major cause for sentinel events.6,20 Artificial, forced hierarchies and role perception among health care team members led to frustration, hostility, and distrust, which compromises quality and patient safety.1
One of our biggest challenges when we started this project was explaining the “Why” to the hospitalist group and nursing staff. Physicians were used to being the dominant partner in the team. Partnering with and engaging nurses in shared decision making and care planning was a seismic shift in culture and work flow within the care team. Early gains helped skeptical team members begin to understand the value in nurse-physician rounding. Near universal adoption of the rounding process at Lee Health has caused improvements in the working relationship and trust among the health care professionals. We have seen improvements in utilization management, as well as appropriateness and timeliness of resource use, because of better communication and understanding of care plans by nursing and physicians. Collaboration with specialists and alignment in care planning are other gains. Hospitalists and nurses are both very satisfied with the decrease in the number of pages during the day, and this has lowered stressors on health care teams.
How we did it
Nurse-physician rounding is a proven method to improve collaboration, communication, and relationships among health care team members in acute care facilities. In the complex health care challenges faced today, this improved work flow for taking care of patients can help advance the Quadruple Aim of high quality, low cost, improved patient experience, physician, and staff satisfaction.21
Lee Health System includes four facilities in Lee County, with a total of 1,216 licensed adult acute care beds. The pilot project was started in 2014.
Initially the vice president of nursing and the hospitalist medical director met to create an education plan for nurses and physicians. We chose one adult medicine unit to pilot the project because there already existed a closely knit nursing and hospitalist team. In our facility there is no strict geographical rounding; each hospitalist carries between three and six patients in the unit. As a first step, a nurse floor assignment sheet was faxed in the morning to the hospitalist office with the direct phone numbers of the nurses. The unit clerk, using physician assignments in the EHR, teamed up the physician and nurses for rounding. Once the physician arrived at the unit, he or she checked in with the unit clerk, who alerted nurses that the hospitalist was available on the floor to commence rounding. If the primary nurse was unavailable because of other duties or breaks, the charge nurse rounded with the physician.
Once in the room with the patient, the duo introduced themselves as members of the treatment team and acknowledged the patient’s needs. During the visit, care plans and treatment were reviewed, the patient’s questions were answered, a physical exam was completed, and lab and imaging results were discussed; the nurse also helped raise questions he or she had received from family members so answers could be communicated to the family later. Patients appreciated knowing that their physicians and nurses were working together as a team for their safety and recovery. During the visit, care was taken to focus specially on the course of hospitalization and discharge planning.
We tracked the rounding with a manual paper process maintained by the charge nurse. Our initial rounding rates were 30%-40%, and we continued to promote this initiative to the team, and eventually the importance and value of these rounds caught on with both nurses and physicians, and now our current average rounding rate is 90%. We then decided to scale this to all units in the hospital.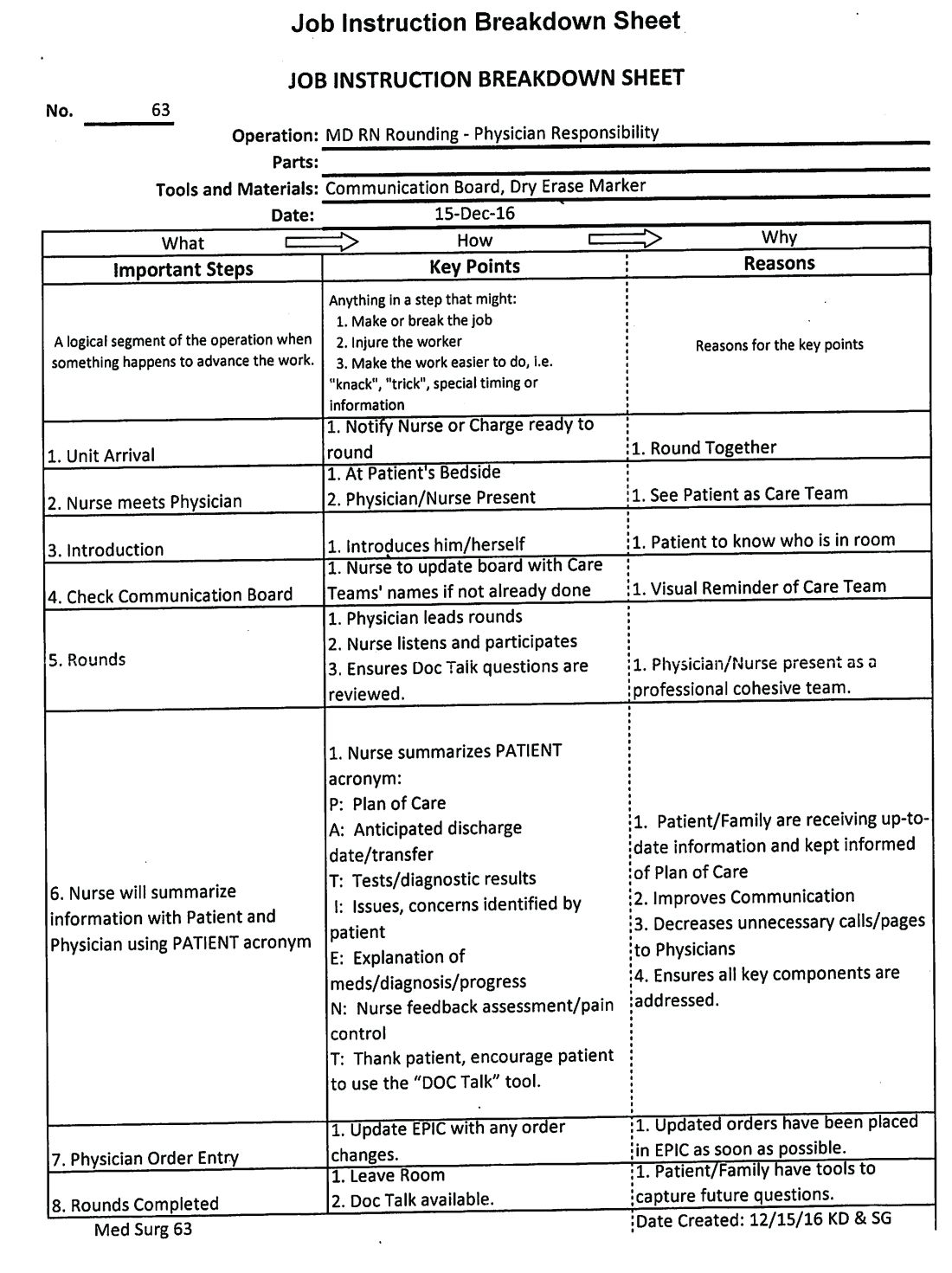
This process was repeated at other hospitals in the system once a standardized work flow was created (See Image 1). This initiative was next presented to the health system board of directors, who agreed that nurse-physician rounding should be the standard of care across our health system. Through partnership and collaboration with the IT department, we developed a tool to track nurse-physician rounding through our EHR system, which gave accountability to both physicians and nurses.
In conclusion, improved communication by timely nurse-physician rounding can lead to better outcomes for patients and also reduce costs and improve patient and staff experience, advancing the Quadruple Aim. Moving forward to build and sustain this work flow, we plan to continue nurse-physician collaboration across the health system consistently and for all areas of acute care operations.
Explaining the “Why,” sharing data on the benefits of the model, and reinforcing documentation of the rounding in our EHR are some steps we have put into action at leadership and staff meetings to sustain the activity. We are soliciting feedback, as well as monitoring and identifying any unaddressed barriers during rounding. Addition of this process measure to our quality improvement bonus opportunity also has helped to sustain performance from our teams.
Dr. Laufer is system medical director of hospital medicine and transitional care at Lee Health in Ft. Myers, Fla. Dr. Prasad is chief medical officer of Lee Physician Group, Ft. Myers, Fla.
References
1. Leape LL et al. Five years after to err is human: What we have learned? JAMA. 2005;293(19):2384-90.
2. Sutcliffe KM et al. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-94.
3. Manojlovich M. Reframing communication with physicians as sensemaking. J Nurs Care Qual. 2013 Oct-Dec;28(4):295-303.
4. Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals. Crit Care Nurse. 2009 Dec;29(6):58-69.
5. Asthon J et al. Qualitative evaluation of regular morning meeting aimed at improving interdisciplinary communication and patient outcomes. Int J Nurs Pract. 2005 Oct;11(5):206-13.
6. Lancaster G et al. Interdisciplinary Communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275-84.
7. McIntosh N et al. Impact of provider coordination on nurse and physician perception of patient care quality. J Nurs Care Qual. 2014 Jul-Sep;29(3):269-79.
8. Jo M et al. An organizational assessment of disruptive clinical behavior. J Nurs Care Qual. 2013 Apr-Jun;28(2):110-21.
9. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, 2010.
10. O’Connor P et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016 Jun;28(3):339-45.
11. Manojlovich M. Nurse/Physician communication through a sense making lens. Med Care. 2010 Nov;48(11):941-6.
12. Monash B et al. Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. J Hosp Med. 2017 Mar;12(3):143-9.
13. O’Leary KJ et al. Effect of patient-centered bedside rounds on hospitalized patients decision control, activation and satisfaction with care. BMJ Qual Saf. 2016 Dec;25(12):921-8.
14. Dutton RP et al. Daily multidisciplinary rounds shorten length of stay for trauma patients. J Trauma. 2003 Nov;55(5):913-9.
15. Manojlovich M et al. Healthy work environments, nurse-physician communication, and patients’ outcomes. Am J Crit Care. 2007 Nov;16(6):536-43.
16. Ramirez J et al. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. 2016 Feb;109(2):112-5.
17. Sollami A et al. Nurse-Physician collaboration: A meta-analytical investigation of survey scores. J Interprof Care. 2015 May;29(3):223-9.
18. House S et al. Nurses and physicians perceptions of nurse-physician collaboration. J Nurs Adm. 2017 Mar;47(3):165-71.
19. Townsend-Gervis M et al. Interdisciplinary rounds and structured communications reduce re-admissions and improve some patients’ outcomes. West J Nurs Res. 2014 Aug;36(7):917-28.
20. The Joint Commission. Sentinel Events. http://www.jointcommission.org/sentinel_event.aspx. Accessed Oct 2017.
21. Bodenheimer T et al. From Triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6.
Quality and safety of hospital care from the patient perspective
Background: Delivery of high-quality, safe care is key to earning the trust and confidence of patients. Patients can be a valuable asset in determining and evaluating the quality and safety of the care they receive. Collectively analyzing patient perceptions remains a challenge.
Study design: Multicenter, wait-list design, cluster-randomized controlled trial.
Setting: Five National Health Service Trusts Hospital sites in the north of England.
Synopsis: Data were collected via validated survey of inpatients; 1,155 patient incident reports were gathered from 579 patients. Patient volunteers were trained to group these reports into 14 categories. Next, clinical researchers and physicians independently reviewed all reports for presence of a patient safety incident (PSI) using a previously determined consensus definition.
One in 10 patients identified a PSI. There was variability in classifying incidents as PSIs in some categories. Of the concerns expressed by patients, 65% were not classified as PSI. Limitations included a focus on patient’s concerns rather than safety, PSI estimates based on patient’s feedback without clinical information, and lack of inter-rater reliability estimates.
Bottom line: Effective translation of patient experience can provide valuable insights about safety and quality of care in hospital.
Citation: O’Hara JK et al. What can patients tell us about the quality and safety of hospital care? Findings from a UK multicentre survey study. BMJ Qual Saf. 2018 Mar 15. doi: 10.1136/bmjqs-2017-006974.
Dr. Chikkanna is an assistant professor in the division of hospital medicine at the University of Kentucky, Lexington.
Background: Delivery of high-quality, safe care is key to earning the trust and confidence of patients. Patients can be a valuable asset in determining and evaluating the quality and safety of the care they receive. Collectively analyzing patient perceptions remains a challenge.
Study design: Multicenter, wait-list design, cluster-randomized controlled trial.
Setting: Five National Health Service Trusts Hospital sites in the north of England.
Synopsis: Data were collected via validated survey of inpatients; 1,155 patient incident reports were gathered from 579 patients. Patient volunteers were trained to group these reports into 14 categories. Next, clinical researchers and physicians independently reviewed all reports for presence of a patient safety incident (PSI) using a previously determined consensus definition.
One in 10 patients identified a PSI. There was variability in classifying incidents as PSIs in some categories. Of the concerns expressed by patients, 65% were not classified as PSI. Limitations included a focus on patient’s concerns rather than safety, PSI estimates based on patient’s feedback without clinical information, and lack of inter-rater reliability estimates.
Bottom line: Effective translation of patient experience can provide valuable insights about safety and quality of care in hospital.
Citation: O’Hara JK et al. What can patients tell us about the quality and safety of hospital care? Findings from a UK multicentre survey study. BMJ Qual Saf. 2018 Mar 15. doi: 10.1136/bmjqs-2017-006974.
Dr. Chikkanna is an assistant professor in the division of hospital medicine at the University of Kentucky, Lexington.
Background: Delivery of high-quality, safe care is key to earning the trust and confidence of patients. Patients can be a valuable asset in determining and evaluating the quality and safety of the care they receive. Collectively analyzing patient perceptions remains a challenge.
Study design: Multicenter, wait-list design, cluster-randomized controlled trial.
Setting: Five National Health Service Trusts Hospital sites in the north of England.
Synopsis: Data were collected via validated survey of inpatients; 1,155 patient incident reports were gathered from 579 patients. Patient volunteers were trained to group these reports into 14 categories. Next, clinical researchers and physicians independently reviewed all reports for presence of a patient safety incident (PSI) using a previously determined consensus definition.
One in 10 patients identified a PSI. There was variability in classifying incidents as PSIs in some categories. Of the concerns expressed by patients, 65% were not classified as PSI. Limitations included a focus on patient’s concerns rather than safety, PSI estimates based on patient’s feedback without clinical information, and lack of inter-rater reliability estimates.
Bottom line: Effective translation of patient experience can provide valuable insights about safety and quality of care in hospital.
Citation: O’Hara JK et al. What can patients tell us about the quality and safety of hospital care? Findings from a UK multicentre survey study. BMJ Qual Saf. 2018 Mar 15. doi: 10.1136/bmjqs-2017-006974.
Dr. Chikkanna is an assistant professor in the division of hospital medicine at the University of Kentucky, Lexington.
Hospitalists target inpatient glycemic control
SHM benchmarks provide ‘objective format’ for improving outcomes
Physicians are trained to manage their patients’ diabetes and often do a meticulous job – one on one. But in order to maximize glycemic control outcomes throughout the hospital, you need a kind of diabetic epidemiology team to focus on the data, said Andjela Drincic, MD, an endocrinologist at Nebraska Medicine, the clinical partner of the University of Nebraska Medical Center in Omaha.
As medical director for diabetes stewardship, Dr. Drincic serves as the epidemiologic lead for her hospital, which has worked systematically to improve inpatient glycemic control since 2012 – with help from the Society of Hospital Medicine.
“You need a team and to set up a system that works, with protocols and some way of knowing if the protocols are succeeding,” Dr. Drincic said. “Quality improvement targets are never static.” She credited SHM’s glycemic control eQUIPS (Electronic Quality Improvement Program), an online quality improvement resource and collaborative of 104 participating hospitals, for providing the support and the data needed to drive glycemic QI efforts at Nebraska Medicine. SHM provided reporting metrics, quarterly benchmarking reports, a library of tools and resources, an implementation guide, educational webinars on demand and, for some participants, mentored implementation with the advice of a leading expert in the field.
One big reason for giving more attention to glycemic control in the hospital is patient safety, said Gregory Maynard, MD, MHM, clinical professor and chief quality officer at the University of California–Davis Medical Center and SHM’s project team leader for eQUIPS.
“Hyperglycemia in hospitalized patients is an extraordinarily common and growing problem, affecting up to 40%-50% of patients in the hospital,” he said. In 2012, 7.7 million hospital stays involved patients with diabetes, the seventh leading cause of death in the United States.1
Hyperglycemia is linked to elevated rates of medical complications, infections, wound complications, hospital mortality, length of stay, readmissions, and ICU admissions, along with other outcomes not directly related to diabetes. Hyperglycemia in hospitalized patients who have not been given a diagnosis of diabetes is, if anything, more dangerous. Add the related risk for hypoglycemia, and clinicians are challenged to keep their patients controlled within the zone between the extremes of hyper- and hypoglycemia. The American Diabetes Association recently issued recommendations with more relaxed glucose targets between 140 and 180 mg/dL for most patients in non–intensive care settings.2
“To not have a standardized way of managing hyperglycemia for your hospital seems like an enormous missed opportunity,” Dr. Maynard said. “If someone comes into the hospital with a chronic condition of diabetes that you ignore, just maintaining them in the hospital and sending them back out into the world without addressing the underlying condition is not good care. You have missed an important opportunity to alter the course of a serious chronic condition.”
Dr. Maynard said SHM recognized this opportunity when it established eQUIPS. “Hospitalists are often tasked with taking care of patients with glycemic issues because there may not be an endocrinologist readily accessible in the hospital,” he said. “We have seen through our benchmarking in eQUIPS incredible variability – with 10-fold differences in hyperglycemia and hypoglycemia rates between the best- and worst-performing sites. The biggest variable is whether the hospital systematically manages glycemic control. We have also shown that achieving high levels of glycemic control and low hypoglycemia rates concurrently is very possible.”
Reliable benchmarks
Nebraska Medicine enrolled in eQUIPS in 2012.
“We utilize SHM’s glucometrics (standardized analyses of inpatient glycemic control data).”3 said Dr. Drincic. “I was looking for a reliable glucometric system and some way to make comparisons with other hospitals when I came across the data Dr. Maynard published about SHM via a PubMed search. We needed outcomes that are validated in the literature and comparison groups.”
Nebraska Medicine has also received a certificate of distinction for inpatient diabetes care from the Joint Commission, and Dr. Drincic is active in PRIDE (Planning Research in Inpatient Diabetes), a national consortium of leading investigators in inpatient diabetes care formed to promote collaborative research. The PRIDE group meets yearly at the ADA conference, communicates regularly by email, and publishes articles.
“Once a year I present our glycemic control data to our administration and to the quality and safety committees at the hospital. I have been pleased with the level of support we have received,” Dr. Drincic said. “We needed a mandate to do this, but when I reported the impact on readmissions and other outcomes, I got the full support of administration. This would have been a lot harder without SHM.”
Engagement with hospitalists is another key to the glucose management project’s success, Dr. Drincic said. “We as endocrinologists think we know how to manage diabetes, but hospitalists have the daunting task of dealing with all of the patient’s medical issues. If we don’t have a strong collaboration, how can we change practice hospitalwide?” Rachel Thompson, MD, SFHM, Nebraska Medicine’s chief of hospital medicine, participates in the glucose management project, Dr. Drincic said.
“We occasionally are guests at hospitalist meetings to share new glucose treatment algorithms,” she said. “We’re also looking at collaborating on other quality initiatives, for example, studying how perioperative dexamethasone affects glycemic control. We built this relationship with hospitalists by establishing trust while trying to shed a reputation as ‘sugar police.’ I don’t want hospitalists saying ‘There she goes again’ whenever I come on the unit. We have tried to establish personal relationships and figure out what the hospitalists need, especially relative to EPIC (the hospital’s electronic medical record software).”
Dr. Thompson said her group’s recent growth to nearly 70 clinicians has increased its footprint hospitalwide and given hospitalists a greater opportunity to influence glycemic control. “We see up to a third of the patients in the hospital outside of the ICU. Glycemic control is something you learn as a hospitalist – It’s a very important frontline quality issue. In the patient list on EPIC every morning we have a field highlighting all patients with glycemic control issues,” she said.
“Poor glucose control is associated with poor outcomes for our patients. We need the right systems in place for patient safety. Moreover, if we are ignoring glycemic control when the patient is in the hospital, we’re sending the wrong message and setting a bad example for our patients when they return home.”
Lack of clear metrics
A significant defect in the infrastructure of many glucose management programs is the lack of clear metrics for outcomes, Dr. Maynard said. Nearly one-third of hospitals in the United States have no standardized metric to track the quality of their inpatient glycemic management, a sobering statistic considering that the first step in any QI initiative is to define and measure the problem at hand.
“I believe the main reason that glycemic control has been left off hospitals’ radar screens is that we still have not adopted national, publicly reported quality measures for glycemic control, although those were proposed recently by a government interagency work group,” Dr. Maynard said. “Until that happens, we’ll continue to see uneven response.”
The first step for frontline hospitalists is to learn and understand the basics of glucose control, for example, basal bolus insulin administration, and to stop writing orders for sliding scale insulin as the sole means of controlling hyperglycemia.
“Develop and adopt standards of practice for insulin administration in your hospital,” Dr. Maynard said. “Be part of the solution, not the problem. Once you get into the weeds – patients on steroids or on total parenteral nutrition – it can get tricky. But it’s important to get the basics right and move beyond inertia on this topic.”
The glycemic team at Nebraska Medicine includes, in addition to Dr. Drincic and Dr. Thompson, an endocrinology fellow, diabetes case managers, resource nurses, nurse leadership, pharmacists, inpatient care transitions coordinators, and representatives from pediatrics and critical care, all working to impact the overall quality of glycemic management in the hospital. Jon Knezevich, PharmD is diabetes stewardship pharmacy coordinator, and Shelly Lautenbaugh, RN, CDE, is diabetes lead care manager and diabetes coordinator for the Joint Commission certificate program. Diabetes stewardship also includes online and live training courses and a class in acute glucose management for the diabetes resource nurses, who bring the knowledge back to their units.
The glucose team’s job is to make sure patients are cared for safely, using appropriate policies and procedures, education, and training, Ms. Lautenbaugh said. “We have a mission as a hospital to transform people’s lives. We try to live our values, and everything follows from the focus on patient safety,” she added. “If our patients can receive extraordinary care and leave better informed about their condition than when they came in, and then we don’t see them again, we’ve achieved our ultimate goal.”
Hyperglycemia is most often not the primary reason why patients are hospitalized, Ms. Lautenbaugh said. “But we need to give them appropriate glucose management regardless. We’ve worked with bedside staff, nurse leadership, and teams to develop plans to raise our outcome scores. We have a lot of different outcomes we examine, and it’s always evolving.”
Quality metrics are incorporated into the electronic medical record, but those reports are not timely enough for day-to-day management, Dr. Knezevich said. “So we created a diabetes dashboard, constantly updated in real time to identify patients who are out of glycemic control.” The measures tracked include a mean patient day glucose score, percentage of readings within recommended limits, mean time between measured low readings and next documented reading or resolution of hypoglycemia, readmission rates, and diabetes nutrition assessments.
For hospitals with diabetes certificates, the Joint Commission also requires that every patient with hyperglycemia receives a clinic visit 30 days after discharge to make sure they are receiving appropriate follow-up care. Other facets of the Nebraska glycemic initiative include utilizing the hospital’s voluntary “Meds to Beds” program, which brings prescribed medications to the patient’s room at discharge. “We offer a diabetes discharge kit for patients who are self-pay, with all of the insulin and medical supplies they will need to get to the 30-day follow-up visit,” Dr. Knezevich said. “We can dream up amazing treatment regimens, but if they can’t afford the medications, what have we accomplished?”
SHM’s external benchmarks have provided an objective format for comparing and improving outcomes, Ms. Lautenbaugh said. “We like to see where we are and use the data to make significant improvements, but we’re also focused on internal assessments. If we make changes for a given metric, how does it affect performance in other areas?” One important metric is percentage of glucose readings within target range hospitalwide. “Our overall goal is 75%. It was 72% in April 2018, and we’ve raised it to 74.4%. It’s a small gain but it shows steady progress. Little steps make small but steady improvement,” she said.
“One area where we were not pleased was the occurrence of hypoglycemia,” Ms. Lautenbaugh said. “We did a root cause analysis of every hypoglycemic event, including several reports for patients who didn’t have diabetes at all. We had to weed out some that weren’t pertinent to our quality questions, but for those that are, the diabetes case manager calls the provider to make sure they were aware of the incident. We were able to identify the outliers in noncritical care, which we’re now able to tackle using a systematic approach.”
Get on the bus
Hospitalists are also integrally involved in a hospital glycemic improvement initiative at Orange Regional Medical Center (ORMC) in Middletown, N.Y.
The Glycemic Improvement Team (GIT) was formed in 2012 when a new hospital campus opened and EPIC was implemented as the hospital’s EMR. But glycemic control has taken on greater focus since 2015, when ORMC enrolled in eQUIPS, said Lorraine Porcaro, RN, the hospital’s diabetes clinical manager. The glycemic control team includes representatives from medicine, nursing, case management, laboratory, nutrition, pharmacy, wound care, and quality improvement.
Implementing the new EMR offered the opportunity to track a number of medical values in real time, Ms. Porcaro said. ORMC has focused its glycemic quality improvement efforts on hypoglycemia and hyperglycemia, with a recent emphasis on the need for improvements related to glucose reassessment 15 minutes post hypoglycemia treatment. More than a hundred “Diabetes Champions” have completed 16 hours of advanced training in diabetes and provide in-unit mentorship for other staff.
The ORMC team’s glycemic improvement “bus” is a rolling cart that goes from unit to unit supplying nurse education, reminders, copies of department-specific policies and protocols, and treats for staff. “It’s what we’re known for,” Ms. Porcaro said. Pens with the motto: “Don’t Miss the Bus! Retest in 15!” summarize the GIT’s current focus on post–hypoglycemia treatment retesting.
Hospitalists were part of the glycemic improvement process at ORMC from the beginning and are still involved, said Adrian Paraschiv, MD, FHM, a hospitalist and assistant director of the medical center, as well as the ORMC director of clinical information technology. ORMC initiated hospitalist coverage in 1998 and now has three HM groups, two of them represented on the glycemic improvement team.
“Like any hospital, we feel we should minimize hypoglycemic events,” Dr. Paraschiv explained. “This became important for other hospital departments, and we recognized we needed a major QI initiative to improve our outcomes hospitalwide. In the process, we noticed what other people were saying: Results from improving glycemic control included reduced length of stay, cost, and infections. That provided motivation for the hospital to support our initiative.”
Glucose management isn’t only about blood sugar, but whether the patient ate or not, their other blood work, the level of education for patient and staff, and a variety of other inputs, Dr. Paraschiv said. “All of these things were in the EMR but all over the place. EPIC had an incipient structure for pulling the data together, and we modified it to show everything that’s going on with the patient’s glycemic control on a single screen. We can build order sets and issue different reports.”
Today at ORMC, hypoglycemia is reassessed within 30 minutes more than 50% of the time. “It will never be at 100%, but we wanted to at least be at the national mean for eQUIPS hospitals. Our stretch goal was to be in the top quartile, and by the end of 2017, we realized that goal,” Ms. Porcaro said. Sometimes, because of changes in patients and staff, the GIT needs to repeat the education and review policies. “Since then, it’s been a matter of continuing staff education; sharing glucose data with stakeholders; talking about goals for ICU and non-ICU units; and, when needed, rolling out the bus.”
Participation in eQUIPS has made it possible to gather this information in one place and present it in a way that makes sense to physicians, Dr. Paraschiv said. “Dr. Maynard and SHM showed us how to put the data together to add value. Using these tools, we started looking at our processes, what needed to change, and what we are able to change. Now we’re examining what happens afterward. Can we use the electronic system to automatically alert physicians to make changes to the treatment regimen in real time? We continue to improve using upgrades to our EMR, such as an alert system with best practice advisories for the clinician. We now think we can actually achieve what we set out to achieve,” he said.
“Our idea was that we needed to market this program throughout the hospital – starting from the kitchen, meal delivery staff, IT, laboratory, medical and nursing staff,” Ms. Porcaro said. “The issue is multifactorial – it’s for the entire hospital. My heart is warmed when I see the woman who delivers the meals asking the patient: ‘Have you gotten your insulin shot?’ ”
References
1. Corvino L et al. “Management of diabetes and hyperglycemia in hospitalized patients.” Updated 2017 Oct 1 in De Groot LJ et al. editors. Endotext. South Dartmouth (MA): MDText.com 2000.
2. American Diabetes Association. Glycemic targets. Diabetes Care 2017 Jan;40(Suppl 1):S48-56.
3. Maynard G et al. “Design and implementation of a web-based reporting and benchmarking center for inpatient glucometrics.” J Diabetes Sci Technol. 2014 May 12;8(4):630-40.
SHM benchmarks provide ‘objective format’ for improving outcomes
SHM benchmarks provide ‘objective format’ for improving outcomes
Physicians are trained to manage their patients’ diabetes and often do a meticulous job – one on one. But in order to maximize glycemic control outcomes throughout the hospital, you need a kind of diabetic epidemiology team to focus on the data, said Andjela Drincic, MD, an endocrinologist at Nebraska Medicine, the clinical partner of the University of Nebraska Medical Center in Omaha.
As medical director for diabetes stewardship, Dr. Drincic serves as the epidemiologic lead for her hospital, which has worked systematically to improve inpatient glycemic control since 2012 – with help from the Society of Hospital Medicine.
“You need a team and to set up a system that works, with protocols and some way of knowing if the protocols are succeeding,” Dr. Drincic said. “Quality improvement targets are never static.” She credited SHM’s glycemic control eQUIPS (Electronic Quality Improvement Program), an online quality improvement resource and collaborative of 104 participating hospitals, for providing the support and the data needed to drive glycemic QI efforts at Nebraska Medicine. SHM provided reporting metrics, quarterly benchmarking reports, a library of tools and resources, an implementation guide, educational webinars on demand and, for some participants, mentored implementation with the advice of a leading expert in the field.
One big reason for giving more attention to glycemic control in the hospital is patient safety, said Gregory Maynard, MD, MHM, clinical professor and chief quality officer at the University of California–Davis Medical Center and SHM’s project team leader for eQUIPS.
“Hyperglycemia in hospitalized patients is an extraordinarily common and growing problem, affecting up to 40%-50% of patients in the hospital,” he said. In 2012, 7.7 million hospital stays involved patients with diabetes, the seventh leading cause of death in the United States.1
Hyperglycemia is linked to elevated rates of medical complications, infections, wound complications, hospital mortality, length of stay, readmissions, and ICU admissions, along with other outcomes not directly related to diabetes. Hyperglycemia in hospitalized patients who have not been given a diagnosis of diabetes is, if anything, more dangerous. Add the related risk for hypoglycemia, and clinicians are challenged to keep their patients controlled within the zone between the extremes of hyper- and hypoglycemia. The American Diabetes Association recently issued recommendations with more relaxed glucose targets between 140 and 180 mg/dL for most patients in non–intensive care settings.2
“To not have a standardized way of managing hyperglycemia for your hospital seems like an enormous missed opportunity,” Dr. Maynard said. “If someone comes into the hospital with a chronic condition of diabetes that you ignore, just maintaining them in the hospital and sending them back out into the world without addressing the underlying condition is not good care. You have missed an important opportunity to alter the course of a serious chronic condition.”
Dr. Maynard said SHM recognized this opportunity when it established eQUIPS. “Hospitalists are often tasked with taking care of patients with glycemic issues because there may not be an endocrinologist readily accessible in the hospital,” he said. “We have seen through our benchmarking in eQUIPS incredible variability – with 10-fold differences in hyperglycemia and hypoglycemia rates between the best- and worst-performing sites. The biggest variable is whether the hospital systematically manages glycemic control. We have also shown that achieving high levels of glycemic control and low hypoglycemia rates concurrently is very possible.”
Reliable benchmarks
Nebraska Medicine enrolled in eQUIPS in 2012.
“We utilize SHM’s glucometrics (standardized analyses of inpatient glycemic control data).”3 said Dr. Drincic. “I was looking for a reliable glucometric system and some way to make comparisons with other hospitals when I came across the data Dr. Maynard published about SHM via a PubMed search. We needed outcomes that are validated in the literature and comparison groups.”
Nebraska Medicine has also received a certificate of distinction for inpatient diabetes care from the Joint Commission, and Dr. Drincic is active in PRIDE (Planning Research in Inpatient Diabetes), a national consortium of leading investigators in inpatient diabetes care formed to promote collaborative research. The PRIDE group meets yearly at the ADA conference, communicates regularly by email, and publishes articles.
“Once a year I present our glycemic control data to our administration and to the quality and safety committees at the hospital. I have been pleased with the level of support we have received,” Dr. Drincic said. “We needed a mandate to do this, but when I reported the impact on readmissions and other outcomes, I got the full support of administration. This would have been a lot harder without SHM.”
Engagement with hospitalists is another key to the glucose management project’s success, Dr. Drincic said. “We as endocrinologists think we know how to manage diabetes, but hospitalists have the daunting task of dealing with all of the patient’s medical issues. If we don’t have a strong collaboration, how can we change practice hospitalwide?” Rachel Thompson, MD, SFHM, Nebraska Medicine’s chief of hospital medicine, participates in the glucose management project, Dr. Drincic said.
“We occasionally are guests at hospitalist meetings to share new glucose treatment algorithms,” she said. “We’re also looking at collaborating on other quality initiatives, for example, studying how perioperative dexamethasone affects glycemic control. We built this relationship with hospitalists by establishing trust while trying to shed a reputation as ‘sugar police.’ I don’t want hospitalists saying ‘There she goes again’ whenever I come on the unit. We have tried to establish personal relationships and figure out what the hospitalists need, especially relative to EPIC (the hospital’s electronic medical record software).”
Dr. Thompson said her group’s recent growth to nearly 70 clinicians has increased its footprint hospitalwide and given hospitalists a greater opportunity to influence glycemic control. “We see up to a third of the patients in the hospital outside of the ICU. Glycemic control is something you learn as a hospitalist – It’s a very important frontline quality issue. In the patient list on EPIC every morning we have a field highlighting all patients with glycemic control issues,” she said.
“Poor glucose control is associated with poor outcomes for our patients. We need the right systems in place for patient safety. Moreover, if we are ignoring glycemic control when the patient is in the hospital, we’re sending the wrong message and setting a bad example for our patients when they return home.”
Lack of clear metrics
A significant defect in the infrastructure of many glucose management programs is the lack of clear metrics for outcomes, Dr. Maynard said. Nearly one-third of hospitals in the United States have no standardized metric to track the quality of their inpatient glycemic management, a sobering statistic considering that the first step in any QI initiative is to define and measure the problem at hand.
“I believe the main reason that glycemic control has been left off hospitals’ radar screens is that we still have not adopted national, publicly reported quality measures for glycemic control, although those were proposed recently by a government interagency work group,” Dr. Maynard said. “Until that happens, we’ll continue to see uneven response.”
The first step for frontline hospitalists is to learn and understand the basics of glucose control, for example, basal bolus insulin administration, and to stop writing orders for sliding scale insulin as the sole means of controlling hyperglycemia.
“Develop and adopt standards of practice for insulin administration in your hospital,” Dr. Maynard said. “Be part of the solution, not the problem. Once you get into the weeds – patients on steroids or on total parenteral nutrition – it can get tricky. But it’s important to get the basics right and move beyond inertia on this topic.”
The glycemic team at Nebraska Medicine includes, in addition to Dr. Drincic and Dr. Thompson, an endocrinology fellow, diabetes case managers, resource nurses, nurse leadership, pharmacists, inpatient care transitions coordinators, and representatives from pediatrics and critical care, all working to impact the overall quality of glycemic management in the hospital. Jon Knezevich, PharmD is diabetes stewardship pharmacy coordinator, and Shelly Lautenbaugh, RN, CDE, is diabetes lead care manager and diabetes coordinator for the Joint Commission certificate program. Diabetes stewardship also includes online and live training courses and a class in acute glucose management for the diabetes resource nurses, who bring the knowledge back to their units.
The glucose team’s job is to make sure patients are cared for safely, using appropriate policies and procedures, education, and training, Ms. Lautenbaugh said. “We have a mission as a hospital to transform people’s lives. We try to live our values, and everything follows from the focus on patient safety,” she added. “If our patients can receive extraordinary care and leave better informed about their condition than when they came in, and then we don’t see them again, we’ve achieved our ultimate goal.”
Hyperglycemia is most often not the primary reason why patients are hospitalized, Ms. Lautenbaugh said. “But we need to give them appropriate glucose management regardless. We’ve worked with bedside staff, nurse leadership, and teams to develop plans to raise our outcome scores. We have a lot of different outcomes we examine, and it’s always evolving.”
Quality metrics are incorporated into the electronic medical record, but those reports are not timely enough for day-to-day management, Dr. Knezevich said. “So we created a diabetes dashboard, constantly updated in real time to identify patients who are out of glycemic control.” The measures tracked include a mean patient day glucose score, percentage of readings within recommended limits, mean time between measured low readings and next documented reading or resolution of hypoglycemia, readmission rates, and diabetes nutrition assessments.
For hospitals with diabetes certificates, the Joint Commission also requires that every patient with hyperglycemia receives a clinic visit 30 days after discharge to make sure they are receiving appropriate follow-up care. Other facets of the Nebraska glycemic initiative include utilizing the hospital’s voluntary “Meds to Beds” program, which brings prescribed medications to the patient’s room at discharge. “We offer a diabetes discharge kit for patients who are self-pay, with all of the insulin and medical supplies they will need to get to the 30-day follow-up visit,” Dr. Knezevich said. “We can dream up amazing treatment regimens, but if they can’t afford the medications, what have we accomplished?”
SHM’s external benchmarks have provided an objective format for comparing and improving outcomes, Ms. Lautenbaugh said. “We like to see where we are and use the data to make significant improvements, but we’re also focused on internal assessments. If we make changes for a given metric, how does it affect performance in other areas?” One important metric is percentage of glucose readings within target range hospitalwide. “Our overall goal is 75%. It was 72% in April 2018, and we’ve raised it to 74.4%. It’s a small gain but it shows steady progress. Little steps make small but steady improvement,” she said.
“One area where we were not pleased was the occurrence of hypoglycemia,” Ms. Lautenbaugh said. “We did a root cause analysis of every hypoglycemic event, including several reports for patients who didn’t have diabetes at all. We had to weed out some that weren’t pertinent to our quality questions, but for those that are, the diabetes case manager calls the provider to make sure they were aware of the incident. We were able to identify the outliers in noncritical care, which we’re now able to tackle using a systematic approach.”
Get on the bus
Hospitalists are also integrally involved in a hospital glycemic improvement initiative at Orange Regional Medical Center (ORMC) in Middletown, N.Y.
The Glycemic Improvement Team (GIT) was formed in 2012 when a new hospital campus opened and EPIC was implemented as the hospital’s EMR. But glycemic control has taken on greater focus since 2015, when ORMC enrolled in eQUIPS, said Lorraine Porcaro, RN, the hospital’s diabetes clinical manager. The glycemic control team includes representatives from medicine, nursing, case management, laboratory, nutrition, pharmacy, wound care, and quality improvement.
Implementing the new EMR offered the opportunity to track a number of medical values in real time, Ms. Porcaro said. ORMC has focused its glycemic quality improvement efforts on hypoglycemia and hyperglycemia, with a recent emphasis on the need for improvements related to glucose reassessment 15 minutes post hypoglycemia treatment. More than a hundred “Diabetes Champions” have completed 16 hours of advanced training in diabetes and provide in-unit mentorship for other staff.
The ORMC team’s glycemic improvement “bus” is a rolling cart that goes from unit to unit supplying nurse education, reminders, copies of department-specific policies and protocols, and treats for staff. “It’s what we’re known for,” Ms. Porcaro said. Pens with the motto: “Don’t Miss the Bus! Retest in 15!” summarize the GIT’s current focus on post–hypoglycemia treatment retesting.
Hospitalists were part of the glycemic improvement process at ORMC from the beginning and are still involved, said Adrian Paraschiv, MD, FHM, a hospitalist and assistant director of the medical center, as well as the ORMC director of clinical information technology. ORMC initiated hospitalist coverage in 1998 and now has three HM groups, two of them represented on the glycemic improvement team.
“Like any hospital, we feel we should minimize hypoglycemic events,” Dr. Paraschiv explained. “This became important for other hospital departments, and we recognized we needed a major QI initiative to improve our outcomes hospitalwide. In the process, we noticed what other people were saying: Results from improving glycemic control included reduced length of stay, cost, and infections. That provided motivation for the hospital to support our initiative.”
Glucose management isn’t only about blood sugar, but whether the patient ate or not, their other blood work, the level of education for patient and staff, and a variety of other inputs, Dr. Paraschiv said. “All of these things were in the EMR but all over the place. EPIC had an incipient structure for pulling the data together, and we modified it to show everything that’s going on with the patient’s glycemic control on a single screen. We can build order sets and issue different reports.”
Today at ORMC, hypoglycemia is reassessed within 30 minutes more than 50% of the time. “It will never be at 100%, but we wanted to at least be at the national mean for eQUIPS hospitals. Our stretch goal was to be in the top quartile, and by the end of 2017, we realized that goal,” Ms. Porcaro said. Sometimes, because of changes in patients and staff, the GIT needs to repeat the education and review policies. “Since then, it’s been a matter of continuing staff education; sharing glucose data with stakeholders; talking about goals for ICU and non-ICU units; and, when needed, rolling out the bus.”
Participation in eQUIPS has made it possible to gather this information in one place and present it in a way that makes sense to physicians, Dr. Paraschiv said. “Dr. Maynard and SHM showed us how to put the data together to add value. Using these tools, we started looking at our processes, what needed to change, and what we are able to change. Now we’re examining what happens afterward. Can we use the electronic system to automatically alert physicians to make changes to the treatment regimen in real time? We continue to improve using upgrades to our EMR, such as an alert system with best practice advisories for the clinician. We now think we can actually achieve what we set out to achieve,” he said.
“Our idea was that we needed to market this program throughout the hospital – starting from the kitchen, meal delivery staff, IT, laboratory, medical and nursing staff,” Ms. Porcaro said. “The issue is multifactorial – it’s for the entire hospital. My heart is warmed when I see the woman who delivers the meals asking the patient: ‘Have you gotten your insulin shot?’ ”
References
1. Corvino L et al. “Management of diabetes and hyperglycemia in hospitalized patients.” Updated 2017 Oct 1 in De Groot LJ et al. editors. Endotext. South Dartmouth (MA): MDText.com 2000.
2. American Diabetes Association. Glycemic targets. Diabetes Care 2017 Jan;40(Suppl 1):S48-56.
3. Maynard G et al. “Design and implementation of a web-based reporting and benchmarking center for inpatient glucometrics.” J Diabetes Sci Technol. 2014 May 12;8(4):630-40.
Physicians are trained to manage their patients’ diabetes and often do a meticulous job – one on one. But in order to maximize glycemic control outcomes throughout the hospital, you need a kind of diabetic epidemiology team to focus on the data, said Andjela Drincic, MD, an endocrinologist at Nebraska Medicine, the clinical partner of the University of Nebraska Medical Center in Omaha.
As medical director for diabetes stewardship, Dr. Drincic serves as the epidemiologic lead for her hospital, which has worked systematically to improve inpatient glycemic control since 2012 – with help from the Society of Hospital Medicine.
“You need a team and to set up a system that works, with protocols and some way of knowing if the protocols are succeeding,” Dr. Drincic said. “Quality improvement targets are never static.” She credited SHM’s glycemic control eQUIPS (Electronic Quality Improvement Program), an online quality improvement resource and collaborative of 104 participating hospitals, for providing the support and the data needed to drive glycemic QI efforts at Nebraska Medicine. SHM provided reporting metrics, quarterly benchmarking reports, a library of tools and resources, an implementation guide, educational webinars on demand and, for some participants, mentored implementation with the advice of a leading expert in the field.
One big reason for giving more attention to glycemic control in the hospital is patient safety, said Gregory Maynard, MD, MHM, clinical professor and chief quality officer at the University of California–Davis Medical Center and SHM’s project team leader for eQUIPS.
“Hyperglycemia in hospitalized patients is an extraordinarily common and growing problem, affecting up to 40%-50% of patients in the hospital,” he said. In 2012, 7.7 million hospital stays involved patients with diabetes, the seventh leading cause of death in the United States.1
Hyperglycemia is linked to elevated rates of medical complications, infections, wound complications, hospital mortality, length of stay, readmissions, and ICU admissions, along with other outcomes not directly related to diabetes. Hyperglycemia in hospitalized patients who have not been given a diagnosis of diabetes is, if anything, more dangerous. Add the related risk for hypoglycemia, and clinicians are challenged to keep their patients controlled within the zone between the extremes of hyper- and hypoglycemia. The American Diabetes Association recently issued recommendations with more relaxed glucose targets between 140 and 180 mg/dL for most patients in non–intensive care settings.2
“To not have a standardized way of managing hyperglycemia for your hospital seems like an enormous missed opportunity,” Dr. Maynard said. “If someone comes into the hospital with a chronic condition of diabetes that you ignore, just maintaining them in the hospital and sending them back out into the world without addressing the underlying condition is not good care. You have missed an important opportunity to alter the course of a serious chronic condition.”
Dr. Maynard said SHM recognized this opportunity when it established eQUIPS. “Hospitalists are often tasked with taking care of patients with glycemic issues because there may not be an endocrinologist readily accessible in the hospital,” he said. “We have seen through our benchmarking in eQUIPS incredible variability – with 10-fold differences in hyperglycemia and hypoglycemia rates between the best- and worst-performing sites. The biggest variable is whether the hospital systematically manages glycemic control. We have also shown that achieving high levels of glycemic control and low hypoglycemia rates concurrently is very possible.”
Reliable benchmarks
Nebraska Medicine enrolled in eQUIPS in 2012.
“We utilize SHM’s glucometrics (standardized analyses of inpatient glycemic control data).”3 said Dr. Drincic. “I was looking for a reliable glucometric system and some way to make comparisons with other hospitals when I came across the data Dr. Maynard published about SHM via a PubMed search. We needed outcomes that are validated in the literature and comparison groups.”
Nebraska Medicine has also received a certificate of distinction for inpatient diabetes care from the Joint Commission, and Dr. Drincic is active in PRIDE (Planning Research in Inpatient Diabetes), a national consortium of leading investigators in inpatient diabetes care formed to promote collaborative research. The PRIDE group meets yearly at the ADA conference, communicates regularly by email, and publishes articles.
“Once a year I present our glycemic control data to our administration and to the quality and safety committees at the hospital. I have been pleased with the level of support we have received,” Dr. Drincic said. “We needed a mandate to do this, but when I reported the impact on readmissions and other outcomes, I got the full support of administration. This would have been a lot harder without SHM.”
Engagement with hospitalists is another key to the glucose management project’s success, Dr. Drincic said. “We as endocrinologists think we know how to manage diabetes, but hospitalists have the daunting task of dealing with all of the patient’s medical issues. If we don’t have a strong collaboration, how can we change practice hospitalwide?” Rachel Thompson, MD, SFHM, Nebraska Medicine’s chief of hospital medicine, participates in the glucose management project, Dr. Drincic said.
“We occasionally are guests at hospitalist meetings to share new glucose treatment algorithms,” she said. “We’re also looking at collaborating on other quality initiatives, for example, studying how perioperative dexamethasone affects glycemic control. We built this relationship with hospitalists by establishing trust while trying to shed a reputation as ‘sugar police.’ I don’t want hospitalists saying ‘There she goes again’ whenever I come on the unit. We have tried to establish personal relationships and figure out what the hospitalists need, especially relative to EPIC (the hospital’s electronic medical record software).”
Dr. Thompson said her group’s recent growth to nearly 70 clinicians has increased its footprint hospitalwide and given hospitalists a greater opportunity to influence glycemic control. “We see up to a third of the patients in the hospital outside of the ICU. Glycemic control is something you learn as a hospitalist – It’s a very important frontline quality issue. In the patient list on EPIC every morning we have a field highlighting all patients with glycemic control issues,” she said.
“Poor glucose control is associated with poor outcomes for our patients. We need the right systems in place for patient safety. Moreover, if we are ignoring glycemic control when the patient is in the hospital, we’re sending the wrong message and setting a bad example for our patients when they return home.”
Lack of clear metrics
A significant defect in the infrastructure of many glucose management programs is the lack of clear metrics for outcomes, Dr. Maynard said. Nearly one-third of hospitals in the United States have no standardized metric to track the quality of their inpatient glycemic management, a sobering statistic considering that the first step in any QI initiative is to define and measure the problem at hand.
“I believe the main reason that glycemic control has been left off hospitals’ radar screens is that we still have not adopted national, publicly reported quality measures for glycemic control, although those were proposed recently by a government interagency work group,” Dr. Maynard said. “Until that happens, we’ll continue to see uneven response.”
The first step for frontline hospitalists is to learn and understand the basics of glucose control, for example, basal bolus insulin administration, and to stop writing orders for sliding scale insulin as the sole means of controlling hyperglycemia.
“Develop and adopt standards of practice for insulin administration in your hospital,” Dr. Maynard said. “Be part of the solution, not the problem. Once you get into the weeds – patients on steroids or on total parenteral nutrition – it can get tricky. But it’s important to get the basics right and move beyond inertia on this topic.”
The glycemic team at Nebraska Medicine includes, in addition to Dr. Drincic and Dr. Thompson, an endocrinology fellow, diabetes case managers, resource nurses, nurse leadership, pharmacists, inpatient care transitions coordinators, and representatives from pediatrics and critical care, all working to impact the overall quality of glycemic management in the hospital. Jon Knezevich, PharmD is diabetes stewardship pharmacy coordinator, and Shelly Lautenbaugh, RN, CDE, is diabetes lead care manager and diabetes coordinator for the Joint Commission certificate program. Diabetes stewardship also includes online and live training courses and a class in acute glucose management for the diabetes resource nurses, who bring the knowledge back to their units.
The glucose team’s job is to make sure patients are cared for safely, using appropriate policies and procedures, education, and training, Ms. Lautenbaugh said. “We have a mission as a hospital to transform people’s lives. We try to live our values, and everything follows from the focus on patient safety,” she added. “If our patients can receive extraordinary care and leave better informed about their condition than when they came in, and then we don’t see them again, we’ve achieved our ultimate goal.”
Hyperglycemia is most often not the primary reason why patients are hospitalized, Ms. Lautenbaugh said. “But we need to give them appropriate glucose management regardless. We’ve worked with bedside staff, nurse leadership, and teams to develop plans to raise our outcome scores. We have a lot of different outcomes we examine, and it’s always evolving.”
Quality metrics are incorporated into the electronic medical record, but those reports are not timely enough for day-to-day management, Dr. Knezevich said. “So we created a diabetes dashboard, constantly updated in real time to identify patients who are out of glycemic control.” The measures tracked include a mean patient day glucose score, percentage of readings within recommended limits, mean time between measured low readings and next documented reading or resolution of hypoglycemia, readmission rates, and diabetes nutrition assessments.
For hospitals with diabetes certificates, the Joint Commission also requires that every patient with hyperglycemia receives a clinic visit 30 days after discharge to make sure they are receiving appropriate follow-up care. Other facets of the Nebraska glycemic initiative include utilizing the hospital’s voluntary “Meds to Beds” program, which brings prescribed medications to the patient’s room at discharge. “We offer a diabetes discharge kit for patients who are self-pay, with all of the insulin and medical supplies they will need to get to the 30-day follow-up visit,” Dr. Knezevich said. “We can dream up amazing treatment regimens, but if they can’t afford the medications, what have we accomplished?”
SHM’s external benchmarks have provided an objective format for comparing and improving outcomes, Ms. Lautenbaugh said. “We like to see where we are and use the data to make significant improvements, but we’re also focused on internal assessments. If we make changes for a given metric, how does it affect performance in other areas?” One important metric is percentage of glucose readings within target range hospitalwide. “Our overall goal is 75%. It was 72% in April 2018, and we’ve raised it to 74.4%. It’s a small gain but it shows steady progress. Little steps make small but steady improvement,” she said.
“One area where we were not pleased was the occurrence of hypoglycemia,” Ms. Lautenbaugh said. “We did a root cause analysis of every hypoglycemic event, including several reports for patients who didn’t have diabetes at all. We had to weed out some that weren’t pertinent to our quality questions, but for those that are, the diabetes case manager calls the provider to make sure they were aware of the incident. We were able to identify the outliers in noncritical care, which we’re now able to tackle using a systematic approach.”
Get on the bus
Hospitalists are also integrally involved in a hospital glycemic improvement initiative at Orange Regional Medical Center (ORMC) in Middletown, N.Y.
The Glycemic Improvement Team (GIT) was formed in 2012 when a new hospital campus opened and EPIC was implemented as the hospital’s EMR. But glycemic control has taken on greater focus since 2015, when ORMC enrolled in eQUIPS, said Lorraine Porcaro, RN, the hospital’s diabetes clinical manager. The glycemic control team includes representatives from medicine, nursing, case management, laboratory, nutrition, pharmacy, wound care, and quality improvement.
Implementing the new EMR offered the opportunity to track a number of medical values in real time, Ms. Porcaro said. ORMC has focused its glycemic quality improvement efforts on hypoglycemia and hyperglycemia, with a recent emphasis on the need for improvements related to glucose reassessment 15 minutes post hypoglycemia treatment. More than a hundred “Diabetes Champions” have completed 16 hours of advanced training in diabetes and provide in-unit mentorship for other staff.
The ORMC team’s glycemic improvement “bus” is a rolling cart that goes from unit to unit supplying nurse education, reminders, copies of department-specific policies and protocols, and treats for staff. “It’s what we’re known for,” Ms. Porcaro said. Pens with the motto: “Don’t Miss the Bus! Retest in 15!” summarize the GIT’s current focus on post–hypoglycemia treatment retesting.
Hospitalists were part of the glycemic improvement process at ORMC from the beginning and are still involved, said Adrian Paraschiv, MD, FHM, a hospitalist and assistant director of the medical center, as well as the ORMC director of clinical information technology. ORMC initiated hospitalist coverage in 1998 and now has three HM groups, two of them represented on the glycemic improvement team.
“Like any hospital, we feel we should minimize hypoglycemic events,” Dr. Paraschiv explained. “This became important for other hospital departments, and we recognized we needed a major QI initiative to improve our outcomes hospitalwide. In the process, we noticed what other people were saying: Results from improving glycemic control included reduced length of stay, cost, and infections. That provided motivation for the hospital to support our initiative.”
Glucose management isn’t only about blood sugar, but whether the patient ate or not, their other blood work, the level of education for patient and staff, and a variety of other inputs, Dr. Paraschiv said. “All of these things were in the EMR but all over the place. EPIC had an incipient structure for pulling the data together, and we modified it to show everything that’s going on with the patient’s glycemic control on a single screen. We can build order sets and issue different reports.”
Today at ORMC, hypoglycemia is reassessed within 30 minutes more than 50% of the time. “It will never be at 100%, but we wanted to at least be at the national mean for eQUIPS hospitals. Our stretch goal was to be in the top quartile, and by the end of 2017, we realized that goal,” Ms. Porcaro said. Sometimes, because of changes in patients and staff, the GIT needs to repeat the education and review policies. “Since then, it’s been a matter of continuing staff education; sharing glucose data with stakeholders; talking about goals for ICU and non-ICU units; and, when needed, rolling out the bus.”
Participation in eQUIPS has made it possible to gather this information in one place and present it in a way that makes sense to physicians, Dr. Paraschiv said. “Dr. Maynard and SHM showed us how to put the data together to add value. Using these tools, we started looking at our processes, what needed to change, and what we are able to change. Now we’re examining what happens afterward. Can we use the electronic system to automatically alert physicians to make changes to the treatment regimen in real time? We continue to improve using upgrades to our EMR, such as an alert system with best practice advisories for the clinician. We now think we can actually achieve what we set out to achieve,” he said.
“Our idea was that we needed to market this program throughout the hospital – starting from the kitchen, meal delivery staff, IT, laboratory, medical and nursing staff,” Ms. Porcaro said. “The issue is multifactorial – it’s for the entire hospital. My heart is warmed when I see the woman who delivers the meals asking the patient: ‘Have you gotten your insulin shot?’ ”
References
1. Corvino L et al. “Management of diabetes and hyperglycemia in hospitalized patients.” Updated 2017 Oct 1 in De Groot LJ et al. editors. Endotext. South Dartmouth (MA): MDText.com 2000.
2. American Diabetes Association. Glycemic targets. Diabetes Care 2017 Jan;40(Suppl 1):S48-56.
3. Maynard G et al. “Design and implementation of a web-based reporting and benchmarking center for inpatient glucometrics.” J Diabetes Sci Technol. 2014 May 12;8(4):630-40.
SHM aids national infection prevention and control effort
Multidisciplinary teams celebrate achievements in getting to zero
The Society of Hospital Medicine is pleased to share successes and resources from a 3-year national quality improvement program called STRIVE (States Targeting Reduction in Infections Via Engagement). This program targeted opportunities to streamline and enhance infection prevention and control efforts in participating hospitals.
SHM was a key partner in the STRIVE program, which was managed by the Health Research & Educational Trust, the not-for-profit research and education affiliate of the American Hospital Association. Other partners included the American Society for Healthcare Engineering, Association for Professionals in Infection Control and Epidemiology, University of Michigan, Ann Arbor, and experts from academic institutions and professional societies such as Cornell University, Ithaca, N.Y.; Rush University, Chicago; and the Association for the Healthcare Environment. SHM provided specific knowledge and experience on HAI prevention and helped develop the STRIVE curriculum and resources. Faculty coaches from SHM also supported STRIVE hospitals by presenting on webinars, attending in-person meetings, and consulting on calls.
Following the U.S. experience with Ebola, the Centers for Disease Control and Infection identified the critical importance of enhancing infection control for all infectious threats to protect both patients and health care personnel. The CDC also recognized that many state and regional organizations and agencies work with the same health care facilities in order to coordinate efforts to address infectious threats. The STRIVE program provided tools and resources to help communities strengthen the relationships among diverse organizations to maximize improvement and coordination.
Closely aligned with SHM’s mission to promote exceptional care for hospitalized patients, the CDC’s STRIVE program goals were as follows:
- To expand the CDC’s Targeting Assessment for Prevention (TAP) strategy of using surveillance data to identify hospitals with a disproportionately high burden of health care–associated infections (HAIs),
- To build and strengthen relationships between state and regional organizations that help hospitals with infection control and prevention, and
- To provide technical assistance to hospitals to improve implementation of infection control practices in existing and newly constructed health care facilities.
The participants in this program included 449 hospitals from 28 states and the District of Columbia. Short-stay and long-term acute care hospitals that had a high burden of Clostridium difficile infection, and a high burden of one or more of the following HAIs – central line–associated bloodstream infection, catheter associated urinary tract infection, and health care–associated methicillin-resistant Staphylococcus aureus (MRSA) bacteremia – were targeted. Each participant had access to specific education modules, webinars, and learning networks designed to enhance collaboration, performance improvement, and understanding of the successes and barriers to coordinating hospital- and community-based services. Hospitals joined the program in cohorts and engaged in a year-long effort to reduce infection burden. During the program implementation period, many hospitals showed measurable improvement by achieving an HAI-specific relative rate reduction or maintenance of a rate of zero between baseline and intervention periods.
Key successes of the program centered around development of multidisciplinary teams that engaged not only the infection preventionists but also such areas as environmental services and other departments that may not have traditionally been included in infection prevention efforts. These teams focused on establishing competency-based trainings and processes for auditing competencies. One series of STRIVE resources helped hospitals learn new ways to implement best practices and communicate with diverse departments so every team member could participate in removing barriers to infection prevention in the hospital.
SHM was especially pleased to be a part of a program that brought together state health departments, state hospital associations, quality innovation network–quality improvement organizations, and other agencies and health systems committed to infection prevention. The collaboration and partnerships among the STRIVE program participants helped minimize duplication of work and improve efficiency and effectiveness of infection prevention efforts lead by hospitals.
To learn more about the STRIVE resources, visit www.hret.org/quality/projects/strive.shtml.
Multidisciplinary teams celebrate achievements in getting to zero
Multidisciplinary teams celebrate achievements in getting to zero
The Society of Hospital Medicine is pleased to share successes and resources from a 3-year national quality improvement program called STRIVE (States Targeting Reduction in Infections Via Engagement). This program targeted opportunities to streamline and enhance infection prevention and control efforts in participating hospitals.
SHM was a key partner in the STRIVE program, which was managed by the Health Research & Educational Trust, the not-for-profit research and education affiliate of the American Hospital Association. Other partners included the American Society for Healthcare Engineering, Association for Professionals in Infection Control and Epidemiology, University of Michigan, Ann Arbor, and experts from academic institutions and professional societies such as Cornell University, Ithaca, N.Y.; Rush University, Chicago; and the Association for the Healthcare Environment. SHM provided specific knowledge and experience on HAI prevention and helped develop the STRIVE curriculum and resources. Faculty coaches from SHM also supported STRIVE hospitals by presenting on webinars, attending in-person meetings, and consulting on calls.
Following the U.S. experience with Ebola, the Centers for Disease Control and Infection identified the critical importance of enhancing infection control for all infectious threats to protect both patients and health care personnel. The CDC also recognized that many state and regional organizations and agencies work with the same health care facilities in order to coordinate efforts to address infectious threats. The STRIVE program provided tools and resources to help communities strengthen the relationships among diverse organizations to maximize improvement and coordination.
Closely aligned with SHM’s mission to promote exceptional care for hospitalized patients, the CDC’s STRIVE program goals were as follows:
- To expand the CDC’s Targeting Assessment for Prevention (TAP) strategy of using surveillance data to identify hospitals with a disproportionately high burden of health care–associated infections (HAIs),
- To build and strengthen relationships between state and regional organizations that help hospitals with infection control and prevention, and
- To provide technical assistance to hospitals to improve implementation of infection control practices in existing and newly constructed health care facilities.
The participants in this program included 449 hospitals from 28 states and the District of Columbia. Short-stay and long-term acute care hospitals that had a high burden of Clostridium difficile infection, and a high burden of one or more of the following HAIs – central line–associated bloodstream infection, catheter associated urinary tract infection, and health care–associated methicillin-resistant Staphylococcus aureus (MRSA) bacteremia – were targeted. Each participant had access to specific education modules, webinars, and learning networks designed to enhance collaboration, performance improvement, and understanding of the successes and barriers to coordinating hospital- and community-based services. Hospitals joined the program in cohorts and engaged in a year-long effort to reduce infection burden. During the program implementation period, many hospitals showed measurable improvement by achieving an HAI-specific relative rate reduction or maintenance of a rate of zero between baseline and intervention periods.
Key successes of the program centered around development of multidisciplinary teams that engaged not only the infection preventionists but also such areas as environmental services and other departments that may not have traditionally been included in infection prevention efforts. These teams focused on establishing competency-based trainings and processes for auditing competencies. One series of STRIVE resources helped hospitals learn new ways to implement best practices and communicate with diverse departments so every team member could participate in removing barriers to infection prevention in the hospital.
SHM was especially pleased to be a part of a program that brought together state health departments, state hospital associations, quality innovation network–quality improvement organizations, and other agencies and health systems committed to infection prevention. The collaboration and partnerships among the STRIVE program participants helped minimize duplication of work and improve efficiency and effectiveness of infection prevention efforts lead by hospitals.
To learn more about the STRIVE resources, visit www.hret.org/quality/projects/strive.shtml.
The Society of Hospital Medicine is pleased to share successes and resources from a 3-year national quality improvement program called STRIVE (States Targeting Reduction in Infections Via Engagement). This program targeted opportunities to streamline and enhance infection prevention and control efforts in participating hospitals.
SHM was a key partner in the STRIVE program, which was managed by the Health Research & Educational Trust, the not-for-profit research and education affiliate of the American Hospital Association. Other partners included the American Society for Healthcare Engineering, Association for Professionals in Infection Control and Epidemiology, University of Michigan, Ann Arbor, and experts from academic institutions and professional societies such as Cornell University, Ithaca, N.Y.; Rush University, Chicago; and the Association for the Healthcare Environment. SHM provided specific knowledge and experience on HAI prevention and helped develop the STRIVE curriculum and resources. Faculty coaches from SHM also supported STRIVE hospitals by presenting on webinars, attending in-person meetings, and consulting on calls.
Following the U.S. experience with Ebola, the Centers for Disease Control and Infection identified the critical importance of enhancing infection control for all infectious threats to protect both patients and health care personnel. The CDC also recognized that many state and regional organizations and agencies work with the same health care facilities in order to coordinate efforts to address infectious threats. The STRIVE program provided tools and resources to help communities strengthen the relationships among diverse organizations to maximize improvement and coordination.
Closely aligned with SHM’s mission to promote exceptional care for hospitalized patients, the CDC’s STRIVE program goals were as follows:
- To expand the CDC’s Targeting Assessment for Prevention (TAP) strategy of using surveillance data to identify hospitals with a disproportionately high burden of health care–associated infections (HAIs),
- To build and strengthen relationships between state and regional organizations that help hospitals with infection control and prevention, and
- To provide technical assistance to hospitals to improve implementation of infection control practices in existing and newly constructed health care facilities.
The participants in this program included 449 hospitals from 28 states and the District of Columbia. Short-stay and long-term acute care hospitals that had a high burden of Clostridium difficile infection, and a high burden of one or more of the following HAIs – central line–associated bloodstream infection, catheter associated urinary tract infection, and health care–associated methicillin-resistant Staphylococcus aureus (MRSA) bacteremia – were targeted. Each participant had access to specific education modules, webinars, and learning networks designed to enhance collaboration, performance improvement, and understanding of the successes and barriers to coordinating hospital- and community-based services. Hospitals joined the program in cohorts and engaged in a year-long effort to reduce infection burden. During the program implementation period, many hospitals showed measurable improvement by achieving an HAI-specific relative rate reduction or maintenance of a rate of zero between baseline and intervention periods.
Key successes of the program centered around development of multidisciplinary teams that engaged not only the infection preventionists but also such areas as environmental services and other departments that may not have traditionally been included in infection prevention efforts. These teams focused on establishing competency-based trainings and processes for auditing competencies. One series of STRIVE resources helped hospitals learn new ways to implement best practices and communicate with diverse departments so every team member could participate in removing barriers to infection prevention in the hospital.
SHM was especially pleased to be a part of a program that brought together state health departments, state hospital associations, quality innovation network–quality improvement organizations, and other agencies and health systems committed to infection prevention. The collaboration and partnerships among the STRIVE program participants helped minimize duplication of work and improve efficiency and effectiveness of infection prevention efforts lead by hospitals.
To learn more about the STRIVE resources, visit www.hret.org/quality/projects/strive.shtml.
Documentation and billing: Tips for hospitalists
Is it AMS, Delirium, or Encephalopathy?
During residency, physicians are trained to care for patients and write notes that are clinically useful. However, physicians are often not taught about how documentation affects reimbursement and quality measures. Our purpose here, and in articles to follow, is to give readers tools to enable them to more accurately reflect the complexity and work that is done for accurate reimbursements.
If you were to get in a car accident, the body shop would document the damage done and submit it to the insurance company. It’s the body shop’s responsibility to record the damage, not the insurance company’s. So while documentation can seem onerous, the insurance company is not going to scour the chart to find diagnoses missed in the note. That would be like the body shop doing repair work without documenting the damage but then somehow expecting to get paid.
For the insurance company, “If you didn’t document it, it didn’t happen.” The body shop should not underdocument and say there were only a few scratches on the right rear panel if it was severely damaged. Likewise, it should not overbill and say the front bumper was damaged if it was not. The goal is not to bill as much as possible but rather to document appropriately.
Terminology
The expected length of stay (LOS) and the expected mortality for a particular patient is determined by how sick the patient appears to be based on the medical record documentation. So documenting all the appropriate diagnoses makes the LOS index (actual LOS divided by expected LOS) and mortality index more accurate as well. It is particularly important to document when a condition is (or is not) “present on admission”.
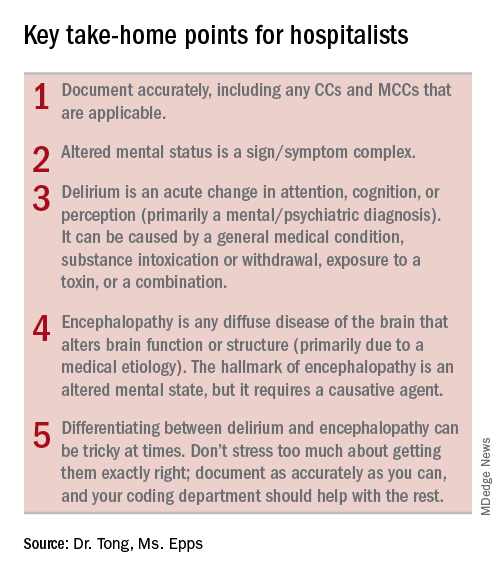
While physician payments can be based on evaluation and management coding, the hospital’s reimbursement is largely determined by physician documentation. Hospitals are paid by Medicare on a capitated basis according to the Acute Inpatient Prospective Payment System. The amount paid is determined by the base rate of the hospital multiplied by the relative weight (RW) of the Medicare Severity Diagnosis Related Group (MS-DRG).
The base rate is adjusted by the wage index of the hospital location. Hospitals that serve a high proportion of low income patients receive a Disproportionate Share Hospital adjustment. The base rate is not something hospitalists have control over.
The RW, however, is determined by the primary diagnosis (reason for admission) and whether or not there are complications or comorbidities (CCs) or major complications or comorbidities (MCCs). The more CCs and MCCs a patient has, the higher the severity of illness and expected increased resources needed to care for that patient.
Diagnoses are currently coded using ICD-10 used by the World Health Organization. The ICD-10 of the primary diagnosis is mapped to an MS-DRG. Many, but not all, MS-DRGs have increasing reimbursements for CCs and MCCs. Coders map the ICD-10 of the principal diagnosis along with any associated CCs or MCCs to the MS-DRG code. The relative weights for different DRGs can found on table 5 of the Medicare website (see reference 1).
Altered mental status versus delirium versus encephalopathy
As an example, let’s look at the difference in RW, LOS, and reimbursement in an otherwise identical patient based on documenting altered mental status (AMS), delirium, or encephalopathy. (see Table 1)
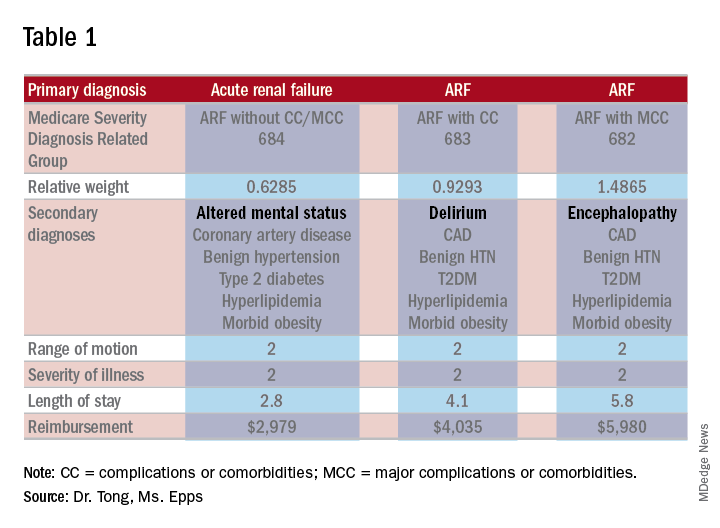
As one can see, RW, estimated LOS, and reimbursement would significantly increase for the patient with delirium (CC) or encephalopathy (MCC) versus AMS (no CC/MCC). A list of which diagnoses are considered CC’s versus MCC’s are on tables 6J and 6I, respectively, on the same Medicare website as table 5.
The difference between AMS, delirium, and encephalopathy
AMS is a sign/symptom complex similar to shortness of breath before an etiology is found. AMS can be the presenting symptom; when a specific etiology is found, however, a more specific diagnosis should be used such as delirium or encephalopathy.
Delirium, according to the DSM-5, is an acute change in the level of attention, cognition, or perception from baseline that developed over hours or days and tends to fluctuate during the course of a day. The change described is not better explained by a preexisting or evolving neurocognitive disorder and does not occur in the context of a severely reduced level of arousal, such as coma. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct consequence of a general medical condition, substance intoxication or withdrawal, exposure to a toxin, or more than one cause.
The National Institute of Neurological Diseases and Stroke defines encephalopathy as “any diffuse disease of the brain that alters brain function or structure. Encephalopathy may be caused by an infectious agent, metabolic or mitochondrial dysfunction, brain tumor or increased intracranial pressure, prolonged exposure to toxic elements, chronic progressive trauma, poor nutrition, or lack of oxygen or blood flow to the brain. The hallmark of encephalopathy is an altered mental state.”
It is confusing since there is a lot of overlap in the definitions of delirium and encephalopathy. One way to tease this out conceptually is noting that delirium is listed under mental, behavioral, and neurodevelopmental disorders, while encephalopathy appears under disorders of the nervous system. One can think of delirium as more of a “mental/psychiatric” diagnosis, while encephalopathy is caused by more “medical” causes.
If a patient who is normally not altered presents with confusion because of an infection or metabolic derangement, one can diagnose and document the cause of an acute encephalopathy. However, let’s say a patient is admitted in the morning with an infection, is started on treatment, but is not initially confused. If he/she later becomes confused at night, one could err conservatively and document delirium caused by sundowning.
Differentiating delirium and encephalopathy can be especially difficult in patients who have dementia with episodic confusion when they present with an infection and confusion. If the confusion is within what family members/caretakers say is “normal,” then one shouldn’t document encephalopathy. As a provider, one shouldn’t focus on all the rules and exceptions, just document as specifically and accurately as possible and the coders should take care of the rest.
Dr. Tong is an assistant professor of hospital medicine and an assistant director of the clinical research program at Emory University, Atlanta. Ms. Epps is director of clinical documentation improvement at Emory Healthcare, Atlanta.
References
1. “Acute Inpatient PPS.” Centers for Medicare and Medicaid Services. Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing, 2013.
3. “Details for title: FY 2018 Final Rule and Correction Notice Tables.” Centers for Medicare and Medicaid Services Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2018-IPPS-Final-Rule-Home-Page-Items/FY2018-IPPS-Final-Rule-Tables.html.
4. “Encephalopathy Information Page.” National Institute of Neurologic Disorders and Stroke. Accessed on 2/17/18. https://www.ninds.nih.gov/Disorders/All-Disorders/Encephalopathy-Information-Page.
5. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. http://apps.who.int/iris/handle/10665/37958.
Is it AMS, Delirium, or Encephalopathy?
Is it AMS, Delirium, or Encephalopathy?
During residency, physicians are trained to care for patients and write notes that are clinically useful. However, physicians are often not taught about how documentation affects reimbursement and quality measures. Our purpose here, and in articles to follow, is to give readers tools to enable them to more accurately reflect the complexity and work that is done for accurate reimbursements.
If you were to get in a car accident, the body shop would document the damage done and submit it to the insurance company. It’s the body shop’s responsibility to record the damage, not the insurance company’s. So while documentation can seem onerous, the insurance company is not going to scour the chart to find diagnoses missed in the note. That would be like the body shop doing repair work without documenting the damage but then somehow expecting to get paid.
For the insurance company, “If you didn’t document it, it didn’t happen.” The body shop should not underdocument and say there were only a few scratches on the right rear panel if it was severely damaged. Likewise, it should not overbill and say the front bumper was damaged if it was not. The goal is not to bill as much as possible but rather to document appropriately.
Terminology
The expected length of stay (LOS) and the expected mortality for a particular patient is determined by how sick the patient appears to be based on the medical record documentation. So documenting all the appropriate diagnoses makes the LOS index (actual LOS divided by expected LOS) and mortality index more accurate as well. It is particularly important to document when a condition is (or is not) “present on admission”.
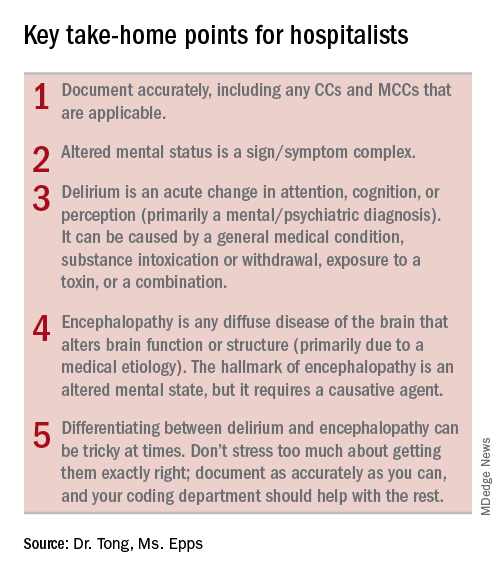
While physician payments can be based on evaluation and management coding, the hospital’s reimbursement is largely determined by physician documentation. Hospitals are paid by Medicare on a capitated basis according to the Acute Inpatient Prospective Payment System. The amount paid is determined by the base rate of the hospital multiplied by the relative weight (RW) of the Medicare Severity Diagnosis Related Group (MS-DRG).
The base rate is adjusted by the wage index of the hospital location. Hospitals that serve a high proportion of low income patients receive a Disproportionate Share Hospital adjustment. The base rate is not something hospitalists have control over.
The RW, however, is determined by the primary diagnosis (reason for admission) and whether or not there are complications or comorbidities (CCs) or major complications or comorbidities (MCCs). The more CCs and MCCs a patient has, the higher the severity of illness and expected increased resources needed to care for that patient.
Diagnoses are currently coded using ICD-10 used by the World Health Organization. The ICD-10 of the primary diagnosis is mapped to an MS-DRG. Many, but not all, MS-DRGs have increasing reimbursements for CCs and MCCs. Coders map the ICD-10 of the principal diagnosis along with any associated CCs or MCCs to the MS-DRG code. The relative weights for different DRGs can found on table 5 of the Medicare website (see reference 1).
Altered mental status versus delirium versus encephalopathy
As an example, let’s look at the difference in RW, LOS, and reimbursement in an otherwise identical patient based on documenting altered mental status (AMS), delirium, or encephalopathy. (see Table 1)
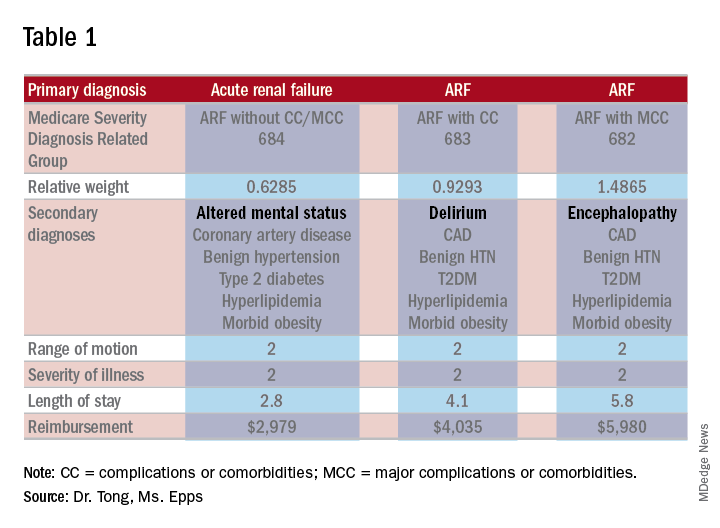
As one can see, RW, estimated LOS, and reimbursement would significantly increase for the patient with delirium (CC) or encephalopathy (MCC) versus AMS (no CC/MCC). A list of which diagnoses are considered CC’s versus MCC’s are on tables 6J and 6I, respectively, on the same Medicare website as table 5.
The difference between AMS, delirium, and encephalopathy
AMS is a sign/symptom complex similar to shortness of breath before an etiology is found. AMS can be the presenting symptom; when a specific etiology is found, however, a more specific diagnosis should be used such as delirium or encephalopathy.
Delirium, according to the DSM-5, is an acute change in the level of attention, cognition, or perception from baseline that developed over hours or days and tends to fluctuate during the course of a day. The change described is not better explained by a preexisting or evolving neurocognitive disorder and does not occur in the context of a severely reduced level of arousal, such as coma. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct consequence of a general medical condition, substance intoxication or withdrawal, exposure to a toxin, or more than one cause.
The National Institute of Neurological Diseases and Stroke defines encephalopathy as “any diffuse disease of the brain that alters brain function or structure. Encephalopathy may be caused by an infectious agent, metabolic or mitochondrial dysfunction, brain tumor or increased intracranial pressure, prolonged exposure to toxic elements, chronic progressive trauma, poor nutrition, or lack of oxygen or blood flow to the brain. The hallmark of encephalopathy is an altered mental state.”
It is confusing since there is a lot of overlap in the definitions of delirium and encephalopathy. One way to tease this out conceptually is noting that delirium is listed under mental, behavioral, and neurodevelopmental disorders, while encephalopathy appears under disorders of the nervous system. One can think of delirium as more of a “mental/psychiatric” diagnosis, while encephalopathy is caused by more “medical” causes.
If a patient who is normally not altered presents with confusion because of an infection or metabolic derangement, one can diagnose and document the cause of an acute encephalopathy. However, let’s say a patient is admitted in the morning with an infection, is started on treatment, but is not initially confused. If he/she later becomes confused at night, one could err conservatively and document delirium caused by sundowning.
Differentiating delirium and encephalopathy can be especially difficult in patients who have dementia with episodic confusion when they present with an infection and confusion. If the confusion is within what family members/caretakers say is “normal,” then one shouldn’t document encephalopathy. As a provider, one shouldn’t focus on all the rules and exceptions, just document as specifically and accurately as possible and the coders should take care of the rest.
Dr. Tong is an assistant professor of hospital medicine and an assistant director of the clinical research program at Emory University, Atlanta. Ms. Epps is director of clinical documentation improvement at Emory Healthcare, Atlanta.
References
1. “Acute Inpatient PPS.” Centers for Medicare and Medicaid Services. Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing, 2013.
3. “Details for title: FY 2018 Final Rule and Correction Notice Tables.” Centers for Medicare and Medicaid Services Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2018-IPPS-Final-Rule-Home-Page-Items/FY2018-IPPS-Final-Rule-Tables.html.
4. “Encephalopathy Information Page.” National Institute of Neurologic Disorders and Stroke. Accessed on 2/17/18. https://www.ninds.nih.gov/Disorders/All-Disorders/Encephalopathy-Information-Page.
5. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. http://apps.who.int/iris/handle/10665/37958.
During residency, physicians are trained to care for patients and write notes that are clinically useful. However, physicians are often not taught about how documentation affects reimbursement and quality measures. Our purpose here, and in articles to follow, is to give readers tools to enable them to more accurately reflect the complexity and work that is done for accurate reimbursements.
If you were to get in a car accident, the body shop would document the damage done and submit it to the insurance company. It’s the body shop’s responsibility to record the damage, not the insurance company’s. So while documentation can seem onerous, the insurance company is not going to scour the chart to find diagnoses missed in the note. That would be like the body shop doing repair work without documenting the damage but then somehow expecting to get paid.
For the insurance company, “If you didn’t document it, it didn’t happen.” The body shop should not underdocument and say there were only a few scratches on the right rear panel if it was severely damaged. Likewise, it should not overbill and say the front bumper was damaged if it was not. The goal is not to bill as much as possible but rather to document appropriately.
Terminology
The expected length of stay (LOS) and the expected mortality for a particular patient is determined by how sick the patient appears to be based on the medical record documentation. So documenting all the appropriate diagnoses makes the LOS index (actual LOS divided by expected LOS) and mortality index more accurate as well. It is particularly important to document when a condition is (or is not) “present on admission”.
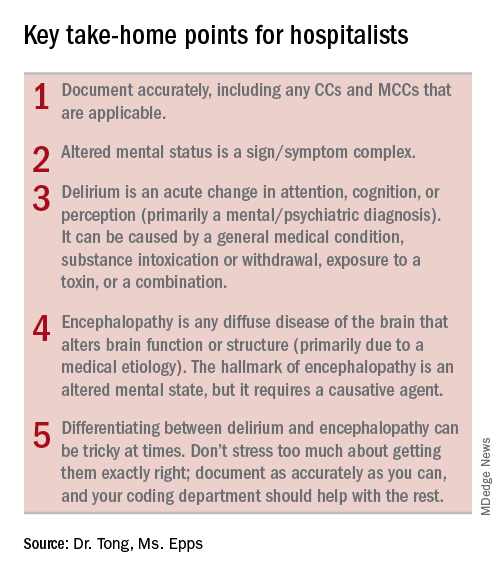
While physician payments can be based on evaluation and management coding, the hospital’s reimbursement is largely determined by physician documentation. Hospitals are paid by Medicare on a capitated basis according to the Acute Inpatient Prospective Payment System. The amount paid is determined by the base rate of the hospital multiplied by the relative weight (RW) of the Medicare Severity Diagnosis Related Group (MS-DRG).
The base rate is adjusted by the wage index of the hospital location. Hospitals that serve a high proportion of low income patients receive a Disproportionate Share Hospital adjustment. The base rate is not something hospitalists have control over.
The RW, however, is determined by the primary diagnosis (reason for admission) and whether or not there are complications or comorbidities (CCs) or major complications or comorbidities (MCCs). The more CCs and MCCs a patient has, the higher the severity of illness and expected increased resources needed to care for that patient.
Diagnoses are currently coded using ICD-10 used by the World Health Organization. The ICD-10 of the primary diagnosis is mapped to an MS-DRG. Many, but not all, MS-DRGs have increasing reimbursements for CCs and MCCs. Coders map the ICD-10 of the principal diagnosis along with any associated CCs or MCCs to the MS-DRG code. The relative weights for different DRGs can found on table 5 of the Medicare website (see reference 1).
Altered mental status versus delirium versus encephalopathy
As an example, let’s look at the difference in RW, LOS, and reimbursement in an otherwise identical patient based on documenting altered mental status (AMS), delirium, or encephalopathy. (see Table 1)
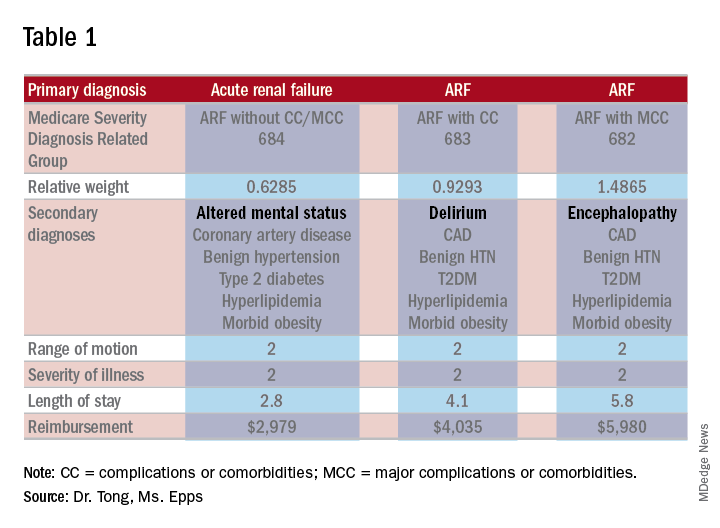
As one can see, RW, estimated LOS, and reimbursement would significantly increase for the patient with delirium (CC) or encephalopathy (MCC) versus AMS (no CC/MCC). A list of which diagnoses are considered CC’s versus MCC’s are on tables 6J and 6I, respectively, on the same Medicare website as table 5.
The difference between AMS, delirium, and encephalopathy
AMS is a sign/symptom complex similar to shortness of breath before an etiology is found. AMS can be the presenting symptom; when a specific etiology is found, however, a more specific diagnosis should be used such as delirium or encephalopathy.
Delirium, according to the DSM-5, is an acute change in the level of attention, cognition, or perception from baseline that developed over hours or days and tends to fluctuate during the course of a day. The change described is not better explained by a preexisting or evolving neurocognitive disorder and does not occur in the context of a severely reduced level of arousal, such as coma. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct consequence of a general medical condition, substance intoxication or withdrawal, exposure to a toxin, or more than one cause.
The National Institute of Neurological Diseases and Stroke defines encephalopathy as “any diffuse disease of the brain that alters brain function or structure. Encephalopathy may be caused by an infectious agent, metabolic or mitochondrial dysfunction, brain tumor or increased intracranial pressure, prolonged exposure to toxic elements, chronic progressive trauma, poor nutrition, or lack of oxygen or blood flow to the brain. The hallmark of encephalopathy is an altered mental state.”
It is confusing since there is a lot of overlap in the definitions of delirium and encephalopathy. One way to tease this out conceptually is noting that delirium is listed under mental, behavioral, and neurodevelopmental disorders, while encephalopathy appears under disorders of the nervous system. One can think of delirium as more of a “mental/psychiatric” diagnosis, while encephalopathy is caused by more “medical” causes.
If a patient who is normally not altered presents with confusion because of an infection or metabolic derangement, one can diagnose and document the cause of an acute encephalopathy. However, let’s say a patient is admitted in the morning with an infection, is started on treatment, but is not initially confused. If he/she later becomes confused at night, one could err conservatively and document delirium caused by sundowning.
Differentiating delirium and encephalopathy can be especially difficult in patients who have dementia with episodic confusion when they present with an infection and confusion. If the confusion is within what family members/caretakers say is “normal,” then one shouldn’t document encephalopathy. As a provider, one shouldn’t focus on all the rules and exceptions, just document as specifically and accurately as possible and the coders should take care of the rest.
Dr. Tong is an assistant professor of hospital medicine and an assistant director of the clinical research program at Emory University, Atlanta. Ms. Epps is director of clinical documentation improvement at Emory Healthcare, Atlanta.
References
1. “Acute Inpatient PPS.” Centers for Medicare and Medicaid Services. Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing, 2013.
3. “Details for title: FY 2018 Final Rule and Correction Notice Tables.” Centers for Medicare and Medicaid Services Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2018-IPPS-Final-Rule-Home-Page-Items/FY2018-IPPS-Final-Rule-Tables.html.
4. “Encephalopathy Information Page.” National Institute of Neurologic Disorders and Stroke. Accessed on 2/17/18. https://www.ninds.nih.gov/Disorders/All-Disorders/Encephalopathy-Information-Page.
5. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. http://apps.who.int/iris/handle/10665/37958.