User login
Innovative therapies in gynecology: The evidence and your practice
As more and more gynecologic therapies move to the outpatient setting, keeping up on the latest data regarding emerging options can be challenging. Furthermore, it can be difficult to justify purchasing expensive equipment for the office when a therapy is not covered by medical insurance plans. However, if a therapy is efficacious and patients are willing to pay out of pocket, clinicians may want to have these options available for their patients.
In an effort to work through these complex issues, a panel of experts was convened at the 47th Annual Scientific Meeting of the Society of Gynecologic Surgeons in Palm Springs, California, on June 29, 2021. This article includes the salient points from that panel discussion.
Fractionated CO2 laser therapy
Fractionated CO2 laser therapy is considered second-line therapy for the treatment of genitourinary syndrome of menopause (GSM). In 2018, the US Food and Drug Administration (FDA) issued a safety warning about the use of CO2 laser therapy and warned patients and clinicians that the FDA had not approved the treatment for vaginal rejuvenation or treatment of vaginal symptoms related to menopause, urinary incontinence, or sexual function. Despite this warning, laser treatments are still performed in many practices.
In 2019, the International Continence Society (ICS) and the International Society for the Study of Vulvovaginal Disease (ISSVD) put out a joint practice consensus statement that essentially did not recommend the routine use of laser treatment for GSM, urinary incontinence, or lichen sclerosus.1 Conversely, the 2020 American Urogynecologic Society (AUGS) published a clinical consensus statement that spoke to the promising results of laser therapy for the treatment of vulvovaginal atrophy, vaginal dryness, and menopausal dyspareunia, with benefits lasting up to 1 year.2 This statement also suggested that the short-term safety profile of the CO2 laser device was favorable.
How CO2 lasers work
Fractionated CO2 laser therapy differs from unfractionated treatment (which often is used in the treatment of condyloma) in that it is not ablative. The laser works by using fractionated beams of light to penetrate the affected tissue to create small wounds in the epithelium and underlying lamina propria, which leads to collagen remodeling and regeneration that then results in the restoration of the superficial epithelium, vaginal rugae, and lubrication.3 Most clinicians perform 3 applications of the laser treatment 6 weeks apart, a recommendation that is based on manufacturer-sponsored studies in menopausal women.
Study results of patient outcomes with laser therapy
GSM. Several retrospective4,5 and prospective studies6-10 have looked at short- and longer-term outcomes in patients undergoing treatment with the CO2 laser. All of these studies showed improvement in patient symptoms related to GSM.
The VeLVET trial, conducted by Paraiso and colleagues, was a randomized trial that compared CO2 laser treatment with vaginal estrogen in women with GSM.11 While the study was underpowered due to cessation of enrollment once the FDA safety warning was issued, the authors reported that at 6 months, both the fractionated CO2 laser therapy group and the vaginal estrogen group had similar improvements, with 70% to 80% of participants reporting satisfaction with treatment. The authors concluded that laser therapy is likely to be as efficacious as vaginal estrogen and may be a good option for patients who cannot use vaginal estrogen to treat GSM.11
Lichen sclerosus. Some data exist on the efficacy of laser therapy for the treatment of lichen sclerosus. One recently published randomized trial showed that at 6 months, fractionated CO2 laser treatment and prior treatment with high potency topical corticosteroids was associated with higher improvement in subjective symptoms and objective measures compared with clobetasol propionate treatment.12 Another trial, however, revealed that laser treatment was not an effective monotherapy treatment for lichen sclerosus when compared with placebo.13 Fewer studies have examined the effect of laser therapy on urinary incontinence.
More prospective data are emerging, evidenced by trials currently registered in ClinicalTrials.gov. While some studies provide evidence that laser therapy may be efficacious in the treatment of vulvovaginal atrophy, additional data are needed to confirm the favorable outcomes observed with laser therapy for the treatment of lichen sclerosus, and a significant amount of data are needed to evaluate the efficacy of laser treatment for urinary incontinence.
Until such evidence is available, fractionated CO2 vaginal laser therapy will remain a fee-for-service treatment option and will be inaccessible to patients who cannot afford the cost of treatment.
Continue to: Hydrogel urethral bulking...
Hydrogel urethral bulking
Urethral bulking agents have been used for 5 decades in the treatment of stress urinary incontinence (SUI) in women. Unlike midurethral slings, in which many medical device companies use the same implant material (microporous, monofilament polypropylene mesh), the material for bulking agents has varied greatly. A 2017 Cochrane review of urethral bulking listed these agents used for this indication: autologous fat, carbon beads, calcium hydroxylapatite, ethylene vinyl alcohol copolymer, glutaraldehyde cross-linked bovine collagen, hyaluronic acid with dextranomer, porcine dermal implant, polytetrafluoroethylene, and silicone particles.14 These agents can be injected through a transurethral or periurethral technique. The review failed to find superiority of one material or injection technique over another.
New bulking agent available
In January 2020, the FDA approved the premarket application for a new bulking agent. This new agent is a permanently implanted, nonresorbable hydrogel that consists of cross-linked polyacrylamide (2.5%) and water (97.5%). It is intended to be used with a transurethral bulking system that includes a rotatable sheath and two 23-guage needles; a total of 1.5 to 2.0 mL of the hydrogel is injected in 3 locations in the proximal urethra per session. Patients may undergo an additional 2 sessions, if needed, at least 4 weeks after the previous session.
Polyacrylamide hydrogel has been used as a bulking agent in cosmetic and ophthalmic surgery for many years, and it was first approved for medical use in Europe in 2001. The initial European data on its use as a urethral bulking agent was published in 2006.15 The first North American data came in 2014 from a multicenter, randomized trial that compared polyacrylamide hydrogel with collagen gel.16 This investigation followed 345 women for 12 months and concluded that the safety and efficacy of polyacrylamide hydrogel was not inferior to collagen, with a little over half of both cohorts demonstrating a 50% or greater decrease in incontinence episodes.
Since these initial studies, 3-year17 and 7-year safety and efficacy data18 have been reported, with reassuring findings, but both studies experienced significant attrition of the original group of patients. The most commonly reported adverse events associated with the procedure are pain at the injection site (4%–14%) and urinary tract infection (3%–7%); transient urinary retention rates range in incidence from 1.5% to 15%.19
Short procedure, long-term results
Given that a urethral bulking procedure can be done in less than 10 minutes in the office under local analgesia, this treatment may lend itself to use in more brittle patient populations. One study of women aged 80 or older showed a greater than 50% decrease in the number of daily pads used for up to 2 years after initial injection.20 Another study found the greatest treatment success in women aged 60 years or older with fewer than 2.5 episodes of SUI per day.21
Platelet-rich plasma therapy
Platelet-rich plasma (PRP) therapy has been used in multiple disciplines for more than 2 decades as a treatment to regenerate damaged tissue, particularly in sports medicine for treating tendonitis as well as in plastic surgery, gynecology, urology, and ophthalmology, and good outcomes have been demonstrated with no serious adverse effects. PRP is a natural product in which high levels of platelets are concentrated through centrifugation with bioactive growth factors, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), fibroblast growth factor (FGF), and insulin growth factor (IGF).22 The activated platelets are then injected autologously back into the patient’s tissue. This process releases activated growth factors that accelerate tissue healing by stimulating the number of reparative cells to create collagen production, angiogenesis, and neurogenesis while fighting infection and downregulating the autoimmune system.
Continue to: Uses for PRP in gynecology...
Uses for PRP in gynecology
In gynecology, dating back to 2007 PRP was shown to facilitate wound healing, when Fanning and colleagues reported PRP applications in gynecologic operative wounds, such as hysterectomies and urogynecologic procedures, to reduce postoperative pain.23 In the last decade, there has been a dramatic increasing trend in the application of PRP injections as an alternative therapy in gynecology to improve intimate health. PRP has been used to treat lichen sclerosus, atrophic vaginitis, SUI, and female sexual dysfunction; however, there is a dearth of studies that compare PRP with traditional therapies.
Runels and colleagues described the effects of localized injections of autologous PRP for the treatment of sexual dysfunction early in 2014.24 Those authors pioneered PRP use in women with dyspareunia and other symptoms related to sexual dysfunction. Women were offered PRP injections into the periurethral area of the Skene glands and the clitoris. Sexual satisfaction and pain were improved but results did not reach statistical significance. The results of this pilot study of 11 patients suggested that PRP injections could perhaps be an effective method to treat certain types of female sexual dysfunction, including desire, arousal, lubrication, and orgasm.
In another pilot study, Long and colleagues looked at the effectiveness of local injection of PRP for treating women with SUI.25 In that study, younger patients with mild severity of SUI had promising results, with up to 75% cured or improved. Results in the older group, with 50% cured or improved, did not reach statistical significance. Other small, limited studies have been conducted under the hypothesis that PRP as an “O-shot” may be a promising treatment that is a safe, effective, nonsurgical, and nonhormonal option for women with dyspareunia from lack of lubrication and related sexual dysfunction, such as decreased libido or arousal.26-29 A pilot study by Behnia-Willison and colleagues demonstrated clinical improvement in PRP use as an alternative to topical steroids for lichen sclerosus.30 Several other studies also have shown efficacy for the treatment of lichen sclerosus.31-34
More evidence of efficacy needed
To date, preliminary studies suggest that PRP holds promise for a host of gynecologic conditions. Since PRP is autologous, there are no significant contraindications, and thus far there have been no known serious adverse effects. However, most health insurers still do not cover this therapy, so for now patients must pay out-of-pocket fees for these treatments.
As we continue to investigate therapies in regenerative medicine, the continued efforts of our discipline are required to conduct well-designed prospective, randomized controlled studies. While initial series suggest that PRP is safe, it is unlikely that this therapy will be embraced widely in the paradigm as an alternative treatment option for many genitourinary symptoms of menopause and vulvar disorders until efficacy is better established.
Radiofrequency therapy
For the past 20 years, radiofrequency (RF) energy has been used through the vagina, urethra, and periurethral tissues for the treatment of genitourinary symptoms, with limited success. More recently, because some patients hesitate to receive mesh implants for treatment of urinary incontinence,35 there has been gravitation to office-based procedures.
In contrast to lasers, which transmit energy through light, RF waves (measured in hertz) transform the kinetic energy of the intracellular atoms, which move and collide, generating thermal energy.36,37 RF therapy has been shown to increase the proportion of smooth muscle and connective tissue; stimulate proliferation of the epithelium, neovascularization, and collagen formation in the lamina propria; and improve natural lubrication.36,38 In addition, RF is:
- ablative when the heat is capable of generating ablation and/or necrosis of the epidermis and dermis
- microablative when energy fractionation produces microscopic columns of ablative thermal lesions in the epidermis and upper dermis, resulting in microscopic columns of treated tissue interspersed with areas of untreated skin,39 and
- nonablative when trauma occurs only in the dermis by heating without causing ablation of the epidermis.39
The RF devices discussed below are used with settings for microablation in the treatment of SUI and sexual health/vaginal laxity, and with nonablative settings in the treatment of GSM.
RF for the treatment of urinary incontinence
Studies with RF have shown its benefits in urinary symptoms as secondary outcomes, such as improvement of SUI.38,40 One theory that favors energy devices as a treatment for SUI is that the treatment strengthens suburethral and pubocervical support, thereby decreasing urethral mobility.41
In 2016, the Viveve system (Viveve) received FDA 510(k) clearance for “use in general surgical procedures for electrocoagulation and hemostasis.” A single-site, randomized, nonblinded pilot study compared 1 treatment (group 1) versus 2 treatments (group 2) with the Viveve system for SUI in 35 participants.42 At 12 months, only for group 2 did mean scores on the Incontinence Impact Questionnaire Short Form (IIQ-7) and the International Consultation on Incontinence Modular Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI-SF) decrease by the minimum clinically important difference of 16 and 2.52 points, respectively, compared with baseline.
The ThermiVa device (ThermiGen, LLC) received FDA clearance for “use in dermatological and general surgical procedures for electrocoagulation and hemostasis” in 2017. A single-site, prospective, double-blind, randomized controlled pilot trial evaluated the efficacy of this device for the treatment of SUI in 20 participants randomly assigned in a 1:1 fashion to active and sham groups.43 At 12 weeks, mean scores of the Urogenital Distress Inventory (UDI-6) and the ICIQ-UI-SF decreased by the minimal clinically important difference only in the treatment group arm. Additionally, 70% of treatment group participants had a negative stress test at 12 weeks compared with 0% of control group participants.43 In another study of 48 patients who were followed longitudinally for 5 months, a substantial improvement in genital appearance was observed.44 Assessment based on validated instruments demonstrated significant improvements in sexual function and SUI.44
A microablative RF device (Wavetronic 6000 Touch Device, Megapulse HF FRAXX system; Loktal Medical Electronics) consists of a vaginal probe with 64 microneedles at the tip, each capable of penetrating to a depth of 1 mm. During activation, delivery of RF energy, which results in vaporization of tissue at 100 °C, occurs in a preset sequence of 8 needles at a time, preventing the overheating of intervening tissue between adjacent needles.
Slongo and colleagues conducted a 3-arm randomized clinical trial that included 117 climacteric women with SUI.45 In group 1, treatment consisted of 3 monthly sessions of RF; group 2 received 12 weekly sessions of pelvic floor muscle training (PFMT); and group 3 received RF treatment plus PFMT simultaneously. Assessments were conducted at baseline and 30 days after the end of therapy using validated questionnaires and scales for urinary, vaginal, and sexual functions, and cytology was used to assess vaginal atrophy. The association between RF and PFMT showed significant improvement in the SUI symptoms assessed by questionnaire. The vaginal symptoms and dryness showed more substantial improvement with the RF treatment, and vaginal laxity showed similar improvement in the 3 treatment groups.45
Continue to: RF for the treatment of GSM...
RF for the treatment of GSM
For women who are not candidates for localized hormone therapy, as well as others who simply do not wish to use hormones, nonablative RF laser therapy may be an alternative for the management of GSM.
The VIVEVE I trial was one of the largest randomized, sham-controlled trials performed to determine the efficacy of vaginal rejuvenation using surface-cooled RF; 174 women received either RF treatment (90 J/cm2) or sham treatment (1 J/cm2).46 Treated participants had a significant improvement in perception of vaginal laxity/looseness and sexual function up to 6 months posttreatment.46 Overall, participants were satisfied with the treatment (77.8%–100%) and reported significant improvements in vaginal laxity and symptoms of atrophy. RF was well tolerated with minimal adverse effects, such as procedure-related erythema and edema of treated tissue, and vaginal discharge. One patient discontinued treatment because of procedural pain.47,48
The ThermiVa system also was evaluated for efficacy in the treatment of GSM in a single-site, double-blind randomized controlled pilot study, the methods of which were previously described above.43 GSM symptoms were evaluated at baseline and 12 weeks using the Vaginal Health Index (VHI) and visual analog scale (VAS). At the 12-week follow-up, compared with baseline scores, VHI scores were unchanged in the control group and improved in the treatment group. Additionally, VAS scores for dyspareunia decreased in the treatment group compared with baseline while VAS for dyspareunia in the sham group did not change from baseline to 12 weeks.
RF treatment for sexual health
The efficacy of the Viveve RF system for female sexual dysfunction was evaluated in an international, randomized, controlled, single-blinded study (n = 154) that compared 6-month outcomes of RF treatment versus sham treatment.46 Although there was a statistically significant improvement in patient-reported sexual dysfunction on validated instruments, it is essential to note that the study was powered for the primary outcome of vaginal laxity. In addition, the study was not adequately powered to evaluate safety; however, the adverse events reported were mild, and the most frequently reported adverse event was vaginal discharge.
Microablative monopolar RF treatment for GSM has been evaluated in 2 single-arm clinical trials that included a total of 70 patients.39,49 Pre- and posttreatment outcomes were analyzed after delivery of 3 treatment sessions 28 to 40 days apart. Although the only significant improvement in quality of life was in the health domain of the World Health Organization Quality of Life Adapted Questionnaire (P = .04), significant improvements in sexual functioning were seen in terms of the desire (P = .002), lubrication (P = .001), satisfaction (P = .003), and pain (P = .007) domains of the Female Sexual Function Index (FSFI) questionnaire except for excitation and orgasm.39 Overall, 100% of participants reported being satisfied or very satisfied with treatments, and 13 of 14 women felt “cured” or “much better.”39 After treatment, significant increases in vaginal Lactobacillus (P<.001), decreases in vaginal pH (P<.001), improvements in maturation of vaginal cellularity (decreased parabasal cells, P<.001; increased superficial cells, P<.001), and increased VHI score (P<.001) alone occurred.49 No adverse events beyond self-limited vaginal burning and redness were reported.39,49 In another study mentioned above, the combination of RF and PFMT in sexual function does not offer benefits superior to those achieved by the therapies alone.45
Evidence on RF treatment does not support marketing efforts
Radiofrequency devices have been marketed for a variety of genitourinary problems in women, with limited high-quality, randomized, comparative evidence of efficacy and durability in the literature. It is unfortunate that RF treatment continues to be promoted by practitioners around the world who cite small, short-term studies that lack biostatistical rigor in their reporting of protocols and results. Statements from both AUGS and the International Urogynecological Association have heeded caution on the use of lasers but they could not even evaluate RF devices due to lack of evidence.2,41
Informed counseling and shared decision making remain the bottom line
By the year 2025, all members of the Baby Boom generation will be aged 60 or older. While in the past there has been a reluctance to discuss women’s sexual health, urinary incontinence, and GSM, the need for open discussion and a variety of treatment options for these conditions has never been more critical.
Many patients prefer office-based therapies over hospital-based procedures, and others are leery of synthetic implants. These concerns are leading toward great interest in the types of treatments covered in this article. However, it is paramount that clinicians are aware of the evidence-based data behind these emerging options so that we can openly and accurately counsel our patients.
As we have shown, the quality of the data behind these officed-based therapies varies significantly. Until a greater body of research data is available, we must carefully balance our desire to meet patient wishes with solid, informed counseling and shared decision making. ●
- Preti M, Viera-Baptista P, Digesu GA, et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: an ICS/ISSVD best practice consensus document. J Lower Genital Tract Dis. 2019;23:151-160.
- Alshiek J, Garcia B, Minassian V, et al. Vaginal energy-based devices: AUGS clinical consensus statement. Female Pelvic Med Reconstr Surg. 2020;26:287-298.
- Streicher LF. Vulvar and vaginal fractional CO2 laser treatments for genitourinary syndrome of menopause: NAMS practice pearl. Menopause. 2018;25:571-573.
- Gardner AN, Aschkenazi SO. The short-term efficacy and safety of fractional CO2 laser therapy for vulvovaginal symptoms in menopause, breast cancer, and lichen sclerosus. Menopause. 2021; 28:511-516.
- Balchander D, Nyirjesy P. Fractionated CO2 laser therapy in recalcitrant lichen sclerosus. J Lower Genital Tract Disease. 2020;24:225-228.
- Pieralli A, Fallani MG, Becorpi A, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294:841-846.
- Pieralli A, Bianchi C, Longinotti M, et al. Long-term reliability of fractionated CO2 laser as a treatment of vulvovaginal atrophy (VVA) symptoms. Arch Gynecol Obstet. 2017; 296:973-978.
- Sokol ER, Karram MM. Use of novel fractional CO2 laser for the treatment of genitourinary syndrome of menopause: 1-year outcomes. Menopause. 2017;24: 810-814.
- Pagano T, Conforti A, Buonfantino C, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. 2020;27:418-422.
- Sindou-Faurie T, Louis-Vahdat C, Oueld Es Cheikh E, et al. Evaluation of the efficacy of fractional CO2 laser in the treatment of vulvar and vaginal menopausal symptoms. Arch Gynecol Obstet. 2021;303:955-963.
- Paraiso MFR, Ferrando CA, Sokol ER, at al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET trial. Menopause. 2019;27:50-56.
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978.
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;136:979-987.
- Kirchin V, Page T, Keegan PE, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD003881.
- Lose G, Mouritsen L, Nielson JB. A new bulking agent (polyacrylamide hydrogel) for treating stress urinary incontinence in women. BJU Int. 2006;98:100-104.
- Sokol ER, Karram MM, Dmochowski R. Efficacy and safety of polyacrylamide hydrogel for the treatment of female stress incontinence: a randomized, prospective, multicenter North American study. J Urol. 2014;192:843-849.
- Pai A, Al-Singary W. Durability, safety and efficacy of polyacrylamide hydrogel (Bulkamid) in the management of stress and mixed urinary incontinence: three year follow up outcomes. Cent European J Urol. 2015;68:428-433.
- Brosche T, Kuhn A, Lobodasch K, et al. Seven-year efficacy and safety outcomes of Bulkamid for the treatment of stress urinary incontinence. Neurourol Urodyn. 2021;40:502-508.
- Kasi AD, Pergialiotis V, Perrea DN, et al. Polyacrylamide hydrogel (Bulkamid) for stress urinary incontinence in women: a systematic review of the literature. Int Urogynecol J. 2016;27:367-375.
- Vecchioli-Scaldazza CV, Smaali C, Morosetti C, et al. Polyacrylamide hydrogel (Bulkamid) in female patients of 80 or more years with urinary incontinence. Int Braz J Urol. 2014;40:37-43.
- Elmelund M, Sokol ER, Darram MM, et al. Patient characteristics that may influence the effect of urethral injection therapy for female stress urinary incontinence. J Urol. 2019;202:125-131.
- Sanoulis V, Nikolettos N, Vlahos N. The use of platelet-rich plasma in the gynecological clinical setting: a review. HJOG. 2019;18:55-65.
- Fanning J, Murrain L, Flora R, et al. Phase I/II prospective trial of autologous platelet tissue graft in gynecologic surgery. J Minim Invasive Gynecol. 2007;14:633-637.
- Runels CE, Melnick H, DeBourbon E, et al. A pilot study of the effect of localized injections of autologous platelet rich plasma (PRP) for the treatment of female sexual dysfunction. J Womens Health Care. 2014;3:4.
- Long CY, Lin KL, Shen CR, et al. A pilot study: effectiveness of local injection of autologous platelet-rich plasma in treating women with stress urinary incontinence. Sci Rep. 2021;11:1584.
- Matz EJ, Pearlman AM, Terlecki RP. Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig Clin Urol. 2018;59:61-65.
- Neto JB. O-Shot: platelets rich plasma in intimate female treatment. J Womens Health Care. 2017;6:5.
- Nikolopoulos KI, Pergialiotis V, Perrea D, et al. Restoration of the pubourethral ligament with platelet rich plasma for the treatment of stress urinary incontinence. Med Hypotheses. 2016;90:29-31.
- Hersant B, SidAhmed-Mezi M, Belkacemi Y, et al. Efficacy of injecting platelet concentrate combined with hyaluronic acid for the treatment of vulvovaginal atrophy in postmenopausal women with a history of breast cancer: a phase 2 pilot study. Menopause. 2018;25:1124-1130.
- Behnia-Willison F, Pour NR, Mohamadi B, et al. Use of platelet-rich plasma for vulvovaginal autoimmune conditions like lichen sclerosus. Plast Reconstr Surg Glob Open. 2016;4:e1124.
- Goldstein AT, King M, Runels C, et al. Intradermal injection of autologous platelet-rich plasma for the treatment of vulvar lichen sclerosus. J Am Acad Dermatol. 2017;76:158-160.
- Casabona F, Priano V, Vallerino V, et al. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plast Reconstr Surg. 2010;126:210e-211e.
- Franic D, Iternica Z, Franic-Ivanisevic M. Platelet-rich plasma (PRP) for the treatment of vulvar lichen sclerosus in a premenopausal woman: a case report. Case Rep Womens Health. 2018;18: e0062.
- Posey LK, Runels C. In office surgery and use of platelet rich plasma for the treatment of vulvar lichen sclerosus to alleviate painful sexual intercourse. J Lower Genital Tract Dis. 2017;21(4S):S14.
- Stachowicz AM, Hoover ML, Karram MM. Clinical utility of radiofrequency energy for female genitourinary dysfunction: past, present, and future. Int Urogynecol J. 2021;32:1345-1350.
- Tadir Y, Gaspar A, Lev-Sagie A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med. 2017;49:137-159.
- US Food and Drug Administration. Statement from FDA Commissioner Scott Gottlieb, MD, on efforts to safeguard women’s health from deceptive health claims and significant risks related to devices marketed for use in medical procedures for “vaginal rejuvenation.” https://www.fda.gov/news-events/pressannouncements/statement-fda-commissioner-scott-gottlieb-mdefforts-safeguard-womens-health-deceptive-health-claims. Updated August 2, 2018. Accessed August 13, 2021.
- Vicariotto F, Raichi M. Technological evolution in the radiofrequency treatment of vaginal laxity and menopausal vulvo-vaginal atrophy and other genitourinary symptoms: first experiences with a novel dynamic quadripolar device. Minerva Ginecol. 2016;68:225-236.
- Kamilos MF, Borrelli CL. New therapeutic option in genitourinary syndrome of menopause: pilot study using microablative fractional radiofrequency. Einstein (Sao Paulo). 2017;15:445-551.
- Caruth JC. Evaluation of the safety and efficacy of a novel radiofrequency device for vaginal treatment. Surg Technol Int. 2018;32:145-149.
- Shobeiri SA, Kerkhof MH, Minassian VA, et al. IUGA committee opinion: laser-based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int Urogynecol J. 2019;30:371-376.
- Allan BB, Bell S, Husarek K. Early feasibility study to evaluate the Viveve system for female stress urinary incontinence: interim 6-month report. J Womens Health (Larchmt). 2020;29:383-389.
- Leibaschoff G, Izasa PG, Cardona JL, et al. Transcutaneous temperature controlled radiofrequency (TTCRF) for the treatment of menopausal vaginal/genitourinary symptoms. Surg Technol Int. 2016;29:149-159.
- Desai SA, Vakil Z, Kroumpouzos G. Transcutaneous temperature-controlled radiofrequency treatment: improvement in female genital appearance, sexual dysfunction, and stress urinary incontinence. Aesthet Surg J. 2021;sjab174. doi: 10.1093/asj/sjab174.
- Slongo H, Lunardi AL, Riccetto CL, et al. Microablative radiofrequency versus pelvic floor muscle training for stress urinary incontinence: a randomized controlled trial. Int Urogynecol J. 2021. doi: 10.1007 /s00192-021-04758-2.
- Krychman M, Rowan CG, Allan BB, et al. Effect of single-treatment, surface-cooled radiofrequency therapy on vaginal laxity and female sexual function: the VIVEVE I randomized controlled trial. J Sex Med. 2017;14:215-225.
- Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30: 429-436.
- Juhasz ML, Korta DZ, Mesinkovska NA. Vaginal rejuvenation: a retrospective review of lasers and radiofrequency devices. Dermatol Surg. 2021;47:489-494.
- Sarmento AC, Fernandes FS, Marconi C, et al. Impact of microablative fractional radiofrequency on the vaginal health, microbiota, and cellularity of postmenopausal women. Clinics (Sao Paulo). 2020;75:e1750.
As more and more gynecologic therapies move to the outpatient setting, keeping up on the latest data regarding emerging options can be challenging. Furthermore, it can be difficult to justify purchasing expensive equipment for the office when a therapy is not covered by medical insurance plans. However, if a therapy is efficacious and patients are willing to pay out of pocket, clinicians may want to have these options available for their patients.
In an effort to work through these complex issues, a panel of experts was convened at the 47th Annual Scientific Meeting of the Society of Gynecologic Surgeons in Palm Springs, California, on June 29, 2021. This article includes the salient points from that panel discussion.
Fractionated CO2 laser therapy
Fractionated CO2 laser therapy is considered second-line therapy for the treatment of genitourinary syndrome of menopause (GSM). In 2018, the US Food and Drug Administration (FDA) issued a safety warning about the use of CO2 laser therapy and warned patients and clinicians that the FDA had not approved the treatment for vaginal rejuvenation or treatment of vaginal symptoms related to menopause, urinary incontinence, or sexual function. Despite this warning, laser treatments are still performed in many practices.
In 2019, the International Continence Society (ICS) and the International Society for the Study of Vulvovaginal Disease (ISSVD) put out a joint practice consensus statement that essentially did not recommend the routine use of laser treatment for GSM, urinary incontinence, or lichen sclerosus.1 Conversely, the 2020 American Urogynecologic Society (AUGS) published a clinical consensus statement that spoke to the promising results of laser therapy for the treatment of vulvovaginal atrophy, vaginal dryness, and menopausal dyspareunia, with benefits lasting up to 1 year.2 This statement also suggested that the short-term safety profile of the CO2 laser device was favorable.
How CO2 lasers work
Fractionated CO2 laser therapy differs from unfractionated treatment (which often is used in the treatment of condyloma) in that it is not ablative. The laser works by using fractionated beams of light to penetrate the affected tissue to create small wounds in the epithelium and underlying lamina propria, which leads to collagen remodeling and regeneration that then results in the restoration of the superficial epithelium, vaginal rugae, and lubrication.3 Most clinicians perform 3 applications of the laser treatment 6 weeks apart, a recommendation that is based on manufacturer-sponsored studies in menopausal women.
Study results of patient outcomes with laser therapy
GSM. Several retrospective4,5 and prospective studies6-10 have looked at short- and longer-term outcomes in patients undergoing treatment with the CO2 laser. All of these studies showed improvement in patient symptoms related to GSM.
The VeLVET trial, conducted by Paraiso and colleagues, was a randomized trial that compared CO2 laser treatment with vaginal estrogen in women with GSM.11 While the study was underpowered due to cessation of enrollment once the FDA safety warning was issued, the authors reported that at 6 months, both the fractionated CO2 laser therapy group and the vaginal estrogen group had similar improvements, with 70% to 80% of participants reporting satisfaction with treatment. The authors concluded that laser therapy is likely to be as efficacious as vaginal estrogen and may be a good option for patients who cannot use vaginal estrogen to treat GSM.11
Lichen sclerosus. Some data exist on the efficacy of laser therapy for the treatment of lichen sclerosus. One recently published randomized trial showed that at 6 months, fractionated CO2 laser treatment and prior treatment with high potency topical corticosteroids was associated with higher improvement in subjective symptoms and objective measures compared with clobetasol propionate treatment.12 Another trial, however, revealed that laser treatment was not an effective monotherapy treatment for lichen sclerosus when compared with placebo.13 Fewer studies have examined the effect of laser therapy on urinary incontinence.
More prospective data are emerging, evidenced by trials currently registered in ClinicalTrials.gov. While some studies provide evidence that laser therapy may be efficacious in the treatment of vulvovaginal atrophy, additional data are needed to confirm the favorable outcomes observed with laser therapy for the treatment of lichen sclerosus, and a significant amount of data are needed to evaluate the efficacy of laser treatment for urinary incontinence.
Until such evidence is available, fractionated CO2 vaginal laser therapy will remain a fee-for-service treatment option and will be inaccessible to patients who cannot afford the cost of treatment.
Continue to: Hydrogel urethral bulking...
Hydrogel urethral bulking
Urethral bulking agents have been used for 5 decades in the treatment of stress urinary incontinence (SUI) in women. Unlike midurethral slings, in which many medical device companies use the same implant material (microporous, monofilament polypropylene mesh), the material for bulking agents has varied greatly. A 2017 Cochrane review of urethral bulking listed these agents used for this indication: autologous fat, carbon beads, calcium hydroxylapatite, ethylene vinyl alcohol copolymer, glutaraldehyde cross-linked bovine collagen, hyaluronic acid with dextranomer, porcine dermal implant, polytetrafluoroethylene, and silicone particles.14 These agents can be injected through a transurethral or periurethral technique. The review failed to find superiority of one material or injection technique over another.
New bulking agent available
In January 2020, the FDA approved the premarket application for a new bulking agent. This new agent is a permanently implanted, nonresorbable hydrogel that consists of cross-linked polyacrylamide (2.5%) and water (97.5%). It is intended to be used with a transurethral bulking system that includes a rotatable sheath and two 23-guage needles; a total of 1.5 to 2.0 mL of the hydrogel is injected in 3 locations in the proximal urethra per session. Patients may undergo an additional 2 sessions, if needed, at least 4 weeks after the previous session.
Polyacrylamide hydrogel has been used as a bulking agent in cosmetic and ophthalmic surgery for many years, and it was first approved for medical use in Europe in 2001. The initial European data on its use as a urethral bulking agent was published in 2006.15 The first North American data came in 2014 from a multicenter, randomized trial that compared polyacrylamide hydrogel with collagen gel.16 This investigation followed 345 women for 12 months and concluded that the safety and efficacy of polyacrylamide hydrogel was not inferior to collagen, with a little over half of both cohorts demonstrating a 50% or greater decrease in incontinence episodes.
Since these initial studies, 3-year17 and 7-year safety and efficacy data18 have been reported, with reassuring findings, but both studies experienced significant attrition of the original group of patients. The most commonly reported adverse events associated with the procedure are pain at the injection site (4%–14%) and urinary tract infection (3%–7%); transient urinary retention rates range in incidence from 1.5% to 15%.19
Short procedure, long-term results
Given that a urethral bulking procedure can be done in less than 10 minutes in the office under local analgesia, this treatment may lend itself to use in more brittle patient populations. One study of women aged 80 or older showed a greater than 50% decrease in the number of daily pads used for up to 2 years after initial injection.20 Another study found the greatest treatment success in women aged 60 years or older with fewer than 2.5 episodes of SUI per day.21
Platelet-rich plasma therapy
Platelet-rich plasma (PRP) therapy has been used in multiple disciplines for more than 2 decades as a treatment to regenerate damaged tissue, particularly in sports medicine for treating tendonitis as well as in plastic surgery, gynecology, urology, and ophthalmology, and good outcomes have been demonstrated with no serious adverse effects. PRP is a natural product in which high levels of platelets are concentrated through centrifugation with bioactive growth factors, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), fibroblast growth factor (FGF), and insulin growth factor (IGF).22 The activated platelets are then injected autologously back into the patient’s tissue. This process releases activated growth factors that accelerate tissue healing by stimulating the number of reparative cells to create collagen production, angiogenesis, and neurogenesis while fighting infection and downregulating the autoimmune system.
Continue to: Uses for PRP in gynecology...
Uses for PRP in gynecology
In gynecology, dating back to 2007 PRP was shown to facilitate wound healing, when Fanning and colleagues reported PRP applications in gynecologic operative wounds, such as hysterectomies and urogynecologic procedures, to reduce postoperative pain.23 In the last decade, there has been a dramatic increasing trend in the application of PRP injections as an alternative therapy in gynecology to improve intimate health. PRP has been used to treat lichen sclerosus, atrophic vaginitis, SUI, and female sexual dysfunction; however, there is a dearth of studies that compare PRP with traditional therapies.
Runels and colleagues described the effects of localized injections of autologous PRP for the treatment of sexual dysfunction early in 2014.24 Those authors pioneered PRP use in women with dyspareunia and other symptoms related to sexual dysfunction. Women were offered PRP injections into the periurethral area of the Skene glands and the clitoris. Sexual satisfaction and pain were improved but results did not reach statistical significance. The results of this pilot study of 11 patients suggested that PRP injections could perhaps be an effective method to treat certain types of female sexual dysfunction, including desire, arousal, lubrication, and orgasm.
In another pilot study, Long and colleagues looked at the effectiveness of local injection of PRP for treating women with SUI.25 In that study, younger patients with mild severity of SUI had promising results, with up to 75% cured or improved. Results in the older group, with 50% cured or improved, did not reach statistical significance. Other small, limited studies have been conducted under the hypothesis that PRP as an “O-shot” may be a promising treatment that is a safe, effective, nonsurgical, and nonhormonal option for women with dyspareunia from lack of lubrication and related sexual dysfunction, such as decreased libido or arousal.26-29 A pilot study by Behnia-Willison and colleagues demonstrated clinical improvement in PRP use as an alternative to topical steroids for lichen sclerosus.30 Several other studies also have shown efficacy for the treatment of lichen sclerosus.31-34
More evidence of efficacy needed
To date, preliminary studies suggest that PRP holds promise for a host of gynecologic conditions. Since PRP is autologous, there are no significant contraindications, and thus far there have been no known serious adverse effects. However, most health insurers still do not cover this therapy, so for now patients must pay out-of-pocket fees for these treatments.
As we continue to investigate therapies in regenerative medicine, the continued efforts of our discipline are required to conduct well-designed prospective, randomized controlled studies. While initial series suggest that PRP is safe, it is unlikely that this therapy will be embraced widely in the paradigm as an alternative treatment option for many genitourinary symptoms of menopause and vulvar disorders until efficacy is better established.
Radiofrequency therapy
For the past 20 years, radiofrequency (RF) energy has been used through the vagina, urethra, and periurethral tissues for the treatment of genitourinary symptoms, with limited success. More recently, because some patients hesitate to receive mesh implants for treatment of urinary incontinence,35 there has been gravitation to office-based procedures.
In contrast to lasers, which transmit energy through light, RF waves (measured in hertz) transform the kinetic energy of the intracellular atoms, which move and collide, generating thermal energy.36,37 RF therapy has been shown to increase the proportion of smooth muscle and connective tissue; stimulate proliferation of the epithelium, neovascularization, and collagen formation in the lamina propria; and improve natural lubrication.36,38 In addition, RF is:
- ablative when the heat is capable of generating ablation and/or necrosis of the epidermis and dermis
- microablative when energy fractionation produces microscopic columns of ablative thermal lesions in the epidermis and upper dermis, resulting in microscopic columns of treated tissue interspersed with areas of untreated skin,39 and
- nonablative when trauma occurs only in the dermis by heating without causing ablation of the epidermis.39
The RF devices discussed below are used with settings for microablation in the treatment of SUI and sexual health/vaginal laxity, and with nonablative settings in the treatment of GSM.
RF for the treatment of urinary incontinence
Studies with RF have shown its benefits in urinary symptoms as secondary outcomes, such as improvement of SUI.38,40 One theory that favors energy devices as a treatment for SUI is that the treatment strengthens suburethral and pubocervical support, thereby decreasing urethral mobility.41
In 2016, the Viveve system (Viveve) received FDA 510(k) clearance for “use in general surgical procedures for electrocoagulation and hemostasis.” A single-site, randomized, nonblinded pilot study compared 1 treatment (group 1) versus 2 treatments (group 2) with the Viveve system for SUI in 35 participants.42 At 12 months, only for group 2 did mean scores on the Incontinence Impact Questionnaire Short Form (IIQ-7) and the International Consultation on Incontinence Modular Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI-SF) decrease by the minimum clinically important difference of 16 and 2.52 points, respectively, compared with baseline.
The ThermiVa device (ThermiGen, LLC) received FDA clearance for “use in dermatological and general surgical procedures for electrocoagulation and hemostasis” in 2017. A single-site, prospective, double-blind, randomized controlled pilot trial evaluated the efficacy of this device for the treatment of SUI in 20 participants randomly assigned in a 1:1 fashion to active and sham groups.43 At 12 weeks, mean scores of the Urogenital Distress Inventory (UDI-6) and the ICIQ-UI-SF decreased by the minimal clinically important difference only in the treatment group arm. Additionally, 70% of treatment group participants had a negative stress test at 12 weeks compared with 0% of control group participants.43 In another study of 48 patients who were followed longitudinally for 5 months, a substantial improvement in genital appearance was observed.44 Assessment based on validated instruments demonstrated significant improvements in sexual function and SUI.44
A microablative RF device (Wavetronic 6000 Touch Device, Megapulse HF FRAXX system; Loktal Medical Electronics) consists of a vaginal probe with 64 microneedles at the tip, each capable of penetrating to a depth of 1 mm. During activation, delivery of RF energy, which results in vaporization of tissue at 100 °C, occurs in a preset sequence of 8 needles at a time, preventing the overheating of intervening tissue between adjacent needles.
Slongo and colleagues conducted a 3-arm randomized clinical trial that included 117 climacteric women with SUI.45 In group 1, treatment consisted of 3 monthly sessions of RF; group 2 received 12 weekly sessions of pelvic floor muscle training (PFMT); and group 3 received RF treatment plus PFMT simultaneously. Assessments were conducted at baseline and 30 days after the end of therapy using validated questionnaires and scales for urinary, vaginal, and sexual functions, and cytology was used to assess vaginal atrophy. The association between RF and PFMT showed significant improvement in the SUI symptoms assessed by questionnaire. The vaginal symptoms and dryness showed more substantial improvement with the RF treatment, and vaginal laxity showed similar improvement in the 3 treatment groups.45
Continue to: RF for the treatment of GSM...
RF for the treatment of GSM
For women who are not candidates for localized hormone therapy, as well as others who simply do not wish to use hormones, nonablative RF laser therapy may be an alternative for the management of GSM.
The VIVEVE I trial was one of the largest randomized, sham-controlled trials performed to determine the efficacy of vaginal rejuvenation using surface-cooled RF; 174 women received either RF treatment (90 J/cm2) or sham treatment (1 J/cm2).46 Treated participants had a significant improvement in perception of vaginal laxity/looseness and sexual function up to 6 months posttreatment.46 Overall, participants were satisfied with the treatment (77.8%–100%) and reported significant improvements in vaginal laxity and symptoms of atrophy. RF was well tolerated with minimal adverse effects, such as procedure-related erythema and edema of treated tissue, and vaginal discharge. One patient discontinued treatment because of procedural pain.47,48
The ThermiVa system also was evaluated for efficacy in the treatment of GSM in a single-site, double-blind randomized controlled pilot study, the methods of which were previously described above.43 GSM symptoms were evaluated at baseline and 12 weeks using the Vaginal Health Index (VHI) and visual analog scale (VAS). At the 12-week follow-up, compared with baseline scores, VHI scores were unchanged in the control group and improved in the treatment group. Additionally, VAS scores for dyspareunia decreased in the treatment group compared with baseline while VAS for dyspareunia in the sham group did not change from baseline to 12 weeks.
RF treatment for sexual health
The efficacy of the Viveve RF system for female sexual dysfunction was evaluated in an international, randomized, controlled, single-blinded study (n = 154) that compared 6-month outcomes of RF treatment versus sham treatment.46 Although there was a statistically significant improvement in patient-reported sexual dysfunction on validated instruments, it is essential to note that the study was powered for the primary outcome of vaginal laxity. In addition, the study was not adequately powered to evaluate safety; however, the adverse events reported were mild, and the most frequently reported adverse event was vaginal discharge.
Microablative monopolar RF treatment for GSM has been evaluated in 2 single-arm clinical trials that included a total of 70 patients.39,49 Pre- and posttreatment outcomes were analyzed after delivery of 3 treatment sessions 28 to 40 days apart. Although the only significant improvement in quality of life was in the health domain of the World Health Organization Quality of Life Adapted Questionnaire (P = .04), significant improvements in sexual functioning were seen in terms of the desire (P = .002), lubrication (P = .001), satisfaction (P = .003), and pain (P = .007) domains of the Female Sexual Function Index (FSFI) questionnaire except for excitation and orgasm.39 Overall, 100% of participants reported being satisfied or very satisfied with treatments, and 13 of 14 women felt “cured” or “much better.”39 After treatment, significant increases in vaginal Lactobacillus (P<.001), decreases in vaginal pH (P<.001), improvements in maturation of vaginal cellularity (decreased parabasal cells, P<.001; increased superficial cells, P<.001), and increased VHI score (P<.001) alone occurred.49 No adverse events beyond self-limited vaginal burning and redness were reported.39,49 In another study mentioned above, the combination of RF and PFMT in sexual function does not offer benefits superior to those achieved by the therapies alone.45
Evidence on RF treatment does not support marketing efforts
Radiofrequency devices have been marketed for a variety of genitourinary problems in women, with limited high-quality, randomized, comparative evidence of efficacy and durability in the literature. It is unfortunate that RF treatment continues to be promoted by practitioners around the world who cite small, short-term studies that lack biostatistical rigor in their reporting of protocols and results. Statements from both AUGS and the International Urogynecological Association have heeded caution on the use of lasers but they could not even evaluate RF devices due to lack of evidence.2,41
Informed counseling and shared decision making remain the bottom line
By the year 2025, all members of the Baby Boom generation will be aged 60 or older. While in the past there has been a reluctance to discuss women’s sexual health, urinary incontinence, and GSM, the need for open discussion and a variety of treatment options for these conditions has never been more critical.
Many patients prefer office-based therapies over hospital-based procedures, and others are leery of synthetic implants. These concerns are leading toward great interest in the types of treatments covered in this article. However, it is paramount that clinicians are aware of the evidence-based data behind these emerging options so that we can openly and accurately counsel our patients.
As we have shown, the quality of the data behind these officed-based therapies varies significantly. Until a greater body of research data is available, we must carefully balance our desire to meet patient wishes with solid, informed counseling and shared decision making. ●
As more and more gynecologic therapies move to the outpatient setting, keeping up on the latest data regarding emerging options can be challenging. Furthermore, it can be difficult to justify purchasing expensive equipment for the office when a therapy is not covered by medical insurance plans. However, if a therapy is efficacious and patients are willing to pay out of pocket, clinicians may want to have these options available for their patients.
In an effort to work through these complex issues, a panel of experts was convened at the 47th Annual Scientific Meeting of the Society of Gynecologic Surgeons in Palm Springs, California, on June 29, 2021. This article includes the salient points from that panel discussion.
Fractionated CO2 laser therapy
Fractionated CO2 laser therapy is considered second-line therapy for the treatment of genitourinary syndrome of menopause (GSM). In 2018, the US Food and Drug Administration (FDA) issued a safety warning about the use of CO2 laser therapy and warned patients and clinicians that the FDA had not approved the treatment for vaginal rejuvenation or treatment of vaginal symptoms related to menopause, urinary incontinence, or sexual function. Despite this warning, laser treatments are still performed in many practices.
In 2019, the International Continence Society (ICS) and the International Society for the Study of Vulvovaginal Disease (ISSVD) put out a joint practice consensus statement that essentially did not recommend the routine use of laser treatment for GSM, urinary incontinence, or lichen sclerosus.1 Conversely, the 2020 American Urogynecologic Society (AUGS) published a clinical consensus statement that spoke to the promising results of laser therapy for the treatment of vulvovaginal atrophy, vaginal dryness, and menopausal dyspareunia, with benefits lasting up to 1 year.2 This statement also suggested that the short-term safety profile of the CO2 laser device was favorable.
How CO2 lasers work
Fractionated CO2 laser therapy differs from unfractionated treatment (which often is used in the treatment of condyloma) in that it is not ablative. The laser works by using fractionated beams of light to penetrate the affected tissue to create small wounds in the epithelium and underlying lamina propria, which leads to collagen remodeling and regeneration that then results in the restoration of the superficial epithelium, vaginal rugae, and lubrication.3 Most clinicians perform 3 applications of the laser treatment 6 weeks apart, a recommendation that is based on manufacturer-sponsored studies in menopausal women.
Study results of patient outcomes with laser therapy
GSM. Several retrospective4,5 and prospective studies6-10 have looked at short- and longer-term outcomes in patients undergoing treatment with the CO2 laser. All of these studies showed improvement in patient symptoms related to GSM.
The VeLVET trial, conducted by Paraiso and colleagues, was a randomized trial that compared CO2 laser treatment with vaginal estrogen in women with GSM.11 While the study was underpowered due to cessation of enrollment once the FDA safety warning was issued, the authors reported that at 6 months, both the fractionated CO2 laser therapy group and the vaginal estrogen group had similar improvements, with 70% to 80% of participants reporting satisfaction with treatment. The authors concluded that laser therapy is likely to be as efficacious as vaginal estrogen and may be a good option for patients who cannot use vaginal estrogen to treat GSM.11
Lichen sclerosus. Some data exist on the efficacy of laser therapy for the treatment of lichen sclerosus. One recently published randomized trial showed that at 6 months, fractionated CO2 laser treatment and prior treatment with high potency topical corticosteroids was associated with higher improvement in subjective symptoms and objective measures compared with clobetasol propionate treatment.12 Another trial, however, revealed that laser treatment was not an effective monotherapy treatment for lichen sclerosus when compared with placebo.13 Fewer studies have examined the effect of laser therapy on urinary incontinence.
More prospective data are emerging, evidenced by trials currently registered in ClinicalTrials.gov. While some studies provide evidence that laser therapy may be efficacious in the treatment of vulvovaginal atrophy, additional data are needed to confirm the favorable outcomes observed with laser therapy for the treatment of lichen sclerosus, and a significant amount of data are needed to evaluate the efficacy of laser treatment for urinary incontinence.
Until such evidence is available, fractionated CO2 vaginal laser therapy will remain a fee-for-service treatment option and will be inaccessible to patients who cannot afford the cost of treatment.
Continue to: Hydrogel urethral bulking...
Hydrogel urethral bulking
Urethral bulking agents have been used for 5 decades in the treatment of stress urinary incontinence (SUI) in women. Unlike midurethral slings, in which many medical device companies use the same implant material (microporous, monofilament polypropylene mesh), the material for bulking agents has varied greatly. A 2017 Cochrane review of urethral bulking listed these agents used for this indication: autologous fat, carbon beads, calcium hydroxylapatite, ethylene vinyl alcohol copolymer, glutaraldehyde cross-linked bovine collagen, hyaluronic acid with dextranomer, porcine dermal implant, polytetrafluoroethylene, and silicone particles.14 These agents can be injected through a transurethral or periurethral technique. The review failed to find superiority of one material or injection technique over another.
New bulking agent available
In January 2020, the FDA approved the premarket application for a new bulking agent. This new agent is a permanently implanted, nonresorbable hydrogel that consists of cross-linked polyacrylamide (2.5%) and water (97.5%). It is intended to be used with a transurethral bulking system that includes a rotatable sheath and two 23-guage needles; a total of 1.5 to 2.0 mL of the hydrogel is injected in 3 locations in the proximal urethra per session. Patients may undergo an additional 2 sessions, if needed, at least 4 weeks after the previous session.
Polyacrylamide hydrogel has been used as a bulking agent in cosmetic and ophthalmic surgery for many years, and it was first approved for medical use in Europe in 2001. The initial European data on its use as a urethral bulking agent was published in 2006.15 The first North American data came in 2014 from a multicenter, randomized trial that compared polyacrylamide hydrogel with collagen gel.16 This investigation followed 345 women for 12 months and concluded that the safety and efficacy of polyacrylamide hydrogel was not inferior to collagen, with a little over half of both cohorts demonstrating a 50% or greater decrease in incontinence episodes.
Since these initial studies, 3-year17 and 7-year safety and efficacy data18 have been reported, with reassuring findings, but both studies experienced significant attrition of the original group of patients. The most commonly reported adverse events associated with the procedure are pain at the injection site (4%–14%) and urinary tract infection (3%–7%); transient urinary retention rates range in incidence from 1.5% to 15%.19
Short procedure, long-term results
Given that a urethral bulking procedure can be done in less than 10 minutes in the office under local analgesia, this treatment may lend itself to use in more brittle patient populations. One study of women aged 80 or older showed a greater than 50% decrease in the number of daily pads used for up to 2 years after initial injection.20 Another study found the greatest treatment success in women aged 60 years or older with fewer than 2.5 episodes of SUI per day.21
Platelet-rich plasma therapy
Platelet-rich plasma (PRP) therapy has been used in multiple disciplines for more than 2 decades as a treatment to regenerate damaged tissue, particularly in sports medicine for treating tendonitis as well as in plastic surgery, gynecology, urology, and ophthalmology, and good outcomes have been demonstrated with no serious adverse effects. PRP is a natural product in which high levels of platelets are concentrated through centrifugation with bioactive growth factors, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), fibroblast growth factor (FGF), and insulin growth factor (IGF).22 The activated platelets are then injected autologously back into the patient’s tissue. This process releases activated growth factors that accelerate tissue healing by stimulating the number of reparative cells to create collagen production, angiogenesis, and neurogenesis while fighting infection and downregulating the autoimmune system.
Continue to: Uses for PRP in gynecology...
Uses for PRP in gynecology
In gynecology, dating back to 2007 PRP was shown to facilitate wound healing, when Fanning and colleagues reported PRP applications in gynecologic operative wounds, such as hysterectomies and urogynecologic procedures, to reduce postoperative pain.23 In the last decade, there has been a dramatic increasing trend in the application of PRP injections as an alternative therapy in gynecology to improve intimate health. PRP has been used to treat lichen sclerosus, atrophic vaginitis, SUI, and female sexual dysfunction; however, there is a dearth of studies that compare PRP with traditional therapies.
Runels and colleagues described the effects of localized injections of autologous PRP for the treatment of sexual dysfunction early in 2014.24 Those authors pioneered PRP use in women with dyspareunia and other symptoms related to sexual dysfunction. Women were offered PRP injections into the periurethral area of the Skene glands and the clitoris. Sexual satisfaction and pain were improved but results did not reach statistical significance. The results of this pilot study of 11 patients suggested that PRP injections could perhaps be an effective method to treat certain types of female sexual dysfunction, including desire, arousal, lubrication, and orgasm.
In another pilot study, Long and colleagues looked at the effectiveness of local injection of PRP for treating women with SUI.25 In that study, younger patients with mild severity of SUI had promising results, with up to 75% cured or improved. Results in the older group, with 50% cured or improved, did not reach statistical significance. Other small, limited studies have been conducted under the hypothesis that PRP as an “O-shot” may be a promising treatment that is a safe, effective, nonsurgical, and nonhormonal option for women with dyspareunia from lack of lubrication and related sexual dysfunction, such as decreased libido or arousal.26-29 A pilot study by Behnia-Willison and colleagues demonstrated clinical improvement in PRP use as an alternative to topical steroids for lichen sclerosus.30 Several other studies also have shown efficacy for the treatment of lichen sclerosus.31-34
More evidence of efficacy needed
To date, preliminary studies suggest that PRP holds promise for a host of gynecologic conditions. Since PRP is autologous, there are no significant contraindications, and thus far there have been no known serious adverse effects. However, most health insurers still do not cover this therapy, so for now patients must pay out-of-pocket fees for these treatments.
As we continue to investigate therapies in regenerative medicine, the continued efforts of our discipline are required to conduct well-designed prospective, randomized controlled studies. While initial series suggest that PRP is safe, it is unlikely that this therapy will be embraced widely in the paradigm as an alternative treatment option for many genitourinary symptoms of menopause and vulvar disorders until efficacy is better established.
Radiofrequency therapy
For the past 20 years, radiofrequency (RF) energy has been used through the vagina, urethra, and periurethral tissues for the treatment of genitourinary symptoms, with limited success. More recently, because some patients hesitate to receive mesh implants for treatment of urinary incontinence,35 there has been gravitation to office-based procedures.
In contrast to lasers, which transmit energy through light, RF waves (measured in hertz) transform the kinetic energy of the intracellular atoms, which move and collide, generating thermal energy.36,37 RF therapy has been shown to increase the proportion of smooth muscle and connective tissue; stimulate proliferation of the epithelium, neovascularization, and collagen formation in the lamina propria; and improve natural lubrication.36,38 In addition, RF is:
- ablative when the heat is capable of generating ablation and/or necrosis of the epidermis and dermis
- microablative when energy fractionation produces microscopic columns of ablative thermal lesions in the epidermis and upper dermis, resulting in microscopic columns of treated tissue interspersed with areas of untreated skin,39 and
- nonablative when trauma occurs only in the dermis by heating without causing ablation of the epidermis.39
The RF devices discussed below are used with settings for microablation in the treatment of SUI and sexual health/vaginal laxity, and with nonablative settings in the treatment of GSM.
RF for the treatment of urinary incontinence
Studies with RF have shown its benefits in urinary symptoms as secondary outcomes, such as improvement of SUI.38,40 One theory that favors energy devices as a treatment for SUI is that the treatment strengthens suburethral and pubocervical support, thereby decreasing urethral mobility.41
In 2016, the Viveve system (Viveve) received FDA 510(k) clearance for “use in general surgical procedures for electrocoagulation and hemostasis.” A single-site, randomized, nonblinded pilot study compared 1 treatment (group 1) versus 2 treatments (group 2) with the Viveve system for SUI in 35 participants.42 At 12 months, only for group 2 did mean scores on the Incontinence Impact Questionnaire Short Form (IIQ-7) and the International Consultation on Incontinence Modular Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI-SF) decrease by the minimum clinically important difference of 16 and 2.52 points, respectively, compared with baseline.
The ThermiVa device (ThermiGen, LLC) received FDA clearance for “use in dermatological and general surgical procedures for electrocoagulation and hemostasis” in 2017. A single-site, prospective, double-blind, randomized controlled pilot trial evaluated the efficacy of this device for the treatment of SUI in 20 participants randomly assigned in a 1:1 fashion to active and sham groups.43 At 12 weeks, mean scores of the Urogenital Distress Inventory (UDI-6) and the ICIQ-UI-SF decreased by the minimal clinically important difference only in the treatment group arm. Additionally, 70% of treatment group participants had a negative stress test at 12 weeks compared with 0% of control group participants.43 In another study of 48 patients who were followed longitudinally for 5 months, a substantial improvement in genital appearance was observed.44 Assessment based on validated instruments demonstrated significant improvements in sexual function and SUI.44
A microablative RF device (Wavetronic 6000 Touch Device, Megapulse HF FRAXX system; Loktal Medical Electronics) consists of a vaginal probe with 64 microneedles at the tip, each capable of penetrating to a depth of 1 mm. During activation, delivery of RF energy, which results in vaporization of tissue at 100 °C, occurs in a preset sequence of 8 needles at a time, preventing the overheating of intervening tissue between adjacent needles.
Slongo and colleagues conducted a 3-arm randomized clinical trial that included 117 climacteric women with SUI.45 In group 1, treatment consisted of 3 monthly sessions of RF; group 2 received 12 weekly sessions of pelvic floor muscle training (PFMT); and group 3 received RF treatment plus PFMT simultaneously. Assessments were conducted at baseline and 30 days after the end of therapy using validated questionnaires and scales for urinary, vaginal, and sexual functions, and cytology was used to assess vaginal atrophy. The association between RF and PFMT showed significant improvement in the SUI symptoms assessed by questionnaire. The vaginal symptoms and dryness showed more substantial improvement with the RF treatment, and vaginal laxity showed similar improvement in the 3 treatment groups.45
Continue to: RF for the treatment of GSM...
RF for the treatment of GSM
For women who are not candidates for localized hormone therapy, as well as others who simply do not wish to use hormones, nonablative RF laser therapy may be an alternative for the management of GSM.
The VIVEVE I trial was one of the largest randomized, sham-controlled trials performed to determine the efficacy of vaginal rejuvenation using surface-cooled RF; 174 women received either RF treatment (90 J/cm2) or sham treatment (1 J/cm2).46 Treated participants had a significant improvement in perception of vaginal laxity/looseness and sexual function up to 6 months posttreatment.46 Overall, participants were satisfied with the treatment (77.8%–100%) and reported significant improvements in vaginal laxity and symptoms of atrophy. RF was well tolerated with minimal adverse effects, such as procedure-related erythema and edema of treated tissue, and vaginal discharge. One patient discontinued treatment because of procedural pain.47,48
The ThermiVa system also was evaluated for efficacy in the treatment of GSM in a single-site, double-blind randomized controlled pilot study, the methods of which were previously described above.43 GSM symptoms were evaluated at baseline and 12 weeks using the Vaginal Health Index (VHI) and visual analog scale (VAS). At the 12-week follow-up, compared with baseline scores, VHI scores were unchanged in the control group and improved in the treatment group. Additionally, VAS scores for dyspareunia decreased in the treatment group compared with baseline while VAS for dyspareunia in the sham group did not change from baseline to 12 weeks.
RF treatment for sexual health
The efficacy of the Viveve RF system for female sexual dysfunction was evaluated in an international, randomized, controlled, single-blinded study (n = 154) that compared 6-month outcomes of RF treatment versus sham treatment.46 Although there was a statistically significant improvement in patient-reported sexual dysfunction on validated instruments, it is essential to note that the study was powered for the primary outcome of vaginal laxity. In addition, the study was not adequately powered to evaluate safety; however, the adverse events reported were mild, and the most frequently reported adverse event was vaginal discharge.
Microablative monopolar RF treatment for GSM has been evaluated in 2 single-arm clinical trials that included a total of 70 patients.39,49 Pre- and posttreatment outcomes were analyzed after delivery of 3 treatment sessions 28 to 40 days apart. Although the only significant improvement in quality of life was in the health domain of the World Health Organization Quality of Life Adapted Questionnaire (P = .04), significant improvements in sexual functioning were seen in terms of the desire (P = .002), lubrication (P = .001), satisfaction (P = .003), and pain (P = .007) domains of the Female Sexual Function Index (FSFI) questionnaire except for excitation and orgasm.39 Overall, 100% of participants reported being satisfied or very satisfied with treatments, and 13 of 14 women felt “cured” or “much better.”39 After treatment, significant increases in vaginal Lactobacillus (P<.001), decreases in vaginal pH (P<.001), improvements in maturation of vaginal cellularity (decreased parabasal cells, P<.001; increased superficial cells, P<.001), and increased VHI score (P<.001) alone occurred.49 No adverse events beyond self-limited vaginal burning and redness were reported.39,49 In another study mentioned above, the combination of RF and PFMT in sexual function does not offer benefits superior to those achieved by the therapies alone.45
Evidence on RF treatment does not support marketing efforts
Radiofrequency devices have been marketed for a variety of genitourinary problems in women, with limited high-quality, randomized, comparative evidence of efficacy and durability in the literature. It is unfortunate that RF treatment continues to be promoted by practitioners around the world who cite small, short-term studies that lack biostatistical rigor in their reporting of protocols and results. Statements from both AUGS and the International Urogynecological Association have heeded caution on the use of lasers but they could not even evaluate RF devices due to lack of evidence.2,41
Informed counseling and shared decision making remain the bottom line
By the year 2025, all members of the Baby Boom generation will be aged 60 or older. While in the past there has been a reluctance to discuss women’s sexual health, urinary incontinence, and GSM, the need for open discussion and a variety of treatment options for these conditions has never been more critical.
Many patients prefer office-based therapies over hospital-based procedures, and others are leery of synthetic implants. These concerns are leading toward great interest in the types of treatments covered in this article. However, it is paramount that clinicians are aware of the evidence-based data behind these emerging options so that we can openly and accurately counsel our patients.
As we have shown, the quality of the data behind these officed-based therapies varies significantly. Until a greater body of research data is available, we must carefully balance our desire to meet patient wishes with solid, informed counseling and shared decision making. ●
- Preti M, Viera-Baptista P, Digesu GA, et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: an ICS/ISSVD best practice consensus document. J Lower Genital Tract Dis. 2019;23:151-160.
- Alshiek J, Garcia B, Minassian V, et al. Vaginal energy-based devices: AUGS clinical consensus statement. Female Pelvic Med Reconstr Surg. 2020;26:287-298.
- Streicher LF. Vulvar and vaginal fractional CO2 laser treatments for genitourinary syndrome of menopause: NAMS practice pearl. Menopause. 2018;25:571-573.
- Gardner AN, Aschkenazi SO. The short-term efficacy and safety of fractional CO2 laser therapy for vulvovaginal symptoms in menopause, breast cancer, and lichen sclerosus. Menopause. 2021; 28:511-516.
- Balchander D, Nyirjesy P. Fractionated CO2 laser therapy in recalcitrant lichen sclerosus. J Lower Genital Tract Disease. 2020;24:225-228.
- Pieralli A, Fallani MG, Becorpi A, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294:841-846.
- Pieralli A, Bianchi C, Longinotti M, et al. Long-term reliability of fractionated CO2 laser as a treatment of vulvovaginal atrophy (VVA) symptoms. Arch Gynecol Obstet. 2017; 296:973-978.
- Sokol ER, Karram MM. Use of novel fractional CO2 laser for the treatment of genitourinary syndrome of menopause: 1-year outcomes. Menopause. 2017;24: 810-814.
- Pagano T, Conforti A, Buonfantino C, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. 2020;27:418-422.
- Sindou-Faurie T, Louis-Vahdat C, Oueld Es Cheikh E, et al. Evaluation of the efficacy of fractional CO2 laser in the treatment of vulvar and vaginal menopausal symptoms. Arch Gynecol Obstet. 2021;303:955-963.
- Paraiso MFR, Ferrando CA, Sokol ER, at al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET trial. Menopause. 2019;27:50-56.
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978.
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;136:979-987.
- Kirchin V, Page T, Keegan PE, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD003881.
- Lose G, Mouritsen L, Nielson JB. A new bulking agent (polyacrylamide hydrogel) for treating stress urinary incontinence in women. BJU Int. 2006;98:100-104.
- Sokol ER, Karram MM, Dmochowski R. Efficacy and safety of polyacrylamide hydrogel for the treatment of female stress incontinence: a randomized, prospective, multicenter North American study. J Urol. 2014;192:843-849.
- Pai A, Al-Singary W. Durability, safety and efficacy of polyacrylamide hydrogel (Bulkamid) in the management of stress and mixed urinary incontinence: three year follow up outcomes. Cent European J Urol. 2015;68:428-433.
- Brosche T, Kuhn A, Lobodasch K, et al. Seven-year efficacy and safety outcomes of Bulkamid for the treatment of stress urinary incontinence. Neurourol Urodyn. 2021;40:502-508.
- Kasi AD, Pergialiotis V, Perrea DN, et al. Polyacrylamide hydrogel (Bulkamid) for stress urinary incontinence in women: a systematic review of the literature. Int Urogynecol J. 2016;27:367-375.
- Vecchioli-Scaldazza CV, Smaali C, Morosetti C, et al. Polyacrylamide hydrogel (Bulkamid) in female patients of 80 or more years with urinary incontinence. Int Braz J Urol. 2014;40:37-43.
- Elmelund M, Sokol ER, Darram MM, et al. Patient characteristics that may influence the effect of urethral injection therapy for female stress urinary incontinence. J Urol. 2019;202:125-131.
- Sanoulis V, Nikolettos N, Vlahos N. The use of platelet-rich plasma in the gynecological clinical setting: a review. HJOG. 2019;18:55-65.
- Fanning J, Murrain L, Flora R, et al. Phase I/II prospective trial of autologous platelet tissue graft in gynecologic surgery. J Minim Invasive Gynecol. 2007;14:633-637.
- Runels CE, Melnick H, DeBourbon E, et al. A pilot study of the effect of localized injections of autologous platelet rich plasma (PRP) for the treatment of female sexual dysfunction. J Womens Health Care. 2014;3:4.
- Long CY, Lin KL, Shen CR, et al. A pilot study: effectiveness of local injection of autologous platelet-rich plasma in treating women with stress urinary incontinence. Sci Rep. 2021;11:1584.
- Matz EJ, Pearlman AM, Terlecki RP. Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig Clin Urol. 2018;59:61-65.
- Neto JB. O-Shot: platelets rich plasma in intimate female treatment. J Womens Health Care. 2017;6:5.
- Nikolopoulos KI, Pergialiotis V, Perrea D, et al. Restoration of the pubourethral ligament with platelet rich plasma for the treatment of stress urinary incontinence. Med Hypotheses. 2016;90:29-31.
- Hersant B, SidAhmed-Mezi M, Belkacemi Y, et al. Efficacy of injecting platelet concentrate combined with hyaluronic acid for the treatment of vulvovaginal atrophy in postmenopausal women with a history of breast cancer: a phase 2 pilot study. Menopause. 2018;25:1124-1130.
- Behnia-Willison F, Pour NR, Mohamadi B, et al. Use of platelet-rich plasma for vulvovaginal autoimmune conditions like lichen sclerosus. Plast Reconstr Surg Glob Open. 2016;4:e1124.
- Goldstein AT, King M, Runels C, et al. Intradermal injection of autologous platelet-rich plasma for the treatment of vulvar lichen sclerosus. J Am Acad Dermatol. 2017;76:158-160.
- Casabona F, Priano V, Vallerino V, et al. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plast Reconstr Surg. 2010;126:210e-211e.
- Franic D, Iternica Z, Franic-Ivanisevic M. Platelet-rich plasma (PRP) for the treatment of vulvar lichen sclerosus in a premenopausal woman: a case report. Case Rep Womens Health. 2018;18: e0062.
- Posey LK, Runels C. In office surgery and use of platelet rich plasma for the treatment of vulvar lichen sclerosus to alleviate painful sexual intercourse. J Lower Genital Tract Dis. 2017;21(4S):S14.
- Stachowicz AM, Hoover ML, Karram MM. Clinical utility of radiofrequency energy for female genitourinary dysfunction: past, present, and future. Int Urogynecol J. 2021;32:1345-1350.
- Tadir Y, Gaspar A, Lev-Sagie A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med. 2017;49:137-159.
- US Food and Drug Administration. Statement from FDA Commissioner Scott Gottlieb, MD, on efforts to safeguard women’s health from deceptive health claims and significant risks related to devices marketed for use in medical procedures for “vaginal rejuvenation.” https://www.fda.gov/news-events/pressannouncements/statement-fda-commissioner-scott-gottlieb-mdefforts-safeguard-womens-health-deceptive-health-claims. Updated August 2, 2018. Accessed August 13, 2021.
- Vicariotto F, Raichi M. Technological evolution in the radiofrequency treatment of vaginal laxity and menopausal vulvo-vaginal atrophy and other genitourinary symptoms: first experiences with a novel dynamic quadripolar device. Minerva Ginecol. 2016;68:225-236.
- Kamilos MF, Borrelli CL. New therapeutic option in genitourinary syndrome of menopause: pilot study using microablative fractional radiofrequency. Einstein (Sao Paulo). 2017;15:445-551.
- Caruth JC. Evaluation of the safety and efficacy of a novel radiofrequency device for vaginal treatment. Surg Technol Int. 2018;32:145-149.
- Shobeiri SA, Kerkhof MH, Minassian VA, et al. IUGA committee opinion: laser-based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int Urogynecol J. 2019;30:371-376.
- Allan BB, Bell S, Husarek K. Early feasibility study to evaluate the Viveve system for female stress urinary incontinence: interim 6-month report. J Womens Health (Larchmt). 2020;29:383-389.
- Leibaschoff G, Izasa PG, Cardona JL, et al. Transcutaneous temperature controlled radiofrequency (TTCRF) for the treatment of menopausal vaginal/genitourinary symptoms. Surg Technol Int. 2016;29:149-159.
- Desai SA, Vakil Z, Kroumpouzos G. Transcutaneous temperature-controlled radiofrequency treatment: improvement in female genital appearance, sexual dysfunction, and stress urinary incontinence. Aesthet Surg J. 2021;sjab174. doi: 10.1093/asj/sjab174.
- Slongo H, Lunardi AL, Riccetto CL, et al. Microablative radiofrequency versus pelvic floor muscle training for stress urinary incontinence: a randomized controlled trial. Int Urogynecol J. 2021. doi: 10.1007 /s00192-021-04758-2.
- Krychman M, Rowan CG, Allan BB, et al. Effect of single-treatment, surface-cooled radiofrequency therapy on vaginal laxity and female sexual function: the VIVEVE I randomized controlled trial. J Sex Med. 2017;14:215-225.
- Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30: 429-436.
- Juhasz ML, Korta DZ, Mesinkovska NA. Vaginal rejuvenation: a retrospective review of lasers and radiofrequency devices. Dermatol Surg. 2021;47:489-494.
- Sarmento AC, Fernandes FS, Marconi C, et al. Impact of microablative fractional radiofrequency on the vaginal health, microbiota, and cellularity of postmenopausal women. Clinics (Sao Paulo). 2020;75:e1750.
- Preti M, Viera-Baptista P, Digesu GA, et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: an ICS/ISSVD best practice consensus document. J Lower Genital Tract Dis. 2019;23:151-160.
- Alshiek J, Garcia B, Minassian V, et al. Vaginal energy-based devices: AUGS clinical consensus statement. Female Pelvic Med Reconstr Surg. 2020;26:287-298.
- Streicher LF. Vulvar and vaginal fractional CO2 laser treatments for genitourinary syndrome of menopause: NAMS practice pearl. Menopause. 2018;25:571-573.
- Gardner AN, Aschkenazi SO. The short-term efficacy and safety of fractional CO2 laser therapy for vulvovaginal symptoms in menopause, breast cancer, and lichen sclerosus. Menopause. 2021; 28:511-516.
- Balchander D, Nyirjesy P. Fractionated CO2 laser therapy in recalcitrant lichen sclerosus. J Lower Genital Tract Disease. 2020;24:225-228.
- Pieralli A, Fallani MG, Becorpi A, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294:841-846.
- Pieralli A, Bianchi C, Longinotti M, et al. Long-term reliability of fractionated CO2 laser as a treatment of vulvovaginal atrophy (VVA) symptoms. Arch Gynecol Obstet. 2017; 296:973-978.
- Sokol ER, Karram MM. Use of novel fractional CO2 laser for the treatment of genitourinary syndrome of menopause: 1-year outcomes. Menopause. 2017;24: 810-814.
- Pagano T, Conforti A, Buonfantino C, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. 2020;27:418-422.
- Sindou-Faurie T, Louis-Vahdat C, Oueld Es Cheikh E, et al. Evaluation of the efficacy of fractional CO2 laser in the treatment of vulvar and vaginal menopausal symptoms. Arch Gynecol Obstet. 2021;303:955-963.
- Paraiso MFR, Ferrando CA, Sokol ER, at al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: the VeLVET trial. Menopause. 2019;27:50-56.
- Burkett LS, Siddique M, Zeymo A, et al. Clobetasol compared with fractionated carbon dioxide laser for lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;137:968-978.
- Mitchell L, Goldstein AT, Heller D, et al. Fractionated carbon dioxide laser for the treatment of vulvar lichen sclerosus: a randomized controlled trial. Obstet Gynecol. 2021;136:979-987.
- Kirchin V, Page T, Keegan PE, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD003881.
- Lose G, Mouritsen L, Nielson JB. A new bulking agent (polyacrylamide hydrogel) for treating stress urinary incontinence in women. BJU Int. 2006;98:100-104.
- Sokol ER, Karram MM, Dmochowski R. Efficacy and safety of polyacrylamide hydrogel for the treatment of female stress incontinence: a randomized, prospective, multicenter North American study. J Urol. 2014;192:843-849.
- Pai A, Al-Singary W. Durability, safety and efficacy of polyacrylamide hydrogel (Bulkamid) in the management of stress and mixed urinary incontinence: three year follow up outcomes. Cent European J Urol. 2015;68:428-433.
- Brosche T, Kuhn A, Lobodasch K, et al. Seven-year efficacy and safety outcomes of Bulkamid for the treatment of stress urinary incontinence. Neurourol Urodyn. 2021;40:502-508.
- Kasi AD, Pergialiotis V, Perrea DN, et al. Polyacrylamide hydrogel (Bulkamid) for stress urinary incontinence in women: a systematic review of the literature. Int Urogynecol J. 2016;27:367-375.
- Vecchioli-Scaldazza CV, Smaali C, Morosetti C, et al. Polyacrylamide hydrogel (Bulkamid) in female patients of 80 or more years with urinary incontinence. Int Braz J Urol. 2014;40:37-43.
- Elmelund M, Sokol ER, Darram MM, et al. Patient characteristics that may influence the effect of urethral injection therapy for female stress urinary incontinence. J Urol. 2019;202:125-131.
- Sanoulis V, Nikolettos N, Vlahos N. The use of platelet-rich plasma in the gynecological clinical setting: a review. HJOG. 2019;18:55-65.
- Fanning J, Murrain L, Flora R, et al. Phase I/II prospective trial of autologous platelet tissue graft in gynecologic surgery. J Minim Invasive Gynecol. 2007;14:633-637.
- Runels CE, Melnick H, DeBourbon E, et al. A pilot study of the effect of localized injections of autologous platelet rich plasma (PRP) for the treatment of female sexual dysfunction. J Womens Health Care. 2014;3:4.
- Long CY, Lin KL, Shen CR, et al. A pilot study: effectiveness of local injection of autologous platelet-rich plasma in treating women with stress urinary incontinence. Sci Rep. 2021;11:1584.
- Matz EJ, Pearlman AM, Terlecki RP. Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig Clin Urol. 2018;59:61-65.
- Neto JB. O-Shot: platelets rich plasma in intimate female treatment. J Womens Health Care. 2017;6:5.
- Nikolopoulos KI, Pergialiotis V, Perrea D, et al. Restoration of the pubourethral ligament with platelet rich plasma for the treatment of stress urinary incontinence. Med Hypotheses. 2016;90:29-31.
- Hersant B, SidAhmed-Mezi M, Belkacemi Y, et al. Efficacy of injecting platelet concentrate combined with hyaluronic acid for the treatment of vulvovaginal atrophy in postmenopausal women with a history of breast cancer: a phase 2 pilot study. Menopause. 2018;25:1124-1130.
- Behnia-Willison F, Pour NR, Mohamadi B, et al. Use of platelet-rich plasma for vulvovaginal autoimmune conditions like lichen sclerosus. Plast Reconstr Surg Glob Open. 2016;4:e1124.
- Goldstein AT, King M, Runels C, et al. Intradermal injection of autologous platelet-rich plasma for the treatment of vulvar lichen sclerosus. J Am Acad Dermatol. 2017;76:158-160.
- Casabona F, Priano V, Vallerino V, et al. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plast Reconstr Surg. 2010;126:210e-211e.
- Franic D, Iternica Z, Franic-Ivanisevic M. Platelet-rich plasma (PRP) for the treatment of vulvar lichen sclerosus in a premenopausal woman: a case report. Case Rep Womens Health. 2018;18: e0062.
- Posey LK, Runels C. In office surgery and use of platelet rich plasma for the treatment of vulvar lichen sclerosus to alleviate painful sexual intercourse. J Lower Genital Tract Dis. 2017;21(4S):S14.
- Stachowicz AM, Hoover ML, Karram MM. Clinical utility of radiofrequency energy for female genitourinary dysfunction: past, present, and future. Int Urogynecol J. 2021;32:1345-1350.
- Tadir Y, Gaspar A, Lev-Sagie A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med. 2017;49:137-159.
- US Food and Drug Administration. Statement from FDA Commissioner Scott Gottlieb, MD, on efforts to safeguard women’s health from deceptive health claims and significant risks related to devices marketed for use in medical procedures for “vaginal rejuvenation.” https://www.fda.gov/news-events/pressannouncements/statement-fda-commissioner-scott-gottlieb-mdefforts-safeguard-womens-health-deceptive-health-claims. Updated August 2, 2018. Accessed August 13, 2021.
- Vicariotto F, Raichi M. Technological evolution in the radiofrequency treatment of vaginal laxity and menopausal vulvo-vaginal atrophy and other genitourinary symptoms: first experiences with a novel dynamic quadripolar device. Minerva Ginecol. 2016;68:225-236.
- Kamilos MF, Borrelli CL. New therapeutic option in genitourinary syndrome of menopause: pilot study using microablative fractional radiofrequency. Einstein (Sao Paulo). 2017;15:445-551.
- Caruth JC. Evaluation of the safety and efficacy of a novel radiofrequency device for vaginal treatment. Surg Technol Int. 2018;32:145-149.
- Shobeiri SA, Kerkhof MH, Minassian VA, et al. IUGA committee opinion: laser-based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int Urogynecol J. 2019;30:371-376.
- Allan BB, Bell S, Husarek K. Early feasibility study to evaluate the Viveve system for female stress urinary incontinence: interim 6-month report. J Womens Health (Larchmt). 2020;29:383-389.
- Leibaschoff G, Izasa PG, Cardona JL, et al. Transcutaneous temperature controlled radiofrequency (TTCRF) for the treatment of menopausal vaginal/genitourinary symptoms. Surg Technol Int. 2016;29:149-159.
- Desai SA, Vakil Z, Kroumpouzos G. Transcutaneous temperature-controlled radiofrequency treatment: improvement in female genital appearance, sexual dysfunction, and stress urinary incontinence. Aesthet Surg J. 2021;sjab174. doi: 10.1093/asj/sjab174.
- Slongo H, Lunardi AL, Riccetto CL, et al. Microablative radiofrequency versus pelvic floor muscle training for stress urinary incontinence: a randomized controlled trial. Int Urogynecol J. 2021. doi: 10.1007 /s00192-021-04758-2.
- Krychman M, Rowan CG, Allan BB, et al. Effect of single-treatment, surface-cooled radiofrequency therapy on vaginal laxity and female sexual function: the VIVEVE I randomized controlled trial. J Sex Med. 2017;14:215-225.
- Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30: 429-436.
- Juhasz ML, Korta DZ, Mesinkovska NA. Vaginal rejuvenation: a retrospective review of lasers and radiofrequency devices. Dermatol Surg. 2021;47:489-494.
- Sarmento AC, Fernandes FS, Marconi C, et al. Impact of microablative fractional radiofrequency on the vaginal health, microbiota, and cellularity of postmenopausal women. Clinics (Sao Paulo). 2020;75:e1750.
A multidisciplinary approach to gyn care: A single center’s experience
In her book The Silo Effect: The Peril of Expertise and the Promise of Breaking Down Barriers, Gillian Tett wrote that “the word ‘silo’ does not just refer to a physical structure or organization (such as a department). It can also be a state of mind. Silos exist in structures. But they exist in our minds and social groups too. Silos breed tribalism. But they can also go hand in hand with tunnel vision.”
Tertiary care referral centers seem to be trending toward being more and more “un-siloed” and collaborative within their own departments and between departments in order to care for patients. The terms multidisciplinary and intradisciplinary have become popular in medicine, and teams are joining forces to create care paths for patients that are intended to improve the efficiency of and the quality of care that is rendered. There is no better example of the move to improve collaboration in medicine than the theme of the 2021 Society of Gynecologic Surgeons annual meeting, “Working Together: How Collaboration Enables Us to Better Help Our Patients.”
In this article, we provide examples of how collaborating with other specialties—within and outside of an ObGyn department—should become the standard of care. We discuss how to make this team approach easier and provide evidence that patients experience favorable outcomes. While data on combined care remain sparse, the existing literature on this topic helps us to guide and counsel patients about what to expect when a combined approach is taken.
Addressing pelvic floor disorders in women with gynecologic malignancy
In 2018, authors of a systematic review that looked at concurrent pelvic floor disorders in gynecologic oncologic survivors found that the prevalence of these disorders was high enough to warrant evaluation and management of these conditions to help improve quality of life for patients.1 Furthermore, it is possible that the prevalence of urinary incontinence is higher in patients who have undergone surgery for a gynecologic malignancy compared with controls, which has been reported in previous studies.2,3 At Cleveland Clinic, we recognize the need to evaluate our patients receiving oncologic care for urinary, fecal, and pelvic organ prolapse symptoms. Our oncologists routinely inquire about these symptoms once their patients have undergone surgery with them, and they make referrals for all their symptomatic patients. They have even learned about our own counseling, and they pre-emptively let patients know what our counseling may encompass.
For instance, many patients who received radiation therapy have stress urinary incontinence that is likely related to a hypomobile urethra, and they may benefit more from transurethral bulking than an anti-incontinence procedure in the operating room. Reassuring patients ahead of time that they do not need major interventions for their symptoms is helpful, as these patients are already experiencing tremendous burden from their oncologic conditions. We have made our referral patterns easy for these patients, and most patients are seen within days to weeks of the referral placed, depending on the urgency of the consult and the need to proceed with their oncologic treatment plan.
Gynecologic oncology patients who present with preoperative stress urinary incontinence and pelvic organ prolapse also are referred to a urogynecology specialist for concurrent care. Care paths have been created to help inform both the urogynecologists and the oncologists about options for patients depending on their respective conditions, as both their malignancy and their pelvic floor disorder(s) are considered in treatment planning. There is agreement in this planning that the oncologic surgery takes priority, and the urogynecologic approach is based on the oncologic plan.
Our urogynecologists routinely ask if future radiation is in the treatment plan, as this usually precludes us from placing a midurethral sling at the time of any surgery. Surgical approach (vaginal versus abdominal; open or minimally invasive) also is determined by the oncologic team. At the time of surgery, patient positioning is considered to optimize access for all of the surgeons. For instance, having the oncologist know that the patient needs to be far down on the bed as their steep Trendelenburg positioning during laparoscopy or robotic surgery may cause the patient to slide cephalad during the case may make a vaginal repair or sling placement at the end of the case challenging. All these small nuances are important, and a collaborative team develops the right plan for each patient in advance.
Data on the outcomes of combined surgery are sparse. In a retrospective matched cohort study, our group compared outcomes in women who underwent concurrent surgery with those who underwent urogynecologic surgery alone.4 We found that concurrent surgeries had an increased incidence of minor but not serious perioperative adverse events. Importantly, we determined that 1 in 10 planned urogynecologic procedures needed to be either modified or abandoned as a result of the oncologic plan. These data help guide our counseling, and both the oncologist and urogynecologist contributing to the combined case counsel patients according to these data.
Continue to: Concurrent colorectal and gynecologic surgery...
Concurrent colorectal and gynecologic surgery
Many women have pelvic floor disorders. As gynecologists, we often compartmentalize these conditions as gynecologic problems; frequently, however, colorectal conditions are at play as well and should be addressed concurrently. For instance, a high incidence of anorectal dysfunction occurs in women who present with pelvic organ prolapse.5 Furthermore, outlet defecation disorders are not always a result of a straightforward rectocele that can be fixed vaginally. Sometimes, a more thorough evaluation is warranted depending on the patient’s concurrent symptoms and history. Outlet symptoms may be attributed to large enteroceles, sigmoidoceles, perineal descent, rectal intussusception, and rectal prolapse.6
As a result, a combined approach to caring for patients with complex pelvic floor disorders is optimal. Several studies describe this type of combined and coordinated patient care.7,8 Ideally, patients are seen by both surgeons in the office so that the surgeons may make a combined plan for their care, especially if the decision is made to proceed with surgery. Urogynecology specialists and colorectal surgeons must decide together whether to approach combined prolapse procedures via a perineal and vaginal approach versus an abdominal approach. Several factors can determine this, including surgeon experience and preference, which is why it is important for surgeons working together to have either well-designed care paths or simply open communication and experience working together for the conditions they are treating.
In an ideal coordinated care approach, both surgeons review the patient records in advance. Any needed imaging or testing is done before the official patient consult; the patient is then seen by both clinicians in the same visit and counseled about the options. This is the most efficient and effective way to see patients, and we have had significant success using this approach.
Complications of combined surgery
The safety of combining procedures such as laparoscopic sacrocolpopexy and concurrent rectopexy has been studied, and intraoperative complications have been reported to be low.9,10 In a cohort study, Wallace and colleagues looked at postoperative outcomes and complications following combined surgery and reported that reoperation for the rectal prolapse component of the surgery was more common than the pelvic organ prolapse component, and that 1 in 5 of their patients experienced a surgical complication within 30 days of their surgery.11 This incidence is higher than that seen with isolated pelvic organ prolapse surgery. These data help us understand that a combined approach requires good patient counseling in the office about both the need for repeat surgery in certain circumstances and the increased risk of complications. Further, combined perineal and vaginal approaches have been compared with abdominal approaches and also have shown no age-adjusted differences in outcomes and complications.12
These data point to the need for surgeons to choose the approach to surgery that best fits their own experiences and to discuss this together before counseling the patient in the office, thus streamlining the effort so that the patient feels comfortable under the care of 2 surgeons.
Patients presenting with urogynecologic and gynecologic conditions also report symptomatic hemorrhoids, and colorectal referral is often made by the gynecologist. Sparse data are available regarding combined approaches to managing hemorrhoids and gynecologic conditions. Our group was the first to publish on outcomes and complications in patients undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery.13 In that retrospective cohort, we found that minor complications, such as postoperative urinary tract infection and transient voiding dysfunction, was more common in patients who underwent combined surgery. From this, we gathered that there is a need to counsel patients appropriately about the risk of combined surgery. That said, for some patients, coordinated care is desirable, and surgeons should make the effort to work together in combining their procedures.
Continue to: Integrating plastic and reconstructive surgery in gynecology...
Integrating plastic and reconstructive surgery in gynecology
Reconstructive gynecologic procedures often require a multidisciplinary approach to what can be very complex reconstructive surgery. The intended goal usually is to achieve a good cosmetic result in the genital area, as well as to restore sexual, defecatory, and/or genitourinary functionality. As a result, surgeons must work together to develop a feasible reconstructive plan for these patients.
Women experience vaginal stenosis or foreshortening for a number of reasons. Women with congenital anomalies often are cared for by specialists in pediatric and adolescent gynecology. Other women, such as those who have undergone vaginectomy and/or pelvic or vaginal radiation for cancer treatment, complications from vaginal mesh placement, and severe vaginal scarring from dermatologic conditions like lichen planus, are cared for by other gynecologic specialists, often general gynecologists or urogynecologists. In some of these cases, a gynecologic surgeon can perform vaginal adhesiolysis followed by vaginal estrogen treatment (when appropriate) and aggressive postoperative vaginal dilation with adjunctive pelvic floor physical therapy as well as sex therapy or counseling. A simple reconstructive approach may be necessary if lysis of adhesions alone is not sufficient. Sometimes, the vaginal apex must be opened vaginally or abdominally, or releasing incisions need to be made to improve the caliber of the vagina in addition to its length. Under these circumstances, the use of additional local skin grafts, local peritoneal flaps, or biologic grafts or xenografts can help achieve a satisfying result. While not all gynecologists are trained to perform these procedures, some are, and certainly gynecologic subspecialists have the skill sets to care for these patients.
Under other circumstances, when the vagina is truly foreshortened, more aggressive reconstructive surgery is necessary and consultation and collaboration with plastic surgery specialists often is helpful. At our center, these patients’ care is initially managed by gynecologists and, when simple approaches to their reconstructive needs are exhausted, collaboration is warranted. As with the other team approaches discussed in this article, the recommendation is for a consistent referral team that has established care paths for patients. Not all plastic surgeons are familiar with neovaginal reconstruction and understand the functional aspects that gynecologists are hoping to achieve for their patients. Therefore, it is important to form cohesive teams that have the same goals for the patient.
The literature on neovaginal reconstruction is sparse. There are no true agreed on approaches or techniques for vaginal reconstruction because there is no “one size fits all” for these repairs. Defects also vary depending on whether they are due to resections or radiation for oncologic treatment, reconstruction as part of the repair of a genitourinary or rectovaginal fistula, or stenosis from other etiologies.
In 2002, Cordeiro and colleagues published a classification system and reconstructive algorithm for acquired vaginal defects.14 Not all reconstructive surgeons subscribe to this algorithm, but it is the only rubric that currently exists. The authors differentiate between “partial” and “circumferential” defects and recommend different types of fasciocutaneous and myocutaneous flaps for reconstruction.
In our experience at our center, we believe that the choice of flap should also depend on whether or not perineal reconstruction is needed. This decision is made by both the gynecologic specialist and the plastic surgeon. Common flap choices include the Singapore flap, a fasciocutaneous flap based on perforators from the pudendal vessels; the gracilis flap, a myocutaneous flap based off the medial circumflex femoral vessels; and the rectus abdominis flap (transverse or vertical), which is also a myocutaneous flap that relies on the blood supply from the deep inferior epigastric vessels.
One of the most important parts of the coordinated effort of neovaginal surgery is postoperative care. Plastic surgeons play a key role in ensuring that the flap survives in the immediate postoperative period. The gynecology team should be responsible for postoperative vaginal dilation teaching and follow-up to ensure that the patient dilates properly and upsizes her dilator appropriately over the postoperative period. In our practice, our advanced practice clinicians often care for these patients and are responsible for continuity and dilation teaching. Patients have easy access to these clinicians, and this enhances the postoperative experience. Referral to a pelvic floor physical therapist knowledgeable about neovaginal surgery also helps to ensure that the dilation process goes successfully. It also helps to have office days on the same days as the plastic surgery team that is following the patient. This way, the patient may be seen by both teams on the same day. This allows for good patient communication with regard to aftercare, as well as a combined approach to teaching the trainees involved in the case. Coordination with pelvic floor physical therapists on those days also enhances the patient experience and is highly recommended.
Continue to: Combining gyn and urogyn procedures with plastic surgery...
Combining gyn and urogyn procedures with plastic surgery
While there are no data on combining gynecologic and urogynecologic procedures with plastic reconstructive surgeries, a team approach to combining surgeries is possible. At our center, we have performed tubal ligation, ovarian surgery, hysterectomy, and sling and prolapse surgery in patients who were undergoing cosmetic procedures, such as breast augmentation and abdominoplasty.
Gender affirmation surgery also can be performed through a combined approach between gynecologists and plastic surgeons. Our gynecologists perform hysterectomy for transmasculine men, and this procedure is sometimes safely and effectively performed in combination with masculinizing chest surgery (mastectomy) performed by our plastic surgeons. Vaginoplasty surgery (feminizing genital surgery) also is performed by urogynecology specialists at our center, and it is sometimes done concurrently at the time of breast augmentation and/or facial feminization surgery.
Case order. Some plastic surgeons vocalize concerns about combining clean procedures with clean contaminated cases, especially in situations in which implants are being placed in the body. During these cases, communication and organization between surgeons is important. For instance, there should be a discussion about case order. In general, the clean procedures should be performed first. In addition, separate operating tables and instruments should be used. Simultaneous operating also should be avoided. Fresh incisions should be dressed and covered before subsequent procedures are performed.
Incision placement. Last, planning around incision placement should be discussed before each case. Laparoscopic and abdominal incisions may interfere with plastic surgery procedures and alter the end cosmesis. These incisions often can be incorporated into the reconstructive procedure. The most important part of the coordinated surgical effort is ensuring that both surgical teams understand each other’s respective surgeries and the approach needed to complete them. When this is achieved, the cases are usually very successful.
Creating collaboration between obstetricians and gynecologic specialists
The impacts of pregnancy and vaginal delivery on the pelvic floor are well established. Urinary and fecal incontinence, pelvic organ prolapse, perineal pain, and dyspareunia are not uncommon in the postpartum period and may persist long term. The effects of obstetric anal sphincter injury (OASI) are significant, with up to 25% of women experiencing wound complications and 17% experiencing fecal incontinence at 6 months postpartum.15,16 Care of women with peripartum pelvic floor disorders and OASIs present an ideal opportunity for collaboration between urogynecologists and obstetricians. The Cleveland Clinic has a multidisciplinary Postpartum Care Clinic (PPCC) where we provide specialized, collaborative care for women with peripartum pelvic floor disorders and complex obstetric lacerations.
Our PPCC accepts referrals up to 1 year postpartum for women who experience OASI, urinary or fecal incontinence, perineal pain or dyspareunia, voiding dysfunction or urinary retention, and wound healing complications. When a woman is diagnosed with an OASI at the time of delivery, a “best practice alert” is released in the medical record recommending a referral to the PPCC to encourage referral of all women with OASI. We strive to see all referrals within 2 weeks of delivery.
At the time of the initial consultation, we collect validated questionnaires on bowel and bladder function, assess pain and healing, and discuss future delivery planning. The success of the PPCC is rooted in communication. When the clinic first opened, we provided education to our obstetrics colleagues on the purpose of the clinic, when and how to refer, and what to expect from our consultations. Open communication between referring obstetric clinicians and the urogynecologists that run the PPCC is key in providing collaborative care where patients know that their clinicians are working as a team. All recommendations are communicated to referring clinicians, and all women are ultimately referred back to their primary clinician for long-term care. Evidence demonstrates that this type of clinic leads to high obstetric clinician satisfaction and increased awareness of OASIs and their impact on maternal health.17
Combined team approach fosters innovation in patient care
A combined approach to the care of the patient who presents with gynecologic conditions is optimal. In this article, we presented examples of care that integrates gynecology, urogynecology, gynecologic oncology, colorectal surgery, plastic surgery, and obstetrics. There are, however, many more existing examples as well as opportunities to create teams that really make a difference in the way patients receive—and perceive—their care. This is a good starting point, and we should strive to use this model to continue to innovate our approach to patient care.
- Ramaseshan AS, Felton J, Roque D, et al. Pelvic floor disorders in women with gynecologic malignancies: a systematic review. Int Urogynecol J. 2018;29:459-476.
- Nakayama N, Tsuji T, Aoyama M, et al. Quality of life and the prevalence of urinary incontinence after surgical treatment for gynecologic cancer: a questionnaire survey. BMC Womens Health. 2020;20:148-157.
- Cascales-Campos PA, Gonzalez-Gil A, Fernandez-Luna E, et al. Urinary and fecal incontinence in patients with advanced ovarian cancer treated with CRS + HIPEC. Surg Oncol. 2021;36:115-119.
- Davidson ER, Woodburn K, AlHilli M, et al. Perioperative adverse events in women undergoing concurrent urogynecologic and gynecologic oncology surgeries for suspected malignancy. Int Urogynecol J. 2019;30:1195-1201.
- Spence-Jones C, Kamm MA, Henry MM, et al. Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and stress urinary incontinence. Br J Obstet Gynaecol. 1994;101:147-152.
- Thompson JR, Chen AH, Pettit PD, et al. Incidence of occult rectal prolapse in patients with clinical rectoceles and defecatory dysfunction. Am J Obstet Gynecol. 2002;187:1494-1500.
- Jallad K, Gurland B. Multidisciplinary approach to the treatment of concomitant rectal and vaginal prolapse. Clin Colon Rectal Surg. 2016;29:101-105.
- Kapoor DS, Sultan AH, Thakar R, et al. Management of complex pelvic floor disorders in a multidisciplinary pelvic floor clinic. Colorectal Dis. 2008;10:118-123.
- Weinberg D, Qeadan F, McKee R, et al. Safety of laparoscopic sacrocolpopexy with concurrent rectopexy: peri-operative morbidity in a nationwide cohort. Int Urogynecol J. 2019;30:385-392.
- Geltzeiler CB, Birnbaum EH, Silviera ML, et al. Combined rectopexy and sacrocolpopexy is safe for correction of pelvic organ prolapse. Int J Colorectal Dis. 2018;33:1453-1459.
- Wallace SL, Syan R, Enemchukwu EA, et al. Surgical approach, complications, and reoperation rates of combined rectal and pelvic organ prolapse surgery. Int Urogynecol J. 2020;31:2101-2108.
- Smith PE, Hade EM, Pandya LK, et al. Perioperative outcomes for combined ventral rectopexy with sacrocolpopexy compared to perineal rectopexy with vaginal apical suspension. Female Pelvic Med Reconstr Surg. 2020;26:376-381.
- Casas-Puig V, Bretschneider CE, Ferrando CA. Perioperative adverse events in women undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery. Female Pelvic Med Reconstr Surg. 2019;25:88-92.
- Cordeiro PG, Pusic AL, Disa JJ. A classification system and reconstructive algorithm for acquired vaginal defects. Plast Reconstr Surg. 2002;110:1058-1065.
- Lewicky-Gaupp C, Leader-Cramer A, Johnson LL, et al. Wound complications after obstetric anal sphincter injuries. Obstet Gynecol. 2015;125:1088-1093.
- Borello-France D, Burgio KL, Richter HE, et al; Pelvic Floor Disorders Network. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006;108:863-872.
- Propst K, Hickman LC. Peripartum pelvic floor disorder clinics inform obstetric provider practices. Int Urogynecol J. 2021;32:1793-1799.
In her book The Silo Effect: The Peril of Expertise and the Promise of Breaking Down Barriers, Gillian Tett wrote that “the word ‘silo’ does not just refer to a physical structure or organization (such as a department). It can also be a state of mind. Silos exist in structures. But they exist in our minds and social groups too. Silos breed tribalism. But they can also go hand in hand with tunnel vision.”
Tertiary care referral centers seem to be trending toward being more and more “un-siloed” and collaborative within their own departments and between departments in order to care for patients. The terms multidisciplinary and intradisciplinary have become popular in medicine, and teams are joining forces to create care paths for patients that are intended to improve the efficiency of and the quality of care that is rendered. There is no better example of the move to improve collaboration in medicine than the theme of the 2021 Society of Gynecologic Surgeons annual meeting, “Working Together: How Collaboration Enables Us to Better Help Our Patients.”
In this article, we provide examples of how collaborating with other specialties—within and outside of an ObGyn department—should become the standard of care. We discuss how to make this team approach easier and provide evidence that patients experience favorable outcomes. While data on combined care remain sparse, the existing literature on this topic helps us to guide and counsel patients about what to expect when a combined approach is taken.
Addressing pelvic floor disorders in women with gynecologic malignancy
In 2018, authors of a systematic review that looked at concurrent pelvic floor disorders in gynecologic oncologic survivors found that the prevalence of these disorders was high enough to warrant evaluation and management of these conditions to help improve quality of life for patients.1 Furthermore, it is possible that the prevalence of urinary incontinence is higher in patients who have undergone surgery for a gynecologic malignancy compared with controls, which has been reported in previous studies.2,3 At Cleveland Clinic, we recognize the need to evaluate our patients receiving oncologic care for urinary, fecal, and pelvic organ prolapse symptoms. Our oncologists routinely inquire about these symptoms once their patients have undergone surgery with them, and they make referrals for all their symptomatic patients. They have even learned about our own counseling, and they pre-emptively let patients know what our counseling may encompass.
For instance, many patients who received radiation therapy have stress urinary incontinence that is likely related to a hypomobile urethra, and they may benefit more from transurethral bulking than an anti-incontinence procedure in the operating room. Reassuring patients ahead of time that they do not need major interventions for their symptoms is helpful, as these patients are already experiencing tremendous burden from their oncologic conditions. We have made our referral patterns easy for these patients, and most patients are seen within days to weeks of the referral placed, depending on the urgency of the consult and the need to proceed with their oncologic treatment plan.
Gynecologic oncology patients who present with preoperative stress urinary incontinence and pelvic organ prolapse also are referred to a urogynecology specialist for concurrent care. Care paths have been created to help inform both the urogynecologists and the oncologists about options for patients depending on their respective conditions, as both their malignancy and their pelvic floor disorder(s) are considered in treatment planning. There is agreement in this planning that the oncologic surgery takes priority, and the urogynecologic approach is based on the oncologic plan.
Our urogynecologists routinely ask if future radiation is in the treatment plan, as this usually precludes us from placing a midurethral sling at the time of any surgery. Surgical approach (vaginal versus abdominal; open or minimally invasive) also is determined by the oncologic team. At the time of surgery, patient positioning is considered to optimize access for all of the surgeons. For instance, having the oncologist know that the patient needs to be far down on the bed as their steep Trendelenburg positioning during laparoscopy or robotic surgery may cause the patient to slide cephalad during the case may make a vaginal repair or sling placement at the end of the case challenging. All these small nuances are important, and a collaborative team develops the right plan for each patient in advance.
Data on the outcomes of combined surgery are sparse. In a retrospective matched cohort study, our group compared outcomes in women who underwent concurrent surgery with those who underwent urogynecologic surgery alone.4 We found that concurrent surgeries had an increased incidence of minor but not serious perioperative adverse events. Importantly, we determined that 1 in 10 planned urogynecologic procedures needed to be either modified or abandoned as a result of the oncologic plan. These data help guide our counseling, and both the oncologist and urogynecologist contributing to the combined case counsel patients according to these data.
Continue to: Concurrent colorectal and gynecologic surgery...
Concurrent colorectal and gynecologic surgery
Many women have pelvic floor disorders. As gynecologists, we often compartmentalize these conditions as gynecologic problems; frequently, however, colorectal conditions are at play as well and should be addressed concurrently. For instance, a high incidence of anorectal dysfunction occurs in women who present with pelvic organ prolapse.5 Furthermore, outlet defecation disorders are not always a result of a straightforward rectocele that can be fixed vaginally. Sometimes, a more thorough evaluation is warranted depending on the patient’s concurrent symptoms and history. Outlet symptoms may be attributed to large enteroceles, sigmoidoceles, perineal descent, rectal intussusception, and rectal prolapse.6
As a result, a combined approach to caring for patients with complex pelvic floor disorders is optimal. Several studies describe this type of combined and coordinated patient care.7,8 Ideally, patients are seen by both surgeons in the office so that the surgeons may make a combined plan for their care, especially if the decision is made to proceed with surgery. Urogynecology specialists and colorectal surgeons must decide together whether to approach combined prolapse procedures via a perineal and vaginal approach versus an abdominal approach. Several factors can determine this, including surgeon experience and preference, which is why it is important for surgeons working together to have either well-designed care paths or simply open communication and experience working together for the conditions they are treating.
In an ideal coordinated care approach, both surgeons review the patient records in advance. Any needed imaging or testing is done before the official patient consult; the patient is then seen by both clinicians in the same visit and counseled about the options. This is the most efficient and effective way to see patients, and we have had significant success using this approach.
Complications of combined surgery
The safety of combining procedures such as laparoscopic sacrocolpopexy and concurrent rectopexy has been studied, and intraoperative complications have been reported to be low.9,10 In a cohort study, Wallace and colleagues looked at postoperative outcomes and complications following combined surgery and reported that reoperation for the rectal prolapse component of the surgery was more common than the pelvic organ prolapse component, and that 1 in 5 of their patients experienced a surgical complication within 30 days of their surgery.11 This incidence is higher than that seen with isolated pelvic organ prolapse surgery. These data help us understand that a combined approach requires good patient counseling in the office about both the need for repeat surgery in certain circumstances and the increased risk of complications. Further, combined perineal and vaginal approaches have been compared with abdominal approaches and also have shown no age-adjusted differences in outcomes and complications.12
These data point to the need for surgeons to choose the approach to surgery that best fits their own experiences and to discuss this together before counseling the patient in the office, thus streamlining the effort so that the patient feels comfortable under the care of 2 surgeons.
Patients presenting with urogynecologic and gynecologic conditions also report symptomatic hemorrhoids, and colorectal referral is often made by the gynecologist. Sparse data are available regarding combined approaches to managing hemorrhoids and gynecologic conditions. Our group was the first to publish on outcomes and complications in patients undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery.13 In that retrospective cohort, we found that minor complications, such as postoperative urinary tract infection and transient voiding dysfunction, was more common in patients who underwent combined surgery. From this, we gathered that there is a need to counsel patients appropriately about the risk of combined surgery. That said, for some patients, coordinated care is desirable, and surgeons should make the effort to work together in combining their procedures.
Continue to: Integrating plastic and reconstructive surgery in gynecology...
Integrating plastic and reconstructive surgery in gynecology
Reconstructive gynecologic procedures often require a multidisciplinary approach to what can be very complex reconstructive surgery. The intended goal usually is to achieve a good cosmetic result in the genital area, as well as to restore sexual, defecatory, and/or genitourinary functionality. As a result, surgeons must work together to develop a feasible reconstructive plan for these patients.
Women experience vaginal stenosis or foreshortening for a number of reasons. Women with congenital anomalies often are cared for by specialists in pediatric and adolescent gynecology. Other women, such as those who have undergone vaginectomy and/or pelvic or vaginal radiation for cancer treatment, complications from vaginal mesh placement, and severe vaginal scarring from dermatologic conditions like lichen planus, are cared for by other gynecologic specialists, often general gynecologists or urogynecologists. In some of these cases, a gynecologic surgeon can perform vaginal adhesiolysis followed by vaginal estrogen treatment (when appropriate) and aggressive postoperative vaginal dilation with adjunctive pelvic floor physical therapy as well as sex therapy or counseling. A simple reconstructive approach may be necessary if lysis of adhesions alone is not sufficient. Sometimes, the vaginal apex must be opened vaginally or abdominally, or releasing incisions need to be made to improve the caliber of the vagina in addition to its length. Under these circumstances, the use of additional local skin grafts, local peritoneal flaps, or biologic grafts or xenografts can help achieve a satisfying result. While not all gynecologists are trained to perform these procedures, some are, and certainly gynecologic subspecialists have the skill sets to care for these patients.
Under other circumstances, when the vagina is truly foreshortened, more aggressive reconstructive surgery is necessary and consultation and collaboration with plastic surgery specialists often is helpful. At our center, these patients’ care is initially managed by gynecologists and, when simple approaches to their reconstructive needs are exhausted, collaboration is warranted. As with the other team approaches discussed in this article, the recommendation is for a consistent referral team that has established care paths for patients. Not all plastic surgeons are familiar with neovaginal reconstruction and understand the functional aspects that gynecologists are hoping to achieve for their patients. Therefore, it is important to form cohesive teams that have the same goals for the patient.
The literature on neovaginal reconstruction is sparse. There are no true agreed on approaches or techniques for vaginal reconstruction because there is no “one size fits all” for these repairs. Defects also vary depending on whether they are due to resections or radiation for oncologic treatment, reconstruction as part of the repair of a genitourinary or rectovaginal fistula, or stenosis from other etiologies.
In 2002, Cordeiro and colleagues published a classification system and reconstructive algorithm for acquired vaginal defects.14 Not all reconstructive surgeons subscribe to this algorithm, but it is the only rubric that currently exists. The authors differentiate between “partial” and “circumferential” defects and recommend different types of fasciocutaneous and myocutaneous flaps for reconstruction.
In our experience at our center, we believe that the choice of flap should also depend on whether or not perineal reconstruction is needed. This decision is made by both the gynecologic specialist and the plastic surgeon. Common flap choices include the Singapore flap, a fasciocutaneous flap based on perforators from the pudendal vessels; the gracilis flap, a myocutaneous flap based off the medial circumflex femoral vessels; and the rectus abdominis flap (transverse or vertical), which is also a myocutaneous flap that relies on the blood supply from the deep inferior epigastric vessels.
One of the most important parts of the coordinated effort of neovaginal surgery is postoperative care. Plastic surgeons play a key role in ensuring that the flap survives in the immediate postoperative period. The gynecology team should be responsible for postoperative vaginal dilation teaching and follow-up to ensure that the patient dilates properly and upsizes her dilator appropriately over the postoperative period. In our practice, our advanced practice clinicians often care for these patients and are responsible for continuity and dilation teaching. Patients have easy access to these clinicians, and this enhances the postoperative experience. Referral to a pelvic floor physical therapist knowledgeable about neovaginal surgery also helps to ensure that the dilation process goes successfully. It also helps to have office days on the same days as the plastic surgery team that is following the patient. This way, the patient may be seen by both teams on the same day. This allows for good patient communication with regard to aftercare, as well as a combined approach to teaching the trainees involved in the case. Coordination with pelvic floor physical therapists on those days also enhances the patient experience and is highly recommended.
Continue to: Combining gyn and urogyn procedures with plastic surgery...
Combining gyn and urogyn procedures with plastic surgery
While there are no data on combining gynecologic and urogynecologic procedures with plastic reconstructive surgeries, a team approach to combining surgeries is possible. At our center, we have performed tubal ligation, ovarian surgery, hysterectomy, and sling and prolapse surgery in patients who were undergoing cosmetic procedures, such as breast augmentation and abdominoplasty.
Gender affirmation surgery also can be performed through a combined approach between gynecologists and plastic surgeons. Our gynecologists perform hysterectomy for transmasculine men, and this procedure is sometimes safely and effectively performed in combination with masculinizing chest surgery (mastectomy) performed by our plastic surgeons. Vaginoplasty surgery (feminizing genital surgery) also is performed by urogynecology specialists at our center, and it is sometimes done concurrently at the time of breast augmentation and/or facial feminization surgery.
Case order. Some plastic surgeons vocalize concerns about combining clean procedures with clean contaminated cases, especially in situations in which implants are being placed in the body. During these cases, communication and organization between surgeons is important. For instance, there should be a discussion about case order. In general, the clean procedures should be performed first. In addition, separate operating tables and instruments should be used. Simultaneous operating also should be avoided. Fresh incisions should be dressed and covered before subsequent procedures are performed.
Incision placement. Last, planning around incision placement should be discussed before each case. Laparoscopic and abdominal incisions may interfere with plastic surgery procedures and alter the end cosmesis. These incisions often can be incorporated into the reconstructive procedure. The most important part of the coordinated surgical effort is ensuring that both surgical teams understand each other’s respective surgeries and the approach needed to complete them. When this is achieved, the cases are usually very successful.
Creating collaboration between obstetricians and gynecologic specialists
The impacts of pregnancy and vaginal delivery on the pelvic floor are well established. Urinary and fecal incontinence, pelvic organ prolapse, perineal pain, and dyspareunia are not uncommon in the postpartum period and may persist long term. The effects of obstetric anal sphincter injury (OASI) are significant, with up to 25% of women experiencing wound complications and 17% experiencing fecal incontinence at 6 months postpartum.15,16 Care of women with peripartum pelvic floor disorders and OASIs present an ideal opportunity for collaboration between urogynecologists and obstetricians. The Cleveland Clinic has a multidisciplinary Postpartum Care Clinic (PPCC) where we provide specialized, collaborative care for women with peripartum pelvic floor disorders and complex obstetric lacerations.
Our PPCC accepts referrals up to 1 year postpartum for women who experience OASI, urinary or fecal incontinence, perineal pain or dyspareunia, voiding dysfunction or urinary retention, and wound healing complications. When a woman is diagnosed with an OASI at the time of delivery, a “best practice alert” is released in the medical record recommending a referral to the PPCC to encourage referral of all women with OASI. We strive to see all referrals within 2 weeks of delivery.
At the time of the initial consultation, we collect validated questionnaires on bowel and bladder function, assess pain and healing, and discuss future delivery planning. The success of the PPCC is rooted in communication. When the clinic first opened, we provided education to our obstetrics colleagues on the purpose of the clinic, when and how to refer, and what to expect from our consultations. Open communication between referring obstetric clinicians and the urogynecologists that run the PPCC is key in providing collaborative care where patients know that their clinicians are working as a team. All recommendations are communicated to referring clinicians, and all women are ultimately referred back to their primary clinician for long-term care. Evidence demonstrates that this type of clinic leads to high obstetric clinician satisfaction and increased awareness of OASIs and their impact on maternal health.17
Combined team approach fosters innovation in patient care
A combined approach to the care of the patient who presents with gynecologic conditions is optimal. In this article, we presented examples of care that integrates gynecology, urogynecology, gynecologic oncology, colorectal surgery, plastic surgery, and obstetrics. There are, however, many more existing examples as well as opportunities to create teams that really make a difference in the way patients receive—and perceive—their care. This is a good starting point, and we should strive to use this model to continue to innovate our approach to patient care.
In her book The Silo Effect: The Peril of Expertise and the Promise of Breaking Down Barriers, Gillian Tett wrote that “the word ‘silo’ does not just refer to a physical structure or organization (such as a department). It can also be a state of mind. Silos exist in structures. But they exist in our minds and social groups too. Silos breed tribalism. But they can also go hand in hand with tunnel vision.”
Tertiary care referral centers seem to be trending toward being more and more “un-siloed” and collaborative within their own departments and between departments in order to care for patients. The terms multidisciplinary and intradisciplinary have become popular in medicine, and teams are joining forces to create care paths for patients that are intended to improve the efficiency of and the quality of care that is rendered. There is no better example of the move to improve collaboration in medicine than the theme of the 2021 Society of Gynecologic Surgeons annual meeting, “Working Together: How Collaboration Enables Us to Better Help Our Patients.”
In this article, we provide examples of how collaborating with other specialties—within and outside of an ObGyn department—should become the standard of care. We discuss how to make this team approach easier and provide evidence that patients experience favorable outcomes. While data on combined care remain sparse, the existing literature on this topic helps us to guide and counsel patients about what to expect when a combined approach is taken.
Addressing pelvic floor disorders in women with gynecologic malignancy
In 2018, authors of a systematic review that looked at concurrent pelvic floor disorders in gynecologic oncologic survivors found that the prevalence of these disorders was high enough to warrant evaluation and management of these conditions to help improve quality of life for patients.1 Furthermore, it is possible that the prevalence of urinary incontinence is higher in patients who have undergone surgery for a gynecologic malignancy compared with controls, which has been reported in previous studies.2,3 At Cleveland Clinic, we recognize the need to evaluate our patients receiving oncologic care for urinary, fecal, and pelvic organ prolapse symptoms. Our oncologists routinely inquire about these symptoms once their patients have undergone surgery with them, and they make referrals for all their symptomatic patients. They have even learned about our own counseling, and they pre-emptively let patients know what our counseling may encompass.
For instance, many patients who received radiation therapy have stress urinary incontinence that is likely related to a hypomobile urethra, and they may benefit more from transurethral bulking than an anti-incontinence procedure in the operating room. Reassuring patients ahead of time that they do not need major interventions for their symptoms is helpful, as these patients are already experiencing tremendous burden from their oncologic conditions. We have made our referral patterns easy for these patients, and most patients are seen within days to weeks of the referral placed, depending on the urgency of the consult and the need to proceed with their oncologic treatment plan.
Gynecologic oncology patients who present with preoperative stress urinary incontinence and pelvic organ prolapse also are referred to a urogynecology specialist for concurrent care. Care paths have been created to help inform both the urogynecologists and the oncologists about options for patients depending on their respective conditions, as both their malignancy and their pelvic floor disorder(s) are considered in treatment planning. There is agreement in this planning that the oncologic surgery takes priority, and the urogynecologic approach is based on the oncologic plan.
Our urogynecologists routinely ask if future radiation is in the treatment plan, as this usually precludes us from placing a midurethral sling at the time of any surgery. Surgical approach (vaginal versus abdominal; open or minimally invasive) also is determined by the oncologic team. At the time of surgery, patient positioning is considered to optimize access for all of the surgeons. For instance, having the oncologist know that the patient needs to be far down on the bed as their steep Trendelenburg positioning during laparoscopy or robotic surgery may cause the patient to slide cephalad during the case may make a vaginal repair or sling placement at the end of the case challenging. All these small nuances are important, and a collaborative team develops the right plan for each patient in advance.
Data on the outcomes of combined surgery are sparse. In a retrospective matched cohort study, our group compared outcomes in women who underwent concurrent surgery with those who underwent urogynecologic surgery alone.4 We found that concurrent surgeries had an increased incidence of minor but not serious perioperative adverse events. Importantly, we determined that 1 in 10 planned urogynecologic procedures needed to be either modified or abandoned as a result of the oncologic plan. These data help guide our counseling, and both the oncologist and urogynecologist contributing to the combined case counsel patients according to these data.
Continue to: Concurrent colorectal and gynecologic surgery...
Concurrent colorectal and gynecologic surgery
Many women have pelvic floor disorders. As gynecologists, we often compartmentalize these conditions as gynecologic problems; frequently, however, colorectal conditions are at play as well and should be addressed concurrently. For instance, a high incidence of anorectal dysfunction occurs in women who present with pelvic organ prolapse.5 Furthermore, outlet defecation disorders are not always a result of a straightforward rectocele that can be fixed vaginally. Sometimes, a more thorough evaluation is warranted depending on the patient’s concurrent symptoms and history. Outlet symptoms may be attributed to large enteroceles, sigmoidoceles, perineal descent, rectal intussusception, and rectal prolapse.6
As a result, a combined approach to caring for patients with complex pelvic floor disorders is optimal. Several studies describe this type of combined and coordinated patient care.7,8 Ideally, patients are seen by both surgeons in the office so that the surgeons may make a combined plan for their care, especially if the decision is made to proceed with surgery. Urogynecology specialists and colorectal surgeons must decide together whether to approach combined prolapse procedures via a perineal and vaginal approach versus an abdominal approach. Several factors can determine this, including surgeon experience and preference, which is why it is important for surgeons working together to have either well-designed care paths or simply open communication and experience working together for the conditions they are treating.
In an ideal coordinated care approach, both surgeons review the patient records in advance. Any needed imaging or testing is done before the official patient consult; the patient is then seen by both clinicians in the same visit and counseled about the options. This is the most efficient and effective way to see patients, and we have had significant success using this approach.
Complications of combined surgery
The safety of combining procedures such as laparoscopic sacrocolpopexy and concurrent rectopexy has been studied, and intraoperative complications have been reported to be low.9,10 In a cohort study, Wallace and colleagues looked at postoperative outcomes and complications following combined surgery and reported that reoperation for the rectal prolapse component of the surgery was more common than the pelvic organ prolapse component, and that 1 in 5 of their patients experienced a surgical complication within 30 days of their surgery.11 This incidence is higher than that seen with isolated pelvic organ prolapse surgery. These data help us understand that a combined approach requires good patient counseling in the office about both the need for repeat surgery in certain circumstances and the increased risk of complications. Further, combined perineal and vaginal approaches have been compared with abdominal approaches and also have shown no age-adjusted differences in outcomes and complications.12
These data point to the need for surgeons to choose the approach to surgery that best fits their own experiences and to discuss this together before counseling the patient in the office, thus streamlining the effort so that the patient feels comfortable under the care of 2 surgeons.
Patients presenting with urogynecologic and gynecologic conditions also report symptomatic hemorrhoids, and colorectal referral is often made by the gynecologist. Sparse data are available regarding combined approaches to managing hemorrhoids and gynecologic conditions. Our group was the first to publish on outcomes and complications in patients undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery.13 In that retrospective cohort, we found that minor complications, such as postoperative urinary tract infection and transient voiding dysfunction, was more common in patients who underwent combined surgery. From this, we gathered that there is a need to counsel patients appropriately about the risk of combined surgery. That said, for some patients, coordinated care is desirable, and surgeons should make the effort to work together in combining their procedures.
Continue to: Integrating plastic and reconstructive surgery in gynecology...
Integrating plastic and reconstructive surgery in gynecology
Reconstructive gynecologic procedures often require a multidisciplinary approach to what can be very complex reconstructive surgery. The intended goal usually is to achieve a good cosmetic result in the genital area, as well as to restore sexual, defecatory, and/or genitourinary functionality. As a result, surgeons must work together to develop a feasible reconstructive plan for these patients.
Women experience vaginal stenosis or foreshortening for a number of reasons. Women with congenital anomalies often are cared for by specialists in pediatric and adolescent gynecology. Other women, such as those who have undergone vaginectomy and/or pelvic or vaginal radiation for cancer treatment, complications from vaginal mesh placement, and severe vaginal scarring from dermatologic conditions like lichen planus, are cared for by other gynecologic specialists, often general gynecologists or urogynecologists. In some of these cases, a gynecologic surgeon can perform vaginal adhesiolysis followed by vaginal estrogen treatment (when appropriate) and aggressive postoperative vaginal dilation with adjunctive pelvic floor physical therapy as well as sex therapy or counseling. A simple reconstructive approach may be necessary if lysis of adhesions alone is not sufficient. Sometimes, the vaginal apex must be opened vaginally or abdominally, or releasing incisions need to be made to improve the caliber of the vagina in addition to its length. Under these circumstances, the use of additional local skin grafts, local peritoneal flaps, or biologic grafts or xenografts can help achieve a satisfying result. While not all gynecologists are trained to perform these procedures, some are, and certainly gynecologic subspecialists have the skill sets to care for these patients.
Under other circumstances, when the vagina is truly foreshortened, more aggressive reconstructive surgery is necessary and consultation and collaboration with plastic surgery specialists often is helpful. At our center, these patients’ care is initially managed by gynecologists and, when simple approaches to their reconstructive needs are exhausted, collaboration is warranted. As with the other team approaches discussed in this article, the recommendation is for a consistent referral team that has established care paths for patients. Not all plastic surgeons are familiar with neovaginal reconstruction and understand the functional aspects that gynecologists are hoping to achieve for their patients. Therefore, it is important to form cohesive teams that have the same goals for the patient.
The literature on neovaginal reconstruction is sparse. There are no true agreed on approaches or techniques for vaginal reconstruction because there is no “one size fits all” for these repairs. Defects also vary depending on whether they are due to resections or radiation for oncologic treatment, reconstruction as part of the repair of a genitourinary or rectovaginal fistula, or stenosis from other etiologies.
In 2002, Cordeiro and colleagues published a classification system and reconstructive algorithm for acquired vaginal defects.14 Not all reconstructive surgeons subscribe to this algorithm, but it is the only rubric that currently exists. The authors differentiate between “partial” and “circumferential” defects and recommend different types of fasciocutaneous and myocutaneous flaps for reconstruction.
In our experience at our center, we believe that the choice of flap should also depend on whether or not perineal reconstruction is needed. This decision is made by both the gynecologic specialist and the plastic surgeon. Common flap choices include the Singapore flap, a fasciocutaneous flap based on perforators from the pudendal vessels; the gracilis flap, a myocutaneous flap based off the medial circumflex femoral vessels; and the rectus abdominis flap (transverse or vertical), which is also a myocutaneous flap that relies on the blood supply from the deep inferior epigastric vessels.
One of the most important parts of the coordinated effort of neovaginal surgery is postoperative care. Plastic surgeons play a key role in ensuring that the flap survives in the immediate postoperative period. The gynecology team should be responsible for postoperative vaginal dilation teaching and follow-up to ensure that the patient dilates properly and upsizes her dilator appropriately over the postoperative period. In our practice, our advanced practice clinicians often care for these patients and are responsible for continuity and dilation teaching. Patients have easy access to these clinicians, and this enhances the postoperative experience. Referral to a pelvic floor physical therapist knowledgeable about neovaginal surgery also helps to ensure that the dilation process goes successfully. It also helps to have office days on the same days as the plastic surgery team that is following the patient. This way, the patient may be seen by both teams on the same day. This allows for good patient communication with regard to aftercare, as well as a combined approach to teaching the trainees involved in the case. Coordination with pelvic floor physical therapists on those days also enhances the patient experience and is highly recommended.
Continue to: Combining gyn and urogyn procedures with plastic surgery...
Combining gyn and urogyn procedures with plastic surgery
While there are no data on combining gynecologic and urogynecologic procedures with plastic reconstructive surgeries, a team approach to combining surgeries is possible. At our center, we have performed tubal ligation, ovarian surgery, hysterectomy, and sling and prolapse surgery in patients who were undergoing cosmetic procedures, such as breast augmentation and abdominoplasty.
Gender affirmation surgery also can be performed through a combined approach between gynecologists and plastic surgeons. Our gynecologists perform hysterectomy for transmasculine men, and this procedure is sometimes safely and effectively performed in combination with masculinizing chest surgery (mastectomy) performed by our plastic surgeons. Vaginoplasty surgery (feminizing genital surgery) also is performed by urogynecology specialists at our center, and it is sometimes done concurrently at the time of breast augmentation and/or facial feminization surgery.
Case order. Some plastic surgeons vocalize concerns about combining clean procedures with clean contaminated cases, especially in situations in which implants are being placed in the body. During these cases, communication and organization between surgeons is important. For instance, there should be a discussion about case order. In general, the clean procedures should be performed first. In addition, separate operating tables and instruments should be used. Simultaneous operating also should be avoided. Fresh incisions should be dressed and covered before subsequent procedures are performed.
Incision placement. Last, planning around incision placement should be discussed before each case. Laparoscopic and abdominal incisions may interfere with plastic surgery procedures and alter the end cosmesis. These incisions often can be incorporated into the reconstructive procedure. The most important part of the coordinated surgical effort is ensuring that both surgical teams understand each other’s respective surgeries and the approach needed to complete them. When this is achieved, the cases are usually very successful.
Creating collaboration between obstetricians and gynecologic specialists
The impacts of pregnancy and vaginal delivery on the pelvic floor are well established. Urinary and fecal incontinence, pelvic organ prolapse, perineal pain, and dyspareunia are not uncommon in the postpartum period and may persist long term. The effects of obstetric anal sphincter injury (OASI) are significant, with up to 25% of women experiencing wound complications and 17% experiencing fecal incontinence at 6 months postpartum.15,16 Care of women with peripartum pelvic floor disorders and OASIs present an ideal opportunity for collaboration between urogynecologists and obstetricians. The Cleveland Clinic has a multidisciplinary Postpartum Care Clinic (PPCC) where we provide specialized, collaborative care for women with peripartum pelvic floor disorders and complex obstetric lacerations.
Our PPCC accepts referrals up to 1 year postpartum for women who experience OASI, urinary or fecal incontinence, perineal pain or dyspareunia, voiding dysfunction or urinary retention, and wound healing complications. When a woman is diagnosed with an OASI at the time of delivery, a “best practice alert” is released in the medical record recommending a referral to the PPCC to encourage referral of all women with OASI. We strive to see all referrals within 2 weeks of delivery.
At the time of the initial consultation, we collect validated questionnaires on bowel and bladder function, assess pain and healing, and discuss future delivery planning. The success of the PPCC is rooted in communication. When the clinic first opened, we provided education to our obstetrics colleagues on the purpose of the clinic, when and how to refer, and what to expect from our consultations. Open communication between referring obstetric clinicians and the urogynecologists that run the PPCC is key in providing collaborative care where patients know that their clinicians are working as a team. All recommendations are communicated to referring clinicians, and all women are ultimately referred back to their primary clinician for long-term care. Evidence demonstrates that this type of clinic leads to high obstetric clinician satisfaction and increased awareness of OASIs and their impact on maternal health.17
Combined team approach fosters innovation in patient care
A combined approach to the care of the patient who presents with gynecologic conditions is optimal. In this article, we presented examples of care that integrates gynecology, urogynecology, gynecologic oncology, colorectal surgery, plastic surgery, and obstetrics. There are, however, many more existing examples as well as opportunities to create teams that really make a difference in the way patients receive—and perceive—their care. This is a good starting point, and we should strive to use this model to continue to innovate our approach to patient care.
- Ramaseshan AS, Felton J, Roque D, et al. Pelvic floor disorders in women with gynecologic malignancies: a systematic review. Int Urogynecol J. 2018;29:459-476.
- Nakayama N, Tsuji T, Aoyama M, et al. Quality of life and the prevalence of urinary incontinence after surgical treatment for gynecologic cancer: a questionnaire survey. BMC Womens Health. 2020;20:148-157.
- Cascales-Campos PA, Gonzalez-Gil A, Fernandez-Luna E, et al. Urinary and fecal incontinence in patients with advanced ovarian cancer treated with CRS + HIPEC. Surg Oncol. 2021;36:115-119.
- Davidson ER, Woodburn K, AlHilli M, et al. Perioperative adverse events in women undergoing concurrent urogynecologic and gynecologic oncology surgeries for suspected malignancy. Int Urogynecol J. 2019;30:1195-1201.
- Spence-Jones C, Kamm MA, Henry MM, et al. Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and stress urinary incontinence. Br J Obstet Gynaecol. 1994;101:147-152.
- Thompson JR, Chen AH, Pettit PD, et al. Incidence of occult rectal prolapse in patients with clinical rectoceles and defecatory dysfunction. Am J Obstet Gynecol. 2002;187:1494-1500.
- Jallad K, Gurland B. Multidisciplinary approach to the treatment of concomitant rectal and vaginal prolapse. Clin Colon Rectal Surg. 2016;29:101-105.
- Kapoor DS, Sultan AH, Thakar R, et al. Management of complex pelvic floor disorders in a multidisciplinary pelvic floor clinic. Colorectal Dis. 2008;10:118-123.
- Weinberg D, Qeadan F, McKee R, et al. Safety of laparoscopic sacrocolpopexy with concurrent rectopexy: peri-operative morbidity in a nationwide cohort. Int Urogynecol J. 2019;30:385-392.
- Geltzeiler CB, Birnbaum EH, Silviera ML, et al. Combined rectopexy and sacrocolpopexy is safe for correction of pelvic organ prolapse. Int J Colorectal Dis. 2018;33:1453-1459.
- Wallace SL, Syan R, Enemchukwu EA, et al. Surgical approach, complications, and reoperation rates of combined rectal and pelvic organ prolapse surgery. Int Urogynecol J. 2020;31:2101-2108.
- Smith PE, Hade EM, Pandya LK, et al. Perioperative outcomes for combined ventral rectopexy with sacrocolpopexy compared to perineal rectopexy with vaginal apical suspension. Female Pelvic Med Reconstr Surg. 2020;26:376-381.
- Casas-Puig V, Bretschneider CE, Ferrando CA. Perioperative adverse events in women undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery. Female Pelvic Med Reconstr Surg. 2019;25:88-92.
- Cordeiro PG, Pusic AL, Disa JJ. A classification system and reconstructive algorithm for acquired vaginal defects. Plast Reconstr Surg. 2002;110:1058-1065.
- Lewicky-Gaupp C, Leader-Cramer A, Johnson LL, et al. Wound complications after obstetric anal sphincter injuries. Obstet Gynecol. 2015;125:1088-1093.
- Borello-France D, Burgio KL, Richter HE, et al; Pelvic Floor Disorders Network. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006;108:863-872.
- Propst K, Hickman LC. Peripartum pelvic floor disorder clinics inform obstetric provider practices. Int Urogynecol J. 2021;32:1793-1799.
- Ramaseshan AS, Felton J, Roque D, et al. Pelvic floor disorders in women with gynecologic malignancies: a systematic review. Int Urogynecol J. 2018;29:459-476.
- Nakayama N, Tsuji T, Aoyama M, et al. Quality of life and the prevalence of urinary incontinence after surgical treatment for gynecologic cancer: a questionnaire survey. BMC Womens Health. 2020;20:148-157.
- Cascales-Campos PA, Gonzalez-Gil A, Fernandez-Luna E, et al. Urinary and fecal incontinence in patients with advanced ovarian cancer treated with CRS + HIPEC. Surg Oncol. 2021;36:115-119.
- Davidson ER, Woodburn K, AlHilli M, et al. Perioperative adverse events in women undergoing concurrent urogynecologic and gynecologic oncology surgeries for suspected malignancy. Int Urogynecol J. 2019;30:1195-1201.
- Spence-Jones C, Kamm MA, Henry MM, et al. Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and stress urinary incontinence. Br J Obstet Gynaecol. 1994;101:147-152.
- Thompson JR, Chen AH, Pettit PD, et al. Incidence of occult rectal prolapse in patients with clinical rectoceles and defecatory dysfunction. Am J Obstet Gynecol. 2002;187:1494-1500.
- Jallad K, Gurland B. Multidisciplinary approach to the treatment of concomitant rectal and vaginal prolapse. Clin Colon Rectal Surg. 2016;29:101-105.
- Kapoor DS, Sultan AH, Thakar R, et al. Management of complex pelvic floor disorders in a multidisciplinary pelvic floor clinic. Colorectal Dis. 2008;10:118-123.
- Weinberg D, Qeadan F, McKee R, et al. Safety of laparoscopic sacrocolpopexy with concurrent rectopexy: peri-operative morbidity in a nationwide cohort. Int Urogynecol J. 2019;30:385-392.
- Geltzeiler CB, Birnbaum EH, Silviera ML, et al. Combined rectopexy and sacrocolpopexy is safe for correction of pelvic organ prolapse. Int J Colorectal Dis. 2018;33:1453-1459.
- Wallace SL, Syan R, Enemchukwu EA, et al. Surgical approach, complications, and reoperation rates of combined rectal and pelvic organ prolapse surgery. Int Urogynecol J. 2020;31:2101-2108.
- Smith PE, Hade EM, Pandya LK, et al. Perioperative outcomes for combined ventral rectopexy with sacrocolpopexy compared to perineal rectopexy with vaginal apical suspension. Female Pelvic Med Reconstr Surg. 2020;26:376-381.
- Casas-Puig V, Bretschneider CE, Ferrando CA. Perioperative adverse events in women undergoing concurrent hemorrhoidectomy at the time of urogynecologic surgery. Female Pelvic Med Reconstr Surg. 2019;25:88-92.
- Cordeiro PG, Pusic AL, Disa JJ. A classification system and reconstructive algorithm for acquired vaginal defects. Plast Reconstr Surg. 2002;110:1058-1065.
- Lewicky-Gaupp C, Leader-Cramer A, Johnson LL, et al. Wound complications after obstetric anal sphincter injuries. Obstet Gynecol. 2015;125:1088-1093.
- Borello-France D, Burgio KL, Richter HE, et al; Pelvic Floor Disorders Network. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006;108:863-872.
- Propst K, Hickman LC. Peripartum pelvic floor disorder clinics inform obstetric provider practices. Int Urogynecol J. 2021;32:1793-1799.
Electrosurgical hysteroscopy: Principles and expert techniques for optimizing the resectoscope loop
Hysteroscopic mechanical morcellators have gained popularity given their ease of use. Consequently, the resectoscope loop is being used less frequently, which has resulted in less familiarity with this device. The resectoscope loop, however, not only is cost effective but also allows for multiple distinct advantages, such as cold loop dissection of myomas and the ability to obtain electrosurgical hemostasis during operative hysteroscopy.
In this article, we review the basics of electrosurgical principles, compare outcomes associated with monopolar and bipolar resectoscopes, and discuss tips and tricks for optimizing surgical techniques when using the resectoscope loop for hysteroscopic myomectomy.
Evolution of hysteroscopy
The term hysteroscopy comes from the Greek words hystera, for uterus, and skopeo, meaning “to see.” The idea to investigate the uterus dates back to the year 1000 when physicians used a mirror with light to peer into the vaginal vault.
The first known successful hysteroscopy occurred in 1869 when Pantaleoni used an endoscope with a light source to identify uterine polyps in a 60-year-old woman with abnormal uterine bleeding. In 1898, Simon Duplay and Spiro Clado published the first textbook on hysteroscopy in which they described several models of hysteroscopic instruments and techniques.
In the 1950s, Harold Horace Hopkins and Karl Storz modified the shape and length of lenses within the endoscope by substituting longer cylindrical lenses for the old spherical lenses; this permitted improved image brightness and sharpness as well as a smaller diameter of the hysteroscope. Between the 1970s and 1980s, technological improvements allowed for the creation of practical and usable hysteroscopic instruments such as the resectoscope. The resectoscope, originally used in urology for transurethral resection of the prostate, was modified for hysteroscopy by incorporating the use of electrosurgical currents to aid in procedures.
Over the past few decades, continued refinements in technology have improved visualization and surgical techniques. For example, image clarity has been markedly improved, and narrow hysteroscope diameters, as small as 3 to 5 mm, require minimal to no cervical dilation.
Monopolar and bipolar resectoscopes
Electrosurgery is the application of an alternating electrical current to tissue to achieve the clinical effects of surgical cutting or hemostasis via cell vaporization or coagulation. Current runs from the electrosurgical unit (ESU) to the active electrode of the surgical instrument, then goes from the active electrode through the patient’s tissue to the return electrode, and then travels back to the ESU. This flow of current creates an electrical circuit (FIGURE).
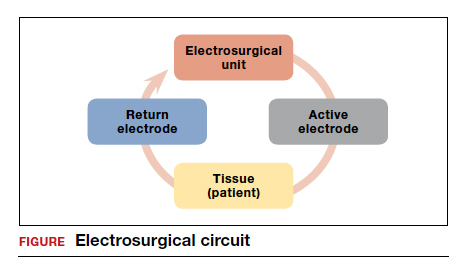
All electrosurgical devices have an active and a return electrode. The difference between monopolar and bipolar resectoscope devices lies in how the resectoscope loop is constructed. Bipolar resectoscope loops house the active and return electrodes on the same tip of the surgical device, which limits how much of the current flows through the patient. Alternatively, monopolar resectoscopes have only the active electrode on the tip of the device and the return electrode is off the surgical field, so the current flows through more of the patient. On monopolar electrosurgical devices, the current runs from the ESU to the active electrode (monopolar loop), which is then applied to tissue to produce the desired tissue effect. The current then travels via a path of least resistance from the surgical field through the patient to the return electrode, which is usually placed on the patient’s thigh, and then back to the ESU. The return electrode is often referred to as the grounding pad.
Continue to: How monopolar energy works...
How monopolar energy works
When first developed, all resectoscopes used monopolar energy. As such, throughout the 1990s, the monopolar resectoscope was the gold standard for performing electrosurgical hysteroscopy. Because the current travels a long distance between the active and the return electrode in a monopolar setup, a hypotonic, nonelectrolyte-rich medium (a poor conductor), such as glycine 1.5%, mannitol 5%, or sorbitol 3%, must be used. If an electrolyte-rich medium, such as normal saline, is used with a monopolar device, the current would be dispersed throughout the medium outside the operative field, causing unwanted tissue effects.
Although nonelectrolyte distension media improve visibility when encountering bleeding, they can be associated with hyponatremia, hyperglycemia, and even lifethreatening cerebral edema. Furthermore, glycine use is contraindicated in patients with renal or hepatic failure since oxidative deamination may cause hyperammonemia. Because of these numerous risk factors, the fluid deficit for hypotonic, nonelectrolyte distension media is limited to 1,000 mL, with a suggested maximum fluid deficit of 750 mL for elderly or fragile patients. Additionally, because the return electrode is off the surgical field in monopolar surgery, there is a risk of current diversion to the cervix, vagina, or vulva because the current travels between the active electrode on the surgical field to the return electrode on the patient’s thigh. The risk of current diversion is greater if there is damage to electrode insulation, loss of contact between the external sheath and the cervix, or direct coupling between the electrode and the surrounding tissue.
Advantages of the bipolar resectoscope
Because of the potential risks associated with the monopolar resectoscope, over the past 25 years the bipolar resectoscope emerged as an alternative due to its numerous benefits (TABLE 1).
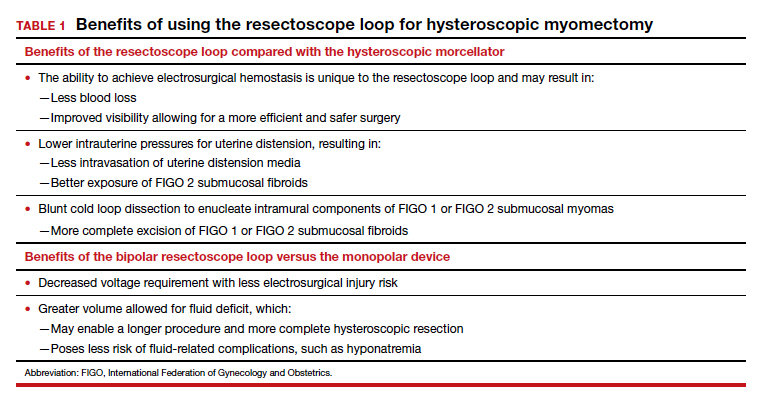
Unlike monopolar resectoscopes, bipolar resectoscopes require an electrolyte-rich distension medium such as 0.9% normal saline or lactated Ringer’s. These isotonic distension media allow a much higher fluid deficit (2,500 mL for healthy patients, 1,500 mL for elderly patients or patients with comorbidities) as the isotonic solution is safer to use. Furthermore, it allows for lower voltage settings and decreased electrical spread compared to the monopolar resectoscope since the current stays between the 2 electrodes. Because isotonic media are miscible with blood, however, a potential drawback is that in cases with bleeding, visibility may be more limited compared to hypotonic distension media.
Evidence on fertility outcomes
Several studies have compared operative and fertility outcomes with the use of monopolar versus bipolar hysteroscopy.
In a randomized controlled trial (RCT) comparing outcomes after hysteroscopy with a monopolar (glycine 1.5%) versus bipolar (0.9% normal saline) 26 French resectoscope loop, Berg and colleagues found that the only significant difference between the 2 groups was that the change in serum sodium pre and postoperatively was greater in the monopolar group despite having a smaller mean fluid deficit (765 mL vs 1,227 mL).1
Similarly, in a study of fertility outcomes after monopolar versus bipolar hysteroscopic myomectomy with use of a 26 French resectoscope Collins knife, Roy and colleagues found no significant differences in postoperative pregnancy rates or successful pregnancy outcomes, operative time, fluid deficit, or improvement in menstrual symptoms.2 However, the monopolar group had a much higher incidence of postoperative hyponatremia (30% vs 0%) that required additional days of hospitalization despite similar fluid deficits of between 600 and 700 mL.2
Similar findings were noted in another RCT that compared operative outcomes between monopolar and bipolar resectoscope usage during metroplasty for infertility, with a postoperative hyponatremia incidence of 17.1% in the monopolar group versus 0% in the bipolar group despite similar fluid deficits.3 Energy type had no effect on reproductive outcomes in either group.3
Continue to: How does the resectoscope compare with mechanical tissue removal systems?...
How does the resectoscope compare with mechanical tissue removal systems?
In 2005, the first hysteroscopic mechanical tissue removal system was introduced in the United States, providing an additional treatment method for such intrauterine masses as fibroids and polyps.
Advantages. Rather than using an electrical current, these tissue removal systems use a rotating blade with suction that is introduced through a specially designed rigid hysteroscopic sheath. As the instrument incises the pathology, the tissue is removed from the intrauterine cavity and collected in a specimen bag inside the fluid management system. This immediate removal of tissue allows for insertion of the device only once during initial entry, decreasing both the risk of perforation and operative times. Furthermore, mechanical tissue removal systems can be used with isotonic media, negating the risks associated with hypotonic media. Currently, the 2 mechanical tissue removal systems available in the United States are the TruClear and the MyoSure hysteroscopic tissue removal systems.
Studies comparing mechanical tissue removal of polyps and myomas with conventional resectoscope resection have found that mechanical tissue removal is associated with reduced operative time, fluid deficit, and number of instrument insertions.4-8 However, studies have found no significant difference in postoperative patient satisfaction.7,9
Additionally, hysteroscopic tissue removal systems have an easier learning curve. Van Dongen and colleagues conducted an RCT to compare resident-in-training comfort levels when learning to use both a mechanical tissue removal system and a traditional resectoscope; they found increased comfort with the hysteroscopic tissue removal system, suggesting greater ease of use.10
Drawbacks. Despite their many benefits, mechanical tissue removal systems have some disadvantages when compared with the resectoscope. First, mechanical tissue removal systems are associated with higher instrument costs. In addition, they have extremely limited ability to achieve hemostasis when encountering blood vessels during resection, resulting in poor visibility especially when resecting large myomas with feeding vessels.
Hysteroscopic mechanical tissue removal systems typically use higher intrauterine pressures for uterine distension compared with the resectoscope, especially when trying to improve visibility in a bloody surgical field. Increasing the intrauterine pressure with the distension media allows for compression of the blood vessels. As a result, however, submucosal fibroids classified as FIGO 2 (International Federation of Gynecology and Obstetrics) may be less visible since the higher intrauterine pressure can compress both blood vessels and submucosal fibroids
Additionally, mechanical tissue removal systems have limited ability to resect the intramural component of FIGO 1 or FIGO 2 submucosal fibroids since the intramural portion is embedded in the myometrium. Use of the resectoscope loop instead allows for a technique called the cold loop dissection, which uses the resectoscope loop to bluntly dissect and enucleate the intramural component of FIGO 1 and FIGO 2 submucosal myomas from the surrounding myometrium without activating the current. This blunt cold loop dissection technique allows for a deeper and more thorough resection. Often, if the pseudocapsule plane is identified, even the intramural component of FIGO 1 or FIGO 2 submucosal fibroids can be resected, enabling complete removal.
Lastly, mechanical tissue removal systems are not always faster than resectoscopes for all pathology. We prefer using the resectoscope for larger myomas (>3 cm) as the resectoscope allows for resection and removal of larger myoma chips, helping to decrease operative times. Given the many benefits of the resectoscope, we argue that the resectoscope loop remains a crucial instrument in operative gynecology and that learners should continue to hone their hysteroscopic skills with both the resectoscope and mechanical tissue removal systems.
Tips and tricks for hysteroscopic myomectomy with the resectoscope loop
In the video below, "Bipolar resectoscope: Optimizing safe myomectomy," we review specific surgical techniques for optimizing outcomes and safety with the resectoscope loop. These include:
- bow-and-arrow technique
- identification of the fibroid anatomy (pseudocapsule plane)
- blunt cold loop dissection
- the push-and-tuck method
- efficient electrosurgical hemostasis (TABLE 2).
Although we use bipolar energy during this resection, the resection technique using the monopolar loop is the same.
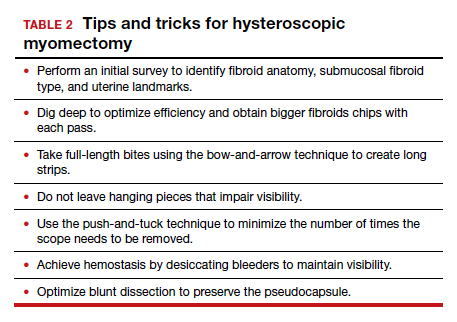

The takeaway
The resectoscope loop is a valuable tool that offers gynecologic surgeons a wider range of techniques for myomectomy. It also offers several surgical and clinical advantages. It is important to train residents in the use of both hysteroscopic mechanical tissue removal systems and resectoscope loops. ●
- Berg A, Sandvik L, Langebrekke A, et al. A randomized trial comparing monopolar electrodes using glycine 1.5% with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril. 2009;91:1273- 1278.
- Roy KK, Metta S, Kansal Y, et al. A prospective randomized study comparing unipolar versus bipolar hysteroscopic myomectomy in infertile women. J Hum Reprod Sci. 2017;10:185-193.
- Roy KK, Kansal Y, Subbaiah M, et al. Hysteroscopic septal resection using unipolar resectoscope versus bipolar resectoscope: prospective, randomized study. J Obstet Gynaecol Res. 2015;41:952-956.
- Borg MH, Shehata A. Uterine morcellator versus resectoscopy in the management of heavy menstrual flow in reproductiveage women. J Gyn Res. 2016;2:1-8.
- Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62-66.
- Smith PP, Middleton LJ, Connor M, et al. Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol. 2014;123:745-751.
- Vitale SG, Sapia F, Rapisarda AMC, et al. Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int. 2017;2017:6848250.
- Stoll F, Lecointre L, Meyer N, et al. Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minimal Invasive Gyn. 2021;28:801-810.
- Lee MM, Matsuzono T. Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection. Hong Kong Med J. 2016;22:56-61.
- van Dongen H, Emanuel MH, Wolterbeek R, et al. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15:466-471.
Hysteroscopic mechanical morcellators have gained popularity given their ease of use. Consequently, the resectoscope loop is being used less frequently, which has resulted in less familiarity with this device. The resectoscope loop, however, not only is cost effective but also allows for multiple distinct advantages, such as cold loop dissection of myomas and the ability to obtain electrosurgical hemostasis during operative hysteroscopy.
In this article, we review the basics of electrosurgical principles, compare outcomes associated with monopolar and bipolar resectoscopes, and discuss tips and tricks for optimizing surgical techniques when using the resectoscope loop for hysteroscopic myomectomy.
Evolution of hysteroscopy
The term hysteroscopy comes from the Greek words hystera, for uterus, and skopeo, meaning “to see.” The idea to investigate the uterus dates back to the year 1000 when physicians used a mirror with light to peer into the vaginal vault.
The first known successful hysteroscopy occurred in 1869 when Pantaleoni used an endoscope with a light source to identify uterine polyps in a 60-year-old woman with abnormal uterine bleeding. In 1898, Simon Duplay and Spiro Clado published the first textbook on hysteroscopy in which they described several models of hysteroscopic instruments and techniques.
In the 1950s, Harold Horace Hopkins and Karl Storz modified the shape and length of lenses within the endoscope by substituting longer cylindrical lenses for the old spherical lenses; this permitted improved image brightness and sharpness as well as a smaller diameter of the hysteroscope. Between the 1970s and 1980s, technological improvements allowed for the creation of practical and usable hysteroscopic instruments such as the resectoscope. The resectoscope, originally used in urology for transurethral resection of the prostate, was modified for hysteroscopy by incorporating the use of electrosurgical currents to aid in procedures.
Over the past few decades, continued refinements in technology have improved visualization and surgical techniques. For example, image clarity has been markedly improved, and narrow hysteroscope diameters, as small as 3 to 5 mm, require minimal to no cervical dilation.
Monopolar and bipolar resectoscopes
Electrosurgery is the application of an alternating electrical current to tissue to achieve the clinical effects of surgical cutting or hemostasis via cell vaporization or coagulation. Current runs from the electrosurgical unit (ESU) to the active electrode of the surgical instrument, then goes from the active electrode through the patient’s tissue to the return electrode, and then travels back to the ESU. This flow of current creates an electrical circuit (FIGURE).
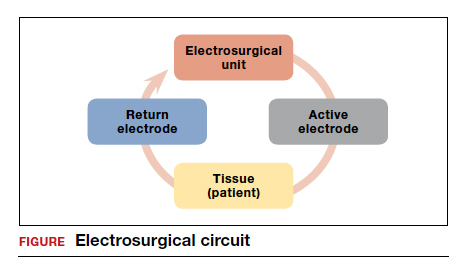
All electrosurgical devices have an active and a return electrode. The difference between monopolar and bipolar resectoscope devices lies in how the resectoscope loop is constructed. Bipolar resectoscope loops house the active and return electrodes on the same tip of the surgical device, which limits how much of the current flows through the patient. Alternatively, monopolar resectoscopes have only the active electrode on the tip of the device and the return electrode is off the surgical field, so the current flows through more of the patient. On monopolar electrosurgical devices, the current runs from the ESU to the active electrode (monopolar loop), which is then applied to tissue to produce the desired tissue effect. The current then travels via a path of least resistance from the surgical field through the patient to the return electrode, which is usually placed on the patient’s thigh, and then back to the ESU. The return electrode is often referred to as the grounding pad.
Continue to: How monopolar energy works...
How monopolar energy works
When first developed, all resectoscopes used monopolar energy. As such, throughout the 1990s, the monopolar resectoscope was the gold standard for performing electrosurgical hysteroscopy. Because the current travels a long distance between the active and the return electrode in a monopolar setup, a hypotonic, nonelectrolyte-rich medium (a poor conductor), such as glycine 1.5%, mannitol 5%, or sorbitol 3%, must be used. If an electrolyte-rich medium, such as normal saline, is used with a monopolar device, the current would be dispersed throughout the medium outside the operative field, causing unwanted tissue effects.
Although nonelectrolyte distension media improve visibility when encountering bleeding, they can be associated with hyponatremia, hyperglycemia, and even lifethreatening cerebral edema. Furthermore, glycine use is contraindicated in patients with renal or hepatic failure since oxidative deamination may cause hyperammonemia. Because of these numerous risk factors, the fluid deficit for hypotonic, nonelectrolyte distension media is limited to 1,000 mL, with a suggested maximum fluid deficit of 750 mL for elderly or fragile patients. Additionally, because the return electrode is off the surgical field in monopolar surgery, there is a risk of current diversion to the cervix, vagina, or vulva because the current travels between the active electrode on the surgical field to the return electrode on the patient’s thigh. The risk of current diversion is greater if there is damage to electrode insulation, loss of contact between the external sheath and the cervix, or direct coupling between the electrode and the surrounding tissue.
Advantages of the bipolar resectoscope
Because of the potential risks associated with the monopolar resectoscope, over the past 25 years the bipolar resectoscope emerged as an alternative due to its numerous benefits (TABLE 1).
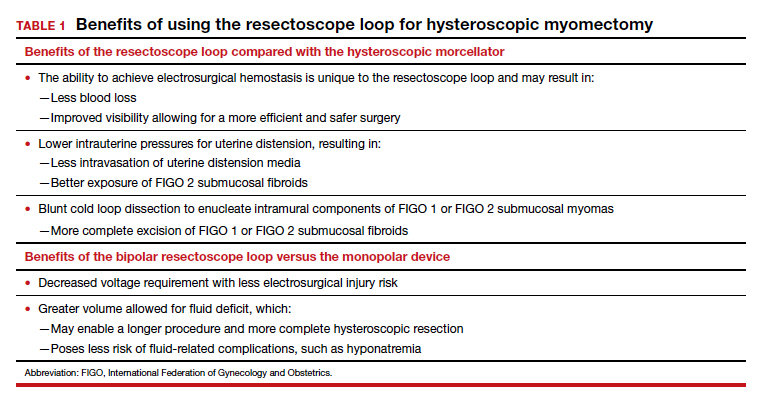
Unlike monopolar resectoscopes, bipolar resectoscopes require an electrolyte-rich distension medium such as 0.9% normal saline or lactated Ringer’s. These isotonic distension media allow a much higher fluid deficit (2,500 mL for healthy patients, 1,500 mL for elderly patients or patients with comorbidities) as the isotonic solution is safer to use. Furthermore, it allows for lower voltage settings and decreased electrical spread compared to the monopolar resectoscope since the current stays between the 2 electrodes. Because isotonic media are miscible with blood, however, a potential drawback is that in cases with bleeding, visibility may be more limited compared to hypotonic distension media.
Evidence on fertility outcomes
Several studies have compared operative and fertility outcomes with the use of monopolar versus bipolar hysteroscopy.
In a randomized controlled trial (RCT) comparing outcomes after hysteroscopy with a monopolar (glycine 1.5%) versus bipolar (0.9% normal saline) 26 French resectoscope loop, Berg and colleagues found that the only significant difference between the 2 groups was that the change in serum sodium pre and postoperatively was greater in the monopolar group despite having a smaller mean fluid deficit (765 mL vs 1,227 mL).1
Similarly, in a study of fertility outcomes after monopolar versus bipolar hysteroscopic myomectomy with use of a 26 French resectoscope Collins knife, Roy and colleagues found no significant differences in postoperative pregnancy rates or successful pregnancy outcomes, operative time, fluid deficit, or improvement in menstrual symptoms.2 However, the monopolar group had a much higher incidence of postoperative hyponatremia (30% vs 0%) that required additional days of hospitalization despite similar fluid deficits of between 600 and 700 mL.2
Similar findings were noted in another RCT that compared operative outcomes between monopolar and bipolar resectoscope usage during metroplasty for infertility, with a postoperative hyponatremia incidence of 17.1% in the monopolar group versus 0% in the bipolar group despite similar fluid deficits.3 Energy type had no effect on reproductive outcomes in either group.3
Continue to: How does the resectoscope compare with mechanical tissue removal systems?...
How does the resectoscope compare with mechanical tissue removal systems?
In 2005, the first hysteroscopic mechanical tissue removal system was introduced in the United States, providing an additional treatment method for such intrauterine masses as fibroids and polyps.
Advantages. Rather than using an electrical current, these tissue removal systems use a rotating blade with suction that is introduced through a specially designed rigid hysteroscopic sheath. As the instrument incises the pathology, the tissue is removed from the intrauterine cavity and collected in a specimen bag inside the fluid management system. This immediate removal of tissue allows for insertion of the device only once during initial entry, decreasing both the risk of perforation and operative times. Furthermore, mechanical tissue removal systems can be used with isotonic media, negating the risks associated with hypotonic media. Currently, the 2 mechanical tissue removal systems available in the United States are the TruClear and the MyoSure hysteroscopic tissue removal systems.
Studies comparing mechanical tissue removal of polyps and myomas with conventional resectoscope resection have found that mechanical tissue removal is associated with reduced operative time, fluid deficit, and number of instrument insertions.4-8 However, studies have found no significant difference in postoperative patient satisfaction.7,9
Additionally, hysteroscopic tissue removal systems have an easier learning curve. Van Dongen and colleagues conducted an RCT to compare resident-in-training comfort levels when learning to use both a mechanical tissue removal system and a traditional resectoscope; they found increased comfort with the hysteroscopic tissue removal system, suggesting greater ease of use.10
Drawbacks. Despite their many benefits, mechanical tissue removal systems have some disadvantages when compared with the resectoscope. First, mechanical tissue removal systems are associated with higher instrument costs. In addition, they have extremely limited ability to achieve hemostasis when encountering blood vessels during resection, resulting in poor visibility especially when resecting large myomas with feeding vessels.
Hysteroscopic mechanical tissue removal systems typically use higher intrauterine pressures for uterine distension compared with the resectoscope, especially when trying to improve visibility in a bloody surgical field. Increasing the intrauterine pressure with the distension media allows for compression of the blood vessels. As a result, however, submucosal fibroids classified as FIGO 2 (International Federation of Gynecology and Obstetrics) may be less visible since the higher intrauterine pressure can compress both blood vessels and submucosal fibroids
Additionally, mechanical tissue removal systems have limited ability to resect the intramural component of FIGO 1 or FIGO 2 submucosal fibroids since the intramural portion is embedded in the myometrium. Use of the resectoscope loop instead allows for a technique called the cold loop dissection, which uses the resectoscope loop to bluntly dissect and enucleate the intramural component of FIGO 1 and FIGO 2 submucosal myomas from the surrounding myometrium without activating the current. This blunt cold loop dissection technique allows for a deeper and more thorough resection. Often, if the pseudocapsule plane is identified, even the intramural component of FIGO 1 or FIGO 2 submucosal fibroids can be resected, enabling complete removal.
Lastly, mechanical tissue removal systems are not always faster than resectoscopes for all pathology. We prefer using the resectoscope for larger myomas (>3 cm) as the resectoscope allows for resection and removal of larger myoma chips, helping to decrease operative times. Given the many benefits of the resectoscope, we argue that the resectoscope loop remains a crucial instrument in operative gynecology and that learners should continue to hone their hysteroscopic skills with both the resectoscope and mechanical tissue removal systems.
Tips and tricks for hysteroscopic myomectomy with the resectoscope loop
In the video below, "Bipolar resectoscope: Optimizing safe myomectomy," we review specific surgical techniques for optimizing outcomes and safety with the resectoscope loop. These include:
- bow-and-arrow technique
- identification of the fibroid anatomy (pseudocapsule plane)
- blunt cold loop dissection
- the push-and-tuck method
- efficient electrosurgical hemostasis (TABLE 2).
Although we use bipolar energy during this resection, the resection technique using the monopolar loop is the same.
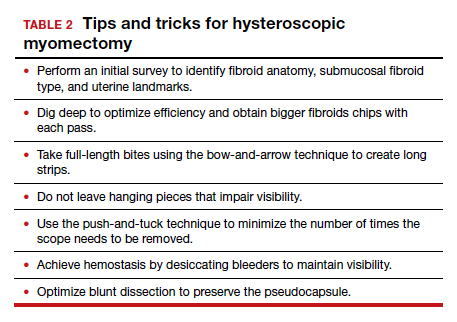

The takeaway
The resectoscope loop is a valuable tool that offers gynecologic surgeons a wider range of techniques for myomectomy. It also offers several surgical and clinical advantages. It is important to train residents in the use of both hysteroscopic mechanical tissue removal systems and resectoscope loops. ●
Hysteroscopic mechanical morcellators have gained popularity given their ease of use. Consequently, the resectoscope loop is being used less frequently, which has resulted in less familiarity with this device. The resectoscope loop, however, not only is cost effective but also allows for multiple distinct advantages, such as cold loop dissection of myomas and the ability to obtain electrosurgical hemostasis during operative hysteroscopy.
In this article, we review the basics of electrosurgical principles, compare outcomes associated with monopolar and bipolar resectoscopes, and discuss tips and tricks for optimizing surgical techniques when using the resectoscope loop for hysteroscopic myomectomy.
Evolution of hysteroscopy
The term hysteroscopy comes from the Greek words hystera, for uterus, and skopeo, meaning “to see.” The idea to investigate the uterus dates back to the year 1000 when physicians used a mirror with light to peer into the vaginal vault.
The first known successful hysteroscopy occurred in 1869 when Pantaleoni used an endoscope with a light source to identify uterine polyps in a 60-year-old woman with abnormal uterine bleeding. In 1898, Simon Duplay and Spiro Clado published the first textbook on hysteroscopy in which they described several models of hysteroscopic instruments and techniques.
In the 1950s, Harold Horace Hopkins and Karl Storz modified the shape and length of lenses within the endoscope by substituting longer cylindrical lenses for the old spherical lenses; this permitted improved image brightness and sharpness as well as a smaller diameter of the hysteroscope. Between the 1970s and 1980s, technological improvements allowed for the creation of practical and usable hysteroscopic instruments such as the resectoscope. The resectoscope, originally used in urology for transurethral resection of the prostate, was modified for hysteroscopy by incorporating the use of electrosurgical currents to aid in procedures.
Over the past few decades, continued refinements in technology have improved visualization and surgical techniques. For example, image clarity has been markedly improved, and narrow hysteroscope diameters, as small as 3 to 5 mm, require minimal to no cervical dilation.
Monopolar and bipolar resectoscopes
Electrosurgery is the application of an alternating electrical current to tissue to achieve the clinical effects of surgical cutting or hemostasis via cell vaporization or coagulation. Current runs from the electrosurgical unit (ESU) to the active electrode of the surgical instrument, then goes from the active electrode through the patient’s tissue to the return electrode, and then travels back to the ESU. This flow of current creates an electrical circuit (FIGURE).
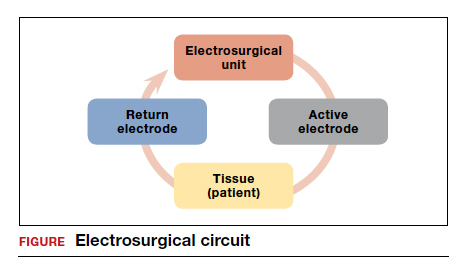
All electrosurgical devices have an active and a return electrode. The difference between monopolar and bipolar resectoscope devices lies in how the resectoscope loop is constructed. Bipolar resectoscope loops house the active and return electrodes on the same tip of the surgical device, which limits how much of the current flows through the patient. Alternatively, monopolar resectoscopes have only the active electrode on the tip of the device and the return electrode is off the surgical field, so the current flows through more of the patient. On monopolar electrosurgical devices, the current runs from the ESU to the active electrode (monopolar loop), which is then applied to tissue to produce the desired tissue effect. The current then travels via a path of least resistance from the surgical field through the patient to the return electrode, which is usually placed on the patient’s thigh, and then back to the ESU. The return electrode is often referred to as the grounding pad.
Continue to: How monopolar energy works...
How monopolar energy works
When first developed, all resectoscopes used monopolar energy. As such, throughout the 1990s, the monopolar resectoscope was the gold standard for performing electrosurgical hysteroscopy. Because the current travels a long distance between the active and the return electrode in a monopolar setup, a hypotonic, nonelectrolyte-rich medium (a poor conductor), such as glycine 1.5%, mannitol 5%, or sorbitol 3%, must be used. If an electrolyte-rich medium, such as normal saline, is used with a monopolar device, the current would be dispersed throughout the medium outside the operative field, causing unwanted tissue effects.
Although nonelectrolyte distension media improve visibility when encountering bleeding, they can be associated with hyponatremia, hyperglycemia, and even lifethreatening cerebral edema. Furthermore, glycine use is contraindicated in patients with renal or hepatic failure since oxidative deamination may cause hyperammonemia. Because of these numerous risk factors, the fluid deficit for hypotonic, nonelectrolyte distension media is limited to 1,000 mL, with a suggested maximum fluid deficit of 750 mL for elderly or fragile patients. Additionally, because the return electrode is off the surgical field in monopolar surgery, there is a risk of current diversion to the cervix, vagina, or vulva because the current travels between the active electrode on the surgical field to the return electrode on the patient’s thigh. The risk of current diversion is greater if there is damage to electrode insulation, loss of contact between the external sheath and the cervix, or direct coupling between the electrode and the surrounding tissue.
Advantages of the bipolar resectoscope
Because of the potential risks associated with the monopolar resectoscope, over the past 25 years the bipolar resectoscope emerged as an alternative due to its numerous benefits (TABLE 1).
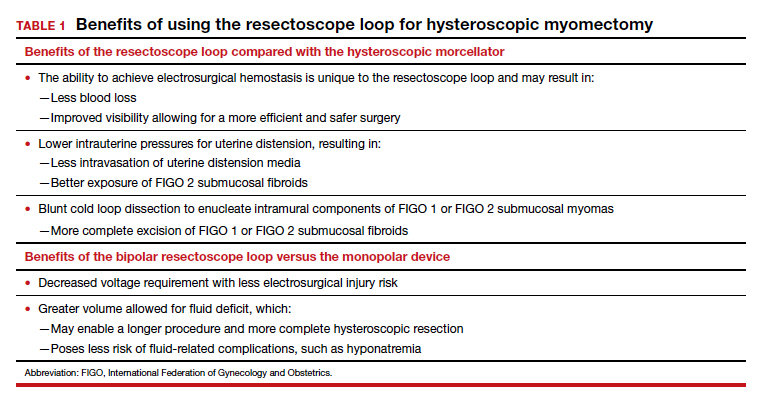
Unlike monopolar resectoscopes, bipolar resectoscopes require an electrolyte-rich distension medium such as 0.9% normal saline or lactated Ringer’s. These isotonic distension media allow a much higher fluid deficit (2,500 mL for healthy patients, 1,500 mL for elderly patients or patients with comorbidities) as the isotonic solution is safer to use. Furthermore, it allows for lower voltage settings and decreased electrical spread compared to the monopolar resectoscope since the current stays between the 2 electrodes. Because isotonic media are miscible with blood, however, a potential drawback is that in cases with bleeding, visibility may be more limited compared to hypotonic distension media.
Evidence on fertility outcomes
Several studies have compared operative and fertility outcomes with the use of monopolar versus bipolar hysteroscopy.
In a randomized controlled trial (RCT) comparing outcomes after hysteroscopy with a monopolar (glycine 1.5%) versus bipolar (0.9% normal saline) 26 French resectoscope loop, Berg and colleagues found that the only significant difference between the 2 groups was that the change in serum sodium pre and postoperatively was greater in the monopolar group despite having a smaller mean fluid deficit (765 mL vs 1,227 mL).1
Similarly, in a study of fertility outcomes after monopolar versus bipolar hysteroscopic myomectomy with use of a 26 French resectoscope Collins knife, Roy and colleagues found no significant differences in postoperative pregnancy rates or successful pregnancy outcomes, operative time, fluid deficit, or improvement in menstrual symptoms.2 However, the monopolar group had a much higher incidence of postoperative hyponatremia (30% vs 0%) that required additional days of hospitalization despite similar fluid deficits of between 600 and 700 mL.2
Similar findings were noted in another RCT that compared operative outcomes between monopolar and bipolar resectoscope usage during metroplasty for infertility, with a postoperative hyponatremia incidence of 17.1% in the monopolar group versus 0% in the bipolar group despite similar fluid deficits.3 Energy type had no effect on reproductive outcomes in either group.3
Continue to: How does the resectoscope compare with mechanical tissue removal systems?...
How does the resectoscope compare with mechanical tissue removal systems?
In 2005, the first hysteroscopic mechanical tissue removal system was introduced in the United States, providing an additional treatment method for such intrauterine masses as fibroids and polyps.
Advantages. Rather than using an electrical current, these tissue removal systems use a rotating blade with suction that is introduced through a specially designed rigid hysteroscopic sheath. As the instrument incises the pathology, the tissue is removed from the intrauterine cavity and collected in a specimen bag inside the fluid management system. This immediate removal of tissue allows for insertion of the device only once during initial entry, decreasing both the risk of perforation and operative times. Furthermore, mechanical tissue removal systems can be used with isotonic media, negating the risks associated with hypotonic media. Currently, the 2 mechanical tissue removal systems available in the United States are the TruClear and the MyoSure hysteroscopic tissue removal systems.
Studies comparing mechanical tissue removal of polyps and myomas with conventional resectoscope resection have found that mechanical tissue removal is associated with reduced operative time, fluid deficit, and number of instrument insertions.4-8 However, studies have found no significant difference in postoperative patient satisfaction.7,9
Additionally, hysteroscopic tissue removal systems have an easier learning curve. Van Dongen and colleagues conducted an RCT to compare resident-in-training comfort levels when learning to use both a mechanical tissue removal system and a traditional resectoscope; they found increased comfort with the hysteroscopic tissue removal system, suggesting greater ease of use.10
Drawbacks. Despite their many benefits, mechanical tissue removal systems have some disadvantages when compared with the resectoscope. First, mechanical tissue removal systems are associated with higher instrument costs. In addition, they have extremely limited ability to achieve hemostasis when encountering blood vessels during resection, resulting in poor visibility especially when resecting large myomas with feeding vessels.
Hysteroscopic mechanical tissue removal systems typically use higher intrauterine pressures for uterine distension compared with the resectoscope, especially when trying to improve visibility in a bloody surgical field. Increasing the intrauterine pressure with the distension media allows for compression of the blood vessels. As a result, however, submucosal fibroids classified as FIGO 2 (International Federation of Gynecology and Obstetrics) may be less visible since the higher intrauterine pressure can compress both blood vessels and submucosal fibroids
Additionally, mechanical tissue removal systems have limited ability to resect the intramural component of FIGO 1 or FIGO 2 submucosal fibroids since the intramural portion is embedded in the myometrium. Use of the resectoscope loop instead allows for a technique called the cold loop dissection, which uses the resectoscope loop to bluntly dissect and enucleate the intramural component of FIGO 1 and FIGO 2 submucosal myomas from the surrounding myometrium without activating the current. This blunt cold loop dissection technique allows for a deeper and more thorough resection. Often, if the pseudocapsule plane is identified, even the intramural component of FIGO 1 or FIGO 2 submucosal fibroids can be resected, enabling complete removal.
Lastly, mechanical tissue removal systems are not always faster than resectoscopes for all pathology. We prefer using the resectoscope for larger myomas (>3 cm) as the resectoscope allows for resection and removal of larger myoma chips, helping to decrease operative times. Given the many benefits of the resectoscope, we argue that the resectoscope loop remains a crucial instrument in operative gynecology and that learners should continue to hone their hysteroscopic skills with both the resectoscope and mechanical tissue removal systems.
Tips and tricks for hysteroscopic myomectomy with the resectoscope loop
In the video below, "Bipolar resectoscope: Optimizing safe myomectomy," we review specific surgical techniques for optimizing outcomes and safety with the resectoscope loop. These include:
- bow-and-arrow technique
- identification of the fibroid anatomy (pseudocapsule plane)
- blunt cold loop dissection
- the push-and-tuck method
- efficient electrosurgical hemostasis (TABLE 2).
Although we use bipolar energy during this resection, the resection technique using the monopolar loop is the same.
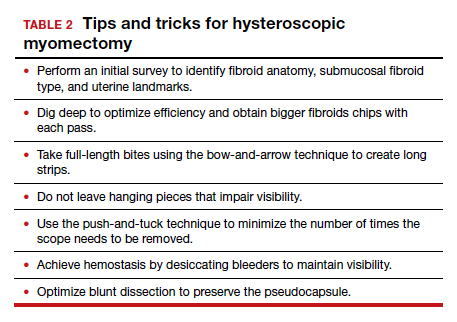

The takeaway
The resectoscope loop is a valuable tool that offers gynecologic surgeons a wider range of techniques for myomectomy. It also offers several surgical and clinical advantages. It is important to train residents in the use of both hysteroscopic mechanical tissue removal systems and resectoscope loops. ●
- Berg A, Sandvik L, Langebrekke A, et al. A randomized trial comparing monopolar electrodes using glycine 1.5% with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril. 2009;91:1273- 1278.
- Roy KK, Metta S, Kansal Y, et al. A prospective randomized study comparing unipolar versus bipolar hysteroscopic myomectomy in infertile women. J Hum Reprod Sci. 2017;10:185-193.
- Roy KK, Kansal Y, Subbaiah M, et al. Hysteroscopic septal resection using unipolar resectoscope versus bipolar resectoscope: prospective, randomized study. J Obstet Gynaecol Res. 2015;41:952-956.
- Borg MH, Shehata A. Uterine morcellator versus resectoscopy in the management of heavy menstrual flow in reproductiveage women. J Gyn Res. 2016;2:1-8.
- Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62-66.
- Smith PP, Middleton LJ, Connor M, et al. Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol. 2014;123:745-751.
- Vitale SG, Sapia F, Rapisarda AMC, et al. Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int. 2017;2017:6848250.
- Stoll F, Lecointre L, Meyer N, et al. Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minimal Invasive Gyn. 2021;28:801-810.
- Lee MM, Matsuzono T. Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection. Hong Kong Med J. 2016;22:56-61.
- van Dongen H, Emanuel MH, Wolterbeek R, et al. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15:466-471.
- Berg A, Sandvik L, Langebrekke A, et al. A randomized trial comparing monopolar electrodes using glycine 1.5% with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril. 2009;91:1273- 1278.
- Roy KK, Metta S, Kansal Y, et al. A prospective randomized study comparing unipolar versus bipolar hysteroscopic myomectomy in infertile women. J Hum Reprod Sci. 2017;10:185-193.
- Roy KK, Kansal Y, Subbaiah M, et al. Hysteroscopic septal resection using unipolar resectoscope versus bipolar resectoscope: prospective, randomized study. J Obstet Gynaecol Res. 2015;41:952-956.
- Borg MH, Shehata A. Uterine morcellator versus resectoscopy in the management of heavy menstrual flow in reproductiveage women. J Gyn Res. 2016;2:1-8.
- Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62-66.
- Smith PP, Middleton LJ, Connor M, et al. Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol. 2014;123:745-751.
- Vitale SG, Sapia F, Rapisarda AMC, et al. Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int. 2017;2017:6848250.
- Stoll F, Lecointre L, Meyer N, et al. Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minimal Invasive Gyn. 2021;28:801-810.
- Lee MM, Matsuzono T. Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection. Hong Kong Med J. 2016;22:56-61.
- van Dongen H, Emanuel MH, Wolterbeek R, et al. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15:466-471.