User login
PPI metabolism may be altered in about one-third of bariatric surgery candidates
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
REPORTING FROM DDW 2019
Sustainable weight loss seen 5 years after endoscopic sleeve gastroplasty

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.
FROM DDW 2019
Key clinical point: Endoscopic sleeve gastroplasty is an effective, minimally invasive weight-loss procedure that results in significant total body weight loss.
Major finding: Between 1 and 5 years after endoscopic sleeve gastroplasty, patients lost 15%-20% of their total body weight.
Study details: A retrospective study of prospectively collected data on 203 patients.
Disclosures: Dr. Sharaiha reported having no financial disclosures.
Study identifies predictors of bariatric surgery attrition
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
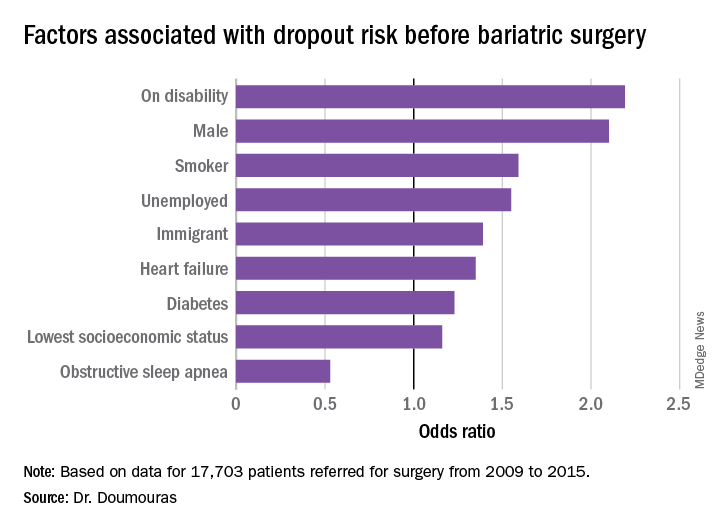
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
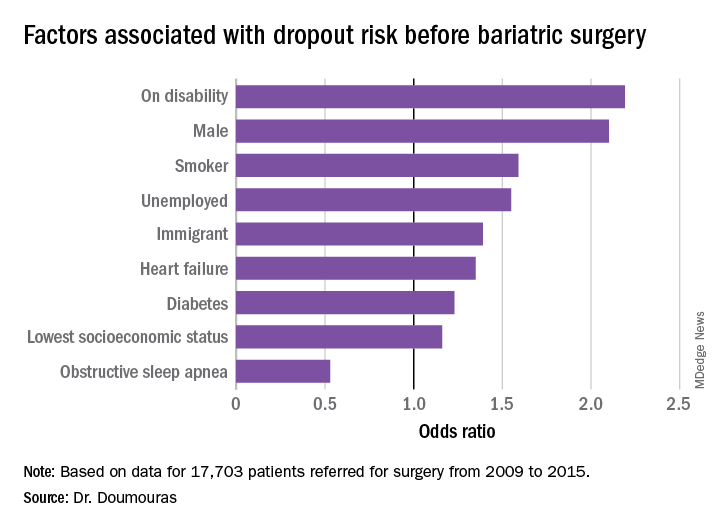
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
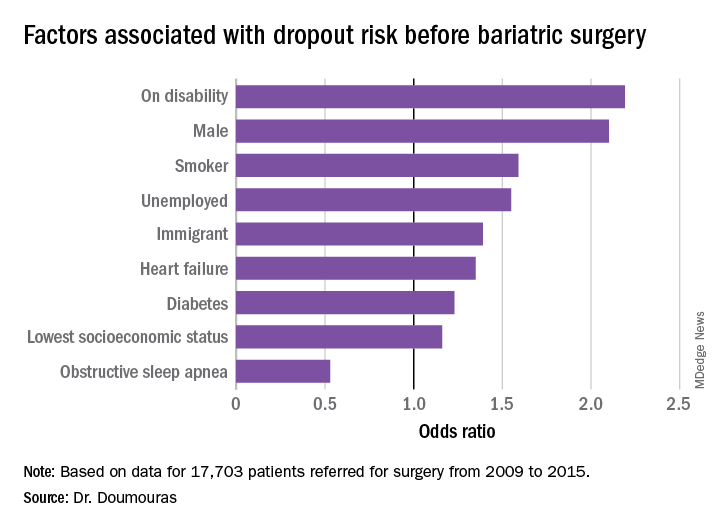
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
REPORTING FROM SAGES 2019
Study finds inconsistencies in MBSAQIP database
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
REPORTING FROM SAGES 2019
Study: Surgeon post-SG reflux rates vary widely
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
REPORTING FROM SAGES 2019
Canagliflozin after metabolic surgery may aid weight loss, reduce glucose levels
LOS ANGELES – Patients who took the sodium-glucose cotransporter-2 inhibitor canagliflozin after undergoing metabolic surgery experienced reductions in blood glucose, body mass index, and truncal body fat, results from a small pilot study have shown.
“We hypothesized that canagliflozin would be a good choice for these patients, because these drugs work independently of insulin,” the study’s principal investigator, Sangeeta R. Kashyap, MD, said in an interview at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists. “They help promote weight loss and improve blood pressure. [After] bariatric surgery, patients have an issue with weight regain, and sometimes their diabetes comes back.”
In what she said is the first prospective, randomized, controlled trial of its kind, Dr. Kashyap, an endocrinologist at the Cleveland Clinic, and her colleagues enrolled 11 women and 5 men with type 2 diabetes who had undergone Roux-en-Y gastric bypass or sleeve gastrectomy to study the effects of canagliflozin on clinical parameters over a period of 6 months. At baseline, the patients’ mean body mass index was 39.2 kg/m2 and their mean hemoglobin A1c level was 7.4%. The researchers used maximum likelihood estimation in a linear mixed-effect model to deduce differences between the treatment and placebo groups. Patients randomized to the study drug were assigned a 6-month course of canagliflozin, starting on 100 mg for 2 weeks titrated up to 300 mg daily.
At 6 months, fasting glucose was significantly reduced in the canagliflozin group, compared with baseline (from 163 to 122 mg/dL; P = .007), but it rose in the placebo group (from 164 to 192 mg/dL), a between-group difference that fell short of statistical significance (P = .12). In addition, C-reactive protein in the treatment group fell from 8.9 mg/L to 3.9 mg/L, but rose from 1.6 mg/L to 4.7 mg/L in the placebo group, a between-group difference that trended toward significance (P = .07).
During the 6-month study period, the mean BMI fell from 39.6 kg/m2 to 38 kg/m2 in the canagliflozin group but increased from 38 to 41 in the placebo group, a between-group difference that reached statistical significance (P = .014). Mean changes in body fat (a reduction of 1.82%), truncal fat (a reduction of 2.67%), and android fat (a reduction of 3%) also reached statistical significance in the treatment group, compared with the placebo group. Reductions in adiponectin, leptin, and high–molecular weight adiponectin did not reach statistical significance.
“I think these drugs have a place in post–bariatric surgery care,” Dr. Kashyap said. “Canagliflozin after metabolic surgery improved weight-loss outcomes and blood sugar levels. It also improved abdominal fat levels, and in this way might even lower cardiovascular disease risk in these patients.”
She acknowledged the study’s small sample size and single-center design as limitations. “It was very difficult to recruit patients for this study,” she said. “Not many patients have recurrent diabetes after bariatric surgery.”
Janssen provided funding to Dr. Kashyap for the trial.
LOS ANGELES – Patients who took the sodium-glucose cotransporter-2 inhibitor canagliflozin after undergoing metabolic surgery experienced reductions in blood glucose, body mass index, and truncal body fat, results from a small pilot study have shown.
“We hypothesized that canagliflozin would be a good choice for these patients, because these drugs work independently of insulin,” the study’s principal investigator, Sangeeta R. Kashyap, MD, said in an interview at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists. “They help promote weight loss and improve blood pressure. [After] bariatric surgery, patients have an issue with weight regain, and sometimes their diabetes comes back.”
In what she said is the first prospective, randomized, controlled trial of its kind, Dr. Kashyap, an endocrinologist at the Cleveland Clinic, and her colleagues enrolled 11 women and 5 men with type 2 diabetes who had undergone Roux-en-Y gastric bypass or sleeve gastrectomy to study the effects of canagliflozin on clinical parameters over a period of 6 months. At baseline, the patients’ mean body mass index was 39.2 kg/m2 and their mean hemoglobin A1c level was 7.4%. The researchers used maximum likelihood estimation in a linear mixed-effect model to deduce differences between the treatment and placebo groups. Patients randomized to the study drug were assigned a 6-month course of canagliflozin, starting on 100 mg for 2 weeks titrated up to 300 mg daily.
At 6 months, fasting glucose was significantly reduced in the canagliflozin group, compared with baseline (from 163 to 122 mg/dL; P = .007), but it rose in the placebo group (from 164 to 192 mg/dL), a between-group difference that fell short of statistical significance (P = .12). In addition, C-reactive protein in the treatment group fell from 8.9 mg/L to 3.9 mg/L, but rose from 1.6 mg/L to 4.7 mg/L in the placebo group, a between-group difference that trended toward significance (P = .07).
During the 6-month study period, the mean BMI fell from 39.6 kg/m2 to 38 kg/m2 in the canagliflozin group but increased from 38 to 41 in the placebo group, a between-group difference that reached statistical significance (P = .014). Mean changes in body fat (a reduction of 1.82%), truncal fat (a reduction of 2.67%), and android fat (a reduction of 3%) also reached statistical significance in the treatment group, compared with the placebo group. Reductions in adiponectin, leptin, and high–molecular weight adiponectin did not reach statistical significance.
“I think these drugs have a place in post–bariatric surgery care,” Dr. Kashyap said. “Canagliflozin after metabolic surgery improved weight-loss outcomes and blood sugar levels. It also improved abdominal fat levels, and in this way might even lower cardiovascular disease risk in these patients.”
She acknowledged the study’s small sample size and single-center design as limitations. “It was very difficult to recruit patients for this study,” she said. “Not many patients have recurrent diabetes after bariatric surgery.”
Janssen provided funding to Dr. Kashyap for the trial.
LOS ANGELES – Patients who took the sodium-glucose cotransporter-2 inhibitor canagliflozin after undergoing metabolic surgery experienced reductions in blood glucose, body mass index, and truncal body fat, results from a small pilot study have shown.
“We hypothesized that canagliflozin would be a good choice for these patients, because these drugs work independently of insulin,” the study’s principal investigator, Sangeeta R. Kashyap, MD, said in an interview at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists. “They help promote weight loss and improve blood pressure. [After] bariatric surgery, patients have an issue with weight regain, and sometimes their diabetes comes back.”
In what she said is the first prospective, randomized, controlled trial of its kind, Dr. Kashyap, an endocrinologist at the Cleveland Clinic, and her colleagues enrolled 11 women and 5 men with type 2 diabetes who had undergone Roux-en-Y gastric bypass or sleeve gastrectomy to study the effects of canagliflozin on clinical parameters over a period of 6 months. At baseline, the patients’ mean body mass index was 39.2 kg/m2 and their mean hemoglobin A1c level was 7.4%. The researchers used maximum likelihood estimation in a linear mixed-effect model to deduce differences between the treatment and placebo groups. Patients randomized to the study drug were assigned a 6-month course of canagliflozin, starting on 100 mg for 2 weeks titrated up to 300 mg daily.
At 6 months, fasting glucose was significantly reduced in the canagliflozin group, compared with baseline (from 163 to 122 mg/dL; P = .007), but it rose in the placebo group (from 164 to 192 mg/dL), a between-group difference that fell short of statistical significance (P = .12). In addition, C-reactive protein in the treatment group fell from 8.9 mg/L to 3.9 mg/L, but rose from 1.6 mg/L to 4.7 mg/L in the placebo group, a between-group difference that trended toward significance (P = .07).
During the 6-month study period, the mean BMI fell from 39.6 kg/m2 to 38 kg/m2 in the canagliflozin group but increased from 38 to 41 in the placebo group, a between-group difference that reached statistical significance (P = .014). Mean changes in body fat (a reduction of 1.82%), truncal fat (a reduction of 2.67%), and android fat (a reduction of 3%) also reached statistical significance in the treatment group, compared with the placebo group. Reductions in adiponectin, leptin, and high–molecular weight adiponectin did not reach statistical significance.
“I think these drugs have a place in post–bariatric surgery care,” Dr. Kashyap said. “Canagliflozin after metabolic surgery improved weight-loss outcomes and blood sugar levels. It also improved abdominal fat levels, and in this way might even lower cardiovascular disease risk in these patients.”
She acknowledged the study’s small sample size and single-center design as limitations. “It was very difficult to recruit patients for this study,” she said. “Not many patients have recurrent diabetes after bariatric surgery.”
Janssen provided funding to Dr. Kashyap for the trial.
REPORTING FROM AACE 2019
Review hints at improved semen quality after bariatric surgery
LOS ANGELES – On the male fertility front, obesity seems to hurt semen quality. So does weight-loss surgery reverse the trend? A new review of existing research suggests that there may be an effect, but the findings aren’t conclusive.
“We found something,” said Sikarin Upala, MD, a second-year endocrinology fellow at the University of Chicago, who pointed out that three of the four reports he and his colleagues reviewed suggested improvement in semen motility. “But we still need to study more about whether bariatric surgery will affect infertility,” he continued.
Dr. Upala, who led the systematic review and meta-analysis of research into bariatric surgery and semen quality, spoke in an interview after his presentation at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
As researchers explained in a 2018 report, “conflicting results have been observed in studies evaluating the correlation between [body mass index] and sperm parameters, such as sperm concentration and total sperm count.” However, they noted that it is “generally accepted” that men with obesity seem to be at higher risk of having a low sperm count or having azoospermia, which is the total lack of sperm in semen.
It’s also not clear whether weight loss directly improves male fertility. “We do know that androgen levels improve after weight-loss surgery, and that might be one factor among several that may contribute to improved male fertility,” Edward Lin, DO, MBA, FACS, professor of surgery and chief of gastrointestinal and general surgery at Emory University, Atlanta, said in an interview.
In their review, Dr. Upala and his colleagues analyzed four studies published between 2012 and 2018 that evaluated the effect of bariatric surgery on semen quality. All of the studies examined semen volume and sperm morphology and motility, and three examined sperm concentration.
A meta-analysis found that motility and volume improved after surgery; however, some of the studies (two for volume, one for motility) failed to show a statistically significant change.
There was no statistically significant difference in sperm morphology or concentration overall, although one study showed a statistically significant improvement in both categories.
Overall, “there might be a little bit of positive effect, but we couldn’t reach a good conclusion because there were too few studies,” Dr. Upala said.
Dr. Lin, director of the Emory Bariatrics Center, agreed that the review findings are limited. He said that although the findings hint at a positive effect on semen quality, “the jury is still out” when it comes to a link between bariatric surgery and male infertility.
“Multiple factors contribute to semen quality,” he added, pointing to vitamin deficiencies, micronutrient levels in the body, enzyme signaling pathways, and sperm chromatin integrity. “In fact, surgically or diet-induced weight loss may be associated with permissive malnutrition, which further exacerbates these deficiencies. Deficiencies in these areas can sometimes take months, if not years, to correct by taking vitamin D or copper or zinc, for example.”
Dr. Lin referred to a small study in which reporters observed semen abnormalities and subfertility after weight-loss surgery despite improvements in androgenic and quality of life levels.
Dr. Upala reported having no relevant disclosures.
LOS ANGELES – On the male fertility front, obesity seems to hurt semen quality. So does weight-loss surgery reverse the trend? A new review of existing research suggests that there may be an effect, but the findings aren’t conclusive.
“We found something,” said Sikarin Upala, MD, a second-year endocrinology fellow at the University of Chicago, who pointed out that three of the four reports he and his colleagues reviewed suggested improvement in semen motility. “But we still need to study more about whether bariatric surgery will affect infertility,” he continued.
Dr. Upala, who led the systematic review and meta-analysis of research into bariatric surgery and semen quality, spoke in an interview after his presentation at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
As researchers explained in a 2018 report, “conflicting results have been observed in studies evaluating the correlation between [body mass index] and sperm parameters, such as sperm concentration and total sperm count.” However, they noted that it is “generally accepted” that men with obesity seem to be at higher risk of having a low sperm count or having azoospermia, which is the total lack of sperm in semen.
It’s also not clear whether weight loss directly improves male fertility. “We do know that androgen levels improve after weight-loss surgery, and that might be one factor among several that may contribute to improved male fertility,” Edward Lin, DO, MBA, FACS, professor of surgery and chief of gastrointestinal and general surgery at Emory University, Atlanta, said in an interview.
In their review, Dr. Upala and his colleagues analyzed four studies published between 2012 and 2018 that evaluated the effect of bariatric surgery on semen quality. All of the studies examined semen volume and sperm morphology and motility, and three examined sperm concentration.
A meta-analysis found that motility and volume improved after surgery; however, some of the studies (two for volume, one for motility) failed to show a statistically significant change.
There was no statistically significant difference in sperm morphology or concentration overall, although one study showed a statistically significant improvement in both categories.
Overall, “there might be a little bit of positive effect, but we couldn’t reach a good conclusion because there were too few studies,” Dr. Upala said.
Dr. Lin, director of the Emory Bariatrics Center, agreed that the review findings are limited. He said that although the findings hint at a positive effect on semen quality, “the jury is still out” when it comes to a link between bariatric surgery and male infertility.
“Multiple factors contribute to semen quality,” he added, pointing to vitamin deficiencies, micronutrient levels in the body, enzyme signaling pathways, and sperm chromatin integrity. “In fact, surgically or diet-induced weight loss may be associated with permissive malnutrition, which further exacerbates these deficiencies. Deficiencies in these areas can sometimes take months, if not years, to correct by taking vitamin D or copper or zinc, for example.”
Dr. Lin referred to a small study in which reporters observed semen abnormalities and subfertility after weight-loss surgery despite improvements in androgenic and quality of life levels.
Dr. Upala reported having no relevant disclosures.
LOS ANGELES – On the male fertility front, obesity seems to hurt semen quality. So does weight-loss surgery reverse the trend? A new review of existing research suggests that there may be an effect, but the findings aren’t conclusive.
“We found something,” said Sikarin Upala, MD, a second-year endocrinology fellow at the University of Chicago, who pointed out that three of the four reports he and his colleagues reviewed suggested improvement in semen motility. “But we still need to study more about whether bariatric surgery will affect infertility,” he continued.
Dr. Upala, who led the systematic review and meta-analysis of research into bariatric surgery and semen quality, spoke in an interview after his presentation at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
As researchers explained in a 2018 report, “conflicting results have been observed in studies evaluating the correlation between [body mass index] and sperm parameters, such as sperm concentration and total sperm count.” However, they noted that it is “generally accepted” that men with obesity seem to be at higher risk of having a low sperm count or having azoospermia, which is the total lack of sperm in semen.
It’s also not clear whether weight loss directly improves male fertility. “We do know that androgen levels improve after weight-loss surgery, and that might be one factor among several that may contribute to improved male fertility,” Edward Lin, DO, MBA, FACS, professor of surgery and chief of gastrointestinal and general surgery at Emory University, Atlanta, said in an interview.
In their review, Dr. Upala and his colleagues analyzed four studies published between 2012 and 2018 that evaluated the effect of bariatric surgery on semen quality. All of the studies examined semen volume and sperm morphology and motility, and three examined sperm concentration.
A meta-analysis found that motility and volume improved after surgery; however, some of the studies (two for volume, one for motility) failed to show a statistically significant change.
There was no statistically significant difference in sperm morphology or concentration overall, although one study showed a statistically significant improvement in both categories.
Overall, “there might be a little bit of positive effect, but we couldn’t reach a good conclusion because there were too few studies,” Dr. Upala said.
Dr. Lin, director of the Emory Bariatrics Center, agreed that the review findings are limited. He said that although the findings hint at a positive effect on semen quality, “the jury is still out” when it comes to a link between bariatric surgery and male infertility.
“Multiple factors contribute to semen quality,” he added, pointing to vitamin deficiencies, micronutrient levels in the body, enzyme signaling pathways, and sperm chromatin integrity. “In fact, surgically or diet-induced weight loss may be associated with permissive malnutrition, which further exacerbates these deficiencies. Deficiencies in these areas can sometimes take months, if not years, to correct by taking vitamin D or copper or zinc, for example.”
Dr. Lin referred to a small study in which reporters observed semen abnormalities and subfertility after weight-loss surgery despite improvements in androgenic and quality of life levels.
Dr. Upala reported having no relevant disclosures.
REPORTING FROM AACE 2019
Machine learning tool may predict LSG outcomes
BALTIMORE – Neural networks are the building blocks of machine learning and artificial intelligence, and researchers from the University of Minnesota have identified a panel of “simple, readily known” preoperative patient factors that they fed into an artificial neural network model that can be predictive of 30-day outcomes after laparoscopic sleeve gastrectomy, one of the researchers reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The biggest limitation to using neural networks clinically is the fact that they’re algorithmic complex,” said Eric S. Wise, MD, of the University of Minnesota, Minneapolis, in presenting the research. “There is an underlying algorithm that’s developed, but it’s very difficult to understand.” He called it “a black box problem.”
Nonetheless, the researchers drew upon 101,721 laparoscopic sleeve gastrectomy cases from the 2016 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program national database to extract factors that were associated with postoperative complications. “More pertinently, we wanted to optimize predictability of a panel of readily obtainable, easily qualifiable preoperative factors and maximize the variants that are contained within those variables to predict the outcome of 30-day morbidity and mortality,” Dr. Wise said.
Essentially, neural networks recognize patterns through a machine-learning process in a manner modeled on the human brain. As Dr. Wise explained, they first emerged in the 1960s to simulate the human brain’s psychological-neurologic systems.
Through bivariate and multivariate analyses, the research identified eight preoperative variables strongly associated with the 30-day endpoints. After univariate analysis, seven of those variables were statistically significant: older age (P = .03), nonwhite race, higher initial body mass index, severe hypertension, history of diabetes, nonindependent functional status, and previous foregut/bariatric surgery (all P less than .001). “Gender was the only factor that was not predictive,” Dr. Wise said.
The factors held up under logistic regression modeling. “We were able to use a traditional logistic regression model that came up with a reasonable area under the curve of 0.572,” he said. Using artificial neural network analysis, the training set, which comprised 80% of patients, was more accurate than logistic regression, with an area under the curve of 0.582.
One limitation was that this was a “small study,” Dr. Wise said, influenced by selection bias inherent in any retrospective data selection. Other major factors that may exist were not considered.
However, he noted, “in the past we’ve had some success translating neural networks into something that’s clinically useful.” His group at Vanderbilt University published a report of artificial neural network modeling to identify five factors predictive of weight loss after Roux-en-Y gastric bypass 2 years ago (Surg Endosc. 2016;30:480-8). “There are ways to translate neural networks clinically,” Dr. Wise said.
Dr. Wise had no financial relationships to disclose.
SOURCE: Wise ES et al. SAGES 2019, Abstract S053.
BALTIMORE – Neural networks are the building blocks of machine learning and artificial intelligence, and researchers from the University of Minnesota have identified a panel of “simple, readily known” preoperative patient factors that they fed into an artificial neural network model that can be predictive of 30-day outcomes after laparoscopic sleeve gastrectomy, one of the researchers reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The biggest limitation to using neural networks clinically is the fact that they’re algorithmic complex,” said Eric S. Wise, MD, of the University of Minnesota, Minneapolis, in presenting the research. “There is an underlying algorithm that’s developed, but it’s very difficult to understand.” He called it “a black box problem.”
Nonetheless, the researchers drew upon 101,721 laparoscopic sleeve gastrectomy cases from the 2016 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program national database to extract factors that were associated with postoperative complications. “More pertinently, we wanted to optimize predictability of a panel of readily obtainable, easily qualifiable preoperative factors and maximize the variants that are contained within those variables to predict the outcome of 30-day morbidity and mortality,” Dr. Wise said.
Essentially, neural networks recognize patterns through a machine-learning process in a manner modeled on the human brain. As Dr. Wise explained, they first emerged in the 1960s to simulate the human brain’s psychological-neurologic systems.
Through bivariate and multivariate analyses, the research identified eight preoperative variables strongly associated with the 30-day endpoints. After univariate analysis, seven of those variables were statistically significant: older age (P = .03), nonwhite race, higher initial body mass index, severe hypertension, history of diabetes, nonindependent functional status, and previous foregut/bariatric surgery (all P less than .001). “Gender was the only factor that was not predictive,” Dr. Wise said.
The factors held up under logistic regression modeling. “We were able to use a traditional logistic regression model that came up with a reasonable area under the curve of 0.572,” he said. Using artificial neural network analysis, the training set, which comprised 80% of patients, was more accurate than logistic regression, with an area under the curve of 0.582.
One limitation was that this was a “small study,” Dr. Wise said, influenced by selection bias inherent in any retrospective data selection. Other major factors that may exist were not considered.
However, he noted, “in the past we’ve had some success translating neural networks into something that’s clinically useful.” His group at Vanderbilt University published a report of artificial neural network modeling to identify five factors predictive of weight loss after Roux-en-Y gastric bypass 2 years ago (Surg Endosc. 2016;30:480-8). “There are ways to translate neural networks clinically,” Dr. Wise said.
Dr. Wise had no financial relationships to disclose.
SOURCE: Wise ES et al. SAGES 2019, Abstract S053.
BALTIMORE – Neural networks are the building blocks of machine learning and artificial intelligence, and researchers from the University of Minnesota have identified a panel of “simple, readily known” preoperative patient factors that they fed into an artificial neural network model that can be predictive of 30-day outcomes after laparoscopic sleeve gastrectomy, one of the researchers reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The biggest limitation to using neural networks clinically is the fact that they’re algorithmic complex,” said Eric S. Wise, MD, of the University of Minnesota, Minneapolis, in presenting the research. “There is an underlying algorithm that’s developed, but it’s very difficult to understand.” He called it “a black box problem.”
Nonetheless, the researchers drew upon 101,721 laparoscopic sleeve gastrectomy cases from the 2016 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program national database to extract factors that were associated with postoperative complications. “More pertinently, we wanted to optimize predictability of a panel of readily obtainable, easily qualifiable preoperative factors and maximize the variants that are contained within those variables to predict the outcome of 30-day morbidity and mortality,” Dr. Wise said.
Essentially, neural networks recognize patterns through a machine-learning process in a manner modeled on the human brain. As Dr. Wise explained, they first emerged in the 1960s to simulate the human brain’s psychological-neurologic systems.
Through bivariate and multivariate analyses, the research identified eight preoperative variables strongly associated with the 30-day endpoints. After univariate analysis, seven of those variables were statistically significant: older age (P = .03), nonwhite race, higher initial body mass index, severe hypertension, history of diabetes, nonindependent functional status, and previous foregut/bariatric surgery (all P less than .001). “Gender was the only factor that was not predictive,” Dr. Wise said.
The factors held up under logistic regression modeling. “We were able to use a traditional logistic regression model that came up with a reasonable area under the curve of 0.572,” he said. Using artificial neural network analysis, the training set, which comprised 80% of patients, was more accurate than logistic regression, with an area under the curve of 0.582.
One limitation was that this was a “small study,” Dr. Wise said, influenced by selection bias inherent in any retrospective data selection. Other major factors that may exist were not considered.
However, he noted, “in the past we’ve had some success translating neural networks into something that’s clinically useful.” His group at Vanderbilt University published a report of artificial neural network modeling to identify five factors predictive of weight loss after Roux-en-Y gastric bypass 2 years ago (Surg Endosc. 2016;30:480-8). “There are ways to translate neural networks clinically,” Dr. Wise said.
Dr. Wise had no financial relationships to disclose.
SOURCE: Wise ES et al. SAGES 2019, Abstract S053.
REPORTING FROM SAGES 2019
Novel strategies may help curb bariatric SSI
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
REPORTING FROM SAGES 2019
Key clinical point: .
Major findings: The BariWound predictive model had an accuracy of area under the curve of 0.73; wound infection rates decreased from 6% to 1.3% after the change in practice.
Study details: Analysis of 274,187 cases from the 2015 MBSAQIP database; and a retrospective analysis of 333 bariatric cases performed from January 2016 to March 2018 at a single center.
Disclosures: Dr. Dang has no relationships to disclose. Dr. Weber has no disclosures, although coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
Sources: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
Staging tool predicts post-RYGB complications
BALTIMORE – A staging scale developed by the bariatric team at the University of Alberta has shown potential as a tool to accurately predict major complications 1 year after Roux-en-Y gastric bypass (RYGB) surgery, surpassing the predictability of body mass index alone, a researcher reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
Researchers at the university validated the predictive utility of the scale, known as the Edmonton Obesity Staging System (EOSS), in a retrospective chart review of 378 patients who had RYGB between December 2009 and November 2015 at Royal Alexandra Hospital in Edmonton, Alt. The EOSS uses a scale from 0 to 4 to score a patient’s risk for complications: the higher the score, the greater the risk of complications.
“The EOSS may help determine risk of major complications after RYGB, and, given its overall simplicity, you can also think of it as analogous to the American Society of Anesthesiologists physical status classification system or the New York Heart Association classification system for congestive heart failure,” said Samuel Skulsky, a 3rd-year medical student at the University of Alberta. “It may have utility as well in communicating to patients their overall risk.”
A previous study applied the EOSS score to the National Health and Human Nutrition Examination Survey to compare it to use of body mass index (BMI) as a predictive marker of mortality (CMAJ. 2011;183:E1059-66). Where the four BMI classifications were clustered on the Kaplan-Meier between 0.7 and 0.9 at 200 months post examination, the four EOSS stages analyzed, 0-3, showed more of a spread, from around 0.55 for stage 3 to near 1.0 for stage 0. This gave the researchers the idea that EOSS could also be used to predict morbidity and mortality specifically in obese patients scheduled for surgery, Mr. Skulsky said. “With the Kaplan-Meier survival curves, the EOSS actually nicely stratifies the patients with their overall survival,” he said. “In comparison, BMI did not do as well in stratifying overall mortality.”
The study reported the following 1-year complication rates in the EOSS stages:
- Stage 0 (n = 14), 7.1%.
- Stage 1 (n = 41), 4.9%.
- Stage 2 (n = 297), 8.8%.
- Stage 3 (n = 26), 23.1%.
There were no stage 4 patients in the study population.
The multivariable logistic regression analysis determined that patients with EOSS stage 3 have a 2.94 adjusted odds ratio of 1-year complications vs. patients of lower stages (P less than .043).
“Although the patients with higher EOSS scores above 3 and … end-organ damage … may benefit from bariatric surgery, they inherently have higher postoperative risk,” Mr. Skulsky said. “We must take that into consideration.”
Among the limitations of the study, Mr. Skulsky acknowledged, were that it included only patients who had RYGB, that it had a bias toward patients with EOSS stage 2 score, and that it included no stage 4 patients. “They’re not commonly operated on,” he noted, “so we didn’t actually get to study the entire scoring system.”
The next step involves moving the analysis forward to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, Mr. Skulsky said. “The results that we found so far are pretty encouraging,” he said.
Mr. Skulsky had no financial relationships to disclose.
SOURCE: Skulsky SL et al. SAGES 2019, Session SS12.
BALTIMORE – A staging scale developed by the bariatric team at the University of Alberta has shown potential as a tool to accurately predict major complications 1 year after Roux-en-Y gastric bypass (RYGB) surgery, surpassing the predictability of body mass index alone, a researcher reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
Researchers at the university validated the predictive utility of the scale, known as the Edmonton Obesity Staging System (EOSS), in a retrospective chart review of 378 patients who had RYGB between December 2009 and November 2015 at Royal Alexandra Hospital in Edmonton, Alt. The EOSS uses a scale from 0 to 4 to score a patient’s risk for complications: the higher the score, the greater the risk of complications.
“The EOSS may help determine risk of major complications after RYGB, and, given its overall simplicity, you can also think of it as analogous to the American Society of Anesthesiologists physical status classification system or the New York Heart Association classification system for congestive heart failure,” said Samuel Skulsky, a 3rd-year medical student at the University of Alberta. “It may have utility as well in communicating to patients their overall risk.”
A previous study applied the EOSS score to the National Health and Human Nutrition Examination Survey to compare it to use of body mass index (BMI) as a predictive marker of mortality (CMAJ. 2011;183:E1059-66). Where the four BMI classifications were clustered on the Kaplan-Meier between 0.7 and 0.9 at 200 months post examination, the four EOSS stages analyzed, 0-3, showed more of a spread, from around 0.55 for stage 3 to near 1.0 for stage 0. This gave the researchers the idea that EOSS could also be used to predict morbidity and mortality specifically in obese patients scheduled for surgery, Mr. Skulsky said. “With the Kaplan-Meier survival curves, the EOSS actually nicely stratifies the patients with their overall survival,” he said. “In comparison, BMI did not do as well in stratifying overall mortality.”
The study reported the following 1-year complication rates in the EOSS stages:
- Stage 0 (n = 14), 7.1%.
- Stage 1 (n = 41), 4.9%.
- Stage 2 (n = 297), 8.8%.
- Stage 3 (n = 26), 23.1%.
There were no stage 4 patients in the study population.
The multivariable logistic regression analysis determined that patients with EOSS stage 3 have a 2.94 adjusted odds ratio of 1-year complications vs. patients of lower stages (P less than .043).
“Although the patients with higher EOSS scores above 3 and … end-organ damage … may benefit from bariatric surgery, they inherently have higher postoperative risk,” Mr. Skulsky said. “We must take that into consideration.”
Among the limitations of the study, Mr. Skulsky acknowledged, were that it included only patients who had RYGB, that it had a bias toward patients with EOSS stage 2 score, and that it included no stage 4 patients. “They’re not commonly operated on,” he noted, “so we didn’t actually get to study the entire scoring system.”
The next step involves moving the analysis forward to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, Mr. Skulsky said. “The results that we found so far are pretty encouraging,” he said.
Mr. Skulsky had no financial relationships to disclose.
SOURCE: Skulsky SL et al. SAGES 2019, Session SS12.
BALTIMORE – A staging scale developed by the bariatric team at the University of Alberta has shown potential as a tool to accurately predict major complications 1 year after Roux-en-Y gastric bypass (RYGB) surgery, surpassing the predictability of body mass index alone, a researcher reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
Researchers at the university validated the predictive utility of the scale, known as the Edmonton Obesity Staging System (EOSS), in a retrospective chart review of 378 patients who had RYGB between December 2009 and November 2015 at Royal Alexandra Hospital in Edmonton, Alt. The EOSS uses a scale from 0 to 4 to score a patient’s risk for complications: the higher the score, the greater the risk of complications.
“The EOSS may help determine risk of major complications after RYGB, and, given its overall simplicity, you can also think of it as analogous to the American Society of Anesthesiologists physical status classification system or the New York Heart Association classification system for congestive heart failure,” said Samuel Skulsky, a 3rd-year medical student at the University of Alberta. “It may have utility as well in communicating to patients their overall risk.”
A previous study applied the EOSS score to the National Health and Human Nutrition Examination Survey to compare it to use of body mass index (BMI) as a predictive marker of mortality (CMAJ. 2011;183:E1059-66). Where the four BMI classifications were clustered on the Kaplan-Meier between 0.7 and 0.9 at 200 months post examination, the four EOSS stages analyzed, 0-3, showed more of a spread, from around 0.55 for stage 3 to near 1.0 for stage 0. This gave the researchers the idea that EOSS could also be used to predict morbidity and mortality specifically in obese patients scheduled for surgery, Mr. Skulsky said. “With the Kaplan-Meier survival curves, the EOSS actually nicely stratifies the patients with their overall survival,” he said. “In comparison, BMI did not do as well in stratifying overall mortality.”
The study reported the following 1-year complication rates in the EOSS stages:
- Stage 0 (n = 14), 7.1%.
- Stage 1 (n = 41), 4.9%.
- Stage 2 (n = 297), 8.8%.
- Stage 3 (n = 26), 23.1%.
There were no stage 4 patients in the study population.
The multivariable logistic regression analysis determined that patients with EOSS stage 3 have a 2.94 adjusted odds ratio of 1-year complications vs. patients of lower stages (P less than .043).
“Although the patients with higher EOSS scores above 3 and … end-organ damage … may benefit from bariatric surgery, they inherently have higher postoperative risk,” Mr. Skulsky said. “We must take that into consideration.”
Among the limitations of the study, Mr. Skulsky acknowledged, were that it included only patients who had RYGB, that it had a bias toward patients with EOSS stage 2 score, and that it included no stage 4 patients. “They’re not commonly operated on,” he noted, “so we didn’t actually get to study the entire scoring system.”
The next step involves moving the analysis forward to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, Mr. Skulsky said. “The results that we found so far are pretty encouraging,” he said.
Mr. Skulsky had no financial relationships to disclose.
SOURCE: Skulsky SL et al. SAGES 2019, Session SS12.
REPORTING FROM SAGES 2019
Key clinical point: The Edmonton Obesity Staging System is predictive of complications after Roux-en-Y gastric bypass surgery.
Major finding: Patients with a score greater than 3 had a threefold greater incidence of complications at 1 year.
Study details: Retrospective chart review of 378 patients who had RYGB at a single center from 2009 through 2015.
Disclosures: Mr. Skulsky has no financial relationships to disclose.
Source: Skulsky SL et al. SAGES 2018, Session SS12.