User login
When 31 is a lower number than 29
Since writing a blog about the 30s ("The magic of 30 and 35"), I have thought about artificial time lines in general but also the skewing of incentives.
The penalties meted out by the Centers for Medicare and Medicaid Services for hospitals that exceed specific 30-day readmission rates for heart failure are based on two very faulty premises. First, that sociodemographics don’t matter, since patient zip code and related factors do not enter the calculation. Second, that there is something meaningfully different about a patient readmitted on day 29 vs. day 31. Does anyone really think that there is a physiological, structural, or other difference? The 30-day construct is artificial, though as I write this sentence I can hear the response from the regulators: "Well, we had to make a cut somewhere!"
Maybe so, but how should we judge a health care system in which a hospital spends significant resources to prevent a 30-day readmission but then may not pay much heed to the initiative once a financial penalty is no longer a risk. In other words, a system in which the penalty for day 31 is lower (zero) than for 29?
It’s also interesting that we talk about length of stay for heart failure, but not quite as much as we used to. Indeed, lengthening the length of stay might reduce readmissions, if we can take a lesson from our European colleagues.
Expounding a bit more on the topic of artificial metrics, why does the Food and Drug Administration want 180 days of safety information for a study in which in-hospital patients are randomized to active study drug versus placebo for acute decompensated heart failure? How about 145.6 days instead? Is the patient with a left-ventricular ejection fraction of 36% safe, while one at 34% is a "must do" defibrillator implant? Does the patient with dyspnea and a b-type natriuretic peptide of 101 pg/mL have heart failure but at 99 pg/mL they are safe? I won’t name names here, but such conversations have been duly noted by your blogger/columnist, which prompts me to discuss receiver operator curves. Unfortunately, I don’t seem to get very far.
Frankly, a small dose of nihilism and a bit more understanding of statistics are needed in our profession. It’s also time to reestablish some common sense. The number 31 is not lower than 29 even if regulations make us (and hospital administrators) think it is.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital. He is an associate editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Since writing a blog about the 30s ("The magic of 30 and 35"), I have thought about artificial time lines in general but also the skewing of incentives.
The penalties meted out by the Centers for Medicare and Medicaid Services for hospitals that exceed specific 30-day readmission rates for heart failure are based on two very faulty premises. First, that sociodemographics don’t matter, since patient zip code and related factors do not enter the calculation. Second, that there is something meaningfully different about a patient readmitted on day 29 vs. day 31. Does anyone really think that there is a physiological, structural, or other difference? The 30-day construct is artificial, though as I write this sentence I can hear the response from the regulators: "Well, we had to make a cut somewhere!"
Maybe so, but how should we judge a health care system in which a hospital spends significant resources to prevent a 30-day readmission but then may not pay much heed to the initiative once a financial penalty is no longer a risk. In other words, a system in which the penalty for day 31 is lower (zero) than for 29?
It’s also interesting that we talk about length of stay for heart failure, but not quite as much as we used to. Indeed, lengthening the length of stay might reduce readmissions, if we can take a lesson from our European colleagues.
Expounding a bit more on the topic of artificial metrics, why does the Food and Drug Administration want 180 days of safety information for a study in which in-hospital patients are randomized to active study drug versus placebo for acute decompensated heart failure? How about 145.6 days instead? Is the patient with a left-ventricular ejection fraction of 36% safe, while one at 34% is a "must do" defibrillator implant? Does the patient with dyspnea and a b-type natriuretic peptide of 101 pg/mL have heart failure but at 99 pg/mL they are safe? I won’t name names here, but such conversations have been duly noted by your blogger/columnist, which prompts me to discuss receiver operator curves. Unfortunately, I don’t seem to get very far.
Frankly, a small dose of nihilism and a bit more understanding of statistics are needed in our profession. It’s also time to reestablish some common sense. The number 31 is not lower than 29 even if regulations make us (and hospital administrators) think it is.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital. He is an associate editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Since writing a blog about the 30s ("The magic of 30 and 35"), I have thought about artificial time lines in general but also the skewing of incentives.
The penalties meted out by the Centers for Medicare and Medicaid Services for hospitals that exceed specific 30-day readmission rates for heart failure are based on two very faulty premises. First, that sociodemographics don’t matter, since patient zip code and related factors do not enter the calculation. Second, that there is something meaningfully different about a patient readmitted on day 29 vs. day 31. Does anyone really think that there is a physiological, structural, or other difference? The 30-day construct is artificial, though as I write this sentence I can hear the response from the regulators: "Well, we had to make a cut somewhere!"
Maybe so, but how should we judge a health care system in which a hospital spends significant resources to prevent a 30-day readmission but then may not pay much heed to the initiative once a financial penalty is no longer a risk. In other words, a system in which the penalty for day 31 is lower (zero) than for 29?
It’s also interesting that we talk about length of stay for heart failure, but not quite as much as we used to. Indeed, lengthening the length of stay might reduce readmissions, if we can take a lesson from our European colleagues.
Expounding a bit more on the topic of artificial metrics, why does the Food and Drug Administration want 180 days of safety information for a study in which in-hospital patients are randomized to active study drug versus placebo for acute decompensated heart failure? How about 145.6 days instead? Is the patient with a left-ventricular ejection fraction of 36% safe, while one at 34% is a "must do" defibrillator implant? Does the patient with dyspnea and a b-type natriuretic peptide of 101 pg/mL have heart failure but at 99 pg/mL they are safe? I won’t name names here, but such conversations have been duly noted by your blogger/columnist, which prompts me to discuss receiver operator curves. Unfortunately, I don’t seem to get very far.
Frankly, a small dose of nihilism and a bit more understanding of statistics are needed in our profession. It’s also time to reestablish some common sense. The number 31 is not lower than 29 even if regulations make us (and hospital administrators) think it is.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital. He is an associate editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Anakinra showed benefits in diastolic heart failure
DALLAS – Interleukin-1 blockade resulted in significantly improved exercise capacity and a corresponding reduction in systemic inflammation in patients with heart failure with preserved ejection fraction in the small, pilot D-HART study.
"These results confirm the role of IL-1 in regulating cardiovascular function and provide the first evidence that an IL-1-targeted therapeutic strategy may be valuable in HFpEF [heart failure with preserved ejection fraction]," Benjamin W. Van Tassell, Pharm.D., declared at the American Heart Association scientific sessions.
The findings are welcome given that there are no approved therapies for HFpEF, which accounts for at least half of all cases of heart failure, noted Dr. Van Tassell of Virginia Commonwealth University, Richmond.
D-HART was a randomized, double-blind, placebo-controlled study involving 12 patients with symptomatic HFpEF and high levels of systemic inflammation as reflected in their elevated baseline high-sensitivity C-reactive protein levels. Patients were placed on 14 days of daily subcutaneous injections of the IL-1 antagonist anakinra (Kineret) at 100 mg or placebo, then crossed over to the other study arm. Half of the subjects had New York Heart Association (NYHA) class II heart failure, the other half class III.
Since heart failure is a syndrome of exercise intolerance secondary to impaired cardiac function, Dr. Van Tassell and his coinvestigators chose change in peak oxygen consumption (VO2) as the primary study endpoint. The median peak VO2 during the anakinra phase of the study was 16.3 mL/kg per minute, which was a 1.2–mL/kg per minute or 8% improvement over the peak value on placebo.
The improvement in peak VO2 correlated with a sharp reduction in high-sensitivity C-reactive protein (hsCRP), a surrogate marker for IL-1 activity. From a baseline of 7.5 mg/L, hsCRP levels plunged by 84% after 14 days on anakinra compared to 10% with placebo.
Ventilatory efficiency (VE) improved with IL-1 blockade as evidenced by a significant increase in the oxygen uptake efficiency slope. However, the VE/VCO2 slope – another measure of ventilatory efficiency – improved significantly with anakinra only in the five patients with above-median values at baseline. Their 12% improvement in this metric during IL-1 inhibition implies that maximum benefit occurs in patients with impaired baseline function, according to Dr. Van Tassell.
He added that these encouraging findings from D-HART provide a sound basis for larger confirmatory randomized trials evaluating IL-1 inhibition in patients with HFpEF. Anakinra is approved for the treatment of rheumatoid arthritis.
D-HART was supported by the American Heart Association and university funds. Dr. Van Tassell reported having no financial conflicts of interest.
DALLAS – Interleukin-1 blockade resulted in significantly improved exercise capacity and a corresponding reduction in systemic inflammation in patients with heart failure with preserved ejection fraction in the small, pilot D-HART study.
"These results confirm the role of IL-1 in regulating cardiovascular function and provide the first evidence that an IL-1-targeted therapeutic strategy may be valuable in HFpEF [heart failure with preserved ejection fraction]," Benjamin W. Van Tassell, Pharm.D., declared at the American Heart Association scientific sessions.
The findings are welcome given that there are no approved therapies for HFpEF, which accounts for at least half of all cases of heart failure, noted Dr. Van Tassell of Virginia Commonwealth University, Richmond.
D-HART was a randomized, double-blind, placebo-controlled study involving 12 patients with symptomatic HFpEF and high levels of systemic inflammation as reflected in their elevated baseline high-sensitivity C-reactive protein levels. Patients were placed on 14 days of daily subcutaneous injections of the IL-1 antagonist anakinra (Kineret) at 100 mg or placebo, then crossed over to the other study arm. Half of the subjects had New York Heart Association (NYHA) class II heart failure, the other half class III.
Since heart failure is a syndrome of exercise intolerance secondary to impaired cardiac function, Dr. Van Tassell and his coinvestigators chose change in peak oxygen consumption (VO2) as the primary study endpoint. The median peak VO2 during the anakinra phase of the study was 16.3 mL/kg per minute, which was a 1.2–mL/kg per minute or 8% improvement over the peak value on placebo.
The improvement in peak VO2 correlated with a sharp reduction in high-sensitivity C-reactive protein (hsCRP), a surrogate marker for IL-1 activity. From a baseline of 7.5 mg/L, hsCRP levels plunged by 84% after 14 days on anakinra compared to 10% with placebo.
Ventilatory efficiency (VE) improved with IL-1 blockade as evidenced by a significant increase in the oxygen uptake efficiency slope. However, the VE/VCO2 slope – another measure of ventilatory efficiency – improved significantly with anakinra only in the five patients with above-median values at baseline. Their 12% improvement in this metric during IL-1 inhibition implies that maximum benefit occurs in patients with impaired baseline function, according to Dr. Van Tassell.
He added that these encouraging findings from D-HART provide a sound basis for larger confirmatory randomized trials evaluating IL-1 inhibition in patients with HFpEF. Anakinra is approved for the treatment of rheumatoid arthritis.
D-HART was supported by the American Heart Association and university funds. Dr. Van Tassell reported having no financial conflicts of interest.
DALLAS – Interleukin-1 blockade resulted in significantly improved exercise capacity and a corresponding reduction in systemic inflammation in patients with heart failure with preserved ejection fraction in the small, pilot D-HART study.
"These results confirm the role of IL-1 in regulating cardiovascular function and provide the first evidence that an IL-1-targeted therapeutic strategy may be valuable in HFpEF [heart failure with preserved ejection fraction]," Benjamin W. Van Tassell, Pharm.D., declared at the American Heart Association scientific sessions.
The findings are welcome given that there are no approved therapies for HFpEF, which accounts for at least half of all cases of heart failure, noted Dr. Van Tassell of Virginia Commonwealth University, Richmond.
D-HART was a randomized, double-blind, placebo-controlled study involving 12 patients with symptomatic HFpEF and high levels of systemic inflammation as reflected in their elevated baseline high-sensitivity C-reactive protein levels. Patients were placed on 14 days of daily subcutaneous injections of the IL-1 antagonist anakinra (Kineret) at 100 mg or placebo, then crossed over to the other study arm. Half of the subjects had New York Heart Association (NYHA) class II heart failure, the other half class III.
Since heart failure is a syndrome of exercise intolerance secondary to impaired cardiac function, Dr. Van Tassell and his coinvestigators chose change in peak oxygen consumption (VO2) as the primary study endpoint. The median peak VO2 during the anakinra phase of the study was 16.3 mL/kg per minute, which was a 1.2–mL/kg per minute or 8% improvement over the peak value on placebo.
The improvement in peak VO2 correlated with a sharp reduction in high-sensitivity C-reactive protein (hsCRP), a surrogate marker for IL-1 activity. From a baseline of 7.5 mg/L, hsCRP levels plunged by 84% after 14 days on anakinra compared to 10% with placebo.
Ventilatory efficiency (VE) improved with IL-1 blockade as evidenced by a significant increase in the oxygen uptake efficiency slope. However, the VE/VCO2 slope – another measure of ventilatory efficiency – improved significantly with anakinra only in the five patients with above-median values at baseline. Their 12% improvement in this metric during IL-1 inhibition implies that maximum benefit occurs in patients with impaired baseline function, according to Dr. Van Tassell.
He added that these encouraging findings from D-HART provide a sound basis for larger confirmatory randomized trials evaluating IL-1 inhibition in patients with HFpEF. Anakinra is approved for the treatment of rheumatoid arthritis.
D-HART was supported by the American Heart Association and university funds. Dr. Van Tassell reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: Patients with heart failure with preserved ejection fraction showed a significant 8% placebo-subtracted gain in peak oxygen consumption after 14 days of interleukin-1 inhibition via daily anakinra. This was accompanied by an 84% reduction in baseline elevated high-sensitivity C-reactive protein levels.
Data source: D-HART, a randomized, double-blind pilot study in which 12 patients with heart failure with preserved ejection fraction were placed on 14 days of daily subcutaneous injections of anakinra at 100 mg or placebo, then crossed to 14 days of the alternative.
Disclosures: D-HART was supported by the American Heart Association and university funds. Dr. Van Tassell reported having no financial conflicts of interest.
Statin reduces MI risk in ischemic heart failure
DALLAS – Rosuvastatin appears to reduce the risk of acute myocardial infarction in patients with ischemic heart failure, according to a meta-analysis of two landmark statin trials.
This finding is at odds with current thinking as expressed in the new American Heart Association/American College of Cardiology (AHA/ACC) guidelines, which don’t specifically recommend statin therapy for heart failure patients because no large randomized trials have shown a significant reduction in cardiovascular events.
That’s probably because those studies relied on traditional statistical techniques of survival analysis rather than the less familiar method of competing risk analysis, which is better suited to detecting a statin benefit in heart failure patients who are simultaneously at risk for multiple types of events, including arrhythmias, cancer, infection, and renal failure, as well as ischemic events, Dr. Matthew Feinstein explained at the American Heart Association scientific sessions.
When he and his coinvestigators applied competing risk analysis in their meta-analysis of the randomized, placebo-controlled CORONA (N. Engl. J. Med. 2007; 357:2248-61) and GISSI-HF trials, they found after accounting for competing risks in close to 10,000 heart failure patients that those on 10 mg/day of rosuvastatin had a 17% reduction in the risk of myocardial infarction during follow-up, compared with those on placebo. This benefit fell just shy of statistical significance. However, when the researchers restricted the analysis to the nearly 7,100 subjects with ischemic heart failure, the resultant 19% reduction in MI risk with rosuvastatin did achieve significance.
While there was a consistent trend for a lower MI risk with rosuvastatin in all prespecified subgroups of patients with ischemic heart failure in the pooled analysis, this trend reached statistical significance in two subgroups: men, who were 22% less likely to have an MI on rosuvastatin than with placebo, and patients with a baseline low-density lipoprotein (LDL) cholesterol above 96 mg/dL, who had a 23% reduction in risk, reported Dr. Feinstein of Northwestern University, Chicago, and his colleagues.
"It’s likely that ischemic heart failure patients do benefit from statin therapy, contrary to current thinking, if they are likely to live long enough to derive benefit from statins in preventing atherothrombotic events," he concluded.
Session chair Dr. Lori Mosca was enthusiastic about the meta-analysis findings and their clinical implications. She also was strongly supportive of the application of competing risk analysis in this setting.
"That was actually a brilliant analysis. I really loved it. The lesson it teaches is that when we design a clinical trial where our nonischemic outcomes are more common than the ischemic outcomes that we’re trying to prevent, we really need to take a look at those competing risks. We might come to completely different conclusions if we do that," said Dr. Mosca, professor of medicine at Columbia University, New York, and director of preventive cardiology at New York-Presbyterian Hospital.
Other important take-home points from this pooled analysis of the CORONA and GISSI-HF trials are that despite all the confusion surrounding the new AHA/ACC prevention guidelines, LDL cholesterol levels still matter in terms of predicting outcomes, and that, as always, it’s important to look at gender interactions in looking at clinical trial outcomes, added Dr. Mosca, who is current chair of the AHA Expert Panel for the Effectiveness-Based Guidelines for the Prevention of Cardiovascular Disease in Women.
Noting that it’s not always possible for a physician to tell whether the cause of a patient’s heart failure is ischemic or nonischemic, she asked Dr. Feinstein if he’d prescribe a statin if he merely suspected that the heart failure was ischemic, perhaps because the patient had evidence of underlying coronary disease.
Yes, he replied, provided the patient had no contraindications to statin therapy, was able to tolerate it, and had a sufficiently long life expectancy to be able to reap the benefits. He added a caveat: Heart failure patients typically have multiple comorbid conditions that could place them at risk with higher doses of statins.
"Rosuvastatin tends to be a somewhat less toxic and better tolerated statin, and 10 mg is a relatively low dose," Dr. Feinstein noted.
The meta-analysis was conducted free of commercial sponsorship. Dr. Feinstein reported having no financial conflicts of interest.
DALLAS – Rosuvastatin appears to reduce the risk of acute myocardial infarction in patients with ischemic heart failure, according to a meta-analysis of two landmark statin trials.
This finding is at odds with current thinking as expressed in the new American Heart Association/American College of Cardiology (AHA/ACC) guidelines, which don’t specifically recommend statin therapy for heart failure patients because no large randomized trials have shown a significant reduction in cardiovascular events.
That’s probably because those studies relied on traditional statistical techniques of survival analysis rather than the less familiar method of competing risk analysis, which is better suited to detecting a statin benefit in heart failure patients who are simultaneously at risk for multiple types of events, including arrhythmias, cancer, infection, and renal failure, as well as ischemic events, Dr. Matthew Feinstein explained at the American Heart Association scientific sessions.
When he and his coinvestigators applied competing risk analysis in their meta-analysis of the randomized, placebo-controlled CORONA (N. Engl. J. Med. 2007; 357:2248-61) and GISSI-HF trials, they found after accounting for competing risks in close to 10,000 heart failure patients that those on 10 mg/day of rosuvastatin had a 17% reduction in the risk of myocardial infarction during follow-up, compared with those on placebo. This benefit fell just shy of statistical significance. However, when the researchers restricted the analysis to the nearly 7,100 subjects with ischemic heart failure, the resultant 19% reduction in MI risk with rosuvastatin did achieve significance.
While there was a consistent trend for a lower MI risk with rosuvastatin in all prespecified subgroups of patients with ischemic heart failure in the pooled analysis, this trend reached statistical significance in two subgroups: men, who were 22% less likely to have an MI on rosuvastatin than with placebo, and patients with a baseline low-density lipoprotein (LDL) cholesterol above 96 mg/dL, who had a 23% reduction in risk, reported Dr. Feinstein of Northwestern University, Chicago, and his colleagues.
"It’s likely that ischemic heart failure patients do benefit from statin therapy, contrary to current thinking, if they are likely to live long enough to derive benefit from statins in preventing atherothrombotic events," he concluded.
Session chair Dr. Lori Mosca was enthusiastic about the meta-analysis findings and their clinical implications. She also was strongly supportive of the application of competing risk analysis in this setting.
"That was actually a brilliant analysis. I really loved it. The lesson it teaches is that when we design a clinical trial where our nonischemic outcomes are more common than the ischemic outcomes that we’re trying to prevent, we really need to take a look at those competing risks. We might come to completely different conclusions if we do that," said Dr. Mosca, professor of medicine at Columbia University, New York, and director of preventive cardiology at New York-Presbyterian Hospital.
Other important take-home points from this pooled analysis of the CORONA and GISSI-HF trials are that despite all the confusion surrounding the new AHA/ACC prevention guidelines, LDL cholesterol levels still matter in terms of predicting outcomes, and that, as always, it’s important to look at gender interactions in looking at clinical trial outcomes, added Dr. Mosca, who is current chair of the AHA Expert Panel for the Effectiveness-Based Guidelines for the Prevention of Cardiovascular Disease in Women.
Noting that it’s not always possible for a physician to tell whether the cause of a patient’s heart failure is ischemic or nonischemic, she asked Dr. Feinstein if he’d prescribe a statin if he merely suspected that the heart failure was ischemic, perhaps because the patient had evidence of underlying coronary disease.
Yes, he replied, provided the patient had no contraindications to statin therapy, was able to tolerate it, and had a sufficiently long life expectancy to be able to reap the benefits. He added a caveat: Heart failure patients typically have multiple comorbid conditions that could place them at risk with higher doses of statins.
"Rosuvastatin tends to be a somewhat less toxic and better tolerated statin, and 10 mg is a relatively low dose," Dr. Feinstein noted.
The meta-analysis was conducted free of commercial sponsorship. Dr. Feinstein reported having no financial conflicts of interest.
DALLAS – Rosuvastatin appears to reduce the risk of acute myocardial infarction in patients with ischemic heart failure, according to a meta-analysis of two landmark statin trials.
This finding is at odds with current thinking as expressed in the new American Heart Association/American College of Cardiology (AHA/ACC) guidelines, which don’t specifically recommend statin therapy for heart failure patients because no large randomized trials have shown a significant reduction in cardiovascular events.
That’s probably because those studies relied on traditional statistical techniques of survival analysis rather than the less familiar method of competing risk analysis, which is better suited to detecting a statin benefit in heart failure patients who are simultaneously at risk for multiple types of events, including arrhythmias, cancer, infection, and renal failure, as well as ischemic events, Dr. Matthew Feinstein explained at the American Heart Association scientific sessions.
When he and his coinvestigators applied competing risk analysis in their meta-analysis of the randomized, placebo-controlled CORONA (N. Engl. J. Med. 2007; 357:2248-61) and GISSI-HF trials, they found after accounting for competing risks in close to 10,000 heart failure patients that those on 10 mg/day of rosuvastatin had a 17% reduction in the risk of myocardial infarction during follow-up, compared with those on placebo. This benefit fell just shy of statistical significance. However, when the researchers restricted the analysis to the nearly 7,100 subjects with ischemic heart failure, the resultant 19% reduction in MI risk with rosuvastatin did achieve significance.
While there was a consistent trend for a lower MI risk with rosuvastatin in all prespecified subgroups of patients with ischemic heart failure in the pooled analysis, this trend reached statistical significance in two subgroups: men, who were 22% less likely to have an MI on rosuvastatin than with placebo, and patients with a baseline low-density lipoprotein (LDL) cholesterol above 96 mg/dL, who had a 23% reduction in risk, reported Dr. Feinstein of Northwestern University, Chicago, and his colleagues.
"It’s likely that ischemic heart failure patients do benefit from statin therapy, contrary to current thinking, if they are likely to live long enough to derive benefit from statins in preventing atherothrombotic events," he concluded.
Session chair Dr. Lori Mosca was enthusiastic about the meta-analysis findings and their clinical implications. She also was strongly supportive of the application of competing risk analysis in this setting.
"That was actually a brilliant analysis. I really loved it. The lesson it teaches is that when we design a clinical trial where our nonischemic outcomes are more common than the ischemic outcomes that we’re trying to prevent, we really need to take a look at those competing risks. We might come to completely different conclusions if we do that," said Dr. Mosca, professor of medicine at Columbia University, New York, and director of preventive cardiology at New York-Presbyterian Hospital.
Other important take-home points from this pooled analysis of the CORONA and GISSI-HF trials are that despite all the confusion surrounding the new AHA/ACC prevention guidelines, LDL cholesterol levels still matter in terms of predicting outcomes, and that, as always, it’s important to look at gender interactions in looking at clinical trial outcomes, added Dr. Mosca, who is current chair of the AHA Expert Panel for the Effectiveness-Based Guidelines for the Prevention of Cardiovascular Disease in Women.
Noting that it’s not always possible for a physician to tell whether the cause of a patient’s heart failure is ischemic or nonischemic, she asked Dr. Feinstein if he’d prescribe a statin if he merely suspected that the heart failure was ischemic, perhaps because the patient had evidence of underlying coronary disease.
Yes, he replied, provided the patient had no contraindications to statin therapy, was able to tolerate it, and had a sufficiently long life expectancy to be able to reap the benefits. He added a caveat: Heart failure patients typically have multiple comorbid conditions that could place them at risk with higher doses of statins.
"Rosuvastatin tends to be a somewhat less toxic and better tolerated statin, and 10 mg is a relatively low dose," Dr. Feinstein noted.
The meta-analysis was conducted free of commercial sponsorship. Dr. Feinstein reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: Rosuvastatin at 10 mg/day resulted in a significant 19% reduction in the risk of MI, compared with placebo, in patients with ischemic heart failure.
Data source: A post hoc meta-analysis of two landmark, randomized, placebo-controlled clinical trials – the CORONA and GISSI-HF trials – totaling nearly 10,000 subjects with heart failure followed prospectively for a median of 33 and 47 months, respectively.
Disclosures: The meta-analysis was conducted free of commercial sponsorship. Dr. Feinstein reported having no financial conflicts of interest.
Married to or divorced from the wedge?
Should we be measuring wedge pressures in patients with decompensated heart failure?
Despite a lot of historical baggage including the ESCAPE trial, which showed that use of a pulmonary artery catheter to titrate therapy aimed at lowering pulmonary capillary wedge pressure did not affect mortality or days hospitalized during the next 6 months, compared with therapy guided solely by clinical assessment (JAMA 2005;294:1625-33), I think so.
The procedure should be done sparingly, of course, but there remains a role for invasive hemodynamics, both from a diagnostic standpoint and for monitoring response to therapy.
And therein lies the conundrum for a pharmaceutical company looking to develop a drug for acute decompensated heart failure.
Here’s a thought experiment: You have a drug that has performed well in the preclinical model. You perform a hemodynamic study and show that the wedge pressure declines (and maybe right atrial and mean pulmonary pressures, too). Will that pass muster at the Food and Drug Administration?
It will not.
Now let’s say that you did all that the FDA requested of you (which makes this more than a thought experiment; it’s a miracle), but you do not have any hemodynamic data. Would clinicians adopt the new drug?
I suspect not.
We still like to have the reassurance that something positive is going on from the standpoint of hemodynamics, even if the drug relieves dyspnea, improves quality-of-life and reduces mortality.
So whither the wedge? Clinically, it can be useful in a limited subset of patients for whom dyspnea is unexplained or low output is suspected. In drug development, it may shed light on mechanism of action and inform dose selection.
As a consequence, we still have a relationship with pulmonary artery catheterization, but it’s no longer a marriage, and it’s not a divorce. Maybe it’s a friend with whom an occasional reunion makes sense?
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at St. Louis University and director of heart failure at St. Louis University Hospital. He is associate editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Should we be measuring wedge pressures in patients with decompensated heart failure?
Despite a lot of historical baggage including the ESCAPE trial, which showed that use of a pulmonary artery catheter to titrate therapy aimed at lowering pulmonary capillary wedge pressure did not affect mortality or days hospitalized during the next 6 months, compared with therapy guided solely by clinical assessment (JAMA 2005;294:1625-33), I think so.
The procedure should be done sparingly, of course, but there remains a role for invasive hemodynamics, both from a diagnostic standpoint and for monitoring response to therapy.
And therein lies the conundrum for a pharmaceutical company looking to develop a drug for acute decompensated heart failure.
Here’s a thought experiment: You have a drug that has performed well in the preclinical model. You perform a hemodynamic study and show that the wedge pressure declines (and maybe right atrial and mean pulmonary pressures, too). Will that pass muster at the Food and Drug Administration?
It will not.
Now let’s say that you did all that the FDA requested of you (which makes this more than a thought experiment; it’s a miracle), but you do not have any hemodynamic data. Would clinicians adopt the new drug?
I suspect not.
We still like to have the reassurance that something positive is going on from the standpoint of hemodynamics, even if the drug relieves dyspnea, improves quality-of-life and reduces mortality.
So whither the wedge? Clinically, it can be useful in a limited subset of patients for whom dyspnea is unexplained or low output is suspected. In drug development, it may shed light on mechanism of action and inform dose selection.
As a consequence, we still have a relationship with pulmonary artery catheterization, but it’s no longer a marriage, and it’s not a divorce. Maybe it’s a friend with whom an occasional reunion makes sense?
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at St. Louis University and director of heart failure at St. Louis University Hospital. He is associate editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Should we be measuring wedge pressures in patients with decompensated heart failure?
Despite a lot of historical baggage including the ESCAPE trial, which showed that use of a pulmonary artery catheter to titrate therapy aimed at lowering pulmonary capillary wedge pressure did not affect mortality or days hospitalized during the next 6 months, compared with therapy guided solely by clinical assessment (JAMA 2005;294:1625-33), I think so.
The procedure should be done sparingly, of course, but there remains a role for invasive hemodynamics, both from a diagnostic standpoint and for monitoring response to therapy.
And therein lies the conundrum for a pharmaceutical company looking to develop a drug for acute decompensated heart failure.
Here’s a thought experiment: You have a drug that has performed well in the preclinical model. You perform a hemodynamic study and show that the wedge pressure declines (and maybe right atrial and mean pulmonary pressures, too). Will that pass muster at the Food and Drug Administration?
It will not.
Now let’s say that you did all that the FDA requested of you (which makes this more than a thought experiment; it’s a miracle), but you do not have any hemodynamic data. Would clinicians adopt the new drug?
I suspect not.
We still like to have the reassurance that something positive is going on from the standpoint of hemodynamics, even if the drug relieves dyspnea, improves quality-of-life and reduces mortality.
So whither the wedge? Clinically, it can be useful in a limited subset of patients for whom dyspnea is unexplained or low output is suspected. In drug development, it may shed light on mechanism of action and inform dose selection.
As a consequence, we still have a relationship with pulmonary artery catheterization, but it’s no longer a marriage, and it’s not a divorce. Maybe it’s a friend with whom an occasional reunion makes sense?
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at St. Louis University and director of heart failure at St. Louis University Hospital. He is associate editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Heart failure exacerbation by saxagliptin called ‘real’
DALLAS – The glycemia-lowering drug saxagliptin led to a "real" excess of hospitalizations for heart failure in a 16,000-patient trial designed to examine the drug’s cardiovascular safety, but given saxagliptin’s overall safety in the study the signal of heart failure exacerbation should not rule out the drug’s use for most patients, even those with preexisting heart failure.
"Every drug has adverse effects. With these data, the calculation about saxagliptin can be made to a much more certain level. Clinicians need to weigh a patient’s risk factors, which drugs they can or cannot take, and a drug’s overall safety for ischemic events," said Dr. Benjamin M. Scirica while presenting a poster at the American Heart Association’s scientific sessions. "At this point, we have no definitive data to a priori say don’t give saxagliptin to patients with heart failure."
This follow-up analysis of data collected in the SAVOR-TIMI 53 (Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus – Thrombolysis in Myocardial Infarction) trial occurred because prior reports on the study’s outcomes had shown a small but statistically significant excess incidence of hospitalization for heart failure among the 8,280 patients treated with saxagliptin, compared with the 8,212 patients randomized to placebo.
Researchers ran the SAVOR-TIMI 53 trial in patients with type 2 diabetes and either established cardiovascular disease or multiple risk factors to explicitly test the cardiovascular safety of saxagliptin (Onglyza), a selective dipeptidyl peptidase 4 (DPP-4) inhibitor, following guidance from the Food and Drug Administration in 2009 (N. Engl. J. Med. 2013;369:1317-26). The primary outcome from the study showed no statistically significant difference in the combined rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke between the saxagliptin and placebo arms during a median 2.1 years of follow-up. The results also showed saxagliptin met the FDA’s recommended safety criterion for cardiovascular safety in a drug meant to treat type 2 diabetes.
More detailed analyses showed a 0.7% absolute increased risk for hospitalization for heart failure in the saxagliptin-treated patients, compared with the placebo group (a 27% increase in relative risk), and that the largest number of increased hospitalizations occurred among the quartile of patients enrolled in the trial with baseline blood levels of NT–pro-brain natriuretic peptide of at least 333 pg/mL. Further analysis reported for the first time by Dr. Scirica in his poster showed that the greatest excess rate of hospitalization for heart failure occurred during the first 6 months of treatment. After the first 6 months, hospitalization rates for this reason were virtually identical in the two treatment arms of the study, said Dr. Scirica, a cardiologist at Brigham and Women’s Hospital and Harvard Medical School in Boston.
His analysis also compared the impact of saxagliptin on hospitalization for heart failure with the same effect of alogliptin, another DPP-4 inhibitor, in results from the EXAMINE (Examination of Cardiovascular Outcomes With Alogliptin vs. Standard of Care) trial (N. Engl. J. Med. 2013;369:1327-35). In EXAMINE the 2,701 patients who received alogliptin (Nesina) had an absolute 0.6% higher rate of hospitalizations for heart failure (an 18% relative increase) that was not statistically significant. EXAMINE also showed no significantly different rate between alogliptin and placebo treatment for the study’s primary, combined cardiovascular endpoint during a median 1.5 years of treatment in patients with type 2 diabetes and acute coronary syndrome.
"One could look at the alogliptin results and say there was no signal [for increased hospitalization for heart failure], or that there was a signal, although not statistically significant. The only way to know for sure is to see what the next trial shows," said Dr. Deepak L. Bhatt, professor of medicine at Harvard Medical School, a cardiologist at Brigham and Women’s Hospital, and senior investigator for SAVOR-TIMI 53. The TECOS (Sitagliptin Cardiovascular Outcome Study) study using sitagliptin (Januvia), a third DPP-4 inhibitor, is slated to finish at the end of 2014. "Whether this is a drug or class effect still very much has yet to be seen," said Dr. Scirica. The mechanism also remains elusive for the time being.
"The most important message is that future trials [of diabetes drugs] need to prospectively look at heart failure rates, adjudicate heart failure events, and really look for any heart failure effect," Dr. Bhatt said.
SAVOR-TIMI 53 was sponsored by Astra Zeneca and Bristol-Myers Squibb. Dr. Scirica said that he has received honoraria as a consultant or adviser to Gilead, Eisai, Lexicon, Arena, St. Jude’s Medical, Decision Resources, and Boston Clinical research Institute, and that he has received research grants from six other drug companies. Dr. Bhatt said that he has received research grants from six other drug or device companies.
On Twitter @mitchelzoler
DALLAS – The glycemia-lowering drug saxagliptin led to a "real" excess of hospitalizations for heart failure in a 16,000-patient trial designed to examine the drug’s cardiovascular safety, but given saxagliptin’s overall safety in the study the signal of heart failure exacerbation should not rule out the drug’s use for most patients, even those with preexisting heart failure.
"Every drug has adverse effects. With these data, the calculation about saxagliptin can be made to a much more certain level. Clinicians need to weigh a patient’s risk factors, which drugs they can or cannot take, and a drug’s overall safety for ischemic events," said Dr. Benjamin M. Scirica while presenting a poster at the American Heart Association’s scientific sessions. "At this point, we have no definitive data to a priori say don’t give saxagliptin to patients with heart failure."
This follow-up analysis of data collected in the SAVOR-TIMI 53 (Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus – Thrombolysis in Myocardial Infarction) trial occurred because prior reports on the study’s outcomes had shown a small but statistically significant excess incidence of hospitalization for heart failure among the 8,280 patients treated with saxagliptin, compared with the 8,212 patients randomized to placebo.
Researchers ran the SAVOR-TIMI 53 trial in patients with type 2 diabetes and either established cardiovascular disease or multiple risk factors to explicitly test the cardiovascular safety of saxagliptin (Onglyza), a selective dipeptidyl peptidase 4 (DPP-4) inhibitor, following guidance from the Food and Drug Administration in 2009 (N. Engl. J. Med. 2013;369:1317-26). The primary outcome from the study showed no statistically significant difference in the combined rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke between the saxagliptin and placebo arms during a median 2.1 years of follow-up. The results also showed saxagliptin met the FDA’s recommended safety criterion for cardiovascular safety in a drug meant to treat type 2 diabetes.
More detailed analyses showed a 0.7% absolute increased risk for hospitalization for heart failure in the saxagliptin-treated patients, compared with the placebo group (a 27% increase in relative risk), and that the largest number of increased hospitalizations occurred among the quartile of patients enrolled in the trial with baseline blood levels of NT–pro-brain natriuretic peptide of at least 333 pg/mL. Further analysis reported for the first time by Dr. Scirica in his poster showed that the greatest excess rate of hospitalization for heart failure occurred during the first 6 months of treatment. After the first 6 months, hospitalization rates for this reason were virtually identical in the two treatment arms of the study, said Dr. Scirica, a cardiologist at Brigham and Women’s Hospital and Harvard Medical School in Boston.
His analysis also compared the impact of saxagliptin on hospitalization for heart failure with the same effect of alogliptin, another DPP-4 inhibitor, in results from the EXAMINE (Examination of Cardiovascular Outcomes With Alogliptin vs. Standard of Care) trial (N. Engl. J. Med. 2013;369:1327-35). In EXAMINE the 2,701 patients who received alogliptin (Nesina) had an absolute 0.6% higher rate of hospitalizations for heart failure (an 18% relative increase) that was not statistically significant. EXAMINE also showed no significantly different rate between alogliptin and placebo treatment for the study’s primary, combined cardiovascular endpoint during a median 1.5 years of treatment in patients with type 2 diabetes and acute coronary syndrome.
"One could look at the alogliptin results and say there was no signal [for increased hospitalization for heart failure], or that there was a signal, although not statistically significant. The only way to know for sure is to see what the next trial shows," said Dr. Deepak L. Bhatt, professor of medicine at Harvard Medical School, a cardiologist at Brigham and Women’s Hospital, and senior investigator for SAVOR-TIMI 53. The TECOS (Sitagliptin Cardiovascular Outcome Study) study using sitagliptin (Januvia), a third DPP-4 inhibitor, is slated to finish at the end of 2014. "Whether this is a drug or class effect still very much has yet to be seen," said Dr. Scirica. The mechanism also remains elusive for the time being.
"The most important message is that future trials [of diabetes drugs] need to prospectively look at heart failure rates, adjudicate heart failure events, and really look for any heart failure effect," Dr. Bhatt said.
SAVOR-TIMI 53 was sponsored by Astra Zeneca and Bristol-Myers Squibb. Dr. Scirica said that he has received honoraria as a consultant or adviser to Gilead, Eisai, Lexicon, Arena, St. Jude’s Medical, Decision Resources, and Boston Clinical research Institute, and that he has received research grants from six other drug companies. Dr. Bhatt said that he has received research grants from six other drug or device companies.
On Twitter @mitchelzoler
DALLAS – The glycemia-lowering drug saxagliptin led to a "real" excess of hospitalizations for heart failure in a 16,000-patient trial designed to examine the drug’s cardiovascular safety, but given saxagliptin’s overall safety in the study the signal of heart failure exacerbation should not rule out the drug’s use for most patients, even those with preexisting heart failure.
"Every drug has adverse effects. With these data, the calculation about saxagliptin can be made to a much more certain level. Clinicians need to weigh a patient’s risk factors, which drugs they can or cannot take, and a drug’s overall safety for ischemic events," said Dr. Benjamin M. Scirica while presenting a poster at the American Heart Association’s scientific sessions. "At this point, we have no definitive data to a priori say don’t give saxagliptin to patients with heart failure."
This follow-up analysis of data collected in the SAVOR-TIMI 53 (Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus – Thrombolysis in Myocardial Infarction) trial occurred because prior reports on the study’s outcomes had shown a small but statistically significant excess incidence of hospitalization for heart failure among the 8,280 patients treated with saxagliptin, compared with the 8,212 patients randomized to placebo.
Researchers ran the SAVOR-TIMI 53 trial in patients with type 2 diabetes and either established cardiovascular disease or multiple risk factors to explicitly test the cardiovascular safety of saxagliptin (Onglyza), a selective dipeptidyl peptidase 4 (DPP-4) inhibitor, following guidance from the Food and Drug Administration in 2009 (N. Engl. J. Med. 2013;369:1317-26). The primary outcome from the study showed no statistically significant difference in the combined rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke between the saxagliptin and placebo arms during a median 2.1 years of follow-up. The results also showed saxagliptin met the FDA’s recommended safety criterion for cardiovascular safety in a drug meant to treat type 2 diabetes.
More detailed analyses showed a 0.7% absolute increased risk for hospitalization for heart failure in the saxagliptin-treated patients, compared with the placebo group (a 27% increase in relative risk), and that the largest number of increased hospitalizations occurred among the quartile of patients enrolled in the trial with baseline blood levels of NT–pro-brain natriuretic peptide of at least 333 pg/mL. Further analysis reported for the first time by Dr. Scirica in his poster showed that the greatest excess rate of hospitalization for heart failure occurred during the first 6 months of treatment. After the first 6 months, hospitalization rates for this reason were virtually identical in the two treatment arms of the study, said Dr. Scirica, a cardiologist at Brigham and Women’s Hospital and Harvard Medical School in Boston.
His analysis also compared the impact of saxagliptin on hospitalization for heart failure with the same effect of alogliptin, another DPP-4 inhibitor, in results from the EXAMINE (Examination of Cardiovascular Outcomes With Alogliptin vs. Standard of Care) trial (N. Engl. J. Med. 2013;369:1327-35). In EXAMINE the 2,701 patients who received alogliptin (Nesina) had an absolute 0.6% higher rate of hospitalizations for heart failure (an 18% relative increase) that was not statistically significant. EXAMINE also showed no significantly different rate between alogliptin and placebo treatment for the study’s primary, combined cardiovascular endpoint during a median 1.5 years of treatment in patients with type 2 diabetes and acute coronary syndrome.
"One could look at the alogliptin results and say there was no signal [for increased hospitalization for heart failure], or that there was a signal, although not statistically significant. The only way to know for sure is to see what the next trial shows," said Dr. Deepak L. Bhatt, professor of medicine at Harvard Medical School, a cardiologist at Brigham and Women’s Hospital, and senior investigator for SAVOR-TIMI 53. The TECOS (Sitagliptin Cardiovascular Outcome Study) study using sitagliptin (Januvia), a third DPP-4 inhibitor, is slated to finish at the end of 2014. "Whether this is a drug or class effect still very much has yet to be seen," said Dr. Scirica. The mechanism also remains elusive for the time being.
"The most important message is that future trials [of diabetes drugs] need to prospectively look at heart failure rates, adjudicate heart failure events, and really look for any heart failure effect," Dr. Bhatt said.
SAVOR-TIMI 53 was sponsored by Astra Zeneca and Bristol-Myers Squibb. Dr. Scirica said that he has received honoraria as a consultant or adviser to Gilead, Eisai, Lexicon, Arena, St. Jude’s Medical, Decision Resources, and Boston Clinical research Institute, and that he has received research grants from six other drug companies. Dr. Bhatt said that he has received research grants from six other drug or device companies.
On Twitter @mitchelzoler
AT THE AHA SCIENTIFIC SESSIONS
Major finding: Treatment with saxagliptin led to a "real" 0.7% increased rate of hospitalization for heart failure, compared with patients on placebo.
Data source: The SAVOR-TIMI 53 study, which randomized 16,492 patients with type 2 diabetes to treatment with saxagliptin or placebo at 788 sites in 26 countries.
Disclosures: SAVOR-TIMI 53 was sponsored by AstraZeneca and Bristol-Myers Squibb. Dr. Scirica said that he has received honoraria as a consultant or adviser to Gilead, Eisai, Lexicon, Arena, St. Jude’s Medical, Decision Resources, and Boston Clinical Research Institute, and that he has received research grants from six other drug companies. Dr. Bhatt said that he has received research grants from six other drug or device companies.
Abrupt increase noted in LVAD thrombosis
An abrupt and unexpected increase in pump thrombosis has occurred since March 2011 in patients with advanced heart failure who received the HeartMate II left ventricular assist device, according to a report published online Nov. 27 in the New England Journal of Medicine.
Those who develop LVAD thrombosis are at substantial risk of death and morbidity unless the device is replaced or cardiac transplantation is performed, said Dr. Randall C. Starling of the Cleveland Clinic and his associates.
The reason for the sudden rise in pump thrombosis is not yet known, but it may be related to excess "deposition of material (fibrin and denatured protein) in proximity to the inflow bearing" of the device, which has been observed by clinicians in at least three cardiac centers.
"Our data suggest that the HeartMate II may have a more narrow tolerance with respect to thrombus formation than originally understood, and may be vulnerable to the timing and intensity of anticoagulation," Dr. Starling and his colleagues noted.
The HeartMate II, made by Thoratec, is a small axial-flow LVAD that "rapidly became integral in the treatment of patients with advanced heart failure" after it was introduced. Early trials and postmarketing approval studies reported a 2%-4% incidence of thrombosis. But a quality review at the Cleveland Clinic showed a sudden, marked increase in that rate beginning in March 2011.
Researchers at the Cleveland Clinic then pooled their data on the HeartMate II (from October 2004 to February 2013) with data on the device from two other high-volume cardiology centers: Washington University Barnes-Jewish Hospital, St. Louis (January 2004 to April 2013) and Duke University Medical Center, Durham, N.C. (May 2005 to May 2013). They now report on their findings from 895 HeartMate II LVADs implanted in 837 patients during that time.
"The HeartMate II may have a more narrow tolerance with respect to thrombus formation than originally understood, and may be vulnerable to the timing and intensity of anticoagulation..."
The mean patient age was 55 years, and 21% of patients were women.
The primary endpoint of the study was confirmed LVAD thrombosis, defined as a finding at pump replacement, urgent transplantation, or autopsy of a thrombus on the blood-contacting surface of the device, its inflow cannula, or its outflow conduit. A total of 72 such thromboses were found in 66 patients; in addition, 36 cases of suspected thromboses occurred.
The rate of confirmed pump thrombosis was initially stable at roughly 2.2% for several years, then rose steeply after March 2011 to 8.4%. This pattern was seen at all three medical centers and across all the cardiac surgeons at those centers.
The median time interval from implantation to pump thrombosis had been 18.6 months before March 2011, but that rate plummeted to 2.7 months during and after March 2011, Dr. Starling and his associates reported (N. Engl. J. Med. 2013 Nov. 27 [doi: 10.1056/NEJMoa1313385]).
The investigators also reviewed serial measurements of lactate dehydrogenase (LDH) that had been taken in recipients of 568 of the devices. Elevated LDH indicates hemolysis that may herald impending thrombosis.
"The graph of the occurrence of LDH levels above 1000 IU per liter ... was nearly superimposable on the graph of the occurrence of confirmed pump thrombosis. The LDH data showed a parallel tendency for elevations to occur early after implantation beginning in approximately March 2011," they said.
The LDH level typically rose from an average of 540 IU/L to an average of 1,490 IU/L during the weeks leading up to LVAD thrombosis at all three medical centers. This confirms that LDH level is a useful clinical biomarker of hemolysis associated with LVAD thrombosis, the researchers said.
Of the 72 pump thromboses, 11 were managed by heart transplantation and 21 by pump replacement. Of the remaining 40 thromboses, 2 were managed by LVAD removal because left ventricular function had improved, and 38 were managed medically, with augmentation of anticoagulation therapy and thrombolytic agents. This stabilized the clinical course in some patients, but others elected withdrawal of care, citing "futility."
Mortality was 48% among the patients who could not be managed by heart transplantation or pump replacement, and this elevated rate was consistent across the three medical centers.
The reasons for this abrupt, dramatic rise in thromboses associated with the HeartMate II are not known. There were no changes in LVAD implantation techniques at any of the three medical centers during the course of this study, "and we could find no association between pump thrombosis and the surgeon performing the implantation." The design of the HeartMate II was changed during this interval – "modification of the outflow graft and bend relief, inflow conduit, and software" was introduced – but these changes have not been linked to pump thrombosis as yet.
Dr. Starling and his associates did note the deposition of fibrin and denatured protein around the inflow bearing, which could narrow the inflow pathway, "increasing shear stress on the red cells and, if the deposition is large enough, decreasing the ability of the pump to unload the left ventricle." But it remains to be seen whether this or other factors played a role.
"Further investigation of predisposing patient and device factors and preventive and therapeutic strategies are urgently needed to resolve this important safety issue," the investigators said.
They added that a fourth cardiology center, the University of Pennsylvania, Philadelphia, found a similar pattern in a preliminary analysis that was reported as the article went to press. In that report on 150 HeartMate II LVADs implanted in 148 patients between November 2005 and September 2013, there were 15 thrombotic events. "Similar to the findings in our study, the event rate has increased abruptly and unexpectedly, with a rate of confirmed thrombosis that continues to rise," Dr. Starling and his associates said.
Dr. Starling reported ties to Thoratec and HeartWare, and his associates reported ties to Thoratec, HeartWare, Abiomed, and Syncardia.
An abrupt and unexpected increase in pump thrombosis has occurred since March 2011 in patients with advanced heart failure who received the HeartMate II left ventricular assist device, according to a report published online Nov. 27 in the New England Journal of Medicine.
Those who develop LVAD thrombosis are at substantial risk of death and morbidity unless the device is replaced or cardiac transplantation is performed, said Dr. Randall C. Starling of the Cleveland Clinic and his associates.
The reason for the sudden rise in pump thrombosis is not yet known, but it may be related to excess "deposition of material (fibrin and denatured protein) in proximity to the inflow bearing" of the device, which has been observed by clinicians in at least three cardiac centers.
"Our data suggest that the HeartMate II may have a more narrow tolerance with respect to thrombus formation than originally understood, and may be vulnerable to the timing and intensity of anticoagulation," Dr. Starling and his colleagues noted.
The HeartMate II, made by Thoratec, is a small axial-flow LVAD that "rapidly became integral in the treatment of patients with advanced heart failure" after it was introduced. Early trials and postmarketing approval studies reported a 2%-4% incidence of thrombosis. But a quality review at the Cleveland Clinic showed a sudden, marked increase in that rate beginning in March 2011.
Researchers at the Cleveland Clinic then pooled their data on the HeartMate II (from October 2004 to February 2013) with data on the device from two other high-volume cardiology centers: Washington University Barnes-Jewish Hospital, St. Louis (January 2004 to April 2013) and Duke University Medical Center, Durham, N.C. (May 2005 to May 2013). They now report on their findings from 895 HeartMate II LVADs implanted in 837 patients during that time.
"The HeartMate II may have a more narrow tolerance with respect to thrombus formation than originally understood, and may be vulnerable to the timing and intensity of anticoagulation..."
The mean patient age was 55 years, and 21% of patients were women.
The primary endpoint of the study was confirmed LVAD thrombosis, defined as a finding at pump replacement, urgent transplantation, or autopsy of a thrombus on the blood-contacting surface of the device, its inflow cannula, or its outflow conduit. A total of 72 such thromboses were found in 66 patients; in addition, 36 cases of suspected thromboses occurred.
The rate of confirmed pump thrombosis was initially stable at roughly 2.2% for several years, then rose steeply after March 2011 to 8.4%. This pattern was seen at all three medical centers and across all the cardiac surgeons at those centers.
The median time interval from implantation to pump thrombosis had been 18.6 months before March 2011, but that rate plummeted to 2.7 months during and after March 2011, Dr. Starling and his associates reported (N. Engl. J. Med. 2013 Nov. 27 [doi: 10.1056/NEJMoa1313385]).
The investigators also reviewed serial measurements of lactate dehydrogenase (LDH) that had been taken in recipients of 568 of the devices. Elevated LDH indicates hemolysis that may herald impending thrombosis.
"The graph of the occurrence of LDH levels above 1000 IU per liter ... was nearly superimposable on the graph of the occurrence of confirmed pump thrombosis. The LDH data showed a parallel tendency for elevations to occur early after implantation beginning in approximately March 2011," they said.
The LDH level typically rose from an average of 540 IU/L to an average of 1,490 IU/L during the weeks leading up to LVAD thrombosis at all three medical centers. This confirms that LDH level is a useful clinical biomarker of hemolysis associated with LVAD thrombosis, the researchers said.
Of the 72 pump thromboses, 11 were managed by heart transplantation and 21 by pump replacement. Of the remaining 40 thromboses, 2 were managed by LVAD removal because left ventricular function had improved, and 38 were managed medically, with augmentation of anticoagulation therapy and thrombolytic agents. This stabilized the clinical course in some patients, but others elected withdrawal of care, citing "futility."
Mortality was 48% among the patients who could not be managed by heart transplantation or pump replacement, and this elevated rate was consistent across the three medical centers.
The reasons for this abrupt, dramatic rise in thromboses associated with the HeartMate II are not known. There were no changes in LVAD implantation techniques at any of the three medical centers during the course of this study, "and we could find no association between pump thrombosis and the surgeon performing the implantation." The design of the HeartMate II was changed during this interval – "modification of the outflow graft and bend relief, inflow conduit, and software" was introduced – but these changes have not been linked to pump thrombosis as yet.
Dr. Starling and his associates did note the deposition of fibrin and denatured protein around the inflow bearing, which could narrow the inflow pathway, "increasing shear stress on the red cells and, if the deposition is large enough, decreasing the ability of the pump to unload the left ventricle." But it remains to be seen whether this or other factors played a role.
"Further investigation of predisposing patient and device factors and preventive and therapeutic strategies are urgently needed to resolve this important safety issue," the investigators said.
They added that a fourth cardiology center, the University of Pennsylvania, Philadelphia, found a similar pattern in a preliminary analysis that was reported as the article went to press. In that report on 150 HeartMate II LVADs implanted in 148 patients between November 2005 and September 2013, there were 15 thrombotic events. "Similar to the findings in our study, the event rate has increased abruptly and unexpectedly, with a rate of confirmed thrombosis that continues to rise," Dr. Starling and his associates said.
Dr. Starling reported ties to Thoratec and HeartWare, and his associates reported ties to Thoratec, HeartWare, Abiomed, and Syncardia.
An abrupt and unexpected increase in pump thrombosis has occurred since March 2011 in patients with advanced heart failure who received the HeartMate II left ventricular assist device, according to a report published online Nov. 27 in the New England Journal of Medicine.
Those who develop LVAD thrombosis are at substantial risk of death and morbidity unless the device is replaced or cardiac transplantation is performed, said Dr. Randall C. Starling of the Cleveland Clinic and his associates.
The reason for the sudden rise in pump thrombosis is not yet known, but it may be related to excess "deposition of material (fibrin and denatured protein) in proximity to the inflow bearing" of the device, which has been observed by clinicians in at least three cardiac centers.
"Our data suggest that the HeartMate II may have a more narrow tolerance with respect to thrombus formation than originally understood, and may be vulnerable to the timing and intensity of anticoagulation," Dr. Starling and his colleagues noted.
The HeartMate II, made by Thoratec, is a small axial-flow LVAD that "rapidly became integral in the treatment of patients with advanced heart failure" after it was introduced. Early trials and postmarketing approval studies reported a 2%-4% incidence of thrombosis. But a quality review at the Cleveland Clinic showed a sudden, marked increase in that rate beginning in March 2011.
Researchers at the Cleveland Clinic then pooled their data on the HeartMate II (from October 2004 to February 2013) with data on the device from two other high-volume cardiology centers: Washington University Barnes-Jewish Hospital, St. Louis (January 2004 to April 2013) and Duke University Medical Center, Durham, N.C. (May 2005 to May 2013). They now report on their findings from 895 HeartMate II LVADs implanted in 837 patients during that time.
"The HeartMate II may have a more narrow tolerance with respect to thrombus formation than originally understood, and may be vulnerable to the timing and intensity of anticoagulation..."
The mean patient age was 55 years, and 21% of patients were women.
The primary endpoint of the study was confirmed LVAD thrombosis, defined as a finding at pump replacement, urgent transplantation, or autopsy of a thrombus on the blood-contacting surface of the device, its inflow cannula, or its outflow conduit. A total of 72 such thromboses were found in 66 patients; in addition, 36 cases of suspected thromboses occurred.
The rate of confirmed pump thrombosis was initially stable at roughly 2.2% for several years, then rose steeply after March 2011 to 8.4%. This pattern was seen at all three medical centers and across all the cardiac surgeons at those centers.
The median time interval from implantation to pump thrombosis had been 18.6 months before March 2011, but that rate plummeted to 2.7 months during and after March 2011, Dr. Starling and his associates reported (N. Engl. J. Med. 2013 Nov. 27 [doi: 10.1056/NEJMoa1313385]).
The investigators also reviewed serial measurements of lactate dehydrogenase (LDH) that had been taken in recipients of 568 of the devices. Elevated LDH indicates hemolysis that may herald impending thrombosis.
"The graph of the occurrence of LDH levels above 1000 IU per liter ... was nearly superimposable on the graph of the occurrence of confirmed pump thrombosis. The LDH data showed a parallel tendency for elevations to occur early after implantation beginning in approximately March 2011," they said.
The LDH level typically rose from an average of 540 IU/L to an average of 1,490 IU/L during the weeks leading up to LVAD thrombosis at all three medical centers. This confirms that LDH level is a useful clinical biomarker of hemolysis associated with LVAD thrombosis, the researchers said.
Of the 72 pump thromboses, 11 were managed by heart transplantation and 21 by pump replacement. Of the remaining 40 thromboses, 2 were managed by LVAD removal because left ventricular function had improved, and 38 were managed medically, with augmentation of anticoagulation therapy and thrombolytic agents. This stabilized the clinical course in some patients, but others elected withdrawal of care, citing "futility."
Mortality was 48% among the patients who could not be managed by heart transplantation or pump replacement, and this elevated rate was consistent across the three medical centers.
The reasons for this abrupt, dramatic rise in thromboses associated with the HeartMate II are not known. There were no changes in LVAD implantation techniques at any of the three medical centers during the course of this study, "and we could find no association between pump thrombosis and the surgeon performing the implantation." The design of the HeartMate II was changed during this interval – "modification of the outflow graft and bend relief, inflow conduit, and software" was introduced – but these changes have not been linked to pump thrombosis as yet.
Dr. Starling and his associates did note the deposition of fibrin and denatured protein around the inflow bearing, which could narrow the inflow pathway, "increasing shear stress on the red cells and, if the deposition is large enough, decreasing the ability of the pump to unload the left ventricle." But it remains to be seen whether this or other factors played a role.
"Further investigation of predisposing patient and device factors and preventive and therapeutic strategies are urgently needed to resolve this important safety issue," the investigators said.
They added that a fourth cardiology center, the University of Pennsylvania, Philadelphia, found a similar pattern in a preliminary analysis that was reported as the article went to press. In that report on 150 HeartMate II LVADs implanted in 148 patients between November 2005 and September 2013, there were 15 thrombotic events. "Similar to the findings in our study, the event rate has increased abruptly and unexpectedly, with a rate of confirmed thrombosis that continues to rise," Dr. Starling and his associates said.
Dr. Starling reported ties to Thoratec and HeartWare, and his associates reported ties to Thoratec, HeartWare, Abiomed, and Syncardia.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major finding: The rate of pump thrombosis was stable at approximately 2.2% for several years, then rose steeply after March 2011 to 8.4%; the median interval from implantation to pump thrombosis, which had been stable at 18.6 months for several years, plummeted to 2.7 months after March 2011.
Data source: A retrospective study involving 837 recipients of 895 HeartMate II LVADs at three U.S. medical centers during 2004-2013, in which 72 LVAD thromboses were confirmed in 66 patients and an additional 36 thromboses were suspected.
Disclosures: Dr. Starling reported ties to Thoratec and HeartWare, and his associates reported ties to Thoratec, HeartWare, Abiomed, and Syncardia.
Advanced pacing slows AF progression in bradycardia
DALLAS – Enhanced pacemaker technology sharply reduced progression of nonpermanent atrial fibrillation to permanent AF in patients with bradycardia and sinus node disease in the large international, randomized MINERVA trial.
In the MINERVA (Minimize Right Ventricular Pacing to Prevent Atrial Fibrillation and Heart Failure) study, the use of dual-chamber pacemakers containing features for atrial preventive pacing and atrial antitachycardia pacing, called DDDRPs, plus managed ventricular pacing (MVP) resulted in a 61% reduction in the incidence of permanent AF during 2 years of prospective follow-up, compared with conventional dual-chamber pacing, Dr. Giuseppe Boriani reported at the American Heart Association scientific sessions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In addition, patients in the enhanced-pacing group experienced a 52% reduction in AF-related hospitalizations and emergency department visits, as well as a 49% decrease in atrial cardioversions relative to controls, added Dr. Boriani of the University of Bologna (Italy).
"This is the first study to show that using these enhanced pacing features in combination not only delays the AF disease progression, but also has an impact on health care utilization," he noted. "With this solid evidence of beneficial results, I think the practice guidelines probably should be updated to state this type of device should be implanted for sinus node disease in patients with a history of atrial fibrillation."
MINERVA included 1,166 patients at 63 European, Asian, and Middle Eastern centers; all had bradycardia, sinus node disease, and a history of nonpermanent AF. They received a commercially available Medtronic dual-chamber pacemaker that was randomized single-blind to operate using both the DDDRP and MVP features, the MVP alone, or conventional dual-chamber pacing with neither enhanced feature.
At 2 years, the primary composite endpoint of death, cardiovascular hospitalization, or permanent AF had occurred in 19.8% of the DDDRP plus MVP group. That amounted to a significant 26% reduction in the endpoint compared with the 26.5% rate in the controls on standard dual-chamber pacing. The 21.4% rate in patients whose device used only the MVP algorithm was not significantly different from the rate in controls.
Most strikingly, the 2-year incidence of progression to permanent AF was 3.8% in patients with the enhanced pacing features, compared with 9.2% in those assigned to conventional dual-chamber pacing, for a 61% relative risk reduction. This means 20 patients would need to be treated for 2 years with a pacemaker utilizing the advanced pacing features in order to prevent one additional case of permanent AF.
In addition, patients whose pacemakers utilized rate response and antitachycardia pacing plus MVP reported better quality of life and less fatigue than did those in the other two study arms.
Dr. Boriani estimated that of the 170,000 patients each year in the United States who undergo pacemaker implantation for bradycardia, roughly 25,000 have sinus node disease and a history of AF and would thus now be considered strong candidates for the enhanced pacing features.
Discussant Dr. Anthony Tang explained that it has been known for years that pacemaker algorithms designed to increase the atrial pacing rate above the intrinsic sinus rate can prevent events that trigger AF. The problem has been that this atrial pacing can have the side effect of also increasing ventricular pacing, which can initiate AF, thus canceling the advantage of the atrial preventive pacing. The MVP algorithm decreases this unnecessary pacing in the right ventricle, with the resultant benefits seen in MINERVA.
In his view, the enhanced pacing features used in MINERVA represent a very good option for patients with severe sinus node dysfunction but preserved atrioventricular node conduction, that is, patients who need atrial pacing for long sinus pauses but don’t need much ventricular pacing.
In contrast, for patients with an indication for a pacemaker but who only occasionally need pacing, such as those with a rare sinus pause or occasional AV block, a simple single-chamber ventricular pacemaker will generally do. For those with second- or third-degree AV block with left ventricular dysfunction and who need both atrial and ventricular pacing most of the time, a cardiac resynchronization therapy device plus either a pacemaker or a defibrillator is appropriate, depending upon the severity of the left ventricular dysfunction, according to Dr. Tang, professor of medicine and chair of cardiovascular population health at Western University, London, Ont.
Discussant Dr. Timothy J. Gardner wasn’t bowled over by the number-needed-to-treat (NNT) of 20 in MINERVA.
"That seems a very modest impact. I wonder from a health care/societal benefit standpoint whether an NNT of 20 for a more complex and expensive technology is appropriate," challenged Dr. Gardner, a heart surgeon and medical director of the Christiana Care Center for Heart and Vascular Health in Newark, Del.
Dr. Boriani replied that the benefits seen with advanced pacing in this 2-year study will only become more pronounced with longer follow-up.
"Permanent atrial fibrillation is the later stage of irreversible AF, when the arrhythmia becomes untreatable. And it is a marker for adverse events, including heart failure, stroke, and death," he said.
The MINERVA trial was sponsored by Medtronic, which markets the proprietary enhanced pacing technology. Dr. Boriani reported having no relevant financial interests.
DALLAS – Enhanced pacemaker technology sharply reduced progression of nonpermanent atrial fibrillation to permanent AF in patients with bradycardia and sinus node disease in the large international, randomized MINERVA trial.
In the MINERVA (Minimize Right Ventricular Pacing to Prevent Atrial Fibrillation and Heart Failure) study, the use of dual-chamber pacemakers containing features for atrial preventive pacing and atrial antitachycardia pacing, called DDDRPs, plus managed ventricular pacing (MVP) resulted in a 61% reduction in the incidence of permanent AF during 2 years of prospective follow-up, compared with conventional dual-chamber pacing, Dr. Giuseppe Boriani reported at the American Heart Association scientific sessions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In addition, patients in the enhanced-pacing group experienced a 52% reduction in AF-related hospitalizations and emergency department visits, as well as a 49% decrease in atrial cardioversions relative to controls, added Dr. Boriani of the University of Bologna (Italy).
"This is the first study to show that using these enhanced pacing features in combination not only delays the AF disease progression, but also has an impact on health care utilization," he noted. "With this solid evidence of beneficial results, I think the practice guidelines probably should be updated to state this type of device should be implanted for sinus node disease in patients with a history of atrial fibrillation."
MINERVA included 1,166 patients at 63 European, Asian, and Middle Eastern centers; all had bradycardia, sinus node disease, and a history of nonpermanent AF. They received a commercially available Medtronic dual-chamber pacemaker that was randomized single-blind to operate using both the DDDRP and MVP features, the MVP alone, or conventional dual-chamber pacing with neither enhanced feature.
At 2 years, the primary composite endpoint of death, cardiovascular hospitalization, or permanent AF had occurred in 19.8% of the DDDRP plus MVP group. That amounted to a significant 26% reduction in the endpoint compared with the 26.5% rate in the controls on standard dual-chamber pacing. The 21.4% rate in patients whose device used only the MVP algorithm was not significantly different from the rate in controls.
Most strikingly, the 2-year incidence of progression to permanent AF was 3.8% in patients with the enhanced pacing features, compared with 9.2% in those assigned to conventional dual-chamber pacing, for a 61% relative risk reduction. This means 20 patients would need to be treated for 2 years with a pacemaker utilizing the advanced pacing features in order to prevent one additional case of permanent AF.
In addition, patients whose pacemakers utilized rate response and antitachycardia pacing plus MVP reported better quality of life and less fatigue than did those in the other two study arms.
Dr. Boriani estimated that of the 170,000 patients each year in the United States who undergo pacemaker implantation for bradycardia, roughly 25,000 have sinus node disease and a history of AF and would thus now be considered strong candidates for the enhanced pacing features.
Discussant Dr. Anthony Tang explained that it has been known for years that pacemaker algorithms designed to increase the atrial pacing rate above the intrinsic sinus rate can prevent events that trigger AF. The problem has been that this atrial pacing can have the side effect of also increasing ventricular pacing, which can initiate AF, thus canceling the advantage of the atrial preventive pacing. The MVP algorithm decreases this unnecessary pacing in the right ventricle, with the resultant benefits seen in MINERVA.
In his view, the enhanced pacing features used in MINERVA represent a very good option for patients with severe sinus node dysfunction but preserved atrioventricular node conduction, that is, patients who need atrial pacing for long sinus pauses but don’t need much ventricular pacing.
In contrast, for patients with an indication for a pacemaker but who only occasionally need pacing, such as those with a rare sinus pause or occasional AV block, a simple single-chamber ventricular pacemaker will generally do. For those with second- or third-degree AV block with left ventricular dysfunction and who need both atrial and ventricular pacing most of the time, a cardiac resynchronization therapy device plus either a pacemaker or a defibrillator is appropriate, depending upon the severity of the left ventricular dysfunction, according to Dr. Tang, professor of medicine and chair of cardiovascular population health at Western University, London, Ont.
Discussant Dr. Timothy J. Gardner wasn’t bowled over by the number-needed-to-treat (NNT) of 20 in MINERVA.
"That seems a very modest impact. I wonder from a health care/societal benefit standpoint whether an NNT of 20 for a more complex and expensive technology is appropriate," challenged Dr. Gardner, a heart surgeon and medical director of the Christiana Care Center for Heart and Vascular Health in Newark, Del.
Dr. Boriani replied that the benefits seen with advanced pacing in this 2-year study will only become more pronounced with longer follow-up.
"Permanent atrial fibrillation is the later stage of irreversible AF, when the arrhythmia becomes untreatable. And it is a marker for adverse events, including heart failure, stroke, and death," he said.
The MINERVA trial was sponsored by Medtronic, which markets the proprietary enhanced pacing technology. Dr. Boriani reported having no relevant financial interests.
DALLAS – Enhanced pacemaker technology sharply reduced progression of nonpermanent atrial fibrillation to permanent AF in patients with bradycardia and sinus node disease in the large international, randomized MINERVA trial.
In the MINERVA (Minimize Right Ventricular Pacing to Prevent Atrial Fibrillation and Heart Failure) study, the use of dual-chamber pacemakers containing features for atrial preventive pacing and atrial antitachycardia pacing, called DDDRPs, plus managed ventricular pacing (MVP) resulted in a 61% reduction in the incidence of permanent AF during 2 years of prospective follow-up, compared with conventional dual-chamber pacing, Dr. Giuseppe Boriani reported at the American Heart Association scientific sessions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
In addition, patients in the enhanced-pacing group experienced a 52% reduction in AF-related hospitalizations and emergency department visits, as well as a 49% decrease in atrial cardioversions relative to controls, added Dr. Boriani of the University of Bologna (Italy).
"This is the first study to show that using these enhanced pacing features in combination not only delays the AF disease progression, but also has an impact on health care utilization," he noted. "With this solid evidence of beneficial results, I think the practice guidelines probably should be updated to state this type of device should be implanted for sinus node disease in patients with a history of atrial fibrillation."
MINERVA included 1,166 patients at 63 European, Asian, and Middle Eastern centers; all had bradycardia, sinus node disease, and a history of nonpermanent AF. They received a commercially available Medtronic dual-chamber pacemaker that was randomized single-blind to operate using both the DDDRP and MVP features, the MVP alone, or conventional dual-chamber pacing with neither enhanced feature.
At 2 years, the primary composite endpoint of death, cardiovascular hospitalization, or permanent AF had occurred in 19.8% of the DDDRP plus MVP group. That amounted to a significant 26% reduction in the endpoint compared with the 26.5% rate in the controls on standard dual-chamber pacing. The 21.4% rate in patients whose device used only the MVP algorithm was not significantly different from the rate in controls.
Most strikingly, the 2-year incidence of progression to permanent AF was 3.8% in patients with the enhanced pacing features, compared with 9.2% in those assigned to conventional dual-chamber pacing, for a 61% relative risk reduction. This means 20 patients would need to be treated for 2 years with a pacemaker utilizing the advanced pacing features in order to prevent one additional case of permanent AF.
In addition, patients whose pacemakers utilized rate response and antitachycardia pacing plus MVP reported better quality of life and less fatigue than did those in the other two study arms.
Dr. Boriani estimated that of the 170,000 patients each year in the United States who undergo pacemaker implantation for bradycardia, roughly 25,000 have sinus node disease and a history of AF and would thus now be considered strong candidates for the enhanced pacing features.
Discussant Dr. Anthony Tang explained that it has been known for years that pacemaker algorithms designed to increase the atrial pacing rate above the intrinsic sinus rate can prevent events that trigger AF. The problem has been that this atrial pacing can have the side effect of also increasing ventricular pacing, which can initiate AF, thus canceling the advantage of the atrial preventive pacing. The MVP algorithm decreases this unnecessary pacing in the right ventricle, with the resultant benefits seen in MINERVA.
In his view, the enhanced pacing features used in MINERVA represent a very good option for patients with severe sinus node dysfunction but preserved atrioventricular node conduction, that is, patients who need atrial pacing for long sinus pauses but don’t need much ventricular pacing.
In contrast, for patients with an indication for a pacemaker but who only occasionally need pacing, such as those with a rare sinus pause or occasional AV block, a simple single-chamber ventricular pacemaker will generally do. For those with second- or third-degree AV block with left ventricular dysfunction and who need both atrial and ventricular pacing most of the time, a cardiac resynchronization therapy device plus either a pacemaker or a defibrillator is appropriate, depending upon the severity of the left ventricular dysfunction, according to Dr. Tang, professor of medicine and chair of cardiovascular population health at Western University, London, Ont.
Discussant Dr. Timothy J. Gardner wasn’t bowled over by the number-needed-to-treat (NNT) of 20 in MINERVA.
"That seems a very modest impact. I wonder from a health care/societal benefit standpoint whether an NNT of 20 for a more complex and expensive technology is appropriate," challenged Dr. Gardner, a heart surgeon and medical director of the Christiana Care Center for Heart and Vascular Health in Newark, Del.
Dr. Boriani replied that the benefits seen with advanced pacing in this 2-year study will only become more pronounced with longer follow-up.
"Permanent atrial fibrillation is the later stage of irreversible AF, when the arrhythmia becomes untreatable. And it is a marker for adverse events, including heart failure, stroke, and death," he said.
The MINERVA trial was sponsored by Medtronic, which markets the proprietary enhanced pacing technology. Dr. Boriani reported having no relevant financial interests.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: Patients with bradycardia, sinus node disease, and a history of atrial fibrillation who were implanted with a dual-chamber pacemaker utilizing enhanced pacing features showed a 61% reduction in progression to permanent AF over 2 years, compared with those randomized to conventional dual-chamber pacing.
Data source: The MINERVA trial, a single-blind, randomized, international, prospective, 2-year trial conducted in 1,166 patients.
Disclosures: The MINERVA trial was sponsored by Medtronic, which markets the proprietary enhanced pacing technology. Dr. Boriani reported having no relevant financial interests.
Diastolic heart failure and TOPCAT
The TOPCAT study, reported at the recent American Heart Association meeting in Dallas, examined the murky world of our understanding of heart failure occurring in patients with preserved left ventricular ejection fraction.
That seeming paradox has been the subject of physiologic and therapeutic controversy for some time. The realization that at least half of the patients admitted to the hospital with heart failure have normal or even supernormal left ventricular ejection fraction (HFpEF) has raised the therapeutic importance of this clinical entity. Of even more importance is the fact that patients with HFpEF exhibit morbidity and mortality similar to those heart failure patients with reduced left ventricular ejection fraction (HFrEF).
In an epidemiologic study in Olmsted County, Minnesota (N. Engl. J. Med. 2006;355:251-9), the 1-year mortality was 29% for HFpEF and 32% for HFrEF. Patients with HFpEF were more likely to be female (65.7% vs. 34.6%) and to have hypertension and atrial fibrillation than were those with HFrEF (62.7% vs. 48% and 41.3% vs. 28.5%, respectively).
Although we have significantly impacted mortality in patients who have HFrEF with the use of cardiac resynchronization therapy, implantable cardiac defibrillators, and medical therapy with beta-blockers and renin angiotensin inhibitors, we have failed to modify clinical outcomes in patients with HFpEF.
This has not been for a lack of trying. Several randomized clinical trials have been conducted with all of the drugs currently being used for HFrEF without any definitive results. An important problem in treating this population has been the heterogeneity of patients and multiple comorbidities, including chronic renal and pulmonary disease, acute hypertension, and atrial fibrillation that patients with HFpEF experience with the acute event. In addition, many of these patients are already receiving a multiplicity of concurrent therapies that have been approved for HFrEF for management.
Our understanding of the pathophysiology of HFpEF also remains cloudy. Both left and right ventricular hypertrophy with concomitant decrease in ventricular diastolic relaxation is the common observed echocardiographic abnormality. We have not as yet developed therapy for the treatment of diastolic dysfunction. Aldosterone antagonists, previously shown to be beneficial in patients with HFrEF, have emerged as likely candidates to improve HFpEF. Small clinical studies have shown improvement in diastolic function in elderly patients with hypertension and chronic renal disease. Consequently, the National Heart, Lung, and Blood Institute embarked on the TOPCAT study in 2006.
TOPCAT randomized 3,345 symptomatic heart failure patients who had a heart failure hospitalization in the previous year and with evidence of fluid retention, a left ventricular ejection fraction of more than 45%, controlled systolic blood pressure of less than 140 mm Hg, and elevated brain natriuretic peptide to treatment with placebo or spironolactone at 25 or 50 mg daily. A history of hypertension was present in 91%, coronary artery disease in 57%, atrial fibrillation in 35%, chronic renal disease in 35%, and diabetes in 32%. Patients included in the study had a mean LVEF of 56%; two thirds were in New York Heart Association class II and one third were in NYHA class III.
Over 80% of patients were receiving an ACE inhibitor or angiotensin receptor blocker, beta-blockers, and a diuretic. The mean dose of spironolactone was 25 mg. There was no significant difference in the primary outcome of cardiovascular death, nonfatal hospitalization or resuscitated cardiac arrest in the placebo and treated groups (20.4% and 18.6%, respectively). There was a significant decrease in heart failure hospitalization in the placebo compared to spironolactone patients (14.2% vs. 12.0%; P = .042). Both hyperkalemia greater than 5.5 mmol/L and an increase in serum creatinine were observed in the treated patients.
The striking observation in this trial, as it has been in previous trials, is the disparity between the epidemiologic mortality and the randomized controlled trial experience: 29% annual mortality in Olmsted County, compared with the 10.2% three-year mortality in TOPCAT. It appears that we are studying two separate diseases. And we are. After all the exclusion criteria included in the design of TOPCAT, we are unable to encapsulate the population at risk in this complex heart failure syndrome.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The TOPCAT study, reported at the recent American Heart Association meeting in Dallas, examined the murky world of our understanding of heart failure occurring in patients with preserved left ventricular ejection fraction.
That seeming paradox has been the subject of physiologic and therapeutic controversy for some time. The realization that at least half of the patients admitted to the hospital with heart failure have normal or even supernormal left ventricular ejection fraction (HFpEF) has raised the therapeutic importance of this clinical entity. Of even more importance is the fact that patients with HFpEF exhibit morbidity and mortality similar to those heart failure patients with reduced left ventricular ejection fraction (HFrEF).
In an epidemiologic study in Olmsted County, Minnesota (N. Engl. J. Med. 2006;355:251-9), the 1-year mortality was 29% for HFpEF and 32% for HFrEF. Patients with HFpEF were more likely to be female (65.7% vs. 34.6%) and to have hypertension and atrial fibrillation than were those with HFrEF (62.7% vs. 48% and 41.3% vs. 28.5%, respectively).
Although we have significantly impacted mortality in patients who have HFrEF with the use of cardiac resynchronization therapy, implantable cardiac defibrillators, and medical therapy with beta-blockers and renin angiotensin inhibitors, we have failed to modify clinical outcomes in patients with HFpEF.
This has not been for a lack of trying. Several randomized clinical trials have been conducted with all of the drugs currently being used for HFrEF without any definitive results. An important problem in treating this population has been the heterogeneity of patients and multiple comorbidities, including chronic renal and pulmonary disease, acute hypertension, and atrial fibrillation that patients with HFpEF experience with the acute event. In addition, many of these patients are already receiving a multiplicity of concurrent therapies that have been approved for HFrEF for management.
Our understanding of the pathophysiology of HFpEF also remains cloudy. Both left and right ventricular hypertrophy with concomitant decrease in ventricular diastolic relaxation is the common observed echocardiographic abnormality. We have not as yet developed therapy for the treatment of diastolic dysfunction. Aldosterone antagonists, previously shown to be beneficial in patients with HFrEF, have emerged as likely candidates to improve HFpEF. Small clinical studies have shown improvement in diastolic function in elderly patients with hypertension and chronic renal disease. Consequently, the National Heart, Lung, and Blood Institute embarked on the TOPCAT study in 2006.
TOPCAT randomized 3,345 symptomatic heart failure patients who had a heart failure hospitalization in the previous year and with evidence of fluid retention, a left ventricular ejection fraction of more than 45%, controlled systolic blood pressure of less than 140 mm Hg, and elevated brain natriuretic peptide to treatment with placebo or spironolactone at 25 or 50 mg daily. A history of hypertension was present in 91%, coronary artery disease in 57%, atrial fibrillation in 35%, chronic renal disease in 35%, and diabetes in 32%. Patients included in the study had a mean LVEF of 56%; two thirds were in New York Heart Association class II and one third were in NYHA class III.
Over 80% of patients were receiving an ACE inhibitor or angiotensin receptor blocker, beta-blockers, and a diuretic. The mean dose of spironolactone was 25 mg. There was no significant difference in the primary outcome of cardiovascular death, nonfatal hospitalization or resuscitated cardiac arrest in the placebo and treated groups (20.4% and 18.6%, respectively). There was a significant decrease in heart failure hospitalization in the placebo compared to spironolactone patients (14.2% vs. 12.0%; P = .042). Both hyperkalemia greater than 5.5 mmol/L and an increase in serum creatinine were observed in the treated patients.
The striking observation in this trial, as it has been in previous trials, is the disparity between the epidemiologic mortality and the randomized controlled trial experience: 29% annual mortality in Olmsted County, compared with the 10.2% three-year mortality in TOPCAT. It appears that we are studying two separate diseases. And we are. After all the exclusion criteria included in the design of TOPCAT, we are unable to encapsulate the population at risk in this complex heart failure syndrome.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The TOPCAT study, reported at the recent American Heart Association meeting in Dallas, examined the murky world of our understanding of heart failure occurring in patients with preserved left ventricular ejection fraction.
That seeming paradox has been the subject of physiologic and therapeutic controversy for some time. The realization that at least half of the patients admitted to the hospital with heart failure have normal or even supernormal left ventricular ejection fraction (HFpEF) has raised the therapeutic importance of this clinical entity. Of even more importance is the fact that patients with HFpEF exhibit morbidity and mortality similar to those heart failure patients with reduced left ventricular ejection fraction (HFrEF).
In an epidemiologic study in Olmsted County, Minnesota (N. Engl. J. Med. 2006;355:251-9), the 1-year mortality was 29% for HFpEF and 32% for HFrEF. Patients with HFpEF were more likely to be female (65.7% vs. 34.6%) and to have hypertension and atrial fibrillation than were those with HFrEF (62.7% vs. 48% and 41.3% vs. 28.5%, respectively).
Although we have significantly impacted mortality in patients who have HFrEF with the use of cardiac resynchronization therapy, implantable cardiac defibrillators, and medical therapy with beta-blockers and renin angiotensin inhibitors, we have failed to modify clinical outcomes in patients with HFpEF.
This has not been for a lack of trying. Several randomized clinical trials have been conducted with all of the drugs currently being used for HFrEF without any definitive results. An important problem in treating this population has been the heterogeneity of patients and multiple comorbidities, including chronic renal and pulmonary disease, acute hypertension, and atrial fibrillation that patients with HFpEF experience with the acute event. In addition, many of these patients are already receiving a multiplicity of concurrent therapies that have been approved for HFrEF for management.
Our understanding of the pathophysiology of HFpEF also remains cloudy. Both left and right ventricular hypertrophy with concomitant decrease in ventricular diastolic relaxation is the common observed echocardiographic abnormality. We have not as yet developed therapy for the treatment of diastolic dysfunction. Aldosterone antagonists, previously shown to be beneficial in patients with HFrEF, have emerged as likely candidates to improve HFpEF. Small clinical studies have shown improvement in diastolic function in elderly patients with hypertension and chronic renal disease. Consequently, the National Heart, Lung, and Blood Institute embarked on the TOPCAT study in 2006.
TOPCAT randomized 3,345 symptomatic heart failure patients who had a heart failure hospitalization in the previous year and with evidence of fluid retention, a left ventricular ejection fraction of more than 45%, controlled systolic blood pressure of less than 140 mm Hg, and elevated brain natriuretic peptide to treatment with placebo or spironolactone at 25 or 50 mg daily. A history of hypertension was present in 91%, coronary artery disease in 57%, atrial fibrillation in 35%, chronic renal disease in 35%, and diabetes in 32%. Patients included in the study had a mean LVEF of 56%; two thirds were in New York Heart Association class II and one third were in NYHA class III.
Over 80% of patients were receiving an ACE inhibitor or angiotensin receptor blocker, beta-blockers, and a diuretic. The mean dose of spironolactone was 25 mg. There was no significant difference in the primary outcome of cardiovascular death, nonfatal hospitalization or resuscitated cardiac arrest in the placebo and treated groups (20.4% and 18.6%, respectively). There was a significant decrease in heart failure hospitalization in the placebo compared to spironolactone patients (14.2% vs. 12.0%; P = .042). Both hyperkalemia greater than 5.5 mmol/L and an increase in serum creatinine were observed in the treated patients.
The striking observation in this trial, as it has been in previous trials, is the disparity between the epidemiologic mortality and the randomized controlled trial experience: 29% annual mortality in Olmsted County, compared with the 10.2% three-year mortality in TOPCAT. It appears that we are studying two separate diseases. And we are. After all the exclusion criteria included in the design of TOPCAT, we are unable to encapsulate the population at risk in this complex heart failure syndrome.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
TOPCAT: Spironolactone cuts hospitalizations for diastolic heart failure
DALLAS – Spironolactone did not hit a home run in the large international "treatment of preserved cardiac function heart failure with an aldosterone antagonist" (TOPCAT) trial, but it did knock out a solid single in the form of significantly reduced hospitalizations for this extremely common, chronic, high morbidity/mortality condition.
It was this positive result for an important prespecified secondary outcome that enabled TOPCAT to avoid becoming roadkill. Technically, TOPCAT was a negative clinical trial in that spironolactone did not significantly outperform placebo on the primary composite outcome of cardiovascular mortality, heart failure hospitalization, or aborted cardiac arrest.
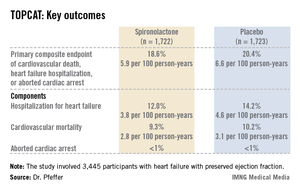
Yet that negative primary outcome was controversial: The aldosterone antagonist actually showed a significant positive result for the composite endpoint in North and South American participants, yet the results were resoundingly negative – and also considerably out of whack with the characteristic arc of progressive heart failure – among the nearly one-half of TOPCAT participants in Russia and the Republic of Georgia.
"What happened in Russia and Georgia we just don’t understand," Dr. Bertram Pitt, TOPCAT steering committee chair, said in an interview, shaking his head. "The event rate with placebo in Eastern Europe was so low it’s not compatible with anything we know about heart failure. The signs and symptoms of HFpEF [heart failure with preserved ejection fraction] are nonspecific; they can be due to obesity, lung disease, and other things. Clearly there are some people getting into the major trials of HFpEF that probably don’t have it."
TOPCAT was a randomized, double-blind clinical trial comprising 3,445 participants with symptomatic HFpEF at 250 sites in the United States and five other countries. They were randomized to spironolactone or placebo and followed prospectively for a mean of 3.3 years. The starting dose of the aldosterone antagonist was 15 mg/day, with a target of 30 mg/day. The drug could be titrated within the range of 15-45 mg/day. Eight months into the trial, the mean daily dose was 25 mg.
Presenting the TOPCAT results at the American Heart Association scientific sessions, Dr. Marc A. Pfeffer noted that the primary composite endpoint occurred in 20.4% of placebo-treated controls and 18.6% on spironolactone, a statistically nonsignificant difference. In contrast, the 17% reduction in the rate of hospitalization for HFpEF in the spironolactone group relative to controls was significant (P = .04). Moreover, the spironolactone-treated patients had a collective 394 HFpEF hospitalizations, markedly fewer than the 475 in controls. This translated to a hospitalization for heart failure with a preserved left ventricular ejection fraction occurring at a rate of 3.8 per 100 person-years in patients randomized to spironolactone, compared with the 4.6 per 100 person-years in placebo-treated controls.
Hyperkalemia in excess of 5.5 mmol/L occurred in 18.7% of the spironolactone group, twice the rate of controls (9.1%). And the incidence of a creatinine level more than double the upper limit of normal was 49% greater in the spironolactone group. That said, neither of these laboratory abnormalities resulted in any serious adverse consequences because investigators adjusted the dose in response, explained Dr. Pfeffer, professor of medicine at Harvard University, Boston.
He drew special attention to two points: The primary composite event rate in placebo-treated patients in the Americas was 31.8% consistent with what has been seen in other studies of HFpEF – compared to a mere 8.4% in Eastern Europe. And patients who qualified for TOPCAT on the basis of an elevated natriuretic peptide level had a primary endpoint rate of 15.9% with spironolactone, a highly significant 35% reduction compared with the 23.6% in controls, suggesting that an elevated baseline natriuretic peptide level may be a biomarker useful in identifying those HFpEF patients most likely to respond to an aldosterone antagonist.
Dr. Pfeffer said that because the pharmaceutical industry has zero interest in spironolactone and the National Heart, Lung, and Blood Institute (NHLBI), which sponsored TOPCAT, has finite resources, he doubts there will be any further large studies of the drug in HFpEF.
"One is going to have to make decisions based on this trial. I don’t see another trial behind us," the cardiologist said.
And while TOPCAT was flawed, he said it contains a compelling message for clinicians: "I think we have an important finding here. We’re very confident that with this generic medication, which costs pennies per day, we can reduce hospitalizations for heart failure, which are the major burden in patients with HFpEF."
Discussant Dr. Margaret M. Redfield was more cautious. While there was a sound rationale for studying spironolactone in HFpEF based upon its impressive benefits in systolic heart failure as shown in earlier landmark clinical trials, given that the drug didn’t result in a significant reduction in all-cause hospitalizations, she said she wants to see evidence of improved patient-centered outcomes, such as quality of life, before prescribing spironolactone for HFpEF.
"One has to worry that the problems with worsening renal function and hyperkalemia may be much more common in clinical practice than in the highly monitored environment of a clinical trial," added Dr. Redfield, professor of medicine at the Mayo Clinic, Rochester, Minn.
Other heart failure experts not involved in TOPCAT took a more positive view of the study.
Dr. Clyde W. Yancy, AHA spokesperson, said in an interview that HFpEF is probably even more common than systolic heart failure, and it is a disease for which physicians have had no proven-effective treatments.
"You can almost justifiably say, ‘Let’s just look at the Americas, where patients had event rates that are consistent with the disease we think we understand.’ And it looks like there’s a signal there. I think that there’s enough evidence in TOPCAT for the clinical pragmatist to be able to be comfortable that spironolactone is probably beneficial and can be given safely. If you are convinced you can give it safely in your own clinical scenario, I think you should use it," said Dr. Yancy, professor of medicine and chief of cardiology at Northwestern University, Chicago.
Dr. Marco Metra, a cardiologist at the University of Brescia (Italy), said he interprets the TOPCAT results as an indication for prescribing spironolactone, at least in HFpEF patients with high natriuretic peptide levels or multiple heart failure hospitalizations.
Dr. Pitt, emeritus professor of cardiovascular medicine at the University of Michigan, Ann Arbor, emphasized that in prescribing spironolactone, whether for HFpEF or systolic heart failure, it’s obligatory to measure potassium and creatinine levels at baseline, when changing the dose, and at each routine follow-up visit, titrating in response to the results. Failure to do so is akin to prescribing warfarin for a patient with atrial fibrillation and then never measuring the INR (international normalized ratio) he said.
TOPCAT was sponsored by the National, Heart, Lung, and Blood Institute. Dr. Pfeffer and Dr. Pitt serve as consultants to numerous pharmaceutical companies that had no involvement in the trial.
DALLAS – Spironolactone did not hit a home run in the large international "treatment of preserved cardiac function heart failure with an aldosterone antagonist" (TOPCAT) trial, but it did knock out a solid single in the form of significantly reduced hospitalizations for this extremely common, chronic, high morbidity/mortality condition.
It was this positive result for an important prespecified secondary outcome that enabled TOPCAT to avoid becoming roadkill. Technically, TOPCAT was a negative clinical trial in that spironolactone did not significantly outperform placebo on the primary composite outcome of cardiovascular mortality, heart failure hospitalization, or aborted cardiac arrest.
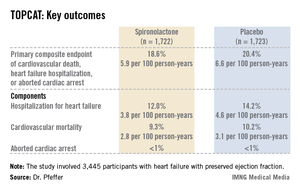
Yet that negative primary outcome was controversial: The aldosterone antagonist actually showed a significant positive result for the composite endpoint in North and South American participants, yet the results were resoundingly negative – and also considerably out of whack with the characteristic arc of progressive heart failure – among the nearly one-half of TOPCAT participants in Russia and the Republic of Georgia.
"What happened in Russia and Georgia we just don’t understand," Dr. Bertram Pitt, TOPCAT steering committee chair, said in an interview, shaking his head. "The event rate with placebo in Eastern Europe was so low it’s not compatible with anything we know about heart failure. The signs and symptoms of HFpEF [heart failure with preserved ejection fraction] are nonspecific; they can be due to obesity, lung disease, and other things. Clearly there are some people getting into the major trials of HFpEF that probably don’t have it."
TOPCAT was a randomized, double-blind clinical trial comprising 3,445 participants with symptomatic HFpEF at 250 sites in the United States and five other countries. They were randomized to spironolactone or placebo and followed prospectively for a mean of 3.3 years. The starting dose of the aldosterone antagonist was 15 mg/day, with a target of 30 mg/day. The drug could be titrated within the range of 15-45 mg/day. Eight months into the trial, the mean daily dose was 25 mg.
Presenting the TOPCAT results at the American Heart Association scientific sessions, Dr. Marc A. Pfeffer noted that the primary composite endpoint occurred in 20.4% of placebo-treated controls and 18.6% on spironolactone, a statistically nonsignificant difference. In contrast, the 17% reduction in the rate of hospitalization for HFpEF in the spironolactone group relative to controls was significant (P = .04). Moreover, the spironolactone-treated patients had a collective 394 HFpEF hospitalizations, markedly fewer than the 475 in controls. This translated to a hospitalization for heart failure with a preserved left ventricular ejection fraction occurring at a rate of 3.8 per 100 person-years in patients randomized to spironolactone, compared with the 4.6 per 100 person-years in placebo-treated controls.
Hyperkalemia in excess of 5.5 mmol/L occurred in 18.7% of the spironolactone group, twice the rate of controls (9.1%). And the incidence of a creatinine level more than double the upper limit of normal was 49% greater in the spironolactone group. That said, neither of these laboratory abnormalities resulted in any serious adverse consequences because investigators adjusted the dose in response, explained Dr. Pfeffer, professor of medicine at Harvard University, Boston.
He drew special attention to two points: The primary composite event rate in placebo-treated patients in the Americas was 31.8% consistent with what has been seen in other studies of HFpEF – compared to a mere 8.4% in Eastern Europe. And patients who qualified for TOPCAT on the basis of an elevated natriuretic peptide level had a primary endpoint rate of 15.9% with spironolactone, a highly significant 35% reduction compared with the 23.6% in controls, suggesting that an elevated baseline natriuretic peptide level may be a biomarker useful in identifying those HFpEF patients most likely to respond to an aldosterone antagonist.
Dr. Pfeffer said that because the pharmaceutical industry has zero interest in spironolactone and the National Heart, Lung, and Blood Institute (NHLBI), which sponsored TOPCAT, has finite resources, he doubts there will be any further large studies of the drug in HFpEF.
"One is going to have to make decisions based on this trial. I don’t see another trial behind us," the cardiologist said.
And while TOPCAT was flawed, he said it contains a compelling message for clinicians: "I think we have an important finding here. We’re very confident that with this generic medication, which costs pennies per day, we can reduce hospitalizations for heart failure, which are the major burden in patients with HFpEF."
Discussant Dr. Margaret M. Redfield was more cautious. While there was a sound rationale for studying spironolactone in HFpEF based upon its impressive benefits in systolic heart failure as shown in earlier landmark clinical trials, given that the drug didn’t result in a significant reduction in all-cause hospitalizations, she said she wants to see evidence of improved patient-centered outcomes, such as quality of life, before prescribing spironolactone for HFpEF.
"One has to worry that the problems with worsening renal function and hyperkalemia may be much more common in clinical practice than in the highly monitored environment of a clinical trial," added Dr. Redfield, professor of medicine at the Mayo Clinic, Rochester, Minn.
Other heart failure experts not involved in TOPCAT took a more positive view of the study.
Dr. Clyde W. Yancy, AHA spokesperson, said in an interview that HFpEF is probably even more common than systolic heart failure, and it is a disease for which physicians have had no proven-effective treatments.
"You can almost justifiably say, ‘Let’s just look at the Americas, where patients had event rates that are consistent with the disease we think we understand.’ And it looks like there’s a signal there. I think that there’s enough evidence in TOPCAT for the clinical pragmatist to be able to be comfortable that spironolactone is probably beneficial and can be given safely. If you are convinced you can give it safely in your own clinical scenario, I think you should use it," said Dr. Yancy, professor of medicine and chief of cardiology at Northwestern University, Chicago.
Dr. Marco Metra, a cardiologist at the University of Brescia (Italy), said he interprets the TOPCAT results as an indication for prescribing spironolactone, at least in HFpEF patients with high natriuretic peptide levels or multiple heart failure hospitalizations.
Dr. Pitt, emeritus professor of cardiovascular medicine at the University of Michigan, Ann Arbor, emphasized that in prescribing spironolactone, whether for HFpEF or systolic heart failure, it’s obligatory to measure potassium and creatinine levels at baseline, when changing the dose, and at each routine follow-up visit, titrating in response to the results. Failure to do so is akin to prescribing warfarin for a patient with atrial fibrillation and then never measuring the INR (international normalized ratio) he said.
TOPCAT was sponsored by the National, Heart, Lung, and Blood Institute. Dr. Pfeffer and Dr. Pitt serve as consultants to numerous pharmaceutical companies that had no involvement in the trial.
DALLAS – Spironolactone did not hit a home run in the large international "treatment of preserved cardiac function heart failure with an aldosterone antagonist" (TOPCAT) trial, but it did knock out a solid single in the form of significantly reduced hospitalizations for this extremely common, chronic, high morbidity/mortality condition.
It was this positive result for an important prespecified secondary outcome that enabled TOPCAT to avoid becoming roadkill. Technically, TOPCAT was a negative clinical trial in that spironolactone did not significantly outperform placebo on the primary composite outcome of cardiovascular mortality, heart failure hospitalization, or aborted cardiac arrest.
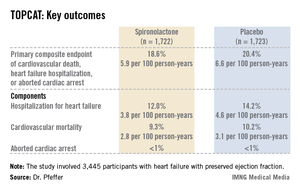
Yet that negative primary outcome was controversial: The aldosterone antagonist actually showed a significant positive result for the composite endpoint in North and South American participants, yet the results were resoundingly negative – and also considerably out of whack with the characteristic arc of progressive heart failure – among the nearly one-half of TOPCAT participants in Russia and the Republic of Georgia.
"What happened in Russia and Georgia we just don’t understand," Dr. Bertram Pitt, TOPCAT steering committee chair, said in an interview, shaking his head. "The event rate with placebo in Eastern Europe was so low it’s not compatible with anything we know about heart failure. The signs and symptoms of HFpEF [heart failure with preserved ejection fraction] are nonspecific; they can be due to obesity, lung disease, and other things. Clearly there are some people getting into the major trials of HFpEF that probably don’t have it."
TOPCAT was a randomized, double-blind clinical trial comprising 3,445 participants with symptomatic HFpEF at 250 sites in the United States and five other countries. They were randomized to spironolactone or placebo and followed prospectively for a mean of 3.3 years. The starting dose of the aldosterone antagonist was 15 mg/day, with a target of 30 mg/day. The drug could be titrated within the range of 15-45 mg/day. Eight months into the trial, the mean daily dose was 25 mg.
Presenting the TOPCAT results at the American Heart Association scientific sessions, Dr. Marc A. Pfeffer noted that the primary composite endpoint occurred in 20.4% of placebo-treated controls and 18.6% on spironolactone, a statistically nonsignificant difference. In contrast, the 17% reduction in the rate of hospitalization for HFpEF in the spironolactone group relative to controls was significant (P = .04). Moreover, the spironolactone-treated patients had a collective 394 HFpEF hospitalizations, markedly fewer than the 475 in controls. This translated to a hospitalization for heart failure with a preserved left ventricular ejection fraction occurring at a rate of 3.8 per 100 person-years in patients randomized to spironolactone, compared with the 4.6 per 100 person-years in placebo-treated controls.
Hyperkalemia in excess of 5.5 mmol/L occurred in 18.7% of the spironolactone group, twice the rate of controls (9.1%). And the incidence of a creatinine level more than double the upper limit of normal was 49% greater in the spironolactone group. That said, neither of these laboratory abnormalities resulted in any serious adverse consequences because investigators adjusted the dose in response, explained Dr. Pfeffer, professor of medicine at Harvard University, Boston.
He drew special attention to two points: The primary composite event rate in placebo-treated patients in the Americas was 31.8% consistent with what has been seen in other studies of HFpEF – compared to a mere 8.4% in Eastern Europe. And patients who qualified for TOPCAT on the basis of an elevated natriuretic peptide level had a primary endpoint rate of 15.9% with spironolactone, a highly significant 35% reduction compared with the 23.6% in controls, suggesting that an elevated baseline natriuretic peptide level may be a biomarker useful in identifying those HFpEF patients most likely to respond to an aldosterone antagonist.
Dr. Pfeffer said that because the pharmaceutical industry has zero interest in spironolactone and the National Heart, Lung, and Blood Institute (NHLBI), which sponsored TOPCAT, has finite resources, he doubts there will be any further large studies of the drug in HFpEF.
"One is going to have to make decisions based on this trial. I don’t see another trial behind us," the cardiologist said.
And while TOPCAT was flawed, he said it contains a compelling message for clinicians: "I think we have an important finding here. We’re very confident that with this generic medication, which costs pennies per day, we can reduce hospitalizations for heart failure, which are the major burden in patients with HFpEF."
Discussant Dr. Margaret M. Redfield was more cautious. While there was a sound rationale for studying spironolactone in HFpEF based upon its impressive benefits in systolic heart failure as shown in earlier landmark clinical trials, given that the drug didn’t result in a significant reduction in all-cause hospitalizations, she said she wants to see evidence of improved patient-centered outcomes, such as quality of life, before prescribing spironolactone for HFpEF.
"One has to worry that the problems with worsening renal function and hyperkalemia may be much more common in clinical practice than in the highly monitored environment of a clinical trial," added Dr. Redfield, professor of medicine at the Mayo Clinic, Rochester, Minn.
Other heart failure experts not involved in TOPCAT took a more positive view of the study.
Dr. Clyde W. Yancy, AHA spokesperson, said in an interview that HFpEF is probably even more common than systolic heart failure, and it is a disease for which physicians have had no proven-effective treatments.
"You can almost justifiably say, ‘Let’s just look at the Americas, where patients had event rates that are consistent with the disease we think we understand.’ And it looks like there’s a signal there. I think that there’s enough evidence in TOPCAT for the clinical pragmatist to be able to be comfortable that spironolactone is probably beneficial and can be given safely. If you are convinced you can give it safely in your own clinical scenario, I think you should use it," said Dr. Yancy, professor of medicine and chief of cardiology at Northwestern University, Chicago.
Dr. Marco Metra, a cardiologist at the University of Brescia (Italy), said he interprets the TOPCAT results as an indication for prescribing spironolactone, at least in HFpEF patients with high natriuretic peptide levels or multiple heart failure hospitalizations.
Dr. Pitt, emeritus professor of cardiovascular medicine at the University of Michigan, Ann Arbor, emphasized that in prescribing spironolactone, whether for HFpEF or systolic heart failure, it’s obligatory to measure potassium and creatinine levels at baseline, when changing the dose, and at each routine follow-up visit, titrating in response to the results. Failure to do so is akin to prescribing warfarin for a patient with atrial fibrillation and then never measuring the INR (international normalized ratio) he said.
TOPCAT was sponsored by the National, Heart, Lung, and Blood Institute. Dr. Pfeffer and Dr. Pitt serve as consultants to numerous pharmaceutical companies that had no involvement in the trial.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: Hospitalization for heart failure with a preserved left ventricular ejection fraction occurred at a rate of 3.8 per 100 person-years in patients randomized to spironolactone, a significant 17% risk reduction compared with the 4.6 per 100 person-years in placebo-treated controls.
Data source: TOPCAT, a randomized, double-blind, six-country clinical trial involving 3,445 patients with symptomatic heart failure and an ejection fraction of 45% or more.
Disclosures:. TOPCAT was sponsored by the National, Heart, Lung, and Blood Institute. Dr. Pfeffer and Dr. Pitt serve as consultants to pharmaceutical companies that had no involvement in the trial.
Improved outcomes with CoreValve in extreme-risk patients
SAN FRANCISCO – Transcatheter aortic valve replacement with the self-expanding CoreValve in patients at extreme surgical risk significantly reduced the rate of death or major stroke at 1 year, from 43% to 26%, in a 487-patient pivotal trial.
The CoreValve Extreme Risk study gathered data from a registry of patients with symptomatic severe aortic stenosis who attempted an iliofemoral implantation procedure with the CoreValve at 40 U.S. sites. Results were compared with an "objective performance goal" derived from two sources: a meta-analysis of five contemporary balloon valvuloplasty series that found a 43% mortality and major stroke rate at 1 year, and the 1-year rate from the PARTNER B trial in inoperable patients (Placement of Aortic Transcatheter Valves, Cohort B), which was 50% but had a lower confidence bound of 43%.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The performance-goal comparison was necessary in the current study because randomizing these patients to medical therapy in a control group is no longer an acceptable option in the United States, Dr. Jeffrey J. Popma said at the Transcatheter Cardiovascular Therapeutics annual meeting.
The 1-year all-cause mortality rate was 24%, and the cardiovascular mortality was 18%, reported Dr. Popma, professor of medicine at Harvard Medical School, Boston.
Two percent of patients developed a major stroke within 1 month and 4% did so within 1 year.
Data from a continued access study involving another 830 extreme-risk patients who received the CoreValve through an iliofemoral approach are showing even better results, with a 16% rate of mortality or major stroke at 6 months, he added.
Among secondary endpoints at 1 year in the main study, 7% of patients developed any kind of stroke, 2% had an MI, 2% need reintervention, 41% had bleeding that met Valve Academic Research Consortium criteria, 8% had major vascular complications, and 27% required implantation of a permanent pacemaker, Dr. Popma reported at the meeting, cosponsored by the American College of Cardiology. Ninety percent of patients improved by at least one New York Heart Association functional class and 60% improved by at least two classes at 1 year of follow-up.
Paravalvular regurgitation of any severity was seen in 53% of patients 1 month after implantation and in 33% at 1 year. Moderate paravalvular leakage (PVL) affected 9% at 1 month and 4% at 1 year, and severe PVL affected 1.6% at 1 month and no patients at 1 year, Dr. Popma said. Among the 11% of patients with moderate PVL at 1 month, 80% of those who survived to 1 year had a reduction in leakage over time.
"We believe that’s why we did not find an association in the study between mild or moderate aortic regurgitation with respect to late-term mortality," though mortality risk was substantially higher with severe regurgitation, he said. One-year mortality rates were 86% with severe PVL and 24% with either moderate or mild PVL, compared with 18% in patients with no PVL.
The improvement in PVL rates over time may be due to use of CT angiography to select appropriate valve sizes for patients and continued expansion of the self-expanding frame over time. "That’s a remarkable finding, and it needs to be confirmed," Dr. Popma said.
The study focused on patients whose severe frailty, comorbidity, or disability put them at extreme risk of at least a 50% chance of death or irreversible morbidity within 30 days had they undergone surgical aortic valve replacement. A second U.S. pivotal trial of the CoreValve is focusing on patients at high (but not extreme) risk.
Most of the sites in the study had no experience with CoreValve before this study, Dr. Michael J. Mack noted at a press briefing. "The results are outstanding, but especially putting it in that light," said Dr. Mack, director of cardiovascular disease for the Baylor Scott & White Health System, Dallas, and a member of the steering committee for the PARTNER trial.
Dr. Popma reported financial associations with Medtronic, which sponsored the study and makes CoreValve, and with six other companies.
On Twitter @sherryboschert
This is a brilliantly executed, rigorously performed study. After doing sham-control studies, as we did, in these extreme-risk patients, it’s difficult to do a randomized trial. I think these investigators did they best that they could. Using a performance goal standard was the right thing to do.
 |
|
I think that the results are good. It’s always difficult to compare study to study. They’re at different points in time, and we learn things over time. The CoreValve device is a lower-profile device, so there were fewer vascular complications, there was less major bleeding. Those things, in fact, can have an impact on 1-year mortality. The overall 1-year mortality was lower than in PARTNER. In PARTNER by intention to treat the mortality rate was 30.7%, and in the CoreValve study it was in the low 20% range. I think that that’s encouraging.
The stroke rates are encouraging. The pacemaker rates are predictable; it’s a by-product of the specific device. The importance of that is debatable, but it’s not really a concern. It was anticipated.
The paravalvular leakage (PVL) rate is interesting. Many studies with CoreValve suggest that either moderate or severe PVL is associated with an increase in late mortality, if not at 1 year later. It’s not a huge sample size; maybe over time with different definitions of PVL we’d begin to see that.
I am surprised by the 30-day to 1-year data that suggest a reduced PVL rate. I can understand how a self-expanding platform might change in the first 30 days; I can’t quite understand how it would change between 1 month and 12 months in a way that PVL would go down.
Martin B. Leon, M.D., is director of the Center for Interventional Vascular Therapy at Columbia University, New York, and served as principal investigator of the PARTNER trial of the competing Sapien valve.
This is a brilliantly executed, rigorously performed study. After doing sham-control studies, as we did, in these extreme-risk patients, it’s difficult to do a randomized trial. I think these investigators did they best that they could. Using a performance goal standard was the right thing to do.
 |
|
I think that the results are good. It’s always difficult to compare study to study. They’re at different points in time, and we learn things over time. The CoreValve device is a lower-profile device, so there were fewer vascular complications, there was less major bleeding. Those things, in fact, can have an impact on 1-year mortality. The overall 1-year mortality was lower than in PARTNER. In PARTNER by intention to treat the mortality rate was 30.7%, and in the CoreValve study it was in the low 20% range. I think that that’s encouraging.
The stroke rates are encouraging. The pacemaker rates are predictable; it’s a by-product of the specific device. The importance of that is debatable, but it’s not really a concern. It was anticipated.
The paravalvular leakage (PVL) rate is interesting. Many studies with CoreValve suggest that either moderate or severe PVL is associated with an increase in late mortality, if not at 1 year later. It’s not a huge sample size; maybe over time with different definitions of PVL we’d begin to see that.
I am surprised by the 30-day to 1-year data that suggest a reduced PVL rate. I can understand how a self-expanding platform might change in the first 30 days; I can’t quite understand how it would change between 1 month and 12 months in a way that PVL would go down.
Martin B. Leon, M.D., is director of the Center for Interventional Vascular Therapy at Columbia University, New York, and served as principal investigator of the PARTNER trial of the competing Sapien valve.
This is a brilliantly executed, rigorously performed study. After doing sham-control studies, as we did, in these extreme-risk patients, it’s difficult to do a randomized trial. I think these investigators did they best that they could. Using a performance goal standard was the right thing to do.
 |
|
I think that the results are good. It’s always difficult to compare study to study. They’re at different points in time, and we learn things over time. The CoreValve device is a lower-profile device, so there were fewer vascular complications, there was less major bleeding. Those things, in fact, can have an impact on 1-year mortality. The overall 1-year mortality was lower than in PARTNER. In PARTNER by intention to treat the mortality rate was 30.7%, and in the CoreValve study it was in the low 20% range. I think that that’s encouraging.
The stroke rates are encouraging. The pacemaker rates are predictable; it’s a by-product of the specific device. The importance of that is debatable, but it’s not really a concern. It was anticipated.
The paravalvular leakage (PVL) rate is interesting. Many studies with CoreValve suggest that either moderate or severe PVL is associated with an increase in late mortality, if not at 1 year later. It’s not a huge sample size; maybe over time with different definitions of PVL we’d begin to see that.
I am surprised by the 30-day to 1-year data that suggest a reduced PVL rate. I can understand how a self-expanding platform might change in the first 30 days; I can’t quite understand how it would change between 1 month and 12 months in a way that PVL would go down.
Martin B. Leon, M.D., is director of the Center for Interventional Vascular Therapy at Columbia University, New York, and served as principal investigator of the PARTNER trial of the competing Sapien valve.
SAN FRANCISCO – Transcatheter aortic valve replacement with the self-expanding CoreValve in patients at extreme surgical risk significantly reduced the rate of death or major stroke at 1 year, from 43% to 26%, in a 487-patient pivotal trial.
The CoreValve Extreme Risk study gathered data from a registry of patients with symptomatic severe aortic stenosis who attempted an iliofemoral implantation procedure with the CoreValve at 40 U.S. sites. Results were compared with an "objective performance goal" derived from two sources: a meta-analysis of five contemporary balloon valvuloplasty series that found a 43% mortality and major stroke rate at 1 year, and the 1-year rate from the PARTNER B trial in inoperable patients (Placement of Aortic Transcatheter Valves, Cohort B), which was 50% but had a lower confidence bound of 43%.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The performance-goal comparison was necessary in the current study because randomizing these patients to medical therapy in a control group is no longer an acceptable option in the United States, Dr. Jeffrey J. Popma said at the Transcatheter Cardiovascular Therapeutics annual meeting.
The 1-year all-cause mortality rate was 24%, and the cardiovascular mortality was 18%, reported Dr. Popma, professor of medicine at Harvard Medical School, Boston.
Two percent of patients developed a major stroke within 1 month and 4% did so within 1 year.
Data from a continued access study involving another 830 extreme-risk patients who received the CoreValve through an iliofemoral approach are showing even better results, with a 16% rate of mortality or major stroke at 6 months, he added.
Among secondary endpoints at 1 year in the main study, 7% of patients developed any kind of stroke, 2% had an MI, 2% need reintervention, 41% had bleeding that met Valve Academic Research Consortium criteria, 8% had major vascular complications, and 27% required implantation of a permanent pacemaker, Dr. Popma reported at the meeting, cosponsored by the American College of Cardiology. Ninety percent of patients improved by at least one New York Heart Association functional class and 60% improved by at least two classes at 1 year of follow-up.
Paravalvular regurgitation of any severity was seen in 53% of patients 1 month after implantation and in 33% at 1 year. Moderate paravalvular leakage (PVL) affected 9% at 1 month and 4% at 1 year, and severe PVL affected 1.6% at 1 month and no patients at 1 year, Dr. Popma said. Among the 11% of patients with moderate PVL at 1 month, 80% of those who survived to 1 year had a reduction in leakage over time.
"We believe that’s why we did not find an association in the study between mild or moderate aortic regurgitation with respect to late-term mortality," though mortality risk was substantially higher with severe regurgitation, he said. One-year mortality rates were 86% with severe PVL and 24% with either moderate or mild PVL, compared with 18% in patients with no PVL.
The improvement in PVL rates over time may be due to use of CT angiography to select appropriate valve sizes for patients and continued expansion of the self-expanding frame over time. "That’s a remarkable finding, and it needs to be confirmed," Dr. Popma said.
The study focused on patients whose severe frailty, comorbidity, or disability put them at extreme risk of at least a 50% chance of death or irreversible morbidity within 30 days had they undergone surgical aortic valve replacement. A second U.S. pivotal trial of the CoreValve is focusing on patients at high (but not extreme) risk.
Most of the sites in the study had no experience with CoreValve before this study, Dr. Michael J. Mack noted at a press briefing. "The results are outstanding, but especially putting it in that light," said Dr. Mack, director of cardiovascular disease for the Baylor Scott & White Health System, Dallas, and a member of the steering committee for the PARTNER trial.
Dr. Popma reported financial associations with Medtronic, which sponsored the study and makes CoreValve, and with six other companies.
On Twitter @sherryboschert
SAN FRANCISCO – Transcatheter aortic valve replacement with the self-expanding CoreValve in patients at extreme surgical risk significantly reduced the rate of death or major stroke at 1 year, from 43% to 26%, in a 487-patient pivotal trial.
The CoreValve Extreme Risk study gathered data from a registry of patients with symptomatic severe aortic stenosis who attempted an iliofemoral implantation procedure with the CoreValve at 40 U.S. sites. Results were compared with an "objective performance goal" derived from two sources: a meta-analysis of five contemporary balloon valvuloplasty series that found a 43% mortality and major stroke rate at 1 year, and the 1-year rate from the PARTNER B trial in inoperable patients (Placement of Aortic Transcatheter Valves, Cohort B), which was 50% but had a lower confidence bound of 43%.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The performance-goal comparison was necessary in the current study because randomizing these patients to medical therapy in a control group is no longer an acceptable option in the United States, Dr. Jeffrey J. Popma said at the Transcatheter Cardiovascular Therapeutics annual meeting.
The 1-year all-cause mortality rate was 24%, and the cardiovascular mortality was 18%, reported Dr. Popma, professor of medicine at Harvard Medical School, Boston.
Two percent of patients developed a major stroke within 1 month and 4% did so within 1 year.
Data from a continued access study involving another 830 extreme-risk patients who received the CoreValve through an iliofemoral approach are showing even better results, with a 16% rate of mortality or major stroke at 6 months, he added.
Among secondary endpoints at 1 year in the main study, 7% of patients developed any kind of stroke, 2% had an MI, 2% need reintervention, 41% had bleeding that met Valve Academic Research Consortium criteria, 8% had major vascular complications, and 27% required implantation of a permanent pacemaker, Dr. Popma reported at the meeting, cosponsored by the American College of Cardiology. Ninety percent of patients improved by at least one New York Heart Association functional class and 60% improved by at least two classes at 1 year of follow-up.
Paravalvular regurgitation of any severity was seen in 53% of patients 1 month after implantation and in 33% at 1 year. Moderate paravalvular leakage (PVL) affected 9% at 1 month and 4% at 1 year, and severe PVL affected 1.6% at 1 month and no patients at 1 year, Dr. Popma said. Among the 11% of patients with moderate PVL at 1 month, 80% of those who survived to 1 year had a reduction in leakage over time.
"We believe that’s why we did not find an association in the study between mild or moderate aortic regurgitation with respect to late-term mortality," though mortality risk was substantially higher with severe regurgitation, he said. One-year mortality rates were 86% with severe PVL and 24% with either moderate or mild PVL, compared with 18% in patients with no PVL.
The improvement in PVL rates over time may be due to use of CT angiography to select appropriate valve sizes for patients and continued expansion of the self-expanding frame over time. "That’s a remarkable finding, and it needs to be confirmed," Dr. Popma said.
The study focused on patients whose severe frailty, comorbidity, or disability put them at extreme risk of at least a 50% chance of death or irreversible morbidity within 30 days had they undergone surgical aortic valve replacement. A second U.S. pivotal trial of the CoreValve is focusing on patients at high (but not extreme) risk.
Most of the sites in the study had no experience with CoreValve before this study, Dr. Michael J. Mack noted at a press briefing. "The results are outstanding, but especially putting it in that light," said Dr. Mack, director of cardiovascular disease for the Baylor Scott & White Health System, Dallas, and a member of the steering committee for the PARTNER trial.
Dr. Popma reported financial associations with Medtronic, which sponsored the study and makes CoreValve, and with six other companies.
On Twitter @sherryboschert
AT TCT 2013
Major finding: The rate of all-cause mortality or stroke at 1 year was 26%, compared with an objective performance goal of 43%.
Data source: Study of registry data on 487 patients with symptomatic severe aortic stenosis and attempted CoreValve implantation via iliofemoral access.
Disclosures: Dr. Popma reported financial associations with Medtronic, which sponsored the study and makes CoreValve, and with six other companies.