User login
New HBV model may open door to more effective antivirals
A new mouse model that better represents chronic infection with hepatitis B virus (HBV) in humans may lead to more effective antiviral therapies for HBV, according to investigators.
During human infection, HBV genomes take the form of covalently closed circular DNA (cccDNA), a structure that has thwarted effective antiviral therapy and, until now, creation of an accurate mouse model, reported lead author Zaichao Xu, PhD, of Wuhan (China) University and colleagues.
“As the viral persistence reservoir plays a central role in HBV infection, HBV cccDNA is the key obstacle for a cure,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
Although several previous mouse models have approximated this phenomenon with recombinant cccDNA-like molecules (rcccDNA), the present model is the first to achieve genuine cccDNA, which does not naturally occur in mice.
“Although rcccDNA supports persistent viral replication and antigen expression, the nature of rcccDNA may differ from authentic cccDNA, as additional sequences, like LoxP or attR, were inserted into the HBV genome,” the investigators noted.
The new model was created by first constructing an adeno-associated virus vector carrying a replication-deficient HBV1.04-fold genome (AAV-HBV1.04). When injected into mice, the vector led to cccDNA formation via ataxia-telangiectasia and Rad3-related protein (ATR)–mediated DNA damage response, a finding that was confirmed by blocking the same process with ATR inhibitors.
Immediately after injection, mice tested positive for both hepatitis B e antigen (HBeAg) and hepatitis B surface antigen (HBsAg), with peak concentrations after either 4 or 8 weeks depending on dose. HBV DNA was also detected in serum after injection, and 50% of hepatocytes exhibited HBsAg and hepatitis B core protein (HBc) after 1 week. At week 66, HBsAg, HBeAg, and HBc were still detectable in the liver.
“The expression of HBc could only be observed in the liver, but not in other organs or tissues, suggesting that the AAV-HBV1.04 only targeted the mouse liver,” the investigators wrote.
Further experimentation involving known cccDNA-binding proteins supported the similarity between cccDNA in the mouse model and natural infection.
“These results suggested that the chromatinization and transcriptional activation of cccDNA formed in this model dose not differ from wild-type cccDNA formed through infection.”
Next, Dr. Xu and colleagues demonstrated that the infected mice could serve as a reliable model for antiviral research. One week after injection with the vector, mice were treated with entecavir, polyinosinic-polycytidylic acid (poly[I:C]), or phosphate-buffered saline (PBS; control). As anticipated, entecavir suppressed circulating HBV DNA, but not HBsAg, HBeAg, or HBV cccDNA, whereas treatment with poly(I:C) reduced all HBV markers.
“This novel mouse model will provide a unique platform for studying HBV cccDNA and developing novel antivirals to achieve HBV cure,” the investigators concluded.
The study was supported by the National Natural Science Foundation of China, the Fundamental Research Funds for the Central Universities, Hubei Province’s Outstanding Medical Academic Leader Program, and others. The investigators reported no conflicts of interest.
On the heels of the wondrous development of curative antiviral agents for hepatitis C virus (HCV), renewed attention has been directed to efforts to bring about the cure of HBV. However, this task will hinge on successful elimination of covalently closed circular DNA (cccDNA), a highly stable form of viral DNA that is exceedingly difficult to eliminate. Efforts to develop successful curative strategies will in turn rely on development of small animal models that support HBV cccDNA formation and virus production, which has until recently proved elusive. In the past several years, several mouse HBV models supporting cccDNA formation have been constructed using adeno-associated vector (AAV)–mediated transduction of a linearized HBV genome. Both the AAV-HBV linear episome and cccDNA have been consistently replicated and detected in these models. While they recapitulate the key steps of the viral life cycle, these models do not, however, lend themselves to direct assessment of cccDNA, which have traditionally required detection of cccDNA in the liver.
Raymond T. Chung, MD, is a professor of medicine at Harvard Medical School and director of the Hepatology and Liver Center at Massachusetts General Hospital, both in Boston. He has no conflicts to disclose.
On the heels of the wondrous development of curative antiviral agents for hepatitis C virus (HCV), renewed attention has been directed to efforts to bring about the cure of HBV. However, this task will hinge on successful elimination of covalently closed circular DNA (cccDNA), a highly stable form of viral DNA that is exceedingly difficult to eliminate. Efforts to develop successful curative strategies will in turn rely on development of small animal models that support HBV cccDNA formation and virus production, which has until recently proved elusive. In the past several years, several mouse HBV models supporting cccDNA formation have been constructed using adeno-associated vector (AAV)–mediated transduction of a linearized HBV genome. Both the AAV-HBV linear episome and cccDNA have been consistently replicated and detected in these models. While they recapitulate the key steps of the viral life cycle, these models do not, however, lend themselves to direct assessment of cccDNA, which have traditionally required detection of cccDNA in the liver.
Raymond T. Chung, MD, is a professor of medicine at Harvard Medical School and director of the Hepatology and Liver Center at Massachusetts General Hospital, both in Boston. He has no conflicts to disclose.
On the heels of the wondrous development of curative antiviral agents for hepatitis C virus (HCV), renewed attention has been directed to efforts to bring about the cure of HBV. However, this task will hinge on successful elimination of covalently closed circular DNA (cccDNA), a highly stable form of viral DNA that is exceedingly difficult to eliminate. Efforts to develop successful curative strategies will in turn rely on development of small animal models that support HBV cccDNA formation and virus production, which has until recently proved elusive. In the past several years, several mouse HBV models supporting cccDNA formation have been constructed using adeno-associated vector (AAV)–mediated transduction of a linearized HBV genome. Both the AAV-HBV linear episome and cccDNA have been consistently replicated and detected in these models. While they recapitulate the key steps of the viral life cycle, these models do not, however, lend themselves to direct assessment of cccDNA, which have traditionally required detection of cccDNA in the liver.
Raymond T. Chung, MD, is a professor of medicine at Harvard Medical School and director of the Hepatology and Liver Center at Massachusetts General Hospital, both in Boston. He has no conflicts to disclose.
A new mouse model that better represents chronic infection with hepatitis B virus (HBV) in humans may lead to more effective antiviral therapies for HBV, according to investigators.
During human infection, HBV genomes take the form of covalently closed circular DNA (cccDNA), a structure that has thwarted effective antiviral therapy and, until now, creation of an accurate mouse model, reported lead author Zaichao Xu, PhD, of Wuhan (China) University and colleagues.
“As the viral persistence reservoir plays a central role in HBV infection, HBV cccDNA is the key obstacle for a cure,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
Although several previous mouse models have approximated this phenomenon with recombinant cccDNA-like molecules (rcccDNA), the present model is the first to achieve genuine cccDNA, which does not naturally occur in mice.
“Although rcccDNA supports persistent viral replication and antigen expression, the nature of rcccDNA may differ from authentic cccDNA, as additional sequences, like LoxP or attR, were inserted into the HBV genome,” the investigators noted.
The new model was created by first constructing an adeno-associated virus vector carrying a replication-deficient HBV1.04-fold genome (AAV-HBV1.04). When injected into mice, the vector led to cccDNA formation via ataxia-telangiectasia and Rad3-related protein (ATR)–mediated DNA damage response, a finding that was confirmed by blocking the same process with ATR inhibitors.
Immediately after injection, mice tested positive for both hepatitis B e antigen (HBeAg) and hepatitis B surface antigen (HBsAg), with peak concentrations after either 4 or 8 weeks depending on dose. HBV DNA was also detected in serum after injection, and 50% of hepatocytes exhibited HBsAg and hepatitis B core protein (HBc) after 1 week. At week 66, HBsAg, HBeAg, and HBc were still detectable in the liver.
“The expression of HBc could only be observed in the liver, but not in other organs or tissues, suggesting that the AAV-HBV1.04 only targeted the mouse liver,” the investigators wrote.
Further experimentation involving known cccDNA-binding proteins supported the similarity between cccDNA in the mouse model and natural infection.
“These results suggested that the chromatinization and transcriptional activation of cccDNA formed in this model dose not differ from wild-type cccDNA formed through infection.”
Next, Dr. Xu and colleagues demonstrated that the infected mice could serve as a reliable model for antiviral research. One week after injection with the vector, mice were treated with entecavir, polyinosinic-polycytidylic acid (poly[I:C]), or phosphate-buffered saline (PBS; control). As anticipated, entecavir suppressed circulating HBV DNA, but not HBsAg, HBeAg, or HBV cccDNA, whereas treatment with poly(I:C) reduced all HBV markers.
“This novel mouse model will provide a unique platform for studying HBV cccDNA and developing novel antivirals to achieve HBV cure,” the investigators concluded.
The study was supported by the National Natural Science Foundation of China, the Fundamental Research Funds for the Central Universities, Hubei Province’s Outstanding Medical Academic Leader Program, and others. The investigators reported no conflicts of interest.
A new mouse model that better represents chronic infection with hepatitis B virus (HBV) in humans may lead to more effective antiviral therapies for HBV, according to investigators.
During human infection, HBV genomes take the form of covalently closed circular DNA (cccDNA), a structure that has thwarted effective antiviral therapy and, until now, creation of an accurate mouse model, reported lead author Zaichao Xu, PhD, of Wuhan (China) University and colleagues.
“As the viral persistence reservoir plays a central role in HBV infection, HBV cccDNA is the key obstacle for a cure,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
Although several previous mouse models have approximated this phenomenon with recombinant cccDNA-like molecules (rcccDNA), the present model is the first to achieve genuine cccDNA, which does not naturally occur in mice.
“Although rcccDNA supports persistent viral replication and antigen expression, the nature of rcccDNA may differ from authentic cccDNA, as additional sequences, like LoxP or attR, were inserted into the HBV genome,” the investigators noted.
The new model was created by first constructing an adeno-associated virus vector carrying a replication-deficient HBV1.04-fold genome (AAV-HBV1.04). When injected into mice, the vector led to cccDNA formation via ataxia-telangiectasia and Rad3-related protein (ATR)–mediated DNA damage response, a finding that was confirmed by blocking the same process with ATR inhibitors.
Immediately after injection, mice tested positive for both hepatitis B e antigen (HBeAg) and hepatitis B surface antigen (HBsAg), with peak concentrations after either 4 or 8 weeks depending on dose. HBV DNA was also detected in serum after injection, and 50% of hepatocytes exhibited HBsAg and hepatitis B core protein (HBc) after 1 week. At week 66, HBsAg, HBeAg, and HBc were still detectable in the liver.
“The expression of HBc could only be observed in the liver, but not in other organs or tissues, suggesting that the AAV-HBV1.04 only targeted the mouse liver,” the investigators wrote.
Further experimentation involving known cccDNA-binding proteins supported the similarity between cccDNA in the mouse model and natural infection.
“These results suggested that the chromatinization and transcriptional activation of cccDNA formed in this model dose not differ from wild-type cccDNA formed through infection.”
Next, Dr. Xu and colleagues demonstrated that the infected mice could serve as a reliable model for antiviral research. One week after injection with the vector, mice were treated with entecavir, polyinosinic-polycytidylic acid (poly[I:C]), or phosphate-buffered saline (PBS; control). As anticipated, entecavir suppressed circulating HBV DNA, but not HBsAg, HBeAg, or HBV cccDNA, whereas treatment with poly(I:C) reduced all HBV markers.
“This novel mouse model will provide a unique platform for studying HBV cccDNA and developing novel antivirals to achieve HBV cure,” the investigators concluded.
The study was supported by the National Natural Science Foundation of China, the Fundamental Research Funds for the Central Universities, Hubei Province’s Outstanding Medical Academic Leader Program, and others. The investigators reported no conflicts of interest.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
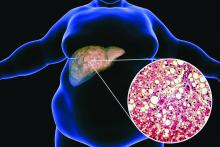
Weekend catch-up sleep may help fatty liver
People who don’t get enough sleep during the week may be able to reduce their risk for nonalcoholic fatty liver disease (NAFLD) by catching up on the weekends, researchers say.
“Our study revealed that people who get enough sleep have a lower risk of developing NAFLD than those who get insufficient sleep,” Sangheun Lee, MD, PhD, from Catholic Kwandong University, Incheon, South Korea, and colleagues wrote in Annals of Hepatology.
However, they cautioned that further research is needed to verify their finding.
Previous studies have associated insufficient sleep with obesity, hypertension, diabetes mellitus, and cardiovascular disease, as well as liver fibrosis.
A busy weekday schedule can make it harder to get enough sleep, and some people try to compensate by sleeping longer on weekends. Studies so far have produced mixed findings on this strategy, with some showing that more sleep on the weekend reduces the risk for obesity, hypertension, and metabolic syndrome, and others showing no effect on metabolic dysregulation or energy balance.
Accessing a nation’s sleep data
To explore the relationship between sleep patterns and NAFLD, Dr. Lee and colleagues analyzed data from Korea National Health and Nutrition Examination Surveys collected from 2008 to 2019. They excluded people aged less than 20 years, those with hepatitis B or C infections, liver cirrhosis or liver cancer, shift workers and others who “slept irregularly,” and those who consumed alcohol excessively, leaving a cohort of 101,138 participants.
The survey didn’t distinguish between sleep on weekdays and weekends until 2016, so the researchers divided their findings into two: 68,759 people surveyed from 2008 to 2015 (set 1) and 32,379 surveyed from 2016 to 2019 (set 2).
Set 1 was further divided into those who averaged more than 7 hours of sleep per day and those who slept less than that. Set 2 was divided into three groups: one that averaged less than 7 hours of sleep per day and did not catch up on weekends, one that averaged less than 7 hours of sleep per day and did catch up on weekends, and one that averaged more than 7 hours of sleep throughout the week.
The researchers used the hepatic steatosis index (HSI) to determine the presence of a fatty liver, calculated as 8 x (ratio of serum ALT to serum AST) + body mass index (+ 2 for female, + 2 in case of diabetes). An HSI of at least36 was considered an indicator of fatty liver.
Less sleep, more risk
Participants in set 1 slept for a mean of 6.8 hours, with 58.6% sleeping more than 7 hours a day. Those in set 2 slept a mean of 6.9 hours during weekdays, with 59.9% sleeping more than 7 hours. They also slept a mean of 7.7 hours on weekends.
In set 1, sleeping at least7 hours was associated with a 16% lower risk for NAFLD (odds ratio, 0.84; 95% confidence interval, 0.79-0.89).
In set 2, sleeping at least 7 hours on weekdays was associated with a 19% reduced risk for NAFLD (OR, 0.81; 95% CI, 0.74-0.89). Sleeping at least 7 hours on the weekend was associated with a 22% reduced risk for NAFLD (OR, 0.78; 95% CI, 0.70-0.87). Compared with those who slept less than 7 hours throughout the week, those who slept less than 7 hours on weekdays and more than 7 hours on weekends had a 20% lower rate of NAFLD (OR, 0.80; 95% CI, 0.70-0.92).
All these associations held true for both men and women.
Why getting your Z’s may have hepatic advantages
One explanation for the link between sleep patterns and NAFLD is that dysregulation of cortisol, inflammatory cytokines, and norepinephrine are associated with both variations in sleep and NAFLD onset, Dr. Lee and colleagues wrote.
They also pointed out that a lack of sleep can reduce the secretion of two hormones that promote satiety: leptin and glucagonlike peptide–1. As a result, people who sleep less may eat more and gain weight, which increases the risk for NAFLD.
Ashwani K. Singal, MD, MS, a professor of medicine at the University of South Dakota, Vermillion, who was not involved in the study, noted that it was based on comparing a cross section of a population instead of following the participants over time.
“So, I think it’s an association rather than a cause and effect,” he said in an interview.
The authors don’t report a multivariate analysis to determine whether comorbidities or other characteristics of the patients could explain the association, he pointed out, noting that obesity, for example, can increase the risk for both NAFLD and sleep apnea.
Still, Dr. Singal said, the paper will influence him to mention sleep in the context of lifestyle factors that can affect fatty liver disease. “I’m going to tell my patients, and tell the community physicians to tell their patients, to follow a good sleep hygiene and make sure that they sleep at least 5-7 hours.”
Dr. Singal and the study authors all reported no relevant financial relationships. The study was supported by the National Research Foundation of Korea.
A version of this article first appeared on Medscape.com.
People who don’t get enough sleep during the week may be able to reduce their risk for nonalcoholic fatty liver disease (NAFLD) by catching up on the weekends, researchers say.
“Our study revealed that people who get enough sleep have a lower risk of developing NAFLD than those who get insufficient sleep,” Sangheun Lee, MD, PhD, from Catholic Kwandong University, Incheon, South Korea, and colleagues wrote in Annals of Hepatology.
However, they cautioned that further research is needed to verify their finding.
Previous studies have associated insufficient sleep with obesity, hypertension, diabetes mellitus, and cardiovascular disease, as well as liver fibrosis.
A busy weekday schedule can make it harder to get enough sleep, and some people try to compensate by sleeping longer on weekends. Studies so far have produced mixed findings on this strategy, with some showing that more sleep on the weekend reduces the risk for obesity, hypertension, and metabolic syndrome, and others showing no effect on metabolic dysregulation or energy balance.
Accessing a nation’s sleep data
To explore the relationship between sleep patterns and NAFLD, Dr. Lee and colleagues analyzed data from Korea National Health and Nutrition Examination Surveys collected from 2008 to 2019. They excluded people aged less than 20 years, those with hepatitis B or C infections, liver cirrhosis or liver cancer, shift workers and others who “slept irregularly,” and those who consumed alcohol excessively, leaving a cohort of 101,138 participants.
The survey didn’t distinguish between sleep on weekdays and weekends until 2016, so the researchers divided their findings into two: 68,759 people surveyed from 2008 to 2015 (set 1) and 32,379 surveyed from 2016 to 2019 (set 2).
Set 1 was further divided into those who averaged more than 7 hours of sleep per day and those who slept less than that. Set 2 was divided into three groups: one that averaged less than 7 hours of sleep per day and did not catch up on weekends, one that averaged less than 7 hours of sleep per day and did catch up on weekends, and one that averaged more than 7 hours of sleep throughout the week.
The researchers used the hepatic steatosis index (HSI) to determine the presence of a fatty liver, calculated as 8 x (ratio of serum ALT to serum AST) + body mass index (+ 2 for female, + 2 in case of diabetes). An HSI of at least36 was considered an indicator of fatty liver.
Less sleep, more risk
Participants in set 1 slept for a mean of 6.8 hours, with 58.6% sleeping more than 7 hours a day. Those in set 2 slept a mean of 6.9 hours during weekdays, with 59.9% sleeping more than 7 hours. They also slept a mean of 7.7 hours on weekends.
In set 1, sleeping at least7 hours was associated with a 16% lower risk for NAFLD (odds ratio, 0.84; 95% confidence interval, 0.79-0.89).
In set 2, sleeping at least 7 hours on weekdays was associated with a 19% reduced risk for NAFLD (OR, 0.81; 95% CI, 0.74-0.89). Sleeping at least 7 hours on the weekend was associated with a 22% reduced risk for NAFLD (OR, 0.78; 95% CI, 0.70-0.87). Compared with those who slept less than 7 hours throughout the week, those who slept less than 7 hours on weekdays and more than 7 hours on weekends had a 20% lower rate of NAFLD (OR, 0.80; 95% CI, 0.70-0.92).
All these associations held true for both men and women.
Why getting your Z’s may have hepatic advantages
One explanation for the link between sleep patterns and NAFLD is that dysregulation of cortisol, inflammatory cytokines, and norepinephrine are associated with both variations in sleep and NAFLD onset, Dr. Lee and colleagues wrote.
They also pointed out that a lack of sleep can reduce the secretion of two hormones that promote satiety: leptin and glucagonlike peptide–1. As a result, people who sleep less may eat more and gain weight, which increases the risk for NAFLD.
Ashwani K. Singal, MD, MS, a professor of medicine at the University of South Dakota, Vermillion, who was not involved in the study, noted that it was based on comparing a cross section of a population instead of following the participants over time.
“So, I think it’s an association rather than a cause and effect,” he said in an interview.
The authors don’t report a multivariate analysis to determine whether comorbidities or other characteristics of the patients could explain the association, he pointed out, noting that obesity, for example, can increase the risk for both NAFLD and sleep apnea.
Still, Dr. Singal said, the paper will influence him to mention sleep in the context of lifestyle factors that can affect fatty liver disease. “I’m going to tell my patients, and tell the community physicians to tell their patients, to follow a good sleep hygiene and make sure that they sleep at least 5-7 hours.”
Dr. Singal and the study authors all reported no relevant financial relationships. The study was supported by the National Research Foundation of Korea.
A version of this article first appeared on Medscape.com.
People who don’t get enough sleep during the week may be able to reduce their risk for nonalcoholic fatty liver disease (NAFLD) by catching up on the weekends, researchers say.
“Our study revealed that people who get enough sleep have a lower risk of developing NAFLD than those who get insufficient sleep,” Sangheun Lee, MD, PhD, from Catholic Kwandong University, Incheon, South Korea, and colleagues wrote in Annals of Hepatology.
However, they cautioned that further research is needed to verify their finding.
Previous studies have associated insufficient sleep with obesity, hypertension, diabetes mellitus, and cardiovascular disease, as well as liver fibrosis.
A busy weekday schedule can make it harder to get enough sleep, and some people try to compensate by sleeping longer on weekends. Studies so far have produced mixed findings on this strategy, with some showing that more sleep on the weekend reduces the risk for obesity, hypertension, and metabolic syndrome, and others showing no effect on metabolic dysregulation or energy balance.
Accessing a nation’s sleep data
To explore the relationship between sleep patterns and NAFLD, Dr. Lee and colleagues analyzed data from Korea National Health and Nutrition Examination Surveys collected from 2008 to 2019. They excluded people aged less than 20 years, those with hepatitis B or C infections, liver cirrhosis or liver cancer, shift workers and others who “slept irregularly,” and those who consumed alcohol excessively, leaving a cohort of 101,138 participants.
The survey didn’t distinguish between sleep on weekdays and weekends until 2016, so the researchers divided their findings into two: 68,759 people surveyed from 2008 to 2015 (set 1) and 32,379 surveyed from 2016 to 2019 (set 2).
Set 1 was further divided into those who averaged more than 7 hours of sleep per day and those who slept less than that. Set 2 was divided into three groups: one that averaged less than 7 hours of sleep per day and did not catch up on weekends, one that averaged less than 7 hours of sleep per day and did catch up on weekends, and one that averaged more than 7 hours of sleep throughout the week.
The researchers used the hepatic steatosis index (HSI) to determine the presence of a fatty liver, calculated as 8 x (ratio of serum ALT to serum AST) + body mass index (+ 2 for female, + 2 in case of diabetes). An HSI of at least36 was considered an indicator of fatty liver.
Less sleep, more risk
Participants in set 1 slept for a mean of 6.8 hours, with 58.6% sleeping more than 7 hours a day. Those in set 2 slept a mean of 6.9 hours during weekdays, with 59.9% sleeping more than 7 hours. They also slept a mean of 7.7 hours on weekends.
In set 1, sleeping at least7 hours was associated with a 16% lower risk for NAFLD (odds ratio, 0.84; 95% confidence interval, 0.79-0.89).
In set 2, sleeping at least 7 hours on weekdays was associated with a 19% reduced risk for NAFLD (OR, 0.81; 95% CI, 0.74-0.89). Sleeping at least 7 hours on the weekend was associated with a 22% reduced risk for NAFLD (OR, 0.78; 95% CI, 0.70-0.87). Compared with those who slept less than 7 hours throughout the week, those who slept less than 7 hours on weekdays and more than 7 hours on weekends had a 20% lower rate of NAFLD (OR, 0.80; 95% CI, 0.70-0.92).
All these associations held true for both men and women.
Why getting your Z’s may have hepatic advantages
One explanation for the link between sleep patterns and NAFLD is that dysregulation of cortisol, inflammatory cytokines, and norepinephrine are associated with both variations in sleep and NAFLD onset, Dr. Lee and colleagues wrote.
They also pointed out that a lack of sleep can reduce the secretion of two hormones that promote satiety: leptin and glucagonlike peptide–1. As a result, people who sleep less may eat more and gain weight, which increases the risk for NAFLD.
Ashwani K. Singal, MD, MS, a professor of medicine at the University of South Dakota, Vermillion, who was not involved in the study, noted that it was based on comparing a cross section of a population instead of following the participants over time.
“So, I think it’s an association rather than a cause and effect,” he said in an interview.
The authors don’t report a multivariate analysis to determine whether comorbidities or other characteristics of the patients could explain the association, he pointed out, noting that obesity, for example, can increase the risk for both NAFLD and sleep apnea.
Still, Dr. Singal said, the paper will influence him to mention sleep in the context of lifestyle factors that can affect fatty liver disease. “I’m going to tell my patients, and tell the community physicians to tell their patients, to follow a good sleep hygiene and make sure that they sleep at least 5-7 hours.”
Dr. Singal and the study authors all reported no relevant financial relationships. The study was supported by the National Research Foundation of Korea.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF HEPATOLOGY
Freiburg index accurately predicts survival in liver procedure
A new prognostic score is more accurate than the commonly used Model for End-Stage Liver Disease (MELD) in predicting post–transjugular intrahepatic portosystemic shunt (TIPS) survival, researchers say.
The Freiburg Index of Post-TIPS Survival (FIPS) could help patients and doctors weigh the benefits and risks of the procedure, said Chongtu Yang, MD, a postgraduate fellow at the Huazhong University of Science and Technology, Wuhan, China.
“For patients defined as high risk, the TIPS procedure may not be the optimal choice, and transplantation may be better,” Dr. Yang told this news organization. He cautioned that FIPS needs further validation before being applied in clinical practice.
The study by Dr. Yang and his colleagues was published online Feb. 9 in the American Journal of Roentgenology. To their knowledge, this is the first study to validate FIPS in a cohort of Asian patients.
Decompensated cirrhosis can cause variceal bleeding and refractory ascites and may be life threatening. TIPS can manage these complications but comes with its own risks.
To determine which patients can best benefit from the procedure, researchers have proposed a variety of prognostic scoring systems. Some were developed for other purposes, such as predicting survival following hospitalization, rather than specifically for TIPS. Additionally, few studies have compared these approaches to each other.
A four-way comparison
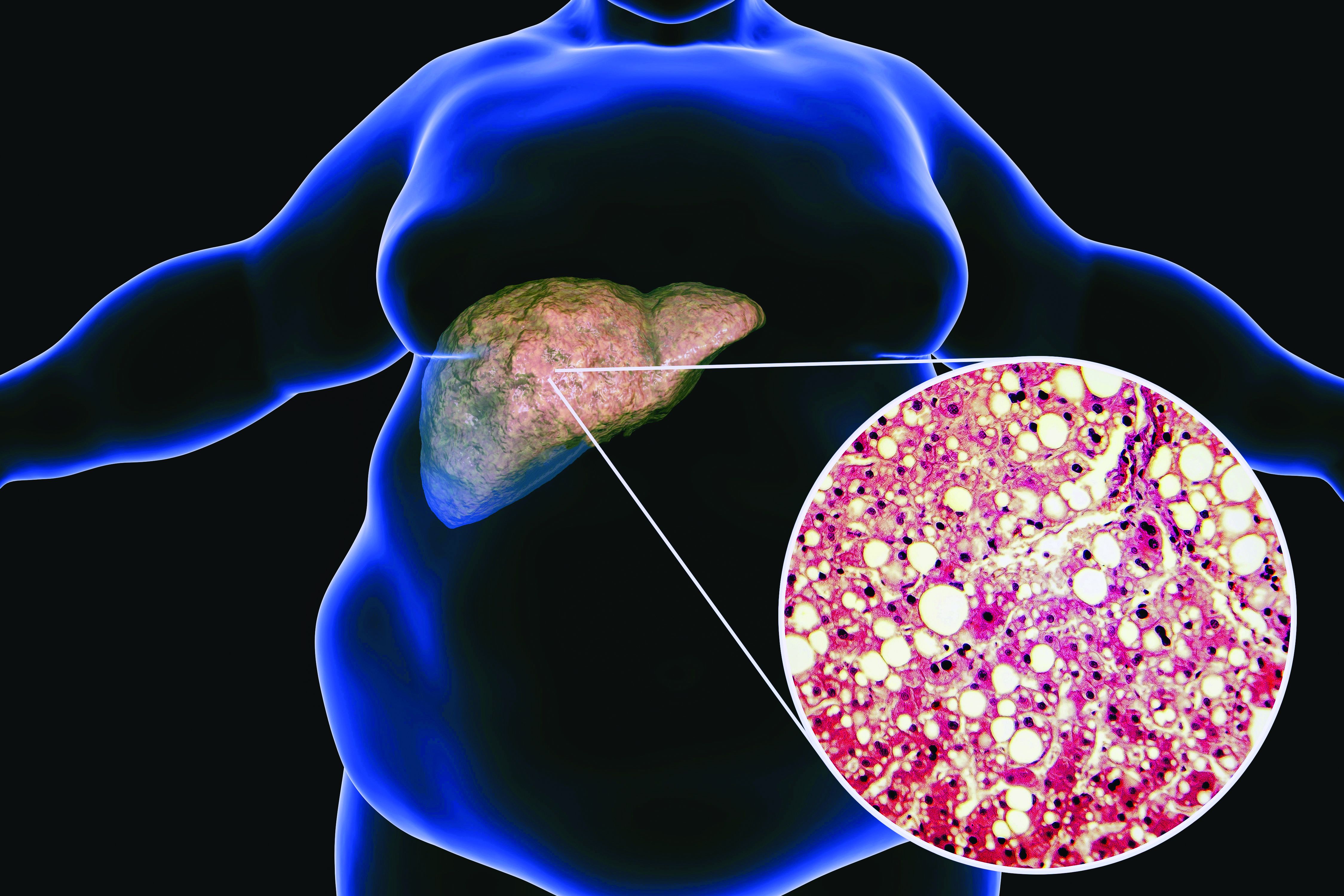
To fill that gap, Dr. Yang and his colleagues compared four predictive models: the MELD, the sodium MELD (MELD-Na), the Chronic Liver Failure–Consortium Acute Decompensation (CLIF-CAD), and FIPS.
The MELD score uses serum bilirubin, serum creatinine, and the international normalized ratio (INR) of prothrombin time. MELD-Na adds sodium to this algorithm. The CLIF-CAD score is calculated using age, serum creatinine, INR, white blood count, and sodium level. FIPS, which was recently devised to predict results with TIPS, uses age, bilirubin, albumin, and creatinine.
To see which yielded more accurate predictions, Dr. Yang and his colleagues followed 383 patients with cirrhosis (mean age, 55 years; 341 with variceal bleeding and 42 with refractory ascites) who underwent TIPS placement at Wuhan Union Hospital between January 2016 and August 2021.
The most common cause of cirrhosis was hepatitis B infection (58.2% of patients), followed by hepatitis C infection (11.7%) and alcohol use (13.6%).
The researchers followed the patients for a median of 23.4 months. They lost track of 31 patients over that time, and another 72 died. The survival rate after TIPS placement was 92.3% at 6 months, 87.8% at 12 months, and 81.2% at 24 months. Thirty-seven patients received a TIPS revision.
In their first measure of the models’ accuracy, the researchers used a concordance index, which compares actual results with predicted results. The number of concordant pairs are divided by the total number of possible evaluation pairs. A score of 1 represents 100% accuracy.
By this measure, the prediction of survival at 6 months was highest for FIPS followed by CLIF-CAD, MELD, and MELD-Na. However, the confidence intervals overlapped.
FIPS also scored highest in the concordance index at 12 and 24 months.
In a second measure of the models’ accuracy, the researchers used Brier scores, which calculate the mean squared error between predicted probabilities and actual values. Like the concordance index, Brier scores range from 0.0 to 1.0 but differ in that the lowest Brier score number represents the highest accuracy.
At 6 months, the CLIF-CAD score was the best, at 0.074. MELD and FIPS were equivalent at 0.075, with MELD-Na coming in at 0.077. However, FIPS attained slightly better scores than the other systems at 12 and 24 months.
Is FIPS worth implementing?
With scores this close, it may not be worth changing the predictive model clinicians use for choosing TIPS candidates, said Nancy Reau, MD, chief of hepatology at Rush University Medical Center, Chicago, who was not involved in the study.
MELD scores are already programmed into many electronic medical record systems in the United States, and clinicians are familiar with using that system to aid in further decisions, such as decisions regarding other kinds of surgery, she told this news organization.
“If you’re going to try to advocate for a new system, you really have to show that the performance of the predictive score is monumentally better than the tried and true,” she said.
Dr. Yang and Dr. Reau report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new prognostic score is more accurate than the commonly used Model for End-Stage Liver Disease (MELD) in predicting post–transjugular intrahepatic portosystemic shunt (TIPS) survival, researchers say.
The Freiburg Index of Post-TIPS Survival (FIPS) could help patients and doctors weigh the benefits and risks of the procedure, said Chongtu Yang, MD, a postgraduate fellow at the Huazhong University of Science and Technology, Wuhan, China.
“For patients defined as high risk, the TIPS procedure may not be the optimal choice, and transplantation may be better,” Dr. Yang told this news organization. He cautioned that FIPS needs further validation before being applied in clinical practice.
The study by Dr. Yang and his colleagues was published online Feb. 9 in the American Journal of Roentgenology. To their knowledge, this is the first study to validate FIPS in a cohort of Asian patients.
Decompensated cirrhosis can cause variceal bleeding and refractory ascites and may be life threatening. TIPS can manage these complications but comes with its own risks.
To determine which patients can best benefit from the procedure, researchers have proposed a variety of prognostic scoring systems. Some were developed for other purposes, such as predicting survival following hospitalization, rather than specifically for TIPS. Additionally, few studies have compared these approaches to each other.
A four-way comparison
To fill that gap, Dr. Yang and his colleagues compared four predictive models: the MELD, the sodium MELD (MELD-Na), the Chronic Liver Failure–Consortium Acute Decompensation (CLIF-CAD), and FIPS.
The MELD score uses serum bilirubin, serum creatinine, and the international normalized ratio (INR) of prothrombin time. MELD-Na adds sodium to this algorithm. The CLIF-CAD score is calculated using age, serum creatinine, INR, white blood count, and sodium level. FIPS, which was recently devised to predict results with TIPS, uses age, bilirubin, albumin, and creatinine.
To see which yielded more accurate predictions, Dr. Yang and his colleagues followed 383 patients with cirrhosis (mean age, 55 years; 341 with variceal bleeding and 42 with refractory ascites) who underwent TIPS placement at Wuhan Union Hospital between January 2016 and August 2021.
The most common cause of cirrhosis was hepatitis B infection (58.2% of patients), followed by hepatitis C infection (11.7%) and alcohol use (13.6%).
The researchers followed the patients for a median of 23.4 months. They lost track of 31 patients over that time, and another 72 died. The survival rate after TIPS placement was 92.3% at 6 months, 87.8% at 12 months, and 81.2% at 24 months. Thirty-seven patients received a TIPS revision.
In their first measure of the models’ accuracy, the researchers used a concordance index, which compares actual results with predicted results. The number of concordant pairs are divided by the total number of possible evaluation pairs. A score of 1 represents 100% accuracy.
By this measure, the prediction of survival at 6 months was highest for FIPS followed by CLIF-CAD, MELD, and MELD-Na. However, the confidence intervals overlapped.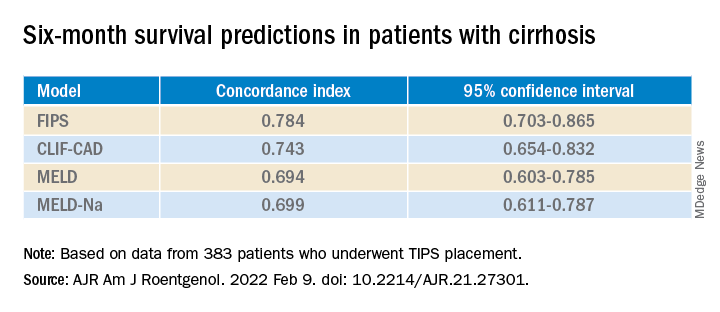
FIPS also scored highest in the concordance index at 12 and 24 months.
In a second measure of the models’ accuracy, the researchers used Brier scores, which calculate the mean squared error between predicted probabilities and actual values. Like the concordance index, Brier scores range from 0.0 to 1.0 but differ in that the lowest Brier score number represents the highest accuracy.
At 6 months, the CLIF-CAD score was the best, at 0.074. MELD and FIPS were equivalent at 0.075, with MELD-Na coming in at 0.077. However, FIPS attained slightly better scores than the other systems at 12 and 24 months.
Is FIPS worth implementing?
With scores this close, it may not be worth changing the predictive model clinicians use for choosing TIPS candidates, said Nancy Reau, MD, chief of hepatology at Rush University Medical Center, Chicago, who was not involved in the study.
MELD scores are already programmed into many electronic medical record systems in the United States, and clinicians are familiar with using that system to aid in further decisions, such as decisions regarding other kinds of surgery, she told this news organization.
“If you’re going to try to advocate for a new system, you really have to show that the performance of the predictive score is monumentally better than the tried and true,” she said.
Dr. Yang and Dr. Reau report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new prognostic score is more accurate than the commonly used Model for End-Stage Liver Disease (MELD) in predicting post–transjugular intrahepatic portosystemic shunt (TIPS) survival, researchers say.
The Freiburg Index of Post-TIPS Survival (FIPS) could help patients and doctors weigh the benefits and risks of the procedure, said Chongtu Yang, MD, a postgraduate fellow at the Huazhong University of Science and Technology, Wuhan, China.
“For patients defined as high risk, the TIPS procedure may not be the optimal choice, and transplantation may be better,” Dr. Yang told this news organization. He cautioned that FIPS needs further validation before being applied in clinical practice.
The study by Dr. Yang and his colleagues was published online Feb. 9 in the American Journal of Roentgenology. To their knowledge, this is the first study to validate FIPS in a cohort of Asian patients.
Decompensated cirrhosis can cause variceal bleeding and refractory ascites and may be life threatening. TIPS can manage these complications but comes with its own risks.
To determine which patients can best benefit from the procedure, researchers have proposed a variety of prognostic scoring systems. Some were developed for other purposes, such as predicting survival following hospitalization, rather than specifically for TIPS. Additionally, few studies have compared these approaches to each other.
A four-way comparison
To fill that gap, Dr. Yang and his colleagues compared four predictive models: the MELD, the sodium MELD (MELD-Na), the Chronic Liver Failure–Consortium Acute Decompensation (CLIF-CAD), and FIPS.
The MELD score uses serum bilirubin, serum creatinine, and the international normalized ratio (INR) of prothrombin time. MELD-Na adds sodium to this algorithm. The CLIF-CAD score is calculated using age, serum creatinine, INR, white blood count, and sodium level. FIPS, which was recently devised to predict results with TIPS, uses age, bilirubin, albumin, and creatinine.
To see which yielded more accurate predictions, Dr. Yang and his colleagues followed 383 patients with cirrhosis (mean age, 55 years; 341 with variceal bleeding and 42 with refractory ascites) who underwent TIPS placement at Wuhan Union Hospital between January 2016 and August 2021.
The most common cause of cirrhosis was hepatitis B infection (58.2% of patients), followed by hepatitis C infection (11.7%) and alcohol use (13.6%).
The researchers followed the patients for a median of 23.4 months. They lost track of 31 patients over that time, and another 72 died. The survival rate after TIPS placement was 92.3% at 6 months, 87.8% at 12 months, and 81.2% at 24 months. Thirty-seven patients received a TIPS revision.
In their first measure of the models’ accuracy, the researchers used a concordance index, which compares actual results with predicted results. The number of concordant pairs are divided by the total number of possible evaluation pairs. A score of 1 represents 100% accuracy.
By this measure, the prediction of survival at 6 months was highest for FIPS followed by CLIF-CAD, MELD, and MELD-Na. However, the confidence intervals overlapped.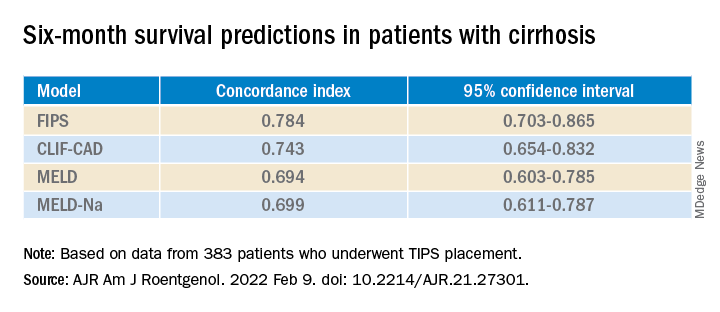
FIPS also scored highest in the concordance index at 12 and 24 months.
In a second measure of the models’ accuracy, the researchers used Brier scores, which calculate the mean squared error between predicted probabilities and actual values. Like the concordance index, Brier scores range from 0.0 to 1.0 but differ in that the lowest Brier score number represents the highest accuracy.
At 6 months, the CLIF-CAD score was the best, at 0.074. MELD and FIPS were equivalent at 0.075, with MELD-Na coming in at 0.077. However, FIPS attained slightly better scores than the other systems at 12 and 24 months.
Is FIPS worth implementing?
With scores this close, it may not be worth changing the predictive model clinicians use for choosing TIPS candidates, said Nancy Reau, MD, chief of hepatology at Rush University Medical Center, Chicago, who was not involved in the study.
MELD scores are already programmed into many electronic medical record systems in the United States, and clinicians are familiar with using that system to aid in further decisions, such as decisions regarding other kinds of surgery, she told this news organization.
“If you’re going to try to advocate for a new system, you really have to show that the performance of the predictive score is monumentally better than the tried and true,” she said.
Dr. Yang and Dr. Reau report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF ROENTGENOLOGY
Novel scoring system emerges for alcoholic hepatitis mortality
A new scoring system proved more accurate than several other available models at predicting the 30-day mortality risk for patients with alcohol-associated hepatitis (AH), according to new data.
The system, called the Mortality Index for Alcohol-Associated Hepatitis (MIAAH), was created by a team of Mayo Clinic researchers, who published their results in Mayo Clinic Proceedings.
Among the currently available prognostic models for assessing AH severity are the Model for End-Stage Liver Disease (MELD); the Age, serum Bilirubin, International normalized ratio, and serum Creatinine (ABIC) score; the Maddrey Discriminant Function (MDF); and the Glasgow Alcoholic Hepatitis Score (GAHS). However, these models have poor accuracy, with the area under the curve between 0.71 and 0.77.
By comparison, the new model has an accuracy of 86% in predicting 30-day mortality for AH, said coauthor Ashwani K. Singal, MD, MS, professor of medicine at the University of South Dakota Sanford School of Medicine, Sioux Falls.
“It’s a better predictor of the outcome, and that’s what sets it apart,” he told this news organization. “I think providers and patients will benefit.”
He said accuracy in determining the likelihood of death can help clinicians better determine treatment options and prepare patients and their families.
Camille Kezer, MD, a Mayo Clinic resident internist and first author of the paper, said in a statement, “MIAAH also has the advantage of performing well in patients, regardless of whether they’ve been treated with steroids, which makes it generalizable.”
Creating and validating the MIAAH
Researchers analyzed the health records of 266 eligible patients diagnosed with AH between 1998 and 2018 at the Mayo Clinic, Rochester, Minn. The patients collectively had a 30-day mortality rate of 19.2%.
They then studied the effect of several variables, of which the following were found to be significantly associated with mortality: age (P = .002), blood urea nitrogen (P = .003), albumin (P = .01), bilirubin (P = .02), and international normalized ratio (P = .001).
Mayo researchers built the MIAAH model using these variables and found that it was able to achieve a C statistic of 0.86, which translates into its being able to accurately predict mortality more than 86% of the time. When tested in the initial cohort of 266 patients, MIAAH had a significantly superior C statistic compared with several other available models, such as the MELD, MDF, and GAHS, although not for the ABIC.
The researchers then tested the MIAAH model in a validation cohort of 249 patients from health care centers at the University of South Dakota, Sioux Falls, and the University of Kansas, Lawrence. In this cohort, the MIAAH’s C statistic decreased to 0.73, which remained significantly more accurate than the MDF but was comparable to that found with the MELD.
Helping with transplant decisions
There are no pharmacologic treatments that can reduce 90-day mortality in severe cases of AH, and only a small survival benefit at 30 days has been reported with prednisolone use.
With a shortage of liver donors, many centers still require 6 months of alcohol abstinence for transplant consideration, although exceptions are sometimes made for cases of early transplant.
A model that more accurately predicts who is at the highest risk of dying within a month can help clinicians decide how best to proceed, Dr. Singal said.
Paul Martin, MD, chief of the division of digestive health and liver diseases, Mandel Chair in gastroenterology, and professor of medicine at the University of Miami, told this news organization that the model is potentially important in light of the rising prevalence of AH.
“The numbers of patients with AH are unequivocally increasing and often in young patients,” he noted, presenting difficult choices of who to treat with steroids and who to refer for a transplant.
“This model is certainly timely,” he said. “We need more accuracy in predicting which patients will recover with medical therapy and which patients won’t in the absence of a liver transplant.”
He noted, however, that the study’s retrospective design requires that it’s validated prospectively: “not only looking at the outcome in terms of mortality of patients, but its potential utility in identifying candidates for liver transplantation who are not going to recover on their own.”
He said it was unlikely that the model would replace others, particularly MELD, which is ingrained in practices in the United States and other countries, but may instead have a complementary role.
Dr. Singal, Dr. Kezer, and Dr. Martin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new scoring system proved more accurate than several other available models at predicting the 30-day mortality risk for patients with alcohol-associated hepatitis (AH), according to new data.
The system, called the Mortality Index for Alcohol-Associated Hepatitis (MIAAH), was created by a team of Mayo Clinic researchers, who published their results in Mayo Clinic Proceedings.
Among the currently available prognostic models for assessing AH severity are the Model for End-Stage Liver Disease (MELD); the Age, serum Bilirubin, International normalized ratio, and serum Creatinine (ABIC) score; the Maddrey Discriminant Function (MDF); and the Glasgow Alcoholic Hepatitis Score (GAHS). However, these models have poor accuracy, with the area under the curve between 0.71 and 0.77.
By comparison, the new model has an accuracy of 86% in predicting 30-day mortality for AH, said coauthor Ashwani K. Singal, MD, MS, professor of medicine at the University of South Dakota Sanford School of Medicine, Sioux Falls.
“It’s a better predictor of the outcome, and that’s what sets it apart,” he told this news organization. “I think providers and patients will benefit.”
He said accuracy in determining the likelihood of death can help clinicians better determine treatment options and prepare patients and their families.
Camille Kezer, MD, a Mayo Clinic resident internist and first author of the paper, said in a statement, “MIAAH also has the advantage of performing well in patients, regardless of whether they’ve been treated with steroids, which makes it generalizable.”
Creating and validating the MIAAH
Researchers analyzed the health records of 266 eligible patients diagnosed with AH between 1998 and 2018 at the Mayo Clinic, Rochester, Minn. The patients collectively had a 30-day mortality rate of 19.2%.
They then studied the effect of several variables, of which the following were found to be significantly associated with mortality: age (P = .002), blood urea nitrogen (P = .003), albumin (P = .01), bilirubin (P = .02), and international normalized ratio (P = .001).
Mayo researchers built the MIAAH model using these variables and found that it was able to achieve a C statistic of 0.86, which translates into its being able to accurately predict mortality more than 86% of the time. When tested in the initial cohort of 266 patients, MIAAH had a significantly superior C statistic compared with several other available models, such as the MELD, MDF, and GAHS, although not for the ABIC.
The researchers then tested the MIAAH model in a validation cohort of 249 patients from health care centers at the University of South Dakota, Sioux Falls, and the University of Kansas, Lawrence. In this cohort, the MIAAH’s C statistic decreased to 0.73, which remained significantly more accurate than the MDF but was comparable to that found with the MELD.
Helping with transplant decisions
There are no pharmacologic treatments that can reduce 90-day mortality in severe cases of AH, and only a small survival benefit at 30 days has been reported with prednisolone use.
With a shortage of liver donors, many centers still require 6 months of alcohol abstinence for transplant consideration, although exceptions are sometimes made for cases of early transplant.
A model that more accurately predicts who is at the highest risk of dying within a month can help clinicians decide how best to proceed, Dr. Singal said.
Paul Martin, MD, chief of the division of digestive health and liver diseases, Mandel Chair in gastroenterology, and professor of medicine at the University of Miami, told this news organization that the model is potentially important in light of the rising prevalence of AH.
“The numbers of patients with AH are unequivocally increasing and often in young patients,” he noted, presenting difficult choices of who to treat with steroids and who to refer for a transplant.
“This model is certainly timely,” he said. “We need more accuracy in predicting which patients will recover with medical therapy and which patients won’t in the absence of a liver transplant.”
He noted, however, that the study’s retrospective design requires that it’s validated prospectively: “not only looking at the outcome in terms of mortality of patients, but its potential utility in identifying candidates for liver transplantation who are not going to recover on their own.”
He said it was unlikely that the model would replace others, particularly MELD, which is ingrained in practices in the United States and other countries, but may instead have a complementary role.
Dr. Singal, Dr. Kezer, and Dr. Martin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new scoring system proved more accurate than several other available models at predicting the 30-day mortality risk for patients with alcohol-associated hepatitis (AH), according to new data.
The system, called the Mortality Index for Alcohol-Associated Hepatitis (MIAAH), was created by a team of Mayo Clinic researchers, who published their results in Mayo Clinic Proceedings.
Among the currently available prognostic models for assessing AH severity are the Model for End-Stage Liver Disease (MELD); the Age, serum Bilirubin, International normalized ratio, and serum Creatinine (ABIC) score; the Maddrey Discriminant Function (MDF); and the Glasgow Alcoholic Hepatitis Score (GAHS). However, these models have poor accuracy, with the area under the curve between 0.71 and 0.77.
By comparison, the new model has an accuracy of 86% in predicting 30-day mortality for AH, said coauthor Ashwani K. Singal, MD, MS, professor of medicine at the University of South Dakota Sanford School of Medicine, Sioux Falls.
“It’s a better predictor of the outcome, and that’s what sets it apart,” he told this news organization. “I think providers and patients will benefit.”
He said accuracy in determining the likelihood of death can help clinicians better determine treatment options and prepare patients and their families.
Camille Kezer, MD, a Mayo Clinic resident internist and first author of the paper, said in a statement, “MIAAH also has the advantage of performing well in patients, regardless of whether they’ve been treated with steroids, which makes it generalizable.”
Creating and validating the MIAAH
Researchers analyzed the health records of 266 eligible patients diagnosed with AH between 1998 and 2018 at the Mayo Clinic, Rochester, Minn. The patients collectively had a 30-day mortality rate of 19.2%.
They then studied the effect of several variables, of which the following were found to be significantly associated with mortality: age (P = .002), blood urea nitrogen (P = .003), albumin (P = .01), bilirubin (P = .02), and international normalized ratio (P = .001).
Mayo researchers built the MIAAH model using these variables and found that it was able to achieve a C statistic of 0.86, which translates into its being able to accurately predict mortality more than 86% of the time. When tested in the initial cohort of 266 patients, MIAAH had a significantly superior C statistic compared with several other available models, such as the MELD, MDF, and GAHS, although not for the ABIC.
The researchers then tested the MIAAH model in a validation cohort of 249 patients from health care centers at the University of South Dakota, Sioux Falls, and the University of Kansas, Lawrence. In this cohort, the MIAAH’s C statistic decreased to 0.73, which remained significantly more accurate than the MDF but was comparable to that found with the MELD.
Helping with transplant decisions
There are no pharmacologic treatments that can reduce 90-day mortality in severe cases of AH, and only a small survival benefit at 30 days has been reported with prednisolone use.
With a shortage of liver donors, many centers still require 6 months of alcohol abstinence for transplant consideration, although exceptions are sometimes made for cases of early transplant.
A model that more accurately predicts who is at the highest risk of dying within a month can help clinicians decide how best to proceed, Dr. Singal said.
Paul Martin, MD, chief of the division of digestive health and liver diseases, Mandel Chair in gastroenterology, and professor of medicine at the University of Miami, told this news organization that the model is potentially important in light of the rising prevalence of AH.
“The numbers of patients with AH are unequivocally increasing and often in young patients,” he noted, presenting difficult choices of who to treat with steroids and who to refer for a transplant.
“This model is certainly timely,” he said. “We need more accuracy in predicting which patients will recover with medical therapy and which patients won’t in the absence of a liver transplant.”
He noted, however, that the study’s retrospective design requires that it’s validated prospectively: “not only looking at the outcome in terms of mortality of patients, but its potential utility in identifying candidates for liver transplantation who are not going to recover on their own.”
He said it was unlikely that the model would replace others, particularly MELD, which is ingrained in practices in the United States and other countries, but may instead have a complementary role.
Dr. Singal, Dr. Kezer, and Dr. Martin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MAYO CLINIC PROCEEDINGS
RECAM vs. RUCAM: Finding a better way to diagnose DILI
Researchers looking for a better way to diagnose drug-induced liver injury (DILI) have found evidence to support the use of the Revised Electronic Causality Assessment Method (RECAM).
The broadly used Roussel Uclaf Causality Assessment Method (RUCAM), introduced in 1993, “has been a valuable clinical framework for DILI diagnosis,” but it has been clouded by subjectivity and poor reliability, wrote the authors, led by Paul H. Hayashi, MD, MPH, with the Food and Drug Administration, in Hepatology. Citing a review from the Journal of Hepatology, Dr. Hayashi and colleagues noted three major problems: “(1) unclear operating instructions and subjectivity leading to poor reliability and usability, (2) unclear validity due to lack of an accepted gold standard and (3) domain criteria that are not evidence-based.”
Currently, a diagnosis of DILI is primarily based on clinicians’ judgment and ruling out alternative diagnoses, the authors of this study wrote. The lack of an evidence-based and reliable diagnostic tool is a significant obstacle in clinical care and research .
Reaching a new method
The researchers used classification tree analysis to set diagnostic cut-offs for RECAM and then compared RECAM with RUCAM for correlation with expert opinion diagnostic categories in 194 DILI cases (98 from the Drug-Induced Liver Injury Network, 96 from the Spanish DILI Registry).
The area under receiver operator curves for identifying at least probable DILI were the same at 0.89 for both RECAM and RUCAM.
The authors wrote, “However, RECAM diagnostic categories have better observed overall agreement with expert opinion (0.62 vs. 0.56 weighted kappa, P = .14), and had better sensitivity to detect extreme diagnostic categories (73 vs. 54 for highly likely or high probable, P = .02; 65 vs. 48 for unlikely/excluded, P = .08) than RUCAM diagnostic categories.”
They concluded that RECAM “is at least as capable as RUCAM in diagnosing DILI compared to expert opinion but is better than RUCAM at the diagnostic extremes.”
RECAM appears to add objectivity and clarity that can improve precision and reliability when diagnosing DILI and improve diagnostic standardization, according to authors. It has automated scoring, which reduces subjective input and should lead to better reliability among raters, something that has limited RUCAM’s adaptation in clinical practice and research.
RECAM has automatic warnings for data inconsistencies, which DILI and RUCAM do not. In RUCAM, a different diagnosis or other data could rule out DILI, but the case would still gain points in other criteria.
The authors explained, “Even when data clearly diagnose acute viral hepatitis or autoimmune hepatitis by simplified autoimmune hepatitis score, points are still given for latency, dechallenge, or underlying hepatotoxicity risk of the drug. In these situations of highly implausible DILI, RECAM gives warnings to stop with an imputed total score of –6. One can over-ride these warnings, if one believes DILI may be concurrent with the non-DILI diagnosis. However, –6 points are still assessed.”
Diagnosis of exclusion
Paul Martin, MD, chief, division of digestive health and liver diseases, Mandel Chair in Gastroenterology and professor of medicine at the University of Miami, said in an interview that he hopes RECAM will become widely used and better address a condition that sometimes doesn’t get enough attention. DILI remains underappreciated, he said, despite it being a major cause of morbidity and mortality in some patients.
“Any algorithm or criteria that can improve diagnostic accuracy is useful because typically it is a diagnosis of exclusion,” Dr. Martin said. “This new system seems to be as good as any other prior algorithms to diagnose drug-induced liver injury.”
He added, “This should help clinicians with individual patients with unexplained liver disease.”
The authors noted some limitations. RECAM was developed in U.S. and Spanish cohorts, so its performance in other regions is unclear. Both registries have minimum enrollment requirements for liver enzyme and bilirubin elevation, so it is not known how effective RECAM is in less severe cases. It also needs to be tested by other clinicians, including nonhepatologists.
The authors also added, “It is currently limited to single-agent medication cases leaving the user to score each medication individually in multidrug cases. However, any competing medication causing loss of points in the RUCAM, probably deserves its own RECAM score.”
The DILIN is structured as a cooperative agreement with funds provided by the National Institute of Diabetes and Digestive and Kidney Diseases.
Dr. Hayashi is employed by the FDA, but the conclusions of this paper do not reflect any opinion of the FDA. One coauthor has advised Pfizer, GSK, and NuCANA through Nottingham University Consultants, and another has received support from Gilead and AbbVie and consulted for Sanofi. The remaining authors have no conflicts. Dr. Martin reports no relevant financial relationships.
Researchers looking for a better way to diagnose drug-induced liver injury (DILI) have found evidence to support the use of the Revised Electronic Causality Assessment Method (RECAM).
The broadly used Roussel Uclaf Causality Assessment Method (RUCAM), introduced in 1993, “has been a valuable clinical framework for DILI diagnosis,” but it has been clouded by subjectivity and poor reliability, wrote the authors, led by Paul H. Hayashi, MD, MPH, with the Food and Drug Administration, in Hepatology. Citing a review from the Journal of Hepatology, Dr. Hayashi and colleagues noted three major problems: “(1) unclear operating instructions and subjectivity leading to poor reliability and usability, (2) unclear validity due to lack of an accepted gold standard and (3) domain criteria that are not evidence-based.”
Currently, a diagnosis of DILI is primarily based on clinicians’ judgment and ruling out alternative diagnoses, the authors of this study wrote. The lack of an evidence-based and reliable diagnostic tool is a significant obstacle in clinical care and research .
Reaching a new method
The researchers used classification tree analysis to set diagnostic cut-offs for RECAM and then compared RECAM with RUCAM for correlation with expert opinion diagnostic categories in 194 DILI cases (98 from the Drug-Induced Liver Injury Network, 96 from the Spanish DILI Registry).
The area under receiver operator curves for identifying at least probable DILI were the same at 0.89 for both RECAM and RUCAM.
The authors wrote, “However, RECAM diagnostic categories have better observed overall agreement with expert opinion (0.62 vs. 0.56 weighted kappa, P = .14), and had better sensitivity to detect extreme diagnostic categories (73 vs. 54 for highly likely or high probable, P = .02; 65 vs. 48 for unlikely/excluded, P = .08) than RUCAM diagnostic categories.”
They concluded that RECAM “is at least as capable as RUCAM in diagnosing DILI compared to expert opinion but is better than RUCAM at the diagnostic extremes.”
RECAM appears to add objectivity and clarity that can improve precision and reliability when diagnosing DILI and improve diagnostic standardization, according to authors. It has automated scoring, which reduces subjective input and should lead to better reliability among raters, something that has limited RUCAM’s adaptation in clinical practice and research.
RECAM has automatic warnings for data inconsistencies, which DILI and RUCAM do not. In RUCAM, a different diagnosis or other data could rule out DILI, but the case would still gain points in other criteria.
The authors explained, “Even when data clearly diagnose acute viral hepatitis or autoimmune hepatitis by simplified autoimmune hepatitis score, points are still given for latency, dechallenge, or underlying hepatotoxicity risk of the drug. In these situations of highly implausible DILI, RECAM gives warnings to stop with an imputed total score of –6. One can over-ride these warnings, if one believes DILI may be concurrent with the non-DILI diagnosis. However, –6 points are still assessed.”
Diagnosis of exclusion
Paul Martin, MD, chief, division of digestive health and liver diseases, Mandel Chair in Gastroenterology and professor of medicine at the University of Miami, said in an interview that he hopes RECAM will become widely used and better address a condition that sometimes doesn’t get enough attention. DILI remains underappreciated, he said, despite it being a major cause of morbidity and mortality in some patients.
“Any algorithm or criteria that can improve diagnostic accuracy is useful because typically it is a diagnosis of exclusion,” Dr. Martin said. “This new system seems to be as good as any other prior algorithms to diagnose drug-induced liver injury.”
He added, “This should help clinicians with individual patients with unexplained liver disease.”
The authors noted some limitations. RECAM was developed in U.S. and Spanish cohorts, so its performance in other regions is unclear. Both registries have minimum enrollment requirements for liver enzyme and bilirubin elevation, so it is not known how effective RECAM is in less severe cases. It also needs to be tested by other clinicians, including nonhepatologists.
The authors also added, “It is currently limited to single-agent medication cases leaving the user to score each medication individually in multidrug cases. However, any competing medication causing loss of points in the RUCAM, probably deserves its own RECAM score.”
The DILIN is structured as a cooperative agreement with funds provided by the National Institute of Diabetes and Digestive and Kidney Diseases.
Dr. Hayashi is employed by the FDA, but the conclusions of this paper do not reflect any opinion of the FDA. One coauthor has advised Pfizer, GSK, and NuCANA through Nottingham University Consultants, and another has received support from Gilead and AbbVie and consulted for Sanofi. The remaining authors have no conflicts. Dr. Martin reports no relevant financial relationships.
Researchers looking for a better way to diagnose drug-induced liver injury (DILI) have found evidence to support the use of the Revised Electronic Causality Assessment Method (RECAM).
The broadly used Roussel Uclaf Causality Assessment Method (RUCAM), introduced in 1993, “has been a valuable clinical framework for DILI diagnosis,” but it has been clouded by subjectivity and poor reliability, wrote the authors, led by Paul H. Hayashi, MD, MPH, with the Food and Drug Administration, in Hepatology. Citing a review from the Journal of Hepatology, Dr. Hayashi and colleagues noted three major problems: “(1) unclear operating instructions and subjectivity leading to poor reliability and usability, (2) unclear validity due to lack of an accepted gold standard and (3) domain criteria that are not evidence-based.”
Currently, a diagnosis of DILI is primarily based on clinicians’ judgment and ruling out alternative diagnoses, the authors of this study wrote. The lack of an evidence-based and reliable diagnostic tool is a significant obstacle in clinical care and research .
Reaching a new method
The researchers used classification tree analysis to set diagnostic cut-offs for RECAM and then compared RECAM with RUCAM for correlation with expert opinion diagnostic categories in 194 DILI cases (98 from the Drug-Induced Liver Injury Network, 96 from the Spanish DILI Registry).
The area under receiver operator curves for identifying at least probable DILI were the same at 0.89 for both RECAM and RUCAM.
The authors wrote, “However, RECAM diagnostic categories have better observed overall agreement with expert opinion (0.62 vs. 0.56 weighted kappa, P = .14), and had better sensitivity to detect extreme diagnostic categories (73 vs. 54 for highly likely or high probable, P = .02; 65 vs. 48 for unlikely/excluded, P = .08) than RUCAM diagnostic categories.”
They concluded that RECAM “is at least as capable as RUCAM in diagnosing DILI compared to expert opinion but is better than RUCAM at the diagnostic extremes.”
RECAM appears to add objectivity and clarity that can improve precision and reliability when diagnosing DILI and improve diagnostic standardization, according to authors. It has automated scoring, which reduces subjective input and should lead to better reliability among raters, something that has limited RUCAM’s adaptation in clinical practice and research.
RECAM has automatic warnings for data inconsistencies, which DILI and RUCAM do not. In RUCAM, a different diagnosis or other data could rule out DILI, but the case would still gain points in other criteria.
The authors explained, “Even when data clearly diagnose acute viral hepatitis or autoimmune hepatitis by simplified autoimmune hepatitis score, points are still given for latency, dechallenge, or underlying hepatotoxicity risk of the drug. In these situations of highly implausible DILI, RECAM gives warnings to stop with an imputed total score of –6. One can over-ride these warnings, if one believes DILI may be concurrent with the non-DILI diagnosis. However, –6 points are still assessed.”
Diagnosis of exclusion
Paul Martin, MD, chief, division of digestive health and liver diseases, Mandel Chair in Gastroenterology and professor of medicine at the University of Miami, said in an interview that he hopes RECAM will become widely used and better address a condition that sometimes doesn’t get enough attention. DILI remains underappreciated, he said, despite it being a major cause of morbidity and mortality in some patients.
“Any algorithm or criteria that can improve diagnostic accuracy is useful because typically it is a diagnosis of exclusion,” Dr. Martin said. “This new system seems to be as good as any other prior algorithms to diagnose drug-induced liver injury.”
He added, “This should help clinicians with individual patients with unexplained liver disease.”
The authors noted some limitations. RECAM was developed in U.S. and Spanish cohorts, so its performance in other regions is unclear. Both registries have minimum enrollment requirements for liver enzyme and bilirubin elevation, so it is not known how effective RECAM is in less severe cases. It also needs to be tested by other clinicians, including nonhepatologists.
The authors also added, “It is currently limited to single-agent medication cases leaving the user to score each medication individually in multidrug cases. However, any competing medication causing loss of points in the RUCAM, probably deserves its own RECAM score.”
The DILIN is structured as a cooperative agreement with funds provided by the National Institute of Diabetes and Digestive and Kidney Diseases.
Dr. Hayashi is employed by the FDA, but the conclusions of this paper do not reflect any opinion of the FDA. One coauthor has advised Pfizer, GSK, and NuCANA through Nottingham University Consultants, and another has received support from Gilead and AbbVie and consulted for Sanofi. The remaining authors have no conflicts. Dr. Martin reports no relevant financial relationships.
FROM HEPATOLOGY
Long COVID associated with risk of metabolic liver disease
Postacute COVID syndrome (PACS), an ongoing inflammatory state following infection with SARS-CoV-2, is associated with greater risk of metabolic-associated fatty liver disease (MAFLD), according to an analysis of patients at a single clinic in Canada published in Open Forum Infectious Diseases.
MAFLD, also known as nonalcoholic fatty liver disease (NAFLD), is considered an indicator of general health and is in turn linked to greater risk of cardiovascular complications and mortality. It may be a multisystem disorder with various underlying causes.
PACS includes symptoms that affect various organ systems, with neurocognitive, autonomic, gastrointestinal, respiratory, musculoskeletal, psychological, sensory, and dermatologic clusters. An estimated 50%-80% of COVID-19 patients experience one or more clusters of symptoms 3 months after leaving the hospital.
But liver problems also appear in the acute phase, said Paul Martin, MD, who was asked to comment on the study. “Up to about half the patients during the acute illness may have elevated liver tests, but there seems to be a subset of patients in whom the abnormality persists. And then there are some reports in the literature of patients developing injury to their bile ducts in the liver over the long term, apparently as a consequence of COVID infection. What this paper suggests is that there may be some metabolic derangements associated with COVID infection, which in turn can accentuate or possibly cause fatty liver,” said Dr. Martin in an interview. He is chief of digestive health and liver diseases and a professor of medicine at the University of Miami.
“It highlights the need to get vaccinated against COVID and to take appropriate precautions because contracting the infection may lead to all sorts of consequences quite apart from having a respiratory illness,” said Dr. Martin.
The researchers retrospectively identified 235 patients hospitalized with COVID-19 between July 2020 and April 2021. Overall, 69% were men, and the median age was 61 years; 19.2% underwent mechanical ventilation and the mean duration of hospitalization was 11.7 days. They were seen for PACS symptoms a median 143 days after COVID-19 symptoms began, with 77.5% having symptoms of at least one PACS cluster. Of these clusters, 34.9% were neurocognitive, 53.2% were respiratory, 26.4% were musculoskeletal, 29.4% were psychological, 25.1% were dermatologic, and 17.5% were sensory.
At the later clinical visit for PACS symptoms, all patients underwent screening for MAFLD, which was defined as the presence of liver steatosis plus overweight/obesity or type 2 diabetes. Hepatic steatosis was determined from controlled attenuation parameter using transient elastrography. The analysis excluded patients with significant alcohol intake or hepatitis B or C. All patients with liver steatosis also had MAFLD, and this included 55.3% of the study population.
The hospital was able to obtain hepatic steatosis index (HSI) scores for 103 of 235 patients. Of these, 50% had MAFLD on admission for acute COVID-19, and 48.1% had MAFLD upon discharge based on this criterion. At the PACS follow-up visit, 71.3% were diagnosed with MAFLD. There was no statistically significant difference in the use of glucocorticoids or tocilizumab during hospitalization between those with and without MAFLD, and remdesivir use was insignificant in the patient population.
Given that the prevalence of MAFLD among the study population is more than double that in the general population, the authors suggest that MAFLD may be a new PACS cluster phenotype that could lead to long-term metabolic and cardiovascular complications. A potential explanation is loss of lean body mass during COVID-19 hospitalization followed by liver fat accumulation during recovery.
Other infections have also shown an association with increased MAFLD incidence, including HIV, Heliobacter pylori, and viral hepatitis. The authors worry that COVID-19 infection could exacerbate underlying conditions to a more severe MAFLD disease state.
The study is limited by a small sample size, limited follow-up, and the lack of a control group. Its retrospective nature leaves it vulnerable to biases.
“The natural history of MAFLD in the context of PACS is unknown at this time, and careful follow-up of these patients is needed to understand the clinical implications of this syndrome in the context of long COVID,” the authors wrote. “We speculate that [MAFLD] may be considered as an independent PACS-cluster phenotype, potentially affecting the metabolic and cardiovascular health of patients with PACS.”
One author has relationships with several pharmaceutical companies, but the remaining authors reported no conflicts of interest. Dr. Martin has no relevant financial disclosures.
Postacute COVID syndrome (PACS), an ongoing inflammatory state following infection with SARS-CoV-2, is associated with greater risk of metabolic-associated fatty liver disease (MAFLD), according to an analysis of patients at a single clinic in Canada published in Open Forum Infectious Diseases.
MAFLD, also known as nonalcoholic fatty liver disease (NAFLD), is considered an indicator of general health and is in turn linked to greater risk of cardiovascular complications and mortality. It may be a multisystem disorder with various underlying causes.
PACS includes symptoms that affect various organ systems, with neurocognitive, autonomic, gastrointestinal, respiratory, musculoskeletal, psychological, sensory, and dermatologic clusters. An estimated 50%-80% of COVID-19 patients experience one or more clusters of symptoms 3 months after leaving the hospital.
But liver problems also appear in the acute phase, said Paul Martin, MD, who was asked to comment on the study. “Up to about half the patients during the acute illness may have elevated liver tests, but there seems to be a subset of patients in whom the abnormality persists. And then there are some reports in the literature of patients developing injury to their bile ducts in the liver over the long term, apparently as a consequence of COVID infection. What this paper suggests is that there may be some metabolic derangements associated with COVID infection, which in turn can accentuate or possibly cause fatty liver,” said Dr. Martin in an interview. He is chief of digestive health and liver diseases and a professor of medicine at the University of Miami.
“It highlights the need to get vaccinated against COVID and to take appropriate precautions because contracting the infection may lead to all sorts of consequences quite apart from having a respiratory illness,” said Dr. Martin.
The researchers retrospectively identified 235 patients hospitalized with COVID-19 between July 2020 and April 2021. Overall, 69% were men, and the median age was 61 years; 19.2% underwent mechanical ventilation and the mean duration of hospitalization was 11.7 days. They were seen for PACS symptoms a median 143 days after COVID-19 symptoms began, with 77.5% having symptoms of at least one PACS cluster. Of these clusters, 34.9% were neurocognitive, 53.2% were respiratory, 26.4% were musculoskeletal, 29.4% were psychological, 25.1% were dermatologic, and 17.5% were sensory.
At the later clinical visit for PACS symptoms, all patients underwent screening for MAFLD, which was defined as the presence of liver steatosis plus overweight/obesity or type 2 diabetes. Hepatic steatosis was determined from controlled attenuation parameter using transient elastrography. The analysis excluded patients with significant alcohol intake or hepatitis B or C. All patients with liver steatosis also had MAFLD, and this included 55.3% of the study population.
The hospital was able to obtain hepatic steatosis index (HSI) scores for 103 of 235 patients. Of these, 50% had MAFLD on admission for acute COVID-19, and 48.1% had MAFLD upon discharge based on this criterion. At the PACS follow-up visit, 71.3% were diagnosed with MAFLD. There was no statistically significant difference in the use of glucocorticoids or tocilizumab during hospitalization between those with and without MAFLD, and remdesivir use was insignificant in the patient population.
Given that the prevalence of MAFLD among the study population is more than double that in the general population, the authors suggest that MAFLD may be a new PACS cluster phenotype that could lead to long-term metabolic and cardiovascular complications. A potential explanation is loss of lean body mass during COVID-19 hospitalization followed by liver fat accumulation during recovery.
Other infections have also shown an association with increased MAFLD incidence, including HIV, Heliobacter pylori, and viral hepatitis. The authors worry that COVID-19 infection could exacerbate underlying conditions to a more severe MAFLD disease state.
The study is limited by a small sample size, limited follow-up, and the lack of a control group. Its retrospective nature leaves it vulnerable to biases.
“The natural history of MAFLD in the context of PACS is unknown at this time, and careful follow-up of these patients is needed to understand the clinical implications of this syndrome in the context of long COVID,” the authors wrote. “We speculate that [MAFLD] may be considered as an independent PACS-cluster phenotype, potentially affecting the metabolic and cardiovascular health of patients with PACS.”
One author has relationships with several pharmaceutical companies, but the remaining authors reported no conflicts of interest. Dr. Martin has no relevant financial disclosures.
Postacute COVID syndrome (PACS), an ongoing inflammatory state following infection with SARS-CoV-2, is associated with greater risk of metabolic-associated fatty liver disease (MAFLD), according to an analysis of patients at a single clinic in Canada published in Open Forum Infectious Diseases.
MAFLD, also known as nonalcoholic fatty liver disease (NAFLD), is considered an indicator of general health and is in turn linked to greater risk of cardiovascular complications and mortality. It may be a multisystem disorder with various underlying causes.
PACS includes symptoms that affect various organ systems, with neurocognitive, autonomic, gastrointestinal, respiratory, musculoskeletal, psychological, sensory, and dermatologic clusters. An estimated 50%-80% of COVID-19 patients experience one or more clusters of symptoms 3 months after leaving the hospital.
But liver problems also appear in the acute phase, said Paul Martin, MD, who was asked to comment on the study. “Up to about half the patients during the acute illness may have elevated liver tests, but there seems to be a subset of patients in whom the abnormality persists. And then there are some reports in the literature of patients developing injury to their bile ducts in the liver over the long term, apparently as a consequence of COVID infection. What this paper suggests is that there may be some metabolic derangements associated with COVID infection, which in turn can accentuate or possibly cause fatty liver,” said Dr. Martin in an interview. He is chief of digestive health and liver diseases and a professor of medicine at the University of Miami.
“It highlights the need to get vaccinated against COVID and to take appropriate precautions because contracting the infection may lead to all sorts of consequences quite apart from having a respiratory illness,” said Dr. Martin.
The researchers retrospectively identified 235 patients hospitalized with COVID-19 between July 2020 and April 2021. Overall, 69% were men, and the median age was 61 years; 19.2% underwent mechanical ventilation and the mean duration of hospitalization was 11.7 days. They were seen for PACS symptoms a median 143 days after COVID-19 symptoms began, with 77.5% having symptoms of at least one PACS cluster. Of these clusters, 34.9% were neurocognitive, 53.2% were respiratory, 26.4% were musculoskeletal, 29.4% were psychological, 25.1% were dermatologic, and 17.5% were sensory.
At the later clinical visit for PACS symptoms, all patients underwent screening for MAFLD, which was defined as the presence of liver steatosis plus overweight/obesity or type 2 diabetes. Hepatic steatosis was determined from controlled attenuation parameter using transient elastrography. The analysis excluded patients with significant alcohol intake or hepatitis B or C. All patients with liver steatosis also had MAFLD, and this included 55.3% of the study population.
The hospital was able to obtain hepatic steatosis index (HSI) scores for 103 of 235 patients. Of these, 50% had MAFLD on admission for acute COVID-19, and 48.1% had MAFLD upon discharge based on this criterion. At the PACS follow-up visit, 71.3% were diagnosed with MAFLD. There was no statistically significant difference in the use of glucocorticoids or tocilizumab during hospitalization between those with and without MAFLD, and remdesivir use was insignificant in the patient population.
Given that the prevalence of MAFLD among the study population is more than double that in the general population, the authors suggest that MAFLD may be a new PACS cluster phenotype that could lead to long-term metabolic and cardiovascular complications. A potential explanation is loss of lean body mass during COVID-19 hospitalization followed by liver fat accumulation during recovery.
Other infections have also shown an association with increased MAFLD incidence, including HIV, Heliobacter pylori, and viral hepatitis. The authors worry that COVID-19 infection could exacerbate underlying conditions to a more severe MAFLD disease state.
The study is limited by a small sample size, limited follow-up, and the lack of a control group. Its retrospective nature leaves it vulnerable to biases.
“The natural history of MAFLD in the context of PACS is unknown at this time, and careful follow-up of these patients is needed to understand the clinical implications of this syndrome in the context of long COVID,” the authors wrote. “We speculate that [MAFLD] may be considered as an independent PACS-cluster phenotype, potentially affecting the metabolic and cardiovascular health of patients with PACS.”
One author has relationships with several pharmaceutical companies, but the remaining authors reported no conflicts of interest. Dr. Martin has no relevant financial disclosures.
FROM OPEN FORUM INFECTIOUS DISEASES
Sleeve, RYGB reduce liver fat in type 2 diabetes
Both Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are effective at improving hepatic steatosis in type 2 diabetes patients, according to a new analysis of a randomized, controlled trial.
Both procedures resulted in near elimination of liver fat 1 year after the surgery, but the effect on liver fibrosis was less clear. The authors called for more research to examine longer-term effects on fibrosis.
“Both gastric bypass and the sleeve had complete resolution of the liver fat based on their MRI findings. That’s impressive,” said Ali Aminian, MD, who was asked to comment on the study. Dr. Aminian is a professor of surgery and director of the Bariatric & Metabolic Institute at the Cleveland Clinic.
About 25% of the general population, and about 90% of people with type 2 diabetes and obesity have nonalcoholic fatty liver disease (NAFLD), which can lead to liver failure or hepatocellular carcinoma. Hepatic steatosis can combine with obesity, insulin resistance, and inflammation to heighten the risk of cardiovascular disease.
Moderate weight loss can clear liver fat and lead to histologic improvement of hepatic steatosis, and retrospective studies have suggested that RYGB may be more effective than SG and gastric banding in countering hepatic steatosis and steatohepatitis.
In fact, Dr. Aminian recently coauthored a paper describing results from the SPLENDOR study, which looked at 650 adults with obesity and nonalcoholic steatohepatitis (NASH) who underwent bariatric surgery at U.S. hospitals between 2004 and 2016, and compared liver biopsy outcomes to 508 patients who went through nonsurgical weight loss protocols.
After a median follow-up of 7 years, 2.3% In the bariatric surgery group had major adverse liver outcomes, compared with 9.6% in the nonsurgical group (adjusted hazard ratio, 0.12; P = .01). The cumulative incidence of major adverse cardiovascular events (MACE) was 8.5% in the bariatric surgery group and 15.7% in the nonsurgery group (aHR, 0.30; P = .007). 0.6% of the surgical group died within the first year after surgery from surgical complications.
Still, the question has not been tested in a randomized, controlled trial.
In the study published online in the Annals of Internal Medicine, researchers led by Kathrine Aglen Seeberg, MD, and Jens Kristoffer Hertel, PhD, of Vestfold Hospital Trust, Tønsberg, Norway, conducted a prespecified secondary analysis of data from 100 patients (65% female, mean age, 47.5 years) with type 2 diabetes who had been randomized to undergo RYGB or SG between January 2013 and February 2018 at their center.
Prior to surgery, the mean liver fat fraction (LFF) was 19% (stand deviation, 12%). In the SG and RYGB groups, 24% and 26% of patients had no or low-grade steatosis (LFF ≤ 10%). LFF declined by 13% in both groups at 5 weeks, and by 20% and 22% at 1 year, respectively, with no significant difference between the two groups.
At 1 year, 100% of the RYGB group had no or low-grade steatosis, as did 94% in the SG group (no significant difference). At 1 year, both groups had similar percentage decreases in the NAFLD liver fat score (between group difference, –0.05) and NAFLD liver fat percentage (between-group difference, –0.3; no significant difference for either).
At baseline, 6% of the RYGB group and 8% of the SG group had severe fibrosis as measured by the enhanced liver fibrosis (ELF) test. At 1 year, the respective frequencies were 9% and 15%, which were not statistically significant changes.
There was much variation in ELF score changes between Individuals, but 18% moved to a higher ELF category and only 5% improved to a lower ELF category at 1 year.
Limitations of the study include the fact that it was conducted at a single center and in a predominantly White population. The study also did not use liver biopsy, which is the standard for measuring fibrosis. Individuals with type 2 diabetes may have more severe NAFLD, which could limit the applicability to individuals without type 2 diabetes.
Together, the studies produce a clear clinical message, according to Dr. Aminian. “It provides compelling evidence for patients and medical providers that, if we can help patients lose weight, we can reverse fatty liver disease,” he said.
The study was funded by the Southeastern Norway Regional Health Authority. Dr. Aminian has received research support from Medtronic.
Both Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are effective at improving hepatic steatosis in type 2 diabetes patients, according to a new analysis of a randomized, controlled trial.
Both procedures resulted in near elimination of liver fat 1 year after the surgery, but the effect on liver fibrosis was less clear. The authors called for more research to examine longer-term effects on fibrosis.
“Both gastric bypass and the sleeve had complete resolution of the liver fat based on their MRI findings. That’s impressive,” said Ali Aminian, MD, who was asked to comment on the study. Dr. Aminian is a professor of surgery and director of the Bariatric & Metabolic Institute at the Cleveland Clinic.
About 25% of the general population, and about 90% of people with type 2 diabetes and obesity have nonalcoholic fatty liver disease (NAFLD), which can lead to liver failure or hepatocellular carcinoma. Hepatic steatosis can combine with obesity, insulin resistance, and inflammation to heighten the risk of cardiovascular disease.
Moderate weight loss can clear liver fat and lead to histologic improvement of hepatic steatosis, and retrospective studies have suggested that RYGB may be more effective than SG and gastric banding in countering hepatic steatosis and steatohepatitis.
In fact, Dr. Aminian recently coauthored a paper describing results from the SPLENDOR study, which looked at 650 adults with obesity and nonalcoholic steatohepatitis (NASH) who underwent bariatric surgery at U.S. hospitals between 2004 and 2016, and compared liver biopsy outcomes to 508 patients who went through nonsurgical weight loss protocols.
After a median follow-up of 7 years, 2.3% In the bariatric surgery group had major adverse liver outcomes, compared with 9.6% in the nonsurgical group (adjusted hazard ratio, 0.12; P = .01). The cumulative incidence of major adverse cardiovascular events (MACE) was 8.5% in the bariatric surgery group and 15.7% in the nonsurgery group (aHR, 0.30; P = .007). 0.6% of the surgical group died within the first year after surgery from surgical complications.
Still, the question has not been tested in a randomized, controlled trial.
In the study published online in the Annals of Internal Medicine, researchers led by Kathrine Aglen Seeberg, MD, and Jens Kristoffer Hertel, PhD, of Vestfold Hospital Trust, Tønsberg, Norway, conducted a prespecified secondary analysis of data from 100 patients (65% female, mean age, 47.5 years) with type 2 diabetes who had been randomized to undergo RYGB or SG between January 2013 and February 2018 at their center.
Prior to surgery, the mean liver fat fraction (LFF) was 19% (stand deviation, 12%). In the SG and RYGB groups, 24% and 26% of patients had no or low-grade steatosis (LFF ≤ 10%). LFF declined by 13% in both groups at 5 weeks, and by 20% and 22% at 1 year, respectively, with no significant difference between the two groups.
At 1 year, 100% of the RYGB group had no or low-grade steatosis, as did 94% in the SG group (no significant difference). At 1 year, both groups had similar percentage decreases in the NAFLD liver fat score (between group difference, –0.05) and NAFLD liver fat percentage (between-group difference, –0.3; no significant difference for either).
At baseline, 6% of the RYGB group and 8% of the SG group had severe fibrosis as measured by the enhanced liver fibrosis (ELF) test. At 1 year, the respective frequencies were 9% and 15%, which were not statistically significant changes.
There was much variation in ELF score changes between Individuals, but 18% moved to a higher ELF category and only 5% improved to a lower ELF category at 1 year.
Limitations of the study include the fact that it was conducted at a single center and in a predominantly White population. The study also did not use liver biopsy, which is the standard for measuring fibrosis. Individuals with type 2 diabetes may have more severe NAFLD, which could limit the applicability to individuals without type 2 diabetes.
Together, the studies produce a clear clinical message, according to Dr. Aminian. “It provides compelling evidence for patients and medical providers that, if we can help patients lose weight, we can reverse fatty liver disease,” he said.
The study was funded by the Southeastern Norway Regional Health Authority. Dr. Aminian has received research support from Medtronic.
Both Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are effective at improving hepatic steatosis in type 2 diabetes patients, according to a new analysis of a randomized, controlled trial.
Both procedures resulted in near elimination of liver fat 1 year after the surgery, but the effect on liver fibrosis was less clear. The authors called for more research to examine longer-term effects on fibrosis.
“Both gastric bypass and the sleeve had complete resolution of the liver fat based on their MRI findings. That’s impressive,” said Ali Aminian, MD, who was asked to comment on the study. Dr. Aminian is a professor of surgery and director of the Bariatric & Metabolic Institute at the Cleveland Clinic.
About 25% of the general population, and about 90% of people with type 2 diabetes and obesity have nonalcoholic fatty liver disease (NAFLD), which can lead to liver failure or hepatocellular carcinoma. Hepatic steatosis can combine with obesity, insulin resistance, and inflammation to heighten the risk of cardiovascular disease.
Moderate weight loss can clear liver fat and lead to histologic improvement of hepatic steatosis, and retrospective studies have suggested that RYGB may be more effective than SG and gastric banding in countering hepatic steatosis and steatohepatitis.
In fact, Dr. Aminian recently coauthored a paper describing results from the SPLENDOR study, which looked at 650 adults with obesity and nonalcoholic steatohepatitis (NASH) who underwent bariatric surgery at U.S. hospitals between 2004 and 2016, and compared liver biopsy outcomes to 508 patients who went through nonsurgical weight loss protocols.
After a median follow-up of 7 years, 2.3% In the bariatric surgery group had major adverse liver outcomes, compared with 9.6% in the nonsurgical group (adjusted hazard ratio, 0.12; P = .01). The cumulative incidence of major adverse cardiovascular events (MACE) was 8.5% in the bariatric surgery group and 15.7% in the nonsurgery group (aHR, 0.30; P = .007). 0.6% of the surgical group died within the first year after surgery from surgical complications.
Still, the question has not been tested in a randomized, controlled trial.
In the study published online in the Annals of Internal Medicine, researchers led by Kathrine Aglen Seeberg, MD, and Jens Kristoffer Hertel, PhD, of Vestfold Hospital Trust, Tønsberg, Norway, conducted a prespecified secondary analysis of data from 100 patients (65% female, mean age, 47.5 years) with type 2 diabetes who had been randomized to undergo RYGB or SG between January 2013 and February 2018 at their center.
Prior to surgery, the mean liver fat fraction (LFF) was 19% (stand deviation, 12%). In the SG and RYGB groups, 24% and 26% of patients had no or low-grade steatosis (LFF ≤ 10%). LFF declined by 13% in both groups at 5 weeks, and by 20% and 22% at 1 year, respectively, with no significant difference between the two groups.
At 1 year, 100% of the RYGB group had no or low-grade steatosis, as did 94% in the SG group (no significant difference). At 1 year, both groups had similar percentage decreases in the NAFLD liver fat score (between group difference, –0.05) and NAFLD liver fat percentage (between-group difference, –0.3; no significant difference for either).
At baseline, 6% of the RYGB group and 8% of the SG group had severe fibrosis as measured by the enhanced liver fibrosis (ELF) test. At 1 year, the respective frequencies were 9% and 15%, which were not statistically significant changes.
There was much variation in ELF score changes between Individuals, but 18% moved to a higher ELF category and only 5% improved to a lower ELF category at 1 year.
Limitations of the study include the fact that it was conducted at a single center and in a predominantly White population. The study also did not use liver biopsy, which is the standard for measuring fibrosis. Individuals with type 2 diabetes may have more severe NAFLD, which could limit the applicability to individuals without type 2 diabetes.
Together, the studies produce a clear clinical message, according to Dr. Aminian. “It provides compelling evidence for patients and medical providers that, if we can help patients lose weight, we can reverse fatty liver disease,” he said.
The study was funded by the Southeastern Norway Regional Health Authority. Dr. Aminian has received research support from Medtronic.
FROM ANNALS OF INTERNAL MEDICINE
Home-based system relieves refractory ascites in cirrhosis
A home-based tunneled peritoneal catheter (PeCa) drainage system provided significant relief for patients with refractory ascites who were not candidates for transjugular intrahepatic portosystemic shunt (TIPS).
For these patients, the current standard of care is repeated large volume paracentesis, but this can require frequent hospital trips that can be costly and onerous.
The PeCa system consists of one part that lays in the peritoneal cavity, then a tunnel through subcutaneous tissue and an external port where the patient can connect drainage bags. It has been tested and found to provide relief for patients with malignant ascites, but there is little data available for patients with cirrhosis, according to Tammo Lambert Tergast, MD, who presented the study at the annual meeting of the American Association for the Study of Liver Diseases. Dr. Tergast is a resident in the department of gastroenterology, hepatology, and endocrinology at Hannover (Germany) Medical School.
“Patients with refractory ascites have a very high risk for rehospitalization, AKI [acute kidney injury], and death. Our data indicate that PeCa could be a valuable new treatment option for patients with refractory ascites and contraindication for TIPS. However, the risk for hyponatremia and AKI has to be considered and further explored,” said Dr. Tergast during his presentation.
The researchers retrospectively analyzed outcomes in 152 patients with refractory ascites who received a PeCa implant and 71 patients who received standard of care (SOC), which included repeated large volume paracentesis and albumin. The median explant-free survival was 74 days, and just under 50% were explant free at 90 days.
52 patients had the PeCa system removed: 54% because of an infection, 15% because of liver transplant, 12% because of dysfunction, and 10% because of accidental removal.
Factors associated with 90-day survival included PeCa (hazard ratio, 0.52; P = .05) and each point of Model for End-Stage Liver Disease (MELD) score (HR, 1.16; P = .001). There was a trend toward a higher incidence of hyponatremia in the PeCa group (P = .09).
Hospitalizations were more common in the PeCa group (P = .035), but there was no significant difference in mortality between the two groups. Reasons for hospitalization included spontaneous bacterial peritonitis (SBP; 18% in PeCa vs. 8% of SOC), hyponatremia (10% vs. 0%), and infections other than SBP (4% and 16%).
A propensity score–matched analysis that included age, history of SBP, platelet count, serum albumin levels, and MELD score found no significant differences between the two groups, but there were trends in the PeCa group towards higher 90-day survival (P = .16) and a higher frequency of acute kidney injury (P = .08).
Although the appropriate patient population for the system would be small, “once you get to refractory ascites, management of these individuals is really, really challenging, especially people that had contraindications to a TIPS procedure. Anything that you can do to improve their quality of life and help with management is definitely desired,” said Nancy Reau, MD, who was asked to comment on the study. Dr. Reau is chief of the section of hepatology at Rush University Medical Center, Chicago.
The study found little difference in infection risk between the PeCa and standard of care group, but there was a trend toward more hyponatremia in the PeCa group. That could be caused by reduced contact with the health system, according to Dr. Reau, since physicians may be keeping an eye on electrolytes, diuretics, and other factors during paracentesis visits. “But as long as you’re setting up home nursing or some other way to make sure that you’re managing them appropriately, that should be something that is overcome with awareness,” said Dr. Reau.
During the question-and-answer following the presentation, Dr. Tergast was asked about the heightened frequency of hospitalizations in the PeCa group. He posited that the observation may be caused by the retrospective nature of the study. His center is a tertiary care center, which accepts referrals from all over Germany. When a problem occurs with a PeCa, patients often get referred back to the tertiary center, leading to a higher number of hospitalizations observed in that group. “So this might be a bias in the analysis,” he said.
“I think if we can optimize the treatment after discharge, we can also minimize the rehospitalization in these patients. Rehospitalization rate because of ascites was quite low,” said Dr. Tergast.
Dr. Tergast and Dr. Reau have no relevant financial disclosures.
A home-based tunneled peritoneal catheter (PeCa) drainage system provided significant relief for patients with refractory ascites who were not candidates for transjugular intrahepatic portosystemic shunt (TIPS).
For these patients, the current standard of care is repeated large volume paracentesis, but this can require frequent hospital trips that can be costly and onerous.
The PeCa system consists of one part that lays in the peritoneal cavity, then a tunnel through subcutaneous tissue and an external port where the patient can connect drainage bags. It has been tested and found to provide relief for patients with malignant ascites, but there is little data available for patients with cirrhosis, according to Tammo Lambert Tergast, MD, who presented the study at the annual meeting of the American Association for the Study of Liver Diseases. Dr. Tergast is a resident in the department of gastroenterology, hepatology, and endocrinology at Hannover (Germany) Medical School.
“Patients with refractory ascites have a very high risk for rehospitalization, AKI [acute kidney injury], and death. Our data indicate that PeCa could be a valuable new treatment option for patients with refractory ascites and contraindication for TIPS. However, the risk for hyponatremia and AKI has to be considered and further explored,” said Dr. Tergast during his presentation.
The researchers retrospectively analyzed outcomes in 152 patients with refractory ascites who received a PeCa implant and 71 patients who received standard of care (SOC), which included repeated large volume paracentesis and albumin. The median explant-free survival was 74 days, and just under 50% were explant free at 90 days.
52 patients had the PeCa system removed: 54% because of an infection, 15% because of liver transplant, 12% because of dysfunction, and 10% because of accidental removal.
Factors associated with 90-day survival included PeCa (hazard ratio, 0.52; P = .05) and each point of Model for End-Stage Liver Disease (MELD) score (HR, 1.16; P = .001). There was a trend toward a higher incidence of hyponatremia in the PeCa group (P = .09).
Hospitalizations were more common in the PeCa group (P = .035), but there was no significant difference in mortality between the two groups. Reasons for hospitalization included spontaneous bacterial peritonitis (SBP; 18% in PeCa vs. 8% of SOC), hyponatremia (10% vs. 0%), and infections other than SBP (4% and 16%).
A propensity score–matched analysis that included age, history of SBP, platelet count, serum albumin levels, and MELD score found no significant differences between the two groups, but there were trends in the PeCa group towards higher 90-day survival (P = .16) and a higher frequency of acute kidney injury (P = .08).
Although the appropriate patient population for the system would be small, “once you get to refractory ascites, management of these individuals is really, really challenging, especially people that had contraindications to a TIPS procedure. Anything that you can do to improve their quality of life and help with management is definitely desired,” said Nancy Reau, MD, who was asked to comment on the study. Dr. Reau is chief of the section of hepatology at Rush University Medical Center, Chicago.
The study found little difference in infection risk between the PeCa and standard of care group, but there was a trend toward more hyponatremia in the PeCa group. That could be caused by reduced contact with the health system, according to Dr. Reau, since physicians may be keeping an eye on electrolytes, diuretics, and other factors during paracentesis visits. “But as long as you’re setting up home nursing or some other way to make sure that you’re managing them appropriately, that should be something that is overcome with awareness,” said Dr. Reau.
During the question-and-answer following the presentation, Dr. Tergast was asked about the heightened frequency of hospitalizations in the PeCa group. He posited that the observation may be caused by the retrospective nature of the study. His center is a tertiary care center, which accepts referrals from all over Germany. When a problem occurs with a PeCa, patients often get referred back to the tertiary center, leading to a higher number of hospitalizations observed in that group. “So this might be a bias in the analysis,” he said.
“I think if we can optimize the treatment after discharge, we can also minimize the rehospitalization in these patients. Rehospitalization rate because of ascites was quite low,” said Dr. Tergast.
Dr. Tergast and Dr. Reau have no relevant financial disclosures.
A home-based tunneled peritoneal catheter (PeCa) drainage system provided significant relief for patients with refractory ascites who were not candidates for transjugular intrahepatic portosystemic shunt (TIPS).
For these patients, the current standard of care is repeated large volume paracentesis, but this can require frequent hospital trips that can be costly and onerous.
The PeCa system consists of one part that lays in the peritoneal cavity, then a tunnel through subcutaneous tissue and an external port where the patient can connect drainage bags. It has been tested and found to provide relief for patients with malignant ascites, but there is little data available for patients with cirrhosis, according to Tammo Lambert Tergast, MD, who presented the study at the annual meeting of the American Association for the Study of Liver Diseases. Dr. Tergast is a resident in the department of gastroenterology, hepatology, and endocrinology at Hannover (Germany) Medical School.
“Patients with refractory ascites have a very high risk for rehospitalization, AKI [acute kidney injury], and death. Our data indicate that PeCa could be a valuable new treatment option for patients with refractory ascites and contraindication for TIPS. However, the risk for hyponatremia and AKI has to be considered and further explored,” said Dr. Tergast during his presentation.
The researchers retrospectively analyzed outcomes in 152 patients with refractory ascites who received a PeCa implant and 71 patients who received standard of care (SOC), which included repeated large volume paracentesis and albumin. The median explant-free survival was 74 days, and just under 50% were explant free at 90 days.
52 patients had the PeCa system removed: 54% because of an infection, 15% because of liver transplant, 12% because of dysfunction, and 10% because of accidental removal.
Factors associated with 90-day survival included PeCa (hazard ratio, 0.52; P = .05) and each point of Model for End-Stage Liver Disease (MELD) score (HR, 1.16; P = .001). There was a trend toward a higher incidence of hyponatremia in the PeCa group (P = .09).
Hospitalizations were more common in the PeCa group (P = .035), but there was no significant difference in mortality between the two groups. Reasons for hospitalization included spontaneous bacterial peritonitis (SBP; 18% in PeCa vs. 8% of SOC), hyponatremia (10% vs. 0%), and infections other than SBP (4% and 16%).
A propensity score–matched analysis that included age, history of SBP, platelet count, serum albumin levels, and MELD score found no significant differences between the two groups, but there were trends in the PeCa group towards higher 90-day survival (P = .16) and a higher frequency of acute kidney injury (P = .08).
Although the appropriate patient population for the system would be small, “once you get to refractory ascites, management of these individuals is really, really challenging, especially people that had contraindications to a TIPS procedure. Anything that you can do to improve their quality of life and help with management is definitely desired,” said Nancy Reau, MD, who was asked to comment on the study. Dr. Reau is chief of the section of hepatology at Rush University Medical Center, Chicago.
The study found little difference in infection risk between the PeCa and standard of care group, but there was a trend toward more hyponatremia in the PeCa group. That could be caused by reduced contact with the health system, according to Dr. Reau, since physicians may be keeping an eye on electrolytes, diuretics, and other factors during paracentesis visits. “But as long as you’re setting up home nursing or some other way to make sure that you’re managing them appropriately, that should be something that is overcome with awareness,” said Dr. Reau.
During the question-and-answer following the presentation, Dr. Tergast was asked about the heightened frequency of hospitalizations in the PeCa group. He posited that the observation may be caused by the retrospective nature of the study. His center is a tertiary care center, which accepts referrals from all over Germany. When a problem occurs with a PeCa, patients often get referred back to the tertiary center, leading to a higher number of hospitalizations observed in that group. “So this might be a bias in the analysis,” he said.
“I think if we can optimize the treatment after discharge, we can also minimize the rehospitalization in these patients. Rehospitalization rate because of ascites was quite low,” said Dr. Tergast.
Dr. Tergast and Dr. Reau have no relevant financial disclosures.
FROM THE LIVER MEETING
FIB-4 could ID liver risk in primary care
Fibrosis-4 index (FIB-4) scores are strongly associated with severe liver disease outcomes in a primary care population, both in patients with known chronic liver disease and those without known CLD. The result could help identify patients with CLD before their condition becomes severe.
FIB-4 has previously shown utility in predicting the risk of advanced fibrosis in patients with viral hepatitis B and C, nonalcoholic fatty liver disease (NAFLD), nonalcoholic steatohepatitis (NASH), and alcohol-related liver disease.
“This is really important in primary care because FIB-4 is easy to calculate. Its inputs are accessible, and it is inexpensive, often taking advantage of labs that we’ve ordered anyway. And if we can use it to find advanced fibrosis, it will be critically important because we know that advanced fibrosis is associated with severe liver outcomes – these are going to be patients that we need to make sure are in touch with our hepatology colleagues,” said Andrew Schreiner, MD, during a presentation of the results at the annual meeting of the American Association for the Study of Liver Diseases. Dr. Schreiner is general internist at the Medical University of South Carolina, Charleston.
He also noted that FIB-4 is playing an important role in the assessment of NAFLD and NASH. Many newer algorithms to manage NAFLD in the primary care setting rely on FIB-4, but that application is limited because NAFLD is underdiagnosed according to administrative database studies, which found rates of about 2%-5% despite the fact that estimates put it at having a prevalence of 25%-30% in the U.S. population.
To determine if FIB-4 scores could assist in identifying primary care patients at risk of severe outcomes, including cirrhosis, hepatocellular carcinoma, and liver transplant, the researchers conducted a retrospective analysis of primary care electronic health care data from 20,556 patients between 2007 and 2018 who were seen at their institution. Participants had ALT and AST values less than 500 IU/L, as well as a platelet count within two months preceding or on the day of the liver enzyme tests. They excluded individuals with known chronic or severe liver disease.
65% of patients were female, 45% were Black, and the mean BMI was 29.8 kg/m2. 64% of participants were ranked as low risk (FIB-4 ≤1.3), 29% with undetermined risk (1.3-2.67), and 7% with high risk (>2.67).
The population had more liver risk than expected. “[It is] a distribution that certainly may have more high risk and indeterminant risks than we would have anticipated, but we have seen this in external studies,” said Dr. Schreiner.
Over a mean follow-up period of 8.2 years, 11% were diagnosed with CLD: 2.3% developed NAFLD, 8.2% another CLD, and 0.5% had NAFLD and another CLD. About 4% developed a severe CLD. A severe liver outcome occurred in 2.2% of those who had been classified as FIB-4 low risk, 4.2% classified as indeterminate risk, and 20.8% of those classified as high risk.
“Troublingly,” said Dr. Schreiner, 49% of those who went on to develop a severe liver outcome had no CLD diagnosis before it occurred. “This is a tremendous opportunity to improve diagnosis in this setting.”
After adjustment for race, gender, marital status, smoking history, BMI, and various comorbidities, the researchers found a higher risk of severe liver disease associated with indeterminate FIB-4 risk score (hazard ratio, 1.62; 95% confidence interval, 1.36-1.92) and a high FIB-4 risk score (HR, 6.64; 95% CI, 5.58-7.90), compared with those with a low FIB-4 risk score. The same was true for individual liver diseases, including NAFLD (indeterminate HR, 1.88; 95% CI, 0.99-3.60; high HR, 7.32; 95% CI, 3.44-15.58), other liver diagnosis (indeterminate HR, 2.65; 95% CI, 1.93-3.63; high HR, 11.39; 95% CI, 8.53-15.20), and NAFLD plus another liver disease (intermediate HR, 2.53; 95% CI, 0.79-8.12; high HR, 6.89; 95% CI, 1.82-26.14).
Dr. Schreiner conceded that the study may not be generalizable, since FIB-4 was not designed for use in general populations, and it was conducted at a single center.
During the question-and-answer session after the talk, Dr. Schreiner was asked if the majority of the 49% who had a severe liver outcome without previous liver disease had NAFLD. He said that was the team’s hypothesis, and they are in the process of examining that data, but a significant number appear to be alcohol related. “For us in the primary care setting, it’s just another opportunity to emphasize that we have to do a better job getting exposure histories, and alcohol histories in particular, and finding ways to document those in ways that we can make diagnoses for patients and for our hepatology colleagues,” said Dr. Schreiner.
Comoderator Kathleen Corey, MD, asked Dr. Schreiner if he had any concerns about false positives from FIB-4 screening, and whether that could lead to overtreatment. “We’ve seen other screening tests leading to patient distress and overutilization of resources. How do you think we might be able to mitigate that?” asked Dr. Corey, who is an assistant professor of medicine at Harvard Medical School and director of the Fatty Liver Clinic at Massachusetts General Hospital, both in Boston.
Dr. Schreiner underscored the need for more physician education about FIB-4, both its potential and its pitfalls, since many primary care providers don’t use it or even know about it. “FIB-4 is very popular in the hepatology literature, but in primary care, we don’t talk about it as often. So I think educational efforts about its possible utility, about some of the drawbacks, or some of the things that might lead to inappropriately positive results – like advanced age, for those of us who see patients 60 and older. Those are really important considerations both for the patient and the provider for management of expectations and concerns. I’m worried too about application in our younger cohorts. The explosion of NAFLD in adolescence, and the likelihood that we might get a false negative in maybe a 28-year-old who might have problematic disease, is a concern as well,” said Dr. Schreiner.
Dr. Schreiner has no relevant financial disclosures. Dr. Corey has been on an advisory committee or review panel for Bristol-Myers Squibb, Novo Nordisk, and Gilead. She has consulted for Novo Nordisk and received research support from BMS, Boehringer Ingelheim, Novartis, and Boehringer Ingelheim.
Fibrosis-4 index (FIB-4) scores are strongly associated with severe liver disease outcomes in a primary care population, both in patients with known chronic liver disease and those without known CLD. The result could help identify patients with CLD before their condition becomes severe.
FIB-4 has previously shown utility in predicting the risk of advanced fibrosis in patients with viral hepatitis B and C, nonalcoholic fatty liver disease (NAFLD), nonalcoholic steatohepatitis (NASH), and alcohol-related liver disease.
“This is really important in primary care because FIB-4 is easy to calculate. Its inputs are accessible, and it is inexpensive, often taking advantage of labs that we’ve ordered anyway. And if we can use it to find advanced fibrosis, it will be critically important because we know that advanced fibrosis is associated with severe liver outcomes – these are going to be patients that we need to make sure are in touch with our hepatology colleagues,” said Andrew Schreiner, MD, during a presentation of the results at the annual meeting of the American Association for the Study of Liver Diseases. Dr. Schreiner is general internist at the Medical University of South Carolina, Charleston.
He also noted that FIB-4 is playing an important role in the assessment of NAFLD and NASH. Many newer algorithms to manage NAFLD in the primary care setting rely on FIB-4, but that application is limited because NAFLD is underdiagnosed according to administrative database studies, which found rates of about 2%-5% despite the fact that estimates put it at having a prevalence of 25%-30% in the U.S. population.
To determine if FIB-4 scores could assist in identifying primary care patients at risk of severe outcomes, including cirrhosis, hepatocellular carcinoma, and liver transplant, the researchers conducted a retrospective analysis of primary care electronic health care data from 20,556 patients between 2007 and 2018 who were seen at their institution. Participants had ALT and AST values less than 500 IU/L, as well as a platelet count within two months preceding or on the day of the liver enzyme tests. They excluded individuals with known chronic or severe liver disease.
65% of patients were female, 45% were Black, and the mean BMI was 29.8 kg/m2. 64% of participants were ranked as low risk (FIB-4 ≤1.3), 29% with undetermined risk (1.3-2.67), and 7% with high risk (>2.67).
The population had more liver risk than expected. “[It is] a distribution that certainly may have more high risk and indeterminant risks than we would have anticipated, but we have seen this in external studies,” said Dr. Schreiner.
Over a mean follow-up period of 8.2 years, 11% were diagnosed with CLD: 2.3% developed NAFLD, 8.2% another CLD, and 0.5% had NAFLD and another CLD. About 4% developed a severe CLD. A severe liver outcome occurred in 2.2% of those who had been classified as FIB-4 low risk, 4.2% classified as indeterminate risk, and 20.8% of those classified as high risk.
“Troublingly,” said Dr. Schreiner, 49% of those who went on to develop a severe liver outcome had no CLD diagnosis before it occurred. “This is a tremendous opportunity to improve diagnosis in this setting.”
After adjustment for race, gender, marital status, smoking history, BMI, and various comorbidities, the researchers found a higher risk of severe liver disease associated with indeterminate FIB-4 risk score (hazard ratio, 1.62; 95% confidence interval, 1.36-1.92) and a high FIB-4 risk score (HR, 6.64; 95% CI, 5.58-7.90), compared with those with a low FIB-4 risk score. The same was true for individual liver diseases, including NAFLD (indeterminate HR, 1.88; 95% CI, 0.99-3.60; high HR, 7.32; 95% CI, 3.44-15.58), other liver diagnosis (indeterminate HR, 2.65; 95% CI, 1.93-3.63; high HR, 11.39; 95% CI, 8.53-15.20), and NAFLD plus another liver disease (intermediate HR, 2.53; 95% CI, 0.79-8.12; high HR, 6.89; 95% CI, 1.82-26.14).
Dr. Schreiner conceded that the study may not be generalizable, since FIB-4 was not designed for use in general populations, and it was conducted at a single center.
During the question-and-answer session after the talk, Dr. Schreiner was asked if the majority of the 49% who had a severe liver outcome without previous liver disease had NAFLD. He said that was the team’s hypothesis, and they are in the process of examining that data, but a significant number appear to be alcohol related. “For us in the primary care setting, it’s just another opportunity to emphasize that we have to do a better job getting exposure histories, and alcohol histories in particular, and finding ways to document those in ways that we can make diagnoses for patients and for our hepatology colleagues,” said Dr. Schreiner.
Comoderator Kathleen Corey, MD, asked Dr. Schreiner if he had any concerns about false positives from FIB-4 screening, and whether that could lead to overtreatment. “We’ve seen other screening tests leading to patient distress and overutilization of resources. How do you think we might be able to mitigate that?” asked Dr. Corey, who is an assistant professor of medicine at Harvard Medical School and director of the Fatty Liver Clinic at Massachusetts General Hospital, both in Boston.
Dr. Schreiner underscored the need for more physician education about FIB-4, both its potential and its pitfalls, since many primary care providers don’t use it or even know about it. “FIB-4 is very popular in the hepatology literature, but in primary care, we don’t talk about it as often. So I think educational efforts about its possible utility, about some of the drawbacks, or some of the things that might lead to inappropriately positive results – like advanced age, for those of us who see patients 60 and older. Those are really important considerations both for the patient and the provider for management of expectations and concerns. I’m worried too about application in our younger cohorts. The explosion of NAFLD in adolescence, and the likelihood that we might get a false negative in maybe a 28-year-old who might have problematic disease, is a concern as well,” said Dr. Schreiner.
Dr. Schreiner has no relevant financial disclosures. Dr. Corey has been on an advisory committee or review panel for Bristol-Myers Squibb, Novo Nordisk, and Gilead. She has consulted for Novo Nordisk and received research support from BMS, Boehringer Ingelheim, Novartis, and Boehringer Ingelheim.
Fibrosis-4 index (FIB-4) scores are strongly associated with severe liver disease outcomes in a primary care population, both in patients with known chronic liver disease and those without known CLD. The result could help identify patients with CLD before their condition becomes severe.
FIB-4 has previously shown utility in predicting the risk of advanced fibrosis in patients with viral hepatitis B and C, nonalcoholic fatty liver disease (NAFLD), nonalcoholic steatohepatitis (NASH), and alcohol-related liver disease.
“This is really important in primary care because FIB-4 is easy to calculate. Its inputs are accessible, and it is inexpensive, often taking advantage of labs that we’ve ordered anyway. And if we can use it to find advanced fibrosis, it will be critically important because we know that advanced fibrosis is associated with severe liver outcomes – these are going to be patients that we need to make sure are in touch with our hepatology colleagues,” said Andrew Schreiner, MD, during a presentation of the results at the annual meeting of the American Association for the Study of Liver Diseases. Dr. Schreiner is general internist at the Medical University of South Carolina, Charleston.
He also noted that FIB-4 is playing an important role in the assessment of NAFLD and NASH. Many newer algorithms to manage NAFLD in the primary care setting rely on FIB-4, but that application is limited because NAFLD is underdiagnosed according to administrative database studies, which found rates of about 2%-5% despite the fact that estimates put it at having a prevalence of 25%-30% in the U.S. population.
To determine if FIB-4 scores could assist in identifying primary care patients at risk of severe outcomes, including cirrhosis, hepatocellular carcinoma, and liver transplant, the researchers conducted a retrospective analysis of primary care electronic health care data from 20,556 patients between 2007 and 2018 who were seen at their institution. Participants had ALT and AST values less than 500 IU/L, as well as a platelet count within two months preceding or on the day of the liver enzyme tests. They excluded individuals with known chronic or severe liver disease.
65% of patients were female, 45% were Black, and the mean BMI was 29.8 kg/m2. 64% of participants were ranked as low risk (FIB-4 ≤1.3), 29% with undetermined risk (1.3-2.67), and 7% with high risk (>2.67).
The population had more liver risk than expected. “[It is] a distribution that certainly may have more high risk and indeterminant risks than we would have anticipated, but we have seen this in external studies,” said Dr. Schreiner.
Over a mean follow-up period of 8.2 years, 11% were diagnosed with CLD: 2.3% developed NAFLD, 8.2% another CLD, and 0.5% had NAFLD and another CLD. About 4% developed a severe CLD. A severe liver outcome occurred in 2.2% of those who had been classified as FIB-4 low risk, 4.2% classified as indeterminate risk, and 20.8% of those classified as high risk.
“Troublingly,” said Dr. Schreiner, 49% of those who went on to develop a severe liver outcome had no CLD diagnosis before it occurred. “This is a tremendous opportunity to improve diagnosis in this setting.”
After adjustment for race, gender, marital status, smoking history, BMI, and various comorbidities, the researchers found a higher risk of severe liver disease associated with indeterminate FIB-4 risk score (hazard ratio, 1.62; 95% confidence interval, 1.36-1.92) and a high FIB-4 risk score (HR, 6.64; 95% CI, 5.58-7.90), compared with those with a low FIB-4 risk score. The same was true for individual liver diseases, including NAFLD (indeterminate HR, 1.88; 95% CI, 0.99-3.60; high HR, 7.32; 95% CI, 3.44-15.58), other liver diagnosis (indeterminate HR, 2.65; 95% CI, 1.93-3.63; high HR, 11.39; 95% CI, 8.53-15.20), and NAFLD plus another liver disease (intermediate HR, 2.53; 95% CI, 0.79-8.12; high HR, 6.89; 95% CI, 1.82-26.14).
Dr. Schreiner conceded that the study may not be generalizable, since FIB-4 was not designed for use in general populations, and it was conducted at a single center.
During the question-and-answer session after the talk, Dr. Schreiner was asked if the majority of the 49% who had a severe liver outcome without previous liver disease had NAFLD. He said that was the team’s hypothesis, and they are in the process of examining that data, but a significant number appear to be alcohol related. “For us in the primary care setting, it’s just another opportunity to emphasize that we have to do a better job getting exposure histories, and alcohol histories in particular, and finding ways to document those in ways that we can make diagnoses for patients and for our hepatology colleagues,” said Dr. Schreiner.
Comoderator Kathleen Corey, MD, asked Dr. Schreiner if he had any concerns about false positives from FIB-4 screening, and whether that could lead to overtreatment. “We’ve seen other screening tests leading to patient distress and overutilization of resources. How do you think we might be able to mitigate that?” asked Dr. Corey, who is an assistant professor of medicine at Harvard Medical School and director of the Fatty Liver Clinic at Massachusetts General Hospital, both in Boston.
Dr. Schreiner underscored the need for more physician education about FIB-4, both its potential and its pitfalls, since many primary care providers don’t use it or even know about it. “FIB-4 is very popular in the hepatology literature, but in primary care, we don’t talk about it as often. So I think educational efforts about its possible utility, about some of the drawbacks, or some of the things that might lead to inappropriately positive results – like advanced age, for those of us who see patients 60 and older. Those are really important considerations both for the patient and the provider for management of expectations and concerns. I’m worried too about application in our younger cohorts. The explosion of NAFLD in adolescence, and the likelihood that we might get a false negative in maybe a 28-year-old who might have problematic disease, is a concern as well,” said Dr. Schreiner.
Dr. Schreiner has no relevant financial disclosures. Dr. Corey has been on an advisory committee or review panel for Bristol-Myers Squibb, Novo Nordisk, and Gilead. She has consulted for Novo Nordisk and received research support from BMS, Boehringer Ingelheim, Novartis, and Boehringer Ingelheim.
FROM THE LIVER MEETING
Bulevirtide shows real-world efficacy versus HDV
A real-world analysis of bulevirtide found a safety and efficacy profile similar to what was seen in earlier clinical trials in the treatment of hepatitis delta virus (HDV) infection.
HDV can only infect patients already carrying hepatitis B virus (HBV), but it causes the most severe form of viral hepatitis as it can progress to cirrhosis within 5 years and to hepatocellular carcinoma within 10 years.
Bulevirtide is a first-in-class medication that mimics the hepatitis B surface antigen, binding to its receptor on hepatocytes and preventing HDV viral particles from binding to it. The drug received conditional marketing approval by the European Medicines Agency in 2020 and has received a breakthrough therapy designation from the U.S. Food and Drug Administration.
The study was presented at the annual meeting of the American Association for the Study of Liver Diseases by Victor De Ledinghen, PhD, who is a professor of hepatology and head of the hepatology and liver transplantation unit at Bordeaux (France) University Hospital.
The early-access program launched after the French National Agency for Medicines and Health Products approved bulevirtide in 2019. It was made available to patients with compensated cirrhosis or severe liver fibrosis (F3) or patients with F2 fibrosis and alanine amino transferase levels more than twice the upper limit of normal for 6 months or more. Patients received bulevirtide alone (n = 77) or in combination with peg-interferon (n = 68), as determined by their physician.
The researchers defined virologic efficacy as HDV RNA levels being undetectable, or decreased by at least 2 log10 from baseline. They defined biochemical efficacy as ALT levels below 40 IU/L.
A per-protocol analysis included all patients in the bulevirtide group, but excluded 12 from the combination group who discontinued peg-interferon (n = 56). Nineteen patients in bulevirtide group had a treatment modification, and seven discontinued treatment. Five in the combination group had a treatment modification, and 14 stopped treatment. At 12 months, there was a greater decline in median log10 IU/mL in the combination group (–5.65 versus –3.64), though the study was not powered to compare the two. At 12 months, the combination group had 93.9% virologic efficacy, compared with 68.3% in the bulevirtide group.
The two groups had similar mean ALT levels at 12 months (48.91 and 48.03 IU/mL, respectively), with more patients in the bulevirtide group having normal ALT levels (<40 IU/L; 48.8% versus 36.4%). At 12 months, 39.0% of the bulevirtide group and 30.3% of the combination group had a combined response, defined as either undetectable HDV RNA or ≥2 log10 from baseline plus normal ALT levels.
Twenty-nine patients in the bulevirtide group had an adverse event, compared with 43 in the combination group. The two groups were similar in the frequency of grade 3-4 adverse events (7 versus 6), discontinuation due to adverse events (2 versus 3), deaths (0 in both), injection-site reactions (2 in both), liver-related adverse events (4 versus 2), and elevated bile acid (76 versus 68).
During the Q&A period following the presentation, Dr. De Ledinghen was asked if he has a preferred regimen for HDV patients. “I think it depends on the tolerance of peg-interferon because of all the side effects with this drug. I think we need to have predictive factors of virological response with or without interferon. At this time, I don’t have a preference, but I think at this time we need to work on predictive factors associated with virologic response,” he said.
The EMA’s conditional bulevirtide approval hinged on results from phase 2 clinical trials, while the phase 3 clinical studies are ongoing. “This was a very unusual step for the EMA to provide what is similar to emergency use approval while the phase 3 clinical trials are still ongoing,” said Anna Lok, MD, who was asked to comment on the study. Dr. Lok is a professor of internal medicine, director of clinical hepatology, and assistant dean for clinical research at the University of Michigan, Ann Arbor.
She noted that the phase 2 studies indicated that the combination with peg-interferon seems to have an additive effect on HDV suppression, while monotherapy with bulevirtide has a greater effect on normalizing ALT levels. The real-world experience confirms these findings.
But the real-world data revealed some concerns. “What really worried me is the large number of patients who required dose modifications or discontinuations, and that seems to be the case in both treatment groups. They didn’t really go into a lot of details [about] why patients needed treatment modifications, but one has to assume that this is due to side effects,” said Dr. Lok.
She also noted that the per-protocol analysis, instead of an intention-to-treat analysis, is a weakness of the study. Additionally, over time, the number of patients analyzed decreased – as many as 40% of patients didn’t have test results at month 12. “It makes you wonder what happened to those patients. Many probably didn’t respond, in which case your overall response rate will be far lower,” said Dr. Lok.
The study was funded by Gilead. Dr. De Ledinghen has financial relationships with Gilead, AbbVie, Echosens, Hologic, Intercept Pharma, Tillotts, Orphalan, Alfasigma, Bristol Myers Squibb, and Siemens Healthineers. Dr. Lok has no relevant financial disclosures.
A real-world analysis of bulevirtide found a safety and efficacy profile similar to what was seen in earlier clinical trials in the treatment of hepatitis delta virus (HDV) infection.
HDV can only infect patients already carrying hepatitis B virus (HBV), but it causes the most severe form of viral hepatitis as it can progress to cirrhosis within 5 years and to hepatocellular carcinoma within 10 years.
Bulevirtide is a first-in-class medication that mimics the hepatitis B surface antigen, binding to its receptor on hepatocytes and preventing HDV viral particles from binding to it. The drug received conditional marketing approval by the European Medicines Agency in 2020 and has received a breakthrough therapy designation from the U.S. Food and Drug Administration.
The study was presented at the annual meeting of the American Association for the Study of Liver Diseases by Victor De Ledinghen, PhD, who is a professor of hepatology and head of the hepatology and liver transplantation unit at Bordeaux (France) University Hospital.
The early-access program launched after the French National Agency for Medicines and Health Products approved bulevirtide in 2019. It was made available to patients with compensated cirrhosis or severe liver fibrosis (F3) or patients with F2 fibrosis and alanine amino transferase levels more than twice the upper limit of normal for 6 months or more. Patients received bulevirtide alone (n = 77) or in combination with peg-interferon (n = 68), as determined by their physician.
The researchers defined virologic efficacy as HDV RNA levels being undetectable, or decreased by at least 2 log10 from baseline. They defined biochemical efficacy as ALT levels below 40 IU/L.
A per-protocol analysis included all patients in the bulevirtide group, but excluded 12 from the combination group who discontinued peg-interferon (n = 56). Nineteen patients in bulevirtide group had a treatment modification, and seven discontinued treatment. Five in the combination group had a treatment modification, and 14 stopped treatment. At 12 months, there was a greater decline in median log10 IU/mL in the combination group (–5.65 versus –3.64), though the study was not powered to compare the two. At 12 months, the combination group had 93.9% virologic efficacy, compared with 68.3% in the bulevirtide group.
The two groups had similar mean ALT levels at 12 months (48.91 and 48.03 IU/mL, respectively), with more patients in the bulevirtide group having normal ALT levels (<40 IU/L; 48.8% versus 36.4%). At 12 months, 39.0% of the bulevirtide group and 30.3% of the combination group had a combined response, defined as either undetectable HDV RNA or ≥2 log10 from baseline plus normal ALT levels.
Twenty-nine patients in the bulevirtide group had an adverse event, compared with 43 in the combination group. The two groups were similar in the frequency of grade 3-4 adverse events (7 versus 6), discontinuation due to adverse events (2 versus 3), deaths (0 in both), injection-site reactions (2 in both), liver-related adverse events (4 versus 2), and elevated bile acid (76 versus 68).
During the Q&A period following the presentation, Dr. De Ledinghen was asked if he has a preferred regimen for HDV patients. “I think it depends on the tolerance of peg-interferon because of all the side effects with this drug. I think we need to have predictive factors of virological response with or without interferon. At this time, I don’t have a preference, but I think at this time we need to work on predictive factors associated with virologic response,” he said.
The EMA’s conditional bulevirtide approval hinged on results from phase 2 clinical trials, while the phase 3 clinical studies are ongoing. “This was a very unusual step for the EMA to provide what is similar to emergency use approval while the phase 3 clinical trials are still ongoing,” said Anna Lok, MD, who was asked to comment on the study. Dr. Lok is a professor of internal medicine, director of clinical hepatology, and assistant dean for clinical research at the University of Michigan, Ann Arbor.
She noted that the phase 2 studies indicated that the combination with peg-interferon seems to have an additive effect on HDV suppression, while monotherapy with bulevirtide has a greater effect on normalizing ALT levels. The real-world experience confirms these findings.
But the real-world data revealed some concerns. “What really worried me is the large number of patients who required dose modifications or discontinuations, and that seems to be the case in both treatment groups. They didn’t really go into a lot of details [about] why patients needed treatment modifications, but one has to assume that this is due to side effects,” said Dr. Lok.
She also noted that the per-protocol analysis, instead of an intention-to-treat analysis, is a weakness of the study. Additionally, over time, the number of patients analyzed decreased – as many as 40% of patients didn’t have test results at month 12. “It makes you wonder what happened to those patients. Many probably didn’t respond, in which case your overall response rate will be far lower,” said Dr. Lok.
The study was funded by Gilead. Dr. De Ledinghen has financial relationships with Gilead, AbbVie, Echosens, Hologic, Intercept Pharma, Tillotts, Orphalan, Alfasigma, Bristol Myers Squibb, and Siemens Healthineers. Dr. Lok has no relevant financial disclosures.
A real-world analysis of bulevirtide found a safety and efficacy profile similar to what was seen in earlier clinical trials in the treatment of hepatitis delta virus (HDV) infection.
HDV can only infect patients already carrying hepatitis B virus (HBV), but it causes the most severe form of viral hepatitis as it can progress to cirrhosis within 5 years and to hepatocellular carcinoma within 10 years.
Bulevirtide is a first-in-class medication that mimics the hepatitis B surface antigen, binding to its receptor on hepatocytes and preventing HDV viral particles from binding to it. The drug received conditional marketing approval by the European Medicines Agency in 2020 and has received a breakthrough therapy designation from the U.S. Food and Drug Administration.
The study was presented at the annual meeting of the American Association for the Study of Liver Diseases by Victor De Ledinghen, PhD, who is a professor of hepatology and head of the hepatology and liver transplantation unit at Bordeaux (France) University Hospital.
The early-access program launched after the French National Agency for Medicines and Health Products approved bulevirtide in 2019. It was made available to patients with compensated cirrhosis or severe liver fibrosis (F3) or patients with F2 fibrosis and alanine amino transferase levels more than twice the upper limit of normal for 6 months or more. Patients received bulevirtide alone (n = 77) or in combination with peg-interferon (n = 68), as determined by their physician.
The researchers defined virologic efficacy as HDV RNA levels being undetectable, or decreased by at least 2 log10 from baseline. They defined biochemical efficacy as ALT levels below 40 IU/L.
A per-protocol analysis included all patients in the bulevirtide group, but excluded 12 from the combination group who discontinued peg-interferon (n = 56). Nineteen patients in bulevirtide group had a treatment modification, and seven discontinued treatment. Five in the combination group had a treatment modification, and 14 stopped treatment. At 12 months, there was a greater decline in median log10 IU/mL in the combination group (–5.65 versus –3.64), though the study was not powered to compare the two. At 12 months, the combination group had 93.9% virologic efficacy, compared with 68.3% in the bulevirtide group.
The two groups had similar mean ALT levels at 12 months (48.91 and 48.03 IU/mL, respectively), with more patients in the bulevirtide group having normal ALT levels (<40 IU/L; 48.8% versus 36.4%). At 12 months, 39.0% of the bulevirtide group and 30.3% of the combination group had a combined response, defined as either undetectable HDV RNA or ≥2 log10 from baseline plus normal ALT levels.
Twenty-nine patients in the bulevirtide group had an adverse event, compared with 43 in the combination group. The two groups were similar in the frequency of grade 3-4 adverse events (7 versus 6), discontinuation due to adverse events (2 versus 3), deaths (0 in both), injection-site reactions (2 in both), liver-related adverse events (4 versus 2), and elevated bile acid (76 versus 68).
During the Q&A period following the presentation, Dr. De Ledinghen was asked if he has a preferred regimen for HDV patients. “I think it depends on the tolerance of peg-interferon because of all the side effects with this drug. I think we need to have predictive factors of virological response with or without interferon. At this time, I don’t have a preference, but I think at this time we need to work on predictive factors associated with virologic response,” he said.
The EMA’s conditional bulevirtide approval hinged on results from phase 2 clinical trials, while the phase 3 clinical studies are ongoing. “This was a very unusual step for the EMA to provide what is similar to emergency use approval while the phase 3 clinical trials are still ongoing,” said Anna Lok, MD, who was asked to comment on the study. Dr. Lok is a professor of internal medicine, director of clinical hepatology, and assistant dean for clinical research at the University of Michigan, Ann Arbor.
She noted that the phase 2 studies indicated that the combination with peg-interferon seems to have an additive effect on HDV suppression, while monotherapy with bulevirtide has a greater effect on normalizing ALT levels. The real-world experience confirms these findings.
But the real-world data revealed some concerns. “What really worried me is the large number of patients who required dose modifications or discontinuations, and that seems to be the case in both treatment groups. They didn’t really go into a lot of details [about] why patients needed treatment modifications, but one has to assume that this is due to side effects,” said Dr. Lok.
She also noted that the per-protocol analysis, instead of an intention-to-treat analysis, is a weakness of the study. Additionally, over time, the number of patients analyzed decreased – as many as 40% of patients didn’t have test results at month 12. “It makes you wonder what happened to those patients. Many probably didn’t respond, in which case your overall response rate will be far lower,” said Dr. Lok.
The study was funded by Gilead. Dr. De Ledinghen has financial relationships with Gilead, AbbVie, Echosens, Hologic, Intercept Pharma, Tillotts, Orphalan, Alfasigma, Bristol Myers Squibb, and Siemens Healthineers. Dr. Lok has no relevant financial disclosures.
FROM THE LIVER MEETING