User login
Zanubrutinib receives breakthrough designation for MCL
The (MCL) who have received at least one prior therapy.
Zanubrutinib (BGB-3111) is a Bruton’s tyrosine kinase inhibitor being developed by BeiGene as a potential treatment for B-cell malignancies.
Researchers have evaluated zanubrutinib in a phase 2 trial (NCT03206970) of patients with relapsed/refractory MCL. Results from this trial were presented at the 2018 annual meeting of the American Society of Hematology (Abstract 148).
As of March 27, 2018, 86 patients had been enrolled in the trial and received treatment. They had a median of two prior lines of therapy and they received zanubrutinib at 160 mg twice daily.
Eighty-five patients were evaluable for efficacy. The overall response rate was 83.5% (71/85), and the complete response rate was 58.8% (50/85). At a median follow-up of 24.1 weeks, the median duration of response and median progression-free survival had not been reached. The estimated 24-week progression-free survival rate was 82%. The most common adverse events (AEs) in this trial were decrease in neutrophil count (31.4%), rash (29.1%), upper respiratory tract infection (29.1%), and decrease in platelet count (22.1%). Common grade 3 or higher AEs included neutrophil count decrease (11.6%) and lung infection (5.8%).
Four patients had fatal treatment-emergent AEs. One death was caused by a traffic accident, one was due to cerebral hemorrhage, and one resulted from pneumonia. The fourth death occurred in a patient with infection, but the cause of death was unknown.
Breakthrough therapy designation is designed to expedite the development and review of a therapy for a serious or life-threatening disease, following preliminary clinical evidence indicating it demonstrates substantial improvement over existing therapies.
The (MCL) who have received at least one prior therapy.
Zanubrutinib (BGB-3111) is a Bruton’s tyrosine kinase inhibitor being developed by BeiGene as a potential treatment for B-cell malignancies.
Researchers have evaluated zanubrutinib in a phase 2 trial (NCT03206970) of patients with relapsed/refractory MCL. Results from this trial were presented at the 2018 annual meeting of the American Society of Hematology (Abstract 148).
As of March 27, 2018, 86 patients had been enrolled in the trial and received treatment. They had a median of two prior lines of therapy and they received zanubrutinib at 160 mg twice daily.
Eighty-five patients were evaluable for efficacy. The overall response rate was 83.5% (71/85), and the complete response rate was 58.8% (50/85). At a median follow-up of 24.1 weeks, the median duration of response and median progression-free survival had not been reached. The estimated 24-week progression-free survival rate was 82%. The most common adverse events (AEs) in this trial were decrease in neutrophil count (31.4%), rash (29.1%), upper respiratory tract infection (29.1%), and decrease in platelet count (22.1%). Common grade 3 or higher AEs included neutrophil count decrease (11.6%) and lung infection (5.8%).
Four patients had fatal treatment-emergent AEs. One death was caused by a traffic accident, one was due to cerebral hemorrhage, and one resulted from pneumonia. The fourth death occurred in a patient with infection, but the cause of death was unknown.
Breakthrough therapy designation is designed to expedite the development and review of a therapy for a serious or life-threatening disease, following preliminary clinical evidence indicating it demonstrates substantial improvement over existing therapies.
The (MCL) who have received at least one prior therapy.
Zanubrutinib (BGB-3111) is a Bruton’s tyrosine kinase inhibitor being developed by BeiGene as a potential treatment for B-cell malignancies.
Researchers have evaluated zanubrutinib in a phase 2 trial (NCT03206970) of patients with relapsed/refractory MCL. Results from this trial were presented at the 2018 annual meeting of the American Society of Hematology (Abstract 148).
As of March 27, 2018, 86 patients had been enrolled in the trial and received treatment. They had a median of two prior lines of therapy and they received zanubrutinib at 160 mg twice daily.
Eighty-five patients were evaluable for efficacy. The overall response rate was 83.5% (71/85), and the complete response rate was 58.8% (50/85). At a median follow-up of 24.1 weeks, the median duration of response and median progression-free survival had not been reached. The estimated 24-week progression-free survival rate was 82%. The most common adverse events (AEs) in this trial were decrease in neutrophil count (31.4%), rash (29.1%), upper respiratory tract infection (29.1%), and decrease in platelet count (22.1%). Common grade 3 or higher AEs included neutrophil count decrease (11.6%) and lung infection (5.8%).
Four patients had fatal treatment-emergent AEs. One death was caused by a traffic accident, one was due to cerebral hemorrhage, and one resulted from pneumonia. The fourth death occurred in a patient with infection, but the cause of death was unknown.
Breakthrough therapy designation is designed to expedite the development and review of a therapy for a serious or life-threatening disease, following preliminary clinical evidence indicating it demonstrates substantial improvement over existing therapies.
Adding umbralisib to ibrutinib produced responses in MCL, CLL
Dual B-cell receptor pathway blockade was tolerable and efficacious for patients with relapsed or refractory chronic lymphocytic leukemia (CLL) or mantle cell lymphoma (MCL) who participated in a multicenter phase 1-1b clinical study that added umbralisib to ibrutinib.
The study “is the first successful combination for two drugs targeting the B-cell receptor pathway,” Matthew S. Davids, MD, of the Dana-Farber Cancer Institute in Boston and his colleagues wrote in the Lancet Haematology.
Of the 21 patients with CLL, 90% (n = 19) achieved an overall response (OR), 62% (n = 13) achieved partial response (PR) or PR with lymphocytosis, and 29% (n = 6) achieved complete response (CR). All patients in complete response still had minimal residual disease (MRD) in bone marrow. No CLL patients had progressive disease.
Of the 21 patients with MCL, 67% (n = 14) had an OR, with 19% (n = 4) showing CR and 48% (n = 10) achieving partial response. Three MCL patients (14%) had progressive disease.
Umbralisib is a next-generation phosphoinositide-3-kinase-delta inhibitor that, when added to the Bruton tyrosine kinase inhibitor (BTKi) ibrutinib, offers once-daily oral dosing. The combination affords the possibility of overcoming the resistance that can come with prolonged ibrutinib monotherapy.
A total of 44 patients were enrolled, and 42 patients (21 with CLL and 21 with MCL) received at least one dose of the study drug and were included in the analysis. At enrollment, patients had received a median of two previous therapies.
Diarrhea was the most frequent adverse event, seen in 22 patients (52%), and half of all patients (n = 21) had infections.
Hematologic toxicities included neutropenia, seen in 9 (43%) of the CLL patients and 8 (38%) of the MCL patients; thrombocytopenia, seen in 6 (29%) of the CLL patients and 10 (48%) of the MCL patients; and anemia, seen in 4 (19%) of the CLL and 9 (43%) of the MCL patients. Grade 3 and 4 hematologic toxicities of any type were less common, occurring in less than 20% of patients. One MCL patient developed febrile neutropenia. According to the study investigators, none of the hematologic toxicities were deemed related to the study drugs.
Adverse events did not appear to be dose-dependent for umbralisib, with the maximum tolerated dose not reached in the study, the investigators wrote. For phase 2 trials, the recommended dose of umbralisib is 800 mg given orally once daily in combination with ibrutinib.
“One unanticipated benefit of doublet B-cell receptor pathway inhibition in this study was the ability to continue one drug when a characteristic toxicity required the other drug to be held,” the investigators wrote.
For MCL patients, 67% achieved OR and 19% achieved CR, figures similar to those reported for ibrutinib monotherapy. However, “the 2-year progression-free survival of 49% and overall survival of 58% suggest that patients who made it to 1 year progression-free had few events during the second year on therapy,” the investigators wrote. They also noted that this MCL population was high risk; more than one-quarter of patients had relapsed after prior autologous stem cell transplantation.
The study was limited by small sample size and a short duration of follow-up, so durability of response can’t yet be assessed. Also, neither pharmacokinetics nor resistance mutations were tracked for participants.
Currently, the doublet regimen is designed to be continuous therapy, and although it’s not known whether this regimen would be effective as time-limited therapy, it’s unlikely because 100% of patients who had CR still had detectable minimal residual disease, the investigators noted.
Umbralisib and ibrutinib are also being explored as part of triplet therapy, with the type 2 CD20 antibody ublituximab, for relapsed or refractory B-cell malignancies (NCT02006485).
“These novel drug-based approaches, along with several others in development, hold promise as highly effective and well-tolerated regimens with the potential to substantially improve outcomes for patients with B-cell malignancies,” the investigators wrote.
The study was supported by TG Therapeutics and the Leukemia and Lymphoma Society Therapy Accelerator Program. The authors reported financial relationships with several pharmaceutical companies, including TG Therapeutics.
SOURCE: Davids MS et al. Lancet Haemtol. 2019;6:e38-47.
Dual B-cell receptor pathway blockade was tolerable and efficacious for patients with relapsed or refractory chronic lymphocytic leukemia (CLL) or mantle cell lymphoma (MCL) who participated in a multicenter phase 1-1b clinical study that added umbralisib to ibrutinib.
The study “is the first successful combination for two drugs targeting the B-cell receptor pathway,” Matthew S. Davids, MD, of the Dana-Farber Cancer Institute in Boston and his colleagues wrote in the Lancet Haematology.
Of the 21 patients with CLL, 90% (n = 19) achieved an overall response (OR), 62% (n = 13) achieved partial response (PR) or PR with lymphocytosis, and 29% (n = 6) achieved complete response (CR). All patients in complete response still had minimal residual disease (MRD) in bone marrow. No CLL patients had progressive disease.
Of the 21 patients with MCL, 67% (n = 14) had an OR, with 19% (n = 4) showing CR and 48% (n = 10) achieving partial response. Three MCL patients (14%) had progressive disease.
Umbralisib is a next-generation phosphoinositide-3-kinase-delta inhibitor that, when added to the Bruton tyrosine kinase inhibitor (BTKi) ibrutinib, offers once-daily oral dosing. The combination affords the possibility of overcoming the resistance that can come with prolonged ibrutinib monotherapy.
A total of 44 patients were enrolled, and 42 patients (21 with CLL and 21 with MCL) received at least one dose of the study drug and were included in the analysis. At enrollment, patients had received a median of two previous therapies.
Diarrhea was the most frequent adverse event, seen in 22 patients (52%), and half of all patients (n = 21) had infections.
Hematologic toxicities included neutropenia, seen in 9 (43%) of the CLL patients and 8 (38%) of the MCL patients; thrombocytopenia, seen in 6 (29%) of the CLL patients and 10 (48%) of the MCL patients; and anemia, seen in 4 (19%) of the CLL and 9 (43%) of the MCL patients. Grade 3 and 4 hematologic toxicities of any type were less common, occurring in less than 20% of patients. One MCL patient developed febrile neutropenia. According to the study investigators, none of the hematologic toxicities were deemed related to the study drugs.
Adverse events did not appear to be dose-dependent for umbralisib, with the maximum tolerated dose not reached in the study, the investigators wrote. For phase 2 trials, the recommended dose of umbralisib is 800 mg given orally once daily in combination with ibrutinib.
“One unanticipated benefit of doublet B-cell receptor pathway inhibition in this study was the ability to continue one drug when a characteristic toxicity required the other drug to be held,” the investigators wrote.
For MCL patients, 67% achieved OR and 19% achieved CR, figures similar to those reported for ibrutinib monotherapy. However, “the 2-year progression-free survival of 49% and overall survival of 58% suggest that patients who made it to 1 year progression-free had few events during the second year on therapy,” the investigators wrote. They also noted that this MCL population was high risk; more than one-quarter of patients had relapsed after prior autologous stem cell transplantation.
The study was limited by small sample size and a short duration of follow-up, so durability of response can’t yet be assessed. Also, neither pharmacokinetics nor resistance mutations were tracked for participants.
Currently, the doublet regimen is designed to be continuous therapy, and although it’s not known whether this regimen would be effective as time-limited therapy, it’s unlikely because 100% of patients who had CR still had detectable minimal residual disease, the investigators noted.
Umbralisib and ibrutinib are also being explored as part of triplet therapy, with the type 2 CD20 antibody ublituximab, for relapsed or refractory B-cell malignancies (NCT02006485).
“These novel drug-based approaches, along with several others in development, hold promise as highly effective and well-tolerated regimens with the potential to substantially improve outcomes for patients with B-cell malignancies,” the investigators wrote.
The study was supported by TG Therapeutics and the Leukemia and Lymphoma Society Therapy Accelerator Program. The authors reported financial relationships with several pharmaceutical companies, including TG Therapeutics.
SOURCE: Davids MS et al. Lancet Haemtol. 2019;6:e38-47.
Dual B-cell receptor pathway blockade was tolerable and efficacious for patients with relapsed or refractory chronic lymphocytic leukemia (CLL) or mantle cell lymphoma (MCL) who participated in a multicenter phase 1-1b clinical study that added umbralisib to ibrutinib.
The study “is the first successful combination for two drugs targeting the B-cell receptor pathway,” Matthew S. Davids, MD, of the Dana-Farber Cancer Institute in Boston and his colleagues wrote in the Lancet Haematology.
Of the 21 patients with CLL, 90% (n = 19) achieved an overall response (OR), 62% (n = 13) achieved partial response (PR) or PR with lymphocytosis, and 29% (n = 6) achieved complete response (CR). All patients in complete response still had minimal residual disease (MRD) in bone marrow. No CLL patients had progressive disease.
Of the 21 patients with MCL, 67% (n = 14) had an OR, with 19% (n = 4) showing CR and 48% (n = 10) achieving partial response. Three MCL patients (14%) had progressive disease.
Umbralisib is a next-generation phosphoinositide-3-kinase-delta inhibitor that, when added to the Bruton tyrosine kinase inhibitor (BTKi) ibrutinib, offers once-daily oral dosing. The combination affords the possibility of overcoming the resistance that can come with prolonged ibrutinib monotherapy.
A total of 44 patients were enrolled, and 42 patients (21 with CLL and 21 with MCL) received at least one dose of the study drug and were included in the analysis. At enrollment, patients had received a median of two previous therapies.
Diarrhea was the most frequent adverse event, seen in 22 patients (52%), and half of all patients (n = 21) had infections.
Hematologic toxicities included neutropenia, seen in 9 (43%) of the CLL patients and 8 (38%) of the MCL patients; thrombocytopenia, seen in 6 (29%) of the CLL patients and 10 (48%) of the MCL patients; and anemia, seen in 4 (19%) of the CLL and 9 (43%) of the MCL patients. Grade 3 and 4 hematologic toxicities of any type were less common, occurring in less than 20% of patients. One MCL patient developed febrile neutropenia. According to the study investigators, none of the hematologic toxicities were deemed related to the study drugs.
Adverse events did not appear to be dose-dependent for umbralisib, with the maximum tolerated dose not reached in the study, the investigators wrote. For phase 2 trials, the recommended dose of umbralisib is 800 mg given orally once daily in combination with ibrutinib.
“One unanticipated benefit of doublet B-cell receptor pathway inhibition in this study was the ability to continue one drug when a characteristic toxicity required the other drug to be held,” the investigators wrote.
For MCL patients, 67% achieved OR and 19% achieved CR, figures similar to those reported for ibrutinib monotherapy. However, “the 2-year progression-free survival of 49% and overall survival of 58% suggest that patients who made it to 1 year progression-free had few events during the second year on therapy,” the investigators wrote. They also noted that this MCL population was high risk; more than one-quarter of patients had relapsed after prior autologous stem cell transplantation.
The study was limited by small sample size and a short duration of follow-up, so durability of response can’t yet be assessed. Also, neither pharmacokinetics nor resistance mutations were tracked for participants.
Currently, the doublet regimen is designed to be continuous therapy, and although it’s not known whether this regimen would be effective as time-limited therapy, it’s unlikely because 100% of patients who had CR still had detectable minimal residual disease, the investigators noted.
Umbralisib and ibrutinib are also being explored as part of triplet therapy, with the type 2 CD20 antibody ublituximab, for relapsed or refractory B-cell malignancies (NCT02006485).
“These novel drug-based approaches, along with several others in development, hold promise as highly effective and well-tolerated regimens with the potential to substantially improve outcomes for patients with B-cell malignancies,” the investigators wrote.
The study was supported by TG Therapeutics and the Leukemia and Lymphoma Society Therapy Accelerator Program. The authors reported financial relationships with several pharmaceutical companies, including TG Therapeutics.
SOURCE: Davids MS et al. Lancet Haemtol. 2019;6:e38-47.
FROM LANCET HAEMATOLOGY
Key clinical point:
Major finding: Of CLL patients, 90% achieved an overall response.
Study details: Phase 1-1b trial of umbralisib and ibrutinib in patients with relapsed or refractory MCL or CLL.
Disclosures: The study was supported by TG Therapeutics and the Leukemia and Lymphoma Therapy Accelerator Program. Dr. Davids and his coauthors reported financial relationships with several pharmaceutical companies, including TG Therapeutics.
Source: Davids MS et al. Lancet Haematol. 2019;6:e38-47.
Lenalidomide maintenance improves MCL survival after ASCT
SAN DIEGO – For patients 65 years or younger with mantle cell lymphoma (MCL) who have undergone autologous stem cell transplantation (ASCT), maintenance therapy with lenalidomide (Revlimid) can significantly improve progression-free survival (PFS), suggest results of the phase, 3 randomized MCL0208 trial.
After a median follow-up of 39 months, the 3-year PFS in an intention-to-treat analysis was 80% for patients treated with ASCT and lenalidomide maintenance, compared with 64% for patients treated with ASCT alone, reported Marco Ladetto, MD, of Azienda Ospedaliera Nazionale SS. Antonio e Biagio e Cesare Arrigo in Alessandria, Italy.
“Lenalidomide maintenance after autologous stem cell transplant has substantial clinical activity in mantle cell lymphoma in terms of progression-free survival,” he said at the annual meeting of the American Society of Hematology. “Follow-up is still too short for meaningful overall survival considerations.”
Dr. Ladetto and his colleagues at centers in Italy and Portugal enrolled patients aged 18-65 years with previously untreated MCL stage III or IV, or stage II with bulky disease (5 cm or greater), and good performance status.
The patients first underwent induction with three cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, and prednisone), which was followed by treatment with rituximab plus high-dose cyclophosphamide and two cycles of rituximab with high-dose cytarabine. Stem cells were collected after the first course of the latter regimen.
The patients then underwent conditioning with BEAM (carmustine, etoposide, cytarabine, melphalan) and ASCT.
Following ASCT, patients with complete or partial remissions were randomized either to maintenance therapy with lenalidomide 15 mg for 21 of 28 days for each cycle or to observation.
Of the 303 patients initially enrolled, 248 went on to ASCT, and 205 went on to randomization – 104 assigned to maintenance and 101 assigned to observation.
A total of 52 patients completed 2 years of maintenance: Of the rest, 2 patients died from toxicities (thrombotic thrombocytopenic purpura and pneumonia), 7 had disease progression, 41 dropped out for nonprogression reasons, and 2 patients were still in maintenance at the time of the data cutoff. In this arm, 6 of 8 patients with partial responses converted to complete responses by the end of maintenance. More than a quarter of patients (28%) received less than 25% of the planned lenalidomide dose.
In the observation arm, 1 patient died from pneumonia, 20 had disease progression, 3 were lost to follow-up, 6 were still under observation, and 71 completed observation. In this arm, 1 of 4 patients with a partial response converted to a complete response at the end of the observation period.
Despite suboptimal dosing in a large proportion of patients, the PFS primary endpoint showed significant benefit for lenalidomide, with an unstratified hazard ratio of 0.52 (P = .015) and a stratified HR of 0.51 (P = .013).
At a median follow-up of 39 months from randomization, 3-year overall survival (OS) rates were 93% with lenalidomide and 86% with observation, a difference that was not statistically significant.
Grade 3 or 4 hematologic toxicities occurred in 63% of patients in the lenalidomide arm, compared with 11% in the observation arm. The respective rates of granulocytopenia were 59% vs. 10%. Nonhematological grade 3 toxicity was comparable in the two arms except for grade 3 or 4 infections, which were more common with lenalidomide. Seven patients in the lenalidomide arm and three patients in the observation arm developed second cancers.
Dr. Ladetto noted that difficulties in delivering the planned dose of lenalidomide may have been caused by an already-stressed hematopoietic compartment; he commented that the question of the relative benefit of a fixed lenalidomide schedule or an until-progression approach still needs to be answered.
Additionally, the induction schedule used in the trial, while feasible, is not superior to “less cumbersome and possibly less toxic regimens,” he said.
The study was supported by the Italian Lymphoma Foundation (Fondazione Italiana Linfomi) with the European Mantle Cell Lymphoma Network. Dr. Ladetto reported honoraria from Roche, Celgene, Acerta, Janssen, AbbVie, and Sandoz, as well as off-label use of lenalidomide.
SOURCE: Ladetto M et al. ASH 2018, Abstract 401.
SAN DIEGO – For patients 65 years or younger with mantle cell lymphoma (MCL) who have undergone autologous stem cell transplantation (ASCT), maintenance therapy with lenalidomide (Revlimid) can significantly improve progression-free survival (PFS), suggest results of the phase, 3 randomized MCL0208 trial.
After a median follow-up of 39 months, the 3-year PFS in an intention-to-treat analysis was 80% for patients treated with ASCT and lenalidomide maintenance, compared with 64% for patients treated with ASCT alone, reported Marco Ladetto, MD, of Azienda Ospedaliera Nazionale SS. Antonio e Biagio e Cesare Arrigo in Alessandria, Italy.
“Lenalidomide maintenance after autologous stem cell transplant has substantial clinical activity in mantle cell lymphoma in terms of progression-free survival,” he said at the annual meeting of the American Society of Hematology. “Follow-up is still too short for meaningful overall survival considerations.”
Dr. Ladetto and his colleagues at centers in Italy and Portugal enrolled patients aged 18-65 years with previously untreated MCL stage III or IV, or stage II with bulky disease (5 cm or greater), and good performance status.
The patients first underwent induction with three cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, and prednisone), which was followed by treatment with rituximab plus high-dose cyclophosphamide and two cycles of rituximab with high-dose cytarabine. Stem cells were collected after the first course of the latter regimen.
The patients then underwent conditioning with BEAM (carmustine, etoposide, cytarabine, melphalan) and ASCT.
Following ASCT, patients with complete or partial remissions were randomized either to maintenance therapy with lenalidomide 15 mg for 21 of 28 days for each cycle or to observation.
Of the 303 patients initially enrolled, 248 went on to ASCT, and 205 went on to randomization – 104 assigned to maintenance and 101 assigned to observation.
A total of 52 patients completed 2 years of maintenance: Of the rest, 2 patients died from toxicities (thrombotic thrombocytopenic purpura and pneumonia), 7 had disease progression, 41 dropped out for nonprogression reasons, and 2 patients were still in maintenance at the time of the data cutoff. In this arm, 6 of 8 patients with partial responses converted to complete responses by the end of maintenance. More than a quarter of patients (28%) received less than 25% of the planned lenalidomide dose.
In the observation arm, 1 patient died from pneumonia, 20 had disease progression, 3 were lost to follow-up, 6 were still under observation, and 71 completed observation. In this arm, 1 of 4 patients with a partial response converted to a complete response at the end of the observation period.
Despite suboptimal dosing in a large proportion of patients, the PFS primary endpoint showed significant benefit for lenalidomide, with an unstratified hazard ratio of 0.52 (P = .015) and a stratified HR of 0.51 (P = .013).
At a median follow-up of 39 months from randomization, 3-year overall survival (OS) rates were 93% with lenalidomide and 86% with observation, a difference that was not statistically significant.
Grade 3 or 4 hematologic toxicities occurred in 63% of patients in the lenalidomide arm, compared with 11% in the observation arm. The respective rates of granulocytopenia were 59% vs. 10%. Nonhematological grade 3 toxicity was comparable in the two arms except for grade 3 or 4 infections, which were more common with lenalidomide. Seven patients in the lenalidomide arm and three patients in the observation arm developed second cancers.
Dr. Ladetto noted that difficulties in delivering the planned dose of lenalidomide may have been caused by an already-stressed hematopoietic compartment; he commented that the question of the relative benefit of a fixed lenalidomide schedule or an until-progression approach still needs to be answered.
Additionally, the induction schedule used in the trial, while feasible, is not superior to “less cumbersome and possibly less toxic regimens,” he said.
The study was supported by the Italian Lymphoma Foundation (Fondazione Italiana Linfomi) with the European Mantle Cell Lymphoma Network. Dr. Ladetto reported honoraria from Roche, Celgene, Acerta, Janssen, AbbVie, and Sandoz, as well as off-label use of lenalidomide.
SOURCE: Ladetto M et al. ASH 2018, Abstract 401.
SAN DIEGO – For patients 65 years or younger with mantle cell lymphoma (MCL) who have undergone autologous stem cell transplantation (ASCT), maintenance therapy with lenalidomide (Revlimid) can significantly improve progression-free survival (PFS), suggest results of the phase, 3 randomized MCL0208 trial.
After a median follow-up of 39 months, the 3-year PFS in an intention-to-treat analysis was 80% for patients treated with ASCT and lenalidomide maintenance, compared with 64% for patients treated with ASCT alone, reported Marco Ladetto, MD, of Azienda Ospedaliera Nazionale SS. Antonio e Biagio e Cesare Arrigo in Alessandria, Italy.
“Lenalidomide maintenance after autologous stem cell transplant has substantial clinical activity in mantle cell lymphoma in terms of progression-free survival,” he said at the annual meeting of the American Society of Hematology. “Follow-up is still too short for meaningful overall survival considerations.”
Dr. Ladetto and his colleagues at centers in Italy and Portugal enrolled patients aged 18-65 years with previously untreated MCL stage III or IV, or stage II with bulky disease (5 cm or greater), and good performance status.
The patients first underwent induction with three cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, and prednisone), which was followed by treatment with rituximab plus high-dose cyclophosphamide and two cycles of rituximab with high-dose cytarabine. Stem cells were collected after the first course of the latter regimen.
The patients then underwent conditioning with BEAM (carmustine, etoposide, cytarabine, melphalan) and ASCT.
Following ASCT, patients with complete or partial remissions were randomized either to maintenance therapy with lenalidomide 15 mg for 21 of 28 days for each cycle or to observation.
Of the 303 patients initially enrolled, 248 went on to ASCT, and 205 went on to randomization – 104 assigned to maintenance and 101 assigned to observation.
A total of 52 patients completed 2 years of maintenance: Of the rest, 2 patients died from toxicities (thrombotic thrombocytopenic purpura and pneumonia), 7 had disease progression, 41 dropped out for nonprogression reasons, and 2 patients were still in maintenance at the time of the data cutoff. In this arm, 6 of 8 patients with partial responses converted to complete responses by the end of maintenance. More than a quarter of patients (28%) received less than 25% of the planned lenalidomide dose.
In the observation arm, 1 patient died from pneumonia, 20 had disease progression, 3 were lost to follow-up, 6 were still under observation, and 71 completed observation. In this arm, 1 of 4 patients with a partial response converted to a complete response at the end of the observation period.
Despite suboptimal dosing in a large proportion of patients, the PFS primary endpoint showed significant benefit for lenalidomide, with an unstratified hazard ratio of 0.52 (P = .015) and a stratified HR of 0.51 (P = .013).
At a median follow-up of 39 months from randomization, 3-year overall survival (OS) rates were 93% with lenalidomide and 86% with observation, a difference that was not statistically significant.
Grade 3 or 4 hematologic toxicities occurred in 63% of patients in the lenalidomide arm, compared with 11% in the observation arm. The respective rates of granulocytopenia were 59% vs. 10%. Nonhematological grade 3 toxicity was comparable in the two arms except for grade 3 or 4 infections, which were more common with lenalidomide. Seven patients in the lenalidomide arm and three patients in the observation arm developed second cancers.
Dr. Ladetto noted that difficulties in delivering the planned dose of lenalidomide may have been caused by an already-stressed hematopoietic compartment; he commented that the question of the relative benefit of a fixed lenalidomide schedule or an until-progression approach still needs to be answered.
Additionally, the induction schedule used in the trial, while feasible, is not superior to “less cumbersome and possibly less toxic regimens,” he said.
The study was supported by the Italian Lymphoma Foundation (Fondazione Italiana Linfomi) with the European Mantle Cell Lymphoma Network. Dr. Ladetto reported honoraria from Roche, Celgene, Acerta, Janssen, AbbVie, and Sandoz, as well as off-label use of lenalidomide.
SOURCE: Ladetto M et al. ASH 2018, Abstract 401.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: The 3-year PFS rate was 80% for patients on lenalidomide maintenance, compared with 64% for patients on observation alone.
Study details: An open-label, randomized, phase 3 trial with 205 patients randomized to lenalidomide or observation.
Disclosures: The study was supported by the Italian Lymphoma Foundation (Fondazione Italiana Linfomi) with the European Mantle Cell Lymphoma Network. Dr. Ladetto reported honoraria from Roche, Celgene, Acerta, Janssen, AbbVie, and Sandoz, as well as off-label use of lenalidomide.
Source: Ladetto M et al. ASH 2018, Abstract 401.
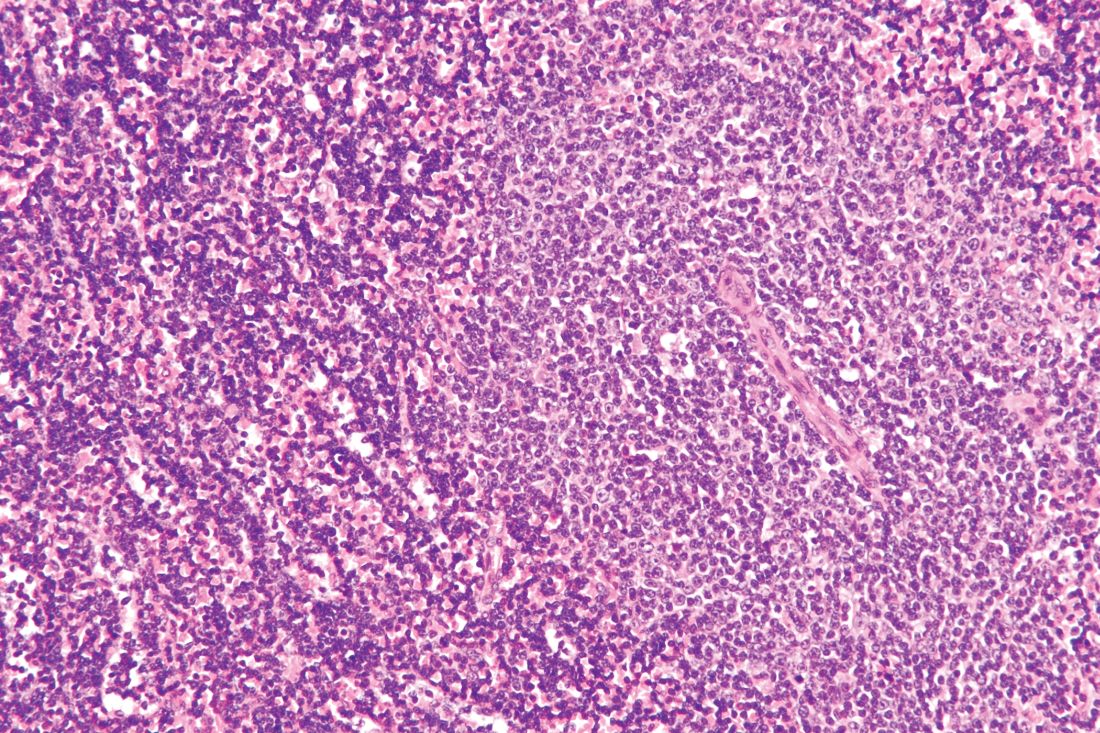
Cortactin expression aids in CLL-MCL differential
The presence or absence in tumor cells of cortactin, a cytoskeleton-remodeling adapter protein, may be a marker to help pathologists distinguish between chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL), investigators suggest.
A study of cortactin expression in tumor samples from patients with B-cell CLL, MCL, and other hematologic malignancies showed that while cortactin was present in 14 of 17 CLL samples, it was not expressed on any of 16 MCL samples, reported Marco Pizzi, MD, PhD, from the University of Padova (Italy) and his colleagues.
“In particular, cortactin may contribute to the differential diagnosis between CLL and MCL, two neoplasms with similar histological features but very different clinical outcome. Further studies are needed to clarify the molecular mechanisms of deranged cortactin expression in MCL and CLL and to investigate any possible relationship between cortactin status and the biological features of these lymphomas,” they wrote in Human Pathology.
Overexpression of cortactin has been reported in several solid tumors, and increased expression of CTTN, the gene encoding for cortactin, has been associated with aggressive, poor prognosis disease, the investigators noted.
To characterize cortactin expression in lymphoid and hematopoietic cells and detect potential associations between cortactin and virulence of hematologic malignancies, the investigators performed immunohistochemical analysis on samples from 131 patients treated at their center. The samples included 17 cases of CLL, 16 of MCL, 25 of follicular lymphoma (FL), 30 of marginal zone lymphoma (MZL), 10 of hairy cell leukemia, three of splenic diffuse red pulp small B-cell lymphomas (SDRPBL), and 30 of diffuse large B-cell lymphoma (DLBCL).
They found that cortactin was expressed in 14 of the 17 CLL samples, all 10 of the HCL samples, and 22 of the 30 DLBCL samples. In contrast, there was no cortactin expression detected in any of either 16 MCL or three SDRPBL samples. The researchers found that 13 of 30 MZL samples had low-level staining. In FL, cortactin was expressed in 2 of the samples but in the remaining 23 cases the researchers found only scattered cortactin-positive lymphoid elements of non–B-cell lineage.
The investigators also found that cortactin expression in CLL correlated with other CLL-specific markers, and found that expression of two or more of the markers had 89.1% sensitivity, 100% specificity, a 100% positive predictive value, and 90.5% negative predictive value for a diagnosis of CLL.
In addition, they saw that the immunohistochemical results were similar to those for CTTN gene expression assessed by in silico analysis.
The investigators noted that CLL and MCL are challenging to differentiate from one another because of morphologic similarities and partially overlapping immunophenotypes.
“In this context, cortactin expression would strongly sustain a diagnosis of CLL over MCL, particularly in association with other CLL markers (i.e., LEF1 and CD200),” they wrote.
The study was internally supported. The authors declared no conflicts of interest.
SOURCE: Pizzi M et al. Hum Pathol. 2018 Nov 17. doi: 10.1016/j.humpath.2018.10.038.
The presence or absence in tumor cells of cortactin, a cytoskeleton-remodeling adapter protein, may be a marker to help pathologists distinguish between chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL), investigators suggest.
A study of cortactin expression in tumor samples from patients with B-cell CLL, MCL, and other hematologic malignancies showed that while cortactin was present in 14 of 17 CLL samples, it was not expressed on any of 16 MCL samples, reported Marco Pizzi, MD, PhD, from the University of Padova (Italy) and his colleagues.
“In particular, cortactin may contribute to the differential diagnosis between CLL and MCL, two neoplasms with similar histological features but very different clinical outcome. Further studies are needed to clarify the molecular mechanisms of deranged cortactin expression in MCL and CLL and to investigate any possible relationship between cortactin status and the biological features of these lymphomas,” they wrote in Human Pathology.
Overexpression of cortactin has been reported in several solid tumors, and increased expression of CTTN, the gene encoding for cortactin, has been associated with aggressive, poor prognosis disease, the investigators noted.
To characterize cortactin expression in lymphoid and hematopoietic cells and detect potential associations between cortactin and virulence of hematologic malignancies, the investigators performed immunohistochemical analysis on samples from 131 patients treated at their center. The samples included 17 cases of CLL, 16 of MCL, 25 of follicular lymphoma (FL), 30 of marginal zone lymphoma (MZL), 10 of hairy cell leukemia, three of splenic diffuse red pulp small B-cell lymphomas (SDRPBL), and 30 of diffuse large B-cell lymphoma (DLBCL).
They found that cortactin was expressed in 14 of the 17 CLL samples, all 10 of the HCL samples, and 22 of the 30 DLBCL samples. In contrast, there was no cortactin expression detected in any of either 16 MCL or three SDRPBL samples. The researchers found that 13 of 30 MZL samples had low-level staining. In FL, cortactin was expressed in 2 of the samples but in the remaining 23 cases the researchers found only scattered cortactin-positive lymphoid elements of non–B-cell lineage.
The investigators also found that cortactin expression in CLL correlated with other CLL-specific markers, and found that expression of two or more of the markers had 89.1% sensitivity, 100% specificity, a 100% positive predictive value, and 90.5% negative predictive value for a diagnosis of CLL.
In addition, they saw that the immunohistochemical results were similar to those for CTTN gene expression assessed by in silico analysis.
The investigators noted that CLL and MCL are challenging to differentiate from one another because of morphologic similarities and partially overlapping immunophenotypes.
“In this context, cortactin expression would strongly sustain a diagnosis of CLL over MCL, particularly in association with other CLL markers (i.e., LEF1 and CD200),” they wrote.
The study was internally supported. The authors declared no conflicts of interest.
SOURCE: Pizzi M et al. Hum Pathol. 2018 Nov 17. doi: 10.1016/j.humpath.2018.10.038.
The presence or absence in tumor cells of cortactin, a cytoskeleton-remodeling adapter protein, may be a marker to help pathologists distinguish between chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL), investigators suggest.
A study of cortactin expression in tumor samples from patients with B-cell CLL, MCL, and other hematologic malignancies showed that while cortactin was present in 14 of 17 CLL samples, it was not expressed on any of 16 MCL samples, reported Marco Pizzi, MD, PhD, from the University of Padova (Italy) and his colleagues.
“In particular, cortactin may contribute to the differential diagnosis between CLL and MCL, two neoplasms with similar histological features but very different clinical outcome. Further studies are needed to clarify the molecular mechanisms of deranged cortactin expression in MCL and CLL and to investigate any possible relationship between cortactin status and the biological features of these lymphomas,” they wrote in Human Pathology.
Overexpression of cortactin has been reported in several solid tumors, and increased expression of CTTN, the gene encoding for cortactin, has been associated with aggressive, poor prognosis disease, the investigators noted.
To characterize cortactin expression in lymphoid and hematopoietic cells and detect potential associations between cortactin and virulence of hematologic malignancies, the investigators performed immunohistochemical analysis on samples from 131 patients treated at their center. The samples included 17 cases of CLL, 16 of MCL, 25 of follicular lymphoma (FL), 30 of marginal zone lymphoma (MZL), 10 of hairy cell leukemia, three of splenic diffuse red pulp small B-cell lymphomas (SDRPBL), and 30 of diffuse large B-cell lymphoma (DLBCL).
They found that cortactin was expressed in 14 of the 17 CLL samples, all 10 of the HCL samples, and 22 of the 30 DLBCL samples. In contrast, there was no cortactin expression detected in any of either 16 MCL or three SDRPBL samples. The researchers found that 13 of 30 MZL samples had low-level staining. In FL, cortactin was expressed in 2 of the samples but in the remaining 23 cases the researchers found only scattered cortactin-positive lymphoid elements of non–B-cell lineage.
The investigators also found that cortactin expression in CLL correlated with other CLL-specific markers, and found that expression of two or more of the markers had 89.1% sensitivity, 100% specificity, a 100% positive predictive value, and 90.5% negative predictive value for a diagnosis of CLL.
In addition, they saw that the immunohistochemical results were similar to those for CTTN gene expression assessed by in silico analysis.
The investigators noted that CLL and MCL are challenging to differentiate from one another because of morphologic similarities and partially overlapping immunophenotypes.
“In this context, cortactin expression would strongly sustain a diagnosis of CLL over MCL, particularly in association with other CLL markers (i.e., LEF1 and CD200),” they wrote.
The study was internally supported. The authors declared no conflicts of interest.
SOURCE: Pizzi M et al. Hum Pathol. 2018 Nov 17. doi: 10.1016/j.humpath.2018.10.038.
FROM HUMAN PATHOLOGY
Key clinical point:
Major finding: Cortactin was expressed on 14 of 17 CLL samples vs. none of 16 MCL samples.
Study details: Immunohistochemistry analysis of samples from 131 patients with B-cell lineage non-Hodgkin lymphomas.
Disclosures: The study was internally supported. The authors reported having no conflicts of interest.
Source: Pizzi M et al. Hum Pathol. 2018 Nov 17. doi: 10.1016/j.humpath.2018.10.038.
Relapsed MCL: Options for treatment
CHICAGO – according to Kristie A. Blum, MD.
Venetoclax and lenalidomide can also be considered in the relapsed mantle cell lymphoma (MCL) setting, Dr. Blum, a professor in the department of hematology and medical oncology at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
“I tend to favor BTK inhibitors as my first line of therapy,” she said, later qualifying that this applies when clinical trial enrollment is unavailable.
Ibrutinib
The BTK inhibitor ibrutinib is well established as a treatment for MCL and for use in the relapsed setting, she said, noting that pooled data from the phase 2 CYC-1104 trial, the phase 2 MCL 2001 (SPARK) trial, and the phase 3 MCL3001 (RAY) trial showed an overall response (OR) rate of 66% in 370 patients and a complete response (CR) rate of 20%.
The median duration of response (DOR) was 18.6 months, median progression-free survival (PFS) was 12.8 months, and median overall survival (OS) was 25 months (Br J Haematol. 2017 Nov;179[3]:430-8).
Adding rituximab to ibrutinib (R-ibrutinib) improved outcomes, at least in one single center phase 2 trial of 50 relapsed patients with a median of three prior therapies, she said. The OR rate in that study was 88%, and the CR rate was 58% (Br J Haematol. 2018 May;182[3]:404-11).
“What was really impressive to me was that the median duration of response was about 46 months. PFS was 43 months, and patients were on [treatment] as long as 56 cycles,” she said.
Acalabrutinib
The newer BTK inhibitor acalabrutinib also shows benefit in the relapsed MCL setting, Dr. Blum said.
In a recent multicenter, open-label, phase 2 study of 124 patients with a median age of 68 years and a median of two prior therapies, acalabrutinib at a dose of 100 mg twice daily was associated with an OR rate of 81% and a CR rate of 40% (Lancet. 2018 Feb 17;391:659-67).
“Seems a little better than what you’d expect with single agent ibrutinib,” she said, noting that median DOR and PFS have not been reached in that study.
The main toxicities have been “headache and some diarrhea,” but follow-up is currently only about 15 months, she added.
Venetoclax
Another option in this setting is the B-cell lymphoma 2 (BCL-2) inhibitor venetoclax, which was shown in a recent phase 1 study of patients with various lymphoma subtypes to have activity in relapsed MCL, Dr. Blum said.
The OR rate in 28 relapsed MCL patients in that study was 75%, and the median PFS was 14 months (J Clin Oncol. 2017 Mar;35:826-33).
Additionally, an “intriguing combination study of venetoclax and ibrutinib” was recently published in the New England Journal of Medicine, she noted.
That study included only 23 patients with relapsed MCL, but they were a “pretty high-risk” group with a median age of 68 years, about half having a TP53 abnormality, and 30% having a prior transplant.
The OR and CR rates at 16 weeks by positron emission tomography were 71% and 62%, respectively (N Engl J Med. 2018 Mar 29;378:1211-23).
“Actually, about 40% achieved [minimal residual disease] negativity, but this was only checked in about half the patients,” she said. “So this is an intriguing combination and hopefully something we’ll see more of in the upcoming years.”
Lenalidomide
In the randomized phase 2 SPRINT study, patients received either single-agent lenolidamine or the investigator’s choice of single-agent rituximab, gemcitabine, fludarabine, chlorambucil, or cytarabine.
The expected OR rate in 170 patients treated with lenalidomide was 40% versus 11% in 84 patients treated with investigator’s choice of treatment, and the respective CR rates were 5% and 0% (Lancet Oncol. 2016 Mar 1;17(3):319-31).
Median DOR was 16 months versus 10.4 months, PFS was 8.7 versus 5.2 months, and median OS was 27.9 versus 21.1 months in the groups, respectively.
Other options
Combination regimens, such as R-CHOP and R-bendamustine, are also options for the treatment of relapsed MCL patients who haven’t received combination therapy in the past, Dr. Blum said. Transplant is another option in some patients.
“I will consider transplants for younger patients if they come to me and they actually hadn’t had one in [their] first CR,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – according to Kristie A. Blum, MD.
Venetoclax and lenalidomide can also be considered in the relapsed mantle cell lymphoma (MCL) setting, Dr. Blum, a professor in the department of hematology and medical oncology at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
“I tend to favor BTK inhibitors as my first line of therapy,” she said, later qualifying that this applies when clinical trial enrollment is unavailable.
Ibrutinib
The BTK inhibitor ibrutinib is well established as a treatment for MCL and for use in the relapsed setting, she said, noting that pooled data from the phase 2 CYC-1104 trial, the phase 2 MCL 2001 (SPARK) trial, and the phase 3 MCL3001 (RAY) trial showed an overall response (OR) rate of 66% in 370 patients and a complete response (CR) rate of 20%.
The median duration of response (DOR) was 18.6 months, median progression-free survival (PFS) was 12.8 months, and median overall survival (OS) was 25 months (Br J Haematol. 2017 Nov;179[3]:430-8).
Adding rituximab to ibrutinib (R-ibrutinib) improved outcomes, at least in one single center phase 2 trial of 50 relapsed patients with a median of three prior therapies, she said. The OR rate in that study was 88%, and the CR rate was 58% (Br J Haematol. 2018 May;182[3]:404-11).
“What was really impressive to me was that the median duration of response was about 46 months. PFS was 43 months, and patients were on [treatment] as long as 56 cycles,” she said.
Acalabrutinib
The newer BTK inhibitor acalabrutinib also shows benefit in the relapsed MCL setting, Dr. Blum said.
In a recent multicenter, open-label, phase 2 study of 124 patients with a median age of 68 years and a median of two prior therapies, acalabrutinib at a dose of 100 mg twice daily was associated with an OR rate of 81% and a CR rate of 40% (Lancet. 2018 Feb 17;391:659-67).
“Seems a little better than what you’d expect with single agent ibrutinib,” she said, noting that median DOR and PFS have not been reached in that study.
The main toxicities have been “headache and some diarrhea,” but follow-up is currently only about 15 months, she added.
Venetoclax
Another option in this setting is the B-cell lymphoma 2 (BCL-2) inhibitor venetoclax, which was shown in a recent phase 1 study of patients with various lymphoma subtypes to have activity in relapsed MCL, Dr. Blum said.
The OR rate in 28 relapsed MCL patients in that study was 75%, and the median PFS was 14 months (J Clin Oncol. 2017 Mar;35:826-33).
Additionally, an “intriguing combination study of venetoclax and ibrutinib” was recently published in the New England Journal of Medicine, she noted.
That study included only 23 patients with relapsed MCL, but they were a “pretty high-risk” group with a median age of 68 years, about half having a TP53 abnormality, and 30% having a prior transplant.
The OR and CR rates at 16 weeks by positron emission tomography were 71% and 62%, respectively (N Engl J Med. 2018 Mar 29;378:1211-23).
“Actually, about 40% achieved [minimal residual disease] negativity, but this was only checked in about half the patients,” she said. “So this is an intriguing combination and hopefully something we’ll see more of in the upcoming years.”
Lenalidomide
In the randomized phase 2 SPRINT study, patients received either single-agent lenolidamine or the investigator’s choice of single-agent rituximab, gemcitabine, fludarabine, chlorambucil, or cytarabine.
The expected OR rate in 170 patients treated with lenalidomide was 40% versus 11% in 84 patients treated with investigator’s choice of treatment, and the respective CR rates were 5% and 0% (Lancet Oncol. 2016 Mar 1;17(3):319-31).
Median DOR was 16 months versus 10.4 months, PFS was 8.7 versus 5.2 months, and median OS was 27.9 versus 21.1 months in the groups, respectively.
Other options
Combination regimens, such as R-CHOP and R-bendamustine, are also options for the treatment of relapsed MCL patients who haven’t received combination therapy in the past, Dr. Blum said. Transplant is another option in some patients.
“I will consider transplants for younger patients if they come to me and they actually hadn’t had one in [their] first CR,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – according to Kristie A. Blum, MD.
Venetoclax and lenalidomide can also be considered in the relapsed mantle cell lymphoma (MCL) setting, Dr. Blum, a professor in the department of hematology and medical oncology at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
“I tend to favor BTK inhibitors as my first line of therapy,” she said, later qualifying that this applies when clinical trial enrollment is unavailable.
Ibrutinib
The BTK inhibitor ibrutinib is well established as a treatment for MCL and for use in the relapsed setting, she said, noting that pooled data from the phase 2 CYC-1104 trial, the phase 2 MCL 2001 (SPARK) trial, and the phase 3 MCL3001 (RAY) trial showed an overall response (OR) rate of 66% in 370 patients and a complete response (CR) rate of 20%.
The median duration of response (DOR) was 18.6 months, median progression-free survival (PFS) was 12.8 months, and median overall survival (OS) was 25 months (Br J Haematol. 2017 Nov;179[3]:430-8).
Adding rituximab to ibrutinib (R-ibrutinib) improved outcomes, at least in one single center phase 2 trial of 50 relapsed patients with a median of three prior therapies, she said. The OR rate in that study was 88%, and the CR rate was 58% (Br J Haematol. 2018 May;182[3]:404-11).
“What was really impressive to me was that the median duration of response was about 46 months. PFS was 43 months, and patients were on [treatment] as long as 56 cycles,” she said.
Acalabrutinib
The newer BTK inhibitor acalabrutinib also shows benefit in the relapsed MCL setting, Dr. Blum said.
In a recent multicenter, open-label, phase 2 study of 124 patients with a median age of 68 years and a median of two prior therapies, acalabrutinib at a dose of 100 mg twice daily was associated with an OR rate of 81% and a CR rate of 40% (Lancet. 2018 Feb 17;391:659-67).
“Seems a little better than what you’d expect with single agent ibrutinib,” she said, noting that median DOR and PFS have not been reached in that study.
The main toxicities have been “headache and some diarrhea,” but follow-up is currently only about 15 months, she added.
Venetoclax
Another option in this setting is the B-cell lymphoma 2 (BCL-2) inhibitor venetoclax, which was shown in a recent phase 1 study of patients with various lymphoma subtypes to have activity in relapsed MCL, Dr. Blum said.
The OR rate in 28 relapsed MCL patients in that study was 75%, and the median PFS was 14 months (J Clin Oncol. 2017 Mar;35:826-33).
Additionally, an “intriguing combination study of venetoclax and ibrutinib” was recently published in the New England Journal of Medicine, she noted.
That study included only 23 patients with relapsed MCL, but they were a “pretty high-risk” group with a median age of 68 years, about half having a TP53 abnormality, and 30% having a prior transplant.
The OR and CR rates at 16 weeks by positron emission tomography were 71% and 62%, respectively (N Engl J Med. 2018 Mar 29;378:1211-23).
“Actually, about 40% achieved [minimal residual disease] negativity, but this was only checked in about half the patients,” she said. “So this is an intriguing combination and hopefully something we’ll see more of in the upcoming years.”
Lenalidomide
In the randomized phase 2 SPRINT study, patients received either single-agent lenolidamine or the investigator’s choice of single-agent rituximab, gemcitabine, fludarabine, chlorambucil, or cytarabine.
The expected OR rate in 170 patients treated with lenalidomide was 40% versus 11% in 84 patients treated with investigator’s choice of treatment, and the respective CR rates were 5% and 0% (Lancet Oncol. 2016 Mar 1;17(3):319-31).
Median DOR was 16 months versus 10.4 months, PFS was 8.7 versus 5.2 months, and median OS was 27.9 versus 21.1 months in the groups, respectively.
Other options
Combination regimens, such as R-CHOP and R-bendamustine, are also options for the treatment of relapsed MCL patients who haven’t received combination therapy in the past, Dr. Blum said. Transplant is another option in some patients.
“I will consider transplants for younger patients if they come to me and they actually hadn’t had one in [their] first CR,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
EXPERT ANALYSIS FROM MHM 2018
First-line bortezomib prolongs survival in MCL
Bortezomib in combination with rituximab plus chemotherapy significantly improved overall survival in transplant-ineligible patients with newly diagnosed mantle cell lymphoma (MCL), compared with standard treatment, according to final results from the international, phase 3 LYM-3002 trial.
After a median follow-up period of 82.0 months, median overall survival was 90.7 months among participants who were given first-line bortezomib in addition to rituximab plus cyclophosphamide, doxorubicin, and prednisone (VR-CAP) versus 55.7 months in the control arm, where patients were given rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP), for a hazard ratio of 0.66 (95% confidence interval, 0.51-0.85; P = .001).
Tadeusz Robak, MD, of the Medical University of Lodz in Poland, and his colleagues also reported that patients in the bortezomib arm experienced two novel adverse effects, which were different from findings reported in the primary analysis. Each case was classified as grade 4; there was one case of gastric cancer and one case of lung adenocarcinoma.
The findings were reported in the Lancet Oncology.
Among 268 patients in the follow-up analysis set, the median age was 66 years and 31% were classified as high risk based on the MCL-specific International Prognostic Index (MIPI). For those considered high risk, no significant difference was noted when comparing the two groups on the basis of overall survival.
“When analyzed according to MIPI risk category, VR-CAP was associated with significantly improved overall survival, compared with R-CHOP in the low-risk and intermediate-risk categories, but not in the high-risk category,” the investigators wrote.
The authors acknowledged a key limitation of the study was that rituximab was not given as a maintenance therapy since it was not considered standard of care at the time of study initiation.
Moving forward, Dr. Robak and his colleagues recommended that bortezomib be investigated in combination with newer targeted therapies in order to establish best practice for treating MCL.
The study was sponsored by Janssen Pharmaceuticals. The authors reported financial ties to Janssen, Celgene, Ipsen Biopharmaceuticals, Johnson & Johnson, Novartis, and others.
SOURCE: Robak T et al. Lancet Oncol. 2018 Oct 19. doi: 10.1016/S1470-2045(18)30685-5.
The proteasome inhibitor, bortezomib, represents a “substantial advance” for the treatment of newly diagnosed mantle cell lymphoma, according to Simon Rule, MD.
In an accompanying commentary, he stated that bortezomib-based VR-CAP (rituximab plus cyclophosphamide, doxorubicin, and prednisone) showed a clear survival benefit in the LYM-3002 trial, compared with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP). However, in order to use this combination in elderly patients, the administration method must be considered. Additionally, it makes sense to routinely use rituximab maintenance.
While the final analysis of the LYM-3002 trial is positive, there are caveats to consider before changing practice, particularly for elderly patients. First, the study had a somewhat younger population and fewer high-risk patients, compared with the only similar study of R-CHOP regimen in an elderly population. The bortezomib plus VR-CAP combination also had significant toxicity that could limit its widespread use in elderly patients.
Dr. Rule also noted that, internationally, bendamustine-based therapy is increasingly being chosen over R-CHOP for older patients with mantle cell lymphoma.
“Whether VR-CAP or the combination of bortezomib and bendamustine-based regimens will be the optimal approach has yet to be established. However, if R-CHOP is being considered, then the long-term survival results reported by Robak and colleagues strongly support the use of VR-CAP as an alternative,” Dr. Rule wrote.
Dr. Rule is with the University of Plymouth (England). These comments are adapted from his commentary (Lancet Oncol. 2018 Oct 19. doi: 10.1016/S1470-2045[18]30743-5). Dr. Rule reported receiving grants and personal fees from Janssen Pharmaceuticals.
The proteasome inhibitor, bortezomib, represents a “substantial advance” for the treatment of newly diagnosed mantle cell lymphoma, according to Simon Rule, MD.
In an accompanying commentary, he stated that bortezomib-based VR-CAP (rituximab plus cyclophosphamide, doxorubicin, and prednisone) showed a clear survival benefit in the LYM-3002 trial, compared with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP). However, in order to use this combination in elderly patients, the administration method must be considered. Additionally, it makes sense to routinely use rituximab maintenance.
While the final analysis of the LYM-3002 trial is positive, there are caveats to consider before changing practice, particularly for elderly patients. First, the study had a somewhat younger population and fewer high-risk patients, compared with the only similar study of R-CHOP regimen in an elderly population. The bortezomib plus VR-CAP combination also had significant toxicity that could limit its widespread use in elderly patients.
Dr. Rule also noted that, internationally, bendamustine-based therapy is increasingly being chosen over R-CHOP for older patients with mantle cell lymphoma.
“Whether VR-CAP or the combination of bortezomib and bendamustine-based regimens will be the optimal approach has yet to be established. However, if R-CHOP is being considered, then the long-term survival results reported by Robak and colleagues strongly support the use of VR-CAP as an alternative,” Dr. Rule wrote.
Dr. Rule is with the University of Plymouth (England). These comments are adapted from his commentary (Lancet Oncol. 2018 Oct 19. doi: 10.1016/S1470-2045[18]30743-5). Dr. Rule reported receiving grants and personal fees from Janssen Pharmaceuticals.
The proteasome inhibitor, bortezomib, represents a “substantial advance” for the treatment of newly diagnosed mantle cell lymphoma, according to Simon Rule, MD.
In an accompanying commentary, he stated that bortezomib-based VR-CAP (rituximab plus cyclophosphamide, doxorubicin, and prednisone) showed a clear survival benefit in the LYM-3002 trial, compared with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP). However, in order to use this combination in elderly patients, the administration method must be considered. Additionally, it makes sense to routinely use rituximab maintenance.
While the final analysis of the LYM-3002 trial is positive, there are caveats to consider before changing practice, particularly for elderly patients. First, the study had a somewhat younger population and fewer high-risk patients, compared with the only similar study of R-CHOP regimen in an elderly population. The bortezomib plus VR-CAP combination also had significant toxicity that could limit its widespread use in elderly patients.
Dr. Rule also noted that, internationally, bendamustine-based therapy is increasingly being chosen over R-CHOP for older patients with mantle cell lymphoma.
“Whether VR-CAP or the combination of bortezomib and bendamustine-based regimens will be the optimal approach has yet to be established. However, if R-CHOP is being considered, then the long-term survival results reported by Robak and colleagues strongly support the use of VR-CAP as an alternative,” Dr. Rule wrote.
Dr. Rule is with the University of Plymouth (England). These comments are adapted from his commentary (Lancet Oncol. 2018 Oct 19. doi: 10.1016/S1470-2045[18]30743-5). Dr. Rule reported receiving grants and personal fees from Janssen Pharmaceuticals.
Bortezomib in combination with rituximab plus chemotherapy significantly improved overall survival in transplant-ineligible patients with newly diagnosed mantle cell lymphoma (MCL), compared with standard treatment, according to final results from the international, phase 3 LYM-3002 trial.
After a median follow-up period of 82.0 months, median overall survival was 90.7 months among participants who were given first-line bortezomib in addition to rituximab plus cyclophosphamide, doxorubicin, and prednisone (VR-CAP) versus 55.7 months in the control arm, where patients were given rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP), for a hazard ratio of 0.66 (95% confidence interval, 0.51-0.85; P = .001).
Tadeusz Robak, MD, of the Medical University of Lodz in Poland, and his colleagues also reported that patients in the bortezomib arm experienced two novel adverse effects, which were different from findings reported in the primary analysis. Each case was classified as grade 4; there was one case of gastric cancer and one case of lung adenocarcinoma.
The findings were reported in the Lancet Oncology.
Among 268 patients in the follow-up analysis set, the median age was 66 years and 31% were classified as high risk based on the MCL-specific International Prognostic Index (MIPI). For those considered high risk, no significant difference was noted when comparing the two groups on the basis of overall survival.
“When analyzed according to MIPI risk category, VR-CAP was associated with significantly improved overall survival, compared with R-CHOP in the low-risk and intermediate-risk categories, but not in the high-risk category,” the investigators wrote.
The authors acknowledged a key limitation of the study was that rituximab was not given as a maintenance therapy since it was not considered standard of care at the time of study initiation.
Moving forward, Dr. Robak and his colleagues recommended that bortezomib be investigated in combination with newer targeted therapies in order to establish best practice for treating MCL.
The study was sponsored by Janssen Pharmaceuticals. The authors reported financial ties to Janssen, Celgene, Ipsen Biopharmaceuticals, Johnson & Johnson, Novartis, and others.
SOURCE: Robak T et al. Lancet Oncol. 2018 Oct 19. doi: 10.1016/S1470-2045(18)30685-5.
Bortezomib in combination with rituximab plus chemotherapy significantly improved overall survival in transplant-ineligible patients with newly diagnosed mantle cell lymphoma (MCL), compared with standard treatment, according to final results from the international, phase 3 LYM-3002 trial.
After a median follow-up period of 82.0 months, median overall survival was 90.7 months among participants who were given first-line bortezomib in addition to rituximab plus cyclophosphamide, doxorubicin, and prednisone (VR-CAP) versus 55.7 months in the control arm, where patients were given rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP), for a hazard ratio of 0.66 (95% confidence interval, 0.51-0.85; P = .001).
Tadeusz Robak, MD, of the Medical University of Lodz in Poland, and his colleagues also reported that patients in the bortezomib arm experienced two novel adverse effects, which were different from findings reported in the primary analysis. Each case was classified as grade 4; there was one case of gastric cancer and one case of lung adenocarcinoma.
The findings were reported in the Lancet Oncology.
Among 268 patients in the follow-up analysis set, the median age was 66 years and 31% were classified as high risk based on the MCL-specific International Prognostic Index (MIPI). For those considered high risk, no significant difference was noted when comparing the two groups on the basis of overall survival.
“When analyzed according to MIPI risk category, VR-CAP was associated with significantly improved overall survival, compared with R-CHOP in the low-risk and intermediate-risk categories, but not in the high-risk category,” the investigators wrote.
The authors acknowledged a key limitation of the study was that rituximab was not given as a maintenance therapy since it was not considered standard of care at the time of study initiation.
Moving forward, Dr. Robak and his colleagues recommended that bortezomib be investigated in combination with newer targeted therapies in order to establish best practice for treating MCL.
The study was sponsored by Janssen Pharmaceuticals. The authors reported financial ties to Janssen, Celgene, Ipsen Biopharmaceuticals, Johnson & Johnson, Novartis, and others.
SOURCE: Robak T et al. Lancet Oncol. 2018 Oct 19. doi: 10.1016/S1470-2045(18)30685-5.
FROM THE LANCET ONCOLOGY
Key clinical point:
Major finding: Median overall survival was 90.7 months in the intervention arm (bortezomib in addition to rituximab plus chemotherapy) versus 55.7 months in the control arm (hazard ratio, 0.66; 95% confidence interval, 0.51-0.85; P = .001).
Study details: LYM-3002 was a phase 3, randomized, open-label study of 487 transplant-ineligible patients with untreated mantle cell lymphoma.
Disclosures: The study was sponsored by Janssen Pharmaceuticals. The authors reported financial ties with Janssen, Celgene, Ipsen Biopharmaceuticals, Johnson & Johnson, Novartis, and others.
Source: Robak T et al. Lancet Oncol. 2018 Oct 19. doi: 10.1016/S1470-2045(18)30685-5.
Ibrutinib discontinuation harms survival in CLL
Discontinuing ibrutinib therapy because of disease progression was associated with worse survival, according to a real-world study of ibrutinib dosing in chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma patients.
Researchers at the University of Rochester Wilmot Cancer Institute in New York, who performed the single-center study, also found that optimal dosing early on in treatment has a significant impact on disease progression.
“Treating physicians need to be aware of these outcomes when initiating therapy on patients with high-risk CLL or lymphoma, as well as those with significant comorbidities or immune deficiencies,” AnnaLynn M. Williams. MS, and her colleagues reported in Clinical Lymphoma, Myeloma and Leukemia.
The researchers examined the impact of ibrutinib discontinuation and dose adherence on overall and progression-free survival in 170 patients with non-Hodgkin lymphoma and CLL treated with the drug at the Wilmot Cancer Institute between Jan. 1, 2014, and Dec. 1, 2016.
The study comprised 115 patients with CLL, 23 patients with Waldenstrom macroglobulinemia, 21 patients with mantle cell lymphoma, and 11 patients with other non-Hodgkin lymphomas. The median age of patients who started ibrutinib was 68 years, and the median treatment duration was 14.3 months. About a third of patients were taking ibrutinib as a first-line treatment.
Overall, 51 patients (30%) permanently discontinued ibrutinib during the study period, with more than half of the discontinuations stemming from adverse events or comorbidities. About 35% of the discontinuations were due to disease progression.
Median overall survival after discontinuation due to disease progression was 1.7 months. When patients discontinued for other reasons, median overall survival was not reached, compared with stopping for disease progression (P = .0008).
The researchers reported that among patients who discontinued for nonprogression reasons, 67% were alive after 1 year. Among CLL patients, 80% were alive after 1 year.
Among 20 patients who had a dose adherence of less than 80% in the first 8 weeks, the researchers found worse progression-free survival (P = .002) and overall survival (P = .021). Among CLL patients only, progression-free survival was significantly worse (P = .043) but overall survival was not (P = .816).
The study also included five patients who reduced their ibrutinib dose in the first 8 weeks – down to 280 mg in two patients, 140 mg in two patients, and 420 mg in one patient. Again, the researchers observed worse progression-free survival (P = .004) and overall survival (P = .014), compared with patients who maintained their dosing level.
Interrupting ibrutinib dosing had an impact on survival but not as much as discontinuation. Among 10 patients who interrupted therapy for more than a week and then restarted, progression-free survival was worse, compared with those who stayed on treatment continuously (P = .047), but overall survival was not significantly worse (P = .577).
“This would suggest that the ideal treatment strategy would be to recommend initiation of therapy at standard dosing and interruption as needed as directed in the [Food and Drug Administration] label,” the researchers wrote.
The study was funded by the National Cancer Institute and the Cadregari Endowment Fund. The researchers reported having no conflicts of interest.
SOURCE: Williams AM et al. Clin Lymphoma Myeloma Leuk. 2018 Oct 12. doi: 10.1016/j.clml.2018.10.005.
Discontinuing ibrutinib therapy because of disease progression was associated with worse survival, according to a real-world study of ibrutinib dosing in chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma patients.
Researchers at the University of Rochester Wilmot Cancer Institute in New York, who performed the single-center study, also found that optimal dosing early on in treatment has a significant impact on disease progression.
“Treating physicians need to be aware of these outcomes when initiating therapy on patients with high-risk CLL or lymphoma, as well as those with significant comorbidities or immune deficiencies,” AnnaLynn M. Williams. MS, and her colleagues reported in Clinical Lymphoma, Myeloma and Leukemia.
The researchers examined the impact of ibrutinib discontinuation and dose adherence on overall and progression-free survival in 170 patients with non-Hodgkin lymphoma and CLL treated with the drug at the Wilmot Cancer Institute between Jan. 1, 2014, and Dec. 1, 2016.
The study comprised 115 patients with CLL, 23 patients with Waldenstrom macroglobulinemia, 21 patients with mantle cell lymphoma, and 11 patients with other non-Hodgkin lymphomas. The median age of patients who started ibrutinib was 68 years, and the median treatment duration was 14.3 months. About a third of patients were taking ibrutinib as a first-line treatment.
Overall, 51 patients (30%) permanently discontinued ibrutinib during the study period, with more than half of the discontinuations stemming from adverse events or comorbidities. About 35% of the discontinuations were due to disease progression.
Median overall survival after discontinuation due to disease progression was 1.7 months. When patients discontinued for other reasons, median overall survival was not reached, compared with stopping for disease progression (P = .0008).
The researchers reported that among patients who discontinued for nonprogression reasons, 67% were alive after 1 year. Among CLL patients, 80% were alive after 1 year.
Among 20 patients who had a dose adherence of less than 80% in the first 8 weeks, the researchers found worse progression-free survival (P = .002) and overall survival (P = .021). Among CLL patients only, progression-free survival was significantly worse (P = .043) but overall survival was not (P = .816).
The study also included five patients who reduced their ibrutinib dose in the first 8 weeks – down to 280 mg in two patients, 140 mg in two patients, and 420 mg in one patient. Again, the researchers observed worse progression-free survival (P = .004) and overall survival (P = .014), compared with patients who maintained their dosing level.
Interrupting ibrutinib dosing had an impact on survival but not as much as discontinuation. Among 10 patients who interrupted therapy for more than a week and then restarted, progression-free survival was worse, compared with those who stayed on treatment continuously (P = .047), but overall survival was not significantly worse (P = .577).
“This would suggest that the ideal treatment strategy would be to recommend initiation of therapy at standard dosing and interruption as needed as directed in the [Food and Drug Administration] label,” the researchers wrote.
The study was funded by the National Cancer Institute and the Cadregari Endowment Fund. The researchers reported having no conflicts of interest.
SOURCE: Williams AM et al. Clin Lymphoma Myeloma Leuk. 2018 Oct 12. doi: 10.1016/j.clml.2018.10.005.
Discontinuing ibrutinib therapy because of disease progression was associated with worse survival, according to a real-world study of ibrutinib dosing in chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma patients.
Researchers at the University of Rochester Wilmot Cancer Institute in New York, who performed the single-center study, also found that optimal dosing early on in treatment has a significant impact on disease progression.
“Treating physicians need to be aware of these outcomes when initiating therapy on patients with high-risk CLL or lymphoma, as well as those with significant comorbidities or immune deficiencies,” AnnaLynn M. Williams. MS, and her colleagues reported in Clinical Lymphoma, Myeloma and Leukemia.
The researchers examined the impact of ibrutinib discontinuation and dose adherence on overall and progression-free survival in 170 patients with non-Hodgkin lymphoma and CLL treated with the drug at the Wilmot Cancer Institute between Jan. 1, 2014, and Dec. 1, 2016.
The study comprised 115 patients with CLL, 23 patients with Waldenstrom macroglobulinemia, 21 patients with mantle cell lymphoma, and 11 patients with other non-Hodgkin lymphomas. The median age of patients who started ibrutinib was 68 years, and the median treatment duration was 14.3 months. About a third of patients were taking ibrutinib as a first-line treatment.
Overall, 51 patients (30%) permanently discontinued ibrutinib during the study period, with more than half of the discontinuations stemming from adverse events or comorbidities. About 35% of the discontinuations were due to disease progression.
Median overall survival after discontinuation due to disease progression was 1.7 months. When patients discontinued for other reasons, median overall survival was not reached, compared with stopping for disease progression (P = .0008).
The researchers reported that among patients who discontinued for nonprogression reasons, 67% were alive after 1 year. Among CLL patients, 80% were alive after 1 year.
Among 20 patients who had a dose adherence of less than 80% in the first 8 weeks, the researchers found worse progression-free survival (P = .002) and overall survival (P = .021). Among CLL patients only, progression-free survival was significantly worse (P = .043) but overall survival was not (P = .816).
The study also included five patients who reduced their ibrutinib dose in the first 8 weeks – down to 280 mg in two patients, 140 mg in two patients, and 420 mg in one patient. Again, the researchers observed worse progression-free survival (P = .004) and overall survival (P = .014), compared with patients who maintained their dosing level.
Interrupting ibrutinib dosing had an impact on survival but not as much as discontinuation. Among 10 patients who interrupted therapy for more than a week and then restarted, progression-free survival was worse, compared with those who stayed on treatment continuously (P = .047), but overall survival was not significantly worse (P = .577).
“This would suggest that the ideal treatment strategy would be to recommend initiation of therapy at standard dosing and interruption as needed as directed in the [Food and Drug Administration] label,” the researchers wrote.
The study was funded by the National Cancer Institute and the Cadregari Endowment Fund. The researchers reported having no conflicts of interest.
SOURCE: Williams AM et al. Clin Lymphoma Myeloma Leuk. 2018 Oct 12. doi: 10.1016/j.clml.2018.10.005.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
Key clinical point:
Major finding: Median overall survival after discontinuation of ibrutinib due to disease progression was 1.7 months.
Study details: A single-institution study of 170 patients with CLL or non-Hodgkin lymphoma who were taking ibrutinib.
Disclosures: The study was funded by the National Cancer Institute and the Cadregari Endowment Fund. The researchers reported having no conflicts of interest.
Source: Williams AM et al. Clin Lymphoma Myeloma Leuk. 2018 Oct 12. doi: 10.1016/j.clml.2018.10.005.
MCL treatment choices depend partly on age
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
EXPERT ANALYSIS FROM MHM 2018
Prognostic factors guide mantle cell treatment decisions
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
REPORTING FROM MHM 2018
Outpatient lenalidomide/rituximab yields long-term MCL remission
After 5 years, the combination of lenalidomide and rituximab as first-line therapy for mantle cell lymphoma (MCL) continues to show durable responses with manageable toxicities, long-term results from a phase 2 clinical trial show.
After a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University, New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote. Their report was published in Blood.
In the multicenter, phase 2 single-arm study, 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase. Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P = .04).
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption. Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting, lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach,” the investigators wrote.
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
SOURCE: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.
After 5 years, the combination of lenalidomide and rituximab as first-line therapy for mantle cell lymphoma (MCL) continues to show durable responses with manageable toxicities, long-term results from a phase 2 clinical trial show.
After a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University, New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote. Their report was published in Blood.
In the multicenter, phase 2 single-arm study, 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase. Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P = .04).
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption. Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting, lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach,” the investigators wrote.
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
SOURCE: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.
After 5 years, the combination of lenalidomide and rituximab as first-line therapy for mantle cell lymphoma (MCL) continues to show durable responses with manageable toxicities, long-term results from a phase 2 clinical trial show.
After a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University, New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote. Their report was published in Blood.
In the multicenter, phase 2 single-arm study, 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase. Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P = .04).
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption. Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting, lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach,” the investigators wrote.
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
SOURCE: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.
FROM BLOOD
Key clinical point:
Major finding: After 64-months of median follow-up, 21 of 33 patients with initial responses remained in remission.
Study details: Five-year follow-up of a phase 2 single arm trial of lenalidomide/rituximab induction and maintenance in 38 patients with mantle cell lymphoma.
Disclosures: The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
Source: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.