User login
Drug receives fast track, orphan designations for PTCL
The US Food and Drug Administration (FDA) has granted orphan drug and fast track designations to tenalisib (RP6530) for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib is a dual PI3K delta/gamma inhibitor being developed by Rhizen Pharmaceuticals.
Research has shown that tenalisib inhibits the growth of immortalized cancerous cell lines and primary leukemia/lymphoma cells.
In preclinical studies, tenalisib reprogrammed macrophages from an immunosuppressive M2-like phenotype (pro-tumor) to an inflammatory M1-like state (anti-tumor).
Researchers are currently conducting a phase 1 study of tenalisib in patients with relapsed/refractory PTCL. Results from this study were presented at the 2017 ASH Annual Meeting (abstract 2791*).
The presentation included data on 50 patients—24 with PTCL and 26 with cutaneous T-cell lymphoma (CTCL).
For the PTCL patients, the median age was 63 (range, 40-89), and 67% were male. The median number of prior therapies was 3 (range, 1-7). All patients had an ECOG status of 0 (n=14) or 1 (n=10). More patients had relapsed disease (n=17, 58%) than refractory disease (n=10, 42%).
For the CTCL patients, the median age was 67 (range, 37-84), and 46% were male. The median number of prior therapies was 5.5 (range, 2-15). All patients had an ECOG status of 0 (n=23) or 1 (n=3). More patients had refractory disease (n=15, 58%) than relapsed disease (n=11, 42%).
In the dose-escalation portion of the study, patients received tenalisib at 200 mg twice daily (BID), 400 mg BID, 800 mg BID fasting, or 800 mg BID fed. The maximum tolerated dose was 800 mg BID fasting, so this dose is being used in the expansion cohort.
Twelve PTCL patients were evaluable for efficacy. The overall response rate in these patients was 58% (7/12), with a 25% complete response rate (3/12).
Sixteen CTCL patients were evaluable for efficacy. The overall response rate was 56% (9/16). All responders had partial responses.
In both PTCL and CTCL patients, treatment-related grade 3 or higher adverse events (AEs) included transaminitis (22%), rash (6%), neutropenia (6%), hypophosphatemia (2%), increased international normalized ratio (2%), diplopia secondary to neuropathy (2%), and sepsis (2%).
Treatment-related serious AEs included sepsis, increased international normalized ratio, diplopia secondary to neuropathy, and pyrexia. Five patients discontinued treatment due to AEs.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available. ![]()
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted orphan drug and fast track designations to tenalisib (RP6530) for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib is a dual PI3K delta/gamma inhibitor being developed by Rhizen Pharmaceuticals.
Research has shown that tenalisib inhibits the growth of immortalized cancerous cell lines and primary leukemia/lymphoma cells.
In preclinical studies, tenalisib reprogrammed macrophages from an immunosuppressive M2-like phenotype (pro-tumor) to an inflammatory M1-like state (anti-tumor).
Researchers are currently conducting a phase 1 study of tenalisib in patients with relapsed/refractory PTCL. Results from this study were presented at the 2017 ASH Annual Meeting (abstract 2791*).
The presentation included data on 50 patients—24 with PTCL and 26 with cutaneous T-cell lymphoma (CTCL).
For the PTCL patients, the median age was 63 (range, 40-89), and 67% were male. The median number of prior therapies was 3 (range, 1-7). All patients had an ECOG status of 0 (n=14) or 1 (n=10). More patients had relapsed disease (n=17, 58%) than refractory disease (n=10, 42%).
For the CTCL patients, the median age was 67 (range, 37-84), and 46% were male. The median number of prior therapies was 5.5 (range, 2-15). All patients had an ECOG status of 0 (n=23) or 1 (n=3). More patients had refractory disease (n=15, 58%) than relapsed disease (n=11, 42%).
In the dose-escalation portion of the study, patients received tenalisib at 200 mg twice daily (BID), 400 mg BID, 800 mg BID fasting, or 800 mg BID fed. The maximum tolerated dose was 800 mg BID fasting, so this dose is being used in the expansion cohort.
Twelve PTCL patients were evaluable for efficacy. The overall response rate in these patients was 58% (7/12), with a 25% complete response rate (3/12).
Sixteen CTCL patients were evaluable for efficacy. The overall response rate was 56% (9/16). All responders had partial responses.
In both PTCL and CTCL patients, treatment-related grade 3 or higher adverse events (AEs) included transaminitis (22%), rash (6%), neutropenia (6%), hypophosphatemia (2%), increased international normalized ratio (2%), diplopia secondary to neuropathy (2%), and sepsis (2%).
Treatment-related serious AEs included sepsis, increased international normalized ratio, diplopia secondary to neuropathy, and pyrexia. Five patients discontinued treatment due to AEs.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available. ![]()
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted orphan drug and fast track designations to tenalisib (RP6530) for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib is a dual PI3K delta/gamma inhibitor being developed by Rhizen Pharmaceuticals.
Research has shown that tenalisib inhibits the growth of immortalized cancerous cell lines and primary leukemia/lymphoma cells.
In preclinical studies, tenalisib reprogrammed macrophages from an immunosuppressive M2-like phenotype (pro-tumor) to an inflammatory M1-like state (anti-tumor).
Researchers are currently conducting a phase 1 study of tenalisib in patients with relapsed/refractory PTCL. Results from this study were presented at the 2017 ASH Annual Meeting (abstract 2791*).
The presentation included data on 50 patients—24 with PTCL and 26 with cutaneous T-cell lymphoma (CTCL).
For the PTCL patients, the median age was 63 (range, 40-89), and 67% were male. The median number of prior therapies was 3 (range, 1-7). All patients had an ECOG status of 0 (n=14) or 1 (n=10). More patients had relapsed disease (n=17, 58%) than refractory disease (n=10, 42%).
For the CTCL patients, the median age was 67 (range, 37-84), and 46% were male. The median number of prior therapies was 5.5 (range, 2-15). All patients had an ECOG status of 0 (n=23) or 1 (n=3). More patients had refractory disease (n=15, 58%) than relapsed disease (n=11, 42%).
In the dose-escalation portion of the study, patients received tenalisib at 200 mg twice daily (BID), 400 mg BID, 800 mg BID fasting, or 800 mg BID fed. The maximum tolerated dose was 800 mg BID fasting, so this dose is being used in the expansion cohort.
Twelve PTCL patients were evaluable for efficacy. The overall response rate in these patients was 58% (7/12), with a 25% complete response rate (3/12).
Sixteen CTCL patients were evaluable for efficacy. The overall response rate was 56% (9/16). All responders had partial responses.
In both PTCL and CTCL patients, treatment-related grade 3 or higher adverse events (AEs) included transaminitis (22%), rash (6%), neutropenia (6%), hypophosphatemia (2%), increased international normalized ratio (2%), diplopia secondary to neuropathy (2%), and sepsis (2%).
Treatment-related serious AEs included sepsis, increased international normalized ratio, diplopia secondary to neuropathy, and pyrexia. Five patients discontinued treatment due to AEs.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available. ![]()
*Data in the abstract differ from the presentation.
Chemo-free combo should be option for rel/ref CLL, doc says
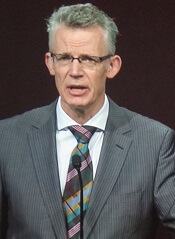
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
Risk stratification may be possible with JCAR017
ATLANTA—Data suggest a therapeutic window may exist for chimeric antigen receptor (CAR) T-cell expansion with JCAR017, according to a preliminary model.
In a core set of 67 patients with diffuse large B-cell lymphoma (DLBCL) who had received JCAR017 in the TRANSCEND NHL 001 trial, investigators observed that baseline high tumor burden and inflammatory biomarkers were associated with high CAR T-cell expansion and increased rates of cytokine release syndrome (CRS) and neurotoxicity.
If the model holds up, researchers say they could potentially identify patients at risk for low or high T-cell expansion levels and develop a strategy to enhance or limit the expansion.
TRANSCEND NHL 001 (NCT02631044) is a multicenter, phase 1 trial in relapsed or refractory non-Hodgkin lymphoma evaluating 2 dose levels of JCAR017, also known as lisocabtagene maraleucel, or liso-cel for short.
Liso-cel is a CD19-directed 4-1BB CAR T cell administered at precise doses of CD4+ and CD8+ CAR T cells. It had previously demonstrated high complete remission (CR) rates and low incidences of CRS and neurotoxicity.
Tanya Saddiqi, MD, of City of Hope National Medical Center in Duarte, California, presented data from the dose-finding and expansion cohorts at the 2017 ASH Annual Meeting (abstract 193*).
Study design
Patients with DLBCL after 2 lines of prior therapy or mantle cell lymphoma after 1 prior line of therapy were eligible to enroll in TRANSCEND NHL 001.
Patients with de novo DLBCL, those who transformed from follicular lymphoma, or those with high-grade B-cell lymphoma made up the pivotal or core population. All DLBCL patients enrolled on the trial comprised the full population.
Patients were screened, enrolled, and underwent apheresis. Bridging therapy was permitted while their CAR T cells were being manufactured.
Patients then had a PET scan and lab tests prior to lymphodepletion.
“This is the time point of our interest,” Dr Saddiqi said, “to see if there are any patient characteristics or biomarkers that we can identify . . . that could help us figure out which patients are at higher risk of toxicity, potentially.”
Lymphodepletion consisted of fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2 for 3 days).
Patients received the JCAR017 infusion, and, at specific time points thereafter, cytokine, pharmacokinetic (PK), and clinical lab evaluations were conducted. PK evaluation and scans were performed every 3 months for the first year after JCAR017 infusion, and safety and viral vector follow-up for 15 years.
Dose levels were 5 x 107 cells as a single or double dose (DL1S) and 1 x 108 cells as a single dose (DL2S). Dose level 2 was chosen for further study, and double dosing was discontinued.
“Double dosing was actually not pursued further,” Dr Saddiqi explained, “because it did not seem to add any benefit over single dosing.”
At the time of the presentation, 91 total patients were treated, 67 of whom were the core population.
Results
Dr Saddiqi reported that patients treated with JCAR017 achieved a relatively high best overall response rate (ORR) and high durable CR rates.
“And this seems to be especially true for the core set of patients and particularly for patients at dose level 2,” she added.
At all dose levels, the core patients had a best ORR of 84% (41/49) and a CR rate of 61% (30/49).
At follow-up of 3 months or longer, the core group had an ORR of 65% (26/40) for all dose levels, 52% (11/21) for dose level 1, and 80% (12/15) for dose level 2.
The 3-month CR rate was 53% (21/40) for all dose levels in the core group, 33% (7/21) in dose level 1, and 73% (11/15) in dose level 2.
Dr Saddiqi noted that CRS and neurotoxicity did not differ by dose level or schedule, and there were no grade 5 events of CRS or neurotoxicity.
“Among the core group, dose level change did not add to their toxicity,” she said. “And so the question is: Is it patient factors, is it tumor factors? What is it that is actually causing the toxicities in these patients?”
Dr Saddiqi focused the presentation on patient factors.
Patient factors
The data showed that tumor burden and lactose dehydrogenase (LDH) levels were higher in patients with CRS and neurotoxicity.
Univariate analysis revealed that CRS and neurotoxicity were associated with a shorter time since diagnosis.
However, prior number of therapies, patient weight, and disease stage were not associated with CRS or neurotoxicity.
Investigators were able to identify preliminary risk boundaries. Core patients with high LDH levels (≥ 500 U/L) and sum of the products of diameters (SPD) ≥ 50 cm2 at baseline had an 8-fold increase in risk of CRS and neurotoxicity.
“Inversely, if these patients did not meet the cutoff for LDH or SPD,” Dr Saddiqi pointed out, “if they were lower than that, they have significantly lower CRS and neurotoxicity events.”
Investigators also observed that baseline markers of inflammation and inflammatory cytokines trended higher in patients with CRS and neurotoxicity. For CRS, this includes ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNFα, and MIP-1β. For neurotoxicity, this includes ferritin, CRP, d-Dimer, IL-6, IL-15, TNFα, and MIP-1α.
The team also observed that tumor burden, baseline markers of inflammation, and inflammatory cytokines trended lower in core patients with durable responses.
“Interestingly, it’s inversely true that patients who did have these higher levels [of inflammation markers], and higher tumor burden, and higher LDH, actually were the ones that were either showing no response at 3 months or had lost their response by the 3-month assessment point,” Dr Saddiqi explained.
And in patients with higher baseline tumor burden and inflammatory cytokine levels, JCAR017 T-cell expansion trended higher.
“Some were deemed to be super expanders because their CAR T-cell levels were very high in their blood,” she added.
The investigators created a preliminary logistic model based on the data that suggests a therapeutic window might be able to limit toxicity and optimize efficacy.
The model indicates that patients with higher tumor burden, higher LDH, and higher inflammatory state at baseline seem to be the ones who are having more CRS and more neurotoxicity after CAR T-cell infusion.
“They are expanding their cells much more, yet their responses at 3 months seem to be affected adversely by this entire situation,” Dr Saddiqi said.
"One explanation, potentially, could be that these CAR T cells are seeing a lot of antigen when they go into the body. They have the perfect cytokine milieu to grow, expand, and go crazy in the body, if you will, and very quickly peter out as well because there’s T-cell exhaustion that happens rather rapidly and clinical responses are then then lost.”
The investigators believe that if they can identify those patients ahead of time who may be at risk of too high expansion or too low expansion of their CAR T cells, they may be able to find strategies to push expansion into the “sweet spot of CAR T-cell expansion and ultimately get the holy grail of having durable responses for all with minimal toxicity,” Dr Saddiqi concluded.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics, Inc. Dr Saddiqi has served on a steering committee for JCAR017. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Data suggest a therapeutic window may exist for chimeric antigen receptor (CAR) T-cell expansion with JCAR017, according to a preliminary model.
In a core set of 67 patients with diffuse large B-cell lymphoma (DLBCL) who had received JCAR017 in the TRANSCEND NHL 001 trial, investigators observed that baseline high tumor burden and inflammatory biomarkers were associated with high CAR T-cell expansion and increased rates of cytokine release syndrome (CRS) and neurotoxicity.
If the model holds up, researchers say they could potentially identify patients at risk for low or high T-cell expansion levels and develop a strategy to enhance or limit the expansion.
TRANSCEND NHL 001 (NCT02631044) is a multicenter, phase 1 trial in relapsed or refractory non-Hodgkin lymphoma evaluating 2 dose levels of JCAR017, also known as lisocabtagene maraleucel, or liso-cel for short.
Liso-cel is a CD19-directed 4-1BB CAR T cell administered at precise doses of CD4+ and CD8+ CAR T cells. It had previously demonstrated high complete remission (CR) rates and low incidences of CRS and neurotoxicity.
Tanya Saddiqi, MD, of City of Hope National Medical Center in Duarte, California, presented data from the dose-finding and expansion cohorts at the 2017 ASH Annual Meeting (abstract 193*).
Study design
Patients with DLBCL after 2 lines of prior therapy or mantle cell lymphoma after 1 prior line of therapy were eligible to enroll in TRANSCEND NHL 001.
Patients with de novo DLBCL, those who transformed from follicular lymphoma, or those with high-grade B-cell lymphoma made up the pivotal or core population. All DLBCL patients enrolled on the trial comprised the full population.
Patients were screened, enrolled, and underwent apheresis. Bridging therapy was permitted while their CAR T cells were being manufactured.
Patients then had a PET scan and lab tests prior to lymphodepletion.
“This is the time point of our interest,” Dr Saddiqi said, “to see if there are any patient characteristics or biomarkers that we can identify . . . that could help us figure out which patients are at higher risk of toxicity, potentially.”
Lymphodepletion consisted of fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2 for 3 days).
Patients received the JCAR017 infusion, and, at specific time points thereafter, cytokine, pharmacokinetic (PK), and clinical lab evaluations were conducted. PK evaluation and scans were performed every 3 months for the first year after JCAR017 infusion, and safety and viral vector follow-up for 15 years.
Dose levels were 5 x 107 cells as a single or double dose (DL1S) and 1 x 108 cells as a single dose (DL2S). Dose level 2 was chosen for further study, and double dosing was discontinued.
“Double dosing was actually not pursued further,” Dr Saddiqi explained, “because it did not seem to add any benefit over single dosing.”
At the time of the presentation, 91 total patients were treated, 67 of whom were the core population.
Results
Dr Saddiqi reported that patients treated with JCAR017 achieved a relatively high best overall response rate (ORR) and high durable CR rates.
“And this seems to be especially true for the core set of patients and particularly for patients at dose level 2,” she added.
At all dose levels, the core patients had a best ORR of 84% (41/49) and a CR rate of 61% (30/49).
At follow-up of 3 months or longer, the core group had an ORR of 65% (26/40) for all dose levels, 52% (11/21) for dose level 1, and 80% (12/15) for dose level 2.
The 3-month CR rate was 53% (21/40) for all dose levels in the core group, 33% (7/21) in dose level 1, and 73% (11/15) in dose level 2.
Dr Saddiqi noted that CRS and neurotoxicity did not differ by dose level or schedule, and there were no grade 5 events of CRS or neurotoxicity.
“Among the core group, dose level change did not add to their toxicity,” she said. “And so the question is: Is it patient factors, is it tumor factors? What is it that is actually causing the toxicities in these patients?”
Dr Saddiqi focused the presentation on patient factors.
Patient factors
The data showed that tumor burden and lactose dehydrogenase (LDH) levels were higher in patients with CRS and neurotoxicity.
Univariate analysis revealed that CRS and neurotoxicity were associated with a shorter time since diagnosis.
However, prior number of therapies, patient weight, and disease stage were not associated with CRS or neurotoxicity.
Investigators were able to identify preliminary risk boundaries. Core patients with high LDH levels (≥ 500 U/L) and sum of the products of diameters (SPD) ≥ 50 cm2 at baseline had an 8-fold increase in risk of CRS and neurotoxicity.
“Inversely, if these patients did not meet the cutoff for LDH or SPD,” Dr Saddiqi pointed out, “if they were lower than that, they have significantly lower CRS and neurotoxicity events.”
Investigators also observed that baseline markers of inflammation and inflammatory cytokines trended higher in patients with CRS and neurotoxicity. For CRS, this includes ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNFα, and MIP-1β. For neurotoxicity, this includes ferritin, CRP, d-Dimer, IL-6, IL-15, TNFα, and MIP-1α.
The team also observed that tumor burden, baseline markers of inflammation, and inflammatory cytokines trended lower in core patients with durable responses.
“Interestingly, it’s inversely true that patients who did have these higher levels [of inflammation markers], and higher tumor burden, and higher LDH, actually were the ones that were either showing no response at 3 months or had lost their response by the 3-month assessment point,” Dr Saddiqi explained.
And in patients with higher baseline tumor burden and inflammatory cytokine levels, JCAR017 T-cell expansion trended higher.
“Some were deemed to be super expanders because their CAR T-cell levels were very high in their blood,” she added.
The investigators created a preliminary logistic model based on the data that suggests a therapeutic window might be able to limit toxicity and optimize efficacy.
The model indicates that patients with higher tumor burden, higher LDH, and higher inflammatory state at baseline seem to be the ones who are having more CRS and more neurotoxicity after CAR T-cell infusion.
“They are expanding their cells much more, yet their responses at 3 months seem to be affected adversely by this entire situation,” Dr Saddiqi said.
"One explanation, potentially, could be that these CAR T cells are seeing a lot of antigen when they go into the body. They have the perfect cytokine milieu to grow, expand, and go crazy in the body, if you will, and very quickly peter out as well because there’s T-cell exhaustion that happens rather rapidly and clinical responses are then then lost.”
The investigators believe that if they can identify those patients ahead of time who may be at risk of too high expansion or too low expansion of their CAR T cells, they may be able to find strategies to push expansion into the “sweet spot of CAR T-cell expansion and ultimately get the holy grail of having durable responses for all with minimal toxicity,” Dr Saddiqi concluded.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics, Inc. Dr Saddiqi has served on a steering committee for JCAR017. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Data suggest a therapeutic window may exist for chimeric antigen receptor (CAR) T-cell expansion with JCAR017, according to a preliminary model.
In a core set of 67 patients with diffuse large B-cell lymphoma (DLBCL) who had received JCAR017 in the TRANSCEND NHL 001 trial, investigators observed that baseline high tumor burden and inflammatory biomarkers were associated with high CAR T-cell expansion and increased rates of cytokine release syndrome (CRS) and neurotoxicity.
If the model holds up, researchers say they could potentially identify patients at risk for low or high T-cell expansion levels and develop a strategy to enhance or limit the expansion.
TRANSCEND NHL 001 (NCT02631044) is a multicenter, phase 1 trial in relapsed or refractory non-Hodgkin lymphoma evaluating 2 dose levels of JCAR017, also known as lisocabtagene maraleucel, or liso-cel for short.
Liso-cel is a CD19-directed 4-1BB CAR T cell administered at precise doses of CD4+ and CD8+ CAR T cells. It had previously demonstrated high complete remission (CR) rates and low incidences of CRS and neurotoxicity.
Tanya Saddiqi, MD, of City of Hope National Medical Center in Duarte, California, presented data from the dose-finding and expansion cohorts at the 2017 ASH Annual Meeting (abstract 193*).
Study design
Patients with DLBCL after 2 lines of prior therapy or mantle cell lymphoma after 1 prior line of therapy were eligible to enroll in TRANSCEND NHL 001.
Patients with de novo DLBCL, those who transformed from follicular lymphoma, or those with high-grade B-cell lymphoma made up the pivotal or core population. All DLBCL patients enrolled on the trial comprised the full population.
Patients were screened, enrolled, and underwent apheresis. Bridging therapy was permitted while their CAR T cells were being manufactured.
Patients then had a PET scan and lab tests prior to lymphodepletion.
“This is the time point of our interest,” Dr Saddiqi said, “to see if there are any patient characteristics or biomarkers that we can identify . . . that could help us figure out which patients are at higher risk of toxicity, potentially.”
Lymphodepletion consisted of fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2 for 3 days).
Patients received the JCAR017 infusion, and, at specific time points thereafter, cytokine, pharmacokinetic (PK), and clinical lab evaluations were conducted. PK evaluation and scans were performed every 3 months for the first year after JCAR017 infusion, and safety and viral vector follow-up for 15 years.
Dose levels were 5 x 107 cells as a single or double dose (DL1S) and 1 x 108 cells as a single dose (DL2S). Dose level 2 was chosen for further study, and double dosing was discontinued.
“Double dosing was actually not pursued further,” Dr Saddiqi explained, “because it did not seem to add any benefit over single dosing.”
At the time of the presentation, 91 total patients were treated, 67 of whom were the core population.
Results
Dr Saddiqi reported that patients treated with JCAR017 achieved a relatively high best overall response rate (ORR) and high durable CR rates.
“And this seems to be especially true for the core set of patients and particularly for patients at dose level 2,” she added.
At all dose levels, the core patients had a best ORR of 84% (41/49) and a CR rate of 61% (30/49).
At follow-up of 3 months or longer, the core group had an ORR of 65% (26/40) for all dose levels, 52% (11/21) for dose level 1, and 80% (12/15) for dose level 2.
The 3-month CR rate was 53% (21/40) for all dose levels in the core group, 33% (7/21) in dose level 1, and 73% (11/15) in dose level 2.
Dr Saddiqi noted that CRS and neurotoxicity did not differ by dose level or schedule, and there were no grade 5 events of CRS or neurotoxicity.
“Among the core group, dose level change did not add to their toxicity,” she said. “And so the question is: Is it patient factors, is it tumor factors? What is it that is actually causing the toxicities in these patients?”
Dr Saddiqi focused the presentation on patient factors.
Patient factors
The data showed that tumor burden and lactose dehydrogenase (LDH) levels were higher in patients with CRS and neurotoxicity.
Univariate analysis revealed that CRS and neurotoxicity were associated with a shorter time since diagnosis.
However, prior number of therapies, patient weight, and disease stage were not associated with CRS or neurotoxicity.
Investigators were able to identify preliminary risk boundaries. Core patients with high LDH levels (≥ 500 U/L) and sum of the products of diameters (SPD) ≥ 50 cm2 at baseline had an 8-fold increase in risk of CRS and neurotoxicity.
“Inversely, if these patients did not meet the cutoff for LDH or SPD,” Dr Saddiqi pointed out, “if they were lower than that, they have significantly lower CRS and neurotoxicity events.”
Investigators also observed that baseline markers of inflammation and inflammatory cytokines trended higher in patients with CRS and neurotoxicity. For CRS, this includes ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNFα, and MIP-1β. For neurotoxicity, this includes ferritin, CRP, d-Dimer, IL-6, IL-15, TNFα, and MIP-1α.
The team also observed that tumor burden, baseline markers of inflammation, and inflammatory cytokines trended lower in core patients with durable responses.
“Interestingly, it’s inversely true that patients who did have these higher levels [of inflammation markers], and higher tumor burden, and higher LDH, actually were the ones that were either showing no response at 3 months or had lost their response by the 3-month assessment point,” Dr Saddiqi explained.
And in patients with higher baseline tumor burden and inflammatory cytokine levels, JCAR017 T-cell expansion trended higher.
“Some were deemed to be super expanders because their CAR T-cell levels were very high in their blood,” she added.
The investigators created a preliminary logistic model based on the data that suggests a therapeutic window might be able to limit toxicity and optimize efficacy.
The model indicates that patients with higher tumor burden, higher LDH, and higher inflammatory state at baseline seem to be the ones who are having more CRS and more neurotoxicity after CAR T-cell infusion.
“They are expanding their cells much more, yet their responses at 3 months seem to be affected adversely by this entire situation,” Dr Saddiqi said.
"One explanation, potentially, could be that these CAR T cells are seeing a lot of antigen when they go into the body. They have the perfect cytokine milieu to grow, expand, and go crazy in the body, if you will, and very quickly peter out as well because there’s T-cell exhaustion that happens rather rapidly and clinical responses are then then lost.”
The investigators believe that if they can identify those patients ahead of time who may be at risk of too high expansion or too low expansion of their CAR T cells, they may be able to find strategies to push expansion into the “sweet spot of CAR T-cell expansion and ultimately get the holy grail of having durable responses for all with minimal toxicity,” Dr Saddiqi concluded.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics, Inc. Dr Saddiqi has served on a steering committee for JCAR017. ![]()
*Data in the presentation differ from the abstract.
Pembrolizumab sBLA receives priority review
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for the anti-PD-1 therapy pembrolizumab (KEYTRUDA).
With this sBLA, Merck is seeking approval for pembrolizumab to treat adult and pediatric patients with refractory primary mediastinal B-cell lymphoma (PMBCL) or patients with PMBCL who have relapsed after 2 or more prior lines of therapy.
The FDA expects to make a decision on the sBLA by April 3, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, microsatellite instability-high cancer, and gastric cancer.
The sBLA for pembrolizumab as a treatment for PMBCL is supported by the phase 2 KEYNOTE-170 trial. Results from this trial were presented at the 2017 ASH Annual Meeting (abstract 2833).
KEYNOTE-170 is an ongoing study in which researchers are evaluating pembrolizumab (given at a 200 mg fixed dose every 3 weeks) in patients with relapsed/refractory PMBCL or relapsed/refractory Richter syndrome.
The PMBCL cohort enrolled patients who relapsed after autologous stem cell transplant (ASCT), were refractory to ASCT, or were ineligible for ASCT. Patients ineligible for ASCT had to have received 2 or more lines of prior therapy.
The median duration of follow-up was 10.5 months (range, 0.1-17.7).
In the efficacy population (n=29), the overall response rate was 41% (n=12), and the complete response rate was 24% (n=7).
The median time to response was 2.8 months (range, 2.4-5.5), and the median duration of response was not reached (range, 1.1+ to 13.6+ months).
Of the 53 patients evaluated for safety, 57% (n=30) experienced treatment-related adverse events (TRAEs), including 21% (n=11) who experienced grade 3-4 TRAEs.
The most common TRAEs (occurring in at least 5% of patients) were neutropenia (n=11), hypothyroidism (n=4), asthenia (n=3), and pyrexia (n=3).
Immune-mediated adverse events of all grades occurred in 11% (n=6) of patients. These include hypothyroidism (n=4), hyperthyroidism (n=2), pneumonitis (n=1), and thyroiditis (n=1). There were no treatment-related deaths. ![]()
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for the anti-PD-1 therapy pembrolizumab (KEYTRUDA).
With this sBLA, Merck is seeking approval for pembrolizumab to treat adult and pediatric patients with refractory primary mediastinal B-cell lymphoma (PMBCL) or patients with PMBCL who have relapsed after 2 or more prior lines of therapy.
The FDA expects to make a decision on the sBLA by April 3, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, microsatellite instability-high cancer, and gastric cancer.
The sBLA for pembrolizumab as a treatment for PMBCL is supported by the phase 2 KEYNOTE-170 trial. Results from this trial were presented at the 2017 ASH Annual Meeting (abstract 2833).
KEYNOTE-170 is an ongoing study in which researchers are evaluating pembrolizumab (given at a 200 mg fixed dose every 3 weeks) in patients with relapsed/refractory PMBCL or relapsed/refractory Richter syndrome.
The PMBCL cohort enrolled patients who relapsed after autologous stem cell transplant (ASCT), were refractory to ASCT, or were ineligible for ASCT. Patients ineligible for ASCT had to have received 2 or more lines of prior therapy.
The median duration of follow-up was 10.5 months (range, 0.1-17.7).
In the efficacy population (n=29), the overall response rate was 41% (n=12), and the complete response rate was 24% (n=7).
The median time to response was 2.8 months (range, 2.4-5.5), and the median duration of response was not reached (range, 1.1+ to 13.6+ months).
Of the 53 patients evaluated for safety, 57% (n=30) experienced treatment-related adverse events (TRAEs), including 21% (n=11) who experienced grade 3-4 TRAEs.
The most common TRAEs (occurring in at least 5% of patients) were neutropenia (n=11), hypothyroidism (n=4), asthenia (n=3), and pyrexia (n=3).
Immune-mediated adverse events of all grades occurred in 11% (n=6) of patients. These include hypothyroidism (n=4), hyperthyroidism (n=2), pneumonitis (n=1), and thyroiditis (n=1). There were no treatment-related deaths. ![]()
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for the anti-PD-1 therapy pembrolizumab (KEYTRUDA).
With this sBLA, Merck is seeking approval for pembrolizumab to treat adult and pediatric patients with refractory primary mediastinal B-cell lymphoma (PMBCL) or patients with PMBCL who have relapsed after 2 or more prior lines of therapy.
The FDA expects to make a decision on the sBLA by April 3, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, microsatellite instability-high cancer, and gastric cancer.
The sBLA for pembrolizumab as a treatment for PMBCL is supported by the phase 2 KEYNOTE-170 trial. Results from this trial were presented at the 2017 ASH Annual Meeting (abstract 2833).
KEYNOTE-170 is an ongoing study in which researchers are evaluating pembrolizumab (given at a 200 mg fixed dose every 3 weeks) in patients with relapsed/refractory PMBCL or relapsed/refractory Richter syndrome.
The PMBCL cohort enrolled patients who relapsed after autologous stem cell transplant (ASCT), were refractory to ASCT, or were ineligible for ASCT. Patients ineligible for ASCT had to have received 2 or more lines of prior therapy.
The median duration of follow-up was 10.5 months (range, 0.1-17.7).
In the efficacy population (n=29), the overall response rate was 41% (n=12), and the complete response rate was 24% (n=7).
The median time to response was 2.8 months (range, 2.4-5.5), and the median duration of response was not reached (range, 1.1+ to 13.6+ months).
Of the 53 patients evaluated for safety, 57% (n=30) experienced treatment-related adverse events (TRAEs), including 21% (n=11) who experienced grade 3-4 TRAEs.
The most common TRAEs (occurring in at least 5% of patients) were neutropenia (n=11), hypothyroidism (n=4), asthenia (n=3), and pyrexia (n=3).
Immune-mediated adverse events of all grades occurred in 11% (n=6) of patients. These include hypothyroidism (n=4), hyperthyroidism (n=2), pneumonitis (n=1), and thyroiditis (n=1). There were no treatment-related deaths. ![]()
*Data in the abstract differ from the presentation.
Technique may be effective for diagnosing NHL
Preclinical research suggests infrared spectroscopy could be used to diagnose non-Hodgkin lymphoma (NHL).
Researchers used mid-infrared spectroscopy to analyze blood serum derived from mice and differentiate mice with NHL and subcutaneous melanoma from each other and from healthy control mice.
The findings suggest infrared spectroscopy can detect biochemical changes induced by NHL and melanoma and therefore has diagnostic potential as a screening technique for these cancers.
A.G. Unil Perera, PhD, of Georgia State University in Atlanta, and his colleagues detailed these findings in Scientific Reports.
The researchers said that Fourier Transform Infrared (FTIR) spectroscopy in Attenuated Total Reflection (ATR) sampling mode provides high-quality results with better reproducibility compared to other vibrational spectroscopy.
With previous work, Dr Perera and his colleagues discovered that a blood test for ulcerative colitis using ATR-FTIR spectroscopy could provide a cheaper, less invasive alternative for screening compared to colonoscopy.
In the current study, the researchers tested ATR-FTIR spectroscopy in mouse models of malignancy—EL4 NHL and B16 subcutaneous melanoma.
The team extracted blood serum from these mice and control mice. Droplets of serum were placed on an ATR crystal of the FTIR instrument.
Incident infrared beams were absorbed and reflected by the serum, creating a wave that was recorded and used to produce an absorbance curve with peaks that identified the presence of certain biomarkers in the sample.
The researchers compared the absorbance curves from the control and cancer mice and assessed biochemical changes induced by NHL and melanoma.
The team found “remarkable” differences between the ATR-FTIR spectra of serum samples from tumor-bearing mice and control mice.
Dr Perera said these findings are applicable to humans because mice and humans have some biomarkers and chemicals in common.
Using the data collected on the biomarkers for NHL and melanoma, the researchers could develop detectors for these particular absorbance peaks, which doctors could use to test patients’ blood samples for these cancers.
“Our final goal is to say we can use this infrared technique to identify various diseases,” Dr Perera said. “This study shows infrared spectroscopy can identify cancer. Right now, when you go to the doctor, they do blood tests for sugar and several other things but not for serious diseases like cancer and colitis.”
“One day, we hope that even these serious diseases can be rapidly screened. Your primary doctor could keep a record of your number and check that every time you come back. Then, if there is some indication of cancer or colitis, they can do biopsies, colonoscopies, etc.” ![]()
Preclinical research suggests infrared spectroscopy could be used to diagnose non-Hodgkin lymphoma (NHL).
Researchers used mid-infrared spectroscopy to analyze blood serum derived from mice and differentiate mice with NHL and subcutaneous melanoma from each other and from healthy control mice.
The findings suggest infrared spectroscopy can detect biochemical changes induced by NHL and melanoma and therefore has diagnostic potential as a screening technique for these cancers.
A.G. Unil Perera, PhD, of Georgia State University in Atlanta, and his colleagues detailed these findings in Scientific Reports.
The researchers said that Fourier Transform Infrared (FTIR) spectroscopy in Attenuated Total Reflection (ATR) sampling mode provides high-quality results with better reproducibility compared to other vibrational spectroscopy.
With previous work, Dr Perera and his colleagues discovered that a blood test for ulcerative colitis using ATR-FTIR spectroscopy could provide a cheaper, less invasive alternative for screening compared to colonoscopy.
In the current study, the researchers tested ATR-FTIR spectroscopy in mouse models of malignancy—EL4 NHL and B16 subcutaneous melanoma.
The team extracted blood serum from these mice and control mice. Droplets of serum were placed on an ATR crystal of the FTIR instrument.
Incident infrared beams were absorbed and reflected by the serum, creating a wave that was recorded and used to produce an absorbance curve with peaks that identified the presence of certain biomarkers in the sample.
The researchers compared the absorbance curves from the control and cancer mice and assessed biochemical changes induced by NHL and melanoma.
The team found “remarkable” differences between the ATR-FTIR spectra of serum samples from tumor-bearing mice and control mice.
Dr Perera said these findings are applicable to humans because mice and humans have some biomarkers and chemicals in common.
Using the data collected on the biomarkers for NHL and melanoma, the researchers could develop detectors for these particular absorbance peaks, which doctors could use to test patients’ blood samples for these cancers.
“Our final goal is to say we can use this infrared technique to identify various diseases,” Dr Perera said. “This study shows infrared spectroscopy can identify cancer. Right now, when you go to the doctor, they do blood tests for sugar and several other things but not for serious diseases like cancer and colitis.”
“One day, we hope that even these serious diseases can be rapidly screened. Your primary doctor could keep a record of your number and check that every time you come back. Then, if there is some indication of cancer or colitis, they can do biopsies, colonoscopies, etc.” ![]()
Preclinical research suggests infrared spectroscopy could be used to diagnose non-Hodgkin lymphoma (NHL).
Researchers used mid-infrared spectroscopy to analyze blood serum derived from mice and differentiate mice with NHL and subcutaneous melanoma from each other and from healthy control mice.
The findings suggest infrared spectroscopy can detect biochemical changes induced by NHL and melanoma and therefore has diagnostic potential as a screening technique for these cancers.
A.G. Unil Perera, PhD, of Georgia State University in Atlanta, and his colleagues detailed these findings in Scientific Reports.
The researchers said that Fourier Transform Infrared (FTIR) spectroscopy in Attenuated Total Reflection (ATR) sampling mode provides high-quality results with better reproducibility compared to other vibrational spectroscopy.
With previous work, Dr Perera and his colleagues discovered that a blood test for ulcerative colitis using ATR-FTIR spectroscopy could provide a cheaper, less invasive alternative for screening compared to colonoscopy.
In the current study, the researchers tested ATR-FTIR spectroscopy in mouse models of malignancy—EL4 NHL and B16 subcutaneous melanoma.
The team extracted blood serum from these mice and control mice. Droplets of serum were placed on an ATR crystal of the FTIR instrument.
Incident infrared beams were absorbed and reflected by the serum, creating a wave that was recorded and used to produce an absorbance curve with peaks that identified the presence of certain biomarkers in the sample.
The researchers compared the absorbance curves from the control and cancer mice and assessed biochemical changes induced by NHL and melanoma.
The team found “remarkable” differences between the ATR-FTIR spectra of serum samples from tumor-bearing mice and control mice.
Dr Perera said these findings are applicable to humans because mice and humans have some biomarkers and chemicals in common.
Using the data collected on the biomarkers for NHL and melanoma, the researchers could develop detectors for these particular absorbance peaks, which doctors could use to test patients’ blood samples for these cancers.
“Our final goal is to say we can use this infrared technique to identify various diseases,” Dr Perera said. “This study shows infrared spectroscopy can identify cancer. Right now, when you go to the doctor, they do blood tests for sugar and several other things but not for serious diseases like cancer and colitis.”
“One day, we hope that even these serious diseases can be rapidly screened. Your primary doctor could keep a record of your number and check that every time you come back. Then, if there is some indication of cancer or colitis, they can do biopsies, colonoscopies, etc.” ![]()
Combo prolongs survival in lymphoma models
Combination treatment with 2 monoclonal antibodies (mAbs) has demonstrated preclinical efficacy against B-cell lymphomas, according to researchers.
The investigators tested different combinations of mAbs to see how they interact with each other and what effect this has on how the immune system fights cancer.
One combination—an anti-CD27 mAb and anti-CD20 mAb—greatly increased survival in mouse models of B-cell lymphoma.
The researchers reported these results in Cancer Cell.
“By combining 2 specific antibodies—anti-CD27 and anti-CD20—we’ve increased the ability of the immune system to destroy cancer cells,” said study author Sean Lim, MBChB, PhD, of the University of Southampton in the UK.
“It’s very exciting to see that this drug combination has an impact on survival of mice with lymphoma, as improvements in treatment are urgently needed. The next stage will be to see if what we’ve discovered can be replicated in patients.”
For this study, Dr Lim and her colleagues tested combinations of tumor-targeting mAbs and immunomodulatory mAbs. The group found that an anti-CD27 mAb enhanced anti-CD20 therapy in various preclinical models.
The investigators first tested anti-CD20 and anti-CD27 (both alone and in combination) in the murine B-cell lymphoma model BCL1.
All control BCL1 mice had died by 30 days from baseline, all mice that received anti-CD20 alone died by day 40, and 30% of mice that received anti-CD27 alone were still alive past 100 days.
In contrast, 100% of mice that received anti-CD20 and anti-CD27 in combination were still alive and lymphoma-free past the 100-day mark.
The researchers also tested the mAbs in the A31 B-cell lymphoma model and the Eµ-TCL1 B-chronic lymphocytic leukemia model.
Results were similar to those observed with the BCL1 model. The combination of anti-CD20 and anti-CD27 significantly improved survival in A31 and Eµ-TCL1 mice, with all mice that received this combination surviving past 100 days.
As far as mechanisms of action, the investigators noted that anti-CD20 binds to B cells and mediates antibody-dependent cellular phagocytosis of the mAb-opsonized cells.
The researchers said the addition of anti-CD27 stimulates CD8+ T cells and natural killer cells, which induces the release of CCL3, CCL4, and CCL5, and this potentially attracts myeloid cells.
In addition, anti-CD27 (via the stimulation of CD8+ T and natural killer cells) induces the release of interferon gamma, which activates macrophages to express more Fc gamma receptor IV and promotes their inflammatory capacity. This increases the number of macrophages available for antibody-dependent cellular phagocytosis as well as the cells’ phagocytic ability.
Based on these findings, researchers are now conducting a phase 2 trial to test the anti-CD20 mAb rituximab and the anti-CD27 mAb varililumab in patients with relapsed and/or refractory B-cell non-Hodgkin lymphoma. ![]()
Combination treatment with 2 monoclonal antibodies (mAbs) has demonstrated preclinical efficacy against B-cell lymphomas, according to researchers.
The investigators tested different combinations of mAbs to see how they interact with each other and what effect this has on how the immune system fights cancer.
One combination—an anti-CD27 mAb and anti-CD20 mAb—greatly increased survival in mouse models of B-cell lymphoma.
The researchers reported these results in Cancer Cell.
“By combining 2 specific antibodies—anti-CD27 and anti-CD20—we’ve increased the ability of the immune system to destroy cancer cells,” said study author Sean Lim, MBChB, PhD, of the University of Southampton in the UK.
“It’s very exciting to see that this drug combination has an impact on survival of mice with lymphoma, as improvements in treatment are urgently needed. The next stage will be to see if what we’ve discovered can be replicated in patients.”
For this study, Dr Lim and her colleagues tested combinations of tumor-targeting mAbs and immunomodulatory mAbs. The group found that an anti-CD27 mAb enhanced anti-CD20 therapy in various preclinical models.
The investigators first tested anti-CD20 and anti-CD27 (both alone and in combination) in the murine B-cell lymphoma model BCL1.
All control BCL1 mice had died by 30 days from baseline, all mice that received anti-CD20 alone died by day 40, and 30% of mice that received anti-CD27 alone were still alive past 100 days.
In contrast, 100% of mice that received anti-CD20 and anti-CD27 in combination were still alive and lymphoma-free past the 100-day mark.
The researchers also tested the mAbs in the A31 B-cell lymphoma model and the Eµ-TCL1 B-chronic lymphocytic leukemia model.
Results were similar to those observed with the BCL1 model. The combination of anti-CD20 and anti-CD27 significantly improved survival in A31 and Eµ-TCL1 mice, with all mice that received this combination surviving past 100 days.
As far as mechanisms of action, the investigators noted that anti-CD20 binds to B cells and mediates antibody-dependent cellular phagocytosis of the mAb-opsonized cells.
The researchers said the addition of anti-CD27 stimulates CD8+ T cells and natural killer cells, which induces the release of CCL3, CCL4, and CCL5, and this potentially attracts myeloid cells.
In addition, anti-CD27 (via the stimulation of CD8+ T and natural killer cells) induces the release of interferon gamma, which activates macrophages to express more Fc gamma receptor IV and promotes their inflammatory capacity. This increases the number of macrophages available for antibody-dependent cellular phagocytosis as well as the cells’ phagocytic ability.
Based on these findings, researchers are now conducting a phase 2 trial to test the anti-CD20 mAb rituximab and the anti-CD27 mAb varililumab in patients with relapsed and/or refractory B-cell non-Hodgkin lymphoma. ![]()
Combination treatment with 2 monoclonal antibodies (mAbs) has demonstrated preclinical efficacy against B-cell lymphomas, according to researchers.
The investigators tested different combinations of mAbs to see how they interact with each other and what effect this has on how the immune system fights cancer.
One combination—an anti-CD27 mAb and anti-CD20 mAb—greatly increased survival in mouse models of B-cell lymphoma.
The researchers reported these results in Cancer Cell.
“By combining 2 specific antibodies—anti-CD27 and anti-CD20—we’ve increased the ability of the immune system to destroy cancer cells,” said study author Sean Lim, MBChB, PhD, of the University of Southampton in the UK.
“It’s very exciting to see that this drug combination has an impact on survival of mice with lymphoma, as improvements in treatment are urgently needed. The next stage will be to see if what we’ve discovered can be replicated in patients.”
For this study, Dr Lim and her colleagues tested combinations of tumor-targeting mAbs and immunomodulatory mAbs. The group found that an anti-CD27 mAb enhanced anti-CD20 therapy in various preclinical models.
The investigators first tested anti-CD20 and anti-CD27 (both alone and in combination) in the murine B-cell lymphoma model BCL1.
All control BCL1 mice had died by 30 days from baseline, all mice that received anti-CD20 alone died by day 40, and 30% of mice that received anti-CD27 alone were still alive past 100 days.
In contrast, 100% of mice that received anti-CD20 and anti-CD27 in combination were still alive and lymphoma-free past the 100-day mark.
The researchers also tested the mAbs in the A31 B-cell lymphoma model and the Eµ-TCL1 B-chronic lymphocytic leukemia model.
Results were similar to those observed with the BCL1 model. The combination of anti-CD20 and anti-CD27 significantly improved survival in A31 and Eµ-TCL1 mice, with all mice that received this combination surviving past 100 days.
As far as mechanisms of action, the investigators noted that anti-CD20 binds to B cells and mediates antibody-dependent cellular phagocytosis of the mAb-opsonized cells.
The researchers said the addition of anti-CD27 stimulates CD8+ T cells and natural killer cells, which induces the release of CCL3, CCL4, and CCL5, and this potentially attracts myeloid cells.
In addition, anti-CD27 (via the stimulation of CD8+ T and natural killer cells) induces the release of interferon gamma, which activates macrophages to express more Fc gamma receptor IV and promotes their inflammatory capacity. This increases the number of macrophages available for antibody-dependent cellular phagocytosis as well as the cells’ phagocytic ability.
Based on these findings, researchers are now conducting a phase 2 trial to test the anti-CD20 mAb rituximab and the anti-CD27 mAb varililumab in patients with relapsed and/or refractory B-cell non-Hodgkin lymphoma. ![]()
Inhibitor exhibits activity against range of lymphomas
Preclinical research suggests the dual PI3K/mTOR inhibitor PQR309 has activity against several types of lymphoma and works well in combination with other agents.
PQR309 exhibited anti-lymphoma activity as a single agent and in combination with venetoclax, panobinostat, ibrutinib, lenalidomide, ARV-825, marizomib, and rituximab.
PQR309 demonstrated greater activity against B-cell lymphoma than T-cell lymphoma, and the inhibitor was able to overcome both primary and acquired resistance to idelalisib.
Francesco Bertoni, MD, of the Institute of Oncology Research in Bellinzona, Switzerland, and his colleagues conducted this research and reported the results in Clinical Cancer Research.
The work was funded by PIQUR Therapeutics AG, the company developing PQR309, and some study authors are PIQUR employees.
The researchers tested PQR309 in 49 human lymphoma cell lines—7 activated B-cell-like (ABC) diffuse large B-cell lymphoma (DLBCL), 18 germinal center B-cell (GCB) DLBCL, 10 mantle cell lymphoma (MCL), 3 splenic marginal zone lymphoma (SMZL), 2 chronic lymphocytic leukemia (CLL), 4 Hodgkin lymphoma, and 5 anaplastic large-cell lymphoma (ALCL).
In most cell lines, PQR309 halted proliferation, mainly due to cell-cycle arrest with a block in G1. However, PQR309 induced apoptosis in 2 cell lines tested—SU-DHL-4 and TMD8.
The researchers noted that PQR309 was significantly more active in the B-cell lymphoma cell lines (DLBCL, MCL, CLL, and SMZL) than in the T-cell lymphoma cell line ALCL (P=0.028).
PQR309 exhibited similar activity in ABC and GCB DLBCL cell lines, de novo DLBCL, and DLBCL derived from transformed follicular lymphoma. TP53, MYC, and BCL2 status also had no significant effect on PQR309 activity.
The researchers compared cell lines that were very sensitive to PQR309 to those with low sensitivity to the drug and identified differences.
The team said that transcripts preferentially expressed in PQR309-sensitive cell lines were significantly enriched of genes involved in BCR pathway/signaling and BLIMP1 targets. Transcripts associated with less sensitive cell lines were enriched of members of proteasome pathway, response to unfolded proteins, MYC targets, XBP1 targets, genes downregulated by mTOR inhibitors, and genes involved in oxidative phosphorylation.
PQR309 demonstrated synergistic effects when combined with the BTK inhibitor ibrutinib, the immunomodulatory drug lenalidomide, the anti-CD20 monoclonal antibody rituximab, and the proteasome inhibitor marizomib.
PQR309 demonstrated synergistic or additive effects when combined with the BCL2 inhibitor venetoclax, the HDAC inhibitor panobinostat, and the PROTAC BET inhibitor ARV-825.
In addition, PQR309 was active in lymphoma cell lines with primary and secondary resistance to the PI3K inhibitor idelalisib.
The researchers believe the results of this study, together with ongoing clinical studies of PQR309, can lead to better treatments for lymphoma patients and better understanding of the mechanisms of anti-lymphoma agents. ![]()
Preclinical research suggests the dual PI3K/mTOR inhibitor PQR309 has activity against several types of lymphoma and works well in combination with other agents.
PQR309 exhibited anti-lymphoma activity as a single agent and in combination with venetoclax, panobinostat, ibrutinib, lenalidomide, ARV-825, marizomib, and rituximab.
PQR309 demonstrated greater activity against B-cell lymphoma than T-cell lymphoma, and the inhibitor was able to overcome both primary and acquired resistance to idelalisib.
Francesco Bertoni, MD, of the Institute of Oncology Research in Bellinzona, Switzerland, and his colleagues conducted this research and reported the results in Clinical Cancer Research.
The work was funded by PIQUR Therapeutics AG, the company developing PQR309, and some study authors are PIQUR employees.
The researchers tested PQR309 in 49 human lymphoma cell lines—7 activated B-cell-like (ABC) diffuse large B-cell lymphoma (DLBCL), 18 germinal center B-cell (GCB) DLBCL, 10 mantle cell lymphoma (MCL), 3 splenic marginal zone lymphoma (SMZL), 2 chronic lymphocytic leukemia (CLL), 4 Hodgkin lymphoma, and 5 anaplastic large-cell lymphoma (ALCL).
In most cell lines, PQR309 halted proliferation, mainly due to cell-cycle arrest with a block in G1. However, PQR309 induced apoptosis in 2 cell lines tested—SU-DHL-4 and TMD8.
The researchers noted that PQR309 was significantly more active in the B-cell lymphoma cell lines (DLBCL, MCL, CLL, and SMZL) than in the T-cell lymphoma cell line ALCL (P=0.028).
PQR309 exhibited similar activity in ABC and GCB DLBCL cell lines, de novo DLBCL, and DLBCL derived from transformed follicular lymphoma. TP53, MYC, and BCL2 status also had no significant effect on PQR309 activity.
The researchers compared cell lines that were very sensitive to PQR309 to those with low sensitivity to the drug and identified differences.
The team said that transcripts preferentially expressed in PQR309-sensitive cell lines were significantly enriched of genes involved in BCR pathway/signaling and BLIMP1 targets. Transcripts associated with less sensitive cell lines were enriched of members of proteasome pathway, response to unfolded proteins, MYC targets, XBP1 targets, genes downregulated by mTOR inhibitors, and genes involved in oxidative phosphorylation.
PQR309 demonstrated synergistic effects when combined with the BTK inhibitor ibrutinib, the immunomodulatory drug lenalidomide, the anti-CD20 monoclonal antibody rituximab, and the proteasome inhibitor marizomib.
PQR309 demonstrated synergistic or additive effects when combined with the BCL2 inhibitor venetoclax, the HDAC inhibitor panobinostat, and the PROTAC BET inhibitor ARV-825.
In addition, PQR309 was active in lymphoma cell lines with primary and secondary resistance to the PI3K inhibitor idelalisib.
The researchers believe the results of this study, together with ongoing clinical studies of PQR309, can lead to better treatments for lymphoma patients and better understanding of the mechanisms of anti-lymphoma agents. ![]()
Preclinical research suggests the dual PI3K/mTOR inhibitor PQR309 has activity against several types of lymphoma and works well in combination with other agents.
PQR309 exhibited anti-lymphoma activity as a single agent and in combination with venetoclax, panobinostat, ibrutinib, lenalidomide, ARV-825, marizomib, and rituximab.
PQR309 demonstrated greater activity against B-cell lymphoma than T-cell lymphoma, and the inhibitor was able to overcome both primary and acquired resistance to idelalisib.
Francesco Bertoni, MD, of the Institute of Oncology Research in Bellinzona, Switzerland, and his colleagues conducted this research and reported the results in Clinical Cancer Research.
The work was funded by PIQUR Therapeutics AG, the company developing PQR309, and some study authors are PIQUR employees.
The researchers tested PQR309 in 49 human lymphoma cell lines—7 activated B-cell-like (ABC) diffuse large B-cell lymphoma (DLBCL), 18 germinal center B-cell (GCB) DLBCL, 10 mantle cell lymphoma (MCL), 3 splenic marginal zone lymphoma (SMZL), 2 chronic lymphocytic leukemia (CLL), 4 Hodgkin lymphoma, and 5 anaplastic large-cell lymphoma (ALCL).
In most cell lines, PQR309 halted proliferation, mainly due to cell-cycle arrest with a block in G1. However, PQR309 induced apoptosis in 2 cell lines tested—SU-DHL-4 and TMD8.
The researchers noted that PQR309 was significantly more active in the B-cell lymphoma cell lines (DLBCL, MCL, CLL, and SMZL) than in the T-cell lymphoma cell line ALCL (P=0.028).
PQR309 exhibited similar activity in ABC and GCB DLBCL cell lines, de novo DLBCL, and DLBCL derived from transformed follicular lymphoma. TP53, MYC, and BCL2 status also had no significant effect on PQR309 activity.
The researchers compared cell lines that were very sensitive to PQR309 to those with low sensitivity to the drug and identified differences.
The team said that transcripts preferentially expressed in PQR309-sensitive cell lines were significantly enriched of genes involved in BCR pathway/signaling and BLIMP1 targets. Transcripts associated with less sensitive cell lines were enriched of members of proteasome pathway, response to unfolded proteins, MYC targets, XBP1 targets, genes downregulated by mTOR inhibitors, and genes involved in oxidative phosphorylation.
PQR309 demonstrated synergistic effects when combined with the BTK inhibitor ibrutinib, the immunomodulatory drug lenalidomide, the anti-CD20 monoclonal antibody rituximab, and the proteasome inhibitor marizomib.
PQR309 demonstrated synergistic or additive effects when combined with the BCL2 inhibitor venetoclax, the HDAC inhibitor panobinostat, and the PROTAC BET inhibitor ARV-825.
In addition, PQR309 was active in lymphoma cell lines with primary and secondary resistance to the PI3K inhibitor idelalisib.
The researchers believe the results of this study, together with ongoing clinical studies of PQR309, can lead to better treatments for lymphoma patients and better understanding of the mechanisms of anti-lymphoma agents.
Mogamulizumab BLA receives priority review
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for mogamulizumab.
Mogamulizumab is a humanized monoclonal antibody directed against CCR4 that is being developed by Kyowa Hakko Kirin Co., Ltd.
The company is seeking FDA approval for mogamulizumab as a treatment for patients with cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
The FDA expects to make a decision on the BLA by June 4, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The BLA for mogamulizumab is supported by data from the MAVORIC study, the largest global randomized clinical trial of systemic therapy in CTCL.
MAVORIC is a phase 3 trial in which researchers evaluated mogamulizumab and an active comparator in 372 patients with CTCL who had failed at least 1 prior systemic treatment. The study was conducted in the US, Europe, Japan, and Australia.
Results from this trial are scheduled to be presented at the 2017 ASH Annual Meeting (abstract 817).
The FDA previously granted mogamulizumab breakthrough therapy designation as a treatment for CTCL patients who have received at least 1 prior systemic therapy.
Breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for mogamulizumab.
Mogamulizumab is a humanized monoclonal antibody directed against CCR4 that is being developed by Kyowa Hakko Kirin Co., Ltd.
The company is seeking FDA approval for mogamulizumab as a treatment for patients with cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
The FDA expects to make a decision on the BLA by June 4, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The BLA for mogamulizumab is supported by data from the MAVORIC study, the largest global randomized clinical trial of systemic therapy in CTCL.
MAVORIC is a phase 3 trial in which researchers evaluated mogamulizumab and an active comparator in 372 patients with CTCL who had failed at least 1 prior systemic treatment. The study was conducted in the US, Europe, Japan, and Australia.
Results from this trial are scheduled to be presented at the 2017 ASH Annual Meeting (abstract 817).
The FDA previously granted mogamulizumab breakthrough therapy designation as a treatment for CTCL patients who have received at least 1 prior systemic therapy.
Breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for mogamulizumab.
Mogamulizumab is a humanized monoclonal antibody directed against CCR4 that is being developed by Kyowa Hakko Kirin Co., Ltd.
The company is seeking FDA approval for mogamulizumab as a treatment for patients with cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
The FDA expects to make a decision on the BLA by June 4, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The BLA for mogamulizumab is supported by data from the MAVORIC study, the largest global randomized clinical trial of systemic therapy in CTCL.
MAVORIC is a phase 3 trial in which researchers evaluated mogamulizumab and an active comparator in 372 patients with CTCL who had failed at least 1 prior systemic treatment. The study was conducted in the US, Europe, Japan, and Australia.
Results from this trial are scheduled to be presented at the 2017 ASH Annual Meeting (abstract 817).
The FDA previously granted mogamulizumab breakthrough therapy designation as a treatment for CTCL patients who have received at least 1 prior systemic therapy.
Breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
How CLL patients weigh treatment efficacy, safety, and cost
New research suggests patients with chronic lymphocytic leukemia (CLL) are willing to trade treatment efficacy for a reduced risk of side effects, but the cost of treatment may trump other factors.
The patients studied placed the highest value on treatments that deliver the longest progression-free survival (PFS), but the patients were also willing to swap some efficacy for a reduced risk of serious adverse events (AEs).
Study results also indicated that factoring out-of-pocket costs into the decision-making process can significantly influence a patient’s choice of treatment.
Carol Mansfield, PhD, of RTI Health Solutions in Research Triangle Park, North Carolina, and her colleagues conducted this study and reported the results in Blood Advances. The study was supported by funding from Genentech, Inc., to RTI Health Solutions.
The researchers surveyed 384 patients with CLL. Patients were asked to choose between hypothetical treatment options, each of which was defined by 5 variable attributes—PFS, mode of administration, typical severity of diarrhea, chance of serious infection, and chance of organ damage.
The attribute patients ranked highest was a change in PFS from 10 months to 60 months. This was followed by a change in infection risk from 30% to 0%, a change in the risk of organ damage from 8% to 0%, a change in diarrhea from severe to none, and a change in the mode of administration from intravenous to oral.
On average, a gain in PFS of 35.9 months was needed for patients to accept a 30% risk of serious infection. A gain in PFS of 26.3 months was needed for patients to accept an 8% risk of organ damage.
A gain in PFS of 21.6 months was needed for patients to accept severe diarrhea. And a gain in PFS of 3.5 months was needed for patients to accept the change from a daily pill to intravenous administration for 6 months.
There were no significant differences in preferences among treatment-naïve patients, first-line patients, and relapsed/refractory patients.
Impact of cost
When the researchers conducted a supplemental cost analysis, they found that out-of-pocket cost had a substantial impact on treatment choice.
The cost analysis included 2 treatments—medicines A and B. Based on the prior analysis, the researchers predicted that 91% of patients would choose medicine B if cost were not a concern because B offered longer PFS than A.
“We used the results from the discrete-choice experiment to forecast the probability that a respondent would pick each hypothetical drug without any mention of cost and then compared that to the choices people made when out-of-pocket costs for these medicines were included,” Dr Mansfield explained.
Patients were asked to choose between medicines A and B under 2 circumstances in which B cost more than A.
When medicine B had a monthly out-of-pocket cost that was $75 more than medicine A, 50% of patients chose medicine A.
When medicine B had a monthly out-of-pocket cost that was $400 more than medicine A, 74% of patients chose medicine A.
“Cost is clearly something that has an impact,” Dr Mansfield said. “When patients get prescribed something they can’t afford, they have to make very difficult choices.”
Dr Mansfield and her colleagues believe their findings will help doctors and patients focus on treatments that account for a patient’s unique circumstances and goals.
“Patients don’t always know that they could be making these tradeoffs,” Dr Mansfield said. “We hope that our findings can help doctors to have frank discussions with their patients about the differences between treatments and how these might affect their lives.”
New research suggests patients with chronic lymphocytic leukemia (CLL) are willing to trade treatment efficacy for a reduced risk of side effects, but the cost of treatment may trump other factors.
The patients studied placed the highest value on treatments that deliver the longest progression-free survival (PFS), but the patients were also willing to swap some efficacy for a reduced risk of serious adverse events (AEs).
Study results also indicated that factoring out-of-pocket costs into the decision-making process can significantly influence a patient’s choice of treatment.
Carol Mansfield, PhD, of RTI Health Solutions in Research Triangle Park, North Carolina, and her colleagues conducted this study and reported the results in Blood Advances. The study was supported by funding from Genentech, Inc., to RTI Health Solutions.
The researchers surveyed 384 patients with CLL. Patients were asked to choose between hypothetical treatment options, each of which was defined by 5 variable attributes—PFS, mode of administration, typical severity of diarrhea, chance of serious infection, and chance of organ damage.
The attribute patients ranked highest was a change in PFS from 10 months to 60 months. This was followed by a change in infection risk from 30% to 0%, a change in the risk of organ damage from 8% to 0%, a change in diarrhea from severe to none, and a change in the mode of administration from intravenous to oral.
On average, a gain in PFS of 35.9 months was needed for patients to accept a 30% risk of serious infection. A gain in PFS of 26.3 months was needed for patients to accept an 8% risk of organ damage.
A gain in PFS of 21.6 months was needed for patients to accept severe diarrhea. And a gain in PFS of 3.5 months was needed for patients to accept the change from a daily pill to intravenous administration for 6 months.
There were no significant differences in preferences among treatment-naïve patients, first-line patients, and relapsed/refractory patients.
Impact of cost
When the researchers conducted a supplemental cost analysis, they found that out-of-pocket cost had a substantial impact on treatment choice.
The cost analysis included 2 treatments—medicines A and B. Based on the prior analysis, the researchers predicted that 91% of patients would choose medicine B if cost were not a concern because B offered longer PFS than A.
“We used the results from the discrete-choice experiment to forecast the probability that a respondent would pick each hypothetical drug without any mention of cost and then compared that to the choices people made when out-of-pocket costs for these medicines were included,” Dr Mansfield explained.
Patients were asked to choose between medicines A and B under 2 circumstances in which B cost more than A.
When medicine B had a monthly out-of-pocket cost that was $75 more than medicine A, 50% of patients chose medicine A.
When medicine B had a monthly out-of-pocket cost that was $400 more than medicine A, 74% of patients chose medicine A.
“Cost is clearly something that has an impact,” Dr Mansfield said. “When patients get prescribed something they can’t afford, they have to make very difficult choices.”
Dr Mansfield and her colleagues believe their findings will help doctors and patients focus on treatments that account for a patient’s unique circumstances and goals.
“Patients don’t always know that they could be making these tradeoffs,” Dr Mansfield said. “We hope that our findings can help doctors to have frank discussions with their patients about the differences between treatments and how these might affect their lives.”
New research suggests patients with chronic lymphocytic leukemia (CLL) are willing to trade treatment efficacy for a reduced risk of side effects, but the cost of treatment may trump other factors.
The patients studied placed the highest value on treatments that deliver the longest progression-free survival (PFS), but the patients were also willing to swap some efficacy for a reduced risk of serious adverse events (AEs).
Study results also indicated that factoring out-of-pocket costs into the decision-making process can significantly influence a patient’s choice of treatment.
Carol Mansfield, PhD, of RTI Health Solutions in Research Triangle Park, North Carolina, and her colleagues conducted this study and reported the results in Blood Advances. The study was supported by funding from Genentech, Inc., to RTI Health Solutions.
The researchers surveyed 384 patients with CLL. Patients were asked to choose between hypothetical treatment options, each of which was defined by 5 variable attributes—PFS, mode of administration, typical severity of diarrhea, chance of serious infection, and chance of organ damage.
The attribute patients ranked highest was a change in PFS from 10 months to 60 months. This was followed by a change in infection risk from 30% to 0%, a change in the risk of organ damage from 8% to 0%, a change in diarrhea from severe to none, and a change in the mode of administration from intravenous to oral.
On average, a gain in PFS of 35.9 months was needed for patients to accept a 30% risk of serious infection. A gain in PFS of 26.3 months was needed for patients to accept an 8% risk of organ damage.
A gain in PFS of 21.6 months was needed for patients to accept severe diarrhea. And a gain in PFS of 3.5 months was needed for patients to accept the change from a daily pill to intravenous administration for 6 months.
There were no significant differences in preferences among treatment-naïve patients, first-line patients, and relapsed/refractory patients.
Impact of cost
When the researchers conducted a supplemental cost analysis, they found that out-of-pocket cost had a substantial impact on treatment choice.
The cost analysis included 2 treatments—medicines A and B. Based on the prior analysis, the researchers predicted that 91% of patients would choose medicine B if cost were not a concern because B offered longer PFS than A.
“We used the results from the discrete-choice experiment to forecast the probability that a respondent would pick each hypothetical drug without any mention of cost and then compared that to the choices people made when out-of-pocket costs for these medicines were included,” Dr Mansfield explained.
Patients were asked to choose between medicines A and B under 2 circumstances in which B cost more than A.
When medicine B had a monthly out-of-pocket cost that was $75 more than medicine A, 50% of patients chose medicine A.
When medicine B had a monthly out-of-pocket cost that was $400 more than medicine A, 74% of patients chose medicine A.
“Cost is clearly something that has an impact,” Dr Mansfield said. “When patients get prescribed something they can’t afford, they have to make very difficult choices.”
Dr Mansfield and her colleagues believe their findings will help doctors and patients focus on treatments that account for a patient’s unique circumstances and goals.
“Patients don’t always know that they could be making these tradeoffs,” Dr Mansfield said. “We hope that our findings can help doctors to have frank discussions with their patients about the differences between treatments and how these might affect their lives.”
Review suggests low incidence of BIA-ALCL in Canada
Results of a safety review suggest there is a low incidence of breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) in Canada.
Health Canada undertook the review because of an increase in reporting of BIA-ALCL internationally.
The review showed that 5 confirmed cases of BIA-ALCL have been reported by Canadian manufacturers in the last 10 years.
This is equal to 1 case of BIA-ALCL per 77,190 implants sold, or 0.0013%.
However, Health Canada acknowledges that some cases may not have been reported to the manufacturers or Health Canada.
Available data suggest that BIA-ALCL is more frequently reported with textured surface implants than smooth surface implants. Textured surface implants account for a quarter of all breast implants sold in Canada.
Four of the 5 reported Canadian cases of BIA-ALCL involved textured implants. The surface type was not reported in the remaining case.
The rate of occurrence of BIA‑ALCL per textured implant sold in Canada is 1 case per 24,177 or 0.0041%.
As a result of its safety review, Health Canada is working with manufacturers to update the safety information on the product labeling for all breast implants.
The agency is also communicating this safety information to Canadians through the Recalls and Safety Alerts database on the Healthy Canadians website.
Health Canada continues to monitor the safety profile of breast implants through its post-market surveillance program.
The agency will also monitor cases of BIA-ALCL through an annual follow-up with manufacturers of breast implants.
Health Canada is recommending that healthcare professionals learn about the signs, symptoms, and testing steps to recognize and diagnose BIA‑ALCL.
In addition, healthcare professionals in Canada should report incidents of BIA-ALCL to Health Canada. These reports should include specific details, such as symptoms, how BIA-ALCL was discovered, the age of the patient at implantation, prior implant history, the age of the patient at discovery, tests conducted to diagnose BIA-ALCL, staging information, the course of therapy, and clinical outcomes.
Reports can be made by calling Health Canada at 1-866-234-2345. Alternatively, visit Health Canada’s webpage on Adverse Reaction Reporting for information on how to report online, by mail, or by fax.
Results of a safety review suggest there is a low incidence of breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) in Canada.
Health Canada undertook the review because of an increase in reporting of BIA-ALCL internationally.
The review showed that 5 confirmed cases of BIA-ALCL have been reported by Canadian manufacturers in the last 10 years.
This is equal to 1 case of BIA-ALCL per 77,190 implants sold, or 0.0013%.
However, Health Canada acknowledges that some cases may not have been reported to the manufacturers or Health Canada.
Available data suggest that BIA-ALCL is more frequently reported with textured surface implants than smooth surface implants. Textured surface implants account for a quarter of all breast implants sold in Canada.
Four of the 5 reported Canadian cases of BIA-ALCL involved textured implants. The surface type was not reported in the remaining case.
The rate of occurrence of BIA‑ALCL per textured implant sold in Canada is 1 case per 24,177 or 0.0041%.
As a result of its safety review, Health Canada is working with manufacturers to update the safety information on the product labeling for all breast implants.
The agency is also communicating this safety information to Canadians through the Recalls and Safety Alerts database on the Healthy Canadians website.
Health Canada continues to monitor the safety profile of breast implants through its post-market surveillance program.
The agency will also monitor cases of BIA-ALCL through an annual follow-up with manufacturers of breast implants.
Health Canada is recommending that healthcare professionals learn about the signs, symptoms, and testing steps to recognize and diagnose BIA‑ALCL.
In addition, healthcare professionals in Canada should report incidents of BIA-ALCL to Health Canada. These reports should include specific details, such as symptoms, how BIA-ALCL was discovered, the age of the patient at implantation, prior implant history, the age of the patient at discovery, tests conducted to diagnose BIA-ALCL, staging information, the course of therapy, and clinical outcomes.
Reports can be made by calling Health Canada at 1-866-234-2345. Alternatively, visit Health Canada’s webpage on Adverse Reaction Reporting for information on how to report online, by mail, or by fax.
Results of a safety review suggest there is a low incidence of breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) in Canada.
Health Canada undertook the review because of an increase in reporting of BIA-ALCL internationally.
The review showed that 5 confirmed cases of BIA-ALCL have been reported by Canadian manufacturers in the last 10 years.
This is equal to 1 case of BIA-ALCL per 77,190 implants sold, or 0.0013%.
However, Health Canada acknowledges that some cases may not have been reported to the manufacturers or Health Canada.
Available data suggest that BIA-ALCL is more frequently reported with textured surface implants than smooth surface implants. Textured surface implants account for a quarter of all breast implants sold in Canada.
Four of the 5 reported Canadian cases of BIA-ALCL involved textured implants. The surface type was not reported in the remaining case.
The rate of occurrence of BIA‑ALCL per textured implant sold in Canada is 1 case per 24,177 or 0.0041%.
As a result of its safety review, Health Canada is working with manufacturers to update the safety information on the product labeling for all breast implants.
The agency is also communicating this safety information to Canadians through the Recalls and Safety Alerts database on the Healthy Canadians website.
Health Canada continues to monitor the safety profile of breast implants through its post-market surveillance program.
The agency will also monitor cases of BIA-ALCL through an annual follow-up with manufacturers of breast implants.
Health Canada is recommending that healthcare professionals learn about the signs, symptoms, and testing steps to recognize and diagnose BIA‑ALCL.
In addition, healthcare professionals in Canada should report incidents of BIA-ALCL to Health Canada. These reports should include specific details, such as symptoms, how BIA-ALCL was discovered, the age of the patient at implantation, prior implant history, the age of the patient at discovery, tests conducted to diagnose BIA-ALCL, staging information, the course of therapy, and clinical outcomes.
Reports can be made by calling Health Canada at 1-866-234-2345. Alternatively, visit Health Canada’s webpage on Adverse Reaction Reporting for information on how to report online, by mail, or by fax.