User login
For MD-IQ on Family Practice News, but a regular topic for Rheumatology News
ACR: Ozone injections reduce pain and improve function in knee OA
SAN FRANCISCO – Intra-articular ozone injections were effective in reducing pain, improving function, and improving quality of life in patients with knee osteoarthritis in the first randomized study to evaluate this approach.
Patients treated with a series of ozone injections achieved significant improvements on all measures, except for the Timed Up and Go Test, compared with patients given placebo, according to study results presented at the annual meeting of the American College of Rheumatology.
“After 8 weeks of treatment, ozone can give patients with knee osteoarthritis [OA] better quality of life with less pain and more independence in performing daily activities. More studies are needed to validate this option in patients with OA. Intra-articular ozone injections are safe with similar complications to placebo. In elderly people with comorbidities requiring chronic medication, this approach is a good option because it doesn’t interact with medications. The only restriction is anticoagulant therapy, as there may be bleeding at the injection site,” said Dr. Virginia Trevisani, professor at the Federal University of São Paulo.
The next series of studies Dr. Trevisani and her coauthors are planning will incorporate MRI imaging to assess the effect of the ozone injections on structural progression in knee OA.
Ozone is thought to have anti-inflammatory effects by reducing oxidative stress. Ozone is being used for medical purposes in countries such as Russia, Germany, and Spain, but it is not currently used clinically in the United States. “You can’t perform these injections in patients without experience. The only requirement is a machine to make ozone that costs about $1,000 USD,” she said.
Before this study, evidence in support of ozone injections in knee OA was anecdotal and from observational studies. The present study is the first randomized trial to evaluate intra-articular ozone injections in patients with knee OA.
The study enrolled 98 patients with documented knee OA between the ages of 60 and 85 years; 63 patients were randomized to intra-articular injections of ozone in the knee with the most pain (one injection per week for 8 consecutive weeks), and 35 were randomized to placebo injections of a small amount of air.
Patients were evaluated at baseline, after 4 and 8 injections, and 8 weeks following the last injection. Two patients in the ozone group withdrew from the study. The only adverse events were three puncture-site wounds – two in the ozone group and one in the placebo group.
Significant improvement was observed on all measures, except for the Timed Up and Go Test (getting up from a chair), at every time point for the ozone injections. Dr. Trevisani said that the ability to get up from a chair without help depends on balance and muscle strength, which may explain why the results were not significant.
Measures of pain on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the visual analog scale improved significantly with ozone, compared with placebo, and by week 16, the P value was .000 for both measures. WOMAC joint stiffness intensity was significantly improved by ozone (P = .075 at week 4; P = .002 at week 8). Quality of life on the Short Form–36 for pain and functional capacity were significantly improved by ozone, compared with placebo (P = .000 at week 16 for both measures).
Dr. Trevisani said ozone injections may be able to delay the need for total joint replacement surgery, and that they are cost effective, compared with surgery and other pharmacologic treatments.
Dr. Trevisani had no relevant financial disclosures.
SAN FRANCISCO – Intra-articular ozone injections were effective in reducing pain, improving function, and improving quality of life in patients with knee osteoarthritis in the first randomized study to evaluate this approach.
Patients treated with a series of ozone injections achieved significant improvements on all measures, except for the Timed Up and Go Test, compared with patients given placebo, according to study results presented at the annual meeting of the American College of Rheumatology.
“After 8 weeks of treatment, ozone can give patients with knee osteoarthritis [OA] better quality of life with less pain and more independence in performing daily activities. More studies are needed to validate this option in patients with OA. Intra-articular ozone injections are safe with similar complications to placebo. In elderly people with comorbidities requiring chronic medication, this approach is a good option because it doesn’t interact with medications. The only restriction is anticoagulant therapy, as there may be bleeding at the injection site,” said Dr. Virginia Trevisani, professor at the Federal University of São Paulo.
The next series of studies Dr. Trevisani and her coauthors are planning will incorporate MRI imaging to assess the effect of the ozone injections on structural progression in knee OA.
Ozone is thought to have anti-inflammatory effects by reducing oxidative stress. Ozone is being used for medical purposes in countries such as Russia, Germany, and Spain, but it is not currently used clinically in the United States. “You can’t perform these injections in patients without experience. The only requirement is a machine to make ozone that costs about $1,000 USD,” she said.
Before this study, evidence in support of ozone injections in knee OA was anecdotal and from observational studies. The present study is the first randomized trial to evaluate intra-articular ozone injections in patients with knee OA.
The study enrolled 98 patients with documented knee OA between the ages of 60 and 85 years; 63 patients were randomized to intra-articular injections of ozone in the knee with the most pain (one injection per week for 8 consecutive weeks), and 35 were randomized to placebo injections of a small amount of air.
Patients were evaluated at baseline, after 4 and 8 injections, and 8 weeks following the last injection. Two patients in the ozone group withdrew from the study. The only adverse events were three puncture-site wounds – two in the ozone group and one in the placebo group.
Significant improvement was observed on all measures, except for the Timed Up and Go Test (getting up from a chair), at every time point for the ozone injections. Dr. Trevisani said that the ability to get up from a chair without help depends on balance and muscle strength, which may explain why the results were not significant.
Measures of pain on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the visual analog scale improved significantly with ozone, compared with placebo, and by week 16, the P value was .000 for both measures. WOMAC joint stiffness intensity was significantly improved by ozone (P = .075 at week 4; P = .002 at week 8). Quality of life on the Short Form–36 for pain and functional capacity were significantly improved by ozone, compared with placebo (P = .000 at week 16 for both measures).
Dr. Trevisani said ozone injections may be able to delay the need for total joint replacement surgery, and that they are cost effective, compared with surgery and other pharmacologic treatments.
Dr. Trevisani had no relevant financial disclosures.
SAN FRANCISCO – Intra-articular ozone injections were effective in reducing pain, improving function, and improving quality of life in patients with knee osteoarthritis in the first randomized study to evaluate this approach.
Patients treated with a series of ozone injections achieved significant improvements on all measures, except for the Timed Up and Go Test, compared with patients given placebo, according to study results presented at the annual meeting of the American College of Rheumatology.
“After 8 weeks of treatment, ozone can give patients with knee osteoarthritis [OA] better quality of life with less pain and more independence in performing daily activities. More studies are needed to validate this option in patients with OA. Intra-articular ozone injections are safe with similar complications to placebo. In elderly people with comorbidities requiring chronic medication, this approach is a good option because it doesn’t interact with medications. The only restriction is anticoagulant therapy, as there may be bleeding at the injection site,” said Dr. Virginia Trevisani, professor at the Federal University of São Paulo.
The next series of studies Dr. Trevisani and her coauthors are planning will incorporate MRI imaging to assess the effect of the ozone injections on structural progression in knee OA.
Ozone is thought to have anti-inflammatory effects by reducing oxidative stress. Ozone is being used for medical purposes in countries such as Russia, Germany, and Spain, but it is not currently used clinically in the United States. “You can’t perform these injections in patients without experience. The only requirement is a machine to make ozone that costs about $1,000 USD,” she said.
Before this study, evidence in support of ozone injections in knee OA was anecdotal and from observational studies. The present study is the first randomized trial to evaluate intra-articular ozone injections in patients with knee OA.
The study enrolled 98 patients with documented knee OA between the ages of 60 and 85 years; 63 patients were randomized to intra-articular injections of ozone in the knee with the most pain (one injection per week for 8 consecutive weeks), and 35 were randomized to placebo injections of a small amount of air.
Patients were evaluated at baseline, after 4 and 8 injections, and 8 weeks following the last injection. Two patients in the ozone group withdrew from the study. The only adverse events were three puncture-site wounds – two in the ozone group and one in the placebo group.
Significant improvement was observed on all measures, except for the Timed Up and Go Test (getting up from a chair), at every time point for the ozone injections. Dr. Trevisani said that the ability to get up from a chair without help depends on balance and muscle strength, which may explain why the results were not significant.
Measures of pain on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the visual analog scale improved significantly with ozone, compared with placebo, and by week 16, the P value was .000 for both measures. WOMAC joint stiffness intensity was significantly improved by ozone (P = .075 at week 4; P = .002 at week 8). Quality of life on the Short Form–36 for pain and functional capacity were significantly improved by ozone, compared with placebo (P = .000 at week 16 for both measures).
Dr. Trevisani said ozone injections may be able to delay the need for total joint replacement surgery, and that they are cost effective, compared with surgery and other pharmacologic treatments.
Dr. Trevisani had no relevant financial disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point:Intra-articular ozone injections reduce pain, improve function, and improve quality of life in patients with knee osteoarthritis.
Major finding: On all measures of pain, function, and quality of life, ozone injections were significantly superior to placebo.
Data source: A randomized, double-blind placebo-controlled trial of 98 patients with knee OA.
Disclosures: Dr. Trevisani had no relevant financial disclosures.
VIDEO: Chondroitin tops celecoxib in reducing knee OA structural progression
SAN FRANCISCO – Patients with symptomatic knee osteoarthritis who received pharmaceutical-grade chondroitin sulfate for 2 years lost about 20% less cartilage volume than did patients treated with celecoxib, according to a randomized, double-blind trial.
Improvements were limited to the medial tibiofemoral compartment, but even such modest structural effects can significantly decrease rates of total knee replacement over time, said lead investigator Dr. Jean-Pierre Pelletier, who presented the findings at the annual meeting of the American College of Rheumatology.
The 194 participants in the study received chondroitin sulfate, 1,200 mg a day, or celecoxib, 200 mg daily. Joint effusion and pain and function improved markedly in both groups, and they had similar rates of adverse events, said Dr. Pelletier, who is a rheumatologist at Institut de recherche en rhumatologie de Montréal. He discussed the findings and plans for future research in an exclusive video interview.
Bioibérica sponsored the study and makes the chondroitin sulfate that participants received. Dr. Pelletier and his associates had no other disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Patients with symptomatic knee osteoarthritis who received pharmaceutical-grade chondroitin sulfate for 2 years lost about 20% less cartilage volume than did patients treated with celecoxib, according to a randomized, double-blind trial.
Improvements were limited to the medial tibiofemoral compartment, but even such modest structural effects can significantly decrease rates of total knee replacement over time, said lead investigator Dr. Jean-Pierre Pelletier, who presented the findings at the annual meeting of the American College of Rheumatology.
The 194 participants in the study received chondroitin sulfate, 1,200 mg a day, or celecoxib, 200 mg daily. Joint effusion and pain and function improved markedly in both groups, and they had similar rates of adverse events, said Dr. Pelletier, who is a rheumatologist at Institut de recherche en rhumatologie de Montréal. He discussed the findings and plans for future research in an exclusive video interview.
Bioibérica sponsored the study and makes the chondroitin sulfate that participants received. Dr. Pelletier and his associates had no other disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Patients with symptomatic knee osteoarthritis who received pharmaceutical-grade chondroitin sulfate for 2 years lost about 20% less cartilage volume than did patients treated with celecoxib, according to a randomized, double-blind trial.
Improvements were limited to the medial tibiofemoral compartment, but even such modest structural effects can significantly decrease rates of total knee replacement over time, said lead investigator Dr. Jean-Pierre Pelletier, who presented the findings at the annual meeting of the American College of Rheumatology.
The 194 participants in the study received chondroitin sulfate, 1,200 mg a day, or celecoxib, 200 mg daily. Joint effusion and pain and function improved markedly in both groups, and they had similar rates of adverse events, said Dr. Pelletier, who is a rheumatologist at Institut de recherche en rhumatologie de Montréal. He discussed the findings and plans for future research in an exclusive video interview.
Bioibérica sponsored the study and makes the chondroitin sulfate that participants received. Dr. Pelletier and his associates had no other disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACR ANNUAL MEETING
Jury still out on cannabinoid therapy for rheumatic diseases
Only four short-term, randomized trials have addressed the safety, efficacy, and tolerability of cannabinoids for treating rheumatic diseases, and all have methodologic weaknesses and a high risk of bias, according to a qualitative review of data published since 1946.
“There is low-quality evidence suggesting that cannabinoids may be associated with improvements in pain and sleep quality in rheumatoid arthritis and fibromyalgia. Clinical positive effects for the studies assessed in this review must be balanced by the reported adverse events,” wrote Dr. Mary-Ann Fitzcharles of McGill University, Montreal, and her colleagues (Arthritis Care Res. 2015 Nov 9. doi: 10.1002/acr.22727).
The four randomized clinical trials, ranging in duration from 2 to 8 weeks, included one with 58 rheumatoid arthritis patients, two with a total of 71 fibromyalgia patients, and one with 74 osteoarthritis patients. Three trials met their respective primary endpoints and found a statistically significant effect of cannabinoids on pain (in two studies), sleep (in two studies), and improved quality of life (in one study). The investigators noted a high incidence (generally observed in 25%-50% of subjects) of mild to moderate side effects (dizziness, drowsiness, nausea, dry mouth) and many methodologic weaknesses in the evaluated data. The study that tested a fatty acid amide hydrolase inhibitor in osteoarthritis patients was stopped early due to futility. The other three completed studies were associated with an overall high risk of bias.
One of the two fibromyalgia studies was a randomized, double-blind, placebo-controlled trial conducted in 2008 that assessed nabilone in 40 fibromyalgia patients. Nabilone treatment led to significant decreases in the visual analog scale for pain (–2.04, P less than .02) at 4 weeks. A second fibromyalgia trial from 2010 compared amitriptyline to nabilone in 31 subjects and found the latter agent to be superior on the primary endpoint of difference in score on the Insomnia Severity Index (difference = 3.2; 95% confidence interval, 1.2-5.3). A 2006 rheumatoid arthritis trial found that cannabis-based Sativex demonstrated a clinically meaningful advantage over placebo for the primary endpoint of morning pain on movement (difference of –0.95, 95% CI, –1.83 to –0.02; P = .044). No trials assessed herbal cannabis.
“It is not currently possible to recommend this category of treatments as therapy for patients with rheumatic diseases. Any conclusions based on these studies remain tenuous and call for larger, well controlled clinical trials to better understand potential benefits and risks as pertaining to rheumatic conditions,” Dr. Fitzcharles and her coauthors wrote.
No relevant financial disclosures were reported.
rhnews@frontlinemedcom.com
Only four short-term, randomized trials have addressed the safety, efficacy, and tolerability of cannabinoids for treating rheumatic diseases, and all have methodologic weaknesses and a high risk of bias, according to a qualitative review of data published since 1946.
“There is low-quality evidence suggesting that cannabinoids may be associated with improvements in pain and sleep quality in rheumatoid arthritis and fibromyalgia. Clinical positive effects for the studies assessed in this review must be balanced by the reported adverse events,” wrote Dr. Mary-Ann Fitzcharles of McGill University, Montreal, and her colleagues (Arthritis Care Res. 2015 Nov 9. doi: 10.1002/acr.22727).
The four randomized clinical trials, ranging in duration from 2 to 8 weeks, included one with 58 rheumatoid arthritis patients, two with a total of 71 fibromyalgia patients, and one with 74 osteoarthritis patients. Three trials met their respective primary endpoints and found a statistically significant effect of cannabinoids on pain (in two studies), sleep (in two studies), and improved quality of life (in one study). The investigators noted a high incidence (generally observed in 25%-50% of subjects) of mild to moderate side effects (dizziness, drowsiness, nausea, dry mouth) and many methodologic weaknesses in the evaluated data. The study that tested a fatty acid amide hydrolase inhibitor in osteoarthritis patients was stopped early due to futility. The other three completed studies were associated with an overall high risk of bias.
One of the two fibromyalgia studies was a randomized, double-blind, placebo-controlled trial conducted in 2008 that assessed nabilone in 40 fibromyalgia patients. Nabilone treatment led to significant decreases in the visual analog scale for pain (–2.04, P less than .02) at 4 weeks. A second fibromyalgia trial from 2010 compared amitriptyline to nabilone in 31 subjects and found the latter agent to be superior on the primary endpoint of difference in score on the Insomnia Severity Index (difference = 3.2; 95% confidence interval, 1.2-5.3). A 2006 rheumatoid arthritis trial found that cannabis-based Sativex demonstrated a clinically meaningful advantage over placebo for the primary endpoint of morning pain on movement (difference of –0.95, 95% CI, –1.83 to –0.02; P = .044). No trials assessed herbal cannabis.
“It is not currently possible to recommend this category of treatments as therapy for patients with rheumatic diseases. Any conclusions based on these studies remain tenuous and call for larger, well controlled clinical trials to better understand potential benefits and risks as pertaining to rheumatic conditions,” Dr. Fitzcharles and her coauthors wrote.
No relevant financial disclosures were reported.
rhnews@frontlinemedcom.com
Only four short-term, randomized trials have addressed the safety, efficacy, and tolerability of cannabinoids for treating rheumatic diseases, and all have methodologic weaknesses and a high risk of bias, according to a qualitative review of data published since 1946.
“There is low-quality evidence suggesting that cannabinoids may be associated with improvements in pain and sleep quality in rheumatoid arthritis and fibromyalgia. Clinical positive effects for the studies assessed in this review must be balanced by the reported adverse events,” wrote Dr. Mary-Ann Fitzcharles of McGill University, Montreal, and her colleagues (Arthritis Care Res. 2015 Nov 9. doi: 10.1002/acr.22727).
The four randomized clinical trials, ranging in duration from 2 to 8 weeks, included one with 58 rheumatoid arthritis patients, two with a total of 71 fibromyalgia patients, and one with 74 osteoarthritis patients. Three trials met their respective primary endpoints and found a statistically significant effect of cannabinoids on pain (in two studies), sleep (in two studies), and improved quality of life (in one study). The investigators noted a high incidence (generally observed in 25%-50% of subjects) of mild to moderate side effects (dizziness, drowsiness, nausea, dry mouth) and many methodologic weaknesses in the evaluated data. The study that tested a fatty acid amide hydrolase inhibitor in osteoarthritis patients was stopped early due to futility. The other three completed studies were associated with an overall high risk of bias.
One of the two fibromyalgia studies was a randomized, double-blind, placebo-controlled trial conducted in 2008 that assessed nabilone in 40 fibromyalgia patients. Nabilone treatment led to significant decreases in the visual analog scale for pain (–2.04, P less than .02) at 4 weeks. A second fibromyalgia trial from 2010 compared amitriptyline to nabilone in 31 subjects and found the latter agent to be superior on the primary endpoint of difference in score on the Insomnia Severity Index (difference = 3.2; 95% confidence interval, 1.2-5.3). A 2006 rheumatoid arthritis trial found that cannabis-based Sativex demonstrated a clinically meaningful advantage over placebo for the primary endpoint of morning pain on movement (difference of –0.95, 95% CI, –1.83 to –0.02; P = .044). No trials assessed herbal cannabis.
“It is not currently possible to recommend this category of treatments as therapy for patients with rheumatic diseases. Any conclusions based on these studies remain tenuous and call for larger, well controlled clinical trials to better understand potential benefits and risks as pertaining to rheumatic conditions,” Dr. Fitzcharles and her coauthors wrote.
No relevant financial disclosures were reported.
rhnews@frontlinemedcom.com
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: Currently, there is insufficient evidence to support cannabinoids as a therapeutic option in rheumatic disease.
Major finding: In two of four reviewed studies, cannabinoids demonstrated a statistically significant effect on pain associated with fibromyalgia and rheumatoid arthritis.
Data source: A qualitative review of four randomized, controlled trials involving 58 patients with rheumatoid arthritis, 71 with fibromyalgia, and 74 with osteoarthritis.
Disclosures: No relevant financial disclosures were reported.
ACR: No long-term benefit for knee OA steroid injections
Regular corticosteroid injections over 2 years were relatively safe for osteoarthritic knees in a trial from Tufts Medical Center in Boston, but they did not slow the progression of joint damage or improve patient outcomes.
The findings come at a time when the role of intra-articular steroid shots is up for debate. They are widely used for knee osteoarthritis (OA) in the hopes of reducing cartilage damage from synovitis, but there’s also concern that they might actually harm cartilage and periarticular bone.
The investigators, led by Dr. Timothy McAlindon, chief of rheumatology at Tufts Medical Center, sought to bring some data to the table. “Our objective was to test the potential for disease modification of synovitic knee OA by triamcinolone hexacetonide [THA] in a clinical trial with comprehensive measurement of effects on cartilage and subchondral bone using MRI and DXA [dual-energy x-ray absorptiometry],” they said.
The investigators randomized 140 patients with symptomatic knee OA (Kellgren-Lawrence grade 2 or 3) and synovitis on ultrasound to either 40 mg THA or saline knee injections every 3 months for 2 years. Randomization was blocked and stratified by gender and Kellgren-Lawrence grade. Patients had clinical assessments at each visit and annual MRIs and DXA knee and hip scans.
There were no significant between-group differences over the course of the study in mean changes on Western Ontario and McMaster Universities Arthritis Index pain (–2.2 for THA vs. –2.8 for placebo; P = .3) and function scores (–7.1 for THA vs. –9.2 for placebo; P = .4), and no differences in chair stand (–1.1 for THA vs. –1.6 for placebo; P = .8) or walk time tests (–0.5 for THA vs. –0.03 for placebo; P = .5).
There were no significant differences on MRI or DXA, except that the steroid group had greater cartilage loss and the placebo group greater progression of fibrillation.
“The greater rate of loss of cartilage thickness ... in the treated group was small in magnitude and of uncertain clinical significance,” said Dr. McAlindon.
The mean body mass index in the study was 31.2 kg/m2. Just over half the subjects were women, and about two-thirds were white. More than 90% of patients in both groups completed the study.
The work was funded by the National Institutes of Health. The investigators have no relevant disclosures.
Regular corticosteroid injections over 2 years were relatively safe for osteoarthritic knees in a trial from Tufts Medical Center in Boston, but they did not slow the progression of joint damage or improve patient outcomes.
The findings come at a time when the role of intra-articular steroid shots is up for debate. They are widely used for knee osteoarthritis (OA) in the hopes of reducing cartilage damage from synovitis, but there’s also concern that they might actually harm cartilage and periarticular bone.
The investigators, led by Dr. Timothy McAlindon, chief of rheumatology at Tufts Medical Center, sought to bring some data to the table. “Our objective was to test the potential for disease modification of synovitic knee OA by triamcinolone hexacetonide [THA] in a clinical trial with comprehensive measurement of effects on cartilage and subchondral bone using MRI and DXA [dual-energy x-ray absorptiometry],” they said.
The investigators randomized 140 patients with symptomatic knee OA (Kellgren-Lawrence grade 2 or 3) and synovitis on ultrasound to either 40 mg THA or saline knee injections every 3 months for 2 years. Randomization was blocked and stratified by gender and Kellgren-Lawrence grade. Patients had clinical assessments at each visit and annual MRIs and DXA knee and hip scans.
There were no significant between-group differences over the course of the study in mean changes on Western Ontario and McMaster Universities Arthritis Index pain (–2.2 for THA vs. –2.8 for placebo; P = .3) and function scores (–7.1 for THA vs. –9.2 for placebo; P = .4), and no differences in chair stand (–1.1 for THA vs. –1.6 for placebo; P = .8) or walk time tests (–0.5 for THA vs. –0.03 for placebo; P = .5).
There were no significant differences on MRI or DXA, except that the steroid group had greater cartilage loss and the placebo group greater progression of fibrillation.
“The greater rate of loss of cartilage thickness ... in the treated group was small in magnitude and of uncertain clinical significance,” said Dr. McAlindon.
The mean body mass index in the study was 31.2 kg/m2. Just over half the subjects were women, and about two-thirds were white. More than 90% of patients in both groups completed the study.
The work was funded by the National Institutes of Health. The investigators have no relevant disclosures.
Regular corticosteroid injections over 2 years were relatively safe for osteoarthritic knees in a trial from Tufts Medical Center in Boston, but they did not slow the progression of joint damage or improve patient outcomes.
The findings come at a time when the role of intra-articular steroid shots is up for debate. They are widely used for knee osteoarthritis (OA) in the hopes of reducing cartilage damage from synovitis, but there’s also concern that they might actually harm cartilage and periarticular bone.
The investigators, led by Dr. Timothy McAlindon, chief of rheumatology at Tufts Medical Center, sought to bring some data to the table. “Our objective was to test the potential for disease modification of synovitic knee OA by triamcinolone hexacetonide [THA] in a clinical trial with comprehensive measurement of effects on cartilage and subchondral bone using MRI and DXA [dual-energy x-ray absorptiometry],” they said.
The investigators randomized 140 patients with symptomatic knee OA (Kellgren-Lawrence grade 2 or 3) and synovitis on ultrasound to either 40 mg THA or saline knee injections every 3 months for 2 years. Randomization was blocked and stratified by gender and Kellgren-Lawrence grade. Patients had clinical assessments at each visit and annual MRIs and DXA knee and hip scans.
There were no significant between-group differences over the course of the study in mean changes on Western Ontario and McMaster Universities Arthritis Index pain (–2.2 for THA vs. –2.8 for placebo; P = .3) and function scores (–7.1 for THA vs. –9.2 for placebo; P = .4), and no differences in chair stand (–1.1 for THA vs. –1.6 for placebo; P = .8) or walk time tests (–0.5 for THA vs. –0.03 for placebo; P = .5).
There were no significant differences on MRI or DXA, except that the steroid group had greater cartilage loss and the placebo group greater progression of fibrillation.
“The greater rate of loss of cartilage thickness ... in the treated group was small in magnitude and of uncertain clinical significance,” said Dr. McAlindon.
The mean body mass index in the study was 31.2 kg/m2. Just over half the subjects were women, and about two-thirds were white. More than 90% of patients in both groups completed the study.
The work was funded by the National Institutes of Health. The investigators have no relevant disclosures.
FROM THE ACR ANNUAL MEETING
Key clinical point: Intra-articular steroid injections do not slow the progression of knee OA or improve patient outcomes.
Major finding: Over 2 years, there were no significant differences between steroid injection and placebo injection patients on Western Ontario and McMaster Universities Arthritis Index pain (–2.2 for THA vs. –2.8 for placebo; P = .3) and function scores (–7.1 for THA vs. –9.2 for placebo; P = .4), and no differences in chair stand (–1.1 for THA vs. –1.6 for placebo; P = .8) or walk time tests (–0.5 for THA vs. –0.03 for placebo; P = .5).
Data source: A randomized, placebo-controlled trial with 140 knee OA patients.
Disclosures: The work was funded by the National Institutes of Health. The investigators have no relevant disclosures.
FDA approves low-dose meloxicam medication for osteoarthritis
The Food and Drug Administration has approved a low-dose formulation of meloxicam for the treatment of osteoarthritis pain, according to manufacturer, Iroko Pharmaceuticals.
The new medication, Vivlodex, is made using a proprietary technology for producing submicron-size particles of meloxicam that are 10 times smaller than their traditional size, decreasing dissolution time. In a 12-week, phase III trial of 402 osteoarthritis patients aged 40 years or older, Vivlodex in 5- and 10-mg doses achieved efficacy at 33% lower doses than with commercially available meloxicam medications. Vivlodex will be available as a once-daily medication in 5- or 10-mg doses.
The FDA and professional medical associations have recommended administering nonsteroidal anti-inflammatory drugs in as small a dose and for as short a duration as possible. Serious adverse events stemming from NSAID treatments are related to dose and risk can increase as treatment continues.
“Meloxicam is the second most commonly prescribed NSAID in the [United States]. The approval of Vivlodex is a welcome option that offers patients an effective, low-dose NSAID,” Dr. Byron Cryer, associate dean at the University of Texas Southwestern Medical Center at Dallas, said in a statement from Iroko.
The Food and Drug Administration has approved a low-dose formulation of meloxicam for the treatment of osteoarthritis pain, according to manufacturer, Iroko Pharmaceuticals.
The new medication, Vivlodex, is made using a proprietary technology for producing submicron-size particles of meloxicam that are 10 times smaller than their traditional size, decreasing dissolution time. In a 12-week, phase III trial of 402 osteoarthritis patients aged 40 years or older, Vivlodex in 5- and 10-mg doses achieved efficacy at 33% lower doses than with commercially available meloxicam medications. Vivlodex will be available as a once-daily medication in 5- or 10-mg doses.
The FDA and professional medical associations have recommended administering nonsteroidal anti-inflammatory drugs in as small a dose and for as short a duration as possible. Serious adverse events stemming from NSAID treatments are related to dose and risk can increase as treatment continues.
“Meloxicam is the second most commonly prescribed NSAID in the [United States]. The approval of Vivlodex is a welcome option that offers patients an effective, low-dose NSAID,” Dr. Byron Cryer, associate dean at the University of Texas Southwestern Medical Center at Dallas, said in a statement from Iroko.
The Food and Drug Administration has approved a low-dose formulation of meloxicam for the treatment of osteoarthritis pain, according to manufacturer, Iroko Pharmaceuticals.
The new medication, Vivlodex, is made using a proprietary technology for producing submicron-size particles of meloxicam that are 10 times smaller than their traditional size, decreasing dissolution time. In a 12-week, phase III trial of 402 osteoarthritis patients aged 40 years or older, Vivlodex in 5- and 10-mg doses achieved efficacy at 33% lower doses than with commercially available meloxicam medications. Vivlodex will be available as a once-daily medication in 5- or 10-mg doses.
The FDA and professional medical associations have recommended administering nonsteroidal anti-inflammatory drugs in as small a dose and for as short a duration as possible. Serious adverse events stemming from NSAID treatments are related to dose and risk can increase as treatment continues.
“Meloxicam is the second most commonly prescribed NSAID in the [United States]. The approval of Vivlodex is a welcome option that offers patients an effective, low-dose NSAID,” Dr. Byron Cryer, associate dean at the University of Texas Southwestern Medical Center at Dallas, said in a statement from Iroko.
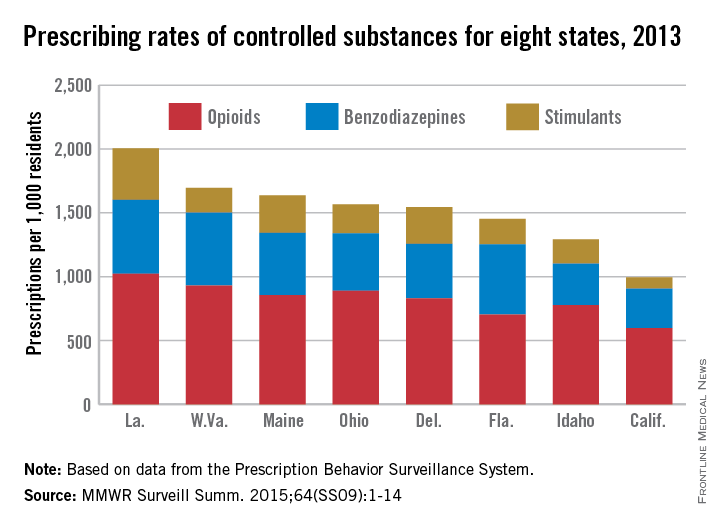
Louisiana goes two for one on controlled substance prescriptions
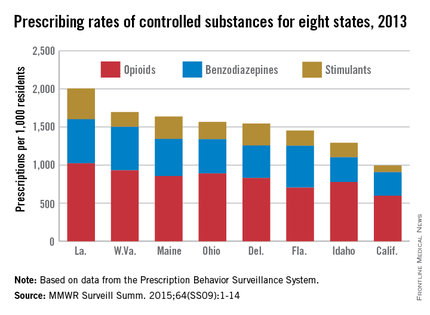
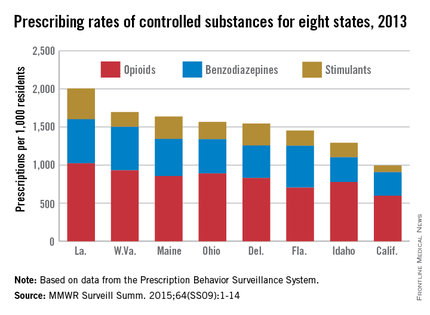
In 2013, enough controlled substances were prescribed in Louisiana – 2006.2 prescriptions per 1,000 population – that each and every person in the state could have received two, according to a report from the Centers for Disease Control and Prevention.
The combined prescribing rate for opioids, benzodiazepines, and stimulants in Louisiana topped the eight states included in the CDC report, with West Virginia in second at 1,695.7 prescriptions per 1,000. At the low end, California was the only one of the eight states where the average controlled substance prescription rate was less than one per person, but just barely at 994.8 per 1,000 people, followed by Idaho at 1,292.3 per 1,000, according to the CDC investigators in a Morbidity and Mortality Weekly Report Surveillance Summary (2015 Oct;64[SS09]:1-14).
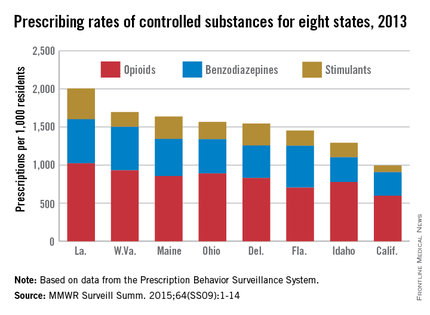
Of the three categories of controlled substances, opioids were by far the most commonly prescribed. At 1,021.7 prescriptions per 1,000 people, the opioid prescription rate in Louisiana was greater than the total controlled substance prescription rate in California. West Virginia had the second highest rate at 929.3, and California had the lowest at 596.3.
Prescription rates for stimulants and benzodiazepines were highest in Louisiana at 403.9 and 580.6 per 1,000 people, respectively. Maine had the next-highest stimulant prescription rate at 293.9, and West Virginia had the second-highest benzodiazepine prescription rate at 572.1. California had the lowest rate in both categories at 87.7 and 310.8, respectively.
Women received opioids and benzodiazepines at much higher rates than did men in every state, but stimulant-prescribing rates were higher for men in five states.
Opioid use was highest in people aged 55-64 years, though use spiked dramatically past the age of 25. People in Louisiana aged 55-64 receiving opioids had the highest controlled substance prescription rate of any measured age group, at 1,715.7 per 1,000 people. Benzodiazepine use was most common in people over 65 years, and stimulant prescriptions were highest in people younger than 18, likely because of the prevalence of childhood attention-deficit/hyperactivity disorder, the CDC investigators said.
The MMWR report used data collected by the Prescription Behavior Surveillance System. The eight states were included because they submitted data to the Prescription Behavior Surveillance System in time for the report, and they represent about one-quarter of the U.S. population.
In 2013, enough controlled substances were prescribed in Louisiana – 2006.2 prescriptions per 1,000 population – that each and every person in the state could have received two, according to a report from the Centers for Disease Control and Prevention.
The combined prescribing rate for opioids, benzodiazepines, and stimulants in Louisiana topped the eight states included in the CDC report, with West Virginia in second at 1,695.7 prescriptions per 1,000. At the low end, California was the only one of the eight states where the average controlled substance prescription rate was less than one per person, but just barely at 994.8 per 1,000 people, followed by Idaho at 1,292.3 per 1,000, according to the CDC investigators in a Morbidity and Mortality Weekly Report Surveillance Summary (2015 Oct;64[SS09]:1-14).
Of the three categories of controlled substances, opioids were by far the most commonly prescribed. At 1,021.7 prescriptions per 1,000 people, the opioid prescription rate in Louisiana was greater than the total controlled substance prescription rate in California. West Virginia had the second highest rate at 929.3, and California had the lowest at 596.3.
Prescription rates for stimulants and benzodiazepines were highest in Louisiana at 403.9 and 580.6 per 1,000 people, respectively. Maine had the next-highest stimulant prescription rate at 293.9, and West Virginia had the second-highest benzodiazepine prescription rate at 572.1. California had the lowest rate in both categories at 87.7 and 310.8, respectively.
Women received opioids and benzodiazepines at much higher rates than did men in every state, but stimulant-prescribing rates were higher for men in five states.
Opioid use was highest in people aged 55-64 years, though use spiked dramatically past the age of 25. People in Louisiana aged 55-64 receiving opioids had the highest controlled substance prescription rate of any measured age group, at 1,715.7 per 1,000 people. Benzodiazepine use was most common in people over 65 years, and stimulant prescriptions were highest in people younger than 18, likely because of the prevalence of childhood attention-deficit/hyperactivity disorder, the CDC investigators said.
The MMWR report used data collected by the Prescription Behavior Surveillance System. The eight states were included because they submitted data to the Prescription Behavior Surveillance System in time for the report, and they represent about one-quarter of the U.S. population.
In 2013, enough controlled substances were prescribed in Louisiana – 2006.2 prescriptions per 1,000 population – that each and every person in the state could have received two, according to a report from the Centers for Disease Control and Prevention.
The combined prescribing rate for opioids, benzodiazepines, and stimulants in Louisiana topped the eight states included in the CDC report, with West Virginia in second at 1,695.7 prescriptions per 1,000. At the low end, California was the only one of the eight states where the average controlled substance prescription rate was less than one per person, but just barely at 994.8 per 1,000 people, followed by Idaho at 1,292.3 per 1,000, according to the CDC investigators in a Morbidity and Mortality Weekly Report Surveillance Summary (2015 Oct;64[SS09]:1-14).
Of the three categories of controlled substances, opioids were by far the most commonly prescribed. At 1,021.7 prescriptions per 1,000 people, the opioid prescription rate in Louisiana was greater than the total controlled substance prescription rate in California. West Virginia had the second highest rate at 929.3, and California had the lowest at 596.3.
Prescription rates for stimulants and benzodiazepines were highest in Louisiana at 403.9 and 580.6 per 1,000 people, respectively. Maine had the next-highest stimulant prescription rate at 293.9, and West Virginia had the second-highest benzodiazepine prescription rate at 572.1. California had the lowest rate in both categories at 87.7 and 310.8, respectively.
Women received opioids and benzodiazepines at much higher rates than did men in every state, but stimulant-prescribing rates were higher for men in five states.
Opioid use was highest in people aged 55-64 years, though use spiked dramatically past the age of 25. People in Louisiana aged 55-64 receiving opioids had the highest controlled substance prescription rate of any measured age group, at 1,715.7 per 1,000 people. Benzodiazepine use was most common in people over 65 years, and stimulant prescriptions were highest in people younger than 18, likely because of the prevalence of childhood attention-deficit/hyperactivity disorder, the CDC investigators said.
The MMWR report used data collected by the Prescription Behavior Surveillance System. The eight states were included because they submitted data to the Prescription Behavior Surveillance System in time for the report, and they represent about one-quarter of the U.S. population.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Benefits, risks of total knee replacement for OA illuminated in trial
Total knee replacement was superior to nonsurgical treatment in relieving pain, restoring function, and improving quality of life for patients with moderate to severe knee osteoarthritis, according to a report published online Oct. 22 in the New England Journal of Medicine.
Even though the number of total knee replacements performed each year is large and steadily increasing – with more than 670,000 done in 2012 in the United States alone – no high-quality randomized, controlled trials have ever compared the effectiveness of the procedure against nonsurgical treatment, said Søren T. Skou, Ph.D., of the Research Unit for Musculoskeletal Function and Physiotherapy, Institute of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense, and his associates.
Dr. Skou and his colleagues remedied that situation by randomly assigning 100 adults (mean age, 66 years) who were eligible for unilateral total knee replacement to either undergo the procedure and then receive a comprehensive nonsurgical intervention (50 patients) or receive the comprehensive nonsurgical intervention alone (50 patients) at two specialized university clinics in Denmark. The 12-week nonsurgical intervention comprised a twice-weekly group exercise program to restore neutral, functional realignment of the legs; two 1-hour education sessions regarding osteoarthritis characteristics, treatments, and self-help strategies; a dietary (weight-loss) program; provision of individually fitted insoles with medial arch support and a lateral wedge if patients had knee-lateral-to-foot positioning; and as-needed pain medication for pain – acetaminophen and ibuprofen – and pantoprazole, a proton-pump inhibitor.
The primary outcome measure in the trial was the between-group difference at 1 year in improvement on four subscales of the Knee Injury and Osteoarthritis Outcome Scores (KOOS) for pain, symptoms, activities of daily living, and quality of life. The surgical group showed a significantly greater improvement (32.5 out of a possible 100 points) than the nonsurgical group (16.0 points) in this outcome. The surgical group also showed significantly greater improvements in all five individual subscales and in a timed chair-rising test, a timed 20-meter walk test, and on a quality-of-life index, the investigators said (N Engl J Med. 2015 373;17:1597-606).
However, it is important to note that patients who had only the nonsurgical intervention showed clinically relevant improvements, and only 26% of them chose to have the surgery after the conclusion of the study. As expected, the surgical group had more serious adverse events than did the nonsurgical group (24 vs. 6), including three cases of deep venous thrombosis and three cases of knee stiffness requiring brisement forcé while the patient was anesthetized, Dr. Skou and his associates said.
This study was supported by the Obel Family Foundation, the Danish Rheumatism Association, the Health Science Foundation of the North Denmark Region, Foot Science International, Spar Nord Foundation, the Bevica Foundation, the Association of Danish Physiotherapists Research Fund, the Medical Specialist Heinrich Kopp’s Grant, and the Danish Medical Association Research Fund. Dr. Skou and his associates reported having no relevant financial disclosures.
 |
Dr. Jeffrey N. Katz |
This study provides the first rigorously controlled data to inform discussions about whether patients should undergo total knee replacement or opt for comprehensive nonsurgical treatment. Surgery proved markedly superior in this trial, with 85% of surgical patients reporting a clinically important improvement in pain and function at 1 year, compared with 68% of nonsurgical patients.
But surgery was associated with several severe adverse events, including deep venous thrombosis, deep wound infection, supracondylar fracture, and stiffness requiring treatment under general anesthesia. Each patient must weigh these considerations; each physician should present the relevant data to their patients and then listen carefully to their preferences.
Dr. Jeffrey N. Katz is in the departments of medicine and orthopedic surgery at Brigham and Women’s Hospital and Harvard University, Boston. He reported having no relevant financial disclosures. Dr. Katz made these remarks in an editorial accompanying Dr. Skou’s report (N Engl J Med. 2015 373;17:1668-9).
 |
Dr. Jeffrey N. Katz |
This study provides the first rigorously controlled data to inform discussions about whether patients should undergo total knee replacement or opt for comprehensive nonsurgical treatment. Surgery proved markedly superior in this trial, with 85% of surgical patients reporting a clinically important improvement in pain and function at 1 year, compared with 68% of nonsurgical patients.
But surgery was associated with several severe adverse events, including deep venous thrombosis, deep wound infection, supracondylar fracture, and stiffness requiring treatment under general anesthesia. Each patient must weigh these considerations; each physician should present the relevant data to their patients and then listen carefully to their preferences.
Dr. Jeffrey N. Katz is in the departments of medicine and orthopedic surgery at Brigham and Women’s Hospital and Harvard University, Boston. He reported having no relevant financial disclosures. Dr. Katz made these remarks in an editorial accompanying Dr. Skou’s report (N Engl J Med. 2015 373;17:1668-9).
 |
Dr. Jeffrey N. Katz |
This study provides the first rigorously controlled data to inform discussions about whether patients should undergo total knee replacement or opt for comprehensive nonsurgical treatment. Surgery proved markedly superior in this trial, with 85% of surgical patients reporting a clinically important improvement in pain and function at 1 year, compared with 68% of nonsurgical patients.
But surgery was associated with several severe adverse events, including deep venous thrombosis, deep wound infection, supracondylar fracture, and stiffness requiring treatment under general anesthesia. Each patient must weigh these considerations; each physician should present the relevant data to their patients and then listen carefully to their preferences.
Dr. Jeffrey N. Katz is in the departments of medicine and orthopedic surgery at Brigham and Women’s Hospital and Harvard University, Boston. He reported having no relevant financial disclosures. Dr. Katz made these remarks in an editorial accompanying Dr. Skou’s report (N Engl J Med. 2015 373;17:1668-9).
Total knee replacement was superior to nonsurgical treatment in relieving pain, restoring function, and improving quality of life for patients with moderate to severe knee osteoarthritis, according to a report published online Oct. 22 in the New England Journal of Medicine.
Even though the number of total knee replacements performed each year is large and steadily increasing – with more than 670,000 done in 2012 in the United States alone – no high-quality randomized, controlled trials have ever compared the effectiveness of the procedure against nonsurgical treatment, said Søren T. Skou, Ph.D., of the Research Unit for Musculoskeletal Function and Physiotherapy, Institute of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense, and his associates.
Dr. Skou and his colleagues remedied that situation by randomly assigning 100 adults (mean age, 66 years) who were eligible for unilateral total knee replacement to either undergo the procedure and then receive a comprehensive nonsurgical intervention (50 patients) or receive the comprehensive nonsurgical intervention alone (50 patients) at two specialized university clinics in Denmark. The 12-week nonsurgical intervention comprised a twice-weekly group exercise program to restore neutral, functional realignment of the legs; two 1-hour education sessions regarding osteoarthritis characteristics, treatments, and self-help strategies; a dietary (weight-loss) program; provision of individually fitted insoles with medial arch support and a lateral wedge if patients had knee-lateral-to-foot positioning; and as-needed pain medication for pain – acetaminophen and ibuprofen – and pantoprazole, a proton-pump inhibitor.
The primary outcome measure in the trial was the between-group difference at 1 year in improvement on four subscales of the Knee Injury and Osteoarthritis Outcome Scores (KOOS) for pain, symptoms, activities of daily living, and quality of life. The surgical group showed a significantly greater improvement (32.5 out of a possible 100 points) than the nonsurgical group (16.0 points) in this outcome. The surgical group also showed significantly greater improvements in all five individual subscales and in a timed chair-rising test, a timed 20-meter walk test, and on a quality-of-life index, the investigators said (N Engl J Med. 2015 373;17:1597-606).
However, it is important to note that patients who had only the nonsurgical intervention showed clinically relevant improvements, and only 26% of them chose to have the surgery after the conclusion of the study. As expected, the surgical group had more serious adverse events than did the nonsurgical group (24 vs. 6), including three cases of deep venous thrombosis and three cases of knee stiffness requiring brisement forcé while the patient was anesthetized, Dr. Skou and his associates said.
This study was supported by the Obel Family Foundation, the Danish Rheumatism Association, the Health Science Foundation of the North Denmark Region, Foot Science International, Spar Nord Foundation, the Bevica Foundation, the Association of Danish Physiotherapists Research Fund, the Medical Specialist Heinrich Kopp’s Grant, and the Danish Medical Association Research Fund. Dr. Skou and his associates reported having no relevant financial disclosures.
Total knee replacement was superior to nonsurgical treatment in relieving pain, restoring function, and improving quality of life for patients with moderate to severe knee osteoarthritis, according to a report published online Oct. 22 in the New England Journal of Medicine.
Even though the number of total knee replacements performed each year is large and steadily increasing – with more than 670,000 done in 2012 in the United States alone – no high-quality randomized, controlled trials have ever compared the effectiveness of the procedure against nonsurgical treatment, said Søren T. Skou, Ph.D., of the Research Unit for Musculoskeletal Function and Physiotherapy, Institute of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense, and his associates.
Dr. Skou and his colleagues remedied that situation by randomly assigning 100 adults (mean age, 66 years) who were eligible for unilateral total knee replacement to either undergo the procedure and then receive a comprehensive nonsurgical intervention (50 patients) or receive the comprehensive nonsurgical intervention alone (50 patients) at two specialized university clinics in Denmark. The 12-week nonsurgical intervention comprised a twice-weekly group exercise program to restore neutral, functional realignment of the legs; two 1-hour education sessions regarding osteoarthritis characteristics, treatments, and self-help strategies; a dietary (weight-loss) program; provision of individually fitted insoles with medial arch support and a lateral wedge if patients had knee-lateral-to-foot positioning; and as-needed pain medication for pain – acetaminophen and ibuprofen – and pantoprazole, a proton-pump inhibitor.
The primary outcome measure in the trial was the between-group difference at 1 year in improvement on four subscales of the Knee Injury and Osteoarthritis Outcome Scores (KOOS) for pain, symptoms, activities of daily living, and quality of life. The surgical group showed a significantly greater improvement (32.5 out of a possible 100 points) than the nonsurgical group (16.0 points) in this outcome. The surgical group also showed significantly greater improvements in all five individual subscales and in a timed chair-rising test, a timed 20-meter walk test, and on a quality-of-life index, the investigators said (N Engl J Med. 2015 373;17:1597-606).
However, it is important to note that patients who had only the nonsurgical intervention showed clinically relevant improvements, and only 26% of them chose to have the surgery after the conclusion of the study. As expected, the surgical group had more serious adverse events than did the nonsurgical group (24 vs. 6), including three cases of deep venous thrombosis and three cases of knee stiffness requiring brisement forcé while the patient was anesthetized, Dr. Skou and his associates said.
This study was supported by the Obel Family Foundation, the Danish Rheumatism Association, the Health Science Foundation of the North Denmark Region, Foot Science International, Spar Nord Foundation, the Bevica Foundation, the Association of Danish Physiotherapists Research Fund, the Medical Specialist Heinrich Kopp’s Grant, and the Danish Medical Association Research Fund. Dr. Skou and his associates reported having no relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Total knee replacement is superior to nonsurgical treatment in decreasing pain and improving function and quality of life.
Major finding: The surgical group showed a significantly greater improvement 1 year from baseline (32.5 out of a possible 100 points) than did the nonsurgical group (16.0 points) in mean Knee Injury and Osteoarthritis Outcome Scores (KOOS) for pain, symptoms, activities of daily living, and quality of life.
Data source: A randomized, controlled trial comparing 1-year outcomes after total knee replacement (50 patients) vs. nonsurgical treatment (50 patients) for osteoarthritis.
Disclosures: This study was supported by the Obel Family Foundation, the Danish Rheumatism Association, the Health Science Foundation of the North Denmark Region, Foot Science International, Spar Nord Foundation, the Bevica Foundation, the Association of Danish Physiotherapists Research Fund, the Medical Specialist Heinrich Kopp’s Grant, and the Danish Medical Association Research Fund. Dr. Skou and his associates reported having no relevant financial disclosures.
Worsening of lesions on MRI predicts knee OA
People without x-ray evidence of osteoarthritis in their knees but with MRI-identified lesions that worsen over time are significantly likelier to develop knee OA, compared with people whose lesions remain stable, according to results from a prospective cohort study.
For their research, published Oct. 14 in Annals of the Rheumatic Diseases, Dr. Leena Sharma of Northwestern University in Chicago and her colleagues recruited more than 1,000 patients at elevated risk of knee OA but with no radiographic evidence yet of disease (Kellgren/Lawrence measures of 0 [KL0] in both knees) to test their hypothesis that lesions seen worsening over time on MRI were predictive of knee OA within 4 years and of persistent symptoms between 4 and 7 years. Patients in the cohort (56% women, mean age 59.6 years) were assessed for cartilage damage, meniscal tears, meniscal extrusions, and bone marrow lesions at 12 and 48 months. Study inclusion required that patients remain at KL0 in both knees at 12 months to continue, and 849 patients had complete data at 12 and 48 months.
Patients with lesions that had worsened on MRI between 12 and 48 months had significantly higher risk of incident radiographic KL1 and KL2 by 48 months, compared with patients whose lesions had not worsened. For example, 6.3% of patients with tibiofemoral cartilage damage that was stable at 48 months developed mild (KL1) disease at 48 months, compared with 9.5% of patients whose damage had worsened in that interval (odds ratio, 2.69; 95% confidence interval, 1.50-4.84). Half of patients with worsening meniscal extrusion developed mild knee OA by the endpoint, compared with 13.6% of patients with a stable lesion (OR, 5.73; 95% CI, 2.94-11.16). Higher risk of KL1 or KL2 at 48 months was significant for all the lesion types studied except bone marrow lesions. Worsening of these lesions between 12 and 48 months was also significantly associated with having persistent symptoms between 4 and 7 years. Having more lesion types that worsened was significantly associated with worse outcomes.
The findings, Dr. Sharma and her colleagues wrote, support the idea of stable and progressive disease phases with early indicators of each and that worsening lesions represent early osteoarthritis. “Given the absence of disease-modifying therapy for OA, widespread clinical application of MRI is difficult to justify,” the investigators wrote in their analysis (Ann Rheum Dis. 2015 Oct 14. doi: 10.1136/annrheumdis-2015-208129).
Nevertheless, they concluded, “prevention or delay of worsening of early-stage lesions should be considered as a target for emerging pharmacological and nonpharmacological treatments in an effort to prevent or delay full-blown disease. Candidate interventions should be studied at this stage, when they are more likely to be effective.” Investigators acknowledged that one limitation of the study was that its findings may not apply in populations not already at higher risk for knee OA.
The study was funded by the Osteoarthritis Initiative, a public-private partnership of the National Institutes of Health and Merck, Novartis, GlaxoSmithKline, and Pfizer, with industry funding administered by NIH.
People without x-ray evidence of osteoarthritis in their knees but with MRI-identified lesions that worsen over time are significantly likelier to develop knee OA, compared with people whose lesions remain stable, according to results from a prospective cohort study.
For their research, published Oct. 14 in Annals of the Rheumatic Diseases, Dr. Leena Sharma of Northwestern University in Chicago and her colleagues recruited more than 1,000 patients at elevated risk of knee OA but with no radiographic evidence yet of disease (Kellgren/Lawrence measures of 0 [KL0] in both knees) to test their hypothesis that lesions seen worsening over time on MRI were predictive of knee OA within 4 years and of persistent symptoms between 4 and 7 years. Patients in the cohort (56% women, mean age 59.6 years) were assessed for cartilage damage, meniscal tears, meniscal extrusions, and bone marrow lesions at 12 and 48 months. Study inclusion required that patients remain at KL0 in both knees at 12 months to continue, and 849 patients had complete data at 12 and 48 months.
Patients with lesions that had worsened on MRI between 12 and 48 months had significantly higher risk of incident radiographic KL1 and KL2 by 48 months, compared with patients whose lesions had not worsened. For example, 6.3% of patients with tibiofemoral cartilage damage that was stable at 48 months developed mild (KL1) disease at 48 months, compared with 9.5% of patients whose damage had worsened in that interval (odds ratio, 2.69; 95% confidence interval, 1.50-4.84). Half of patients with worsening meniscal extrusion developed mild knee OA by the endpoint, compared with 13.6% of patients with a stable lesion (OR, 5.73; 95% CI, 2.94-11.16). Higher risk of KL1 or KL2 at 48 months was significant for all the lesion types studied except bone marrow lesions. Worsening of these lesions between 12 and 48 months was also significantly associated with having persistent symptoms between 4 and 7 years. Having more lesion types that worsened was significantly associated with worse outcomes.
The findings, Dr. Sharma and her colleagues wrote, support the idea of stable and progressive disease phases with early indicators of each and that worsening lesions represent early osteoarthritis. “Given the absence of disease-modifying therapy for OA, widespread clinical application of MRI is difficult to justify,” the investigators wrote in their analysis (Ann Rheum Dis. 2015 Oct 14. doi: 10.1136/annrheumdis-2015-208129).
Nevertheless, they concluded, “prevention or delay of worsening of early-stage lesions should be considered as a target for emerging pharmacological and nonpharmacological treatments in an effort to prevent or delay full-blown disease. Candidate interventions should be studied at this stage, when they are more likely to be effective.” Investigators acknowledged that one limitation of the study was that its findings may not apply in populations not already at higher risk for knee OA.
The study was funded by the Osteoarthritis Initiative, a public-private partnership of the National Institutes of Health and Merck, Novartis, GlaxoSmithKline, and Pfizer, with industry funding administered by NIH.
People without x-ray evidence of osteoarthritis in their knees but with MRI-identified lesions that worsen over time are significantly likelier to develop knee OA, compared with people whose lesions remain stable, according to results from a prospective cohort study.
For their research, published Oct. 14 in Annals of the Rheumatic Diseases, Dr. Leena Sharma of Northwestern University in Chicago and her colleagues recruited more than 1,000 patients at elevated risk of knee OA but with no radiographic evidence yet of disease (Kellgren/Lawrence measures of 0 [KL0] in both knees) to test their hypothesis that lesions seen worsening over time on MRI were predictive of knee OA within 4 years and of persistent symptoms between 4 and 7 years. Patients in the cohort (56% women, mean age 59.6 years) were assessed for cartilage damage, meniscal tears, meniscal extrusions, and bone marrow lesions at 12 and 48 months. Study inclusion required that patients remain at KL0 in both knees at 12 months to continue, and 849 patients had complete data at 12 and 48 months.
Patients with lesions that had worsened on MRI between 12 and 48 months had significantly higher risk of incident radiographic KL1 and KL2 by 48 months, compared with patients whose lesions had not worsened. For example, 6.3% of patients with tibiofemoral cartilage damage that was stable at 48 months developed mild (KL1) disease at 48 months, compared with 9.5% of patients whose damage had worsened in that interval (odds ratio, 2.69; 95% confidence interval, 1.50-4.84). Half of patients with worsening meniscal extrusion developed mild knee OA by the endpoint, compared with 13.6% of patients with a stable lesion (OR, 5.73; 95% CI, 2.94-11.16). Higher risk of KL1 or KL2 at 48 months was significant for all the lesion types studied except bone marrow lesions. Worsening of these lesions between 12 and 48 months was also significantly associated with having persistent symptoms between 4 and 7 years. Having more lesion types that worsened was significantly associated with worse outcomes.
The findings, Dr. Sharma and her colleagues wrote, support the idea of stable and progressive disease phases with early indicators of each and that worsening lesions represent early osteoarthritis. “Given the absence of disease-modifying therapy for OA, widespread clinical application of MRI is difficult to justify,” the investigators wrote in their analysis (Ann Rheum Dis. 2015 Oct 14. doi: 10.1136/annrheumdis-2015-208129).
Nevertheless, they concluded, “prevention or delay of worsening of early-stage lesions should be considered as a target for emerging pharmacological and nonpharmacological treatments in an effort to prevent or delay full-blown disease. Candidate interventions should be studied at this stage, when they are more likely to be effective.” Investigators acknowledged that one limitation of the study was that its findings may not apply in populations not already at higher risk for knee OA.
The study was funded by the Osteoarthritis Initiative, a public-private partnership of the National Institutes of Health and Merck, Novartis, GlaxoSmithKline, and Pfizer, with industry funding administered by NIH.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: People with knee cartilage damage, meniscal tear, meniscal extrusion, and bone marrow lesions on MRI were likelier to have developed knee osteoarthritis at 48 months, compared with people with stable lesions; more lesion types at baseline were associated with worse outcomes.
Major finding: Higher-risk mild or moderate radiographic knee OA at 48 months was significant for most types of lesions that had worsened after 12 months.
Data source: A prospective cohort study of 849 people at high risk of knee osteoarthritis evaluated on radiography (for evidence of knee OA) and MRI (for lesions) at baseline, 12 months, and 48 months and followed up for symptoms through 84 months.
Disclosures: The study was funded by the Osteoarthritis Initiative, a public-private partnership of the National Institutes of Health and Merck, Novartis, GlaxoSmithKline, and Pfizer, with industry funding administered by NIH. The study authors disclosed no conflicts of interest.
Serum HA cutoff predicts progression in knee OA
Serum concentration of hyaluronic acid correlated with the severity of knee osteoarthritis in a longitudinal population-based cohort, with concentrations above 51.9 ng/mL significantly associated with progression in people with moderate disease.
While previous studies have suggested cutoff values for serum hyaluronic acid (HA) as biomarkers for progression of knee osteoarthritis, this study, conducted by Dr. Eiji Sasaki of Hirosaki (Japan) University and his colleagues, is the first to report a serum HA cutoff value from a longitudinal study.
The investigators prospectively enrolled 720 volunteers into a community-based preventive medicine program with intent to follow them for 5 years. They excluded patients with renal failure, liver failure, rheumatoid arthritis, or cancer, as all of these can increase serum HA. HA concentrations and knee radiography were taken at baseline and at 5-year follow-up, with complete data from 444 patients (mean age 55, 64% female) entered into analysis. Dr. Sasaki and his colleagues measured severity of knee osteoarthritis using Kellgren-Lawrence grades. Higher serum HA at baseline correlated with KL grade progression in the cohort as a whole (P = .004), and HA concentration was linked to joint space narrowing in knees with no disease or mild disease (KL grades 0-1) and moderate disease (KL grades 2 or 3) at baseline (P = .021 and P = .008, respectively).
Serum HA of 51.9 ng/mL was predictive of knee osteoarthritis progression in subjects (n = 119) with KL grades 2 or 3 disease (area under curve [AUC], 0.707), and associated with a fivefold increase (odds ratio, 4.89) in risk of joint space narrowing over 5 years. For people with mild or no disease at baseline (n = 323), Dr. Sasaki and his colleagues identified a cutoff of 35.1 ng/mL for the development of OA, but it was not a robust indicator with an AUC of 0.603 (Arthritis Res Ther. 2015;17:283. doi: 10.1186/s13075-015-0793-0).
“Further clinical studies are needed to determine whether serum HA can predict the incidence of OA, which was not determined in the present study,” Dr. Sasaki and his colleagues wrote in their analysis. They noted that the cutoff value of 51.9 ng/mL “should be useful during screening for abnormal knee conditions or as an additional evaluation for the risk of OA progression when used in combination with conventional imaging tools.”
The study was funded by grants from the Japanese government, the Japanese Society for the Promotion of Science, and the Japanese Orthopedic Association. Dr. Sasaki and colleagues declared no conflicts of interest.
Serum concentration of hyaluronic acid correlated with the severity of knee osteoarthritis in a longitudinal population-based cohort, with concentrations above 51.9 ng/mL significantly associated with progression in people with moderate disease.
While previous studies have suggested cutoff values for serum hyaluronic acid (HA) as biomarkers for progression of knee osteoarthritis, this study, conducted by Dr. Eiji Sasaki of Hirosaki (Japan) University and his colleagues, is the first to report a serum HA cutoff value from a longitudinal study.
The investigators prospectively enrolled 720 volunteers into a community-based preventive medicine program with intent to follow them for 5 years. They excluded patients with renal failure, liver failure, rheumatoid arthritis, or cancer, as all of these can increase serum HA. HA concentrations and knee radiography were taken at baseline and at 5-year follow-up, with complete data from 444 patients (mean age 55, 64% female) entered into analysis. Dr. Sasaki and his colleagues measured severity of knee osteoarthritis using Kellgren-Lawrence grades. Higher serum HA at baseline correlated with KL grade progression in the cohort as a whole (P = .004), and HA concentration was linked to joint space narrowing in knees with no disease or mild disease (KL grades 0-1) and moderate disease (KL grades 2 or 3) at baseline (P = .021 and P = .008, respectively).
Serum HA of 51.9 ng/mL was predictive of knee osteoarthritis progression in subjects (n = 119) with KL grades 2 or 3 disease (area under curve [AUC], 0.707), and associated with a fivefold increase (odds ratio, 4.89) in risk of joint space narrowing over 5 years. For people with mild or no disease at baseline (n = 323), Dr. Sasaki and his colleagues identified a cutoff of 35.1 ng/mL for the development of OA, but it was not a robust indicator with an AUC of 0.603 (Arthritis Res Ther. 2015;17:283. doi: 10.1186/s13075-015-0793-0).
“Further clinical studies are needed to determine whether serum HA can predict the incidence of OA, which was not determined in the present study,” Dr. Sasaki and his colleagues wrote in their analysis. They noted that the cutoff value of 51.9 ng/mL “should be useful during screening for abnormal knee conditions or as an additional evaluation for the risk of OA progression when used in combination with conventional imaging tools.”
The study was funded by grants from the Japanese government, the Japanese Society for the Promotion of Science, and the Japanese Orthopedic Association. Dr. Sasaki and colleagues declared no conflicts of interest.
Serum concentration of hyaluronic acid correlated with the severity of knee osteoarthritis in a longitudinal population-based cohort, with concentrations above 51.9 ng/mL significantly associated with progression in people with moderate disease.
While previous studies have suggested cutoff values for serum hyaluronic acid (HA) as biomarkers for progression of knee osteoarthritis, this study, conducted by Dr. Eiji Sasaki of Hirosaki (Japan) University and his colleagues, is the first to report a serum HA cutoff value from a longitudinal study.
The investigators prospectively enrolled 720 volunteers into a community-based preventive medicine program with intent to follow them for 5 years. They excluded patients with renal failure, liver failure, rheumatoid arthritis, or cancer, as all of these can increase serum HA. HA concentrations and knee radiography were taken at baseline and at 5-year follow-up, with complete data from 444 patients (mean age 55, 64% female) entered into analysis. Dr. Sasaki and his colleagues measured severity of knee osteoarthritis using Kellgren-Lawrence grades. Higher serum HA at baseline correlated with KL grade progression in the cohort as a whole (P = .004), and HA concentration was linked to joint space narrowing in knees with no disease or mild disease (KL grades 0-1) and moderate disease (KL grades 2 or 3) at baseline (P = .021 and P = .008, respectively).
Serum HA of 51.9 ng/mL was predictive of knee osteoarthritis progression in subjects (n = 119) with KL grades 2 or 3 disease (area under curve [AUC], 0.707), and associated with a fivefold increase (odds ratio, 4.89) in risk of joint space narrowing over 5 years. For people with mild or no disease at baseline (n = 323), Dr. Sasaki and his colleagues identified a cutoff of 35.1 ng/mL for the development of OA, but it was not a robust indicator with an AUC of 0.603 (Arthritis Res Ther. 2015;17:283. doi: 10.1186/s13075-015-0793-0).
“Further clinical studies are needed to determine whether serum HA can predict the incidence of OA, which was not determined in the present study,” Dr. Sasaki and his colleagues wrote in their analysis. They noted that the cutoff value of 51.9 ng/mL “should be useful during screening for abnormal knee conditions or as an additional evaluation for the risk of OA progression when used in combination with conventional imaging tools.”
The study was funded by grants from the Japanese government, the Japanese Society for the Promotion of Science, and the Japanese Orthopedic Association. Dr. Sasaki and colleagues declared no conflicts of interest.
FROM ARTHRITIS RESEARCH & THERAPY
Key clinical point: Serum HA of 51.9 ng/mL predicts a fivefold increase in risk of progression of existing knee osteoarthritis over 5 years.
Major Finding: Higher sHA concentration was positively correlated with progression of joint space narrowing in people with none-to-mild (P = .021) and moderate (P = .008) knee OA at baseline. Higher concentrations correlated with OA progression as measured by Kellgren-Lawrence grades (P = .004).
Data source: A population-based cohort of 866 people from a community in Japan; 444 subjects received knee radiography and serum HA analysis at baseline and 5-year follow-up.
Disclosures: The study was funded by government and foundation grants in Japan; the investigators disclosed no conflicts of interest.
Study reveals patterns of concurrent MRI lesions in knee OA
Groupings of coexisting MRI lesions of the tibiofemoral and patellofemoral joints were linked to the risk of subsequent radiographic osteoarthritis, investigators reported. Their analysis of data from the prospective, observational MOST study was published online Sept. 28 in Arthritis and Rheumatism.
“The magnitude of lesions such as cartilage damage and coexisting meniscal damage appear to be the main distinction between the subgroups,” said Dr. Jingbo Niu of Boston University and her associates. Several studies have linked individual MRI lesions with incident knee OA, but patterns of coexisting lesions more accurately reflect real-world injuries, such as anterior cruciate ligament tears, which tend to affect more than one knee structure, the investigators noted.
Because directly comparing lesions in a multivariate model does not account for chronology, the investigators used latent class analysis to identify subgroups of coexisting MRI lesions of the tibiofemoral and patellofemoral joints, such as cartilage damage, meniscal tear, meniscal extrusion, synovitis, and effusion. Then they modeled associations between these subgroups and incident OA of the knee (Arthritis Rheum. 2015 Sep 28. doi: 10.1002/art.3943).
Among 885 knees from the MOST study, 203 developed radiographic tibiofemoral OA and 64 developed patellofemoral OA after up to 84 months of follow-up, the researchers reported. Latent class analysis identified four groups of MRI lesions for each knee joint, which exhibited sequentially increasing baseline severity for all MRI features except meniscal damage, the investigators added.
For the patellofemoral joint, the odds of incident knee OA rose sequentially with increasing MRI severity, ranging from 1.0 for minimal lesions to 13.7 for severe lesions (95% confidence interval, 5.0-37.0), according to the study. In contrast, the odds of incident knee radiographic OA (ROA) of the tibiofemoral joint were highest for the “mild” and “severe” groups, which had the most meniscal damage and the most extensive history of knee injury and surgery. Odds ratios for these two groups were 5.6 (95% CI, 3.4-9.4) and 5.0 (95% CI, 2.8-9.0), respectively, said the researchers. “Meniscal damage might play a prominent role in the development of incident ROA in the tibiofemoral joint but not the patellofemoral joint,” they added.
Patients in the MOST study had a high risk of knee OA at baseline, which could limit the generalizability of the findings, Dr. Niu and her associates noted.
The National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Disease, both a part of the National Institutes of Health, supported the study. The investigators did not report conflicts of interest.
It was not until recently that the osteoarthritis community directed a shift toward new ways of halting joint damage rather than the palliative approach of analgesics followed by joint replacement. However, the sequential failures of novel disease-modifying therapies attempting to target diverse pathogenic mechanisms have highlighted the need to target early disease and to better identify and target distinct disease phenotypes. In this light of recent efforts to uncover the various mechanisms leading to joint deterioration, Niu et al. have used a novel approach to detect distinct clusters of multiple joint abnormalities on MRI at the preradiographic stage. They also examined the association between each cluster and the risk of radiographic OA during follow-up.
Probably the most important [conclusion from this study] is that it is possible to identify distinct phenotypes of joint damage as early as at the preradiographic phase. Consequently, it is intuitive that alternative pathways caused by various risk factors exist and play diverse roles in the process of joint destruction. Phenotyping patients in regards to their genetic profile, serologic, and MRI markers, demographic features, metabolic status, etc., is promising and probably the best solution to achieve improvements in the way we are treating OA patients.
The use of these results to assess prognosis seems premature in clinical research and inappropriate in the clinical setting. Nevertheless, the latent class analysis is an attractive approach in the field of OA and can aid in unraveling the pathogenesis of this enigmatic disease.
Dr. Leticia A. Deveza and Dr. David J. Hunter are with the department of rheumatology at the University of Sydney. They declared no conflicts of interest. These comments are from their accompanying editorial (Arthritis Rheum. 2015 Sep 28 doi: 10.1002/art.39439).
It was not until recently that the osteoarthritis community directed a shift toward new ways of halting joint damage rather than the palliative approach of analgesics followed by joint replacement. However, the sequential failures of novel disease-modifying therapies attempting to target diverse pathogenic mechanisms have highlighted the need to target early disease and to better identify and target distinct disease phenotypes. In this light of recent efforts to uncover the various mechanisms leading to joint deterioration, Niu et al. have used a novel approach to detect distinct clusters of multiple joint abnormalities on MRI at the preradiographic stage. They also examined the association between each cluster and the risk of radiographic OA during follow-up.
Probably the most important [conclusion from this study] is that it is possible to identify distinct phenotypes of joint damage as early as at the preradiographic phase. Consequently, it is intuitive that alternative pathways caused by various risk factors exist and play diverse roles in the process of joint destruction. Phenotyping patients in regards to their genetic profile, serologic, and MRI markers, demographic features, metabolic status, etc., is promising and probably the best solution to achieve improvements in the way we are treating OA patients.
The use of these results to assess prognosis seems premature in clinical research and inappropriate in the clinical setting. Nevertheless, the latent class analysis is an attractive approach in the field of OA and can aid in unraveling the pathogenesis of this enigmatic disease.
Dr. Leticia A. Deveza and Dr. David J. Hunter are with the department of rheumatology at the University of Sydney. They declared no conflicts of interest. These comments are from their accompanying editorial (Arthritis Rheum. 2015 Sep 28 doi: 10.1002/art.39439).
It was not until recently that the osteoarthritis community directed a shift toward new ways of halting joint damage rather than the palliative approach of analgesics followed by joint replacement. However, the sequential failures of novel disease-modifying therapies attempting to target diverse pathogenic mechanisms have highlighted the need to target early disease and to better identify and target distinct disease phenotypes. In this light of recent efforts to uncover the various mechanisms leading to joint deterioration, Niu et al. have used a novel approach to detect distinct clusters of multiple joint abnormalities on MRI at the preradiographic stage. They also examined the association between each cluster and the risk of radiographic OA during follow-up.
Probably the most important [conclusion from this study] is that it is possible to identify distinct phenotypes of joint damage as early as at the preradiographic phase. Consequently, it is intuitive that alternative pathways caused by various risk factors exist and play diverse roles in the process of joint destruction. Phenotyping patients in regards to their genetic profile, serologic, and MRI markers, demographic features, metabolic status, etc., is promising and probably the best solution to achieve improvements in the way we are treating OA patients.
The use of these results to assess prognosis seems premature in clinical research and inappropriate in the clinical setting. Nevertheless, the latent class analysis is an attractive approach in the field of OA and can aid in unraveling the pathogenesis of this enigmatic disease.
Dr. Leticia A. Deveza and Dr. David J. Hunter are with the department of rheumatology at the University of Sydney. They declared no conflicts of interest. These comments are from their accompanying editorial (Arthritis Rheum. 2015 Sep 28 doi: 10.1002/art.39439).
Groupings of coexisting MRI lesions of the tibiofemoral and patellofemoral joints were linked to the risk of subsequent radiographic osteoarthritis, investigators reported. Their analysis of data from the prospective, observational MOST study was published online Sept. 28 in Arthritis and Rheumatism.
“The magnitude of lesions such as cartilage damage and coexisting meniscal damage appear to be the main distinction between the subgroups,” said Dr. Jingbo Niu of Boston University and her associates. Several studies have linked individual MRI lesions with incident knee OA, but patterns of coexisting lesions more accurately reflect real-world injuries, such as anterior cruciate ligament tears, which tend to affect more than one knee structure, the investigators noted.
Because directly comparing lesions in a multivariate model does not account for chronology, the investigators used latent class analysis to identify subgroups of coexisting MRI lesions of the tibiofemoral and patellofemoral joints, such as cartilage damage, meniscal tear, meniscal extrusion, synovitis, and effusion. Then they modeled associations between these subgroups and incident OA of the knee (Arthritis Rheum. 2015 Sep 28. doi: 10.1002/art.3943).
Among 885 knees from the MOST study, 203 developed radiographic tibiofemoral OA and 64 developed patellofemoral OA after up to 84 months of follow-up, the researchers reported. Latent class analysis identified four groups of MRI lesions for each knee joint, which exhibited sequentially increasing baseline severity for all MRI features except meniscal damage, the investigators added.
For the patellofemoral joint, the odds of incident knee OA rose sequentially with increasing MRI severity, ranging from 1.0 for minimal lesions to 13.7 for severe lesions (95% confidence interval, 5.0-37.0), according to the study. In contrast, the odds of incident knee radiographic OA (ROA) of the tibiofemoral joint were highest for the “mild” and “severe” groups, which had the most meniscal damage and the most extensive history of knee injury and surgery. Odds ratios for these two groups were 5.6 (95% CI, 3.4-9.4) and 5.0 (95% CI, 2.8-9.0), respectively, said the researchers. “Meniscal damage might play a prominent role in the development of incident ROA in the tibiofemoral joint but not the patellofemoral joint,” they added.
Patients in the MOST study had a high risk of knee OA at baseline, which could limit the generalizability of the findings, Dr. Niu and her associates noted.
The National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Disease, both a part of the National Institutes of Health, supported the study. The investigators did not report conflicts of interest.
Groupings of coexisting MRI lesions of the tibiofemoral and patellofemoral joints were linked to the risk of subsequent radiographic osteoarthritis, investigators reported. Their analysis of data from the prospective, observational MOST study was published online Sept. 28 in Arthritis and Rheumatism.
“The magnitude of lesions such as cartilage damage and coexisting meniscal damage appear to be the main distinction between the subgroups,” said Dr. Jingbo Niu of Boston University and her associates. Several studies have linked individual MRI lesions with incident knee OA, but patterns of coexisting lesions more accurately reflect real-world injuries, such as anterior cruciate ligament tears, which tend to affect more than one knee structure, the investigators noted.
Because directly comparing lesions in a multivariate model does not account for chronology, the investigators used latent class analysis to identify subgroups of coexisting MRI lesions of the tibiofemoral and patellofemoral joints, such as cartilage damage, meniscal tear, meniscal extrusion, synovitis, and effusion. Then they modeled associations between these subgroups and incident OA of the knee (Arthritis Rheum. 2015 Sep 28. doi: 10.1002/art.3943).
Among 885 knees from the MOST study, 203 developed radiographic tibiofemoral OA and 64 developed patellofemoral OA after up to 84 months of follow-up, the researchers reported. Latent class analysis identified four groups of MRI lesions for each knee joint, which exhibited sequentially increasing baseline severity for all MRI features except meniscal damage, the investigators added.
For the patellofemoral joint, the odds of incident knee OA rose sequentially with increasing MRI severity, ranging from 1.0 for minimal lesions to 13.7 for severe lesions (95% confidence interval, 5.0-37.0), according to the study. In contrast, the odds of incident knee radiographic OA (ROA) of the tibiofemoral joint were highest for the “mild” and “severe” groups, which had the most meniscal damage and the most extensive history of knee injury and surgery. Odds ratios for these two groups were 5.6 (95% CI, 3.4-9.4) and 5.0 (95% CI, 2.8-9.0), respectively, said the researchers. “Meniscal damage might play a prominent role in the development of incident ROA in the tibiofemoral joint but not the patellofemoral joint,” they added.
Patients in the MOST study had a high risk of knee OA at baseline, which could limit the generalizability of the findings, Dr. Niu and her associates noted.
The National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Disease, both a part of the National Institutes of Health, supported the study. The investigators did not report conflicts of interest.
FROM ARTHRITIS & RHEUMATISM
Key clinical point: Phenotypes of MRI lesions of the tibiofemoral and patellofemoral joints were differentially associated with risk of incident radiographic osteoarthritis.
Major finding: An MRI of the tibiofemoral and patellofemoral joints revealed minimal, mild, moderate, and severe lesions, with corresponding changes in the odds of incident OA.
Data source: Analysis of cohort data for 885 knees from the multicenter, prospective, observational MOST study.
Disclosures: The National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Disease, both a part of the National Institutes of Health, supported the study. The investigators did not report conflicts of interest.