User login
Which Medications Can Cause Edema?
Edema in the feet and legs is a common complaint in our practices. It can cause pain, weakness, heaviness, discomfort, limited movement, and a negative body image. Medications can contribute to edema, either alone or in combination with other health issues.
Therefore, it is important to know how to treat or prevent medication-induced edema.
There are four main causes of edema, and all can facilitate medication-induced edema.
- Increased capillary pressure. Conditions such as heart failure, renal dysfunction, venous insufficiency, deep vein thrombosis, and cirrhosis can increase capillary pressure, leading to edema.
- Decreased oncotic pressure. Hypoalbuminemia, a primary cause of reduced colloid oncotic pressure, can result from nephrotic syndrome, diabetic nephropathy, lupus nephropathy, amyloidosis, nephropathies, cirrhosis, chronic liver disease, and malabsorption or malnutrition.
- Increased capillary permeability. Vascular injury, often associated with diabetes, can increase capillary permeability and contribute to edema.
- Impaired lymphatic drainage. Lymphatic obstruction is common in patients with lymphedema, tumors, inflammation, fibrosis, certain infections, surgery, and congenital anomalies. Conditions such as thyroid disorders can also cause an increase in interstitial albumin and other proteins without a corresponding increase in lymphatic flow, leading to lymphedema.
Medications That Can Cause Edema
- Calcium channel blockers (CCBs). Drugs such as nifedipine and amlodipine can increase hydrostatic pressure by causing selective vasodilation of precapillary vessels, leading to increased intracapillary pressures. Newer lipophilic CCBs (eg, levamlodipine) exhibit lower rates of edema. Reducing the dose is often effective. Diuretics are not very effective for vasodilation-induced edema. Combining CCBs with angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), which induce postcapillary dilation and normalize intracapillary pressure, may reduce fluid leakage into the interstitial space. This combination may be more beneficial than high-dose CCB monotherapy.
- Thiazolidinedione (eg, pioglitazone). These increase vascular permeability and hydrostatic pressure. They work by stimulating the peroxisome proliferator–activated gamma receptor, increasing vascular endothelial permeability, vascular endothelial growth factor secretion, and renal retention of sodium and fluids. Because of other adverse effects, their use is now limited.
- Agents for neuropathic pain (gabapentin and pregabalin). These drugs can induce selective vasodilation of arterioles through a mechanism similar to that of CCBs, causing increased intracapillary pressures. Edema usually begins within the first month of treatment or dose increase and often regresses after dose reduction or drug discontinuation.
- Antiparkinsonian dopamine agonists. These increase hydrostatic pressure by reducing sympathetic tone and dilating arterioles through alpha-2 adrenergic receptor activity.
- New antipsychotics. Drugs like clozapine, iloperidone, lurasidone, olanzapine, quetiapine, risperidone, and ziprasidone can increase hydrostatic pressure through antagonistic effects on alpha-1 adrenergic receptors, causing vasodilation.
- Nitrates. These drugs increase hydrostatic pressure by causing preferential venous dilation, leading to increased venous pooling.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). These drugs can increase hydrostatic pressure by inhibiting vasodilation of afferent renal arterioles, decreasing the glomerular filtration rate, and stimulating the renin-angiotensin-aldosterone system, which leads to sodium and water retention. These adverse effects warrant cautious use of these agents.
- ACE inhibitors. Drugs such as enalapril and ramipril can increase vascular permeability. They reduce the metabolism and accumulation of bradykinin, which increases vascular permeability and fluid leakage. These effects are rare and are usually related to allergic responses.
- Insulin. Insulin decreases capillary oncotic pressure and increases vascular permeability. Rapid correction of hyperglycemia can cause a loss of oncotic pressure, while chronic hyperglycemia can damage vascular membranes, increasing permeability. These effects are generally benign and can be managed with careful dose titration, sodium restriction, or diuretics.
- Steroids. Steroids with mineralocorticoid activity can increase renal sodium and water retention, leading to increased blood volume. Fludrocortisone has the highest mineralocorticoid activity, while dexamethasone and methylprednisolone have negligible activity.
Implications
Understanding how these medications cause edema is important for effective management. For example, in the case of those causing edema due to reduced oncotic pressure, like insulin, slow dose titrations can help adapt to osmolarity changes. For drugs causing edema due to increased hydrostatic pressure, diuretics are more effective in acute management.
The key takeaways from this review are:
- Awareness of drug-induced edema. Many drugs besides CCBs can cause edema.
- Combination therapy. Combining ACE inhibitors or ARBs with CCBs can prevent or reduce CCB-induced edema.
- Edema management strategies. Strategies to manage or prevent edema should include dose reductions or replacement of the problematic medication, especially in severe or refractory cases.
Dr. Wajngarten, professor of cardiology, University of São Paulo, Brazil, has disclosed no relevant financial relationships.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Edema in the feet and legs is a common complaint in our practices. It can cause pain, weakness, heaviness, discomfort, limited movement, and a negative body image. Medications can contribute to edema, either alone or in combination with other health issues.
Therefore, it is important to know how to treat or prevent medication-induced edema.
There are four main causes of edema, and all can facilitate medication-induced edema.
- Increased capillary pressure. Conditions such as heart failure, renal dysfunction, venous insufficiency, deep vein thrombosis, and cirrhosis can increase capillary pressure, leading to edema.
- Decreased oncotic pressure. Hypoalbuminemia, a primary cause of reduced colloid oncotic pressure, can result from nephrotic syndrome, diabetic nephropathy, lupus nephropathy, amyloidosis, nephropathies, cirrhosis, chronic liver disease, and malabsorption or malnutrition.
- Increased capillary permeability. Vascular injury, often associated with diabetes, can increase capillary permeability and contribute to edema.
- Impaired lymphatic drainage. Lymphatic obstruction is common in patients with lymphedema, tumors, inflammation, fibrosis, certain infections, surgery, and congenital anomalies. Conditions such as thyroid disorders can also cause an increase in interstitial albumin and other proteins without a corresponding increase in lymphatic flow, leading to lymphedema.
Medications That Can Cause Edema
- Calcium channel blockers (CCBs). Drugs such as nifedipine and amlodipine can increase hydrostatic pressure by causing selective vasodilation of precapillary vessels, leading to increased intracapillary pressures. Newer lipophilic CCBs (eg, levamlodipine) exhibit lower rates of edema. Reducing the dose is often effective. Diuretics are not very effective for vasodilation-induced edema. Combining CCBs with angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), which induce postcapillary dilation and normalize intracapillary pressure, may reduce fluid leakage into the interstitial space. This combination may be more beneficial than high-dose CCB monotherapy.
- Thiazolidinedione (eg, pioglitazone). These increase vascular permeability and hydrostatic pressure. They work by stimulating the peroxisome proliferator–activated gamma receptor, increasing vascular endothelial permeability, vascular endothelial growth factor secretion, and renal retention of sodium and fluids. Because of other adverse effects, their use is now limited.
- Agents for neuropathic pain (gabapentin and pregabalin). These drugs can induce selective vasodilation of arterioles through a mechanism similar to that of CCBs, causing increased intracapillary pressures. Edema usually begins within the first month of treatment or dose increase and often regresses after dose reduction or drug discontinuation.
- Antiparkinsonian dopamine agonists. These increase hydrostatic pressure by reducing sympathetic tone and dilating arterioles through alpha-2 adrenergic receptor activity.
- New antipsychotics. Drugs like clozapine, iloperidone, lurasidone, olanzapine, quetiapine, risperidone, and ziprasidone can increase hydrostatic pressure through antagonistic effects on alpha-1 adrenergic receptors, causing vasodilation.
- Nitrates. These drugs increase hydrostatic pressure by causing preferential venous dilation, leading to increased venous pooling.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). These drugs can increase hydrostatic pressure by inhibiting vasodilation of afferent renal arterioles, decreasing the glomerular filtration rate, and stimulating the renin-angiotensin-aldosterone system, which leads to sodium and water retention. These adverse effects warrant cautious use of these agents.
- ACE inhibitors. Drugs such as enalapril and ramipril can increase vascular permeability. They reduce the metabolism and accumulation of bradykinin, which increases vascular permeability and fluid leakage. These effects are rare and are usually related to allergic responses.
- Insulin. Insulin decreases capillary oncotic pressure and increases vascular permeability. Rapid correction of hyperglycemia can cause a loss of oncotic pressure, while chronic hyperglycemia can damage vascular membranes, increasing permeability. These effects are generally benign and can be managed with careful dose titration, sodium restriction, or diuretics.
- Steroids. Steroids with mineralocorticoid activity can increase renal sodium and water retention, leading to increased blood volume. Fludrocortisone has the highest mineralocorticoid activity, while dexamethasone and methylprednisolone have negligible activity.
Implications
Understanding how these medications cause edema is important for effective management. For example, in the case of those causing edema due to reduced oncotic pressure, like insulin, slow dose titrations can help adapt to osmolarity changes. For drugs causing edema due to increased hydrostatic pressure, diuretics are more effective in acute management.
The key takeaways from this review are:
- Awareness of drug-induced edema. Many drugs besides CCBs can cause edema.
- Combination therapy. Combining ACE inhibitors or ARBs with CCBs can prevent or reduce CCB-induced edema.
- Edema management strategies. Strategies to manage or prevent edema should include dose reductions or replacement of the problematic medication, especially in severe or refractory cases.
Dr. Wajngarten, professor of cardiology, University of São Paulo, Brazil, has disclosed no relevant financial relationships.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Edema in the feet and legs is a common complaint in our practices. It can cause pain, weakness, heaviness, discomfort, limited movement, and a negative body image. Medications can contribute to edema, either alone or in combination with other health issues.
Therefore, it is important to know how to treat or prevent medication-induced edema.
There are four main causes of edema, and all can facilitate medication-induced edema.
- Increased capillary pressure. Conditions such as heart failure, renal dysfunction, venous insufficiency, deep vein thrombosis, and cirrhosis can increase capillary pressure, leading to edema.
- Decreased oncotic pressure. Hypoalbuminemia, a primary cause of reduced colloid oncotic pressure, can result from nephrotic syndrome, diabetic nephropathy, lupus nephropathy, amyloidosis, nephropathies, cirrhosis, chronic liver disease, and malabsorption or malnutrition.
- Increased capillary permeability. Vascular injury, often associated with diabetes, can increase capillary permeability and contribute to edema.
- Impaired lymphatic drainage. Lymphatic obstruction is common in patients with lymphedema, tumors, inflammation, fibrosis, certain infections, surgery, and congenital anomalies. Conditions such as thyroid disorders can also cause an increase in interstitial albumin and other proteins without a corresponding increase in lymphatic flow, leading to lymphedema.
Medications That Can Cause Edema
- Calcium channel blockers (CCBs). Drugs such as nifedipine and amlodipine can increase hydrostatic pressure by causing selective vasodilation of precapillary vessels, leading to increased intracapillary pressures. Newer lipophilic CCBs (eg, levamlodipine) exhibit lower rates of edema. Reducing the dose is often effective. Diuretics are not very effective for vasodilation-induced edema. Combining CCBs with angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), which induce postcapillary dilation and normalize intracapillary pressure, may reduce fluid leakage into the interstitial space. This combination may be more beneficial than high-dose CCB monotherapy.
- Thiazolidinedione (eg, pioglitazone). These increase vascular permeability and hydrostatic pressure. They work by stimulating the peroxisome proliferator–activated gamma receptor, increasing vascular endothelial permeability, vascular endothelial growth factor secretion, and renal retention of sodium and fluids. Because of other adverse effects, their use is now limited.
- Agents for neuropathic pain (gabapentin and pregabalin). These drugs can induce selective vasodilation of arterioles through a mechanism similar to that of CCBs, causing increased intracapillary pressures. Edema usually begins within the first month of treatment or dose increase and often regresses after dose reduction or drug discontinuation.
- Antiparkinsonian dopamine agonists. These increase hydrostatic pressure by reducing sympathetic tone and dilating arterioles through alpha-2 adrenergic receptor activity.
- New antipsychotics. Drugs like clozapine, iloperidone, lurasidone, olanzapine, quetiapine, risperidone, and ziprasidone can increase hydrostatic pressure through antagonistic effects on alpha-1 adrenergic receptors, causing vasodilation.
- Nitrates. These drugs increase hydrostatic pressure by causing preferential venous dilation, leading to increased venous pooling.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). These drugs can increase hydrostatic pressure by inhibiting vasodilation of afferent renal arterioles, decreasing the glomerular filtration rate, and stimulating the renin-angiotensin-aldosterone system, which leads to sodium and water retention. These adverse effects warrant cautious use of these agents.
- ACE inhibitors. Drugs such as enalapril and ramipril can increase vascular permeability. They reduce the metabolism and accumulation of bradykinin, which increases vascular permeability and fluid leakage. These effects are rare and are usually related to allergic responses.
- Insulin. Insulin decreases capillary oncotic pressure and increases vascular permeability. Rapid correction of hyperglycemia can cause a loss of oncotic pressure, while chronic hyperglycemia can damage vascular membranes, increasing permeability. These effects are generally benign and can be managed with careful dose titration, sodium restriction, or diuretics.
- Steroids. Steroids with mineralocorticoid activity can increase renal sodium and water retention, leading to increased blood volume. Fludrocortisone has the highest mineralocorticoid activity, while dexamethasone and methylprednisolone have negligible activity.
Implications
Understanding how these medications cause edema is important for effective management. For example, in the case of those causing edema due to reduced oncotic pressure, like insulin, slow dose titrations can help adapt to osmolarity changes. For drugs causing edema due to increased hydrostatic pressure, diuretics are more effective in acute management.
The key takeaways from this review are:
- Awareness of drug-induced edema. Many drugs besides CCBs can cause edema.
- Combination therapy. Combining ACE inhibitors or ARBs with CCBs can prevent or reduce CCB-induced edema.
- Edema management strategies. Strategies to manage or prevent edema should include dose reductions or replacement of the problematic medication, especially in severe or refractory cases.
Dr. Wajngarten, professor of cardiology, University of São Paulo, Brazil, has disclosed no relevant financial relationships.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Vasculopathy Can Vary in Patients With Idiopathic Pulmonary Arterial Hypertension
Approximately half of adults with idiopathic pulmonary arterial hypertension (IPAH) had nonplexiform vasculopathy characterized in part by severe pulmonary microvascular remodeling, based on data from 50 individuals.
The clinical phenotype of IPAH was historically described as a rapidly progressive rare disease in young women and characterized by plexiform lesions, wrote Esther J. Nossent, MD, of Amsterdam University Medical Centers, Amsterdam, the Netherlands, and colleagues. However, the patient population with IPAH has become older and predominantly men, and the nature of vascular phenotypes and histologic patterns in patients with contemporary IPAH has not been well studied, the researchers said.
In a cross-sectional study published in CHEST, the researchers reviewed lung histology data from 50 adults with IPAH that had been assessed by two experienced pathologists. The mean age of the patients was 52 years and 58% were women. Based on a histopathologic evaluation, 24 patients had nonplexiform vasculopathy (48%) and 26 had plexiform vasculopathy (52%). Notably, microvascular remodeling involving arterioles and venules was substantial in patients with nonplexiform vasculopathy but mild or absent in those with plexiform vasculopathy, the researchers wrote.
The researchers also compared the clinical characteristics of patients with plexiform vs nonplexiform vasculopathy. Hemodynamic parameters were similar in both patient groups. However, those with nonplexiform vasculopathy were significantly older than those with plexiform vasculopathy (60 years vs 44 years), were more likely to be men (67% vs 20%), and had a lower diffusing capacity of the lungs for carbon monoxide (DLCO) at diagnosis (all P < .001). Patients with nonplexiform vasculopathy also were significantly more likely than those with plexiform vasculopathy to have a history of smoking (P = .03). Genetic testing revealed no mutations in established PAH genes in the nonplexiform group.
Low DLCO has been associated with worse outcomes regardless of hemodynamic response, the researchers noted. In the current study, “a DLCO of < 45% almost perfectly identified patients with nonplexiform vasculopathy with prominent pulmonary microvascular disease,” they said.
The findings were limited by several factors, including the small study population and the higher frequency of surgical lung biopsies in the nonplexiform group vs the plexiform group, which is not part of the general workup of patients with IPAH, the researchers noted.
, they said. However, the results suggest that differences between patients with IPAH with plexiform vasculopathy and those with nonplexiform vasculopathy could ultimately inform targeted treatment strategies.
“Recognizing these clinical phenotypes allows revisiting current datasets to understand better the potential future clinical consequences of the vascular phenotypes for treatment response and clinical outcome,” the researchers concluded.
Findings May Inform More Targeted Therapy
“Any investigation that adds substantive insight into a complex disease that can translate into a better understanding of clinical patient phenotypes and eventually into improved treatments and patient outcomes has relevance at any time,” Paul Forfia, MD, professor of medicine at the Lewis Katz School of Medicine at Temple University, Philadelphia, said in an interview.
“There is focus on the antiproliferative forms of pulmonary arterial hypertension–specific therapy, and the results of the current study may have implications to these therapies,” said Dr. Forfia, who was not involved in the current study.
“In the current study, the investigators show that 48% of patients that were traditionally categorized as IPAH had a vascular phenotype that is not considered ‘typical’ or classic for IPAH,” Dr. Forfia told this news organization. “These findings highlight a significant heterogeneity of the pulmonary vascular phenotype within IPAH, which raises the question of whether the nonplexiform patient would be less responsive to the novel, antiproliferative forms of therapy,” he said.
The new findings are quite interesting but not surprising, Dr. Forfia said. “The World Symposia diagnostic groupings for pulmonary hypertension are a very important and necessary form of categorization and differentiation amongst forms of PH [pulmonary hypertension], and these groupings make a best attempt based on available evidence to separate patients of varying PH pathophysiology, both in terms of diagnosis and in how PH patients are treated,” he explained.
“However, clinical experts in PH have known that subphenotypes of PH pathophysiology exist within group I PAH, as well as in PH related to left heart disease (group 2), chronic respiratory disease (group 3), and chronic thromboembolic disease (group 4),” he said.
Findings from the current study reinforce the importance of clinical and physiological phenotyping of each patient, which can help in terms of therapy selection and in managing expectations in response to therapy, Dr. Forfia added.
“Perhaps the most evident and important clinical implication from the current study is to remind clinicians treating patients with PH that heterogeneity exists within the vascular phenotype and clinical makeup of patients even within the same type of PAH,” Dr. Forfia said. “With this insight, clinicians are more informed and thus more apt to consider nuances in the diagnosis, treatment, and expectations for treatment response within PAH,” he said.
Dr. Forfia also highlighted the potential implications of the association between cigarette smoking and the nonplexiform vascular phenotype. “This association was present in the absence of radiographic evidence of emphysema and raises the provocative notion that cigarette smoking may lead to pulmonary vascular abnormalities, perhaps even PAH, in patients without a diagnosis of emphysema,” he said.
“An important limitation from the current study is that the vascular phenotypes observed within their cohort of IPAH patients were obtained from histopathology specimens at the time of autopsy, explant at the time of lung transplantation, and surgical lung biopsy spanning over a 22-year period,” Dr. Forfia noted. Additional research is needed to explore how vascular phenotypic differences can be appreciated in the absence of histopathology and how these differences could impact therapy selection and patient outcomes, he said.
The study received no outside funding. Dr. Nossent disclosed receiving speaker fees from Janssen, MSD, and United Therapeutics/Ferrer and consulting fees from Janssen and United Therapeutics/Ferrer. Dr. Forfia had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Approximately half of adults with idiopathic pulmonary arterial hypertension (IPAH) had nonplexiform vasculopathy characterized in part by severe pulmonary microvascular remodeling, based on data from 50 individuals.
The clinical phenotype of IPAH was historically described as a rapidly progressive rare disease in young women and characterized by plexiform lesions, wrote Esther J. Nossent, MD, of Amsterdam University Medical Centers, Amsterdam, the Netherlands, and colleagues. However, the patient population with IPAH has become older and predominantly men, and the nature of vascular phenotypes and histologic patterns in patients with contemporary IPAH has not been well studied, the researchers said.
In a cross-sectional study published in CHEST, the researchers reviewed lung histology data from 50 adults with IPAH that had been assessed by two experienced pathologists. The mean age of the patients was 52 years and 58% were women. Based on a histopathologic evaluation, 24 patients had nonplexiform vasculopathy (48%) and 26 had plexiform vasculopathy (52%). Notably, microvascular remodeling involving arterioles and venules was substantial in patients with nonplexiform vasculopathy but mild or absent in those with plexiform vasculopathy, the researchers wrote.
The researchers also compared the clinical characteristics of patients with plexiform vs nonplexiform vasculopathy. Hemodynamic parameters were similar in both patient groups. However, those with nonplexiform vasculopathy were significantly older than those with plexiform vasculopathy (60 years vs 44 years), were more likely to be men (67% vs 20%), and had a lower diffusing capacity of the lungs for carbon monoxide (DLCO) at diagnosis (all P < .001). Patients with nonplexiform vasculopathy also were significantly more likely than those with plexiform vasculopathy to have a history of smoking (P = .03). Genetic testing revealed no mutations in established PAH genes in the nonplexiform group.
Low DLCO has been associated with worse outcomes regardless of hemodynamic response, the researchers noted. In the current study, “a DLCO of < 45% almost perfectly identified patients with nonplexiform vasculopathy with prominent pulmonary microvascular disease,” they said.
The findings were limited by several factors, including the small study population and the higher frequency of surgical lung biopsies in the nonplexiform group vs the plexiform group, which is not part of the general workup of patients with IPAH, the researchers noted.
, they said. However, the results suggest that differences between patients with IPAH with plexiform vasculopathy and those with nonplexiform vasculopathy could ultimately inform targeted treatment strategies.
“Recognizing these clinical phenotypes allows revisiting current datasets to understand better the potential future clinical consequences of the vascular phenotypes for treatment response and clinical outcome,” the researchers concluded.
Findings May Inform More Targeted Therapy
“Any investigation that adds substantive insight into a complex disease that can translate into a better understanding of clinical patient phenotypes and eventually into improved treatments and patient outcomes has relevance at any time,” Paul Forfia, MD, professor of medicine at the Lewis Katz School of Medicine at Temple University, Philadelphia, said in an interview.
“There is focus on the antiproliferative forms of pulmonary arterial hypertension–specific therapy, and the results of the current study may have implications to these therapies,” said Dr. Forfia, who was not involved in the current study.
“In the current study, the investigators show that 48% of patients that were traditionally categorized as IPAH had a vascular phenotype that is not considered ‘typical’ or classic for IPAH,” Dr. Forfia told this news organization. “These findings highlight a significant heterogeneity of the pulmonary vascular phenotype within IPAH, which raises the question of whether the nonplexiform patient would be less responsive to the novel, antiproliferative forms of therapy,” he said.
The new findings are quite interesting but not surprising, Dr. Forfia said. “The World Symposia diagnostic groupings for pulmonary hypertension are a very important and necessary form of categorization and differentiation amongst forms of PH [pulmonary hypertension], and these groupings make a best attempt based on available evidence to separate patients of varying PH pathophysiology, both in terms of diagnosis and in how PH patients are treated,” he explained.
“However, clinical experts in PH have known that subphenotypes of PH pathophysiology exist within group I PAH, as well as in PH related to left heart disease (group 2), chronic respiratory disease (group 3), and chronic thromboembolic disease (group 4),” he said.
Findings from the current study reinforce the importance of clinical and physiological phenotyping of each patient, which can help in terms of therapy selection and in managing expectations in response to therapy, Dr. Forfia added.
“Perhaps the most evident and important clinical implication from the current study is to remind clinicians treating patients with PH that heterogeneity exists within the vascular phenotype and clinical makeup of patients even within the same type of PAH,” Dr. Forfia said. “With this insight, clinicians are more informed and thus more apt to consider nuances in the diagnosis, treatment, and expectations for treatment response within PAH,” he said.
Dr. Forfia also highlighted the potential implications of the association between cigarette smoking and the nonplexiform vascular phenotype. “This association was present in the absence of radiographic evidence of emphysema and raises the provocative notion that cigarette smoking may lead to pulmonary vascular abnormalities, perhaps even PAH, in patients without a diagnosis of emphysema,” he said.
“An important limitation from the current study is that the vascular phenotypes observed within their cohort of IPAH patients were obtained from histopathology specimens at the time of autopsy, explant at the time of lung transplantation, and surgical lung biopsy spanning over a 22-year period,” Dr. Forfia noted. Additional research is needed to explore how vascular phenotypic differences can be appreciated in the absence of histopathology and how these differences could impact therapy selection and patient outcomes, he said.
The study received no outside funding. Dr. Nossent disclosed receiving speaker fees from Janssen, MSD, and United Therapeutics/Ferrer and consulting fees from Janssen and United Therapeutics/Ferrer. Dr. Forfia had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Approximately half of adults with idiopathic pulmonary arterial hypertension (IPAH) had nonplexiform vasculopathy characterized in part by severe pulmonary microvascular remodeling, based on data from 50 individuals.
The clinical phenotype of IPAH was historically described as a rapidly progressive rare disease in young women and characterized by plexiform lesions, wrote Esther J. Nossent, MD, of Amsterdam University Medical Centers, Amsterdam, the Netherlands, and colleagues. However, the patient population with IPAH has become older and predominantly men, and the nature of vascular phenotypes and histologic patterns in patients with contemporary IPAH has not been well studied, the researchers said.
In a cross-sectional study published in CHEST, the researchers reviewed lung histology data from 50 adults with IPAH that had been assessed by two experienced pathologists. The mean age of the patients was 52 years and 58% were women. Based on a histopathologic evaluation, 24 patients had nonplexiform vasculopathy (48%) and 26 had plexiform vasculopathy (52%). Notably, microvascular remodeling involving arterioles and venules was substantial in patients with nonplexiform vasculopathy but mild or absent in those with plexiform vasculopathy, the researchers wrote.
The researchers also compared the clinical characteristics of patients with plexiform vs nonplexiform vasculopathy. Hemodynamic parameters were similar in both patient groups. However, those with nonplexiform vasculopathy were significantly older than those with plexiform vasculopathy (60 years vs 44 years), were more likely to be men (67% vs 20%), and had a lower diffusing capacity of the lungs for carbon monoxide (DLCO) at diagnosis (all P < .001). Patients with nonplexiform vasculopathy also were significantly more likely than those with plexiform vasculopathy to have a history of smoking (P = .03). Genetic testing revealed no mutations in established PAH genes in the nonplexiform group.
Low DLCO has been associated with worse outcomes regardless of hemodynamic response, the researchers noted. In the current study, “a DLCO of < 45% almost perfectly identified patients with nonplexiform vasculopathy with prominent pulmonary microvascular disease,” they said.
The findings were limited by several factors, including the small study population and the higher frequency of surgical lung biopsies in the nonplexiform group vs the plexiform group, which is not part of the general workup of patients with IPAH, the researchers noted.
, they said. However, the results suggest that differences between patients with IPAH with plexiform vasculopathy and those with nonplexiform vasculopathy could ultimately inform targeted treatment strategies.
“Recognizing these clinical phenotypes allows revisiting current datasets to understand better the potential future clinical consequences of the vascular phenotypes for treatment response and clinical outcome,” the researchers concluded.
Findings May Inform More Targeted Therapy
“Any investigation that adds substantive insight into a complex disease that can translate into a better understanding of clinical patient phenotypes and eventually into improved treatments and patient outcomes has relevance at any time,” Paul Forfia, MD, professor of medicine at the Lewis Katz School of Medicine at Temple University, Philadelphia, said in an interview.
“There is focus on the antiproliferative forms of pulmonary arterial hypertension–specific therapy, and the results of the current study may have implications to these therapies,” said Dr. Forfia, who was not involved in the current study.
“In the current study, the investigators show that 48% of patients that were traditionally categorized as IPAH had a vascular phenotype that is not considered ‘typical’ or classic for IPAH,” Dr. Forfia told this news organization. “These findings highlight a significant heterogeneity of the pulmonary vascular phenotype within IPAH, which raises the question of whether the nonplexiform patient would be less responsive to the novel, antiproliferative forms of therapy,” he said.
The new findings are quite interesting but not surprising, Dr. Forfia said. “The World Symposia diagnostic groupings for pulmonary hypertension are a very important and necessary form of categorization and differentiation amongst forms of PH [pulmonary hypertension], and these groupings make a best attempt based on available evidence to separate patients of varying PH pathophysiology, both in terms of diagnosis and in how PH patients are treated,” he explained.
“However, clinical experts in PH have known that subphenotypes of PH pathophysiology exist within group I PAH, as well as in PH related to left heart disease (group 2), chronic respiratory disease (group 3), and chronic thromboembolic disease (group 4),” he said.
Findings from the current study reinforce the importance of clinical and physiological phenotyping of each patient, which can help in terms of therapy selection and in managing expectations in response to therapy, Dr. Forfia added.
“Perhaps the most evident and important clinical implication from the current study is to remind clinicians treating patients with PH that heterogeneity exists within the vascular phenotype and clinical makeup of patients even within the same type of PAH,” Dr. Forfia said. “With this insight, clinicians are more informed and thus more apt to consider nuances in the diagnosis, treatment, and expectations for treatment response within PAH,” he said.
Dr. Forfia also highlighted the potential implications of the association between cigarette smoking and the nonplexiform vascular phenotype. “This association was present in the absence of radiographic evidence of emphysema and raises the provocative notion that cigarette smoking may lead to pulmonary vascular abnormalities, perhaps even PAH, in patients without a diagnosis of emphysema,” he said.
“An important limitation from the current study is that the vascular phenotypes observed within their cohort of IPAH patients were obtained from histopathology specimens at the time of autopsy, explant at the time of lung transplantation, and surgical lung biopsy spanning over a 22-year period,” Dr. Forfia noted. Additional research is needed to explore how vascular phenotypic differences can be appreciated in the absence of histopathology and how these differences could impact therapy selection and patient outcomes, he said.
The study received no outside funding. Dr. Nossent disclosed receiving speaker fees from Janssen, MSD, and United Therapeutics/Ferrer and consulting fees from Janssen and United Therapeutics/Ferrer. Dr. Forfia had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
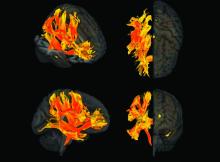
High Blood Sugar May Drive Dementia, German Researchers Warn
On World Brain Day (July 22, 2024), the German Society of Neurology (DGN) and the German Brain Foundation pointed out that too much sugar can harm the brain. The current results of the Global Burden of Diseases study shows that stroke and dementia are among the top 10 causes of death. A healthy, active lifestyle with sufficient exercise and sleep, along with the avoidance of harmful substances like alcohol, nicotine, or excessive sugar, protects the brain.
“Of course, the dose makes the poison as the brain, being the body’s powerhouse, needs glucose to function,” said Frank Erbguth, MD, PhD, president of the German Brain Foundation, in a press release from DGN and the German Brain Foundation. “However, with a permanent increase in blood sugar levels due to too many, too lavish meals and constant snacking on the side, we overload the system and fuel the development of neurologic diseases, particularly dementia and stroke.”
The per capita consumption of sugar was 33.2 kg in 2021/2022, which is almost twice the recommended amount. The German Nutrition Society recommends that no more than 10% of energy come from sugar. With a goal of 2000 kilocalories, that’s 50 g per day, or 18 kg per year. This total includes not only added sugar but also naturally occurring sugar, such as in fruits, honey, or juices.
What’s the Mechanism?
In Germany, around 250,000 people are diagnosed with dementia annually, and 15%-25% have vascular dementia. That proportion represents between 40,000 and 60,000 new cases each year.
In addition, glycosaminoglycans, which are complex sugar molecules, can directly impair cognition. They affect the function of synapses between nerve cells and, thus, affect neuronal plasticity. Experimental data presented at the 2023 American Chemical Society Congress have shown this phenomenon.
Twenty years ago, a study provided evidence that a diet high in fat and sugar disrupts neuronal plasticity and can impair the function of the hippocampus in the long term. A recent meta-analysis confirms these findings: Although mental performance improves at 2-12 hours after sugar consumption, sustained sugar intake can permanently damage cognitive function.
Diabetes mellitus can indirectly cause brain damage. Since the 1990s, it has been known that patients with type 2 diabetes have a significantly higher risk for dementia. It is suspected that glucose metabolism is also disrupted in neurons, thus contributing to the development of Alzheimer’s disease. Insulin also plays a role in the formation of Alzheimer’s plaques.
The Max Planck Institute for Metabolism Research demonstrated in 2023 that regular consumption of high-sugar and high-fat foods can change the brain. This leads to an increased craving for high-sugar and high-fat foods, which in turn promotes the development of obesity and type 2 diabetes.
Reduce Sugar Consumption
DGN and the German Brain Foundation advise minimizing sugar consumption. This process is often challenging, as even a small dose of sugar can trigger the gut to send signals to the brain via the vagus nerve, thus causing a strong craving for more sugar. “This could be the reason why some people quickly eat a whole chocolate bar after just one piece,” said Dr. Erbguth. In addition, dopamine, a “feel-good hormone,” is released in the brain when consuming sugar, thus leading to a desire for more.
“It is wise to break free from this cycle by largely avoiding sugar,” said Peter Berlit, MD, secretary general and spokesperson for DGN. “The effort is worth it, as 40% of all dementia cases and 90% of all strokes are preventable, with many of them linked to industrial sugar,” said Dr. Berlit. DGN and the German Brain Foundation support the call for a tax on particularly sugary beverages. They also pointed out that foods like yogurt or tomato ketchup contain sugar, and alcohol can also significantly raise blood sugar levels.
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
On World Brain Day (July 22, 2024), the German Society of Neurology (DGN) and the German Brain Foundation pointed out that too much sugar can harm the brain. The current results of the Global Burden of Diseases study shows that stroke and dementia are among the top 10 causes of death. A healthy, active lifestyle with sufficient exercise and sleep, along with the avoidance of harmful substances like alcohol, nicotine, or excessive sugar, protects the brain.
“Of course, the dose makes the poison as the brain, being the body’s powerhouse, needs glucose to function,” said Frank Erbguth, MD, PhD, president of the German Brain Foundation, in a press release from DGN and the German Brain Foundation. “However, with a permanent increase in blood sugar levels due to too many, too lavish meals and constant snacking on the side, we overload the system and fuel the development of neurologic diseases, particularly dementia and stroke.”
The per capita consumption of sugar was 33.2 kg in 2021/2022, which is almost twice the recommended amount. The German Nutrition Society recommends that no more than 10% of energy come from sugar. With a goal of 2000 kilocalories, that’s 50 g per day, or 18 kg per year. This total includes not only added sugar but also naturally occurring sugar, such as in fruits, honey, or juices.
What’s the Mechanism?
In Germany, around 250,000 people are diagnosed with dementia annually, and 15%-25% have vascular dementia. That proportion represents between 40,000 and 60,000 new cases each year.
In addition, glycosaminoglycans, which are complex sugar molecules, can directly impair cognition. They affect the function of synapses between nerve cells and, thus, affect neuronal plasticity. Experimental data presented at the 2023 American Chemical Society Congress have shown this phenomenon.
Twenty years ago, a study provided evidence that a diet high in fat and sugar disrupts neuronal plasticity and can impair the function of the hippocampus in the long term. A recent meta-analysis confirms these findings: Although mental performance improves at 2-12 hours after sugar consumption, sustained sugar intake can permanently damage cognitive function.
Diabetes mellitus can indirectly cause brain damage. Since the 1990s, it has been known that patients with type 2 diabetes have a significantly higher risk for dementia. It is suspected that glucose metabolism is also disrupted in neurons, thus contributing to the development of Alzheimer’s disease. Insulin also plays a role in the formation of Alzheimer’s plaques.
The Max Planck Institute for Metabolism Research demonstrated in 2023 that regular consumption of high-sugar and high-fat foods can change the brain. This leads to an increased craving for high-sugar and high-fat foods, which in turn promotes the development of obesity and type 2 diabetes.
Reduce Sugar Consumption
DGN and the German Brain Foundation advise minimizing sugar consumption. This process is often challenging, as even a small dose of sugar can trigger the gut to send signals to the brain via the vagus nerve, thus causing a strong craving for more sugar. “This could be the reason why some people quickly eat a whole chocolate bar after just one piece,” said Dr. Erbguth. In addition, dopamine, a “feel-good hormone,” is released in the brain when consuming sugar, thus leading to a desire for more.
“It is wise to break free from this cycle by largely avoiding sugar,” said Peter Berlit, MD, secretary general and spokesperson for DGN. “The effort is worth it, as 40% of all dementia cases and 90% of all strokes are preventable, with many of them linked to industrial sugar,” said Dr. Berlit. DGN and the German Brain Foundation support the call for a tax on particularly sugary beverages. They also pointed out that foods like yogurt or tomato ketchup contain sugar, and alcohol can also significantly raise blood sugar levels.
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
On World Brain Day (July 22, 2024), the German Society of Neurology (DGN) and the German Brain Foundation pointed out that too much sugar can harm the brain. The current results of the Global Burden of Diseases study shows that stroke and dementia are among the top 10 causes of death. A healthy, active lifestyle with sufficient exercise and sleep, along with the avoidance of harmful substances like alcohol, nicotine, or excessive sugar, protects the brain.
“Of course, the dose makes the poison as the brain, being the body’s powerhouse, needs glucose to function,” said Frank Erbguth, MD, PhD, president of the German Brain Foundation, in a press release from DGN and the German Brain Foundation. “However, with a permanent increase in blood sugar levels due to too many, too lavish meals and constant snacking on the side, we overload the system and fuel the development of neurologic diseases, particularly dementia and stroke.”
The per capita consumption of sugar was 33.2 kg in 2021/2022, which is almost twice the recommended amount. The German Nutrition Society recommends that no more than 10% of energy come from sugar. With a goal of 2000 kilocalories, that’s 50 g per day, or 18 kg per year. This total includes not only added sugar but also naturally occurring sugar, such as in fruits, honey, or juices.
What’s the Mechanism?
In Germany, around 250,000 people are diagnosed with dementia annually, and 15%-25% have vascular dementia. That proportion represents between 40,000 and 60,000 new cases each year.
In addition, glycosaminoglycans, which are complex sugar molecules, can directly impair cognition. They affect the function of synapses between nerve cells and, thus, affect neuronal plasticity. Experimental data presented at the 2023 American Chemical Society Congress have shown this phenomenon.
Twenty years ago, a study provided evidence that a diet high in fat and sugar disrupts neuronal plasticity and can impair the function of the hippocampus in the long term. A recent meta-analysis confirms these findings: Although mental performance improves at 2-12 hours after sugar consumption, sustained sugar intake can permanently damage cognitive function.
Diabetes mellitus can indirectly cause brain damage. Since the 1990s, it has been known that patients with type 2 diabetes have a significantly higher risk for dementia. It is suspected that glucose metabolism is also disrupted in neurons, thus contributing to the development of Alzheimer’s disease. Insulin also plays a role in the formation of Alzheimer’s plaques.
The Max Planck Institute for Metabolism Research demonstrated in 2023 that regular consumption of high-sugar and high-fat foods can change the brain. This leads to an increased craving for high-sugar and high-fat foods, which in turn promotes the development of obesity and type 2 diabetes.
Reduce Sugar Consumption
DGN and the German Brain Foundation advise minimizing sugar consumption. This process is often challenging, as even a small dose of sugar can trigger the gut to send signals to the brain via the vagus nerve, thus causing a strong craving for more sugar. “This could be the reason why some people quickly eat a whole chocolate bar after just one piece,” said Dr. Erbguth. In addition, dopamine, a “feel-good hormone,” is released in the brain when consuming sugar, thus leading to a desire for more.
“It is wise to break free from this cycle by largely avoiding sugar,” said Peter Berlit, MD, secretary general and spokesperson for DGN. “The effort is worth it, as 40% of all dementia cases and 90% of all strokes are preventable, with many of them linked to industrial sugar,” said Dr. Berlit. DGN and the German Brain Foundation support the call for a tax on particularly sugary beverages. They also pointed out that foods like yogurt or tomato ketchup contain sugar, and alcohol can also significantly raise blood sugar levels.
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Arterial Stiffness May Predict Risk for Glaucoma
TOPLINE:
Arterial stiffness increases the risk for developing glaucoma, a new study found.
METHODOLOGY:
- To study the link between arterial stiffness and glaucoma, the researchers evaluated 4713 individuals (mean age, 66 years; 58% men) without the eye condition at baseline between April 2011 and November 2012.
- They assessed arterial stiffness by measuring aortic pulse wave velocity, estimated carotid-femoral pulse wave velocity, and aortic pulse pressure.
- The primary outcome was incident glaucoma, identified from prescriptions for eye drops or hospital records.
TAKEAWAY:
- Overall, 301 people in the study developed glaucoma over a mean follow-up period of 10.5 years.
- Incident glaucoma increased across all quartiles of arterial stiffness, with the highest risk observed in the fourth quartile for aortic pulse wave velocity (HR, 2.41; 95% CI, 1.36-4.26), estimated carotid-femoral pulse wave velocity (HR, 2.29; 95% CI, 1.27-4.13), and aortic pulse pressure (HR, 1.76; 95% CI, 1.10-2.82).
- The cumulative incidence of glaucoma rose with increases in arterial stiffness. This trend was statistically significant for both aortic and estimated pulse wave velocity (P < .0001) and aortic pulse pressure (P = .02).
IN PRACTICE:
“Arterial stiffness…which can be easily and accurately measured, could be used as a tool in clinical practice [as part of routine blood pressure measurement] to help identify people at risk of glaucoma and as a therapeutic target to prevent glaucoma progression,” the authors wrote.
SOURCE:
This study was led by Angela L. Beros, MPH, of the School of Population Health at the University of Auckland, Auckland, New Zealand, and published online in the American Journal of Ophthalmology.
LIMITATIONS:
The cohort study did not clinically assess for glaucoma, potentially leading to the inclusion of individuals with the condition. Not all participants with incident glaucoma, particularly those unaware of their diagnosis, may have been identified. Intraocular pressure and central corneal thickness, which are common risk factors for glaucoma, were not included in the multivariate analysis.
DISCLOSURES:
The study did not receive any funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Arterial stiffness increases the risk for developing glaucoma, a new study found.
METHODOLOGY:
- To study the link between arterial stiffness and glaucoma, the researchers evaluated 4713 individuals (mean age, 66 years; 58% men) without the eye condition at baseline between April 2011 and November 2012.
- They assessed arterial stiffness by measuring aortic pulse wave velocity, estimated carotid-femoral pulse wave velocity, and aortic pulse pressure.
- The primary outcome was incident glaucoma, identified from prescriptions for eye drops or hospital records.
TAKEAWAY:
- Overall, 301 people in the study developed glaucoma over a mean follow-up period of 10.5 years.
- Incident glaucoma increased across all quartiles of arterial stiffness, with the highest risk observed in the fourth quartile for aortic pulse wave velocity (HR, 2.41; 95% CI, 1.36-4.26), estimated carotid-femoral pulse wave velocity (HR, 2.29; 95% CI, 1.27-4.13), and aortic pulse pressure (HR, 1.76; 95% CI, 1.10-2.82).
- The cumulative incidence of glaucoma rose with increases in arterial stiffness. This trend was statistically significant for both aortic and estimated pulse wave velocity (P < .0001) and aortic pulse pressure (P = .02).
IN PRACTICE:
“Arterial stiffness…which can be easily and accurately measured, could be used as a tool in clinical practice [as part of routine blood pressure measurement] to help identify people at risk of glaucoma and as a therapeutic target to prevent glaucoma progression,” the authors wrote.
SOURCE:
This study was led by Angela L. Beros, MPH, of the School of Population Health at the University of Auckland, Auckland, New Zealand, and published online in the American Journal of Ophthalmology.
LIMITATIONS:
The cohort study did not clinically assess for glaucoma, potentially leading to the inclusion of individuals with the condition. Not all participants with incident glaucoma, particularly those unaware of their diagnosis, may have been identified. Intraocular pressure and central corneal thickness, which are common risk factors for glaucoma, were not included in the multivariate analysis.
DISCLOSURES:
The study did not receive any funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Arterial stiffness increases the risk for developing glaucoma, a new study found.
METHODOLOGY:
- To study the link between arterial stiffness and glaucoma, the researchers evaluated 4713 individuals (mean age, 66 years; 58% men) without the eye condition at baseline between April 2011 and November 2012.
- They assessed arterial stiffness by measuring aortic pulse wave velocity, estimated carotid-femoral pulse wave velocity, and aortic pulse pressure.
- The primary outcome was incident glaucoma, identified from prescriptions for eye drops or hospital records.
TAKEAWAY:
- Overall, 301 people in the study developed glaucoma over a mean follow-up period of 10.5 years.
- Incident glaucoma increased across all quartiles of arterial stiffness, with the highest risk observed in the fourth quartile for aortic pulse wave velocity (HR, 2.41; 95% CI, 1.36-4.26), estimated carotid-femoral pulse wave velocity (HR, 2.29; 95% CI, 1.27-4.13), and aortic pulse pressure (HR, 1.76; 95% CI, 1.10-2.82).
- The cumulative incidence of glaucoma rose with increases in arterial stiffness. This trend was statistically significant for both aortic and estimated pulse wave velocity (P < .0001) and aortic pulse pressure (P = .02).
IN PRACTICE:
“Arterial stiffness…which can be easily and accurately measured, could be used as a tool in clinical practice [as part of routine blood pressure measurement] to help identify people at risk of glaucoma and as a therapeutic target to prevent glaucoma progression,” the authors wrote.
SOURCE:
This study was led by Angela L. Beros, MPH, of the School of Population Health at the University of Auckland, Auckland, New Zealand, and published online in the American Journal of Ophthalmology.
LIMITATIONS:
The cohort study did not clinically assess for glaucoma, potentially leading to the inclusion of individuals with the condition. Not all participants with incident glaucoma, particularly those unaware of their diagnosis, may have been identified. Intraocular pressure and central corneal thickness, which are common risk factors for glaucoma, were not included in the multivariate analysis.
DISCLOSURES:
The study did not receive any funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
Home-based exercise benefits patients with PAD
TOPLINE:
Compared with supervised treadmill workouts at a gym, which is considered first-line therapy for walking impairment in lower extremity peripheral artery disease (PAD), exercising at home significantly improves 6-minute walking (6MW) distance, but not maximal treadmill walking distance, results of a new meta-analysis show.
METHODOLOGY:
- The analysis included five randomized clinical trials with a total of 719 participants, mean age 68.6 years, all led by researchers at Northwestern University, Chicago, that compared either supervised treadmill or home-based walking exercise with a nonexercise control group in people with PAD (defined as Ankle Brachial Index ≤ 0.90).
- All trials measured 6-minute walk (6MW) distance (walking as far as possible in 6 minutes), treadmill walking performance, and outcomes from the Walking Impairment Questionnaire (WIQ), which includes distance, walking speed, and stair-climbing domains, at baseline and at 6 months.
- Supervised treadmill exercise interventions included three individualized exercise sessions per week with an exercise physiologist at an exercise center, and home-based exercises involved walking near home 5 days per week, both for up to 50 minutes per session.
TAKEAWAY:
- After adjusting for study, age, sex, race, smoking, history of myocardial infarction, heart failure, and baseline 6MW distance, the study found both exercise interventions were better than nonexercise controls for 6MW distance.
- Compared with supervised treadmill exercise, home-based walking was associated with significantly improved mean 6MW distance (31.8 m vs. 55.6 m; adjusted between-group difference: −23.8 m; 95% confidence interval, −44.0 to −3.6; P = .021), and significantly improved WIQ walking speed score.
- However, home-based walking was associated with significantly less improvement in maximal treadmill walking distance, compared with supervised treadmill exercise (adjusted between-group difference: 132.5 m; 95% CI, 72.1-192.9; P < .001).
IN PRACTICE:
Home-based walking exercise “circumvents” barriers to accessing supervised exercise such as having to travel to a facility, said the authors, who noted the new data “demonstrated a large and consistent effect of home-based walking exercise on improved 6MW distance and also significantly improved the WIQ walking speed score, compared with supervised treadmill exercise.”
SOURCE:
The study was conducted by Neela D. Thangada, MD, Northwestern University, Chicago, and colleagues. It was published online in JAMA Network Open.
LIMITATIONS:
Data were combined from different randomized clinical trials that were led by one investigative team, and reported comparisons were not prespecified. Comparisons between supervised and home-based exercise lacked statistical power for the WIQ distance and stair-climbing measures.
DISCLOSURES:
The study was sponsored by the National Center for Research Resources and the National Heart, Lung, and Blood Institute of the National Institutes of Health. Dr. Thangada reports no relevant financial relationships. Disclosures for study coauthors can be found with the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
Compared with supervised treadmill workouts at a gym, which is considered first-line therapy for walking impairment in lower extremity peripheral artery disease (PAD), exercising at home significantly improves 6-minute walking (6MW) distance, but not maximal treadmill walking distance, results of a new meta-analysis show.
METHODOLOGY:
- The analysis included five randomized clinical trials with a total of 719 participants, mean age 68.6 years, all led by researchers at Northwestern University, Chicago, that compared either supervised treadmill or home-based walking exercise with a nonexercise control group in people with PAD (defined as Ankle Brachial Index ≤ 0.90).
- All trials measured 6-minute walk (6MW) distance (walking as far as possible in 6 minutes), treadmill walking performance, and outcomes from the Walking Impairment Questionnaire (WIQ), which includes distance, walking speed, and stair-climbing domains, at baseline and at 6 months.
- Supervised treadmill exercise interventions included three individualized exercise sessions per week with an exercise physiologist at an exercise center, and home-based exercises involved walking near home 5 days per week, both for up to 50 minutes per session.
TAKEAWAY:
- After adjusting for study, age, sex, race, smoking, history of myocardial infarction, heart failure, and baseline 6MW distance, the study found both exercise interventions were better than nonexercise controls for 6MW distance.
- Compared with supervised treadmill exercise, home-based walking was associated with significantly improved mean 6MW distance (31.8 m vs. 55.6 m; adjusted between-group difference: −23.8 m; 95% confidence interval, −44.0 to −3.6; P = .021), and significantly improved WIQ walking speed score.
- However, home-based walking was associated with significantly less improvement in maximal treadmill walking distance, compared with supervised treadmill exercise (adjusted between-group difference: 132.5 m; 95% CI, 72.1-192.9; P < .001).
IN PRACTICE:
Home-based walking exercise “circumvents” barriers to accessing supervised exercise such as having to travel to a facility, said the authors, who noted the new data “demonstrated a large and consistent effect of home-based walking exercise on improved 6MW distance and also significantly improved the WIQ walking speed score, compared with supervised treadmill exercise.”
SOURCE:
The study was conducted by Neela D. Thangada, MD, Northwestern University, Chicago, and colleagues. It was published online in JAMA Network Open.
LIMITATIONS:
Data were combined from different randomized clinical trials that were led by one investigative team, and reported comparisons were not prespecified. Comparisons between supervised and home-based exercise lacked statistical power for the WIQ distance and stair-climbing measures.
DISCLOSURES:
The study was sponsored by the National Center for Research Resources and the National Heart, Lung, and Blood Institute of the National Institutes of Health. Dr. Thangada reports no relevant financial relationships. Disclosures for study coauthors can be found with the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
Compared with supervised treadmill workouts at a gym, which is considered first-line therapy for walking impairment in lower extremity peripheral artery disease (PAD), exercising at home significantly improves 6-minute walking (6MW) distance, but not maximal treadmill walking distance, results of a new meta-analysis show.
METHODOLOGY:
- The analysis included five randomized clinical trials with a total of 719 participants, mean age 68.6 years, all led by researchers at Northwestern University, Chicago, that compared either supervised treadmill or home-based walking exercise with a nonexercise control group in people with PAD (defined as Ankle Brachial Index ≤ 0.90).
- All trials measured 6-minute walk (6MW) distance (walking as far as possible in 6 minutes), treadmill walking performance, and outcomes from the Walking Impairment Questionnaire (WIQ), which includes distance, walking speed, and stair-climbing domains, at baseline and at 6 months.
- Supervised treadmill exercise interventions included three individualized exercise sessions per week with an exercise physiologist at an exercise center, and home-based exercises involved walking near home 5 days per week, both for up to 50 minutes per session.
TAKEAWAY:
- After adjusting for study, age, sex, race, smoking, history of myocardial infarction, heart failure, and baseline 6MW distance, the study found both exercise interventions were better than nonexercise controls for 6MW distance.
- Compared with supervised treadmill exercise, home-based walking was associated with significantly improved mean 6MW distance (31.8 m vs. 55.6 m; adjusted between-group difference: −23.8 m; 95% confidence interval, −44.0 to −3.6; P = .021), and significantly improved WIQ walking speed score.
- However, home-based walking was associated with significantly less improvement in maximal treadmill walking distance, compared with supervised treadmill exercise (adjusted between-group difference: 132.5 m; 95% CI, 72.1-192.9; P < .001).
IN PRACTICE:
Home-based walking exercise “circumvents” barriers to accessing supervised exercise such as having to travel to a facility, said the authors, who noted the new data “demonstrated a large and consistent effect of home-based walking exercise on improved 6MW distance and also significantly improved the WIQ walking speed score, compared with supervised treadmill exercise.”
SOURCE:
The study was conducted by Neela D. Thangada, MD, Northwestern University, Chicago, and colleagues. It was published online in JAMA Network Open.
LIMITATIONS:
Data were combined from different randomized clinical trials that were led by one investigative team, and reported comparisons were not prespecified. Comparisons between supervised and home-based exercise lacked statistical power for the WIQ distance and stair-climbing measures.
DISCLOSURES:
The study was sponsored by the National Center for Research Resources and the National Heart, Lung, and Blood Institute of the National Institutes of Health. Dr. Thangada reports no relevant financial relationships. Disclosures for study coauthors can be found with the original article.
A version of this article first appeared on Medscape.com.
PET scan at diagnosis may help to predict aneurysm risk in patients with giant cell arteritis
PET scans may serve as both a diagnostic and prognostic tool in giant cell arteritis (GCA), according to a new study.
In over 100 patients with GCA who underwent 18F-fluorodeoxyglucose PET imaging, those with elevated FDG uptake at diagnosis were more likely to develop thoracic aortic aneurysms.
“PET-CT has an excellent diagnostic accuracy for the diagnosis of GCA, certainly if both extracranial and intracranial vessels were assessed. This study shows that performing PET imaging at diagnosis in patients with GCA may also help estimate the future risk for aortic aneurysm formation,” lead author Lien Moreel, MD, of the department of internal medicine at University Hospitals Leuven (Belgium), wrote in an email. “PET imaging at diagnosis can provide both diagnostic and prognostic information in one imaging tool in patients with GCA.”
Previous retrospective studies have found an association between FDG uptake at diagnosis and risk for aortic complications, but “prospective studies confirming these findings are lacking,” the investigators wrote. The study was published online in Annals of Internal Medicine.
In the study, Dr. Moreel and colleagues prospectively followed 106 individuals diagnosed with GCA who received FDG-PET within 3 days after starting glucocorticoids. Patients also had CT imaging at diagnosis and then CT imaging annually for up to 10 years.
A PET scan was considered positive with an FDG uptake of grade 2 or higher in any of seven vascular regions (thoracic and abdominal aorta, subclavian, axillary, carotid, iliac, and femoral arteries). Researchers also used the results to quantify a total vascular score (TVS). Out of the entire cohort, 75 patients had a positive PET scan result.
These patients had a larger increase in the diameter of the ascending aorta and the descending aorta, as well the volume of thoracic aorta after 5 years, compared with those who had a negative PET scan result. These changes were also associated with higher TVS at diagnosis. Of the 23 patients who developed an aortic aneurysm, 18 had a positive PET scan at diagnosis.
The risk of incident thoracic aortic aneurysms was calculated to be 10 times higher in patients with positive PET scans. Fourteen of the 15 patients (93%) with an incident thoracic aortic aneurysm had positive PET results.
Up to now, “we’ve had no way of predicting which patients might be at risk of this potentially serious complication,” Kenneth Warrington, MD, chair of the department of rheumatology and director of the Vasculitis Clinic at the Mayo Clinic in Rochester, Minn., said in an interview. He was not involved with the research.
He hopes that the findings will help inform clinicians on how patients with GCA should be evaluated and monitored. Although the American College of Rheumatology conditionally recommends noninvasive imaging in patients newly diagnosed with GCA, guidance for follow-up on these patients is less clear.
“There are no clear guidelines, but most clinicians who take care of patients with GCA do obtain imaging periodically,” he said. “There is a lot of variability in the practice in terms of which type of scan is used and how often it’s done.”
Although this study did not specifically look at the benefit of screening patients, “we think that follow-up of aortic dimensions seems to be warranted in GCA patients with a positive PET scan result, especially in those with high intensity and broad extent of vascular inflammation,” Dr. Moreel said. “However, the added value of screening and the interval required should be addressed in future studies.”
Applying this study’s protocol in practice in the United States might be difficult, Dr. Warrington noted, as it can be challenging logistically to get imaging done within 3 days of starting steroids. However, Dr. Moreel said it is possible to delay the start of glucocorticoids until the PET scan is performed in patients without visual symptoms or jaw claudication.
PET scans are also expensive, and it can be difficult to get insurance coverage in the United States. However, other imaging modalities could potentially be used in similar ways, Dr. Warrington said. “One could potentially extrapolate to say that if there is difficulty with accessing PET scan, we could use other modalities like CT or MRI basically to see whether the aorta is inflamed or not.”
Dr. Moreel disclosed no relevant financial relationships. Dr. Warrington has received compensation for consulting activities with Sanofi. Eli Lilly, Kiniksa, and Bristol-Myers Squibb have provided support to the Mayo Clinic for clinical trials related to GCA, of which Dr. Warrington served as subinvestigator.
A version of this article appeared on Medscape.com.
PET scans may serve as both a diagnostic and prognostic tool in giant cell arteritis (GCA), according to a new study.
In over 100 patients with GCA who underwent 18F-fluorodeoxyglucose PET imaging, those with elevated FDG uptake at diagnosis were more likely to develop thoracic aortic aneurysms.
“PET-CT has an excellent diagnostic accuracy for the diagnosis of GCA, certainly if both extracranial and intracranial vessels were assessed. This study shows that performing PET imaging at diagnosis in patients with GCA may also help estimate the future risk for aortic aneurysm formation,” lead author Lien Moreel, MD, of the department of internal medicine at University Hospitals Leuven (Belgium), wrote in an email. “PET imaging at diagnosis can provide both diagnostic and prognostic information in one imaging tool in patients with GCA.”
Previous retrospective studies have found an association between FDG uptake at diagnosis and risk for aortic complications, but “prospective studies confirming these findings are lacking,” the investigators wrote. The study was published online in Annals of Internal Medicine.
In the study, Dr. Moreel and colleagues prospectively followed 106 individuals diagnosed with GCA who received FDG-PET within 3 days after starting glucocorticoids. Patients also had CT imaging at diagnosis and then CT imaging annually for up to 10 years.
A PET scan was considered positive with an FDG uptake of grade 2 or higher in any of seven vascular regions (thoracic and abdominal aorta, subclavian, axillary, carotid, iliac, and femoral arteries). Researchers also used the results to quantify a total vascular score (TVS). Out of the entire cohort, 75 patients had a positive PET scan result.
These patients had a larger increase in the diameter of the ascending aorta and the descending aorta, as well the volume of thoracic aorta after 5 years, compared with those who had a negative PET scan result. These changes were also associated with higher TVS at diagnosis. Of the 23 patients who developed an aortic aneurysm, 18 had a positive PET scan at diagnosis.
The risk of incident thoracic aortic aneurysms was calculated to be 10 times higher in patients with positive PET scans. Fourteen of the 15 patients (93%) with an incident thoracic aortic aneurysm had positive PET results.
Up to now, “we’ve had no way of predicting which patients might be at risk of this potentially serious complication,” Kenneth Warrington, MD, chair of the department of rheumatology and director of the Vasculitis Clinic at the Mayo Clinic in Rochester, Minn., said in an interview. He was not involved with the research.
He hopes that the findings will help inform clinicians on how patients with GCA should be evaluated and monitored. Although the American College of Rheumatology conditionally recommends noninvasive imaging in patients newly diagnosed with GCA, guidance for follow-up on these patients is less clear.
“There are no clear guidelines, but most clinicians who take care of patients with GCA do obtain imaging periodically,” he said. “There is a lot of variability in the practice in terms of which type of scan is used and how often it’s done.”
Although this study did not specifically look at the benefit of screening patients, “we think that follow-up of aortic dimensions seems to be warranted in GCA patients with a positive PET scan result, especially in those with high intensity and broad extent of vascular inflammation,” Dr. Moreel said. “However, the added value of screening and the interval required should be addressed in future studies.”
Applying this study’s protocol in practice in the United States might be difficult, Dr. Warrington noted, as it can be challenging logistically to get imaging done within 3 days of starting steroids. However, Dr. Moreel said it is possible to delay the start of glucocorticoids until the PET scan is performed in patients without visual symptoms or jaw claudication.
PET scans are also expensive, and it can be difficult to get insurance coverage in the United States. However, other imaging modalities could potentially be used in similar ways, Dr. Warrington said. “One could potentially extrapolate to say that if there is difficulty with accessing PET scan, we could use other modalities like CT or MRI basically to see whether the aorta is inflamed or not.”
Dr. Moreel disclosed no relevant financial relationships. Dr. Warrington has received compensation for consulting activities with Sanofi. Eli Lilly, Kiniksa, and Bristol-Myers Squibb have provided support to the Mayo Clinic for clinical trials related to GCA, of which Dr. Warrington served as subinvestigator.
A version of this article appeared on Medscape.com.
PET scans may serve as both a diagnostic and prognostic tool in giant cell arteritis (GCA), according to a new study.
In over 100 patients with GCA who underwent 18F-fluorodeoxyglucose PET imaging, those with elevated FDG uptake at diagnosis were more likely to develop thoracic aortic aneurysms.
“PET-CT has an excellent diagnostic accuracy for the diagnosis of GCA, certainly if both extracranial and intracranial vessels were assessed. This study shows that performing PET imaging at diagnosis in patients with GCA may also help estimate the future risk for aortic aneurysm formation,” lead author Lien Moreel, MD, of the department of internal medicine at University Hospitals Leuven (Belgium), wrote in an email. “PET imaging at diagnosis can provide both diagnostic and prognostic information in one imaging tool in patients with GCA.”
Previous retrospective studies have found an association between FDG uptake at diagnosis and risk for aortic complications, but “prospective studies confirming these findings are lacking,” the investigators wrote. The study was published online in Annals of Internal Medicine.
In the study, Dr. Moreel and colleagues prospectively followed 106 individuals diagnosed with GCA who received FDG-PET within 3 days after starting glucocorticoids. Patients also had CT imaging at diagnosis and then CT imaging annually for up to 10 years.
A PET scan was considered positive with an FDG uptake of grade 2 or higher in any of seven vascular regions (thoracic and abdominal aorta, subclavian, axillary, carotid, iliac, and femoral arteries). Researchers also used the results to quantify a total vascular score (TVS). Out of the entire cohort, 75 patients had a positive PET scan result.
These patients had a larger increase in the diameter of the ascending aorta and the descending aorta, as well the volume of thoracic aorta after 5 years, compared with those who had a negative PET scan result. These changes were also associated with higher TVS at diagnosis. Of the 23 patients who developed an aortic aneurysm, 18 had a positive PET scan at diagnosis.
The risk of incident thoracic aortic aneurysms was calculated to be 10 times higher in patients with positive PET scans. Fourteen of the 15 patients (93%) with an incident thoracic aortic aneurysm had positive PET results.
Up to now, “we’ve had no way of predicting which patients might be at risk of this potentially serious complication,” Kenneth Warrington, MD, chair of the department of rheumatology and director of the Vasculitis Clinic at the Mayo Clinic in Rochester, Minn., said in an interview. He was not involved with the research.
He hopes that the findings will help inform clinicians on how patients with GCA should be evaluated and monitored. Although the American College of Rheumatology conditionally recommends noninvasive imaging in patients newly diagnosed with GCA, guidance for follow-up on these patients is less clear.
“There are no clear guidelines, but most clinicians who take care of patients with GCA do obtain imaging periodically,” he said. “There is a lot of variability in the practice in terms of which type of scan is used and how often it’s done.”
Although this study did not specifically look at the benefit of screening patients, “we think that follow-up of aortic dimensions seems to be warranted in GCA patients with a positive PET scan result, especially in those with high intensity and broad extent of vascular inflammation,” Dr. Moreel said. “However, the added value of screening and the interval required should be addressed in future studies.”
Applying this study’s protocol in practice in the United States might be difficult, Dr. Warrington noted, as it can be challenging logistically to get imaging done within 3 days of starting steroids. However, Dr. Moreel said it is possible to delay the start of glucocorticoids until the PET scan is performed in patients without visual symptoms or jaw claudication.
PET scans are also expensive, and it can be difficult to get insurance coverage in the United States. However, other imaging modalities could potentially be used in similar ways, Dr. Warrington said. “One could potentially extrapolate to say that if there is difficulty with accessing PET scan, we could use other modalities like CT or MRI basically to see whether the aorta is inflamed or not.”
Dr. Moreel disclosed no relevant financial relationships. Dr. Warrington has received compensation for consulting activities with Sanofi. Eli Lilly, Kiniksa, and Bristol-Myers Squibb have provided support to the Mayo Clinic for clinical trials related to GCA, of which Dr. Warrington served as subinvestigator.
A version of this article appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
PAD procedure overuse: A field in peril or ‘a few bad apples’?
On May 24, the news outlet ProPublica published a scathing investigation of Jeffery Dormu, DO, said to have performed hundreds of “medically unnecessary and invasive vascular procedures” in his Laurel, Md. office, putting patients’ limbs and lives at risk.
On July 15, The New York Times published a broader-based investigation of several vascular specialists said to have performed “risky” procedures on patients with peripheral artery disease (PAD) who subsequently had to have amputations, or died. The focus was mainly on Michigan-based interventional cardiologist Jihad Mustapha, MD.
This follows a 2019 analysis of Medicare claims data that identified outlier physicians with a high early intervention rate for patients newly diagnosed with claudication. According to the American Heart Association statistics, PAD affects approximately 8.5 million U.S. adults age 40 and older (some claim that’s an underestimate); most cases don’t require invasive treatment.
Responding to the Times’ revelations, Joseph L. Mills, MD, president of the Society for Vascular Surgery, wrote on the society’s website: “The overwhelming majority of vascular surgeons, and a vast majority of other specialists that receive some training and play a role in the care of vascular patients, including those trained in vascular medicine, interventional cardiology, and interventional radiology are providing high-quality, evidence-based care with safety and the best patient outcomes in mind.
“This is a complex issue that requires the examination not only of the events detailed in this story ... but of the underlying health care economic, legal and regulatory policies that created fertile soil for this behavior to germinate and take root.”
‘A few bad apples’
“I think it’s a case of a few bad apples,” Sunil V. Rao, MD, director of interventional cardiology at NYU Langone Health, New York, said in an interview. “In general, I think physicians who take care of patients with vascular issues are trying to do the right thing. I think all of us who take care of patients with vascular disease see patients who are very, very complex, and there are going to be some procedures that have complications.
“Without knowing the clinical details, it’s hard to know whether the procedures described in the articles were overuse or unnecessary, or exactly what led to the amputations,” he said. “All we know is that these physicians are outliers in terms of the number of procedures they were billing for.
“But although correlation is not causation, it certainly is cause for concern because you would expect that the use of procedures for specific indications would fall within a certain range,” he added.
Lifestyle changes first
PAD is often asymptomatic or mild, making it difficult to diagnose. Revascularization procedures usually are reserved for the 5%-8% of patients at risk for chronic limb-threatening ischemia (CLTI) or those in whom the cornerstones of PAD treatment – lifestyle changes and, if needed, medication – fail.
Revascularization options include balloon angioplasty or stent placement; atherectomy to remove plaques from the artery; or bypass surgery if a long portion of a leg artery is completely blocked. All carry a risk of long-term adverse outcomes, but the rates are highest for atherectomy.
Lifestyle changes include regular exercise, following a healthy diet, quitting smoking, and controlling diabetes and high blood pressure. When PAD continues or progresses despite these modifications, medications such as antiplatelet agents, antihypertensives, and/or lipid-lowering drugs may be prescribed.
‘Medically unnecessary’
According to the latest American Heart Association/American College of Cardiology guideline on managing patients with lower-extremity PAD, patients should be selected for revascularization based on symptom severity.
Factors to consider include a significant disability as assessed by the patient, and adequacy of response to medical and structured exercise therapy.
There’s the rub regarding the clinicians investigated in the Times and ProPublica. Many patients, apparently, were not encouraged to make lifestyle changes, nor did they receive medication. Instead, they were advised from the get-go to undergo invasive procedures, and often multiple times. Underuse of prevention and lifestyle counseling n the management of PAD has long been a concern.
Furthermore, in at least some cases, patients without any symptoms were encouraged to be screened for blockages that were then treated invasively, according to the Times.
Dr. Dormu, as highlighted in ProPublica, positioned his practice as “life and limb saving.” Yet, in investigative findings that led to a suspension of Dr. Dormu’s license to practice medicine in Maryland, peer reviewers expressed concern regarding his repeated use of invasive and medically unnecessary procedures, exposing patients to “potential risks such as bleeding, infection, blood vessel injuries which could acutely or chronically worsen the patient’s circulation, and limb loss.”
The peer reviewers concurred that Dr. Dormu failed to use conservative management techniques to address the patients’ vascular complaints before resorting to invasive procedures.
Dr. Mustapha is described in the Times as a “high-volume” atherectomy provider. From 2017 to 2021, about half of Medicare’s atherectomy payments – $1.4 billion – went to 200 high-volume providers, with Dr. Mustapha near the top of the list.
Some of Dr. Mustapha’s patients underwent multiple procedures said to help prevent leg amputation, but their legs were amputated anyway, possibly because of the multiple atherectomies, according to the Times.
Judith Lin, MD, MBA, who treated some of Dr. Mustapha’s former patients, was among those who complained about his practice to Michigan’s licensing board. Some of the patients she treated needed amputations; others needed to have leftover wires extracted from their legs.
In 2020, the board investigated Dr. Lin’s complaint and referred it to Michigan’s attorney general, who brought a disciplinary action against Dr. Mustapha. An expert hired by the state to review eight patient cases concluded that Dr. Mustapha’s practice “was characterized by overtreatment and poor documentation.” In some cases, the expert wrote, “unnecessary procedures hastened amputations.”
The statement issued by Dr. Mills, the president of SVS, noted that the society’s practice guideline proposes a threshold of at least 2 years of likely durability for an intervention performed for claudication.
“The growing frequency of multiple, repeated procedures [is] emblematic of poor patient selection and inadequate durability of the chosen procedure, leading to a vicious cycle of repetitive interventions that is not only costly, but also dangerous,” he wrote.
Financial incentives to blame?
In 2008, Medicare created incentives for physicians to perform vascular procedures in offices rather than hospitals, in an effort to reduce medical costs, according to both investigative articles. But the effort backfired.
Before the changes, an office provider inserting a stent could make about $1,700 from Medicare; deploying a balloon could bring in roughly $3,800. By 2011, the payments rose to about $6,400 and $4,800, respectively.
Office-based atherectomies soared when, in 2011, the Centers for Medicare & Medicaid Services started reimbursing $13,500 per procedure, as opposed to roughly $11,450 in a hospital. Atherectomies increased by 60% from 2011 to 2014, and Medicare’s overall costs for peripheral vascular treatments climbed by nearly half a billion dollars.
“The government is really to blame for setting these tremendously high reimbursement values without looking into whether these procedures are helping people or are just worthless procedures or, in fact, are hurting people,” Dipankar Mukherjee, MD, a vascular surgeon and chief of vascular surgery at Inova Fairfax (Va.) Hospital, said in ProPublica.
The result, noted Dr. Rao, is that “there can be perverse or nefarious incentives for doing these procedures. People are incentivized by reimbursement to do something that really falls in the area of clinical judgment and guidelines.”
Major incentives also come from device manufacturers, who often reward physicians who do the most vascular procedures with payments for consulting and other services, according to the Times. In addition, these companies lend money to help physicians or their clinics to finance the purchase of equipment used to perform the procedures.
“Vascular medicine now is the frontier of the Wild West,” Marty Makary, MD, MPH, a professor of surgery and health care quality researcher at Johns Hopkins University, Baltimore, told ProPublica. “People are flying blind walking into the clinics of these doctors with egregious practice patterns, and we know that their pattern is indefensible.”
Recognizing that the situation posed a threat to patients and also damaged the credibility of his specialty, Kim J. Hodgson, MD, a former SVS president, told attendees at the 2021 annual meeting of the SVS, “Somebody has to address what should never have been allowed to get to this level of threat to us and our patients in the first place. We can play whack-a-mole every time the bad actors surface until the cows come home, but that leaves a trail of harmed patients and wasted resources.”
Dr. Hodgson described atherectomy as “a procedure that many believe provides no demonstrable value whatsoever to the patient” and challenged those who disagree to prove it.
Multidisciplinary teams needed
Other experts believe there are times that revascularization procedures, including atherectomy, are appropriate. However, the majority of patients with PAD do not require a procedure, Soo Hyun (Esther) Kim, MD, MPH, director of the Center for Women’s Cardiovascular Health at Atrium Health Sanger Heart and Vascular Institute in Charlotte, N.C., said in an interview. In fact, “many patients do not even know they have leg artery blockages.”
Invasive procedures may well be appropriate for patients with severe PAD, especially those with CLTI, and disparities may be keeping those who truly need such interventions – or for whom they may be at least considered – from accessing them. If PAD is not diagnosed and treated in a timely way, Dr. Kim said, those individuals “do indeed lose their limbs.”
Multidisciplinary teams can help, Dr. Kim said. “Specialists from multiple different training backgrounds [can] take good care of patients with PAD,” she said. This is important when access to a particular type of specialist is limited, and because patients with PAD often have complex medical problems that can benefit from a team approach.
Transcatheter aortic valve replacement heart teams and complex coronary disease heart teams are two examples, Dr. Kim noted. “When a high-stakes procedure is being considered, the patient’s case is reviewed by multiple stakeholders to ensure appropriateness of the procedure and collaboratively evaluate risk.”
Dr. Rao also emphasized a team approach. “PAD does not belong to a single specialty,” he said. The revelations from the Times, ProPublica, and other sources “point to the fact that we all – cardiologists, vascular surgeons, interventional radiologists – should start thinking about how best to police ourselves and also account for the variation in clinical judgment.”
Use of a multidisciplinary team is a “guideline-recommended approach” for coronary artery revascularization, he said, “I think the same should apply for PAD.”
PAD is a sign of systemic atherosclerosis, Dr. Kim noted. “The treatment of PAD includes addressing leg pain and wounds with procedures, but the interventions that will keep people alive are the medications we use to prevent heart attack and stroke. Patients with PAD need to understand that treatment is much more than opening up a blockage in the leg.”
Dr. Rao and Dr. Kim disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
On May 24, the news outlet ProPublica published a scathing investigation of Jeffery Dormu, DO, said to have performed hundreds of “medically unnecessary and invasive vascular procedures” in his Laurel, Md. office, putting patients’ limbs and lives at risk.
On July 15, The New York Times published a broader-based investigation of several vascular specialists said to have performed “risky” procedures on patients with peripheral artery disease (PAD) who subsequently had to have amputations, or died. The focus was mainly on Michigan-based interventional cardiologist Jihad Mustapha, MD.
This follows a 2019 analysis of Medicare claims data that identified outlier physicians with a high early intervention rate for patients newly diagnosed with claudication. According to the American Heart Association statistics, PAD affects approximately 8.5 million U.S. adults age 40 and older (some claim that’s an underestimate); most cases don’t require invasive treatment.
Responding to the Times’ revelations, Joseph L. Mills, MD, president of the Society for Vascular Surgery, wrote on the society’s website: “The overwhelming majority of vascular surgeons, and a vast majority of other specialists that receive some training and play a role in the care of vascular patients, including those trained in vascular medicine, interventional cardiology, and interventional radiology are providing high-quality, evidence-based care with safety and the best patient outcomes in mind.
“This is a complex issue that requires the examination not only of the events detailed in this story ... but of the underlying health care economic, legal and regulatory policies that created fertile soil for this behavior to germinate and take root.”
‘A few bad apples’
“I think it’s a case of a few bad apples,” Sunil V. Rao, MD, director of interventional cardiology at NYU Langone Health, New York, said in an interview. “In general, I think physicians who take care of patients with vascular issues are trying to do the right thing. I think all of us who take care of patients with vascular disease see patients who are very, very complex, and there are going to be some procedures that have complications.
“Without knowing the clinical details, it’s hard to know whether the procedures described in the articles were overuse or unnecessary, or exactly what led to the amputations,” he said. “All we know is that these physicians are outliers in terms of the number of procedures they were billing for.
“But although correlation is not causation, it certainly is cause for concern because you would expect that the use of procedures for specific indications would fall within a certain range,” he added.
Lifestyle changes first
PAD is often asymptomatic or mild, making it difficult to diagnose. Revascularization procedures usually are reserved for the 5%-8% of patients at risk for chronic limb-threatening ischemia (CLTI) or those in whom the cornerstones of PAD treatment – lifestyle changes and, if needed, medication – fail.
Revascularization options include balloon angioplasty or stent placement; atherectomy to remove plaques from the artery; or bypass surgery if a long portion of a leg artery is completely blocked. All carry a risk of long-term adverse outcomes, but the rates are highest for atherectomy.
Lifestyle changes include regular exercise, following a healthy diet, quitting smoking, and controlling diabetes and high blood pressure. When PAD continues or progresses despite these modifications, medications such as antiplatelet agents, antihypertensives, and/or lipid-lowering drugs may be prescribed.
‘Medically unnecessary’
According to the latest American Heart Association/American College of Cardiology guideline on managing patients with lower-extremity PAD, patients should be selected for revascularization based on symptom severity.
Factors to consider include a significant disability as assessed by the patient, and adequacy of response to medical and structured exercise therapy.
There’s the rub regarding the clinicians investigated in the Times and ProPublica. Many patients, apparently, were not encouraged to make lifestyle changes, nor did they receive medication. Instead, they were advised from the get-go to undergo invasive procedures, and often multiple times. Underuse of prevention and lifestyle counseling n the management of PAD has long been a concern.
Furthermore, in at least some cases, patients without any symptoms were encouraged to be screened for blockages that were then treated invasively, according to the Times.
Dr. Dormu, as highlighted in ProPublica, positioned his practice as “life and limb saving.” Yet, in investigative findings that led to a suspension of Dr. Dormu’s license to practice medicine in Maryland, peer reviewers expressed concern regarding his repeated use of invasive and medically unnecessary procedures, exposing patients to “potential risks such as bleeding, infection, blood vessel injuries which could acutely or chronically worsen the patient’s circulation, and limb loss.”
The peer reviewers concurred that Dr. Dormu failed to use conservative management techniques to address the patients’ vascular complaints before resorting to invasive procedures.
Dr. Mustapha is described in the Times as a “high-volume” atherectomy provider. From 2017 to 2021, about half of Medicare’s atherectomy payments – $1.4 billion – went to 200 high-volume providers, with Dr. Mustapha near the top of the list.
Some of Dr. Mustapha’s patients underwent multiple procedures said to help prevent leg amputation, but their legs were amputated anyway, possibly because of the multiple atherectomies, according to the Times.
Judith Lin, MD, MBA, who treated some of Dr. Mustapha’s former patients, was among those who complained about his practice to Michigan’s licensing board. Some of the patients she treated needed amputations; others needed to have leftover wires extracted from their legs.
In 2020, the board investigated Dr. Lin’s complaint and referred it to Michigan’s attorney general, who brought a disciplinary action against Dr. Mustapha. An expert hired by the state to review eight patient cases concluded that Dr. Mustapha’s practice “was characterized by overtreatment and poor documentation.” In some cases, the expert wrote, “unnecessary procedures hastened amputations.”
The statement issued by Dr. Mills, the president of SVS, noted that the society’s practice guideline proposes a threshold of at least 2 years of likely durability for an intervention performed for claudication.
“The growing frequency of multiple, repeated procedures [is] emblematic of poor patient selection and inadequate durability of the chosen procedure, leading to a vicious cycle of repetitive interventions that is not only costly, but also dangerous,” he wrote.
Financial incentives to blame?
In 2008, Medicare created incentives for physicians to perform vascular procedures in offices rather than hospitals, in an effort to reduce medical costs, according to both investigative articles. But the effort backfired.
Before the changes, an office provider inserting a stent could make about $1,700 from Medicare; deploying a balloon could bring in roughly $3,800. By 2011, the payments rose to about $6,400 and $4,800, respectively.
Office-based atherectomies soared when, in 2011, the Centers for Medicare & Medicaid Services started reimbursing $13,500 per procedure, as opposed to roughly $11,450 in a hospital. Atherectomies increased by 60% from 2011 to 2014, and Medicare’s overall costs for peripheral vascular treatments climbed by nearly half a billion dollars.
“The government is really to blame for setting these tremendously high reimbursement values without looking into whether these procedures are helping people or are just worthless procedures or, in fact, are hurting people,” Dipankar Mukherjee, MD, a vascular surgeon and chief of vascular surgery at Inova Fairfax (Va.) Hospital, said in ProPublica.
The result, noted Dr. Rao, is that “there can be perverse or nefarious incentives for doing these procedures. People are incentivized by reimbursement to do something that really falls in the area of clinical judgment and guidelines.”
Major incentives also come from device manufacturers, who often reward physicians who do the most vascular procedures with payments for consulting and other services, according to the Times. In addition, these companies lend money to help physicians or their clinics to finance the purchase of equipment used to perform the procedures.
“Vascular medicine now is the frontier of the Wild West,” Marty Makary, MD, MPH, a professor of surgery and health care quality researcher at Johns Hopkins University, Baltimore, told ProPublica. “People are flying blind walking into the clinics of these doctors with egregious practice patterns, and we know that their pattern is indefensible.”
Recognizing that the situation posed a threat to patients and also damaged the credibility of his specialty, Kim J. Hodgson, MD, a former SVS president, told attendees at the 2021 annual meeting of the SVS, “Somebody has to address what should never have been allowed to get to this level of threat to us and our patients in the first place. We can play whack-a-mole every time the bad actors surface until the cows come home, but that leaves a trail of harmed patients and wasted resources.”
Dr. Hodgson described atherectomy as “a procedure that many believe provides no demonstrable value whatsoever to the patient” and challenged those who disagree to prove it.
Multidisciplinary teams needed
Other experts believe there are times that revascularization procedures, including atherectomy, are appropriate. However, the majority of patients with PAD do not require a procedure, Soo Hyun (Esther) Kim, MD, MPH, director of the Center for Women’s Cardiovascular Health at Atrium Health Sanger Heart and Vascular Institute in Charlotte, N.C., said in an interview. In fact, “many patients do not even know they have leg artery blockages.”
Invasive procedures may well be appropriate for patients with severe PAD, especially those with CLTI, and disparities may be keeping those who truly need such interventions – or for whom they may be at least considered – from accessing them. If PAD is not diagnosed and treated in a timely way, Dr. Kim said, those individuals “do indeed lose their limbs.”
Multidisciplinary teams can help, Dr. Kim said. “Specialists from multiple different training backgrounds [can] take good care of patients with PAD,” she said. This is important when access to a particular type of specialist is limited, and because patients with PAD often have complex medical problems that can benefit from a team approach.
Transcatheter aortic valve replacement heart teams and complex coronary disease heart teams are two examples, Dr. Kim noted. “When a high-stakes procedure is being considered, the patient’s case is reviewed by multiple stakeholders to ensure appropriateness of the procedure and collaboratively evaluate risk.”
Dr. Rao also emphasized a team approach. “PAD does not belong to a single specialty,” he said. The revelations from the Times, ProPublica, and other sources “point to the fact that we all – cardiologists, vascular surgeons, interventional radiologists – should start thinking about how best to police ourselves and also account for the variation in clinical judgment.”
Use of a multidisciplinary team is a “guideline-recommended approach” for coronary artery revascularization, he said, “I think the same should apply for PAD.”
PAD is a sign of systemic atherosclerosis, Dr. Kim noted. “The treatment of PAD includes addressing leg pain and wounds with procedures, but the interventions that will keep people alive are the medications we use to prevent heart attack and stroke. Patients with PAD need to understand that treatment is much more than opening up a blockage in the leg.”
Dr. Rao and Dr. Kim disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
On May 24, the news outlet ProPublica published a scathing investigation of Jeffery Dormu, DO, said to have performed hundreds of “medically unnecessary and invasive vascular procedures” in his Laurel, Md. office, putting patients’ limbs and lives at risk.
On July 15, The New York Times published a broader-based investigation of several vascular specialists said to have performed “risky” procedures on patients with peripheral artery disease (PAD) who subsequently had to have amputations, or died. The focus was mainly on Michigan-based interventional cardiologist Jihad Mustapha, MD.
This follows a 2019 analysis of Medicare claims data that identified outlier physicians with a high early intervention rate for patients newly diagnosed with claudication. According to the American Heart Association statistics, PAD affects approximately 8.5 million U.S. adults age 40 and older (some claim that’s an underestimate); most cases don’t require invasive treatment.
Responding to the Times’ revelations, Joseph L. Mills, MD, president of the Society for Vascular Surgery, wrote on the society’s website: “The overwhelming majority of vascular surgeons, and a vast majority of other specialists that receive some training and play a role in the care of vascular patients, including those trained in vascular medicine, interventional cardiology, and interventional radiology are providing high-quality, evidence-based care with safety and the best patient outcomes in mind.
“This is a complex issue that requires the examination not only of the events detailed in this story ... but of the underlying health care economic, legal and regulatory policies that created fertile soil for this behavior to germinate and take root.”
‘A few bad apples’
“I think it’s a case of a few bad apples,” Sunil V. Rao, MD, director of interventional cardiology at NYU Langone Health, New York, said in an interview. “In general, I think physicians who take care of patients with vascular issues are trying to do the right thing. I think all of us who take care of patients with vascular disease see patients who are very, very complex, and there are going to be some procedures that have complications.
“Without knowing the clinical details, it’s hard to know whether the procedures described in the articles were overuse or unnecessary, or exactly what led to the amputations,” he said. “All we know is that these physicians are outliers in terms of the number of procedures they were billing for.
“But although correlation is not causation, it certainly is cause for concern because you would expect that the use of procedures for specific indications would fall within a certain range,” he added.
Lifestyle changes first
PAD is often asymptomatic or mild, making it difficult to diagnose. Revascularization procedures usually are reserved for the 5%-8% of patients at risk for chronic limb-threatening ischemia (CLTI) or those in whom the cornerstones of PAD treatment – lifestyle changes and, if needed, medication – fail.
Revascularization options include balloon angioplasty or stent placement; atherectomy to remove plaques from the artery; or bypass surgery if a long portion of a leg artery is completely blocked. All carry a risk of long-term adverse outcomes, but the rates are highest for atherectomy.
Lifestyle changes include regular exercise, following a healthy diet, quitting smoking, and controlling diabetes and high blood pressure. When PAD continues or progresses despite these modifications, medications such as antiplatelet agents, antihypertensives, and/or lipid-lowering drugs may be prescribed.
‘Medically unnecessary’
According to the latest American Heart Association/American College of Cardiology guideline on managing patients with lower-extremity PAD, patients should be selected for revascularization based on symptom severity.
Factors to consider include a significant disability as assessed by the patient, and adequacy of response to medical and structured exercise therapy.
There’s the rub regarding the clinicians investigated in the Times and ProPublica. Many patients, apparently, were not encouraged to make lifestyle changes, nor did they receive medication. Instead, they were advised from the get-go to undergo invasive procedures, and often multiple times. Underuse of prevention and lifestyle counseling n the management of PAD has long been a concern.
Furthermore, in at least some cases, patients without any symptoms were encouraged to be screened for blockages that were then treated invasively, according to the Times.
Dr. Dormu, as highlighted in ProPublica, positioned his practice as “life and limb saving.” Yet, in investigative findings that led to a suspension of Dr. Dormu’s license to practice medicine in Maryland, peer reviewers expressed concern regarding his repeated use of invasive and medically unnecessary procedures, exposing patients to “potential risks such as bleeding, infection, blood vessel injuries which could acutely or chronically worsen the patient’s circulation, and limb loss.”
The peer reviewers concurred that Dr. Dormu failed to use conservative management techniques to address the patients’ vascular complaints before resorting to invasive procedures.
Dr. Mustapha is described in the Times as a “high-volume” atherectomy provider. From 2017 to 2021, about half of Medicare’s atherectomy payments – $1.4 billion – went to 200 high-volume providers, with Dr. Mustapha near the top of the list.
Some of Dr. Mustapha’s patients underwent multiple procedures said to help prevent leg amputation, but their legs were amputated anyway, possibly because of the multiple atherectomies, according to the Times.
Judith Lin, MD, MBA, who treated some of Dr. Mustapha’s former patients, was among those who complained about his practice to Michigan’s licensing board. Some of the patients she treated needed amputations; others needed to have leftover wires extracted from their legs.
In 2020, the board investigated Dr. Lin’s complaint and referred it to Michigan’s attorney general, who brought a disciplinary action against Dr. Mustapha. An expert hired by the state to review eight patient cases concluded that Dr. Mustapha’s practice “was characterized by overtreatment and poor documentation.” In some cases, the expert wrote, “unnecessary procedures hastened amputations.”
The statement issued by Dr. Mills, the president of SVS, noted that the society’s practice guideline proposes a threshold of at least 2 years of likely durability for an intervention performed for claudication.
“The growing frequency of multiple, repeated procedures [is] emblematic of poor patient selection and inadequate durability of the chosen procedure, leading to a vicious cycle of repetitive interventions that is not only costly, but also dangerous,” he wrote.
Financial incentives to blame?
In 2008, Medicare created incentives for physicians to perform vascular procedures in offices rather than hospitals, in an effort to reduce medical costs, according to both investigative articles. But the effort backfired.
Before the changes, an office provider inserting a stent could make about $1,700 from Medicare; deploying a balloon could bring in roughly $3,800. By 2011, the payments rose to about $6,400 and $4,800, respectively.
Office-based atherectomies soared when, in 2011, the Centers for Medicare & Medicaid Services started reimbursing $13,500 per procedure, as opposed to roughly $11,450 in a hospital. Atherectomies increased by 60% from 2011 to 2014, and Medicare’s overall costs for peripheral vascular treatments climbed by nearly half a billion dollars.
“The government is really to blame for setting these tremendously high reimbursement values without looking into whether these procedures are helping people or are just worthless procedures or, in fact, are hurting people,” Dipankar Mukherjee, MD, a vascular surgeon and chief of vascular surgery at Inova Fairfax (Va.) Hospital, said in ProPublica.
The result, noted Dr. Rao, is that “there can be perverse or nefarious incentives for doing these procedures. People are incentivized by reimbursement to do something that really falls in the area of clinical judgment and guidelines.”
Major incentives also come from device manufacturers, who often reward physicians who do the most vascular procedures with payments for consulting and other services, according to the Times. In addition, these companies lend money to help physicians or their clinics to finance the purchase of equipment used to perform the procedures.
“Vascular medicine now is the frontier of the Wild West,” Marty Makary, MD, MPH, a professor of surgery and health care quality researcher at Johns Hopkins University, Baltimore, told ProPublica. “People are flying blind walking into the clinics of these doctors with egregious practice patterns, and we know that their pattern is indefensible.”
Recognizing that the situation posed a threat to patients and also damaged the credibility of his specialty, Kim J. Hodgson, MD, a former SVS president, told attendees at the 2021 annual meeting of the SVS, “Somebody has to address what should never have been allowed to get to this level of threat to us and our patients in the first place. We can play whack-a-mole every time the bad actors surface until the cows come home, but that leaves a trail of harmed patients and wasted resources.”
Dr. Hodgson described atherectomy as “a procedure that many believe provides no demonstrable value whatsoever to the patient” and challenged those who disagree to prove it.
Multidisciplinary teams needed
Other experts believe there are times that revascularization procedures, including atherectomy, are appropriate. However, the majority of patients with PAD do not require a procedure, Soo Hyun (Esther) Kim, MD, MPH, director of the Center for Women’s Cardiovascular Health at Atrium Health Sanger Heart and Vascular Institute in Charlotte, N.C., said in an interview. In fact, “many patients do not even know they have leg artery blockages.”
Invasive procedures may well be appropriate for patients with severe PAD, especially those with CLTI, and disparities may be keeping those who truly need such interventions – or for whom they may be at least considered – from accessing them. If PAD is not diagnosed and treated in a timely way, Dr. Kim said, those individuals “do indeed lose their limbs.”
Multidisciplinary teams can help, Dr. Kim said. “Specialists from multiple different training backgrounds [can] take good care of patients with PAD,” she said. This is important when access to a particular type of specialist is limited, and because patients with PAD often have complex medical problems that can benefit from a team approach.
Transcatheter aortic valve replacement heart teams and complex coronary disease heart teams are two examples, Dr. Kim noted. “When a high-stakes procedure is being considered, the patient’s case is reviewed by multiple stakeholders to ensure appropriateness of the procedure and collaboratively evaluate risk.”
Dr. Rao also emphasized a team approach. “PAD does not belong to a single specialty,” he said. The revelations from the Times, ProPublica, and other sources “point to the fact that we all – cardiologists, vascular surgeons, interventional radiologists – should start thinking about how best to police ourselves and also account for the variation in clinical judgment.”
Use of a multidisciplinary team is a “guideline-recommended approach” for coronary artery revascularization, he said, “I think the same should apply for PAD.”
PAD is a sign of systemic atherosclerosis, Dr. Kim noted. “The treatment of PAD includes addressing leg pain and wounds with procedures, but the interventions that will keep people alive are the medications we use to prevent heart attack and stroke. Patients with PAD need to understand that treatment is much more than opening up a blockage in the leg.”
Dr. Rao and Dr. Kim disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Marijuana linked to higher PAD risk
But death, intervention rates same
PHOENIX – although there was no greater risk of death from myocardial infarction or other cardiac causes or need for revascularization.
The researchers noted, however, that the study population was young, with an average age of 37.4 years, and that the study period, from 2016 to 2019, predates the legalization of recreational marijuana in a number of states.
Nonetheless, even in this young study population, marijuana users’ risk of developing peripheral artery disease (PAD) was 3.68 times greater (P < .001) than that of nonusers. PAD at a young age could precede worse outcomes later in life, the study authors said.
“Basically, marijuana users were at increased risk of being diagnosed with peripheral artery disease, but there was no increased risk for them requiring any intervention, such as a peripheral vascular intervention, nor were they at increased risk of death from what we found,” said Hirva Vyas, DO, an internal medicine resident at Hackensack University Medical Center in New Jersey, who presented the results at the Society for Cardiovascular Angiography & Interventions annual scientific sessions.
The study used data on 623,768 marijuana users from the National Inpatient Sample, a nationwide database of inpatient visits covered by all public and commercial payers, then extracted a diagnosis for PAD from all 30 million–plus patient encounters to compare PAD rates between marijuana users and nonusers. Marijuana users were more likely to be White and to have elective rather than emergency admissions (P < .001). The researchers used diagnostic codes to identify marijuana users and PAD patients.
Recreational marijuana is legal in 22 states and the District of Columbia, according to ProCon.org. Since 2019, the last year of the study, 11 states have legalized marijuana for recreational use. “It’s a data point that we studied at one point in time, only from 2016 to 2019,” Dr. Vyas said in an interview.
“As we’ve seen over the past 4-5 years, legalization has skyrocketed and recreational use has become more and more favorable not only among younger folks but older folks,” study coauthor Harsh Jain, MD, a second-year internal medicine resident at Montefiore Medical Center in New York, said in the interview. “It would be really refreshing to see how these data change as we look at endpoints from 2019 to 2023.”
Because of the young age of the study population, Dr. Jain said, these findings may not accurately represent the true cardiovascular risks of marijuana use, especially later in life.
“One of the biggest secondary endpoints that we wanted to study was the development of chronic conditions that lead to multiple rehospitalizations, the most significant one of which would be the development of heart failure,” Dr. Jain said. “However, it was difficult to stratify because, again, many of these patients were very young and so they did not carry the diagnosis for heart failure, so we couldn’t complete that subset analysis.”
The goal is to extend the study period out to 2023, Dr. Jain said. “We know that these are very crude and rudimentary data findings that we presented so far, but we’re hoping that the final paper gives us a chance to flesh out all the details of our study and also gives us a chance to expand going forward,” he said.
The findings are in line with other research into the effects of marijuana and cardiovascular disease, said Carl “Chip” Lavie, MD, medical director for cardiac rehabilitation and prevention at the John Ochsner Heart and Vascular Institute in New Orleans who’s published a number of studies on PAD and substance use, including marijuana.
“It is known that cannabis is associated with more vasoconstriction, has sympathomimetic effects, causes endothelial dysfunction and increased platelet aggregation, and is known to increase the risk of acute myocardial infarction, especially in the hour or so after use,” he said in written comments sent to this news organization.
“It is also well known to be a cause of thromboangiitis obliterans, which is in the PAD family,” he added. “Based on these mechanisms, one would expect an increased PAD and, especially, PAD events. The 3.7-fold increased risk is supportive of this increased PAD.”
One study strength, Dr. Lavie pointed out, is that it’s one of the few studies that found an association between marijuana and PAD, which hasn’t been studied as well as other cardiovascular endpoints. “However,” he said, “the limitation is this is just an inpatient sample, and it is all based on coding – e.g., a patient could have PAD and it may not have been coded.”
But death, intervention rates same
But death, intervention rates same
PHOENIX – although there was no greater risk of death from myocardial infarction or other cardiac causes or need for revascularization.
The researchers noted, however, that the study population was young, with an average age of 37.4 years, and that the study period, from 2016 to 2019, predates the legalization of recreational marijuana in a number of states.
Nonetheless, even in this young study population, marijuana users’ risk of developing peripheral artery disease (PAD) was 3.68 times greater (P < .001) than that of nonusers. PAD at a young age could precede worse outcomes later in life, the study authors said.
“Basically, marijuana users were at increased risk of being diagnosed with peripheral artery disease, but there was no increased risk for them requiring any intervention, such as a peripheral vascular intervention, nor were they at increased risk of death from what we found,” said Hirva Vyas, DO, an internal medicine resident at Hackensack University Medical Center in New Jersey, who presented the results at the Society for Cardiovascular Angiography & Interventions annual scientific sessions.
The study used data on 623,768 marijuana users from the National Inpatient Sample, a nationwide database of inpatient visits covered by all public and commercial payers, then extracted a diagnosis for PAD from all 30 million–plus patient encounters to compare PAD rates between marijuana users and nonusers. Marijuana users were more likely to be White and to have elective rather than emergency admissions (P < .001). The researchers used diagnostic codes to identify marijuana users and PAD patients.
Recreational marijuana is legal in 22 states and the District of Columbia, according to ProCon.org. Since 2019, the last year of the study, 11 states have legalized marijuana for recreational use. “It’s a data point that we studied at one point in time, only from 2016 to 2019,” Dr. Vyas said in an interview.
“As we’ve seen over the past 4-5 years, legalization has skyrocketed and recreational use has become more and more favorable not only among younger folks but older folks,” study coauthor Harsh Jain, MD, a second-year internal medicine resident at Montefiore Medical Center in New York, said in the interview. “It would be really refreshing to see how these data change as we look at endpoints from 2019 to 2023.”
Because of the young age of the study population, Dr. Jain said, these findings may not accurately represent the true cardiovascular risks of marijuana use, especially later in life.
“One of the biggest secondary endpoints that we wanted to study was the development of chronic conditions that lead to multiple rehospitalizations, the most significant one of which would be the development of heart failure,” Dr. Jain said. “However, it was difficult to stratify because, again, many of these patients were very young and so they did not carry the diagnosis for heart failure, so we couldn’t complete that subset analysis.”
The goal is to extend the study period out to 2023, Dr. Jain said. “We know that these are very crude and rudimentary data findings that we presented so far, but we’re hoping that the final paper gives us a chance to flesh out all the details of our study and also gives us a chance to expand going forward,” he said.
The findings are in line with other research into the effects of marijuana and cardiovascular disease, said Carl “Chip” Lavie, MD, medical director for cardiac rehabilitation and prevention at the John Ochsner Heart and Vascular Institute in New Orleans who’s published a number of studies on PAD and substance use, including marijuana.
“It is known that cannabis is associated with more vasoconstriction, has sympathomimetic effects, causes endothelial dysfunction and increased platelet aggregation, and is known to increase the risk of acute myocardial infarction, especially in the hour or so after use,” he said in written comments sent to this news organization.
“It is also well known to be a cause of thromboangiitis obliterans, which is in the PAD family,” he added. “Based on these mechanisms, one would expect an increased PAD and, especially, PAD events. The 3.7-fold increased risk is supportive of this increased PAD.”
One study strength, Dr. Lavie pointed out, is that it’s one of the few studies that found an association between marijuana and PAD, which hasn’t been studied as well as other cardiovascular endpoints. “However,” he said, “the limitation is this is just an inpatient sample, and it is all based on coding – e.g., a patient could have PAD and it may not have been coded.”
PHOENIX – although there was no greater risk of death from myocardial infarction or other cardiac causes or need for revascularization.
The researchers noted, however, that the study population was young, with an average age of 37.4 years, and that the study period, from 2016 to 2019, predates the legalization of recreational marijuana in a number of states.
Nonetheless, even in this young study population, marijuana users’ risk of developing peripheral artery disease (PAD) was 3.68 times greater (P < .001) than that of nonusers. PAD at a young age could precede worse outcomes later in life, the study authors said.
“Basically, marijuana users were at increased risk of being diagnosed with peripheral artery disease, but there was no increased risk for them requiring any intervention, such as a peripheral vascular intervention, nor were they at increased risk of death from what we found,” said Hirva Vyas, DO, an internal medicine resident at Hackensack University Medical Center in New Jersey, who presented the results at the Society for Cardiovascular Angiography & Interventions annual scientific sessions.
The study used data on 623,768 marijuana users from the National Inpatient Sample, a nationwide database of inpatient visits covered by all public and commercial payers, then extracted a diagnosis for PAD from all 30 million–plus patient encounters to compare PAD rates between marijuana users and nonusers. Marijuana users were more likely to be White and to have elective rather than emergency admissions (P < .001). The researchers used diagnostic codes to identify marijuana users and PAD patients.
Recreational marijuana is legal in 22 states and the District of Columbia, according to ProCon.org. Since 2019, the last year of the study, 11 states have legalized marijuana for recreational use. “It’s a data point that we studied at one point in time, only from 2016 to 2019,” Dr. Vyas said in an interview.
“As we’ve seen over the past 4-5 years, legalization has skyrocketed and recreational use has become more and more favorable not only among younger folks but older folks,” study coauthor Harsh Jain, MD, a second-year internal medicine resident at Montefiore Medical Center in New York, said in the interview. “It would be really refreshing to see how these data change as we look at endpoints from 2019 to 2023.”
Because of the young age of the study population, Dr. Jain said, these findings may not accurately represent the true cardiovascular risks of marijuana use, especially later in life.
“One of the biggest secondary endpoints that we wanted to study was the development of chronic conditions that lead to multiple rehospitalizations, the most significant one of which would be the development of heart failure,” Dr. Jain said. “However, it was difficult to stratify because, again, many of these patients were very young and so they did not carry the diagnosis for heart failure, so we couldn’t complete that subset analysis.”
The goal is to extend the study period out to 2023, Dr. Jain said. “We know that these are very crude and rudimentary data findings that we presented so far, but we’re hoping that the final paper gives us a chance to flesh out all the details of our study and also gives us a chance to expand going forward,” he said.
The findings are in line with other research into the effects of marijuana and cardiovascular disease, said Carl “Chip” Lavie, MD, medical director for cardiac rehabilitation and prevention at the John Ochsner Heart and Vascular Institute in New Orleans who’s published a number of studies on PAD and substance use, including marijuana.
“It is known that cannabis is associated with more vasoconstriction, has sympathomimetic effects, causes endothelial dysfunction and increased platelet aggregation, and is known to increase the risk of acute myocardial infarction, especially in the hour or so after use,” he said in written comments sent to this news organization.
“It is also well known to be a cause of thromboangiitis obliterans, which is in the PAD family,” he added. “Based on these mechanisms, one would expect an increased PAD and, especially, PAD events. The 3.7-fold increased risk is supportive of this increased PAD.”
One study strength, Dr. Lavie pointed out, is that it’s one of the few studies that found an association between marijuana and PAD, which hasn’t been studied as well as other cardiovascular endpoints. “However,” he said, “the limitation is this is just an inpatient sample, and it is all based on coding – e.g., a patient could have PAD and it may not have been coded.”
AT SCAI 2023
Endovascular approach best for below-knee limb-threatening ischemia?
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
FROM THE LANCET
Specific brain damage links hypertension to cognitive impairment
Researchers have identified specific regions of the brain that appear to be damaged by high blood pressure. The finding may explain the link between hypertension and cognitive impairment.
They used genetic information from genome-wide association studies (GWASs) and MRI scans of the brain to study the relationship between hypertension, changes in brain structures, and cognitive impairment. Using Mendelian randomization techniques, they identified nine brain structures related to cognitive impairment that are affected by blood pressure.
“We knew before that raised blood pressure was related to changes in the brain, but our research has narrowed down the changes to those that appear to be potentially causally related to cognitive impairment,” senior author Tomasz Guzik, professor of cardiovascular medicine, at the University of Edinburgh and of the Jagiellonian University, Krakow, Poland, told this news organization.
“Our study confirms a potentially causal relationship between raised blood pressure and cognitive impairment, emphasizing the importance of preventing and treating hypertension,” Prof. Guzik noted.
“But it also identifies the brain culprits of this relationship,” he added.
In the future, it may be possible to assess these nine brain structures in people with high blood pressure to identify those at increased risk of developing cognitive impairment, he said. “These patients may need more intensive care for their blood pressure. We can also investigate these brain structures for potential signaling pathways and molecular changes to see if we can find new targets for treatment to prevent cognitive impairment.”
For this report, the investigators married together different research datasets to identify brain structures potentially responsible for the effects of blood pressure on cognitive function, using results from previous GWASs and observational data from 39,000 people in the UK Biobank registry for whom brain MRI data were available.
First, they mapped brain structures potentially influenced by blood pressure in midlife using MRI scans from people in the UK Biobank registry. Then they examined the relationship between blood pressure and cognitive function in the UK Biobank registry. Next, of the brain structures affected by blood pressure, they identified those that are causally linked to cognitive impairment.
This was possible thanks to genetic markers coding for increased blood pressure, brain structure imaging phenotypes, and those coding for cognitive impairment that could be used in Mendelian randomization studies.
“We looked at 3935 brain magnetic resonance imaging–derived phenotypes in the brain and cognitive function defined by fluid intelligence score to identify genetically predicted causal relationships,” Prof. Guzik said.
They identified 200 brain structures that were causally affected by systolic blood pressure. Of these, nine were also causally related to cognitive impairment. The results were validated in a second prospective cohort of patients with hypertension.
“Some of these structures, including putamen and the white matter regions spanning between the anterior corona radiata, anterior thalamic radiation, and anterior limb of the internal capsule, may represent the target brain regions at which systolic blood pressure acts on cognitive function,” the authors comment.
In an accompanying editorial, Ernesto Schiffrin, MD, and James Engert, PhD, McGill University, Montreal, say that further mechanistic studies of the effects of blood pressure on cognitive function are required to determine precise causal pathways and the roles of relevant brain regions.
“Eventually, biomarkers could be developed to inform antihypertensive trials. Whether clinical trials targeting the specific brain structures will be feasible or if specific antihypertensives could be found that target specific structures remains to be demonstrated,” they write.
“Thus, these new studies could lead to an understanding of the signaling pathways that explain how these structures relate vascular damage to cognitive impairment in hypertension, and contribute to the development of novel interventions to more successfully address the scourge of cognitive decline and dementia in the future,” the editorialists conclude.
The study was funded by the European Research Council, the British Heart Foundation, and the Italian Ministry of Health.
A version of this article first appeared on Medscape.com.
Researchers have identified specific regions of the brain that appear to be damaged by high blood pressure. The finding may explain the link between hypertension and cognitive impairment.
They used genetic information from genome-wide association studies (GWASs) and MRI scans of the brain to study the relationship between hypertension, changes in brain structures, and cognitive impairment. Using Mendelian randomization techniques, they identified nine brain structures related to cognitive impairment that are affected by blood pressure.
“We knew before that raised blood pressure was related to changes in the brain, but our research has narrowed down the changes to those that appear to be potentially causally related to cognitive impairment,” senior author Tomasz Guzik, professor of cardiovascular medicine, at the University of Edinburgh and of the Jagiellonian University, Krakow, Poland, told this news organization.
“Our study confirms a potentially causal relationship between raised blood pressure and cognitive impairment, emphasizing the importance of preventing and treating hypertension,” Prof. Guzik noted.
“But it also identifies the brain culprits of this relationship,” he added.
In the future, it may be possible to assess these nine brain structures in people with high blood pressure to identify those at increased risk of developing cognitive impairment, he said. “These patients may need more intensive care for their blood pressure. We can also investigate these brain structures for potential signaling pathways and molecular changes to see if we can find new targets for treatment to prevent cognitive impairment.”
For this report, the investigators married together different research datasets to identify brain structures potentially responsible for the effects of blood pressure on cognitive function, using results from previous GWASs and observational data from 39,000 people in the UK Biobank registry for whom brain MRI data were available.
First, they mapped brain structures potentially influenced by blood pressure in midlife using MRI scans from people in the UK Biobank registry. Then they examined the relationship between blood pressure and cognitive function in the UK Biobank registry. Next, of the brain structures affected by blood pressure, they identified those that are causally linked to cognitive impairment.
This was possible thanks to genetic markers coding for increased blood pressure, brain structure imaging phenotypes, and those coding for cognitive impairment that could be used in Mendelian randomization studies.
“We looked at 3935 brain magnetic resonance imaging–derived phenotypes in the brain and cognitive function defined by fluid intelligence score to identify genetically predicted causal relationships,” Prof. Guzik said.
They identified 200 brain structures that were causally affected by systolic blood pressure. Of these, nine were also causally related to cognitive impairment. The results were validated in a second prospective cohort of patients with hypertension.
“Some of these structures, including putamen and the white matter regions spanning between the anterior corona radiata, anterior thalamic radiation, and anterior limb of the internal capsule, may represent the target brain regions at which systolic blood pressure acts on cognitive function,” the authors comment.
In an accompanying editorial, Ernesto Schiffrin, MD, and James Engert, PhD, McGill University, Montreal, say that further mechanistic studies of the effects of blood pressure on cognitive function are required to determine precise causal pathways and the roles of relevant brain regions.
“Eventually, biomarkers could be developed to inform antihypertensive trials. Whether clinical trials targeting the specific brain structures will be feasible or if specific antihypertensives could be found that target specific structures remains to be demonstrated,” they write.
“Thus, these new studies could lead to an understanding of the signaling pathways that explain how these structures relate vascular damage to cognitive impairment in hypertension, and contribute to the development of novel interventions to more successfully address the scourge of cognitive decline and dementia in the future,” the editorialists conclude.
The study was funded by the European Research Council, the British Heart Foundation, and the Italian Ministry of Health.
A version of this article first appeared on Medscape.com.
Researchers have identified specific regions of the brain that appear to be damaged by high blood pressure. The finding may explain the link between hypertension and cognitive impairment.
They used genetic information from genome-wide association studies (GWASs) and MRI scans of the brain to study the relationship between hypertension, changes in brain structures, and cognitive impairment. Using Mendelian randomization techniques, they identified nine brain structures related to cognitive impairment that are affected by blood pressure.
“We knew before that raised blood pressure was related to changes in the brain, but our research has narrowed down the changes to those that appear to be potentially causally related to cognitive impairment,” senior author Tomasz Guzik, professor of cardiovascular medicine, at the University of Edinburgh and of the Jagiellonian University, Krakow, Poland, told this news organization.
“Our study confirms a potentially causal relationship between raised blood pressure and cognitive impairment, emphasizing the importance of preventing and treating hypertension,” Prof. Guzik noted.
“But it also identifies the brain culprits of this relationship,” he added.
In the future, it may be possible to assess these nine brain structures in people with high blood pressure to identify those at increased risk of developing cognitive impairment, he said. “These patients may need more intensive care for their blood pressure. We can also investigate these brain structures for potential signaling pathways and molecular changes to see if we can find new targets for treatment to prevent cognitive impairment.”
For this report, the investigators married together different research datasets to identify brain structures potentially responsible for the effects of blood pressure on cognitive function, using results from previous GWASs and observational data from 39,000 people in the UK Biobank registry for whom brain MRI data were available.
First, they mapped brain structures potentially influenced by blood pressure in midlife using MRI scans from people in the UK Biobank registry. Then they examined the relationship between blood pressure and cognitive function in the UK Biobank registry. Next, of the brain structures affected by blood pressure, they identified those that are causally linked to cognitive impairment.
This was possible thanks to genetic markers coding for increased blood pressure, brain structure imaging phenotypes, and those coding for cognitive impairment that could be used in Mendelian randomization studies.
“We looked at 3935 brain magnetic resonance imaging–derived phenotypes in the brain and cognitive function defined by fluid intelligence score to identify genetically predicted causal relationships,” Prof. Guzik said.
They identified 200 brain structures that were causally affected by systolic blood pressure. Of these, nine were also causally related to cognitive impairment. The results were validated in a second prospective cohort of patients with hypertension.
“Some of these structures, including putamen and the white matter regions spanning between the anterior corona radiata, anterior thalamic radiation, and anterior limb of the internal capsule, may represent the target brain regions at which systolic blood pressure acts on cognitive function,” the authors comment.
In an accompanying editorial, Ernesto Schiffrin, MD, and James Engert, PhD, McGill University, Montreal, say that further mechanistic studies of the effects of blood pressure on cognitive function are required to determine precise causal pathways and the roles of relevant brain regions.
“Eventually, biomarkers could be developed to inform antihypertensive trials. Whether clinical trials targeting the specific brain structures will be feasible or if specific antihypertensives could be found that target specific structures remains to be demonstrated,” they write.
“Thus, these new studies could lead to an understanding of the signaling pathways that explain how these structures relate vascular damage to cognitive impairment in hypertension, and contribute to the development of novel interventions to more successfully address the scourge of cognitive decline and dementia in the future,” the editorialists conclude.
The study was funded by the European Research Council, the British Heart Foundation, and the Italian Ministry of Health.
A version of this article first appeared on Medscape.com.