Ulcerative colitis is a chronic inflammatory condition that characteristically involves the large bowel. Disease activity usually follows a pattern of periods of active inflammation alternating with periods of remission. Approximately 15% of patients experience an aggressive course of ulcerative colitis. Acute severe ulcerative colitis (ASUC) is a life-threatening medical emergency, which may require hospitalization for prompt medical treatment and colectomy if medical treatment fails. Predictors of an aggressive disease course and colectomy include young age at the time of diagnosis, extensive disease, severe endoscopic disease activity, presence of extraintestinal manifestations, elevated inflammatory markers, and early need for corticosteroids.
The diagnosis of ASUC is based on the Mayo Clinic Score and the Truelove and Witts criteria which consists of the presence of six or more bloody stools per day and at least one of these signs of systemic toxicity:
• Pulse rate > 90 beats/min
• Temperature > 100.04 °F
• Hemoglobin < 10.5 g/dL
• Erythrocyte sedimentation rate (ESR) > 30 mm/h
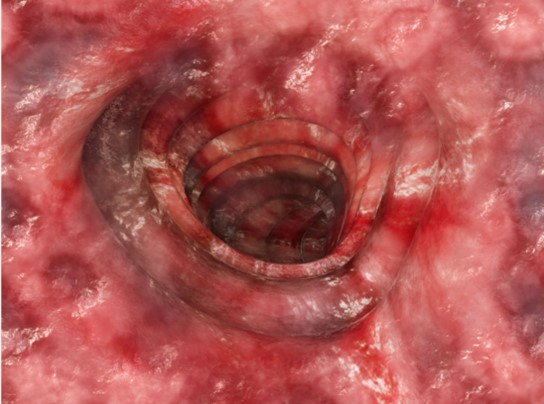
Further evaluation in patients with suspected ASUC aims to exclude alternative diagnoses and to determine the severity and extent of disease. Abdominal radiographs are obtained to rule out colonic dilatation and to evaluate for the possibility of microperforations. Stool studies should be obtained to evaluate for infections such as C difficile. To assess for the severity of mucosal disease a limited lower endoscopy is usually performed in hospitalized patients with ASUC. In addition, it allows for the opportunity to perform a biopsy to rule out cytomegalovirus as the cause of the disease flare. However, a colonoscopy should be avoided in these patients because of the increased risk for colonic dilation and perforation; a carefully performed flexible sigmoidoscopy with minimal insufflation by an experienced operator is sufficient for most patients. Endoscopic features of ASUC include erythema, absent vascular pattern, friability, erosions, and ulcerations.
The mainstay of management of hospitalized individuals with ASUC is intravenous corticosteroids. However, up to one third of patients may not show improvement in clinical or biochemical markers after treatment with steroids. In hospitalized patients with ASUC refractory to 3 to 5 days of intravenous corticosteroids infliximab or cyclosporin are suggested. Colectomy is a treatment option for patients unresponsive to medical therapy or for patients who develop life-threatening complications (colonic perforation, toxic megacolon, etc.)
Leyla Ghazi, MD, Physician, Dartmouth Health, GI Associates, Concord, New Hampshire.
Leyla Ghazi, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.