User login
A Better Approach to the Diagnosis of PE
Penny E, a 48-year-old woman with a history of asthma, presents with wheezing and respiratory distress. There are no clinical signs of deep vein thrombosis or hemoptysis. PE is not your most likely diagnosis, but it is included in the differential, so you order a D
PE is the third most common type of cardiovascular disease after coronary artery disease and stroke, with an estimated incidence in the United States of 1-2/1000 individuals and a 30-day mortality rate between 10% and 30%.2 Improved adherence to a clinical decision support system has been shown to significantly decrease the number of diagnostic tests performed and the number of diagnostic failures.3
A diagnostic algorithm that includes the Wells criteria and a
Further, it is common for a
Three items of the original Wells criteria—clinical signs of deep vein thrombosis, hemoptysis, and whether PE is the most likely diagnosis—are the most predictive for PE.8 The development of a more efficient algorithm based on these 3 items that uses differential D
STUDY SUMMARY
Simplified algorithm diagnoses PE with fewer CTPAs
The YEARS study was a prospective cohort study conducted in 12 hospitals in the Netherlands that included 3616 patients with clinically suspected PE.1 A total of 151 patients met exclusion criteria (life expectancy < 3 months, ongoing anticoagulation treatment, pregnancy, and contraindication to CTPA). Investigators managed the remaining 3465 study patients according to the YEARS algorithm, which calls for obtaining a
PE was considered excluded if a patient had a
[polldaddy:10428150]
Continue to: Of the 1743 patients...
Of the 1743 patients who had none of the 3 YEARS items, 1320 had a D
Eighteen of the 2964 patients who had PE ruled out by the YEARS algorithm at baseline were found to have symptomatic VTE during the follow-up period (0.61%), with 6 patients (0.20%) sustaining a fatal PE. The 3-month incidence of VTE in patients who did not have CTPA was 0.43%, which is similar to the 0.34% reported in a previous meta-analysis of the Wells rule algorithm.13 Overall, fatal PE occurred in 0.3% of patients in the YEARS cohort vs 0.6% in a meta-analysis of studies using standard algorithms.14
Using an intention-to-diagnose analysis, 1611 (46%) patients did not have a CTPA indicated by the YEARS algorithm compared with 1174 (34%) using the Wells algorithm, for an absolute difference of 13% and estimated cost savings of $283,176 in this sample. The per-protocol analysis also had a decrease of CTPA examinations in favor of the YEARS algorithm, ruling out 1651 (48%) patients—a decrease of 14% and an estimated savings of $309,096.
WHAT’S NEW
High-level evidence says 14% fewer CTPAs
The YEARS study provides a high level of evidence that a new, simple diagnostic algorithm can reliably and efficiently exclude PE and decrease the need for CTPA by 14% (absolute difference) when compared with using the Wells rule and fixed
CAVEATS
No adjusting D -dimer for age
The YEARS criteria do not consider an age-adjusted
Continue to: CHALLENGES TO IMPLEMENTATION
CHALLENGES TO IMPLEMENTATION
None to speak of
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2019. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2019;68[5]:286-287,295).
1. van der Hulle T, Cheung WY, Kooij S, et al; YEARS study group. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390:289-297.
2. Beckman MG, Hooper WC, Critchley SE, et al. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38(suppl 4):S495-S501.
3. Douma RA, Mos ICM, Erkens PMG, et al; Prometheus Study Group. Performance of 4 clinical decision rules in the diagnostic management of acute pulmonary embolism. Ann Intern Med. 2011;154:709-718.
4. van Es N, van der Hulle T, van Es J, et al. Wells Rule and d -dimer testing to rule out pulmonary embolism: a systematic review and individual-patient data meta-analysis. Ann Intern Med. 2016;165:253-261.
5. Roy P-M, Meyer G, Vielle B, et al; EMDEPU Study Group. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006;144:157-164.
6. Newnham M, Stone H, Summerfield R, et al. Performance of algorithms and pre-test probability scores is often overlooked in the diagnosis of pulmonary embolism. BMJ. 2013;346:f1557.
7. Righini M, Van Es J, Den Exter PL, et al. Age-adjusted d -dimer cutoff levels to rule out pulmonary embolism. JAMA. 2014;311:1117-1124.
8. van Es J, Beenen LFM, Douma RA, et al. A simple decision rule including d -dimer to reduce the need for computed tomography scanning in patients with suspected pulmonary embolism. J Thromb Haemost. 2015;13:1428-1435.
9. Kooiman J, Klok FA, Mos ICM, et al. Incidence and predictors of contrast-induced nephropathy following CT-angiography for clinically suspected acute pulmonary embolism. J Thromb Haemost. 2010;8:409-411.
10. Sarma A, Heilbrun ME, Conner KE, et al. Radiation and chest CT scan examinations: what do we know? Chest. 2012;142:750-760.
11. Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071-2077.
12. Verma K, Legnani C, Palareti G. Cost-minimization analysis of venous thromboembolism diagnosis: comparison of standalone imaging with a strategy incorporating d -dimer for exclusion of venous thromboembolism. Res Pract Thromb Haemost. 2017;1:57-61.
13. Pasha SM, Klok FA, Snoep JD, et al. Safety of excluding acute pulmonary embolism based on an unlikely clinical probability by the Wells rule and normal d -dimer concentration: a meta-analysis. Thromb Res. 2010;125:e123-e127.
14. Mos ICM, Klok FA, Kroft LJM, et al. Safety of ruling out acute pulmonary embolism by normal computed tomography pulmonary angiography in patients with an indication for computed tomography: systematic review and meta-analysis. J Thromb Haemost. 2009;7:1491-1498.
Penny E, a 48-year-old woman with a history of asthma, presents with wheezing and respiratory distress. There are no clinical signs of deep vein thrombosis or hemoptysis. PE is not your most likely diagnosis, but it is included in the differential, so you order a D
PE is the third most common type of cardiovascular disease after coronary artery disease and stroke, with an estimated incidence in the United States of 1-2/1000 individuals and a 30-day mortality rate between 10% and 30%.2 Improved adherence to a clinical decision support system has been shown to significantly decrease the number of diagnostic tests performed and the number of diagnostic failures.3
A diagnostic algorithm that includes the Wells criteria and a
Further, it is common for a
Three items of the original Wells criteria—clinical signs of deep vein thrombosis, hemoptysis, and whether PE is the most likely diagnosis—are the most predictive for PE.8 The development of a more efficient algorithm based on these 3 items that uses differential D
STUDY SUMMARY
Simplified algorithm diagnoses PE with fewer CTPAs
The YEARS study was a prospective cohort study conducted in 12 hospitals in the Netherlands that included 3616 patients with clinically suspected PE.1 A total of 151 patients met exclusion criteria (life expectancy < 3 months, ongoing anticoagulation treatment, pregnancy, and contraindication to CTPA). Investigators managed the remaining 3465 study patients according to the YEARS algorithm, which calls for obtaining a
PE was considered excluded if a patient had a
[polldaddy:10428150]
Continue to: Of the 1743 patients...
Of the 1743 patients who had none of the 3 YEARS items, 1320 had a D
Eighteen of the 2964 patients who had PE ruled out by the YEARS algorithm at baseline were found to have symptomatic VTE during the follow-up period (0.61%), with 6 patients (0.20%) sustaining a fatal PE. The 3-month incidence of VTE in patients who did not have CTPA was 0.43%, which is similar to the 0.34% reported in a previous meta-analysis of the Wells rule algorithm.13 Overall, fatal PE occurred in 0.3% of patients in the YEARS cohort vs 0.6% in a meta-analysis of studies using standard algorithms.14
Using an intention-to-diagnose analysis, 1611 (46%) patients did not have a CTPA indicated by the YEARS algorithm compared with 1174 (34%) using the Wells algorithm, for an absolute difference of 13% and estimated cost savings of $283,176 in this sample. The per-protocol analysis also had a decrease of CTPA examinations in favor of the YEARS algorithm, ruling out 1651 (48%) patients—a decrease of 14% and an estimated savings of $309,096.
WHAT’S NEW
High-level evidence says 14% fewer CTPAs
The YEARS study provides a high level of evidence that a new, simple diagnostic algorithm can reliably and efficiently exclude PE and decrease the need for CTPA by 14% (absolute difference) when compared with using the Wells rule and fixed
CAVEATS
No adjusting D -dimer for age
The YEARS criteria do not consider an age-adjusted
Continue to: CHALLENGES TO IMPLEMENTATION
CHALLENGES TO IMPLEMENTATION
None to speak of
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2019. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2019;68[5]:286-287,295).
Penny E, a 48-year-old woman with a history of asthma, presents with wheezing and respiratory distress. There are no clinical signs of deep vein thrombosis or hemoptysis. PE is not your most likely diagnosis, but it is included in the differential, so you order a D
PE is the third most common type of cardiovascular disease after coronary artery disease and stroke, with an estimated incidence in the United States of 1-2/1000 individuals and a 30-day mortality rate between 10% and 30%.2 Improved adherence to a clinical decision support system has been shown to significantly decrease the number of diagnostic tests performed and the number of diagnostic failures.3
A diagnostic algorithm that includes the Wells criteria and a
Further, it is common for a
Three items of the original Wells criteria—clinical signs of deep vein thrombosis, hemoptysis, and whether PE is the most likely diagnosis—are the most predictive for PE.8 The development of a more efficient algorithm based on these 3 items that uses differential D
STUDY SUMMARY
Simplified algorithm diagnoses PE with fewer CTPAs
The YEARS study was a prospective cohort study conducted in 12 hospitals in the Netherlands that included 3616 patients with clinically suspected PE.1 A total of 151 patients met exclusion criteria (life expectancy < 3 months, ongoing anticoagulation treatment, pregnancy, and contraindication to CTPA). Investigators managed the remaining 3465 study patients according to the YEARS algorithm, which calls for obtaining a
PE was considered excluded if a patient had a
[polldaddy:10428150]
Continue to: Of the 1743 patients...
Of the 1743 patients who had none of the 3 YEARS items, 1320 had a D
Eighteen of the 2964 patients who had PE ruled out by the YEARS algorithm at baseline were found to have symptomatic VTE during the follow-up period (0.61%), with 6 patients (0.20%) sustaining a fatal PE. The 3-month incidence of VTE in patients who did not have CTPA was 0.43%, which is similar to the 0.34% reported in a previous meta-analysis of the Wells rule algorithm.13 Overall, fatal PE occurred in 0.3% of patients in the YEARS cohort vs 0.6% in a meta-analysis of studies using standard algorithms.14
Using an intention-to-diagnose analysis, 1611 (46%) patients did not have a CTPA indicated by the YEARS algorithm compared with 1174 (34%) using the Wells algorithm, for an absolute difference of 13% and estimated cost savings of $283,176 in this sample. The per-protocol analysis also had a decrease of CTPA examinations in favor of the YEARS algorithm, ruling out 1651 (48%) patients—a decrease of 14% and an estimated savings of $309,096.
WHAT’S NEW
High-level evidence says 14% fewer CTPAs
The YEARS study provides a high level of evidence that a new, simple diagnostic algorithm can reliably and efficiently exclude PE and decrease the need for CTPA by 14% (absolute difference) when compared with using the Wells rule and fixed
CAVEATS
No adjusting D -dimer for age
The YEARS criteria do not consider an age-adjusted
Continue to: CHALLENGES TO IMPLEMENTATION
CHALLENGES TO IMPLEMENTATION
None to speak of
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2019. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2019;68[5]:286-287,295).
1. van der Hulle T, Cheung WY, Kooij S, et al; YEARS study group. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390:289-297.
2. Beckman MG, Hooper WC, Critchley SE, et al. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38(suppl 4):S495-S501.
3. Douma RA, Mos ICM, Erkens PMG, et al; Prometheus Study Group. Performance of 4 clinical decision rules in the diagnostic management of acute pulmonary embolism. Ann Intern Med. 2011;154:709-718.
4. van Es N, van der Hulle T, van Es J, et al. Wells Rule and d -dimer testing to rule out pulmonary embolism: a systematic review and individual-patient data meta-analysis. Ann Intern Med. 2016;165:253-261.
5. Roy P-M, Meyer G, Vielle B, et al; EMDEPU Study Group. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006;144:157-164.
6. Newnham M, Stone H, Summerfield R, et al. Performance of algorithms and pre-test probability scores is often overlooked in the diagnosis of pulmonary embolism. BMJ. 2013;346:f1557.
7. Righini M, Van Es J, Den Exter PL, et al. Age-adjusted d -dimer cutoff levels to rule out pulmonary embolism. JAMA. 2014;311:1117-1124.
8. van Es J, Beenen LFM, Douma RA, et al. A simple decision rule including d -dimer to reduce the need for computed tomography scanning in patients with suspected pulmonary embolism. J Thromb Haemost. 2015;13:1428-1435.
9. Kooiman J, Klok FA, Mos ICM, et al. Incidence and predictors of contrast-induced nephropathy following CT-angiography for clinically suspected acute pulmonary embolism. J Thromb Haemost. 2010;8:409-411.
10. Sarma A, Heilbrun ME, Conner KE, et al. Radiation and chest CT scan examinations: what do we know? Chest. 2012;142:750-760.
11. Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071-2077.
12. Verma K, Legnani C, Palareti G. Cost-minimization analysis of venous thromboembolism diagnosis: comparison of standalone imaging with a strategy incorporating d -dimer for exclusion of venous thromboembolism. Res Pract Thromb Haemost. 2017;1:57-61.
13. Pasha SM, Klok FA, Snoep JD, et al. Safety of excluding acute pulmonary embolism based on an unlikely clinical probability by the Wells rule and normal d -dimer concentration: a meta-analysis. Thromb Res. 2010;125:e123-e127.
14. Mos ICM, Klok FA, Kroft LJM, et al. Safety of ruling out acute pulmonary embolism by normal computed tomography pulmonary angiography in patients with an indication for computed tomography: systematic review and meta-analysis. J Thromb Haemost. 2009;7:1491-1498.
1. van der Hulle T, Cheung WY, Kooij S, et al; YEARS study group. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390:289-297.
2. Beckman MG, Hooper WC, Critchley SE, et al. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38(suppl 4):S495-S501.
3. Douma RA, Mos ICM, Erkens PMG, et al; Prometheus Study Group. Performance of 4 clinical decision rules in the diagnostic management of acute pulmonary embolism. Ann Intern Med. 2011;154:709-718.
4. van Es N, van der Hulle T, van Es J, et al. Wells Rule and d -dimer testing to rule out pulmonary embolism: a systematic review and individual-patient data meta-analysis. Ann Intern Med. 2016;165:253-261.
5. Roy P-M, Meyer G, Vielle B, et al; EMDEPU Study Group. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006;144:157-164.
6. Newnham M, Stone H, Summerfield R, et al. Performance of algorithms and pre-test probability scores is often overlooked in the diagnosis of pulmonary embolism. BMJ. 2013;346:f1557.
7. Righini M, Van Es J, Den Exter PL, et al. Age-adjusted d -dimer cutoff levels to rule out pulmonary embolism. JAMA. 2014;311:1117-1124.
8. van Es J, Beenen LFM, Douma RA, et al. A simple decision rule including d -dimer to reduce the need for computed tomography scanning in patients with suspected pulmonary embolism. J Thromb Haemost. 2015;13:1428-1435.
9. Kooiman J, Klok FA, Mos ICM, et al. Incidence and predictors of contrast-induced nephropathy following CT-angiography for clinically suspected acute pulmonary embolism. J Thromb Haemost. 2010;8:409-411.
10. Sarma A, Heilbrun ME, Conner KE, et al. Radiation and chest CT scan examinations: what do we know? Chest. 2012;142:750-760.
11. Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071-2077.
12. Verma K, Legnani C, Palareti G. Cost-minimization analysis of venous thromboembolism diagnosis: comparison of standalone imaging with a strategy incorporating d -dimer for exclusion of venous thromboembolism. Res Pract Thromb Haemost. 2017;1:57-61.
13. Pasha SM, Klok FA, Snoep JD, et al. Safety of excluding acute pulmonary embolism based on an unlikely clinical probability by the Wells rule and normal d -dimer concentration: a meta-analysis. Thromb Res. 2010;125:e123-e127.
14. Mos ICM, Klok FA, Kroft LJM, et al. Safety of ruling out acute pulmonary embolism by normal computed tomography pulmonary angiography in patients with an indication for computed tomography: systematic review and meta-analysis. J Thromb Haemost. 2009;7:1491-1498.
A better approach to the diagnosis of PE
ILLUSTRATIVE CASE
Penny E is a 48-year-old woman with a history of asthma who presents with wheezing and respiratory distress. There are no clinical signs of deep vein thrombosis or hemoptysis. Pulmonary embolism (PE) is not your most likely diagnosis, but it is included in the differential, so you order a D-dimer concentration and it returns at 700 ng/mL. Should you order computed tomography pulmonary angiography (CTPA) to evaluate for PE?
PE is the third most common type of cardiovascular disease after coronary artery disease and stroke, with an estimated incidence in the United States of 1-2 people/1000 population and a 30-day mortality rate between 10% and 30%.2 Improved adherence to a clinical decision support system has been shown to significantly decrease the number of diagnostic tests performed and the number of diagnostic failures.3
The use of a diagnostic algorithm that includes the Wells’ criteria and a
Further, it is common for a
Three items of the original Wells’ criteria—clinical signs of deep vein thrombosis, hemoptysis, and whether PE is the most likely diagnosis—are the most predictive for PE.8 The development of a more efficient algorithm based on these 3 items that uses differential D
STUDY SUMMARY
Simplified algorithm diagnoses PE with fewer CTPAs
The YEARS study was a prospective cohort study conducted in 12 hospitals in the Netherlands that included 3616 patients with clinically suspected PE.1 After excluding 151 patients who met exclusion criteria (life expectancy < 3 months, ongoing anticoagulation treatment, pregnancy, and contraindication to CTPA), investigators managed 3465 study patients according to the YEARS algorithm. This algorithm called for obtaining a
Of the 1743 patients who had none of the 3 YEARS items, 1320 had a
Continue to: Eighteen of the 2964 patients...
Eighteen of the 2964 patients who had PE ruled out by the YEARS algorithm at baseline were found to have symptomatic VTE during the follow-up period (0.61%; 95% CI, 0.36-0.96), with 6 patients (0.20%; 95% CI, 0.07-0.44) sustaining a fatal PE. The 3-month incidence of VTE in patients who did not have CTPA was 0.43% (95% CI, 0.17-0.88), which is similar to the 0.34% (0.036-0.96) reported in a previous meta-analysis of the Wells’ rule algorithm.13 Overall, fatal PE occurred in 0.3% (95% CI, 0.12-0.78) of patients in the YEARS cohort vs 0.6% (0.4-1.1) in a meta-analysis of studies using standard algorithms.14
Using an intention-to-diagnose analysis, 1611 (46%) patients did not have a CTPA indicated by the YEARS algorithm compared with 1174 (34%) using the Wells’ algorithm, for an absolute difference of 13% (95% CI, 10-15) and estimated cost savings of $283,176 in this sample. The per-protocol analysis also had a decrease of CTPA examinations in favor of the YEARS algorithm, ruling out 1651 (48%) patients—a decrease of 14% (95% CI, 12-16) and an estimated savings of $309,096.
WHAT’S NEW
High-level evidence says 14% fewer CTPAs
The YEARS study provides a high level of evidence that a new, simple diagnostic algorithm can reliably and efficiently exclude PE and decrease the need for CTPA by 14% (absolute difference; 95% CI, 12-16) when compared with using the Wells’ rule and fixed
CAVEATS
No adjusting D -dimer for age
The YEARS criteria does not consider an age-adjusted
CHALLENGES TO IMPLEMENTATION
None to speak of
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. van der Hulle T, Cheung WY, Kooij S, et al. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390:289-297.
2. Beckman MG, Hooper WC, Critchley SE, et al. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38:S495-S501.
3. Douma RA, Mos ICM, Erkens PMG, et al. Performance of 4 clinical decision rules in the diagnostic management of acute pulmonary embolism. Ann Intern Med. 2011;154:709-718.
4. van Es N, van der Hulle T, van Es J, et al. Wells Rule and D-dimer testing to rule out pulmonary embolism. Ann Intern Med. 2016;165:253-261.
5. Roy P-M, Meyer G, Vielle B, et al. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006;144:157-164.
6. Newnham M, Stone H, Summerfield R, et al. Performance of algorithms and pre-test probability scores is often overlooked in the diagnosis of pulmonary embolism. BMJ. 2013;346:f1557.
7. Righini M, Van Es J, Den Exter PL, et al. Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism. JAMA. 2014;311:1117-1124.
8. van Es J, Beenen LFM, Douma RA, et al. A simple decision rule including D-dimer to reduce the need for computed tomography scanning in patients with suspected pulmonary embolism. J Thromb Haemost. 2015;13:1428-1435.
9. Kooiman J, Klok FA, Mos ICM, et al. Incidence and predictors of contrast-induced nephropathy following CT-angiography for clinically suspected acute pulmonary embolism. J Thromb Haemost. 2010;8:409-411.
10. Sarma A, Heilbrun ME, Conner KE, et al. Radiation and chest CT scan examinations: what do we know? Chest. 2012;142:750-760.
11. Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071-2077.
12. Verma K, Legnani C, Palareti G. Cost-minimization analysis of venous thromboembolism diagnosis: comparison of standalone imaging with a strategy incorporating D-dimer for exclusion of venous thromboembolism. Res Pract Thromb Haemost. 2017;1:57-61.
13. Pasha SM, Klok FA, Snoep JD, et al. Safety of excluding acute pulmonary embolism based on an unlikely clinical probability by the Wells rule and normal D-dimer concentration: a meta-analysis. Thromb Res. 2010;125:e123-e127.
14. Mos ICM, Klok FA, Kroft LJM, et al. Safety of ruling out acute pulmonary embolism by normal computed tomography pulmonary angiography in patients with an indication for computed tomography: systematic review and meta-analysis. J Thromb Haemost. 2009;7:1491-1498.
ILLUSTRATIVE CASE
Penny E is a 48-year-old woman with a history of asthma who presents with wheezing and respiratory distress. There are no clinical signs of deep vein thrombosis or hemoptysis. Pulmonary embolism (PE) is not your most likely diagnosis, but it is included in the differential, so you order a D-dimer concentration and it returns at 700 ng/mL. Should you order computed tomography pulmonary angiography (CTPA) to evaluate for PE?
PE is the third most common type of cardiovascular disease after coronary artery disease and stroke, with an estimated incidence in the United States of 1-2 people/1000 population and a 30-day mortality rate between 10% and 30%.2 Improved adherence to a clinical decision support system has been shown to significantly decrease the number of diagnostic tests performed and the number of diagnostic failures.3
The use of a diagnostic algorithm that includes the Wells’ criteria and a
Further, it is common for a
Three items of the original Wells’ criteria—clinical signs of deep vein thrombosis, hemoptysis, and whether PE is the most likely diagnosis—are the most predictive for PE.8 The development of a more efficient algorithm based on these 3 items that uses differential D
STUDY SUMMARY
Simplified algorithm diagnoses PE with fewer CTPAs
The YEARS study was a prospective cohort study conducted in 12 hospitals in the Netherlands that included 3616 patients with clinically suspected PE.1 After excluding 151 patients who met exclusion criteria (life expectancy < 3 months, ongoing anticoagulation treatment, pregnancy, and contraindication to CTPA), investigators managed 3465 study patients according to the YEARS algorithm. This algorithm called for obtaining a
Of the 1743 patients who had none of the 3 YEARS items, 1320 had a
Continue to: Eighteen of the 2964 patients...
Eighteen of the 2964 patients who had PE ruled out by the YEARS algorithm at baseline were found to have symptomatic VTE during the follow-up period (0.61%; 95% CI, 0.36-0.96), with 6 patients (0.20%; 95% CI, 0.07-0.44) sustaining a fatal PE. The 3-month incidence of VTE in patients who did not have CTPA was 0.43% (95% CI, 0.17-0.88), which is similar to the 0.34% (0.036-0.96) reported in a previous meta-analysis of the Wells’ rule algorithm.13 Overall, fatal PE occurred in 0.3% (95% CI, 0.12-0.78) of patients in the YEARS cohort vs 0.6% (0.4-1.1) in a meta-analysis of studies using standard algorithms.14
Using an intention-to-diagnose analysis, 1611 (46%) patients did not have a CTPA indicated by the YEARS algorithm compared with 1174 (34%) using the Wells’ algorithm, for an absolute difference of 13% (95% CI, 10-15) and estimated cost savings of $283,176 in this sample. The per-protocol analysis also had a decrease of CTPA examinations in favor of the YEARS algorithm, ruling out 1651 (48%) patients—a decrease of 14% (95% CI, 12-16) and an estimated savings of $309,096.
WHAT’S NEW
High-level evidence says 14% fewer CTPAs
The YEARS study provides a high level of evidence that a new, simple diagnostic algorithm can reliably and efficiently exclude PE and decrease the need for CTPA by 14% (absolute difference; 95% CI, 12-16) when compared with using the Wells’ rule and fixed
CAVEATS
No adjusting D -dimer for age
The YEARS criteria does not consider an age-adjusted
CHALLENGES TO IMPLEMENTATION
None to speak of
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
Penny E is a 48-year-old woman with a history of asthma who presents with wheezing and respiratory distress. There are no clinical signs of deep vein thrombosis or hemoptysis. Pulmonary embolism (PE) is not your most likely diagnosis, but it is included in the differential, so you order a D-dimer concentration and it returns at 700 ng/mL. Should you order computed tomography pulmonary angiography (CTPA) to evaluate for PE?
PE is the third most common type of cardiovascular disease after coronary artery disease and stroke, with an estimated incidence in the United States of 1-2 people/1000 population and a 30-day mortality rate between 10% and 30%.2 Improved adherence to a clinical decision support system has been shown to significantly decrease the number of diagnostic tests performed and the number of diagnostic failures.3
The use of a diagnostic algorithm that includes the Wells’ criteria and a
Further, it is common for a
Three items of the original Wells’ criteria—clinical signs of deep vein thrombosis, hemoptysis, and whether PE is the most likely diagnosis—are the most predictive for PE.8 The development of a more efficient algorithm based on these 3 items that uses differential D
STUDY SUMMARY
Simplified algorithm diagnoses PE with fewer CTPAs
The YEARS study was a prospective cohort study conducted in 12 hospitals in the Netherlands that included 3616 patients with clinically suspected PE.1 After excluding 151 patients who met exclusion criteria (life expectancy < 3 months, ongoing anticoagulation treatment, pregnancy, and contraindication to CTPA), investigators managed 3465 study patients according to the YEARS algorithm. This algorithm called for obtaining a
Of the 1743 patients who had none of the 3 YEARS items, 1320 had a
Continue to: Eighteen of the 2964 patients...
Eighteen of the 2964 patients who had PE ruled out by the YEARS algorithm at baseline were found to have symptomatic VTE during the follow-up period (0.61%; 95% CI, 0.36-0.96), with 6 patients (0.20%; 95% CI, 0.07-0.44) sustaining a fatal PE. The 3-month incidence of VTE in patients who did not have CTPA was 0.43% (95% CI, 0.17-0.88), which is similar to the 0.34% (0.036-0.96) reported in a previous meta-analysis of the Wells’ rule algorithm.13 Overall, fatal PE occurred in 0.3% (95% CI, 0.12-0.78) of patients in the YEARS cohort vs 0.6% (0.4-1.1) in a meta-analysis of studies using standard algorithms.14
Using an intention-to-diagnose analysis, 1611 (46%) patients did not have a CTPA indicated by the YEARS algorithm compared with 1174 (34%) using the Wells’ algorithm, for an absolute difference of 13% (95% CI, 10-15) and estimated cost savings of $283,176 in this sample. The per-protocol analysis also had a decrease of CTPA examinations in favor of the YEARS algorithm, ruling out 1651 (48%) patients—a decrease of 14% (95% CI, 12-16) and an estimated savings of $309,096.
WHAT’S NEW
High-level evidence says 14% fewer CTPAs
The YEARS study provides a high level of evidence that a new, simple diagnostic algorithm can reliably and efficiently exclude PE and decrease the need for CTPA by 14% (absolute difference; 95% CI, 12-16) when compared with using the Wells’ rule and fixed
CAVEATS
No adjusting D -dimer for age
The YEARS criteria does not consider an age-adjusted
CHALLENGES TO IMPLEMENTATION
None to speak of
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. van der Hulle T, Cheung WY, Kooij S, et al. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390:289-297.
2. Beckman MG, Hooper WC, Critchley SE, et al. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38:S495-S501.
3. Douma RA, Mos ICM, Erkens PMG, et al. Performance of 4 clinical decision rules in the diagnostic management of acute pulmonary embolism. Ann Intern Med. 2011;154:709-718.
4. van Es N, van der Hulle T, van Es J, et al. Wells Rule and D-dimer testing to rule out pulmonary embolism. Ann Intern Med. 2016;165:253-261.
5. Roy P-M, Meyer G, Vielle B, et al. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006;144:157-164.
6. Newnham M, Stone H, Summerfield R, et al. Performance of algorithms and pre-test probability scores is often overlooked in the diagnosis of pulmonary embolism. BMJ. 2013;346:f1557.
7. Righini M, Van Es J, Den Exter PL, et al. Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism. JAMA. 2014;311:1117-1124.
8. van Es J, Beenen LFM, Douma RA, et al. A simple decision rule including D-dimer to reduce the need for computed tomography scanning in patients with suspected pulmonary embolism. J Thromb Haemost. 2015;13:1428-1435.
9. Kooiman J, Klok FA, Mos ICM, et al. Incidence and predictors of contrast-induced nephropathy following CT-angiography for clinically suspected acute pulmonary embolism. J Thromb Haemost. 2010;8:409-411.
10. Sarma A, Heilbrun ME, Conner KE, et al. Radiation and chest CT scan examinations: what do we know? Chest. 2012;142:750-760.
11. Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071-2077.
12. Verma K, Legnani C, Palareti G. Cost-minimization analysis of venous thromboembolism diagnosis: comparison of standalone imaging with a strategy incorporating D-dimer for exclusion of venous thromboembolism. Res Pract Thromb Haemost. 2017;1:57-61.
13. Pasha SM, Klok FA, Snoep JD, et al. Safety of excluding acute pulmonary embolism based on an unlikely clinical probability by the Wells rule and normal D-dimer concentration: a meta-analysis. Thromb Res. 2010;125:e123-e127.
14. Mos ICM, Klok FA, Kroft LJM, et al. Safety of ruling out acute pulmonary embolism by normal computed tomography pulmonary angiography in patients with an indication for computed tomography: systematic review and meta-analysis. J Thromb Haemost. 2009;7:1491-1498.
1. van der Hulle T, Cheung WY, Kooij S, et al. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390:289-297.
2. Beckman MG, Hooper WC, Critchley SE, et al. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38:S495-S501.
3. Douma RA, Mos ICM, Erkens PMG, et al. Performance of 4 clinical decision rules in the diagnostic management of acute pulmonary embolism. Ann Intern Med. 2011;154:709-718.
4. van Es N, van der Hulle T, van Es J, et al. Wells Rule and D-dimer testing to rule out pulmonary embolism. Ann Intern Med. 2016;165:253-261.
5. Roy P-M, Meyer G, Vielle B, et al. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006;144:157-164.
6. Newnham M, Stone H, Summerfield R, et al. Performance of algorithms and pre-test probability scores is often overlooked in the diagnosis of pulmonary embolism. BMJ. 2013;346:f1557.
7. Righini M, Van Es J, Den Exter PL, et al. Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism. JAMA. 2014;311:1117-1124.
8. van Es J, Beenen LFM, Douma RA, et al. A simple decision rule including D-dimer to reduce the need for computed tomography scanning in patients with suspected pulmonary embolism. J Thromb Haemost. 2015;13:1428-1435.
9. Kooiman J, Klok FA, Mos ICM, et al. Incidence and predictors of contrast-induced nephropathy following CT-angiography for clinically suspected acute pulmonary embolism. J Thromb Haemost. 2010;8:409-411.
10. Sarma A, Heilbrun ME, Conner KE, et al. Radiation and chest CT scan examinations: what do we know? Chest. 2012;142:750-760.
11. Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071-2077.
12. Verma K, Legnani C, Palareti G. Cost-minimization analysis of venous thromboembolism diagnosis: comparison of standalone imaging with a strategy incorporating D-dimer for exclusion of venous thromboembolism. Res Pract Thromb Haemost. 2017;1:57-61.
13. Pasha SM, Klok FA, Snoep JD, et al. Safety of excluding acute pulmonary embolism based on an unlikely clinical probability by the Wells rule and normal D-dimer concentration: a meta-analysis. Thromb Res. 2010;125:e123-e127.
14. Mos ICM, Klok FA, Kroft LJM, et al. Safety of ruling out acute pulmonary embolism by normal computed tomography pulmonary angiography in patients with an indication for computed tomography: systematic review and meta-analysis. J Thromb Haemost. 2009;7:1491-1498.
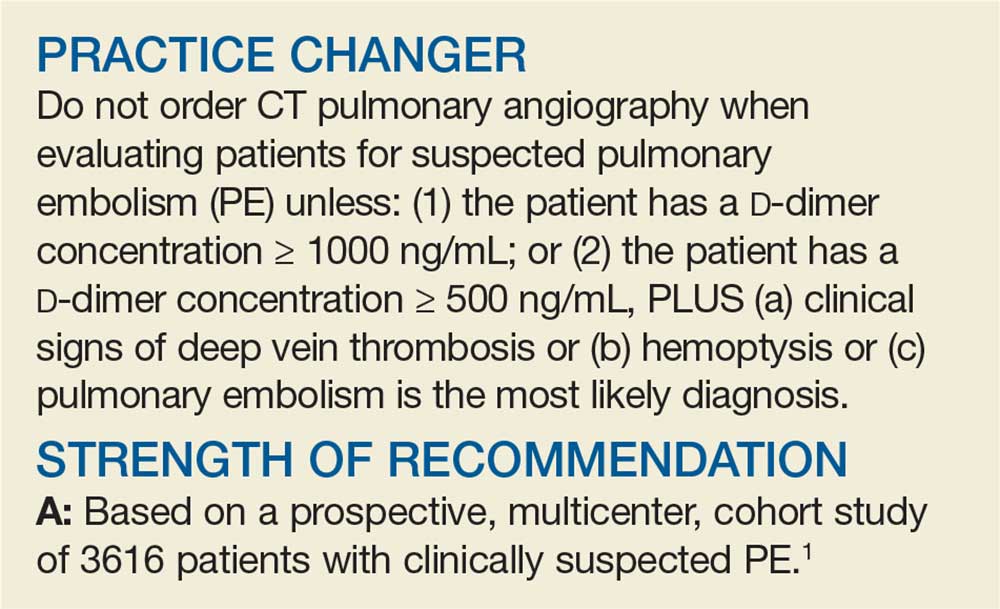
PRACTICE CHANGER
Do not order computed tomography pulmonary angiography when evaluating patients for suspected pulmonary embolism unless: (1) the patient has a
STRENGTH OF RECOMMENDATION
A: Based on a prospective, multicenter, cohort study of 3616 patients with clinically suspected pulmonary embolism.1
van der Hulle T, Cheung WY, Kooij S, et al. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet. 2017;390:289-297.
Best uses of osteopathic manipulation
Interest in osteopathy continues to rise in this country. Currently, more than 20% of medical students in the United States are training to be osteopathic physicians.1 In addition, the 2007 National Health Interview Survey found that spinal manipulation was among the most common complementary and alternative medicine (CAM) therapies used; with 8.6% of US adults reporting that they used it within the previous 12 months.2
With the growing number of DOs and the high utilization of osteopathic manipulative treatment (OMT), it is important for all physicians to understand the role OMT can play in the treatment of conditions ranging from low back pain to irritable bowel syndrome so that patients may be offered, or referred for, the treatment when appropriate.
To clarify when OMT may be most beneficial, we performed a literature review. Our findings are summarized here. But first, a word about osteopathic medicine and what OMT entails.
Osteopathic physicians view the body as a whole
According to the American Osteopathic Association, “the osteopathic philosophy of medicine sees an interrelated unity in all systems of the body, with each working with the other to heal in times of illness."3 This “whole-person approach to medicine” focuses on looking beyond symptoms alone to understand how lifestyle and environmental factors impact well-being.
As part of their education, DOs receive special training in the musculoskeletal system and in OMT. OMT is the process by which DOs use their hands to diagnose illness and injury and then mobilize a patient’s joints and soft tissues using techniques that include muscle activation, stretching, joint articulation, and gentle pressure to encourage the body’s natural tendency to heal itself.
These patients with low back pain will likely benefit
In the past, studies with small sample sizes, blinding issues, differing controls, and subjective outcome measurements have marred research efforts to demonstrate the effectiveness of OMT. More recently, researchers have attempted to minimize these issues, particularly when evaluating the efficacy of OMT for low back pain.
In addition to increasing sample size, studies have compared OMT to usual care, to sham manipulation, and more recently to other manual modalities including ultrasound to equalize the subjective effects of interventions.4 With improved study designs, there has been increased awareness of the effectiveness of spinal manipulation by organizations that develop guidelines for the care of patients with low back pain. The most recent clinical practice guideline from the American College of Physicians includes spinal manipulation as a treatment modality that should be considered by clinicians for patients who have acute, subacute, or chronic low back pain.5
Chronic nonspecific low back pain. Looking at OMT vs other interventions for chronic nonspecific low back pain, a 2014 meta-analysis found moderate quality evidence for clinically relevant effects of OMT on low back pain and function. In 6 studies that evaluated 769 patients with chronic nonspecific low back pain, there was a significant difference in pain—equivalent to a 1.5-point improvement (mean difference [MD]= -14.93; 95% confidence interval [CI], -25.18
Acute and chronic nonspecific low back pain. Similarly, in the same 2014 meta-analysis, 1141 participants with acute and chronic nonspecific low back pain in 10 studies had the equivalent of 1.3 points more pain relief with OMT compared with controls (MD= -12.91; 95% CI, -20.00 to -5.82). The authors used the standardized mean difference (SMD), which is the difference in means divided by the standard deviation, to interpret the magnitude of difference in function between participants who received OMT and those in the control groups. Further, 1046 participants with acute and chronic nonspecific low back pain in 9 studies had a small improvement in functional status using the Roland-Morris Disability Questionnaire (RMDQ) or Oswestry-Disability Index (SMD= -0.36; 95% CI, -0.58 to -0.14).6
A 2005 meta-analysis that evaluated 6 randomized controlled trials (RCTs) involving 549 patients with low back pain found that 318 patients who received OMT had significantly less low back pain compared with 231 controls (effect size= -0.30; 95% CI, -0.47 to -0.13; P=.001).7 Although significant, an effect size of this magnitude is characterized as small.8
Other benefits of OMT include increased patient satisfaction, fewer meds
A randomized double-blind, sham-controlled study involving 455 patients with chronic low back pain compared outcomes of OMT to sham OMT applied in 6 treatment sessions over 8 weeks.9 Intention-to-treat analysis was performed to measure moderate and substantial improvements in low back pain at Week 12 (≥30% and ≥50% pain reductions from baseline, respectively). Based on the Cochrane Back Review Group criteria for effect sizes, response ratios were calculated to determine if the differences seen were considered clinically relevant.10
Patients receiving OMT were more likely to achieve moderate (response ratio=1.38; 95% CI, 1.16-1.64; P<.001) and substantial (response ratio=1.41; 95% CI, 1.13-1.76; P=.002) improvements in low back pain at Week 12. The calculated number needed to treat (NNT) for moderate and significant improvement in pain at 12 weeks was 6 and 7, respectively. In addition, patients in the OMT group were more likely to be very satisfied with their care (P<.001) with an NNT of 5, and used fewer medications than did patients in the sham group during the 12 weeks of the study (use ratio=0.66; 95% CI, 0.43-1.00; P=.048; NNT=15).9
Pregnant women may benefit from OMT in the third trimester
A 2013 RCT involving 144 patients randomized to OMT, sham ultrasound, or usual obstetric care found that 68 patients (47%) experienced back-specific dysfunction during their third trimester of pregnancy (defined by a ≥2-point increase in the RMDQ).11
OMT reduced the risk of back-specific dysfunction by 40% vs the ultrasound group (relative risk [RR]=0.6; 95% CI, 0.3-1; P=.046) and 60% vs the usual obstetric care group (RR=0.4; 95% CI, 0.2-0.7; P<.001). The corresponding NNTs were 5.1 (95% CI, 2.7-282.2) for the OMT group vs the ultrasound group and 2.5 (95% CI, 1.8-4.9) vs the usual care group. The outcomes of this study were not conclusive because the initial RMDQ score was 1.8 points worse for the OMT group than for the usual care group.11
Subsequently, the PROMOTE (Pregnancy Research on Osteopathic Manipulation Optimizing Treatment Effects) study involving 400 patients demonstrated that a standard OMT protocol was effective for decreasing pain and function deterioration compared with usual obstetric care.12 However, results from the OMT group did not differ significantly from those of the ultrasound group, which were labeled as subtherapeutic in the study.12
The most recent Cochrane Review on low back pain in pregnancy noted that there was moderate quality evidence (due to study design limitations or imprecision) that OMT significantly reduced low back pain and function disability.13
OMT for other conditions? The evidence is limited
To date, studies on conditions other than low back pain have not demonstrated the same robust improvements in design as have those concerning low back pain (ie, larger sample sizes, comparisons to usual care and other treatments, etc.), and available data are not sufficiently significant to compel a change in clinical practice. Despite this, patients seek out, and receive, OMT as an alternative or adjunctive treatment for many conditions other than low back pain,2 and family physicians should be aware of the current evidence for OMT in those conditions.
OMT for acute neck pain: A comparison with ketorolac
Researchers randomized 58 patients presenting to 3 emergency departments with neck pain of less than 3 weeks’ duration to receive either OMT or 30 mg IM ketorolac.14 OMT techniques were provided at the discretion of the physician based on patient needs. Patients rated their pain intensity on an 11-point numerical scale at the time of presentation and one hour after treatment. Patients receiving ketorolac or OMT had significant reductions in pain intensity with improvements of 1.7 +/- 1.6 (95% CI, 1.1-2.3; P<.001) and 2.8 +/- 1.7 (95% CI, 2.1-3.4; P<.001), respectively.
Although the pain reduction changes were statistically significant in both groups, the improvements were small enough to question if they were functionally significant. Compared to those receiving ketorolac, those receiving OMT reported a significantly greater decrease in their pain intensity (2.8 vs 1.7; 95% CI, 0.2-1.9; P=.02), but it’s worth noting that the dose of ketorolac was half the recommended dose for moderate or severe pain.14
Patients may have more headache-free days with OMT
To assess the use of OMT to treat chronic migraine, researchers conducted a prospective, single-blind RCT in which 105 chronic migraine sufferers (average of 22.5 migraine days/month) were split into 3 treatment groups: OMT plus medications, sham OMT plus medications, and medications alone.15
OMT led to fewer days with migraines compared with the medication group (MD= -21.06; 95% CI, -23.19 to -18.92; P<.001) and sham OMT group (MD= -17.43; 95% CI, -19.57 to -15.29; P<.001), resulting in less functional disability (P<.001).15 Caution should be taken in interpreting the results of this small trial, however, as an effect of this size has not been replicated in other studies.
A small (N=29) single-blind RCT looked at progressive muscular relaxation with and without OMT for the treatment of tension headache. Patients who completed relaxation exercises plus 3 sessions of OMT experienced significantly more headache-free days (1.79 vs 0.21; P=.016).16 Despite this finding, headache intensity and headache diary ratings were not different between the 2 groups in this study.
Postoperative OMT may decrease length of stay
In a retrospective study evaluating the effect of OMT on postoperative outcomes in 55 patients who underwent gastrointestinal surgery, a total of 17 patients who received a single OMT session within 48 hours of surgery had a mean time to flatus of 3.1 days compared with 4.7 days in the usual care control group (P=.035).17 The mean length of stay was 6.1 days in the OMT group and 11.5 days in the non-OMT group (P=.006).
Major limitations of this study include that it was retrospective in design and that only 17 of 55 patients had OMT performed, indicating a possible selection bias.
Pneumonia: OMT may reduce LOS and duration of antibiotic usage
The Multicenter Osteopathic Pneumonia Study in the Elderly (MOPSE), a double-blind RCT, looked at 406 patients ≥50 years hospitalized with pneumonia. Researchers randomized the group to receive either conventional care (CC; antibiotic treatment only), OMT and antibiotic therapy, or light-touch sham therapy with antibiotics.18 The researchers found no significant differences between the groups for any outcomes in the intention-to-treat analysis.
In results obtained from the per protocol analysis, however, the median length of stay for those in the OMT group was 3.5 days, compared with 4.5 days for those in the CC group (95% CI, 3.2-4.0; P=.01). Multiple comparisons also indicated a reduction in mean duration of intravenous antibiotic use of 3 days in the OMT group (95% CI, 2.7-3.5) vs 3.5 days in the CC group (95% CI, 3.2-3.9). The treatment end-points of either death or respiratory failure occurred significantly less frequently in the OMT group compared with the CC group (P=.006).18
A Cochrane review of RCTs assessing the efficacy of adjunctive techniques compared with conventional therapy for patients with pneumonia revealed a reduction in hospital stay of 2 days (95% CI, -3.5 to -0.6) for patients who received OMT and positive expiratory pressure vs those who received neither intervention.19 Additionally, the duration of IV antibiotics and total duration of all (IV and oral) antibiotic treatment required in those treated adjunctively with OMT was shorter (MD for IV antibiotics= -2.1 days; 95% CI, -3.4 to -0.9 and MD for all antibiotics= -1.9 days; 95% CI, -3.1 to -0.7).19 The review was notable for a small sample size, with only 79 patients assessed.
OMT may improve IBS symptoms
A crossover study of 31 patients that compared visceral manipulation and sacral articulation OMT with sham therapy for the treatment of irritable bowel syndrome (IBS) demonstrated that OMT significantly decreased self-reported diarrhea (P=.016), abdominal distention (P=.043), abdominal pain (P=.013), and rectal sensitivity (P<.001), but did not significantly affect constipation.20
In another study, researchers randomized 30 patients with IBS in a 2:1 distribution to OMT vs sham treatment.21 OMT included abdominal visceral techniques and direct and indirect spine techniques. All of the patients received 2 treatment sessions, and the researchers evaluated them at 7 and 28 days. At 7 days, both groups demonstrated a significant reduction in IBS symptoms, although the OMT group had significantly greater improvement (P=.01). At 28 days, however, neither group showed a significant reduction in symptoms.21
The lack of a control group (in the first study due to the crossover design), small sample sizes, and self-reported symptoms are major limitations to applying these studies to IBS treatment recommendations.
CORRESPONDENCE
Andrew H. Slattengren, DO, Broadway Family Medicine Clinic, 1020 West Broadway Avenue, Minneapolis, MN 55411; aslatten@umn.edu.
1. American Association of Colleges of Osteopathic Medicine. What is osteopathic medicine? Available at: https://www.aacom.org/become-a-doctor/about-om. Accessed July 10, 2017.
2. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-23. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19361005. Accessed November 10, 2015.
3. American Osteopathic Association. What is osteopathic medicine? Available at: http://www.osteopathic.org/osteopathic-health/Pages/what-is-osteopathic-medicine.aspx. Accessed November 17, 2017.
4. Licciardone JC, Russo DP. Blinding Protocols, Treatment Credibility, and Expectancy: Methodologic Issues in Clinical Trials of Osteopathic Manipulative Treatment. J Am Osteopath Assoc. 2006;106:457-463.
5. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166:514-530.
6. Franke H, Franke JD, Fryer G. Osteopathic manipulative treatment for nonspecific low back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2014;15:286.
7. Licciardone JC, Brimhall AK, King LN. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet Disord. 2005;6:43.
8. Cohen J. Statistical Power Analysis for the Behavioral Sciences.82nd ed. Hillsdale NJ: Lawrence Erlbaum Associates; 1988.
9. Licciardone JC, Minotti DE, Gatchel RJ, et al. Osteopathic manual treatment and ultrasound therapy for chronic low back pain: a randomized controlled trial. Ann Fam Med. 2013;11:122-129.
10. Furlan AD, Pennick V, Bombardier C, et al, Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34:1929-1941.
11. Licciardone JC, Aryal S. Prevention of progressive back-specific dysfunction during pregnancy: an assessment of osteopathic manual treatment based on Cochrane Back Review Group criteria. J Am Osteopath Assoc. 2013;113:728-736.
12. Hensel KL, Buchanan S, Brown SK, et al. Pregnancy Research on Osteopathic Manipulation Optimizing Treatment Effects: the PROMOTE study. Am J Obstet Gynecol. 2015;212:108.e1-e9.
13. Pennick V, Liddle SD. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev. 2013;8:CD001139.
14. McReynolds TM, Sheridan BJ. Intramuscular ketorolac versus osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. J Am Osteopath Assoc. 2005;105:57-68.
15. Cerritelli F, Ginevri L, Messi G, et al. Clinical effectiveness of osteopathic treatment in chronic migraine: 3-armed randomized controlled trial. Complement Ther Med. 2015;23:149-156.
16. Anderson RE, Seniscal C. A comparison of selected osteopathic treatment and relaxation for tension-type headaches. Headache. 2006;46:1273-1280.
17. Baltazar GA, Betler MP, Akella K, et al. Effect of osteopathic manipulative treatment on incidence of postoperative ileus and hospital length of stay in general surgical patients. J Am Osteopath Assoc. 2013;113:204-209.
18. Noll DR, Degenhardt BF, Morley TF, et al. Efficacy of osteopathic manipulation as an adjunctive treatment for hospitalized patients with pneumonia: a randomized controlled trial. Osteopath Med Prim Care. 2010;4:2.
19. Yang M, Yan Y, Yin X, et al. Chest physiotherapy for pneumonia in adults. Cochrane Database Syst Rev. 2013;2:CD006338.
20. Attali TV, Bouchoucha M, Benamouzig R. Treatment of refractory irritable bowel syndrome with visceral osteopathy: short-term and long-term results of a randomized trial. J Dig Dis. 2013;14:654-661.
21. Florance BM, Frin G, Dainese R, et al. Osteopathy improves the severity of irritable bowel syndrome: a pilot randomized sham-controlled study. Eur J Gastroenterol Hepatol. 2012;24:944-949.
Interest in osteopathy continues to rise in this country. Currently, more than 20% of medical students in the United States are training to be osteopathic physicians.1 In addition, the 2007 National Health Interview Survey found that spinal manipulation was among the most common complementary and alternative medicine (CAM) therapies used; with 8.6% of US adults reporting that they used it within the previous 12 months.2
With the growing number of DOs and the high utilization of osteopathic manipulative treatment (OMT), it is important for all physicians to understand the role OMT can play in the treatment of conditions ranging from low back pain to irritable bowel syndrome so that patients may be offered, or referred for, the treatment when appropriate.
To clarify when OMT may be most beneficial, we performed a literature review. Our findings are summarized here. But first, a word about osteopathic medicine and what OMT entails.
Osteopathic physicians view the body as a whole
According to the American Osteopathic Association, “the osteopathic philosophy of medicine sees an interrelated unity in all systems of the body, with each working with the other to heal in times of illness."3 This “whole-person approach to medicine” focuses on looking beyond symptoms alone to understand how lifestyle and environmental factors impact well-being.
As part of their education, DOs receive special training in the musculoskeletal system and in OMT. OMT is the process by which DOs use their hands to diagnose illness and injury and then mobilize a patient’s joints and soft tissues using techniques that include muscle activation, stretching, joint articulation, and gentle pressure to encourage the body’s natural tendency to heal itself.
These patients with low back pain will likely benefit
In the past, studies with small sample sizes, blinding issues, differing controls, and subjective outcome measurements have marred research efforts to demonstrate the effectiveness of OMT. More recently, researchers have attempted to minimize these issues, particularly when evaluating the efficacy of OMT for low back pain.
In addition to increasing sample size, studies have compared OMT to usual care, to sham manipulation, and more recently to other manual modalities including ultrasound to equalize the subjective effects of interventions.4 With improved study designs, there has been increased awareness of the effectiveness of spinal manipulation by organizations that develop guidelines for the care of patients with low back pain. The most recent clinical practice guideline from the American College of Physicians includes spinal manipulation as a treatment modality that should be considered by clinicians for patients who have acute, subacute, or chronic low back pain.5
Chronic nonspecific low back pain. Looking at OMT vs other interventions for chronic nonspecific low back pain, a 2014 meta-analysis found moderate quality evidence for clinically relevant effects of OMT on low back pain and function. In 6 studies that evaluated 769 patients with chronic nonspecific low back pain, there was a significant difference in pain—equivalent to a 1.5-point improvement (mean difference [MD]= -14.93; 95% confidence interval [CI], -25.18
Acute and chronic nonspecific low back pain. Similarly, in the same 2014 meta-analysis, 1141 participants with acute and chronic nonspecific low back pain in 10 studies had the equivalent of 1.3 points more pain relief with OMT compared with controls (MD= -12.91; 95% CI, -20.00 to -5.82). The authors used the standardized mean difference (SMD), which is the difference in means divided by the standard deviation, to interpret the magnitude of difference in function between participants who received OMT and those in the control groups. Further, 1046 participants with acute and chronic nonspecific low back pain in 9 studies had a small improvement in functional status using the Roland-Morris Disability Questionnaire (RMDQ) or Oswestry-Disability Index (SMD= -0.36; 95% CI, -0.58 to -0.14).6
A 2005 meta-analysis that evaluated 6 randomized controlled trials (RCTs) involving 549 patients with low back pain found that 318 patients who received OMT had significantly less low back pain compared with 231 controls (effect size= -0.30; 95% CI, -0.47 to -0.13; P=.001).7 Although significant, an effect size of this magnitude is characterized as small.8
Other benefits of OMT include increased patient satisfaction, fewer meds
A randomized double-blind, sham-controlled study involving 455 patients with chronic low back pain compared outcomes of OMT to sham OMT applied in 6 treatment sessions over 8 weeks.9 Intention-to-treat analysis was performed to measure moderate and substantial improvements in low back pain at Week 12 (≥30% and ≥50% pain reductions from baseline, respectively). Based on the Cochrane Back Review Group criteria for effect sizes, response ratios were calculated to determine if the differences seen were considered clinically relevant.10
Patients receiving OMT were more likely to achieve moderate (response ratio=1.38; 95% CI, 1.16-1.64; P<.001) and substantial (response ratio=1.41; 95% CI, 1.13-1.76; P=.002) improvements in low back pain at Week 12. The calculated number needed to treat (NNT) for moderate and significant improvement in pain at 12 weeks was 6 and 7, respectively. In addition, patients in the OMT group were more likely to be very satisfied with their care (P<.001) with an NNT of 5, and used fewer medications than did patients in the sham group during the 12 weeks of the study (use ratio=0.66; 95% CI, 0.43-1.00; P=.048; NNT=15).9
Pregnant women may benefit from OMT in the third trimester
A 2013 RCT involving 144 patients randomized to OMT, sham ultrasound, or usual obstetric care found that 68 patients (47%) experienced back-specific dysfunction during their third trimester of pregnancy (defined by a ≥2-point increase in the RMDQ).11
OMT reduced the risk of back-specific dysfunction by 40% vs the ultrasound group (relative risk [RR]=0.6; 95% CI, 0.3-1; P=.046) and 60% vs the usual obstetric care group (RR=0.4; 95% CI, 0.2-0.7; P<.001). The corresponding NNTs were 5.1 (95% CI, 2.7-282.2) for the OMT group vs the ultrasound group and 2.5 (95% CI, 1.8-4.9) vs the usual care group. The outcomes of this study were not conclusive because the initial RMDQ score was 1.8 points worse for the OMT group than for the usual care group.11
Subsequently, the PROMOTE (Pregnancy Research on Osteopathic Manipulation Optimizing Treatment Effects) study involving 400 patients demonstrated that a standard OMT protocol was effective for decreasing pain and function deterioration compared with usual obstetric care.12 However, results from the OMT group did not differ significantly from those of the ultrasound group, which were labeled as subtherapeutic in the study.12
The most recent Cochrane Review on low back pain in pregnancy noted that there was moderate quality evidence (due to study design limitations or imprecision) that OMT significantly reduced low back pain and function disability.13
OMT for other conditions? The evidence is limited
To date, studies on conditions other than low back pain have not demonstrated the same robust improvements in design as have those concerning low back pain (ie, larger sample sizes, comparisons to usual care and other treatments, etc.), and available data are not sufficiently significant to compel a change in clinical practice. Despite this, patients seek out, and receive, OMT as an alternative or adjunctive treatment for many conditions other than low back pain,2 and family physicians should be aware of the current evidence for OMT in those conditions.
OMT for acute neck pain: A comparison with ketorolac
Researchers randomized 58 patients presenting to 3 emergency departments with neck pain of less than 3 weeks’ duration to receive either OMT or 30 mg IM ketorolac.14 OMT techniques were provided at the discretion of the physician based on patient needs. Patients rated their pain intensity on an 11-point numerical scale at the time of presentation and one hour after treatment. Patients receiving ketorolac or OMT had significant reductions in pain intensity with improvements of 1.7 +/- 1.6 (95% CI, 1.1-2.3; P<.001) and 2.8 +/- 1.7 (95% CI, 2.1-3.4; P<.001), respectively.
Although the pain reduction changes were statistically significant in both groups, the improvements were small enough to question if they were functionally significant. Compared to those receiving ketorolac, those receiving OMT reported a significantly greater decrease in their pain intensity (2.8 vs 1.7; 95% CI, 0.2-1.9; P=.02), but it’s worth noting that the dose of ketorolac was half the recommended dose for moderate or severe pain.14
Patients may have more headache-free days with OMT
To assess the use of OMT to treat chronic migraine, researchers conducted a prospective, single-blind RCT in which 105 chronic migraine sufferers (average of 22.5 migraine days/month) were split into 3 treatment groups: OMT plus medications, sham OMT plus medications, and medications alone.15
OMT led to fewer days with migraines compared with the medication group (MD= -21.06; 95% CI, -23.19 to -18.92; P<.001) and sham OMT group (MD= -17.43; 95% CI, -19.57 to -15.29; P<.001), resulting in less functional disability (P<.001).15 Caution should be taken in interpreting the results of this small trial, however, as an effect of this size has not been replicated in other studies.
A small (N=29) single-blind RCT looked at progressive muscular relaxation with and without OMT for the treatment of tension headache. Patients who completed relaxation exercises plus 3 sessions of OMT experienced significantly more headache-free days (1.79 vs 0.21; P=.016).16 Despite this finding, headache intensity and headache diary ratings were not different between the 2 groups in this study.
Postoperative OMT may decrease length of stay
In a retrospective study evaluating the effect of OMT on postoperative outcomes in 55 patients who underwent gastrointestinal surgery, a total of 17 patients who received a single OMT session within 48 hours of surgery had a mean time to flatus of 3.1 days compared with 4.7 days in the usual care control group (P=.035).17 The mean length of stay was 6.1 days in the OMT group and 11.5 days in the non-OMT group (P=.006).
Major limitations of this study include that it was retrospective in design and that only 17 of 55 patients had OMT performed, indicating a possible selection bias.
Pneumonia: OMT may reduce LOS and duration of antibiotic usage
The Multicenter Osteopathic Pneumonia Study in the Elderly (MOPSE), a double-blind RCT, looked at 406 patients ≥50 years hospitalized with pneumonia. Researchers randomized the group to receive either conventional care (CC; antibiotic treatment only), OMT and antibiotic therapy, or light-touch sham therapy with antibiotics.18 The researchers found no significant differences between the groups for any outcomes in the intention-to-treat analysis.
In results obtained from the per protocol analysis, however, the median length of stay for those in the OMT group was 3.5 days, compared with 4.5 days for those in the CC group (95% CI, 3.2-4.0; P=.01). Multiple comparisons also indicated a reduction in mean duration of intravenous antibiotic use of 3 days in the OMT group (95% CI, 2.7-3.5) vs 3.5 days in the CC group (95% CI, 3.2-3.9). The treatment end-points of either death or respiratory failure occurred significantly less frequently in the OMT group compared with the CC group (P=.006).18
A Cochrane review of RCTs assessing the efficacy of adjunctive techniques compared with conventional therapy for patients with pneumonia revealed a reduction in hospital stay of 2 days (95% CI, -3.5 to -0.6) for patients who received OMT and positive expiratory pressure vs those who received neither intervention.19 Additionally, the duration of IV antibiotics and total duration of all (IV and oral) antibiotic treatment required in those treated adjunctively with OMT was shorter (MD for IV antibiotics= -2.1 days; 95% CI, -3.4 to -0.9 and MD for all antibiotics= -1.9 days; 95% CI, -3.1 to -0.7).19 The review was notable for a small sample size, with only 79 patients assessed.
OMT may improve IBS symptoms
A crossover study of 31 patients that compared visceral manipulation and sacral articulation OMT with sham therapy for the treatment of irritable bowel syndrome (IBS) demonstrated that OMT significantly decreased self-reported diarrhea (P=.016), abdominal distention (P=.043), abdominal pain (P=.013), and rectal sensitivity (P<.001), but did not significantly affect constipation.20
In another study, researchers randomized 30 patients with IBS in a 2:1 distribution to OMT vs sham treatment.21 OMT included abdominal visceral techniques and direct and indirect spine techniques. All of the patients received 2 treatment sessions, and the researchers evaluated them at 7 and 28 days. At 7 days, both groups demonstrated a significant reduction in IBS symptoms, although the OMT group had significantly greater improvement (P=.01). At 28 days, however, neither group showed a significant reduction in symptoms.21
The lack of a control group (in the first study due to the crossover design), small sample sizes, and self-reported symptoms are major limitations to applying these studies to IBS treatment recommendations.
CORRESPONDENCE
Andrew H. Slattengren, DO, Broadway Family Medicine Clinic, 1020 West Broadway Avenue, Minneapolis, MN 55411; aslatten@umn.edu.
Interest in osteopathy continues to rise in this country. Currently, more than 20% of medical students in the United States are training to be osteopathic physicians.1 In addition, the 2007 National Health Interview Survey found that spinal manipulation was among the most common complementary and alternative medicine (CAM) therapies used; with 8.6% of US adults reporting that they used it within the previous 12 months.2
With the growing number of DOs and the high utilization of osteopathic manipulative treatment (OMT), it is important for all physicians to understand the role OMT can play in the treatment of conditions ranging from low back pain to irritable bowel syndrome so that patients may be offered, or referred for, the treatment when appropriate.
To clarify when OMT may be most beneficial, we performed a literature review. Our findings are summarized here. But first, a word about osteopathic medicine and what OMT entails.
Osteopathic physicians view the body as a whole
According to the American Osteopathic Association, “the osteopathic philosophy of medicine sees an interrelated unity in all systems of the body, with each working with the other to heal in times of illness."3 This “whole-person approach to medicine” focuses on looking beyond symptoms alone to understand how lifestyle and environmental factors impact well-being.
As part of their education, DOs receive special training in the musculoskeletal system and in OMT. OMT is the process by which DOs use their hands to diagnose illness and injury and then mobilize a patient’s joints and soft tissues using techniques that include muscle activation, stretching, joint articulation, and gentle pressure to encourage the body’s natural tendency to heal itself.
These patients with low back pain will likely benefit
In the past, studies with small sample sizes, blinding issues, differing controls, and subjective outcome measurements have marred research efforts to demonstrate the effectiveness of OMT. More recently, researchers have attempted to minimize these issues, particularly when evaluating the efficacy of OMT for low back pain.
In addition to increasing sample size, studies have compared OMT to usual care, to sham manipulation, and more recently to other manual modalities including ultrasound to equalize the subjective effects of interventions.4 With improved study designs, there has been increased awareness of the effectiveness of spinal manipulation by organizations that develop guidelines for the care of patients with low back pain. The most recent clinical practice guideline from the American College of Physicians includes spinal manipulation as a treatment modality that should be considered by clinicians for patients who have acute, subacute, or chronic low back pain.5
Chronic nonspecific low back pain. Looking at OMT vs other interventions for chronic nonspecific low back pain, a 2014 meta-analysis found moderate quality evidence for clinically relevant effects of OMT on low back pain and function. In 6 studies that evaluated 769 patients with chronic nonspecific low back pain, there was a significant difference in pain—equivalent to a 1.5-point improvement (mean difference [MD]= -14.93; 95% confidence interval [CI], -25.18
Acute and chronic nonspecific low back pain. Similarly, in the same 2014 meta-analysis, 1141 participants with acute and chronic nonspecific low back pain in 10 studies had the equivalent of 1.3 points more pain relief with OMT compared with controls (MD= -12.91; 95% CI, -20.00 to -5.82). The authors used the standardized mean difference (SMD), which is the difference in means divided by the standard deviation, to interpret the magnitude of difference in function between participants who received OMT and those in the control groups. Further, 1046 participants with acute and chronic nonspecific low back pain in 9 studies had a small improvement in functional status using the Roland-Morris Disability Questionnaire (RMDQ) or Oswestry-Disability Index (SMD= -0.36; 95% CI, -0.58 to -0.14).6
A 2005 meta-analysis that evaluated 6 randomized controlled trials (RCTs) involving 549 patients with low back pain found that 318 patients who received OMT had significantly less low back pain compared with 231 controls (effect size= -0.30; 95% CI, -0.47 to -0.13; P=.001).7 Although significant, an effect size of this magnitude is characterized as small.8
Other benefits of OMT include increased patient satisfaction, fewer meds
A randomized double-blind, sham-controlled study involving 455 patients with chronic low back pain compared outcomes of OMT to sham OMT applied in 6 treatment sessions over 8 weeks.9 Intention-to-treat analysis was performed to measure moderate and substantial improvements in low back pain at Week 12 (≥30% and ≥50% pain reductions from baseline, respectively). Based on the Cochrane Back Review Group criteria for effect sizes, response ratios were calculated to determine if the differences seen were considered clinically relevant.10
Patients receiving OMT were more likely to achieve moderate (response ratio=1.38; 95% CI, 1.16-1.64; P<.001) and substantial (response ratio=1.41; 95% CI, 1.13-1.76; P=.002) improvements in low back pain at Week 12. The calculated number needed to treat (NNT) for moderate and significant improvement in pain at 12 weeks was 6 and 7, respectively. In addition, patients in the OMT group were more likely to be very satisfied with their care (P<.001) with an NNT of 5, and used fewer medications than did patients in the sham group during the 12 weeks of the study (use ratio=0.66; 95% CI, 0.43-1.00; P=.048; NNT=15).9
Pregnant women may benefit from OMT in the third trimester
A 2013 RCT involving 144 patients randomized to OMT, sham ultrasound, or usual obstetric care found that 68 patients (47%) experienced back-specific dysfunction during their third trimester of pregnancy (defined by a ≥2-point increase in the RMDQ).11
OMT reduced the risk of back-specific dysfunction by 40% vs the ultrasound group (relative risk [RR]=0.6; 95% CI, 0.3-1; P=.046) and 60% vs the usual obstetric care group (RR=0.4; 95% CI, 0.2-0.7; P<.001). The corresponding NNTs were 5.1 (95% CI, 2.7-282.2) for the OMT group vs the ultrasound group and 2.5 (95% CI, 1.8-4.9) vs the usual care group. The outcomes of this study were not conclusive because the initial RMDQ score was 1.8 points worse for the OMT group than for the usual care group.11
Subsequently, the PROMOTE (Pregnancy Research on Osteopathic Manipulation Optimizing Treatment Effects) study involving 400 patients demonstrated that a standard OMT protocol was effective for decreasing pain and function deterioration compared with usual obstetric care.12 However, results from the OMT group did not differ significantly from those of the ultrasound group, which were labeled as subtherapeutic in the study.12
The most recent Cochrane Review on low back pain in pregnancy noted that there was moderate quality evidence (due to study design limitations or imprecision) that OMT significantly reduced low back pain and function disability.13
OMT for other conditions? The evidence is limited
To date, studies on conditions other than low back pain have not demonstrated the same robust improvements in design as have those concerning low back pain (ie, larger sample sizes, comparisons to usual care and other treatments, etc.), and available data are not sufficiently significant to compel a change in clinical practice. Despite this, patients seek out, and receive, OMT as an alternative or adjunctive treatment for many conditions other than low back pain,2 and family physicians should be aware of the current evidence for OMT in those conditions.
OMT for acute neck pain: A comparison with ketorolac
Researchers randomized 58 patients presenting to 3 emergency departments with neck pain of less than 3 weeks’ duration to receive either OMT or 30 mg IM ketorolac.14 OMT techniques were provided at the discretion of the physician based on patient needs. Patients rated their pain intensity on an 11-point numerical scale at the time of presentation and one hour after treatment. Patients receiving ketorolac or OMT had significant reductions in pain intensity with improvements of 1.7 +/- 1.6 (95% CI, 1.1-2.3; P<.001) and 2.8 +/- 1.7 (95% CI, 2.1-3.4; P<.001), respectively.
Although the pain reduction changes were statistically significant in both groups, the improvements were small enough to question if they were functionally significant. Compared to those receiving ketorolac, those receiving OMT reported a significantly greater decrease in their pain intensity (2.8 vs 1.7; 95% CI, 0.2-1.9; P=.02), but it’s worth noting that the dose of ketorolac was half the recommended dose for moderate or severe pain.14
Patients may have more headache-free days with OMT
To assess the use of OMT to treat chronic migraine, researchers conducted a prospective, single-blind RCT in which 105 chronic migraine sufferers (average of 22.5 migraine days/month) were split into 3 treatment groups: OMT plus medications, sham OMT plus medications, and medications alone.15
OMT led to fewer days with migraines compared with the medication group (MD= -21.06; 95% CI, -23.19 to -18.92; P<.001) and sham OMT group (MD= -17.43; 95% CI, -19.57 to -15.29; P<.001), resulting in less functional disability (P<.001).15 Caution should be taken in interpreting the results of this small trial, however, as an effect of this size has not been replicated in other studies.
A small (N=29) single-blind RCT looked at progressive muscular relaxation with and without OMT for the treatment of tension headache. Patients who completed relaxation exercises plus 3 sessions of OMT experienced significantly more headache-free days (1.79 vs 0.21; P=.016).16 Despite this finding, headache intensity and headache diary ratings were not different between the 2 groups in this study.
Postoperative OMT may decrease length of stay
In a retrospective study evaluating the effect of OMT on postoperative outcomes in 55 patients who underwent gastrointestinal surgery, a total of 17 patients who received a single OMT session within 48 hours of surgery had a mean time to flatus of 3.1 days compared with 4.7 days in the usual care control group (P=.035).17 The mean length of stay was 6.1 days in the OMT group and 11.5 days in the non-OMT group (P=.006).
Major limitations of this study include that it was retrospective in design and that only 17 of 55 patients had OMT performed, indicating a possible selection bias.
Pneumonia: OMT may reduce LOS and duration of antibiotic usage
The Multicenter Osteopathic Pneumonia Study in the Elderly (MOPSE), a double-blind RCT, looked at 406 patients ≥50 years hospitalized with pneumonia. Researchers randomized the group to receive either conventional care (CC; antibiotic treatment only), OMT and antibiotic therapy, or light-touch sham therapy with antibiotics.18 The researchers found no significant differences between the groups for any outcomes in the intention-to-treat analysis.
In results obtained from the per protocol analysis, however, the median length of stay for those in the OMT group was 3.5 days, compared with 4.5 days for those in the CC group (95% CI, 3.2-4.0; P=.01). Multiple comparisons also indicated a reduction in mean duration of intravenous antibiotic use of 3 days in the OMT group (95% CI, 2.7-3.5) vs 3.5 days in the CC group (95% CI, 3.2-3.9). The treatment end-points of either death or respiratory failure occurred significantly less frequently in the OMT group compared with the CC group (P=.006).18
A Cochrane review of RCTs assessing the efficacy of adjunctive techniques compared with conventional therapy for patients with pneumonia revealed a reduction in hospital stay of 2 days (95% CI, -3.5 to -0.6) for patients who received OMT and positive expiratory pressure vs those who received neither intervention.19 Additionally, the duration of IV antibiotics and total duration of all (IV and oral) antibiotic treatment required in those treated adjunctively with OMT was shorter (MD for IV antibiotics= -2.1 days; 95% CI, -3.4 to -0.9 and MD for all antibiotics= -1.9 days; 95% CI, -3.1 to -0.7).19 The review was notable for a small sample size, with only 79 patients assessed.
OMT may improve IBS symptoms
A crossover study of 31 patients that compared visceral manipulation and sacral articulation OMT with sham therapy for the treatment of irritable bowel syndrome (IBS) demonstrated that OMT significantly decreased self-reported diarrhea (P=.016), abdominal distention (P=.043), abdominal pain (P=.013), and rectal sensitivity (P<.001), but did not significantly affect constipation.20
In another study, researchers randomized 30 patients with IBS in a 2:1 distribution to OMT vs sham treatment.21 OMT included abdominal visceral techniques and direct and indirect spine techniques. All of the patients received 2 treatment sessions, and the researchers evaluated them at 7 and 28 days. At 7 days, both groups demonstrated a significant reduction in IBS symptoms, although the OMT group had significantly greater improvement (P=.01). At 28 days, however, neither group showed a significant reduction in symptoms.21
The lack of a control group (in the first study due to the crossover design), small sample sizes, and self-reported symptoms are major limitations to applying these studies to IBS treatment recommendations.
CORRESPONDENCE
Andrew H. Slattengren, DO, Broadway Family Medicine Clinic, 1020 West Broadway Avenue, Minneapolis, MN 55411; aslatten@umn.edu.
1. American Association of Colleges of Osteopathic Medicine. What is osteopathic medicine? Available at: https://www.aacom.org/become-a-doctor/about-om. Accessed July 10, 2017.
2. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-23. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19361005. Accessed November 10, 2015.
3. American Osteopathic Association. What is osteopathic medicine? Available at: http://www.osteopathic.org/osteopathic-health/Pages/what-is-osteopathic-medicine.aspx. Accessed November 17, 2017.
4. Licciardone JC, Russo DP. Blinding Protocols, Treatment Credibility, and Expectancy: Methodologic Issues in Clinical Trials of Osteopathic Manipulative Treatment. J Am Osteopath Assoc. 2006;106:457-463.
5. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166:514-530.
6. Franke H, Franke JD, Fryer G. Osteopathic manipulative treatment for nonspecific low back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2014;15:286.
7. Licciardone JC, Brimhall AK, King LN. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet Disord. 2005;6:43.
8. Cohen J. Statistical Power Analysis for the Behavioral Sciences.82nd ed. Hillsdale NJ: Lawrence Erlbaum Associates; 1988.
9. Licciardone JC, Minotti DE, Gatchel RJ, et al. Osteopathic manual treatment and ultrasound therapy for chronic low back pain: a randomized controlled trial. Ann Fam Med. 2013;11:122-129.
10. Furlan AD, Pennick V, Bombardier C, et al, Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34:1929-1941.
11. Licciardone JC, Aryal S. Prevention of progressive back-specific dysfunction during pregnancy: an assessment of osteopathic manual treatment based on Cochrane Back Review Group criteria. J Am Osteopath Assoc. 2013;113:728-736.
12. Hensel KL, Buchanan S, Brown SK, et al. Pregnancy Research on Osteopathic Manipulation Optimizing Treatment Effects: the PROMOTE study. Am J Obstet Gynecol. 2015;212:108.e1-e9.
13. Pennick V, Liddle SD. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev. 2013;8:CD001139.
14. McReynolds TM, Sheridan BJ. Intramuscular ketorolac versus osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. J Am Osteopath Assoc. 2005;105:57-68.
15. Cerritelli F, Ginevri L, Messi G, et al. Clinical effectiveness of osteopathic treatment in chronic migraine: 3-armed randomized controlled trial. Complement Ther Med. 2015;23:149-156.
16. Anderson RE, Seniscal C. A comparison of selected osteopathic treatment and relaxation for tension-type headaches. Headache. 2006;46:1273-1280.
17. Baltazar GA, Betler MP, Akella K, et al. Effect of osteopathic manipulative treatment on incidence of postoperative ileus and hospital length of stay in general surgical patients. J Am Osteopath Assoc. 2013;113:204-209.
18. Noll DR, Degenhardt BF, Morley TF, et al. Efficacy of osteopathic manipulation as an adjunctive treatment for hospitalized patients with pneumonia: a randomized controlled trial. Osteopath Med Prim Care. 2010;4:2.
19. Yang M, Yan Y, Yin X, et al. Chest physiotherapy for pneumonia in adults. Cochrane Database Syst Rev. 2013;2:CD006338.
20. Attali TV, Bouchoucha M, Benamouzig R. Treatment of refractory irritable bowel syndrome with visceral osteopathy: short-term and long-term results of a randomized trial. J Dig Dis. 2013;14:654-661.
21. Florance BM, Frin G, Dainese R, et al. Osteopathy improves the severity of irritable bowel syndrome: a pilot randomized sham-controlled study. Eur J Gastroenterol Hepatol. 2012;24:944-949.
1. American Association of Colleges of Osteopathic Medicine. What is osteopathic medicine? Available at: https://www.aacom.org/become-a-doctor/about-om. Accessed July 10, 2017.
2. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-23. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19361005. Accessed November 10, 2015.
3. American Osteopathic Association. What is osteopathic medicine? Available at: http://www.osteopathic.org/osteopathic-health/Pages/what-is-osteopathic-medicine.aspx. Accessed November 17, 2017.
4. Licciardone JC, Russo DP. Blinding Protocols, Treatment Credibility, and Expectancy: Methodologic Issues in Clinical Trials of Osteopathic Manipulative Treatment. J Am Osteopath Assoc. 2006;106:457-463.
5. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166:514-530.
6. Franke H, Franke JD, Fryer G. Osteopathic manipulative treatment for nonspecific low back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2014;15:286.
7. Licciardone JC, Brimhall AK, King LN. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet Disord. 2005;6:43.
8. Cohen J. Statistical Power Analysis for the Behavioral Sciences.82nd ed. Hillsdale NJ: Lawrence Erlbaum Associates; 1988.
9. Licciardone JC, Minotti DE, Gatchel RJ, et al. Osteopathic manual treatment and ultrasound therapy for chronic low back pain: a randomized controlled trial. Ann Fam Med. 2013;11:122-129.
10. Furlan AD, Pennick V, Bombardier C, et al, Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34:1929-1941.
11. Licciardone JC, Aryal S. Prevention of progressive back-specific dysfunction during pregnancy: an assessment of osteopathic manual treatment based on Cochrane Back Review Group criteria. J Am Osteopath Assoc. 2013;113:728-736.
12. Hensel KL, Buchanan S, Brown SK, et al. Pregnancy Research on Osteopathic Manipulation Optimizing Treatment Effects: the PROMOTE study. Am J Obstet Gynecol. 2015;212:108.e1-e9.
13. Pennick V, Liddle SD. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev. 2013;8:CD001139.
14. McReynolds TM, Sheridan BJ. Intramuscular ketorolac versus osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. J Am Osteopath Assoc. 2005;105:57-68.
15. Cerritelli F, Ginevri L, Messi G, et al. Clinical effectiveness of osteopathic treatment in chronic migraine: 3-armed randomized controlled trial. Complement Ther Med. 2015;23:149-156.
16. Anderson RE, Seniscal C. A comparison of selected osteopathic treatment and relaxation for tension-type headaches. Headache. 2006;46:1273-1280.
17. Baltazar GA, Betler MP, Akella K, et al. Effect of osteopathic manipulative treatment on incidence of postoperative ileus and hospital length of stay in general surgical patients. J Am Osteopath Assoc. 2013;113:204-209.
18. Noll DR, Degenhardt BF, Morley TF, et al. Efficacy of osteopathic manipulation as an adjunctive treatment for hospitalized patients with pneumonia: a randomized controlled trial. Osteopath Med Prim Care. 2010;4:2.
19. Yang M, Yan Y, Yin X, et al. Chest physiotherapy for pneumonia in adults. Cochrane Database Syst Rev. 2013;2:CD006338.
20. Attali TV, Bouchoucha M, Benamouzig R. Treatment of refractory irritable bowel syndrome with visceral osteopathy: short-term and long-term results of a randomized trial. J Dig Dis. 2013;14:654-661.
21. Florance BM, Frin G, Dainese R, et al. Osteopathy improves the severity of irritable bowel syndrome: a pilot randomized sham-controlled study. Eur J Gastroenterol Hepatol. 2012;24:944-949.
PRACTICE RECOMMENDATIONS
› Recommend osteopathic manipulative treatment to your patients with low back pain, as those who receive OMT have decreased pain, improved function, and use less medication. B
› Consider OMT as an adjunctive modality to decrease back-specific dysfunction in the third trimester of pregnancy. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Kidney Stones? It’s Time to Rethink Those Meds
PRACTICE CHANGER
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones that are ≤ 10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial (RCT).1
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. CT of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤ 10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications.
Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple RCTs suggest that an α-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk for bias.
Continue for the study summary >>
STUDY SUMMARY
MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 with a single ureteric stone measuring ≤ 10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones > 10 mm typically require surgery or lithotripsy.)
In this RCT, 1,167 adults were randomized to take tamsulosin (0.4 mg/d), nifedipine (30 mg/d), or placebo for four weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At four weeks, 1,136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤ 5 mm vs > 5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21% of) participants. The mean days to stone passage was 15.9 (n = 84) for placebo, 16.5 (n = 79) for tamsulosin, and 16.2 (n = 74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, –2.9 to 3.9; P = .78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first four weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, –1.6 to 2.8; P = .45).
There was no difference between groups in the VAS pain score at four weeks. The MET vs placebo difference was 0.0 (95% CI, –0.4 to 0.4; P = .96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT’S NEW
This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, well-designed, multicenter RCT.9
Continue for caveats >>
CAVEATS
This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
References
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr, Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CW, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013; 189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40: 280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2016. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2016;65(2):118-120.
PRACTICE CHANGER
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones that are ≤ 10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial (RCT).1
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. CT of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤ 10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications.
Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple RCTs suggest that an α-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk for bias.
Continue for the study summary >>
STUDY SUMMARY
MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 with a single ureteric stone measuring ≤ 10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones > 10 mm typically require surgery or lithotripsy.)
In this RCT, 1,167 adults were randomized to take tamsulosin (0.4 mg/d), nifedipine (30 mg/d), or placebo for four weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At four weeks, 1,136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤ 5 mm vs > 5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21% of) participants. The mean days to stone passage was 15.9 (n = 84) for placebo, 16.5 (n = 79) for tamsulosin, and 16.2 (n = 74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, –2.9 to 3.9; P = .78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first four weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, –1.6 to 2.8; P = .45).
There was no difference between groups in the VAS pain score at four weeks. The MET vs placebo difference was 0.0 (95% CI, –0.4 to 0.4; P = .96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT’S NEW
This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, well-designed, multicenter RCT.9
Continue for caveats >>
CAVEATS
This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
References
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr, Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CW, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013; 189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40: 280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2016. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2016;65(2):118-120.
PRACTICE CHANGER
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones that are ≤ 10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial (RCT).1
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. CT of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤ 10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications.
Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple RCTs suggest that an α-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk for bias.
Continue for the study summary >>
STUDY SUMMARY
MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 with a single ureteric stone measuring ≤ 10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones > 10 mm typically require surgery or lithotripsy.)
In this RCT, 1,167 adults were randomized to take tamsulosin (0.4 mg/d), nifedipine (30 mg/d), or placebo for four weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At four weeks, 1,136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤ 5 mm vs > 5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21% of) participants. The mean days to stone passage was 15.9 (n = 84) for placebo, 16.5 (n = 79) for tamsulosin, and 16.2 (n = 74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, –2.9 to 3.9; P = .78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first four weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, –1.6 to 2.8; P = .45).
There was no difference between groups in the VAS pain score at four weeks. The MET vs placebo difference was 0.0 (95% CI, –0.4 to 0.4; P = .96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT’S NEW
This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, well-designed, multicenter RCT.9
Continue for caveats >>
CAVEATS
This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
References
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr, Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CW, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013; 189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40: 280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2016. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2016;65(2):118-120.
Kidney stones? It’s time to rethink those meds
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones ≤10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial.
Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
Illustrative case
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. A computed tomography scan of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications. Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple randomized controlled trials (RCTs) suggest that an alpha-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk of bias.
STUDY SUMMARY: MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 years with a single ureteric stone measuring ≤10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones >10 mm typically require surgery or lithotripsy.)
In this RCT, 1167 adults were randomized to take tamsulosin 0.4 mg/d, nifedipine 30 mg/d, or placebo for 4 weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At 4 weeks, 1136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤5 mm vs >5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21%) of participants. The mean days to stone passage was 15.9 (n=84) for placebo, 16.5 (n=79) for tamsulosin and 16.2 (n=74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, -2.9 to 3.9; P=.78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first 4 weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, -1.6 to 2.8; P=.45).
There was no difference between groups in the VAS pain score at 4 weeks. The MET vs placebo difference was 0.0 (95% CI, -0.4 to 0.4; P=.96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT'S NEW: This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, multicenter, well-designed RCT.9
CAVEATS: This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr., Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CU, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013;189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40:280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones ≤10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial.
Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
Illustrative case
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. A computed tomography scan of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications. Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple randomized controlled trials (RCTs) suggest that an alpha-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk of bias.
STUDY SUMMARY: MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 years with a single ureteric stone measuring ≤10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones >10 mm typically require surgery or lithotripsy.)
In this RCT, 1167 adults were randomized to take tamsulosin 0.4 mg/d, nifedipine 30 mg/d, or placebo for 4 weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At 4 weeks, 1136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤5 mm vs >5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21%) of participants. The mean days to stone passage was 15.9 (n=84) for placebo, 16.5 (n=79) for tamsulosin and 16.2 (n=74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, -2.9 to 3.9; P=.78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first 4 weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, -1.6 to 2.8; P=.45).
There was no difference between groups in the VAS pain score at 4 weeks. The MET vs placebo difference was 0.0 (95% CI, -0.4 to 0.4; P=.96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT'S NEW: This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, multicenter, well-designed RCT.9
CAVEATS: This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones ≤10 mm.1
Strength of recommendation
A: Based on a high-quality randomized controlled trial.
Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
Illustrative case
Bob Z, age 48, presents to the emergency department (ED) with unspecified groin pain. A computed tomography scan of the kidney, ureter, and bladder (CT KUB) finds evidence of a single ureteral stone measuring 8 mm. He’s prescribed medication for the pain and discharged. The day after his ED visit, he comes to your office to discuss further treatment options. Should you prescribe tamsulosin or nifedipine to help him pass the stone?
The most recent National Health and Nutrition Examination Survey found kidney stones affect 8.8% of the population.2 Outpatient therapy is indicated for patients with ureteric colic secondary to stones ≤10 mm who do not have uncontrolled pain, impaired kidney function, or severe infection. Routine outpatient care includes oral hydration, antiemetics, and pain medications. Medical expulsive therapy (MET) is also used to facilitate stone passage. MET is increasingly becoming part of routine care; use of MET in kidney stone patients in the United States has grown from 14% in 2009 to 64% in 2012.3,4
The joint European Association of Urology/American Urological Association Nephrolithiasis Guideline Panel supports the use of MET.5 Meta-analyses of multiple randomized controlled trials (RCTs) suggest that an alpha-blocker (tamsulosin) or a calcium channel blocker (nifedipine) can reduce pain and lead to quicker stone passage and a higher rate of eventual stone passage when compared to placebo or observation.6,7 However, these reviews included small, heterogeneous studies with a high or unclear risk of bias.
STUDY SUMMARY: MET doesn’t increase the rate of stone passage
The SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial1 was a multicenter RCT designed to determine the effectiveness of tamsulosin or nifedipine as MET for patients ages 18 to 65 years with a single ureteric stone measuring ≤10 mm on CT KUB, which has 98% diagnostic accuracy.8 (Stones >10 mm typically require surgery or lithotripsy.)
In this RCT, 1167 adults were randomized to take tamsulosin 0.4 mg/d, nifedipine 30 mg/d, or placebo for 4 weeks or until the stone spontaneously passed, whichever came first. The participants, clinicians, and research staff were blinded to treatment assignment. The primary outcome was the proportion of participants who spontaneously passed their stone, as indicated in patient self-reported questionnaires and case-report forms completed by researchers. Secondary outcomes were time to stone passage and pain as assessed by analgesic use and a visual analogue scale (VAS).
At 4 weeks, 1136 (97%) of the randomized participants had data available for analysis. The proportion of participants who passed their stone did not differ between MET and placebo; 80% of the placebo group (303 of 379 participants) passed the stone, compared with 81% (307 of 378) of the tamsulosin group and 80% (304 of 379) of the nifedipine group. The odds ratio (OR) for MET vs placebo was 1.04 (95% confidence interval [CI], 0.77 to 1.43) and the OR for tamsulosin vs nifedipine was 1.07 (95% CI, 0.74 to 1.53). These findings did not change with further subgroup analysis, including by sex, stone size (≤5 mm vs >5 mm), or stone location.
There were no differences between groups in time to stone passage as measured by clinical report and confirmed by imaging. Time to passage of stone was available for 237 (21%) of participants. The mean days to stone passage was 15.9 (n=84) for placebo, 16.5 (n=79) for tamsulosin and 16.2 (n=74) for nifedipine, with a MET vs placebo difference of 0.5 days (95% CI, -2.9 to 3.9; P=.78). Sensitivity analysis accounting for bias from missing data did not change this outcome.
No differences in analgesic use or pain. Self-reported use of pain medication during the first 4 weeks was similar between groups: 59% (placebo patients), 56% (tamsulosin), and 56% (nifedipine). The mean days of pain medication use was 10.5 for placebo, 11.6 for tamsulosin, and 10.7 for nifedipine, with a MET vs placebo difference of 0.6 days (95% CI, -1.6 to 2.8; P=.45).
There was no difference between groups in the VAS pain score at 4 weeks. The MET vs placebo difference was 0.0 (95% CI, -0.4 to 0.4; P=.96) and the mean VAS pain score was 1.2 for placebo, 1.0 for tamsulosin, and 1.3 for nifedipine.
WHAT'S NEW: This large RCT contradicts results from previous meta-analyses
The SUSPEND study is the first large, multicenter RCT of MET with tamsulosin or nifedipine for kidney stones that used patient-oriented outcomes to find no benefit for stone expulsion, analgesic use, or reported pain compared to placebo. The discrepancy with prior meta-analyses is not unusual. Up to one-third of meta-analyses that show positive outcomes of a therapy are subsequently altered by the inclusion of results from a single, large, multicenter, well-designed RCT.9
CAVEATS: This trial included fewer women than previous studies
The SUSPEND study included a smaller proportion of women than previously published case series due to a need for a diagnostic CT KUB, which excluded more women than men due to radiation concerns. However, the proportion of women was balanced across all groups in this trial, and there was no evidence that sex impacted the efficacy of treatment for the primary outcome.1
CHALLENGES TO IMPLEMENTATION
We see no challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr., Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CU, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013;189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40:280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
1. Pickard R, Starr K, MacLennan G, et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet. 2015;386:341-349.
2. Scales CD Jr., Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160-165.
3. Fwu CU, Eggers PW, Kimmel PL, et al. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;89:479-486.
4. Bagga H, Appa A, Wang R, et al. 2257 medical expulsion therapy is underutilized in women presenting to an emergency department with acute urinary stone disease. J Urol. 2013;189:e925-e926.
5. Preminger GM, Tiselius HG, Assimos DG, et al; American Urological Association Education and Research, Inc; European Association of Urology. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610-1631.
6. Campschroer T, Zhu Y, Duijvesz D, et al. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2014;4:CD008509.
7. Seitz C, Liatsikos E, Porpiglia F, et al. Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol. 2009;56:455-471.
8. Worster A, Preyra I, Weaver B, et al. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann Emerg Med. 2002;40:280-286.
9. LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536-542.
Copyright © 2016. The Family Physicians Inquiries Network. All rights reserved.
Prolotherapy: A nontraditional approach to knee osteoarthritis
Recommend prolotherapy for patients with knee osteoarthritis (OA) that does not respond to conventional therapies.1
Strength of recommendation
B: Based on a 3-arm, blinded, randomized controlled trial (RCT).
Rabago D, Patterson JJ, Mundt M, et al. Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial. Ann Fam Med. 2013;11:229-237.
Illustrative case
A 59-year-old woman with OA comes to your office with chronic knee pain. She has tried acetaminophen, ibuprofen, intra-articular corticosteroid injections, and physical therapy without significant improvement in pain or functioning. She wants to avoid daily medications or surgery and wonders if there are any interventions that will not lead to prolonged time away from work. What would you consider?
Additional options needed for knee OA
More than 25% of adults ages 55 years and older suffer from knee pain, and OA is an increasingly common cause.2 Knee pain is a major source of morbidity in the United States; it limits patients’ activities and increases comorbidities such as depression and obesity.
Conventional outpatient treatments for knee pain range from acetaminophen, nonsteroidal anti-inflammatory drugs, glucosamine, chondroitin, and opiates to topical capsaicin therapy, intra-articular hyaluronic acid, and corticosteroid injections. Cost, efficacy, and safety limit these therapies.3
Prolotherapy is another option used to treat musculoskeletal pain. It involves repeatedly injecting a sclerosing solution (usually dextrose) into the sites of chronic musculoskeletal pain.4 The mechanism of action is thought to be the result of local tissue irritation stimulating inflammatory pathways, which leads to the release of growth factors and subsequent healing.4,5 Previous studies evaluating the usefulness of prolotherapy have lacked methodological rigor, have not been randomized adequately, or have lacked a placebo comparison.6-9
STUDY SUMMARY: Prolotherapy reduces pain more than exercise or placebo
Rabago et al1 randomized 90 participants to dextrose prolotherapy, placebo saline injections, or at-home exercise. Participants had a ≥3 month history of painful knee OA based on a self-reported pain scale, radiographic evidence of knee OA within the past 5 years, and tenderness of ≥1 or more anterior knee structures on exam.
Sixty-six percent of participants were female. The mean age was 56.7 years and 74% were overweight (body mass index [BMI], 25-29.9) or obese (BMI ≥30). Participants chose to have one or both knees treated; 43 knees were injected in the dextrose group, 41 received saline injections, and 47 were assessed in the exercise group. There were no significant differences among groups at baseline.
Participants in the prolotherapy and saline groups received injections at 1, 5, and 9 weeks, plus optional injections at 13 and 17 weeks per physician and participant preference. Injections were administered both extra- and intra-articularly. Intra-articular injections were delivered using a 25-gauge needle with a mixture of 25% dextrose, 1% saline, and 1% lidocaine for a total volume of 6 mL. Extra-articular injections were delivered with a peppering technique with a maximum of 15 punctures over painful ligaments and tendons around the knee. The extra-articular solution was similar to the intra-articular except 15% dextrose was used, with a total maximum volume of 22.5 mL.
The placebo injection group received injections in the same pattern and technique, but the solution was the same quantity of 1% lidocaine plus 1% saline to achieve the same volume. The injector, outcome assessor, primary investigator, and participants were blinded to injection group.
In the exercise group, a study coordinator taught participants knee exercises and gave them a pamphlet with 10 exercises to perform at home. Adherence to at-home exercises was assessed with monthly logs that participants mailed in for the first 20 weeks of the study. Seventy-seven percent of participants reported doing their at-home exercises.
The primary outcome measure was change in composite score on the Western Ontario McMaster Universities Osteoarthritis Index (WOMAC), a validated questionnaire used to evaluate knee-related quality of life that features subscales for pain, stiffness, and function.10 The minimal clinically important difference in change in score on this 100-point instrument is 12 points; higher scores indicate better quality of life.11 The secondary outcome was change in score on the Knee Pain Scale (KPS), a validated questionnaire that uses a 4-point scale to measure pain frequency and a 5-point scale to measure pain severity; higher scores indicate worse symptoms.12
Improvements seen in both scores
Using an intention-to-treat analysis for all groups, WOMAC composite scores improved at 9 weeks and remained improved through 52 weeks. At 9 weeks, the dextrose group increased 13.91 points, compared with 6.75 (P=.020) in the saline group and 2.51 (P=.001) points in the exercise group.
At 52 weeks, the dextrose group showed an improvement of 15.32 points compared with 7.59 (P=.022) in the saline group and 8.24 (P=.034) in the exercise group. Fifty percent (15/30) of participants in the dextrose group had clinically meaningful improvement as measured by an increase of ≥12 points on the WOMAC, compared with 34% (10/29) and 26% (8/31) in the saline and exercise groups, respectively. At 52 weeks, the dextrose group had significantly decreased KPS knee pain frequency scores compared with the saline group (mean difference [MD], -1.20 vs. -0.60; P<.05) and exercise group (MD, -1.20 vs. -0.40; P<.05). Knee pain severity scores also decreased in the dextrose group compared to the saline (MD, -0.92 vs. -0.32, P<.05) and exercise groups (MD, -0.92 vs. -0.11; P<.05). There were no significant differences in KPS score decreases between the saline and exercise groups.
What about patient satisfaction?
At week 52, all participants were asked, “Would you recommend the therapy you received in this study to others with knee OA like yours?” Ninety-one percent of the dextrose group, 82% of the saline group, and 89% of the exercise group answered “Yes.”
All participants who received injections reported mild to moderate post-injection pain. Five participants in the saline group and 3 in the dextrose group experienced bruising. No other side effects or adverse events were documented. According to daily logs of medication use in the 7 days after injection, 74% of patients in the dextrose group used acetaminophen and 47% used oxycodone, compared with 63% and 43%, respectively, in the saline group. The study authors did not comment on the significance of these differences.
WHAT'S NEW: A randomized study provides support for prolotherapy
This study is the first to adequately demonstrate improvement in knee-related quality of life with prolotherapy compared with placebo (saline) or exercise. Family physicians can now add this therapy to their “toolbox” for patient complaints of OA pain.
CAVEATS: Efficacy is unknown in patients with certain comorbidities
Efficacy is unknown in patients with certain comorbidities Of 894 people screened, only 118 met initial eligibility criteria. This study did not include patients who were taking daily opioids, had diabetes, or had a BMI >40, so its results may not be generalizable to such patients.
Also, while the study demonstrated no side effects or adverse events other than bruising in 8 patients, the sample size may have been too small to detect less common adverse events. However, prior studies of prolotherapy have not revealed any substantial adverse effects.7
Strong evidence for some conditions… not for others. The strongest data support the efficacy of prolotherapy for focal tendinopathy (lateral epicondylosis) and knee OA. Evidence supporting prolotherapy for multimodal conditions, such as chronic low back pain, is less robust.4
CHALLENGES TO IMPLEMENTATION: Finding a prolotherapist near you may not be easy
The main challenge to implementation is finding a certified prolotherapist, or obtaining training in the technique. The prolotherapy knee protocol can be performed in an outpatient setting in less than 15 minutes, but the technique requires training. Prolotherapy training is available from multiple organizations, including the American Association of Orthopaedic Medicine, which requires 100 course hours for prolotherapy certification.4 No formal survey on the number of prolotherapists in the United States has been conducted since 1993,13 but Rabago et al1 estimated that the number is in the hundreds.
Insurance coverage frequently is a challenge. Most third-party payers do not cover prolotherapy, and currently most patients pay out-of-pocket. Rabago et al1 indicated that at their institution, the cost is $218 per injection session. Another study published in 2010 put the average total cost of 4 to 6 prolotherapy sessions at $1800.14
And from the patient’s perspective … The multiple needle sticks involved in prolotherapy can be painful.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center of Research Resources or the National Institutes of Health.
1. Rabago D, Patterson JJ, Mundt M, et al. Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial. Ann Fam Med. 2013;11:229-237.
2. Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91-97.
3. Lawrence RC, Felson DT, Helmick CG, et al; National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26-35.
4. Rabago D, Slattengren A, Zgierska A. Prolotherapy in primary care practice. Prim Care. 2010;37:65-80.
5. Hackett GS, Hemwall GA, Montgomery GA. Ligament and Tendon Relaxation Treated by Prolotherapy. 5th ed. Oak Park, IL: Institute in Basic Life Principles; 1991.
6. Schultz LW. A treatment for subluxation of the temporomandibular joint. JAMA. 1937;109:1032-1035.
7. Rabago D, Best TM, Beamsley M, et al. A systematic review of prolotherapy for chronic musculoskeletal pain. Clin J Sport Med. 2005;15:376-380.
8. Reeves KD, Hassanein KM. Long-term effects of dextrose prolotherapy for anterior cruciate ligament laxity. Altern Ther Health Med. 2003;9:58-62.
9. Reeves KD, Hassanein K. Randomized prospective double-blind placebo-controlled study of dextrose prolotherapy for knee osteoarthritis with or without ACL laxity. Altern Ther Health Med. 2000;6:68-74,77-80.
10. Roos EM, Klässbo M, Lohmander LS. WOMAC osteoarthritis index. Reliability, validity, and responsiveness in patients with arthroscopically assessed osteoarthritis. Western Ontario and MacMaster Universities. Scand J Rheumatol. 1999;28:210-215.
11. Ehrich EW, Davies GM, Watson DJ, et al. Minimal perceptible clinical improvement with the Western Ontario and McMaster Universities osteoarthritis index questionnaire and global assessments in patients with osteoarthritis. J Rheumatol. 2000;27:2635-2641.
12. Rejeski WJ, Ettinger WH Jr, Shumaker S, et al. The evaluation of pain in patients with knee osteoarthritis: the knee pain scale. J Rheumatol. 1995;22:1124-1129.
13. Dorman TA. Prolotherapy: A survey. J Orthop Med. 1993;15:28-32.
14. Hauser RA, Hauser MA, Baird NM, et al. Prolotherapy as an alternative to surgery: A prospective pilot study of 34 patients from a private medical practice. J Prolotherapy. 2010;2:272-281.
Recommend prolotherapy for patients with knee osteoarthritis (OA) that does not respond to conventional therapies.1
Strength of recommendation
B: Based on a 3-arm, blinded, randomized controlled trial (RCT).
Rabago D, Patterson JJ, Mundt M, et al. Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial. Ann Fam Med. 2013;11:229-237.
Illustrative case
A 59-year-old woman with OA comes to your office with chronic knee pain. She has tried acetaminophen, ibuprofen, intra-articular corticosteroid injections, and physical therapy without significant improvement in pain or functioning. She wants to avoid daily medications or surgery and wonders if there are any interventions that will not lead to prolonged time away from work. What would you consider?
Additional options needed for knee OA
More than 25% of adults ages 55 years and older suffer from knee pain, and OA is an increasingly common cause.2 Knee pain is a major source of morbidity in the United States; it limits patients’ activities and increases comorbidities such as depression and obesity.
Conventional outpatient treatments for knee pain range from acetaminophen, nonsteroidal anti-inflammatory drugs, glucosamine, chondroitin, and opiates to topical capsaicin therapy, intra-articular hyaluronic acid, and corticosteroid injections. Cost, efficacy, and safety limit these therapies.3
Prolotherapy is another option used to treat musculoskeletal pain. It involves repeatedly injecting a sclerosing solution (usually dextrose) into the sites of chronic musculoskeletal pain.4 The mechanism of action is thought to be the result of local tissue irritation stimulating inflammatory pathways, which leads to the release of growth factors and subsequent healing.4,5 Previous studies evaluating the usefulness of prolotherapy have lacked methodological rigor, have not been randomized adequately, or have lacked a placebo comparison.6-9
STUDY SUMMARY: Prolotherapy reduces pain more than exercise or placebo
Rabago et al1 randomized 90 participants to dextrose prolotherapy, placebo saline injections, or at-home exercise. Participants had a ≥3 month history of painful knee OA based on a self-reported pain scale, radiographic evidence of knee OA within the past 5 years, and tenderness of ≥1 or more anterior knee structures on exam.
Sixty-six percent of participants were female. The mean age was 56.7 years and 74% were overweight (body mass index [BMI], 25-29.9) or obese (BMI ≥30). Participants chose to have one or both knees treated; 43 knees were injected in the dextrose group, 41 received saline injections, and 47 were assessed in the exercise group. There were no significant differences among groups at baseline.
Participants in the prolotherapy and saline groups received injections at 1, 5, and 9 weeks, plus optional injections at 13 and 17 weeks per physician and participant preference. Injections were administered both extra- and intra-articularly. Intra-articular injections were delivered using a 25-gauge needle with a mixture of 25% dextrose, 1% saline, and 1% lidocaine for a total volume of 6 mL. Extra-articular injections were delivered with a peppering technique with a maximum of 15 punctures over painful ligaments and tendons around the knee. The extra-articular solution was similar to the intra-articular except 15% dextrose was used, with a total maximum volume of 22.5 mL.
The placebo injection group received injections in the same pattern and technique, but the solution was the same quantity of 1% lidocaine plus 1% saline to achieve the same volume. The injector, outcome assessor, primary investigator, and participants were blinded to injection group.
In the exercise group, a study coordinator taught participants knee exercises and gave them a pamphlet with 10 exercises to perform at home. Adherence to at-home exercises was assessed with monthly logs that participants mailed in for the first 20 weeks of the study. Seventy-seven percent of participants reported doing their at-home exercises.
The primary outcome measure was change in composite score on the Western Ontario McMaster Universities Osteoarthritis Index (WOMAC), a validated questionnaire used to evaluate knee-related quality of life that features subscales for pain, stiffness, and function.10 The minimal clinically important difference in change in score on this 100-point instrument is 12 points; higher scores indicate better quality of life.11 The secondary outcome was change in score on the Knee Pain Scale (KPS), a validated questionnaire that uses a 4-point scale to measure pain frequency and a 5-point scale to measure pain severity; higher scores indicate worse symptoms.12
Improvements seen in both scores
Using an intention-to-treat analysis for all groups, WOMAC composite scores improved at 9 weeks and remained improved through 52 weeks. At 9 weeks, the dextrose group increased 13.91 points, compared with 6.75 (P=.020) in the saline group and 2.51 (P=.001) points in the exercise group.
At 52 weeks, the dextrose group showed an improvement of 15.32 points compared with 7.59 (P=.022) in the saline group and 8.24 (P=.034) in the exercise group. Fifty percent (15/30) of participants in the dextrose group had clinically meaningful improvement as measured by an increase of ≥12 points on the WOMAC, compared with 34% (10/29) and 26% (8/31) in the saline and exercise groups, respectively. At 52 weeks, the dextrose group had significantly decreased KPS knee pain frequency scores compared with the saline group (mean difference [MD], -1.20 vs. -0.60; P<.05) and exercise group (MD, -1.20 vs. -0.40; P<.05). Knee pain severity scores also decreased in the dextrose group compared to the saline (MD, -0.92 vs. -0.32, P<.05) and exercise groups (MD, -0.92 vs. -0.11; P<.05). There were no significant differences in KPS score decreases between the saline and exercise groups.
What about patient satisfaction?
At week 52, all participants were asked, “Would you recommend the therapy you received in this study to others with knee OA like yours?” Ninety-one percent of the dextrose group, 82% of the saline group, and 89% of the exercise group answered “Yes.”
All participants who received injections reported mild to moderate post-injection pain. Five participants in the saline group and 3 in the dextrose group experienced bruising. No other side effects or adverse events were documented. According to daily logs of medication use in the 7 days after injection, 74% of patients in the dextrose group used acetaminophen and 47% used oxycodone, compared with 63% and 43%, respectively, in the saline group. The study authors did not comment on the significance of these differences.
WHAT'S NEW: A randomized study provides support for prolotherapy
This study is the first to adequately demonstrate improvement in knee-related quality of life with prolotherapy compared with placebo (saline) or exercise. Family physicians can now add this therapy to their “toolbox” for patient complaints of OA pain.
CAVEATS: Efficacy is unknown in patients with certain comorbidities
Efficacy is unknown in patients with certain comorbidities Of 894 people screened, only 118 met initial eligibility criteria. This study did not include patients who were taking daily opioids, had diabetes, or had a BMI >40, so its results may not be generalizable to such patients.
Also, while the study demonstrated no side effects or adverse events other than bruising in 8 patients, the sample size may have been too small to detect less common adverse events. However, prior studies of prolotherapy have not revealed any substantial adverse effects.7
Strong evidence for some conditions… not for others. The strongest data support the efficacy of prolotherapy for focal tendinopathy (lateral epicondylosis) and knee OA. Evidence supporting prolotherapy for multimodal conditions, such as chronic low back pain, is less robust.4
CHALLENGES TO IMPLEMENTATION: Finding a prolotherapist near you may not be easy
The main challenge to implementation is finding a certified prolotherapist, or obtaining training in the technique. The prolotherapy knee protocol can be performed in an outpatient setting in less than 15 minutes, but the technique requires training. Prolotherapy training is available from multiple organizations, including the American Association of Orthopaedic Medicine, which requires 100 course hours for prolotherapy certification.4 No formal survey on the number of prolotherapists in the United States has been conducted since 1993,13 but Rabago et al1 estimated that the number is in the hundreds.
Insurance coverage frequently is a challenge. Most third-party payers do not cover prolotherapy, and currently most patients pay out-of-pocket. Rabago et al1 indicated that at their institution, the cost is $218 per injection session. Another study published in 2010 put the average total cost of 4 to 6 prolotherapy sessions at $1800.14
And from the patient’s perspective … The multiple needle sticks involved in prolotherapy can be painful.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center of Research Resources or the National Institutes of Health.
Recommend prolotherapy for patients with knee osteoarthritis (OA) that does not respond to conventional therapies.1
Strength of recommendation
B: Based on a 3-arm, blinded, randomized controlled trial (RCT).
Rabago D, Patterson JJ, Mundt M, et al. Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial. Ann Fam Med. 2013;11:229-237.
Illustrative case
A 59-year-old woman with OA comes to your office with chronic knee pain. She has tried acetaminophen, ibuprofen, intra-articular corticosteroid injections, and physical therapy without significant improvement in pain or functioning. She wants to avoid daily medications or surgery and wonders if there are any interventions that will not lead to prolonged time away from work. What would you consider?
Additional options needed for knee OA
More than 25% of adults ages 55 years and older suffer from knee pain, and OA is an increasingly common cause.2 Knee pain is a major source of morbidity in the United States; it limits patients’ activities and increases comorbidities such as depression and obesity.
Conventional outpatient treatments for knee pain range from acetaminophen, nonsteroidal anti-inflammatory drugs, glucosamine, chondroitin, and opiates to topical capsaicin therapy, intra-articular hyaluronic acid, and corticosteroid injections. Cost, efficacy, and safety limit these therapies.3
Prolotherapy is another option used to treat musculoskeletal pain. It involves repeatedly injecting a sclerosing solution (usually dextrose) into the sites of chronic musculoskeletal pain.4 The mechanism of action is thought to be the result of local tissue irritation stimulating inflammatory pathways, which leads to the release of growth factors and subsequent healing.4,5 Previous studies evaluating the usefulness of prolotherapy have lacked methodological rigor, have not been randomized adequately, or have lacked a placebo comparison.6-9
STUDY SUMMARY: Prolotherapy reduces pain more than exercise or placebo
Rabago et al1 randomized 90 participants to dextrose prolotherapy, placebo saline injections, or at-home exercise. Participants had a ≥3 month history of painful knee OA based on a self-reported pain scale, radiographic evidence of knee OA within the past 5 years, and tenderness of ≥1 or more anterior knee structures on exam.
Sixty-six percent of participants were female. The mean age was 56.7 years and 74% were overweight (body mass index [BMI], 25-29.9) or obese (BMI ≥30). Participants chose to have one or both knees treated; 43 knees were injected in the dextrose group, 41 received saline injections, and 47 were assessed in the exercise group. There were no significant differences among groups at baseline.
Participants in the prolotherapy and saline groups received injections at 1, 5, and 9 weeks, plus optional injections at 13 and 17 weeks per physician and participant preference. Injections were administered both extra- and intra-articularly. Intra-articular injections were delivered using a 25-gauge needle with a mixture of 25% dextrose, 1% saline, and 1% lidocaine for a total volume of 6 mL. Extra-articular injections were delivered with a peppering technique with a maximum of 15 punctures over painful ligaments and tendons around the knee. The extra-articular solution was similar to the intra-articular except 15% dextrose was used, with a total maximum volume of 22.5 mL.
The placebo injection group received injections in the same pattern and technique, but the solution was the same quantity of 1% lidocaine plus 1% saline to achieve the same volume. The injector, outcome assessor, primary investigator, and participants were blinded to injection group.
In the exercise group, a study coordinator taught participants knee exercises and gave them a pamphlet with 10 exercises to perform at home. Adherence to at-home exercises was assessed with monthly logs that participants mailed in for the first 20 weeks of the study. Seventy-seven percent of participants reported doing their at-home exercises.
The primary outcome measure was change in composite score on the Western Ontario McMaster Universities Osteoarthritis Index (WOMAC), a validated questionnaire used to evaluate knee-related quality of life that features subscales for pain, stiffness, and function.10 The minimal clinically important difference in change in score on this 100-point instrument is 12 points; higher scores indicate better quality of life.11 The secondary outcome was change in score on the Knee Pain Scale (KPS), a validated questionnaire that uses a 4-point scale to measure pain frequency and a 5-point scale to measure pain severity; higher scores indicate worse symptoms.12
Improvements seen in both scores
Using an intention-to-treat analysis for all groups, WOMAC composite scores improved at 9 weeks and remained improved through 52 weeks. At 9 weeks, the dextrose group increased 13.91 points, compared with 6.75 (P=.020) in the saline group and 2.51 (P=.001) points in the exercise group.
At 52 weeks, the dextrose group showed an improvement of 15.32 points compared with 7.59 (P=.022) in the saline group and 8.24 (P=.034) in the exercise group. Fifty percent (15/30) of participants in the dextrose group had clinically meaningful improvement as measured by an increase of ≥12 points on the WOMAC, compared with 34% (10/29) and 26% (8/31) in the saline and exercise groups, respectively. At 52 weeks, the dextrose group had significantly decreased KPS knee pain frequency scores compared with the saline group (mean difference [MD], -1.20 vs. -0.60; P<.05) and exercise group (MD, -1.20 vs. -0.40; P<.05). Knee pain severity scores also decreased in the dextrose group compared to the saline (MD, -0.92 vs. -0.32, P<.05) and exercise groups (MD, -0.92 vs. -0.11; P<.05). There were no significant differences in KPS score decreases between the saline and exercise groups.
What about patient satisfaction?
At week 52, all participants were asked, “Would you recommend the therapy you received in this study to others with knee OA like yours?” Ninety-one percent of the dextrose group, 82% of the saline group, and 89% of the exercise group answered “Yes.”
All participants who received injections reported mild to moderate post-injection pain. Five participants in the saline group and 3 in the dextrose group experienced bruising. No other side effects or adverse events were documented. According to daily logs of medication use in the 7 days after injection, 74% of patients in the dextrose group used acetaminophen and 47% used oxycodone, compared with 63% and 43%, respectively, in the saline group. The study authors did not comment on the significance of these differences.
WHAT'S NEW: A randomized study provides support for prolotherapy
This study is the first to adequately demonstrate improvement in knee-related quality of life with prolotherapy compared with placebo (saline) or exercise. Family physicians can now add this therapy to their “toolbox” for patient complaints of OA pain.
CAVEATS: Efficacy is unknown in patients with certain comorbidities
Efficacy is unknown in patients with certain comorbidities Of 894 people screened, only 118 met initial eligibility criteria. This study did not include patients who were taking daily opioids, had diabetes, or had a BMI >40, so its results may not be generalizable to such patients.
Also, while the study demonstrated no side effects or adverse events other than bruising in 8 patients, the sample size may have been too small to detect less common adverse events. However, prior studies of prolotherapy have not revealed any substantial adverse effects.7
Strong evidence for some conditions… not for others. The strongest data support the efficacy of prolotherapy for focal tendinopathy (lateral epicondylosis) and knee OA. Evidence supporting prolotherapy for multimodal conditions, such as chronic low back pain, is less robust.4
CHALLENGES TO IMPLEMENTATION: Finding a prolotherapist near you may not be easy
The main challenge to implementation is finding a certified prolotherapist, or obtaining training in the technique. The prolotherapy knee protocol can be performed in an outpatient setting in less than 15 minutes, but the technique requires training. Prolotherapy training is available from multiple organizations, including the American Association of Orthopaedic Medicine, which requires 100 course hours for prolotherapy certification.4 No formal survey on the number of prolotherapists in the United States has been conducted since 1993,13 but Rabago et al1 estimated that the number is in the hundreds.
Insurance coverage frequently is a challenge. Most third-party payers do not cover prolotherapy, and currently most patients pay out-of-pocket. Rabago et al1 indicated that at their institution, the cost is $218 per injection session. Another study published in 2010 put the average total cost of 4 to 6 prolotherapy sessions at $1800.14
And from the patient’s perspective … The multiple needle sticks involved in prolotherapy can be painful.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center of Research Resources or the National Institutes of Health.
1. Rabago D, Patterson JJ, Mundt M, et al. Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial. Ann Fam Med. 2013;11:229-237.
2. Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91-97.
3. Lawrence RC, Felson DT, Helmick CG, et al; National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26-35.
4. Rabago D, Slattengren A, Zgierska A. Prolotherapy in primary care practice. Prim Care. 2010;37:65-80.
5. Hackett GS, Hemwall GA, Montgomery GA. Ligament and Tendon Relaxation Treated by Prolotherapy. 5th ed. Oak Park, IL: Institute in Basic Life Principles; 1991.
6. Schultz LW. A treatment for subluxation of the temporomandibular joint. JAMA. 1937;109:1032-1035.
7. Rabago D, Best TM, Beamsley M, et al. A systematic review of prolotherapy for chronic musculoskeletal pain. Clin J Sport Med. 2005;15:376-380.
8. Reeves KD, Hassanein KM. Long-term effects of dextrose prolotherapy for anterior cruciate ligament laxity. Altern Ther Health Med. 2003;9:58-62.
9. Reeves KD, Hassanein K. Randomized prospective double-blind placebo-controlled study of dextrose prolotherapy for knee osteoarthritis with or without ACL laxity. Altern Ther Health Med. 2000;6:68-74,77-80.
10. Roos EM, Klässbo M, Lohmander LS. WOMAC osteoarthritis index. Reliability, validity, and responsiveness in patients with arthroscopically assessed osteoarthritis. Western Ontario and MacMaster Universities. Scand J Rheumatol. 1999;28:210-215.
11. Ehrich EW, Davies GM, Watson DJ, et al. Minimal perceptible clinical improvement with the Western Ontario and McMaster Universities osteoarthritis index questionnaire and global assessments in patients with osteoarthritis. J Rheumatol. 2000;27:2635-2641.
12. Rejeski WJ, Ettinger WH Jr, Shumaker S, et al. The evaluation of pain in patients with knee osteoarthritis: the knee pain scale. J Rheumatol. 1995;22:1124-1129.
13. Dorman TA. Prolotherapy: A survey. J Orthop Med. 1993;15:28-32.
14. Hauser RA, Hauser MA, Baird NM, et al. Prolotherapy as an alternative to surgery: A prospective pilot study of 34 patients from a private medical practice. J Prolotherapy. 2010;2:272-281.
1. Rabago D, Patterson JJ, Mundt M, et al. Dextrose prolotherapy for knee osteoarthritis: a randomized controlled trial. Ann Fam Med. 2013;11:229-237.
2. Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91-97.
3. Lawrence RC, Felson DT, Helmick CG, et al; National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26-35.
4. Rabago D, Slattengren A, Zgierska A. Prolotherapy in primary care practice. Prim Care. 2010;37:65-80.
5. Hackett GS, Hemwall GA, Montgomery GA. Ligament and Tendon Relaxation Treated by Prolotherapy. 5th ed. Oak Park, IL: Institute in Basic Life Principles; 1991.
6. Schultz LW. A treatment for subluxation of the temporomandibular joint. JAMA. 1937;109:1032-1035.
7. Rabago D, Best TM, Beamsley M, et al. A systematic review of prolotherapy for chronic musculoskeletal pain. Clin J Sport Med. 2005;15:376-380.
8. Reeves KD, Hassanein KM. Long-term effects of dextrose prolotherapy for anterior cruciate ligament laxity. Altern Ther Health Med. 2003;9:58-62.
9. Reeves KD, Hassanein K. Randomized prospective double-blind placebo-controlled study of dextrose prolotherapy for knee osteoarthritis with or without ACL laxity. Altern Ther Health Med. 2000;6:68-74,77-80.
10. Roos EM, Klässbo M, Lohmander LS. WOMAC osteoarthritis index. Reliability, validity, and responsiveness in patients with arthroscopically assessed osteoarthritis. Western Ontario and MacMaster Universities. Scand J Rheumatol. 1999;28:210-215.
11. Ehrich EW, Davies GM, Watson DJ, et al. Minimal perceptible clinical improvement with the Western Ontario and McMaster Universities osteoarthritis index questionnaire and global assessments in patients with osteoarthritis. J Rheumatol. 2000;27:2635-2641.
12. Rejeski WJ, Ettinger WH Jr, Shumaker S, et al. The evaluation of pain in patients with knee osteoarthritis: the knee pain scale. J Rheumatol. 1995;22:1124-1129.
13. Dorman TA. Prolotherapy: A survey. J Orthop Med. 1993;15:28-32.
14. Hauser RA, Hauser MA, Baird NM, et al. Prolotherapy as an alternative to surgery: A prospective pilot study of 34 patients from a private medical practice. J Prolotherapy. 2010;2:272-281.
Copyright © 2014 Family Physicians Inquiries Network. All rights reserved.
Should you screen for postpartum depression?
Make depression screening a routine part of the postpartum visit.1
Strength of recommendation
B: Based on a single blinded randomized controlled trial (RCT).
Yawn BP, Dietrich AJ, Wollan P, et al. TRIPPD practices. TRIPPD: a practice-based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10:320-329.
Illustrative case
A 20-year-old patient comes in at 6 weeks’ postpartum for routine care. Should you screen her for postpartum depression?
The incidence of depression in the first 3 months’ postpartum is estimated at about 14%,2,3 and the consequences can be severe. A new mom with a mood disorder in the first year of her child’s life can disrupt the mother-infant relationship, thereby contributing to both short- and long-term adverse outcomes for the child. These include behavior problems, low self-esteem, poor self-regulation, and an increased risk of impaired mental and motor development.4,5
Postpartum depression often goes undetected
Despite this correlation, postpartum depression is both under-recognized and undertreated.6 A prospective randomized study of 5169 women who were screened for postpartum depression bears this out. Researchers found that about one in 4 (26%) of the 674 mothers who had positive screens were not asked about their emotional state by their clinicians.2
This may be due to a lack of evidence of the efficacy of screening for postpartum depression. In the Healthy Start Depression Initiative (n=1336), universal screening—with referrals to mental health care outside of the primary care physicians’ offices—did not alter either the level of depressive symptoms over a 10-month period or depression treatment.7
The American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice noted in 2010 (and reaffirmed in 2012) that there is insufficient evidence to support a firm recommendation for universal postpartum screening for depression.8 Neither the US Preventive Services Task Force nor the American Academy of Family Physicians has a specific recommendation regarding postpartum depression.
STUDY SUMMARY
Screening—with follow-up—leads to better outcomes
The study by Yawn et al included 28 family medicine practices in 21 states, randomized to either usual care or intervention.1 Eligible practices had to have provided well-baby or maternity care to more than 30 patients in the previous year, but not to routinely screen for postpartum depression. A total of 2343 women aged 18 years or older—all of whom were between 5 and 12 weeks’ postpartum and planning on continuing care at the family medicine practice at the time they entered the study—were enrolled.
Staff at the 14 intervention sites received training in postpartum depression screening and diagnosis. They were also given a set of tools to facilitate management of postpartum depression, including an outline for follow-up visits and scripts for nurses to use for telephone calls relating to antidepressants. Therapy options were left to the discretion of the physician and the patient, with the help of tools that detailed the doses and adverse effects of various medications and described cognitive behavioral therapy.
At the start of the study, participants at all 28 sites were given survey packets containing the Edinburgh Postnatal Depression Scale (EPDS) and the 9-item Patient Health Questionnaire (PHQ-9). Patients subsequently received surveys by mail at 6 and 12 months’ postpartum for self-reported outcomes. Clinicians at the intervention sites had routine access to the EPDS and PHQ-9 scores; those at the usual care sites did not.
The primary outcome was ≥5 point drop in the PHQ-9 score from baseline at 6 or 12 months’ postpartum, considered to be an indicator of clinical improvement and/or response to therapy. The PHQ-9 is a validated measure of depression severity, with the proven ability to detect changes over time.9,10
Of the 2343 women initially enrolled in the study, 1897 (81%) provided outcome information and were included in the analysis. The rates of women with elevated depression scores (EPDS and/or PHQ-9 ≥10) at the start were comparable between the intervention and usual care groups (29.5% vs 25.8%, respectively).
Of those whose scores were initially elevated, 219 women in the intervention group and 178 women in the usual care group returned surveys at 12 months and were included in the final analysis. The results: 45% of those in the intervention group met the primary outcome—a decline in self-reported depressive symptom levels, as indicated by a PHQ-9 decrease ≥5 points—compared with 35% of the women in the usual care group (odds ratio, 1.8; 95% confidence interval, 1.14-2.9; P=.001). Not surprisingly, medical record review also indicated that those in the intervention group who initially had elevated depression scores were more likely to have received a diagnosis (66% vs 41%; P=.0006) and therapy (20% vs 11%; P=.02) for postpartum depression.
WHAT'S NEW?
We now have evidence of the efficacy of postpartum screening
This is the first large study of a primary care-based approach to screening, diagnosis, and management of postpartum depression to show any improvement in maternal outcomes at 12 months. Prior universal screening and referral support in the Healthy Start program was done by paraprofessionals, who referred women with positive screens for mental health care outside of the primary care setting and did not reduce the rate of depression in perinatal women.7
CAVEATS
Dropout rate, socioeconomic status may affect results
Among the women who initially were found to be positive for postpartum depression, 38% did not return questionnaires at 12 months’ postpartum. While this loss to follow-up is high, it is comparable to that of most effectiveness trials11 with similar rates in the intervention and usual care groups.
Within the intervention group, there was no statistical difference between women who did and did not return the questionnaires with regard to marital status, history of depression, income, or uninsured status. However, women in the usual care group who did not return the 12-month questionnaire were more likely to be poor (89% vs 57%; P<.01) and uninsured (49% vs 29%; P<.01) than those who did return the questionnaire.
The impact of these differences and the loss to follow-up in this study is unknown. However, low socioeconomic status has been shown to be a strong risk factor for the development of postpartum depression.12 The authors of the study suggest (and we agree) that the difference in socioeconomic status in women who did not return the questionnaire may underestimate the positive impact of this screening approach.
CHALLENGES TO IMPLEMENTATION
Screening requires extra work
Personnel at the intervention sites received a half day of training in postpartum depression screening, diagnosis, and nursing telephone follow-up. The workload at these sites also increased, as most women found to have postpartum depression received one to 2 follow-up telephone calls and an average of one to 2 follow-up visits after the start of therapy. These measures, while seemingly modest, could pose a challenge to implementation. This could potentially be alleviated by the additional payments for care coordination promised in the Patient Protection and Affordable Care Act.13
ACKNOWLEDGEMENT
The PURLs Surveillance System was developed in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to The University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center of Research Resources or the National Institutes of Health.
1. Yawn BP, Dietrich AJ, Wollan P, et al; TRIPPD practices. TRIPPD: a practice-based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10:320-329.
2. Horowitz JA, Murphy CA, Gregory KE, et al. Best practices: community-based postpartum depression screening: results from the CARE study. Psychiatr Serv. 2009;60:1432-1434.
3. Gaynes BN, Gavin N, Meltzer-Brody S, et al. Perinatal Depression: Prevalence, Screening Accuracy, and Screening Outcomes: Summary. AHRQ Evidence Report Summaries. Rockville, MD: Agency for Healthcare Research and Quality; Feb, 2005.
4. Murray L, Cooper PJ. The impact of postpartum depression on child development. In: Goodyer I, ed. Aetiological Mechanisms in Developmental Psychopathology. Oxford, England: Oxford University Press; 2003.
5. Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106:458-490.
6. Pearlstein T, Howard M, Salisbury A, et al. Postpartum depression. Am J Obstet Gynecol. 2009;200:357-364.
7. Yonkers KA, Smith MV, Lin H, et al. Depression screening of perinatal women: an evaluation of the healthy start depression initiative. Psychiatr Serv. 2009;60:322-328.
8. American College of Obstetricians and Gynecologists. Committee on Obstetric Practice. Committee opinion no. 453: Screening for depression during and after pregnancy. Obstet Gynecol. 2010;115(2 pt 1):394-395.
9. Löwe B, Kroenke K, Herzog W, et al. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81:61-66.
10. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613.
11. Ribisl KM, Walton MA, Mowbray CT, et al. Minimizing participant attrition in panel studies through the use of effective retention and tracking strategies: review and recommendations. Eval Program Planning. 1996;19:1-25.
12. Dolbier CL, Rush TE, Sahadeo LS, et al; Community Health Network Investigators. Relationships of race and socioeconomic status to postpartum depressive symptoms in rural african american and non-Hispanic white women. Matern Child Health J. 2013;17:1277-1287.
13. Centers for Medicare and Medicaid Services. The Affordable Care Act: Helping Providers Help Patients. Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ACO/downloads/ACO-Menu-Of-Options.pdf. Accessed September 6, 2013.
Make depression screening a routine part of the postpartum visit.1
Strength of recommendation
B: Based on a single blinded randomized controlled trial (RCT).
Yawn BP, Dietrich AJ, Wollan P, et al. TRIPPD practices. TRIPPD: a practice-based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10:320-329.
Illustrative case
A 20-year-old patient comes in at 6 weeks’ postpartum for routine care. Should you screen her for postpartum depression?
The incidence of depression in the first 3 months’ postpartum is estimated at about 14%,2,3 and the consequences can be severe. A new mom with a mood disorder in the first year of her child’s life can disrupt the mother-infant relationship, thereby contributing to both short- and long-term adverse outcomes for the child. These include behavior problems, low self-esteem, poor self-regulation, and an increased risk of impaired mental and motor development.4,5
Postpartum depression often goes undetected
Despite this correlation, postpartum depression is both under-recognized and undertreated.6 A prospective randomized study of 5169 women who were screened for postpartum depression bears this out. Researchers found that about one in 4 (26%) of the 674 mothers who had positive screens were not asked about their emotional state by their clinicians.2
This may be due to a lack of evidence of the efficacy of screening for postpartum depression. In the Healthy Start Depression Initiative (n=1336), universal screening—with referrals to mental health care outside of the primary care physicians’ offices—did not alter either the level of depressive symptoms over a 10-month period or depression treatment.7
The American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice noted in 2010 (and reaffirmed in 2012) that there is insufficient evidence to support a firm recommendation for universal postpartum screening for depression.8 Neither the US Preventive Services Task Force nor the American Academy of Family Physicians has a specific recommendation regarding postpartum depression.
STUDY SUMMARY
Screening—with follow-up—leads to better outcomes
The study by Yawn et al included 28 family medicine practices in 21 states, randomized to either usual care or intervention.1 Eligible practices had to have provided well-baby or maternity care to more than 30 patients in the previous year, but not to routinely screen for postpartum depression. A total of 2343 women aged 18 years or older—all of whom were between 5 and 12 weeks’ postpartum and planning on continuing care at the family medicine practice at the time they entered the study—were enrolled.
Staff at the 14 intervention sites received training in postpartum depression screening and diagnosis. They were also given a set of tools to facilitate management of postpartum depression, including an outline for follow-up visits and scripts for nurses to use for telephone calls relating to antidepressants. Therapy options were left to the discretion of the physician and the patient, with the help of tools that detailed the doses and adverse effects of various medications and described cognitive behavioral therapy.
At the start of the study, participants at all 28 sites were given survey packets containing the Edinburgh Postnatal Depression Scale (EPDS) and the 9-item Patient Health Questionnaire (PHQ-9). Patients subsequently received surveys by mail at 6 and 12 months’ postpartum for self-reported outcomes. Clinicians at the intervention sites had routine access to the EPDS and PHQ-9 scores; those at the usual care sites did not.
The primary outcome was ≥5 point drop in the PHQ-9 score from baseline at 6 or 12 months’ postpartum, considered to be an indicator of clinical improvement and/or response to therapy. The PHQ-9 is a validated measure of depression severity, with the proven ability to detect changes over time.9,10
Of the 2343 women initially enrolled in the study, 1897 (81%) provided outcome information and were included in the analysis. The rates of women with elevated depression scores (EPDS and/or PHQ-9 ≥10) at the start were comparable between the intervention and usual care groups (29.5% vs 25.8%, respectively).
Of those whose scores were initially elevated, 219 women in the intervention group and 178 women in the usual care group returned surveys at 12 months and were included in the final analysis. The results: 45% of those in the intervention group met the primary outcome—a decline in self-reported depressive symptom levels, as indicated by a PHQ-9 decrease ≥5 points—compared with 35% of the women in the usual care group (odds ratio, 1.8; 95% confidence interval, 1.14-2.9; P=.001). Not surprisingly, medical record review also indicated that those in the intervention group who initially had elevated depression scores were more likely to have received a diagnosis (66% vs 41%; P=.0006) and therapy (20% vs 11%; P=.02) for postpartum depression.
WHAT'S NEW?
We now have evidence of the efficacy of postpartum screening
This is the first large study of a primary care-based approach to screening, diagnosis, and management of postpartum depression to show any improvement in maternal outcomes at 12 months. Prior universal screening and referral support in the Healthy Start program was done by paraprofessionals, who referred women with positive screens for mental health care outside of the primary care setting and did not reduce the rate of depression in perinatal women.7
CAVEATS
Dropout rate, socioeconomic status may affect results
Among the women who initially were found to be positive for postpartum depression, 38% did not return questionnaires at 12 months’ postpartum. While this loss to follow-up is high, it is comparable to that of most effectiveness trials11 with similar rates in the intervention and usual care groups.
Within the intervention group, there was no statistical difference between women who did and did not return the questionnaires with regard to marital status, history of depression, income, or uninsured status. However, women in the usual care group who did not return the 12-month questionnaire were more likely to be poor (89% vs 57%; P<.01) and uninsured (49% vs 29%; P<.01) than those who did return the questionnaire.
The impact of these differences and the loss to follow-up in this study is unknown. However, low socioeconomic status has been shown to be a strong risk factor for the development of postpartum depression.12 The authors of the study suggest (and we agree) that the difference in socioeconomic status in women who did not return the questionnaire may underestimate the positive impact of this screening approach.
CHALLENGES TO IMPLEMENTATION
Screening requires extra work
Personnel at the intervention sites received a half day of training in postpartum depression screening, diagnosis, and nursing telephone follow-up. The workload at these sites also increased, as most women found to have postpartum depression received one to 2 follow-up telephone calls and an average of one to 2 follow-up visits after the start of therapy. These measures, while seemingly modest, could pose a challenge to implementation. This could potentially be alleviated by the additional payments for care coordination promised in the Patient Protection and Affordable Care Act.13
ACKNOWLEDGEMENT
The PURLs Surveillance System was developed in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to The University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center of Research Resources or the National Institutes of Health.
Make depression screening a routine part of the postpartum visit.1
Strength of recommendation
B: Based on a single blinded randomized controlled trial (RCT).
Yawn BP, Dietrich AJ, Wollan P, et al. TRIPPD practices. TRIPPD: a practice-based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10:320-329.
Illustrative case
A 20-year-old patient comes in at 6 weeks’ postpartum for routine care. Should you screen her for postpartum depression?
The incidence of depression in the first 3 months’ postpartum is estimated at about 14%,2,3 and the consequences can be severe. A new mom with a mood disorder in the first year of her child’s life can disrupt the mother-infant relationship, thereby contributing to both short- and long-term adverse outcomes for the child. These include behavior problems, low self-esteem, poor self-regulation, and an increased risk of impaired mental and motor development.4,5
Postpartum depression often goes undetected
Despite this correlation, postpartum depression is both under-recognized and undertreated.6 A prospective randomized study of 5169 women who were screened for postpartum depression bears this out. Researchers found that about one in 4 (26%) of the 674 mothers who had positive screens were not asked about their emotional state by their clinicians.2
This may be due to a lack of evidence of the efficacy of screening for postpartum depression. In the Healthy Start Depression Initiative (n=1336), universal screening—with referrals to mental health care outside of the primary care physicians’ offices—did not alter either the level of depressive symptoms over a 10-month period or depression treatment.7
The American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice noted in 2010 (and reaffirmed in 2012) that there is insufficient evidence to support a firm recommendation for universal postpartum screening for depression.8 Neither the US Preventive Services Task Force nor the American Academy of Family Physicians has a specific recommendation regarding postpartum depression.
STUDY SUMMARY
Screening—with follow-up—leads to better outcomes
The study by Yawn et al included 28 family medicine practices in 21 states, randomized to either usual care or intervention.1 Eligible practices had to have provided well-baby or maternity care to more than 30 patients in the previous year, but not to routinely screen for postpartum depression. A total of 2343 women aged 18 years or older—all of whom were between 5 and 12 weeks’ postpartum and planning on continuing care at the family medicine practice at the time they entered the study—were enrolled.
Staff at the 14 intervention sites received training in postpartum depression screening and diagnosis. They were also given a set of tools to facilitate management of postpartum depression, including an outline for follow-up visits and scripts for nurses to use for telephone calls relating to antidepressants. Therapy options were left to the discretion of the physician and the patient, with the help of tools that detailed the doses and adverse effects of various medications and described cognitive behavioral therapy.
At the start of the study, participants at all 28 sites were given survey packets containing the Edinburgh Postnatal Depression Scale (EPDS) and the 9-item Patient Health Questionnaire (PHQ-9). Patients subsequently received surveys by mail at 6 and 12 months’ postpartum for self-reported outcomes. Clinicians at the intervention sites had routine access to the EPDS and PHQ-9 scores; those at the usual care sites did not.
The primary outcome was ≥5 point drop in the PHQ-9 score from baseline at 6 or 12 months’ postpartum, considered to be an indicator of clinical improvement and/or response to therapy. The PHQ-9 is a validated measure of depression severity, with the proven ability to detect changes over time.9,10
Of the 2343 women initially enrolled in the study, 1897 (81%) provided outcome information and were included in the analysis. The rates of women with elevated depression scores (EPDS and/or PHQ-9 ≥10) at the start were comparable between the intervention and usual care groups (29.5% vs 25.8%, respectively).
Of those whose scores were initially elevated, 219 women in the intervention group and 178 women in the usual care group returned surveys at 12 months and were included in the final analysis. The results: 45% of those in the intervention group met the primary outcome—a decline in self-reported depressive symptom levels, as indicated by a PHQ-9 decrease ≥5 points—compared with 35% of the women in the usual care group (odds ratio, 1.8; 95% confidence interval, 1.14-2.9; P=.001). Not surprisingly, medical record review also indicated that those in the intervention group who initially had elevated depression scores were more likely to have received a diagnosis (66% vs 41%; P=.0006) and therapy (20% vs 11%; P=.02) for postpartum depression.
WHAT'S NEW?
We now have evidence of the efficacy of postpartum screening
This is the first large study of a primary care-based approach to screening, diagnosis, and management of postpartum depression to show any improvement in maternal outcomes at 12 months. Prior universal screening and referral support in the Healthy Start program was done by paraprofessionals, who referred women with positive screens for mental health care outside of the primary care setting and did not reduce the rate of depression in perinatal women.7
CAVEATS
Dropout rate, socioeconomic status may affect results
Among the women who initially were found to be positive for postpartum depression, 38% did not return questionnaires at 12 months’ postpartum. While this loss to follow-up is high, it is comparable to that of most effectiveness trials11 with similar rates in the intervention and usual care groups.
Within the intervention group, there was no statistical difference between women who did and did not return the questionnaires with regard to marital status, history of depression, income, or uninsured status. However, women in the usual care group who did not return the 12-month questionnaire were more likely to be poor (89% vs 57%; P<.01) and uninsured (49% vs 29%; P<.01) than those who did return the questionnaire.
The impact of these differences and the loss to follow-up in this study is unknown. However, low socioeconomic status has been shown to be a strong risk factor for the development of postpartum depression.12 The authors of the study suggest (and we agree) that the difference in socioeconomic status in women who did not return the questionnaire may underestimate the positive impact of this screening approach.
CHALLENGES TO IMPLEMENTATION
Screening requires extra work
Personnel at the intervention sites received a half day of training in postpartum depression screening, diagnosis, and nursing telephone follow-up. The workload at these sites also increased, as most women found to have postpartum depression received one to 2 follow-up telephone calls and an average of one to 2 follow-up visits after the start of therapy. These measures, while seemingly modest, could pose a challenge to implementation. This could potentially be alleviated by the additional payments for care coordination promised in the Patient Protection and Affordable Care Act.13
ACKNOWLEDGEMENT
The PURLs Surveillance System was developed in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to The University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center of Research Resources or the National Institutes of Health.
1. Yawn BP, Dietrich AJ, Wollan P, et al; TRIPPD practices. TRIPPD: a practice-based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10:320-329.
2. Horowitz JA, Murphy CA, Gregory KE, et al. Best practices: community-based postpartum depression screening: results from the CARE study. Psychiatr Serv. 2009;60:1432-1434.
3. Gaynes BN, Gavin N, Meltzer-Brody S, et al. Perinatal Depression: Prevalence, Screening Accuracy, and Screening Outcomes: Summary. AHRQ Evidence Report Summaries. Rockville, MD: Agency for Healthcare Research and Quality; Feb, 2005.
4. Murray L, Cooper PJ. The impact of postpartum depression on child development. In: Goodyer I, ed. Aetiological Mechanisms in Developmental Psychopathology. Oxford, England: Oxford University Press; 2003.
5. Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106:458-490.
6. Pearlstein T, Howard M, Salisbury A, et al. Postpartum depression. Am J Obstet Gynecol. 2009;200:357-364.
7. Yonkers KA, Smith MV, Lin H, et al. Depression screening of perinatal women: an evaluation of the healthy start depression initiative. Psychiatr Serv. 2009;60:322-328.
8. American College of Obstetricians and Gynecologists. Committee on Obstetric Practice. Committee opinion no. 453: Screening for depression during and after pregnancy. Obstet Gynecol. 2010;115(2 pt 1):394-395.
9. Löwe B, Kroenke K, Herzog W, et al. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81:61-66.
10. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613.
11. Ribisl KM, Walton MA, Mowbray CT, et al. Minimizing participant attrition in panel studies through the use of effective retention and tracking strategies: review and recommendations. Eval Program Planning. 1996;19:1-25.
12. Dolbier CL, Rush TE, Sahadeo LS, et al; Community Health Network Investigators. Relationships of race and socioeconomic status to postpartum depressive symptoms in rural african american and non-Hispanic white women. Matern Child Health J. 2013;17:1277-1287.
13. Centers for Medicare and Medicaid Services. The Affordable Care Act: Helping Providers Help Patients. Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ACO/downloads/ACO-Menu-Of-Options.pdf. Accessed September 6, 2013.
1. Yawn BP, Dietrich AJ, Wollan P, et al; TRIPPD practices. TRIPPD: a practice-based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10:320-329.
2. Horowitz JA, Murphy CA, Gregory KE, et al. Best practices: community-based postpartum depression screening: results from the CARE study. Psychiatr Serv. 2009;60:1432-1434.
3. Gaynes BN, Gavin N, Meltzer-Brody S, et al. Perinatal Depression: Prevalence, Screening Accuracy, and Screening Outcomes: Summary. AHRQ Evidence Report Summaries. Rockville, MD: Agency for Healthcare Research and Quality; Feb, 2005.
4. Murray L, Cooper PJ. The impact of postpartum depression on child development. In: Goodyer I, ed. Aetiological Mechanisms in Developmental Psychopathology. Oxford, England: Oxford University Press; 2003.
5. Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106:458-490.
6. Pearlstein T, Howard M, Salisbury A, et al. Postpartum depression. Am J Obstet Gynecol. 2009;200:357-364.
7. Yonkers KA, Smith MV, Lin H, et al. Depression screening of perinatal women: an evaluation of the healthy start depression initiative. Psychiatr Serv. 2009;60:322-328.
8. American College of Obstetricians and Gynecologists. Committee on Obstetric Practice. Committee opinion no. 453: Screening for depression during and after pregnancy. Obstet Gynecol. 2010;115(2 pt 1):394-395.
9. Löwe B, Kroenke K, Herzog W, et al. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81:61-66.
10. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613.
11. Ribisl KM, Walton MA, Mowbray CT, et al. Minimizing participant attrition in panel studies through the use of effective retention and tracking strategies: review and recommendations. Eval Program Planning. 1996;19:1-25.
12. Dolbier CL, Rush TE, Sahadeo LS, et al; Community Health Network Investigators. Relationships of race and socioeconomic status to postpartum depressive symptoms in rural african american and non-Hispanic white women. Matern Child Health J. 2013;17:1277-1287.
13. Centers for Medicare and Medicaid Services. The Affordable Care Act: Helping Providers Help Patients. Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ACO/downloads/ACO-Menu-Of-Options.pdf. Accessed September 6, 2013.
Copyright © 2013 Family Physicians Inquiries Network. All rights reserved.
Is this pregnancy viable?
Measure serum progesterone levels of women with bleeding or pain and inconclusive ultrasound in early pregnancy to rule out viability, potentially eliminating the need for serial b-hormone human chorionic gonadotropin (b-hCG) testing.1
STRENGTH OF RECOMMENDATION
A: Based on a systematic review and meta-analysis of 26 diagnostic accuracy studies.
Verhaegen J, Gallos ID, van Mello NM, et al. Accuracy of a single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies. BMJ. 2012;345:e6077.
Illustrative case
A 20-year-old woman with an estimated gestational age of 7 weeks comes to your clinic because of vaginal bleeding, which started 4 hours ago. A transvaginal ultrasound is inconclusive for an intrauterine pregnancy. Should you obtain a serum progesterone measurement?
Between 21% and 27% of pregnant women experience vaginal bleeding in their first trimester.2,3 This leads to concern, both for patients and physicians, as it can be the first sign of a miscarriage or an ectopic pregnancy. A longitudinal population-based Swedish study of women who had ever been pregnant found that one in 4 had experienced an early pregnancy failure. Overall, about 12% of clinically recognized pregnancies ended in miscarriage.4
Our ability to predict early pregnancy loss is limited
Tools used by clinicians to evaluate vaginal bleeding or pain in the first trimester include transvaginal ultrasound (TVUS) and serial serum β-hCG measurements.5 Even when combined with risk factors for pregnancy loss (serum levels of estradiol, inhibin A, and inhibin B; maternal age; smoking; past history of spontaneous miscarriage; and vaginal bleeding), TVUS is not accurate at predicting early pregnancy loss.6,7
A suboptimal rise in β-hCG (<66%) after 48 hours has historically been used to indicate possible miscarriage or ectopic pregnancy,1but studies have found similarly low rates of increase in some viable pregnancies, as well.8,9 And β-hCG measurements need to be done on more than one occasion, making this an inconvenient means of predicting miscarriage.
Moreover, β-hCG levels vary based on gestational age, leaving family physicians with no solid diagnostic rule regarding the appropriate level of rise in a viable pregnancy.10 Thus, there is a need for a test that complements TVUS and β-hCG to increase diagnostic accuracy in predicting nonviable pregnancies.
Can serum progesterone testing fill the gap?
Serum progesterone measurement is a noninvasive predictive tool, with low values associated with miscarriage and ectopic pregnancy and higher levels with a viable pregnancy.10 Studies have found that serum progesterone combined with β-hCG measurements has the highest reliability in predicting nonviable pregnancy, with a diagnostic accuracy of 85.7% (sensitivity, 88.1%; specificity, 84.3%). This compares with a diagnostic accuracy of 72.5% (sensitivity, 76.1%; specificity, 70.4%) for a single progesterone test alone, and 74.8% (sensitivity, 64.1%; specificity, 81.4%) for β-hCG alone.10-12 The data are from older studies, including a meta-analysis, that did not include the use of TVUS.10-12 But TVUS is now in widespread use and included in the systematic review and meta-analysis this PURL addresses.
Study summary:
Progesterone test is predictive—when combined with ultrasound
Verhaegen et al performed a comprehensive literature search to identify studies in which a single serum progesterone measurement was used to predict the viability of pregnancy vs miscarriage or ectopic pregnancy. They included studies of women with spontaneous pregnancy of <14 weeks. Trials of women who had conceived after ovulation induction or in vitro fertilization or received progesterone supplementation were excluded.
Twenty-six cohort studies met the inclusion criteria. These included 7 mostly high-quality studies, with a total of 2379 women with pain or bleeding and inconclusive TVUS, and 19 intermediate-quality studies (n=7057) of women who had pain or bleeding but no ultrasound.
Five of the 7 studies in women with symptoms and inconclusive TVUS had a similar progesterone test cutoff value (3.2-6 ng/mL). In these 5 studies (n=1998), the progesterone test predicted a nonviable pregnancy with a pooled sensitivity of 74.6% (95% CI, 50.6%-89.4%) and specificity of 98.4% (95% CI, 90.9%-99.7%), a positive likelihood ratio of 45 (7.1- 289) and a negative likelihood ratio of 0.26 (0.12-0.57). When progesterone was below the cutoff value, the probability of a nonviable pregnancy increased to 99.2%. In women with pain or bleeding but no ultrasound, a single progesterone test is less accurate in ruling out a viable pregnancy.
What's new
This test can end days of anxious waiting
This meta-analysis provides strong evidence that a single progesterone measurement is useful in predicting nonviable pregnancies in women with pain or bleeding when TVUS is inconclusive. In such patients, a low serum progesterone is highly predictive of a nonviable pregnancy.1 This finding enables the physician to counsel the woman immediately on the likely pregnancy loss, without waiting days for serial β-hCG results.
Caveats
Progesterone is a poor predictor of ectopic pregnancy
An important caveat to our recommendation is that a single serum progesterone test has a poor predictive value for ectopic pregnancy and should not be used for this purpose. A combination of TVUS and serial β-hCG remains the optimal strategy for diagnosing ectopic pregnancy.13
It is important to note that there is no universally accepted definition of a low serum progesterone level: This meta-analysis included studies with a cutoff value of 3.2 to 6 ng/mL in women who had had a previous ultrasound. What’s more, these studies did not evaluate the predictive value of a serum progesterone test combined with β-hCG measurements.
Challenges to implementation
There are none
We do not see any challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center of Research Resources or the National Institutes of Health.
1. Verhaegen J, Gallos ID, van Mello NM, et al. Accuracy of single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies. BMJ. 2012;345:e6077.
2. Hasan R, Baird DD, Herring AH, et al. Patterns and predictors of vaginal bleeding in the first trimester of pregnancy. Ann Epidemiol. 2010;20:524-531.
3. Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. BMJ. 1997;315:32-34.
4. Blohm F, Friden B, Milsom I. A prospective longitudinal population-based study of clinical miscarriage in an urban Swedish population. BJOG. 2008;115:176-183.
Chen BA, Creinin MD. Contemporary management of early pregnancy failure. Clin Obstet Gynecol. 2007;50:67-88.
5. Jauniaux E, Johns J, Burton GJ. The role of ultrasound imaging in diagnosing and investigating early pregnancy failure. Ultrasound Obstet Gynecol. 2005;25:613–624.
6. Gagnon A, Wilson RD, Audibert F, et al. Obstetrical complications associated with abnormal maternal serum markers analytes.J Obstet Gynaecol Can. 2008;30:918-949.
7. Barnhart KT, Sammel MD, Rinaudo PF, et al. Symptomatic patients with an early viable intrauterine pregnancy; hCG curves redefined. Obstet Gynecol. 2004;104:50-54.
8. Morse CB, Sammel MD, Shaunik A, et al. Performance of human chorionic gonadotropin curves in women at risk for ectopic pregnancy: exceptions to the rules. Fertil Steril. 2012;97:101e2-106.e2.
9. Mol BW, Lijmer JG, Ankum WM, et al. The accuracy of single serum progesterone measurement in the diagnosis of ectopic pregnancy: a meta-analysis. Hum Reprod. 1998;13:3220-3227.
10. Duan L, Yan D, Zeng W, et al. Predictive power of progesterone combined with beta human chorionic gonadotropin measurements in the outcome of threatened miscarriage. Arch Gynecol Obstet. 2011;283:431-4355.
11. Phipps MG, Hogan JW, Peipert JF, et al. Progesterone, inhibin, and hCG multiple marker strategy to differentiate viable from nonviable pregnancies. Obstet Gynecol. 2000;95:227-231.
12. American College of Obstetricians and Gynecologists. Practice Bulletin no. 94: Medical management of ectopic pregnancy. Obstet Gynecol. 2008;111:1479-1485.
Measure serum progesterone levels of women with bleeding or pain and inconclusive ultrasound in early pregnancy to rule out viability, potentially eliminating the need for serial b-hormone human chorionic gonadotropin (b-hCG) testing.1
STRENGTH OF RECOMMENDATION
A: Based on a systematic review and meta-analysis of 26 diagnostic accuracy studies.
Verhaegen J, Gallos ID, van Mello NM, et al. Accuracy of a single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies. BMJ. 2012;345:e6077.
Illustrative case
A 20-year-old woman with an estimated gestational age of 7 weeks comes to your clinic because of vaginal bleeding, which started 4 hours ago. A transvaginal ultrasound is inconclusive for an intrauterine pregnancy. Should you obtain a serum progesterone measurement?
Between 21% and 27% of pregnant women experience vaginal bleeding in their first trimester.2,3 This leads to concern, both for patients and physicians, as it can be the first sign of a miscarriage or an ectopic pregnancy. A longitudinal population-based Swedish study of women who had ever been pregnant found that one in 4 had experienced an early pregnancy failure. Overall, about 12% of clinically recognized pregnancies ended in miscarriage.4
Our ability to predict early pregnancy loss is limited
Tools used by clinicians to evaluate vaginal bleeding or pain in the first trimester include transvaginal ultrasound (TVUS) and serial serum β-hCG measurements.5 Even when combined with risk factors for pregnancy loss (serum levels of estradiol, inhibin A, and inhibin B; maternal age; smoking; past history of spontaneous miscarriage; and vaginal bleeding), TVUS is not accurate at predicting early pregnancy loss.6,7
A suboptimal rise in β-hCG (<66%) after 48 hours has historically been used to indicate possible miscarriage or ectopic pregnancy,1but studies have found similarly low rates of increase in some viable pregnancies, as well.8,9 And β-hCG measurements need to be done on more than one occasion, making this an inconvenient means of predicting miscarriage.
Moreover, β-hCG levels vary based on gestational age, leaving family physicians with no solid diagnostic rule regarding the appropriate level of rise in a viable pregnancy.10 Thus, there is a need for a test that complements TVUS and β-hCG to increase diagnostic accuracy in predicting nonviable pregnancies.
Can serum progesterone testing fill the gap?
Serum progesterone measurement is a noninvasive predictive tool, with low values associated with miscarriage and ectopic pregnancy and higher levels with a viable pregnancy.10 Studies have found that serum progesterone combined with β-hCG measurements has the highest reliability in predicting nonviable pregnancy, with a diagnostic accuracy of 85.7% (sensitivity, 88.1%; specificity, 84.3%). This compares with a diagnostic accuracy of 72.5% (sensitivity, 76.1%; specificity, 70.4%) for a single progesterone test alone, and 74.8% (sensitivity, 64.1%; specificity, 81.4%) for β-hCG alone.10-12 The data are from older studies, including a meta-analysis, that did not include the use of TVUS.10-12 But TVUS is now in widespread use and included in the systematic review and meta-analysis this PURL addresses.
Study summary:
Progesterone test is predictive—when combined with ultrasound
Verhaegen et al performed a comprehensive literature search to identify studies in which a single serum progesterone measurement was used to predict the viability of pregnancy vs miscarriage or ectopic pregnancy. They included studies of women with spontaneous pregnancy of <14 weeks. Trials of women who had conceived after ovulation induction or in vitro fertilization or received progesterone supplementation were excluded.
Twenty-six cohort studies met the inclusion criteria. These included 7 mostly high-quality studies, with a total of 2379 women with pain or bleeding and inconclusive TVUS, and 19 intermediate-quality studies (n=7057) of women who had pain or bleeding but no ultrasound.
Five of the 7 studies in women with symptoms and inconclusive TVUS had a similar progesterone test cutoff value (3.2-6 ng/mL). In these 5 studies (n=1998), the progesterone test predicted a nonviable pregnancy with a pooled sensitivity of 74.6% (95% CI, 50.6%-89.4%) and specificity of 98.4% (95% CI, 90.9%-99.7%), a positive likelihood ratio of 45 (7.1- 289) and a negative likelihood ratio of 0.26 (0.12-0.57). When progesterone was below the cutoff value, the probability of a nonviable pregnancy increased to 99.2%. In women with pain or bleeding but no ultrasound, a single progesterone test is less accurate in ruling out a viable pregnancy.
What's new
This test can end days of anxious waiting
This meta-analysis provides strong evidence that a single progesterone measurement is useful in predicting nonviable pregnancies in women with pain or bleeding when TVUS is inconclusive. In such patients, a low serum progesterone is highly predictive of a nonviable pregnancy.1 This finding enables the physician to counsel the woman immediately on the likely pregnancy loss, without waiting days for serial β-hCG results.
Caveats
Progesterone is a poor predictor of ectopic pregnancy
An important caveat to our recommendation is that a single serum progesterone test has a poor predictive value for ectopic pregnancy and should not be used for this purpose. A combination of TVUS and serial β-hCG remains the optimal strategy for diagnosing ectopic pregnancy.13
It is important to note that there is no universally accepted definition of a low serum progesterone level: This meta-analysis included studies with a cutoff value of 3.2 to 6 ng/mL in women who had had a previous ultrasound. What’s more, these studies did not evaluate the predictive value of a serum progesterone test combined with β-hCG measurements.
Challenges to implementation
There are none
We do not see any challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center of Research Resources or the National Institutes of Health.
Measure serum progesterone levels of women with bleeding or pain and inconclusive ultrasound in early pregnancy to rule out viability, potentially eliminating the need for serial b-hormone human chorionic gonadotropin (b-hCG) testing.1
STRENGTH OF RECOMMENDATION
A: Based on a systematic review and meta-analysis of 26 diagnostic accuracy studies.
Verhaegen J, Gallos ID, van Mello NM, et al. Accuracy of a single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies. BMJ. 2012;345:e6077.
Illustrative case
A 20-year-old woman with an estimated gestational age of 7 weeks comes to your clinic because of vaginal bleeding, which started 4 hours ago. A transvaginal ultrasound is inconclusive for an intrauterine pregnancy. Should you obtain a serum progesterone measurement?
Between 21% and 27% of pregnant women experience vaginal bleeding in their first trimester.2,3 This leads to concern, both for patients and physicians, as it can be the first sign of a miscarriage or an ectopic pregnancy. A longitudinal population-based Swedish study of women who had ever been pregnant found that one in 4 had experienced an early pregnancy failure. Overall, about 12% of clinically recognized pregnancies ended in miscarriage.4
Our ability to predict early pregnancy loss is limited
Tools used by clinicians to evaluate vaginal bleeding or pain in the first trimester include transvaginal ultrasound (TVUS) and serial serum β-hCG measurements.5 Even when combined with risk factors for pregnancy loss (serum levels of estradiol, inhibin A, and inhibin B; maternal age; smoking; past history of spontaneous miscarriage; and vaginal bleeding), TVUS is not accurate at predicting early pregnancy loss.6,7
A suboptimal rise in β-hCG (<66%) after 48 hours has historically been used to indicate possible miscarriage or ectopic pregnancy,1but studies have found similarly low rates of increase in some viable pregnancies, as well.8,9 And β-hCG measurements need to be done on more than one occasion, making this an inconvenient means of predicting miscarriage.
Moreover, β-hCG levels vary based on gestational age, leaving family physicians with no solid diagnostic rule regarding the appropriate level of rise in a viable pregnancy.10 Thus, there is a need for a test that complements TVUS and β-hCG to increase diagnostic accuracy in predicting nonviable pregnancies.
Can serum progesterone testing fill the gap?
Serum progesterone measurement is a noninvasive predictive tool, with low values associated with miscarriage and ectopic pregnancy and higher levels with a viable pregnancy.10 Studies have found that serum progesterone combined with β-hCG measurements has the highest reliability in predicting nonviable pregnancy, with a diagnostic accuracy of 85.7% (sensitivity, 88.1%; specificity, 84.3%). This compares with a diagnostic accuracy of 72.5% (sensitivity, 76.1%; specificity, 70.4%) for a single progesterone test alone, and 74.8% (sensitivity, 64.1%; specificity, 81.4%) for β-hCG alone.10-12 The data are from older studies, including a meta-analysis, that did not include the use of TVUS.10-12 But TVUS is now in widespread use and included in the systematic review and meta-analysis this PURL addresses.
Study summary:
Progesterone test is predictive—when combined with ultrasound
Verhaegen et al performed a comprehensive literature search to identify studies in which a single serum progesterone measurement was used to predict the viability of pregnancy vs miscarriage or ectopic pregnancy. They included studies of women with spontaneous pregnancy of <14 weeks. Trials of women who had conceived after ovulation induction or in vitro fertilization or received progesterone supplementation were excluded.
Twenty-six cohort studies met the inclusion criteria. These included 7 mostly high-quality studies, with a total of 2379 women with pain or bleeding and inconclusive TVUS, and 19 intermediate-quality studies (n=7057) of women who had pain or bleeding but no ultrasound.
Five of the 7 studies in women with symptoms and inconclusive TVUS had a similar progesterone test cutoff value (3.2-6 ng/mL). In these 5 studies (n=1998), the progesterone test predicted a nonviable pregnancy with a pooled sensitivity of 74.6% (95% CI, 50.6%-89.4%) and specificity of 98.4% (95% CI, 90.9%-99.7%), a positive likelihood ratio of 45 (7.1- 289) and a negative likelihood ratio of 0.26 (0.12-0.57). When progesterone was below the cutoff value, the probability of a nonviable pregnancy increased to 99.2%. In women with pain or bleeding but no ultrasound, a single progesterone test is less accurate in ruling out a viable pregnancy.
What's new
This test can end days of anxious waiting
This meta-analysis provides strong evidence that a single progesterone measurement is useful in predicting nonviable pregnancies in women with pain or bleeding when TVUS is inconclusive. In such patients, a low serum progesterone is highly predictive of a nonviable pregnancy.1 This finding enables the physician to counsel the woman immediately on the likely pregnancy loss, without waiting days for serial β-hCG results.
Caveats
Progesterone is a poor predictor of ectopic pregnancy
An important caveat to our recommendation is that a single serum progesterone test has a poor predictive value for ectopic pregnancy and should not be used for this purpose. A combination of TVUS and serial β-hCG remains the optimal strategy for diagnosing ectopic pregnancy.13
It is important to note that there is no universally accepted definition of a low serum progesterone level: This meta-analysis included studies with a cutoff value of 3.2 to 6 ng/mL in women who had had a previous ultrasound. What’s more, these studies did not evaluate the predictive value of a serum progesterone test combined with β-hCG measurements.
Challenges to implementation
There are none
We do not see any challenges to the implementation of this recommendation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center of Research Resources or the National Institutes of Health.
1. Verhaegen J, Gallos ID, van Mello NM, et al. Accuracy of single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies. BMJ. 2012;345:e6077.
2. Hasan R, Baird DD, Herring AH, et al. Patterns and predictors of vaginal bleeding in the first trimester of pregnancy. Ann Epidemiol. 2010;20:524-531.
3. Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. BMJ. 1997;315:32-34.
4. Blohm F, Friden B, Milsom I. A prospective longitudinal population-based study of clinical miscarriage in an urban Swedish population. BJOG. 2008;115:176-183.
Chen BA, Creinin MD. Contemporary management of early pregnancy failure. Clin Obstet Gynecol. 2007;50:67-88.
5. Jauniaux E, Johns J, Burton GJ. The role of ultrasound imaging in diagnosing and investigating early pregnancy failure. Ultrasound Obstet Gynecol. 2005;25:613–624.
6. Gagnon A, Wilson RD, Audibert F, et al. Obstetrical complications associated with abnormal maternal serum markers analytes.J Obstet Gynaecol Can. 2008;30:918-949.
7. Barnhart KT, Sammel MD, Rinaudo PF, et al. Symptomatic patients with an early viable intrauterine pregnancy; hCG curves redefined. Obstet Gynecol. 2004;104:50-54.
8. Morse CB, Sammel MD, Shaunik A, et al. Performance of human chorionic gonadotropin curves in women at risk for ectopic pregnancy: exceptions to the rules. Fertil Steril. 2012;97:101e2-106.e2.
9. Mol BW, Lijmer JG, Ankum WM, et al. The accuracy of single serum progesterone measurement in the diagnosis of ectopic pregnancy: a meta-analysis. Hum Reprod. 1998;13:3220-3227.
10. Duan L, Yan D, Zeng W, et al. Predictive power of progesterone combined with beta human chorionic gonadotropin measurements in the outcome of threatened miscarriage. Arch Gynecol Obstet. 2011;283:431-4355.
11. Phipps MG, Hogan JW, Peipert JF, et al. Progesterone, inhibin, and hCG multiple marker strategy to differentiate viable from nonviable pregnancies. Obstet Gynecol. 2000;95:227-231.
12. American College of Obstetricians and Gynecologists. Practice Bulletin no. 94: Medical management of ectopic pregnancy. Obstet Gynecol. 2008;111:1479-1485.
1. Verhaegen J, Gallos ID, van Mello NM, et al. Accuracy of single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies. BMJ. 2012;345:e6077.
2. Hasan R, Baird DD, Herring AH, et al. Patterns and predictors of vaginal bleeding in the first trimester of pregnancy. Ann Epidemiol. 2010;20:524-531.
3. Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. BMJ. 1997;315:32-34.
4. Blohm F, Friden B, Milsom I. A prospective longitudinal population-based study of clinical miscarriage in an urban Swedish population. BJOG. 2008;115:176-183.
Chen BA, Creinin MD. Contemporary management of early pregnancy failure. Clin Obstet Gynecol. 2007;50:67-88.
5. Jauniaux E, Johns J, Burton GJ. The role of ultrasound imaging in diagnosing and investigating early pregnancy failure. Ultrasound Obstet Gynecol. 2005;25:613–624.
6. Gagnon A, Wilson RD, Audibert F, et al. Obstetrical complications associated with abnormal maternal serum markers analytes.J Obstet Gynaecol Can. 2008;30:918-949.
7. Barnhart KT, Sammel MD, Rinaudo PF, et al. Symptomatic patients with an early viable intrauterine pregnancy; hCG curves redefined. Obstet Gynecol. 2004;104:50-54.
8. Morse CB, Sammel MD, Shaunik A, et al. Performance of human chorionic gonadotropin curves in women at risk for ectopic pregnancy: exceptions to the rules. Fertil Steril. 2012;97:101e2-106.e2.
9. Mol BW, Lijmer JG, Ankum WM, et al. The accuracy of single serum progesterone measurement in the diagnosis of ectopic pregnancy: a meta-analysis. Hum Reprod. 1998;13:3220-3227.
10. Duan L, Yan D, Zeng W, et al. Predictive power of progesterone combined with beta human chorionic gonadotropin measurements in the outcome of threatened miscarriage. Arch Gynecol Obstet. 2011;283:431-4355.
11. Phipps MG, Hogan JW, Peipert JF, et al. Progesterone, inhibin, and hCG multiple marker strategy to differentiate viable from nonviable pregnancies. Obstet Gynecol. 2000;95:227-231.
12. American College of Obstetricians and Gynecologists. Practice Bulletin no. 94: Medical management of ectopic pregnancy. Obstet Gynecol. 2008;111:1479-1485.
Copyright © 2013. The Family Physicians Inquiries Network. All rights reserved.