User login
Posttraumatic stress disorder: From pathophysiology to pharmacology
Posttraumatic stress disorder (PTSD) occurs acutely and chronically in the aftermath of severe and potentially life-threatening trauma.1 The prevalence of PTSD varies significantly across countries and by type of trauma (Box1-7).
Box
In the general population, the prevalence of posttraumatic stress disorder (PTSD) varies from as low as 0.3% in China to as high as 6.1% in New Zealand1 and 6.8% in the United States.2 These rates are actually much lower than expected when one considers that severe trauma is experienced by 60.7% of men and 51.2% of women.3,4 Although the majority of individuals exposed to trauma experience emotional distress immediately following a traumatic event, most of them do not develop PTSD.5
It appears that the context of trauma is important: 12% to 15% of veterans experience PTSD, compared with 19% to 75% of crime victims and 80% of rape victims.1 The lifetime risk for PTSD is twice as high in women as it is in men,6 and genetic vulnerability may play a role. For example, twin studies showed that approximately 30% of the risk for PTSD may be mediated by genetic predisposition.7
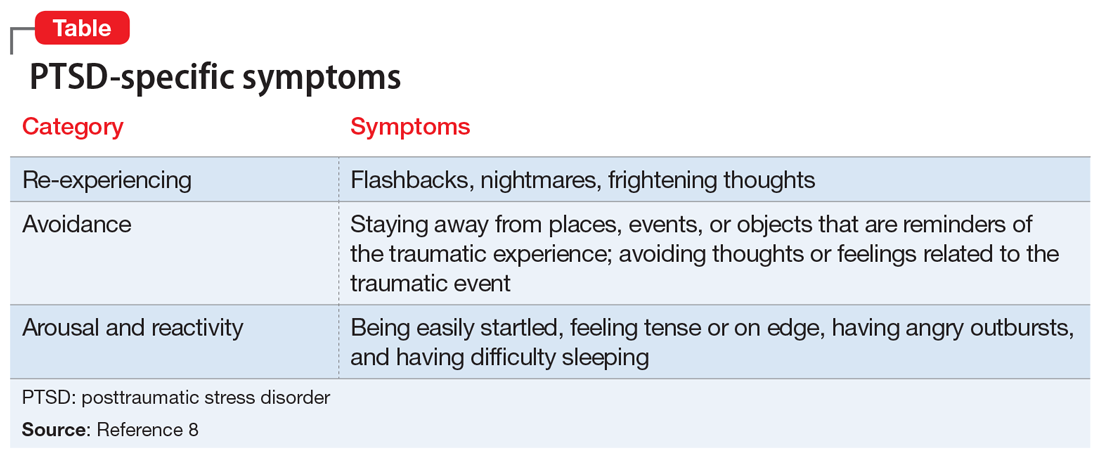
Individuals who develop PTSD experience a wide range of symptoms.8 These can be categorized as PTSD-specific symptoms, or nonspecific symptoms. PTSD-specific symptoms include nightmares, flashbacks, dissociative reactions, hyperreactivity or hyperarousal, distress with reminders of trauma, and avoidance of trauma-related physical reminders and thoughts/feelings (Table8). Nonspecific symptoms include depressive and anxiety symptoms and significant problems in social, relationship, or work situations.8
While successful treatment necessitates taking all of these symptoms into account, understanding the pathophysiology of PTSD can inform a more focused and rational treatment approach. In this article, we describe some key pathophysiologic PTSD studies, and focus on PTSD-specific psychopathology to inform treatment.
Brain systems implicated in PTSD
Neuropeptide Y (NPY) is an anxiolytic endogenous peptide that has connections to the hypothalamic-pituitary-adrenal (HPA) axis. Its levels can be modulated by stress.9 Preclinical and clinical studies strongly support a potential role of NPY dysfunction in the pathophysiology of PTSD. Lower concentrations of NPY increase susceptibility to PTSD in combat veterans10 and in animal models.11 Three single-nucleotide polymorphisms (SNPs) appear to mediate this effect.12 These findings strongly support pharmaceutical targeting this system as a useful therapeutic approach.13,14 Indeed, intranasal NPY administered as a single dose reduces anxiety in animal models15 and in humans,16 but this work has not yet translated into clinical tools.
Corticotropin-releasing hormone receptor (CRHR1) gene. Corticotropin-releasing hormone has been implicated in PTSD.17 Corticotropin-releasing hormone receptors (CRHR) are important mediators in response to stress.18,19 They bind corticotropin-releasing hormone and contribute to the integration of autonomic, behavioral, and immune responses to stress.20 Single-nucleotide polymorphisms in the regulatory portion of the CRHR1 gene are associated with an increased risk for depression in adults who have a history of child abuse.21
The CRHR1 receptor antagonist GSK561679 is an investigational agent for the treatment of mood and anxiety disorders.22 In exploratory studies,23,24 GSK561679 was found to inhibit fear-potentiated startle in patients with PTSD, but not overall PTSD symptoms, although a subset of women with a specific genetic variant of the CRHR1 gene (rs110402) experienced significant benefit.25,26 This suggests that we must learn more about this system before we proceed.27
Brain-derived neurotrophic factor (BDNF). The synthesis of BDNF is influenced by neuronal activity in the brain and plays a role in synaptic transmission and plasticity.28 Brain-derived neurotrophic factor is encoded by the BDNF gene, which has been implicated in stress vulnerability.29 A common SNP in the pro-region of the human BDNF gene results in a valine-to-methionine substitution at the 66th amino acid (Val66Met). The functional Val66Met polymorphism may have a role in the risk of developing PTSD. However, not all studies support this finding. One study found that an SNP with a resulting Val66Met polymorphism is associated with adult PTSD symptoms after childhood abuse, while a meta-analysis of 7 studies did not confirm this.30,31 We need to learn more about BDNF before we proceed.32
Continue to: Serotonin transporter (5-HTT) gene
Serotonin transporter (5-HTT) gene. Serotonin transporter is a monoamine transporter protein that terminates the neurotransmitter signal by transporting serotonin from the synaptic cleft back into the presynaptic neuron. It is encoded by the SLC6A4 gene, which resides on the long arm of chromosome 17(17q11.1-q12). It is a large gene with 31 kilo bases and 14 separate exons (transcribed regions).33,34
This gene has several variants. The best-studied is a variation in the promoter region. A 44-bp insertion or deletion yields the “long” and “short” alleles, respectively. The proteins produced by the 2 alleles are identical, but the amount of expressed protein is different. The short allele (“S”) is associated with a nearly 50% reduction in 5-HTT expression in both homozygotes and heterozygotes.35 A greater incidence of serotonin transporter promoter region (5-HTTLPR) S has been found in individuals with PTSD compared with those without PTSD,36-38 and 5-HTTLPR S increases the risk of PTSD in individuals with low social support39 or after very few traumatic events.40 The short allele variant is also associated with depression in individuals who face adversity.35,41
The overrepresentation of the short form of 5-HTTLPR in individuals who develop PTSD may represent a potential problem with current treatment paradigms, in which an antidepressant is the first-line treatment, because this allele is associated with reduced response to antidepressants.42,43 More distressing is the possible association of this allele with increased suicide risk, particularly violent suicide44 or repeated suicide attempts.45
Furthermore, a functional MRI study of patients who were anxious revealed that in individuals with the short allele, administration of
Catechol-o-methyltransferase (COMT) is one of the enzymes that degrades catecholamines such as dopamine, epinephrine, and norepinephrine (NE).47 In humans, COMT protein is encoded by the COMT gene. This gene is associated with allelic variants; the best-studied of these is Val158Met. COMT Val158Met polymorphism (rs4860) has been linked to deficits in stress response and emotional resilience.48,49 Val158Met is associated with a 40% reduction in enzyme activity and slower catalysis of catecholamines, resulting in increases in catecholamines levels in the brain, which may increase the risk of developing PTSD.50 Individuals homozygous for this SNP (Met/Met) are highly susceptible to develop PTSD independently of the severity of the trauma they experienced.51 The Val158Met polymorphism may be associated with other abnormalities, such as cognitive problems with specific frontal cortical activity, and also with improved antidepressant response (valine homozygotes less responsive than methionine homozygotes).52 This gene is available on gene testing profiles.
Continue to: The role of norepinephrine in PTSD
The role of norepinephrine in PTSD
Perhaps the greatest advance in the understanding of the pathophysiology of PTSD relates to changes in brain NE. The HPA axis is responsible for coordinating the hormonal response to stress. Dysregulation of this axis and increased activity of the central and peripheral noradrenergic systems are usually observed in patients with PTSD.53 Several monoamine neurotransmitters are important in the regulation and function of the HPA axis. Norepinephrine plays a major role in stress.
The clinical PTSD-specific criteria are all descriptions of excessive noradrenergic tone.54 For example, hypervigilance and hyperstartle are clearly anticipated as evidence of NE stimulation. Flashbacks, particularly those that might be precipitated by environmental cues, also can be a manifestation of the vigilance induced by NE. Sleep disturbances (insomnia and nightmares) are present; insomnia is reported more often than nightmares.55 Increased catecholamine levels, particularly NE, are a feature of sleep disturbances associated with middle insomnia. Dreams can be remembered only if you wake up during dreaming. Catecholamines do not change the content of dreams, just recall.56
In a study of central noradrenergic tone in patients with PTSD, 6 hourly CSF samples were collected from 11 male combat veterans with PTSD and 8 healthy controls.57 Participants with PTSD had significantly higher CSF NE concentrations (0.55 ± 0.17 pmol/ml vs 0.39 ± 0.16 pmol/mL in the PTSD and control groups, respectively; F = 4.49, P < .05).57 Overall PTSD symptoms correlated significantly with CSF NE levels (r = 0.82, P <.005), and PTSD-specific symptoms such as avoidance (r = 0.79, P = .004). Intrusive thoughts (r = 0.57, P = .07) and hyperarousal (r = 0.54, P = .09) were also related.57 This relationship is unique; patients with PTSD with predominant depressive symptoms do not have elevated plasma NE levels.58
In the human brain, there are 3 main groups of NE receptors: alpha-1 receptors, alpha-2 receptors, and beta receptors.59 Alpha-1 receptors (alpha-1A, alpha-1B, and alpha-1D) are postsynaptic and mediate increase in inositol trisphosphate (IP3) and intracellular calcium (Ca2+). Alpha-2 receptors (alpha-2A, alpha-2B, alpha-2C) in the CNS are presynaptic autoreceptors and serve to reduce NE release. Beta receptors (beta-1, beta-2, beta-3) inhibit cyclic adenosine monophosphate (cAMP) production.59 The effects of inhibition of alpha or beta receptors are different. Inhibition of beta receptors is associated with depressive symptoms and depressive syndrome, inhibition of peripheral beta receptors is associated with reductions in anxiety (generally reduction of pulse, sweating, tremor),60 and inhibition of central alpha-1 receptors is associated with reduced PTSD symptoms.61
Choice of agents for PTSD-specific symptoms
As outlined in the Table,8 PTSD is characterized by 3 types of symptoms that are specific for PTSD. Trauma-focused psychotherapy62,63 and selective serotonin reuptake inhibitors (SSRIs)64 are considered first-line therapy for PTSD. Only
Continue to: Serotonin transporter promoter...
Serotonin transporter promoter region gene short-type variants, which possibly increase an individual’s predisposition to developing PTSD, may explain the abundance of depressive symptoms in this condition and the subdued response to antidepressants. Specifically, an anticipated preponderance of these alleles may be associated with poorer outcomes. Non-SSRI treatments, such as low-dose
On the other hand, animal models support antagonism of the postsynaptic alpha-1 adrenergic receptor of the CNS as a target for PTSD treatment.71 Although
Quetiapine might be another non-SSRI option for treating patients with PTSD. It is an antagonist with high affinity tothehistamine-1 receptor at low doses. Norquetiapine is an alpha-2 antagonist that increases brain NE levels. Both quetiapine and norquetiapine are alpha-1 antagonists. There is no beta blockade and no SSRI effect, but some 5HT2A blockade, which may be anxiolytic. Compared with placebo, an average quetiapine dose of 258 mg/d resulted in significantly greater reductions in Clinician-Administered PTSD Scale total score, re-experiencing score, and hyperarousal score.73
Unfortunately, none of the non-SSRI options have been adequately evaluated. For now, clinicians need to continue to use SSRIs, and researchers need to continue to explore mechanism-guided alternatives.
Bottom Line
Understanding the mechanisms of the pathophysiology of posttraumatic stress disorder (PTSD) may allow clinicians to “jump ahead” of clinical studies and FDA indications. Clinicians may reasonably use alpha-1 antagonists (eg, prazosin, quetiapine) for general clinical improvement of patients with PTSD, particularly for PTSD-specific symptoms. Using antihistamines to reduce anxiety (especially in patients who have the COMT Val158Met polymorphism) may also be reasonable.
Related Resources
- North CS, Hong BA, Downs DL. PTSD: a systematic approach to diagnosis and treatment. Current Psychiatry. 2018;17(4):35-43.
- Zhang Y, Ren R, Sanford LD, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2019; 67:225-231.
Drug Brand Names
Aripiprazole • Abilify
Citalopram • Celexa
Paroxetine • Paxil
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
1. Javidi H, Yadollahie M. Post-traumatic stress disorder. Int J Occup Environ Med. 2012;3(1):2-9.
2. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060.
4. Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626-632.
5. Cerda M, Sagdeo A, Johnson J, et al. Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord. 2010;126(1-2):14-38.
6. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. doi: 10.1038/nrdp.2015.57.
7. True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50(4):257-264.
8. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:271-280.
9. Reichmann F, Holzer P. Neuropeptide Y: a stressful review. Neuropeptides. 2016;55:99-109.
10. Yehuda R, Brand S, Yang RK. Plasma neuropeptide Y concentrations in combat exposed veterans: relationship to trauma exposure, recovery from PTSD, and coping. Biol Psychiatry. 2006;59(7):660-663.
11. Cohen H, Liu T, Kozlovsky N, et al. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350-363.
12. Donner J, Sipilä T, Ripatti S, et al. Support for involvement of glutamate decarboxylase 1 and neuropeptide Y in anxiety susceptibility. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(3):316-327.
13. Schmeltzer SN, Herman JP, Sah R. Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): a translational update. Exp Neurol. 2016;284(pt B):196-210.
14. Kautz M, Charney DS, Murrough JW. Neuropeptide Y, resilience, and PTSD therapeutics. Neurosci Lett. 2017;649:164-169.
15. Serova LI, Laukova M, Alaluf LG, et al. Intranasal neuropeptide Y reverses anxiety and depressive-like behavior impaired by single prolonged stress PTSD model. Eur Neuropsychopharmacol. 2014;24(1):142-147.
16. Sayed S, Van Dam NT, Horn SR, et al. A randomized dose-ranging study of neuropeptide Y in patients with posttraumatic stress disorder. Int J Neuropsychopharmacol. 2018;21(1):3-11.
17. Toth M, Flandreau EI, Deslauriers J, et al. Overexpression of forebrain CRH during early life increases trauma susceptibility in adulthood. Neuropsychopharmacology. 2016;41(6):1681-1690.
18. White S, Acierno R, Ruggiero KJ, et al. Association of CRHR1 variants and posttraumatic stress symptoms in hurricane exposed adults. J Anxiety Disord. 2013;27(7):678-683.
19. Wolf EJ, Mitchell KS, Logue MW, et al. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depress Anxiety. 2013;30(12):1161-1169.
20. Whitnall MH. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog Neurobiol. 1993;40(5):573-629.
21. Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008;65(2):190-200.
22. Tellew JE, Lanier M, Moorjani M, et al. Discovery of NBI-77860/GSK561679, a potent corticotropin-releasing factor (CRF1) receptor antagonist with improved pharmacokinetic properties. Bioorg Med Chem Lett. 2010;20(24):7259-7264.
23. Dunlop BW, Rothbaum BO, Binder EB, et al. Evaluation of a corticotropin releasing hormone type 1 receptor antagonist in women with posttraumatic stress disorder: study protocol for a randomized controlled trial. Trials. 2014;15:240. doi: 10.1186/1745-6215-15-240.
24. Jovanovic T, Duncan EJ, Kaye J, et al. Psychophysiological treatment outcomes: Corticotropin-releasing factor type 1 receptor antagonist increases inhibition of fear-potentiated startle in PTSD patients. Psychophysiology. 2019:e13356. doi: 10.1111/psyp.13356.
25. Dunlop BW, Binder EB, Iosifescu D, et al. Corticotropin-releasing factor receptor 1 antagonism is ineffective for women with posttraumatic stress disorder. Biol Psychiatry. 2017;82(12):866-874.
26. Pape JC, Carrillo-Roa T, Rothbaum BO, et al. DNA methylation levels are associated with CRF1 receptor antagonist treatment outcome in women with post-traumatic stress disorder. Clin Epigenetics. 2018;10(1):136. doi: 10.1186/s13148-018-0569-x.
27. Murrough JW, Charney DS. Corticotropin-releasing factor type 1 receptor antagonists for stress-related disorders: time to call it quits? Biol Psychiatry. 2017;82(12):858-860.
28. Leal G, Bramham CR, Duarte CB. BDNF and hippocampal synaptic plasticity. Vitam Horm. 2017;104:153-195.
29. Groves JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12:1079-1088.
30. Frustaci A, Pozzi G, Gianfagna F, et al. Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology. 2008;58(3-4):163-170.
31. Gatt JM, Nemeroff CB, Dobson-Stone C, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. 2009;14(7):681-695.
32. Ragen BJ, Seidel J, Chollak C, et al. Investigational drugs under development for the treatment of PTSD. Expert Opin Investig Drugs. 2015;24(5):659-672.
33. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
34. Murphy DL, Fox MA, Timpano KR, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55(6):932-960.
35. Luddington NS, Mandadapu A, Husk M, et al. Clinical implications of genetic variation in the serotonin transporter promoter region: a review. Prim Care Compan J Clin Psychiatry. 2009;11:(3):93-102.
36. Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21(3):135-139.
37. Liu Y, Garrett ME, Dennis MF, et al. An examination of the association between 5-HTTLPR, combat exposure, and PTSD diagnosis among U.S. veterans. PLoS One. 2015;10(3):e0119998. doi: 10.1371/journal.pone.0119998.
38. Mehta D, Voisey J, Bruenig D, et al. Transcriptome analysis reveals novel genes and immune networks dysregulated in veterans with PTSD. Brain Behav Immun. 2018;74:133-142. doi: 10.1016/j.bbi.2018.08.014.
39. Kilpatrick DG, Koenen KC, Ruggiero KJ, et al. The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. Am J Psychiatry. 2007;164(11):1693-1699.
40. Kolassa IT, Ertl V, Eckart C, et al. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. J Clin Psychiatry. 2010;71(5):543-547.
41. Bryant RA, Felmingham KL, Falconer EM, et al. Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder. Biol Psychiatry. 2010;67(12):1217-1219.
42. Mrazek DA, Rush AJ, Biernacka JM, et al. SLC6A4 variation and citalopram response. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):341-351.
43. Shiroma PR, Drews MS, Geske JR, et al. SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a Sequenced Treatment Alternatives to Relieve Depression (STAR*D) report. Am J Geriatr Psychiatry. 2014;22(11):1140-1148.
44. Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375-387.
45. Courtet P, Picot MC, Bellivier F, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biol Psychiatry. 2003;55(1):46-51.
46. Outhred T, Das P, Dobson-Stone C, et al. The impact of 5-HTTLPR on acute serotonin transporter blockade by escitalopram on emotion processing: Preliminary findings from a randomised, crossover fMRI study. Aust NZ J Psychiatry. 2014;48(12):1115-1125.
47. Lachman HM, Papolos DF, Saito T, et al. Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics. 1996;6(3):243-250.
48. Valente NL, Vallada H, Cordeiro Q, et al. Catechol-O-methyltransferase (COMT) val158met polymorphism as a risk factor for PTSD after urban violence. J Mol Neurosci. 2011;43(3):516-523.
49. van Rooij SJ, Stevens JS, Ely TD, et al. Childhood trauma and COMT genotype interact to increase hippocampal activation in resilient individuals. Front Psychiatry. 2016;7:156. doi: 10.3389/fpsyt.2016.00156.
50. Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neuroscience. 2013;7:10. doi: 10.3389/fnbeh.2013.00010.
51. Kolassa I, Kolassa S, Ertl V, et al. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-O-methyltransferase Val(158)Met polymorphism. Biol Psychiatry. 2010;67(4):304-308.
52. Bruder GE, Keilp JG, Xu H, et al. Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry. 2005;58(11):901-907.
53. Strawn JR, Geracioti TD Jr. Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder. Depress Anxiety. 2008;25(3):260-271.
54. Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(pt B):181-195.
55. Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929-933.
56. Roehrs TA, Roth T. Hyperarousal in insomnia and hypnotic dose escalation. Sleep Med. 2016;23:16-20.
57. Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF Norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158(8):1227-1230.
58. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44(1):56-63.
59. Molinoff PB. Alpha- and beta-adrenergic receptor subtypes properties, distribution and regulation. Drugs. 1984;28(suppl 2):1-15.
60. El-Mallakh RS. The use of beta-blockers in psychiatry. Res Staff Phys. 1989;35:49-52,59,62.
61. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
62. Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388.
63. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489-500.
64. Hoskins M, Pearce J, Bethell A, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93-100.
65. Belkin MR, Schwartz TL. Alpha-2 receptor agonists for the treatment of posttraumatic stress disorder. Drugs Context. 2015;4:212286. doi: 10.7573/dic.212286.
66. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837-1844.
67. Davidson JRT, Landerman LR, Farfel GM, et al. Characterizing the effects of sertraline in post-traumatic stress disorder. Psychol Med. 2002;32(4):661-670.
68. Hertzberg MA, Feldman ME, Beckham JC, et al. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry. 2000;12(2):101-105.
69. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711-720.
70. Mello MF, Costa MCP, Schoedl AF, et al. Aripiprazole in the treatment of posttraumatic stress disorder: an open-label trial. Rev Bras Psiquiatr. 2008;30(4):358-361.
71. Birnbaum S, Gobeske KT, Auerbach J, et al. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266-1274.
72. Ahmadpanah M, Sabzeiee P, Hosseini SM, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235-242.
73. Villarreal G, Hamner MB, Cañive JM, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205-1212.
Posttraumatic stress disorder (PTSD) occurs acutely and chronically in the aftermath of severe and potentially life-threatening trauma.1 The prevalence of PTSD varies significantly across countries and by type of trauma (Box1-7).
Box
In the general population, the prevalence of posttraumatic stress disorder (PTSD) varies from as low as 0.3% in China to as high as 6.1% in New Zealand1 and 6.8% in the United States.2 These rates are actually much lower than expected when one considers that severe trauma is experienced by 60.7% of men and 51.2% of women.3,4 Although the majority of individuals exposed to trauma experience emotional distress immediately following a traumatic event, most of them do not develop PTSD.5
It appears that the context of trauma is important: 12% to 15% of veterans experience PTSD, compared with 19% to 75% of crime victims and 80% of rape victims.1 The lifetime risk for PTSD is twice as high in women as it is in men,6 and genetic vulnerability may play a role. For example, twin studies showed that approximately 30% of the risk for PTSD may be mediated by genetic predisposition.7
Individuals who develop PTSD experience a wide range of symptoms.8 These can be categorized as PTSD-specific symptoms, or nonspecific symptoms. PTSD-specific symptoms include nightmares, flashbacks, dissociative reactions, hyperreactivity or hyperarousal, distress with reminders of trauma, and avoidance of trauma-related physical reminders and thoughts/feelings (Table8). Nonspecific symptoms include depressive and anxiety symptoms and significant problems in social, relationship, or work situations.8
While successful treatment necessitates taking all of these symptoms into account, understanding the pathophysiology of PTSD can inform a more focused and rational treatment approach. In this article, we describe some key pathophysiologic PTSD studies, and focus on PTSD-specific psychopathology to inform treatment.
Brain systems implicated in PTSD
Neuropeptide Y (NPY) is an anxiolytic endogenous peptide that has connections to the hypothalamic-pituitary-adrenal (HPA) axis. Its levels can be modulated by stress.9 Preclinical and clinical studies strongly support a potential role of NPY dysfunction in the pathophysiology of PTSD. Lower concentrations of NPY increase susceptibility to PTSD in combat veterans10 and in animal models.11 Three single-nucleotide polymorphisms (SNPs) appear to mediate this effect.12 These findings strongly support pharmaceutical targeting this system as a useful therapeutic approach.13,14 Indeed, intranasal NPY administered as a single dose reduces anxiety in animal models15 and in humans,16 but this work has not yet translated into clinical tools.
Corticotropin-releasing hormone receptor (CRHR1) gene. Corticotropin-releasing hormone has been implicated in PTSD.17 Corticotropin-releasing hormone receptors (CRHR) are important mediators in response to stress.18,19 They bind corticotropin-releasing hormone and contribute to the integration of autonomic, behavioral, and immune responses to stress.20 Single-nucleotide polymorphisms in the regulatory portion of the CRHR1 gene are associated with an increased risk for depression in adults who have a history of child abuse.21
The CRHR1 receptor antagonist GSK561679 is an investigational agent for the treatment of mood and anxiety disorders.22 In exploratory studies,23,24 GSK561679 was found to inhibit fear-potentiated startle in patients with PTSD, but not overall PTSD symptoms, although a subset of women with a specific genetic variant of the CRHR1 gene (rs110402) experienced significant benefit.25,26 This suggests that we must learn more about this system before we proceed.27
Brain-derived neurotrophic factor (BDNF). The synthesis of BDNF is influenced by neuronal activity in the brain and plays a role in synaptic transmission and plasticity.28 Brain-derived neurotrophic factor is encoded by the BDNF gene, which has been implicated in stress vulnerability.29 A common SNP in the pro-region of the human BDNF gene results in a valine-to-methionine substitution at the 66th amino acid (Val66Met). The functional Val66Met polymorphism may have a role in the risk of developing PTSD. However, not all studies support this finding. One study found that an SNP with a resulting Val66Met polymorphism is associated with adult PTSD symptoms after childhood abuse, while a meta-analysis of 7 studies did not confirm this.30,31 We need to learn more about BDNF before we proceed.32
Continue to: Serotonin transporter (5-HTT) gene
Serotonin transporter (5-HTT) gene. Serotonin transporter is a monoamine transporter protein that terminates the neurotransmitter signal by transporting serotonin from the synaptic cleft back into the presynaptic neuron. It is encoded by the SLC6A4 gene, which resides on the long arm of chromosome 17(17q11.1-q12). It is a large gene with 31 kilo bases and 14 separate exons (transcribed regions).33,34
This gene has several variants. The best-studied is a variation in the promoter region. A 44-bp insertion or deletion yields the “long” and “short” alleles, respectively. The proteins produced by the 2 alleles are identical, but the amount of expressed protein is different. The short allele (“S”) is associated with a nearly 50% reduction in 5-HTT expression in both homozygotes and heterozygotes.35 A greater incidence of serotonin transporter promoter region (5-HTTLPR) S has been found in individuals with PTSD compared with those without PTSD,36-38 and 5-HTTLPR S increases the risk of PTSD in individuals with low social support39 or after very few traumatic events.40 The short allele variant is also associated with depression in individuals who face adversity.35,41
The overrepresentation of the short form of 5-HTTLPR in individuals who develop PTSD may represent a potential problem with current treatment paradigms, in which an antidepressant is the first-line treatment, because this allele is associated with reduced response to antidepressants.42,43 More distressing is the possible association of this allele with increased suicide risk, particularly violent suicide44 or repeated suicide attempts.45
Furthermore, a functional MRI study of patients who were anxious revealed that in individuals with the short allele, administration of
Catechol-o-methyltransferase (COMT) is one of the enzymes that degrades catecholamines such as dopamine, epinephrine, and norepinephrine (NE).47 In humans, COMT protein is encoded by the COMT gene. This gene is associated with allelic variants; the best-studied of these is Val158Met. COMT Val158Met polymorphism (rs4860) has been linked to deficits in stress response and emotional resilience.48,49 Val158Met is associated with a 40% reduction in enzyme activity and slower catalysis of catecholamines, resulting in increases in catecholamines levels in the brain, which may increase the risk of developing PTSD.50 Individuals homozygous for this SNP (Met/Met) are highly susceptible to develop PTSD independently of the severity of the trauma they experienced.51 The Val158Met polymorphism may be associated with other abnormalities, such as cognitive problems with specific frontal cortical activity, and also with improved antidepressant response (valine homozygotes less responsive than methionine homozygotes).52 This gene is available on gene testing profiles.
Continue to: The role of norepinephrine in PTSD
The role of norepinephrine in PTSD
Perhaps the greatest advance in the understanding of the pathophysiology of PTSD relates to changes in brain NE. The HPA axis is responsible for coordinating the hormonal response to stress. Dysregulation of this axis and increased activity of the central and peripheral noradrenergic systems are usually observed in patients with PTSD.53 Several monoamine neurotransmitters are important in the regulation and function of the HPA axis. Norepinephrine plays a major role in stress.
The clinical PTSD-specific criteria are all descriptions of excessive noradrenergic tone.54 For example, hypervigilance and hyperstartle are clearly anticipated as evidence of NE stimulation. Flashbacks, particularly those that might be precipitated by environmental cues, also can be a manifestation of the vigilance induced by NE. Sleep disturbances (insomnia and nightmares) are present; insomnia is reported more often than nightmares.55 Increased catecholamine levels, particularly NE, are a feature of sleep disturbances associated with middle insomnia. Dreams can be remembered only if you wake up during dreaming. Catecholamines do not change the content of dreams, just recall.56
In a study of central noradrenergic tone in patients with PTSD, 6 hourly CSF samples were collected from 11 male combat veterans with PTSD and 8 healthy controls.57 Participants with PTSD had significantly higher CSF NE concentrations (0.55 ± 0.17 pmol/ml vs 0.39 ± 0.16 pmol/mL in the PTSD and control groups, respectively; F = 4.49, P < .05).57 Overall PTSD symptoms correlated significantly with CSF NE levels (r = 0.82, P <.005), and PTSD-specific symptoms such as avoidance (r = 0.79, P = .004). Intrusive thoughts (r = 0.57, P = .07) and hyperarousal (r = 0.54, P = .09) were also related.57 This relationship is unique; patients with PTSD with predominant depressive symptoms do not have elevated plasma NE levels.58
In the human brain, there are 3 main groups of NE receptors: alpha-1 receptors, alpha-2 receptors, and beta receptors.59 Alpha-1 receptors (alpha-1A, alpha-1B, and alpha-1D) are postsynaptic and mediate increase in inositol trisphosphate (IP3) and intracellular calcium (Ca2+). Alpha-2 receptors (alpha-2A, alpha-2B, alpha-2C) in the CNS are presynaptic autoreceptors and serve to reduce NE release. Beta receptors (beta-1, beta-2, beta-3) inhibit cyclic adenosine monophosphate (cAMP) production.59 The effects of inhibition of alpha or beta receptors are different. Inhibition of beta receptors is associated with depressive symptoms and depressive syndrome, inhibition of peripheral beta receptors is associated with reductions in anxiety (generally reduction of pulse, sweating, tremor),60 and inhibition of central alpha-1 receptors is associated with reduced PTSD symptoms.61
Choice of agents for PTSD-specific symptoms
As outlined in the Table,8 PTSD is characterized by 3 types of symptoms that are specific for PTSD. Trauma-focused psychotherapy62,63 and selective serotonin reuptake inhibitors (SSRIs)64 are considered first-line therapy for PTSD. Only
Continue to: Serotonin transporter promoter...
Serotonin transporter promoter region gene short-type variants, which possibly increase an individual’s predisposition to developing PTSD, may explain the abundance of depressive symptoms in this condition and the subdued response to antidepressants. Specifically, an anticipated preponderance of these alleles may be associated with poorer outcomes. Non-SSRI treatments, such as low-dose
On the other hand, animal models support antagonism of the postsynaptic alpha-1 adrenergic receptor of the CNS as a target for PTSD treatment.71 Although
Quetiapine might be another non-SSRI option for treating patients with PTSD. It is an antagonist with high affinity tothehistamine-1 receptor at low doses. Norquetiapine is an alpha-2 antagonist that increases brain NE levels. Both quetiapine and norquetiapine are alpha-1 antagonists. There is no beta blockade and no SSRI effect, but some 5HT2A blockade, which may be anxiolytic. Compared with placebo, an average quetiapine dose of 258 mg/d resulted in significantly greater reductions in Clinician-Administered PTSD Scale total score, re-experiencing score, and hyperarousal score.73
Unfortunately, none of the non-SSRI options have been adequately evaluated. For now, clinicians need to continue to use SSRIs, and researchers need to continue to explore mechanism-guided alternatives.
Bottom Line
Understanding the mechanisms of the pathophysiology of posttraumatic stress disorder (PTSD) may allow clinicians to “jump ahead” of clinical studies and FDA indications. Clinicians may reasonably use alpha-1 antagonists (eg, prazosin, quetiapine) for general clinical improvement of patients with PTSD, particularly for PTSD-specific symptoms. Using antihistamines to reduce anxiety (especially in patients who have the COMT Val158Met polymorphism) may also be reasonable.
Related Resources
- North CS, Hong BA, Downs DL. PTSD: a systematic approach to diagnosis and treatment. Current Psychiatry. 2018;17(4):35-43.
- Zhang Y, Ren R, Sanford LD, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2019; 67:225-231.
Drug Brand Names
Aripiprazole • Abilify
Citalopram • Celexa
Paroxetine • Paxil
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
Posttraumatic stress disorder (PTSD) occurs acutely and chronically in the aftermath of severe and potentially life-threatening trauma.1 The prevalence of PTSD varies significantly across countries and by type of trauma (Box1-7).
Box
In the general population, the prevalence of posttraumatic stress disorder (PTSD) varies from as low as 0.3% in China to as high as 6.1% in New Zealand1 and 6.8% in the United States.2 These rates are actually much lower than expected when one considers that severe trauma is experienced by 60.7% of men and 51.2% of women.3,4 Although the majority of individuals exposed to trauma experience emotional distress immediately following a traumatic event, most of them do not develop PTSD.5
It appears that the context of trauma is important: 12% to 15% of veterans experience PTSD, compared with 19% to 75% of crime victims and 80% of rape victims.1 The lifetime risk for PTSD is twice as high in women as it is in men,6 and genetic vulnerability may play a role. For example, twin studies showed that approximately 30% of the risk for PTSD may be mediated by genetic predisposition.7
Individuals who develop PTSD experience a wide range of symptoms.8 These can be categorized as PTSD-specific symptoms, or nonspecific symptoms. PTSD-specific symptoms include nightmares, flashbacks, dissociative reactions, hyperreactivity or hyperarousal, distress with reminders of trauma, and avoidance of trauma-related physical reminders and thoughts/feelings (Table8). Nonspecific symptoms include depressive and anxiety symptoms and significant problems in social, relationship, or work situations.8
While successful treatment necessitates taking all of these symptoms into account, understanding the pathophysiology of PTSD can inform a more focused and rational treatment approach. In this article, we describe some key pathophysiologic PTSD studies, and focus on PTSD-specific psychopathology to inform treatment.
Brain systems implicated in PTSD
Neuropeptide Y (NPY) is an anxiolytic endogenous peptide that has connections to the hypothalamic-pituitary-adrenal (HPA) axis. Its levels can be modulated by stress.9 Preclinical and clinical studies strongly support a potential role of NPY dysfunction in the pathophysiology of PTSD. Lower concentrations of NPY increase susceptibility to PTSD in combat veterans10 and in animal models.11 Three single-nucleotide polymorphisms (SNPs) appear to mediate this effect.12 These findings strongly support pharmaceutical targeting this system as a useful therapeutic approach.13,14 Indeed, intranasal NPY administered as a single dose reduces anxiety in animal models15 and in humans,16 but this work has not yet translated into clinical tools.
Corticotropin-releasing hormone receptor (CRHR1) gene. Corticotropin-releasing hormone has been implicated in PTSD.17 Corticotropin-releasing hormone receptors (CRHR) are important mediators in response to stress.18,19 They bind corticotropin-releasing hormone and contribute to the integration of autonomic, behavioral, and immune responses to stress.20 Single-nucleotide polymorphisms in the regulatory portion of the CRHR1 gene are associated with an increased risk for depression in adults who have a history of child abuse.21
The CRHR1 receptor antagonist GSK561679 is an investigational agent for the treatment of mood and anxiety disorders.22 In exploratory studies,23,24 GSK561679 was found to inhibit fear-potentiated startle in patients with PTSD, but not overall PTSD symptoms, although a subset of women with a specific genetic variant of the CRHR1 gene (rs110402) experienced significant benefit.25,26 This suggests that we must learn more about this system before we proceed.27
Brain-derived neurotrophic factor (BDNF). The synthesis of BDNF is influenced by neuronal activity in the brain and plays a role in synaptic transmission and plasticity.28 Brain-derived neurotrophic factor is encoded by the BDNF gene, which has been implicated in stress vulnerability.29 A common SNP in the pro-region of the human BDNF gene results in a valine-to-methionine substitution at the 66th amino acid (Val66Met). The functional Val66Met polymorphism may have a role in the risk of developing PTSD. However, not all studies support this finding. One study found that an SNP with a resulting Val66Met polymorphism is associated with adult PTSD symptoms after childhood abuse, while a meta-analysis of 7 studies did not confirm this.30,31 We need to learn more about BDNF before we proceed.32
Continue to: Serotonin transporter (5-HTT) gene
Serotonin transporter (5-HTT) gene. Serotonin transporter is a monoamine transporter protein that terminates the neurotransmitter signal by transporting serotonin from the synaptic cleft back into the presynaptic neuron. It is encoded by the SLC6A4 gene, which resides on the long arm of chromosome 17(17q11.1-q12). It is a large gene with 31 kilo bases and 14 separate exons (transcribed regions).33,34
This gene has several variants. The best-studied is a variation in the promoter region. A 44-bp insertion or deletion yields the “long” and “short” alleles, respectively. The proteins produced by the 2 alleles are identical, but the amount of expressed protein is different. The short allele (“S”) is associated with a nearly 50% reduction in 5-HTT expression in both homozygotes and heterozygotes.35 A greater incidence of serotonin transporter promoter region (5-HTTLPR) S has been found in individuals with PTSD compared with those without PTSD,36-38 and 5-HTTLPR S increases the risk of PTSD in individuals with low social support39 or after very few traumatic events.40 The short allele variant is also associated with depression in individuals who face adversity.35,41
The overrepresentation of the short form of 5-HTTLPR in individuals who develop PTSD may represent a potential problem with current treatment paradigms, in which an antidepressant is the first-line treatment, because this allele is associated with reduced response to antidepressants.42,43 More distressing is the possible association of this allele with increased suicide risk, particularly violent suicide44 or repeated suicide attempts.45
Furthermore, a functional MRI study of patients who were anxious revealed that in individuals with the short allele, administration of
Catechol-o-methyltransferase (COMT) is one of the enzymes that degrades catecholamines such as dopamine, epinephrine, and norepinephrine (NE).47 In humans, COMT protein is encoded by the COMT gene. This gene is associated with allelic variants; the best-studied of these is Val158Met. COMT Val158Met polymorphism (rs4860) has been linked to deficits in stress response and emotional resilience.48,49 Val158Met is associated with a 40% reduction in enzyme activity and slower catalysis of catecholamines, resulting in increases in catecholamines levels in the brain, which may increase the risk of developing PTSD.50 Individuals homozygous for this SNP (Met/Met) are highly susceptible to develop PTSD independently of the severity of the trauma they experienced.51 The Val158Met polymorphism may be associated with other abnormalities, such as cognitive problems with specific frontal cortical activity, and also with improved antidepressant response (valine homozygotes less responsive than methionine homozygotes).52 This gene is available on gene testing profiles.
Continue to: The role of norepinephrine in PTSD
The role of norepinephrine in PTSD
Perhaps the greatest advance in the understanding of the pathophysiology of PTSD relates to changes in brain NE. The HPA axis is responsible for coordinating the hormonal response to stress. Dysregulation of this axis and increased activity of the central and peripheral noradrenergic systems are usually observed in patients with PTSD.53 Several monoamine neurotransmitters are important in the regulation and function of the HPA axis. Norepinephrine plays a major role in stress.
The clinical PTSD-specific criteria are all descriptions of excessive noradrenergic tone.54 For example, hypervigilance and hyperstartle are clearly anticipated as evidence of NE stimulation. Flashbacks, particularly those that might be precipitated by environmental cues, also can be a manifestation of the vigilance induced by NE. Sleep disturbances (insomnia and nightmares) are present; insomnia is reported more often than nightmares.55 Increased catecholamine levels, particularly NE, are a feature of sleep disturbances associated with middle insomnia. Dreams can be remembered only if you wake up during dreaming. Catecholamines do not change the content of dreams, just recall.56
In a study of central noradrenergic tone in patients with PTSD, 6 hourly CSF samples were collected from 11 male combat veterans with PTSD and 8 healthy controls.57 Participants with PTSD had significantly higher CSF NE concentrations (0.55 ± 0.17 pmol/ml vs 0.39 ± 0.16 pmol/mL in the PTSD and control groups, respectively; F = 4.49, P < .05).57 Overall PTSD symptoms correlated significantly with CSF NE levels (r = 0.82, P <.005), and PTSD-specific symptoms such as avoidance (r = 0.79, P = .004). Intrusive thoughts (r = 0.57, P = .07) and hyperarousal (r = 0.54, P = .09) were also related.57 This relationship is unique; patients with PTSD with predominant depressive symptoms do not have elevated plasma NE levels.58
In the human brain, there are 3 main groups of NE receptors: alpha-1 receptors, alpha-2 receptors, and beta receptors.59 Alpha-1 receptors (alpha-1A, alpha-1B, and alpha-1D) are postsynaptic and mediate increase in inositol trisphosphate (IP3) and intracellular calcium (Ca2+). Alpha-2 receptors (alpha-2A, alpha-2B, alpha-2C) in the CNS are presynaptic autoreceptors and serve to reduce NE release. Beta receptors (beta-1, beta-2, beta-3) inhibit cyclic adenosine monophosphate (cAMP) production.59 The effects of inhibition of alpha or beta receptors are different. Inhibition of beta receptors is associated with depressive symptoms and depressive syndrome, inhibition of peripheral beta receptors is associated with reductions in anxiety (generally reduction of pulse, sweating, tremor),60 and inhibition of central alpha-1 receptors is associated with reduced PTSD symptoms.61
Choice of agents for PTSD-specific symptoms
As outlined in the Table,8 PTSD is characterized by 3 types of symptoms that are specific for PTSD. Trauma-focused psychotherapy62,63 and selective serotonin reuptake inhibitors (SSRIs)64 are considered first-line therapy for PTSD. Only
Continue to: Serotonin transporter promoter...
Serotonin transporter promoter region gene short-type variants, which possibly increase an individual’s predisposition to developing PTSD, may explain the abundance of depressive symptoms in this condition and the subdued response to antidepressants. Specifically, an anticipated preponderance of these alleles may be associated with poorer outcomes. Non-SSRI treatments, such as low-dose
On the other hand, animal models support antagonism of the postsynaptic alpha-1 adrenergic receptor of the CNS as a target for PTSD treatment.71 Although
Quetiapine might be another non-SSRI option for treating patients with PTSD. It is an antagonist with high affinity tothehistamine-1 receptor at low doses. Norquetiapine is an alpha-2 antagonist that increases brain NE levels. Both quetiapine and norquetiapine are alpha-1 antagonists. There is no beta blockade and no SSRI effect, but some 5HT2A blockade, which may be anxiolytic. Compared with placebo, an average quetiapine dose of 258 mg/d resulted in significantly greater reductions in Clinician-Administered PTSD Scale total score, re-experiencing score, and hyperarousal score.73
Unfortunately, none of the non-SSRI options have been adequately evaluated. For now, clinicians need to continue to use SSRIs, and researchers need to continue to explore mechanism-guided alternatives.
Bottom Line
Understanding the mechanisms of the pathophysiology of posttraumatic stress disorder (PTSD) may allow clinicians to “jump ahead” of clinical studies and FDA indications. Clinicians may reasonably use alpha-1 antagonists (eg, prazosin, quetiapine) for general clinical improvement of patients with PTSD, particularly for PTSD-specific symptoms. Using antihistamines to reduce anxiety (especially in patients who have the COMT Val158Met polymorphism) may also be reasonable.
Related Resources
- North CS, Hong BA, Downs DL. PTSD: a systematic approach to diagnosis and treatment. Current Psychiatry. 2018;17(4):35-43.
- Zhang Y, Ren R, Sanford LD, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2019; 67:225-231.
Drug Brand Names
Aripiprazole • Abilify
Citalopram • Celexa
Paroxetine • Paxil
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
1. Javidi H, Yadollahie M. Post-traumatic stress disorder. Int J Occup Environ Med. 2012;3(1):2-9.
2. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060.
4. Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626-632.
5. Cerda M, Sagdeo A, Johnson J, et al. Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord. 2010;126(1-2):14-38.
6. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. doi: 10.1038/nrdp.2015.57.
7. True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50(4):257-264.
8. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:271-280.
9. Reichmann F, Holzer P. Neuropeptide Y: a stressful review. Neuropeptides. 2016;55:99-109.
10. Yehuda R, Brand S, Yang RK. Plasma neuropeptide Y concentrations in combat exposed veterans: relationship to trauma exposure, recovery from PTSD, and coping. Biol Psychiatry. 2006;59(7):660-663.
11. Cohen H, Liu T, Kozlovsky N, et al. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350-363.
12. Donner J, Sipilä T, Ripatti S, et al. Support for involvement of glutamate decarboxylase 1 and neuropeptide Y in anxiety susceptibility. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(3):316-327.
13. Schmeltzer SN, Herman JP, Sah R. Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): a translational update. Exp Neurol. 2016;284(pt B):196-210.
14. Kautz M, Charney DS, Murrough JW. Neuropeptide Y, resilience, and PTSD therapeutics. Neurosci Lett. 2017;649:164-169.
15. Serova LI, Laukova M, Alaluf LG, et al. Intranasal neuropeptide Y reverses anxiety and depressive-like behavior impaired by single prolonged stress PTSD model. Eur Neuropsychopharmacol. 2014;24(1):142-147.
16. Sayed S, Van Dam NT, Horn SR, et al. A randomized dose-ranging study of neuropeptide Y in patients with posttraumatic stress disorder. Int J Neuropsychopharmacol. 2018;21(1):3-11.
17. Toth M, Flandreau EI, Deslauriers J, et al. Overexpression of forebrain CRH during early life increases trauma susceptibility in adulthood. Neuropsychopharmacology. 2016;41(6):1681-1690.
18. White S, Acierno R, Ruggiero KJ, et al. Association of CRHR1 variants and posttraumatic stress symptoms in hurricane exposed adults. J Anxiety Disord. 2013;27(7):678-683.
19. Wolf EJ, Mitchell KS, Logue MW, et al. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depress Anxiety. 2013;30(12):1161-1169.
20. Whitnall MH. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog Neurobiol. 1993;40(5):573-629.
21. Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008;65(2):190-200.
22. Tellew JE, Lanier M, Moorjani M, et al. Discovery of NBI-77860/GSK561679, a potent corticotropin-releasing factor (CRF1) receptor antagonist with improved pharmacokinetic properties. Bioorg Med Chem Lett. 2010;20(24):7259-7264.
23. Dunlop BW, Rothbaum BO, Binder EB, et al. Evaluation of a corticotropin releasing hormone type 1 receptor antagonist in women with posttraumatic stress disorder: study protocol for a randomized controlled trial. Trials. 2014;15:240. doi: 10.1186/1745-6215-15-240.
24. Jovanovic T, Duncan EJ, Kaye J, et al. Psychophysiological treatment outcomes: Corticotropin-releasing factor type 1 receptor antagonist increases inhibition of fear-potentiated startle in PTSD patients. Psychophysiology. 2019:e13356. doi: 10.1111/psyp.13356.
25. Dunlop BW, Binder EB, Iosifescu D, et al. Corticotropin-releasing factor receptor 1 antagonism is ineffective for women with posttraumatic stress disorder. Biol Psychiatry. 2017;82(12):866-874.
26. Pape JC, Carrillo-Roa T, Rothbaum BO, et al. DNA methylation levels are associated with CRF1 receptor antagonist treatment outcome in women with post-traumatic stress disorder. Clin Epigenetics. 2018;10(1):136. doi: 10.1186/s13148-018-0569-x.
27. Murrough JW, Charney DS. Corticotropin-releasing factor type 1 receptor antagonists for stress-related disorders: time to call it quits? Biol Psychiatry. 2017;82(12):858-860.
28. Leal G, Bramham CR, Duarte CB. BDNF and hippocampal synaptic plasticity. Vitam Horm. 2017;104:153-195.
29. Groves JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12:1079-1088.
30. Frustaci A, Pozzi G, Gianfagna F, et al. Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology. 2008;58(3-4):163-170.
31. Gatt JM, Nemeroff CB, Dobson-Stone C, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. 2009;14(7):681-695.
32. Ragen BJ, Seidel J, Chollak C, et al. Investigational drugs under development for the treatment of PTSD. Expert Opin Investig Drugs. 2015;24(5):659-672.
33. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
34. Murphy DL, Fox MA, Timpano KR, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55(6):932-960.
35. Luddington NS, Mandadapu A, Husk M, et al. Clinical implications of genetic variation in the serotonin transporter promoter region: a review. Prim Care Compan J Clin Psychiatry. 2009;11:(3):93-102.
36. Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21(3):135-139.
37. Liu Y, Garrett ME, Dennis MF, et al. An examination of the association between 5-HTTLPR, combat exposure, and PTSD diagnosis among U.S. veterans. PLoS One. 2015;10(3):e0119998. doi: 10.1371/journal.pone.0119998.
38. Mehta D, Voisey J, Bruenig D, et al. Transcriptome analysis reveals novel genes and immune networks dysregulated in veterans with PTSD. Brain Behav Immun. 2018;74:133-142. doi: 10.1016/j.bbi.2018.08.014.
39. Kilpatrick DG, Koenen KC, Ruggiero KJ, et al. The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. Am J Psychiatry. 2007;164(11):1693-1699.
40. Kolassa IT, Ertl V, Eckart C, et al. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. J Clin Psychiatry. 2010;71(5):543-547.
41. Bryant RA, Felmingham KL, Falconer EM, et al. Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder. Biol Psychiatry. 2010;67(12):1217-1219.
42. Mrazek DA, Rush AJ, Biernacka JM, et al. SLC6A4 variation and citalopram response. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):341-351.
43. Shiroma PR, Drews MS, Geske JR, et al. SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a Sequenced Treatment Alternatives to Relieve Depression (STAR*D) report. Am J Geriatr Psychiatry. 2014;22(11):1140-1148.
44. Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375-387.
45. Courtet P, Picot MC, Bellivier F, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biol Psychiatry. 2003;55(1):46-51.
46. Outhred T, Das P, Dobson-Stone C, et al. The impact of 5-HTTLPR on acute serotonin transporter blockade by escitalopram on emotion processing: Preliminary findings from a randomised, crossover fMRI study. Aust NZ J Psychiatry. 2014;48(12):1115-1125.
47. Lachman HM, Papolos DF, Saito T, et al. Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics. 1996;6(3):243-250.
48. Valente NL, Vallada H, Cordeiro Q, et al. Catechol-O-methyltransferase (COMT) val158met polymorphism as a risk factor for PTSD after urban violence. J Mol Neurosci. 2011;43(3):516-523.
49. van Rooij SJ, Stevens JS, Ely TD, et al. Childhood trauma and COMT genotype interact to increase hippocampal activation in resilient individuals. Front Psychiatry. 2016;7:156. doi: 10.3389/fpsyt.2016.00156.
50. Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neuroscience. 2013;7:10. doi: 10.3389/fnbeh.2013.00010.
51. Kolassa I, Kolassa S, Ertl V, et al. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-O-methyltransferase Val(158)Met polymorphism. Biol Psychiatry. 2010;67(4):304-308.
52. Bruder GE, Keilp JG, Xu H, et al. Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry. 2005;58(11):901-907.
53. Strawn JR, Geracioti TD Jr. Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder. Depress Anxiety. 2008;25(3):260-271.
54. Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(pt B):181-195.
55. Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929-933.
56. Roehrs TA, Roth T. Hyperarousal in insomnia and hypnotic dose escalation. Sleep Med. 2016;23:16-20.
57. Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF Norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158(8):1227-1230.
58. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44(1):56-63.
59. Molinoff PB. Alpha- and beta-adrenergic receptor subtypes properties, distribution and regulation. Drugs. 1984;28(suppl 2):1-15.
60. El-Mallakh RS. The use of beta-blockers in psychiatry. Res Staff Phys. 1989;35:49-52,59,62.
61. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
62. Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388.
63. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489-500.
64. Hoskins M, Pearce J, Bethell A, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93-100.
65. Belkin MR, Schwartz TL. Alpha-2 receptor agonists for the treatment of posttraumatic stress disorder. Drugs Context. 2015;4:212286. doi: 10.7573/dic.212286.
66. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837-1844.
67. Davidson JRT, Landerman LR, Farfel GM, et al. Characterizing the effects of sertraline in post-traumatic stress disorder. Psychol Med. 2002;32(4):661-670.
68. Hertzberg MA, Feldman ME, Beckham JC, et al. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry. 2000;12(2):101-105.
69. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711-720.
70. Mello MF, Costa MCP, Schoedl AF, et al. Aripiprazole in the treatment of posttraumatic stress disorder: an open-label trial. Rev Bras Psiquiatr. 2008;30(4):358-361.
71. Birnbaum S, Gobeske KT, Auerbach J, et al. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266-1274.
72. Ahmadpanah M, Sabzeiee P, Hosseini SM, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235-242.
73. Villarreal G, Hamner MB, Cañive JM, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205-1212.
1. Javidi H, Yadollahie M. Post-traumatic stress disorder. Int J Occup Environ Med. 2012;3(1):2-9.
2. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060.
4. Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626-632.
5. Cerda M, Sagdeo A, Johnson J, et al. Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord. 2010;126(1-2):14-38.
6. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. doi: 10.1038/nrdp.2015.57.
7. True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50(4):257-264.
8. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:271-280.
9. Reichmann F, Holzer P. Neuropeptide Y: a stressful review. Neuropeptides. 2016;55:99-109.
10. Yehuda R, Brand S, Yang RK. Plasma neuropeptide Y concentrations in combat exposed veterans: relationship to trauma exposure, recovery from PTSD, and coping. Biol Psychiatry. 2006;59(7):660-663.
11. Cohen H, Liu T, Kozlovsky N, et al. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350-363.
12. Donner J, Sipilä T, Ripatti S, et al. Support for involvement of glutamate decarboxylase 1 and neuropeptide Y in anxiety susceptibility. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(3):316-327.
13. Schmeltzer SN, Herman JP, Sah R. Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): a translational update. Exp Neurol. 2016;284(pt B):196-210.
14. Kautz M, Charney DS, Murrough JW. Neuropeptide Y, resilience, and PTSD therapeutics. Neurosci Lett. 2017;649:164-169.
15. Serova LI, Laukova M, Alaluf LG, et al. Intranasal neuropeptide Y reverses anxiety and depressive-like behavior impaired by single prolonged stress PTSD model. Eur Neuropsychopharmacol. 2014;24(1):142-147.
16. Sayed S, Van Dam NT, Horn SR, et al. A randomized dose-ranging study of neuropeptide Y in patients with posttraumatic stress disorder. Int J Neuropsychopharmacol. 2018;21(1):3-11.
17. Toth M, Flandreau EI, Deslauriers J, et al. Overexpression of forebrain CRH during early life increases trauma susceptibility in adulthood. Neuropsychopharmacology. 2016;41(6):1681-1690.
18. White S, Acierno R, Ruggiero KJ, et al. Association of CRHR1 variants and posttraumatic stress symptoms in hurricane exposed adults. J Anxiety Disord. 2013;27(7):678-683.
19. Wolf EJ, Mitchell KS, Logue MW, et al. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depress Anxiety. 2013;30(12):1161-1169.
20. Whitnall MH. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog Neurobiol. 1993;40(5):573-629.
21. Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008;65(2):190-200.
22. Tellew JE, Lanier M, Moorjani M, et al. Discovery of NBI-77860/GSK561679, a potent corticotropin-releasing factor (CRF1) receptor antagonist with improved pharmacokinetic properties. Bioorg Med Chem Lett. 2010;20(24):7259-7264.
23. Dunlop BW, Rothbaum BO, Binder EB, et al. Evaluation of a corticotropin releasing hormone type 1 receptor antagonist in women with posttraumatic stress disorder: study protocol for a randomized controlled trial. Trials. 2014;15:240. doi: 10.1186/1745-6215-15-240.
24. Jovanovic T, Duncan EJ, Kaye J, et al. Psychophysiological treatment outcomes: Corticotropin-releasing factor type 1 receptor antagonist increases inhibition of fear-potentiated startle in PTSD patients. Psychophysiology. 2019:e13356. doi: 10.1111/psyp.13356.
25. Dunlop BW, Binder EB, Iosifescu D, et al. Corticotropin-releasing factor receptor 1 antagonism is ineffective for women with posttraumatic stress disorder. Biol Psychiatry. 2017;82(12):866-874.
26. Pape JC, Carrillo-Roa T, Rothbaum BO, et al. DNA methylation levels are associated with CRF1 receptor antagonist treatment outcome in women with post-traumatic stress disorder. Clin Epigenetics. 2018;10(1):136. doi: 10.1186/s13148-018-0569-x.
27. Murrough JW, Charney DS. Corticotropin-releasing factor type 1 receptor antagonists for stress-related disorders: time to call it quits? Biol Psychiatry. 2017;82(12):858-860.
28. Leal G, Bramham CR, Duarte CB. BDNF and hippocampal synaptic plasticity. Vitam Horm. 2017;104:153-195.
29. Groves JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12:1079-1088.
30. Frustaci A, Pozzi G, Gianfagna F, et al. Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology. 2008;58(3-4):163-170.
31. Gatt JM, Nemeroff CB, Dobson-Stone C, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. 2009;14(7):681-695.
32. Ragen BJ, Seidel J, Chollak C, et al. Investigational drugs under development for the treatment of PTSD. Expert Opin Investig Drugs. 2015;24(5):659-672.
33. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
34. Murphy DL, Fox MA, Timpano KR, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55(6):932-960.
35. Luddington NS, Mandadapu A, Husk M, et al. Clinical implications of genetic variation in the serotonin transporter promoter region: a review. Prim Care Compan J Clin Psychiatry. 2009;11:(3):93-102.
36. Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21(3):135-139.
37. Liu Y, Garrett ME, Dennis MF, et al. An examination of the association between 5-HTTLPR, combat exposure, and PTSD diagnosis among U.S. veterans. PLoS One. 2015;10(3):e0119998. doi: 10.1371/journal.pone.0119998.
38. Mehta D, Voisey J, Bruenig D, et al. Transcriptome analysis reveals novel genes and immune networks dysregulated in veterans with PTSD. Brain Behav Immun. 2018;74:133-142. doi: 10.1016/j.bbi.2018.08.014.
39. Kilpatrick DG, Koenen KC, Ruggiero KJ, et al. The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. Am J Psychiatry. 2007;164(11):1693-1699.
40. Kolassa IT, Ertl V, Eckart C, et al. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. J Clin Psychiatry. 2010;71(5):543-547.
41. Bryant RA, Felmingham KL, Falconer EM, et al. Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder. Biol Psychiatry. 2010;67(12):1217-1219.
42. Mrazek DA, Rush AJ, Biernacka JM, et al. SLC6A4 variation and citalopram response. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):341-351.
43. Shiroma PR, Drews MS, Geske JR, et al. SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a Sequenced Treatment Alternatives to Relieve Depression (STAR*D) report. Am J Geriatr Psychiatry. 2014;22(11):1140-1148.
44. Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375-387.
45. Courtet P, Picot MC, Bellivier F, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biol Psychiatry. 2003;55(1):46-51.
46. Outhred T, Das P, Dobson-Stone C, et al. The impact of 5-HTTLPR on acute serotonin transporter blockade by escitalopram on emotion processing: Preliminary findings from a randomised, crossover fMRI study. Aust NZ J Psychiatry. 2014;48(12):1115-1125.
47. Lachman HM, Papolos DF, Saito T, et al. Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics. 1996;6(3):243-250.
48. Valente NL, Vallada H, Cordeiro Q, et al. Catechol-O-methyltransferase (COMT) val158met polymorphism as a risk factor for PTSD after urban violence. J Mol Neurosci. 2011;43(3):516-523.
49. van Rooij SJ, Stevens JS, Ely TD, et al. Childhood trauma and COMT genotype interact to increase hippocampal activation in resilient individuals. Front Psychiatry. 2016;7:156. doi: 10.3389/fpsyt.2016.00156.
50. Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neuroscience. 2013;7:10. doi: 10.3389/fnbeh.2013.00010.
51. Kolassa I, Kolassa S, Ertl V, et al. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-O-methyltransferase Val(158)Met polymorphism. Biol Psychiatry. 2010;67(4):304-308.
52. Bruder GE, Keilp JG, Xu H, et al. Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry. 2005;58(11):901-907.
53. Strawn JR, Geracioti TD Jr. Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder. Depress Anxiety. 2008;25(3):260-271.
54. Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(pt B):181-195.
55. Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929-933.
56. Roehrs TA, Roth T. Hyperarousal in insomnia and hypnotic dose escalation. Sleep Med. 2016;23:16-20.
57. Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF Norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158(8):1227-1230.
58. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44(1):56-63.
59. Molinoff PB. Alpha- and beta-adrenergic receptor subtypes properties, distribution and regulation. Drugs. 1984;28(suppl 2):1-15.
60. El-Mallakh RS. The use of beta-blockers in psychiatry. Res Staff Phys. 1989;35:49-52,59,62.
61. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
62. Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388.
63. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489-500.
64. Hoskins M, Pearce J, Bethell A, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93-100.
65. Belkin MR, Schwartz TL. Alpha-2 receptor agonists for the treatment of posttraumatic stress disorder. Drugs Context. 2015;4:212286. doi: 10.7573/dic.212286.
66. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837-1844.
67. Davidson JRT, Landerman LR, Farfel GM, et al. Characterizing the effects of sertraline in post-traumatic stress disorder. Psychol Med. 2002;32(4):661-670.
68. Hertzberg MA, Feldman ME, Beckham JC, et al. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry. 2000;12(2):101-105.
69. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711-720.
70. Mello MF, Costa MCP, Schoedl AF, et al. Aripiprazole in the treatment of posttraumatic stress disorder: an open-label trial. Rev Bras Psiquiatr. 2008;30(4):358-361.
71. Birnbaum S, Gobeske KT, Auerbach J, et al. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266-1274.
72. Ahmadpanah M, Sabzeiee P, Hosseini SM, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235-242.
73. Villarreal G, Hamner MB, Cañive JM, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205-1212.