User login
Prospective cohort study of hospitalized adults with advanced cancer: Associations between complications, comorbidity, and utilization
Of the major chronic conditions that affect adult patients in the United States, cancer accounts for the highest levels of per capita spending.1 Cost growth for cancer treatment has been substantial and persistent, from $72 billion in 2004 to $125 billion in 2010, and is projected to increase to $173 billion by 2020.2 Thirty-five percent of US direct medical cancer costs are attributable to inpatient hospital stays.3 Policy responses that can provide financially sustainable, high-quality models of care for patients with advanced cancer and other serious illness are urgently sought.4-7
Patterns and levels of resource utilization in providing healthcare to patients with serious illness reflect not only treatment choices but a complex set of relationships among demographic, clinical, and system factors.8-10 Patient-level factors previously identified as potentially significant drivers of resource utilization among cancer populations specifically include age,11 sex,12 primary diagnosis,13 and comorbidities.11 Among end-of-life populations, significant associations have been found between cost and ethnicity,14 socioeconomic status,15 advance directive status,16 insurance status,16 and functional status.17
Evidence on factors strongly associated with cost of hospital admission for patients with advanced cancer can therefore inform provision and planning of healthcare. For example, when a specific diagnosis or clinical condition is found to be associated with high cost, then improving coordination and provision of care for this patient group may reduce avoidable utilization. Determining associations between sociodemographics and hospital care cost can help in identifying possible disparities in care, such as those that might occur when care differs by race, class, or insurance status.
We conducted the Palliative Care for Cancer (PC4C) study, a prospective multisite cohort study of the palliative care consultation team intervention for hospitalized adults with advanced cancer.18,19 In our primary analysis, we controlled for receipt of palliative care and analyzed a rich patient-reported dataset to examine associations between hospital care cost, and sociodemographic factors, clinical variables, and prior healthcare utilization. The results provide evidence regarding the factors most associated with the cost of hospital-based cancer care.
METHODS
Design, Setting, Participants, Data Sources
The PC4C study has been described in detail by authors who estimated the impact of specialist palliative care consultation teams on hospitalization cost.19-21 We prospectively collected sociodemographic, clinical, prior utilization, and cost data for adult patients with a primary diagnosis of advanced cancer admitted to 4 large US hospitals between 2007 and 2011.
All 4 of these high-volume tertiary-care medical centers were selected for their high patient volume (to facilitate sample size) and research capacity (to facilitate proficient recruitment and data collection). Before the study was initiated, it was approved by the institutional review board of each facility. In addition, approval was sought from each attending physician at each hospital site; patients whose physician did not grant approval were not considered for enrollment. More than 95% of physicians gave their approval.
Patients were at least 18 years old and had a primary diagnosis of metastatic solid tumor; central nervous system malignancy; locally advanced head, neck, or pancreas cancer; metastatic melanoma; or transplant-ineligible lymphoma or multiple myeloma. Patients were excluded if they did not speak English, had a diagnosis of dementia, were unresponsive or nonverbal, had been admitted for routine chemotherapy, died or were discharged within 48 hours of admission, or had had a previous palliative care consultation.
Eligible patients were identified through daily review of admissions records and administrative databases. For each potential study patient identified, that patient’s bedside nurse inquired about willingness to participate in the study. Then, for each willing patient, a trained clinical interviewer approached to explain the study and obtain informed consent. With the patient’s consent, family members were also approached and enrolled with written informed consent.
Quantitative Variables
Independent variables. In the dataset, we identified 17 patient-level variables we hypothesized could be significantly associated with hospitalization cost. These variables covered 4 domains:
- Demographics: age, sex, race.
- Socioeconomics/systems: education level, insurance status, presence of advance directive (living will or healthcare proxy).
- Clinical care: primary cancer diagnosis, admitting diagnosis, comorbidities (Elixhauser index22), symptom burden and severity (Condensed Memorial Symptom Assessment Scale [CMSAS]23), and activities of daily living24 or presence of a hospital-acquired condition or complication.25
- Prior utilization: visiting homecare nurse and home health aide within 2 weeks before admission, and analgesic use in morphine sulfate equivalents within week before admission.
Data were collected through a combination of medical record review (age, sex, diagnoses, comorbidities, complications), patient interview (race, education, advance directive, CMSAS, activities of daily living, prior utilization), and hospital administrative databases (insurance). For use in regression, variables were divided into categories when appropriate. Table 1 lists these predictors and their prevalence in the analytic sample.
Dependent variable. The outcome of interest in this analysis was total direct cost of hospital stay. Direct costs are those attributable to the care of a specific patient, as distinct from indirect costs, the shared overhead costs of running a hospital.26 Cost data were extracted from hospital accounting databases and therefore reflect actual costs, the US dollar cost to the hospitals of care provided, also known as direct measurement.27 Costs were standardized for geographical region using the Medicare Wage Index28 and year using the Consumer Price Index29 and are presented here in US dollars for 2011, the final year of data collection.
Statistical Methods
Primary analyses. We regressed total direct hospital costs against all predictors listed in Table 1. To control for receipt of palliative care, we used additional independent variables—a fixed-effects variable for each of 3 hospitals (the fourth hospital was used as the reference case) and a binary treatment variable (whether or not the patient was seen by a palliative care consultation team within 2 days of hospital admission).19,20
Associations between cost and patient-level covariates were derived with use of a generalized linear model with a γ distribution and a log link,30 selected after comparative evaluation of performance for multiple linear and nonlinear modeling options.31
For each patient-level covariate, we estimated average marginal effects. For continuous variables, we estimated the marginal increase in cost associated with a 1-unit increase in the variable. For binary variables, we estimated the average incremental effect, the increase in cost associated with a move from the reference group, holding all other covariates to their original values. All analyses were performed with Stata Version 12.32
Secondary analyses. Primary analyses showed that number of patient comorbidities (Elixhauser index) was strongly associated with complications and comorbidity count. Prior analyses with these data have shown that palliative care had a larger cost-saving effect for patients with a larger number of comorbidities.20 Additional analyses were therefore performed to examine associations between complications, utilization, and palliative care. First, we cross-tabulated the sample by complications status (none; minor or major) and receipt of timely palliative care, and we present their summary utilization data. Second, we estimated the effect for each complications stratum (none; minor or major) of receiving timely palliative care on cost. These estimates are calculated consistent with prior work with these data: We used propensity scores to balance patients who received the treatment (palliative care) with patients who did not (usual care only),33,34 and we used a generalized linear model with a γ distribution and a log link to regress the direct hospital care cost on the binary treatment variable and all predictors listed in Table 1.19-21
RESULTS
Participants
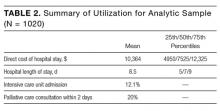
We have previously detailed that in our study there were 1023 patients eligible for cost analysis,19 of whom three were missing data in a field in Table 1 and excluded from this paper. The final analytic sample (N = 1020) is presented according to baseline covariates in Table 1 and according to summary utilization measures in Table 2.
Main Results
The results of the primary analysis, estimating the association between patient-level factors and cost of hospitalization, are presented in Table 3.
These results show the evidence of an association with cost is strongest for 3 clinical factors: a major complication (+$8267; 95% confidence interval [CI], $4509-$12,025), a minor but not a major complication (+$5289; CI, $3480-$7097), and number of comorbidities (+$852; CI, $550-$1153). In addition, there is evidence of associations between lower cost and admitting diagnosis of electrolyte disorders (–$4759; CI, –$7928 to –$1590) and older age (–$53; CI, –$99 to –$6). There is no significant association between primary diagnosis, symptom burden or other clinical factors, sociodemographic factors or healthcare utilization prior to admission and direct hospitalization costs.
Results of the secondary analyses of associations between complications, utilization, and palliative care are listed in Table 4. Patients are stratified by complication (none; major | minor) and their direct cost of hospital care and hospital length of stay (LOS) presented by treatment group (palliative care; usual care only). The data show that within each strata patients who received palliative care had lower costs and LOS than those who received usual care only. Estimated effects of palliative care on utilization is found to be statistically significant in all four quadrants, with a larger cost-effect in the complications stratum than the non-complications stratum.
Sensitivity Analysis
Fifty-one patients died during admission. After removing these cases, because of concerns about possible unobserved heterogeneity,35 we checked our primary (Table 3) and secondary (Table 4) results. Patients discharged alive had results substantively similar to those of the entire sample.
DISCUSSION
Results from our primary analysis (Table 3) suggest that complications and number of comorbidities are the key drivers of hospitalization cost for adults with advanced cancer. Hospitalization for electrolyte disorders and age are both negatively associated with cost.
The association found between higher cost and hospital-acquired complications (HACs) is consistent with other studies’ finding that HACs often result in higher cost, longer LOS, and increased inhospital mortality.36 Since those studies were reported, policy attention has been increasingly focused on HACs.37 Our findings are notable in that, though prior evidence has also suggested high hospital cost is multifactorial, driven by a diversity of demographic, socioeconomic, and clinical factors, this rich patient-reported dataset suggests that, compared with other variables, HACs are emphatically the largest driver of cost. Moreover, cancer patients typically are a vulnerable population, more prone to complications and thus also to potentially avoidable treatments and higher cost. Our prior work suggested earlier palliative care consultation can reduce cost, in part by shortening LOS and reducing the opportunity for HACs to develop19,20; our secondary analysis (Table 4) suggested a palliative care team’s involvement in HAC treatment can significantly reduce cost of care as well. These associations possibly derive from changed treatment choices and shorter LOS. Further work is needed to better elucidate the role of palliative care in the prevention of HACs in seriously ill patients.
That the number of comorbidities was found to be a key driver of hospitalization cost is consistent with recent findings that high spending on seriously ill patients is associated with having multiple chronic conditions rather than any specific primary diagnosis.38,39 It is important to note that, unlike impending complications, serious chronic conditions generally are known at admission and can be addressed prospectively through provision and policy. A prior analysis with these data found that palliative care consultation was more cost-effective for patients with a larger number of comorbidities.20 Our 2 studies together suggest that, notwithstanding the preferable alternative of avoiding hospitalization entirely, palliative care and other skilled coordination of care services ought to be prioritized for inpatients with multiple serious illnesses and the highest medical complexity. This patient group has both the highest costs and the greatest amenability to skilled transdisciplinary intervention, possibly because multiple chronic conditions affect patients interactively, complicating identification of appropriate polypharmacy responses and prioritization of treatments.
Our findings also may help direct appropriate use of palliative care services. The recently published American Society of Clinical Oncology palliative care guidelines note that all patients with advanced cancer (eg, those enrolled in our study) should receive dedicated palliative care services, early in the disease course, concurrent with active treatment.40 Workforce estimates suggest that the current and future numbers of palliative care practitioners will be unable to meet the ASCO recommendations alone never mind patients with other serious illnesses (eg, advanced heart failure, COPD, CKD).41 As such, specialized palliative care services will need to be targeted to the patient populations that can benefit most from these services. Whereas cost should not be the principle driver specialized palliative care provision, it will likely be an important component due to both the necessity of allocating scarce resources in the most effective way and the evidence that in care of the seriously-ill lower costs are often a proxy for improved patient experience.
These findings also have implications for research: Different conditions and presumably different combinations of conditions have very different implications for hospital care costs for a cohort of adults with advanced cancer. Given the increasing number of co-occurring conditions among seriously ill patients, and the increasing costs of cancer care and of treating multimorbidity cases, it is essential to further our understanding of the relationship between comorbidities and costs in order to plan and finance care for advanced cancer patients.
Limitations and Generalizability
In this observational study, reported associations may be attributable to unobserved confounding that our analyses failed to control.
Our results reflect associations in a prospective multisite study of advanced cancer patients hospitalized in the United States. It is not clear how generalizable our findings are to patients without cancer, to patients in nonhospital settings, and to patients in other health systems and countries. Analyzing cost from the hospital perspective does not take into account that the most impactful way to reduce cost is to avoid hospitalization entirely.
Results of our secondary analysis will not necessarily be robust to patient groups, as specific weights likely will vary by sample. The idea that costs vary by condition, however, is important nevertheless. Elixhauser total was derived with use of the enhanced ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) algorithm from Quan et al.42 and does not include subsequent Elixhauser Comorbidity Software updates recommended by the Healthcare Cost and Utilization Project (HCUP; Agency for Healthcare Research and Quality).43 The Elixhauser index is recommended over Charlson and other comorbidity indices by both HCUP45 and a recent systematic review.44
One possible unobserved factor is prior chemotherapy, which is associated with increased hospitalization risk. Related factors that are somewhat controlled for in the study include cancer stage (advanced cancer was an eligibility criterion) and receipt of analgesics within the week before admission (patients admitted for routine chemotherapy were excluded from analyses at the outset).
CONCLUSION
Other studies have identified a wide range of sociodemographic, clinical, and health system factors associated with healthcare utilization. Our results suggest that, for cost of hospital admission among adults with advanced cancer, the most important drivers of utilization are complications and comorbidities. Hospital costs for patients with advanced cancer constitute a major part of US healthcare spending, and these results suggest the need to prioritize high-quality, cost-effective care for patients with multiple serious illnesses.
Acknowledgments
The authors thank Robert Arnold, Phil Santa Emma, Mary Beth Happ, Tim Smith, and David Weissman for contributing to the Palliative Care for Cancer (PC4C) project.
Disclosure
The study was funded by grant R01 CA116227 from the National Cancer Institute and the National Institute of Nursing Research. The study sponsors had no role in design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the US government. All authors are independent of the study sponsors. Dr. May was supported by a HRB/NCI Health Economics Fellowship during this work. Dr. Garrido is supported by a Veterans Affairs HSR&D career development award (CDA 11-201/CDP 12-255). Dr. Kelley’s time was funded by the National Institute on Aging (1K23AG040774-01A1) and the American Federation for Aging. Dr. Smith is funded by the NCI Core Grant P 30 006973, 1-R01 CA177562-01A1, 1-R01 NR014050 01, and the Harry J. Duffey Family Endowment for Palliative Care. Dr. Morrison was the recipient of a Midcareer Investigator Award in Patient-Oriented Research (5K24AG022345) during the course of this work. This work was supported by the NIA, Claude D. Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai [5P30AG028741], and the National Palliative Care Research Center.
1. Soni A. Top 10 Most Costly Conditions Among Men and Women, 2008: Estimates for the U.S. Civilian Noninstitutionalized Adult Population, Age 18 and Older. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
2. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. PubMed
3. American Cancer Society. Cancer Facts and Figures 2015. Atlanta, GA: American Cancer Society; 2015.
4. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065. PubMed
5. Levit L, Balogh E, Nass S, Ganz PA, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: Institute of Medicine/National Academies Press; 2013. PubMed
7. Anderson GF. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
8. Tibi-Levy Y, Le Vaillant M, de Pouvourville G. Determinants of resource utilization in four palliative care units. Palliat Med. 2006;20(2):95-106. PubMed
9. Simoens S, Kutten B, Keirse E, et al. The costs of treating terminal patients. J Pain Symptom Manage. 2010;40(3):436-448. PubMed
10. Groeneveld I, Murtagh F, Kaloki Y, Bausewein C, Higginson I. Determinants of healthcare costs in the last year of life. Annual Assembly of American Academy of Hospice and Palliative Medicine & Hospice and Palliative Nurses Association; March 14, 2013; New Orleans, LA.
11. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures at the end of life for colorectal cancer decedents. J Womens Health. 2007;16(2):214-227. PubMed
12. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures and service utilization at the end of life for lung cancer decedents. Womens Health Issues. 2008;18(3):199-209. PubMed
13. Walker H, Anderson M, Farahati F, et al. Resource use and costs of end-of-life/palliative care: Ontario adult cancer patients dying during 2002 and 2003. J Palliat Care. 2011;27(2):79-88. PubMed
14. Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169(5):493-501. PubMed
15. Hanratty B, Burstrom B, Walander A, Whitehead M. Inequality in the face of death? Public expenditure on health care for different socioeconomic groups in the last year of life. J Health Serv Res Policy. 2007;12(2):90-94. PubMed
16. Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154(4):235-242. PubMed
17. Guerriere DN, Zagorski B, Fassbender K, Masucci L, Librach L, Coyte PC. Cost variations in ambulatory and home-based palliative care. Palliat Med. 2010;24(5):523-532. PubMed
18. US Department of Health and Human Services, National Institutes of Health. Palliative Care for Hospitalized Cancer Patients [project information]. Bethesda, MD: US Dept of Health and Human Services, National Institutes of Health; 2006. Project 5R01CA116227-04. https://projectreporter.nih.gov/project_info_description.cfm?projectnumber=5R01CA116227-04. Published 2006. Accessed August 1, 2015.
19. May P, Garrido MM, Cassel JB, et al. Prospective cohort study of hospital palliative care teams for inpatients with advanced cancer: earlier consultation is associated with larger cost-saving effect. J Clin Oncol. 2015;33(25):2745-2752. PubMed
20. May P, Garrido MM, Cassel JB, et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff. 2016;35(1):44-53. PubMed
21. May P, Garrido MM, Cassel JB, Morrison RS, Normand C. Using length of stay to control for unobserved heterogeneity when estimating treatment effect on hospital costs with observational data: issues of reliability, robustness and usefulness. Health Serv Res. 2016;51(5):2020-2043. PubMed
22. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. PubMed
23. Chang VT, Hwang SS, Kasimis B, Thaler HT. Shorter symptom assessment instruments: the Condensed Memorial Symptom Assessment Scale (CMSAS). Cancer Invest. 2004;22(4):526-536. PubMed
24. Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. The index of ADL: a standardized measure of biological and psychological function. JAMA. 1963;185(12):914-919. PubMed
25. McLaughlin MA, Orosz GM, Magaziner J, et al. Preoperative status and risk of complications in patients with hip fracture. J Gen Intern Med. 2006;21(3):219-225. PubMed
26. Taheri PA, Butz D, Griffes LC, Morlock DR, Greenfield LJ. Physician impact on the total cost of care. Ann Surg. 2000;231(3):432-435. PubMed
27. US Department of Veterans Affairs, Health Economics Resource Center. Determining costs. Washington, DC: US Dept of Veterans Affairs, Health Economics Resource Center; 2016. http://www.herc.research.va.gov/include/page.asp?id=determining-costs. Published 2016. Accessed September 7, 2016.
28. US Department of Health and Human Services, Center for Medicare & Medicaid Services. FY 2011 Wage Index [Table 2]. Baltimore, MD: US Dept of Health and Human Services, Center for Medicare & Medicaid Services; 2011. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/CMS1234173.html. Published 2011. Accessed September 2, 2014.
29. US Department of Labor, Bureau of Labor Statistics. All Urban Consumers (Current Series) [Consumer Price Index database]. US Dept of Labor, Bureau of Labor Statistics; 2015. http://www.bls.gov/cpi/data.htm. Published 2015. Accessed August 15, 2016.
30. Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465-488. PubMed
31. Jones AM, Rice N, Bago d’Uva T, Balia S. Applied Health Economics. 2nd ed. Oxford, England: Routledge; 2013.
32. Stata [computer program]. Version 12. College Station, TX: StataCorp; 2011.
33. Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing
propensity scores. Health Serv Res. 2014;49(5):1701-1720. PubMed
34. R Core Team. R: A Language and Environment for Statistical Computing. Vienna,
Austria: R Foundation for Statistical Computing; 2016.
35. Cassel JB, Kerr K, Pantilat S, Smith TJ. Palliative care consultation and hospital
length of stay. J Palliat Med. 2010;13(6):761-767. PubMed
36. US Department of Health and Human Services, Agency for Healthcare Research
and Quality. Efforts to Improve Patient Safety Result in 1.3 Million Fewer Patient
Harms: Interim Update on 2013 Annual Hospital-Acquired Condition Rate and
Estimates of Cost Savings and Deaths Averted From 2010 to 2013. Rockville,
MD: US Dept of Health and Human Services, Agency for Healthcare Research
and Quality; 2015. http://www.ahrq.gov/professionals/quality-patient-safety/pfp/
interimhacrate2013.html. Published 2015. Updated November 2015. Accessed
November 18, 2016.
37. Cassidy A. Health Policy Brief: Medicare’s Hospital-Acquired Condition Reduction
Program. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_
id=142. Published August 6, 2015. Accessed April 24, 2017.
38. Davis MA, Nallamothu BK, Banerjee M, Bynum JP. Identification of four unique
spending patterns among older adults in the last year of life challenges standard
assumptions. Health Aff. 2016;35(7):1316-1323. PubMed
39. Aldridge MD, Kelley AS. The myth regarding the high cost of end-of-life care.
Am J Public Health. 2015;105(12):2411-2415. PubMed
40. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard
oncology care: American Society of Clinical Oncology clinical practice guideline
update. J Clin Oncol. 2017;35(1):96-112. PubMed
41. Spetz J, Dudley N, Trupin L, Rogers M, Meier DE, Dumanovsky T. Few hospital
palliative care programs meet national staffing recommendations. Health Aff.
2016;35(9):1690-1697. PubMed
42. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities
in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. PubMed
43. HCUP [Healthcare Cost and Utilization Project] Elixhauser Comorbidity Software
[computer program]. Version 3.7. Rockville, MD: Agency for Healthcare
Research and Quality; 2016. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/
comorbidity.jsp. Published 2016. Accessed November 9, 2016.
44. Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for
administrative data. Med Care. 2012;50(12):1109-1118. PubMed
Of the major chronic conditions that affect adult patients in the United States, cancer accounts for the highest levels of per capita spending.1 Cost growth for cancer treatment has been substantial and persistent, from $72 billion in 2004 to $125 billion in 2010, and is projected to increase to $173 billion by 2020.2 Thirty-five percent of US direct medical cancer costs are attributable to inpatient hospital stays.3 Policy responses that can provide financially sustainable, high-quality models of care for patients with advanced cancer and other serious illness are urgently sought.4-7
Patterns and levels of resource utilization in providing healthcare to patients with serious illness reflect not only treatment choices but a complex set of relationships among demographic, clinical, and system factors.8-10 Patient-level factors previously identified as potentially significant drivers of resource utilization among cancer populations specifically include age,11 sex,12 primary diagnosis,13 and comorbidities.11 Among end-of-life populations, significant associations have been found between cost and ethnicity,14 socioeconomic status,15 advance directive status,16 insurance status,16 and functional status.17
Evidence on factors strongly associated with cost of hospital admission for patients with advanced cancer can therefore inform provision and planning of healthcare. For example, when a specific diagnosis or clinical condition is found to be associated with high cost, then improving coordination and provision of care for this patient group may reduce avoidable utilization. Determining associations between sociodemographics and hospital care cost can help in identifying possible disparities in care, such as those that might occur when care differs by race, class, or insurance status.
We conducted the Palliative Care for Cancer (PC4C) study, a prospective multisite cohort study of the palliative care consultation team intervention for hospitalized adults with advanced cancer.18,19 In our primary analysis, we controlled for receipt of palliative care and analyzed a rich patient-reported dataset to examine associations between hospital care cost, and sociodemographic factors, clinical variables, and prior healthcare utilization. The results provide evidence regarding the factors most associated with the cost of hospital-based cancer care.
METHODS
Design, Setting, Participants, Data Sources
The PC4C study has been described in detail by authors who estimated the impact of specialist palliative care consultation teams on hospitalization cost.19-21 We prospectively collected sociodemographic, clinical, prior utilization, and cost data for adult patients with a primary diagnosis of advanced cancer admitted to 4 large US hospitals between 2007 and 2011.
All 4 of these high-volume tertiary-care medical centers were selected for their high patient volume (to facilitate sample size) and research capacity (to facilitate proficient recruitment and data collection). Before the study was initiated, it was approved by the institutional review board of each facility. In addition, approval was sought from each attending physician at each hospital site; patients whose physician did not grant approval were not considered for enrollment. More than 95% of physicians gave their approval.
Patients were at least 18 years old and had a primary diagnosis of metastatic solid tumor; central nervous system malignancy; locally advanced head, neck, or pancreas cancer; metastatic melanoma; or transplant-ineligible lymphoma or multiple myeloma. Patients were excluded if they did not speak English, had a diagnosis of dementia, were unresponsive or nonverbal, had been admitted for routine chemotherapy, died or were discharged within 48 hours of admission, or had had a previous palliative care consultation.
Eligible patients were identified through daily review of admissions records and administrative databases. For each potential study patient identified, that patient’s bedside nurse inquired about willingness to participate in the study. Then, for each willing patient, a trained clinical interviewer approached to explain the study and obtain informed consent. With the patient’s consent, family members were also approached and enrolled with written informed consent.
Quantitative Variables
Independent variables. In the dataset, we identified 17 patient-level variables we hypothesized could be significantly associated with hospitalization cost. These variables covered 4 domains:
- Demographics: age, sex, race.
- Socioeconomics/systems: education level, insurance status, presence of advance directive (living will or healthcare proxy).
- Clinical care: primary cancer diagnosis, admitting diagnosis, comorbidities (Elixhauser index22), symptom burden and severity (Condensed Memorial Symptom Assessment Scale [CMSAS]23), and activities of daily living24 or presence of a hospital-acquired condition or complication.25
- Prior utilization: visiting homecare nurse and home health aide within 2 weeks before admission, and analgesic use in morphine sulfate equivalents within week before admission.
Data were collected through a combination of medical record review (age, sex, diagnoses, comorbidities, complications), patient interview (race, education, advance directive, CMSAS, activities of daily living, prior utilization), and hospital administrative databases (insurance). For use in regression, variables were divided into categories when appropriate. Table 1 lists these predictors and their prevalence in the analytic sample.
Dependent variable. The outcome of interest in this analysis was total direct cost of hospital stay. Direct costs are those attributable to the care of a specific patient, as distinct from indirect costs, the shared overhead costs of running a hospital.26 Cost data were extracted from hospital accounting databases and therefore reflect actual costs, the US dollar cost to the hospitals of care provided, also known as direct measurement.27 Costs were standardized for geographical region using the Medicare Wage Index28 and year using the Consumer Price Index29 and are presented here in US dollars for 2011, the final year of data collection.
Statistical Methods
Primary analyses. We regressed total direct hospital costs against all predictors listed in Table 1. To control for receipt of palliative care, we used additional independent variables—a fixed-effects variable for each of 3 hospitals (the fourth hospital was used as the reference case) and a binary treatment variable (whether or not the patient was seen by a palliative care consultation team within 2 days of hospital admission).19,20
Associations between cost and patient-level covariates were derived with use of a generalized linear model with a γ distribution and a log link,30 selected after comparative evaluation of performance for multiple linear and nonlinear modeling options.31
For each patient-level covariate, we estimated average marginal effects. For continuous variables, we estimated the marginal increase in cost associated with a 1-unit increase in the variable. For binary variables, we estimated the average incremental effect, the increase in cost associated with a move from the reference group, holding all other covariates to their original values. All analyses were performed with Stata Version 12.32
Secondary analyses. Primary analyses showed that number of patient comorbidities (Elixhauser index) was strongly associated with complications and comorbidity count. Prior analyses with these data have shown that palliative care had a larger cost-saving effect for patients with a larger number of comorbidities.20 Additional analyses were therefore performed to examine associations between complications, utilization, and palliative care. First, we cross-tabulated the sample by complications status (none; minor or major) and receipt of timely palliative care, and we present their summary utilization data. Second, we estimated the effect for each complications stratum (none; minor or major) of receiving timely palliative care on cost. These estimates are calculated consistent with prior work with these data: We used propensity scores to balance patients who received the treatment (palliative care) with patients who did not (usual care only),33,34 and we used a generalized linear model with a γ distribution and a log link to regress the direct hospital care cost on the binary treatment variable and all predictors listed in Table 1.19-21
RESULTS
Participants
We have previously detailed that in our study there were 1023 patients eligible for cost analysis,19 of whom three were missing data in a field in Table 1 and excluded from this paper. The final analytic sample (N = 1020) is presented according to baseline covariates in Table 1 and according to summary utilization measures in Table 2.
Main Results
The results of the primary analysis, estimating the association between patient-level factors and cost of hospitalization, are presented in Table 3.
These results show the evidence of an association with cost is strongest for 3 clinical factors: a major complication (+$8267; 95% confidence interval [CI], $4509-$12,025), a minor but not a major complication (+$5289; CI, $3480-$7097), and number of comorbidities (+$852; CI, $550-$1153). In addition, there is evidence of associations between lower cost and admitting diagnosis of electrolyte disorders (–$4759; CI, –$7928 to –$1590) and older age (–$53; CI, –$99 to –$6). There is no significant association between primary diagnosis, symptom burden or other clinical factors, sociodemographic factors or healthcare utilization prior to admission and direct hospitalization costs.
Results of the secondary analyses of associations between complications, utilization, and palliative care are listed in Table 4. Patients are stratified by complication (none; major | minor) and their direct cost of hospital care and hospital length of stay (LOS) presented by treatment group (palliative care; usual care only). The data show that within each strata patients who received palliative care had lower costs and LOS than those who received usual care only. Estimated effects of palliative care on utilization is found to be statistically significant in all four quadrants, with a larger cost-effect in the complications stratum than the non-complications stratum.
Sensitivity Analysis
Fifty-one patients died during admission. After removing these cases, because of concerns about possible unobserved heterogeneity,35 we checked our primary (Table 3) and secondary (Table 4) results. Patients discharged alive had results substantively similar to those of the entire sample.
DISCUSSION
Results from our primary analysis (Table 3) suggest that complications and number of comorbidities are the key drivers of hospitalization cost for adults with advanced cancer. Hospitalization for electrolyte disorders and age are both negatively associated with cost.
The association found between higher cost and hospital-acquired complications (HACs) is consistent with other studies’ finding that HACs often result in higher cost, longer LOS, and increased inhospital mortality.36 Since those studies were reported, policy attention has been increasingly focused on HACs.37 Our findings are notable in that, though prior evidence has also suggested high hospital cost is multifactorial, driven by a diversity of demographic, socioeconomic, and clinical factors, this rich patient-reported dataset suggests that, compared with other variables, HACs are emphatically the largest driver of cost. Moreover, cancer patients typically are a vulnerable population, more prone to complications and thus also to potentially avoidable treatments and higher cost. Our prior work suggested earlier palliative care consultation can reduce cost, in part by shortening LOS and reducing the opportunity for HACs to develop19,20; our secondary analysis (Table 4) suggested a palliative care team’s involvement in HAC treatment can significantly reduce cost of care as well. These associations possibly derive from changed treatment choices and shorter LOS. Further work is needed to better elucidate the role of palliative care in the prevention of HACs in seriously ill patients.
That the number of comorbidities was found to be a key driver of hospitalization cost is consistent with recent findings that high spending on seriously ill patients is associated with having multiple chronic conditions rather than any specific primary diagnosis.38,39 It is important to note that, unlike impending complications, serious chronic conditions generally are known at admission and can be addressed prospectively through provision and policy. A prior analysis with these data found that palliative care consultation was more cost-effective for patients with a larger number of comorbidities.20 Our 2 studies together suggest that, notwithstanding the preferable alternative of avoiding hospitalization entirely, palliative care and other skilled coordination of care services ought to be prioritized for inpatients with multiple serious illnesses and the highest medical complexity. This patient group has both the highest costs and the greatest amenability to skilled transdisciplinary intervention, possibly because multiple chronic conditions affect patients interactively, complicating identification of appropriate polypharmacy responses and prioritization of treatments.
Our findings also may help direct appropriate use of palliative care services. The recently published American Society of Clinical Oncology palliative care guidelines note that all patients with advanced cancer (eg, those enrolled in our study) should receive dedicated palliative care services, early in the disease course, concurrent with active treatment.40 Workforce estimates suggest that the current and future numbers of palliative care practitioners will be unable to meet the ASCO recommendations alone never mind patients with other serious illnesses (eg, advanced heart failure, COPD, CKD).41 As such, specialized palliative care services will need to be targeted to the patient populations that can benefit most from these services. Whereas cost should not be the principle driver specialized palliative care provision, it will likely be an important component due to both the necessity of allocating scarce resources in the most effective way and the evidence that in care of the seriously-ill lower costs are often a proxy for improved patient experience.
These findings also have implications for research: Different conditions and presumably different combinations of conditions have very different implications for hospital care costs for a cohort of adults with advanced cancer. Given the increasing number of co-occurring conditions among seriously ill patients, and the increasing costs of cancer care and of treating multimorbidity cases, it is essential to further our understanding of the relationship between comorbidities and costs in order to plan and finance care for advanced cancer patients.
Limitations and Generalizability
In this observational study, reported associations may be attributable to unobserved confounding that our analyses failed to control.
Our results reflect associations in a prospective multisite study of advanced cancer patients hospitalized in the United States. It is not clear how generalizable our findings are to patients without cancer, to patients in nonhospital settings, and to patients in other health systems and countries. Analyzing cost from the hospital perspective does not take into account that the most impactful way to reduce cost is to avoid hospitalization entirely.
Results of our secondary analysis will not necessarily be robust to patient groups, as specific weights likely will vary by sample. The idea that costs vary by condition, however, is important nevertheless. Elixhauser total was derived with use of the enhanced ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) algorithm from Quan et al.42 and does not include subsequent Elixhauser Comorbidity Software updates recommended by the Healthcare Cost and Utilization Project (HCUP; Agency for Healthcare Research and Quality).43 The Elixhauser index is recommended over Charlson and other comorbidity indices by both HCUP45 and a recent systematic review.44
One possible unobserved factor is prior chemotherapy, which is associated with increased hospitalization risk. Related factors that are somewhat controlled for in the study include cancer stage (advanced cancer was an eligibility criterion) and receipt of analgesics within the week before admission (patients admitted for routine chemotherapy were excluded from analyses at the outset).
CONCLUSION
Other studies have identified a wide range of sociodemographic, clinical, and health system factors associated with healthcare utilization. Our results suggest that, for cost of hospital admission among adults with advanced cancer, the most important drivers of utilization are complications and comorbidities. Hospital costs for patients with advanced cancer constitute a major part of US healthcare spending, and these results suggest the need to prioritize high-quality, cost-effective care for patients with multiple serious illnesses.
Acknowledgments
The authors thank Robert Arnold, Phil Santa Emma, Mary Beth Happ, Tim Smith, and David Weissman for contributing to the Palliative Care for Cancer (PC4C) project.
Disclosure
The study was funded by grant R01 CA116227 from the National Cancer Institute and the National Institute of Nursing Research. The study sponsors had no role in design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the US government. All authors are independent of the study sponsors. Dr. May was supported by a HRB/NCI Health Economics Fellowship during this work. Dr. Garrido is supported by a Veterans Affairs HSR&D career development award (CDA 11-201/CDP 12-255). Dr. Kelley’s time was funded by the National Institute on Aging (1K23AG040774-01A1) and the American Federation for Aging. Dr. Smith is funded by the NCI Core Grant P 30 006973, 1-R01 CA177562-01A1, 1-R01 NR014050 01, and the Harry J. Duffey Family Endowment for Palliative Care. Dr. Morrison was the recipient of a Midcareer Investigator Award in Patient-Oriented Research (5K24AG022345) during the course of this work. This work was supported by the NIA, Claude D. Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai [5P30AG028741], and the National Palliative Care Research Center.
Of the major chronic conditions that affect adult patients in the United States, cancer accounts for the highest levels of per capita spending.1 Cost growth for cancer treatment has been substantial and persistent, from $72 billion in 2004 to $125 billion in 2010, and is projected to increase to $173 billion by 2020.2 Thirty-five percent of US direct medical cancer costs are attributable to inpatient hospital stays.3 Policy responses that can provide financially sustainable, high-quality models of care for patients with advanced cancer and other serious illness are urgently sought.4-7
Patterns and levels of resource utilization in providing healthcare to patients with serious illness reflect not only treatment choices but a complex set of relationships among demographic, clinical, and system factors.8-10 Patient-level factors previously identified as potentially significant drivers of resource utilization among cancer populations specifically include age,11 sex,12 primary diagnosis,13 and comorbidities.11 Among end-of-life populations, significant associations have been found between cost and ethnicity,14 socioeconomic status,15 advance directive status,16 insurance status,16 and functional status.17
Evidence on factors strongly associated with cost of hospital admission for patients with advanced cancer can therefore inform provision and planning of healthcare. For example, when a specific diagnosis or clinical condition is found to be associated with high cost, then improving coordination and provision of care for this patient group may reduce avoidable utilization. Determining associations between sociodemographics and hospital care cost can help in identifying possible disparities in care, such as those that might occur when care differs by race, class, or insurance status.
We conducted the Palliative Care for Cancer (PC4C) study, a prospective multisite cohort study of the palliative care consultation team intervention for hospitalized adults with advanced cancer.18,19 In our primary analysis, we controlled for receipt of palliative care and analyzed a rich patient-reported dataset to examine associations between hospital care cost, and sociodemographic factors, clinical variables, and prior healthcare utilization. The results provide evidence regarding the factors most associated with the cost of hospital-based cancer care.
METHODS
Design, Setting, Participants, Data Sources
The PC4C study has been described in detail by authors who estimated the impact of specialist palliative care consultation teams on hospitalization cost.19-21 We prospectively collected sociodemographic, clinical, prior utilization, and cost data for adult patients with a primary diagnosis of advanced cancer admitted to 4 large US hospitals between 2007 and 2011.
All 4 of these high-volume tertiary-care medical centers were selected for their high patient volume (to facilitate sample size) and research capacity (to facilitate proficient recruitment and data collection). Before the study was initiated, it was approved by the institutional review board of each facility. In addition, approval was sought from each attending physician at each hospital site; patients whose physician did not grant approval were not considered for enrollment. More than 95% of physicians gave their approval.
Patients were at least 18 years old and had a primary diagnosis of metastatic solid tumor; central nervous system malignancy; locally advanced head, neck, or pancreas cancer; metastatic melanoma; or transplant-ineligible lymphoma or multiple myeloma. Patients were excluded if they did not speak English, had a diagnosis of dementia, were unresponsive or nonverbal, had been admitted for routine chemotherapy, died or were discharged within 48 hours of admission, or had had a previous palliative care consultation.
Eligible patients were identified through daily review of admissions records and administrative databases. For each potential study patient identified, that patient’s bedside nurse inquired about willingness to participate in the study. Then, for each willing patient, a trained clinical interviewer approached to explain the study and obtain informed consent. With the patient’s consent, family members were also approached and enrolled with written informed consent.
Quantitative Variables
Independent variables. In the dataset, we identified 17 patient-level variables we hypothesized could be significantly associated with hospitalization cost. These variables covered 4 domains:
- Demographics: age, sex, race.
- Socioeconomics/systems: education level, insurance status, presence of advance directive (living will or healthcare proxy).
- Clinical care: primary cancer diagnosis, admitting diagnosis, comorbidities (Elixhauser index22), symptom burden and severity (Condensed Memorial Symptom Assessment Scale [CMSAS]23), and activities of daily living24 or presence of a hospital-acquired condition or complication.25
- Prior utilization: visiting homecare nurse and home health aide within 2 weeks before admission, and analgesic use in morphine sulfate equivalents within week before admission.
Data were collected through a combination of medical record review (age, sex, diagnoses, comorbidities, complications), patient interview (race, education, advance directive, CMSAS, activities of daily living, prior utilization), and hospital administrative databases (insurance). For use in regression, variables were divided into categories when appropriate. Table 1 lists these predictors and their prevalence in the analytic sample.
Dependent variable. The outcome of interest in this analysis was total direct cost of hospital stay. Direct costs are those attributable to the care of a specific patient, as distinct from indirect costs, the shared overhead costs of running a hospital.26 Cost data were extracted from hospital accounting databases and therefore reflect actual costs, the US dollar cost to the hospitals of care provided, also known as direct measurement.27 Costs were standardized for geographical region using the Medicare Wage Index28 and year using the Consumer Price Index29 and are presented here in US dollars for 2011, the final year of data collection.
Statistical Methods
Primary analyses. We regressed total direct hospital costs against all predictors listed in Table 1. To control for receipt of palliative care, we used additional independent variables—a fixed-effects variable for each of 3 hospitals (the fourth hospital was used as the reference case) and a binary treatment variable (whether or not the patient was seen by a palliative care consultation team within 2 days of hospital admission).19,20
Associations between cost and patient-level covariates were derived with use of a generalized linear model with a γ distribution and a log link,30 selected after comparative evaluation of performance for multiple linear and nonlinear modeling options.31
For each patient-level covariate, we estimated average marginal effects. For continuous variables, we estimated the marginal increase in cost associated with a 1-unit increase in the variable. For binary variables, we estimated the average incremental effect, the increase in cost associated with a move from the reference group, holding all other covariates to their original values. All analyses were performed with Stata Version 12.32
Secondary analyses. Primary analyses showed that number of patient comorbidities (Elixhauser index) was strongly associated with complications and comorbidity count. Prior analyses with these data have shown that palliative care had a larger cost-saving effect for patients with a larger number of comorbidities.20 Additional analyses were therefore performed to examine associations between complications, utilization, and palliative care. First, we cross-tabulated the sample by complications status (none; minor or major) and receipt of timely palliative care, and we present their summary utilization data. Second, we estimated the effect for each complications stratum (none; minor or major) of receiving timely palliative care on cost. These estimates are calculated consistent with prior work with these data: We used propensity scores to balance patients who received the treatment (palliative care) with patients who did not (usual care only),33,34 and we used a generalized linear model with a γ distribution and a log link to regress the direct hospital care cost on the binary treatment variable and all predictors listed in Table 1.19-21
RESULTS
Participants
We have previously detailed that in our study there were 1023 patients eligible for cost analysis,19 of whom three were missing data in a field in Table 1 and excluded from this paper. The final analytic sample (N = 1020) is presented according to baseline covariates in Table 1 and according to summary utilization measures in Table 2.
Main Results
The results of the primary analysis, estimating the association between patient-level factors and cost of hospitalization, are presented in Table 3.
These results show the evidence of an association with cost is strongest for 3 clinical factors: a major complication (+$8267; 95% confidence interval [CI], $4509-$12,025), a minor but not a major complication (+$5289; CI, $3480-$7097), and number of comorbidities (+$852; CI, $550-$1153). In addition, there is evidence of associations between lower cost and admitting diagnosis of electrolyte disorders (–$4759; CI, –$7928 to –$1590) and older age (–$53; CI, –$99 to –$6). There is no significant association between primary diagnosis, symptom burden or other clinical factors, sociodemographic factors or healthcare utilization prior to admission and direct hospitalization costs.
Results of the secondary analyses of associations between complications, utilization, and palliative care are listed in Table 4. Patients are stratified by complication (none; major | minor) and their direct cost of hospital care and hospital length of stay (LOS) presented by treatment group (palliative care; usual care only). The data show that within each strata patients who received palliative care had lower costs and LOS than those who received usual care only. Estimated effects of palliative care on utilization is found to be statistically significant in all four quadrants, with a larger cost-effect in the complications stratum than the non-complications stratum.
Sensitivity Analysis
Fifty-one patients died during admission. After removing these cases, because of concerns about possible unobserved heterogeneity,35 we checked our primary (Table 3) and secondary (Table 4) results. Patients discharged alive had results substantively similar to those of the entire sample.
DISCUSSION
Results from our primary analysis (Table 3) suggest that complications and number of comorbidities are the key drivers of hospitalization cost for adults with advanced cancer. Hospitalization for electrolyte disorders and age are both negatively associated with cost.
The association found between higher cost and hospital-acquired complications (HACs) is consistent with other studies’ finding that HACs often result in higher cost, longer LOS, and increased inhospital mortality.36 Since those studies were reported, policy attention has been increasingly focused on HACs.37 Our findings are notable in that, though prior evidence has also suggested high hospital cost is multifactorial, driven by a diversity of demographic, socioeconomic, and clinical factors, this rich patient-reported dataset suggests that, compared with other variables, HACs are emphatically the largest driver of cost. Moreover, cancer patients typically are a vulnerable population, more prone to complications and thus also to potentially avoidable treatments and higher cost. Our prior work suggested earlier palliative care consultation can reduce cost, in part by shortening LOS and reducing the opportunity for HACs to develop19,20; our secondary analysis (Table 4) suggested a palliative care team’s involvement in HAC treatment can significantly reduce cost of care as well. These associations possibly derive from changed treatment choices and shorter LOS. Further work is needed to better elucidate the role of palliative care in the prevention of HACs in seriously ill patients.
That the number of comorbidities was found to be a key driver of hospitalization cost is consistent with recent findings that high spending on seriously ill patients is associated with having multiple chronic conditions rather than any specific primary diagnosis.38,39 It is important to note that, unlike impending complications, serious chronic conditions generally are known at admission and can be addressed prospectively through provision and policy. A prior analysis with these data found that palliative care consultation was more cost-effective for patients with a larger number of comorbidities.20 Our 2 studies together suggest that, notwithstanding the preferable alternative of avoiding hospitalization entirely, palliative care and other skilled coordination of care services ought to be prioritized for inpatients with multiple serious illnesses and the highest medical complexity. This patient group has both the highest costs and the greatest amenability to skilled transdisciplinary intervention, possibly because multiple chronic conditions affect patients interactively, complicating identification of appropriate polypharmacy responses and prioritization of treatments.
Our findings also may help direct appropriate use of palliative care services. The recently published American Society of Clinical Oncology palliative care guidelines note that all patients with advanced cancer (eg, those enrolled in our study) should receive dedicated palliative care services, early in the disease course, concurrent with active treatment.40 Workforce estimates suggest that the current and future numbers of palliative care practitioners will be unable to meet the ASCO recommendations alone never mind patients with other serious illnesses (eg, advanced heart failure, COPD, CKD).41 As such, specialized palliative care services will need to be targeted to the patient populations that can benefit most from these services. Whereas cost should not be the principle driver specialized palliative care provision, it will likely be an important component due to both the necessity of allocating scarce resources in the most effective way and the evidence that in care of the seriously-ill lower costs are often a proxy for improved patient experience.
These findings also have implications for research: Different conditions and presumably different combinations of conditions have very different implications for hospital care costs for a cohort of adults with advanced cancer. Given the increasing number of co-occurring conditions among seriously ill patients, and the increasing costs of cancer care and of treating multimorbidity cases, it is essential to further our understanding of the relationship between comorbidities and costs in order to plan and finance care for advanced cancer patients.
Limitations and Generalizability
In this observational study, reported associations may be attributable to unobserved confounding that our analyses failed to control.
Our results reflect associations in a prospective multisite study of advanced cancer patients hospitalized in the United States. It is not clear how generalizable our findings are to patients without cancer, to patients in nonhospital settings, and to patients in other health systems and countries. Analyzing cost from the hospital perspective does not take into account that the most impactful way to reduce cost is to avoid hospitalization entirely.
Results of our secondary analysis will not necessarily be robust to patient groups, as specific weights likely will vary by sample. The idea that costs vary by condition, however, is important nevertheless. Elixhauser total was derived with use of the enhanced ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) algorithm from Quan et al.42 and does not include subsequent Elixhauser Comorbidity Software updates recommended by the Healthcare Cost and Utilization Project (HCUP; Agency for Healthcare Research and Quality).43 The Elixhauser index is recommended over Charlson and other comorbidity indices by both HCUP45 and a recent systematic review.44
One possible unobserved factor is prior chemotherapy, which is associated with increased hospitalization risk. Related factors that are somewhat controlled for in the study include cancer stage (advanced cancer was an eligibility criterion) and receipt of analgesics within the week before admission (patients admitted for routine chemotherapy were excluded from analyses at the outset).
CONCLUSION
Other studies have identified a wide range of sociodemographic, clinical, and health system factors associated with healthcare utilization. Our results suggest that, for cost of hospital admission among adults with advanced cancer, the most important drivers of utilization are complications and comorbidities. Hospital costs for patients with advanced cancer constitute a major part of US healthcare spending, and these results suggest the need to prioritize high-quality, cost-effective care for patients with multiple serious illnesses.
Acknowledgments
The authors thank Robert Arnold, Phil Santa Emma, Mary Beth Happ, Tim Smith, and David Weissman for contributing to the Palliative Care for Cancer (PC4C) project.
Disclosure
The study was funded by grant R01 CA116227 from the National Cancer Institute and the National Institute of Nursing Research. The study sponsors had no role in design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the US government. All authors are independent of the study sponsors. Dr. May was supported by a HRB/NCI Health Economics Fellowship during this work. Dr. Garrido is supported by a Veterans Affairs HSR&D career development award (CDA 11-201/CDP 12-255). Dr. Kelley’s time was funded by the National Institute on Aging (1K23AG040774-01A1) and the American Federation for Aging. Dr. Smith is funded by the NCI Core Grant P 30 006973, 1-R01 CA177562-01A1, 1-R01 NR014050 01, and the Harry J. Duffey Family Endowment for Palliative Care. Dr. Morrison was the recipient of a Midcareer Investigator Award in Patient-Oriented Research (5K24AG022345) during the course of this work. This work was supported by the NIA, Claude D. Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai [5P30AG028741], and the National Palliative Care Research Center.
1. Soni A. Top 10 Most Costly Conditions Among Men and Women, 2008: Estimates for the U.S. Civilian Noninstitutionalized Adult Population, Age 18 and Older. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
2. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. PubMed
3. American Cancer Society. Cancer Facts and Figures 2015. Atlanta, GA: American Cancer Society; 2015.
4. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065. PubMed
5. Levit L, Balogh E, Nass S, Ganz PA, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: Institute of Medicine/National Academies Press; 2013. PubMed
7. Anderson GF. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
8. Tibi-Levy Y, Le Vaillant M, de Pouvourville G. Determinants of resource utilization in four palliative care units. Palliat Med. 2006;20(2):95-106. PubMed
9. Simoens S, Kutten B, Keirse E, et al. The costs of treating terminal patients. J Pain Symptom Manage. 2010;40(3):436-448. PubMed
10. Groeneveld I, Murtagh F, Kaloki Y, Bausewein C, Higginson I. Determinants of healthcare costs in the last year of life. Annual Assembly of American Academy of Hospice and Palliative Medicine & Hospice and Palliative Nurses Association; March 14, 2013; New Orleans, LA.
11. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures at the end of life for colorectal cancer decedents. J Womens Health. 2007;16(2):214-227. PubMed
12. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures and service utilization at the end of life for lung cancer decedents. Womens Health Issues. 2008;18(3):199-209. PubMed
13. Walker H, Anderson M, Farahati F, et al. Resource use and costs of end-of-life/palliative care: Ontario adult cancer patients dying during 2002 and 2003. J Palliat Care. 2011;27(2):79-88. PubMed
14. Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169(5):493-501. PubMed
15. Hanratty B, Burstrom B, Walander A, Whitehead M. Inequality in the face of death? Public expenditure on health care for different socioeconomic groups in the last year of life. J Health Serv Res Policy. 2007;12(2):90-94. PubMed
16. Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154(4):235-242. PubMed
17. Guerriere DN, Zagorski B, Fassbender K, Masucci L, Librach L, Coyte PC. Cost variations in ambulatory and home-based palliative care. Palliat Med. 2010;24(5):523-532. PubMed
18. US Department of Health and Human Services, National Institutes of Health. Palliative Care for Hospitalized Cancer Patients [project information]. Bethesda, MD: US Dept of Health and Human Services, National Institutes of Health; 2006. Project 5R01CA116227-04. https://projectreporter.nih.gov/project_info_description.cfm?projectnumber=5R01CA116227-04. Published 2006. Accessed August 1, 2015.
19. May P, Garrido MM, Cassel JB, et al. Prospective cohort study of hospital palliative care teams for inpatients with advanced cancer: earlier consultation is associated with larger cost-saving effect. J Clin Oncol. 2015;33(25):2745-2752. PubMed
20. May P, Garrido MM, Cassel JB, et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff. 2016;35(1):44-53. PubMed
21. May P, Garrido MM, Cassel JB, Morrison RS, Normand C. Using length of stay to control for unobserved heterogeneity when estimating treatment effect on hospital costs with observational data: issues of reliability, robustness and usefulness. Health Serv Res. 2016;51(5):2020-2043. PubMed
22. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. PubMed
23. Chang VT, Hwang SS, Kasimis B, Thaler HT. Shorter symptom assessment instruments: the Condensed Memorial Symptom Assessment Scale (CMSAS). Cancer Invest. 2004;22(4):526-536. PubMed
24. Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. The index of ADL: a standardized measure of biological and psychological function. JAMA. 1963;185(12):914-919. PubMed
25. McLaughlin MA, Orosz GM, Magaziner J, et al. Preoperative status and risk of complications in patients with hip fracture. J Gen Intern Med. 2006;21(3):219-225. PubMed
26. Taheri PA, Butz D, Griffes LC, Morlock DR, Greenfield LJ. Physician impact on the total cost of care. Ann Surg. 2000;231(3):432-435. PubMed
27. US Department of Veterans Affairs, Health Economics Resource Center. Determining costs. Washington, DC: US Dept of Veterans Affairs, Health Economics Resource Center; 2016. http://www.herc.research.va.gov/include/page.asp?id=determining-costs. Published 2016. Accessed September 7, 2016.
28. US Department of Health and Human Services, Center for Medicare & Medicaid Services. FY 2011 Wage Index [Table 2]. Baltimore, MD: US Dept of Health and Human Services, Center for Medicare & Medicaid Services; 2011. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/CMS1234173.html. Published 2011. Accessed September 2, 2014.
29. US Department of Labor, Bureau of Labor Statistics. All Urban Consumers (Current Series) [Consumer Price Index database]. US Dept of Labor, Bureau of Labor Statistics; 2015. http://www.bls.gov/cpi/data.htm. Published 2015. Accessed August 15, 2016.
30. Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465-488. PubMed
31. Jones AM, Rice N, Bago d’Uva T, Balia S. Applied Health Economics. 2nd ed. Oxford, England: Routledge; 2013.
32. Stata [computer program]. Version 12. College Station, TX: StataCorp; 2011.
33. Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing
propensity scores. Health Serv Res. 2014;49(5):1701-1720. PubMed
34. R Core Team. R: A Language and Environment for Statistical Computing. Vienna,
Austria: R Foundation for Statistical Computing; 2016.
35. Cassel JB, Kerr K, Pantilat S, Smith TJ. Palliative care consultation and hospital
length of stay. J Palliat Med. 2010;13(6):761-767. PubMed
36. US Department of Health and Human Services, Agency for Healthcare Research
and Quality. Efforts to Improve Patient Safety Result in 1.3 Million Fewer Patient
Harms: Interim Update on 2013 Annual Hospital-Acquired Condition Rate and
Estimates of Cost Savings and Deaths Averted From 2010 to 2013. Rockville,
MD: US Dept of Health and Human Services, Agency for Healthcare Research
and Quality; 2015. http://www.ahrq.gov/professionals/quality-patient-safety/pfp/
interimhacrate2013.html. Published 2015. Updated November 2015. Accessed
November 18, 2016.
37. Cassidy A. Health Policy Brief: Medicare’s Hospital-Acquired Condition Reduction
Program. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_
id=142. Published August 6, 2015. Accessed April 24, 2017.
38. Davis MA, Nallamothu BK, Banerjee M, Bynum JP. Identification of four unique
spending patterns among older adults in the last year of life challenges standard
assumptions. Health Aff. 2016;35(7):1316-1323. PubMed
39. Aldridge MD, Kelley AS. The myth regarding the high cost of end-of-life care.
Am J Public Health. 2015;105(12):2411-2415. PubMed
40. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard
oncology care: American Society of Clinical Oncology clinical practice guideline
update. J Clin Oncol. 2017;35(1):96-112. PubMed
41. Spetz J, Dudley N, Trupin L, Rogers M, Meier DE, Dumanovsky T. Few hospital
palliative care programs meet national staffing recommendations. Health Aff.
2016;35(9):1690-1697. PubMed
42. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities
in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. PubMed
43. HCUP [Healthcare Cost and Utilization Project] Elixhauser Comorbidity Software
[computer program]. Version 3.7. Rockville, MD: Agency for Healthcare
Research and Quality; 2016. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/
comorbidity.jsp. Published 2016. Accessed November 9, 2016.
44. Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for
administrative data. Med Care. 2012;50(12):1109-1118. PubMed
1. Soni A. Top 10 Most Costly Conditions Among Men and Women, 2008: Estimates for the U.S. Civilian Noninstitutionalized Adult Population, Age 18 and Older. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
2. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. PubMed
3. American Cancer Society. Cancer Facts and Figures 2015. Atlanta, GA: American Cancer Society; 2015.
4. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065. PubMed
5. Levit L, Balogh E, Nass S, Ganz PA, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: Institute of Medicine/National Academies Press; 2013. PubMed
7. Anderson GF. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
8. Tibi-Levy Y, Le Vaillant M, de Pouvourville G. Determinants of resource utilization in four palliative care units. Palliat Med. 2006;20(2):95-106. PubMed
9. Simoens S, Kutten B, Keirse E, et al. The costs of treating terminal patients. J Pain Symptom Manage. 2010;40(3):436-448. PubMed
10. Groeneveld I, Murtagh F, Kaloki Y, Bausewein C, Higginson I. Determinants of healthcare costs in the last year of life. Annual Assembly of American Academy of Hospice and Palliative Medicine & Hospice and Palliative Nurses Association; March 14, 2013; New Orleans, LA.
11. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures at the end of life for colorectal cancer decedents. J Womens Health. 2007;16(2):214-227. PubMed
12. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures and service utilization at the end of life for lung cancer decedents. Womens Health Issues. 2008;18(3):199-209. PubMed
13. Walker H, Anderson M, Farahati F, et al. Resource use and costs of end-of-life/palliative care: Ontario adult cancer patients dying during 2002 and 2003. J Palliat Care. 2011;27(2):79-88. PubMed
14. Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169(5):493-501. PubMed
15. Hanratty B, Burstrom B, Walander A, Whitehead M. Inequality in the face of death? Public expenditure on health care for different socioeconomic groups in the last year of life. J Health Serv Res Policy. 2007;12(2):90-94. PubMed
16. Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154(4):235-242. PubMed
17. Guerriere DN, Zagorski B, Fassbender K, Masucci L, Librach L, Coyte PC. Cost variations in ambulatory and home-based palliative care. Palliat Med. 2010;24(5):523-532. PubMed
18. US Department of Health and Human Services, National Institutes of Health. Palliative Care for Hospitalized Cancer Patients [project information]. Bethesda, MD: US Dept of Health and Human Services, National Institutes of Health; 2006. Project 5R01CA116227-04. https://projectreporter.nih.gov/project_info_description.cfm?projectnumber=5R01CA116227-04. Published 2006. Accessed August 1, 2015.
19. May P, Garrido MM, Cassel JB, et al. Prospective cohort study of hospital palliative care teams for inpatients with advanced cancer: earlier consultation is associated with larger cost-saving effect. J Clin Oncol. 2015;33(25):2745-2752. PubMed
20. May P, Garrido MM, Cassel JB, et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff. 2016;35(1):44-53. PubMed
21. May P, Garrido MM, Cassel JB, Morrison RS, Normand C. Using length of stay to control for unobserved heterogeneity when estimating treatment effect on hospital costs with observational data: issues of reliability, robustness and usefulness. Health Serv Res. 2016;51(5):2020-2043. PubMed
22. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. PubMed
23. Chang VT, Hwang SS, Kasimis B, Thaler HT. Shorter symptom assessment instruments: the Condensed Memorial Symptom Assessment Scale (CMSAS). Cancer Invest. 2004;22(4):526-536. PubMed
24. Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. The index of ADL: a standardized measure of biological and psychological function. JAMA. 1963;185(12):914-919. PubMed
25. McLaughlin MA, Orosz GM, Magaziner J, et al. Preoperative status and risk of complications in patients with hip fracture. J Gen Intern Med. 2006;21(3):219-225. PubMed
26. Taheri PA, Butz D, Griffes LC, Morlock DR, Greenfield LJ. Physician impact on the total cost of care. Ann Surg. 2000;231(3):432-435. PubMed
27. US Department of Veterans Affairs, Health Economics Resource Center. Determining costs. Washington, DC: US Dept of Veterans Affairs, Health Economics Resource Center; 2016. http://www.herc.research.va.gov/include/page.asp?id=determining-costs. Published 2016. Accessed September 7, 2016.
28. US Department of Health and Human Services, Center for Medicare & Medicaid Services. FY 2011 Wage Index [Table 2]. Baltimore, MD: US Dept of Health and Human Services, Center for Medicare & Medicaid Services; 2011. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/CMS1234173.html. Published 2011. Accessed September 2, 2014.
29. US Department of Labor, Bureau of Labor Statistics. All Urban Consumers (Current Series) [Consumer Price Index database]. US Dept of Labor, Bureau of Labor Statistics; 2015. http://www.bls.gov/cpi/data.htm. Published 2015. Accessed August 15, 2016.
30. Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465-488. PubMed
31. Jones AM, Rice N, Bago d’Uva T, Balia S. Applied Health Economics. 2nd ed. Oxford, England: Routledge; 2013.
32. Stata [computer program]. Version 12. College Station, TX: StataCorp; 2011.
33. Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing
propensity scores. Health Serv Res. 2014;49(5):1701-1720. PubMed
34. R Core Team. R: A Language and Environment for Statistical Computing. Vienna,
Austria: R Foundation for Statistical Computing; 2016.
35. Cassel JB, Kerr K, Pantilat S, Smith TJ. Palliative care consultation and hospital
length of stay. J Palliat Med. 2010;13(6):761-767. PubMed
36. US Department of Health and Human Services, Agency for Healthcare Research
and Quality. Efforts to Improve Patient Safety Result in 1.3 Million Fewer Patient
Harms: Interim Update on 2013 Annual Hospital-Acquired Condition Rate and
Estimates of Cost Savings and Deaths Averted From 2010 to 2013. Rockville,
MD: US Dept of Health and Human Services, Agency for Healthcare Research
and Quality; 2015. http://www.ahrq.gov/professionals/quality-patient-safety/pfp/
interimhacrate2013.html. Published 2015. Updated November 2015. Accessed
November 18, 2016.
37. Cassidy A. Health Policy Brief: Medicare’s Hospital-Acquired Condition Reduction
Program. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_
id=142. Published August 6, 2015. Accessed April 24, 2017.
38. Davis MA, Nallamothu BK, Banerjee M, Bynum JP. Identification of four unique
spending patterns among older adults in the last year of life challenges standard
assumptions. Health Aff. 2016;35(7):1316-1323. PubMed
39. Aldridge MD, Kelley AS. The myth regarding the high cost of end-of-life care.
Am J Public Health. 2015;105(12):2411-2415. PubMed
40. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard
oncology care: American Society of Clinical Oncology clinical practice guideline
update. J Clin Oncol. 2017;35(1):96-112. PubMed
41. Spetz J, Dudley N, Trupin L, Rogers M, Meier DE, Dumanovsky T. Few hospital
palliative care programs meet national staffing recommendations. Health Aff.
2016;35(9):1690-1697. PubMed
42. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities
in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. PubMed
43. HCUP [Healthcare Cost and Utilization Project] Elixhauser Comorbidity Software
[computer program]. Version 3.7. Rockville, MD: Agency for Healthcare
Research and Quality; 2016. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/
comorbidity.jsp. Published 2016. Accessed November 9, 2016.
44. Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for
administrative data. Med Care. 2012;50(12):1109-1118. PubMed
© 2017 Society of Hospital Medicine
Palliative Care in Hospitals
The field of palliative care has grown rapidly in recent years in response to patient need and clinician interest in effective approaches to managing chronic life‐threatening illness.1 This article reviews the clinical, educational, demographic, and financial imperatives driving this growth, describes the clinical components of palliative care and the range of service models available, defines the relationship of hospital‐based palliative care to hospice, summarizes the literature on palliative care outcomes, and presents practical resources for clinicians seeking knowledge and skills in the field.
DEFINITION
Palliative care is medical care focused on the relief of suffering and support for the best possible quality of life for patients facing serious, life‐threatening illness and their families. It aims to identify and address the physical, psychological, and practical burdens of illness. Palliative care in the United States grew out of the hospice movement that originated in both the United Kingdom and the United States about 30 years ago. Hospice care was developed specifically to address the needs of the dying and their families and was codified in the United States by the addition in 1983 of a federal Medicare benefit for hospice care. In the last 30 years the Medicare hospice benefit has enabled more than 7 million patients and their families to receive intensive palliative care for the terminally ill, primarily in the home. The growth in the number and needs of seriously and chronically ill patients who are not clearly terminally ill has led to the development of palliative care services outside the hospice benefit provided by Medicare (and other insurers). Both hospice and nonhospice professionals have participated in extending the hospice approach through development of palliative care services. Palliative care may be delivered simultaneously with all appropriate curative and life‐prolonging interventions. In practice, palliative care practitioners provide assessment and treatment of pain and other symptom distress; employ communication skills with patients, families, and colleagues; support complex medical decision making and goal setting based on identifying and respecting patient wishes and goals; and promote medically informed care coordination, continuity, and practical support for patients, family caregivers, and professional colleagues across healthcare settings and through the trajectory of an illness.1, 2
Palliative care is both a general approach to health care and a growing practice specialty for professionals committing most or all of their time to the delivery of palliative care services.3 The term palliative medicine refers to the physician discipline within the larger field of palliative care. As of 2005, more than 1890 physicians have received specialty certification through a palliative care credentialing exam given by the American Board of Hospice and Palliative Medicine.4 Formal recognition of the subspecialty is currently being sought in collaboration with the American Board of Medical Specialties.5 As of August 2005, there were more than 50 postgraduate palliative care subspecialty fellowship programs in the United States.6 Between 2000 and 2003, the American Hospital Association (AHA) annual survey recorded a 67% growth in the number of hospital‐based palliative care programs reported, from 632 to 1027, for a total of 25% of responding AHA member hospitals.7
REASONS FOR GROWTH IN PALLIATIVE CARE
A primary justification for the rapid growth in palliative care programs in institutional settings is the abundant data demonstrating the high prevalence of pain and symptom distress in hospitals,811 nursing homes,12, 13 and community settings.14 Virtually all persons with serious illness spend at least some time in a hospital, usually on multiple occasions, in the course of their disease or condition.15 Despite the finding that when polled more than 90% of Americans say they would prefer to die at home, more than 75% of adult deaths occur in institutional settings (hospital or nursing homes)more than 50% in hospitals and 25% in nursing homesand 85% of pediatric deaths occur in hospitals.16, 17 Further, more than half of persons older than age 85 die in a nursing home and 43% of persons older than age 65 reside in a long‐term care facility at some time before they die,1821 a figure projected to rise substantially over the next several decades. The much larger number of patients who are not dying but are living with chronic, debilitating, and life‐threatening illness also need expert symptom management, communication and decision‐making support, and coordination of care across settings. In one national survey, physicians reported that poor care coordination resulted in patient communication problems, lack of emotional support for patients, adverse drug reactions, unnecessary hospitalization, patients not functioning to potential, and unnecessary pain.22 In addition to studies demonstrating high degrees of symptom distress across all age groups in hospitalized and nursing home patients,814 other works have shown high use of burdensome, nonbeneficial technologies among the seriously ill,2327 caregiver burden on families,2831 and communication problems between these patients, their families, and their treating physicians about the goals of care and the medical decisions that should follow.32, 33 Other studies have reported broad dissatisfaction with the general quality of care for the seriously ill and dying in hospitals and nursing homes,18, 34 specifically, perceptions of impersonal and indifferent care. Several studies of patients and their families have identified relief of suffering, practical support needs, open communication, and opportunities to relieve burdens on and strengthen relationships with family as the top‐priority needs from the healthcare system.3440
The growth in the number and needs of the elderly with multiple chronic conditions who will turn to the healthcare system in coming years underscores the need to create a delivery system in the United States that can be responsive to these priorities. By 2030 the number of persons with chronic conditions will exceed 157 million.4144 With the possible exception of advanced cancer conditions (accounting for 24% of adult deaths), in which prognosis is somewhat more reliably linked to performance status,4243 prognostication of outcome is a highly inexact science for the chronically ill of all ages and in a range of diagnostic categories, including stroke, dementia, and end‐stage cardiac, renal, hepatic, and pulmonary diseases. This has been a major part of the impetus for the growth in palliative care services not predicated on a link to terminal prognoses.4143 Hospitals and nursing homes are under increasing pressure to structure care processes in a manner fitted to the needs of the seriously ill because of studies demonstrating poor quality of care, demands from patients and families, accreditation requirements, and the costs of care for this patient population. More than 95% of Medicare spending goes to the 63% of Medicare patients with two or more chronic conditions, and three quarters of Medicare dollars go to hospitals.44 Hospital costs have risen nearly 10% per year in each of the last 2 years, because of both the increasing numbers of patients turning to them for care and the growth in the number and expense of effective life‐prolonging therapies. These forces have stimulated the development of new models for the efficient and effective care of patients with serious and complex illness.2227, 44
CLINICAL COMPONENTS
The three primary domains of palliative care clinical practice are assessment and treatment of pain and other symptom distress, including psychiatric symptoms64; communication about goals of care and support for complex medical decision making; and provision of practical and psychosocial support, care coordination, and continuity, as well as bereavement services if death occurs.1, 2, 65 Palliative care specialists work to support primary and specialist physicians in the care of complex and seriously ill patients by providing intensive bedside treatment and reassessment of multiple‐symptom distress, by helping with time‐consuming and difficult interactions with distressed patients and family members, and by attempting to ensure a seamless, safe, and well‐communicated discharge and follow‐up process after the patient leaves the hospital.66 Resources for physicians seeking more knowledge or training in the treatment of symptom distress and other aspects of palliative care are given in Table 1.
| Palliative care clinical competencies |
|---|
|
|
Education on Palliative and End of Life Care ( |
|
End of Life/Palliative Education Resource Center ( |
|
Department of Pain Medicine and Palliative Medicine at Beth Israel Medical Center ( |
|
|
|
American Academy of Hospice and Palliative Medicine ( |
|
American Board of Hospice and Palliative Medicine ( |
|
Center for Palliative Care at Harvard Medical School ( |
|
National Consensus Project on Quality Palliative Care ( |
|
American Geriatrics Society ( |
| Palliative care program development |
|
Center to Advance Palliative Care ( |
|
Palliative Care Leadership Centers ( |
|
Promoting Excellence in End of Life Care ( |
The core components of symptom management67, 68 include: 1) Routine and repeated formal assessment, without which most symptoms will be neither identified nor addressed; 2) Expertise in prescribing, including the safe use of opioid analgesics, adjuvant approaches to pain management, and management of a wide range of other common and distressing symptoms and syndromes including, for example, delirium, dyspnea, fatigue, nausea, bowel obstruction, and depression69; and 3) Skillful management of treatment side effects, which is required to successfully control symptoms.
Communication skills and effective support for making decisions about clinical care goals include not only fundamental physician responsibilities such as communicating bad news and elucidating patient wishes for future care, but also the ability to promote communication and consensus about care goals among multiple specialist consultants, to address and resolve disagreements and conflicts among patients, families, and providers about goals of care, and to assist in the evolving process of balancing the benefits with the burdens of various medical interventions.32, 7073
The great majority of care for an illness is provided at home by family members neither trained nor emotionally prepared for these responsibilities.51, 74 The burden on family caregivers is one of the top concerns of seriously ill patients.35 Patients and families often struggle with anxieties about doing the wrong thing, difficulty traveling to physicians' offices, social isolation, and a high prevalence of preventable suffering of all types.3440 Palliative care clinicians attempt to improve the success and sustainability of the discharge plan by providing medically informed and therefore more appropriate care management recommendations and by mobilizing a range of community resources to increase the likelihood that families will be able to manage the care at home with the necessary supports and backups in place, including appropriate screening and referrals for complicated grief and bereavement.51, 75, 76 Several small prospective studies of palliative care have suggested that palliative care has resulted in reduction in the number of emergency department visits and hospitalizations and in the length of hospital stays, presumably because of the efficacy and comprehensiveness of care coordination in averting crises.54, 55, 61, 9798
CLINICAL MODELS
Given the multifaceted approach needed to support patient quality of life throughout advanced illness, one profession or individual cannot be expected to provide all aspects of palliative care. As described in the recently completed National Consensus Project Guidelines for Quality Palliative Care,2 specialty‐level palliative care is optimally delivered through an interdisciplinary team consisting of appropriately trained and credentialed physicians, nurses, and social workers with additional support and contributions from chaplains, rehabilitative experts, psychiatrists, and other professionals as indicated. Clearly, however, the staffing of a palliative care program will depend critically on the needs and capacities of the setting. A full interdisciplinary team is needed for a large tertiary‐care teaching hospital, whereas a part‐time advance‐practice nurse with backup from colleagues as needed may suffice for a small rural hospital or long‐term care setting. Specialist‐level palliative care is delivered through a range of clinical models and settings, including inpatient consultation services, dedicated inpatient units, and outpatient practices, among others.77, 78 Programs within the United States are housed in a range of clinical subspecialties including oncology, geriatrics, nursing, case management, hospitalist, and other programs, depending on the locus of leadership and administrative support.77, 78 Most programs are supported by utilizing diverse sources,77 including physician and nurse‐practitioner billing through insurers such as Medicare Part B,53, 81 as well as hospital support typically predicated on cost avoidance analyses, foundation and other grants, and philanthropy. Detailed guidance on appropriate documentation and billing for palliative care physician services may be found in Schapiro et al.,53 von Gunten,79 and on the Web site of the Center to Advance Palliative Care (
RELATIONSHIP TO HOSPICE
Although new clinical specialties in palliative medicine and nursing are emerging, in the United States palliative care for those in the terminal stages of illness has been delivered through hospice programs for more than 30 years. Under current regulatory and payment guidelines hospice care is delivered to patients who are certified by their physicians as likely to die within 6 months if the disease follows its usual course and who are willing to give up insurance coverage for medical treatment primarily focused on cure or prolongation of life. It is noteworthy that there is great variability among United States hospices, with some able to support continued disease‐modifying treatments such as chemotherapy and radiation if a patient so desires.2 Hospice programs aim to create increased opportunity for death at home, focusing on symptom control and the psychological and spiritual issues that are paramount to persons in the terminal phases of illness. Once the hospice benefit has been accessed, patients and families receive comprehensive case‐managed services across all settings of care (although the great majority of hospice care is delivered at home) from an interdisciplinary team, coverage for medications and equipment related to the terminal illness, and practical, psychosocial, respite, and bereavement support for caregivers.80, 81 Several recent studies have confirmed the findings of an earlier work82 in demonstrating the beneficial outcomes of hospice care including reduced mortality in spouses and high levels of family satisfaction.18, 83 Palliative care programs based in both hospital and community settings have led to increases in hospice referral rates and hospice length of stay, promoting continuity of palliative care and the intensive palliation and family support needed as death approaches.55 Coordination and partnerships between palliative care and hospice programs are critical to achieving continuity of palliative care throughout the full course of an illness and across the continuum of care settings.2
IMPACT OF PALLIATIVE CARE ON QUALITY OF CARE
Reports on palliative care specialist services utilizing diverse models and approaches have suggested a range of benefits from palliative care, including reduced pain4547 and other symptom distress,45, 48, 49 improved health‐related quality of life,95 high patient and family satisfaction18, 4951, 96 with care and with physician communication, and increased likelihood of the location of death being outside a hospital.33, 49, 52, 9799
Because it can help to demonstrate care structures, processes, and outcomes associated with improved quality (such as routine assessment of pain in the hospital), a palliative care program may help hospitals measure and meet Joint Commission for Accreditation of Healthcare Organizations (JCAHO) requirements in the domains of pain management, communication, family and patient education, and continuity of care, among others.53 Several groups have reported marked increases in hospice referral rate and hospice length of stay as a result of hospital‐ and nursing‐home‐based palliative care programs, presumably as a result of enhanced case identification, counseling, and referral processes.54, 55 Case control and observational studies of palliative care and ethics consultation services have demonstrated reductions in costs per day and in hospital and ICU lengths of stay, presumably because of enhanced support for discussions about the goals of care and the resulting facilitation of patient and family decisions about the types and settings of future care.50, 5561 Hospitals have begun to invest in palliative care services, both to enhance quality of care and because of their measurable impact on reducing ICU and total bed days and their efficacy in supporting transitions from high‐intensity, high‐cost hospital settings to more appropriate and desired care settings, such as the home.5563, 9798 Observational studies have yielded no differences in mortality between patients receiving palliative care and controls receiving the usual care.48, 55, 56
EDUCATION IN PALLIATIVE CARE
Curricular content on palliative care has been noticeably lacking from medical and nursing education curricula, textbooks, and certifying examinations, although this is beginning to change.8491 Both the Liaison Committee for Medical Education (LCME) and the Accreditation Council for Graduate Medical Education (ACGME) now require or strongly encourage programs to provide under‐ and postgraduate training in palliative care in order to be accredited.89, 90 As of 2005, more than 50% of teaching hospitals had established palliative care clinical services,92 which constitute the necessary platform for clinical training. The rapid growth in the availability of postgraduate fellowship training in palliative medicine will produce the faculty leaders needed for these educational and research programs in medical school and residency training programs.93, 94 Physicians in practice may gain knowledge and skills through a range of national courses and Web‐based resources and through preparation for the certifying exam given annually by the American Board of Hospice and Palliative Medicine4 (Table 1).
CONCLUSIONS
The growth in palliative care specialists and programs in hospitals in the United States represents a grass roots professional response to the needs of a patient population with chronic advanced illnesses and family care burdens within a healthcare system structured to provide care for acute intercurrent illness. Rapid increases in the number of new hospital programs, as well as early studies indicating improved clinical, satisfaction, and utilization outcomes, suggest that palliative care services are likely to become a routine and well‐integrated part of the healthcare continuum in the United States over the next several years. A number of resources are available to healthcare professionals seeking more training as well as to hospitals or nursing homes wishing to establish their own clinical or educational programs. Such programs have provided a platform for both newly graduated and seasoned professionals to continue to serve the needs of their patients through the assessment and relief of suffering, provided simultaneously with efforts to cure or mitigate disease.
- ,.Clinical practice: palliative care.N Engl J Med.2004;350:2582–2590.
- National Consensus Project for Quality Palliative Care: The development of practice guidelines 2004. Available from URL:http://www.nationalconsensusproject.org. [accessed August 10, 2005].
- ,.Palliative medicine: an emerging field of specialization.Cancer Invest.2000;18:761–767.
- American Board of Hospice and Palliative Medicine. Available from URL:http://www.abhpm.org[accessed August 10, 2005].
- ,,, et al.Physician board certification in hospice and palliative medicine.J Palliat Med.2000;3:441–447.
- American Academy of Hospice and Palliative Medicine. Available from URL:http://www.aahpm.org[accessed August 10, 2005].
- American Hospital Association. Hospital Statistics 2004. Available from URL:http://www.ahastatistics.org[accessed August 10, 2005].
- ,,.Pain and satisfaction with pain control in hospitalized medical patients.Arch Intern Med.2004;164:175–180.
- ,,, et al.Pain and discomfort associated with common hospital procedures and experiences.J Pain Symptom Manage.1998;15:91–101.
- ,,, et al. The symptom burden of seriously ill hospitalized patients.J Pain Symptom Manage.1999;17:248–255.
- A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT).The SUPPORT Principal Investigators.JAMA.1995;274:1591–1598.
- ,,, et al.Persistent pain in nursing home residents.JAMA.2001;285:2081.
- ,,, et al.Management of pain in elderly patients with cancer. SAGE Study Group. Systematic assessment of geriatric drug use via epidemiology.JAMA.1998;279:1877–1882.
- ,,, et al.Pain and its treatment in outpatients with metastatic cancer.N Engl J Med.1994;330:592–596.
- Dartmouth Atlas. Available from URL: http://www.dartmouthatlas.org/endoflife/end_of_life.php[accessed August 10, 2005].
- Institute of Medicine.Approaching death: improving care at the end of life.Washington, DC:National Academy Press,1997.
- Institute of Medicine.When Children die: improving palliative and end of life care for children and their families.Washington, DC:National Academies Press,2002.
- ,,, et al.Family perspectives on end‐of‐life care at the last place of care.JAMA.2004;291:88–93.
- . Brown Atlas. Available from URL:http://www.chcr.brown.edu/dying/brownatlas.htm[accessed August 10, 2005].
- .Creating excellent palliative care in nursing homes.J Palliat Med.2003;6:7–9.
- ,,, et al.Needs of the dying in nursing homes.J Palliat Med.2002;5:895–901.
- Mathematica Policy Research, Inc.National public engagement campaign on chronic illness—physician survey, final report.Princeton, NJ:Mathematica Policy Research, Inc.,2001.
- ,,,.Patterns of use of common major procedures in medical care of older adults.J Am Geriatr Soc.1999;47:553–558.
- ,.Dying to pay: the cost of end of life care.J Palliat Care.1998;14:5–15.
- ,,, et al.Older age, aggressiveness of care, and survival for seriously ill, hospitalized adults. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments.Ann Intern Med.1999;131:721–728.
- .Demands of an aging population for critical care and pulmonary services.JAMA.2001;285:1016–1017.
- ,,,.Medicare beneficiaries' costs of care in the last year of life.Health Aff.2001;20:188–195.
- ,,,.Stress in caregivers of hospitalized oldest‐old patients.J Gerontol A Biol Sci Med Sci.2001;56:M231–M235.
- ,.Caregiving as a risk factor for mortality: the Caregiver Health Effects Study.JAMA.1999;282:2215–2219.
- ,,,,,.Assistance from family members, friends, paid care givers, and volunteers in the care of terminally ill patients.N Engl J Med.1999;341:956–963.
- ,,, et al.The impact of serious illness on patients' families.JAMA.1994;272:1839–1844.
- .Doctor–patient communication. In:Morrison RS,Meier DE, editors.Geriatric palliative care.New York:Oxford University Press,2003.
- ,.Communicating sad, bad, and difficult news in medicine.Lancet.2004;363:312–319.
- ,,,.Understanding economic and other burdens of terminal illness: the experience of patients and their caregivers.Ann Intern Med.2000;132:451–459.
- ,,.Quality end‐of‐life care: patients' perspectives.JAMA.1999;281:163–168.
- ,,, et al.Preparing for the end of life: preferences of patients, families, physicians, and other care providers.J Pain Symptom Manage.2001;22:727–737.
- ,,, et al.Factors considered important at the end of life by patients, family, physicians, and other care providers.JAMA.2000;284:2476–2482.
- ,,,,,.In search of a good death: observations of patients, families, and providers.Ann Intern Med.2000;132:825–832.
- ,,, et al.Measurement of quality of care and quality of life at the end of life.Gerontologist.2002;42:71–80.
- ,,, et al.Family reports of barriers to optimal care of the dying.Nurs Res.2000;49:310–317.
- ,,, et al.Patterns of functional decline at the end of life.JAMA.2003;289:2387–2392.
- ,, Cohn F, et al. Prognoses of seriously ill hospitalized patients on the days before death: implications for patient care and public policy.New Horizons.1997;5:56–61.
- ,,, et al.The last 2 years of life: functional trajectories of frail older people.J Am Geriatr Soc.2003;51:492–498.
- Partnership for Solutions. Chronic Conditions:Making the Case for Ongoing Care.Baltimore:Johns Hopkins University,2002.
- ,,, et al.Is there evidence that palliative care teams alter end‐of‐life experiences of patients and their caregivers?J Pain Symptom Manage.2003;25:150–168.
- ,,, et al.Implementing guidelines for cancer pain management: results of a randomized controlled clinical trial.J Clin Oncol.1999;17:361–370.
- ,,, et al.Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug‐related toxicity, and survival.J Clin Oncol2002;20:4040–4049.
- ,,, et al.The comprehensive care team: a controlled trial of outpatient palliative medicine consultation.Arch Intern Med.2004;164:83–91.
- ,,, et al.Palliative care consultations: how do they impact the care of hospitalized patients?J Pain Symptom Manage.2000;20:166–173.
- ,,, et al.An intensive communication intervention for the critically ill.Am J Med.2000;109:469–475.
- ,,.The moderating influence of service use on negative caregiving consequences.J Gerontol B Psychol Sci Soc Sci.1996;51:S121–131.
- ,,.Communication skills training for health care professionals working with cancer patients, their families and/or carers (Cochrane Review).The Cochrane Library. Chichester, UK:John Wiley 21:1412–1415.
- ,,, et al. Living and dying well with cancer: Successfully integrating palliative care and cancer treatment. Available from URL:http://www.promotingexcellence.org[accessed August 10, 2005].
- ,,, et al.A high‐volume specialist palliative care unit and team may reduce in‐hospital end‐of‐life care costs.J Palliat Med.2003;6:699–705.
- ,,, et al.Effect of ethics consultations on nonbeneficial life‐sustaining treatments in the intensive care setting.JAMA.2003;290:1166–1172.
- ,.Impact of a proactive approach to improve end‐of‐life care in a medical ICU.Chest.2003;123:266–271.
- ,,, et al.A randomized controlled trial of the cost‐effectiveness of a district co‐ordinating service for terminally ill cancer patients.Palliat Med.1996;10:151–161.
- ,,, et al.The impact of a regional palliative care program on the cost of palliative care delivery.J Palliat Med.1999;3:181–186.
- ,,.Effectiveness of a home‐based palliative care program for end‐of‐life.J Palliat Med.2003;6:715–724.
- ,,.A study of proactive ethics consultation for critically and terminally ill patients with extended lengths of stay.Crit Care Med.1998;26:252–259.
- ,.Experience with an end‐of‐life practice at a university hospital.Crit Care Med.1997;25:197–202.
- .Perspectives on care at the close of life. Psychological considerations, growth, and transcendence at the end of life: the art of the possible.JAMA.2001;285:2898–2905.
- ,,.Improving palliative care.Ann Intern Med.1997;127:225–230.
- .Completing the continuum of cancer care: integrating life‐prolongation and palliation.CA Cancer J Clin.2000;50:123–132.
- ,.Pain management: pharmacological approaches.Cancer Treat Res.1999;100:1–29.
- ,.Pain and symptom management in palliative care.Cancer Control.1996;3:204–213.
- .ABC of palliative care. Anorexia, cachexia, and nutrition.BMJ.1997;315:1219–1222.
- .Perspectives on care at the close of life. Initiating end‐of‐life discussions with seriously ill patients: addressing the “elephant in the room.”JAMA.2000;284:2502–2507.
- ,,.“I wish things were different”: expressing wishes in response to loss, futility, and unrealistic hopes.Ann Intern Med.2001;135:551–555.
- ,,.Discussing palliative care with patients. ACP‐ASIM End‐of‐Life Care Consensus Panel.Ann Intern Med.1999;130:744–749.
- ,,.The patient‐physician relationship. Ensuring competency in end‐of‐life care: communication and relational skills.JAMA.2000;284:3051–3057.
- .The loneliness of the long‐term care giver.N Engl J Med.1999;340:1587–1590.
- ,,,,,.Integrating case management and palliative care.J Palliat Med.2004;7:121–136.
- ,,.The influence of caregiving and bereavement support on adjusting to an older relative's death.Gerontologist.1991;31:32–42.
- Center to Advance Palliative Care. A guide to developing a hospital‐based palliative care program. Available from URL:http://www.capc.org[accessed August 10, 2005].
- .Secondary and tertiary palliative care in US hospitals.JAMA.2002;287:875–881.
- .Coding and reimbursement mechanisms for physician services in hospice and palliative care.J Palliat Med.2000;2:157–164.
- National Hospice and Palliative Care Organization. NHPCO facts and figures. Available from URL:http://www.nhpco.org[accessed August 10, 2005].
- .When pain and suffering do not require a prognosis: Working toward meaningful hospital–hospice partnership.J Palliat Med.2003;6:109–115.
- ,,, et al.An alternative in terminal care: results of the National Hospice Study.J Chronic Dis.1986;39:9–26.
- ,.The health impact of health care on families: a matched cohort study of hospice use by decedents and mortality outcomes in surviving, widowed spouses.Soc Sci Med.2003;57:465–475.
- ,.Educational programs in US medical schools, 2002–2003.JAMA.2003;290:1190–1196.
- .Medical education in end‐of‐life care: the status of reform.J Palliat Med.2002;5:243–248.
- ,.ACGME requirements for end‐of‐life training in selected residency and fellowship programs: a status report.Acad Med.2002;77:299–304.
- ,,, et al.Recommendations for incorporating palliative care education into the acute care hospital setting.Acad Med.1999;74:871–877.
- ,,.The status of medical education in end‐of‐life care: a national report.J Gen Intern Med.2003;18:685–695.
- Liaison Committee on Medical Education. Available from URL: http://www.lcme.org[accessed August 10, 2005].
- Accreditation Council for Graduate Medical Education.Program requirements for residency education in the subspecialties of internal medicine. Graduate Medical Education Directory 2000–2001. Chicago,2000.
- ,.Palliative care in undergraduate medical education. Status report and future directions.JAMA.1997;278:733–738.
- ,.Survey of palliative care programs in United States teaching hospitals.J Palliat Med.2001;4:309–314.
- ,,, et al.Initial voluntary program standards for fellowship training in palliative medicine.J Palliat Med.2002;5:23–33.
- American Academy of Hospice and Palliative Medicine. Fellowship Program Directory. Available from URL:http://www.aahpm.org/fellowship/directory/htm[accessed August 10, 2005].
- ,,, et al.Quality of life in palliative cancer care. Results from a cluster randomized trial.J Clin Oncol.2001;19:3884–3894.
- ,,.Family satisfaction with end‐of‐life care for cancer patients in a cluster randomized trial.J Pain Symptom Manage.2002;24:53–63.
- ,,, et al.A palliative care intervention and death at home: a cluster randomized trial.Lancet.2000;356:888–893.
- ,,.Impact of palliative care case management on resource use by patients dying of cancer at a Veterans Affairs medical center.J Palliat Med.2005;8:26–35.
- ,,.Family satisfaction with end‐of‐life care for cancer patients in a cluster randomized trial.J Pain Symptom Manage.2002;24:53–63
The field of palliative care has grown rapidly in recent years in response to patient need and clinician interest in effective approaches to managing chronic life‐threatening illness.1 This article reviews the clinical, educational, demographic, and financial imperatives driving this growth, describes the clinical components of palliative care and the range of service models available, defines the relationship of hospital‐based palliative care to hospice, summarizes the literature on palliative care outcomes, and presents practical resources for clinicians seeking knowledge and skills in the field.
DEFINITION
Palliative care is medical care focused on the relief of suffering and support for the best possible quality of life for patients facing serious, life‐threatening illness and their families. It aims to identify and address the physical, psychological, and practical burdens of illness. Palliative care in the United States grew out of the hospice movement that originated in both the United Kingdom and the United States about 30 years ago. Hospice care was developed specifically to address the needs of the dying and their families and was codified in the United States by the addition in 1983 of a federal Medicare benefit for hospice care. In the last 30 years the Medicare hospice benefit has enabled more than 7 million patients and their families to receive intensive palliative care for the terminally ill, primarily in the home. The growth in the number and needs of seriously and chronically ill patients who are not clearly terminally ill has led to the development of palliative care services outside the hospice benefit provided by Medicare (and other insurers). Both hospice and nonhospice professionals have participated in extending the hospice approach through development of palliative care services. Palliative care may be delivered simultaneously with all appropriate curative and life‐prolonging interventions. In practice, palliative care practitioners provide assessment and treatment of pain and other symptom distress; employ communication skills with patients, families, and colleagues; support complex medical decision making and goal setting based on identifying and respecting patient wishes and goals; and promote medically informed care coordination, continuity, and practical support for patients, family caregivers, and professional colleagues across healthcare settings and through the trajectory of an illness.1, 2
Palliative care is both a general approach to health care and a growing practice specialty for professionals committing most or all of their time to the delivery of palliative care services.3 The term palliative medicine refers to the physician discipline within the larger field of palliative care. As of 2005, more than 1890 physicians have received specialty certification through a palliative care credentialing exam given by the American Board of Hospice and Palliative Medicine.4 Formal recognition of the subspecialty is currently being sought in collaboration with the American Board of Medical Specialties.5 As of August 2005, there were more than 50 postgraduate palliative care subspecialty fellowship programs in the United States.6 Between 2000 and 2003, the American Hospital Association (AHA) annual survey recorded a 67% growth in the number of hospital‐based palliative care programs reported, from 632 to 1027, for a total of 25% of responding AHA member hospitals.7
REASONS FOR GROWTH IN PALLIATIVE CARE
A primary justification for the rapid growth in palliative care programs in institutional settings is the abundant data demonstrating the high prevalence of pain and symptom distress in hospitals,811 nursing homes,12, 13 and community settings.14 Virtually all persons with serious illness spend at least some time in a hospital, usually on multiple occasions, in the course of their disease or condition.15 Despite the finding that when polled more than 90% of Americans say they would prefer to die at home, more than 75% of adult deaths occur in institutional settings (hospital or nursing homes)more than 50% in hospitals and 25% in nursing homesand 85% of pediatric deaths occur in hospitals.16, 17 Further, more than half of persons older than age 85 die in a nursing home and 43% of persons older than age 65 reside in a long‐term care facility at some time before they die,1821 a figure projected to rise substantially over the next several decades. The much larger number of patients who are not dying but are living with chronic, debilitating, and life‐threatening illness also need expert symptom management, communication and decision‐making support, and coordination of care across settings. In one national survey, physicians reported that poor care coordination resulted in patient communication problems, lack of emotional support for patients, adverse drug reactions, unnecessary hospitalization, patients not functioning to potential, and unnecessary pain.22 In addition to studies demonstrating high degrees of symptom distress across all age groups in hospitalized and nursing home patients,814 other works have shown high use of burdensome, nonbeneficial technologies among the seriously ill,2327 caregiver burden on families,2831 and communication problems between these patients, their families, and their treating physicians about the goals of care and the medical decisions that should follow.32, 33 Other studies have reported broad dissatisfaction with the general quality of care for the seriously ill and dying in hospitals and nursing homes,18, 34 specifically, perceptions of impersonal and indifferent care. Several studies of patients and their families have identified relief of suffering, practical support needs, open communication, and opportunities to relieve burdens on and strengthen relationships with family as the top‐priority needs from the healthcare system.3440
The growth in the number and needs of the elderly with multiple chronic conditions who will turn to the healthcare system in coming years underscores the need to create a delivery system in the United States that can be responsive to these priorities. By 2030 the number of persons with chronic conditions will exceed 157 million.4144 With the possible exception of advanced cancer conditions (accounting for 24% of adult deaths), in which prognosis is somewhat more reliably linked to performance status,4243 prognostication of outcome is a highly inexact science for the chronically ill of all ages and in a range of diagnostic categories, including stroke, dementia, and end‐stage cardiac, renal, hepatic, and pulmonary diseases. This has been a major part of the impetus for the growth in palliative care services not predicated on a link to terminal prognoses.4143 Hospitals and nursing homes are under increasing pressure to structure care processes in a manner fitted to the needs of the seriously ill because of studies demonstrating poor quality of care, demands from patients and families, accreditation requirements, and the costs of care for this patient population. More than 95% of Medicare spending goes to the 63% of Medicare patients with two or more chronic conditions, and three quarters of Medicare dollars go to hospitals.44 Hospital costs have risen nearly 10% per year in each of the last 2 years, because of both the increasing numbers of patients turning to them for care and the growth in the number and expense of effective life‐prolonging therapies. These forces have stimulated the development of new models for the efficient and effective care of patients with serious and complex illness.2227, 44
CLINICAL COMPONENTS
The three primary domains of palliative care clinical practice are assessment and treatment of pain and other symptom distress, including psychiatric symptoms64; communication about goals of care and support for complex medical decision making; and provision of practical and psychosocial support, care coordination, and continuity, as well as bereavement services if death occurs.1, 2, 65 Palliative care specialists work to support primary and specialist physicians in the care of complex and seriously ill patients by providing intensive bedside treatment and reassessment of multiple‐symptom distress, by helping with time‐consuming and difficult interactions with distressed patients and family members, and by attempting to ensure a seamless, safe, and well‐communicated discharge and follow‐up process after the patient leaves the hospital.66 Resources for physicians seeking more knowledge or training in the treatment of symptom distress and other aspects of palliative care are given in Table 1.
| Palliative care clinical competencies |
|---|
|
|
Education on Palliative and End of Life Care ( |
|
End of Life/Palliative Education Resource Center ( |
|
Department of Pain Medicine and Palliative Medicine at Beth Israel Medical Center ( |
|
|
|
American Academy of Hospice and Palliative Medicine ( |
|
American Board of Hospice and Palliative Medicine ( |
|
Center for Palliative Care at Harvard Medical School ( |
|
National Consensus Project on Quality Palliative Care ( |
|
American Geriatrics Society ( |
| Palliative care program development |
|
Center to Advance Palliative Care ( |
|
Palliative Care Leadership Centers ( |
|
Promoting Excellence in End of Life Care ( |
The core components of symptom management67, 68 include: 1) Routine and repeated formal assessment, without which most symptoms will be neither identified nor addressed; 2) Expertise in prescribing, including the safe use of opioid analgesics, adjuvant approaches to pain management, and management of a wide range of other common and distressing symptoms and syndromes including, for example, delirium, dyspnea, fatigue, nausea, bowel obstruction, and depression69; and 3) Skillful management of treatment side effects, which is required to successfully control symptoms.
Communication skills and effective support for making decisions about clinical care goals include not only fundamental physician responsibilities such as communicating bad news and elucidating patient wishes for future care, but also the ability to promote communication and consensus about care goals among multiple specialist consultants, to address and resolve disagreements and conflicts among patients, families, and providers about goals of care, and to assist in the evolving process of balancing the benefits with the burdens of various medical interventions.32, 7073
The great majority of care for an illness is provided at home by family members neither trained nor emotionally prepared for these responsibilities.51, 74 The burden on family caregivers is one of the top concerns of seriously ill patients.35 Patients and families often struggle with anxieties about doing the wrong thing, difficulty traveling to physicians' offices, social isolation, and a high prevalence of preventable suffering of all types.3440 Palliative care clinicians attempt to improve the success and sustainability of the discharge plan by providing medically informed and therefore more appropriate care management recommendations and by mobilizing a range of community resources to increase the likelihood that families will be able to manage the care at home with the necessary supports and backups in place, including appropriate screening and referrals for complicated grief and bereavement.51, 75, 76 Several small prospective studies of palliative care have suggested that palliative care has resulted in reduction in the number of emergency department visits and hospitalizations and in the length of hospital stays, presumably because of the efficacy and comprehensiveness of care coordination in averting crises.54, 55, 61, 9798
CLINICAL MODELS
Given the multifaceted approach needed to support patient quality of life throughout advanced illness, one profession or individual cannot be expected to provide all aspects of palliative care. As described in the recently completed National Consensus Project Guidelines for Quality Palliative Care,2 specialty‐level palliative care is optimally delivered through an interdisciplinary team consisting of appropriately trained and credentialed physicians, nurses, and social workers with additional support and contributions from chaplains, rehabilitative experts, psychiatrists, and other professionals as indicated. Clearly, however, the staffing of a palliative care program will depend critically on the needs and capacities of the setting. A full interdisciplinary team is needed for a large tertiary‐care teaching hospital, whereas a part‐time advance‐practice nurse with backup from colleagues as needed may suffice for a small rural hospital or long‐term care setting. Specialist‐level palliative care is delivered through a range of clinical models and settings, including inpatient consultation services, dedicated inpatient units, and outpatient practices, among others.77, 78 Programs within the United States are housed in a range of clinical subspecialties including oncology, geriatrics, nursing, case management, hospitalist, and other programs, depending on the locus of leadership and administrative support.77, 78 Most programs are supported by utilizing diverse sources,77 including physician and nurse‐practitioner billing through insurers such as Medicare Part B,53, 81 as well as hospital support typically predicated on cost avoidance analyses, foundation and other grants, and philanthropy. Detailed guidance on appropriate documentation and billing for palliative care physician services may be found in Schapiro et al.,53 von Gunten,79 and on the Web site of the Center to Advance Palliative Care (
RELATIONSHIP TO HOSPICE
Although new clinical specialties in palliative medicine and nursing are emerging, in the United States palliative care for those in the terminal stages of illness has been delivered through hospice programs for more than 30 years. Under current regulatory and payment guidelines hospice care is delivered to patients who are certified by their physicians as likely to die within 6 months if the disease follows its usual course and who are willing to give up insurance coverage for medical treatment primarily focused on cure or prolongation of life. It is noteworthy that there is great variability among United States hospices, with some able to support continued disease‐modifying treatments such as chemotherapy and radiation if a patient so desires.2 Hospice programs aim to create increased opportunity for death at home, focusing on symptom control and the psychological and spiritual issues that are paramount to persons in the terminal phases of illness. Once the hospice benefit has been accessed, patients and families receive comprehensive case‐managed services across all settings of care (although the great majority of hospice care is delivered at home) from an interdisciplinary team, coverage for medications and equipment related to the terminal illness, and practical, psychosocial, respite, and bereavement support for caregivers.80, 81 Several recent studies have confirmed the findings of an earlier work82 in demonstrating the beneficial outcomes of hospice care including reduced mortality in spouses and high levels of family satisfaction.18, 83 Palliative care programs based in both hospital and community settings have led to increases in hospice referral rates and hospice length of stay, promoting continuity of palliative care and the intensive palliation and family support needed as death approaches.55 Coordination and partnerships between palliative care and hospice programs are critical to achieving continuity of palliative care throughout the full course of an illness and across the continuum of care settings.2
IMPACT OF PALLIATIVE CARE ON QUALITY OF CARE
Reports on palliative care specialist services utilizing diverse models and approaches have suggested a range of benefits from palliative care, including reduced pain4547 and other symptom distress,45, 48, 49 improved health‐related quality of life,95 high patient and family satisfaction18, 4951, 96 with care and with physician communication, and increased likelihood of the location of death being outside a hospital.33, 49, 52, 9799
Because it can help to demonstrate care structures, processes, and outcomes associated with improved quality (such as routine assessment of pain in the hospital), a palliative care program may help hospitals measure and meet Joint Commission for Accreditation of Healthcare Organizations (JCAHO) requirements in the domains of pain management, communication, family and patient education, and continuity of care, among others.53 Several groups have reported marked increases in hospice referral rate and hospice length of stay as a result of hospital‐ and nursing‐home‐based palliative care programs, presumably as a result of enhanced case identification, counseling, and referral processes.54, 55 Case control and observational studies of palliative care and ethics consultation services have demonstrated reductions in costs per day and in hospital and ICU lengths of stay, presumably because of enhanced support for discussions about the goals of care and the resulting facilitation of patient and family decisions about the types and settings of future care.50, 5561 Hospitals have begun to invest in palliative care services, both to enhance quality of care and because of their measurable impact on reducing ICU and total bed days and their efficacy in supporting transitions from high‐intensity, high‐cost hospital settings to more appropriate and desired care settings, such as the home.5563, 9798 Observational studies have yielded no differences in mortality between patients receiving palliative care and controls receiving the usual care.48, 55, 56
EDUCATION IN PALLIATIVE CARE
Curricular content on palliative care has been noticeably lacking from medical and nursing education curricula, textbooks, and certifying examinations, although this is beginning to change.8491 Both the Liaison Committee for Medical Education (LCME) and the Accreditation Council for Graduate Medical Education (ACGME) now require or strongly encourage programs to provide under‐ and postgraduate training in palliative care in order to be accredited.89, 90 As of 2005, more than 50% of teaching hospitals had established palliative care clinical services,92 which constitute the necessary platform for clinical training. The rapid growth in the availability of postgraduate fellowship training in palliative medicine will produce the faculty leaders needed for these educational and research programs in medical school and residency training programs.93, 94 Physicians in practice may gain knowledge and skills through a range of national courses and Web‐based resources and through preparation for the certifying exam given annually by the American Board of Hospice and Palliative Medicine4 (Table 1).
CONCLUSIONS
The growth in palliative care specialists and programs in hospitals in the United States represents a grass roots professional response to the needs of a patient population with chronic advanced illnesses and family care burdens within a healthcare system structured to provide care for acute intercurrent illness. Rapid increases in the number of new hospital programs, as well as early studies indicating improved clinical, satisfaction, and utilization outcomes, suggest that palliative care services are likely to become a routine and well‐integrated part of the healthcare continuum in the United States over the next several years. A number of resources are available to healthcare professionals seeking more training as well as to hospitals or nursing homes wishing to establish their own clinical or educational programs. Such programs have provided a platform for both newly graduated and seasoned professionals to continue to serve the needs of their patients through the assessment and relief of suffering, provided simultaneously with efforts to cure or mitigate disease.
The field of palliative care has grown rapidly in recent years in response to patient need and clinician interest in effective approaches to managing chronic life‐threatening illness.1 This article reviews the clinical, educational, demographic, and financial imperatives driving this growth, describes the clinical components of palliative care and the range of service models available, defines the relationship of hospital‐based palliative care to hospice, summarizes the literature on palliative care outcomes, and presents practical resources for clinicians seeking knowledge and skills in the field.
DEFINITION
Palliative care is medical care focused on the relief of suffering and support for the best possible quality of life for patients facing serious, life‐threatening illness and their families. It aims to identify and address the physical, psychological, and practical burdens of illness. Palliative care in the United States grew out of the hospice movement that originated in both the United Kingdom and the United States about 30 years ago. Hospice care was developed specifically to address the needs of the dying and their families and was codified in the United States by the addition in 1983 of a federal Medicare benefit for hospice care. In the last 30 years the Medicare hospice benefit has enabled more than 7 million patients and their families to receive intensive palliative care for the terminally ill, primarily in the home. The growth in the number and needs of seriously and chronically ill patients who are not clearly terminally ill has led to the development of palliative care services outside the hospice benefit provided by Medicare (and other insurers). Both hospice and nonhospice professionals have participated in extending the hospice approach through development of palliative care services. Palliative care may be delivered simultaneously with all appropriate curative and life‐prolonging interventions. In practice, palliative care practitioners provide assessment and treatment of pain and other symptom distress; employ communication skills with patients, families, and colleagues; support complex medical decision making and goal setting based on identifying and respecting patient wishes and goals; and promote medically informed care coordination, continuity, and practical support for patients, family caregivers, and professional colleagues across healthcare settings and through the trajectory of an illness.1, 2
Palliative care is both a general approach to health care and a growing practice specialty for professionals committing most or all of their time to the delivery of palliative care services.3 The term palliative medicine refers to the physician discipline within the larger field of palliative care. As of 2005, more than 1890 physicians have received specialty certification through a palliative care credentialing exam given by the American Board of Hospice and Palliative Medicine.4 Formal recognition of the subspecialty is currently being sought in collaboration with the American Board of Medical Specialties.5 As of August 2005, there were more than 50 postgraduate palliative care subspecialty fellowship programs in the United States.6 Between 2000 and 2003, the American Hospital Association (AHA) annual survey recorded a 67% growth in the number of hospital‐based palliative care programs reported, from 632 to 1027, for a total of 25% of responding AHA member hospitals.7
REASONS FOR GROWTH IN PALLIATIVE CARE
A primary justification for the rapid growth in palliative care programs in institutional settings is the abundant data demonstrating the high prevalence of pain and symptom distress in hospitals,811 nursing homes,12, 13 and community settings.14 Virtually all persons with serious illness spend at least some time in a hospital, usually on multiple occasions, in the course of their disease or condition.15 Despite the finding that when polled more than 90% of Americans say they would prefer to die at home, more than 75% of adult deaths occur in institutional settings (hospital or nursing homes)more than 50% in hospitals and 25% in nursing homesand 85% of pediatric deaths occur in hospitals.16, 17 Further, more than half of persons older than age 85 die in a nursing home and 43% of persons older than age 65 reside in a long‐term care facility at some time before they die,1821 a figure projected to rise substantially over the next several decades. The much larger number of patients who are not dying but are living with chronic, debilitating, and life‐threatening illness also need expert symptom management, communication and decision‐making support, and coordination of care across settings. In one national survey, physicians reported that poor care coordination resulted in patient communication problems, lack of emotional support for patients, adverse drug reactions, unnecessary hospitalization, patients not functioning to potential, and unnecessary pain.22 In addition to studies demonstrating high degrees of symptom distress across all age groups in hospitalized and nursing home patients,814 other works have shown high use of burdensome, nonbeneficial technologies among the seriously ill,2327 caregiver burden on families,2831 and communication problems between these patients, their families, and their treating physicians about the goals of care and the medical decisions that should follow.32, 33 Other studies have reported broad dissatisfaction with the general quality of care for the seriously ill and dying in hospitals and nursing homes,18, 34 specifically, perceptions of impersonal and indifferent care. Several studies of patients and their families have identified relief of suffering, practical support needs, open communication, and opportunities to relieve burdens on and strengthen relationships with family as the top‐priority needs from the healthcare system.3440
The growth in the number and needs of the elderly with multiple chronic conditions who will turn to the healthcare system in coming years underscores the need to create a delivery system in the United States that can be responsive to these priorities. By 2030 the number of persons with chronic conditions will exceed 157 million.4144 With the possible exception of advanced cancer conditions (accounting for 24% of adult deaths), in which prognosis is somewhat more reliably linked to performance status,4243 prognostication of outcome is a highly inexact science for the chronically ill of all ages and in a range of diagnostic categories, including stroke, dementia, and end‐stage cardiac, renal, hepatic, and pulmonary diseases. This has been a major part of the impetus for the growth in palliative care services not predicated on a link to terminal prognoses.4143 Hospitals and nursing homes are under increasing pressure to structure care processes in a manner fitted to the needs of the seriously ill because of studies demonstrating poor quality of care, demands from patients and families, accreditation requirements, and the costs of care for this patient population. More than 95% of Medicare spending goes to the 63% of Medicare patients with two or more chronic conditions, and three quarters of Medicare dollars go to hospitals.44 Hospital costs have risen nearly 10% per year in each of the last 2 years, because of both the increasing numbers of patients turning to them for care and the growth in the number and expense of effective life‐prolonging therapies. These forces have stimulated the development of new models for the efficient and effective care of patients with serious and complex illness.2227, 44
CLINICAL COMPONENTS
The three primary domains of palliative care clinical practice are assessment and treatment of pain and other symptom distress, including psychiatric symptoms64; communication about goals of care and support for complex medical decision making; and provision of practical and psychosocial support, care coordination, and continuity, as well as bereavement services if death occurs.1, 2, 65 Palliative care specialists work to support primary and specialist physicians in the care of complex and seriously ill patients by providing intensive bedside treatment and reassessment of multiple‐symptom distress, by helping with time‐consuming and difficult interactions with distressed patients and family members, and by attempting to ensure a seamless, safe, and well‐communicated discharge and follow‐up process after the patient leaves the hospital.66 Resources for physicians seeking more knowledge or training in the treatment of symptom distress and other aspects of palliative care are given in Table 1.
| Palliative care clinical competencies |
|---|
|
|
Education on Palliative and End of Life Care ( |
|
End of Life/Palliative Education Resource Center ( |
|
Department of Pain Medicine and Palliative Medicine at Beth Israel Medical Center ( |
|
|
|
American Academy of Hospice and Palliative Medicine ( |
|
American Board of Hospice and Palliative Medicine ( |
|
Center for Palliative Care at Harvard Medical School ( |
|
National Consensus Project on Quality Palliative Care ( |
|
American Geriatrics Society ( |
| Palliative care program development |
|
Center to Advance Palliative Care ( |
|
Palliative Care Leadership Centers ( |
|
Promoting Excellence in End of Life Care ( |
The core components of symptom management67, 68 include: 1) Routine and repeated formal assessment, without which most symptoms will be neither identified nor addressed; 2) Expertise in prescribing, including the safe use of opioid analgesics, adjuvant approaches to pain management, and management of a wide range of other common and distressing symptoms and syndromes including, for example, delirium, dyspnea, fatigue, nausea, bowel obstruction, and depression69; and 3) Skillful management of treatment side effects, which is required to successfully control symptoms.
Communication skills and effective support for making decisions about clinical care goals include not only fundamental physician responsibilities such as communicating bad news and elucidating patient wishes for future care, but also the ability to promote communication and consensus about care goals among multiple specialist consultants, to address and resolve disagreements and conflicts among patients, families, and providers about goals of care, and to assist in the evolving process of balancing the benefits with the burdens of various medical interventions.32, 7073
The great majority of care for an illness is provided at home by family members neither trained nor emotionally prepared for these responsibilities.51, 74 The burden on family caregivers is one of the top concerns of seriously ill patients.35 Patients and families often struggle with anxieties about doing the wrong thing, difficulty traveling to physicians' offices, social isolation, and a high prevalence of preventable suffering of all types.3440 Palliative care clinicians attempt to improve the success and sustainability of the discharge plan by providing medically informed and therefore more appropriate care management recommendations and by mobilizing a range of community resources to increase the likelihood that families will be able to manage the care at home with the necessary supports and backups in place, including appropriate screening and referrals for complicated grief and bereavement.51, 75, 76 Several small prospective studies of palliative care have suggested that palliative care has resulted in reduction in the number of emergency department visits and hospitalizations and in the length of hospital stays, presumably because of the efficacy and comprehensiveness of care coordination in averting crises.54, 55, 61, 9798
CLINICAL MODELS
Given the multifaceted approach needed to support patient quality of life throughout advanced illness, one profession or individual cannot be expected to provide all aspects of palliative care. As described in the recently completed National Consensus Project Guidelines for Quality Palliative Care,2 specialty‐level palliative care is optimally delivered through an interdisciplinary team consisting of appropriately trained and credentialed physicians, nurses, and social workers with additional support and contributions from chaplains, rehabilitative experts, psychiatrists, and other professionals as indicated. Clearly, however, the staffing of a palliative care program will depend critically on the needs and capacities of the setting. A full interdisciplinary team is needed for a large tertiary‐care teaching hospital, whereas a part‐time advance‐practice nurse with backup from colleagues as needed may suffice for a small rural hospital or long‐term care setting. Specialist‐level palliative care is delivered through a range of clinical models and settings, including inpatient consultation services, dedicated inpatient units, and outpatient practices, among others.77, 78 Programs within the United States are housed in a range of clinical subspecialties including oncology, geriatrics, nursing, case management, hospitalist, and other programs, depending on the locus of leadership and administrative support.77, 78 Most programs are supported by utilizing diverse sources,77 including physician and nurse‐practitioner billing through insurers such as Medicare Part B,53, 81 as well as hospital support typically predicated on cost avoidance analyses, foundation and other grants, and philanthropy. Detailed guidance on appropriate documentation and billing for palliative care physician services may be found in Schapiro et al.,53 von Gunten,79 and on the Web site of the Center to Advance Palliative Care (
RELATIONSHIP TO HOSPICE
Although new clinical specialties in palliative medicine and nursing are emerging, in the United States palliative care for those in the terminal stages of illness has been delivered through hospice programs for more than 30 years. Under current regulatory and payment guidelines hospice care is delivered to patients who are certified by their physicians as likely to die within 6 months if the disease follows its usual course and who are willing to give up insurance coverage for medical treatment primarily focused on cure or prolongation of life. It is noteworthy that there is great variability among United States hospices, with some able to support continued disease‐modifying treatments such as chemotherapy and radiation if a patient so desires.2 Hospice programs aim to create increased opportunity for death at home, focusing on symptom control and the psychological and spiritual issues that are paramount to persons in the terminal phases of illness. Once the hospice benefit has been accessed, patients and families receive comprehensive case‐managed services across all settings of care (although the great majority of hospice care is delivered at home) from an interdisciplinary team, coverage for medications and equipment related to the terminal illness, and practical, psychosocial, respite, and bereavement support for caregivers.80, 81 Several recent studies have confirmed the findings of an earlier work82 in demonstrating the beneficial outcomes of hospice care including reduced mortality in spouses and high levels of family satisfaction.18, 83 Palliative care programs based in both hospital and community settings have led to increases in hospice referral rates and hospice length of stay, promoting continuity of palliative care and the intensive palliation and family support needed as death approaches.55 Coordination and partnerships between palliative care and hospice programs are critical to achieving continuity of palliative care throughout the full course of an illness and across the continuum of care settings.2
IMPACT OF PALLIATIVE CARE ON QUALITY OF CARE
Reports on palliative care specialist services utilizing diverse models and approaches have suggested a range of benefits from palliative care, including reduced pain4547 and other symptom distress,45, 48, 49 improved health‐related quality of life,95 high patient and family satisfaction18, 4951, 96 with care and with physician communication, and increased likelihood of the location of death being outside a hospital.33, 49, 52, 9799
Because it can help to demonstrate care structures, processes, and outcomes associated with improved quality (such as routine assessment of pain in the hospital), a palliative care program may help hospitals measure and meet Joint Commission for Accreditation of Healthcare Organizations (JCAHO) requirements in the domains of pain management, communication, family and patient education, and continuity of care, among others.53 Several groups have reported marked increases in hospice referral rate and hospice length of stay as a result of hospital‐ and nursing‐home‐based palliative care programs, presumably as a result of enhanced case identification, counseling, and referral processes.54, 55 Case control and observational studies of palliative care and ethics consultation services have demonstrated reductions in costs per day and in hospital and ICU lengths of stay, presumably because of enhanced support for discussions about the goals of care and the resulting facilitation of patient and family decisions about the types and settings of future care.50, 5561 Hospitals have begun to invest in palliative care services, both to enhance quality of care and because of their measurable impact on reducing ICU and total bed days and their efficacy in supporting transitions from high‐intensity, high‐cost hospital settings to more appropriate and desired care settings, such as the home.5563, 9798 Observational studies have yielded no differences in mortality between patients receiving palliative care and controls receiving the usual care.48, 55, 56
EDUCATION IN PALLIATIVE CARE
Curricular content on palliative care has been noticeably lacking from medical and nursing education curricula, textbooks, and certifying examinations, although this is beginning to change.8491 Both the Liaison Committee for Medical Education (LCME) and the Accreditation Council for Graduate Medical Education (ACGME) now require or strongly encourage programs to provide under‐ and postgraduate training in palliative care in order to be accredited.89, 90 As of 2005, more than 50% of teaching hospitals had established palliative care clinical services,92 which constitute the necessary platform for clinical training. The rapid growth in the availability of postgraduate fellowship training in palliative medicine will produce the faculty leaders needed for these educational and research programs in medical school and residency training programs.93, 94 Physicians in practice may gain knowledge and skills through a range of national courses and Web‐based resources and through preparation for the certifying exam given annually by the American Board of Hospice and Palliative Medicine4 (Table 1).
CONCLUSIONS
The growth in palliative care specialists and programs in hospitals in the United States represents a grass roots professional response to the needs of a patient population with chronic advanced illnesses and family care burdens within a healthcare system structured to provide care for acute intercurrent illness. Rapid increases in the number of new hospital programs, as well as early studies indicating improved clinical, satisfaction, and utilization outcomes, suggest that palliative care services are likely to become a routine and well‐integrated part of the healthcare continuum in the United States over the next several years. A number of resources are available to healthcare professionals seeking more training as well as to hospitals or nursing homes wishing to establish their own clinical or educational programs. Such programs have provided a platform for both newly graduated and seasoned professionals to continue to serve the needs of their patients through the assessment and relief of suffering, provided simultaneously with efforts to cure or mitigate disease.
- ,.Clinical practice: palliative care.N Engl J Med.2004;350:2582–2590.
- National Consensus Project for Quality Palliative Care: The development of practice guidelines 2004. Available from URL:http://www.nationalconsensusproject.org. [accessed August 10, 2005].
- ,.Palliative medicine: an emerging field of specialization.Cancer Invest.2000;18:761–767.
- American Board of Hospice and Palliative Medicine. Available from URL:http://www.abhpm.org[accessed August 10, 2005].
- ,,, et al.Physician board certification in hospice and palliative medicine.J Palliat Med.2000;3:441–447.
- American Academy of Hospice and Palliative Medicine. Available from URL:http://www.aahpm.org[accessed August 10, 2005].
- American Hospital Association. Hospital Statistics 2004. Available from URL:http://www.ahastatistics.org[accessed August 10, 2005].
- ,,.Pain and satisfaction with pain control in hospitalized medical patients.Arch Intern Med.2004;164:175–180.
- ,,, et al.Pain and discomfort associated with common hospital procedures and experiences.J Pain Symptom Manage.1998;15:91–101.
- ,,, et al. The symptom burden of seriously ill hospitalized patients.J Pain Symptom Manage.1999;17:248–255.
- A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT).The SUPPORT Principal Investigators.JAMA.1995;274:1591–1598.
- ,,, et al.Persistent pain in nursing home residents.JAMA.2001;285:2081.
- ,,, et al.Management of pain in elderly patients with cancer. SAGE Study Group. Systematic assessment of geriatric drug use via epidemiology.JAMA.1998;279:1877–1882.
- ,,, et al.Pain and its treatment in outpatients with metastatic cancer.N Engl J Med.1994;330:592–596.
- Dartmouth Atlas. Available from URL: http://www.dartmouthatlas.org/endoflife/end_of_life.php[accessed August 10, 2005].
- Institute of Medicine.Approaching death: improving care at the end of life.Washington, DC:National Academy Press,1997.
- Institute of Medicine.When Children die: improving palliative and end of life care for children and their families.Washington, DC:National Academies Press,2002.
- ,,, et al.Family perspectives on end‐of‐life care at the last place of care.JAMA.2004;291:88–93.
- . Brown Atlas. Available from URL:http://www.chcr.brown.edu/dying/brownatlas.htm[accessed August 10, 2005].
- .Creating excellent palliative care in nursing homes.J Palliat Med.2003;6:7–9.
- ,,, et al.Needs of the dying in nursing homes.J Palliat Med.2002;5:895–901.
- Mathematica Policy Research, Inc.National public engagement campaign on chronic illness—physician survey, final report.Princeton, NJ:Mathematica Policy Research, Inc.,2001.
- ,,,.Patterns of use of common major procedures in medical care of older adults.J Am Geriatr Soc.1999;47:553–558.
- ,.Dying to pay: the cost of end of life care.J Palliat Care.1998;14:5–15.
- ,,, et al.Older age, aggressiveness of care, and survival for seriously ill, hospitalized adults. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments.Ann Intern Med.1999;131:721–728.
- .Demands of an aging population for critical care and pulmonary services.JAMA.2001;285:1016–1017.
- ,,,.Medicare beneficiaries' costs of care in the last year of life.Health Aff.2001;20:188–195.
- ,,,.Stress in caregivers of hospitalized oldest‐old patients.J Gerontol A Biol Sci Med Sci.2001;56:M231–M235.
- ,.Caregiving as a risk factor for mortality: the Caregiver Health Effects Study.JAMA.1999;282:2215–2219.
- ,,,,,.Assistance from family members, friends, paid care givers, and volunteers in the care of terminally ill patients.N Engl J Med.1999;341:956–963.
- ,,, et al.The impact of serious illness on patients' families.JAMA.1994;272:1839–1844.
- .Doctor–patient communication. In:Morrison RS,Meier DE, editors.Geriatric palliative care.New York:Oxford University Press,2003.
- ,.Communicating sad, bad, and difficult news in medicine.Lancet.2004;363:312–319.
- ,,,.Understanding economic and other burdens of terminal illness: the experience of patients and their caregivers.Ann Intern Med.2000;132:451–459.
- ,,.Quality end‐of‐life care: patients' perspectives.JAMA.1999;281:163–168.
- ,,, et al.Preparing for the end of life: preferences of patients, families, physicians, and other care providers.J Pain Symptom Manage.2001;22:727–737.
- ,,, et al.Factors considered important at the end of life by patients, family, physicians, and other care providers.JAMA.2000;284:2476–2482.
- ,,,,,.In search of a good death: observations of patients, families, and providers.Ann Intern Med.2000;132:825–832.
- ,,, et al.Measurement of quality of care and quality of life at the end of life.Gerontologist.2002;42:71–80.
- ,,, et al.Family reports of barriers to optimal care of the dying.Nurs Res.2000;49:310–317.
- ,,, et al.Patterns of functional decline at the end of life.JAMA.2003;289:2387–2392.
- ,, Cohn F, et al. Prognoses of seriously ill hospitalized patients on the days before death: implications for patient care and public policy.New Horizons.1997;5:56–61.
- ,,, et al.The last 2 years of life: functional trajectories of frail older people.J Am Geriatr Soc.2003;51:492–498.
- Partnership for Solutions. Chronic Conditions:Making the Case for Ongoing Care.Baltimore:Johns Hopkins University,2002.
- ,,, et al.Is there evidence that palliative care teams alter end‐of‐life experiences of patients and their caregivers?J Pain Symptom Manage.2003;25:150–168.
- ,,, et al.Implementing guidelines for cancer pain management: results of a randomized controlled clinical trial.J Clin Oncol.1999;17:361–370.
- ,,, et al.Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug‐related toxicity, and survival.J Clin Oncol2002;20:4040–4049.
- ,,, et al.The comprehensive care team: a controlled trial of outpatient palliative medicine consultation.Arch Intern Med.2004;164:83–91.
- ,,, et al.Palliative care consultations: how do they impact the care of hospitalized patients?J Pain Symptom Manage.2000;20:166–173.
- ,,, et al.An intensive communication intervention for the critically ill.Am J Med.2000;109:469–475.
- ,,.The moderating influence of service use on negative caregiving consequences.J Gerontol B Psychol Sci Soc Sci.1996;51:S121–131.
- ,,.Communication skills training for health care professionals working with cancer patients, their families and/or carers (Cochrane Review).The Cochrane Library. Chichester, UK:John Wiley 21:1412–1415.
- ,,, et al. Living and dying well with cancer: Successfully integrating palliative care and cancer treatment. Available from URL:http://www.promotingexcellence.org[accessed August 10, 2005].
- ,,, et al.A high‐volume specialist palliative care unit and team may reduce in‐hospital end‐of‐life care costs.J Palliat Med.2003;6:699–705.
- ,,, et al.Effect of ethics consultations on nonbeneficial life‐sustaining treatments in the intensive care setting.JAMA.2003;290:1166–1172.
- ,.Impact of a proactive approach to improve end‐of‐life care in a medical ICU.Chest.2003;123:266–271.
- ,,, et al.A randomized controlled trial of the cost‐effectiveness of a district co‐ordinating service for terminally ill cancer patients.Palliat Med.1996;10:151–161.
- ,,, et al.The impact of a regional palliative care program on the cost of palliative care delivery.J Palliat Med.1999;3:181–186.
- ,,.Effectiveness of a home‐based palliative care program for end‐of‐life.J Palliat Med.2003;6:715–724.
- ,,.A study of proactive ethics consultation for critically and terminally ill patients with extended lengths of stay.Crit Care Med.1998;26:252–259.
- ,.Experience with an end‐of‐life practice at a university hospital.Crit Care Med.1997;25:197–202.
- .Perspectives on care at the close of life. Psychological considerations, growth, and transcendence at the end of life: the art of the possible.JAMA.2001;285:2898–2905.
- ,,.Improving palliative care.Ann Intern Med.1997;127:225–230.
- .Completing the continuum of cancer care: integrating life‐prolongation and palliation.CA Cancer J Clin.2000;50:123–132.
- ,.Pain management: pharmacological approaches.Cancer Treat Res.1999;100:1–29.
- ,.Pain and symptom management in palliative care.Cancer Control.1996;3:204–213.
- .ABC of palliative care. Anorexia, cachexia, and nutrition.BMJ.1997;315:1219–1222.
- .Perspectives on care at the close of life. Initiating end‐of‐life discussions with seriously ill patients: addressing the “elephant in the room.”JAMA.2000;284:2502–2507.
- ,,.“I wish things were different”: expressing wishes in response to loss, futility, and unrealistic hopes.Ann Intern Med.2001;135:551–555.
- ,,.Discussing palliative care with patients. ACP‐ASIM End‐of‐Life Care Consensus Panel.Ann Intern Med.1999;130:744–749.
- ,,.The patient‐physician relationship. Ensuring competency in end‐of‐life care: communication and relational skills.JAMA.2000;284:3051–3057.
- .The loneliness of the long‐term care giver.N Engl J Med.1999;340:1587–1590.
- ,,,,,.Integrating case management and palliative care.J Palliat Med.2004;7:121–136.
- ,,.The influence of caregiving and bereavement support on adjusting to an older relative's death.Gerontologist.1991;31:32–42.
- Center to Advance Palliative Care. A guide to developing a hospital‐based palliative care program. Available from URL:http://www.capc.org[accessed August 10, 2005].
- .Secondary and tertiary palliative care in US hospitals.JAMA.2002;287:875–881.
- .Coding and reimbursement mechanisms for physician services in hospice and palliative care.J Palliat Med.2000;2:157–164.
- National Hospice and Palliative Care Organization. NHPCO facts and figures. Available from URL:http://www.nhpco.org[accessed August 10, 2005].
- .When pain and suffering do not require a prognosis: Working toward meaningful hospital–hospice partnership.J Palliat Med.2003;6:109–115.
- ,,, et al.An alternative in terminal care: results of the National Hospice Study.J Chronic Dis.1986;39:9–26.
- ,.The health impact of health care on families: a matched cohort study of hospice use by decedents and mortality outcomes in surviving, widowed spouses.Soc Sci Med.2003;57:465–475.
- ,.Educational programs in US medical schools, 2002–2003.JAMA.2003;290:1190–1196.
- .Medical education in end‐of‐life care: the status of reform.J Palliat Med.2002;5:243–248.
- ,.ACGME requirements for end‐of‐life training in selected residency and fellowship programs: a status report.Acad Med.2002;77:299–304.
- ,,, et al.Recommendations for incorporating palliative care education into the acute care hospital setting.Acad Med.1999;74:871–877.
- ,,.The status of medical education in end‐of‐life care: a national report.J Gen Intern Med.2003;18:685–695.
- Liaison Committee on Medical Education. Available from URL: http://www.lcme.org[accessed August 10, 2005].
- Accreditation Council for Graduate Medical Education.Program requirements for residency education in the subspecialties of internal medicine. Graduate Medical Education Directory 2000–2001. Chicago,2000.
- ,.Palliative care in undergraduate medical education. Status report and future directions.JAMA.1997;278:733–738.
- ,.Survey of palliative care programs in United States teaching hospitals.J Palliat Med.2001;4:309–314.
- ,,, et al.Initial voluntary program standards for fellowship training in palliative medicine.J Palliat Med.2002;5:23–33.
- American Academy of Hospice and Palliative Medicine. Fellowship Program Directory. Available from URL:http://www.aahpm.org/fellowship/directory/htm[accessed August 10, 2005].
- ,,, et al.Quality of life in palliative cancer care. Results from a cluster randomized trial.J Clin Oncol.2001;19:3884–3894.
- ,,.Family satisfaction with end‐of‐life care for cancer patients in a cluster randomized trial.J Pain Symptom Manage.2002;24:53–63.
- ,,, et al.A palliative care intervention and death at home: a cluster randomized trial.Lancet.2000;356:888–893.
- ,,.Impact of palliative care case management on resource use by patients dying of cancer at a Veterans Affairs medical center.J Palliat Med.2005;8:26–35.
- ,,.Family satisfaction with end‐of‐life care for cancer patients in a cluster randomized trial.J Pain Symptom Manage.2002;24:53–63
- ,.Clinical practice: palliative care.N Engl J Med.2004;350:2582–2590.
- National Consensus Project for Quality Palliative Care: The development of practice guidelines 2004. Available from URL:http://www.nationalconsensusproject.org. [accessed August 10, 2005].
- ,.Palliative medicine: an emerging field of specialization.Cancer Invest.2000;18:761–767.
- American Board of Hospice and Palliative Medicine. Available from URL:http://www.abhpm.org[accessed August 10, 2005].
- ,,, et al.Physician board certification in hospice and palliative medicine.J Palliat Med.2000;3:441–447.
- American Academy of Hospice and Palliative Medicine. Available from URL:http://www.aahpm.org[accessed August 10, 2005].
- American Hospital Association. Hospital Statistics 2004. Available from URL:http://www.ahastatistics.org[accessed August 10, 2005].
- ,,.Pain and satisfaction with pain control in hospitalized medical patients.Arch Intern Med.2004;164:175–180.
- ,,, et al.Pain and discomfort associated with common hospital procedures and experiences.J Pain Symptom Manage.1998;15:91–101.
- ,,, et al. The symptom burden of seriously ill hospitalized patients.J Pain Symptom Manage.1999;17:248–255.
- A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT).The SUPPORT Principal Investigators.JAMA.1995;274:1591–1598.
- ,,, et al.Persistent pain in nursing home residents.JAMA.2001;285:2081.
- ,,, et al.Management of pain in elderly patients with cancer. SAGE Study Group. Systematic assessment of geriatric drug use via epidemiology.JAMA.1998;279:1877–1882.
- ,,, et al.Pain and its treatment in outpatients with metastatic cancer.N Engl J Med.1994;330:592–596.
- Dartmouth Atlas. Available from URL: http://www.dartmouthatlas.org/endoflife/end_of_life.php[accessed August 10, 2005].
- Institute of Medicine.Approaching death: improving care at the end of life.Washington, DC:National Academy Press,1997.
- Institute of Medicine.When Children die: improving palliative and end of life care for children and their families.Washington, DC:National Academies Press,2002.
- ,,, et al.Family perspectives on end‐of‐life care at the last place of care.JAMA.2004;291:88–93.
- . Brown Atlas. Available from URL:http://www.chcr.brown.edu/dying/brownatlas.htm[accessed August 10, 2005].
- .Creating excellent palliative care in nursing homes.J Palliat Med.2003;6:7–9.
- ,,, et al.Needs of the dying in nursing homes.J Palliat Med.2002;5:895–901.
- Mathematica Policy Research, Inc.National public engagement campaign on chronic illness—physician survey, final report.Princeton, NJ:Mathematica Policy Research, Inc.,2001.
- ,,,.Patterns of use of common major procedures in medical care of older adults.J Am Geriatr Soc.1999;47:553–558.
- ,.Dying to pay: the cost of end of life care.J Palliat Care.1998;14:5–15.
- ,,, et al.Older age, aggressiveness of care, and survival for seriously ill, hospitalized adults. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments.Ann Intern Med.1999;131:721–728.
- .Demands of an aging population for critical care and pulmonary services.JAMA.2001;285:1016–1017.
- ,,,.Medicare beneficiaries' costs of care in the last year of life.Health Aff.2001;20:188–195.
- ,,,.Stress in caregivers of hospitalized oldest‐old patients.J Gerontol A Biol Sci Med Sci.2001;56:M231–M235.
- ,.Caregiving as a risk factor for mortality: the Caregiver Health Effects Study.JAMA.1999;282:2215–2219.
- ,,,,,.Assistance from family members, friends, paid care givers, and volunteers in the care of terminally ill patients.N Engl J Med.1999;341:956–963.
- ,,, et al.The impact of serious illness on patients' families.JAMA.1994;272:1839–1844.
- .Doctor–patient communication. In:Morrison RS,Meier DE, editors.Geriatric palliative care.New York:Oxford University Press,2003.
- ,.Communicating sad, bad, and difficult news in medicine.Lancet.2004;363:312–319.
- ,,,.Understanding economic and other burdens of terminal illness: the experience of patients and their caregivers.Ann Intern Med.2000;132:451–459.
- ,,.Quality end‐of‐life care: patients' perspectives.JAMA.1999;281:163–168.
- ,,, et al.Preparing for the end of life: preferences of patients, families, physicians, and other care providers.J Pain Symptom Manage.2001;22:727–737.
- ,,, et al.Factors considered important at the end of life by patients, family, physicians, and other care providers.JAMA.2000;284:2476–2482.
- ,,,,,.In search of a good death: observations of patients, families, and providers.Ann Intern Med.2000;132:825–832.
- ,,, et al.Measurement of quality of care and quality of life at the end of life.Gerontologist.2002;42:71–80.
- ,,, et al.Family reports of barriers to optimal care of the dying.Nurs Res.2000;49:310–317.
- ,,, et al.Patterns of functional decline at the end of life.JAMA.2003;289:2387–2392.
- ,, Cohn F, et al. Prognoses of seriously ill hospitalized patients on the days before death: implications for patient care and public policy.New Horizons.1997;5:56–61.
- ,,, et al.The last 2 years of life: functional trajectories of frail older people.J Am Geriatr Soc.2003;51:492–498.
- Partnership for Solutions. Chronic Conditions:Making the Case for Ongoing Care.Baltimore:Johns Hopkins University,2002.
- ,,, et al.Is there evidence that palliative care teams alter end‐of‐life experiences of patients and their caregivers?J Pain Symptom Manage.2003;25:150–168.
- ,,, et al.Implementing guidelines for cancer pain management: results of a randomized controlled clinical trial.J Clin Oncol.1999;17:361–370.
- ,,, et al.Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug‐related toxicity, and survival.J Clin Oncol2002;20:4040–4049.
- ,,, et al.The comprehensive care team: a controlled trial of outpatient palliative medicine consultation.Arch Intern Med.2004;164:83–91.
- ,,, et al.Palliative care consultations: how do they impact the care of hospitalized patients?J Pain Symptom Manage.2000;20:166–173.
- ,,, et al.An intensive communication intervention for the critically ill.Am J Med.2000;109:469–475.
- ,,.The moderating influence of service use on negative caregiving consequences.J Gerontol B Psychol Sci Soc Sci.1996;51:S121–131.
- ,,.Communication skills training for health care professionals working with cancer patients, their families and/or carers (Cochrane Review).The Cochrane Library. Chichester, UK:John Wiley 21:1412–1415.
- ,,, et al. Living and dying well with cancer: Successfully integrating palliative care and cancer treatment. Available from URL:http://www.promotingexcellence.org[accessed August 10, 2005].
- ,,, et al.A high‐volume specialist palliative care unit and team may reduce in‐hospital end‐of‐life care costs.J Palliat Med.2003;6:699–705.
- ,,, et al.Effect of ethics consultations on nonbeneficial life‐sustaining treatments in the intensive care setting.JAMA.2003;290:1166–1172.
- ,.Impact of a proactive approach to improve end‐of‐life care in a medical ICU.Chest.2003;123:266–271.
- ,,, et al.A randomized controlled trial of the cost‐effectiveness of a district co‐ordinating service for terminally ill cancer patients.Palliat Med.1996;10:151–161.
- ,,, et al.The impact of a regional palliative care program on the cost of palliative care delivery.J Palliat Med.1999;3:181–186.
- ,,.Effectiveness of a home‐based palliative care program for end‐of‐life.J Palliat Med.2003;6:715–724.
- ,,.A study of proactive ethics consultation for critically and terminally ill patients with extended lengths of stay.Crit Care Med.1998;26:252–259.
- ,.Experience with an end‐of‐life practice at a university hospital.Crit Care Med.1997;25:197–202.
- .Perspectives on care at the close of life. Psychological considerations, growth, and transcendence at the end of life: the art of the possible.JAMA.2001;285:2898–2905.
- ,,.Improving palliative care.Ann Intern Med.1997;127:225–230.
- .Completing the continuum of cancer care: integrating life‐prolongation and palliation.CA Cancer J Clin.2000;50:123–132.
- ,.Pain management: pharmacological approaches.Cancer Treat Res.1999;100:1–29.
- ,.Pain and symptom management in palliative care.Cancer Control.1996;3:204–213.
- .ABC of palliative care. Anorexia, cachexia, and nutrition.BMJ.1997;315:1219–1222.
- .Perspectives on care at the close of life. Initiating end‐of‐life discussions with seriously ill patients: addressing the “elephant in the room.”JAMA.2000;284:2502–2507.
- ,,.“I wish things were different”: expressing wishes in response to loss, futility, and unrealistic hopes.Ann Intern Med.2001;135:551–555.
- ,,.Discussing palliative care with patients. ACP‐ASIM End‐of‐Life Care Consensus Panel.Ann Intern Med.1999;130:744–749.
- ,,.The patient‐physician relationship. Ensuring competency in end‐of‐life care: communication and relational skills.JAMA.2000;284:3051–3057.
- .The loneliness of the long‐term care giver.N Engl J Med.1999;340:1587–1590.
- ,,,,,.Integrating case management and palliative care.J Palliat Med.2004;7:121–136.
- ,,.The influence of caregiving and bereavement support on adjusting to an older relative's death.Gerontologist.1991;31:32–42.
- Center to Advance Palliative Care. A guide to developing a hospital‐based palliative care program. Available from URL:http://www.capc.org[accessed August 10, 2005].
- .Secondary and tertiary palliative care in US hospitals.JAMA.2002;287:875–881.
- .Coding and reimbursement mechanisms for physician services in hospice and palliative care.J Palliat Med.2000;2:157–164.
- National Hospice and Palliative Care Organization. NHPCO facts and figures. Available from URL:http://www.nhpco.org[accessed August 10, 2005].
- .When pain and suffering do not require a prognosis: Working toward meaningful hospital–hospice partnership.J Palliat Med.2003;6:109–115.
- ,,, et al.An alternative in terminal care: results of the National Hospice Study.J Chronic Dis.1986;39:9–26.
- ,.The health impact of health care on families: a matched cohort study of hospice use by decedents and mortality outcomes in surviving, widowed spouses.Soc Sci Med.2003;57:465–475.
- ,.Educational programs in US medical schools, 2002–2003.JAMA.2003;290:1190–1196.
- .Medical education in end‐of‐life care: the status of reform.J Palliat Med.2002;5:243–248.
- ,.ACGME requirements for end‐of‐life training in selected residency and fellowship programs: a status report.Acad Med.2002;77:299–304.
- ,,, et al.Recommendations for incorporating palliative care education into the acute care hospital setting.Acad Med.1999;74:871–877.
- ,,.The status of medical education in end‐of‐life care: a national report.J Gen Intern Med.2003;18:685–695.
- Liaison Committee on Medical Education. Available from URL: http://www.lcme.org[accessed August 10, 2005].
- Accreditation Council for Graduate Medical Education.Program requirements for residency education in the subspecialties of internal medicine. Graduate Medical Education Directory 2000–2001. Chicago,2000.
- ,.Palliative care in undergraduate medical education. Status report and future directions.JAMA.1997;278:733–738.
- ,.Survey of palliative care programs in United States teaching hospitals.J Palliat Med.2001;4:309–314.
- ,,, et al.Initial voluntary program standards for fellowship training in palliative medicine.J Palliat Med.2002;5:23–33.
- American Academy of Hospice and Palliative Medicine. Fellowship Program Directory. Available from URL:http://www.aahpm.org/fellowship/directory/htm[accessed August 10, 2005].
- ,,, et al.Quality of life in palliative cancer care. Results from a cluster randomized trial.J Clin Oncol.2001;19:3884–3894.
- ,,.Family satisfaction with end‐of‐life care for cancer patients in a cluster randomized trial.J Pain Symptom Manage.2002;24:53–63.
- ,,, et al.A palliative care intervention and death at home: a cluster randomized trial.Lancet.2000;356:888–893.
- ,,.Impact of palliative care case management on resource use by patients dying of cancer at a Veterans Affairs medical center.J Palliat Med.2005;8:26–35.
- ,,.Family satisfaction with end‐of‐life care for cancer patients in a cluster randomized trial.J Pain Symptom Manage.2002;24:53–63