User login
Prospective cohort study of hospitalized adults with advanced cancer: Associations between complications, comorbidity, and utilization
Of the major chronic conditions that affect adult patients in the United States, cancer accounts for the highest levels of per capita spending.1 Cost growth for cancer treatment has been substantial and persistent, from $72 billion in 2004 to $125 billion in 2010, and is projected to increase to $173 billion by 2020.2 Thirty-five percent of US direct medical cancer costs are attributable to inpatient hospital stays.3 Policy responses that can provide financially sustainable, high-quality models of care for patients with advanced cancer and other serious illness are urgently sought.4-7
Patterns and levels of resource utilization in providing healthcare to patients with serious illness reflect not only treatment choices but a complex set of relationships among demographic, clinical, and system factors.8-10 Patient-level factors previously identified as potentially significant drivers of resource utilization among cancer populations specifically include age,11 sex,12 primary diagnosis,13 and comorbidities.11 Among end-of-life populations, significant associations have been found between cost and ethnicity,14 socioeconomic status,15 advance directive status,16 insurance status,16 and functional status.17
Evidence on factors strongly associated with cost of hospital admission for patients with advanced cancer can therefore inform provision and planning of healthcare. For example, when a specific diagnosis or clinical condition is found to be associated with high cost, then improving coordination and provision of care for this patient group may reduce avoidable utilization. Determining associations between sociodemographics and hospital care cost can help in identifying possible disparities in care, such as those that might occur when care differs by race, class, or insurance status.
We conducted the Palliative Care for Cancer (PC4C) study, a prospective multisite cohort study of the palliative care consultation team intervention for hospitalized adults with advanced cancer.18,19 In our primary analysis, we controlled for receipt of palliative care and analyzed a rich patient-reported dataset to examine associations between hospital care cost, and sociodemographic factors, clinical variables, and prior healthcare utilization. The results provide evidence regarding the factors most associated with the cost of hospital-based cancer care.
METHODS
Design, Setting, Participants, Data Sources
The PC4C study has been described in detail by authors who estimated the impact of specialist palliative care consultation teams on hospitalization cost.19-21 We prospectively collected sociodemographic, clinical, prior utilization, and cost data for adult patients with a primary diagnosis of advanced cancer admitted to 4 large US hospitals between 2007 and 2011.
All 4 of these high-volume tertiary-care medical centers were selected for their high patient volume (to facilitate sample size) and research capacity (to facilitate proficient recruitment and data collection). Before the study was initiated, it was approved by the institutional review board of each facility. In addition, approval was sought from each attending physician at each hospital site; patients whose physician did not grant approval were not considered for enrollment. More than 95% of physicians gave their approval.
Patients were at least 18 years old and had a primary diagnosis of metastatic solid tumor; central nervous system malignancy; locally advanced head, neck, or pancreas cancer; metastatic melanoma; or transplant-ineligible lymphoma or multiple myeloma. Patients were excluded if they did not speak English, had a diagnosis of dementia, were unresponsive or nonverbal, had been admitted for routine chemotherapy, died or were discharged within 48 hours of admission, or had had a previous palliative care consultation.
Eligible patients were identified through daily review of admissions records and administrative databases. For each potential study patient identified, that patient’s bedside nurse inquired about willingness to participate in the study. Then, for each willing patient, a trained clinical interviewer approached to explain the study and obtain informed consent. With the patient’s consent, family members were also approached and enrolled with written informed consent.
Quantitative Variables
Independent variables. In the dataset, we identified 17 patient-level variables we hypothesized could be significantly associated with hospitalization cost. These variables covered 4 domains:
- Demographics: age, sex, race.
- Socioeconomics/systems: education level, insurance status, presence of advance directive (living will or healthcare proxy).
- Clinical care: primary cancer diagnosis, admitting diagnosis, comorbidities (Elixhauser index22), symptom burden and severity (Condensed Memorial Symptom Assessment Scale [CMSAS]23), and activities of daily living24 or presence of a hospital-acquired condition or complication.25
- Prior utilization: visiting homecare nurse and home health aide within 2 weeks before admission, and analgesic use in morphine sulfate equivalents within week before admission.
Data were collected through a combination of medical record review (age, sex, diagnoses, comorbidities, complications), patient interview (race, education, advance directive, CMSAS, activities of daily living, prior utilization), and hospital administrative databases (insurance). For use in regression, variables were divided into categories when appropriate. Table 1 lists these predictors and their prevalence in the analytic sample.
Dependent variable. The outcome of interest in this analysis was total direct cost of hospital stay. Direct costs are those attributable to the care of a specific patient, as distinct from indirect costs, the shared overhead costs of running a hospital.26 Cost data were extracted from hospital accounting databases and therefore reflect actual costs, the US dollar cost to the hospitals of care provided, also known as direct measurement.27 Costs were standardized for geographical region using the Medicare Wage Index28 and year using the Consumer Price Index29 and are presented here in US dollars for 2011, the final year of data collection.
Statistical Methods
Primary analyses. We regressed total direct hospital costs against all predictors listed in Table 1. To control for receipt of palliative care, we used additional independent variables—a fixed-effects variable for each of 3 hospitals (the fourth hospital was used as the reference case) and a binary treatment variable (whether or not the patient was seen by a palliative care consultation team within 2 days of hospital admission).19,20
Associations between cost and patient-level covariates were derived with use of a generalized linear model with a γ distribution and a log link,30 selected after comparative evaluation of performance for multiple linear and nonlinear modeling options.31
For each patient-level covariate, we estimated average marginal effects. For continuous variables, we estimated the marginal increase in cost associated with a 1-unit increase in the variable. For binary variables, we estimated the average incremental effect, the increase in cost associated with a move from the reference group, holding all other covariates to their original values. All analyses were performed with Stata Version 12.32
Secondary analyses. Primary analyses showed that number of patient comorbidities (Elixhauser index) was strongly associated with complications and comorbidity count. Prior analyses with these data have shown that palliative care had a larger cost-saving effect for patients with a larger number of comorbidities.20 Additional analyses were therefore performed to examine associations between complications, utilization, and palliative care. First, we cross-tabulated the sample by complications status (none; minor or major) and receipt of timely palliative care, and we present their summary utilization data. Second, we estimated the effect for each complications stratum (none; minor or major) of receiving timely palliative care on cost. These estimates are calculated consistent with prior work with these data: We used propensity scores to balance patients who received the treatment (palliative care) with patients who did not (usual care only),33,34 and we used a generalized linear model with a γ distribution and a log link to regress the direct hospital care cost on the binary treatment variable and all predictors listed in Table 1.19-21
RESULTS
Participants
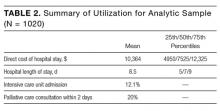
We have previously detailed that in our study there were 1023 patients eligible for cost analysis,19 of whom three were missing data in a field in Table 1 and excluded from this paper. The final analytic sample (N = 1020) is presented according to baseline covariates in Table 1 and according to summary utilization measures in Table 2.
Main Results
The results of the primary analysis, estimating the association between patient-level factors and cost of hospitalization, are presented in Table 3.
These results show the evidence of an association with cost is strongest for 3 clinical factors: a major complication (+$8267; 95% confidence interval [CI], $4509-$12,025), a minor but not a major complication (+$5289; CI, $3480-$7097), and number of comorbidities (+$852; CI, $550-$1153). In addition, there is evidence of associations between lower cost and admitting diagnosis of electrolyte disorders (–$4759; CI, –$7928 to –$1590) and older age (–$53; CI, –$99 to –$6). There is no significant association between primary diagnosis, symptom burden or other clinical factors, sociodemographic factors or healthcare utilization prior to admission and direct hospitalization costs.
Results of the secondary analyses of associations between complications, utilization, and palliative care are listed in Table 4. Patients are stratified by complication (none; major | minor) and their direct cost of hospital care and hospital length of stay (LOS) presented by treatment group (palliative care; usual care only). The data show that within each strata patients who received palliative care had lower costs and LOS than those who received usual care only. Estimated effects of palliative care on utilization is found to be statistically significant in all four quadrants, with a larger cost-effect in the complications stratum than the non-complications stratum.
Sensitivity Analysis
Fifty-one patients died during admission. After removing these cases, because of concerns about possible unobserved heterogeneity,35 we checked our primary (Table 3) and secondary (Table 4) results. Patients discharged alive had results substantively similar to those of the entire sample.
DISCUSSION
Results from our primary analysis (Table 3) suggest that complications and number of comorbidities are the key drivers of hospitalization cost for adults with advanced cancer. Hospitalization for electrolyte disorders and age are both negatively associated with cost.
The association found between higher cost and hospital-acquired complications (HACs) is consistent with other studies’ finding that HACs often result in higher cost, longer LOS, and increased inhospital mortality.36 Since those studies were reported, policy attention has been increasingly focused on HACs.37 Our findings are notable in that, though prior evidence has also suggested high hospital cost is multifactorial, driven by a diversity of demographic, socioeconomic, and clinical factors, this rich patient-reported dataset suggests that, compared with other variables, HACs are emphatically the largest driver of cost. Moreover, cancer patients typically are a vulnerable population, more prone to complications and thus also to potentially avoidable treatments and higher cost. Our prior work suggested earlier palliative care consultation can reduce cost, in part by shortening LOS and reducing the opportunity for HACs to develop19,20; our secondary analysis (Table 4) suggested a palliative care team’s involvement in HAC treatment can significantly reduce cost of care as well. These associations possibly derive from changed treatment choices and shorter LOS. Further work is needed to better elucidate the role of palliative care in the prevention of HACs in seriously ill patients.
That the number of comorbidities was found to be a key driver of hospitalization cost is consistent with recent findings that high spending on seriously ill patients is associated with having multiple chronic conditions rather than any specific primary diagnosis.38,39 It is important to note that, unlike impending complications, serious chronic conditions generally are known at admission and can be addressed prospectively through provision and policy. A prior analysis with these data found that palliative care consultation was more cost-effective for patients with a larger number of comorbidities.20 Our 2 studies together suggest that, notwithstanding the preferable alternative of avoiding hospitalization entirely, palliative care and other skilled coordination of care services ought to be prioritized for inpatients with multiple serious illnesses and the highest medical complexity. This patient group has both the highest costs and the greatest amenability to skilled transdisciplinary intervention, possibly because multiple chronic conditions affect patients interactively, complicating identification of appropriate polypharmacy responses and prioritization of treatments.
Our findings also may help direct appropriate use of palliative care services. The recently published American Society of Clinical Oncology palliative care guidelines note that all patients with advanced cancer (eg, those enrolled in our study) should receive dedicated palliative care services, early in the disease course, concurrent with active treatment.40 Workforce estimates suggest that the current and future numbers of palliative care practitioners will be unable to meet the ASCO recommendations alone never mind patients with other serious illnesses (eg, advanced heart failure, COPD, CKD).41 As such, specialized palliative care services will need to be targeted to the patient populations that can benefit most from these services. Whereas cost should not be the principle driver specialized palliative care provision, it will likely be an important component due to both the necessity of allocating scarce resources in the most effective way and the evidence that in care of the seriously-ill lower costs are often a proxy for improved patient experience.
These findings also have implications for research: Different conditions and presumably different combinations of conditions have very different implications for hospital care costs for a cohort of adults with advanced cancer. Given the increasing number of co-occurring conditions among seriously ill patients, and the increasing costs of cancer care and of treating multimorbidity cases, it is essential to further our understanding of the relationship between comorbidities and costs in order to plan and finance care for advanced cancer patients.
Limitations and Generalizability
In this observational study, reported associations may be attributable to unobserved confounding that our analyses failed to control.
Our results reflect associations in a prospective multisite study of advanced cancer patients hospitalized in the United States. It is not clear how generalizable our findings are to patients without cancer, to patients in nonhospital settings, and to patients in other health systems and countries. Analyzing cost from the hospital perspective does not take into account that the most impactful way to reduce cost is to avoid hospitalization entirely.
Results of our secondary analysis will not necessarily be robust to patient groups, as specific weights likely will vary by sample. The idea that costs vary by condition, however, is important nevertheless. Elixhauser total was derived with use of the enhanced ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) algorithm from Quan et al.42 and does not include subsequent Elixhauser Comorbidity Software updates recommended by the Healthcare Cost and Utilization Project (HCUP; Agency for Healthcare Research and Quality).43 The Elixhauser index is recommended over Charlson and other comorbidity indices by both HCUP45 and a recent systematic review.44
One possible unobserved factor is prior chemotherapy, which is associated with increased hospitalization risk. Related factors that are somewhat controlled for in the study include cancer stage (advanced cancer was an eligibility criterion) and receipt of analgesics within the week before admission (patients admitted for routine chemotherapy were excluded from analyses at the outset).
CONCLUSION
Other studies have identified a wide range of sociodemographic, clinical, and health system factors associated with healthcare utilization. Our results suggest that, for cost of hospital admission among adults with advanced cancer, the most important drivers of utilization are complications and comorbidities. Hospital costs for patients with advanced cancer constitute a major part of US healthcare spending, and these results suggest the need to prioritize high-quality, cost-effective care for patients with multiple serious illnesses.
Acknowledgments
The authors thank Robert Arnold, Phil Santa Emma, Mary Beth Happ, Tim Smith, and David Weissman for contributing to the Palliative Care for Cancer (PC4C) project.
Disclosure
The study was funded by grant R01 CA116227 from the National Cancer Institute and the National Institute of Nursing Research. The study sponsors had no role in design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the US government. All authors are independent of the study sponsors. Dr. May was supported by a HRB/NCI Health Economics Fellowship during this work. Dr. Garrido is supported by a Veterans Affairs HSR&D career development award (CDA 11-201/CDP 12-255). Dr. Kelley’s time was funded by the National Institute on Aging (1K23AG040774-01A1) and the American Federation for Aging. Dr. Smith is funded by the NCI Core Grant P 30 006973, 1-R01 CA177562-01A1, 1-R01 NR014050 01, and the Harry J. Duffey Family Endowment for Palliative Care. Dr. Morrison was the recipient of a Midcareer Investigator Award in Patient-Oriented Research (5K24AG022345) during the course of this work. This work was supported by the NIA, Claude D. Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai [5P30AG028741], and the National Palliative Care Research Center.
1. Soni A. Top 10 Most Costly Conditions Among Men and Women, 2008: Estimates for the U.S. Civilian Noninstitutionalized Adult Population, Age 18 and Older. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
2. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. PubMed
3. American Cancer Society. Cancer Facts and Figures 2015. Atlanta, GA: American Cancer Society; 2015.
4. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065. PubMed
5. Levit L, Balogh E, Nass S, Ganz PA, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: Institute of Medicine/National Academies Press; 2013. PubMed
7. Anderson GF. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
8. Tibi-Levy Y, Le Vaillant M, de Pouvourville G. Determinants of resource utilization in four palliative care units. Palliat Med. 2006;20(2):95-106. PubMed
9. Simoens S, Kutten B, Keirse E, et al. The costs of treating terminal patients. J Pain Symptom Manage. 2010;40(3):436-448. PubMed
10. Groeneveld I, Murtagh F, Kaloki Y, Bausewein C, Higginson I. Determinants of healthcare costs in the last year of life. Annual Assembly of American Academy of Hospice and Palliative Medicine & Hospice and Palliative Nurses Association; March 14, 2013; New Orleans, LA.
11. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures at the end of life for colorectal cancer decedents. J Womens Health. 2007;16(2):214-227. PubMed
12. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures and service utilization at the end of life for lung cancer decedents. Womens Health Issues. 2008;18(3):199-209. PubMed
13. Walker H, Anderson M, Farahati F, et al. Resource use and costs of end-of-life/palliative care: Ontario adult cancer patients dying during 2002 and 2003. J Palliat Care. 2011;27(2):79-88. PubMed
14. Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169(5):493-501. PubMed
15. Hanratty B, Burstrom B, Walander A, Whitehead M. Inequality in the face of death? Public expenditure on health care for different socioeconomic groups in the last year of life. J Health Serv Res Policy. 2007;12(2):90-94. PubMed
16. Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154(4):235-242. PubMed
17. Guerriere DN, Zagorski B, Fassbender K, Masucci L, Librach L, Coyte PC. Cost variations in ambulatory and home-based palliative care. Palliat Med. 2010;24(5):523-532. PubMed
18. US Department of Health and Human Services, National Institutes of Health. Palliative Care for Hospitalized Cancer Patients [project information]. Bethesda, MD: US Dept of Health and Human Services, National Institutes of Health; 2006. Project 5R01CA116227-04. https://projectreporter.nih.gov/project_info_description.cfm?projectnumber=5R01CA116227-04. Published 2006. Accessed August 1, 2015.
19. May P, Garrido MM, Cassel JB, et al. Prospective cohort study of hospital palliative care teams for inpatients with advanced cancer: earlier consultation is associated with larger cost-saving effect. J Clin Oncol. 2015;33(25):2745-2752. PubMed
20. May P, Garrido MM, Cassel JB, et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff. 2016;35(1):44-53. PubMed
21. May P, Garrido MM, Cassel JB, Morrison RS, Normand C. Using length of stay to control for unobserved heterogeneity when estimating treatment effect on hospital costs with observational data: issues of reliability, robustness and usefulness. Health Serv Res. 2016;51(5):2020-2043. PubMed
22. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. PubMed
23. Chang VT, Hwang SS, Kasimis B, Thaler HT. Shorter symptom assessment instruments: the Condensed Memorial Symptom Assessment Scale (CMSAS). Cancer Invest. 2004;22(4):526-536. PubMed
24. Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. The index of ADL: a standardized measure of biological and psychological function. JAMA. 1963;185(12):914-919. PubMed
25. McLaughlin MA, Orosz GM, Magaziner J, et al. Preoperative status and risk of complications in patients with hip fracture. J Gen Intern Med. 2006;21(3):219-225. PubMed
26. Taheri PA, Butz D, Griffes LC, Morlock DR, Greenfield LJ. Physician impact on the total cost of care. Ann Surg. 2000;231(3):432-435. PubMed
27. US Department of Veterans Affairs, Health Economics Resource Center. Determining costs. Washington, DC: US Dept of Veterans Affairs, Health Economics Resource Center; 2016. http://www.herc.research.va.gov/include/page.asp?id=determining-costs. Published 2016. Accessed September 7, 2016.
28. US Department of Health and Human Services, Center for Medicare & Medicaid Services. FY 2011 Wage Index [Table 2]. Baltimore, MD: US Dept of Health and Human Services, Center for Medicare & Medicaid Services; 2011. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/CMS1234173.html. Published 2011. Accessed September 2, 2014.
29. US Department of Labor, Bureau of Labor Statistics. All Urban Consumers (Current Series) [Consumer Price Index database]. US Dept of Labor, Bureau of Labor Statistics; 2015. http://www.bls.gov/cpi/data.htm. Published 2015. Accessed August 15, 2016.
30. Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465-488. PubMed
31. Jones AM, Rice N, Bago d’Uva T, Balia S. Applied Health Economics. 2nd ed. Oxford, England: Routledge; 2013.
32. Stata [computer program]. Version 12. College Station, TX: StataCorp; 2011.
33. Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing
propensity scores. Health Serv Res. 2014;49(5):1701-1720. PubMed
34. R Core Team. R: A Language and Environment for Statistical Computing. Vienna,
Austria: R Foundation for Statistical Computing; 2016.
35. Cassel JB, Kerr K, Pantilat S, Smith TJ. Palliative care consultation and hospital
length of stay. J Palliat Med. 2010;13(6):761-767. PubMed
36. US Department of Health and Human Services, Agency for Healthcare Research
and Quality. Efforts to Improve Patient Safety Result in 1.3 Million Fewer Patient
Harms: Interim Update on 2013 Annual Hospital-Acquired Condition Rate and
Estimates of Cost Savings and Deaths Averted From 2010 to 2013. Rockville,
MD: US Dept of Health and Human Services, Agency for Healthcare Research
and Quality; 2015. http://www.ahrq.gov/professionals/quality-patient-safety/pfp/
interimhacrate2013.html. Published 2015. Updated November 2015. Accessed
November 18, 2016.
37. Cassidy A. Health Policy Brief: Medicare’s Hospital-Acquired Condition Reduction
Program. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_
id=142. Published August 6, 2015. Accessed April 24, 2017.
38. Davis MA, Nallamothu BK, Banerjee M, Bynum JP. Identification of four unique
spending patterns among older adults in the last year of life challenges standard
assumptions. Health Aff. 2016;35(7):1316-1323. PubMed
39. Aldridge MD, Kelley AS. The myth regarding the high cost of end-of-life care.
Am J Public Health. 2015;105(12):2411-2415. PubMed
40. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard
oncology care: American Society of Clinical Oncology clinical practice guideline
update. J Clin Oncol. 2017;35(1):96-112. PubMed
41. Spetz J, Dudley N, Trupin L, Rogers M, Meier DE, Dumanovsky T. Few hospital
palliative care programs meet national staffing recommendations. Health Aff.
2016;35(9):1690-1697. PubMed
42. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities
in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. PubMed
43. HCUP [Healthcare Cost and Utilization Project] Elixhauser Comorbidity Software
[computer program]. Version 3.7. Rockville, MD: Agency for Healthcare
Research and Quality; 2016. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/
comorbidity.jsp. Published 2016. Accessed November 9, 2016.
44. Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for
administrative data. Med Care. 2012;50(12):1109-1118. PubMed
Of the major chronic conditions that affect adult patients in the United States, cancer accounts for the highest levels of per capita spending.1 Cost growth for cancer treatment has been substantial and persistent, from $72 billion in 2004 to $125 billion in 2010, and is projected to increase to $173 billion by 2020.2 Thirty-five percent of US direct medical cancer costs are attributable to inpatient hospital stays.3 Policy responses that can provide financially sustainable, high-quality models of care for patients with advanced cancer and other serious illness are urgently sought.4-7
Patterns and levels of resource utilization in providing healthcare to patients with serious illness reflect not only treatment choices but a complex set of relationships among demographic, clinical, and system factors.8-10 Patient-level factors previously identified as potentially significant drivers of resource utilization among cancer populations specifically include age,11 sex,12 primary diagnosis,13 and comorbidities.11 Among end-of-life populations, significant associations have been found between cost and ethnicity,14 socioeconomic status,15 advance directive status,16 insurance status,16 and functional status.17
Evidence on factors strongly associated with cost of hospital admission for patients with advanced cancer can therefore inform provision and planning of healthcare. For example, when a specific diagnosis or clinical condition is found to be associated with high cost, then improving coordination and provision of care for this patient group may reduce avoidable utilization. Determining associations between sociodemographics and hospital care cost can help in identifying possible disparities in care, such as those that might occur when care differs by race, class, or insurance status.
We conducted the Palliative Care for Cancer (PC4C) study, a prospective multisite cohort study of the palliative care consultation team intervention for hospitalized adults with advanced cancer.18,19 In our primary analysis, we controlled for receipt of palliative care and analyzed a rich patient-reported dataset to examine associations between hospital care cost, and sociodemographic factors, clinical variables, and prior healthcare utilization. The results provide evidence regarding the factors most associated with the cost of hospital-based cancer care.
METHODS
Design, Setting, Participants, Data Sources
The PC4C study has been described in detail by authors who estimated the impact of specialist palliative care consultation teams on hospitalization cost.19-21 We prospectively collected sociodemographic, clinical, prior utilization, and cost data for adult patients with a primary diagnosis of advanced cancer admitted to 4 large US hospitals between 2007 and 2011.
All 4 of these high-volume tertiary-care medical centers were selected for their high patient volume (to facilitate sample size) and research capacity (to facilitate proficient recruitment and data collection). Before the study was initiated, it was approved by the institutional review board of each facility. In addition, approval was sought from each attending physician at each hospital site; patients whose physician did not grant approval were not considered for enrollment. More than 95% of physicians gave their approval.
Patients were at least 18 years old and had a primary diagnosis of metastatic solid tumor; central nervous system malignancy; locally advanced head, neck, or pancreas cancer; metastatic melanoma; or transplant-ineligible lymphoma or multiple myeloma. Patients were excluded if they did not speak English, had a diagnosis of dementia, were unresponsive or nonverbal, had been admitted for routine chemotherapy, died or were discharged within 48 hours of admission, or had had a previous palliative care consultation.
Eligible patients were identified through daily review of admissions records and administrative databases. For each potential study patient identified, that patient’s bedside nurse inquired about willingness to participate in the study. Then, for each willing patient, a trained clinical interviewer approached to explain the study and obtain informed consent. With the patient’s consent, family members were also approached and enrolled with written informed consent.
Quantitative Variables
Independent variables. In the dataset, we identified 17 patient-level variables we hypothesized could be significantly associated with hospitalization cost. These variables covered 4 domains:
- Demographics: age, sex, race.
- Socioeconomics/systems: education level, insurance status, presence of advance directive (living will or healthcare proxy).
- Clinical care: primary cancer diagnosis, admitting diagnosis, comorbidities (Elixhauser index22), symptom burden and severity (Condensed Memorial Symptom Assessment Scale [CMSAS]23), and activities of daily living24 or presence of a hospital-acquired condition or complication.25
- Prior utilization: visiting homecare nurse and home health aide within 2 weeks before admission, and analgesic use in morphine sulfate equivalents within week before admission.
Data were collected through a combination of medical record review (age, sex, diagnoses, comorbidities, complications), patient interview (race, education, advance directive, CMSAS, activities of daily living, prior utilization), and hospital administrative databases (insurance). For use in regression, variables were divided into categories when appropriate. Table 1 lists these predictors and their prevalence in the analytic sample.
Dependent variable. The outcome of interest in this analysis was total direct cost of hospital stay. Direct costs are those attributable to the care of a specific patient, as distinct from indirect costs, the shared overhead costs of running a hospital.26 Cost data were extracted from hospital accounting databases and therefore reflect actual costs, the US dollar cost to the hospitals of care provided, also known as direct measurement.27 Costs were standardized for geographical region using the Medicare Wage Index28 and year using the Consumer Price Index29 and are presented here in US dollars for 2011, the final year of data collection.
Statistical Methods
Primary analyses. We regressed total direct hospital costs against all predictors listed in Table 1. To control for receipt of palliative care, we used additional independent variables—a fixed-effects variable for each of 3 hospitals (the fourth hospital was used as the reference case) and a binary treatment variable (whether or not the patient was seen by a palliative care consultation team within 2 days of hospital admission).19,20
Associations between cost and patient-level covariates were derived with use of a generalized linear model with a γ distribution and a log link,30 selected after comparative evaluation of performance for multiple linear and nonlinear modeling options.31
For each patient-level covariate, we estimated average marginal effects. For continuous variables, we estimated the marginal increase in cost associated with a 1-unit increase in the variable. For binary variables, we estimated the average incremental effect, the increase in cost associated with a move from the reference group, holding all other covariates to their original values. All analyses were performed with Stata Version 12.32
Secondary analyses. Primary analyses showed that number of patient comorbidities (Elixhauser index) was strongly associated with complications and comorbidity count. Prior analyses with these data have shown that palliative care had a larger cost-saving effect for patients with a larger number of comorbidities.20 Additional analyses were therefore performed to examine associations between complications, utilization, and palliative care. First, we cross-tabulated the sample by complications status (none; minor or major) and receipt of timely palliative care, and we present their summary utilization data. Second, we estimated the effect for each complications stratum (none; minor or major) of receiving timely palliative care on cost. These estimates are calculated consistent with prior work with these data: We used propensity scores to balance patients who received the treatment (palliative care) with patients who did not (usual care only),33,34 and we used a generalized linear model with a γ distribution and a log link to regress the direct hospital care cost on the binary treatment variable and all predictors listed in Table 1.19-21
RESULTS
Participants
We have previously detailed that in our study there were 1023 patients eligible for cost analysis,19 of whom three were missing data in a field in Table 1 and excluded from this paper. The final analytic sample (N = 1020) is presented according to baseline covariates in Table 1 and according to summary utilization measures in Table 2.
Main Results
The results of the primary analysis, estimating the association between patient-level factors and cost of hospitalization, are presented in Table 3.
These results show the evidence of an association with cost is strongest for 3 clinical factors: a major complication (+$8267; 95% confidence interval [CI], $4509-$12,025), a minor but not a major complication (+$5289; CI, $3480-$7097), and number of comorbidities (+$852; CI, $550-$1153). In addition, there is evidence of associations between lower cost and admitting diagnosis of electrolyte disorders (–$4759; CI, –$7928 to –$1590) and older age (–$53; CI, –$99 to –$6). There is no significant association between primary diagnosis, symptom burden or other clinical factors, sociodemographic factors or healthcare utilization prior to admission and direct hospitalization costs.
Results of the secondary analyses of associations between complications, utilization, and palliative care are listed in Table 4. Patients are stratified by complication (none; major | minor) and their direct cost of hospital care and hospital length of stay (LOS) presented by treatment group (palliative care; usual care only). The data show that within each strata patients who received palliative care had lower costs and LOS than those who received usual care only. Estimated effects of palliative care on utilization is found to be statistically significant in all four quadrants, with a larger cost-effect in the complications stratum than the non-complications stratum.
Sensitivity Analysis
Fifty-one patients died during admission. After removing these cases, because of concerns about possible unobserved heterogeneity,35 we checked our primary (Table 3) and secondary (Table 4) results. Patients discharged alive had results substantively similar to those of the entire sample.
DISCUSSION
Results from our primary analysis (Table 3) suggest that complications and number of comorbidities are the key drivers of hospitalization cost for adults with advanced cancer. Hospitalization for electrolyte disorders and age are both negatively associated with cost.
The association found between higher cost and hospital-acquired complications (HACs) is consistent with other studies’ finding that HACs often result in higher cost, longer LOS, and increased inhospital mortality.36 Since those studies were reported, policy attention has been increasingly focused on HACs.37 Our findings are notable in that, though prior evidence has also suggested high hospital cost is multifactorial, driven by a diversity of demographic, socioeconomic, and clinical factors, this rich patient-reported dataset suggests that, compared with other variables, HACs are emphatically the largest driver of cost. Moreover, cancer patients typically are a vulnerable population, more prone to complications and thus also to potentially avoidable treatments and higher cost. Our prior work suggested earlier palliative care consultation can reduce cost, in part by shortening LOS and reducing the opportunity for HACs to develop19,20; our secondary analysis (Table 4) suggested a palliative care team’s involvement in HAC treatment can significantly reduce cost of care as well. These associations possibly derive from changed treatment choices and shorter LOS. Further work is needed to better elucidate the role of palliative care in the prevention of HACs in seriously ill patients.
That the number of comorbidities was found to be a key driver of hospitalization cost is consistent with recent findings that high spending on seriously ill patients is associated with having multiple chronic conditions rather than any specific primary diagnosis.38,39 It is important to note that, unlike impending complications, serious chronic conditions generally are known at admission and can be addressed prospectively through provision and policy. A prior analysis with these data found that palliative care consultation was more cost-effective for patients with a larger number of comorbidities.20 Our 2 studies together suggest that, notwithstanding the preferable alternative of avoiding hospitalization entirely, palliative care and other skilled coordination of care services ought to be prioritized for inpatients with multiple serious illnesses and the highest medical complexity. This patient group has both the highest costs and the greatest amenability to skilled transdisciplinary intervention, possibly because multiple chronic conditions affect patients interactively, complicating identification of appropriate polypharmacy responses and prioritization of treatments.
Our findings also may help direct appropriate use of palliative care services. The recently published American Society of Clinical Oncology palliative care guidelines note that all patients with advanced cancer (eg, those enrolled in our study) should receive dedicated palliative care services, early in the disease course, concurrent with active treatment.40 Workforce estimates suggest that the current and future numbers of palliative care practitioners will be unable to meet the ASCO recommendations alone never mind patients with other serious illnesses (eg, advanced heart failure, COPD, CKD).41 As such, specialized palliative care services will need to be targeted to the patient populations that can benefit most from these services. Whereas cost should not be the principle driver specialized palliative care provision, it will likely be an important component due to both the necessity of allocating scarce resources in the most effective way and the evidence that in care of the seriously-ill lower costs are often a proxy for improved patient experience.
These findings also have implications for research: Different conditions and presumably different combinations of conditions have very different implications for hospital care costs for a cohort of adults with advanced cancer. Given the increasing number of co-occurring conditions among seriously ill patients, and the increasing costs of cancer care and of treating multimorbidity cases, it is essential to further our understanding of the relationship between comorbidities and costs in order to plan and finance care for advanced cancer patients.
Limitations and Generalizability
In this observational study, reported associations may be attributable to unobserved confounding that our analyses failed to control.
Our results reflect associations in a prospective multisite study of advanced cancer patients hospitalized in the United States. It is not clear how generalizable our findings are to patients without cancer, to patients in nonhospital settings, and to patients in other health systems and countries. Analyzing cost from the hospital perspective does not take into account that the most impactful way to reduce cost is to avoid hospitalization entirely.
Results of our secondary analysis will not necessarily be robust to patient groups, as specific weights likely will vary by sample. The idea that costs vary by condition, however, is important nevertheless. Elixhauser total was derived with use of the enhanced ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) algorithm from Quan et al.42 and does not include subsequent Elixhauser Comorbidity Software updates recommended by the Healthcare Cost and Utilization Project (HCUP; Agency for Healthcare Research and Quality).43 The Elixhauser index is recommended over Charlson and other comorbidity indices by both HCUP45 and a recent systematic review.44
One possible unobserved factor is prior chemotherapy, which is associated with increased hospitalization risk. Related factors that are somewhat controlled for in the study include cancer stage (advanced cancer was an eligibility criterion) and receipt of analgesics within the week before admission (patients admitted for routine chemotherapy were excluded from analyses at the outset).
CONCLUSION
Other studies have identified a wide range of sociodemographic, clinical, and health system factors associated with healthcare utilization. Our results suggest that, for cost of hospital admission among adults with advanced cancer, the most important drivers of utilization are complications and comorbidities. Hospital costs for patients with advanced cancer constitute a major part of US healthcare spending, and these results suggest the need to prioritize high-quality, cost-effective care for patients with multiple serious illnesses.
Acknowledgments
The authors thank Robert Arnold, Phil Santa Emma, Mary Beth Happ, Tim Smith, and David Weissman for contributing to the Palliative Care for Cancer (PC4C) project.
Disclosure
The study was funded by grant R01 CA116227 from the National Cancer Institute and the National Institute of Nursing Research. The study sponsors had no role in design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the US government. All authors are independent of the study sponsors. Dr. May was supported by a HRB/NCI Health Economics Fellowship during this work. Dr. Garrido is supported by a Veterans Affairs HSR&D career development award (CDA 11-201/CDP 12-255). Dr. Kelley’s time was funded by the National Institute on Aging (1K23AG040774-01A1) and the American Federation for Aging. Dr. Smith is funded by the NCI Core Grant P 30 006973, 1-R01 CA177562-01A1, 1-R01 NR014050 01, and the Harry J. Duffey Family Endowment for Palliative Care. Dr. Morrison was the recipient of a Midcareer Investigator Award in Patient-Oriented Research (5K24AG022345) during the course of this work. This work was supported by the NIA, Claude D. Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai [5P30AG028741], and the National Palliative Care Research Center.
Of the major chronic conditions that affect adult patients in the United States, cancer accounts for the highest levels of per capita spending.1 Cost growth for cancer treatment has been substantial and persistent, from $72 billion in 2004 to $125 billion in 2010, and is projected to increase to $173 billion by 2020.2 Thirty-five percent of US direct medical cancer costs are attributable to inpatient hospital stays.3 Policy responses that can provide financially sustainable, high-quality models of care for patients with advanced cancer and other serious illness are urgently sought.4-7
Patterns and levels of resource utilization in providing healthcare to patients with serious illness reflect not only treatment choices but a complex set of relationships among demographic, clinical, and system factors.8-10 Patient-level factors previously identified as potentially significant drivers of resource utilization among cancer populations specifically include age,11 sex,12 primary diagnosis,13 and comorbidities.11 Among end-of-life populations, significant associations have been found between cost and ethnicity,14 socioeconomic status,15 advance directive status,16 insurance status,16 and functional status.17
Evidence on factors strongly associated with cost of hospital admission for patients with advanced cancer can therefore inform provision and planning of healthcare. For example, when a specific diagnosis or clinical condition is found to be associated with high cost, then improving coordination and provision of care for this patient group may reduce avoidable utilization. Determining associations between sociodemographics and hospital care cost can help in identifying possible disparities in care, such as those that might occur when care differs by race, class, or insurance status.
We conducted the Palliative Care for Cancer (PC4C) study, a prospective multisite cohort study of the palliative care consultation team intervention for hospitalized adults with advanced cancer.18,19 In our primary analysis, we controlled for receipt of palliative care and analyzed a rich patient-reported dataset to examine associations between hospital care cost, and sociodemographic factors, clinical variables, and prior healthcare utilization. The results provide evidence regarding the factors most associated with the cost of hospital-based cancer care.
METHODS
Design, Setting, Participants, Data Sources
The PC4C study has been described in detail by authors who estimated the impact of specialist palliative care consultation teams on hospitalization cost.19-21 We prospectively collected sociodemographic, clinical, prior utilization, and cost data for adult patients with a primary diagnosis of advanced cancer admitted to 4 large US hospitals between 2007 and 2011.
All 4 of these high-volume tertiary-care medical centers were selected for their high patient volume (to facilitate sample size) and research capacity (to facilitate proficient recruitment and data collection). Before the study was initiated, it was approved by the institutional review board of each facility. In addition, approval was sought from each attending physician at each hospital site; patients whose physician did not grant approval were not considered for enrollment. More than 95% of physicians gave their approval.
Patients were at least 18 years old and had a primary diagnosis of metastatic solid tumor; central nervous system malignancy; locally advanced head, neck, or pancreas cancer; metastatic melanoma; or transplant-ineligible lymphoma or multiple myeloma. Patients were excluded if they did not speak English, had a diagnosis of dementia, were unresponsive or nonverbal, had been admitted for routine chemotherapy, died or were discharged within 48 hours of admission, or had had a previous palliative care consultation.
Eligible patients were identified through daily review of admissions records and administrative databases. For each potential study patient identified, that patient’s bedside nurse inquired about willingness to participate in the study. Then, for each willing patient, a trained clinical interviewer approached to explain the study and obtain informed consent. With the patient’s consent, family members were also approached and enrolled with written informed consent.
Quantitative Variables
Independent variables. In the dataset, we identified 17 patient-level variables we hypothesized could be significantly associated with hospitalization cost. These variables covered 4 domains:
- Demographics: age, sex, race.
- Socioeconomics/systems: education level, insurance status, presence of advance directive (living will or healthcare proxy).
- Clinical care: primary cancer diagnosis, admitting diagnosis, comorbidities (Elixhauser index22), symptom burden and severity (Condensed Memorial Symptom Assessment Scale [CMSAS]23), and activities of daily living24 or presence of a hospital-acquired condition or complication.25
- Prior utilization: visiting homecare nurse and home health aide within 2 weeks before admission, and analgesic use in morphine sulfate equivalents within week before admission.
Data were collected through a combination of medical record review (age, sex, diagnoses, comorbidities, complications), patient interview (race, education, advance directive, CMSAS, activities of daily living, prior utilization), and hospital administrative databases (insurance). For use in regression, variables were divided into categories when appropriate. Table 1 lists these predictors and their prevalence in the analytic sample.
Dependent variable. The outcome of interest in this analysis was total direct cost of hospital stay. Direct costs are those attributable to the care of a specific patient, as distinct from indirect costs, the shared overhead costs of running a hospital.26 Cost data were extracted from hospital accounting databases and therefore reflect actual costs, the US dollar cost to the hospitals of care provided, also known as direct measurement.27 Costs were standardized for geographical region using the Medicare Wage Index28 and year using the Consumer Price Index29 and are presented here in US dollars for 2011, the final year of data collection.
Statistical Methods
Primary analyses. We regressed total direct hospital costs against all predictors listed in Table 1. To control for receipt of palliative care, we used additional independent variables—a fixed-effects variable for each of 3 hospitals (the fourth hospital was used as the reference case) and a binary treatment variable (whether or not the patient was seen by a palliative care consultation team within 2 days of hospital admission).19,20
Associations between cost and patient-level covariates were derived with use of a generalized linear model with a γ distribution and a log link,30 selected after comparative evaluation of performance for multiple linear and nonlinear modeling options.31
For each patient-level covariate, we estimated average marginal effects. For continuous variables, we estimated the marginal increase in cost associated with a 1-unit increase in the variable. For binary variables, we estimated the average incremental effect, the increase in cost associated with a move from the reference group, holding all other covariates to their original values. All analyses were performed with Stata Version 12.32
Secondary analyses. Primary analyses showed that number of patient comorbidities (Elixhauser index) was strongly associated with complications and comorbidity count. Prior analyses with these data have shown that palliative care had a larger cost-saving effect for patients with a larger number of comorbidities.20 Additional analyses were therefore performed to examine associations between complications, utilization, and palliative care. First, we cross-tabulated the sample by complications status (none; minor or major) and receipt of timely palliative care, and we present their summary utilization data. Second, we estimated the effect for each complications stratum (none; minor or major) of receiving timely palliative care on cost. These estimates are calculated consistent with prior work with these data: We used propensity scores to balance patients who received the treatment (palliative care) with patients who did not (usual care only),33,34 and we used a generalized linear model with a γ distribution and a log link to regress the direct hospital care cost on the binary treatment variable and all predictors listed in Table 1.19-21
RESULTS
Participants
We have previously detailed that in our study there were 1023 patients eligible for cost analysis,19 of whom three were missing data in a field in Table 1 and excluded from this paper. The final analytic sample (N = 1020) is presented according to baseline covariates in Table 1 and according to summary utilization measures in Table 2.
Main Results
The results of the primary analysis, estimating the association between patient-level factors and cost of hospitalization, are presented in Table 3.
These results show the evidence of an association with cost is strongest for 3 clinical factors: a major complication (+$8267; 95% confidence interval [CI], $4509-$12,025), a minor but not a major complication (+$5289; CI, $3480-$7097), and number of comorbidities (+$852; CI, $550-$1153). In addition, there is evidence of associations between lower cost and admitting diagnosis of electrolyte disorders (–$4759; CI, –$7928 to –$1590) and older age (–$53; CI, –$99 to –$6). There is no significant association between primary diagnosis, symptom burden or other clinical factors, sociodemographic factors or healthcare utilization prior to admission and direct hospitalization costs.
Results of the secondary analyses of associations between complications, utilization, and palliative care are listed in Table 4. Patients are stratified by complication (none; major | minor) and their direct cost of hospital care and hospital length of stay (LOS) presented by treatment group (palliative care; usual care only). The data show that within each strata patients who received palliative care had lower costs and LOS than those who received usual care only. Estimated effects of palliative care on utilization is found to be statistically significant in all four quadrants, with a larger cost-effect in the complications stratum than the non-complications stratum.
Sensitivity Analysis
Fifty-one patients died during admission. After removing these cases, because of concerns about possible unobserved heterogeneity,35 we checked our primary (Table 3) and secondary (Table 4) results. Patients discharged alive had results substantively similar to those of the entire sample.
DISCUSSION
Results from our primary analysis (Table 3) suggest that complications and number of comorbidities are the key drivers of hospitalization cost for adults with advanced cancer. Hospitalization for electrolyte disorders and age are both negatively associated with cost.
The association found between higher cost and hospital-acquired complications (HACs) is consistent with other studies’ finding that HACs often result in higher cost, longer LOS, and increased inhospital mortality.36 Since those studies were reported, policy attention has been increasingly focused on HACs.37 Our findings are notable in that, though prior evidence has also suggested high hospital cost is multifactorial, driven by a diversity of demographic, socioeconomic, and clinical factors, this rich patient-reported dataset suggests that, compared with other variables, HACs are emphatically the largest driver of cost. Moreover, cancer patients typically are a vulnerable population, more prone to complications and thus also to potentially avoidable treatments and higher cost. Our prior work suggested earlier palliative care consultation can reduce cost, in part by shortening LOS and reducing the opportunity for HACs to develop19,20; our secondary analysis (Table 4) suggested a palliative care team’s involvement in HAC treatment can significantly reduce cost of care as well. These associations possibly derive from changed treatment choices and shorter LOS. Further work is needed to better elucidate the role of palliative care in the prevention of HACs in seriously ill patients.
That the number of comorbidities was found to be a key driver of hospitalization cost is consistent with recent findings that high spending on seriously ill patients is associated with having multiple chronic conditions rather than any specific primary diagnosis.38,39 It is important to note that, unlike impending complications, serious chronic conditions generally are known at admission and can be addressed prospectively through provision and policy. A prior analysis with these data found that palliative care consultation was more cost-effective for patients with a larger number of comorbidities.20 Our 2 studies together suggest that, notwithstanding the preferable alternative of avoiding hospitalization entirely, palliative care and other skilled coordination of care services ought to be prioritized for inpatients with multiple serious illnesses and the highest medical complexity. This patient group has both the highest costs and the greatest amenability to skilled transdisciplinary intervention, possibly because multiple chronic conditions affect patients interactively, complicating identification of appropriate polypharmacy responses and prioritization of treatments.
Our findings also may help direct appropriate use of palliative care services. The recently published American Society of Clinical Oncology palliative care guidelines note that all patients with advanced cancer (eg, those enrolled in our study) should receive dedicated palliative care services, early in the disease course, concurrent with active treatment.40 Workforce estimates suggest that the current and future numbers of palliative care practitioners will be unable to meet the ASCO recommendations alone never mind patients with other serious illnesses (eg, advanced heart failure, COPD, CKD).41 As such, specialized palliative care services will need to be targeted to the patient populations that can benefit most from these services. Whereas cost should not be the principle driver specialized palliative care provision, it will likely be an important component due to both the necessity of allocating scarce resources in the most effective way and the evidence that in care of the seriously-ill lower costs are often a proxy for improved patient experience.
These findings also have implications for research: Different conditions and presumably different combinations of conditions have very different implications for hospital care costs for a cohort of adults with advanced cancer. Given the increasing number of co-occurring conditions among seriously ill patients, and the increasing costs of cancer care and of treating multimorbidity cases, it is essential to further our understanding of the relationship between comorbidities and costs in order to plan and finance care for advanced cancer patients.
Limitations and Generalizability
In this observational study, reported associations may be attributable to unobserved confounding that our analyses failed to control.
Our results reflect associations in a prospective multisite study of advanced cancer patients hospitalized in the United States. It is not clear how generalizable our findings are to patients without cancer, to patients in nonhospital settings, and to patients in other health systems and countries. Analyzing cost from the hospital perspective does not take into account that the most impactful way to reduce cost is to avoid hospitalization entirely.
Results of our secondary analysis will not necessarily be robust to patient groups, as specific weights likely will vary by sample. The idea that costs vary by condition, however, is important nevertheless. Elixhauser total was derived with use of the enhanced ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) algorithm from Quan et al.42 and does not include subsequent Elixhauser Comorbidity Software updates recommended by the Healthcare Cost and Utilization Project (HCUP; Agency for Healthcare Research and Quality).43 The Elixhauser index is recommended over Charlson and other comorbidity indices by both HCUP45 and a recent systematic review.44
One possible unobserved factor is prior chemotherapy, which is associated with increased hospitalization risk. Related factors that are somewhat controlled for in the study include cancer stage (advanced cancer was an eligibility criterion) and receipt of analgesics within the week before admission (patients admitted for routine chemotherapy were excluded from analyses at the outset).
CONCLUSION
Other studies have identified a wide range of sociodemographic, clinical, and health system factors associated with healthcare utilization. Our results suggest that, for cost of hospital admission among adults with advanced cancer, the most important drivers of utilization are complications and comorbidities. Hospital costs for patients with advanced cancer constitute a major part of US healthcare spending, and these results suggest the need to prioritize high-quality, cost-effective care for patients with multiple serious illnesses.
Acknowledgments
The authors thank Robert Arnold, Phil Santa Emma, Mary Beth Happ, Tim Smith, and David Weissman for contributing to the Palliative Care for Cancer (PC4C) project.
Disclosure
The study was funded by grant R01 CA116227 from the National Cancer Institute and the National Institute of Nursing Research. The study sponsors had no role in design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the US government. All authors are independent of the study sponsors. Dr. May was supported by a HRB/NCI Health Economics Fellowship during this work. Dr. Garrido is supported by a Veterans Affairs HSR&D career development award (CDA 11-201/CDP 12-255). Dr. Kelley’s time was funded by the National Institute on Aging (1K23AG040774-01A1) and the American Federation for Aging. Dr. Smith is funded by the NCI Core Grant P 30 006973, 1-R01 CA177562-01A1, 1-R01 NR014050 01, and the Harry J. Duffey Family Endowment for Palliative Care. Dr. Morrison was the recipient of a Midcareer Investigator Award in Patient-Oriented Research (5K24AG022345) during the course of this work. This work was supported by the NIA, Claude D. Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai [5P30AG028741], and the National Palliative Care Research Center.
1. Soni A. Top 10 Most Costly Conditions Among Men and Women, 2008: Estimates for the U.S. Civilian Noninstitutionalized Adult Population, Age 18 and Older. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
2. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. PubMed
3. American Cancer Society. Cancer Facts and Figures 2015. Atlanta, GA: American Cancer Society; 2015.
4. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065. PubMed
5. Levit L, Balogh E, Nass S, Ganz PA, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: Institute of Medicine/National Academies Press; 2013. PubMed
7. Anderson GF. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
8. Tibi-Levy Y, Le Vaillant M, de Pouvourville G. Determinants of resource utilization in four palliative care units. Palliat Med. 2006;20(2):95-106. PubMed
9. Simoens S, Kutten B, Keirse E, et al. The costs of treating terminal patients. J Pain Symptom Manage. 2010;40(3):436-448. PubMed
10. Groeneveld I, Murtagh F, Kaloki Y, Bausewein C, Higginson I. Determinants of healthcare costs in the last year of life. Annual Assembly of American Academy of Hospice and Palliative Medicine & Hospice and Palliative Nurses Association; March 14, 2013; New Orleans, LA.
11. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures at the end of life for colorectal cancer decedents. J Womens Health. 2007;16(2):214-227. PubMed
12. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures and service utilization at the end of life for lung cancer decedents. Womens Health Issues. 2008;18(3):199-209. PubMed
13. Walker H, Anderson M, Farahati F, et al. Resource use and costs of end-of-life/palliative care: Ontario adult cancer patients dying during 2002 and 2003. J Palliat Care. 2011;27(2):79-88. PubMed
14. Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169(5):493-501. PubMed
15. Hanratty B, Burstrom B, Walander A, Whitehead M. Inequality in the face of death? Public expenditure on health care for different socioeconomic groups in the last year of life. J Health Serv Res Policy. 2007;12(2):90-94. PubMed
16. Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154(4):235-242. PubMed
17. Guerriere DN, Zagorski B, Fassbender K, Masucci L, Librach L, Coyte PC. Cost variations in ambulatory and home-based palliative care. Palliat Med. 2010;24(5):523-532. PubMed
18. US Department of Health and Human Services, National Institutes of Health. Palliative Care for Hospitalized Cancer Patients [project information]. Bethesda, MD: US Dept of Health and Human Services, National Institutes of Health; 2006. Project 5R01CA116227-04. https://projectreporter.nih.gov/project_info_description.cfm?projectnumber=5R01CA116227-04. Published 2006. Accessed August 1, 2015.
19. May P, Garrido MM, Cassel JB, et al. Prospective cohort study of hospital palliative care teams for inpatients with advanced cancer: earlier consultation is associated with larger cost-saving effect. J Clin Oncol. 2015;33(25):2745-2752. PubMed
20. May P, Garrido MM, Cassel JB, et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff. 2016;35(1):44-53. PubMed
21. May P, Garrido MM, Cassel JB, Morrison RS, Normand C. Using length of stay to control for unobserved heterogeneity when estimating treatment effect on hospital costs with observational data: issues of reliability, robustness and usefulness. Health Serv Res. 2016;51(5):2020-2043. PubMed
22. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. PubMed
23. Chang VT, Hwang SS, Kasimis B, Thaler HT. Shorter symptom assessment instruments: the Condensed Memorial Symptom Assessment Scale (CMSAS). Cancer Invest. 2004;22(4):526-536. PubMed
24. Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. The index of ADL: a standardized measure of biological and psychological function. JAMA. 1963;185(12):914-919. PubMed
25. McLaughlin MA, Orosz GM, Magaziner J, et al. Preoperative status and risk of complications in patients with hip fracture. J Gen Intern Med. 2006;21(3):219-225. PubMed
26. Taheri PA, Butz D, Griffes LC, Morlock DR, Greenfield LJ. Physician impact on the total cost of care. Ann Surg. 2000;231(3):432-435. PubMed
27. US Department of Veterans Affairs, Health Economics Resource Center. Determining costs. Washington, DC: US Dept of Veterans Affairs, Health Economics Resource Center; 2016. http://www.herc.research.va.gov/include/page.asp?id=determining-costs. Published 2016. Accessed September 7, 2016.
28. US Department of Health and Human Services, Center for Medicare & Medicaid Services. FY 2011 Wage Index [Table 2]. Baltimore, MD: US Dept of Health and Human Services, Center for Medicare & Medicaid Services; 2011. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/CMS1234173.html. Published 2011. Accessed September 2, 2014.
29. US Department of Labor, Bureau of Labor Statistics. All Urban Consumers (Current Series) [Consumer Price Index database]. US Dept of Labor, Bureau of Labor Statistics; 2015. http://www.bls.gov/cpi/data.htm. Published 2015. Accessed August 15, 2016.
30. Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465-488. PubMed
31. Jones AM, Rice N, Bago d’Uva T, Balia S. Applied Health Economics. 2nd ed. Oxford, England: Routledge; 2013.
32. Stata [computer program]. Version 12. College Station, TX: StataCorp; 2011.
33. Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing
propensity scores. Health Serv Res. 2014;49(5):1701-1720. PubMed
34. R Core Team. R: A Language and Environment for Statistical Computing. Vienna,
Austria: R Foundation for Statistical Computing; 2016.
35. Cassel JB, Kerr K, Pantilat S, Smith TJ. Palliative care consultation and hospital
length of stay. J Palliat Med. 2010;13(6):761-767. PubMed
36. US Department of Health and Human Services, Agency for Healthcare Research
and Quality. Efforts to Improve Patient Safety Result in 1.3 Million Fewer Patient
Harms: Interim Update on 2013 Annual Hospital-Acquired Condition Rate and
Estimates of Cost Savings and Deaths Averted From 2010 to 2013. Rockville,
MD: US Dept of Health and Human Services, Agency for Healthcare Research
and Quality; 2015. http://www.ahrq.gov/professionals/quality-patient-safety/pfp/
interimhacrate2013.html. Published 2015. Updated November 2015. Accessed
November 18, 2016.
37. Cassidy A. Health Policy Brief: Medicare’s Hospital-Acquired Condition Reduction
Program. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_
id=142. Published August 6, 2015. Accessed April 24, 2017.
38. Davis MA, Nallamothu BK, Banerjee M, Bynum JP. Identification of four unique
spending patterns among older adults in the last year of life challenges standard
assumptions. Health Aff. 2016;35(7):1316-1323. PubMed
39. Aldridge MD, Kelley AS. The myth regarding the high cost of end-of-life care.
Am J Public Health. 2015;105(12):2411-2415. PubMed
40. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard
oncology care: American Society of Clinical Oncology clinical practice guideline
update. J Clin Oncol. 2017;35(1):96-112. PubMed
41. Spetz J, Dudley N, Trupin L, Rogers M, Meier DE, Dumanovsky T. Few hospital
palliative care programs meet national staffing recommendations. Health Aff.
2016;35(9):1690-1697. PubMed
42. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities
in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. PubMed
43. HCUP [Healthcare Cost and Utilization Project] Elixhauser Comorbidity Software
[computer program]. Version 3.7. Rockville, MD: Agency for Healthcare
Research and Quality; 2016. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/
comorbidity.jsp. Published 2016. Accessed November 9, 2016.
44. Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for
administrative data. Med Care. 2012;50(12):1109-1118. PubMed
1. Soni A. Top 10 Most Costly Conditions Among Men and Women, 2008: Estimates for the U.S. Civilian Noninstitutionalized Adult Population, Age 18 and Older. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
2. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. PubMed
3. American Cancer Society. Cancer Facts and Figures 2015. Atlanta, GA: American Cancer Society; 2015.
4. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065. PubMed
5. Levit L, Balogh E, Nass S, Ganz PA, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: Institute of Medicine/National Academies Press; 2013. PubMed
7. Anderson GF. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
8. Tibi-Levy Y, Le Vaillant M, de Pouvourville G. Determinants of resource utilization in four palliative care units. Palliat Med. 2006;20(2):95-106. PubMed
9. Simoens S, Kutten B, Keirse E, et al. The costs of treating terminal patients. J Pain Symptom Manage. 2010;40(3):436-448. PubMed
10. Groeneveld I, Murtagh F, Kaloki Y, Bausewein C, Higginson I. Determinants of healthcare costs in the last year of life. Annual Assembly of American Academy of Hospice and Palliative Medicine & Hospice and Palliative Nurses Association; March 14, 2013; New Orleans, LA.
11. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures at the end of life for colorectal cancer decedents. J Womens Health. 2007;16(2):214-227. PubMed
12. Shugarman LR, Bird CE, Schuster CR, Lynn J. Age and gender differences in Medicare expenditures and service utilization at the end of life for lung cancer decedents. Womens Health Issues. 2008;18(3):199-209. PubMed
13. Walker H, Anderson M, Farahati F, et al. Resource use and costs of end-of-life/palliative care: Ontario adult cancer patients dying during 2002 and 2003. J Palliat Care. 2011;27(2):79-88. PubMed
14. Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169(5):493-501. PubMed
15. Hanratty B, Burstrom B, Walander A, Whitehead M. Inequality in the face of death? Public expenditure on health care for different socioeconomic groups in the last year of life. J Health Serv Res Policy. 2007;12(2):90-94. PubMed
16. Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154(4):235-242. PubMed
17. Guerriere DN, Zagorski B, Fassbender K, Masucci L, Librach L, Coyte PC. Cost variations in ambulatory and home-based palliative care. Palliat Med. 2010;24(5):523-532. PubMed
18. US Department of Health and Human Services, National Institutes of Health. Palliative Care for Hospitalized Cancer Patients [project information]. Bethesda, MD: US Dept of Health and Human Services, National Institutes of Health; 2006. Project 5R01CA116227-04. https://projectreporter.nih.gov/project_info_description.cfm?projectnumber=5R01CA116227-04. Published 2006. Accessed August 1, 2015.
19. May P, Garrido MM, Cassel JB, et al. Prospective cohort study of hospital palliative care teams for inpatients with advanced cancer: earlier consultation is associated with larger cost-saving effect. J Clin Oncol. 2015;33(25):2745-2752. PubMed
20. May P, Garrido MM, Cassel JB, et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff. 2016;35(1):44-53. PubMed
21. May P, Garrido MM, Cassel JB, Morrison RS, Normand C. Using length of stay to control for unobserved heterogeneity when estimating treatment effect on hospital costs with observational data: issues of reliability, robustness and usefulness. Health Serv Res. 2016;51(5):2020-2043. PubMed
22. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. PubMed
23. Chang VT, Hwang SS, Kasimis B, Thaler HT. Shorter symptom assessment instruments: the Condensed Memorial Symptom Assessment Scale (CMSAS). Cancer Invest. 2004;22(4):526-536. PubMed
24. Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. The index of ADL: a standardized measure of biological and psychological function. JAMA. 1963;185(12):914-919. PubMed
25. McLaughlin MA, Orosz GM, Magaziner J, et al. Preoperative status and risk of complications in patients with hip fracture. J Gen Intern Med. 2006;21(3):219-225. PubMed
26. Taheri PA, Butz D, Griffes LC, Morlock DR, Greenfield LJ. Physician impact on the total cost of care. Ann Surg. 2000;231(3):432-435. PubMed
27. US Department of Veterans Affairs, Health Economics Resource Center. Determining costs. Washington, DC: US Dept of Veterans Affairs, Health Economics Resource Center; 2016. http://www.herc.research.va.gov/include/page.asp?id=determining-costs. Published 2016. Accessed September 7, 2016.
28. US Department of Health and Human Services, Center for Medicare & Medicaid Services. FY 2011 Wage Index [Table 2]. Baltimore, MD: US Dept of Health and Human Services, Center for Medicare & Medicaid Services; 2011. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/CMS1234173.html. Published 2011. Accessed September 2, 2014.
29. US Department of Labor, Bureau of Labor Statistics. All Urban Consumers (Current Series) [Consumer Price Index database]. US Dept of Labor, Bureau of Labor Statistics; 2015. http://www.bls.gov/cpi/data.htm. Published 2015. Accessed August 15, 2016.
30. Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465-488. PubMed
31. Jones AM, Rice N, Bago d’Uva T, Balia S. Applied Health Economics. 2nd ed. Oxford, England: Routledge; 2013.
32. Stata [computer program]. Version 12. College Station, TX: StataCorp; 2011.
33. Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing
propensity scores. Health Serv Res. 2014;49(5):1701-1720. PubMed
34. R Core Team. R: A Language and Environment for Statistical Computing. Vienna,
Austria: R Foundation for Statistical Computing; 2016.
35. Cassel JB, Kerr K, Pantilat S, Smith TJ. Palliative care consultation and hospital
length of stay. J Palliat Med. 2010;13(6):761-767. PubMed
36. US Department of Health and Human Services, Agency for Healthcare Research
and Quality. Efforts to Improve Patient Safety Result in 1.3 Million Fewer Patient
Harms: Interim Update on 2013 Annual Hospital-Acquired Condition Rate and
Estimates of Cost Savings and Deaths Averted From 2010 to 2013. Rockville,
MD: US Dept of Health and Human Services, Agency for Healthcare Research
and Quality; 2015. http://www.ahrq.gov/professionals/quality-patient-safety/pfp/
interimhacrate2013.html. Published 2015. Updated November 2015. Accessed
November 18, 2016.
37. Cassidy A. Health Policy Brief: Medicare’s Hospital-Acquired Condition Reduction
Program. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_
id=142. Published August 6, 2015. Accessed April 24, 2017.
38. Davis MA, Nallamothu BK, Banerjee M, Bynum JP. Identification of four unique
spending patterns among older adults in the last year of life challenges standard
assumptions. Health Aff. 2016;35(7):1316-1323. PubMed
39. Aldridge MD, Kelley AS. The myth regarding the high cost of end-of-life care.
Am J Public Health. 2015;105(12):2411-2415. PubMed
40. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard
oncology care: American Society of Clinical Oncology clinical practice guideline
update. J Clin Oncol. 2017;35(1):96-112. PubMed
41. Spetz J, Dudley N, Trupin L, Rogers M, Meier DE, Dumanovsky T. Few hospital
palliative care programs meet national staffing recommendations. Health Aff.
2016;35(9):1690-1697. PubMed
42. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities
in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. PubMed
43. HCUP [Healthcare Cost and Utilization Project] Elixhauser Comorbidity Software
[computer program]. Version 3.7. Rockville, MD: Agency for Healthcare
Research and Quality; 2016. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/
comorbidity.jsp. Published 2016. Accessed November 9, 2016.
44. Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for
administrative data. Med Care. 2012;50(12):1109-1118. PubMed
© 2017 Society of Hospital Medicine
Advanced Measures in Palliative Care
The approach to clinical conundrums by an expert clinician is revealed through the presentation of an actual patient's case in an approach typical of a morning report. Similarly to patient care, sequential pieces of information are provided to the clinician, who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
Resuscitation status and patient wishes in terms of advanced cardiopulmonary support must be addressed during inpatient hospital admissions. However, the lack of clarity of the patients' wishes and the variability in physicians' comfort addressing these issues often leads to ambiguity in an emergency setting. This may result in inappropriately aggressive management, and conversely, it may also lead to withholding potentially lifesaving therapy due to Do Not Resuscitate (DNR) designation. We report a case of hemodynamic instability due to acute supraventricular tachycardia (SVT) in a patient with a DNR designation. He was successfully treated according to the advanced cardiac life support (ACLS) protocol for SVT. We also discuss some of the ethical challenges of providing potential life‐sustaining interventions in palliative medicine, as well as the dilemma of whether or not to provide such interventions to patients who have DNR status.
Case Presentation
A 45‐year‐old man with advanced tonsillar cancer was admitted to an inpatient palliative care unit for evaluation and treatment of anorexia, progressive pain, and asthenia. He had undergone tumor debulking and neck dissection followed by adjuvant chemotherapy and external beam radiation therapy. Despite maximal therapy, the patient developed locally recurrent disease (leading to more surgery) and later, progressive metastatic disease (treated with palliative radiation therapy). With ongoing weight loss and failure to thrive, a percutaneous gastrostomy tube was placed for nutritional support. Still, the patient suffered from significant stomatitis, esophagitis, and diarrhea consistent with radiation‐induced injury, and had several admissions for dehydration and pain control.
During this and prior admissions, the patient clearly articulated his preference for DNR status. The patient was clinically declining, but was still functional, with and estimated survival of weeks to a few months. As with previous admissions, he was given intravenous fluids and parenteral opioids, and his electrolytes and vital signs normalized to his baseline. On the day of anticipated discharge, the patient was at his hemodynamic baseline (pulse of 100 beats per minute, blood pressure of 98/60 mmHg). Upon returning to bed after a shower, the patient developed acute dyspnea, weakness, and diaphoresis. Heart rate was 170 beats per minute and blood pressure was 70/50 mmHg. Intravenous normal saline boluses were given while electrocardiogram (EKG) was obtained. EKG revealed SVT with changes suggestive of demand myocardial ischemia. Carotid massage and Valsalva maneuvers were unsuccessful in converting the rhythm to sinus.
At that point, consideration was given to his DNR designation. The treating physician and patient briefly discussed the alternatives of no treatment of his arrhythmia, or alternatively, more aggressive treatment options on the Palliative Care Unit, including intravenous (IV) adenosine and direct current cardioversion. He did not have a detailed advanced directive discussing similar scenarios; he had only completed a commonly‐used, state‐issued Durable DNR form. All decided the SVT was potentially reversible and appeared to be causing many of the patient's acute symptoms; hence, aggressive treatment of the arrhythmia was in his best interest.
Despite absence of telemetry monitoring, consideration was given to IV diltiazem or metoprolol, either of which could precipitate worsening hypotension. However, the goals were to restore his previous rhythm, to relieve symptoms with a minimum of side effects and unintended effects, and to avoid intensive care unit (ICU) transfer. Intravenous adenosine and esmolol were also considered, given their shorter half‐life, potentially lower side effect profile, and ability to produce relief of the patient's distress without further complication. The pros and cons of the situation were discussed with the patient. While he desperately wanted to feel better, he wished to stay with his family where he was. He consented to a trial of adenosine, and agreed to remain on the Palliative Care Unit. The therapeutic plan was a trial of IV adenosine, and then metoprolol if necessary. He was assured that if this was unsuccessful, we would do all we could to keep him comfortable without ICU transfer. While the patient was monitored with a portable 12‐lead EKG machine, the Palliative Medicine fellow administered adenosine 6 mg IV. Predictably, the patient noted flushing, a sense of impending doom, and a short pause of asystole. This was followed by electrocardiographic conversion to sinus tachycardia at a rate of 100 beats per minute and hemodynamic and symptomatic improvement. The patient noted that his dyspnea and generalized sense of not feeling well resolved, and he was monitored for about 30 minutes without return of the SVT. The remainder of his hospitalization was uneventful, and he was discharged to home hospice the following day. He survived for another 3 weeks without return of symptoms of arrhythmia.
Discussion
Patient preferences in terms of advanced cardiopulmonary support must be addressed during hospital admission. This is in accord with recommendations from the Patient Self‐Determination Act of 1990, as well as the Joint Commission on Accreditation of Healthcare Organizations.1 Nevertheless, the number of U.S. adults with completed advance directives to guide care providers and families with preferences if personally unable to articulate them is estimated at 5% to 25%.2 Clearly‐documented wishes are particularly important in patients with advanced cancer; however, early studies show that this happens as little as 27% of the time3 in seriously ill cancer patients. In fact, oncology physicians report direct discussions about death with only 37% of their dying patients4 and cancer patients are found to have discussions at far lower rates than patients with amyotrophic lateral sclerosis despite worse survival.5
Cardiopulmonary resuscitation (CPR) and the advanced cardiac life support (ACLS) algorithms were established to treat life‐threatening arrhythmias (namely ventricular tachycardia/fibrillation) in otherwise healthy patients who experienced witnessed intraoperative arrest. Original reports of closed chest compressions were in the intraoperative or perioperative setting.6 However, benefits of rapid initiation of CPR in witnessed out‐of‐hospital cardiac arrest were later noted as providing the only reasonable hope for reduced mortality and improved neurologic outcomes.7, 8
While CPR has shown this marginal but significant difference in outcomes of witnessed out‐of‐hospital cardiac arrest, patient with advanced life‐limiting or life threatening illness tend to have even worse outcomes even if cardiac arrest is witnessed. Survival of all cardiac arrest patients to discharge has been estimated at 3% to 14% if cardiac arrest occurs outside of the hospital and 10% to 20% for witnessed, in‐hospital cardiac arrest.912 However, a recent meta‐analysis of resuscitation for cancer patients estimates overall survival to discharge at 6.2%, and less when factoring in metastatic disease (5.6%), or ICU care at time of arrest (2.2%).13
Multiple reasons have been cited regarding why patients choose to forego resuscitation or proceed with full resuscitation status despite advanced life‐threatening illness. Factors associated with refusal of CPR include being older, female, living in a nursing home and having a worsening functional status, depression, and/or an expected poor outcome.14, 15 One can speculate that fear of no longer being cared for or being abandoned may be inferred or directly stated, and this may or may not be related to socioeconomic factors, stressors outside of the medical system, or underlying depressive symptomatology, especially hopelessness. Alternatively, 1 study revealed that an unclear expectation of outcome and prognosis after cardiopulmonary arrest led some to proceed with full resuscitative measures.15
Reports differ regarding the advanced care trajectory based on patient wishes. One study of 872 critically ill cancer patients found no significant difference in application of life‐sustaining therapies regardless of presence of an advance directive.3 The SUPPORT study mentioned above was specifically designed to understand preferences for CPR.14 While SUPPORT found that foregoing CPR may be associated with a small reduction in intensity of care, there was no difference in overall hospital survival.14 Last, although advance directives are static in terms of patient's stated wishes, a patient with decision‐making capacity is able to request a shift in goals of care at any time. However, a case‐based survey of 241 responding physicians concluded that a DNR order may indeed be associated with less aggressive and/or life‐prolonging interventions, CPR notwithstanding.16 This concept of treating those with DNR status less aggressively is often born out in terms of popular perception.17 A recent study has demonstrated that patients who discuss these issues with physicians and elect a DNR status not only have fewer aggressive interventions, but also report a higher quality of life.4
A particular nidus for this confusion may be how one interprets the DNR directive. Although DNR is specifically associated with 3 basic tenets (no endotracheal intubation, no chest compressions, and no defibrillation in the setting of cardiopulmonary arrest), this designation does not substitute for intact patient decision‐making capacity in considering other supportive measures. Intermediate steps such as limited aggressive therapy orders have been suggested to provide time‐limited and goal‐limited advanced care.9 While this offers a broader array of scenarios to be considered prior to and during clinical encounters, this may also muddy the picture with impractical options and further lack of clarity in already complex situations. The Physician Orders for Life‐Sustaining Treatment (POLST) movement has taken roots in several states, targeting seriously ill patients such as the frail and elderly. The POLST provides more explicit information regarding limited advanced measures such as nutrition or antibiotics, and may be particularly useful as a prehospital decision aid.18 While the POLST, just as the traditional advance directive, may provide clinical guidance outside of situations described explicitly therein,, it may not provide further information about goals of care, (ie, Is there a situation when 1 of these measures may be acceptable?). To reiterate what was stated about traditional directives, the POLST also applies only in situations where a patient is lacking decision‐making capacity at the time of an acute event.
The designation of DNR may indeed allow for introduction of advanced care measures that may be in accord with the patient's overall wishes and clinical prognosis. Several interventions may be appropriate on a time‐limited basis. In addition to administration of adenosine or antiarrhythmics, as in the case of our patient, the use of broad‐spectrum antimicrobial therapy, vasoactive medications, and consideration for intensive monitoring may all be appropriate on a time‐limited basis. Nevertheless, without a clear understanding of the goals of limited aggressive therapy, some would argue there is always a slippery slope in terms of technology and the implementation of advanced care measures. Hence, expectations regarding perceived outcomes, goals to be achieved by the therapy, and reasonable time lines may further clarify the patient's wishes.
In this patient scenario, the administration of adenosine is generally safe, but may lead to prolonged asystole, atrial fibrillation, and ventricular tachyarrhythmias.1921 This may lead one to consider further downstream ACLS interventions, including defibrillation or atropine. From an ethical standpoint, it is valuable to consider what would have been the next step beyond this step, in terms of advanced care measures. In the case of our patient, these measures were considered, and all accepted the goals of our intervention and its limitations. While virtually all treatments provided by physicians may predispose patients to iatrogenesis, the risks and benefits of interventions are particularly important considerations in the seriously ill patient with limited life expectancy.
Iatrogenic adverse events can be serious and fatal, and occur in 4% to 9% of hospitalized patients.2224 There has been much debate about what to do for iatrogenic adverse events, particularly when patients have clearly articulated advanced directives and DNR requests. While some argue there is a higher moral duty to reverse complications resulting from physician error or treatment‐induced complication, others would feel that the fiduciary obligation is to the patient's request.25, 26 Again, in the setting of our clinical scenario, having clear, up‐front expectations about goals of care and limitation inherent were articulated as much as able.
With increasing complexity of inpatient care and team‐based models of care becoming the norm, discerning patient's wishes continuously throughout a hospital course is critical. While this responsibility previously would have fallen to the 1 coordinating clinician (ie, the primary care physician, or the patient's subspecialist), it is increasingly becoming the responsibility of all members of the team. While provider's level of prior education, exposure, and comfort may vary, several resources have attempted to address these concerns and attempted to lay a framework for overcoming barriers to these discussion and tips on empathetic and effective communication.17, 2729
Skills notwithstanding, hospitalists particularly face a challenge in communicating these tenuous issues with patients. While there is intrinsic value in having an standardized approach to these situations, hospitalists are often thrown into these difficult situations in a fragmented, nonlongitudinal fashion, further heightening the clinical and ethical tension.28, 30 However, hospitalists are also is an area where they can truly make an impact in these patients' lives at a critical juncture. Evidence suggests that regardless of the provider who broaches the subject, patients have a desire to talk about these issues.4, 14 Hospitalists may be in an advantageous position compared to their primary care or subspecialist colleagues, in that they can offer a fresh perspective and the ability to have a dialog with the patient about these issues.
Implications
While patients are entitled to die free from the intrusion of chest compression and endotracheal tubes, they are also entitled to have symptoms aggressively managed. Advanced care measures may be appropriate for symptom palliation in complex clinical situations. A careful understanding of the patient's wishes and goals of care, after thoughtful exploration, may include therapies that in isolation, appear to be extraordinary or excessive. SVT is often quickly and successfully treated at the bedside. Despite a firm DNR status, treatment with IV adenosine allowed our patient time to return home with his family.
Acknowledgements
Special thanks to Dr. Paul S. Mueller for his thoughtful review and commentary regarding this manuscript.
- 2006 Comprehensive Accreditation Manual for Hospitals: The Official Handbook (CAMH).Oak Brook Terrace, IL:Joint Commission Resources;2006.
- ,,.Advance directives and do‐not‐resuscitate orders on general medical wards versus the intensive care unit.Mil Med.204;169:433–436.
- ,,.Advance directives in critically ill cancer patients.Crit Care Nurs Clin North Am.2000;12:373–383.
- ,,, et al.Associations between end‐of‐life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment.JAMA.2008;300:1665–1673.
- ,,, et al.Decision‐making in patients with advanced cancer compared with amyotrophic lateral sclerosis.J Med Ethics.2008;34:664–668.
- ,,.Closed‐chest cardiac massage.JAMA.1960;173:1064–1067.
- ,,, et al.Modifiable factors associated with improved cardiac arrest survival in a multicenter basic life support/defibrillation system: OPALS Study Phase I results. Ontario prehospital advanced life support.Ann Emerg Med.1999;33:44–50.
- ,,, et al.Effect of bystander initiated cardiopulmonary resuscitation on ventricular fibrillation and survival after witnessed cardiac arrest outside hospital.Br Heart J.1994;72:408–412.
- ,,.CPR for patients labeled DNR: the role of the limited aggressive therapy order.Ann Intern Med.2003;138:65–68.
- ,,, et al.A comparison of repeated high doses and repeated standard doses of epinephrine for cardiac arrest outside the hospital. European Epinephrine Study Group.N Engl J Med.1998;339:1595–1601.
- ,,,.Does age affect outcomes of out‐of‐hospital cardiopulmonary resuscitation?JAMA.1990;264:2109–2110.
- ,,, et al.A comparison of standard cardiopulmonary resuscitation and active compression‐decompression resuscitation for out‐of‐hospital cardiac arrest. French Active Compression‐Decompression Cardiopulmonary Resuscitation Study Group.N Engl J Med.1999;341:569–575.
- ,,,,,.Survival in cancer patients undergoing in‐hospital cardiopulmonary resuscitation: a meta‐analysis.Resuscitation.2006;71:152–160.
- ,,, et al.Choices of seriously ill patients about cardiopulmonary resuscitation: correlates and outcomes. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments.Am J Med.1996:128–137.
- ,,,,,.Preferences for life‐sustaining treatments in advance care planning and surrogate decision making.J Palliat Med.2000;3(1):37–48.
- ,.The effect of do‐not‐resuscitate orders on physician‐making.J Am Geriatr Soc.2002;50:2057–2061.
- ,,, et al.A staff dialogue on do not resuscitate orders: psychosocial issues faced by patients, their families, and caregivers.Oncologist.1999;4:256–262.
- ,,,.Hope for the future: achieving the original intent of advance directives.Hastings Cent Rep.2005;12S:S26–S30.
- ,.Adenosine‐induced non‐sustained polymorphic ventricular tachycardia.Eur Heart J.1994;15:281–282.
- ,,,.Adenosine induced ventricular arrhythmias in the emergency room.Pacing Clin Electrophysiol.2001;24:450–455.
- ,.Torsades de pointes after intravenous adenosine in the presence of prolonged QT syndrome.Am Heart J.1992;123:794–796.
- ,,, et al.Incidence of adverse events and negligence in hospitalized patients—results of the Harvard Medical Practice Study I.N Engl J Med.1991;324:370–376.
- .The hazards of hospitalization.Ann Intern Med.1964;60:100–110.
- ,,,.Iatrogenic illness on a general medical service at a university hospital.N Engl J Med.1981;304:638–642.
- ,.Overriding a patient's refusal of treatment after an iatrogenic complication.N Engl J Med.1997;336:1908–1910.
- ,,.Would physicians override a do‐not‐resuscitate order when a cardiac arrest is iatrogenic?J Gen Intern Med.1999;14:35–38.
- ,,.Discussing resuscitation preferences with patients: challenges and rewards.J Hosp Med.2006;1:231–240.
- .Decision making at a time of crisis near the end of life.JAMA.2004;292:1738–1743.
- ,,,.Advance care planning as a process: structuring the discussions in practice.J Am Geriatr Soc.1995;43:440–446.
- .Addressing end‐of‐life issues.JAMA.2005;293:162.
The approach to clinical conundrums by an expert clinician is revealed through the presentation of an actual patient's case in an approach typical of a morning report. Similarly to patient care, sequential pieces of information are provided to the clinician, who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
Resuscitation status and patient wishes in terms of advanced cardiopulmonary support must be addressed during inpatient hospital admissions. However, the lack of clarity of the patients' wishes and the variability in physicians' comfort addressing these issues often leads to ambiguity in an emergency setting. This may result in inappropriately aggressive management, and conversely, it may also lead to withholding potentially lifesaving therapy due to Do Not Resuscitate (DNR) designation. We report a case of hemodynamic instability due to acute supraventricular tachycardia (SVT) in a patient with a DNR designation. He was successfully treated according to the advanced cardiac life support (ACLS) protocol for SVT. We also discuss some of the ethical challenges of providing potential life‐sustaining interventions in palliative medicine, as well as the dilemma of whether or not to provide such interventions to patients who have DNR status.
Case Presentation
A 45‐year‐old man with advanced tonsillar cancer was admitted to an inpatient palliative care unit for evaluation and treatment of anorexia, progressive pain, and asthenia. He had undergone tumor debulking and neck dissection followed by adjuvant chemotherapy and external beam radiation therapy. Despite maximal therapy, the patient developed locally recurrent disease (leading to more surgery) and later, progressive metastatic disease (treated with palliative radiation therapy). With ongoing weight loss and failure to thrive, a percutaneous gastrostomy tube was placed for nutritional support. Still, the patient suffered from significant stomatitis, esophagitis, and diarrhea consistent with radiation‐induced injury, and had several admissions for dehydration and pain control.
During this and prior admissions, the patient clearly articulated his preference for DNR status. The patient was clinically declining, but was still functional, with and estimated survival of weeks to a few months. As with previous admissions, he was given intravenous fluids and parenteral opioids, and his electrolytes and vital signs normalized to his baseline. On the day of anticipated discharge, the patient was at his hemodynamic baseline (pulse of 100 beats per minute, blood pressure of 98/60 mmHg). Upon returning to bed after a shower, the patient developed acute dyspnea, weakness, and diaphoresis. Heart rate was 170 beats per minute and blood pressure was 70/50 mmHg. Intravenous normal saline boluses were given while electrocardiogram (EKG) was obtained. EKG revealed SVT with changes suggestive of demand myocardial ischemia. Carotid massage and Valsalva maneuvers were unsuccessful in converting the rhythm to sinus.
At that point, consideration was given to his DNR designation. The treating physician and patient briefly discussed the alternatives of no treatment of his arrhythmia, or alternatively, more aggressive treatment options on the Palliative Care Unit, including intravenous (IV) adenosine and direct current cardioversion. He did not have a detailed advanced directive discussing similar scenarios; he had only completed a commonly‐used, state‐issued Durable DNR form. All decided the SVT was potentially reversible and appeared to be causing many of the patient's acute symptoms; hence, aggressive treatment of the arrhythmia was in his best interest.
Despite absence of telemetry monitoring, consideration was given to IV diltiazem or metoprolol, either of which could precipitate worsening hypotension. However, the goals were to restore his previous rhythm, to relieve symptoms with a minimum of side effects and unintended effects, and to avoid intensive care unit (ICU) transfer. Intravenous adenosine and esmolol were also considered, given their shorter half‐life, potentially lower side effect profile, and ability to produce relief of the patient's distress without further complication. The pros and cons of the situation were discussed with the patient. While he desperately wanted to feel better, he wished to stay with his family where he was. He consented to a trial of adenosine, and agreed to remain on the Palliative Care Unit. The therapeutic plan was a trial of IV adenosine, and then metoprolol if necessary. He was assured that if this was unsuccessful, we would do all we could to keep him comfortable without ICU transfer. While the patient was monitored with a portable 12‐lead EKG machine, the Palliative Medicine fellow administered adenosine 6 mg IV. Predictably, the patient noted flushing, a sense of impending doom, and a short pause of asystole. This was followed by electrocardiographic conversion to sinus tachycardia at a rate of 100 beats per minute and hemodynamic and symptomatic improvement. The patient noted that his dyspnea and generalized sense of not feeling well resolved, and he was monitored for about 30 minutes without return of the SVT. The remainder of his hospitalization was uneventful, and he was discharged to home hospice the following day. He survived for another 3 weeks without return of symptoms of arrhythmia.
Discussion
Patient preferences in terms of advanced cardiopulmonary support must be addressed during hospital admission. This is in accord with recommendations from the Patient Self‐Determination Act of 1990, as well as the Joint Commission on Accreditation of Healthcare Organizations.1 Nevertheless, the number of U.S. adults with completed advance directives to guide care providers and families with preferences if personally unable to articulate them is estimated at 5% to 25%.2 Clearly‐documented wishes are particularly important in patients with advanced cancer; however, early studies show that this happens as little as 27% of the time3 in seriously ill cancer patients. In fact, oncology physicians report direct discussions about death with only 37% of their dying patients4 and cancer patients are found to have discussions at far lower rates than patients with amyotrophic lateral sclerosis despite worse survival.5
Cardiopulmonary resuscitation (CPR) and the advanced cardiac life support (ACLS) algorithms were established to treat life‐threatening arrhythmias (namely ventricular tachycardia/fibrillation) in otherwise healthy patients who experienced witnessed intraoperative arrest. Original reports of closed chest compressions were in the intraoperative or perioperative setting.6 However, benefits of rapid initiation of CPR in witnessed out‐of‐hospital cardiac arrest were later noted as providing the only reasonable hope for reduced mortality and improved neurologic outcomes.7, 8
While CPR has shown this marginal but significant difference in outcomes of witnessed out‐of‐hospital cardiac arrest, patient with advanced life‐limiting or life threatening illness tend to have even worse outcomes even if cardiac arrest is witnessed. Survival of all cardiac arrest patients to discharge has been estimated at 3% to 14% if cardiac arrest occurs outside of the hospital and 10% to 20% for witnessed, in‐hospital cardiac arrest.912 However, a recent meta‐analysis of resuscitation for cancer patients estimates overall survival to discharge at 6.2%, and less when factoring in metastatic disease (5.6%), or ICU care at time of arrest (2.2%).13
Multiple reasons have been cited regarding why patients choose to forego resuscitation or proceed with full resuscitation status despite advanced life‐threatening illness. Factors associated with refusal of CPR include being older, female, living in a nursing home and having a worsening functional status, depression, and/or an expected poor outcome.14, 15 One can speculate that fear of no longer being cared for or being abandoned may be inferred or directly stated, and this may or may not be related to socioeconomic factors, stressors outside of the medical system, or underlying depressive symptomatology, especially hopelessness. Alternatively, 1 study revealed that an unclear expectation of outcome and prognosis after cardiopulmonary arrest led some to proceed with full resuscitative measures.15
Reports differ regarding the advanced care trajectory based on patient wishes. One study of 872 critically ill cancer patients found no significant difference in application of life‐sustaining therapies regardless of presence of an advance directive.3 The SUPPORT study mentioned above was specifically designed to understand preferences for CPR.14 While SUPPORT found that foregoing CPR may be associated with a small reduction in intensity of care, there was no difference in overall hospital survival.14 Last, although advance directives are static in terms of patient's stated wishes, a patient with decision‐making capacity is able to request a shift in goals of care at any time. However, a case‐based survey of 241 responding physicians concluded that a DNR order may indeed be associated with less aggressive and/or life‐prolonging interventions, CPR notwithstanding.16 This concept of treating those with DNR status less aggressively is often born out in terms of popular perception.17 A recent study has demonstrated that patients who discuss these issues with physicians and elect a DNR status not only have fewer aggressive interventions, but also report a higher quality of life.4
A particular nidus for this confusion may be how one interprets the DNR directive. Although DNR is specifically associated with 3 basic tenets (no endotracheal intubation, no chest compressions, and no defibrillation in the setting of cardiopulmonary arrest), this designation does not substitute for intact patient decision‐making capacity in considering other supportive measures. Intermediate steps such as limited aggressive therapy orders have been suggested to provide time‐limited and goal‐limited advanced care.9 While this offers a broader array of scenarios to be considered prior to and during clinical encounters, this may also muddy the picture with impractical options and further lack of clarity in already complex situations. The Physician Orders for Life‐Sustaining Treatment (POLST) movement has taken roots in several states, targeting seriously ill patients such as the frail and elderly. The POLST provides more explicit information regarding limited advanced measures such as nutrition or antibiotics, and may be particularly useful as a prehospital decision aid.18 While the POLST, just as the traditional advance directive, may provide clinical guidance outside of situations described explicitly therein,, it may not provide further information about goals of care, (ie, Is there a situation when 1 of these measures may be acceptable?). To reiterate what was stated about traditional directives, the POLST also applies only in situations where a patient is lacking decision‐making capacity at the time of an acute event.
The designation of DNR may indeed allow for introduction of advanced care measures that may be in accord with the patient's overall wishes and clinical prognosis. Several interventions may be appropriate on a time‐limited basis. In addition to administration of adenosine or antiarrhythmics, as in the case of our patient, the use of broad‐spectrum antimicrobial therapy, vasoactive medications, and consideration for intensive monitoring may all be appropriate on a time‐limited basis. Nevertheless, without a clear understanding of the goals of limited aggressive therapy, some would argue there is always a slippery slope in terms of technology and the implementation of advanced care measures. Hence, expectations regarding perceived outcomes, goals to be achieved by the therapy, and reasonable time lines may further clarify the patient's wishes.
In this patient scenario, the administration of adenosine is generally safe, but may lead to prolonged asystole, atrial fibrillation, and ventricular tachyarrhythmias.1921 This may lead one to consider further downstream ACLS interventions, including defibrillation or atropine. From an ethical standpoint, it is valuable to consider what would have been the next step beyond this step, in terms of advanced care measures. In the case of our patient, these measures were considered, and all accepted the goals of our intervention and its limitations. While virtually all treatments provided by physicians may predispose patients to iatrogenesis, the risks and benefits of interventions are particularly important considerations in the seriously ill patient with limited life expectancy.
Iatrogenic adverse events can be serious and fatal, and occur in 4% to 9% of hospitalized patients.2224 There has been much debate about what to do for iatrogenic adverse events, particularly when patients have clearly articulated advanced directives and DNR requests. While some argue there is a higher moral duty to reverse complications resulting from physician error or treatment‐induced complication, others would feel that the fiduciary obligation is to the patient's request.25, 26 Again, in the setting of our clinical scenario, having clear, up‐front expectations about goals of care and limitation inherent were articulated as much as able.
With increasing complexity of inpatient care and team‐based models of care becoming the norm, discerning patient's wishes continuously throughout a hospital course is critical. While this responsibility previously would have fallen to the 1 coordinating clinician (ie, the primary care physician, or the patient's subspecialist), it is increasingly becoming the responsibility of all members of the team. While provider's level of prior education, exposure, and comfort may vary, several resources have attempted to address these concerns and attempted to lay a framework for overcoming barriers to these discussion and tips on empathetic and effective communication.17, 2729
Skills notwithstanding, hospitalists particularly face a challenge in communicating these tenuous issues with patients. While there is intrinsic value in having an standardized approach to these situations, hospitalists are often thrown into these difficult situations in a fragmented, nonlongitudinal fashion, further heightening the clinical and ethical tension.28, 30 However, hospitalists are also is an area where they can truly make an impact in these patients' lives at a critical juncture. Evidence suggests that regardless of the provider who broaches the subject, patients have a desire to talk about these issues.4, 14 Hospitalists may be in an advantageous position compared to their primary care or subspecialist colleagues, in that they can offer a fresh perspective and the ability to have a dialog with the patient about these issues.
Implications
While patients are entitled to die free from the intrusion of chest compression and endotracheal tubes, they are also entitled to have symptoms aggressively managed. Advanced care measures may be appropriate for symptom palliation in complex clinical situations. A careful understanding of the patient's wishes and goals of care, after thoughtful exploration, may include therapies that in isolation, appear to be extraordinary or excessive. SVT is often quickly and successfully treated at the bedside. Despite a firm DNR status, treatment with IV adenosine allowed our patient time to return home with his family.
Acknowledgements
Special thanks to Dr. Paul S. Mueller for his thoughtful review and commentary regarding this manuscript.
The approach to clinical conundrums by an expert clinician is revealed through the presentation of an actual patient's case in an approach typical of a morning report. Similarly to patient care, sequential pieces of information are provided to the clinician, who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
Resuscitation status and patient wishes in terms of advanced cardiopulmonary support must be addressed during inpatient hospital admissions. However, the lack of clarity of the patients' wishes and the variability in physicians' comfort addressing these issues often leads to ambiguity in an emergency setting. This may result in inappropriately aggressive management, and conversely, it may also lead to withholding potentially lifesaving therapy due to Do Not Resuscitate (DNR) designation. We report a case of hemodynamic instability due to acute supraventricular tachycardia (SVT) in a patient with a DNR designation. He was successfully treated according to the advanced cardiac life support (ACLS) protocol for SVT. We also discuss some of the ethical challenges of providing potential life‐sustaining interventions in palliative medicine, as well as the dilemma of whether or not to provide such interventions to patients who have DNR status.
Case Presentation
A 45‐year‐old man with advanced tonsillar cancer was admitted to an inpatient palliative care unit for evaluation and treatment of anorexia, progressive pain, and asthenia. He had undergone tumor debulking and neck dissection followed by adjuvant chemotherapy and external beam radiation therapy. Despite maximal therapy, the patient developed locally recurrent disease (leading to more surgery) and later, progressive metastatic disease (treated with palliative radiation therapy). With ongoing weight loss and failure to thrive, a percutaneous gastrostomy tube was placed for nutritional support. Still, the patient suffered from significant stomatitis, esophagitis, and diarrhea consistent with radiation‐induced injury, and had several admissions for dehydration and pain control.
During this and prior admissions, the patient clearly articulated his preference for DNR status. The patient was clinically declining, but was still functional, with and estimated survival of weeks to a few months. As with previous admissions, he was given intravenous fluids and parenteral opioids, and his electrolytes and vital signs normalized to his baseline. On the day of anticipated discharge, the patient was at his hemodynamic baseline (pulse of 100 beats per minute, blood pressure of 98/60 mmHg). Upon returning to bed after a shower, the patient developed acute dyspnea, weakness, and diaphoresis. Heart rate was 170 beats per minute and blood pressure was 70/50 mmHg. Intravenous normal saline boluses were given while electrocardiogram (EKG) was obtained. EKG revealed SVT with changes suggestive of demand myocardial ischemia. Carotid massage and Valsalva maneuvers were unsuccessful in converting the rhythm to sinus.
At that point, consideration was given to his DNR designation. The treating physician and patient briefly discussed the alternatives of no treatment of his arrhythmia, or alternatively, more aggressive treatment options on the Palliative Care Unit, including intravenous (IV) adenosine and direct current cardioversion. He did not have a detailed advanced directive discussing similar scenarios; he had only completed a commonly‐used, state‐issued Durable DNR form. All decided the SVT was potentially reversible and appeared to be causing many of the patient's acute symptoms; hence, aggressive treatment of the arrhythmia was in his best interest.
Despite absence of telemetry monitoring, consideration was given to IV diltiazem or metoprolol, either of which could precipitate worsening hypotension. However, the goals were to restore his previous rhythm, to relieve symptoms with a minimum of side effects and unintended effects, and to avoid intensive care unit (ICU) transfer. Intravenous adenosine and esmolol were also considered, given their shorter half‐life, potentially lower side effect profile, and ability to produce relief of the patient's distress without further complication. The pros and cons of the situation were discussed with the patient. While he desperately wanted to feel better, he wished to stay with his family where he was. He consented to a trial of adenosine, and agreed to remain on the Palliative Care Unit. The therapeutic plan was a trial of IV adenosine, and then metoprolol if necessary. He was assured that if this was unsuccessful, we would do all we could to keep him comfortable without ICU transfer. While the patient was monitored with a portable 12‐lead EKG machine, the Palliative Medicine fellow administered adenosine 6 mg IV. Predictably, the patient noted flushing, a sense of impending doom, and a short pause of asystole. This was followed by electrocardiographic conversion to sinus tachycardia at a rate of 100 beats per minute and hemodynamic and symptomatic improvement. The patient noted that his dyspnea and generalized sense of not feeling well resolved, and he was monitored for about 30 minutes without return of the SVT. The remainder of his hospitalization was uneventful, and he was discharged to home hospice the following day. He survived for another 3 weeks without return of symptoms of arrhythmia.
Discussion
Patient preferences in terms of advanced cardiopulmonary support must be addressed during hospital admission. This is in accord with recommendations from the Patient Self‐Determination Act of 1990, as well as the Joint Commission on Accreditation of Healthcare Organizations.1 Nevertheless, the number of U.S. adults with completed advance directives to guide care providers and families with preferences if personally unable to articulate them is estimated at 5% to 25%.2 Clearly‐documented wishes are particularly important in patients with advanced cancer; however, early studies show that this happens as little as 27% of the time3 in seriously ill cancer patients. In fact, oncology physicians report direct discussions about death with only 37% of their dying patients4 and cancer patients are found to have discussions at far lower rates than patients with amyotrophic lateral sclerosis despite worse survival.5
Cardiopulmonary resuscitation (CPR) and the advanced cardiac life support (ACLS) algorithms were established to treat life‐threatening arrhythmias (namely ventricular tachycardia/fibrillation) in otherwise healthy patients who experienced witnessed intraoperative arrest. Original reports of closed chest compressions were in the intraoperative or perioperative setting.6 However, benefits of rapid initiation of CPR in witnessed out‐of‐hospital cardiac arrest were later noted as providing the only reasonable hope for reduced mortality and improved neurologic outcomes.7, 8
While CPR has shown this marginal but significant difference in outcomes of witnessed out‐of‐hospital cardiac arrest, patient with advanced life‐limiting or life threatening illness tend to have even worse outcomes even if cardiac arrest is witnessed. Survival of all cardiac arrest patients to discharge has been estimated at 3% to 14% if cardiac arrest occurs outside of the hospital and 10% to 20% for witnessed, in‐hospital cardiac arrest.912 However, a recent meta‐analysis of resuscitation for cancer patients estimates overall survival to discharge at 6.2%, and less when factoring in metastatic disease (5.6%), or ICU care at time of arrest (2.2%).13
Multiple reasons have been cited regarding why patients choose to forego resuscitation or proceed with full resuscitation status despite advanced life‐threatening illness. Factors associated with refusal of CPR include being older, female, living in a nursing home and having a worsening functional status, depression, and/or an expected poor outcome.14, 15 One can speculate that fear of no longer being cared for or being abandoned may be inferred or directly stated, and this may or may not be related to socioeconomic factors, stressors outside of the medical system, or underlying depressive symptomatology, especially hopelessness. Alternatively, 1 study revealed that an unclear expectation of outcome and prognosis after cardiopulmonary arrest led some to proceed with full resuscitative measures.15
Reports differ regarding the advanced care trajectory based on patient wishes. One study of 872 critically ill cancer patients found no significant difference in application of life‐sustaining therapies regardless of presence of an advance directive.3 The SUPPORT study mentioned above was specifically designed to understand preferences for CPR.14 While SUPPORT found that foregoing CPR may be associated with a small reduction in intensity of care, there was no difference in overall hospital survival.14 Last, although advance directives are static in terms of patient's stated wishes, a patient with decision‐making capacity is able to request a shift in goals of care at any time. However, a case‐based survey of 241 responding physicians concluded that a DNR order may indeed be associated with less aggressive and/or life‐prolonging interventions, CPR notwithstanding.16 This concept of treating those with DNR status less aggressively is often born out in terms of popular perception.17 A recent study has demonstrated that patients who discuss these issues with physicians and elect a DNR status not only have fewer aggressive interventions, but also report a higher quality of life.4
A particular nidus for this confusion may be how one interprets the DNR directive. Although DNR is specifically associated with 3 basic tenets (no endotracheal intubation, no chest compressions, and no defibrillation in the setting of cardiopulmonary arrest), this designation does not substitute for intact patient decision‐making capacity in considering other supportive measures. Intermediate steps such as limited aggressive therapy orders have been suggested to provide time‐limited and goal‐limited advanced care.9 While this offers a broader array of scenarios to be considered prior to and during clinical encounters, this may also muddy the picture with impractical options and further lack of clarity in already complex situations. The Physician Orders for Life‐Sustaining Treatment (POLST) movement has taken roots in several states, targeting seriously ill patients such as the frail and elderly. The POLST provides more explicit information regarding limited advanced measures such as nutrition or antibiotics, and may be particularly useful as a prehospital decision aid.18 While the POLST, just as the traditional advance directive, may provide clinical guidance outside of situations described explicitly therein,, it may not provide further information about goals of care, (ie, Is there a situation when 1 of these measures may be acceptable?). To reiterate what was stated about traditional directives, the POLST also applies only in situations where a patient is lacking decision‐making capacity at the time of an acute event.
The designation of DNR may indeed allow for introduction of advanced care measures that may be in accord with the patient's overall wishes and clinical prognosis. Several interventions may be appropriate on a time‐limited basis. In addition to administration of adenosine or antiarrhythmics, as in the case of our patient, the use of broad‐spectrum antimicrobial therapy, vasoactive medications, and consideration for intensive monitoring may all be appropriate on a time‐limited basis. Nevertheless, without a clear understanding of the goals of limited aggressive therapy, some would argue there is always a slippery slope in terms of technology and the implementation of advanced care measures. Hence, expectations regarding perceived outcomes, goals to be achieved by the therapy, and reasonable time lines may further clarify the patient's wishes.
In this patient scenario, the administration of adenosine is generally safe, but may lead to prolonged asystole, atrial fibrillation, and ventricular tachyarrhythmias.1921 This may lead one to consider further downstream ACLS interventions, including defibrillation or atropine. From an ethical standpoint, it is valuable to consider what would have been the next step beyond this step, in terms of advanced care measures. In the case of our patient, these measures were considered, and all accepted the goals of our intervention and its limitations. While virtually all treatments provided by physicians may predispose patients to iatrogenesis, the risks and benefits of interventions are particularly important considerations in the seriously ill patient with limited life expectancy.
Iatrogenic adverse events can be serious and fatal, and occur in 4% to 9% of hospitalized patients.2224 There has been much debate about what to do for iatrogenic adverse events, particularly when patients have clearly articulated advanced directives and DNR requests. While some argue there is a higher moral duty to reverse complications resulting from physician error or treatment‐induced complication, others would feel that the fiduciary obligation is to the patient's request.25, 26 Again, in the setting of our clinical scenario, having clear, up‐front expectations about goals of care and limitation inherent were articulated as much as able.
With increasing complexity of inpatient care and team‐based models of care becoming the norm, discerning patient's wishes continuously throughout a hospital course is critical. While this responsibility previously would have fallen to the 1 coordinating clinician (ie, the primary care physician, or the patient's subspecialist), it is increasingly becoming the responsibility of all members of the team. While provider's level of prior education, exposure, and comfort may vary, several resources have attempted to address these concerns and attempted to lay a framework for overcoming barriers to these discussion and tips on empathetic and effective communication.17, 2729
Skills notwithstanding, hospitalists particularly face a challenge in communicating these tenuous issues with patients. While there is intrinsic value in having an standardized approach to these situations, hospitalists are often thrown into these difficult situations in a fragmented, nonlongitudinal fashion, further heightening the clinical and ethical tension.28, 30 However, hospitalists are also is an area where they can truly make an impact in these patients' lives at a critical juncture. Evidence suggests that regardless of the provider who broaches the subject, patients have a desire to talk about these issues.4, 14 Hospitalists may be in an advantageous position compared to their primary care or subspecialist colleagues, in that they can offer a fresh perspective and the ability to have a dialog with the patient about these issues.
Implications
While patients are entitled to die free from the intrusion of chest compression and endotracheal tubes, they are also entitled to have symptoms aggressively managed. Advanced care measures may be appropriate for symptom palliation in complex clinical situations. A careful understanding of the patient's wishes and goals of care, after thoughtful exploration, may include therapies that in isolation, appear to be extraordinary or excessive. SVT is often quickly and successfully treated at the bedside. Despite a firm DNR status, treatment with IV adenosine allowed our patient time to return home with his family.
Acknowledgements
Special thanks to Dr. Paul S. Mueller for his thoughtful review and commentary regarding this manuscript.
- 2006 Comprehensive Accreditation Manual for Hospitals: The Official Handbook (CAMH).Oak Brook Terrace, IL:Joint Commission Resources;2006.
- ,,.Advance directives and do‐not‐resuscitate orders on general medical wards versus the intensive care unit.Mil Med.204;169:433–436.
- ,,.Advance directives in critically ill cancer patients.Crit Care Nurs Clin North Am.2000;12:373–383.
- ,,, et al.Associations between end‐of‐life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment.JAMA.2008;300:1665–1673.
- ,,, et al.Decision‐making in patients with advanced cancer compared with amyotrophic lateral sclerosis.J Med Ethics.2008;34:664–668.
- ,,.Closed‐chest cardiac massage.JAMA.1960;173:1064–1067.
- ,,, et al.Modifiable factors associated with improved cardiac arrest survival in a multicenter basic life support/defibrillation system: OPALS Study Phase I results. Ontario prehospital advanced life support.Ann Emerg Med.1999;33:44–50.
- ,,, et al.Effect of bystander initiated cardiopulmonary resuscitation on ventricular fibrillation and survival after witnessed cardiac arrest outside hospital.Br Heart J.1994;72:408–412.
- ,,.CPR for patients labeled DNR: the role of the limited aggressive therapy order.Ann Intern Med.2003;138:65–68.
- ,,, et al.A comparison of repeated high doses and repeated standard doses of epinephrine for cardiac arrest outside the hospital. European Epinephrine Study Group.N Engl J Med.1998;339:1595–1601.
- ,,,.Does age affect outcomes of out‐of‐hospital cardiopulmonary resuscitation?JAMA.1990;264:2109–2110.
- ,,, et al.A comparison of standard cardiopulmonary resuscitation and active compression‐decompression resuscitation for out‐of‐hospital cardiac arrest. French Active Compression‐Decompression Cardiopulmonary Resuscitation Study Group.N Engl J Med.1999;341:569–575.
- ,,,,,.Survival in cancer patients undergoing in‐hospital cardiopulmonary resuscitation: a meta‐analysis.Resuscitation.2006;71:152–160.
- ,,, et al.Choices of seriously ill patients about cardiopulmonary resuscitation: correlates and outcomes. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments.Am J Med.1996:128–137.
- ,,,,,.Preferences for life‐sustaining treatments in advance care planning and surrogate decision making.J Palliat Med.2000;3(1):37–48.
- ,.The effect of do‐not‐resuscitate orders on physician‐making.J Am Geriatr Soc.2002;50:2057–2061.
- ,,, et al.A staff dialogue on do not resuscitate orders: psychosocial issues faced by patients, their families, and caregivers.Oncologist.1999;4:256–262.
- ,,,.Hope for the future: achieving the original intent of advance directives.Hastings Cent Rep.2005;12S:S26–S30.
- ,.Adenosine‐induced non‐sustained polymorphic ventricular tachycardia.Eur Heart J.1994;15:281–282.
- ,,,.Adenosine induced ventricular arrhythmias in the emergency room.Pacing Clin Electrophysiol.2001;24:450–455.
- ,.Torsades de pointes after intravenous adenosine in the presence of prolonged QT syndrome.Am Heart J.1992;123:794–796.
- ,,, et al.Incidence of adverse events and negligence in hospitalized patients—results of the Harvard Medical Practice Study I.N Engl J Med.1991;324:370–376.
- .The hazards of hospitalization.Ann Intern Med.1964;60:100–110.
- ,,,.Iatrogenic illness on a general medical service at a university hospital.N Engl J Med.1981;304:638–642.
- ,.Overriding a patient's refusal of treatment after an iatrogenic complication.N Engl J Med.1997;336:1908–1910.
- ,,.Would physicians override a do‐not‐resuscitate order when a cardiac arrest is iatrogenic?J Gen Intern Med.1999;14:35–38.
- ,,.Discussing resuscitation preferences with patients: challenges and rewards.J Hosp Med.2006;1:231–240.
- .Decision making at a time of crisis near the end of life.JAMA.2004;292:1738–1743.
- ,,,.Advance care planning as a process: structuring the discussions in practice.J Am Geriatr Soc.1995;43:440–446.
- .Addressing end‐of‐life issues.JAMA.2005;293:162.
- 2006 Comprehensive Accreditation Manual for Hospitals: The Official Handbook (CAMH).Oak Brook Terrace, IL:Joint Commission Resources;2006.
- ,,.Advance directives and do‐not‐resuscitate orders on general medical wards versus the intensive care unit.Mil Med.204;169:433–436.
- ,,.Advance directives in critically ill cancer patients.Crit Care Nurs Clin North Am.2000;12:373–383.
- ,,, et al.Associations between end‐of‐life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment.JAMA.2008;300:1665–1673.
- ,,, et al.Decision‐making in patients with advanced cancer compared with amyotrophic lateral sclerosis.J Med Ethics.2008;34:664–668.
- ,,.Closed‐chest cardiac massage.JAMA.1960;173:1064–1067.
- ,,, et al.Modifiable factors associated with improved cardiac arrest survival in a multicenter basic life support/defibrillation system: OPALS Study Phase I results. Ontario prehospital advanced life support.Ann Emerg Med.1999;33:44–50.
- ,,, et al.Effect of bystander initiated cardiopulmonary resuscitation on ventricular fibrillation and survival after witnessed cardiac arrest outside hospital.Br Heart J.1994;72:408–412.
- ,,.CPR for patients labeled DNR: the role of the limited aggressive therapy order.Ann Intern Med.2003;138:65–68.
- ,,, et al.A comparison of repeated high doses and repeated standard doses of epinephrine for cardiac arrest outside the hospital. European Epinephrine Study Group.N Engl J Med.1998;339:1595–1601.
- ,,,.Does age affect outcomes of out‐of‐hospital cardiopulmonary resuscitation?JAMA.1990;264:2109–2110.
- ,,, et al.A comparison of standard cardiopulmonary resuscitation and active compression‐decompression resuscitation for out‐of‐hospital cardiac arrest. French Active Compression‐Decompression Cardiopulmonary Resuscitation Study Group.N Engl J Med.1999;341:569–575.
- ,,,,,.Survival in cancer patients undergoing in‐hospital cardiopulmonary resuscitation: a meta‐analysis.Resuscitation.2006;71:152–160.
- ,,, et al.Choices of seriously ill patients about cardiopulmonary resuscitation: correlates and outcomes. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments.Am J Med.1996:128–137.
- ,,,,,.Preferences for life‐sustaining treatments in advance care planning and surrogate decision making.J Palliat Med.2000;3(1):37–48.
- ,.The effect of do‐not‐resuscitate orders on physician‐making.J Am Geriatr Soc.2002;50:2057–2061.
- ,,, et al.A staff dialogue on do not resuscitate orders: psychosocial issues faced by patients, their families, and caregivers.Oncologist.1999;4:256–262.
- ,,,.Hope for the future: achieving the original intent of advance directives.Hastings Cent Rep.2005;12S:S26–S30.
- ,.Adenosine‐induced non‐sustained polymorphic ventricular tachycardia.Eur Heart J.1994;15:281–282.
- ,,,.Adenosine induced ventricular arrhythmias in the emergency room.Pacing Clin Electrophysiol.2001;24:450–455.
- ,.Torsades de pointes after intravenous adenosine in the presence of prolonged QT syndrome.Am Heart J.1992;123:794–796.
- ,,, et al.Incidence of adverse events and negligence in hospitalized patients—results of the Harvard Medical Practice Study I.N Engl J Med.1991;324:370–376.
- .The hazards of hospitalization.Ann Intern Med.1964;60:100–110.
- ,,,.Iatrogenic illness on a general medical service at a university hospital.N Engl J Med.1981;304:638–642.
- ,.Overriding a patient's refusal of treatment after an iatrogenic complication.N Engl J Med.1997;336:1908–1910.
- ,,.Would physicians override a do‐not‐resuscitate order when a cardiac arrest is iatrogenic?J Gen Intern Med.1999;14:35–38.
- ,,.Discussing resuscitation preferences with patients: challenges and rewards.J Hosp Med.2006;1:231–240.
- .Decision making at a time of crisis near the end of life.JAMA.2004;292:1738–1743.
- ,,,.Advance care planning as a process: structuring the discussions in practice.J Am Geriatr Soc.1995;43:440–446.
- .Addressing end‐of‐life issues.JAMA.2005;293:162.