User login
Physician Groups Target Needless Procedures
Early imaging for lower back pain and Pap smears for women younger than 21 years are among eight common – but unnecessary – procedures that should be dropped from primary care physicians’ to-do lists, according to new recommendations from two primary care organizations.
The American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) highlighted eight procedures and tests that are overused and unnecessary. The recommendations are part of the ABIM (American Board of Internal Medicine) Foundation’s Choosing Wisely campaign, which targets commonly used yet ineffective procedures.
Physicians often stick with an ineffective practice (such as initially prescribing antibiotics for sinus infections) because it’s what they’re used to and it’s what patients expect, said AAFP President Glen R. Stream in an interview. The Choosing Wisely campaign is about empowering physicians and patients to break out of that cycle, Dr. Stream said.
"We have limited resources to provide health care to the people in this country, and we don’t want to waste them on things that don’t add any benefit to anyone’s health," he explained. "By focusing on these [procedures], we can avoid unnecessary x-ray exposure and medication side effects, and reserve limited medical resources to focus on things that we do know help people."
As part of their "Five Things Physicians and Patients Should Question" fact sheets, AAFP and ACP made the following recommendations:
• Don’t perform imaging for lower back pain in the first 6 weeks unless there are red flags (AAFP). Red flags include a suspected underlying condition such as osteomyelitis or spinal abnormality, or severe or progressive neurologic deficits. ACP advises physicians not to perform imaging studies in patients who have nonspecific low back pain that can’t be attributed to a specific disease or spinal abnormality.
• When treating mild to moderate sinusitis, wait at least 7 days, or until symptoms worsen, before prescribing antibiotics (AAFP). Most sinusitis is cause by a viral infection and will resolve on its own. Despite that evidence, antibiotics are prescribed in 80% of cases of acute sinusitis.
• Don’t perform Pap smears on women younger than 21 years or in those who have had a hysterectomy (AAFP). Most abnormalities in young adults occur spontaneously, so a Pap smear could just cause unnecessary anxiety, according to the AAFP. In addition, there’s little evidence that Pap smears for those who have had a hysterectomy for a noncancer disease will result in improved outcomes.
• Don’t use DXA (dual-energy x-ray absorptiometry) screening for women younger than 65 years or men younger than 70 years with no risk factors (AAFP). DXA is most cost effective for elderly patients.
• Don’t order an EKG or any other cardiac screening for low-risk patients without symptoms (AAFP). False positives can lead to invasive procedures, overtreatment, and misdiagnosis. There’s little evidence that an EKG for low-risk patients improves outcomes. The ACP recommends against screening exercise EKGs in asymptomatic patients who are at low risk for coronary heart disease.
• Don’t use brain imaging for a patient with simple syncope and a normal neurologic exam (ACP). The likelihood of fainting caused by an issue in the central nervous system is low. Therefore, brain imaging (CT or MRI) would not improve outcomes for patients with simple syncope who don’t exhibit any signs of seizure or other neurologic symptoms.
• Start with high-sensitive d-dimer measurement, not imaging, for patients with low pretest probability of venous thromboembolism (ACP). A negative, high-sensitivity d-dimer measurement can eliminate the possibility of VTE and avoid costly imaging procedures.
• In the absence of cardiopulmonary symptoms, don’t order preoperative chest radiography (ACP). Without such symptoms, radiography rarely changes management or improves patient outcomes.
In addition to the AAFP and ACP, seven other physician organizations released their own recommendations as a part of the Choosing Wisely campaign, including the American Academy of Allergy, Asthma, and Immunology; the American Society of Clinical Oncology; the American Society of Nephrology; the American College of Cardiology; the American College of Radiology; the American Gastroenterological Association; and the American Society of Nuclear Cardiology.
"Physicians, working together with patients, can help ensure the right care is delivered at the right time for the right patient," said Dr. Christine Cassel, president and CEO of the ABIM Foundation, in a statement. Through its partnership with Consumer Reports, the foundation will release resources to 11 consumer-related organizations to provide patient education about the unnecessary procedures.
"By identifying tests and procedures that might warrant additional conversations between doctors and patients, we are able to help patients receive better care through easy-to-use and accessible information," said James Guest, president and CEO of Consumer Reports, in a statement.
Early imaging for lower back pain and Pap smears for women younger than 21 years are among eight common – but unnecessary – procedures that should be dropped from primary care physicians’ to-do lists, according to new recommendations from two primary care organizations.
The American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) highlighted eight procedures and tests that are overused and unnecessary. The recommendations are part of the ABIM (American Board of Internal Medicine) Foundation’s Choosing Wisely campaign, which targets commonly used yet ineffective procedures.
Physicians often stick with an ineffective practice (such as initially prescribing antibiotics for sinus infections) because it’s what they’re used to and it’s what patients expect, said AAFP President Glen R. Stream in an interview. The Choosing Wisely campaign is about empowering physicians and patients to break out of that cycle, Dr. Stream said.
"We have limited resources to provide health care to the people in this country, and we don’t want to waste them on things that don’t add any benefit to anyone’s health," he explained. "By focusing on these [procedures], we can avoid unnecessary x-ray exposure and medication side effects, and reserve limited medical resources to focus on things that we do know help people."
As part of their "Five Things Physicians and Patients Should Question" fact sheets, AAFP and ACP made the following recommendations:
• Don’t perform imaging for lower back pain in the first 6 weeks unless there are red flags (AAFP). Red flags include a suspected underlying condition such as osteomyelitis or spinal abnormality, or severe or progressive neurologic deficits. ACP advises physicians not to perform imaging studies in patients who have nonspecific low back pain that can’t be attributed to a specific disease or spinal abnormality.
• When treating mild to moderate sinusitis, wait at least 7 days, or until symptoms worsen, before prescribing antibiotics (AAFP). Most sinusitis is cause by a viral infection and will resolve on its own. Despite that evidence, antibiotics are prescribed in 80% of cases of acute sinusitis.
• Don’t perform Pap smears on women younger than 21 years or in those who have had a hysterectomy (AAFP). Most abnormalities in young adults occur spontaneously, so a Pap smear could just cause unnecessary anxiety, according to the AAFP. In addition, there’s little evidence that Pap smears for those who have had a hysterectomy for a noncancer disease will result in improved outcomes.
• Don’t use DXA (dual-energy x-ray absorptiometry) screening for women younger than 65 years or men younger than 70 years with no risk factors (AAFP). DXA is most cost effective for elderly patients.
• Don’t order an EKG or any other cardiac screening for low-risk patients without symptoms (AAFP). False positives can lead to invasive procedures, overtreatment, and misdiagnosis. There’s little evidence that an EKG for low-risk patients improves outcomes. The ACP recommends against screening exercise EKGs in asymptomatic patients who are at low risk for coronary heart disease.
• Don’t use brain imaging for a patient with simple syncope and a normal neurologic exam (ACP). The likelihood of fainting caused by an issue in the central nervous system is low. Therefore, brain imaging (CT or MRI) would not improve outcomes for patients with simple syncope who don’t exhibit any signs of seizure or other neurologic symptoms.
• Start with high-sensitive d-dimer measurement, not imaging, for patients with low pretest probability of venous thromboembolism (ACP). A negative, high-sensitivity d-dimer measurement can eliminate the possibility of VTE and avoid costly imaging procedures.
• In the absence of cardiopulmonary symptoms, don’t order preoperative chest radiography (ACP). Without such symptoms, radiography rarely changes management or improves patient outcomes.
In addition to the AAFP and ACP, seven other physician organizations released their own recommendations as a part of the Choosing Wisely campaign, including the American Academy of Allergy, Asthma, and Immunology; the American Society of Clinical Oncology; the American Society of Nephrology; the American College of Cardiology; the American College of Radiology; the American Gastroenterological Association; and the American Society of Nuclear Cardiology.
"Physicians, working together with patients, can help ensure the right care is delivered at the right time for the right patient," said Dr. Christine Cassel, president and CEO of the ABIM Foundation, in a statement. Through its partnership with Consumer Reports, the foundation will release resources to 11 consumer-related organizations to provide patient education about the unnecessary procedures.
"By identifying tests and procedures that might warrant additional conversations between doctors and patients, we are able to help patients receive better care through easy-to-use and accessible information," said James Guest, president and CEO of Consumer Reports, in a statement.
Early imaging for lower back pain and Pap smears for women younger than 21 years are among eight common – but unnecessary – procedures that should be dropped from primary care physicians’ to-do lists, according to new recommendations from two primary care organizations.
The American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) highlighted eight procedures and tests that are overused and unnecessary. The recommendations are part of the ABIM (American Board of Internal Medicine) Foundation’s Choosing Wisely campaign, which targets commonly used yet ineffective procedures.
Physicians often stick with an ineffective practice (such as initially prescribing antibiotics for sinus infections) because it’s what they’re used to and it’s what patients expect, said AAFP President Glen R. Stream in an interview. The Choosing Wisely campaign is about empowering physicians and patients to break out of that cycle, Dr. Stream said.
"We have limited resources to provide health care to the people in this country, and we don’t want to waste them on things that don’t add any benefit to anyone’s health," he explained. "By focusing on these [procedures], we can avoid unnecessary x-ray exposure and medication side effects, and reserve limited medical resources to focus on things that we do know help people."
As part of their "Five Things Physicians and Patients Should Question" fact sheets, AAFP and ACP made the following recommendations:
• Don’t perform imaging for lower back pain in the first 6 weeks unless there are red flags (AAFP). Red flags include a suspected underlying condition such as osteomyelitis or spinal abnormality, or severe or progressive neurologic deficits. ACP advises physicians not to perform imaging studies in patients who have nonspecific low back pain that can’t be attributed to a specific disease or spinal abnormality.
• When treating mild to moderate sinusitis, wait at least 7 days, or until symptoms worsen, before prescribing antibiotics (AAFP). Most sinusitis is cause by a viral infection and will resolve on its own. Despite that evidence, antibiotics are prescribed in 80% of cases of acute sinusitis.
• Don’t perform Pap smears on women younger than 21 years or in those who have had a hysterectomy (AAFP). Most abnormalities in young adults occur spontaneously, so a Pap smear could just cause unnecessary anxiety, according to the AAFP. In addition, there’s little evidence that Pap smears for those who have had a hysterectomy for a noncancer disease will result in improved outcomes.
• Don’t use DXA (dual-energy x-ray absorptiometry) screening for women younger than 65 years or men younger than 70 years with no risk factors (AAFP). DXA is most cost effective for elderly patients.
• Don’t order an EKG or any other cardiac screening for low-risk patients without symptoms (AAFP). False positives can lead to invasive procedures, overtreatment, and misdiagnosis. There’s little evidence that an EKG for low-risk patients improves outcomes. The ACP recommends against screening exercise EKGs in asymptomatic patients who are at low risk for coronary heart disease.
• Don’t use brain imaging for a patient with simple syncope and a normal neurologic exam (ACP). The likelihood of fainting caused by an issue in the central nervous system is low. Therefore, brain imaging (CT or MRI) would not improve outcomes for patients with simple syncope who don’t exhibit any signs of seizure or other neurologic symptoms.
• Start with high-sensitive d-dimer measurement, not imaging, for patients with low pretest probability of venous thromboembolism (ACP). A negative, high-sensitivity d-dimer measurement can eliminate the possibility of VTE and avoid costly imaging procedures.
• In the absence of cardiopulmonary symptoms, don’t order preoperative chest radiography (ACP). Without such symptoms, radiography rarely changes management or improves patient outcomes.
In addition to the AAFP and ACP, seven other physician organizations released their own recommendations as a part of the Choosing Wisely campaign, including the American Academy of Allergy, Asthma, and Immunology; the American Society of Clinical Oncology; the American Society of Nephrology; the American College of Cardiology; the American College of Radiology; the American Gastroenterological Association; and the American Society of Nuclear Cardiology.
"Physicians, working together with patients, can help ensure the right care is delivered at the right time for the right patient," said Dr. Christine Cassel, president and CEO of the ABIM Foundation, in a statement. Through its partnership with Consumer Reports, the foundation will release resources to 11 consumer-related organizations to provide patient education about the unnecessary procedures.
"By identifying tests and procedures that might warrant additional conversations between doctors and patients, we are able to help patients receive better care through easy-to-use and accessible information," said James Guest, president and CEO of Consumer Reports, in a statement.
Primary Care Groups Target Needless Procedures
Early imaging for lower back pain and Pap smears for women younger than 21 years are among eight common – but unnecessary – procedures that should be dropped from primary care physicians’ to-do lists, according to new recommendations from two primary care organizations.
The American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) highlighted eight procedures and tests that are overused and unnecessary.
The recommendations are part of the ABIM (American Board of Internal Medicine) Foundation’s Choosing Wisely campaign, which targets commonly used yet ineffective procedures.
Physicians often stick with an ineffective practice (such as initially prescribing antibiotics for sinus infections) because it’s what they’re used to and it’s what patients expect, said AAFP President Glen R. Stream in an interview. The Choosing Wisely campaign is about empowering physicians and patients to break out of that cycle, Dr. Stream said.
"We have limited resources to provide health care to the people in this country, and we don’t want to waste them on things that don’t add any benefit to anyone’s health," he explained. "By focusing on these [procedures], we can avoid unnecessary x-ray exposure and medication side effects, and reserve limited medical resources to focus on things that we do know help people."
5 Things List - Embargoed Until April 4
As part of their "Five Things Physicians and Patients Should Question" fact sheets, AAFP and ACP made the following recommendations:
• Don’t perform imaging for lower back pain in the first 6 weeks unless there are red flags (AAFP). Red flags include a suspected underlying condition such as osteomyelitis or spinal abnormality, or severe or progressive neurologic deficits. ACP advises physicians not to perform imaging studies in patients who have nonspecific low back pain that can’t be attributed to a specific disease or spinal abnormality.
• When treating mild to moderate sinusitis, wait at least 7 days, or until symptoms worsen, before prescribing antibiotics (AAFP). Most sinusitis is cause by a viral infection and will resolve on its own. Despite that evidence, antibiotics are prescribed in 80% of cases of acute sinusitis.
• Don’t perform Pap smears on women younger than 21 years or in those who have had a hysterectomy (AAFP). Most abnormalities in young adults occur spontaneously, so a Pap smear could just cause unnecessary anxiety, according to the AAFP. In addition, there’s little evidence that Pap smears for those who have had a hysterectomy for a noncancer disease will result in improved outcomes.
• Don’t use DXA (dual-energy x-ray absorptiometry) screening for women younger than 65 years or men younger than 70 years with no risk factors (AAFP). DXA is most cost effective for elderly patients.
• Don’t order an EKG or any other cardiac screening for low-risk patients without symptoms (AAFP). False positives can lead to invasive procedures, overtreatment, and misdiagnosis. There’s little evidence that an EKG for low-risk patients improves outcomes. The ACP recommends against screening exercise EKGs in asymptomatic patients who are at low risk for coronary heart disease.
• Don’t use brain imaging for a patient with simple syncope and a normal neurologic exam (ACP). The likelihood of fainting caused by an issue in the central nervous system is low. Therefore, brain imaging (CT or MRI) would not improve outcomes for patients with simple syncope who don’t exhibit any signs of seizure or other neurologic symptoms.
• Start with high-sensitive d-dimer measurement, not imaging, for patients with low pretest probability of venous thromboembolism (ACP). A negative, high-sensitivity d-dimer measurement can eliminate the possibility of VTE and avoid costly imaging procedures.
• In the absence of cardiopulmonary symptoms, don’t order preoperative chest radiography (ACP). Without such symptoms, radiography rarely changes management or improves patient outcomes.
In addition to the AAFP and ACP, seven other physician organizations released their own recommendations as a part of the Choosing Wisely campaign, including the American Academy of Allergy, Asthma, and Immunology; the American Society of Clinical Oncology; the American Society of Nephrology; the American College of Cardiology; the American College of Radiology; the American Gastroenterological Association; and the American Society of Nuclear Cardiology.
"Physicians, working together with patients, can help ensure the right care is delivered at the right time for the right patient," said Dr. Christine Cassel, president and CEO of the ABIM Foundation, in a statement. Through its partnership with Consumer Reports, the foundation will release resources to 11 consumer-related organizations to provide patient education about the unnecessary procedures.
"By identifying tests and procedures that might warrant additional conversations between doctors and patients, we are able to help patients receive better care through easy-to-use and accessible information," said James Guest, president and CEO of Consumer Reports, in a statement.
Early imaging for lower back pain and Pap smears for women younger than 21 years are among eight common – but unnecessary – procedures that should be dropped from primary care physicians’ to-do lists, according to new recommendations from two primary care organizations.
The American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) highlighted eight procedures and tests that are overused and unnecessary.
The recommendations are part of the ABIM (American Board of Internal Medicine) Foundation’s Choosing Wisely campaign, which targets commonly used yet ineffective procedures.
Physicians often stick with an ineffective practice (such as initially prescribing antibiotics for sinus infections) because it’s what they’re used to and it’s what patients expect, said AAFP President Glen R. Stream in an interview. The Choosing Wisely campaign is about empowering physicians and patients to break out of that cycle, Dr. Stream said.
"We have limited resources to provide health care to the people in this country, and we don’t want to waste them on things that don’t add any benefit to anyone’s health," he explained. "By focusing on these [procedures], we can avoid unnecessary x-ray exposure and medication side effects, and reserve limited medical resources to focus on things that we do know help people."
5 Things List - Embargoed Until April 4
As part of their "Five Things Physicians and Patients Should Question" fact sheets, AAFP and ACP made the following recommendations:
• Don’t perform imaging for lower back pain in the first 6 weeks unless there are red flags (AAFP). Red flags include a suspected underlying condition such as osteomyelitis or spinal abnormality, or severe or progressive neurologic deficits. ACP advises physicians not to perform imaging studies in patients who have nonspecific low back pain that can’t be attributed to a specific disease or spinal abnormality.
• When treating mild to moderate sinusitis, wait at least 7 days, or until symptoms worsen, before prescribing antibiotics (AAFP). Most sinusitis is cause by a viral infection and will resolve on its own. Despite that evidence, antibiotics are prescribed in 80% of cases of acute sinusitis.
• Don’t perform Pap smears on women younger than 21 years or in those who have had a hysterectomy (AAFP). Most abnormalities in young adults occur spontaneously, so a Pap smear could just cause unnecessary anxiety, according to the AAFP. In addition, there’s little evidence that Pap smears for those who have had a hysterectomy for a noncancer disease will result in improved outcomes.
• Don’t use DXA (dual-energy x-ray absorptiometry) screening for women younger than 65 years or men younger than 70 years with no risk factors (AAFP). DXA is most cost effective for elderly patients.
• Don’t order an EKG or any other cardiac screening for low-risk patients without symptoms (AAFP). False positives can lead to invasive procedures, overtreatment, and misdiagnosis. There’s little evidence that an EKG for low-risk patients improves outcomes. The ACP recommends against screening exercise EKGs in asymptomatic patients who are at low risk for coronary heart disease.
• Don’t use brain imaging for a patient with simple syncope and a normal neurologic exam (ACP). The likelihood of fainting caused by an issue in the central nervous system is low. Therefore, brain imaging (CT or MRI) would not improve outcomes for patients with simple syncope who don’t exhibit any signs of seizure or other neurologic symptoms.
• Start with high-sensitive d-dimer measurement, not imaging, for patients with low pretest probability of venous thromboembolism (ACP). A negative, high-sensitivity d-dimer measurement can eliminate the possibility of VTE and avoid costly imaging procedures.
• In the absence of cardiopulmonary symptoms, don’t order preoperative chest radiography (ACP). Without such symptoms, radiography rarely changes management or improves patient outcomes.
In addition to the AAFP and ACP, seven other physician organizations released their own recommendations as a part of the Choosing Wisely campaign, including the American Academy of Allergy, Asthma, and Immunology; the American Society of Clinical Oncology; the American Society of Nephrology; the American College of Cardiology; the American College of Radiology; the American Gastroenterological Association; and the American Society of Nuclear Cardiology.
"Physicians, working together with patients, can help ensure the right care is delivered at the right time for the right patient," said Dr. Christine Cassel, president and CEO of the ABIM Foundation, in a statement. Through its partnership with Consumer Reports, the foundation will release resources to 11 consumer-related organizations to provide patient education about the unnecessary procedures.
"By identifying tests and procedures that might warrant additional conversations between doctors and patients, we are able to help patients receive better care through easy-to-use and accessible information," said James Guest, president and CEO of Consumer Reports, in a statement.
Early imaging for lower back pain and Pap smears for women younger than 21 years are among eight common – but unnecessary – procedures that should be dropped from primary care physicians’ to-do lists, according to new recommendations from two primary care organizations.
The American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) highlighted eight procedures and tests that are overused and unnecessary.
The recommendations are part of the ABIM (American Board of Internal Medicine) Foundation’s Choosing Wisely campaign, which targets commonly used yet ineffective procedures.
Physicians often stick with an ineffective practice (such as initially prescribing antibiotics for sinus infections) because it’s what they’re used to and it’s what patients expect, said AAFP President Glen R. Stream in an interview. The Choosing Wisely campaign is about empowering physicians and patients to break out of that cycle, Dr. Stream said.
"We have limited resources to provide health care to the people in this country, and we don’t want to waste them on things that don’t add any benefit to anyone’s health," he explained. "By focusing on these [procedures], we can avoid unnecessary x-ray exposure and medication side effects, and reserve limited medical resources to focus on things that we do know help people."
5 Things List - Embargoed Until April 4
As part of their "Five Things Physicians and Patients Should Question" fact sheets, AAFP and ACP made the following recommendations:
• Don’t perform imaging for lower back pain in the first 6 weeks unless there are red flags (AAFP). Red flags include a suspected underlying condition such as osteomyelitis or spinal abnormality, or severe or progressive neurologic deficits. ACP advises physicians not to perform imaging studies in patients who have nonspecific low back pain that can’t be attributed to a specific disease or spinal abnormality.
• When treating mild to moderate sinusitis, wait at least 7 days, or until symptoms worsen, before prescribing antibiotics (AAFP). Most sinusitis is cause by a viral infection and will resolve on its own. Despite that evidence, antibiotics are prescribed in 80% of cases of acute sinusitis.
• Don’t perform Pap smears on women younger than 21 years or in those who have had a hysterectomy (AAFP). Most abnormalities in young adults occur spontaneously, so a Pap smear could just cause unnecessary anxiety, according to the AAFP. In addition, there’s little evidence that Pap smears for those who have had a hysterectomy for a noncancer disease will result in improved outcomes.
• Don’t use DXA (dual-energy x-ray absorptiometry) screening for women younger than 65 years or men younger than 70 years with no risk factors (AAFP). DXA is most cost effective for elderly patients.
• Don’t order an EKG or any other cardiac screening for low-risk patients without symptoms (AAFP). False positives can lead to invasive procedures, overtreatment, and misdiagnosis. There’s little evidence that an EKG for low-risk patients improves outcomes. The ACP recommends against screening exercise EKGs in asymptomatic patients who are at low risk for coronary heart disease.
• Don’t use brain imaging for a patient with simple syncope and a normal neurologic exam (ACP). The likelihood of fainting caused by an issue in the central nervous system is low. Therefore, brain imaging (CT or MRI) would not improve outcomes for patients with simple syncope who don’t exhibit any signs of seizure or other neurologic symptoms.
• Start with high-sensitive d-dimer measurement, not imaging, for patients with low pretest probability of venous thromboembolism (ACP). A negative, high-sensitivity d-dimer measurement can eliminate the possibility of VTE and avoid costly imaging procedures.
• In the absence of cardiopulmonary symptoms, don’t order preoperative chest radiography (ACP). Without such symptoms, radiography rarely changes management or improves patient outcomes.
In addition to the AAFP and ACP, seven other physician organizations released their own recommendations as a part of the Choosing Wisely campaign, including the American Academy of Allergy, Asthma, and Immunology; the American Society of Clinical Oncology; the American Society of Nephrology; the American College of Cardiology; the American College of Radiology; the American Gastroenterological Association; and the American Society of Nuclear Cardiology.
"Physicians, working together with patients, can help ensure the right care is delivered at the right time for the right patient," said Dr. Christine Cassel, president and CEO of the ABIM Foundation, in a statement. Through its partnership with Consumer Reports, the foundation will release resources to 11 consumer-related organizations to provide patient education about the unnecessary procedures.
"By identifying tests and procedures that might warrant additional conversations between doctors and patients, we are able to help patients receive better care through easy-to-use and accessible information," said James Guest, president and CEO of Consumer Reports, in a statement.
Nearly Half of States Implementing Health Reform
Two years after enactment of the Affordable Care Act, almost every state in the union has implemented at least one item from the law’s early market reforms, the Patient's Bill of Rights, an analysis from the Commonwealth Fund has found.
Of the 49 states that have taken some action, 23 (and the District of Columbia) passed legislation or enacted regulations addressing at least one of the reforms. Twelve states addressed all the reforms. An additional 15 issued guidance for insurers on the reforms, and 11 states took no action but reported that regulators were reviewing insurers’ policy forms for compliance with reforms.
Only Arizona has done nothing to enact ACA reforms
Early market reforms that comprise the Patient’s Bill of Rights include:
• Coverage for dependents until age 26 years.
• Coverage for children younger than age 19 years, regardless of preexisting conditions.
• Prohibition of lifetime limits on essential health benefits.
• Phasing out of annual limits on the cost of essential health benefits.
• Access to a gynecologist without a referral.
• Access to copayment-free preventive services.
• Prohibition of canceling insurance except in cases of fraud or intentional misrepresentation.
• Increased flexibility in choosing a pediatrician.
• Increased flexibility in choosing a primary care provider.
• Expanded coverage of emergency services.
The Commonwealth analysis did not examine state action on other insurance reforms, including medical loss ratio requirements or standards for insurance premiums.
Even as the Supreme Court readies to examine a host of legal challenges to the ACA, states seem to be supporting the law’s implementation, at least through their actions, according to Katie Keith, lead author of the analysis.
"The vast majority of states have been very busy on health reform, at least on these early market reforms," Ms. Keith said in an interview. "You can see [the reforms] being really baked into state law and regulatory practice in all 50 states."
As the law currently stands, if states don’t implement the Patient’s Bill of Rights by Jan. 1, 2014, the federal government will do it for them. States that have not acted on these ACA reforms already may have stronger patient protections or their laws already may allow enforcement of the ACA, Ms. Keith said.
But while the ACA brings unprecedented coverage, opponents say the costs outweigh the benefits.
"For individuals and employers, the results from these new federal regulations will be across-the-board increases in health insurance costs and premiums ... These additional costs will likely exceed any possible savings from lower administrative costs for insurers," according to a report from the Heritage Foundation.
The Obama administration contends that overall, reforms that create transparency in the market will result in lower costs.
Two years after enactment of the Affordable Care Act, almost every state in the union has implemented at least one item from the law’s early market reforms, the Patient's Bill of Rights, an analysis from the Commonwealth Fund has found.
Of the 49 states that have taken some action, 23 (and the District of Columbia) passed legislation or enacted regulations addressing at least one of the reforms. Twelve states addressed all the reforms. An additional 15 issued guidance for insurers on the reforms, and 11 states took no action but reported that regulators were reviewing insurers’ policy forms for compliance with reforms.
Only Arizona has done nothing to enact ACA reforms
Early market reforms that comprise the Patient’s Bill of Rights include:
• Coverage for dependents until age 26 years.
• Coverage for children younger than age 19 years, regardless of preexisting conditions.
• Prohibition of lifetime limits on essential health benefits.
• Phasing out of annual limits on the cost of essential health benefits.
• Access to a gynecologist without a referral.
• Access to copayment-free preventive services.
• Prohibition of canceling insurance except in cases of fraud or intentional misrepresentation.
• Increased flexibility in choosing a pediatrician.
• Increased flexibility in choosing a primary care provider.
• Expanded coverage of emergency services.
The Commonwealth analysis did not examine state action on other insurance reforms, including medical loss ratio requirements or standards for insurance premiums.
Even as the Supreme Court readies to examine a host of legal challenges to the ACA, states seem to be supporting the law’s implementation, at least through their actions, according to Katie Keith, lead author of the analysis.
"The vast majority of states have been very busy on health reform, at least on these early market reforms," Ms. Keith said in an interview. "You can see [the reforms] being really baked into state law and regulatory practice in all 50 states."
As the law currently stands, if states don’t implement the Patient’s Bill of Rights by Jan. 1, 2014, the federal government will do it for them. States that have not acted on these ACA reforms already may have stronger patient protections or their laws already may allow enforcement of the ACA, Ms. Keith said.
But while the ACA brings unprecedented coverage, opponents say the costs outweigh the benefits.
"For individuals and employers, the results from these new federal regulations will be across-the-board increases in health insurance costs and premiums ... These additional costs will likely exceed any possible savings from lower administrative costs for insurers," according to a report from the Heritage Foundation.
The Obama administration contends that overall, reforms that create transparency in the market will result in lower costs.
Two years after enactment of the Affordable Care Act, almost every state in the union has implemented at least one item from the law’s early market reforms, the Patient's Bill of Rights, an analysis from the Commonwealth Fund has found.
Of the 49 states that have taken some action, 23 (and the District of Columbia) passed legislation or enacted regulations addressing at least one of the reforms. Twelve states addressed all the reforms. An additional 15 issued guidance for insurers on the reforms, and 11 states took no action but reported that regulators were reviewing insurers’ policy forms for compliance with reforms.
Only Arizona has done nothing to enact ACA reforms
Early market reforms that comprise the Patient’s Bill of Rights include:
• Coverage for dependents until age 26 years.
• Coverage for children younger than age 19 years, regardless of preexisting conditions.
• Prohibition of lifetime limits on essential health benefits.
• Phasing out of annual limits on the cost of essential health benefits.
• Access to a gynecologist without a referral.
• Access to copayment-free preventive services.
• Prohibition of canceling insurance except in cases of fraud or intentional misrepresentation.
• Increased flexibility in choosing a pediatrician.
• Increased flexibility in choosing a primary care provider.
• Expanded coverage of emergency services.
The Commonwealth analysis did not examine state action on other insurance reforms, including medical loss ratio requirements or standards for insurance premiums.
Even as the Supreme Court readies to examine a host of legal challenges to the ACA, states seem to be supporting the law’s implementation, at least through their actions, according to Katie Keith, lead author of the analysis.
"The vast majority of states have been very busy on health reform, at least on these early market reforms," Ms. Keith said in an interview. "You can see [the reforms] being really baked into state law and regulatory practice in all 50 states."
As the law currently stands, if states don’t implement the Patient’s Bill of Rights by Jan. 1, 2014, the federal government will do it for them. States that have not acted on these ACA reforms already may have stronger patient protections or their laws already may allow enforcement of the ACA, Ms. Keith said.
But while the ACA brings unprecedented coverage, opponents say the costs outweigh the benefits.
"For individuals and employers, the results from these new federal regulations will be across-the-board increases in health insurance costs and premiums ... These additional costs will likely exceed any possible savings from lower administrative costs for insurers," according to a report from the Heritage Foundation.
The Obama administration contends that overall, reforms that create transparency in the market will result in lower costs.
FROM AN ANALYSIS BY THE COMMONWEALTH FUND
MedPAC Report Pushes SGR Repeal, Offsets
WASHINGTON – By implementing a series of payment reforms now – and adopting MedPAC’s recommendations on replacing the SGR – Congress can fix the Medicare physician pay problem and come closer to paying for it, too.
That’s the bottom line of the March 2012 Report to Congress from the Medicare Payment Advisory Commission (MedPAC), released March 15.
While the recommended cuts may cause some physicians to wince, according to Mark Miller, the blow would be much harder if Congress allows the nearly 30% physician pay cut called for by the Medicare Sustainable Growth Rate formula to go through, Mr. Miller, MedPAC executive director, said at the press conference.
The MedPAC report – on of two Congress requires the group to produce each year – repeats the SGR replacement recommendationsthe commission made last October. Key among those recommendations was freezing most Medicare payments to primary care physicians for 10 years and cutting specialists’ payments by 17% over 3 years, followed by a freeze for 7 years more.
"That’s hard medicine," Mr. Miller said at the press conference. "But one of the things that it does is it reduces the cost of the fix."
MedPAC estimates their recommendations will bring the price tag of repealing the SGR to approximately $200 billion. He added that while Medicare reimbursement would go down under their proposal, historical trends show that the volume of services would go up, increasing their overall net pay.
To pick up another $60 billion to $65 billion in savings, the MedPAC March report lists 29 recommended program and policy changes.*
Key among the changes:
• Freeze payments to skilled nursing facilities in 2013, then cut them by 4% in 2014.
• Equalize payments for office-based and hospital outpatient services. Currently, Medicare pays nearly 80% for certain services when they are provided in a hospital outpatient setting vs. the physician’s office, the report said.
"If the fee schedule assumes that something takes 35 minutes ... and the efficient physician is knocking it off in 15 minutes, then the Medicare program is systematically overpaying for that service," Mr. Miller said. The idea, he said, is to promote a more equal pay between specialty and primary care services.
• Modify Medicare Part D low-income subsidies to favor more generic drugs in certain therapeutic classes.
Mr. Miller added that protecting and encouraging expansion in primary care is the commission’s top priority, one that is not perpetuated through the current payment system.
"There continues to be this concern in the commission that the fee schedule is imbalanced, that it favors procedural services and it undervalues cognitive visit-based [evaluation and management] type of services," Mr. Miller said.
While Congress has yet to solve the SGR problem, Mr. Miller said that the MedPAC commissioners recognize that lawmakers face a seemingly insurmountable challenge.
"The biggest reason that Congress doesn’t move forward on this issue is that it costs $300 billion ... it’s a big cost."
*Correction 3/29/12: A previous version of this story reported an incorrect dollar amount of savings through recommended program and policy changes.
WASHINGTON – By implementing a series of payment reforms now – and adopting MedPAC’s recommendations on replacing the SGR – Congress can fix the Medicare physician pay problem and come closer to paying for it, too.
That’s the bottom line of the March 2012 Report to Congress from the Medicare Payment Advisory Commission (MedPAC), released March 15.
While the recommended cuts may cause some physicians to wince, according to Mark Miller, the blow would be much harder if Congress allows the nearly 30% physician pay cut called for by the Medicare Sustainable Growth Rate formula to go through, Mr. Miller, MedPAC executive director, said at the press conference.
The MedPAC report – on of two Congress requires the group to produce each year – repeats the SGR replacement recommendationsthe commission made last October. Key among those recommendations was freezing most Medicare payments to primary care physicians for 10 years and cutting specialists’ payments by 17% over 3 years, followed by a freeze for 7 years more.
"That’s hard medicine," Mr. Miller said at the press conference. "But one of the things that it does is it reduces the cost of the fix."
MedPAC estimates their recommendations will bring the price tag of repealing the SGR to approximately $200 billion. He added that while Medicare reimbursement would go down under their proposal, historical trends show that the volume of services would go up, increasing their overall net pay.
To pick up another $60 billion to $65 billion in savings, the MedPAC March report lists 29 recommended program and policy changes.*
Key among the changes:
• Freeze payments to skilled nursing facilities in 2013, then cut them by 4% in 2014.
• Equalize payments for office-based and hospital outpatient services. Currently, Medicare pays nearly 80% for certain services when they are provided in a hospital outpatient setting vs. the physician’s office, the report said.
"If the fee schedule assumes that something takes 35 minutes ... and the efficient physician is knocking it off in 15 minutes, then the Medicare program is systematically overpaying for that service," Mr. Miller said. The idea, he said, is to promote a more equal pay between specialty and primary care services.
• Modify Medicare Part D low-income subsidies to favor more generic drugs in certain therapeutic classes.
Mr. Miller added that protecting and encouraging expansion in primary care is the commission’s top priority, one that is not perpetuated through the current payment system.
"There continues to be this concern in the commission that the fee schedule is imbalanced, that it favors procedural services and it undervalues cognitive visit-based [evaluation and management] type of services," Mr. Miller said.
While Congress has yet to solve the SGR problem, Mr. Miller said that the MedPAC commissioners recognize that lawmakers face a seemingly insurmountable challenge.
"The biggest reason that Congress doesn’t move forward on this issue is that it costs $300 billion ... it’s a big cost."
*Correction 3/29/12: A previous version of this story reported an incorrect dollar amount of savings through recommended program and policy changes.
WASHINGTON – By implementing a series of payment reforms now – and adopting MedPAC’s recommendations on replacing the SGR – Congress can fix the Medicare physician pay problem and come closer to paying for it, too.
That’s the bottom line of the March 2012 Report to Congress from the Medicare Payment Advisory Commission (MedPAC), released March 15.
While the recommended cuts may cause some physicians to wince, according to Mark Miller, the blow would be much harder if Congress allows the nearly 30% physician pay cut called for by the Medicare Sustainable Growth Rate formula to go through, Mr. Miller, MedPAC executive director, said at the press conference.
The MedPAC report – on of two Congress requires the group to produce each year – repeats the SGR replacement recommendationsthe commission made last October. Key among those recommendations was freezing most Medicare payments to primary care physicians for 10 years and cutting specialists’ payments by 17% over 3 years, followed by a freeze for 7 years more.
"That’s hard medicine," Mr. Miller said at the press conference. "But one of the things that it does is it reduces the cost of the fix."
MedPAC estimates their recommendations will bring the price tag of repealing the SGR to approximately $200 billion. He added that while Medicare reimbursement would go down under their proposal, historical trends show that the volume of services would go up, increasing their overall net pay.
To pick up another $60 billion to $65 billion in savings, the MedPAC March report lists 29 recommended program and policy changes.*
Key among the changes:
• Freeze payments to skilled nursing facilities in 2013, then cut them by 4% in 2014.
• Equalize payments for office-based and hospital outpatient services. Currently, Medicare pays nearly 80% for certain services when they are provided in a hospital outpatient setting vs. the physician’s office, the report said.
"If the fee schedule assumes that something takes 35 minutes ... and the efficient physician is knocking it off in 15 minutes, then the Medicare program is systematically overpaying for that service," Mr. Miller said. The idea, he said, is to promote a more equal pay between specialty and primary care services.
• Modify Medicare Part D low-income subsidies to favor more generic drugs in certain therapeutic classes.
Mr. Miller added that protecting and encouraging expansion in primary care is the commission’s top priority, one that is not perpetuated through the current payment system.
"There continues to be this concern in the commission that the fee schedule is imbalanced, that it favors procedural services and it undervalues cognitive visit-based [evaluation and management] type of services," Mr. Miller said.
While Congress has yet to solve the SGR problem, Mr. Miller said that the MedPAC commissioners recognize that lawmakers face a seemingly insurmountable challenge.
"The biggest reason that Congress doesn’t move forward on this issue is that it costs $300 billion ... it’s a big cost."
*Correction 3/29/12: A previous version of this story reported an incorrect dollar amount of savings through recommended program and policy changes.
FROM A PRESS CONFERENCE CALLED BY THE MEDICARE PAYMENT ADVISORY COMMISSION
Medicaid Project Tests Emergency Care at Psych Hospitals
A $75 million demonstration project aims to see if Medicaid patients with a psychiatric emergency would get better, more efficient care from a psychiatric hospital.
Under current law, Medicaid cannot pay for care provided in psychiatric hospitals. Patients with a psychiatric emergency – those expressing homicidal or suicidal thoughts or actions – generally are treated in the emergency department, which may not be staffed or equipped provide adequate care for them, officials from the Centers for Medicare and Medicaid Services said in announcing the demonstration March 13.
"This new demonstration will help ensure patients receive appropriate, high quality care when they need it most and save states money," acting CMS administrator Marilyn Tavenner said in a statement.
The three-year project – funded under the Affordable Care Act – covers Medicaid enrollees aged 21-64 years in 11 states and the District of Columbia. The project was designed based on proposals from the participating states: Alabama, California, Connecticut, Illinois, Maine, Maryland, Missouri, North Carolina, Rhode Island, Washington, and West Virginia.
Medicaid programs in participating states will receive federal matching funds to help pay for services needed by Medicaid patients being treated at private psychiatric hospitals. They'll also be required to match nearly 45% of federal dollars, resulting in $115 million to $120 million in total spending, said Mark Covall, president and CEO of the National Association of Psychiatric Health Systems. Following the demonstration, Medicaid programs will participate in a survey to evaluate changes in quality of care and program costs.
The American Psychiatric Association has opposed the Medicaid exclusion of private psychiatric hospitals since long before passage of the Affordable Care Act, Nicholas Meyers, APA director of government relations, said in an interview. He added that the organization is relieved that CMS is listening.
"We’re delighted to see that CMS has moved forward with this," Mr. Meyers said. "It will test what happened when a contradiction in federal law is eliminated and thus it will help insure that patients get the appropriate treatment and hospitals get reimbursed for the services they’re required to be providing."
Mr. Covall said the demonstration was approved because of both the increased awareness of the need for inpatient psychiatric care and the burden on the emergency care system. Since most emergency rooms don’t have enough beds to meet the demand, Mr. Covall said patients are often forced to stay in emergency rooms for hours, days, and sometimes even weeks. He added that the demonstration will help address barriers to access as well as cost implications.
"This will allow those patients that are in these emergency departments to be quickly triaged and sent over to the freestanding psychiatric hospital where they will be able to be fully assessed and then admitted to an impatient psychiatric unit," Mr. Covall said in an interview.
In addition to testing the affect of Medicaid reimbursement on the quality of care at psychiatric emergency facilities, the demonstration is also test whether expanded coverage will reduce the burden on general acute care hospital emergency departments.
A $75 million demonstration project aims to see if Medicaid patients with a psychiatric emergency would get better, more efficient care from a psychiatric hospital.
Under current law, Medicaid cannot pay for care provided in psychiatric hospitals. Patients with a psychiatric emergency – those expressing homicidal or suicidal thoughts or actions – generally are treated in the emergency department, which may not be staffed or equipped provide adequate care for them, officials from the Centers for Medicare and Medicaid Services said in announcing the demonstration March 13.
"This new demonstration will help ensure patients receive appropriate, high quality care when they need it most and save states money," acting CMS administrator Marilyn Tavenner said in a statement.
The three-year project – funded under the Affordable Care Act – covers Medicaid enrollees aged 21-64 years in 11 states and the District of Columbia. The project was designed based on proposals from the participating states: Alabama, California, Connecticut, Illinois, Maine, Maryland, Missouri, North Carolina, Rhode Island, Washington, and West Virginia.
Medicaid programs in participating states will receive federal matching funds to help pay for services needed by Medicaid patients being treated at private psychiatric hospitals. They'll also be required to match nearly 45% of federal dollars, resulting in $115 million to $120 million in total spending, said Mark Covall, president and CEO of the National Association of Psychiatric Health Systems. Following the demonstration, Medicaid programs will participate in a survey to evaluate changes in quality of care and program costs.
The American Psychiatric Association has opposed the Medicaid exclusion of private psychiatric hospitals since long before passage of the Affordable Care Act, Nicholas Meyers, APA director of government relations, said in an interview. He added that the organization is relieved that CMS is listening.
"We’re delighted to see that CMS has moved forward with this," Mr. Meyers said. "It will test what happened when a contradiction in federal law is eliminated and thus it will help insure that patients get the appropriate treatment and hospitals get reimbursed for the services they’re required to be providing."
Mr. Covall said the demonstration was approved because of both the increased awareness of the need for inpatient psychiatric care and the burden on the emergency care system. Since most emergency rooms don’t have enough beds to meet the demand, Mr. Covall said patients are often forced to stay in emergency rooms for hours, days, and sometimes even weeks. He added that the demonstration will help address barriers to access as well as cost implications.
"This will allow those patients that are in these emergency departments to be quickly triaged and sent over to the freestanding psychiatric hospital where they will be able to be fully assessed and then admitted to an impatient psychiatric unit," Mr. Covall said in an interview.
In addition to testing the affect of Medicaid reimbursement on the quality of care at psychiatric emergency facilities, the demonstration is also test whether expanded coverage will reduce the burden on general acute care hospital emergency departments.
A $75 million demonstration project aims to see if Medicaid patients with a psychiatric emergency would get better, more efficient care from a psychiatric hospital.
Under current law, Medicaid cannot pay for care provided in psychiatric hospitals. Patients with a psychiatric emergency – those expressing homicidal or suicidal thoughts or actions – generally are treated in the emergency department, which may not be staffed or equipped provide adequate care for them, officials from the Centers for Medicare and Medicaid Services said in announcing the demonstration March 13.
"This new demonstration will help ensure patients receive appropriate, high quality care when they need it most and save states money," acting CMS administrator Marilyn Tavenner said in a statement.
The three-year project – funded under the Affordable Care Act – covers Medicaid enrollees aged 21-64 years in 11 states and the District of Columbia. The project was designed based on proposals from the participating states: Alabama, California, Connecticut, Illinois, Maine, Maryland, Missouri, North Carolina, Rhode Island, Washington, and West Virginia.
Medicaid programs in participating states will receive federal matching funds to help pay for services needed by Medicaid patients being treated at private psychiatric hospitals. They'll also be required to match nearly 45% of federal dollars, resulting in $115 million to $120 million in total spending, said Mark Covall, president and CEO of the National Association of Psychiatric Health Systems. Following the demonstration, Medicaid programs will participate in a survey to evaluate changes in quality of care and program costs.
The American Psychiatric Association has opposed the Medicaid exclusion of private psychiatric hospitals since long before passage of the Affordable Care Act, Nicholas Meyers, APA director of government relations, said in an interview. He added that the organization is relieved that CMS is listening.
"We’re delighted to see that CMS has moved forward with this," Mr. Meyers said. "It will test what happened when a contradiction in federal law is eliminated and thus it will help insure that patients get the appropriate treatment and hospitals get reimbursed for the services they’re required to be providing."
Mr. Covall said the demonstration was approved because of both the increased awareness of the need for inpatient psychiatric care and the burden on the emergency care system. Since most emergency rooms don’t have enough beds to meet the demand, Mr. Covall said patients are often forced to stay in emergency rooms for hours, days, and sometimes even weeks. He added that the demonstration will help address barriers to access as well as cost implications.
"This will allow those patients that are in these emergency departments to be quickly triaged and sent over to the freestanding psychiatric hospital where they will be able to be fully assessed and then admitted to an impatient psychiatric unit," Mr. Covall said in an interview.
In addition to testing the affect of Medicaid reimbursement on the quality of care at psychiatric emergency facilities, the demonstration is also test whether expanded coverage will reduce the burden on general acute care hospital emergency departments.
Surgeon General: Decline in Tobacco Use Stalls
Approximately 3,800 children smoke their first cigarette every day and the rates of tobacco initiation are no longer declining, according to the Surgeon General’s report, "Preventing Tobacco Use Among Youth and Young Adults."
"Every day, 1,200 Americans die from smoking and each of those people are replaced by two young smokers," Surgeon General Regina Benjamin said at a press conference. "We know that prevention is the key ... If we can just get [young people] to remain smoke free until they’re 26, then less than 1% of them will ever start."
Among adults who smoke daily, 88% smoked their first cigarette before their 18th birthday; nearly all (99%) did so before their 26th.
According to the report, nearly 25% of high school seniors are current smokers, compared with about 33% of young adults, and about 20% of adults. And it’s not all cigarettes: About 1 in 10 male high school seniors currently uses smokeless tobacco and about 1 in 5 smokes cigars, according to the report.
The report, which updates the 1994 Surgeon General report on tobacco use in youth, highlights the immediate and long-term health consequences to which children and young adults are most vulnerable. These include cardiovascular damage, reduced lung function and growth, and risk of chronic obstructive pulmonary disease.
Because they’re impressionable, young adults and children also are vulnerable to tobacco advertising and targeted products. Even though the landmark 1998 Master Settlement Agreement drastically restricted the way tobacco can be marketed, one-third of the top grossing children’s movies in 2010 contained images of smoking, according to the report.
"Far too many kids still see smoking images and messages every day that normalize this dependence," said Dr. Howard Koh, assistant secretary for health in the Health and Human Services department. "Kids see smoking in the movies they watch, the video games they play, the websites they visit, and in the communities where they live."
Physician organizations voiced support of the report and recommended that it be used to help protect young people from using tobacco products.
"As pediatricians, and parents, we need to send a clear message to the studios that this must stop now," Dr. Robert W. Block, AAP president, said in a statement. Dr. Block added that the Surgeon General’s report should be used to help overturn a recent federal court decision that called graphic cigarette warning labels unconstitutional.
"Warning labels play a critical role in educating children, teens, and parents about the negative health impacts of tobacco. By ignoring health harms from tobacco, we are not only sustaining incredible costs in health care, but we are also risking the lives of youth and young adults. This is simply irresponsible," he said.
"If we can just get [young people] to remain smoke free until they’re 26, then less than 1% of them will ever start."
In a statement, Dr. Jack Lewin, chief executive officer of the American College of Cardiology said, "the Surgeon General’s decision to reinvigorate efforts to keep children and young adults from smoking and to encourage smoking cessation will help us continue downward the trend of mortality due to heart disease and save millions in spending on health care."
The American Medical Association called for better funding of smoking cessation programs. The AMA "is concerned that these smokers will not get the support and assistance needed to combat their addiction," Dr. Peter Carmel, the association’s president, said in a statement. "Increasing the price of tobacco and adopting comprehensive smoke-free laws throughout the entire nation would also help reduce the health, social, and economic consequences associated with tobacco use among our youth."
The American Heart Association called the report a wake-up call. "This insightful new report makes it clear that we cannot let our guard down for a minute when it comes to tobacco addiction," CEO Nancy Brown said in a statement. While many Americans may think tobacco use is fading away, the evidence in this report tells a dramatically different story."
Approximately 3,800 children smoke their first cigarette every day and the rates of tobacco initiation are no longer declining, according to the Surgeon General’s report, "Preventing Tobacco Use Among Youth and Young Adults."
"Every day, 1,200 Americans die from smoking and each of those people are replaced by two young smokers," Surgeon General Regina Benjamin said at a press conference. "We know that prevention is the key ... If we can just get [young people] to remain smoke free until they’re 26, then less than 1% of them will ever start."
Among adults who smoke daily, 88% smoked their first cigarette before their 18th birthday; nearly all (99%) did so before their 26th.
According to the report, nearly 25% of high school seniors are current smokers, compared with about 33% of young adults, and about 20% of adults. And it’s not all cigarettes: About 1 in 10 male high school seniors currently uses smokeless tobacco and about 1 in 5 smokes cigars, according to the report.
The report, which updates the 1994 Surgeon General report on tobacco use in youth, highlights the immediate and long-term health consequences to which children and young adults are most vulnerable. These include cardiovascular damage, reduced lung function and growth, and risk of chronic obstructive pulmonary disease.
Because they’re impressionable, young adults and children also are vulnerable to tobacco advertising and targeted products. Even though the landmark 1998 Master Settlement Agreement drastically restricted the way tobacco can be marketed, one-third of the top grossing children’s movies in 2010 contained images of smoking, according to the report.
"Far too many kids still see smoking images and messages every day that normalize this dependence," said Dr. Howard Koh, assistant secretary for health in the Health and Human Services department. "Kids see smoking in the movies they watch, the video games they play, the websites they visit, and in the communities where they live."
Physician organizations voiced support of the report and recommended that it be used to help protect young people from using tobacco products.
"As pediatricians, and parents, we need to send a clear message to the studios that this must stop now," Dr. Robert W. Block, AAP president, said in a statement. Dr. Block added that the Surgeon General’s report should be used to help overturn a recent federal court decision that called graphic cigarette warning labels unconstitutional.
"Warning labels play a critical role in educating children, teens, and parents about the negative health impacts of tobacco. By ignoring health harms from tobacco, we are not only sustaining incredible costs in health care, but we are also risking the lives of youth and young adults. This is simply irresponsible," he said.
"If we can just get [young people] to remain smoke free until they’re 26, then less than 1% of them will ever start."
In a statement, Dr. Jack Lewin, chief executive officer of the American College of Cardiology said, "the Surgeon General’s decision to reinvigorate efforts to keep children and young adults from smoking and to encourage smoking cessation will help us continue downward the trend of mortality due to heart disease and save millions in spending on health care."
The American Medical Association called for better funding of smoking cessation programs. The AMA "is concerned that these smokers will not get the support and assistance needed to combat their addiction," Dr. Peter Carmel, the association’s president, said in a statement. "Increasing the price of tobacco and adopting comprehensive smoke-free laws throughout the entire nation would also help reduce the health, social, and economic consequences associated with tobacco use among our youth."
The American Heart Association called the report a wake-up call. "This insightful new report makes it clear that we cannot let our guard down for a minute when it comes to tobacco addiction," CEO Nancy Brown said in a statement. While many Americans may think tobacco use is fading away, the evidence in this report tells a dramatically different story."
Approximately 3,800 children smoke their first cigarette every day and the rates of tobacco initiation are no longer declining, according to the Surgeon General’s report, "Preventing Tobacco Use Among Youth and Young Adults."
"Every day, 1,200 Americans die from smoking and each of those people are replaced by two young smokers," Surgeon General Regina Benjamin said at a press conference. "We know that prevention is the key ... If we can just get [young people] to remain smoke free until they’re 26, then less than 1% of them will ever start."
Among adults who smoke daily, 88% smoked their first cigarette before their 18th birthday; nearly all (99%) did so before their 26th.
According to the report, nearly 25% of high school seniors are current smokers, compared with about 33% of young adults, and about 20% of adults. And it’s not all cigarettes: About 1 in 10 male high school seniors currently uses smokeless tobacco and about 1 in 5 smokes cigars, according to the report.
The report, which updates the 1994 Surgeon General report on tobacco use in youth, highlights the immediate and long-term health consequences to which children and young adults are most vulnerable. These include cardiovascular damage, reduced lung function and growth, and risk of chronic obstructive pulmonary disease.
Because they’re impressionable, young adults and children also are vulnerable to tobacco advertising and targeted products. Even though the landmark 1998 Master Settlement Agreement drastically restricted the way tobacco can be marketed, one-third of the top grossing children’s movies in 2010 contained images of smoking, according to the report.
"Far too many kids still see smoking images and messages every day that normalize this dependence," said Dr. Howard Koh, assistant secretary for health in the Health and Human Services department. "Kids see smoking in the movies they watch, the video games they play, the websites they visit, and in the communities where they live."
Physician organizations voiced support of the report and recommended that it be used to help protect young people from using tobacco products.
"As pediatricians, and parents, we need to send a clear message to the studios that this must stop now," Dr. Robert W. Block, AAP president, said in a statement. Dr. Block added that the Surgeon General’s report should be used to help overturn a recent federal court decision that called graphic cigarette warning labels unconstitutional.
"Warning labels play a critical role in educating children, teens, and parents about the negative health impacts of tobacco. By ignoring health harms from tobacco, we are not only sustaining incredible costs in health care, but we are also risking the lives of youth and young adults. This is simply irresponsible," he said.
"If we can just get [young people] to remain smoke free until they’re 26, then less than 1% of them will ever start."
In a statement, Dr. Jack Lewin, chief executive officer of the American College of Cardiology said, "the Surgeon General’s decision to reinvigorate efforts to keep children and young adults from smoking and to encourage smoking cessation will help us continue downward the trend of mortality due to heart disease and save millions in spending on health care."
The American Medical Association called for better funding of smoking cessation programs. The AMA "is concerned that these smokers will not get the support and assistance needed to combat their addiction," Dr. Peter Carmel, the association’s president, said in a statement. "Increasing the price of tobacco and adopting comprehensive smoke-free laws throughout the entire nation would also help reduce the health, social, and economic consequences associated with tobacco use among our youth."
The American Heart Association called the report a wake-up call. "This insightful new report makes it clear that we cannot let our guard down for a minute when it comes to tobacco addiction," CEO Nancy Brown said in a statement. While many Americans may think tobacco use is fading away, the evidence in this report tells a dramatically different story."
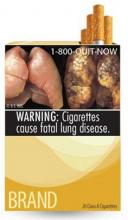
Judge Calls Cigarette Warnings Unconstitutional
The federal regulation requiring tobacco companies to display graphic antismoking images on cigarette packs is unconstitutional, a district judge in Washington, D.C., ruled on Feb. 29.
"For corporations as for individuals, the choice to speak includes within it the choice of what not to say," Judge Richard J. Leon, district judge for the District of Columbia, wrote in the court memorandum. "The Government may engage in advocacy using its own voice ... [but] it may not force others, such as Plaintiffs, to serve as its unwilling mouthpiece."
Five tobacco companies – R.J. Reynolds Tobacco Company, Lorillard, Commonwealth Brands, Liggett Group, and Sante Fe Natural Tobacco Company – brought suit against the regulations in August 2011.
The Food and Drug Administration unveiled the nine graphic labels in June 2011, after proposed labels and associated regulations were available during a public comment period. In addition to the contrasting lungs, other graphic images included a man breathing through an oxygen mask, a bare-chested male cadaver, a woman weeping uncontrollably, a diseased mouth with what appears to be cancerous lesions, and a cartoon of a premature baby in an incubator.
Under the regulation, cigarette manufacturers would be required to display one of nine textual warnings on all cigarette packages distributed. Warnings include: "Smoking can kill you" and "Cigarettes are addictive."
While the court recognized the government’s right to require certain disclosures for clarity, Judge Leon ruled that "purely factual and uncontroversial information may still violate the First Amendment if they are unjustified and unduly burdensome."
Reactions to the judge’s ruling spurred vehement reaction from traditional tobacco opponents.
The ruling ignores the science and puts children at risk, according to a statement from the American Academy of Pediatrics.
"Judge Leon’s dangerous ruling blatantly ignores significant scientific evidence supporting the effectiveness of larger, graphic warning labels in communicating the health dangers of tobacco use," the AAP statement said. "If allowed to stand, this ruling would make it impossible to implement any effective warning labels and will therefore harm the health and well-being of millions of children."
The Obama administration vowed to continue pursuit of the warnings.
"This administration is determined to do everything we can to warn young people about the dangers of smoking, which remains the leading cause of preventable death in America," the Health and Human Services department said in a statement. "This public health initiative will be an effective tool in our efforts to stop teenagers from starting in the first place and taking up this deadly habit. We are confident that efforts to stop these important warnings from going forward will ultimately fail."
Rep. Henry Waxman (D-Calif.) also criticized the decision.
"These provisions were informed by scientific evidence showing that current warning labels have run their course and that labels with graphic warnings would be more effective in protecting the public’s health from tobacco’s addictive and toxic qualities," Rep. Waxman said in a statement. "Congress did, in fact, carefully consider the First Amendment issues involved and carefully tailored the legislation to ensure the FDA could act as it has proposed with graphic warning labels for tobacco products."
Rep. Waxman said he expects the ruling to be appealed and its constitutionality affirmed.
The federal regulation requiring tobacco companies to display graphic antismoking images on cigarette packs is unconstitutional, a district judge in Washington, D.C., ruled on Feb. 29.
"For corporations as for individuals, the choice to speak includes within it the choice of what not to say," Judge Richard J. Leon, district judge for the District of Columbia, wrote in the court memorandum. "The Government may engage in advocacy using its own voice ... [but] it may not force others, such as Plaintiffs, to serve as its unwilling mouthpiece."
Five tobacco companies – R.J. Reynolds Tobacco Company, Lorillard, Commonwealth Brands, Liggett Group, and Sante Fe Natural Tobacco Company – brought suit against the regulations in August 2011.
The Food and Drug Administration unveiled the nine graphic labels in June 2011, after proposed labels and associated regulations were available during a public comment period. In addition to the contrasting lungs, other graphic images included a man breathing through an oxygen mask, a bare-chested male cadaver, a woman weeping uncontrollably, a diseased mouth with what appears to be cancerous lesions, and a cartoon of a premature baby in an incubator.
Under the regulation, cigarette manufacturers would be required to display one of nine textual warnings on all cigarette packages distributed. Warnings include: "Smoking can kill you" and "Cigarettes are addictive."
While the court recognized the government’s right to require certain disclosures for clarity, Judge Leon ruled that "purely factual and uncontroversial information may still violate the First Amendment if they are unjustified and unduly burdensome."
Reactions to the judge’s ruling spurred vehement reaction from traditional tobacco opponents.
The ruling ignores the science and puts children at risk, according to a statement from the American Academy of Pediatrics.
"Judge Leon’s dangerous ruling blatantly ignores significant scientific evidence supporting the effectiveness of larger, graphic warning labels in communicating the health dangers of tobacco use," the AAP statement said. "If allowed to stand, this ruling would make it impossible to implement any effective warning labels and will therefore harm the health and well-being of millions of children."
The Obama administration vowed to continue pursuit of the warnings.
"This administration is determined to do everything we can to warn young people about the dangers of smoking, which remains the leading cause of preventable death in America," the Health and Human Services department said in a statement. "This public health initiative will be an effective tool in our efforts to stop teenagers from starting in the first place and taking up this deadly habit. We are confident that efforts to stop these important warnings from going forward will ultimately fail."
Rep. Henry Waxman (D-Calif.) also criticized the decision.
"These provisions were informed by scientific evidence showing that current warning labels have run their course and that labels with graphic warnings would be more effective in protecting the public’s health from tobacco’s addictive and toxic qualities," Rep. Waxman said in a statement. "Congress did, in fact, carefully consider the First Amendment issues involved and carefully tailored the legislation to ensure the FDA could act as it has proposed with graphic warning labels for tobacco products."
Rep. Waxman said he expects the ruling to be appealed and its constitutionality affirmed.
The federal regulation requiring tobacco companies to display graphic antismoking images on cigarette packs is unconstitutional, a district judge in Washington, D.C., ruled on Feb. 29.
"For corporations as for individuals, the choice to speak includes within it the choice of what not to say," Judge Richard J. Leon, district judge for the District of Columbia, wrote in the court memorandum. "The Government may engage in advocacy using its own voice ... [but] it may not force others, such as Plaintiffs, to serve as its unwilling mouthpiece."
Five tobacco companies – R.J. Reynolds Tobacco Company, Lorillard, Commonwealth Brands, Liggett Group, and Sante Fe Natural Tobacco Company – brought suit against the regulations in August 2011.
The Food and Drug Administration unveiled the nine graphic labels in June 2011, after proposed labels and associated regulations were available during a public comment period. In addition to the contrasting lungs, other graphic images included a man breathing through an oxygen mask, a bare-chested male cadaver, a woman weeping uncontrollably, a diseased mouth with what appears to be cancerous lesions, and a cartoon of a premature baby in an incubator.
Under the regulation, cigarette manufacturers would be required to display one of nine textual warnings on all cigarette packages distributed. Warnings include: "Smoking can kill you" and "Cigarettes are addictive."
While the court recognized the government’s right to require certain disclosures for clarity, Judge Leon ruled that "purely factual and uncontroversial information may still violate the First Amendment if they are unjustified and unduly burdensome."
Reactions to the judge’s ruling spurred vehement reaction from traditional tobacco opponents.
The ruling ignores the science and puts children at risk, according to a statement from the American Academy of Pediatrics.
"Judge Leon’s dangerous ruling blatantly ignores significant scientific evidence supporting the effectiveness of larger, graphic warning labels in communicating the health dangers of tobacco use," the AAP statement said. "If allowed to stand, this ruling would make it impossible to implement any effective warning labels and will therefore harm the health and well-being of millions of children."
The Obama administration vowed to continue pursuit of the warnings.
"This administration is determined to do everything we can to warn young people about the dangers of smoking, which remains the leading cause of preventable death in America," the Health and Human Services department said in a statement. "This public health initiative will be an effective tool in our efforts to stop teenagers from starting in the first place and taking up this deadly habit. We are confident that efforts to stop these important warnings from going forward will ultimately fail."
Rep. Henry Waxman (D-Calif.) also criticized the decision.
"These provisions were informed by scientific evidence showing that current warning labels have run their course and that labels with graphic warnings would be more effective in protecting the public’s health from tobacco’s addictive and toxic qualities," Rep. Waxman said in a statement. "Congress did, in fact, carefully consider the First Amendment issues involved and carefully tailored the legislation to ensure the FDA could act as it has proposed with graphic warning labels for tobacco products."
Rep. Waxman said he expects the ruling to be appealed and its constitutionality affirmed.
Implementation Gets Tricky: The Policy & Practice Podcast
Controversy is heating up over the health reform law's package of essential health benefits -- specifically, over the law's requirement of coverage of co-pay free contraception and other women's reproductive health benefits. Seven state attorneys general have filed suit in federal court, calling that provision a violation of the First Amendment.
In other big news, the administration released its proposed rules for the next stage of meaningful use of health IT. The proposal would provide more flexibility for doctors, but also a bit more work.
Finally, the Obama administration touted the success of its Pre-existing Conditions Insurance Plan, another part of the Affordable Care Act. Since PCIP's implementation, 50,000 people have gained coverage. Although getting into the program requires being uninsured for 6 months and then paying a hefty premium, the administration said it was receiving 8,000 applications per month by the end of last year.
For more on that, listen to this week's Policy & Practice Podcast.
Controversy is heating up over the health reform law's package of essential health benefits -- specifically, over the law's requirement of coverage of co-pay free contraception and other women's reproductive health benefits. Seven state attorneys general have filed suit in federal court, calling that provision a violation of the First Amendment.
In other big news, the administration released its proposed rules for the next stage of meaningful use of health IT. The proposal would provide more flexibility for doctors, but also a bit more work.
Finally, the Obama administration touted the success of its Pre-existing Conditions Insurance Plan, another part of the Affordable Care Act. Since PCIP's implementation, 50,000 people have gained coverage. Although getting into the program requires being uninsured for 6 months and then paying a hefty premium, the administration said it was receiving 8,000 applications per month by the end of last year.
For more on that, listen to this week's Policy & Practice Podcast.
Controversy is heating up over the health reform law's package of essential health benefits -- specifically, over the law's requirement of coverage of co-pay free contraception and other women's reproductive health benefits. Seven state attorneys general have filed suit in federal court, calling that provision a violation of the First Amendment.
In other big news, the administration released its proposed rules for the next stage of meaningful use of health IT. The proposal would provide more flexibility for doctors, but also a bit more work.
Finally, the Obama administration touted the success of its Pre-existing Conditions Insurance Plan, another part of the Affordable Care Act. Since PCIP's implementation, 50,000 people have gained coverage. Although getting into the program requires being uninsured for 6 months and then paying a hefty premium, the administration said it was receiving 8,000 applications per month by the end of last year.
For more on that, listen to this week's Policy & Practice Podcast.
Setting Realistic Expectations Is Key to Happy Patients
To avoid unsatisfied patients, dermatologists should ensure patients have realistic expectations, according to Dr. Howard K. Steinman.
Dermatologists are often faced with patients with vague expectations, he said at the annual Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF). "They don’t know what they want improved, they’re just unhappy with the way they look, and they’re among the most difficult patients to deal with," said Dr. Steinman, director of dermatologic and skin cancer surgery at Scott and White Healthcare in Temple, Tex.
To successfully avoid leaving patients unsatisfied, he recommends the following strategies:
• Get the specifics. When meeting with a new patient, the first thing Dr. Steinman does is hand them a mirror and ask what they want changed. If there are several concerns, ask them to narrow it down to the top three.
• Burst their bubble. Make sure their expectations are realistic. Patients may be seeking a procedure that they saw in a magazine but it may not work for them. Patients with minor damage may request major treatments and vice versa. Be certain to clarify what each treatment will and will not accomplish.
• Rephrase. Summarize the patient’s concerns to ensure it was understood, he said.
• Assess lifestyle. To guarantee a successful experience, make sure patients will be able to tolerate the healing process and any possible complications. Ensure the patient has a supportive caregiver to assist in the process and that, after the procedure, the wound will be properly cared for.
• Overestimate. Depending on the procedure, make sure the patient understands how many treatments are required (include the cost for each treatment). When in doubt, overestimate. If the procedure requires between four and eight treatments, they’ll likely hear four, said Dr. Steinman. Make sure they are also aware of any necessary maintenance or touch-ups that may be needed.
• Base time frames on holidays. Patients are anxious to see results so they may hear 6 weeks when what was really said was 6 months. Therefore, pick a holiday closest to when patients are likely to see results; they’ll be more likely to remember it, and it’ll be easier for clinicians to keep track.
• Get on the same page. Make sure patient expectations match the likely results before they leave the office, he recommended. If the patient’s desires cannot fully be understood because of language or cultural barriers, refer the patient to another physician who can meet their needs.
Dr. Steinman did not have any relevant disclosures to report. SDEF and this news organization are owned by Elsevier.
To avoid unsatisfied patients, dermatologists should ensure patients have realistic expectations, according to Dr. Howard K. Steinman.
Dermatologists are often faced with patients with vague expectations, he said at the annual Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF). "They don’t know what they want improved, they’re just unhappy with the way they look, and they’re among the most difficult patients to deal with," said Dr. Steinman, director of dermatologic and skin cancer surgery at Scott and White Healthcare in Temple, Tex.
To successfully avoid leaving patients unsatisfied, he recommends the following strategies:
• Get the specifics. When meeting with a new patient, the first thing Dr. Steinman does is hand them a mirror and ask what they want changed. If there are several concerns, ask them to narrow it down to the top three.
• Burst their bubble. Make sure their expectations are realistic. Patients may be seeking a procedure that they saw in a magazine but it may not work for them. Patients with minor damage may request major treatments and vice versa. Be certain to clarify what each treatment will and will not accomplish.
• Rephrase. Summarize the patient’s concerns to ensure it was understood, he said.
• Assess lifestyle. To guarantee a successful experience, make sure patients will be able to tolerate the healing process and any possible complications. Ensure the patient has a supportive caregiver to assist in the process and that, after the procedure, the wound will be properly cared for.
• Overestimate. Depending on the procedure, make sure the patient understands how many treatments are required (include the cost for each treatment). When in doubt, overestimate. If the procedure requires between four and eight treatments, they’ll likely hear four, said Dr. Steinman. Make sure they are also aware of any necessary maintenance or touch-ups that may be needed.
• Base time frames on holidays. Patients are anxious to see results so they may hear 6 weeks when what was really said was 6 months. Therefore, pick a holiday closest to when patients are likely to see results; they’ll be more likely to remember it, and it’ll be easier for clinicians to keep track.
• Get on the same page. Make sure patient expectations match the likely results before they leave the office, he recommended. If the patient’s desires cannot fully be understood because of language or cultural barriers, refer the patient to another physician who can meet their needs.
Dr. Steinman did not have any relevant disclosures to report. SDEF and this news organization are owned by Elsevier.
To avoid unsatisfied patients, dermatologists should ensure patients have realistic expectations, according to Dr. Howard K. Steinman.
Dermatologists are often faced with patients with vague expectations, he said at the annual Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF). "They don’t know what they want improved, they’re just unhappy with the way they look, and they’re among the most difficult patients to deal with," said Dr. Steinman, director of dermatologic and skin cancer surgery at Scott and White Healthcare in Temple, Tex.
To successfully avoid leaving patients unsatisfied, he recommends the following strategies:
• Get the specifics. When meeting with a new patient, the first thing Dr. Steinman does is hand them a mirror and ask what they want changed. If there are several concerns, ask them to narrow it down to the top three.
• Burst their bubble. Make sure their expectations are realistic. Patients may be seeking a procedure that they saw in a magazine but it may not work for them. Patients with minor damage may request major treatments and vice versa. Be certain to clarify what each treatment will and will not accomplish.
• Rephrase. Summarize the patient’s concerns to ensure it was understood, he said.
• Assess lifestyle. To guarantee a successful experience, make sure patients will be able to tolerate the healing process and any possible complications. Ensure the patient has a supportive caregiver to assist in the process and that, after the procedure, the wound will be properly cared for.
• Overestimate. Depending on the procedure, make sure the patient understands how many treatments are required (include the cost for each treatment). When in doubt, overestimate. If the procedure requires between four and eight treatments, they’ll likely hear four, said Dr. Steinman. Make sure they are also aware of any necessary maintenance or touch-ups that may be needed.
• Base time frames on holidays. Patients are anxious to see results so they may hear 6 weeks when what was really said was 6 months. Therefore, pick a holiday closest to when patients are likely to see results; they’ll be more likely to remember it, and it’ll be easier for clinicians to keep track.
• Get on the same page. Make sure patient expectations match the likely results before they leave the office, he recommended. If the patient’s desires cannot fully be understood because of language or cultural barriers, refer the patient to another physician who can meet their needs.
Dr. Steinman did not have any relevant disclosures to report. SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM THE SDEF HAWAII DERMATOLOGY SEMINAR
Congress Serves Up Short-Term SGR Fix
UPDATE: The House of Representatives passed the payroll tax extension/SGR fix bill Feb. 17 by a vote of 293-132. The bill now moves on to the Senate.
After weeks of debate, congressional negotiators at press time were poised to grant a 10-month reprieve from the looming 27% cut in Medicare physician fees called for by the Sustainable Growth Rate formula.
The House/Senate conference committee tasked to solve that problem – while finding a way to extend the payroll tax holiday and benefits for the long-term unemployed – reached an agreement in the wee hours of Feb. 16. Their compromise would hold Medicare fees steady through the end of 2012.
Officials at the American Medical Association expressed both relief and disappointment with the deal.
"Congress had an opportunity to permanently end this problem, which is the sound, fiscally prudent policy choice," Dr. Peter W. Carmel, AMA president, said in a statement. "We appreciate efforts by members of Congress on both sides of the aisle who publicly supported a framework for a permanent end to this perennial problem. We are deeply disappointed that Congress chose to just do another patch – kicking the can, growing the problem and missing a clear opportunity to protect access to care for patients."
The short-term SGR fix does not come as a surprise, however. At the AMA National Advocacy Conference this week, Sen. Jon Kyl (R-Ariz.) warned physicians that negotiators would not agree to repeal the SGR. He added that negotiators were wrestling between a 2-year and a 10-month update.
At press time, the compromise was not official and full details had not been reported.
Both houses of Congress were expected to vote on the measure before taking a weeklong recess for the Presidents’ Day holiday.
UPDATE: The House of Representatives passed the payroll tax extension/SGR fix bill Feb. 17 by a vote of 293-132. The bill now moves on to the Senate.
After weeks of debate, congressional negotiators at press time were poised to grant a 10-month reprieve from the looming 27% cut in Medicare physician fees called for by the Sustainable Growth Rate formula.
The House/Senate conference committee tasked to solve that problem – while finding a way to extend the payroll tax holiday and benefits for the long-term unemployed – reached an agreement in the wee hours of Feb. 16. Their compromise would hold Medicare fees steady through the end of 2012.
Officials at the American Medical Association expressed both relief and disappointment with the deal.
"Congress had an opportunity to permanently end this problem, which is the sound, fiscally prudent policy choice," Dr. Peter W. Carmel, AMA president, said in a statement. "We appreciate efforts by members of Congress on both sides of the aisle who publicly supported a framework for a permanent end to this perennial problem. We are deeply disappointed that Congress chose to just do another patch – kicking the can, growing the problem and missing a clear opportunity to protect access to care for patients."
The short-term SGR fix does not come as a surprise, however. At the AMA National Advocacy Conference this week, Sen. Jon Kyl (R-Ariz.) warned physicians that negotiators would not agree to repeal the SGR. He added that negotiators were wrestling between a 2-year and a 10-month update.
At press time, the compromise was not official and full details had not been reported.
Both houses of Congress were expected to vote on the measure before taking a weeklong recess for the Presidents’ Day holiday.
UPDATE: The House of Representatives passed the payroll tax extension/SGR fix bill Feb. 17 by a vote of 293-132. The bill now moves on to the Senate.
After weeks of debate, congressional negotiators at press time were poised to grant a 10-month reprieve from the looming 27% cut in Medicare physician fees called for by the Sustainable Growth Rate formula.
The House/Senate conference committee tasked to solve that problem – while finding a way to extend the payroll tax holiday and benefits for the long-term unemployed – reached an agreement in the wee hours of Feb. 16. Their compromise would hold Medicare fees steady through the end of 2012.
Officials at the American Medical Association expressed both relief and disappointment with the deal.
"Congress had an opportunity to permanently end this problem, which is the sound, fiscally prudent policy choice," Dr. Peter W. Carmel, AMA president, said in a statement. "We appreciate efforts by members of Congress on both sides of the aisle who publicly supported a framework for a permanent end to this perennial problem. We are deeply disappointed that Congress chose to just do another patch – kicking the can, growing the problem and missing a clear opportunity to protect access to care for patients."
The short-term SGR fix does not come as a surprise, however. At the AMA National Advocacy Conference this week, Sen. Jon Kyl (R-Ariz.) warned physicians that negotiators would not agree to repeal the SGR. He added that negotiators were wrestling between a 2-year and a 10-month update.
At press time, the compromise was not official and full details had not been reported.
Both houses of Congress were expected to vote on the measure before taking a weeklong recess for the Presidents’ Day holiday.