User login
Hypertension in the elderly: Some practical considerations
The management of hypertension has advanced significantly in the last few decades. But the race for more effective means to control this epidemic and its associated complications is far from won. A high percentage of patients in the United States have hypertension that is uncontrolled. Most of these belong to the most rapidly growing demographic group in the United States, ie, the elderly.
It is estimated that more than 70% of medical practice will be directed to geriatric needs in the coming years. It is therefore very important for clinicians to be comfortable with managing hypertension in the elderly.
A GROWING PROBLEM IN AN AGING POPULATION
Between 1980 and 2009, the US population age 65 and older increased from 25.6 million to 39.6 million, of which 42% are men and 58% women.1 This number is expected to reach 75 million by the year 2040. People over 85 years of age are the fastest growing subset of the US population.2 As many as 50% of people who were born recently in countries such as the United States, the United Kingdom, France, Denmark, and Japan will live to celebrate their 100th birthday.3
According to the Framingham Heart Study, by age 60 approximately 60% of the population develops hypertension, and by 70 years about 65% of men and about 75% of women have the disease. In the same study, 90% of those who were normotensive at age 55 went on to develop hypertension. The elderly also are more likely to suffer from the complications of hypertension and are more likely to have uncontrolled disease.
Compared with younger patients with similar blood pressure, elderly hypertensive patients have lower cardiac output, higher peripheral resistance, wider pulse pressure, lower intravascular volume, and lower renal blood flow.4 These age-related pathophysiologic differences must be considered when treating antihypertension in the elderly.
IS TREATING THE ELDERLY BENEFICIAL?
Most elderly hypertensive patients have multiple comorbidities, which tremendously affect the management of their hypertension. They are also more likely than younger patients to have resistant hypertension and to need multiple drugs to control their blood pressure. In the process, these frail patients are exposed to a host of drug-related adverse effects. Thus, it is relevant to question the net benefit of treatment in this age group.
Many studies have indeed shown that treating hypertension reduces the risk of stroke and other adverse cardiovascular events. A decade ago, Staessen et al,5 in a meta-analysis of more than 15,000 patients between ages 62 and 76, showed that treating isolated systolic hypertension substantially reduced morbidity and mortality rates. Moreover, a 2011 meta-analysis of randomized controlled trials in hypertensive patients age 75 and over also concluded that treatment reduced cardiovascular morbidity and mortality rates and the incidence of heart failure, even though the total mortality rate was not affected.6
Opinion on treating the very elderly (≥ 80 years of age) was divided until the results of the Hypertension in the Very Elderly trial (HYVET)7 came out in 2008. This study documented major benefits of treatment in the very elderly age group as well.
The consensus, therefore, is that it is appropriate, even imperative, to treat elderly hypertensive patients (with some cautions—see the sections that follow).
GOAL OF TREATMENT IN THE ELDERLY
Targets for blood pressure management have been based primarily on observational data in middle-aged patients. There is no such thing as an ideal blood pressure that has been derived from randomized controlled trials for any population, let alone the elderly. The generally recommended blood pressure goal of 140/90 mm Hg for elderly hypertensive patients is based on expert opinion.
Moreover, it is unclear if the same target should apply to octogenarians. According to a 2011 American College of Cardiology/American Heart Association (ACC/AHA) expert consensus report,8 an achieved systolic blood pressure of 140 to 145 mm Hg, if tolerated, can be acceptable in this age group.
An orthostatic decline in blood pressure accompanies advanced age and is an inevitable adverse effect of some antihypertensive drugs. Accordingly, systolic blood pressure lower than 130 and diastolic blood pressure lower than 70 mm Hg are best avoided in octogenarians.8 Therefore, when hypertension is complicated by coexisting conditions that require a specific blood pressure goal, it would seem reasonable to not pursue the lower target as aggressively in octogenarians as in elderly patients under age 80.
Having stated the limitations in the quality of data at hand—largely observational—it is relevant to mention the Systolic Blood Pressure Intervention trial (SPRINT).9 This ongoing randomized, multicenter trial, launched by the National Institutes of Health, is assessing whether maintaining blood pressure levels lower than current recommendations further reduces the risk of cardiovascular and kidney diseases or, in the SPRINT-MIND substudy, of age-related cognitive decline, regardless of the type of antihypertensive drug taken. Initially planning to enroll close to 10,000 participants over the age of 55 without specifying any agegroup ranges, the investigators later decided to conduct a substudy called SPRINT Senior that will enroll about 1,750 participants over the age of 75 to determine whether a lower blood pressure range will have the same beneficial effects in older adults.
Given the limitations in the quality and applicability of published data (coming from small, nonrandomized studies with no long-term follow-up), SPRINT is expected to provide the evidence needed to support standard vs aggressive hypertension control among the elderly. The trial is projected to run until late 2018.
MANAGEMENT APPROACH IN THE ELDERLY
Blood pressure should be recorded in both arms before a diagnosis is made. In a number of patients, particularly the elderly, there are significant differences in blood pressure readings between the two arms. The higher reading should be relied on and the corresponding arm used for subsequent measurements.
Lifestyle interventions
Similar to the approach in younger patients with hypertension, lifestyle interventions are the first step to managing high blood pressure in the elderly. The diet and exercise interventions in the Dietary Approaches to Stop Hypertension (DASH) trial have both been shown to lower blood pressure.10,11
Restricting sodium intake has been shown to lower blood pressure more in older adults than in younger adults. In the DASH trial,12 systolic blood pressure decreased by 8.1 mm Hg with sodium restriction in hypertensive patients age 55 to 76 years, compared with 4.8 mm Hg for adults aged 23 to 41 years. In the Trial of Nonpharmacologic Interventions in the Elderly (TONE),13 in people ages 60 to 80 who were randomized to reduce their salt intake, urinary sodium excretion was 40 mmol/day lower and blood pressure was 4.3/2.0 mm Hg lower than in a group that received usual care. Accordingly, reducing salt intake is particularly valuable for blood pressure management in the salt-sensitive elderly.14
Drug therapy
The hypertension pandemic has driven extensive pharmaceutical research, and new drugs continue to be introduced. The major classes of drugs commonly used for treating hypertension are diuretics, calcium channel blockers, and renin-angiotensin system blockers. Each class has specific benefits and adverse-effect profiles.
It is appropriate to start antihypertensive drug therapy with the lowest dose and to monitor for adverse effects, including orthostatic hypotension. The choice of drug should be guided by the patient’s comorbid conditions (Table 1) and the other drugs the patient is taking.15 If the blood pressure response is inadequate, a second drug from a different class should be added. In the same manner, a third drug from a different class should be added if the blood pressure remains outside the optimal range on two drugs.
The average elderly American is on more than six medications.16 Some of these are for high blood pressure, but others interact with antihypertensive drugs (Table 2), and some, including nonsteroidal anti-inflammatory drugs (NSAIDs) and steroids, directly affect blood pressure. Therefore, the drug regimen of an elderly hypertensive patient should be reviewed carefully at every visit. The Screening Tool of Older Person’s Prescriptions (STOPP), a list of 65 rules relating to the most common and most potentially dangerous instances of inappropriate prescribing and overprescribing in the elderly,17 has been found to be a reliable tool in this regard, with a kappa-coefficient of 0.75. Together with the Screening Tool to Alert Doctors to Right [ie, Appropriate, Indicated] Treatment (START),17 which lists 22 evidence-based prescribing indicators for common conditions in the elderly, these criteria provide clinicians with an easy screening tool to combat polypharmacy.
Given the multitude of factors that go into deciding on a specific management strategy in the elderly, it is not possible to discuss individualized care in all patients in the scope of one paper. Below, we present several case scenarios that internists commonly encounter, and suggest ways to approach each.
CASE 1: SECONDARY HYPERTENSION
A 69-year-old obese man who has hypertension of recent onset, long-standing gastroesophageal reflux disease, and benign prostatic hypertrophy comes to your office, accompanied by his wife. He has never had hypertension before. His body mass index is 34 kg/m2. On physical examination, his blood pressure is 180/112 mm Hg.
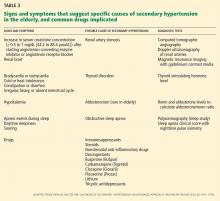
We start with this case to emphasize the importance of considering causes of secondary hypertension in all patients with the disease (Table 3).18 Further workup should be pursued in those who appear to have “inappropriate” hypertension. This could present as refractory hypertension, abrupt-onset hypertension, hypertension that is first diagnosed before age 20 or after age 60, or loss of control over previously well-controlled blood pressure. Secondary hypertension must always be considered when the history or physical examination suggests a possible cause.
Renal artery stenosis increases in incidence with age. Its prevalence is reported to be as high as 50% in elderly patients with other signs of atherosclerosis such as widespread peripheral artery disease.19
Obstructive sleep apnea also commonly coexists with hypertension and its prevalence also increases with age. In addition, elderly patients with obstructive sleep apnea have a higher incidence of cardiovascular complications, including hypertension, than middle-aged people.20 Numerous studies have found that the severity of obstructive sleep apnea corresponds with the likelihood of systemic hypertension.21–23 Randomized trials and meta-analyses have also concluded that effective treatment with continuous positive airway pressure reduces systemic blood pressure,24–27 although by less than antihypertensive medications do.
A causal relationship between obstructive sleep apnea and hypertension has not been established with certainty. It is recommended, however, that patients with resistant hypertension be screened for obstructive sleep apnea as a possible cause of their disease.
Other causes of secondary hypertension to keep in mind when evaluating patients who have inappropriate hypertension include thyroid disorders, alcohol and tobacco use, and chronic steroid or NSAID use. Pheochromocytoma and adrenal adenoma, though possible, are less prevalent in the elderly.
Case continued
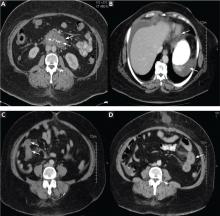
Physical examination in the above patient revealed an epigastric systolic-diastolic bruit, a sign that, although not sensitive, is highly specific for renal artery stenosis, raising the suspicion of this condition. Duplex ultrasonography of the renal arteries confirmed this suspicion. The patient underwent angiography and revascularization, resulting in a distinct fall in, but not normalization of, his blood pressure.
Detecting and treating renal artery stenosis
Though we do not intend to detail the diagnostic approaches and treatments for the various causes of secondary hypertension, we need to briefly mention those for renal artery stenosis.
According to the 2006 ACC/AHA guidelines on peripheral artery disease,28 testing for renal artery stenosis is indicated only if a subsequent corrective procedure is a viable option.
Renal arteriography remains the gold standard for diagnosing renal artery stenosis. However, noninvasive imaging has largely replaced it.
Duplex Doppler ultrasonography, compared with angiography, has a sensitivity of 84% to 98% depending on operator experience, and a specificity of 62% to 99% for detecting renal artery stenosis.29 Some of its limiting factors are the time needed to do the study, its steep learning curve and operator-dependence, and interference with the results by body fat and intestinal gas.
Computed tomographic angiography has a sensitivity of over 90% for detecting renal artery stenosis, and its specificity has been shown to be as high as 99% in certain studies.29 Use of contrast can be a limiting factor in some clinical settings.
Magnetic resonance angiography also offers a sensitivity of 90% to 100% and specificities of 76% to 94% for detecting renal artery stenosis.29 On the other hand, it is costly, and the gadolinium contrast solution used is nephrotoxic, though not as toxic as the contrast used in computed tomographic angiography.
As previously stated, these imaging studies should be used only if corrective measures will be undertaken if clinically significant renal artery stenosis is found. Even in such cases, revascularization may not be curative in all cases. Its effectiveness has been compared with that of medical management alone in a number of studies.30,31 A meta-analysis32 of six key trials involving more than 1,200 patients showed no difference in systolic and diastolic blood pressures and other clinical outcomes, including all-cause mortality, between the two treatment groups over a 29-month follow-up period.
Hence, although we advise that causes of secondary hypertension be considered in cases of inappropriate hypertension, aggressive management must be pursued on a case-by-case basis.
CASE 2: DRUG ADVERSE EFFECTS
A 75-year-old Hispanic woman with a history of treated breast cancer was recently diagnosed with hypertension. Her blood pressure is controlled on amlodipine (Norvasc) 10 mg daily, and her blood pressure today is 128/80 mm Hg. Her only complaint during this office visit is some swelling of her ankles.
Edema and dihydropyridine calcium channel blockers
Like all drugs, antihypertensive medications come with their own set of adverse effects. These are more common as people age—hence the importance of identifying and effectively managing them in the elderly population.
Calcium channel blockers, especially the dihydropyridines—ie, nifedipine (Adalat), amlodipine, felodipine (Plendil), and isradipine (DynaCirc)—are known to cause peripheral vasodilation. Peripheral edema is a common dose-related effect in people on these drugs. In one study, median leg weight increased by 80 g after amlodipine 5 mg was given for 4 weeks, and by another 68 g on a 10-mg dose.33
Ankle swelling, encountered more in women, can be very bothersome. The swelling is related to hyperfiltration of fluid into the interstitial space secondary to intracapillary hypertension. Calcium channel blockers predominantly cause arteriolar dilation by paralyzing the precapillary sphincter, thereby elevating intracapillary pressure.
Traditionally, physicians have lowered the dose of the calcium channel blocker, switched to another drug, or added a diuretic to alleviate the swelling. However, giving a diuretic for edema induced by a calcium channel blocker may not relieve the edema.34
Peripheral edema is much less encountered when a calcium channel blocker is given with an inhibitor of the renin-angiotensin system.35 A meta-analysis concluded that the incidence of peripheral edema was lowered by 38% with such a combination. The same study found angiotensin-converting enzyme (ACE) inhibitors significantly more efficacious for this effect than angiotensin receptor blockers (ARBs).35
ACE inhibitors and ARBs are known to cause venodilation, thereby lowering intra-capillary pressure. It is probable that this effect helps remove the extra fluid sequestered in the capillary bed by the arteriolar dilation from the calcium channel blocker.
Pedal edema associated with use of a calcium channel blocker occurs much more commonly in the elderly than in the young. It is clearly dose-dependent, and the incidence peaks after 6 months of therapy. In the patient described above, adding a low dose of an ACE inhibitor or an ARB (if the patient is ACE inhibitor-intolerant) should relieve the swelling.
Hyponatremia and diuretics
Electrolyte imbalances are another common problem encountered in the elderly. Even though for years attention has been directed to the potassium level, hyponatremia has been equally associated with adverse effects in the elderly, such as an increased risk of fractures as shown in the Rotterdam study.36
In 180 hypertensive inpatients, mean age 76.4, Sharabi et al37 found the incidence of hyponatremia to be three times higher in women than in men (odds ratio 3.10, 95% confidence interval 2.07 to 4.67). Patients were 10 times more likely to be affected after age 65 and 14 times more likely after age 75. Most of the patients affected (74.5%) used a thiazide-type diuretic. Even though in many of the patients diuretics were used for more than 1 year before hyponatremia developed, susceptible patients—such as the frail elderly—can develop severe hyponatremia within days of starting to use a thiazide.38
Severe hyponatremia is potentially life-threatening. Most cases are caused by thiazide rather than loop diuretics.38 Thiazides inhibit electrolyte transport at the cortical diluting sites. As they decrease the glomerular filtration rate acutely, they increase proximal water reabsorption (making the plasma hypotonic), reducing water delivery distally. Loop diuretics, on the other hand, have their main effect at the thick ascending limb, reducing the osmolality at the medullary interstitium and not affecting proximal water reabsorption. Additionally, loop diuretics have a shorter half-life than thiazides, which makes hyponatremia more likely to happen with thiazides.
In patients who develop hyponatremia secondary to diuretic use, appropriate treatment includes stopping the medication, restricting water intake, and repleting electrolyte stores.38 As with any cause of chronic hyponatremia, correction must be cautiously monitored and not hastily done.
Therefore, we advise adding a thiazide diuric with caution in the elderly, and we advise avoiding thiazides in patients with high water or alcohol intake.
CASE 3: DEMENTIA AND HYPERTENSION
A 74-year-old man with long-standing hypertension, gout, and chronic obstructive pulmonary disease was recently diagnosed with Alzheimer dementia. He takes enalapril (Vasotec) 10 mg daily for his blood pressure. His blood pressure is 130/78 mm Hg.
Dementia is one of the most important and common neurologic disorders in the elderly. With the rise in average life expectancy, its magnitude has grown to cause a substantial emotional and economic burden on society and health care.
Midlife hypertension has been demonstrated to be an important modifiable risk factor for late-life cognitive decline,39 mild cognitive impairment,40 and dementia of all causes.41 It has been suggested that hypertension might be part of the pathogenesis of dementia, and targeting high blood pressure might prevent its onset.
Moreover, a significant reduction in both Alzheimer and vascular dementia was demonstrated (risk reduction 55%) with the use of a long-acting dihydropyridine calcium channel blocker (nitrendipine) in the Syst-Eur study.42 However, data from studies such as Systolic Hypertension in the Elderly Program (SHEP) and the HYVET substudy of cognitive function assessement43 showed no difference in dementia between placebo and active therapy with chlorthalidone (Hygroton) (in SHEP) or indapamide (Lozol) (in the HYVET substudy).
Disorders of calcium homeostasis are associated with the brain’s aging process. Probably, the neuroprotective effect of nitrendipine seen in Syst-Eur was due to its ability to affect this process, independent of its blood pressure-lowering effect.
In another prospective study, people over 60 years of age who complained of subjective memory loss showed a significant and positive association between memory scores and the use of calcium channel blockers (+0.14 ± 0.09 in users vs −0.12 ± 0.06 in nonusers; P = .016) independently of age, sex, white matter hyperintensities, and carotid wall cross-sectional area, all of which were associated with worse memory scores.44
Drugs that block the renin-angiotensin system have also been proposed to delay the onset and slow the progression of dementia.45 A small randomized, controlled trial suggested that centrally active ACE inhibitors—those that cross the blood-brain barrier, such as captopril (Capoten), lisinopril (Prinivil), ramipril (Altace), and fosinopril (Monopril)—slow cognitive decline in Alzheimer dementia more than non-centrally active ACE inhibitors or calcium channel blockers.46
Sink et al47 examined data from participants in the Cognition Substudy of the Cardiovascular Health Study48 on the effect of ACE inhibitors on cognitive decline. ACE inhibitors, as a class, showed no benefit in reducing the risk of dementia compared with other antihypertensive drug classes. However, centrally active ACE inhibitors, compared with other medications, were associated with a 65% reduction in cognitive decline per year of drug exposure (P = .01). Non-centrally active ACE inhibitors worsened cognitive decline.
It appears that the brain’s renin-angiotensin system plays a role in the pathogenesis of dementia. Indeed, ACE has been shown to degrade amyloid-beta protein, and its level was increased in brain tissue of Alzheimer patients postmortem.49
The relationship between blood pressure and cognitive function appears to be curvilinear, so that low blood pressure in late life is also associated with dementia and Alzheimer dementia.50 In 5,816 patients age 65 and older, Morris et al51 calculated the percentile scores of four cognitive tests according to the level of blood pressure. Patients with systolic blood pressures of 100 mm Hg, 120 mm Hg, and 180 mm Hg scored lower on the Mini Mental State Examination than those in the 140 to 160 mm Hg range. Patients with diastolic blood pressures between 80 and 90 mm Hg appeared to have the best cognitive function. This further emphasizes that blood pressure control must be pursued in the very elderly, albeit less aggressively. The MIND substudy of the SPRINT trial9 is likely to shed more light on this relationship.
When needed for optimal blood pressure control in a hypertensive patient at risk of dementia, a calcium channel blocker of the dihydropyridine type or a centrally active ACE inhibitor, or both, is preferable.
CASE 4: LABILE HYPERTENSION
A 74-year-old man with hypertension and diabetes mellitus comes to see you in the office. On physical examination, his blood pressure is 175/110 mm Hg. His blood pressure during his last visit 3 months ago was 120/75. He brings a log with him that shows random fluctuations in his blood pressure readings. He takes hydrochlorothiazide 25 mg daily for his blood pressure.
Hypertension in some patients continuously fluctuates between low and high levels. A study in Canada found that up to 15% of all adult hypertensive patients might have labile hypertension.52 In the presence of a normal average blood pressure, visit-to-visit blood pressure variability is usually considered a trivial matter. However, some but not all studies have shown that such visit-to-visit variability in blood pressure is an independent predictor of future cardiovascular events in hypertensive patients, independent of the mean systolic blood pressure.52–54
Blood pressure fluctuates from heartbeat to heartbeat, from morning to night, from winter to summer, and from sitting to standing, and it is prone to increase with exertion, stress, and other factors. But excessive fluctuations in the elderly are most likely the result of excessive stiffness of the arterial tree and a decrease in the windkessel (cushioning) function of the aorta. As a consequence, even small-volume changes in the intravascular system can trigger large blood pressure fluctuations.
There is some evidence that antihypertensive drug classes may differ in their effects on visit-to-visit blood pressure variability. In a 2010 study comparing the effects of different antihypertensive drugs on blood pressure variation, calcium channel blockers and non-loop diuretics were associated with less variation in systolic blood pressure, and calcium channel blockers reduced it the most.55
In the patient described above, switching to a low-dose calcium channel blocker with a thorough follow-up is a reasonable plan.
CASE 5: ORTHOSTATIC HYPOTENSION
A 73-year-old woman with long-standing hypertension complains of some dizziness, especially when getting out of bed in the morning. On physical examination, her blood pressure is 134/100 mm Hg sitting and 115/90 standing. She takes amlodipine 10 mg daily, enalapril 10 mg daily, and chlorthalidone 25 mg daily. Chlorthalidone had been added on her last visit 1 month before.
As a result of the increase in the number of elderly patients with hypertension and guidelines recommending better control in this age group, the number of elderly patients on anti-hypertensive drugs has risen significantly. At the same time, the elderly have increasingly presented with adverse effects of treatment.
Orthostatic hypotension is a drop in systolic pressure of 20 mm Hg or more or a drop in diastolic pressure of 10 mm Hg or more on standing, with or without symptoms. These are caused by cerebral hypoperfusion and include dizziness, lightheadedness, generalized weakness, visual blurring, and, in severe cases, syncope.
Alpha-blockers and nitrates have been most commonly implicated in causing orthostatic hypotension, due to venous pooling. Clearly, not all antihypertensive drugs are equal with regard to their venodilatory effects. Thiazide diuretics, by causing fluid volume depletion, and beta-blockers, by interfering with compensatory cardioacceleration with upright posture, are also commonly involved in causing an excessive blood pressure drop with standing.
Systolic orthostatic hypotension has been shown to be a significant and independent predictor of cardiovascular morbidity and death.56 Moreover, syncope and subsequent falls are an important cause of injury and death in the elderly.57 The clinical combination of hypertension and orthostatic hypotension is, therefore, especially challenging. A compromise between accepting a higher cardiovascular risk at either end of the spectrum with an added higher risk for fall at the lower end has to be made.
To prevent orthostatic hypotension in the elderly, it is important to avoid prescribing high-risk drugs. When starting antihypertensive therapy, a low dose should be used, and the dose should be titrated upward very slowly and cautiously. If orthostatic hypotension is suggested by the history or by the orthostatic test, which is warranted in all elderly hypertensive patients before starting or significantly altering therapy, the potential culprit drug should be withdrawn and the patient reassessed. Improved hydration, elevating the head of the bed, and taking the antihypertensive drug at night are ways to improve symptoms, but these remain largely unproven.
In this patient, the newly added chlorthalidone was stopped, and her symptoms improved.
PSEUDOHYPERTENSION
Since hypertension is defined by a numerical value, it is prudent that this value be accurate. Treating a falsely high reading or leaving a falsely low reading untreated will predispose the elderly patient to increased risk either way. One rare condition in the elderly that can give a falsely high blood pressure reading is pseudohypertension.
Pseudohypertension is a condition in which indirect blood pressure measured by the cuff method overestimates the true intra-arterial blood pressure due to marked underlying arteriosclerosis. The Osler maneuver can be used to differentiate true hypertension from pseudohypertension.58 This is performed by palpating the pulseless radial or brachial artery distal to the inflated cuff. If the artery is palpable despite being pulseless, the patient is said to be “Osler-positive” and likely has pseudohypertension.58
Pseudohypertension should be suspected if the patient has orthostatic hypotension despite normal blood pressure sitting and standing. Also, elevated blood pressure without appropriate target organ disease should raise the suspicion of pseudohypertension. Apart from the Osler maneuver, measuring the intraarterial pressure can confirm this diagnosis.
- US Census Bureau. The 2011 statistical abstract. The national data book. http://www.census.gov/compendia/statab/2011/2011edition.html. Accessed July 24, 2012.
- He W, Sengupta M, Velkoff VA, DeBarros KA. US Census Bureau. Current Population Reports, P23-209. 65+ in the United States: 2005. http://www.census.gov/prod/2006pubs/p23-209.pdf. Accessed July 24, 2012.
- Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet 2009; 374:1196–1208.
- Messerli FH, Sundgaard-Riise K, Ventura HO, Dunn FG, Glade LB, Frohlich ED. Essential hypertension in the elderly: haemodynamics, intravascular volume, plasma renin activity, and circulating catecholamine levels. Lancet 1983; 2:983–986.
- Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet 2000; 355:865–872.
- Schall P, Wehling M. Treatment of arterial hypertension in the very elderly: a meta-analysis of clinical trials. Arzneimittelforschung 2011; 61:221–228.
- Beckett NS, Peters R, Fletcher AE, et al; HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008; 358:1887–1898.
- Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Soc Hypertens 2011; 5:259–352.
- Wake Forest University, Winston-Salem NC. SPRINT: Systolic Blood Pressure Intervention Trial. http://www.sprinttrial.org/public/dspHome.cfm. Accessed July 24, 2012.
- Sacks FM, Svetkey LP, Vollmer WM, et al; DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001; 344:3–10.
- Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 2002; 136:493–503.
- Bray GA, Vollmer WM, Sacks FM, Obarzanek E, Svetkey LP, Appel LJ; DASH Collaborative Research Group. A further subgroup analysis of the effects of the DASH diet and three dietary sodium levels on blood pressure: results of the DASH-Sodium Trial. Am J Cardiol 2004; 94:222–227.
- Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR. Effects of reduced sodium intake on hypertension control in older individuals: results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE). Arch Intern Med 2001; 161:685–693.
- Frisoli TM, Schmieder RE, Grodzicki T, Messerli FH. Salt and hypertension: is salt dietary reduction worth the effort? Am J Med 2012; 125:433–439.
- National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, MD: National Heart, Lung, and Blood Institute; 2004. http://www.ncbi.nlm.nih.gov/books/NBK9630/Accessed July 30, 2012.
- Mitka M. New guidance covers ways to prevent and treat hypertension in elderly patients. JAMA 2011; 305:2394,2398.
- Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008; 46:72–83.
- Viera AJ, Neutze DM. Diagnosis of secondary hypertension: an age-based approach. Am Fam Physician 2010; 82:1471–1478.
- Rihal CS, Textor SC, Breen JF, et al. Incidental renal artery stenosis among a prospective cohort of hypertensive patients undergoing coronary angiography. Mayo Clin Proc 2002; 77:309–316.
- Wang Y, Li Y. [Clinical and polysomnographic characteristics in elderly patients with obstructive sleep apnea hypopnea syndrome]. [In Chinese] Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2008; 22:222–225.
- Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ 2000; 320:479–482.
- Nieto FJ, Young TB, Lind BK, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 2000; 283:1829–1836.
- Bixler EO, Vgontzas AN, Lin HM, et al. Association of hypertension and sleep-disordered breathing. Arch Intern Med 2000; 160:2289–2295.
- Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, et al. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet 2002; 359:204–210.
- Becker HF, Jerrentrup A, Ploch T, et al. Effect of nasal continuous positive airway pressure treatment on blood pressure in patients with obstructive sleep apnea. Circulation 2003; 107:68–73.
- Dimsdale JE, Loredo JS, Profant J. Effect of continuous positive air-way pressure on blood pressure: a placebo trial. Hypertension 2000; 35:144–147.
- Sharma SK, Agrawal S, Damodaran D, et al. CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med 2011; 365:2277–2286.
- White CJ, Jaff MR, Haskal ZJ, et al; American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Indications for renal arteriography at the time of coronary arteriography: a science advisory from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology, and the Councils on Cardiovascular Radiology and Intervention and on Kidney in Cardiovascular Disease. Circulation 2006; 114:1892–1895.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al; American Association for Vascular Surgery. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol 2006; 47:1239–1312.
- Bax L, Woittiez AJ, Kouwenberg HJ, et al. Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med 2009; 150:840–848,W150–W151.
- ASTRAL Investigators; Wheatley K, Ives N, Gray R, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953–1962.
- Kumbhani DJ, Bavry AA, Harvey JE, et al. Clinical outcomes after percutaneous revascularization versus medical management in patients with significant renal artery stenosis: a meta-analysis of randomized controlled trials. Am Heart J 2011; 161:622.e1–630.e1.
- Pedrinelli R, Dell’Omo G, Melillo E, Mariani M. Amlodipine, enalapril, and dependent leg edema in essential hypertension. Hypertension 2000; 35:621–625.
- van Hamersvelt HW, Kloke HJ, de Jong DJ, Koene RA, Huysmans FT. Oedema formation with the vasodilators nifedipine and diazoxide: direct local effect or sodium retention? J Hypertens 1996; 14:1041–1045.
- Makani H, Bangalore S, Romero J, Wever-Pinzon O, Messerli FH. Effect of renin-angiotensin system blockade on calcium channel blocker-associated peripheral edema. Am J Med 2011; 124:128–135.
- Hoorn EJ, Rivadeneira F, van Meurs JB, et al. Mild hyponatremia as a risk factor for fractures: the Rotterdam Study. J Bone Miner Res 2011; 26:1822–1828.
- Sharabi Y, Illan R, Kamari Y, et al. Diuretic induced hyponatraemia in elderly hypertensive women. J Hum Hypertens 2002; 16:631–635.
- Spital A. Diuretic-induced hyponatremia. Am J Nephrol 1999; 19:447–452.
- Knopman D, Boland LL, Mosley T, et al; Atherosclerosis Risk in Communities (ARIC) Study Investigators. Cardiovascular risk factors and cognitive decline in middle-aged adults. Neurology 2001; 56:42–48.
- Reitz C, Tang MX, Manly J, Mayeux R, Luchsinger JA. Hypertension and the risk of mild cognitive impairment. Arch Neurol 2007; 64:1734–1740.
- Launer LJ, Ross GW, Petrovitch H, et al. Midlife blood pressure and dementia: the Honolulu-Asia aging study. Neurobiol Aging 2000; 21:49–55.
- Forette F, Seux ML, Staessen JA, et al Prevention of dementia in randomised double-blind placebo-controlled Systolic Hypertension in Europe (Syst-Eur) trial. Lancet 1998; 352:1347–1351.
- Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol 2008. www.thelancet.com/journals/laneur/article/PIIS1474-4422(08)70143-1/fulltext. Accessed August 23, 2012.
- Watfa G, Rossignol P, Kearney-Schwartz A, et al. Use of calcium channel blockers is associated with better cognitive performance in older hypertensive patients with subjective memory complaints. J Hypertens 2010; 28:2485–2493.
- Tzourio C, Anderson C, Chapman N, et al; PROGRESS Collaborative Group. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Arch Intern Med 2003; 163:1069–1075.
- Ohrui T, Tomita N, Sato-Nakagawa T, et al. Effects of brain-penetrating ACE inhibitors on Alzheimer disease progression. Neurology 2004; 63:1324–1325.
- Sink KM, Leng X, Williamson J, et al. Angiotensin-converting enzyme inhibitors and cognitive decline in older adults with hypertension: results from the Cardiovascular Health Study. Arch Intern Med 2009; 169:1195–1202.
- Lopez OL, Kuller LH, Fitzpatrick A, Ives D, Becker JT, Beauchamp N. Evaluation of dementia in the cardiovascular health cognition study. Neuroepidemiology 2003; 22:1–12.
- Hemming ML, Selkoe DJ. Amyloid beta-protein is degraded by cellular angiotensin-converting enzyme (ACE) and elevated by an ACE inhibitor. J Biol Chem 2005; 280:37644–37650.
- Nilsson SE, Read S, Berg S, Johansson B, Melander A, Lindblad U. Low systolic blood pressure is associated with impaired cognitive function in the oldest old: longitudinal observations in a population-based sample 80 years and older. Aging Clin Exp Res 2007; 19:41–47.
- Morris MC, Scherr PA, Hebert LE, et al. Association between blood pressure and cognitive function in a biracial community population of older persons. Neuroepidemiology 2002; 21:123–130.
- Joffres MR, Hamet P, Rabkin SW, Gelskey D, Hogan K, Fodor G. Prevalence, control and awareness of high blood pressure among Canadian adults. Canadian Heart Health Surveys Research Group. CMAJ 1992; 146:1997–2005.
- Schillaci G, Pucci G. The importance of instability and visit-to-visit variability of blood pressure. Expert Rev Cardiovasc Ther 2010; 8:1095–1097.
- Mancia G, Facchetti R, Parati G, Zanchetti A. Visit-to-visit blood pressure variability, carotid atherosclerosis, and cardiovascular events in the European Lacidipine Study on Atherosclerosis. Circulation 2012; 126:569–578.
- Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet 2010; 375:906–915.
- Fagard RH, De Cort P. Orthostatic hypotension is a more robust predictor of cardiovascular events than nighttime reverse dipping in elderly. Hypertension 2010; 56:56–61.
- Kearney F, Moore A. Treatment of combined hypertension and orthostatic hypotension in older adults: more questions than answers still remain. Expert Rev Cardiovasc Ther 2009; 7:557–560.
- Messerli FH, Ventura HO, Amodeo C. Osler’s maneuver and pseudohypertension. N Engl J Med 1985; 312:1548–1551.
The management of hypertension has advanced significantly in the last few decades. But the race for more effective means to control this epidemic and its associated complications is far from won. A high percentage of patients in the United States have hypertension that is uncontrolled. Most of these belong to the most rapidly growing demographic group in the United States, ie, the elderly.
It is estimated that more than 70% of medical practice will be directed to geriatric needs in the coming years. It is therefore very important for clinicians to be comfortable with managing hypertension in the elderly.
A GROWING PROBLEM IN AN AGING POPULATION
Between 1980 and 2009, the US population age 65 and older increased from 25.6 million to 39.6 million, of which 42% are men and 58% women.1 This number is expected to reach 75 million by the year 2040. People over 85 years of age are the fastest growing subset of the US population.2 As many as 50% of people who were born recently in countries such as the United States, the United Kingdom, France, Denmark, and Japan will live to celebrate their 100th birthday.3
According to the Framingham Heart Study, by age 60 approximately 60% of the population develops hypertension, and by 70 years about 65% of men and about 75% of women have the disease. In the same study, 90% of those who were normotensive at age 55 went on to develop hypertension. The elderly also are more likely to suffer from the complications of hypertension and are more likely to have uncontrolled disease.
Compared with younger patients with similar blood pressure, elderly hypertensive patients have lower cardiac output, higher peripheral resistance, wider pulse pressure, lower intravascular volume, and lower renal blood flow.4 These age-related pathophysiologic differences must be considered when treating antihypertension in the elderly.
IS TREATING THE ELDERLY BENEFICIAL?
Most elderly hypertensive patients have multiple comorbidities, which tremendously affect the management of their hypertension. They are also more likely than younger patients to have resistant hypertension and to need multiple drugs to control their blood pressure. In the process, these frail patients are exposed to a host of drug-related adverse effects. Thus, it is relevant to question the net benefit of treatment in this age group.
Many studies have indeed shown that treating hypertension reduces the risk of stroke and other adverse cardiovascular events. A decade ago, Staessen et al,5 in a meta-analysis of more than 15,000 patients between ages 62 and 76, showed that treating isolated systolic hypertension substantially reduced morbidity and mortality rates. Moreover, a 2011 meta-analysis of randomized controlled trials in hypertensive patients age 75 and over also concluded that treatment reduced cardiovascular morbidity and mortality rates and the incidence of heart failure, even though the total mortality rate was not affected.6
Opinion on treating the very elderly (≥ 80 years of age) was divided until the results of the Hypertension in the Very Elderly trial (HYVET)7 came out in 2008. This study documented major benefits of treatment in the very elderly age group as well.
The consensus, therefore, is that it is appropriate, even imperative, to treat elderly hypertensive patients (with some cautions—see the sections that follow).
GOAL OF TREATMENT IN THE ELDERLY
Targets for blood pressure management have been based primarily on observational data in middle-aged patients. There is no such thing as an ideal blood pressure that has been derived from randomized controlled trials for any population, let alone the elderly. The generally recommended blood pressure goal of 140/90 mm Hg for elderly hypertensive patients is based on expert opinion.
Moreover, it is unclear if the same target should apply to octogenarians. According to a 2011 American College of Cardiology/American Heart Association (ACC/AHA) expert consensus report,8 an achieved systolic blood pressure of 140 to 145 mm Hg, if tolerated, can be acceptable in this age group.
An orthostatic decline in blood pressure accompanies advanced age and is an inevitable adverse effect of some antihypertensive drugs. Accordingly, systolic blood pressure lower than 130 and diastolic blood pressure lower than 70 mm Hg are best avoided in octogenarians.8 Therefore, when hypertension is complicated by coexisting conditions that require a specific blood pressure goal, it would seem reasonable to not pursue the lower target as aggressively in octogenarians as in elderly patients under age 80.
Having stated the limitations in the quality of data at hand—largely observational—it is relevant to mention the Systolic Blood Pressure Intervention trial (SPRINT).9 This ongoing randomized, multicenter trial, launched by the National Institutes of Health, is assessing whether maintaining blood pressure levels lower than current recommendations further reduces the risk of cardiovascular and kidney diseases or, in the SPRINT-MIND substudy, of age-related cognitive decline, regardless of the type of antihypertensive drug taken. Initially planning to enroll close to 10,000 participants over the age of 55 without specifying any agegroup ranges, the investigators later decided to conduct a substudy called SPRINT Senior that will enroll about 1,750 participants over the age of 75 to determine whether a lower blood pressure range will have the same beneficial effects in older adults.
Given the limitations in the quality and applicability of published data (coming from small, nonrandomized studies with no long-term follow-up), SPRINT is expected to provide the evidence needed to support standard vs aggressive hypertension control among the elderly. The trial is projected to run until late 2018.
MANAGEMENT APPROACH IN THE ELDERLY
Blood pressure should be recorded in both arms before a diagnosis is made. In a number of patients, particularly the elderly, there are significant differences in blood pressure readings between the two arms. The higher reading should be relied on and the corresponding arm used for subsequent measurements.
Lifestyle interventions
Similar to the approach in younger patients with hypertension, lifestyle interventions are the first step to managing high blood pressure in the elderly. The diet and exercise interventions in the Dietary Approaches to Stop Hypertension (DASH) trial have both been shown to lower blood pressure.10,11
Restricting sodium intake has been shown to lower blood pressure more in older adults than in younger adults. In the DASH trial,12 systolic blood pressure decreased by 8.1 mm Hg with sodium restriction in hypertensive patients age 55 to 76 years, compared with 4.8 mm Hg for adults aged 23 to 41 years. In the Trial of Nonpharmacologic Interventions in the Elderly (TONE),13 in people ages 60 to 80 who were randomized to reduce their salt intake, urinary sodium excretion was 40 mmol/day lower and blood pressure was 4.3/2.0 mm Hg lower than in a group that received usual care. Accordingly, reducing salt intake is particularly valuable for blood pressure management in the salt-sensitive elderly.14
Drug therapy
The hypertension pandemic has driven extensive pharmaceutical research, and new drugs continue to be introduced. The major classes of drugs commonly used for treating hypertension are diuretics, calcium channel blockers, and renin-angiotensin system blockers. Each class has specific benefits and adverse-effect profiles.
It is appropriate to start antihypertensive drug therapy with the lowest dose and to monitor for adverse effects, including orthostatic hypotension. The choice of drug should be guided by the patient’s comorbid conditions (Table 1) and the other drugs the patient is taking.15 If the blood pressure response is inadequate, a second drug from a different class should be added. In the same manner, a third drug from a different class should be added if the blood pressure remains outside the optimal range on two drugs.
The average elderly American is on more than six medications.16 Some of these are for high blood pressure, but others interact with antihypertensive drugs (Table 2), and some, including nonsteroidal anti-inflammatory drugs (NSAIDs) and steroids, directly affect blood pressure. Therefore, the drug regimen of an elderly hypertensive patient should be reviewed carefully at every visit. The Screening Tool of Older Person’s Prescriptions (STOPP), a list of 65 rules relating to the most common and most potentially dangerous instances of inappropriate prescribing and overprescribing in the elderly,17 has been found to be a reliable tool in this regard, with a kappa-coefficient of 0.75. Together with the Screening Tool to Alert Doctors to Right [ie, Appropriate, Indicated] Treatment (START),17 which lists 22 evidence-based prescribing indicators for common conditions in the elderly, these criteria provide clinicians with an easy screening tool to combat polypharmacy.
Given the multitude of factors that go into deciding on a specific management strategy in the elderly, it is not possible to discuss individualized care in all patients in the scope of one paper. Below, we present several case scenarios that internists commonly encounter, and suggest ways to approach each.
CASE 1: SECONDARY HYPERTENSION
A 69-year-old obese man who has hypertension of recent onset, long-standing gastroesophageal reflux disease, and benign prostatic hypertrophy comes to your office, accompanied by his wife. He has never had hypertension before. His body mass index is 34 kg/m2. On physical examination, his blood pressure is 180/112 mm Hg.
We start with this case to emphasize the importance of considering causes of secondary hypertension in all patients with the disease (Table 3).18 Further workup should be pursued in those who appear to have “inappropriate” hypertension. This could present as refractory hypertension, abrupt-onset hypertension, hypertension that is first diagnosed before age 20 or after age 60, or loss of control over previously well-controlled blood pressure. Secondary hypertension must always be considered when the history or physical examination suggests a possible cause.
Renal artery stenosis increases in incidence with age. Its prevalence is reported to be as high as 50% in elderly patients with other signs of atherosclerosis such as widespread peripheral artery disease.19
Obstructive sleep apnea also commonly coexists with hypertension and its prevalence also increases with age. In addition, elderly patients with obstructive sleep apnea have a higher incidence of cardiovascular complications, including hypertension, than middle-aged people.20 Numerous studies have found that the severity of obstructive sleep apnea corresponds with the likelihood of systemic hypertension.21–23 Randomized trials and meta-analyses have also concluded that effective treatment with continuous positive airway pressure reduces systemic blood pressure,24–27 although by less than antihypertensive medications do.
A causal relationship between obstructive sleep apnea and hypertension has not been established with certainty. It is recommended, however, that patients with resistant hypertension be screened for obstructive sleep apnea as a possible cause of their disease.
Other causes of secondary hypertension to keep in mind when evaluating patients who have inappropriate hypertension include thyroid disorders, alcohol and tobacco use, and chronic steroid or NSAID use. Pheochromocytoma and adrenal adenoma, though possible, are less prevalent in the elderly.
Case continued
Physical examination in the above patient revealed an epigastric systolic-diastolic bruit, a sign that, although not sensitive, is highly specific for renal artery stenosis, raising the suspicion of this condition. Duplex ultrasonography of the renal arteries confirmed this suspicion. The patient underwent angiography and revascularization, resulting in a distinct fall in, but not normalization of, his blood pressure.
Detecting and treating renal artery stenosis
Though we do not intend to detail the diagnostic approaches and treatments for the various causes of secondary hypertension, we need to briefly mention those for renal artery stenosis.
According to the 2006 ACC/AHA guidelines on peripheral artery disease,28 testing for renal artery stenosis is indicated only if a subsequent corrective procedure is a viable option.
Renal arteriography remains the gold standard for diagnosing renal artery stenosis. However, noninvasive imaging has largely replaced it.
Duplex Doppler ultrasonography, compared with angiography, has a sensitivity of 84% to 98% depending on operator experience, and a specificity of 62% to 99% for detecting renal artery stenosis.29 Some of its limiting factors are the time needed to do the study, its steep learning curve and operator-dependence, and interference with the results by body fat and intestinal gas.
Computed tomographic angiography has a sensitivity of over 90% for detecting renal artery stenosis, and its specificity has been shown to be as high as 99% in certain studies.29 Use of contrast can be a limiting factor in some clinical settings.
Magnetic resonance angiography also offers a sensitivity of 90% to 100% and specificities of 76% to 94% for detecting renal artery stenosis.29 On the other hand, it is costly, and the gadolinium contrast solution used is nephrotoxic, though not as toxic as the contrast used in computed tomographic angiography.
As previously stated, these imaging studies should be used only if corrective measures will be undertaken if clinically significant renal artery stenosis is found. Even in such cases, revascularization may not be curative in all cases. Its effectiveness has been compared with that of medical management alone in a number of studies.30,31 A meta-analysis32 of six key trials involving more than 1,200 patients showed no difference in systolic and diastolic blood pressures and other clinical outcomes, including all-cause mortality, between the two treatment groups over a 29-month follow-up period.
Hence, although we advise that causes of secondary hypertension be considered in cases of inappropriate hypertension, aggressive management must be pursued on a case-by-case basis.
CASE 2: DRUG ADVERSE EFFECTS
A 75-year-old Hispanic woman with a history of treated breast cancer was recently diagnosed with hypertension. Her blood pressure is controlled on amlodipine (Norvasc) 10 mg daily, and her blood pressure today is 128/80 mm Hg. Her only complaint during this office visit is some swelling of her ankles.
Edema and dihydropyridine calcium channel blockers
Like all drugs, antihypertensive medications come with their own set of adverse effects. These are more common as people age—hence the importance of identifying and effectively managing them in the elderly population.
Calcium channel blockers, especially the dihydropyridines—ie, nifedipine (Adalat), amlodipine, felodipine (Plendil), and isradipine (DynaCirc)—are known to cause peripheral vasodilation. Peripheral edema is a common dose-related effect in people on these drugs. In one study, median leg weight increased by 80 g after amlodipine 5 mg was given for 4 weeks, and by another 68 g on a 10-mg dose.33
Ankle swelling, encountered more in women, can be very bothersome. The swelling is related to hyperfiltration of fluid into the interstitial space secondary to intracapillary hypertension. Calcium channel blockers predominantly cause arteriolar dilation by paralyzing the precapillary sphincter, thereby elevating intracapillary pressure.
Traditionally, physicians have lowered the dose of the calcium channel blocker, switched to another drug, or added a diuretic to alleviate the swelling. However, giving a diuretic for edema induced by a calcium channel blocker may not relieve the edema.34
Peripheral edema is much less encountered when a calcium channel blocker is given with an inhibitor of the renin-angiotensin system.35 A meta-analysis concluded that the incidence of peripheral edema was lowered by 38% with such a combination. The same study found angiotensin-converting enzyme (ACE) inhibitors significantly more efficacious for this effect than angiotensin receptor blockers (ARBs).35
ACE inhibitors and ARBs are known to cause venodilation, thereby lowering intra-capillary pressure. It is probable that this effect helps remove the extra fluid sequestered in the capillary bed by the arteriolar dilation from the calcium channel blocker.
Pedal edema associated with use of a calcium channel blocker occurs much more commonly in the elderly than in the young. It is clearly dose-dependent, and the incidence peaks after 6 months of therapy. In the patient described above, adding a low dose of an ACE inhibitor or an ARB (if the patient is ACE inhibitor-intolerant) should relieve the swelling.
Hyponatremia and diuretics
Electrolyte imbalances are another common problem encountered in the elderly. Even though for years attention has been directed to the potassium level, hyponatremia has been equally associated with adverse effects in the elderly, such as an increased risk of fractures as shown in the Rotterdam study.36
In 180 hypertensive inpatients, mean age 76.4, Sharabi et al37 found the incidence of hyponatremia to be three times higher in women than in men (odds ratio 3.10, 95% confidence interval 2.07 to 4.67). Patients were 10 times more likely to be affected after age 65 and 14 times more likely after age 75. Most of the patients affected (74.5%) used a thiazide-type diuretic. Even though in many of the patients diuretics were used for more than 1 year before hyponatremia developed, susceptible patients—such as the frail elderly—can develop severe hyponatremia within days of starting to use a thiazide.38
Severe hyponatremia is potentially life-threatening. Most cases are caused by thiazide rather than loop diuretics.38 Thiazides inhibit electrolyte transport at the cortical diluting sites. As they decrease the glomerular filtration rate acutely, they increase proximal water reabsorption (making the plasma hypotonic), reducing water delivery distally. Loop diuretics, on the other hand, have their main effect at the thick ascending limb, reducing the osmolality at the medullary interstitium and not affecting proximal water reabsorption. Additionally, loop diuretics have a shorter half-life than thiazides, which makes hyponatremia more likely to happen with thiazides.
In patients who develop hyponatremia secondary to diuretic use, appropriate treatment includes stopping the medication, restricting water intake, and repleting electrolyte stores.38 As with any cause of chronic hyponatremia, correction must be cautiously monitored and not hastily done.
Therefore, we advise adding a thiazide diuric with caution in the elderly, and we advise avoiding thiazides in patients with high water or alcohol intake.
CASE 3: DEMENTIA AND HYPERTENSION
A 74-year-old man with long-standing hypertension, gout, and chronic obstructive pulmonary disease was recently diagnosed with Alzheimer dementia. He takes enalapril (Vasotec) 10 mg daily for his blood pressure. His blood pressure is 130/78 mm Hg.
Dementia is one of the most important and common neurologic disorders in the elderly. With the rise in average life expectancy, its magnitude has grown to cause a substantial emotional and economic burden on society and health care.
Midlife hypertension has been demonstrated to be an important modifiable risk factor for late-life cognitive decline,39 mild cognitive impairment,40 and dementia of all causes.41 It has been suggested that hypertension might be part of the pathogenesis of dementia, and targeting high blood pressure might prevent its onset.
Moreover, a significant reduction in both Alzheimer and vascular dementia was demonstrated (risk reduction 55%) with the use of a long-acting dihydropyridine calcium channel blocker (nitrendipine) in the Syst-Eur study.42 However, data from studies such as Systolic Hypertension in the Elderly Program (SHEP) and the HYVET substudy of cognitive function assessement43 showed no difference in dementia between placebo and active therapy with chlorthalidone (Hygroton) (in SHEP) or indapamide (Lozol) (in the HYVET substudy).
Disorders of calcium homeostasis are associated with the brain’s aging process. Probably, the neuroprotective effect of nitrendipine seen in Syst-Eur was due to its ability to affect this process, independent of its blood pressure-lowering effect.
In another prospective study, people over 60 years of age who complained of subjective memory loss showed a significant and positive association between memory scores and the use of calcium channel blockers (+0.14 ± 0.09 in users vs −0.12 ± 0.06 in nonusers; P = .016) independently of age, sex, white matter hyperintensities, and carotid wall cross-sectional area, all of which were associated with worse memory scores.44
Drugs that block the renin-angiotensin system have also been proposed to delay the onset and slow the progression of dementia.45 A small randomized, controlled trial suggested that centrally active ACE inhibitors—those that cross the blood-brain barrier, such as captopril (Capoten), lisinopril (Prinivil), ramipril (Altace), and fosinopril (Monopril)—slow cognitive decline in Alzheimer dementia more than non-centrally active ACE inhibitors or calcium channel blockers.46
Sink et al47 examined data from participants in the Cognition Substudy of the Cardiovascular Health Study48 on the effect of ACE inhibitors on cognitive decline. ACE inhibitors, as a class, showed no benefit in reducing the risk of dementia compared with other antihypertensive drug classes. However, centrally active ACE inhibitors, compared with other medications, were associated with a 65% reduction in cognitive decline per year of drug exposure (P = .01). Non-centrally active ACE inhibitors worsened cognitive decline.
It appears that the brain’s renin-angiotensin system plays a role in the pathogenesis of dementia. Indeed, ACE has been shown to degrade amyloid-beta protein, and its level was increased in brain tissue of Alzheimer patients postmortem.49
The relationship between blood pressure and cognitive function appears to be curvilinear, so that low blood pressure in late life is also associated with dementia and Alzheimer dementia.50 In 5,816 patients age 65 and older, Morris et al51 calculated the percentile scores of four cognitive tests according to the level of blood pressure. Patients with systolic blood pressures of 100 mm Hg, 120 mm Hg, and 180 mm Hg scored lower on the Mini Mental State Examination than those in the 140 to 160 mm Hg range. Patients with diastolic blood pressures between 80 and 90 mm Hg appeared to have the best cognitive function. This further emphasizes that blood pressure control must be pursued in the very elderly, albeit less aggressively. The MIND substudy of the SPRINT trial9 is likely to shed more light on this relationship.
When needed for optimal blood pressure control in a hypertensive patient at risk of dementia, a calcium channel blocker of the dihydropyridine type or a centrally active ACE inhibitor, or both, is preferable.
CASE 4: LABILE HYPERTENSION
A 74-year-old man with hypertension and diabetes mellitus comes to see you in the office. On physical examination, his blood pressure is 175/110 mm Hg. His blood pressure during his last visit 3 months ago was 120/75. He brings a log with him that shows random fluctuations in his blood pressure readings. He takes hydrochlorothiazide 25 mg daily for his blood pressure.
Hypertension in some patients continuously fluctuates between low and high levels. A study in Canada found that up to 15% of all adult hypertensive patients might have labile hypertension.52 In the presence of a normal average blood pressure, visit-to-visit blood pressure variability is usually considered a trivial matter. However, some but not all studies have shown that such visit-to-visit variability in blood pressure is an independent predictor of future cardiovascular events in hypertensive patients, independent of the mean systolic blood pressure.52–54
Blood pressure fluctuates from heartbeat to heartbeat, from morning to night, from winter to summer, and from sitting to standing, and it is prone to increase with exertion, stress, and other factors. But excessive fluctuations in the elderly are most likely the result of excessive stiffness of the arterial tree and a decrease in the windkessel (cushioning) function of the aorta. As a consequence, even small-volume changes in the intravascular system can trigger large blood pressure fluctuations.
There is some evidence that antihypertensive drug classes may differ in their effects on visit-to-visit blood pressure variability. In a 2010 study comparing the effects of different antihypertensive drugs on blood pressure variation, calcium channel blockers and non-loop diuretics were associated with less variation in systolic blood pressure, and calcium channel blockers reduced it the most.55
In the patient described above, switching to a low-dose calcium channel blocker with a thorough follow-up is a reasonable plan.
CASE 5: ORTHOSTATIC HYPOTENSION
A 73-year-old woman with long-standing hypertension complains of some dizziness, especially when getting out of bed in the morning. On physical examination, her blood pressure is 134/100 mm Hg sitting and 115/90 standing. She takes amlodipine 10 mg daily, enalapril 10 mg daily, and chlorthalidone 25 mg daily. Chlorthalidone had been added on her last visit 1 month before.
As a result of the increase in the number of elderly patients with hypertension and guidelines recommending better control in this age group, the number of elderly patients on anti-hypertensive drugs has risen significantly. At the same time, the elderly have increasingly presented with adverse effects of treatment.
Orthostatic hypotension is a drop in systolic pressure of 20 mm Hg or more or a drop in diastolic pressure of 10 mm Hg or more on standing, with or without symptoms. These are caused by cerebral hypoperfusion and include dizziness, lightheadedness, generalized weakness, visual blurring, and, in severe cases, syncope.
Alpha-blockers and nitrates have been most commonly implicated in causing orthostatic hypotension, due to venous pooling. Clearly, not all antihypertensive drugs are equal with regard to their venodilatory effects. Thiazide diuretics, by causing fluid volume depletion, and beta-blockers, by interfering with compensatory cardioacceleration with upright posture, are also commonly involved in causing an excessive blood pressure drop with standing.
Systolic orthostatic hypotension has been shown to be a significant and independent predictor of cardiovascular morbidity and death.56 Moreover, syncope and subsequent falls are an important cause of injury and death in the elderly.57 The clinical combination of hypertension and orthostatic hypotension is, therefore, especially challenging. A compromise between accepting a higher cardiovascular risk at either end of the spectrum with an added higher risk for fall at the lower end has to be made.
To prevent orthostatic hypotension in the elderly, it is important to avoid prescribing high-risk drugs. When starting antihypertensive therapy, a low dose should be used, and the dose should be titrated upward very slowly and cautiously. If orthostatic hypotension is suggested by the history or by the orthostatic test, which is warranted in all elderly hypertensive patients before starting or significantly altering therapy, the potential culprit drug should be withdrawn and the patient reassessed. Improved hydration, elevating the head of the bed, and taking the antihypertensive drug at night are ways to improve symptoms, but these remain largely unproven.
In this patient, the newly added chlorthalidone was stopped, and her symptoms improved.
PSEUDOHYPERTENSION
Since hypertension is defined by a numerical value, it is prudent that this value be accurate. Treating a falsely high reading or leaving a falsely low reading untreated will predispose the elderly patient to increased risk either way. One rare condition in the elderly that can give a falsely high blood pressure reading is pseudohypertension.
Pseudohypertension is a condition in which indirect blood pressure measured by the cuff method overestimates the true intra-arterial blood pressure due to marked underlying arteriosclerosis. The Osler maneuver can be used to differentiate true hypertension from pseudohypertension.58 This is performed by palpating the pulseless radial or brachial artery distal to the inflated cuff. If the artery is palpable despite being pulseless, the patient is said to be “Osler-positive” and likely has pseudohypertension.58
Pseudohypertension should be suspected if the patient has orthostatic hypotension despite normal blood pressure sitting and standing. Also, elevated blood pressure without appropriate target organ disease should raise the suspicion of pseudohypertension. Apart from the Osler maneuver, measuring the intraarterial pressure can confirm this diagnosis.
The management of hypertension has advanced significantly in the last few decades. But the race for more effective means to control this epidemic and its associated complications is far from won. A high percentage of patients in the United States have hypertension that is uncontrolled. Most of these belong to the most rapidly growing demographic group in the United States, ie, the elderly.
It is estimated that more than 70% of medical practice will be directed to geriatric needs in the coming years. It is therefore very important for clinicians to be comfortable with managing hypertension in the elderly.
A GROWING PROBLEM IN AN AGING POPULATION
Between 1980 and 2009, the US population age 65 and older increased from 25.6 million to 39.6 million, of which 42% are men and 58% women.1 This number is expected to reach 75 million by the year 2040. People over 85 years of age are the fastest growing subset of the US population.2 As many as 50% of people who were born recently in countries such as the United States, the United Kingdom, France, Denmark, and Japan will live to celebrate their 100th birthday.3
According to the Framingham Heart Study, by age 60 approximately 60% of the population develops hypertension, and by 70 years about 65% of men and about 75% of women have the disease. In the same study, 90% of those who were normotensive at age 55 went on to develop hypertension. The elderly also are more likely to suffer from the complications of hypertension and are more likely to have uncontrolled disease.
Compared with younger patients with similar blood pressure, elderly hypertensive patients have lower cardiac output, higher peripheral resistance, wider pulse pressure, lower intravascular volume, and lower renal blood flow.4 These age-related pathophysiologic differences must be considered when treating antihypertension in the elderly.
IS TREATING THE ELDERLY BENEFICIAL?
Most elderly hypertensive patients have multiple comorbidities, which tremendously affect the management of their hypertension. They are also more likely than younger patients to have resistant hypertension and to need multiple drugs to control their blood pressure. In the process, these frail patients are exposed to a host of drug-related adverse effects. Thus, it is relevant to question the net benefit of treatment in this age group.
Many studies have indeed shown that treating hypertension reduces the risk of stroke and other adverse cardiovascular events. A decade ago, Staessen et al,5 in a meta-analysis of more than 15,000 patients between ages 62 and 76, showed that treating isolated systolic hypertension substantially reduced morbidity and mortality rates. Moreover, a 2011 meta-analysis of randomized controlled trials in hypertensive patients age 75 and over also concluded that treatment reduced cardiovascular morbidity and mortality rates and the incidence of heart failure, even though the total mortality rate was not affected.6
Opinion on treating the very elderly (≥ 80 years of age) was divided until the results of the Hypertension in the Very Elderly trial (HYVET)7 came out in 2008. This study documented major benefits of treatment in the very elderly age group as well.
The consensus, therefore, is that it is appropriate, even imperative, to treat elderly hypertensive patients (with some cautions—see the sections that follow).
GOAL OF TREATMENT IN THE ELDERLY
Targets for blood pressure management have been based primarily on observational data in middle-aged patients. There is no such thing as an ideal blood pressure that has been derived from randomized controlled trials for any population, let alone the elderly. The generally recommended blood pressure goal of 140/90 mm Hg for elderly hypertensive patients is based on expert opinion.
Moreover, it is unclear if the same target should apply to octogenarians. According to a 2011 American College of Cardiology/American Heart Association (ACC/AHA) expert consensus report,8 an achieved systolic blood pressure of 140 to 145 mm Hg, if tolerated, can be acceptable in this age group.
An orthostatic decline in blood pressure accompanies advanced age and is an inevitable adverse effect of some antihypertensive drugs. Accordingly, systolic blood pressure lower than 130 and diastolic blood pressure lower than 70 mm Hg are best avoided in octogenarians.8 Therefore, when hypertension is complicated by coexisting conditions that require a specific blood pressure goal, it would seem reasonable to not pursue the lower target as aggressively in octogenarians as in elderly patients under age 80.
Having stated the limitations in the quality of data at hand—largely observational—it is relevant to mention the Systolic Blood Pressure Intervention trial (SPRINT).9 This ongoing randomized, multicenter trial, launched by the National Institutes of Health, is assessing whether maintaining blood pressure levels lower than current recommendations further reduces the risk of cardiovascular and kidney diseases or, in the SPRINT-MIND substudy, of age-related cognitive decline, regardless of the type of antihypertensive drug taken. Initially planning to enroll close to 10,000 participants over the age of 55 without specifying any agegroup ranges, the investigators later decided to conduct a substudy called SPRINT Senior that will enroll about 1,750 participants over the age of 75 to determine whether a lower blood pressure range will have the same beneficial effects in older adults.
Given the limitations in the quality and applicability of published data (coming from small, nonrandomized studies with no long-term follow-up), SPRINT is expected to provide the evidence needed to support standard vs aggressive hypertension control among the elderly. The trial is projected to run until late 2018.
MANAGEMENT APPROACH IN THE ELDERLY
Blood pressure should be recorded in both arms before a diagnosis is made. In a number of patients, particularly the elderly, there are significant differences in blood pressure readings between the two arms. The higher reading should be relied on and the corresponding arm used for subsequent measurements.
Lifestyle interventions
Similar to the approach in younger patients with hypertension, lifestyle interventions are the first step to managing high blood pressure in the elderly. The diet and exercise interventions in the Dietary Approaches to Stop Hypertension (DASH) trial have both been shown to lower blood pressure.10,11
Restricting sodium intake has been shown to lower blood pressure more in older adults than in younger adults. In the DASH trial,12 systolic blood pressure decreased by 8.1 mm Hg with sodium restriction in hypertensive patients age 55 to 76 years, compared with 4.8 mm Hg for adults aged 23 to 41 years. In the Trial of Nonpharmacologic Interventions in the Elderly (TONE),13 in people ages 60 to 80 who were randomized to reduce their salt intake, urinary sodium excretion was 40 mmol/day lower and blood pressure was 4.3/2.0 mm Hg lower than in a group that received usual care. Accordingly, reducing salt intake is particularly valuable for blood pressure management in the salt-sensitive elderly.14
Drug therapy
The hypertension pandemic has driven extensive pharmaceutical research, and new drugs continue to be introduced. The major classes of drugs commonly used for treating hypertension are diuretics, calcium channel blockers, and renin-angiotensin system blockers. Each class has specific benefits and adverse-effect profiles.
It is appropriate to start antihypertensive drug therapy with the lowest dose and to monitor for adverse effects, including orthostatic hypotension. The choice of drug should be guided by the patient’s comorbid conditions (Table 1) and the other drugs the patient is taking.15 If the blood pressure response is inadequate, a second drug from a different class should be added. In the same manner, a third drug from a different class should be added if the blood pressure remains outside the optimal range on two drugs.
The average elderly American is on more than six medications.16 Some of these are for high blood pressure, but others interact with antihypertensive drugs (Table 2), and some, including nonsteroidal anti-inflammatory drugs (NSAIDs) and steroids, directly affect blood pressure. Therefore, the drug regimen of an elderly hypertensive patient should be reviewed carefully at every visit. The Screening Tool of Older Person’s Prescriptions (STOPP), a list of 65 rules relating to the most common and most potentially dangerous instances of inappropriate prescribing and overprescribing in the elderly,17 has been found to be a reliable tool in this regard, with a kappa-coefficient of 0.75. Together with the Screening Tool to Alert Doctors to Right [ie, Appropriate, Indicated] Treatment (START),17 which lists 22 evidence-based prescribing indicators for common conditions in the elderly, these criteria provide clinicians with an easy screening tool to combat polypharmacy.
Given the multitude of factors that go into deciding on a specific management strategy in the elderly, it is not possible to discuss individualized care in all patients in the scope of one paper. Below, we present several case scenarios that internists commonly encounter, and suggest ways to approach each.
CASE 1: SECONDARY HYPERTENSION
A 69-year-old obese man who has hypertension of recent onset, long-standing gastroesophageal reflux disease, and benign prostatic hypertrophy comes to your office, accompanied by his wife. He has never had hypertension before. His body mass index is 34 kg/m2. On physical examination, his blood pressure is 180/112 mm Hg.
We start with this case to emphasize the importance of considering causes of secondary hypertension in all patients with the disease (Table 3).18 Further workup should be pursued in those who appear to have “inappropriate” hypertension. This could present as refractory hypertension, abrupt-onset hypertension, hypertension that is first diagnosed before age 20 or after age 60, or loss of control over previously well-controlled blood pressure. Secondary hypertension must always be considered when the history or physical examination suggests a possible cause.
Renal artery stenosis increases in incidence with age. Its prevalence is reported to be as high as 50% in elderly patients with other signs of atherosclerosis such as widespread peripheral artery disease.19
Obstructive sleep apnea also commonly coexists with hypertension and its prevalence also increases with age. In addition, elderly patients with obstructive sleep apnea have a higher incidence of cardiovascular complications, including hypertension, than middle-aged people.20 Numerous studies have found that the severity of obstructive sleep apnea corresponds with the likelihood of systemic hypertension.21–23 Randomized trials and meta-analyses have also concluded that effective treatment with continuous positive airway pressure reduces systemic blood pressure,24–27 although by less than antihypertensive medications do.
A causal relationship between obstructive sleep apnea and hypertension has not been established with certainty. It is recommended, however, that patients with resistant hypertension be screened for obstructive sleep apnea as a possible cause of their disease.
Other causes of secondary hypertension to keep in mind when evaluating patients who have inappropriate hypertension include thyroid disorders, alcohol and tobacco use, and chronic steroid or NSAID use. Pheochromocytoma and adrenal adenoma, though possible, are less prevalent in the elderly.
Case continued
Physical examination in the above patient revealed an epigastric systolic-diastolic bruit, a sign that, although not sensitive, is highly specific for renal artery stenosis, raising the suspicion of this condition. Duplex ultrasonography of the renal arteries confirmed this suspicion. The patient underwent angiography and revascularization, resulting in a distinct fall in, but not normalization of, his blood pressure.
Detecting and treating renal artery stenosis
Though we do not intend to detail the diagnostic approaches and treatments for the various causes of secondary hypertension, we need to briefly mention those for renal artery stenosis.
According to the 2006 ACC/AHA guidelines on peripheral artery disease,28 testing for renal artery stenosis is indicated only if a subsequent corrective procedure is a viable option.
Renal arteriography remains the gold standard for diagnosing renal artery stenosis. However, noninvasive imaging has largely replaced it.
Duplex Doppler ultrasonography, compared with angiography, has a sensitivity of 84% to 98% depending on operator experience, and a specificity of 62% to 99% for detecting renal artery stenosis.29 Some of its limiting factors are the time needed to do the study, its steep learning curve and operator-dependence, and interference with the results by body fat and intestinal gas.
Computed tomographic angiography has a sensitivity of over 90% for detecting renal artery stenosis, and its specificity has been shown to be as high as 99% in certain studies.29 Use of contrast can be a limiting factor in some clinical settings.
Magnetic resonance angiography also offers a sensitivity of 90% to 100% and specificities of 76% to 94% for detecting renal artery stenosis.29 On the other hand, it is costly, and the gadolinium contrast solution used is nephrotoxic, though not as toxic as the contrast used in computed tomographic angiography.
As previously stated, these imaging studies should be used only if corrective measures will be undertaken if clinically significant renal artery stenosis is found. Even in such cases, revascularization may not be curative in all cases. Its effectiveness has been compared with that of medical management alone in a number of studies.30,31 A meta-analysis32 of six key trials involving more than 1,200 patients showed no difference in systolic and diastolic blood pressures and other clinical outcomes, including all-cause mortality, between the two treatment groups over a 29-month follow-up period.
Hence, although we advise that causes of secondary hypertension be considered in cases of inappropriate hypertension, aggressive management must be pursued on a case-by-case basis.
CASE 2: DRUG ADVERSE EFFECTS
A 75-year-old Hispanic woman with a history of treated breast cancer was recently diagnosed with hypertension. Her blood pressure is controlled on amlodipine (Norvasc) 10 mg daily, and her blood pressure today is 128/80 mm Hg. Her only complaint during this office visit is some swelling of her ankles.
Edema and dihydropyridine calcium channel blockers
Like all drugs, antihypertensive medications come with their own set of adverse effects. These are more common as people age—hence the importance of identifying and effectively managing them in the elderly population.
Calcium channel blockers, especially the dihydropyridines—ie, nifedipine (Adalat), amlodipine, felodipine (Plendil), and isradipine (DynaCirc)—are known to cause peripheral vasodilation. Peripheral edema is a common dose-related effect in people on these drugs. In one study, median leg weight increased by 80 g after amlodipine 5 mg was given for 4 weeks, and by another 68 g on a 10-mg dose.33
Ankle swelling, encountered more in women, can be very bothersome. The swelling is related to hyperfiltration of fluid into the interstitial space secondary to intracapillary hypertension. Calcium channel blockers predominantly cause arteriolar dilation by paralyzing the precapillary sphincter, thereby elevating intracapillary pressure.
Traditionally, physicians have lowered the dose of the calcium channel blocker, switched to another drug, or added a diuretic to alleviate the swelling. However, giving a diuretic for edema induced by a calcium channel blocker may not relieve the edema.34
Peripheral edema is much less encountered when a calcium channel blocker is given with an inhibitor of the renin-angiotensin system.35 A meta-analysis concluded that the incidence of peripheral edema was lowered by 38% with such a combination. The same study found angiotensin-converting enzyme (ACE) inhibitors significantly more efficacious for this effect than angiotensin receptor blockers (ARBs).35
ACE inhibitors and ARBs are known to cause venodilation, thereby lowering intra-capillary pressure. It is probable that this effect helps remove the extra fluid sequestered in the capillary bed by the arteriolar dilation from the calcium channel blocker.
Pedal edema associated with use of a calcium channel blocker occurs much more commonly in the elderly than in the young. It is clearly dose-dependent, and the incidence peaks after 6 months of therapy. In the patient described above, adding a low dose of an ACE inhibitor or an ARB (if the patient is ACE inhibitor-intolerant) should relieve the swelling.
Hyponatremia and diuretics
Electrolyte imbalances are another common problem encountered in the elderly. Even though for years attention has been directed to the potassium level, hyponatremia has been equally associated with adverse effects in the elderly, such as an increased risk of fractures as shown in the Rotterdam study.36
In 180 hypertensive inpatients, mean age 76.4, Sharabi et al37 found the incidence of hyponatremia to be three times higher in women than in men (odds ratio 3.10, 95% confidence interval 2.07 to 4.67). Patients were 10 times more likely to be affected after age 65 and 14 times more likely after age 75. Most of the patients affected (74.5%) used a thiazide-type diuretic. Even though in many of the patients diuretics were used for more than 1 year before hyponatremia developed, susceptible patients—such as the frail elderly—can develop severe hyponatremia within days of starting to use a thiazide.38
Severe hyponatremia is potentially life-threatening. Most cases are caused by thiazide rather than loop diuretics.38 Thiazides inhibit electrolyte transport at the cortical diluting sites. As they decrease the glomerular filtration rate acutely, they increase proximal water reabsorption (making the plasma hypotonic), reducing water delivery distally. Loop diuretics, on the other hand, have their main effect at the thick ascending limb, reducing the osmolality at the medullary interstitium and not affecting proximal water reabsorption. Additionally, loop diuretics have a shorter half-life than thiazides, which makes hyponatremia more likely to happen with thiazides.
In patients who develop hyponatremia secondary to diuretic use, appropriate treatment includes stopping the medication, restricting water intake, and repleting electrolyte stores.38 As with any cause of chronic hyponatremia, correction must be cautiously monitored and not hastily done.
Therefore, we advise adding a thiazide diuric with caution in the elderly, and we advise avoiding thiazides in patients with high water or alcohol intake.
CASE 3: DEMENTIA AND HYPERTENSION
A 74-year-old man with long-standing hypertension, gout, and chronic obstructive pulmonary disease was recently diagnosed with Alzheimer dementia. He takes enalapril (Vasotec) 10 mg daily for his blood pressure. His blood pressure is 130/78 mm Hg.
Dementia is one of the most important and common neurologic disorders in the elderly. With the rise in average life expectancy, its magnitude has grown to cause a substantial emotional and economic burden on society and health care.
Midlife hypertension has been demonstrated to be an important modifiable risk factor for late-life cognitive decline,39 mild cognitive impairment,40 and dementia of all causes.41 It has been suggested that hypertension might be part of the pathogenesis of dementia, and targeting high blood pressure might prevent its onset.
Moreover, a significant reduction in both Alzheimer and vascular dementia was demonstrated (risk reduction 55%) with the use of a long-acting dihydropyridine calcium channel blocker (nitrendipine) in the Syst-Eur study.42 However, data from studies such as Systolic Hypertension in the Elderly Program (SHEP) and the HYVET substudy of cognitive function assessement43 showed no difference in dementia between placebo and active therapy with chlorthalidone (Hygroton) (in SHEP) or indapamide (Lozol) (in the HYVET substudy).
Disorders of calcium homeostasis are associated with the brain’s aging process. Probably, the neuroprotective effect of nitrendipine seen in Syst-Eur was due to its ability to affect this process, independent of its blood pressure-lowering effect.
In another prospective study, people over 60 years of age who complained of subjective memory loss showed a significant and positive association between memory scores and the use of calcium channel blockers (+0.14 ± 0.09 in users vs −0.12 ± 0.06 in nonusers; P = .016) independently of age, sex, white matter hyperintensities, and carotid wall cross-sectional area, all of which were associated with worse memory scores.44
Drugs that block the renin-angiotensin system have also been proposed to delay the onset and slow the progression of dementia.45 A small randomized, controlled trial suggested that centrally active ACE inhibitors—those that cross the blood-brain barrier, such as captopril (Capoten), lisinopril (Prinivil), ramipril (Altace), and fosinopril (Monopril)—slow cognitive decline in Alzheimer dementia more than non-centrally active ACE inhibitors or calcium channel blockers.46
Sink et al47 examined data from participants in the Cognition Substudy of the Cardiovascular Health Study48 on the effect of ACE inhibitors on cognitive decline. ACE inhibitors, as a class, showed no benefit in reducing the risk of dementia compared with other antihypertensive drug classes. However, centrally active ACE inhibitors, compared with other medications, were associated with a 65% reduction in cognitive decline per year of drug exposure (P = .01). Non-centrally active ACE inhibitors worsened cognitive decline.
It appears that the brain’s renin-angiotensin system plays a role in the pathogenesis of dementia. Indeed, ACE has been shown to degrade amyloid-beta protein, and its level was increased in brain tissue of Alzheimer patients postmortem.49
The relationship between blood pressure and cognitive function appears to be curvilinear, so that low blood pressure in late life is also associated with dementia and Alzheimer dementia.50 In 5,816 patients age 65 and older, Morris et al51 calculated the percentile scores of four cognitive tests according to the level of blood pressure. Patients with systolic blood pressures of 100 mm Hg, 120 mm Hg, and 180 mm Hg scored lower on the Mini Mental State Examination than those in the 140 to 160 mm Hg range. Patients with diastolic blood pressures between 80 and 90 mm Hg appeared to have the best cognitive function. This further emphasizes that blood pressure control must be pursued in the very elderly, albeit less aggressively. The MIND substudy of the SPRINT trial9 is likely to shed more light on this relationship.
When needed for optimal blood pressure control in a hypertensive patient at risk of dementia, a calcium channel blocker of the dihydropyridine type or a centrally active ACE inhibitor, or both, is preferable.
CASE 4: LABILE HYPERTENSION
A 74-year-old man with hypertension and diabetes mellitus comes to see you in the office. On physical examination, his blood pressure is 175/110 mm Hg. His blood pressure during his last visit 3 months ago was 120/75. He brings a log with him that shows random fluctuations in his blood pressure readings. He takes hydrochlorothiazide 25 mg daily for his blood pressure.
Hypertension in some patients continuously fluctuates between low and high levels. A study in Canada found that up to 15% of all adult hypertensive patients might have labile hypertension.52 In the presence of a normal average blood pressure, visit-to-visit blood pressure variability is usually considered a trivial matter. However, some but not all studies have shown that such visit-to-visit variability in blood pressure is an independent predictor of future cardiovascular events in hypertensive patients, independent of the mean systolic blood pressure.52–54
Blood pressure fluctuates from heartbeat to heartbeat, from morning to night, from winter to summer, and from sitting to standing, and it is prone to increase with exertion, stress, and other factors. But excessive fluctuations in the elderly are most likely the result of excessive stiffness of the arterial tree and a decrease in the windkessel (cushioning) function of the aorta. As a consequence, even small-volume changes in the intravascular system can trigger large blood pressure fluctuations.
There is some evidence that antihypertensive drug classes may differ in their effects on visit-to-visit blood pressure variability. In a 2010 study comparing the effects of different antihypertensive drugs on blood pressure variation, calcium channel blockers and non-loop diuretics were associated with less variation in systolic blood pressure, and calcium channel blockers reduced it the most.55
In the patient described above, switching to a low-dose calcium channel blocker with a thorough follow-up is a reasonable plan.
CASE 5: ORTHOSTATIC HYPOTENSION
A 73-year-old woman with long-standing hypertension complains of some dizziness, especially when getting out of bed in the morning. On physical examination, her blood pressure is 134/100 mm Hg sitting and 115/90 standing. She takes amlodipine 10 mg daily, enalapril 10 mg daily, and chlorthalidone 25 mg daily. Chlorthalidone had been added on her last visit 1 month before.
As a result of the increase in the number of elderly patients with hypertension and guidelines recommending better control in this age group, the number of elderly patients on anti-hypertensive drugs has risen significantly. At the same time, the elderly have increasingly presented with adverse effects of treatment.
Orthostatic hypotension is a drop in systolic pressure of 20 mm Hg or more or a drop in diastolic pressure of 10 mm Hg or more on standing, with or without symptoms. These are caused by cerebral hypoperfusion and include dizziness, lightheadedness, generalized weakness, visual blurring, and, in severe cases, syncope.
Alpha-blockers and nitrates have been most commonly implicated in causing orthostatic hypotension, due to venous pooling. Clearly, not all antihypertensive drugs are equal with regard to their venodilatory effects. Thiazide diuretics, by causing fluid volume depletion, and beta-blockers, by interfering with compensatory cardioacceleration with upright posture, are also commonly involved in causing an excessive blood pressure drop with standing.
Systolic orthostatic hypotension has been shown to be a significant and independent predictor of cardiovascular morbidity and death.56 Moreover, syncope and subsequent falls are an important cause of injury and death in the elderly.57 The clinical combination of hypertension and orthostatic hypotension is, therefore, especially challenging. A compromise between accepting a higher cardiovascular risk at either end of the spectrum with an added higher risk for fall at the lower end has to be made.
To prevent orthostatic hypotension in the elderly, it is important to avoid prescribing high-risk drugs. When starting antihypertensive therapy, a low dose should be used, and the dose should be titrated upward very slowly and cautiously. If orthostatic hypotension is suggested by the history or by the orthostatic test, which is warranted in all elderly hypertensive patients before starting or significantly altering therapy, the potential culprit drug should be withdrawn and the patient reassessed. Improved hydration, elevating the head of the bed, and taking the antihypertensive drug at night are ways to improve symptoms, but these remain largely unproven.
In this patient, the newly added chlorthalidone was stopped, and her symptoms improved.
PSEUDOHYPERTENSION
Since hypertension is defined by a numerical value, it is prudent that this value be accurate. Treating a falsely high reading or leaving a falsely low reading untreated will predispose the elderly patient to increased risk either way. One rare condition in the elderly that can give a falsely high blood pressure reading is pseudohypertension.
Pseudohypertension is a condition in which indirect blood pressure measured by the cuff method overestimates the true intra-arterial blood pressure due to marked underlying arteriosclerosis. The Osler maneuver can be used to differentiate true hypertension from pseudohypertension.58 This is performed by palpating the pulseless radial or brachial artery distal to the inflated cuff. If the artery is palpable despite being pulseless, the patient is said to be “Osler-positive” and likely has pseudohypertension.58
Pseudohypertension should be suspected if the patient has orthostatic hypotension despite normal blood pressure sitting and standing. Also, elevated blood pressure without appropriate target organ disease should raise the suspicion of pseudohypertension. Apart from the Osler maneuver, measuring the intraarterial pressure can confirm this diagnosis.
- US Census Bureau. The 2011 statistical abstract. The national data book. http://www.census.gov/compendia/statab/2011/2011edition.html. Accessed July 24, 2012.
- He W, Sengupta M, Velkoff VA, DeBarros KA. US Census Bureau. Current Population Reports, P23-209. 65+ in the United States: 2005. http://www.census.gov/prod/2006pubs/p23-209.pdf. Accessed July 24, 2012.
- Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet 2009; 374:1196–1208.
- Messerli FH, Sundgaard-Riise K, Ventura HO, Dunn FG, Glade LB, Frohlich ED. Essential hypertension in the elderly: haemodynamics, intravascular volume, plasma renin activity, and circulating catecholamine levels. Lancet 1983; 2:983–986.
- Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet 2000; 355:865–872.
- Schall P, Wehling M. Treatment of arterial hypertension in the very elderly: a meta-analysis of clinical trials. Arzneimittelforschung 2011; 61:221–228.
- Beckett NS, Peters R, Fletcher AE, et al; HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008; 358:1887–1898.
- Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Soc Hypertens 2011; 5:259–352.
- Wake Forest University, Winston-Salem NC. SPRINT: Systolic Blood Pressure Intervention Trial. http://www.sprinttrial.org/public/dspHome.cfm. Accessed July 24, 2012.
- Sacks FM, Svetkey LP, Vollmer WM, et al; DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001; 344:3–10.
- Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 2002; 136:493–503.
- Bray GA, Vollmer WM, Sacks FM, Obarzanek E, Svetkey LP, Appel LJ; DASH Collaborative Research Group. A further subgroup analysis of the effects of the DASH diet and three dietary sodium levels on blood pressure: results of the DASH-Sodium Trial. Am J Cardiol 2004; 94:222–227.
- Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR. Effects of reduced sodium intake on hypertension control in older individuals: results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE). Arch Intern Med 2001; 161:685–693.
- Frisoli TM, Schmieder RE, Grodzicki T, Messerli FH. Salt and hypertension: is salt dietary reduction worth the effort? Am J Med 2012; 125:433–439.
- National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, MD: National Heart, Lung, and Blood Institute; 2004. http://www.ncbi.nlm.nih.gov/books/NBK9630/Accessed July 30, 2012.
- Mitka M. New guidance covers ways to prevent and treat hypertension in elderly patients. JAMA 2011; 305:2394,2398.
- Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008; 46:72–83.
- Viera AJ, Neutze DM. Diagnosis of secondary hypertension: an age-based approach. Am Fam Physician 2010; 82:1471–1478.
- Rihal CS, Textor SC, Breen JF, et al. Incidental renal artery stenosis among a prospective cohort of hypertensive patients undergoing coronary angiography. Mayo Clin Proc 2002; 77:309–316.
- Wang Y, Li Y. [Clinical and polysomnographic characteristics in elderly patients with obstructive sleep apnea hypopnea syndrome]. [In Chinese] Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2008; 22:222–225.
- Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ 2000; 320:479–482.
- Nieto FJ, Young TB, Lind BK, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 2000; 283:1829–1836.
- Bixler EO, Vgontzas AN, Lin HM, et al. Association of hypertension and sleep-disordered breathing. Arch Intern Med 2000; 160:2289–2295.
- Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, et al. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet 2002; 359:204–210.
- Becker HF, Jerrentrup A, Ploch T, et al. Effect of nasal continuous positive airway pressure treatment on blood pressure in patients with obstructive sleep apnea. Circulation 2003; 107:68–73.
- Dimsdale JE, Loredo JS, Profant J. Effect of continuous positive air-way pressure on blood pressure: a placebo trial. Hypertension 2000; 35:144–147.
- Sharma SK, Agrawal S, Damodaran D, et al. CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med 2011; 365:2277–2286.
- White CJ, Jaff MR, Haskal ZJ, et al; American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Indications for renal arteriography at the time of coronary arteriography: a science advisory from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology, and the Councils on Cardiovascular Radiology and Intervention and on Kidney in Cardiovascular Disease. Circulation 2006; 114:1892–1895.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al; American Association for Vascular Surgery. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol 2006; 47:1239–1312.
- Bax L, Woittiez AJ, Kouwenberg HJ, et al. Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med 2009; 150:840–848,W150–W151.
- ASTRAL Investigators; Wheatley K, Ives N, Gray R, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953–1962.
- Kumbhani DJ, Bavry AA, Harvey JE, et al. Clinical outcomes after percutaneous revascularization versus medical management in patients with significant renal artery stenosis: a meta-analysis of randomized controlled trials. Am Heart J 2011; 161:622.e1–630.e1.
- Pedrinelli R, Dell’Omo G, Melillo E, Mariani M. Amlodipine, enalapril, and dependent leg edema in essential hypertension. Hypertension 2000; 35:621–625.
- van Hamersvelt HW, Kloke HJ, de Jong DJ, Koene RA, Huysmans FT. Oedema formation with the vasodilators nifedipine and diazoxide: direct local effect or sodium retention? J Hypertens 1996; 14:1041–1045.
- Makani H, Bangalore S, Romero J, Wever-Pinzon O, Messerli FH. Effect of renin-angiotensin system blockade on calcium channel blocker-associated peripheral edema. Am J Med 2011; 124:128–135.
- Hoorn EJ, Rivadeneira F, van Meurs JB, et al. Mild hyponatremia as a risk factor for fractures: the Rotterdam Study. J Bone Miner Res 2011; 26:1822–1828.
- Sharabi Y, Illan R, Kamari Y, et al. Diuretic induced hyponatraemia in elderly hypertensive women. J Hum Hypertens 2002; 16:631–635.
- Spital A. Diuretic-induced hyponatremia. Am J Nephrol 1999; 19:447–452.
- Knopman D, Boland LL, Mosley T, et al; Atherosclerosis Risk in Communities (ARIC) Study Investigators. Cardiovascular risk factors and cognitive decline in middle-aged adults. Neurology 2001; 56:42–48.
- Reitz C, Tang MX, Manly J, Mayeux R, Luchsinger JA. Hypertension and the risk of mild cognitive impairment. Arch Neurol 2007; 64:1734–1740.
- Launer LJ, Ross GW, Petrovitch H, et al. Midlife blood pressure and dementia: the Honolulu-Asia aging study. Neurobiol Aging 2000; 21:49–55.
- Forette F, Seux ML, Staessen JA, et al Prevention of dementia in randomised double-blind placebo-controlled Systolic Hypertension in Europe (Syst-Eur) trial. Lancet 1998; 352:1347–1351.
- Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol 2008. www.thelancet.com/journals/laneur/article/PIIS1474-4422(08)70143-1/fulltext. Accessed August 23, 2012.
- Watfa G, Rossignol P, Kearney-Schwartz A, et al. Use of calcium channel blockers is associated with better cognitive performance in older hypertensive patients with subjective memory complaints. J Hypertens 2010; 28:2485–2493.
- Tzourio C, Anderson C, Chapman N, et al; PROGRESS Collaborative Group. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Arch Intern Med 2003; 163:1069–1075.
- Ohrui T, Tomita N, Sato-Nakagawa T, et al. Effects of brain-penetrating ACE inhibitors on Alzheimer disease progression. Neurology 2004; 63:1324–1325.
- Sink KM, Leng X, Williamson J, et al. Angiotensin-converting enzyme inhibitors and cognitive decline in older adults with hypertension: results from the Cardiovascular Health Study. Arch Intern Med 2009; 169:1195–1202.
- Lopez OL, Kuller LH, Fitzpatrick A, Ives D, Becker JT, Beauchamp N. Evaluation of dementia in the cardiovascular health cognition study. Neuroepidemiology 2003; 22:1–12.
- Hemming ML, Selkoe DJ. Amyloid beta-protein is degraded by cellular angiotensin-converting enzyme (ACE) and elevated by an ACE inhibitor. J Biol Chem 2005; 280:37644–37650.
- Nilsson SE, Read S, Berg S, Johansson B, Melander A, Lindblad U. Low systolic blood pressure is associated with impaired cognitive function in the oldest old: longitudinal observations in a population-based sample 80 years and older. Aging Clin Exp Res 2007; 19:41–47.
- Morris MC, Scherr PA, Hebert LE, et al. Association between blood pressure and cognitive function in a biracial community population of older persons. Neuroepidemiology 2002; 21:123–130.
- Joffres MR, Hamet P, Rabkin SW, Gelskey D, Hogan K, Fodor G. Prevalence, control and awareness of high blood pressure among Canadian adults. Canadian Heart Health Surveys Research Group. CMAJ 1992; 146:1997–2005.
- Schillaci G, Pucci G. The importance of instability and visit-to-visit variability of blood pressure. Expert Rev Cardiovasc Ther 2010; 8:1095–1097.
- Mancia G, Facchetti R, Parati G, Zanchetti A. Visit-to-visit blood pressure variability, carotid atherosclerosis, and cardiovascular events in the European Lacidipine Study on Atherosclerosis. Circulation 2012; 126:569–578.
- Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet 2010; 375:906–915.
- Fagard RH, De Cort P. Orthostatic hypotension is a more robust predictor of cardiovascular events than nighttime reverse dipping in elderly. Hypertension 2010; 56:56–61.
- Kearney F, Moore A. Treatment of combined hypertension and orthostatic hypotension in older adults: more questions than answers still remain. Expert Rev Cardiovasc Ther 2009; 7:557–560.
- Messerli FH, Ventura HO, Amodeo C. Osler’s maneuver and pseudohypertension. N Engl J Med 1985; 312:1548–1551.
- US Census Bureau. The 2011 statistical abstract. The national data book. http://www.census.gov/compendia/statab/2011/2011edition.html. Accessed July 24, 2012.
- He W, Sengupta M, Velkoff VA, DeBarros KA. US Census Bureau. Current Population Reports, P23-209. 65+ in the United States: 2005. http://www.census.gov/prod/2006pubs/p23-209.pdf. Accessed July 24, 2012.
- Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet 2009; 374:1196–1208.
- Messerli FH, Sundgaard-Riise K, Ventura HO, Dunn FG, Glade LB, Frohlich ED. Essential hypertension in the elderly: haemodynamics, intravascular volume, plasma renin activity, and circulating catecholamine levels. Lancet 1983; 2:983–986.
- Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet 2000; 355:865–872.
- Schall P, Wehling M. Treatment of arterial hypertension in the very elderly: a meta-analysis of clinical trials. Arzneimittelforschung 2011; 61:221–228.
- Beckett NS, Peters R, Fletcher AE, et al; HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008; 358:1887–1898.
- Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Soc Hypertens 2011; 5:259–352.
- Wake Forest University, Winston-Salem NC. SPRINT: Systolic Blood Pressure Intervention Trial. http://www.sprinttrial.org/public/dspHome.cfm. Accessed July 24, 2012.
- Sacks FM, Svetkey LP, Vollmer WM, et al; DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001; 344:3–10.
- Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 2002; 136:493–503.
- Bray GA, Vollmer WM, Sacks FM, Obarzanek E, Svetkey LP, Appel LJ; DASH Collaborative Research Group. A further subgroup analysis of the effects of the DASH diet and three dietary sodium levels on blood pressure: results of the DASH-Sodium Trial. Am J Cardiol 2004; 94:222–227.
- Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR. Effects of reduced sodium intake on hypertension control in older individuals: results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE). Arch Intern Med 2001; 161:685–693.
- Frisoli TM, Schmieder RE, Grodzicki T, Messerli FH. Salt and hypertension: is salt dietary reduction worth the effort? Am J Med 2012; 125:433–439.
- National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, MD: National Heart, Lung, and Blood Institute; 2004. http://www.ncbi.nlm.nih.gov/books/NBK9630/Accessed July 30, 2012.
- Mitka M. New guidance covers ways to prevent and treat hypertension in elderly patients. JAMA 2011; 305:2394,2398.
- Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008; 46:72–83.
- Viera AJ, Neutze DM. Diagnosis of secondary hypertension: an age-based approach. Am Fam Physician 2010; 82:1471–1478.
- Rihal CS, Textor SC, Breen JF, et al. Incidental renal artery stenosis among a prospective cohort of hypertensive patients undergoing coronary angiography. Mayo Clin Proc 2002; 77:309–316.
- Wang Y, Li Y. [Clinical and polysomnographic characteristics in elderly patients with obstructive sleep apnea hypopnea syndrome]. [In Chinese] Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2008; 22:222–225.
- Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ 2000; 320:479–482.
- Nieto FJ, Young TB, Lind BK, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 2000; 283:1829–1836.
- Bixler EO, Vgontzas AN, Lin HM, et al. Association of hypertension and sleep-disordered breathing. Arch Intern Med 2000; 160:2289–2295.
- Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, et al. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet 2002; 359:204–210.
- Becker HF, Jerrentrup A, Ploch T, et al. Effect of nasal continuous positive airway pressure treatment on blood pressure in patients with obstructive sleep apnea. Circulation 2003; 107:68–73.
- Dimsdale JE, Loredo JS, Profant J. Effect of continuous positive air-way pressure on blood pressure: a placebo trial. Hypertension 2000; 35:144–147.
- Sharma SK, Agrawal S, Damodaran D, et al. CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med 2011; 365:2277–2286.
- White CJ, Jaff MR, Haskal ZJ, et al; American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Indications for renal arteriography at the time of coronary arteriography: a science advisory from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology, and the Councils on Cardiovascular Radiology and Intervention and on Kidney in Cardiovascular Disease. Circulation 2006; 114:1892–1895.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al; American Association for Vascular Surgery. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol 2006; 47:1239–1312.
- Bax L, Woittiez AJ, Kouwenberg HJ, et al. Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med 2009; 150:840–848,W150–W151.
- ASTRAL Investigators; Wheatley K, Ives N, Gray R, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953–1962.
- Kumbhani DJ, Bavry AA, Harvey JE, et al. Clinical outcomes after percutaneous revascularization versus medical management in patients with significant renal artery stenosis: a meta-analysis of randomized controlled trials. Am Heart J 2011; 161:622.e1–630.e1.
- Pedrinelli R, Dell’Omo G, Melillo E, Mariani M. Amlodipine, enalapril, and dependent leg edema in essential hypertension. Hypertension 2000; 35:621–625.
- van Hamersvelt HW, Kloke HJ, de Jong DJ, Koene RA, Huysmans FT. Oedema formation with the vasodilators nifedipine and diazoxide: direct local effect or sodium retention? J Hypertens 1996; 14:1041–1045.
- Makani H, Bangalore S, Romero J, Wever-Pinzon O, Messerli FH. Effect of renin-angiotensin system blockade on calcium channel blocker-associated peripheral edema. Am J Med 2011; 124:128–135.
- Hoorn EJ, Rivadeneira F, van Meurs JB, et al. Mild hyponatremia as a risk factor for fractures: the Rotterdam Study. J Bone Miner Res 2011; 26:1822–1828.
- Sharabi Y, Illan R, Kamari Y, et al. Diuretic induced hyponatraemia in elderly hypertensive women. J Hum Hypertens 2002; 16:631–635.
- Spital A. Diuretic-induced hyponatremia. Am J Nephrol 1999; 19:447–452.
- Knopman D, Boland LL, Mosley T, et al; Atherosclerosis Risk in Communities (ARIC) Study Investigators. Cardiovascular risk factors and cognitive decline in middle-aged adults. Neurology 2001; 56:42–48.
- Reitz C, Tang MX, Manly J, Mayeux R, Luchsinger JA. Hypertension and the risk of mild cognitive impairment. Arch Neurol 2007; 64:1734–1740.
- Launer LJ, Ross GW, Petrovitch H, et al. Midlife blood pressure and dementia: the Honolulu-Asia aging study. Neurobiol Aging 2000; 21:49–55.
- Forette F, Seux ML, Staessen JA, et al Prevention of dementia in randomised double-blind placebo-controlled Systolic Hypertension in Europe (Syst-Eur) trial. Lancet 1998; 352:1347–1351.
- Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol 2008. www.thelancet.com/journals/laneur/article/PIIS1474-4422(08)70143-1/fulltext. Accessed August 23, 2012.
- Watfa G, Rossignol P, Kearney-Schwartz A, et al. Use of calcium channel blockers is associated with better cognitive performance in older hypertensive patients with subjective memory complaints. J Hypertens 2010; 28:2485–2493.
- Tzourio C, Anderson C, Chapman N, et al; PROGRESS Collaborative Group. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Arch Intern Med 2003; 163:1069–1075.
- Ohrui T, Tomita N, Sato-Nakagawa T, et al. Effects of brain-penetrating ACE inhibitors on Alzheimer disease progression. Neurology 2004; 63:1324–1325.
- Sink KM, Leng X, Williamson J, et al. Angiotensin-converting enzyme inhibitors and cognitive decline in older adults with hypertension: results from the Cardiovascular Health Study. Arch Intern Med 2009; 169:1195–1202.
- Lopez OL, Kuller LH, Fitzpatrick A, Ives D, Becker JT, Beauchamp N. Evaluation of dementia in the cardiovascular health cognition study. Neuroepidemiology 2003; 22:1–12.
- Hemming ML, Selkoe DJ. Amyloid beta-protein is degraded by cellular angiotensin-converting enzyme (ACE) and elevated by an ACE inhibitor. J Biol Chem 2005; 280:37644–37650.
- Nilsson SE, Read S, Berg S, Johansson B, Melander A, Lindblad U. Low systolic blood pressure is associated with impaired cognitive function in the oldest old: longitudinal observations in a population-based sample 80 years and older. Aging Clin Exp Res 2007; 19:41–47.
- Morris MC, Scherr PA, Hebert LE, et al. Association between blood pressure and cognitive function in a biracial community population of older persons. Neuroepidemiology 2002; 21:123–130.
- Joffres MR, Hamet P, Rabkin SW, Gelskey D, Hogan K, Fodor G. Prevalence, control and awareness of high blood pressure among Canadian adults. Canadian Heart Health Surveys Research Group. CMAJ 1992; 146:1997–2005.
- Schillaci G, Pucci G. The importance of instability and visit-to-visit variability of blood pressure. Expert Rev Cardiovasc Ther 2010; 8:1095–1097.
- Mancia G, Facchetti R, Parati G, Zanchetti A. Visit-to-visit blood pressure variability, carotid atherosclerosis, and cardiovascular events in the European Lacidipine Study on Atherosclerosis. Circulation 2012; 126:569–578.
- Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet 2010; 375:906–915.
- Fagard RH, De Cort P. Orthostatic hypotension is a more robust predictor of cardiovascular events than nighttime reverse dipping in elderly. Hypertension 2010; 56:56–61.
- Kearney F, Moore A. Treatment of combined hypertension and orthostatic hypotension in older adults: more questions than answers still remain. Expert Rev Cardiovasc Ther 2009; 7:557–560.
- Messerli FH, Ventura HO, Amodeo C. Osler’s maneuver and pseudohypertension. N Engl J Med 1985; 312:1548–1551.
KEY POINTS
- Therapy should be considered in all aging hypertensive patients, even the very elderly (> 80 years old).
- Most antihypertensive drugs can be used as first-line treatment in the absence of a compelling indication for a specific class, with the possible exception of alpha-blockers and beta-blockers.
- An initial goal of less than 140/90 mm Hg is reasonable in elderly patients, and an achieved systolic blood pressure of 140 to 145 mm Hg is acceptable in octogenarians.
- Start with low doses; titrate upward slowly; and monitor closely for adverse effects.
- Thiazide diuretics should be used with caution in the elderly because of the risk of hyponatremia.
In reply: Angioedema due to the renin inhibitor aliskiren
In Reply: We agree with Dr. Khan that the duration of ACE inhibitor therapy should never be used to rule out ACE inhibitor-associated angioedema. In an Italian study of 85 cases of angioedema with ACE inhibitor therapy, the mean ACE inhibitor exposure was a full 12 months before angioedema was diagnosed.1 More disturbing was the fact that another 12 months elapsed before the ACE inhibitor actually was discontinued. This would indicate that neither the patient nor the physician related the angioedema to ACE inhibitor therapy. In patients with visceral angioedema, since the diagnosis is unusually challenging, even a further delay can be expected.
Angioedema has been reported with aliskiren, but the 0.04% incidence reported by White et al2 may reflect very simply that physicians are more alert and on the lookout now more than they ever were when ACE inhibitors were first available. Obviously, greater awareness will lead to more frequent diagnosis. As Dr. Khan points out, there is no known mechanism by which aliskiren should cause angioedema, whereas there is fairly solid evidence that ACE inhibitor-associated angioedema is mediated by bradykinin.3,4
- Zingale LC, Beltrami L, Zanichelli A, et al. Angioedema without urticaria: a large clinical survey. CMAJ 2006; 175:1065–1070.
- White WB, Bresalier R, Kaplan AP, et al. Safety and tolerability of the direct renin inhibitor aliskiren: a pooled analysis of clinical experience in more than 12,000 patients with hypertension. J Clin Hypertens (Greenwich) 2010; 12:765–775.
- Molinaro G, Cugno M, Perez M, et al. Angiotensin-converting enzyme inhibitor-associated angioedema is characterized by a slower degradation of des-arginine(9)-bradykinin. J Pharmacol Exp Ther 2002; 303:232–237.
- Cunnion KM Wagner E, Frank MM. Complement and kinin. In: Parlow TG, Stites DP, Imboden JB, editors. Medical Immunology, 10th Ed. New York, NY: Lange Medical Books; 2001:186-888.
In Reply: We agree with Dr. Khan that the duration of ACE inhibitor therapy should never be used to rule out ACE inhibitor-associated angioedema. In an Italian study of 85 cases of angioedema with ACE inhibitor therapy, the mean ACE inhibitor exposure was a full 12 months before angioedema was diagnosed.1 More disturbing was the fact that another 12 months elapsed before the ACE inhibitor actually was discontinued. This would indicate that neither the patient nor the physician related the angioedema to ACE inhibitor therapy. In patients with visceral angioedema, since the diagnosis is unusually challenging, even a further delay can be expected.
Angioedema has been reported with aliskiren, but the 0.04% incidence reported by White et al2 may reflect very simply that physicians are more alert and on the lookout now more than they ever were when ACE inhibitors were first available. Obviously, greater awareness will lead to more frequent diagnosis. As Dr. Khan points out, there is no known mechanism by which aliskiren should cause angioedema, whereas there is fairly solid evidence that ACE inhibitor-associated angioedema is mediated by bradykinin.3,4
In Reply: We agree with Dr. Khan that the duration of ACE inhibitor therapy should never be used to rule out ACE inhibitor-associated angioedema. In an Italian study of 85 cases of angioedema with ACE inhibitor therapy, the mean ACE inhibitor exposure was a full 12 months before angioedema was diagnosed.1 More disturbing was the fact that another 12 months elapsed before the ACE inhibitor actually was discontinued. This would indicate that neither the patient nor the physician related the angioedema to ACE inhibitor therapy. In patients with visceral angioedema, since the diagnosis is unusually challenging, even a further delay can be expected.
Angioedema has been reported with aliskiren, but the 0.04% incidence reported by White et al2 may reflect very simply that physicians are more alert and on the lookout now more than they ever were when ACE inhibitors were first available. Obviously, greater awareness will lead to more frequent diagnosis. As Dr. Khan points out, there is no known mechanism by which aliskiren should cause angioedema, whereas there is fairly solid evidence that ACE inhibitor-associated angioedema is mediated by bradykinin.3,4
- Zingale LC, Beltrami L, Zanichelli A, et al. Angioedema without urticaria: a large clinical survey. CMAJ 2006; 175:1065–1070.
- White WB, Bresalier R, Kaplan AP, et al. Safety and tolerability of the direct renin inhibitor aliskiren: a pooled analysis of clinical experience in more than 12,000 patients with hypertension. J Clin Hypertens (Greenwich) 2010; 12:765–775.
- Molinaro G, Cugno M, Perez M, et al. Angiotensin-converting enzyme inhibitor-associated angioedema is characterized by a slower degradation of des-arginine(9)-bradykinin. J Pharmacol Exp Ther 2002; 303:232–237.
- Cunnion KM Wagner E, Frank MM. Complement and kinin. In: Parlow TG, Stites DP, Imboden JB, editors. Medical Immunology, 10th Ed. New York, NY: Lange Medical Books; 2001:186-888.
- Zingale LC, Beltrami L, Zanichelli A, et al. Angioedema without urticaria: a large clinical survey. CMAJ 2006; 175:1065–1070.
- White WB, Bresalier R, Kaplan AP, et al. Safety and tolerability of the direct renin inhibitor aliskiren: a pooled analysis of clinical experience in more than 12,000 patients with hypertension. J Clin Hypertens (Greenwich) 2010; 12:765–775.
- Molinaro G, Cugno M, Perez M, et al. Angiotensin-converting enzyme inhibitor-associated angioedema is characterized by a slower degradation of des-arginine(9)-bradykinin. J Pharmacol Exp Ther 2002; 303:232–237.
- Cunnion KM Wagner E, Frank MM. Complement and kinin. In: Parlow TG, Stites DP, Imboden JB, editors. Medical Immunology, 10th Ed. New York, NY: Lange Medical Books; 2001:186-888.
Visceral angioedema due to angiotensin-converting enzyme inhibitor therapy
A 57-year-old black woman presented to the emergency department with severe, dull abdominal pain associated with nonbilious vomiting and nausea. She had diabetes mellitus and hypertension, for which she had been taking metformin (Glucophage) 500 mg twice a day and lisinopril (available as Prinivil and Zestril) 20 mg daily for the last 4 years.
Multiple admissions in the past 4 years
The patient started taking lisinopril 10 mg daily in 2005, and she presented to her medical provider 2 weeks later with abdominal discomfort. Colonoscopy was performed, which revealed a benign polyp. She continued taking her medications, including lisinopril.
She continued to occasionally have abdominal pain of variable severity, but it was tolerable until 6 months later, when she presented to the emergency department with severe recurrent abdominal pain.
In view of the clinical picture, her physicians decided to treat her for small bowel obstruction, and an exploratory laparotomy was performed. The surgeons noted that she had moderate ascites, adhesions on the omentum, and a thickened high loop of the small bowel that was unequivocally viable and hyperemic, with thickening of the mesentery. Ascitic fluid was evacuated, adhesions were lysed, and the abdomen was closed. She was discharged with the same medications, including lisinopril; the dose was subsequently increased for better control of her hypertension.
The woman was admitted three more times within the same year for the same symptoms and underwent multiple workups for pancreatitis, gastritis, small-bowel obstruction, and other common gastrointestinal diseases.
Present admission
On review of systems, she denied any dry cough, weight loss or gain, food allergies, new medications, or hematochezia.
On physical examination, she had hypoactive bowel sounds and diffuse tenderness with guarding around the epigastric area.
Laboratory tests did not reveal any abnormalities; in particular, her C1 esterase concentration was normal. Stool studies were negative for infectious diseases.
Plain radiography of the abdomen showed a nonobstructive bowel-gas pattern.
She was diagnosed with gastrointestinal angioedema secondary to angiotensin-converting enzyme (ACE) inhibitor therapy. Her lisinopril was discontinued, and the symptoms resolved completely in 24 hours. On follow-up 8 weeks and 16 months later, her symptoms had not returned.
A RARE COMPLICATION OF ACE-INHIBITOR THERAPY
Angioedema occurs in 0.1% to 0.7% of patients taking ACE inhibitors, and it can affect about 1 of 2,500 patients during the first week of exposure.1–3 It usually manifests as swelling of the face, tongue, and lips, and in rare cases, the gastrointestinal wall. Thus, visceral angioedema is a rare complication of ACE-inhibitor therapy.
Because angioedema is less obvious when it involves abdominal organs, it presents a diagnostic challenge. It is placed lower in the differential diagnosis, as other, more common, and occasionally more high-risk medical conditions are generally considered first. Most of the time, the diagnosis is missed. Some physicians may not be aware of this problem, since only a few case reports have been published. Nevertheless, this potential complication needs to be considered when any patient receiving ACE inhibitors for treatment of hypertension, myocardial infarction, heart failure, or diabetic nephropathy presents with diffuse abdominal pain, diarrhea, or edema of the upper airways.4–8
If a high level of suspicion is applied along with good clinical judgment, then hospitalizations, unnecessary procedures, patient discomfort, and unnecessary health care costs can be prevented.
A MEDLINE SEARCH
To investigate the characteristics associated with this unusual presentation, including the time of symptom onset, the types of symptoms, and the diagnostic studies performed on the patients with visceral angioedema, we performed a MEDLINE search to identify case reports and case series published in English from 1980 to 2010 on the topic of abdominal or visceral angioedema. The search terms used were “visceral,” “intestinal angioedema,” “ACE-inhibitor side effects,” and the names of various ACE inhibitors.
Pertinent articles were identified, and clinical characteristics were collected, including demographics, onset of symptoms, the drug’s name, and others. In our summary below, data are presented as the mean and standard deviation for continuous variables and percentages for categorical variables.
SUMMARY OF REPORTED CASES
Our search revealed 27 reported cases of visceral angioedema associated with ACE inhibitors (a table summarizing our findings is available).9–34 The drug most often involved was lisinopril (11 cases), followed by enalapril (Vasotec) (8 cases).
Twenty-three (82%) of the cases were in women. The mean age of the patients was 49.5 ± 12.2 years (range 29–77 years); the mean age was 46.7 ± 11.7 years in women and 57 ± 13 years in men. Unfortunately, the race and ethnicity of the patients was documented in only some cases.
In 15 (54%) of the cases, the patient presented to a physician or emergency department within 72 hours (41.1 ± 17.4) of starting therapy, and in 8 cases the patient presented between 2 weeks and 18 months.
In 10 cases (including the case we are reporting here), the patients were kept on ACE inhibitors from 2 to 9 years after the initial presentation, as the diagnosis was missed.9,12,14,18,20,31,32 In 2 cases, the dose of the ACE inhibitor had been increased after the patient presented with the abdominal pain.
All of the patients were hospitalized for further diagnostic workup.
As for the presenting symptoms, all the patients had abdominal pain, 24 (86%) had emesis, 14 (50%) had diarrhea, and 20 (71%) had ascites. Laboratory results were mostly nonspecific. Twelve (44%) of the patients had leukocytosis. The C1 esterase inhibitor concentration was measured in 18 patients, and the results were normal in all of them.
Twenty-four (86%) of the patients underwent abdominal and pelvic CT or ultrasonography as part of the initial diagnostic evaluation, and intestinal wall-thickening was found in 21 (87.5%) of them.
Either surgery or gastrointestinal biopsy was performed in 16 (57%) of the patients; the surgical procedures included 2 cholecystectomies and 1 bone marrow biopsy. Only 1 case was diagnosed on the basis of clinical suspicion and abdominal radiographs alone.
The combination of intestinal and stomach angioedema was found in only 2 cases.
Two patients were kept on an ACE inhibitor in spite of symptoms and intestinal wall edema that showed a migratory pattern on imaging after chronic exposure.
The thickening involved the jejunum in 14 patients (50%), the ileum in 8 (29%), the duodenum in 5 (18%), the stomach in 2, and the sigmoid colon in 1.
In 12 cases (43%), visceral angioedema and its symptoms resolved within 48 hours of stopping the ACE inhibitor.
A DIAGNOSIS TO KEEP IN MIND
As we have seen, the diagnosis of visceral angioedema needs to be kept in mind when a patient—especially a middle-aged woman—taking an ACE inhibitor presents with abdominal pain, vomiting, diarrhea, leukocytosis, ascites, and wall-thickening of the small bowel on imaging studies.9,35,36
The diagnosis is hard to establish, and in the interim the patient may undergo invasive and unnecessary procedures, which can be avoided by a heightened awareness of this complication. In all of the reported cases, the patients required hospitalization because of the severity of symptoms and attempts to exclude other possible diseases.36
POSSIBLY DUE TO BRADYKININ
Several theories have been proposed to explain how visceral angioedema is induced by ACE inhibitors. The possible mechanisms that have been described include the following:
- The accumulation of bradykinin and substance P secondary to the effect of the ACE inhibitor, which may lead to the inflammatory response, therefore increasing permeability of the vascular compartment
- Deficiency of complement and the enzymes carboxypeptidase N and alpha-1 antitrypsin
- An antibody-antigen reaction37
- Hormones such as estrogen and progesterone (suggested by the greater number of women represented38)
- Contrast media used for imaging39
- Genetic predisposition
- Inflammation due to acute-phase proteins
- C1-inhibitor deficiency or dysfunction (however, the levels of C1/C4 and the C1-esterase inhibitor functional activity usually are normal2,10,40).
Many other theories are being explored.11,12,38,41–53
The most plausible mechanism is an increase in the levels of bradykinin and its metabolites.45 The absence of ACE can lead to breakdown of bradykinin to des-Arg bradykinin via the minor pathway, which can lead to more pronounced vasodilation and vascular permeability.54,55 During an acute attack of angioedema secondary to ACE inhibition, the bradykinin concentration can increase to more than 10 times the normal level.56
Moreover, C-reactive protein levels were higher (mean 4.42 mg/dL ± 0.15 mg/dL) in patients with ACE-inhibitor-induced angioedema than in those with other causes of angioedema (P < .0001).52 The patients taking ACE inhibitors without any previous angioedema had normal C-reactive protein levels (0.39 mg/dL ± 0.1 mg/dL).52
INCIDENCE RATES
In our review of the literature, all of the patients were taking an ACE inhibitor, and some were taking both an ACE inhibitor and an angiotensin-receptor blocker (ARB).
Initially, the incidence rate of angioedema was thought to be 0.1% to 0.2%, but recently the Omapatrilat Cardiovascular Treatment Assessment vs Enalapril (OCTAVE) trial had more than 12,000 patients on enalapril and reported the incidence of angioedema to be 0.68%,57 with a higher risk in women than in men (0.84% vs 0.54%)58 and a relative risk of 3.03 for blacks compared with whites.59
Even though ARBs seem to be safer, angioedema can recur in up to one-third of patients who switch from an ACE inhibitor to an ARB.60–63
Moreover, one study in the United States found that the frequency of hospital admission of patients with angioedema increased from 8,839 per year in 1998 to 11,925 in 2005, and the cost was estimated to be close to $123 million in 2005.64
Interestingly, when angioedema involved the face, it developed within the first week in 60% of cases,65 whereas when visceral angioedema developed, it did so within the first week in 59% of cases. Therefore, the timing of the onset is similar regardless of the body area involved.
Smokers who developed ACE-inhibitor-induced cough had a higher risk of ACE-inhibitor-induced angioedema in a retrospective cohort study by Morimoto,66 but no relationship to the area of involvement was made.
ON IMAGING, A THICKENED BOWEL WALL
Computed tomography can reveal bowel edema and ascites more reliably than plain radiography or barium studies. Edema thickens the bowel wall, with increased contrast enhancement that makes mesenteric vessels show up on the study. In some instances edema is so significant that edematous submucosa can be differentiated from the serosa due to impressive thickening of the mucosal wall.15,16 Oral contrast can be seen in the middle of the lumen, giving it a target-sign appearance. Edema of the small bowel and ascites can lead to fluid sequestration in the abdomen, resulting in a presentation with shock.67
Magnetic resonance imaging can be even more useful in identifying gastrointestinal angioedema, but it would not be cost-effective, and based on our study, CT and ultrasonography of the abdomen were diagnostic in most cases.
AVOIDING UNNECESSARY TESTING
Hemodynamic instability and abdominal pain usually trigger a surgical consult and a more extensive workup, but with a good clinical approach, unnecessary testing and invasive diagnostic procedures can be avoided under the right circumstances.
Numerous surgical procedures have been reported in patients presenting with visceral angioedema secondary to ACE inhibitors.67 Although a thorough history and physical examination can give us a clue in the diagnosis of drug-induced gastrointestinal angioedema, CT is extremely helpful, as it shows dilated loops, thickened mucosal folds, perihepatic fluid, ascites, mesenteric edema, and a “doughnut” or “stacked coin” appearance.17,68
So far, there have been only two reports of angioedema of the stomach (the case reported by Shahzad et al10 and the current report). Angioedema can affect any visceral organ, but we usually see involvement of the jejunum followed by the ileum and duodenum.40
FINDINGS ON ENDOSCOPY
Usually, endoscopic examination of the upper and lower gastrointestinal tract does not reveal any specific pathology, but endoscopy and biopsy can rule out other causes of abdominal pain, such as Crohn disease, ulcerative colitis, infection, malignancy, granuloma, and vasculitis. Also, hereditary or acquired C1-esterase deficiency and other autoimmune disorders should be considered in the workup.18,69 In the reported cases, endoscopy revealed petechial bleeding with generalized edema.19
Biopsy often demonstrates an expanded edematous submucosal layer with inflammatory cell infiltration and protrusion of the proper muscular layer into the submucosal layer.15 A proper muscular layer and an edematous submucosal layer can produce edema so severe as to obstruct the intestine.15
Ultrasonography or CT provides essential information as to location, structure, and size, and it rules out other diagnoses. Therefore, consideration should be given to noninvasive imaging studies and laboratory testing (C1-esterase inhibitor, complement, antinuclear antibody, complete metabolic panel, complete blood cell count) before resorting to endoscopy or exploratory laparotomy.20,70 In three case reports,29,30,32 abdominal ultrasonography did not show any thickening of the small-bowel wall. Several cases have been diagnosed with the help of endoscopy.
Symptoms usually resolve when the ACE inhibitor is stopped
There is no standard treatment for ACE-inhibitor-induced visceral angioedema. In most patients, stopping the drug, giving nothing by mouth, and giving intravenous fluids to prevent dehydration are sufficient. Symptoms usually resolve within 48 hours.
In several case reports, fresh-frozen plasma was used to increase the levels of kininase II, which can degrade high levels of bradykinin.51,71,72 However, no randomized controlled trial of fresh-frozen plasma for ACE-inhibitor-induced angioedema has been published.
Drugs for hereditary angioedema—eg, recombinant C1-INH, the kallikrein inhibitor ecallantide (Kalbitor), and the BKR-2-antagonist icatibant (Firazyr)73—have not been prospectively studied in gastrointestinal angioedema associated with ACE inhibitors. Icatibant has been shown to be effective in the treatment of hereditary angioedema and could be promising in treating angioedema secondary to ACE inhibitors.8 Rosenberg et al21 described a patient who was on prednisone when she developed intestinal angioedema, thus calling into question the efficacy of steroids in the treatment of visceral angioedema.
RAISING AWARENESS
More than 40 million patients are currently taking ACE inhibitors or ARBs.9 Therefore, we suggest that patients with a known history of angioedema in response to these drugs should wear an identification bracelet to increase awareness and to prevent recurrence of angioedema.
- Brown NJ, Snowden M, Griffin MR. Recurrent angiotensin-converting enzyme inhibitor–associated angioedema. JAMA 1997; 278:232–233.
- Israili ZH, Hall WD. Cough and angioneurotic edema associated with angiotensin-converting enzyme inhibitor therapy. A review of the literature and pathophysiology. Ann Intern Med 1992; 117:234–242.
- Messerli FH, Nussberger J. Vasopeptidase inhibition and angiooedema. Lancet 2000; 356:608–609.
- Jessup M, Brozena S. Heart failure. N Engl J Med 2003; 348:2007–2018.
- Jessup M. The less familiar face of heart failure. J Am Coll Cardiol 2003; 41:224–226.
- Chobanian AV. Clinical practice. Isolated systolic hypertension in the elderly. N Engl J Med 2007; 357:789–796.
- Casas JP, Chua W, Loukogeorgakis S, et al. Effect of inhibitors of the renin-angiotensin system and other antihypertensive drugs on renal outcomes: systematic review and meta-analysis. Lancet 2005; 366:2026–2033.
- Weber MA, Messerli FH. Angiotensin-converting enzyme inhibitors and angioedema: estimating the risk. Hypertension 2008; 51:1465–1467.
- Oudit G, Girgrah N, Allard J. ACE inhibitor-induced angioedema of the intestine: Case report, incidence, pathophysiology, diagnosis and management. Can J Gastroenterol 2001; 15:827–832.
- Shahzad G, Korsten MA, Blatt C, Motwani P. Angiotensin-converting enzyme (ACE) inhibitor-associated angioedema of the stomach and small intestine: a case report. Mt Sinai J Med 2006; 73:1123–1125.
- Chase MP, Fiarman GS, Scholz FJ, MacDermott RP. Angioedema of the small bowel due to an angiotensin-converting enzyme inhibitor. J Clin Gastroenterol 2000; 31:254–257.
- Mullins RJ, Shanahan TM, Dobson RT. Visceral angioedema related to treatment with an ACE inhibitor. Med J Aust 1996; 165:319–321.
- Schmidt TD, McGrath KM. Angiotensin-converting enzyme inhibitor angioedema of the intestine: a case report and review of the literature. Am J Med Sci 2002; 324:106–108.
- Smoger SH, Sayed MA. Simultaneous mucosal and small bowel angioedema due to captopril. South Med J 1998; 91:1060–1063.
- Tojo A, Onozato ML, Fujita T. Repeated subileus due to angioedema during renin-angiotensin system blockade. Am J Med Sci 2006; 332:36–38.
- De Backer AI, De Schepper AM, Vandevenne JE, Schoeters P, Michielsen P, Stevens WJ. CT of angioedema of the small bowel. AJR Am J Roentgenol 2001; 176:649–652.
- Marmery H, Mirvis SE. Angiotensin-converting enzyme inhibitor-induced visceral angioedema. Clin Radiol 2006; 61:979–982.
- Orr KK, Myers JR. Intermittent visceral edema induced by long-term enalapril administration. Ann Pharmacother 2004; 38:825–827.
- Spahn TW, Grosse-Thie W, Mueller MK. Endoscopic visualization of angiotensin-converting enzyme inhibitor-induced small bowel angioedema as a cause of relapsing abdominal pain using double-balloon enteroscopy. Dig Dis Sci 2008; 53:1257–1260.
- Byrne TJ, Douglas DD, Landis ME, Heppell JP. Isolated visceral angioedema: an underdiagnosed complication of ACE inhibitors? Mayo Clin Proc 2000; 75:1201–1204.
- Rosenberg EI, Mishra G, Abdelmalek MF. Angiotensin-converting enzyme inhibitor-induced isolated visceral angioedema in a liver transplant recipient. Transplantation 2003; 75:730–732.
- Salloum H, Locher C, Chenard A, et al. [Small bowel angioedema due to perindopril]. Gastroenterol Clin Biol 2005; 29:1180–1181.
- Arakawa M, Murata Y, Rikimaru Y, Sasaki Y. Drug-induced isolated visceral angioneurotic edema. Intern Med 2005; 44:975–978.
- Abdelmalek MF, Douglas DD. Lisinopril-induced isolated visceral angioedema: review of ACE-inhibitor-induced small bowel angioedema. Dig Dis Sci 1997; 42:847–850.
- Gregory KW, Davis RC. Images in clinical medicine. Angioedema of the intestine. N Engl J Med 1996; 334:1641.
- Farraye FA, Peppercorn MA, Steer ML, Joffe N, Rees M. Acute small-bowel mucosal edema following enalapril use. JAMA 1988; 259:3131.
- Jacobs RL, Hoberman LJ, Goldstein HM. Angioedema of the small bowel caused by an angiotensin-converting enzyme inhibitor. Am J Gastroenterol 1994; 89:127–128.
- Herman L, Jocums SB, Coleman MD. A 29-year-old woman with crampy abdominal pain. Tenn Med 1999; 92:272–273.
- Guy C, Cathébras P, Rousset H. Suspected angioedema of abdominal viscera. Ann Intern Med 1994; 121:900.
- Dupasquier E. [A rare clinical form of angioneurotic edema caused by enalapril: acute abdomen]. Arch Mal Coeur Vaiss 1994; 87:1371–1374.
- Jardine DL, Anderson JC, McClintock AD. Delayed diagnosis of recurrent visceral angio-oedema secondary to ACE inhibitor therapy. Aust N Z J Med 1999; 29:377–378.
- Matsumura M, Haruki K, Kajinami K, Takada T. Angioedema likely related to angiotensin converting enzyme inhibitors. Intern Med 1993; 32:424–426.
- Khan MU, Baig MA, Javed RA, et al. Benazepril induced isolated visceral angioedema: a rare and under diagnosed adverse effect of angiotensin converting enzyme inhibitors. Int J Cardiol 2007; 118:e68–e69.
- Adhikari SP, Schneider JI. An unusual cause of abdominal pain and hypotension: angioedema of the bowel. J Emerg Med 2009; 36:23–25.
- Gibbs CR, Lip GY, Beevers DG. Angioedema due to ACE inhibitors: increased risk in patients of African origin. Br J Clin Pharmacol 1999; 48:861–865.
- Johnsen SP, Jacobsen J, Monster TB, Friis S, McLaughlin JK, Sørensen HT. Risk of first-time hospitalization for angioedema among users of ACE inhibitors and angiotensin receptor antagonists. Am J Med 2005; 118:1428–1329.
- Bi CK, Soltani K, Sloan JB, Weber RR, Elliott WJ, Murphy MB. Tissue-specific autoantibodies induced by captopril. Clin Res 1987; 35:922A.
- Bork K, Dewald G. Hereditary angioedema type III, angioedema associated with angiotensin II receptor antagonists, and female sex. Am J Med 2004; 116:644–645.
- Witten DM, Hirsch FD, Hartman GW. Acute reactions to urographic contrast medium: incidence, clinical characteristics and relationship to history of hypersensitivity states. Am J Roentgenol Radium Ther Nucl Med 1973; 119:832–840.
- Eck SL, Morse JH, Janssen DA, Emerson SG, Markovitz DM. Angioedema presenting as chronic gastrointestinal symptoms. Am J Gastroenterol 1993; 88:436–439.
- Coleman JW, Yeung JH, Roberts DH, Breckenridge AM, Park BK. Drug-specific antibodies in patients receiving captopril. Br J Clin Pharmacol 1986; 22:161–165.
- Kallenberg CG. Autoantibodies during captopril treatment. Arthritis Rheum 1985; 28:597–598.
- Inman WH, Rawson NS, Wilton LV, Pearce GL, Speirs CJ. Postmarketing surveillance of enalapril. I: Results of prescription-event monitoring. BMJ 1988; 297:826–829.
- Lefebvre J, Murphey LJ, Hartert TV, Jiao Shan R, Simmons WH, Brown NJ. Dipeptidyl peptidase IV activity in patients with ACE-inhibitor-associated angioedema. Hypertension 2002; 39:460–464.
- Molinaro G, Cugno M, Perez M, et al. Angiotensin-converting enzyme inhibitor-associated angioedema is characterized by a slower degradation of des-arginine(9)-bradykinin. J Pharmacol Exp Ther 2002; 303:232–237.
- Adam A, Cugno M, Molinaro G, Perez M, Lepage Y, Agostoni A. Aminopeptidase P in individuals with a history of angiooedema on ACE inhibitors. Lancet 2002; 359:2088–2089.
- Binkley KE, Davis A. Clinical, biochemical, and genetic characterization of a novel estrogen-dependent inherited form of angioedema. J Allergy Clin Immunol 2000; 106:546–550.
- Yeung JH, Coleman JW, Park BK. Drug-protein conjugates—IX. Immunogenicity of captopril-protein conjugates. Biochem Pharmacol 1985; 34:4005–4012.
- Abbosh J, Anderson JA, Levine AB, Kupin WL. Angiotensin converting enzyme inhibitor-induced angioedema more prevalent in transplant patients. Ann Allergy Asthma Immunol 1999; 82:473–476.
- Pichler WJ, Lehner R, Späth PJ. Recurrent angioedema associated with hypogonadism or anti-androgen therapy. Ann Allergy 1989; 63:301–305.
- Bass G, Honan D. Octaplas is not equivalent to fresh frozen plasma in the treatment of acute angioedema. Eur J Anaesthesiol 2007; 24:1062–1063.
- Bas M, Hoffmann TK, Bier H, Kojda G. Increased C-reactive protein in ACE-inhibitor-induced angioedema. Br J Clin Pharmacol 2005; 59:233–238.
- Herman AG. Differences in structure of angiotensin-converting enzyme inhibitors might predict differences in action. Am J Cardiol 1992; 70:102C–108C.
- Cunnion KM, Lee JC, Frank MM. Capsule production and growth phase influence binding of complement to Staphylococcus aureus. Infect Immunol 2001; 69:6796–6803.
- Cunnion KM, Wagner E, Frank MM. Complement and kinins. In:Parlow TG, Stites DP, Imboden JB, editors. Medical Immunology. 10th ed. New York, NY: Lange Medical Books; 2001:186–188.
- Pellacani A, Brunner HR, Nussberger J. Plasma kinins increase after angiotensin-converting enzyme inhibition in human subjects. Clin Sci (Lond) 1994; 87:567–574.
- Bristol-Myers Squibb Pharmaceutical Research Institute. FDA Advisory Committee Briefing Book for OMAPATRILAT Tablets NDA 21-188. www.fda.gov/ohrms/dockets/ac/02/briefing/3877B2_01_BristolMeyersSquibb.pdf. Accessed 2/4/2011.
- Kostis JB, Kim HJ, Rusnak J, et al. Incidence and characteristics of angioedema associated with enalapril. Arch Intern Med 2005; 165:1637–1642.
- Mahoney EJ, Devaiah AK. Angioedema and angiotensin-converting enzyme inhibitors: are demographics a risk? Otolaryngol Head Neck Surg 2008; 139:105–108.
- Warner KK, Visconti JA, Tschampel MM. Angiotensin II receptor blockers in patients with ACE inhibitor-induced angioedema. Ann Pharmacother 2000; 34:526–528.
- Kyrmizakis DE, Papadakis CE, Liolios AD, et al. Angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists. Arch Otolaryngol Head Neck Surg 2004; 130:1416–1419.
- MacLean JA, Hannaway PJ. Angioedema and AT1 receptor blockers: proceed with caution. Arch Intern Med 2003; 163:1488–1489,
- Abdi R, Dong VM, Lee CJ, Ntoso KA. Angiotensin II receptor blocker-associated angioedema: on the heels of ACE inhibitor angioedema. Pharmacotherapy 2002; 22:1173–1175.
- Lin RY, Shah SN. Increasing hospitalizations due to angioedema in the United States. Ann Allergy Asthma Immunol 2008; 101:185–192.
- Slater EE, Merrill DD, Guess HA, et al. Clinical profile of angioedema associated with angiotensin converting-enzyme inhibition. JAMA 1988; 260:967–970.
- Morimoto T, Gandhi TK, Fiskio JM, et al. An evaluation of risk factors for adverse drug events associated with angiotensin-converting enzyme inhibitors. J Eval Clin Pract 2004; 10:499–509.
- Cohen N, Sharon A, Golik A, Zaidenstein R, Modai D. Hereditary angioneurotic edema with severe hypovolemic shock. J Clin Gastroenterol 1993; 16:237–239.
- Ciaccia D, Brazer SR, Baker ME. Acquired C1 esterase inhibitor deficiency causing intestinal angioedema: CT appearance. AJR Am J Roentgenol 1993; 161:1215–1216.
- Malcolm A, Prather CM. Intestinal angioedema mimicking Crohn’s disease. Med J Aust 1999; 171:418–420.
- Schmidt TD, McGrath KM. Angiotensin-converting enzyme inhibitor angioedema of the intestine: a case report and review of the literature. Am J Med Sci 2002; 324:106–108.
- Karim MY, Masood A. Fresh-frozen plasma as a treatment for life-threatening ACE-inhibitor angioedema. J Allergy Clin Immunol 2002; 109:370–371.
- Warrier MR, Copilevitz CA, Dykewicz MS, Slavin RG. Fresh frozen plasma in the treatment of resistant angiotensin-converting enzyme inhibitor angioedema. Ann Allergy Asthma Immunol 2004; 92:573–575.
- Bas M, Adams V, Suvorava T, Niehues T, Hoffmann TK, Kojda G. Nonallergic angioedema: role of bradykinin. Allergy 2007; 62:842–856.
- Agostoni A, Cicardi M, Cugno M, Zingale LC, Gioffré D, Nussberger J. Angioedema due to angiotensin-converting enzyme inhibitors. Immunopharmacology 1999; 44:21–25.
A 57-year-old black woman presented to the emergency department with severe, dull abdominal pain associated with nonbilious vomiting and nausea. She had diabetes mellitus and hypertension, for which she had been taking metformin (Glucophage) 500 mg twice a day and lisinopril (available as Prinivil and Zestril) 20 mg daily for the last 4 years.
Multiple admissions in the past 4 years
The patient started taking lisinopril 10 mg daily in 2005, and she presented to her medical provider 2 weeks later with abdominal discomfort. Colonoscopy was performed, which revealed a benign polyp. She continued taking her medications, including lisinopril.
She continued to occasionally have abdominal pain of variable severity, but it was tolerable until 6 months later, when she presented to the emergency department with severe recurrent abdominal pain.
In view of the clinical picture, her physicians decided to treat her for small bowel obstruction, and an exploratory laparotomy was performed. The surgeons noted that she had moderate ascites, adhesions on the omentum, and a thickened high loop of the small bowel that was unequivocally viable and hyperemic, with thickening of the mesentery. Ascitic fluid was evacuated, adhesions were lysed, and the abdomen was closed. She was discharged with the same medications, including lisinopril; the dose was subsequently increased for better control of her hypertension.
The woman was admitted three more times within the same year for the same symptoms and underwent multiple workups for pancreatitis, gastritis, small-bowel obstruction, and other common gastrointestinal diseases.
Present admission
On review of systems, she denied any dry cough, weight loss or gain, food allergies, new medications, or hematochezia.
On physical examination, she had hypoactive bowel sounds and diffuse tenderness with guarding around the epigastric area.
Laboratory tests did not reveal any abnormalities; in particular, her C1 esterase concentration was normal. Stool studies were negative for infectious diseases.
Plain radiography of the abdomen showed a nonobstructive bowel-gas pattern.
She was diagnosed with gastrointestinal angioedema secondary to angiotensin-converting enzyme (ACE) inhibitor therapy. Her lisinopril was discontinued, and the symptoms resolved completely in 24 hours. On follow-up 8 weeks and 16 months later, her symptoms had not returned.
A RARE COMPLICATION OF ACE-INHIBITOR THERAPY
Angioedema occurs in 0.1% to 0.7% of patients taking ACE inhibitors, and it can affect about 1 of 2,500 patients during the first week of exposure.1–3 It usually manifests as swelling of the face, tongue, and lips, and in rare cases, the gastrointestinal wall. Thus, visceral angioedema is a rare complication of ACE-inhibitor therapy.
Because angioedema is less obvious when it involves abdominal organs, it presents a diagnostic challenge. It is placed lower in the differential diagnosis, as other, more common, and occasionally more high-risk medical conditions are generally considered first. Most of the time, the diagnosis is missed. Some physicians may not be aware of this problem, since only a few case reports have been published. Nevertheless, this potential complication needs to be considered when any patient receiving ACE inhibitors for treatment of hypertension, myocardial infarction, heart failure, or diabetic nephropathy presents with diffuse abdominal pain, diarrhea, or edema of the upper airways.4–8
If a high level of suspicion is applied along with good clinical judgment, then hospitalizations, unnecessary procedures, patient discomfort, and unnecessary health care costs can be prevented.
A MEDLINE SEARCH
To investigate the characteristics associated with this unusual presentation, including the time of symptom onset, the types of symptoms, and the diagnostic studies performed on the patients with visceral angioedema, we performed a MEDLINE search to identify case reports and case series published in English from 1980 to 2010 on the topic of abdominal or visceral angioedema. The search terms used were “visceral,” “intestinal angioedema,” “ACE-inhibitor side effects,” and the names of various ACE inhibitors.
Pertinent articles were identified, and clinical characteristics were collected, including demographics, onset of symptoms, the drug’s name, and others. In our summary below, data are presented as the mean and standard deviation for continuous variables and percentages for categorical variables.
SUMMARY OF REPORTED CASES
Our search revealed 27 reported cases of visceral angioedema associated with ACE inhibitors (a table summarizing our findings is available).9–34 The drug most often involved was lisinopril (11 cases), followed by enalapril (Vasotec) (8 cases).
Twenty-three (82%) of the cases were in women. The mean age of the patients was 49.5 ± 12.2 years (range 29–77 years); the mean age was 46.7 ± 11.7 years in women and 57 ± 13 years in men. Unfortunately, the race and ethnicity of the patients was documented in only some cases.
In 15 (54%) of the cases, the patient presented to a physician or emergency department within 72 hours (41.1 ± 17.4) of starting therapy, and in 8 cases the patient presented between 2 weeks and 18 months.
In 10 cases (including the case we are reporting here), the patients were kept on ACE inhibitors from 2 to 9 years after the initial presentation, as the diagnosis was missed.9,12,14,18,20,31,32 In 2 cases, the dose of the ACE inhibitor had been increased after the patient presented with the abdominal pain.
All of the patients were hospitalized for further diagnostic workup.
As for the presenting symptoms, all the patients had abdominal pain, 24 (86%) had emesis, 14 (50%) had diarrhea, and 20 (71%) had ascites. Laboratory results were mostly nonspecific. Twelve (44%) of the patients had leukocytosis. The C1 esterase inhibitor concentration was measured in 18 patients, and the results were normal in all of them.
Twenty-four (86%) of the patients underwent abdominal and pelvic CT or ultrasonography as part of the initial diagnostic evaluation, and intestinal wall-thickening was found in 21 (87.5%) of them.
Either surgery or gastrointestinal biopsy was performed in 16 (57%) of the patients; the surgical procedures included 2 cholecystectomies and 1 bone marrow biopsy. Only 1 case was diagnosed on the basis of clinical suspicion and abdominal radiographs alone.
The combination of intestinal and stomach angioedema was found in only 2 cases.
Two patients were kept on an ACE inhibitor in spite of symptoms and intestinal wall edema that showed a migratory pattern on imaging after chronic exposure.
The thickening involved the jejunum in 14 patients (50%), the ileum in 8 (29%), the duodenum in 5 (18%), the stomach in 2, and the sigmoid colon in 1.
In 12 cases (43%), visceral angioedema and its symptoms resolved within 48 hours of stopping the ACE inhibitor.
A DIAGNOSIS TO KEEP IN MIND
As we have seen, the diagnosis of visceral angioedema needs to be kept in mind when a patient—especially a middle-aged woman—taking an ACE inhibitor presents with abdominal pain, vomiting, diarrhea, leukocytosis, ascites, and wall-thickening of the small bowel on imaging studies.9,35,36
The diagnosis is hard to establish, and in the interim the patient may undergo invasive and unnecessary procedures, which can be avoided by a heightened awareness of this complication. In all of the reported cases, the patients required hospitalization because of the severity of symptoms and attempts to exclude other possible diseases.36
POSSIBLY DUE TO BRADYKININ
Several theories have been proposed to explain how visceral angioedema is induced by ACE inhibitors. The possible mechanisms that have been described include the following:
- The accumulation of bradykinin and substance P secondary to the effect of the ACE inhibitor, which may lead to the inflammatory response, therefore increasing permeability of the vascular compartment
- Deficiency of complement and the enzymes carboxypeptidase N and alpha-1 antitrypsin
- An antibody-antigen reaction37
- Hormones such as estrogen and progesterone (suggested by the greater number of women represented38)
- Contrast media used for imaging39
- Genetic predisposition
- Inflammation due to acute-phase proteins
- C1-inhibitor deficiency or dysfunction (however, the levels of C1/C4 and the C1-esterase inhibitor functional activity usually are normal2,10,40).
Many other theories are being explored.11,12,38,41–53
The most plausible mechanism is an increase in the levels of bradykinin and its metabolites.45 The absence of ACE can lead to breakdown of bradykinin to des-Arg bradykinin via the minor pathway, which can lead to more pronounced vasodilation and vascular permeability.54,55 During an acute attack of angioedema secondary to ACE inhibition, the bradykinin concentration can increase to more than 10 times the normal level.56
Moreover, C-reactive protein levels were higher (mean 4.42 mg/dL ± 0.15 mg/dL) in patients with ACE-inhibitor-induced angioedema than in those with other causes of angioedema (P < .0001).52 The patients taking ACE inhibitors without any previous angioedema had normal C-reactive protein levels (0.39 mg/dL ± 0.1 mg/dL).52
INCIDENCE RATES
In our review of the literature, all of the patients were taking an ACE inhibitor, and some were taking both an ACE inhibitor and an angiotensin-receptor blocker (ARB).
Initially, the incidence rate of angioedema was thought to be 0.1% to 0.2%, but recently the Omapatrilat Cardiovascular Treatment Assessment vs Enalapril (OCTAVE) trial had more than 12,000 patients on enalapril and reported the incidence of angioedema to be 0.68%,57 with a higher risk in women than in men (0.84% vs 0.54%)58 and a relative risk of 3.03 for blacks compared with whites.59
Even though ARBs seem to be safer, angioedema can recur in up to one-third of patients who switch from an ACE inhibitor to an ARB.60–63
Moreover, one study in the United States found that the frequency of hospital admission of patients with angioedema increased from 8,839 per year in 1998 to 11,925 in 2005, and the cost was estimated to be close to $123 million in 2005.64
Interestingly, when angioedema involved the face, it developed within the first week in 60% of cases,65 whereas when visceral angioedema developed, it did so within the first week in 59% of cases. Therefore, the timing of the onset is similar regardless of the body area involved.
Smokers who developed ACE-inhibitor-induced cough had a higher risk of ACE-inhibitor-induced angioedema in a retrospective cohort study by Morimoto,66 but no relationship to the area of involvement was made.
ON IMAGING, A THICKENED BOWEL WALL
Computed tomography can reveal bowel edema and ascites more reliably than plain radiography or barium studies. Edema thickens the bowel wall, with increased contrast enhancement that makes mesenteric vessels show up on the study. In some instances edema is so significant that edematous submucosa can be differentiated from the serosa due to impressive thickening of the mucosal wall.15,16 Oral contrast can be seen in the middle of the lumen, giving it a target-sign appearance. Edema of the small bowel and ascites can lead to fluid sequestration in the abdomen, resulting in a presentation with shock.67
Magnetic resonance imaging can be even more useful in identifying gastrointestinal angioedema, but it would not be cost-effective, and based on our study, CT and ultrasonography of the abdomen were diagnostic in most cases.
AVOIDING UNNECESSARY TESTING
Hemodynamic instability and abdominal pain usually trigger a surgical consult and a more extensive workup, but with a good clinical approach, unnecessary testing and invasive diagnostic procedures can be avoided under the right circumstances.
Numerous surgical procedures have been reported in patients presenting with visceral angioedema secondary to ACE inhibitors.67 Although a thorough history and physical examination can give us a clue in the diagnosis of drug-induced gastrointestinal angioedema, CT is extremely helpful, as it shows dilated loops, thickened mucosal folds, perihepatic fluid, ascites, mesenteric edema, and a “doughnut” or “stacked coin” appearance.17,68
So far, there have been only two reports of angioedema of the stomach (the case reported by Shahzad et al10 and the current report). Angioedema can affect any visceral organ, but we usually see involvement of the jejunum followed by the ileum and duodenum.40
FINDINGS ON ENDOSCOPY
Usually, endoscopic examination of the upper and lower gastrointestinal tract does not reveal any specific pathology, but endoscopy and biopsy can rule out other causes of abdominal pain, such as Crohn disease, ulcerative colitis, infection, malignancy, granuloma, and vasculitis. Also, hereditary or acquired C1-esterase deficiency and other autoimmune disorders should be considered in the workup.18,69 In the reported cases, endoscopy revealed petechial bleeding with generalized edema.19
Biopsy often demonstrates an expanded edematous submucosal layer with inflammatory cell infiltration and protrusion of the proper muscular layer into the submucosal layer.15 A proper muscular layer and an edematous submucosal layer can produce edema so severe as to obstruct the intestine.15
Ultrasonography or CT provides essential information as to location, structure, and size, and it rules out other diagnoses. Therefore, consideration should be given to noninvasive imaging studies and laboratory testing (C1-esterase inhibitor, complement, antinuclear antibody, complete metabolic panel, complete blood cell count) before resorting to endoscopy or exploratory laparotomy.20,70 In three case reports,29,30,32 abdominal ultrasonography did not show any thickening of the small-bowel wall. Several cases have been diagnosed with the help of endoscopy.
Symptoms usually resolve when the ACE inhibitor is stopped
There is no standard treatment for ACE-inhibitor-induced visceral angioedema. In most patients, stopping the drug, giving nothing by mouth, and giving intravenous fluids to prevent dehydration are sufficient. Symptoms usually resolve within 48 hours.
In several case reports, fresh-frozen plasma was used to increase the levels of kininase II, which can degrade high levels of bradykinin.51,71,72 However, no randomized controlled trial of fresh-frozen plasma for ACE-inhibitor-induced angioedema has been published.
Drugs for hereditary angioedema—eg, recombinant C1-INH, the kallikrein inhibitor ecallantide (Kalbitor), and the BKR-2-antagonist icatibant (Firazyr)73—have not been prospectively studied in gastrointestinal angioedema associated with ACE inhibitors. Icatibant has been shown to be effective in the treatment of hereditary angioedema and could be promising in treating angioedema secondary to ACE inhibitors.8 Rosenberg et al21 described a patient who was on prednisone when she developed intestinal angioedema, thus calling into question the efficacy of steroids in the treatment of visceral angioedema.
RAISING AWARENESS
More than 40 million patients are currently taking ACE inhibitors or ARBs.9 Therefore, we suggest that patients with a known history of angioedema in response to these drugs should wear an identification bracelet to increase awareness and to prevent recurrence of angioedema.
A 57-year-old black woman presented to the emergency department with severe, dull abdominal pain associated with nonbilious vomiting and nausea. She had diabetes mellitus and hypertension, for which she had been taking metformin (Glucophage) 500 mg twice a day and lisinopril (available as Prinivil and Zestril) 20 mg daily for the last 4 years.
Multiple admissions in the past 4 years
The patient started taking lisinopril 10 mg daily in 2005, and she presented to her medical provider 2 weeks later with abdominal discomfort. Colonoscopy was performed, which revealed a benign polyp. She continued taking her medications, including lisinopril.
She continued to occasionally have abdominal pain of variable severity, but it was tolerable until 6 months later, when she presented to the emergency department with severe recurrent abdominal pain.
In view of the clinical picture, her physicians decided to treat her for small bowel obstruction, and an exploratory laparotomy was performed. The surgeons noted that she had moderate ascites, adhesions on the omentum, and a thickened high loop of the small bowel that was unequivocally viable and hyperemic, with thickening of the mesentery. Ascitic fluid was evacuated, adhesions were lysed, and the abdomen was closed. She was discharged with the same medications, including lisinopril; the dose was subsequently increased for better control of her hypertension.
The woman was admitted three more times within the same year for the same symptoms and underwent multiple workups for pancreatitis, gastritis, small-bowel obstruction, and other common gastrointestinal diseases.
Present admission
On review of systems, she denied any dry cough, weight loss or gain, food allergies, new medications, or hematochezia.
On physical examination, she had hypoactive bowel sounds and diffuse tenderness with guarding around the epigastric area.
Laboratory tests did not reveal any abnormalities; in particular, her C1 esterase concentration was normal. Stool studies were negative for infectious diseases.
Plain radiography of the abdomen showed a nonobstructive bowel-gas pattern.
She was diagnosed with gastrointestinal angioedema secondary to angiotensin-converting enzyme (ACE) inhibitor therapy. Her lisinopril was discontinued, and the symptoms resolved completely in 24 hours. On follow-up 8 weeks and 16 months later, her symptoms had not returned.
A RARE COMPLICATION OF ACE-INHIBITOR THERAPY
Angioedema occurs in 0.1% to 0.7% of patients taking ACE inhibitors, and it can affect about 1 of 2,500 patients during the first week of exposure.1–3 It usually manifests as swelling of the face, tongue, and lips, and in rare cases, the gastrointestinal wall. Thus, visceral angioedema is a rare complication of ACE-inhibitor therapy.
Because angioedema is less obvious when it involves abdominal organs, it presents a diagnostic challenge. It is placed lower in the differential diagnosis, as other, more common, and occasionally more high-risk medical conditions are generally considered first. Most of the time, the diagnosis is missed. Some physicians may not be aware of this problem, since only a few case reports have been published. Nevertheless, this potential complication needs to be considered when any patient receiving ACE inhibitors for treatment of hypertension, myocardial infarction, heart failure, or diabetic nephropathy presents with diffuse abdominal pain, diarrhea, or edema of the upper airways.4–8
If a high level of suspicion is applied along with good clinical judgment, then hospitalizations, unnecessary procedures, patient discomfort, and unnecessary health care costs can be prevented.
A MEDLINE SEARCH
To investigate the characteristics associated with this unusual presentation, including the time of symptom onset, the types of symptoms, and the diagnostic studies performed on the patients with visceral angioedema, we performed a MEDLINE search to identify case reports and case series published in English from 1980 to 2010 on the topic of abdominal or visceral angioedema. The search terms used were “visceral,” “intestinal angioedema,” “ACE-inhibitor side effects,” and the names of various ACE inhibitors.
Pertinent articles were identified, and clinical characteristics were collected, including demographics, onset of symptoms, the drug’s name, and others. In our summary below, data are presented as the mean and standard deviation for continuous variables and percentages for categorical variables.
SUMMARY OF REPORTED CASES
Our search revealed 27 reported cases of visceral angioedema associated with ACE inhibitors (a table summarizing our findings is available).9–34 The drug most often involved was lisinopril (11 cases), followed by enalapril (Vasotec) (8 cases).
Twenty-three (82%) of the cases were in women. The mean age of the patients was 49.5 ± 12.2 years (range 29–77 years); the mean age was 46.7 ± 11.7 years in women and 57 ± 13 years in men. Unfortunately, the race and ethnicity of the patients was documented in only some cases.
In 15 (54%) of the cases, the patient presented to a physician or emergency department within 72 hours (41.1 ± 17.4) of starting therapy, and in 8 cases the patient presented between 2 weeks and 18 months.
In 10 cases (including the case we are reporting here), the patients were kept on ACE inhibitors from 2 to 9 years after the initial presentation, as the diagnosis was missed.9,12,14,18,20,31,32 In 2 cases, the dose of the ACE inhibitor had been increased after the patient presented with the abdominal pain.
All of the patients were hospitalized for further diagnostic workup.
As for the presenting symptoms, all the patients had abdominal pain, 24 (86%) had emesis, 14 (50%) had diarrhea, and 20 (71%) had ascites. Laboratory results were mostly nonspecific. Twelve (44%) of the patients had leukocytosis. The C1 esterase inhibitor concentration was measured in 18 patients, and the results were normal in all of them.
Twenty-four (86%) of the patients underwent abdominal and pelvic CT or ultrasonography as part of the initial diagnostic evaluation, and intestinal wall-thickening was found in 21 (87.5%) of them.
Either surgery or gastrointestinal biopsy was performed in 16 (57%) of the patients; the surgical procedures included 2 cholecystectomies and 1 bone marrow biopsy. Only 1 case was diagnosed on the basis of clinical suspicion and abdominal radiographs alone.
The combination of intestinal and stomach angioedema was found in only 2 cases.
Two patients were kept on an ACE inhibitor in spite of symptoms and intestinal wall edema that showed a migratory pattern on imaging after chronic exposure.
The thickening involved the jejunum in 14 patients (50%), the ileum in 8 (29%), the duodenum in 5 (18%), the stomach in 2, and the sigmoid colon in 1.
In 12 cases (43%), visceral angioedema and its symptoms resolved within 48 hours of stopping the ACE inhibitor.
A DIAGNOSIS TO KEEP IN MIND
As we have seen, the diagnosis of visceral angioedema needs to be kept in mind when a patient—especially a middle-aged woman—taking an ACE inhibitor presents with abdominal pain, vomiting, diarrhea, leukocytosis, ascites, and wall-thickening of the small bowel on imaging studies.9,35,36
The diagnosis is hard to establish, and in the interim the patient may undergo invasive and unnecessary procedures, which can be avoided by a heightened awareness of this complication. In all of the reported cases, the patients required hospitalization because of the severity of symptoms and attempts to exclude other possible diseases.36
POSSIBLY DUE TO BRADYKININ
Several theories have been proposed to explain how visceral angioedema is induced by ACE inhibitors. The possible mechanisms that have been described include the following:
- The accumulation of bradykinin and substance P secondary to the effect of the ACE inhibitor, which may lead to the inflammatory response, therefore increasing permeability of the vascular compartment
- Deficiency of complement and the enzymes carboxypeptidase N and alpha-1 antitrypsin
- An antibody-antigen reaction37
- Hormones such as estrogen and progesterone (suggested by the greater number of women represented38)
- Contrast media used for imaging39
- Genetic predisposition
- Inflammation due to acute-phase proteins
- C1-inhibitor deficiency or dysfunction (however, the levels of C1/C4 and the C1-esterase inhibitor functional activity usually are normal2,10,40).
Many other theories are being explored.11,12,38,41–53
The most plausible mechanism is an increase in the levels of bradykinin and its metabolites.45 The absence of ACE can lead to breakdown of bradykinin to des-Arg bradykinin via the minor pathway, which can lead to more pronounced vasodilation and vascular permeability.54,55 During an acute attack of angioedema secondary to ACE inhibition, the bradykinin concentration can increase to more than 10 times the normal level.56
Moreover, C-reactive protein levels were higher (mean 4.42 mg/dL ± 0.15 mg/dL) in patients with ACE-inhibitor-induced angioedema than in those with other causes of angioedema (P < .0001).52 The patients taking ACE inhibitors without any previous angioedema had normal C-reactive protein levels (0.39 mg/dL ± 0.1 mg/dL).52
INCIDENCE RATES
In our review of the literature, all of the patients were taking an ACE inhibitor, and some were taking both an ACE inhibitor and an angiotensin-receptor blocker (ARB).
Initially, the incidence rate of angioedema was thought to be 0.1% to 0.2%, but recently the Omapatrilat Cardiovascular Treatment Assessment vs Enalapril (OCTAVE) trial had more than 12,000 patients on enalapril and reported the incidence of angioedema to be 0.68%,57 with a higher risk in women than in men (0.84% vs 0.54%)58 and a relative risk of 3.03 for blacks compared with whites.59
Even though ARBs seem to be safer, angioedema can recur in up to one-third of patients who switch from an ACE inhibitor to an ARB.60–63
Moreover, one study in the United States found that the frequency of hospital admission of patients with angioedema increased from 8,839 per year in 1998 to 11,925 in 2005, and the cost was estimated to be close to $123 million in 2005.64
Interestingly, when angioedema involved the face, it developed within the first week in 60% of cases,65 whereas when visceral angioedema developed, it did so within the first week in 59% of cases. Therefore, the timing of the onset is similar regardless of the body area involved.
Smokers who developed ACE-inhibitor-induced cough had a higher risk of ACE-inhibitor-induced angioedema in a retrospective cohort study by Morimoto,66 but no relationship to the area of involvement was made.
ON IMAGING, A THICKENED BOWEL WALL
Computed tomography can reveal bowel edema and ascites more reliably than plain radiography or barium studies. Edema thickens the bowel wall, with increased contrast enhancement that makes mesenteric vessels show up on the study. In some instances edema is so significant that edematous submucosa can be differentiated from the serosa due to impressive thickening of the mucosal wall.15,16 Oral contrast can be seen in the middle of the lumen, giving it a target-sign appearance. Edema of the small bowel and ascites can lead to fluid sequestration in the abdomen, resulting in a presentation with shock.67
Magnetic resonance imaging can be even more useful in identifying gastrointestinal angioedema, but it would not be cost-effective, and based on our study, CT and ultrasonography of the abdomen were diagnostic in most cases.
AVOIDING UNNECESSARY TESTING
Hemodynamic instability and abdominal pain usually trigger a surgical consult and a more extensive workup, but with a good clinical approach, unnecessary testing and invasive diagnostic procedures can be avoided under the right circumstances.
Numerous surgical procedures have been reported in patients presenting with visceral angioedema secondary to ACE inhibitors.67 Although a thorough history and physical examination can give us a clue in the diagnosis of drug-induced gastrointestinal angioedema, CT is extremely helpful, as it shows dilated loops, thickened mucosal folds, perihepatic fluid, ascites, mesenteric edema, and a “doughnut” or “stacked coin” appearance.17,68
So far, there have been only two reports of angioedema of the stomach (the case reported by Shahzad et al10 and the current report). Angioedema can affect any visceral organ, but we usually see involvement of the jejunum followed by the ileum and duodenum.40
FINDINGS ON ENDOSCOPY
Usually, endoscopic examination of the upper and lower gastrointestinal tract does not reveal any specific pathology, but endoscopy and biopsy can rule out other causes of abdominal pain, such as Crohn disease, ulcerative colitis, infection, malignancy, granuloma, and vasculitis. Also, hereditary or acquired C1-esterase deficiency and other autoimmune disorders should be considered in the workup.18,69 In the reported cases, endoscopy revealed petechial bleeding with generalized edema.19
Biopsy often demonstrates an expanded edematous submucosal layer with inflammatory cell infiltration and protrusion of the proper muscular layer into the submucosal layer.15 A proper muscular layer and an edematous submucosal layer can produce edema so severe as to obstruct the intestine.15
Ultrasonography or CT provides essential information as to location, structure, and size, and it rules out other diagnoses. Therefore, consideration should be given to noninvasive imaging studies and laboratory testing (C1-esterase inhibitor, complement, antinuclear antibody, complete metabolic panel, complete blood cell count) before resorting to endoscopy or exploratory laparotomy.20,70 In three case reports,29,30,32 abdominal ultrasonography did not show any thickening of the small-bowel wall. Several cases have been diagnosed with the help of endoscopy.
Symptoms usually resolve when the ACE inhibitor is stopped
There is no standard treatment for ACE-inhibitor-induced visceral angioedema. In most patients, stopping the drug, giving nothing by mouth, and giving intravenous fluids to prevent dehydration are sufficient. Symptoms usually resolve within 48 hours.
In several case reports, fresh-frozen plasma was used to increase the levels of kininase II, which can degrade high levels of bradykinin.51,71,72 However, no randomized controlled trial of fresh-frozen plasma for ACE-inhibitor-induced angioedema has been published.
Drugs for hereditary angioedema—eg, recombinant C1-INH, the kallikrein inhibitor ecallantide (Kalbitor), and the BKR-2-antagonist icatibant (Firazyr)73—have not been prospectively studied in gastrointestinal angioedema associated with ACE inhibitors. Icatibant has been shown to be effective in the treatment of hereditary angioedema and could be promising in treating angioedema secondary to ACE inhibitors.8 Rosenberg et al21 described a patient who was on prednisone when she developed intestinal angioedema, thus calling into question the efficacy of steroids in the treatment of visceral angioedema.
RAISING AWARENESS
More than 40 million patients are currently taking ACE inhibitors or ARBs.9 Therefore, we suggest that patients with a known history of angioedema in response to these drugs should wear an identification bracelet to increase awareness and to prevent recurrence of angioedema.
- Brown NJ, Snowden M, Griffin MR. Recurrent angiotensin-converting enzyme inhibitor–associated angioedema. JAMA 1997; 278:232–233.
- Israili ZH, Hall WD. Cough and angioneurotic edema associated with angiotensin-converting enzyme inhibitor therapy. A review of the literature and pathophysiology. Ann Intern Med 1992; 117:234–242.
- Messerli FH, Nussberger J. Vasopeptidase inhibition and angiooedema. Lancet 2000; 356:608–609.
- Jessup M, Brozena S. Heart failure. N Engl J Med 2003; 348:2007–2018.
- Jessup M. The less familiar face of heart failure. J Am Coll Cardiol 2003; 41:224–226.
- Chobanian AV. Clinical practice. Isolated systolic hypertension in the elderly. N Engl J Med 2007; 357:789–796.
- Casas JP, Chua W, Loukogeorgakis S, et al. Effect of inhibitors of the renin-angiotensin system and other antihypertensive drugs on renal outcomes: systematic review and meta-analysis. Lancet 2005; 366:2026–2033.
- Weber MA, Messerli FH. Angiotensin-converting enzyme inhibitors and angioedema: estimating the risk. Hypertension 2008; 51:1465–1467.
- Oudit G, Girgrah N, Allard J. ACE inhibitor-induced angioedema of the intestine: Case report, incidence, pathophysiology, diagnosis and management. Can J Gastroenterol 2001; 15:827–832.
- Shahzad G, Korsten MA, Blatt C, Motwani P. Angiotensin-converting enzyme (ACE) inhibitor-associated angioedema of the stomach and small intestine: a case report. Mt Sinai J Med 2006; 73:1123–1125.
- Chase MP, Fiarman GS, Scholz FJ, MacDermott RP. Angioedema of the small bowel due to an angiotensin-converting enzyme inhibitor. J Clin Gastroenterol 2000; 31:254–257.
- Mullins RJ, Shanahan TM, Dobson RT. Visceral angioedema related to treatment with an ACE inhibitor. Med J Aust 1996; 165:319–321.
- Schmidt TD, McGrath KM. Angiotensin-converting enzyme inhibitor angioedema of the intestine: a case report and review of the literature. Am J Med Sci 2002; 324:106–108.
- Smoger SH, Sayed MA. Simultaneous mucosal and small bowel angioedema due to captopril. South Med J 1998; 91:1060–1063.
- Tojo A, Onozato ML, Fujita T. Repeated subileus due to angioedema during renin-angiotensin system blockade. Am J Med Sci 2006; 332:36–38.
- De Backer AI, De Schepper AM, Vandevenne JE, Schoeters P, Michielsen P, Stevens WJ. CT of angioedema of the small bowel. AJR Am J Roentgenol 2001; 176:649–652.
- Marmery H, Mirvis SE. Angiotensin-converting enzyme inhibitor-induced visceral angioedema. Clin Radiol 2006; 61:979–982.
- Orr KK, Myers JR. Intermittent visceral edema induced by long-term enalapril administration. Ann Pharmacother 2004; 38:825–827.
- Spahn TW, Grosse-Thie W, Mueller MK. Endoscopic visualization of angiotensin-converting enzyme inhibitor-induced small bowel angioedema as a cause of relapsing abdominal pain using double-balloon enteroscopy. Dig Dis Sci 2008; 53:1257–1260.
- Byrne TJ, Douglas DD, Landis ME, Heppell JP. Isolated visceral angioedema: an underdiagnosed complication of ACE inhibitors? Mayo Clin Proc 2000; 75:1201–1204.
- Rosenberg EI, Mishra G, Abdelmalek MF. Angiotensin-converting enzyme inhibitor-induced isolated visceral angioedema in a liver transplant recipient. Transplantation 2003; 75:730–732.
- Salloum H, Locher C, Chenard A, et al. [Small bowel angioedema due to perindopril]. Gastroenterol Clin Biol 2005; 29:1180–1181.
- Arakawa M, Murata Y, Rikimaru Y, Sasaki Y. Drug-induced isolated visceral angioneurotic edema. Intern Med 2005; 44:975–978.
- Abdelmalek MF, Douglas DD. Lisinopril-induced isolated visceral angioedema: review of ACE-inhibitor-induced small bowel angioedema. Dig Dis Sci 1997; 42:847–850.
- Gregory KW, Davis RC. Images in clinical medicine. Angioedema of the intestine. N Engl J Med 1996; 334:1641.
- Farraye FA, Peppercorn MA, Steer ML, Joffe N, Rees M. Acute small-bowel mucosal edema following enalapril use. JAMA 1988; 259:3131.
- Jacobs RL, Hoberman LJ, Goldstein HM. Angioedema of the small bowel caused by an angiotensin-converting enzyme inhibitor. Am J Gastroenterol 1994; 89:127–128.
- Herman L, Jocums SB, Coleman MD. A 29-year-old woman with crampy abdominal pain. Tenn Med 1999; 92:272–273.
- Guy C, Cathébras P, Rousset H. Suspected angioedema of abdominal viscera. Ann Intern Med 1994; 121:900.
- Dupasquier E. [A rare clinical form of angioneurotic edema caused by enalapril: acute abdomen]. Arch Mal Coeur Vaiss 1994; 87:1371–1374.
- Jardine DL, Anderson JC, McClintock AD. Delayed diagnosis of recurrent visceral angio-oedema secondary to ACE inhibitor therapy. Aust N Z J Med 1999; 29:377–378.
- Matsumura M, Haruki K, Kajinami K, Takada T. Angioedema likely related to angiotensin converting enzyme inhibitors. Intern Med 1993; 32:424–426.
- Khan MU, Baig MA, Javed RA, et al. Benazepril induced isolated visceral angioedema: a rare and under diagnosed adverse effect of angiotensin converting enzyme inhibitors. Int J Cardiol 2007; 118:e68–e69.
- Adhikari SP, Schneider JI. An unusual cause of abdominal pain and hypotension: angioedema of the bowel. J Emerg Med 2009; 36:23–25.
- Gibbs CR, Lip GY, Beevers DG. Angioedema due to ACE inhibitors: increased risk in patients of African origin. Br J Clin Pharmacol 1999; 48:861–865.
- Johnsen SP, Jacobsen J, Monster TB, Friis S, McLaughlin JK, Sørensen HT. Risk of first-time hospitalization for angioedema among users of ACE inhibitors and angiotensin receptor antagonists. Am J Med 2005; 118:1428–1329.
- Bi CK, Soltani K, Sloan JB, Weber RR, Elliott WJ, Murphy MB. Tissue-specific autoantibodies induced by captopril. Clin Res 1987; 35:922A.
- Bork K, Dewald G. Hereditary angioedema type III, angioedema associated with angiotensin II receptor antagonists, and female sex. Am J Med 2004; 116:644–645.
- Witten DM, Hirsch FD, Hartman GW. Acute reactions to urographic contrast medium: incidence, clinical characteristics and relationship to history of hypersensitivity states. Am J Roentgenol Radium Ther Nucl Med 1973; 119:832–840.
- Eck SL, Morse JH, Janssen DA, Emerson SG, Markovitz DM. Angioedema presenting as chronic gastrointestinal symptoms. Am J Gastroenterol 1993; 88:436–439.
- Coleman JW, Yeung JH, Roberts DH, Breckenridge AM, Park BK. Drug-specific antibodies in patients receiving captopril. Br J Clin Pharmacol 1986; 22:161–165.
- Kallenberg CG. Autoantibodies during captopril treatment. Arthritis Rheum 1985; 28:597–598.
- Inman WH, Rawson NS, Wilton LV, Pearce GL, Speirs CJ. Postmarketing surveillance of enalapril. I: Results of prescription-event monitoring. BMJ 1988; 297:826–829.
- Lefebvre J, Murphey LJ, Hartert TV, Jiao Shan R, Simmons WH, Brown NJ. Dipeptidyl peptidase IV activity in patients with ACE-inhibitor-associated angioedema. Hypertension 2002; 39:460–464.
- Molinaro G, Cugno M, Perez M, et al. Angiotensin-converting enzyme inhibitor-associated angioedema is characterized by a slower degradation of des-arginine(9)-bradykinin. J Pharmacol Exp Ther 2002; 303:232–237.
- Adam A, Cugno M, Molinaro G, Perez M, Lepage Y, Agostoni A. Aminopeptidase P in individuals with a history of angiooedema on ACE inhibitors. Lancet 2002; 359:2088–2089.
- Binkley KE, Davis A. Clinical, biochemical, and genetic characterization of a novel estrogen-dependent inherited form of angioedema. J Allergy Clin Immunol 2000; 106:546–550.
- Yeung JH, Coleman JW, Park BK. Drug-protein conjugates—IX. Immunogenicity of captopril-protein conjugates. Biochem Pharmacol 1985; 34:4005–4012.
- Abbosh J, Anderson JA, Levine AB, Kupin WL. Angiotensin converting enzyme inhibitor-induced angioedema more prevalent in transplant patients. Ann Allergy Asthma Immunol 1999; 82:473–476.
- Pichler WJ, Lehner R, Späth PJ. Recurrent angioedema associated with hypogonadism or anti-androgen therapy. Ann Allergy 1989; 63:301–305.
- Bass G, Honan D. Octaplas is not equivalent to fresh frozen plasma in the treatment of acute angioedema. Eur J Anaesthesiol 2007; 24:1062–1063.
- Bas M, Hoffmann TK, Bier H, Kojda G. Increased C-reactive protein in ACE-inhibitor-induced angioedema. Br J Clin Pharmacol 2005; 59:233–238.
- Herman AG. Differences in structure of angiotensin-converting enzyme inhibitors might predict differences in action. Am J Cardiol 1992; 70:102C–108C.
- Cunnion KM, Lee JC, Frank MM. Capsule production and growth phase influence binding of complement to Staphylococcus aureus. Infect Immunol 2001; 69:6796–6803.
- Cunnion KM, Wagner E, Frank MM. Complement and kinins. In:Parlow TG, Stites DP, Imboden JB, editors. Medical Immunology. 10th ed. New York, NY: Lange Medical Books; 2001:186–188.
- Pellacani A, Brunner HR, Nussberger J. Plasma kinins increase after angiotensin-converting enzyme inhibition in human subjects. Clin Sci (Lond) 1994; 87:567–574.
- Bristol-Myers Squibb Pharmaceutical Research Institute. FDA Advisory Committee Briefing Book for OMAPATRILAT Tablets NDA 21-188. www.fda.gov/ohrms/dockets/ac/02/briefing/3877B2_01_BristolMeyersSquibb.pdf. Accessed 2/4/2011.
- Kostis JB, Kim HJ, Rusnak J, et al. Incidence and characteristics of angioedema associated with enalapril. Arch Intern Med 2005; 165:1637–1642.
- Mahoney EJ, Devaiah AK. Angioedema and angiotensin-converting enzyme inhibitors: are demographics a risk? Otolaryngol Head Neck Surg 2008; 139:105–108.
- Warner KK, Visconti JA, Tschampel MM. Angiotensin II receptor blockers in patients with ACE inhibitor-induced angioedema. Ann Pharmacother 2000; 34:526–528.
- Kyrmizakis DE, Papadakis CE, Liolios AD, et al. Angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists. Arch Otolaryngol Head Neck Surg 2004; 130:1416–1419.
- MacLean JA, Hannaway PJ. Angioedema and AT1 receptor blockers: proceed with caution. Arch Intern Med 2003; 163:1488–1489,
- Abdi R, Dong VM, Lee CJ, Ntoso KA. Angiotensin II receptor blocker-associated angioedema: on the heels of ACE inhibitor angioedema. Pharmacotherapy 2002; 22:1173–1175.
- Lin RY, Shah SN. Increasing hospitalizations due to angioedema in the United States. Ann Allergy Asthma Immunol 2008; 101:185–192.
- Slater EE, Merrill DD, Guess HA, et al. Clinical profile of angioedema associated with angiotensin converting-enzyme inhibition. JAMA 1988; 260:967–970.
- Morimoto T, Gandhi TK, Fiskio JM, et al. An evaluation of risk factors for adverse drug events associated with angiotensin-converting enzyme inhibitors. J Eval Clin Pract 2004; 10:499–509.
- Cohen N, Sharon A, Golik A, Zaidenstein R, Modai D. Hereditary angioneurotic edema with severe hypovolemic shock. J Clin Gastroenterol 1993; 16:237–239.
- Ciaccia D, Brazer SR, Baker ME. Acquired C1 esterase inhibitor deficiency causing intestinal angioedema: CT appearance. AJR Am J Roentgenol 1993; 161:1215–1216.
- Malcolm A, Prather CM. Intestinal angioedema mimicking Crohn’s disease. Med J Aust 1999; 171:418–420.
- Schmidt TD, McGrath KM. Angiotensin-converting enzyme inhibitor angioedema of the intestine: a case report and review of the literature. Am J Med Sci 2002; 324:106–108.
- Karim MY, Masood A. Fresh-frozen plasma as a treatment for life-threatening ACE-inhibitor angioedema. J Allergy Clin Immunol 2002; 109:370–371.
- Warrier MR, Copilevitz CA, Dykewicz MS, Slavin RG. Fresh frozen plasma in the treatment of resistant angiotensin-converting enzyme inhibitor angioedema. Ann Allergy Asthma Immunol 2004; 92:573–575.
- Bas M, Adams V, Suvorava T, Niehues T, Hoffmann TK, Kojda G. Nonallergic angioedema: role of bradykinin. Allergy 2007; 62:842–856.
- Agostoni A, Cicardi M, Cugno M, Zingale LC, Gioffré D, Nussberger J. Angioedema due to angiotensin-converting enzyme inhibitors. Immunopharmacology 1999; 44:21–25.
- Brown NJ, Snowden M, Griffin MR. Recurrent angiotensin-converting enzyme inhibitor–associated angioedema. JAMA 1997; 278:232–233.
- Israili ZH, Hall WD. Cough and angioneurotic edema associated with angiotensin-converting enzyme inhibitor therapy. A review of the literature and pathophysiology. Ann Intern Med 1992; 117:234–242.
- Messerli FH, Nussberger J. Vasopeptidase inhibition and angiooedema. Lancet 2000; 356:608–609.
- Jessup M, Brozena S. Heart failure. N Engl J Med 2003; 348:2007–2018.
- Jessup M. The less familiar face of heart failure. J Am Coll Cardiol 2003; 41:224–226.
- Chobanian AV. Clinical practice. Isolated systolic hypertension in the elderly. N Engl J Med 2007; 357:789–796.
- Casas JP, Chua W, Loukogeorgakis S, et al. Effect of inhibitors of the renin-angiotensin system and other antihypertensive drugs on renal outcomes: systematic review and meta-analysis. Lancet 2005; 366:2026–2033.
- Weber MA, Messerli FH. Angiotensin-converting enzyme inhibitors and angioedema: estimating the risk. Hypertension 2008; 51:1465–1467.
- Oudit G, Girgrah N, Allard J. ACE inhibitor-induced angioedema of the intestine: Case report, incidence, pathophysiology, diagnosis and management. Can J Gastroenterol 2001; 15:827–832.
- Shahzad G, Korsten MA, Blatt C, Motwani P. Angiotensin-converting enzyme (ACE) inhibitor-associated angioedema of the stomach and small intestine: a case report. Mt Sinai J Med 2006; 73:1123–1125.
- Chase MP, Fiarman GS, Scholz FJ, MacDermott RP. Angioedema of the small bowel due to an angiotensin-converting enzyme inhibitor. J Clin Gastroenterol 2000; 31:254–257.
- Mullins RJ, Shanahan TM, Dobson RT. Visceral angioedema related to treatment with an ACE inhibitor. Med J Aust 1996; 165:319–321.
- Schmidt TD, McGrath KM. Angiotensin-converting enzyme inhibitor angioedema of the intestine: a case report and review of the literature. Am J Med Sci 2002; 324:106–108.
- Smoger SH, Sayed MA. Simultaneous mucosal and small bowel angioedema due to captopril. South Med J 1998; 91:1060–1063.
- Tojo A, Onozato ML, Fujita T. Repeated subileus due to angioedema during renin-angiotensin system blockade. Am J Med Sci 2006; 332:36–38.
- De Backer AI, De Schepper AM, Vandevenne JE, Schoeters P, Michielsen P, Stevens WJ. CT of angioedema of the small bowel. AJR Am J Roentgenol 2001; 176:649–652.
- Marmery H, Mirvis SE. Angiotensin-converting enzyme inhibitor-induced visceral angioedema. Clin Radiol 2006; 61:979–982.
- Orr KK, Myers JR. Intermittent visceral edema induced by long-term enalapril administration. Ann Pharmacother 2004; 38:825–827.
- Spahn TW, Grosse-Thie W, Mueller MK. Endoscopic visualization of angiotensin-converting enzyme inhibitor-induced small bowel angioedema as a cause of relapsing abdominal pain using double-balloon enteroscopy. Dig Dis Sci 2008; 53:1257–1260.
- Byrne TJ, Douglas DD, Landis ME, Heppell JP. Isolated visceral angioedema: an underdiagnosed complication of ACE inhibitors? Mayo Clin Proc 2000; 75:1201–1204.
- Rosenberg EI, Mishra G, Abdelmalek MF. Angiotensin-converting enzyme inhibitor-induced isolated visceral angioedema in a liver transplant recipient. Transplantation 2003; 75:730–732.
- Salloum H, Locher C, Chenard A, et al. [Small bowel angioedema due to perindopril]. Gastroenterol Clin Biol 2005; 29:1180–1181.
- Arakawa M, Murata Y, Rikimaru Y, Sasaki Y. Drug-induced isolated visceral angioneurotic edema. Intern Med 2005; 44:975–978.
- Abdelmalek MF, Douglas DD. Lisinopril-induced isolated visceral angioedema: review of ACE-inhibitor-induced small bowel angioedema. Dig Dis Sci 1997; 42:847–850.
- Gregory KW, Davis RC. Images in clinical medicine. Angioedema of the intestine. N Engl J Med 1996; 334:1641.
- Farraye FA, Peppercorn MA, Steer ML, Joffe N, Rees M. Acute small-bowel mucosal edema following enalapril use. JAMA 1988; 259:3131.
- Jacobs RL, Hoberman LJ, Goldstein HM. Angioedema of the small bowel caused by an angiotensin-converting enzyme inhibitor. Am J Gastroenterol 1994; 89:127–128.
- Herman L, Jocums SB, Coleman MD. A 29-year-old woman with crampy abdominal pain. Tenn Med 1999; 92:272–273.
- Guy C, Cathébras P, Rousset H. Suspected angioedema of abdominal viscera. Ann Intern Med 1994; 121:900.
- Dupasquier E. [A rare clinical form of angioneurotic edema caused by enalapril: acute abdomen]. Arch Mal Coeur Vaiss 1994; 87:1371–1374.
- Jardine DL, Anderson JC, McClintock AD. Delayed diagnosis of recurrent visceral angio-oedema secondary to ACE inhibitor therapy. Aust N Z J Med 1999; 29:377–378.
- Matsumura M, Haruki K, Kajinami K, Takada T. Angioedema likely related to angiotensin converting enzyme inhibitors. Intern Med 1993; 32:424–426.
- Khan MU, Baig MA, Javed RA, et al. Benazepril induced isolated visceral angioedema: a rare and under diagnosed adverse effect of angiotensin converting enzyme inhibitors. Int J Cardiol 2007; 118:e68–e69.
- Adhikari SP, Schneider JI. An unusual cause of abdominal pain and hypotension: angioedema of the bowel. J Emerg Med 2009; 36:23–25.
- Gibbs CR, Lip GY, Beevers DG. Angioedema due to ACE inhibitors: increased risk in patients of African origin. Br J Clin Pharmacol 1999; 48:861–865.
- Johnsen SP, Jacobsen J, Monster TB, Friis S, McLaughlin JK, Sørensen HT. Risk of first-time hospitalization for angioedema among users of ACE inhibitors and angiotensin receptor antagonists. Am J Med 2005; 118:1428–1329.
- Bi CK, Soltani K, Sloan JB, Weber RR, Elliott WJ, Murphy MB. Tissue-specific autoantibodies induced by captopril. Clin Res 1987; 35:922A.
- Bork K, Dewald G. Hereditary angioedema type III, angioedema associated with angiotensin II receptor antagonists, and female sex. Am J Med 2004; 116:644–645.
- Witten DM, Hirsch FD, Hartman GW. Acute reactions to urographic contrast medium: incidence, clinical characteristics and relationship to history of hypersensitivity states. Am J Roentgenol Radium Ther Nucl Med 1973; 119:832–840.
- Eck SL, Morse JH, Janssen DA, Emerson SG, Markovitz DM. Angioedema presenting as chronic gastrointestinal symptoms. Am J Gastroenterol 1993; 88:436–439.
- Coleman JW, Yeung JH, Roberts DH, Breckenridge AM, Park BK. Drug-specific antibodies in patients receiving captopril. Br J Clin Pharmacol 1986; 22:161–165.
- Kallenberg CG. Autoantibodies during captopril treatment. Arthritis Rheum 1985; 28:597–598.
- Inman WH, Rawson NS, Wilton LV, Pearce GL, Speirs CJ. Postmarketing surveillance of enalapril. I: Results of prescription-event monitoring. BMJ 1988; 297:826–829.
- Lefebvre J, Murphey LJ, Hartert TV, Jiao Shan R, Simmons WH, Brown NJ. Dipeptidyl peptidase IV activity in patients with ACE-inhibitor-associated angioedema. Hypertension 2002; 39:460–464.
- Molinaro G, Cugno M, Perez M, et al. Angiotensin-converting enzyme inhibitor-associated angioedema is characterized by a slower degradation of des-arginine(9)-bradykinin. J Pharmacol Exp Ther 2002; 303:232–237.
- Adam A, Cugno M, Molinaro G, Perez M, Lepage Y, Agostoni A. Aminopeptidase P in individuals with a history of angiooedema on ACE inhibitors. Lancet 2002; 359:2088–2089.
- Binkley KE, Davis A. Clinical, biochemical, and genetic characterization of a novel estrogen-dependent inherited form of angioedema. J Allergy Clin Immunol 2000; 106:546–550.
- Yeung JH, Coleman JW, Park BK. Drug-protein conjugates—IX. Immunogenicity of captopril-protein conjugates. Biochem Pharmacol 1985; 34:4005–4012.
- Abbosh J, Anderson JA, Levine AB, Kupin WL. Angiotensin converting enzyme inhibitor-induced angioedema more prevalent in transplant patients. Ann Allergy Asthma Immunol 1999; 82:473–476.
- Pichler WJ, Lehner R, Späth PJ. Recurrent angioedema associated with hypogonadism or anti-androgen therapy. Ann Allergy 1989; 63:301–305.
- Bass G, Honan D. Octaplas is not equivalent to fresh frozen plasma in the treatment of acute angioedema. Eur J Anaesthesiol 2007; 24:1062–1063.
- Bas M, Hoffmann TK, Bier H, Kojda G. Increased C-reactive protein in ACE-inhibitor-induced angioedema. Br J Clin Pharmacol 2005; 59:233–238.
- Herman AG. Differences in structure of angiotensin-converting enzyme inhibitors might predict differences in action. Am J Cardiol 1992; 70:102C–108C.
- Cunnion KM, Lee JC, Frank MM. Capsule production and growth phase influence binding of complement to Staphylococcus aureus. Infect Immunol 2001; 69:6796–6803.
- Cunnion KM, Wagner E, Frank MM. Complement and kinins. In:Parlow TG, Stites DP, Imboden JB, editors. Medical Immunology. 10th ed. New York, NY: Lange Medical Books; 2001:186–188.
- Pellacani A, Brunner HR, Nussberger J. Plasma kinins increase after angiotensin-converting enzyme inhibition in human subjects. Clin Sci (Lond) 1994; 87:567–574.
- Bristol-Myers Squibb Pharmaceutical Research Institute. FDA Advisory Committee Briefing Book for OMAPATRILAT Tablets NDA 21-188. www.fda.gov/ohrms/dockets/ac/02/briefing/3877B2_01_BristolMeyersSquibb.pdf. Accessed 2/4/2011.
- Kostis JB, Kim HJ, Rusnak J, et al. Incidence and characteristics of angioedema associated with enalapril. Arch Intern Med 2005; 165:1637–1642.
- Mahoney EJ, Devaiah AK. Angioedema and angiotensin-converting enzyme inhibitors: are demographics a risk? Otolaryngol Head Neck Surg 2008; 139:105–108.
- Warner KK, Visconti JA, Tschampel MM. Angiotensin II receptor blockers in patients with ACE inhibitor-induced angioedema. Ann Pharmacother 2000; 34:526–528.
- Kyrmizakis DE, Papadakis CE, Liolios AD, et al. Angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists. Arch Otolaryngol Head Neck Surg 2004; 130:1416–1419.
- MacLean JA, Hannaway PJ. Angioedema and AT1 receptor blockers: proceed with caution. Arch Intern Med 2003; 163:1488–1489,
- Abdi R, Dong VM, Lee CJ, Ntoso KA. Angiotensin II receptor blocker-associated angioedema: on the heels of ACE inhibitor angioedema. Pharmacotherapy 2002; 22:1173–1175.
- Lin RY, Shah SN. Increasing hospitalizations due to angioedema in the United States. Ann Allergy Asthma Immunol 2008; 101:185–192.
- Slater EE, Merrill DD, Guess HA, et al. Clinical profile of angioedema associated with angiotensin converting-enzyme inhibition. JAMA 1988; 260:967–970.
- Morimoto T, Gandhi TK, Fiskio JM, et al. An evaluation of risk factors for adverse drug events associated with angiotensin-converting enzyme inhibitors. J Eval Clin Pract 2004; 10:499–509.
- Cohen N, Sharon A, Golik A, Zaidenstein R, Modai D. Hereditary angioneurotic edema with severe hypovolemic shock. J Clin Gastroenterol 1993; 16:237–239.
- Ciaccia D, Brazer SR, Baker ME. Acquired C1 esterase inhibitor deficiency causing intestinal angioedema: CT appearance. AJR Am J Roentgenol 1993; 161:1215–1216.
- Malcolm A, Prather CM. Intestinal angioedema mimicking Crohn’s disease. Med J Aust 1999; 171:418–420.
- Schmidt TD, McGrath KM. Angiotensin-converting enzyme inhibitor angioedema of the intestine: a case report and review of the literature. Am J Med Sci 2002; 324:106–108.
- Karim MY, Masood A. Fresh-frozen plasma as a treatment for life-threatening ACE-inhibitor angioedema. J Allergy Clin Immunol 2002; 109:370–371.
- Warrier MR, Copilevitz CA, Dykewicz MS, Slavin RG. Fresh frozen plasma in the treatment of resistant angiotensin-converting enzyme inhibitor angioedema. Ann Allergy Asthma Immunol 2004; 92:573–575.
- Bas M, Adams V, Suvorava T, Niehues T, Hoffmann TK, Kojda G. Nonallergic angioedema: role of bradykinin. Allergy 2007; 62:842–856.
- Agostoni A, Cicardi M, Cugno M, Zingale LC, Gioffré D, Nussberger J. Angioedema due to angiotensin-converting enzyme inhibitors. Immunopharmacology 1999; 44:21–25.
KEY POINTS
- Visceral angioedema due to ACE-inhibitor therapy can easily be diagnosed by clinical suspicion and abdominal computed tomography (CT).
- Many physicians are not aware of this condition and so may subject patients to unnecessary invasive procedures, including surgery and endoscopy.
- If a middle-aged woman taking an ACE inhibitor presents with abdominal pain and emesis, the differential diagnosis should include visceral angioedema, and CT should be strongly considered.
Should alpha-blockers ever be used as antihypertensive drugs?
Alpha-blockers should not be used as first-line therapy for hypertension. However, an alpha-blocker can be considered as a second-line or third-line add-on in a patient whose blood pressure is not under control despite treatment with other drugs.
In addition, alpha-blockers are useful in relieving lower urinary tract symptoms in patients with benign prostatic hypertrophy. However, even in a patient who has both hypertension and benign prostatic hypertrophy, we advise physicians to use alpha-blockers primarily to relieve the urinary symptoms, and we recommend lowering the blood pressure with a drug of a class shown to reduce rates of illness and death.
NOT FIRST-LINE THERAPY
All antihypertensive drugs, including alpha-blockers, lower blood pressure. Alpha-blockers have been approved by the US Food and Drug Administration for treating high blood pressure, and they are just as effective as other antihypertensive drugs—if efficacy is defined as a decrease in millimeters of mercury.
However, lowering the blood pressure is not the main goal of antihypertensive therapy. What we want to achieve when prescribing antihypertensive drugs is to reduce the rates of heart attacks, strokes, and other adverse cardiovascular adverse outcomes, including death.
Unfortunately, alpha-blockers fall short in this regard. In the Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack (ALLHAT) trial,1,2 doxazosin (Cardura) was found to carry a higher risk of combined cardiovascular disease (relative risk 1.19, P = .04), mostly stroke. Alarmingly, the incidence of symptomatic heart failure in patients on doxazosin was twice that in patients on chlorthalidone (relative risk 2.04, P < .001). Doxazosin was minimally more effective in lowering blood pressure than chlorthalidone, but the small difference in blood pressure was unlikely to have accounted for the significant difference in the risk of heart failure.3
This experience with doxazosin illustrates a key drawback to surrogate end points: a treatment may produce a favorable outcome in the surrogate end point (blood pressure) but produce little or no benefit in terms of the real end point (stroke, myocardial infarction, and heart failure).4
Based on the ALLHAT data as well as on a Veterans Administration study in patients with chronic heart failure in which survival with prazosin (Minipress) was no better than with placebo,5 it seems reasonable to no longer use alpha-blockers as initial therapy for hypertension. This view is reflected by current European6 and American7 guidelines.
ALPHA-BLOCKERS AS PART OF COMBINATION THERAPY
In several clinical trials, alpha-blockers were allowed8 or were specified9,10 as add-on therapy if other drugs failed to control the blood pressure, but they were not used in a randomized fashion. Thus, we cannot judge their effect on cardiovascular outcomes such as heart attack and stroke.
The choice of drugs for combination therapy very often is still empirical and based on personal preference. Doxazosin as add-on therapy, in general, has been shown to be safe and well tolerated.11 But even if it is acceptable, it is not a preferred combination.
In the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT),9 patients received extended-release doxazosin as a third drug if they did not reach their goal blood pressure with either the combination of amlodipine (Norvasc) plus perindopril (Aceon) or atenolol (Tenormin) plus bendroflumethiazide. Extended-release doxazosin was an effective add-on, and there was no apparent excess rate of heart failure in doxazosin users.
In other studies, in patients with uncontrolled hypertension, adding doxazosin as a second- or third-line agent to a gold-standard drug—calcium channel blocker, diuretic, beta-blocker, angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or combinations of these—allowed significantly more participants to achieve their blood pressure goal.11
Personally, we consider doxazosin in patients whose blood pressure is not controlled with triple therapy with a renin-angiotensin system blocker, a diuretic, and a calcium channel antagonist in full doses. In patients with stage 3 or stage 4 kidney disease who can no longer tolerate renin-angiotensin system blockers, doxazosin may also be a useful adjunct. Whether the metabolic effects of alpha-blockers, such as a reduction in insulin resistance and a decrease in total and low-density lipoprotein cholesterol, will result in lower rates of morbidity and death has not been conclusively determined.
A point of view somewhat more favorable to the use of alpha-blockers has recently been put forward by Chapman et al.12
ALPHA-BLOCKERS ALLEVIATE SYMPTOMS OF BENIGN PROSTATIC HYPERTROPHY
Doxazosin and other alpha-blockers are commonly used to alleviate lower urinary tract symptoms in patients with benign prostatic hypertrophy.
Both high blood pressure and benign prostatic hypertrophy become more common with advancing age, and it has been estimated that both are present in more than 25% of men over age 60.13 Indeed, two trials documented that a significant reduction in symptoms of benign prostatic hypertrophy and in systolic and diastolic blood pressure can be achieved with an alpha-blocker.13,14
This raises the question whether such a “twofer” (treating two disease states with one drug) should be used in clinical practice. We have to consider that the principle of the twofer has never been tested and agree with Davis et al,3 who, in a further analysis of the ALLHAT data, stated that, “In older men with benign prostatic hypertrophy in whom an [alpha]-adrenergic blocker seems like the best treatment for the uropathy, coexisting hypertension should be treated with another antihypertensive drug as well.”3
Again, this would clearly relegate doxazosin to second-line or third-line status, even in patients with benign prostatic hypertrophy, in whom it has been shown to be indicated.
ADVERSE EFFECTS OF ALPHA-BLOCKERS
Dizziness, fatigue, and somnolence are occasionally reported but appear to be well tolerated. Postural hypotension is much less common with proper titration of standard doxazosin or with the use of controlled-release formulations.9–15 However, in patients with impaired autonomic function, even long-acting alpha-blockers can cause postural hypotension and syncope.
Patients using phosphodiesterase type 5 inhibitors—sildenafil (Viagra), vardenafil (Levitra), or tadalafil (Cialis)—for erectile dysfunction should avoid alpha-blockers because the blood-pressure-lowering effects of the two drug classes may be additive.
- Messerli FH. Implications of discontinuation of doxazosin arm of ALLHAT. Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (commentary). Lancet 2000; 355:863–864.
- Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalidone: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). ALLHAT Collaborative Research Group. JAMA 2000; 283:1967–1975.
- Davis BR, Cutler JA, Furberg CD, et al; ALLHAT Collaborative Research Group. Relationship of antihypertensive treatment regimens and change in blood pressure to risk for heart failure in hypertensive patients randomly assigned to doxazosin or chlorthalidone: further analyses from the Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial. Ann Intern Med 2002; 137:313–320.
- Messerli FH. Doxazosin and congestive heart failure (viewpoint). J Am Coll Cardiol 2001; 38:1295–1296.
- Cohn JN, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative Study. N Engl J Med 1986; 314:1547–1552.
- Mancia G, De Backer G, Dominiczak A, et al; ESH-ESC Task Force on the Management of Arterial Hypertension. 2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens 2007; 25:1751–1762.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA 2003; 289:2560–2572.
- Jamerson K, Weber MA, Bakris GL, et al; for the ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008; 359:2417–2428.
- Chapman N, Chang CL, Dahlöf B, Sever PS, Wedel H, Poulter NR; ASCOT Investigators. Effect of doxazosin gastrointestinal therapeutic system as third-line antihypertensive therapy on blood pressure and lipids in the Anglo-Scandinavian Cardiac Outcomes Trial. Circulation 2008; 118:42–48.
- de Alvaro F, Hernandez-Presa MAASOCIA Study. Effect of doxazosin gastrointestinal therapeutic system on patients with uncontrolled hypertension: the ASOCIA Study. J Cardiovasc Pharmacol 2006; 47:271–276.
- Black HR. Doxazosin as combination therapy for patients with stage 1 and stage 2 hypertension. J Cardiovasc Pharmacol 2003; 41:866–869.
- Chapman N, Chen C-Y, Fujita T, et al. Time to re-appraise the role of alpha-1 adrenoceptor antagonists in the management of hypertension? J Hypertens 2010; 28:1796–1803.
- Steers WD, Kirby RS. Clinical ease of using doxazosin in BPH patients with and without hypertension. Prostate Cancer Prostatic Dis 2005; 8:152–157.
- Guthrie RM, Siegel RL. A multicenter, community-based study of doxazosin in the treatment of concomitant hypertension and symptomatic benign prostatic hyperplasia: the Hypertension and BPH Intervention Trial (HABIT). Clin Ther 1999; 21:1732–1748.
- MacDonald R, Wilt TJ, Howe RW. Doxazosin for treating lower urinary tract symptoms compatible with benign prostatic obstruction: a systematic review of efficacy and adverse effects. BJU Int 2004; 94:1263–1270.
Alpha-blockers should not be used as first-line therapy for hypertension. However, an alpha-blocker can be considered as a second-line or third-line add-on in a patient whose blood pressure is not under control despite treatment with other drugs.
In addition, alpha-blockers are useful in relieving lower urinary tract symptoms in patients with benign prostatic hypertrophy. However, even in a patient who has both hypertension and benign prostatic hypertrophy, we advise physicians to use alpha-blockers primarily to relieve the urinary symptoms, and we recommend lowering the blood pressure with a drug of a class shown to reduce rates of illness and death.
NOT FIRST-LINE THERAPY
All antihypertensive drugs, including alpha-blockers, lower blood pressure. Alpha-blockers have been approved by the US Food and Drug Administration for treating high blood pressure, and they are just as effective as other antihypertensive drugs—if efficacy is defined as a decrease in millimeters of mercury.
However, lowering the blood pressure is not the main goal of antihypertensive therapy. What we want to achieve when prescribing antihypertensive drugs is to reduce the rates of heart attacks, strokes, and other adverse cardiovascular adverse outcomes, including death.
Unfortunately, alpha-blockers fall short in this regard. In the Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack (ALLHAT) trial,1,2 doxazosin (Cardura) was found to carry a higher risk of combined cardiovascular disease (relative risk 1.19, P = .04), mostly stroke. Alarmingly, the incidence of symptomatic heart failure in patients on doxazosin was twice that in patients on chlorthalidone (relative risk 2.04, P < .001). Doxazosin was minimally more effective in lowering blood pressure than chlorthalidone, but the small difference in blood pressure was unlikely to have accounted for the significant difference in the risk of heart failure.3
This experience with doxazosin illustrates a key drawback to surrogate end points: a treatment may produce a favorable outcome in the surrogate end point (blood pressure) but produce little or no benefit in terms of the real end point (stroke, myocardial infarction, and heart failure).4
Based on the ALLHAT data as well as on a Veterans Administration study in patients with chronic heart failure in which survival with prazosin (Minipress) was no better than with placebo,5 it seems reasonable to no longer use alpha-blockers as initial therapy for hypertension. This view is reflected by current European6 and American7 guidelines.
ALPHA-BLOCKERS AS PART OF COMBINATION THERAPY
In several clinical trials, alpha-blockers were allowed8 or were specified9,10 as add-on therapy if other drugs failed to control the blood pressure, but they were not used in a randomized fashion. Thus, we cannot judge their effect on cardiovascular outcomes such as heart attack and stroke.
The choice of drugs for combination therapy very often is still empirical and based on personal preference. Doxazosin as add-on therapy, in general, has been shown to be safe and well tolerated.11 But even if it is acceptable, it is not a preferred combination.
In the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT),9 patients received extended-release doxazosin as a third drug if they did not reach their goal blood pressure with either the combination of amlodipine (Norvasc) plus perindopril (Aceon) or atenolol (Tenormin) plus bendroflumethiazide. Extended-release doxazosin was an effective add-on, and there was no apparent excess rate of heart failure in doxazosin users.
In other studies, in patients with uncontrolled hypertension, adding doxazosin as a second- or third-line agent to a gold-standard drug—calcium channel blocker, diuretic, beta-blocker, angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or combinations of these—allowed significantly more participants to achieve their blood pressure goal.11
Personally, we consider doxazosin in patients whose blood pressure is not controlled with triple therapy with a renin-angiotensin system blocker, a diuretic, and a calcium channel antagonist in full doses. In patients with stage 3 or stage 4 kidney disease who can no longer tolerate renin-angiotensin system blockers, doxazosin may also be a useful adjunct. Whether the metabolic effects of alpha-blockers, such as a reduction in insulin resistance and a decrease in total and low-density lipoprotein cholesterol, will result in lower rates of morbidity and death has not been conclusively determined.
A point of view somewhat more favorable to the use of alpha-blockers has recently been put forward by Chapman et al.12
ALPHA-BLOCKERS ALLEVIATE SYMPTOMS OF BENIGN PROSTATIC HYPERTROPHY
Doxazosin and other alpha-blockers are commonly used to alleviate lower urinary tract symptoms in patients with benign prostatic hypertrophy.
Both high blood pressure and benign prostatic hypertrophy become more common with advancing age, and it has been estimated that both are present in more than 25% of men over age 60.13 Indeed, two trials documented that a significant reduction in symptoms of benign prostatic hypertrophy and in systolic and diastolic blood pressure can be achieved with an alpha-blocker.13,14
This raises the question whether such a “twofer” (treating two disease states with one drug) should be used in clinical practice. We have to consider that the principle of the twofer has never been tested and agree with Davis et al,3 who, in a further analysis of the ALLHAT data, stated that, “In older men with benign prostatic hypertrophy in whom an [alpha]-adrenergic blocker seems like the best treatment for the uropathy, coexisting hypertension should be treated with another antihypertensive drug as well.”3
Again, this would clearly relegate doxazosin to second-line or third-line status, even in patients with benign prostatic hypertrophy, in whom it has been shown to be indicated.
ADVERSE EFFECTS OF ALPHA-BLOCKERS
Dizziness, fatigue, and somnolence are occasionally reported but appear to be well tolerated. Postural hypotension is much less common with proper titration of standard doxazosin or with the use of controlled-release formulations.9–15 However, in patients with impaired autonomic function, even long-acting alpha-blockers can cause postural hypotension and syncope.
Patients using phosphodiesterase type 5 inhibitors—sildenafil (Viagra), vardenafil (Levitra), or tadalafil (Cialis)—for erectile dysfunction should avoid alpha-blockers because the blood-pressure-lowering effects of the two drug classes may be additive.
Alpha-blockers should not be used as first-line therapy for hypertension. However, an alpha-blocker can be considered as a second-line or third-line add-on in a patient whose blood pressure is not under control despite treatment with other drugs.
In addition, alpha-blockers are useful in relieving lower urinary tract symptoms in patients with benign prostatic hypertrophy. However, even in a patient who has both hypertension and benign prostatic hypertrophy, we advise physicians to use alpha-blockers primarily to relieve the urinary symptoms, and we recommend lowering the blood pressure with a drug of a class shown to reduce rates of illness and death.
NOT FIRST-LINE THERAPY
All antihypertensive drugs, including alpha-blockers, lower blood pressure. Alpha-blockers have been approved by the US Food and Drug Administration for treating high blood pressure, and they are just as effective as other antihypertensive drugs—if efficacy is defined as a decrease in millimeters of mercury.
However, lowering the blood pressure is not the main goal of antihypertensive therapy. What we want to achieve when prescribing antihypertensive drugs is to reduce the rates of heart attacks, strokes, and other adverse cardiovascular adverse outcomes, including death.
Unfortunately, alpha-blockers fall short in this regard. In the Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack (ALLHAT) trial,1,2 doxazosin (Cardura) was found to carry a higher risk of combined cardiovascular disease (relative risk 1.19, P = .04), mostly stroke. Alarmingly, the incidence of symptomatic heart failure in patients on doxazosin was twice that in patients on chlorthalidone (relative risk 2.04, P < .001). Doxazosin was minimally more effective in lowering blood pressure than chlorthalidone, but the small difference in blood pressure was unlikely to have accounted for the significant difference in the risk of heart failure.3
This experience with doxazosin illustrates a key drawback to surrogate end points: a treatment may produce a favorable outcome in the surrogate end point (blood pressure) but produce little or no benefit in terms of the real end point (stroke, myocardial infarction, and heart failure).4
Based on the ALLHAT data as well as on a Veterans Administration study in patients with chronic heart failure in which survival with prazosin (Minipress) was no better than with placebo,5 it seems reasonable to no longer use alpha-blockers as initial therapy for hypertension. This view is reflected by current European6 and American7 guidelines.
ALPHA-BLOCKERS AS PART OF COMBINATION THERAPY
In several clinical trials, alpha-blockers were allowed8 or were specified9,10 as add-on therapy if other drugs failed to control the blood pressure, but they were not used in a randomized fashion. Thus, we cannot judge their effect on cardiovascular outcomes such as heart attack and stroke.
The choice of drugs for combination therapy very often is still empirical and based on personal preference. Doxazosin as add-on therapy, in general, has been shown to be safe and well tolerated.11 But even if it is acceptable, it is not a preferred combination.
In the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT),9 patients received extended-release doxazosin as a third drug if they did not reach their goal blood pressure with either the combination of amlodipine (Norvasc) plus perindopril (Aceon) or atenolol (Tenormin) plus bendroflumethiazide. Extended-release doxazosin was an effective add-on, and there was no apparent excess rate of heart failure in doxazosin users.
In other studies, in patients with uncontrolled hypertension, adding doxazosin as a second- or third-line agent to a gold-standard drug—calcium channel blocker, diuretic, beta-blocker, angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or combinations of these—allowed significantly more participants to achieve their blood pressure goal.11
Personally, we consider doxazosin in patients whose blood pressure is not controlled with triple therapy with a renin-angiotensin system blocker, a diuretic, and a calcium channel antagonist in full doses. In patients with stage 3 or stage 4 kidney disease who can no longer tolerate renin-angiotensin system blockers, doxazosin may also be a useful adjunct. Whether the metabolic effects of alpha-blockers, such as a reduction in insulin resistance and a decrease in total and low-density lipoprotein cholesterol, will result in lower rates of morbidity and death has not been conclusively determined.
A point of view somewhat more favorable to the use of alpha-blockers has recently been put forward by Chapman et al.12
ALPHA-BLOCKERS ALLEVIATE SYMPTOMS OF BENIGN PROSTATIC HYPERTROPHY
Doxazosin and other alpha-blockers are commonly used to alleviate lower urinary tract symptoms in patients with benign prostatic hypertrophy.
Both high blood pressure and benign prostatic hypertrophy become more common with advancing age, and it has been estimated that both are present in more than 25% of men over age 60.13 Indeed, two trials documented that a significant reduction in symptoms of benign prostatic hypertrophy and in systolic and diastolic blood pressure can be achieved with an alpha-blocker.13,14
This raises the question whether such a “twofer” (treating two disease states with one drug) should be used in clinical practice. We have to consider that the principle of the twofer has never been tested and agree with Davis et al,3 who, in a further analysis of the ALLHAT data, stated that, “In older men with benign prostatic hypertrophy in whom an [alpha]-adrenergic blocker seems like the best treatment for the uropathy, coexisting hypertension should be treated with another antihypertensive drug as well.”3
Again, this would clearly relegate doxazosin to second-line or third-line status, even in patients with benign prostatic hypertrophy, in whom it has been shown to be indicated.
ADVERSE EFFECTS OF ALPHA-BLOCKERS
Dizziness, fatigue, and somnolence are occasionally reported but appear to be well tolerated. Postural hypotension is much less common with proper titration of standard doxazosin or with the use of controlled-release formulations.9–15 However, in patients with impaired autonomic function, even long-acting alpha-blockers can cause postural hypotension and syncope.
Patients using phosphodiesterase type 5 inhibitors—sildenafil (Viagra), vardenafil (Levitra), or tadalafil (Cialis)—for erectile dysfunction should avoid alpha-blockers because the blood-pressure-lowering effects of the two drug classes may be additive.
- Messerli FH. Implications of discontinuation of doxazosin arm of ALLHAT. Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (commentary). Lancet 2000; 355:863–864.
- Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalidone: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). ALLHAT Collaborative Research Group. JAMA 2000; 283:1967–1975.
- Davis BR, Cutler JA, Furberg CD, et al; ALLHAT Collaborative Research Group. Relationship of antihypertensive treatment regimens and change in blood pressure to risk for heart failure in hypertensive patients randomly assigned to doxazosin or chlorthalidone: further analyses from the Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial. Ann Intern Med 2002; 137:313–320.
- Messerli FH. Doxazosin and congestive heart failure (viewpoint). J Am Coll Cardiol 2001; 38:1295–1296.
- Cohn JN, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative Study. N Engl J Med 1986; 314:1547–1552.
- Mancia G, De Backer G, Dominiczak A, et al; ESH-ESC Task Force on the Management of Arterial Hypertension. 2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens 2007; 25:1751–1762.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA 2003; 289:2560–2572.
- Jamerson K, Weber MA, Bakris GL, et al; for the ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008; 359:2417–2428.
- Chapman N, Chang CL, Dahlöf B, Sever PS, Wedel H, Poulter NR; ASCOT Investigators. Effect of doxazosin gastrointestinal therapeutic system as third-line antihypertensive therapy on blood pressure and lipids in the Anglo-Scandinavian Cardiac Outcomes Trial. Circulation 2008; 118:42–48.
- de Alvaro F, Hernandez-Presa MAASOCIA Study. Effect of doxazosin gastrointestinal therapeutic system on patients with uncontrolled hypertension: the ASOCIA Study. J Cardiovasc Pharmacol 2006; 47:271–276.
- Black HR. Doxazosin as combination therapy for patients with stage 1 and stage 2 hypertension. J Cardiovasc Pharmacol 2003; 41:866–869.
- Chapman N, Chen C-Y, Fujita T, et al. Time to re-appraise the role of alpha-1 adrenoceptor antagonists in the management of hypertension? J Hypertens 2010; 28:1796–1803.
- Steers WD, Kirby RS. Clinical ease of using doxazosin in BPH patients with and without hypertension. Prostate Cancer Prostatic Dis 2005; 8:152–157.
- Guthrie RM, Siegel RL. A multicenter, community-based study of doxazosin in the treatment of concomitant hypertension and symptomatic benign prostatic hyperplasia: the Hypertension and BPH Intervention Trial (HABIT). Clin Ther 1999; 21:1732–1748.
- MacDonald R, Wilt TJ, Howe RW. Doxazosin for treating lower urinary tract symptoms compatible with benign prostatic obstruction: a systematic review of efficacy and adverse effects. BJU Int 2004; 94:1263–1270.
- Messerli FH. Implications of discontinuation of doxazosin arm of ALLHAT. Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (commentary). Lancet 2000; 355:863–864.
- Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalidone: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). ALLHAT Collaborative Research Group. JAMA 2000; 283:1967–1975.
- Davis BR, Cutler JA, Furberg CD, et al; ALLHAT Collaborative Research Group. Relationship of antihypertensive treatment regimens and change in blood pressure to risk for heart failure in hypertensive patients randomly assigned to doxazosin or chlorthalidone: further analyses from the Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial. Ann Intern Med 2002; 137:313–320.
- Messerli FH. Doxazosin and congestive heart failure (viewpoint). J Am Coll Cardiol 2001; 38:1295–1296.
- Cohn JN, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative Study. N Engl J Med 1986; 314:1547–1552.
- Mancia G, De Backer G, Dominiczak A, et al; ESH-ESC Task Force on the Management of Arterial Hypertension. 2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens 2007; 25:1751–1762.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA 2003; 289:2560–2572.
- Jamerson K, Weber MA, Bakris GL, et al; for the ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008; 359:2417–2428.
- Chapman N, Chang CL, Dahlöf B, Sever PS, Wedel H, Poulter NR; ASCOT Investigators. Effect of doxazosin gastrointestinal therapeutic system as third-line antihypertensive therapy on blood pressure and lipids in the Anglo-Scandinavian Cardiac Outcomes Trial. Circulation 2008; 118:42–48.
- de Alvaro F, Hernandez-Presa MAASOCIA Study. Effect of doxazosin gastrointestinal therapeutic system on patients with uncontrolled hypertension: the ASOCIA Study. J Cardiovasc Pharmacol 2006; 47:271–276.
- Black HR. Doxazosin as combination therapy for patients with stage 1 and stage 2 hypertension. J Cardiovasc Pharmacol 2003; 41:866–869.
- Chapman N, Chen C-Y, Fujita T, et al. Time to re-appraise the role of alpha-1 adrenoceptor antagonists in the management of hypertension? J Hypertens 2010; 28:1796–1803.
- Steers WD, Kirby RS. Clinical ease of using doxazosin in BPH patients with and without hypertension. Prostate Cancer Prostatic Dis 2005; 8:152–157.
- Guthrie RM, Siegel RL. A multicenter, community-based study of doxazosin in the treatment of concomitant hypertension and symptomatic benign prostatic hyperplasia: the Hypertension and BPH Intervention Trial (HABIT). Clin Ther 1999; 21:1732–1748.
- MacDonald R, Wilt TJ, Howe RW. Doxazosin for treating lower urinary tract symptoms compatible with benign prostatic obstruction: a systematic review of efficacy and adverse effects. BJU Int 2004; 94:1263–1270.