User login
Treatment costs threaten cancer program growth
Treatment costs are the greatest threat to the growth of cancer programs, according to a survey of nearly 300 cancer program administrators and providers.
Sixty-eight percent of survey respondents said treatment costs were among the biggest threats to future cancer program growth at their organization.
Other top threats to growth included physician alignment around services and program goals—cited by 47% of respondents—and changes in healthcare coverage—cited by 46%.
This survey—the “2017 Trending Now in Cancer Care Survey”—was conducted by the Association of Community Cancer Centers (ACCC) and Advisory Board’s Oncology Roundtable. It was supported by Pfizer Oncology.
The survey was distributed via email on July 24, 2017. Respondents included 293 cancer program administrators and providers from 209 institutions. They submitted responses over 6 weeks.
Respondents identified the following “biggest threats” to cancer program growth:
- Cost of drugs and/or new treatment modalities—68%
- Physician alignment around services and program goals—47%
- Changes in healthcare coverage—46%
- Cuts to fee-for-service reimbursement—44%
- Shifting reimbursement to value-based care—43%
- Marketplace competition—35%
- Workforce planning (eg, managing staff shortages)—34%
- Network strategy and integration—33%
- Site of care policies issued by private payers—27%
- Access to capital—26%
- Quality reporting requirements—22%
- Health information technology—21%
- Other—6%.
When asked to identify their greatest opportunities for cost savings, respondents overwhelmingly pointed toward clinical standardization (63%) and drugs (62%).
Other opportunities included:
- Supplies—28%
- Capital expenses (eg, imaging technology)—24%
- Non-clinical staff (eg, billing and coding specialists)—22%
- Technology maintenance—20%
- Clinical staff—16%
- Retail pharmacy—14%
- Clinical research—10%
- Support services (eg, acupuncture)—9%
- Other—4%.
Respondents also said the investments most likely to yield a return for their cancer program were:
- Increasing the number of sub-specialists (eg, breast surgeons)—59%
- Marketing—41%
- Specialty pharmacy—36%
- Increasing the number of general oncology physicians—34%
- Screening services (eg, mobile screening unit)—29%
- Capital investments—24%
- Clinical research—16%
- Support services—15%
- Retail pharmacy—14%
- Building upgrades—14%.
More details on the “2017 Trending Now in Cancer Care Survey” can be found on the ACCC website. ![]()
Treatment costs are the greatest threat to the growth of cancer programs, according to a survey of nearly 300 cancer program administrators and providers.
Sixty-eight percent of survey respondents said treatment costs were among the biggest threats to future cancer program growth at their organization.
Other top threats to growth included physician alignment around services and program goals—cited by 47% of respondents—and changes in healthcare coverage—cited by 46%.
This survey—the “2017 Trending Now in Cancer Care Survey”—was conducted by the Association of Community Cancer Centers (ACCC) and Advisory Board’s Oncology Roundtable. It was supported by Pfizer Oncology.
The survey was distributed via email on July 24, 2017. Respondents included 293 cancer program administrators and providers from 209 institutions. They submitted responses over 6 weeks.
Respondents identified the following “biggest threats” to cancer program growth:
- Cost of drugs and/or new treatment modalities—68%
- Physician alignment around services and program goals—47%
- Changes in healthcare coverage—46%
- Cuts to fee-for-service reimbursement—44%
- Shifting reimbursement to value-based care—43%
- Marketplace competition—35%
- Workforce planning (eg, managing staff shortages)—34%
- Network strategy and integration—33%
- Site of care policies issued by private payers—27%
- Access to capital—26%
- Quality reporting requirements—22%
- Health information technology—21%
- Other—6%.
When asked to identify their greatest opportunities for cost savings, respondents overwhelmingly pointed toward clinical standardization (63%) and drugs (62%).
Other opportunities included:
- Supplies—28%
- Capital expenses (eg, imaging technology)—24%
- Non-clinical staff (eg, billing and coding specialists)—22%
- Technology maintenance—20%
- Clinical staff—16%
- Retail pharmacy—14%
- Clinical research—10%
- Support services (eg, acupuncture)—9%
- Other—4%.
Respondents also said the investments most likely to yield a return for their cancer program were:
- Increasing the number of sub-specialists (eg, breast surgeons)—59%
- Marketing—41%
- Specialty pharmacy—36%
- Increasing the number of general oncology physicians—34%
- Screening services (eg, mobile screening unit)—29%
- Capital investments—24%
- Clinical research—16%
- Support services—15%
- Retail pharmacy—14%
- Building upgrades—14%.
More details on the “2017 Trending Now in Cancer Care Survey” can be found on the ACCC website. ![]()
Treatment costs are the greatest threat to the growth of cancer programs, according to a survey of nearly 300 cancer program administrators and providers.
Sixty-eight percent of survey respondents said treatment costs were among the biggest threats to future cancer program growth at their organization.
Other top threats to growth included physician alignment around services and program goals—cited by 47% of respondents—and changes in healthcare coverage—cited by 46%.
This survey—the “2017 Trending Now in Cancer Care Survey”—was conducted by the Association of Community Cancer Centers (ACCC) and Advisory Board’s Oncology Roundtable. It was supported by Pfizer Oncology.
The survey was distributed via email on July 24, 2017. Respondents included 293 cancer program administrators and providers from 209 institutions. They submitted responses over 6 weeks.
Respondents identified the following “biggest threats” to cancer program growth:
- Cost of drugs and/or new treatment modalities—68%
- Physician alignment around services and program goals—47%
- Changes in healthcare coverage—46%
- Cuts to fee-for-service reimbursement—44%
- Shifting reimbursement to value-based care—43%
- Marketplace competition—35%
- Workforce planning (eg, managing staff shortages)—34%
- Network strategy and integration—33%
- Site of care policies issued by private payers—27%
- Access to capital—26%
- Quality reporting requirements—22%
- Health information technology—21%
- Other—6%.
When asked to identify their greatest opportunities for cost savings, respondents overwhelmingly pointed toward clinical standardization (63%) and drugs (62%).
Other opportunities included:
- Supplies—28%
- Capital expenses (eg, imaging technology)—24%
- Non-clinical staff (eg, billing and coding specialists)—22%
- Technology maintenance—20%
- Clinical staff—16%
- Retail pharmacy—14%
- Clinical research—10%
- Support services (eg, acupuncture)—9%
- Other—4%.
Respondents also said the investments most likely to yield a return for their cancer program were:
- Increasing the number of sub-specialists (eg, breast surgeons)—59%
- Marketing—41%
- Specialty pharmacy—36%
- Increasing the number of general oncology physicians—34%
- Screening services (eg, mobile screening unit)—29%
- Capital investments—24%
- Clinical research—16%
- Support services—15%
- Retail pharmacy—14%
- Building upgrades—14%.
More details on the “2017 Trending Now in Cancer Care Survey” can be found on the ACCC website. ![]()
Technique could aid treatment of CLL
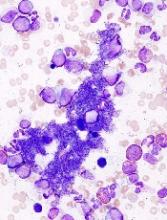
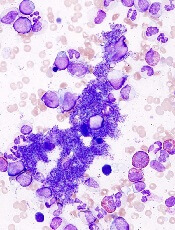
Researchers say they have developed a new technique for assessing chromosomal abnormalities in chronic lymphocytic leukemia (CLL).
The team believes their method, called immuno-flowFISH, could be used at the time of CLL diagnosis for disease stratification and after treatment to assess residual disease.
Kathryn A. Fuller, PhD, of The University of Western Australia in Crawley, Australia, and her colleagues described immuno-flowFISH in the journal Methods.
The name “immuno-flowFISH” acknowledges what has been incorporated into this technology.
“Immuno” recognizes that immunology testing is used to identify the CLL cells. “Flow” is used because the machine is an imaging flow cytometer. And “FISH” is the test that identifies the chromosomes inside the cells.
The researchers said they found that immuno-flowFISH could detect trisomic chromosomal abnormalities in cells with the phenotype of CLL.
And immuno-flowFISH provided greater specificity and sensitivity than standard FISH.
In particular, the researchers were able to analyze 10,000 to 20,000 cells in each sample, which is 100 to 200 times greater than traditional FISH methods.
“The imaging cytometer can analyze samples at a rate of up to 2000 cells per second, which means we can investigate a large number of cells in a relatively short amount of time, giving us greater sensitivity,” Dr Fuller said.
“This immuno-flowFISH method is an exciting development in personalizing pathology testing for leukemia,” added study author Wendy N. Erber, MD, DPhil, PhD, of The University of Western Australia.
Dr Erber and her colleagues are now expanding immuno-flowFISH so it can be applied to other malignancies as well. ![]()
Researchers say they have developed a new technique for assessing chromosomal abnormalities in chronic lymphocytic leukemia (CLL).
The team believes their method, called immuno-flowFISH, could be used at the time of CLL diagnosis for disease stratification and after treatment to assess residual disease.
Kathryn A. Fuller, PhD, of The University of Western Australia in Crawley, Australia, and her colleagues described immuno-flowFISH in the journal Methods.
The name “immuno-flowFISH” acknowledges what has been incorporated into this technology.
“Immuno” recognizes that immunology testing is used to identify the CLL cells. “Flow” is used because the machine is an imaging flow cytometer. And “FISH” is the test that identifies the chromosomes inside the cells.
The researchers said they found that immuno-flowFISH could detect trisomic chromosomal abnormalities in cells with the phenotype of CLL.
And immuno-flowFISH provided greater specificity and sensitivity than standard FISH.
In particular, the researchers were able to analyze 10,000 to 20,000 cells in each sample, which is 100 to 200 times greater than traditional FISH methods.
“The imaging cytometer can analyze samples at a rate of up to 2000 cells per second, which means we can investigate a large number of cells in a relatively short amount of time, giving us greater sensitivity,” Dr Fuller said.
“This immuno-flowFISH method is an exciting development in personalizing pathology testing for leukemia,” added study author Wendy N. Erber, MD, DPhil, PhD, of The University of Western Australia.
Dr Erber and her colleagues are now expanding immuno-flowFISH so it can be applied to other malignancies as well. ![]()
Researchers say they have developed a new technique for assessing chromosomal abnormalities in chronic lymphocytic leukemia (CLL).
The team believes their method, called immuno-flowFISH, could be used at the time of CLL diagnosis for disease stratification and after treatment to assess residual disease.
Kathryn A. Fuller, PhD, of The University of Western Australia in Crawley, Australia, and her colleagues described immuno-flowFISH in the journal Methods.
The name “immuno-flowFISH” acknowledges what has been incorporated into this technology.
“Immuno” recognizes that immunology testing is used to identify the CLL cells. “Flow” is used because the machine is an imaging flow cytometer. And “FISH” is the test that identifies the chromosomes inside the cells.
The researchers said they found that immuno-flowFISH could detect trisomic chromosomal abnormalities in cells with the phenotype of CLL.
And immuno-flowFISH provided greater specificity and sensitivity than standard FISH.
In particular, the researchers were able to analyze 10,000 to 20,000 cells in each sample, which is 100 to 200 times greater than traditional FISH methods.
“The imaging cytometer can analyze samples at a rate of up to 2000 cells per second, which means we can investigate a large number of cells in a relatively short amount of time, giving us greater sensitivity,” Dr Fuller said.
“This immuno-flowFISH method is an exciting development in personalizing pathology testing for leukemia,” added study author Wendy N. Erber, MD, DPhil, PhD, of The University of Western Australia.
Dr Erber and her colleagues are now expanding immuno-flowFISH so it can be applied to other malignancies as well. ![]()
FDA approves test to diagnose MPNs
The US Food and Drug Administration (FDA) has cleared use of QIAGEN’s ipsogen JAK2 RGQ PCR Kit (ipsogen JAK2 assay) for the diagnosis of all myeloproliferative neoplasms (MPNs).
The ipsogen JAK2 assay is a qualitative, in vitro diagnostic test designed to detect the JAK2 V617F/G1849T allele in genomic DNA extracted from EDTA whole blood.
The assay was previously cleared by the FDA for use in conjunction with other clinicopathological factors to aid the diagnosis of polycythemia vera.
Now, the FDA has cleared use of the assay for 2 additional MPNs—essential thrombocythemia and primary myelofibrosis.
“We are eager to expand the use of our ipsogen JAK2 assay, which is already available in Europe and other markets, for use in a wider range of patients in the US,” said Thierry Bernard, senior vice president and head of QIAGEN’s Molecular Diagnostics Business Area.
“Our JAK2 assay makes it easier for hematologists and oncologists to follow recommended diagnostic testing algorithms and international guidelines for their patients suspected of having MPNs.”
The ipsogen JAK2 assay is a real-time PCR test performed on the QIAGEN Rotor-Gene Q MDx instrument.
The test is intended for use as an adjunct to the evaluation of suspected MPNs, in conjunction with other clinicopathological factors.
The ipsogen JAK2 assay does not detect less common JAK2 mutations associated with MPNs, including mutations in exon 12, and is not intended for stand-alone diagnosis of MPNs. ![]()
The US Food and Drug Administration (FDA) has cleared use of QIAGEN’s ipsogen JAK2 RGQ PCR Kit (ipsogen JAK2 assay) for the diagnosis of all myeloproliferative neoplasms (MPNs).
The ipsogen JAK2 assay is a qualitative, in vitro diagnostic test designed to detect the JAK2 V617F/G1849T allele in genomic DNA extracted from EDTA whole blood.
The assay was previously cleared by the FDA for use in conjunction with other clinicopathological factors to aid the diagnosis of polycythemia vera.
Now, the FDA has cleared use of the assay for 2 additional MPNs—essential thrombocythemia and primary myelofibrosis.
“We are eager to expand the use of our ipsogen JAK2 assay, which is already available in Europe and other markets, for use in a wider range of patients in the US,” said Thierry Bernard, senior vice president and head of QIAGEN’s Molecular Diagnostics Business Area.
“Our JAK2 assay makes it easier for hematologists and oncologists to follow recommended diagnostic testing algorithms and international guidelines for their patients suspected of having MPNs.”
The ipsogen JAK2 assay is a real-time PCR test performed on the QIAGEN Rotor-Gene Q MDx instrument.
The test is intended for use as an adjunct to the evaluation of suspected MPNs, in conjunction with other clinicopathological factors.
The ipsogen JAK2 assay does not detect less common JAK2 mutations associated with MPNs, including mutations in exon 12, and is not intended for stand-alone diagnosis of MPNs. ![]()
The US Food and Drug Administration (FDA) has cleared use of QIAGEN’s ipsogen JAK2 RGQ PCR Kit (ipsogen JAK2 assay) for the diagnosis of all myeloproliferative neoplasms (MPNs).
The ipsogen JAK2 assay is a qualitative, in vitro diagnostic test designed to detect the JAK2 V617F/G1849T allele in genomic DNA extracted from EDTA whole blood.
The assay was previously cleared by the FDA for use in conjunction with other clinicopathological factors to aid the diagnosis of polycythemia vera.
Now, the FDA has cleared use of the assay for 2 additional MPNs—essential thrombocythemia and primary myelofibrosis.
“We are eager to expand the use of our ipsogen JAK2 assay, which is already available in Europe and other markets, for use in a wider range of patients in the US,” said Thierry Bernard, senior vice president and head of QIAGEN’s Molecular Diagnostics Business Area.
“Our JAK2 assay makes it easier for hematologists and oncologists to follow recommended diagnostic testing algorithms and international guidelines for their patients suspected of having MPNs.”
The ipsogen JAK2 assay is a real-time PCR test performed on the QIAGEN Rotor-Gene Q MDx instrument.
The test is intended for use as an adjunct to the evaluation of suspected MPNs, in conjunction with other clinicopathological factors.
The ipsogen JAK2 assay does not detect less common JAK2 mutations associated with MPNs, including mutations in exon 12, and is not intended for stand-alone diagnosis of MPNs. ![]()
Adjunct to HSCT receives orphan designation
The European Commission (EC) has granted orphan designation to NLA101 as an adjunct to hematopoietic stem cell transplant (HSCT).
NLA101 is a universal, off-the-shelf, stem and progenitor cell therapy intended to provide a short-term bridge for hematopoietic recovery while also providing long-term immunologic and clinical benefits in HSCT recipients.
NLA101 is a product of Nohla Therapeutics Inc.
The company says more than 125 infusions of NLA101 have been administered since 2009. The therapy is under investigation in patients receiving intensive chemotherapy as well as in HSCT recipients.
Results from a pilot study of NLA101 in HSCT recipients were presented at the 2014 ASH Annual Meeting.
In this study, 15 patients with hematologic malignancies underwent myeloablative cord blood transplant, with or without NLA101.
Patients who received NLA101 had a significantly reduced median time to platelet and neutrophil recovery, compared to controls. At 5 years, disease-free survival was 86% in the NLA101 group and 67% in the control group.
The rate of grade 3-4 acute graft-versus-host disease was 0% in the NLA101 group and 29% in the control group. The rate of transplant-related mortality was 0% and 22%, respectively.
Phase 2 studies of NLA101 in chemotherapy and HSCT recipients are ongoing.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
The European Commission (EC) has granted orphan designation to NLA101 as an adjunct to hematopoietic stem cell transplant (HSCT).
NLA101 is a universal, off-the-shelf, stem and progenitor cell therapy intended to provide a short-term bridge for hematopoietic recovery while also providing long-term immunologic and clinical benefits in HSCT recipients.
NLA101 is a product of Nohla Therapeutics Inc.
The company says more than 125 infusions of NLA101 have been administered since 2009. The therapy is under investigation in patients receiving intensive chemotherapy as well as in HSCT recipients.
Results from a pilot study of NLA101 in HSCT recipients were presented at the 2014 ASH Annual Meeting.
In this study, 15 patients with hematologic malignancies underwent myeloablative cord blood transplant, with or without NLA101.
Patients who received NLA101 had a significantly reduced median time to platelet and neutrophil recovery, compared to controls. At 5 years, disease-free survival was 86% in the NLA101 group and 67% in the control group.
The rate of grade 3-4 acute graft-versus-host disease was 0% in the NLA101 group and 29% in the control group. The rate of transplant-related mortality was 0% and 22%, respectively.
Phase 2 studies of NLA101 in chemotherapy and HSCT recipients are ongoing.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
The European Commission (EC) has granted orphan designation to NLA101 as an adjunct to hematopoietic stem cell transplant (HSCT).
NLA101 is a universal, off-the-shelf, stem and progenitor cell therapy intended to provide a short-term bridge for hematopoietic recovery while also providing long-term immunologic and clinical benefits in HSCT recipients.
NLA101 is a product of Nohla Therapeutics Inc.
The company says more than 125 infusions of NLA101 have been administered since 2009. The therapy is under investigation in patients receiving intensive chemotherapy as well as in HSCT recipients.
Results from a pilot study of NLA101 in HSCT recipients were presented at the 2014 ASH Annual Meeting.
In this study, 15 patients with hematologic malignancies underwent myeloablative cord blood transplant, with or without NLA101.
Patients who received NLA101 had a significantly reduced median time to platelet and neutrophil recovery, compared to controls. At 5 years, disease-free survival was 86% in the NLA101 group and 67% in the control group.
The rate of grade 3-4 acute graft-versus-host disease was 0% in the NLA101 group and 29% in the control group. The rate of transplant-related mortality was 0% and 22%, respectively.
Phase 2 studies of NLA101 in chemotherapy and HSCT recipients are ongoing.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
Low inhibitor rate observed in PUPs with hemophilia A
Researchers have observed a low inhibitor rate in previously untreated patients (PUPs) with severe hemophilia A who received treatment with Octanate®.
The study included 51 PUPs who received octanate, a plasma-derived, von Willebrand factor-stabilized coagulation factor VIII (FVIII) concentrate.
Five of these patients (9.8%) developed FVIII inhibitors, all of whom were receiving on-demand treatment.
The hemostatic efficacy of octanate was rated as “excellent” for 99.6% of all infusions, and tolerability was rated “very good” for 99.98% of infusions.
“We are very excited by the low inhibitor rates and the excellent efficacy and tolerability achieved with octanate® in this particularly challenging patient population,” said Larisa Belyanskaya, head of IBU Haematology at Octapharma AG, the company marketing octanate.
Octapharma sponsored this study, the results of which were published in Haemophilia.
The study enrolled 51 Caucasian males with previously untreated, severe hemophilia A. They had a median age at study entry of 7.7 months (range, 0.1 months to 67.3 months).
Patients received octanate, either prophylactically or on-demand, for 100 exposure days (EDs) or 5 years, whichever came first.
There were a mean of 136.33 (±246.3) EDs, and the mean dose of octanate was 38.4 (±28.6) IU/kg/ED. Most patients (78.4%) had at least 100 EDs. The total number of EDs was 6953.
Prophylaxis accounted for 3027 EDs, immune tolerance induction for 1869 EDs, treatment of bleeds for 1817 EDs, surgical procedures for 149 EDs, and in vivo recovery assessments for 106 EDs.
Inhibitors
Five patients developed FVIII inhibitors, 4 of which were high titer and 1 low titer.
In 3 cases, the inhibitors were considered clinically relevant. In the other 2 cases, the inhibitors disappeared without a change in dose or treatment frequency.
All inhibitors developed during on-demand treatment, and all 4 high-titer inhibitors developed within the first 20 EDs.
All patients who developed inhibitors had major F8 gene defects (intron 22 inversions or large deletions of exons 7-12) that are associated with a high risk of inhibitor development.
Efficacy
The hemostatic efficacy of octanate was rated as “excellent” in 99.6% of infusions (n=4700), “good” in 0.3% (n=15), and “moderate” in 0.02% (n=1).
Most bleeds resolved within 1 day of treatment (81.2%) or within 2 days (14.3%).
Efficacy was rated as “excellent” for all but 1 of the 2611 prophylactic infusions. One was rated as “good.”
For treatment of bleeds, efficacy was rated as “excellent” for 99.2% of infusions (n=1809), “good” for 0.8% (n=14), and “moderate” for 0.05% (n=1).
There were 23 evaluable surgical procedures in 19 patients. The efficacy of octanate was rated as “excellent” in all cases (201 infusions).
Safety
There were 260 treatment-emergent adverse events (AEs) in 45 patients (88.2%). Seventy-eight of these AEs were serious.
Twenty-one AEs were considered probably or possibly related to octanate—asymptomatic parvovirus B19 seroconversions (n=16) and FVIII inhibitor development (n=5). These were classified as serious AEs according to the study protocol.
The tolerability of octanate was considered “very good” in 99.98% of infusions (n=8674) and “good” in 0.02% (n=2). ![]()
Researchers have observed a low inhibitor rate in previously untreated patients (PUPs) with severe hemophilia A who received treatment with Octanate®.
The study included 51 PUPs who received octanate, a plasma-derived, von Willebrand factor-stabilized coagulation factor VIII (FVIII) concentrate.
Five of these patients (9.8%) developed FVIII inhibitors, all of whom were receiving on-demand treatment.
The hemostatic efficacy of octanate was rated as “excellent” for 99.6% of all infusions, and tolerability was rated “very good” for 99.98% of infusions.
“We are very excited by the low inhibitor rates and the excellent efficacy and tolerability achieved with octanate® in this particularly challenging patient population,” said Larisa Belyanskaya, head of IBU Haematology at Octapharma AG, the company marketing octanate.
Octapharma sponsored this study, the results of which were published in Haemophilia.
The study enrolled 51 Caucasian males with previously untreated, severe hemophilia A. They had a median age at study entry of 7.7 months (range, 0.1 months to 67.3 months).
Patients received octanate, either prophylactically or on-demand, for 100 exposure days (EDs) or 5 years, whichever came first.
There were a mean of 136.33 (±246.3) EDs, and the mean dose of octanate was 38.4 (±28.6) IU/kg/ED. Most patients (78.4%) had at least 100 EDs. The total number of EDs was 6953.
Prophylaxis accounted for 3027 EDs, immune tolerance induction for 1869 EDs, treatment of bleeds for 1817 EDs, surgical procedures for 149 EDs, and in vivo recovery assessments for 106 EDs.
Inhibitors
Five patients developed FVIII inhibitors, 4 of which were high titer and 1 low titer.
In 3 cases, the inhibitors were considered clinically relevant. In the other 2 cases, the inhibitors disappeared without a change in dose or treatment frequency.
All inhibitors developed during on-demand treatment, and all 4 high-titer inhibitors developed within the first 20 EDs.
All patients who developed inhibitors had major F8 gene defects (intron 22 inversions or large deletions of exons 7-12) that are associated with a high risk of inhibitor development.
Efficacy
The hemostatic efficacy of octanate was rated as “excellent” in 99.6% of infusions (n=4700), “good” in 0.3% (n=15), and “moderate” in 0.02% (n=1).
Most bleeds resolved within 1 day of treatment (81.2%) or within 2 days (14.3%).
Efficacy was rated as “excellent” for all but 1 of the 2611 prophylactic infusions. One was rated as “good.”
For treatment of bleeds, efficacy was rated as “excellent” for 99.2% of infusions (n=1809), “good” for 0.8% (n=14), and “moderate” for 0.05% (n=1).
There were 23 evaluable surgical procedures in 19 patients. The efficacy of octanate was rated as “excellent” in all cases (201 infusions).
Safety
There were 260 treatment-emergent adverse events (AEs) in 45 patients (88.2%). Seventy-eight of these AEs were serious.
Twenty-one AEs were considered probably or possibly related to octanate—asymptomatic parvovirus B19 seroconversions (n=16) and FVIII inhibitor development (n=5). These were classified as serious AEs according to the study protocol.
The tolerability of octanate was considered “very good” in 99.98% of infusions (n=8674) and “good” in 0.02% (n=2). ![]()
Researchers have observed a low inhibitor rate in previously untreated patients (PUPs) with severe hemophilia A who received treatment with Octanate®.
The study included 51 PUPs who received octanate, a plasma-derived, von Willebrand factor-stabilized coagulation factor VIII (FVIII) concentrate.
Five of these patients (9.8%) developed FVIII inhibitors, all of whom were receiving on-demand treatment.
The hemostatic efficacy of octanate was rated as “excellent” for 99.6% of all infusions, and tolerability was rated “very good” for 99.98% of infusions.
“We are very excited by the low inhibitor rates and the excellent efficacy and tolerability achieved with octanate® in this particularly challenging patient population,” said Larisa Belyanskaya, head of IBU Haematology at Octapharma AG, the company marketing octanate.
Octapharma sponsored this study, the results of which were published in Haemophilia.
The study enrolled 51 Caucasian males with previously untreated, severe hemophilia A. They had a median age at study entry of 7.7 months (range, 0.1 months to 67.3 months).
Patients received octanate, either prophylactically or on-demand, for 100 exposure days (EDs) or 5 years, whichever came first.
There were a mean of 136.33 (±246.3) EDs, and the mean dose of octanate was 38.4 (±28.6) IU/kg/ED. Most patients (78.4%) had at least 100 EDs. The total number of EDs was 6953.
Prophylaxis accounted for 3027 EDs, immune tolerance induction for 1869 EDs, treatment of bleeds for 1817 EDs, surgical procedures for 149 EDs, and in vivo recovery assessments for 106 EDs.
Inhibitors
Five patients developed FVIII inhibitors, 4 of which were high titer and 1 low titer.
In 3 cases, the inhibitors were considered clinically relevant. In the other 2 cases, the inhibitors disappeared without a change in dose or treatment frequency.
All inhibitors developed during on-demand treatment, and all 4 high-titer inhibitors developed within the first 20 EDs.
All patients who developed inhibitors had major F8 gene defects (intron 22 inversions or large deletions of exons 7-12) that are associated with a high risk of inhibitor development.
Efficacy
The hemostatic efficacy of octanate was rated as “excellent” in 99.6% of infusions (n=4700), “good” in 0.3% (n=15), and “moderate” in 0.02% (n=1).
Most bleeds resolved within 1 day of treatment (81.2%) or within 2 days (14.3%).
Efficacy was rated as “excellent” for all but 1 of the 2611 prophylactic infusions. One was rated as “good.”
For treatment of bleeds, efficacy was rated as “excellent” for 99.2% of infusions (n=1809), “good” for 0.8% (n=14), and “moderate” for 0.05% (n=1).
There were 23 evaluable surgical procedures in 19 patients. The efficacy of octanate was rated as “excellent” in all cases (201 infusions).
Safety
There were 260 treatment-emergent adverse events (AEs) in 45 patients (88.2%). Seventy-eight of these AEs were serious.
Twenty-one AEs were considered probably or possibly related to octanate—asymptomatic parvovirus B19 seroconversions (n=16) and FVIII inhibitor development (n=5). These were classified as serious AEs according to the study protocol.
The tolerability of octanate was considered “very good” in 99.98% of infusions (n=8674) and “good” in 0.02% (n=2). ![]()
FDA approves ready-to-use bivalirudin
The US Food and Drug Administration (FDA) has approved a ready-to-use formulation of bivalirudin for use as an anticoagulant in patients undergoing percutaneous coronary intervention.
Baxter International Inc. expects to launch this frozen, premixed formulation of bivalirudin—Bivalirudin in 0.9% Sodium Chloride Injection—in the US early this year.
The product will be available in 2 commonly prescribed dosage forms and strengths: 250 mg of bivalirudin per 50 mL (5 mg/mL) and 500 mg of bivalirudin per 100 mL (5 mg/mL).
This frozen, premixed, ready-to-use bivalirudin makes use of Baxter’s proprietary frozen GALAXY container technology, a non-PVC and non-DEHP system specifically designed to create a ready-to-use format for unstable molecules.
Baxter’s premixed medications are manufactured to current Good Manufacturing Practice regulations established and monitored by the FDA. ![]()
The US Food and Drug Administration (FDA) has approved a ready-to-use formulation of bivalirudin for use as an anticoagulant in patients undergoing percutaneous coronary intervention.
Baxter International Inc. expects to launch this frozen, premixed formulation of bivalirudin—Bivalirudin in 0.9% Sodium Chloride Injection—in the US early this year.
The product will be available in 2 commonly prescribed dosage forms and strengths: 250 mg of bivalirudin per 50 mL (5 mg/mL) and 500 mg of bivalirudin per 100 mL (5 mg/mL).
This frozen, premixed, ready-to-use bivalirudin makes use of Baxter’s proprietary frozen GALAXY container technology, a non-PVC and non-DEHP system specifically designed to create a ready-to-use format for unstable molecules.
Baxter’s premixed medications are manufactured to current Good Manufacturing Practice regulations established and monitored by the FDA. ![]()
The US Food and Drug Administration (FDA) has approved a ready-to-use formulation of bivalirudin for use as an anticoagulant in patients undergoing percutaneous coronary intervention.
Baxter International Inc. expects to launch this frozen, premixed formulation of bivalirudin—Bivalirudin in 0.9% Sodium Chloride Injection—in the US early this year.
The product will be available in 2 commonly prescribed dosage forms and strengths: 250 mg of bivalirudin per 50 mL (5 mg/mL) and 500 mg of bivalirudin per 100 mL (5 mg/mL).
This frozen, premixed, ready-to-use bivalirudin makes use of Baxter’s proprietary frozen GALAXY container technology, a non-PVC and non-DEHP system specifically designed to create a ready-to-use format for unstable molecules.
Baxter’s premixed medications are manufactured to current Good Manufacturing Practice regulations established and monitored by the FDA. ![]()
EC grants orphan designation to gilteritinib for AML
The European Commission (EC) has granted orphan designation to gilteritinib for the treatment of patients with acute myeloid leukemia (AML).
Gilteritinib is an investigational compound that has demonstrated inhibitory activity against FLT3 internal tandem duplication, FLT3 tyrosine kinase domain, and the AXL receptor.
Astellas Pharma Inc. is currently investigating gilteritinib in phase 3 trials of AML patients.
Results from a phase 1/2 study of gilteritinib in AML were published in The Lancet Oncology last June.
The study enrolled 252 adults with relapsed/refractory AML. They received gilteritinib once daily in 1 of 7 dose-escalation (n=23) or dose-expansion (n=229) cohorts.
The maximum tolerated dose was 300 mg/day. There were 2 dose-limiting toxicities in the 450 mg dose-escalation cohort—grade 3 diarrhea and grade 3 elevated aspartate aminotransferase.
Common treatment-related adverse events were diarrhea (37%), anemia (34%), fatigue (33%), elevated aspartate aminotransferase (26%), and increased alanine aminotransferase (19%).
Serious adverse events related to treatment included febrile neutropenia (n=5), sepsis (n=2), acute renal failure (n=5), pyrexia (n=3), and bacteremia (n=1).
There were 7 deaths considered possibly or probably related to treatment—pulmonary embolism (200 mg/day), respiratory failure (120 mg/day), hemoptysis (80 mg/day), intracranial hemorrhage (20 mg/day), ventricular fibrillation (120 mg/day), septic shock (80 mg/day), and neutropenia (120 mg/day).
The overall response rate was 40% (100/249), and the complete response (CR) rate was 8% (n=19).
Four percent of patients (n=10) had a CR with incomplete platelet recovery, 18% (n=46) had a CR with incomplete hematological recovery, and 10% (n=25) had a partial response.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
The European Commission (EC) has granted orphan designation to gilteritinib for the treatment of patients with acute myeloid leukemia (AML).
Gilteritinib is an investigational compound that has demonstrated inhibitory activity against FLT3 internal tandem duplication, FLT3 tyrosine kinase domain, and the AXL receptor.
Astellas Pharma Inc. is currently investigating gilteritinib in phase 3 trials of AML patients.
Results from a phase 1/2 study of gilteritinib in AML were published in The Lancet Oncology last June.
The study enrolled 252 adults with relapsed/refractory AML. They received gilteritinib once daily in 1 of 7 dose-escalation (n=23) or dose-expansion (n=229) cohorts.
The maximum tolerated dose was 300 mg/day. There were 2 dose-limiting toxicities in the 450 mg dose-escalation cohort—grade 3 diarrhea and grade 3 elevated aspartate aminotransferase.
Common treatment-related adverse events were diarrhea (37%), anemia (34%), fatigue (33%), elevated aspartate aminotransferase (26%), and increased alanine aminotransferase (19%).
Serious adverse events related to treatment included febrile neutropenia (n=5), sepsis (n=2), acute renal failure (n=5), pyrexia (n=3), and bacteremia (n=1).
There were 7 deaths considered possibly or probably related to treatment—pulmonary embolism (200 mg/day), respiratory failure (120 mg/day), hemoptysis (80 mg/day), intracranial hemorrhage (20 mg/day), ventricular fibrillation (120 mg/day), septic shock (80 mg/day), and neutropenia (120 mg/day).
The overall response rate was 40% (100/249), and the complete response (CR) rate was 8% (n=19).
Four percent of patients (n=10) had a CR with incomplete platelet recovery, 18% (n=46) had a CR with incomplete hematological recovery, and 10% (n=25) had a partial response.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
The European Commission (EC) has granted orphan designation to gilteritinib for the treatment of patients with acute myeloid leukemia (AML).
Gilteritinib is an investigational compound that has demonstrated inhibitory activity against FLT3 internal tandem duplication, FLT3 tyrosine kinase domain, and the AXL receptor.
Astellas Pharma Inc. is currently investigating gilteritinib in phase 3 trials of AML patients.
Results from a phase 1/2 study of gilteritinib in AML were published in The Lancet Oncology last June.
The study enrolled 252 adults with relapsed/refractory AML. They received gilteritinib once daily in 1 of 7 dose-escalation (n=23) or dose-expansion (n=229) cohorts.
The maximum tolerated dose was 300 mg/day. There were 2 dose-limiting toxicities in the 450 mg dose-escalation cohort—grade 3 diarrhea and grade 3 elevated aspartate aminotransferase.
Common treatment-related adverse events were diarrhea (37%), anemia (34%), fatigue (33%), elevated aspartate aminotransferase (26%), and increased alanine aminotransferase (19%).
Serious adverse events related to treatment included febrile neutropenia (n=5), sepsis (n=2), acute renal failure (n=5), pyrexia (n=3), and bacteremia (n=1).
There were 7 deaths considered possibly or probably related to treatment—pulmonary embolism (200 mg/day), respiratory failure (120 mg/day), hemoptysis (80 mg/day), intracranial hemorrhage (20 mg/day), ventricular fibrillation (120 mg/day), septic shock (80 mg/day), and neutropenia (120 mg/day).
The overall response rate was 40% (100/249), and the complete response (CR) rate was 8% (n=19).
Four percent of patients (n=10) had a CR with incomplete platelet recovery, 18% (n=46) had a CR with incomplete hematological recovery, and 10% (n=25) had a partial response.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
EC authorizes brentuximab vedotin for CTCL
The European Commission (EC) has extended the conditional marketing authorization for brentuximab vedotin (Adcetris®).
The drug is now approved for use in adults with CD30-positive cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
Brentuximab vedotin can be marketed for this indication in the member states of the European Union as well as in Norway, Liechtenstein, and Iceland.
Conditional marketing authorization from the EC is valid for 1 year and is reviewed annually.
With conditional authorization, drug developers are required to provide comprehensive data confirming a drug’s benefit-risk balance is positive. Once these data are available, a conditional marketing authorization may be converted to a standard marketing authorization.
Drugs are eligible for conditional marketing authorization if they are designated as orphan medicines, intended for use in emergency situations, or designed to treat, prevent, or diagnose seriously debilitating or life-threatening diseases.
The EC previously granted brentuximab vedotin conditional marketing authorization for the treatment of:
- Adults with CD30+ Hodgkin lymphoma who are at an increased risk of relapse or progression following autologous hematopoietic stem cell transplant (auto-HSCT)
- Adults with relapsed or refractory CD30+ Hodgkin lymphoma after auto-HSCT or after at least 2 prior therapies when auto-HSCT or multi-agent chemotherapy is not a treatment option
- Adults with relapsed or refractory systemic anaplastic large-cell lymphoma.
Brentuximab vedotin is under joint development by Seattle Genetics and Takeda Pharmaceutical Company Limited.
Phase 3 data
The EC’s latest authorization for brentuximab vedotin is based on data from the phase 3 ALCANZA trial.
Updated results from ALCANZA were presented at the 2017 ASH Annual Meeting in December. Results were previously presented at the 9th Annual T-cell Lymphoma Forum in January 2017 and published in The Lancet in June 2017.
The trial included 128 evaluable patients with CD30-positive CTCL who had received at least 1 prior systemic therapy.
Sixty-four patients were assigned to receive brentuximab vedotin, and 64 were assigned to receive the investigator’s choice of methotrexate or bexarotene (control arm). Patients received treatment for up to 1 year.
For the update, the median follow-up was 33.9 months.
There was a significant improvement in the rate of objective response lasting at least 4 months (ORR4) in the brentuximab vedotin arm compared to the control arm. The ORR4 was 60.9% and 7.8%, respectively (P<0.001). The complete response rate was 18.8% and 0%, respectively (P<0.001).
The median progression-free survival was 15.8 months in the brentuximab vedotin arm and 3.6 months in the control arm (hazard ratio=0.373; 95% CI, 0.245-0.569; P<0.001).
At time of analysis, 73% of patients in the brentuximab vedotin arm and 75% in the control arm had received 1 or more subsequent skin-directed or systemic therapies. The median time to next treatment was 14.2 months in the brentuximab vedotin arm and 6.1 months in the control arm (P<0.001).
Peripheral neuropathy was the most commonly reported adverse event in patients who received brentuximab vedotin. The incidence was 67% in these patients and 6% in controls.
In the brentuximab arm, 86% of patients reported resolution or improvement in peripheral neuropathy. Eighteen patients had ongoing peripheral neuropathy events, including 15 patients with grade 1 and 3 patients with grade 2 events.
The European Commission (EC) has extended the conditional marketing authorization for brentuximab vedotin (Adcetris®).
The drug is now approved for use in adults with CD30-positive cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
Brentuximab vedotin can be marketed for this indication in the member states of the European Union as well as in Norway, Liechtenstein, and Iceland.
Conditional marketing authorization from the EC is valid for 1 year and is reviewed annually.
With conditional authorization, drug developers are required to provide comprehensive data confirming a drug’s benefit-risk balance is positive. Once these data are available, a conditional marketing authorization may be converted to a standard marketing authorization.
Drugs are eligible for conditional marketing authorization if they are designated as orphan medicines, intended for use in emergency situations, or designed to treat, prevent, or diagnose seriously debilitating or life-threatening diseases.
The EC previously granted brentuximab vedotin conditional marketing authorization for the treatment of:
- Adults with CD30+ Hodgkin lymphoma who are at an increased risk of relapse or progression following autologous hematopoietic stem cell transplant (auto-HSCT)
- Adults with relapsed or refractory CD30+ Hodgkin lymphoma after auto-HSCT or after at least 2 prior therapies when auto-HSCT or multi-agent chemotherapy is not a treatment option
- Adults with relapsed or refractory systemic anaplastic large-cell lymphoma.
Brentuximab vedotin is under joint development by Seattle Genetics and Takeda Pharmaceutical Company Limited.
Phase 3 data
The EC’s latest authorization for brentuximab vedotin is based on data from the phase 3 ALCANZA trial.
Updated results from ALCANZA were presented at the 2017 ASH Annual Meeting in December. Results were previously presented at the 9th Annual T-cell Lymphoma Forum in January 2017 and published in The Lancet in June 2017.
The trial included 128 evaluable patients with CD30-positive CTCL who had received at least 1 prior systemic therapy.
Sixty-four patients were assigned to receive brentuximab vedotin, and 64 were assigned to receive the investigator’s choice of methotrexate or bexarotene (control arm). Patients received treatment for up to 1 year.
For the update, the median follow-up was 33.9 months.
There was a significant improvement in the rate of objective response lasting at least 4 months (ORR4) in the brentuximab vedotin arm compared to the control arm. The ORR4 was 60.9% and 7.8%, respectively (P<0.001). The complete response rate was 18.8% and 0%, respectively (P<0.001).
The median progression-free survival was 15.8 months in the brentuximab vedotin arm and 3.6 months in the control arm (hazard ratio=0.373; 95% CI, 0.245-0.569; P<0.001).
At time of analysis, 73% of patients in the brentuximab vedotin arm and 75% in the control arm had received 1 or more subsequent skin-directed or systemic therapies. The median time to next treatment was 14.2 months in the brentuximab vedotin arm and 6.1 months in the control arm (P<0.001).
Peripheral neuropathy was the most commonly reported adverse event in patients who received brentuximab vedotin. The incidence was 67% in these patients and 6% in controls.
In the brentuximab arm, 86% of patients reported resolution or improvement in peripheral neuropathy. Eighteen patients had ongoing peripheral neuropathy events, including 15 patients with grade 1 and 3 patients with grade 2 events.
The European Commission (EC) has extended the conditional marketing authorization for brentuximab vedotin (Adcetris®).
The drug is now approved for use in adults with CD30-positive cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
Brentuximab vedotin can be marketed for this indication in the member states of the European Union as well as in Norway, Liechtenstein, and Iceland.
Conditional marketing authorization from the EC is valid for 1 year and is reviewed annually.
With conditional authorization, drug developers are required to provide comprehensive data confirming a drug’s benefit-risk balance is positive. Once these data are available, a conditional marketing authorization may be converted to a standard marketing authorization.
Drugs are eligible for conditional marketing authorization if they are designated as orphan medicines, intended for use in emergency situations, or designed to treat, prevent, or diagnose seriously debilitating or life-threatening diseases.
The EC previously granted brentuximab vedotin conditional marketing authorization for the treatment of:
- Adults with CD30+ Hodgkin lymphoma who are at an increased risk of relapse or progression following autologous hematopoietic stem cell transplant (auto-HSCT)
- Adults with relapsed or refractory CD30+ Hodgkin lymphoma after auto-HSCT or after at least 2 prior therapies when auto-HSCT or multi-agent chemotherapy is not a treatment option
- Adults with relapsed or refractory systemic anaplastic large-cell lymphoma.
Brentuximab vedotin is under joint development by Seattle Genetics and Takeda Pharmaceutical Company Limited.
Phase 3 data
The EC’s latest authorization for brentuximab vedotin is based on data from the phase 3 ALCANZA trial.
Updated results from ALCANZA were presented at the 2017 ASH Annual Meeting in December. Results were previously presented at the 9th Annual T-cell Lymphoma Forum in January 2017 and published in The Lancet in June 2017.
The trial included 128 evaluable patients with CD30-positive CTCL who had received at least 1 prior systemic therapy.
Sixty-four patients were assigned to receive brentuximab vedotin, and 64 were assigned to receive the investigator’s choice of methotrexate or bexarotene (control arm). Patients received treatment for up to 1 year.
For the update, the median follow-up was 33.9 months.
There was a significant improvement in the rate of objective response lasting at least 4 months (ORR4) in the brentuximab vedotin arm compared to the control arm. The ORR4 was 60.9% and 7.8%, respectively (P<0.001). The complete response rate was 18.8% and 0%, respectively (P<0.001).
The median progression-free survival was 15.8 months in the brentuximab vedotin arm and 3.6 months in the control arm (hazard ratio=0.373; 95% CI, 0.245-0.569; P<0.001).
At time of analysis, 73% of patients in the brentuximab vedotin arm and 75% in the control arm had received 1 or more subsequent skin-directed or systemic therapies. The median time to next treatment was 14.2 months in the brentuximab vedotin arm and 6.1 months in the control arm (P<0.001).
Peripheral neuropathy was the most commonly reported adverse event in patients who received brentuximab vedotin. The incidence was 67% in these patients and 6% in controls.
In the brentuximab arm, 86% of patients reported resolution or improvement in peripheral neuropathy. Eighteen patients had ongoing peripheral neuropathy events, including 15 patients with grade 1 and 3 patients with grade 2 events.
Ofatumumab to be pulled from non-US markets
Novartis is planning to stop marketing ofatumumab (Arzerra®) outside the US, but the drug will still be available for certain patients.
The company plans to work with regulatory authorities to establish compassionate use programs for chronic lymphocytic leukemia (CLL) patients outside the US who are currently receiving ofatumumab.
Patients accessing these programs will be offered continued treatment with ofatumumab for as long as they benefit from it, free of charge.
And Novartis will continue to market ofatumumab for CLL in the US.
“Novartis’s intention to transition Arzerra to compassionate use programs in the non-US markets reflects the fact that many more drugs have become available for CLL over the last 5 years and that there is a low number of patients using Arzerra outside of the US market,” said Jan van de Winkel, PhD, chief executive officer of Genmab.
Ofatumumab is marketed under a collaboration agreement between Genmab and Novartis.
Because Novartis has decided to pull ofatumumab from non-US markets, the company will pay Genmab a lump sum of $50 million (USD) for lost potential milestones and royalties. Royalties will continue to be earned on net sales of the drug.
Novartis intends to start the transition to compassionate use programs as soon as the company and regulatory authorities have agreed to a plan.
The two phase 3 studies of ofatumumab in relapsing multiple sclerosis and the study in indolent non-Hodgkin lymphoma will not be affected by this change. All 3 trials will continue.
About ofatumumab
Ofatumumab is a monoclonal antibody designed to target CD20 on the surface of CLL cells and normal B lymphocytes.
In more than 60 countries worldwide, including the US and European Union member countries, ofatumumab is approved as monotherapy for CLL patients who are refractory to treatment with fludarabine and alemtuzumab.
Other approved indications for ofatumumab in the European Union include:
- In combination with chlorambucil or bendamustine to treat CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy
- In combination with fludarabine and cyclophosphamide to treat adults with relapsed CLL.
Other approved indications for ofatumumab in the US include:
- In combination with chlorambucil to treat previously untreated CLL patients for whom fludarabine-based therapy is considered inappropriate
- In combination with fludarabine and cyclophosphamide to treat patients with relapsed CLL
- For extended treatment of patients who are in complete or partial response after at least 2 lines of therapy for recurrent or progressive CLL.
Novartis is planning to stop marketing ofatumumab (Arzerra®) outside the US, but the drug will still be available for certain patients.
The company plans to work with regulatory authorities to establish compassionate use programs for chronic lymphocytic leukemia (CLL) patients outside the US who are currently receiving ofatumumab.
Patients accessing these programs will be offered continued treatment with ofatumumab for as long as they benefit from it, free of charge.
And Novartis will continue to market ofatumumab for CLL in the US.
“Novartis’s intention to transition Arzerra to compassionate use programs in the non-US markets reflects the fact that many more drugs have become available for CLL over the last 5 years and that there is a low number of patients using Arzerra outside of the US market,” said Jan van de Winkel, PhD, chief executive officer of Genmab.
Ofatumumab is marketed under a collaboration agreement between Genmab and Novartis.
Because Novartis has decided to pull ofatumumab from non-US markets, the company will pay Genmab a lump sum of $50 million (USD) for lost potential milestones and royalties. Royalties will continue to be earned on net sales of the drug.
Novartis intends to start the transition to compassionate use programs as soon as the company and regulatory authorities have agreed to a plan.
The two phase 3 studies of ofatumumab in relapsing multiple sclerosis and the study in indolent non-Hodgkin lymphoma will not be affected by this change. All 3 trials will continue.
About ofatumumab
Ofatumumab is a monoclonal antibody designed to target CD20 on the surface of CLL cells and normal B lymphocytes.
In more than 60 countries worldwide, including the US and European Union member countries, ofatumumab is approved as monotherapy for CLL patients who are refractory to treatment with fludarabine and alemtuzumab.
Other approved indications for ofatumumab in the European Union include:
- In combination with chlorambucil or bendamustine to treat CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy
- In combination with fludarabine and cyclophosphamide to treat adults with relapsed CLL.
Other approved indications for ofatumumab in the US include:
- In combination with chlorambucil to treat previously untreated CLL patients for whom fludarabine-based therapy is considered inappropriate
- In combination with fludarabine and cyclophosphamide to treat patients with relapsed CLL
- For extended treatment of patients who are in complete or partial response after at least 2 lines of therapy for recurrent or progressive CLL.
Novartis is planning to stop marketing ofatumumab (Arzerra®) outside the US, but the drug will still be available for certain patients.
The company plans to work with regulatory authorities to establish compassionate use programs for chronic lymphocytic leukemia (CLL) patients outside the US who are currently receiving ofatumumab.
Patients accessing these programs will be offered continued treatment with ofatumumab for as long as they benefit from it, free of charge.
And Novartis will continue to market ofatumumab for CLL in the US.
“Novartis’s intention to transition Arzerra to compassionate use programs in the non-US markets reflects the fact that many more drugs have become available for CLL over the last 5 years and that there is a low number of patients using Arzerra outside of the US market,” said Jan van de Winkel, PhD, chief executive officer of Genmab.
Ofatumumab is marketed under a collaboration agreement between Genmab and Novartis.
Because Novartis has decided to pull ofatumumab from non-US markets, the company will pay Genmab a lump sum of $50 million (USD) for lost potential milestones and royalties. Royalties will continue to be earned on net sales of the drug.
Novartis intends to start the transition to compassionate use programs as soon as the company and regulatory authorities have agreed to a plan.
The two phase 3 studies of ofatumumab in relapsing multiple sclerosis and the study in indolent non-Hodgkin lymphoma will not be affected by this change. All 3 trials will continue.
About ofatumumab
Ofatumumab is a monoclonal antibody designed to target CD20 on the surface of CLL cells and normal B lymphocytes.
In more than 60 countries worldwide, including the US and European Union member countries, ofatumumab is approved as monotherapy for CLL patients who are refractory to treatment with fludarabine and alemtuzumab.
Other approved indications for ofatumumab in the European Union include:
- In combination with chlorambucil or bendamustine to treat CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy
- In combination with fludarabine and cyclophosphamide to treat adults with relapsed CLL.
Other approved indications for ofatumumab in the US include:
- In combination with chlorambucil to treat previously untreated CLL patients for whom fludarabine-based therapy is considered inappropriate
- In combination with fludarabine and cyclophosphamide to treat patients with relapsed CLL
- For extended treatment of patients who are in complete or partial response after at least 2 lines of therapy for recurrent or progressive CLL.
Health systems plan to produce drugs themselves
A group of US health systems is planning to form a not-for-profit generic drug company with the goal of ending drug shortages and reducing prices for patients.
The company will either directly manufacture generic drugs or subcontract manufacturing to organizations it deems reputable.
“For people in the United States, there is a dangerous gap today between the demand and supply of affordable prescription drugs,” said Richard J. Gilfillan, MD, chief executive officer of Trinity Health, one of the health systems involved in this project.
“If the only way to provide our communities with affordable drugs is to produce them ourselves, then that is what we will do. We look forward to more healthcare systems around the country joining this people-centered effort.”
The organizations involved in this project include Intermountain Healthcare, Ascension, SSM Health, and Trinity Health, as well as the US Department of Veterans Affairs (although the department has not provided financial support for the project).
The 5 organizations represent more than 450 hospitals around the US, and other health systems are set to join the initiative as well.
“It’s an ambitious plan, but healthcare systems are in the best position to fix the problems in the generic drug market,” said Marc Harrison, MD, president and chief executive officer of Intermountain Healthcare.
“We witness, on a daily basis, how shortages of essential generic medications or egregious cost increases for those same drugs affect our patients. We are confident we can improve the situation for our patients by bringing much-needed competition to the generic drug market.”
The formation of this not-for-profit generic drug company will be guided by an advisory committee, which will include:
- Madhu Balachandran, retired executive vice-president of Global Operations, Amgen
- Don Berwick, MD, president emeritus and senior fellow, Institute for Healthcare Improvement; former Centers for Medicare & Medicaid Services administrator
- Clayton Christensen, professor at Harvard Business School and founder of Innosight
- Bob Kerrey, managing director, Allen & Company; former Nebraska governor and US senator
- Martin VanTrieste, retired senior vice-president and chief quality officer, Amgen
- Senior-level leaders from the organizations founding the company.
A group of US health systems is planning to form a not-for-profit generic drug company with the goal of ending drug shortages and reducing prices for patients.
The company will either directly manufacture generic drugs or subcontract manufacturing to organizations it deems reputable.
“For people in the United States, there is a dangerous gap today between the demand and supply of affordable prescription drugs,” said Richard J. Gilfillan, MD, chief executive officer of Trinity Health, one of the health systems involved in this project.
“If the only way to provide our communities with affordable drugs is to produce them ourselves, then that is what we will do. We look forward to more healthcare systems around the country joining this people-centered effort.”
The organizations involved in this project include Intermountain Healthcare, Ascension, SSM Health, and Trinity Health, as well as the US Department of Veterans Affairs (although the department has not provided financial support for the project).
The 5 organizations represent more than 450 hospitals around the US, and other health systems are set to join the initiative as well.
“It’s an ambitious plan, but healthcare systems are in the best position to fix the problems in the generic drug market,” said Marc Harrison, MD, president and chief executive officer of Intermountain Healthcare.
“We witness, on a daily basis, how shortages of essential generic medications or egregious cost increases for those same drugs affect our patients. We are confident we can improve the situation for our patients by bringing much-needed competition to the generic drug market.”
The formation of this not-for-profit generic drug company will be guided by an advisory committee, which will include:
- Madhu Balachandran, retired executive vice-president of Global Operations, Amgen
- Don Berwick, MD, president emeritus and senior fellow, Institute for Healthcare Improvement; former Centers for Medicare & Medicaid Services administrator
- Clayton Christensen, professor at Harvard Business School and founder of Innosight
- Bob Kerrey, managing director, Allen & Company; former Nebraska governor and US senator
- Martin VanTrieste, retired senior vice-president and chief quality officer, Amgen
- Senior-level leaders from the organizations founding the company.
A group of US health systems is planning to form a not-for-profit generic drug company with the goal of ending drug shortages and reducing prices for patients.
The company will either directly manufacture generic drugs or subcontract manufacturing to organizations it deems reputable.
“For people in the United States, there is a dangerous gap today between the demand and supply of affordable prescription drugs,” said Richard J. Gilfillan, MD, chief executive officer of Trinity Health, one of the health systems involved in this project.
“If the only way to provide our communities with affordable drugs is to produce them ourselves, then that is what we will do. We look forward to more healthcare systems around the country joining this people-centered effort.”
The organizations involved in this project include Intermountain Healthcare, Ascension, SSM Health, and Trinity Health, as well as the US Department of Veterans Affairs (although the department has not provided financial support for the project).
The 5 organizations represent more than 450 hospitals around the US, and other health systems are set to join the initiative as well.
“It’s an ambitious plan, but healthcare systems are in the best position to fix the problems in the generic drug market,” said Marc Harrison, MD, president and chief executive officer of Intermountain Healthcare.
“We witness, on a daily basis, how shortages of essential generic medications or egregious cost increases for those same drugs affect our patients. We are confident we can improve the situation for our patients by bringing much-needed competition to the generic drug market.”
The formation of this not-for-profit generic drug company will be guided by an advisory committee, which will include:
- Madhu Balachandran, retired executive vice-president of Global Operations, Amgen
- Don Berwick, MD, president emeritus and senior fellow, Institute for Healthcare Improvement; former Centers for Medicare & Medicaid Services administrator
- Clayton Christensen, professor at Harvard Business School and founder of Innosight
- Bob Kerrey, managing director, Allen & Company; former Nebraska governor and US senator
- Martin VanTrieste, retired senior vice-president and chief quality officer, Amgen
- Senior-level leaders from the organizations founding the company.