User login
Nurse education boosts proper use of VTE prophylaxis
Online education programs for nurses can improve the administration of prophylaxis for venous thromboembolism (VTE), a new study suggests.
The research was spurred by a documented need to boost the administration of prescribed VTE prophylaxis in hospitalized patients.
Data had shown that patients’ refusal of VTE prophylaxis frequently resulted in nurses not administering the prescribed therapy.
The new research indicates that online education modules helped nurses communicate to patients the need for VTE prophylaxis and therefore improved rates of use.
“We teach in hopes of improving patient care, but there’s actually very little evidence that online professional education can have a measurable impact. Our results show that it does,” said Elliott Haut, MD, PhD, of The Johns Hopkins University School of Medicine in Baltimore, Maryland.
Dr Haut and his colleagues reported these results in PLOS ONE.
For this study, the researchers developed 2 online education modules about the importance of pharmacologic VTE prevention and tactics for better communicating its importance to patients.
One of the modules was “dynamic,” requiring nurses to select responses to clinical scenarios, such as how to respond to a patient who was refusing a prophylactic medication dose. The other module was “static,” involving a PowerPoint slide show with a traditional voice-over explaining the information.
The study included 933 permanently employed nurses on 21 medical or surgical floors at The Johns Hopkins Hospital.
Between April 1, 2014, and March 31, 2015, 445 nurses on 11 of the floors were randomized to the dynamic education arm of the study, and 488 nurses on 10 floors were enrolled in the static arm.
To track non-administration of VTE prophylaxis, the researchers retrieved data from the hospital’s electronic health record system. The team collected data for 1 year and divided it into 3 time periods: baseline, during the educational intervention, and post-education.
Over the entire study period, 214,478 doses of pharmacologic VTE prophylaxis were prescribed to patients on the 21 hospital floors.
After education, non-administration of prescribed VTE prophylaxis decreased from 12.4% to 11.1% (conditional odds ratio [cOR]=0.87, P=0.002).
Nurses who completed the dynamic education module saw a greater reduction in non-administration—from 10.8% to 9.2% (cOR=0.83)—than nurses who completed the static education module—14.5% to 13.5% (cOR=0.92). However, the difference between the study arms was not significant (P=0.26).
“Our study adds to evidence that the way something is taught to professionals has a great influence on whether they retain information and apply it,” said Brandyn Lau, of The Johns Hopkins University School of Medicine.
“Active learning seems to get better results than passive learning, showing that it’s not just what you teach, but also how you teach it.”
“Now that we’ve shown the modules can be effective in improving practice, we want to make [them] available to the more than 3 million nurses practicing in the US,” Dr Haut added. ![]()
Online education programs for nurses can improve the administration of prophylaxis for venous thromboembolism (VTE), a new study suggests.
The research was spurred by a documented need to boost the administration of prescribed VTE prophylaxis in hospitalized patients.
Data had shown that patients’ refusal of VTE prophylaxis frequently resulted in nurses not administering the prescribed therapy.
The new research indicates that online education modules helped nurses communicate to patients the need for VTE prophylaxis and therefore improved rates of use.
“We teach in hopes of improving patient care, but there’s actually very little evidence that online professional education can have a measurable impact. Our results show that it does,” said Elliott Haut, MD, PhD, of The Johns Hopkins University School of Medicine in Baltimore, Maryland.
Dr Haut and his colleagues reported these results in PLOS ONE.
For this study, the researchers developed 2 online education modules about the importance of pharmacologic VTE prevention and tactics for better communicating its importance to patients.
One of the modules was “dynamic,” requiring nurses to select responses to clinical scenarios, such as how to respond to a patient who was refusing a prophylactic medication dose. The other module was “static,” involving a PowerPoint slide show with a traditional voice-over explaining the information.
The study included 933 permanently employed nurses on 21 medical or surgical floors at The Johns Hopkins Hospital.
Between April 1, 2014, and March 31, 2015, 445 nurses on 11 of the floors were randomized to the dynamic education arm of the study, and 488 nurses on 10 floors were enrolled in the static arm.
To track non-administration of VTE prophylaxis, the researchers retrieved data from the hospital’s electronic health record system. The team collected data for 1 year and divided it into 3 time periods: baseline, during the educational intervention, and post-education.
Over the entire study period, 214,478 doses of pharmacologic VTE prophylaxis were prescribed to patients on the 21 hospital floors.
After education, non-administration of prescribed VTE prophylaxis decreased from 12.4% to 11.1% (conditional odds ratio [cOR]=0.87, P=0.002).
Nurses who completed the dynamic education module saw a greater reduction in non-administration—from 10.8% to 9.2% (cOR=0.83)—than nurses who completed the static education module—14.5% to 13.5% (cOR=0.92). However, the difference between the study arms was not significant (P=0.26).
“Our study adds to evidence that the way something is taught to professionals has a great influence on whether they retain information and apply it,” said Brandyn Lau, of The Johns Hopkins University School of Medicine.
“Active learning seems to get better results than passive learning, showing that it’s not just what you teach, but also how you teach it.”
“Now that we’ve shown the modules can be effective in improving practice, we want to make [them] available to the more than 3 million nurses practicing in the US,” Dr Haut added. ![]()
Online education programs for nurses can improve the administration of prophylaxis for venous thromboembolism (VTE), a new study suggests.
The research was spurred by a documented need to boost the administration of prescribed VTE prophylaxis in hospitalized patients.
Data had shown that patients’ refusal of VTE prophylaxis frequently resulted in nurses not administering the prescribed therapy.
The new research indicates that online education modules helped nurses communicate to patients the need for VTE prophylaxis and therefore improved rates of use.
“We teach in hopes of improving patient care, but there’s actually very little evidence that online professional education can have a measurable impact. Our results show that it does,” said Elliott Haut, MD, PhD, of The Johns Hopkins University School of Medicine in Baltimore, Maryland.
Dr Haut and his colleagues reported these results in PLOS ONE.
For this study, the researchers developed 2 online education modules about the importance of pharmacologic VTE prevention and tactics for better communicating its importance to patients.
One of the modules was “dynamic,” requiring nurses to select responses to clinical scenarios, such as how to respond to a patient who was refusing a prophylactic medication dose. The other module was “static,” involving a PowerPoint slide show with a traditional voice-over explaining the information.
The study included 933 permanently employed nurses on 21 medical or surgical floors at The Johns Hopkins Hospital.
Between April 1, 2014, and March 31, 2015, 445 nurses on 11 of the floors were randomized to the dynamic education arm of the study, and 488 nurses on 10 floors were enrolled in the static arm.
To track non-administration of VTE prophylaxis, the researchers retrieved data from the hospital’s electronic health record system. The team collected data for 1 year and divided it into 3 time periods: baseline, during the educational intervention, and post-education.
Over the entire study period, 214,478 doses of pharmacologic VTE prophylaxis were prescribed to patients on the 21 hospital floors.
After education, non-administration of prescribed VTE prophylaxis decreased from 12.4% to 11.1% (conditional odds ratio [cOR]=0.87, P=0.002).
Nurses who completed the dynamic education module saw a greater reduction in non-administration—from 10.8% to 9.2% (cOR=0.83)—than nurses who completed the static education module—14.5% to 13.5% (cOR=0.92). However, the difference between the study arms was not significant (P=0.26).
“Our study adds to evidence that the way something is taught to professionals has a great influence on whether they retain information and apply it,” said Brandyn Lau, of The Johns Hopkins University School of Medicine.
“Active learning seems to get better results than passive learning, showing that it’s not just what you teach, but also how you teach it.”
“Now that we’ve shown the modules can be effective in improving practice, we want to make [them] available to the more than 3 million nurses practicing in the US,” Dr Haut added. ![]()
Drug granted priority review for CTCL
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) seeking approval for brentuximab vedotin (Adcetris) as a treatment for cutaneous T-cell lymphoma (CTCL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sBLA for brentuximab vedotin by December 16, 2017.
The sBLA is supported by data from the phase 3 ALCANZA trial and a pair of phase 2 investigator-sponsored trials.
About brentuximab vedotin
Brentuximab vedotin is an antibody-drug conjugate directed to CD30, which is expressed on skin lesions in approximately 50% of patients with CTCL. The drug is being developed by Seattle Genetics and Takeda Pharmaceutical Company Limited.
Brentuximab vedotin is currently FDA-approved for 3 indications.
The drug is approved to treat patients with classical Hodgkin lymphoma after failure of autologous hematopoietic stem cell transplant (auto-HSCT) or after failure of at least 2 prior multi-agent chemotherapy regimens in patients who are not auto-HSCT candidates. Brentuximab vedotin initially had accelerated approval for this indication, but it was later converted to full approval.
Brentuximab vedotin also has full approval as consolidation for patients with classical Hodgkin lymphoma who have a high risk of relapse or progression after auto-HSCT.
And the drug has accelerated approval for the treatment of patients with systemic anaplastic large-cell lymphoma (sALCL) after failure of at least 1 prior multi-agent chemotherapy regimen. This accelerated approval is based on overall response rate. Continued approval for the sALCL indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Brentuximab vedotin previously received breakthrough therapy designation from the FDA for the treatment of patients with CD30-expressing mycosis fungoides (MF) and patients with primary cutaneous ALCL who require systemic therapy and have received 1 prior systemic therapy.
Brentuximab vedotin also has orphan drug designation from the FDA for the treatment of MF. ![]()
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) seeking approval for brentuximab vedotin (Adcetris) as a treatment for cutaneous T-cell lymphoma (CTCL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sBLA for brentuximab vedotin by December 16, 2017.
The sBLA is supported by data from the phase 3 ALCANZA trial and a pair of phase 2 investigator-sponsored trials.
About brentuximab vedotin
Brentuximab vedotin is an antibody-drug conjugate directed to CD30, which is expressed on skin lesions in approximately 50% of patients with CTCL. The drug is being developed by Seattle Genetics and Takeda Pharmaceutical Company Limited.
Brentuximab vedotin is currently FDA-approved for 3 indications.
The drug is approved to treat patients with classical Hodgkin lymphoma after failure of autologous hematopoietic stem cell transplant (auto-HSCT) or after failure of at least 2 prior multi-agent chemotherapy regimens in patients who are not auto-HSCT candidates. Brentuximab vedotin initially had accelerated approval for this indication, but it was later converted to full approval.
Brentuximab vedotin also has full approval as consolidation for patients with classical Hodgkin lymphoma who have a high risk of relapse or progression after auto-HSCT.
And the drug has accelerated approval for the treatment of patients with systemic anaplastic large-cell lymphoma (sALCL) after failure of at least 1 prior multi-agent chemotherapy regimen. This accelerated approval is based on overall response rate. Continued approval for the sALCL indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Brentuximab vedotin previously received breakthrough therapy designation from the FDA for the treatment of patients with CD30-expressing mycosis fungoides (MF) and patients with primary cutaneous ALCL who require systemic therapy and have received 1 prior systemic therapy.
Brentuximab vedotin also has orphan drug designation from the FDA for the treatment of MF. ![]()
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) seeking approval for brentuximab vedotin (Adcetris) as a treatment for cutaneous T-cell lymphoma (CTCL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sBLA for brentuximab vedotin by December 16, 2017.
The sBLA is supported by data from the phase 3 ALCANZA trial and a pair of phase 2 investigator-sponsored trials.
About brentuximab vedotin
Brentuximab vedotin is an antibody-drug conjugate directed to CD30, which is expressed on skin lesions in approximately 50% of patients with CTCL. The drug is being developed by Seattle Genetics and Takeda Pharmaceutical Company Limited.
Brentuximab vedotin is currently FDA-approved for 3 indications.
The drug is approved to treat patients with classical Hodgkin lymphoma after failure of autologous hematopoietic stem cell transplant (auto-HSCT) or after failure of at least 2 prior multi-agent chemotherapy regimens in patients who are not auto-HSCT candidates. Brentuximab vedotin initially had accelerated approval for this indication, but it was later converted to full approval.
Brentuximab vedotin also has full approval as consolidation for patients with classical Hodgkin lymphoma who have a high risk of relapse or progression after auto-HSCT.
And the drug has accelerated approval for the treatment of patients with systemic anaplastic large-cell lymphoma (sALCL) after failure of at least 1 prior multi-agent chemotherapy regimen. This accelerated approval is based on overall response rate. Continued approval for the sALCL indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Brentuximab vedotin previously received breakthrough therapy designation from the FDA for the treatment of patients with CD30-expressing mycosis fungoides (MF) and patients with primary cutaneous ALCL who require systemic therapy and have received 1 prior systemic therapy.
Brentuximab vedotin also has orphan drug designation from the FDA for the treatment of MF. ![]()
Thrombotic events prompt device recall
The US Food and Drug Administration (FDA) has announced that Cook Medical Inc. is recalling the Zenith Alpha Thoracic Endovascular Graft.
The company found that when the device is used for the treatment of blunt traumatic aortic injury (BTAI), thrombi can form and the device can become occluded. This can lead to serious adverse events, including death.
There have been 5 reports of thrombosis/occlusion with this product, all in patients treated for BTAI. In 1 case, a patient died.
Therefore, Cook Medical Inc. is recalling all lots of the Zenith Alpha Thoracic Endovascular Graft that were manufactured from April 10, 2015, to January 3, 2017, and distributed from October 29, 2015, to March 10, 2017.
On March 22, 2017, Cook Medical Inc. sent an “Urgent: Medical Device Correction and Removal” notification to all affected customers.
This recall notification included a description of the problem and reason for the recall, list of affected products, and customer actions to be taken in response to the recall notification.
On June 22, 2017, the company sent an updated notification to all affected customers.
This recall notification informed customers that the instructions for use (IFU) for the Zenith Alpha Thoracic Endovascular Graft were updated to remove the indication for BTAI.
Because of the IFU correction to remove BTAI from the indication, it is necessary to remove specific sizes of this device (grafts with a proximal or distal diameter of 18-22 mm) that would likely be used only for BTAI.
About 500 of these devices (18 to 22 mm) will be removed, and roughly 4500 will be relabeled. A Cook Medical sales representative will follow-up with affected customers and provide a corrected IFU.
The company recommends that patients already treated with the Zenith Thoracic Endovascular Graft for the BTAI indication be followed according the current IFU and with considerations outlined in Cook Medical’s March 22, 2017, medical device correction notification.
Customers with questions about this recall may contact Cook Medical Customer Relations at 800-457-4500 or 812-339-2235.
Healthcare professionals and patients are encouraged to report adverse events related to the Zenith Thoracic Endovascular Graft to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program. ![]()
The US Food and Drug Administration (FDA) has announced that Cook Medical Inc. is recalling the Zenith Alpha Thoracic Endovascular Graft.
The company found that when the device is used for the treatment of blunt traumatic aortic injury (BTAI), thrombi can form and the device can become occluded. This can lead to serious adverse events, including death.
There have been 5 reports of thrombosis/occlusion with this product, all in patients treated for BTAI. In 1 case, a patient died.
Therefore, Cook Medical Inc. is recalling all lots of the Zenith Alpha Thoracic Endovascular Graft that were manufactured from April 10, 2015, to January 3, 2017, and distributed from October 29, 2015, to March 10, 2017.
On March 22, 2017, Cook Medical Inc. sent an “Urgent: Medical Device Correction and Removal” notification to all affected customers.
This recall notification included a description of the problem and reason for the recall, list of affected products, and customer actions to be taken in response to the recall notification.
On June 22, 2017, the company sent an updated notification to all affected customers.
This recall notification informed customers that the instructions for use (IFU) for the Zenith Alpha Thoracic Endovascular Graft were updated to remove the indication for BTAI.
Because of the IFU correction to remove BTAI from the indication, it is necessary to remove specific sizes of this device (grafts with a proximal or distal diameter of 18-22 mm) that would likely be used only for BTAI.
About 500 of these devices (18 to 22 mm) will be removed, and roughly 4500 will be relabeled. A Cook Medical sales representative will follow-up with affected customers and provide a corrected IFU.
The company recommends that patients already treated with the Zenith Thoracic Endovascular Graft for the BTAI indication be followed according the current IFU and with considerations outlined in Cook Medical’s March 22, 2017, medical device correction notification.
Customers with questions about this recall may contact Cook Medical Customer Relations at 800-457-4500 or 812-339-2235.
Healthcare professionals and patients are encouraged to report adverse events related to the Zenith Thoracic Endovascular Graft to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program. ![]()
The US Food and Drug Administration (FDA) has announced that Cook Medical Inc. is recalling the Zenith Alpha Thoracic Endovascular Graft.
The company found that when the device is used for the treatment of blunt traumatic aortic injury (BTAI), thrombi can form and the device can become occluded. This can lead to serious adverse events, including death.
There have been 5 reports of thrombosis/occlusion with this product, all in patients treated for BTAI. In 1 case, a patient died.
Therefore, Cook Medical Inc. is recalling all lots of the Zenith Alpha Thoracic Endovascular Graft that were manufactured from April 10, 2015, to January 3, 2017, and distributed from October 29, 2015, to March 10, 2017.
On March 22, 2017, Cook Medical Inc. sent an “Urgent: Medical Device Correction and Removal” notification to all affected customers.
This recall notification included a description of the problem and reason for the recall, list of affected products, and customer actions to be taken in response to the recall notification.
On June 22, 2017, the company sent an updated notification to all affected customers.
This recall notification informed customers that the instructions for use (IFU) for the Zenith Alpha Thoracic Endovascular Graft were updated to remove the indication for BTAI.
Because of the IFU correction to remove BTAI from the indication, it is necessary to remove specific sizes of this device (grafts with a proximal or distal diameter of 18-22 mm) that would likely be used only for BTAI.
About 500 of these devices (18 to 22 mm) will be removed, and roughly 4500 will be relabeled. A Cook Medical sales representative will follow-up with affected customers and provide a corrected IFU.
The company recommends that patients already treated with the Zenith Thoracic Endovascular Graft for the BTAI indication be followed according the current IFU and with considerations outlined in Cook Medical’s March 22, 2017, medical device correction notification.
Customers with questions about this recall may contact Cook Medical Customer Relations at 800-457-4500 or 812-339-2235.
Healthcare professionals and patients are encouraged to report adverse events related to the Zenith Thoracic Endovascular Graft to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program. ![]()
Lenalidomide maintenance prolongs PFS, OS in MM
Lenalidomide maintenance can be considered a standard of care for multiple myeloma (MM) patients who have undergone hematopoietic stem cell transplant (HSCT), according to researchers.
A meta-analysis of data from 3 trials showed that lenalidomide maintenance extended both progression-free survival (PFS) and overall survival (OS) in these patients.
Philip L. McCarthy, MD, of Roswell Park Cancer Institute in Buffalo, New York, and his colleagues reported results of the analysis in the Journal of Clinical Oncology.
The researchers analyzed data from 3 large, randomized trials conducted in the US, France, and Italy. The studies included patients with newly diagnosed MM who underwent autologous HSCT and then received continuous lenalidomide (n=605) or no maintenance/placebo (n=603).
Patient demographics and disease-related characteristics were generally balanced between the treatment groups.
The mean duration of maintenance was 28 months (range, 0-108) in the lenalidomide group and 22 months (range, 0-86) in the control group.
Fewer patients in the lenalidomide group (52.6%) started second-line anti-MM therapy than patients in the control group (70.8%). And the time to second-line anti-MM treatment was longer with lenalidomide than with control (hazard ratio [HR]=0.57; 95% CI, 0.49 to 0.66).
PFS and OS
Patients who received lenalidomide maintenance had significantly longer PFS and OS than patients in the control group.
The median PFS was 52.8 months and 23.5 months, respectively (HR=0.48; 95% CI, 0.41 to 0.55).
The median OS was not reached in the lenalidomide group and was 86.0 months in the control group (HR=0.75; 95% CI, 0.63 to 0.90; P=0.001),
At a median follow-up of 79.5 months, the OS rate was 64% in the lenalidomide group and 54% in the control group. The 7-year OS rates were 62% and 50%, respectively.
Safety
Safety data were not available for the Italian study. In the other 2 studies, 29.1% of patients in the lenalidomide group had treatment-emergent adverse events that led to discontinuation, as did 12.2% of patients in the control group.
Treatment-emergent adverse events leading to treatment discontinuation (in the lenalidomide and control groups, respectively) included neutropenia (2.3% vs 0.2%), thrombocytopenia (1.7% vs 1.1%), general disorders and administration site conditions (4.7% vs 1.5%), neoplasms (4.3% vs 1.0%), skin and subcutaneous tissue disorders (3.4% vs 1.9%), nervous system disorders (3.4% vs 1.7%), gastrointestinal disorders (3.4% vs 0.2%), infections and infestations (1.7% vs 0.8%), and musculoskeletal and connective tissue disorders (1.1% and 1.3%).
There was a higher frequency of second primary malignancies (SPMs) in the lenalidomide group than in the control group.
The incidence of hematologic SPMs occurring before disease progression was 5.3% and 0.8%, respectively. The incidence before and after progression was 6.1% and 2.8%, respectively.
The incidence of solid tumor SPMs occurring before disease progression was 5.8% and 2.0%, respectively. The incidence before and after progression was 7.3% and 4.2%, respectively.
“With this complete and mature data from 3 large, multinational studies, we now have clear evidence that ongoing treatment with lenalidomide can prevent disease progression and extend survival in patients with multiple myeloma who’ve received a stem cell transplant,” Dr McCarthy said.
“All the investigators wish to express enormous gratitude to the patients who took part in these trials. Many others will benefit from their role in this research.” ![]()
Lenalidomide maintenance can be considered a standard of care for multiple myeloma (MM) patients who have undergone hematopoietic stem cell transplant (HSCT), according to researchers.
A meta-analysis of data from 3 trials showed that lenalidomide maintenance extended both progression-free survival (PFS) and overall survival (OS) in these patients.
Philip L. McCarthy, MD, of Roswell Park Cancer Institute in Buffalo, New York, and his colleagues reported results of the analysis in the Journal of Clinical Oncology.
The researchers analyzed data from 3 large, randomized trials conducted in the US, France, and Italy. The studies included patients with newly diagnosed MM who underwent autologous HSCT and then received continuous lenalidomide (n=605) or no maintenance/placebo (n=603).
Patient demographics and disease-related characteristics were generally balanced between the treatment groups.
The mean duration of maintenance was 28 months (range, 0-108) in the lenalidomide group and 22 months (range, 0-86) in the control group.
Fewer patients in the lenalidomide group (52.6%) started second-line anti-MM therapy than patients in the control group (70.8%). And the time to second-line anti-MM treatment was longer with lenalidomide than with control (hazard ratio [HR]=0.57; 95% CI, 0.49 to 0.66).
PFS and OS
Patients who received lenalidomide maintenance had significantly longer PFS and OS than patients in the control group.
The median PFS was 52.8 months and 23.5 months, respectively (HR=0.48; 95% CI, 0.41 to 0.55).
The median OS was not reached in the lenalidomide group and was 86.0 months in the control group (HR=0.75; 95% CI, 0.63 to 0.90; P=0.001),
At a median follow-up of 79.5 months, the OS rate was 64% in the lenalidomide group and 54% in the control group. The 7-year OS rates were 62% and 50%, respectively.
Safety
Safety data were not available for the Italian study. In the other 2 studies, 29.1% of patients in the lenalidomide group had treatment-emergent adverse events that led to discontinuation, as did 12.2% of patients in the control group.
Treatment-emergent adverse events leading to treatment discontinuation (in the lenalidomide and control groups, respectively) included neutropenia (2.3% vs 0.2%), thrombocytopenia (1.7% vs 1.1%), general disorders and administration site conditions (4.7% vs 1.5%), neoplasms (4.3% vs 1.0%), skin and subcutaneous tissue disorders (3.4% vs 1.9%), nervous system disorders (3.4% vs 1.7%), gastrointestinal disorders (3.4% vs 0.2%), infections and infestations (1.7% vs 0.8%), and musculoskeletal and connective tissue disorders (1.1% and 1.3%).
There was a higher frequency of second primary malignancies (SPMs) in the lenalidomide group than in the control group.
The incidence of hematologic SPMs occurring before disease progression was 5.3% and 0.8%, respectively. The incidence before and after progression was 6.1% and 2.8%, respectively.
The incidence of solid tumor SPMs occurring before disease progression was 5.8% and 2.0%, respectively. The incidence before and after progression was 7.3% and 4.2%, respectively.
“With this complete and mature data from 3 large, multinational studies, we now have clear evidence that ongoing treatment with lenalidomide can prevent disease progression and extend survival in patients with multiple myeloma who’ve received a stem cell transplant,” Dr McCarthy said.
“All the investigators wish to express enormous gratitude to the patients who took part in these trials. Many others will benefit from their role in this research.” ![]()
Lenalidomide maintenance can be considered a standard of care for multiple myeloma (MM) patients who have undergone hematopoietic stem cell transplant (HSCT), according to researchers.
A meta-analysis of data from 3 trials showed that lenalidomide maintenance extended both progression-free survival (PFS) and overall survival (OS) in these patients.
Philip L. McCarthy, MD, of Roswell Park Cancer Institute in Buffalo, New York, and his colleagues reported results of the analysis in the Journal of Clinical Oncology.
The researchers analyzed data from 3 large, randomized trials conducted in the US, France, and Italy. The studies included patients with newly diagnosed MM who underwent autologous HSCT and then received continuous lenalidomide (n=605) or no maintenance/placebo (n=603).
Patient demographics and disease-related characteristics were generally balanced between the treatment groups.
The mean duration of maintenance was 28 months (range, 0-108) in the lenalidomide group and 22 months (range, 0-86) in the control group.
Fewer patients in the lenalidomide group (52.6%) started second-line anti-MM therapy than patients in the control group (70.8%). And the time to second-line anti-MM treatment was longer with lenalidomide than with control (hazard ratio [HR]=0.57; 95% CI, 0.49 to 0.66).
PFS and OS
Patients who received lenalidomide maintenance had significantly longer PFS and OS than patients in the control group.
The median PFS was 52.8 months and 23.5 months, respectively (HR=0.48; 95% CI, 0.41 to 0.55).
The median OS was not reached in the lenalidomide group and was 86.0 months in the control group (HR=0.75; 95% CI, 0.63 to 0.90; P=0.001),
At a median follow-up of 79.5 months, the OS rate was 64% in the lenalidomide group and 54% in the control group. The 7-year OS rates were 62% and 50%, respectively.
Safety
Safety data were not available for the Italian study. In the other 2 studies, 29.1% of patients in the lenalidomide group had treatment-emergent adverse events that led to discontinuation, as did 12.2% of patients in the control group.
Treatment-emergent adverse events leading to treatment discontinuation (in the lenalidomide and control groups, respectively) included neutropenia (2.3% vs 0.2%), thrombocytopenia (1.7% vs 1.1%), general disorders and administration site conditions (4.7% vs 1.5%), neoplasms (4.3% vs 1.0%), skin and subcutaneous tissue disorders (3.4% vs 1.9%), nervous system disorders (3.4% vs 1.7%), gastrointestinal disorders (3.4% vs 0.2%), infections and infestations (1.7% vs 0.8%), and musculoskeletal and connective tissue disorders (1.1% and 1.3%).
There was a higher frequency of second primary malignancies (SPMs) in the lenalidomide group than in the control group.
The incidence of hematologic SPMs occurring before disease progression was 5.3% and 0.8%, respectively. The incidence before and after progression was 6.1% and 2.8%, respectively.
The incidence of solid tumor SPMs occurring before disease progression was 5.8% and 2.0%, respectively. The incidence before and after progression was 7.3% and 4.2%, respectively.
“With this complete and mature data from 3 large, multinational studies, we now have clear evidence that ongoing treatment with lenalidomide can prevent disease progression and extend survival in patients with multiple myeloma who’ve received a stem cell transplant,” Dr McCarthy said.
“All the investigators wish to express enormous gratitude to the patients who took part in these trials. Many others will benefit from their role in this research.” ![]()
Post-approval trials for accelerated drugs fall short
New research has revealed shortcomings of post-approval studies for drugs granted accelerated approval in the US.
Researchers found that, for drugs granted accelerated approval from 2009 to 2013, both pre-approval and post-approval trials had limitations in their design and the endpoints used.
“One might expect accelerated approval confirmatory trials to be much more rigorous than the pre-approval trials,” said study author Aaron S. Kesselheim, MD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“But we found that there were few differences in these key design features of the trials conducted before or after approval.”
Dr Kesselheim and his colleagues reported these findings in JAMA.
The researchers examined pre- and post-approval clinical trials of drugs granted accelerated approval by the US Food and Drug Administration (FDA) between 2009 and 2013.
During that time, the FDA granted 22 drugs accelerated approval for 24 indications (15 of them for hematologic disorders).
Fourteen of the indications were approved on the basis of single-intervention-group studies that enrolled a median of 132 patients.
The FDA ordered 38 post-approval studies to confirm the safety and efficacy of the drugs.
Three years after the last drug’s approval, half of those studies (n=19) were not complete. Eight (42%) of the incomplete studies were either terminated or delayed by more than 1 year.
For 14 of the 24 indications (58%), results from the post-approval studies were not available after a median of 5 years of follow-up.
Study comparison
Published reports were available for 18 of the 19 completed post-approval studies. The characteristics of these studies did not differ much from the 30 pre-approval studies.
There were no statistically significant differences with regard to median patient enrollment (P=0.17), the use of randomized (P=0.31) or double-blind trials (P=0.17), the use of placebo as a comparator (P=0.17), or the lack of a comparator (P=0.21).
However, there was a significant difference in the use of an active comparator (P=0.02), with more post-approval studies using an active comparator.
The researchers also found that 17 of the 18 post-approval trials still used surrogate measures of effect as primary endpoints.
There was no significant difference between pre- and post-approval trials when it came to the use of disease response (P=0.17) or most other surrogate measures (P=0.21) as the trials’ primary endpoint.
The same was true for overall survival (P=0.20), although significantly more post-approval studies used progression-free survival (P=0.001) as a primary endpoint.
“It is important to use clinical endpoints in testing investigational drugs whenever possible because there are numerous cases of drugs approved on the basis of a surrogate measure that turn out to later not effect actual clinical outcomes—or even make them worse,” Dr Kesselheim said.
To address these issues and improve the quality of confirmatory studies, Dr Kesselheim suggested the FDA clearly describe the limitations in the pre-approval data that will need to be addressed in post-approval studies.
He also suggested the agency work with manufacturers to ensure that post-approval studies are conducted using design features that will be optimally useful for confirming the efficacy of the drug. ![]()
New research has revealed shortcomings of post-approval studies for drugs granted accelerated approval in the US.
Researchers found that, for drugs granted accelerated approval from 2009 to 2013, both pre-approval and post-approval trials had limitations in their design and the endpoints used.
“One might expect accelerated approval confirmatory trials to be much more rigorous than the pre-approval trials,” said study author Aaron S. Kesselheim, MD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“But we found that there were few differences in these key design features of the trials conducted before or after approval.”
Dr Kesselheim and his colleagues reported these findings in JAMA.
The researchers examined pre- and post-approval clinical trials of drugs granted accelerated approval by the US Food and Drug Administration (FDA) between 2009 and 2013.
During that time, the FDA granted 22 drugs accelerated approval for 24 indications (15 of them for hematologic disorders).
Fourteen of the indications were approved on the basis of single-intervention-group studies that enrolled a median of 132 patients.
The FDA ordered 38 post-approval studies to confirm the safety and efficacy of the drugs.
Three years after the last drug’s approval, half of those studies (n=19) were not complete. Eight (42%) of the incomplete studies were either terminated or delayed by more than 1 year.
For 14 of the 24 indications (58%), results from the post-approval studies were not available after a median of 5 years of follow-up.
Study comparison
Published reports were available for 18 of the 19 completed post-approval studies. The characteristics of these studies did not differ much from the 30 pre-approval studies.
There were no statistically significant differences with regard to median patient enrollment (P=0.17), the use of randomized (P=0.31) or double-blind trials (P=0.17), the use of placebo as a comparator (P=0.17), or the lack of a comparator (P=0.21).
However, there was a significant difference in the use of an active comparator (P=0.02), with more post-approval studies using an active comparator.
The researchers also found that 17 of the 18 post-approval trials still used surrogate measures of effect as primary endpoints.
There was no significant difference between pre- and post-approval trials when it came to the use of disease response (P=0.17) or most other surrogate measures (P=0.21) as the trials’ primary endpoint.
The same was true for overall survival (P=0.20), although significantly more post-approval studies used progression-free survival (P=0.001) as a primary endpoint.
“It is important to use clinical endpoints in testing investigational drugs whenever possible because there are numerous cases of drugs approved on the basis of a surrogate measure that turn out to later not effect actual clinical outcomes—or even make them worse,” Dr Kesselheim said.
To address these issues and improve the quality of confirmatory studies, Dr Kesselheim suggested the FDA clearly describe the limitations in the pre-approval data that will need to be addressed in post-approval studies.
He also suggested the agency work with manufacturers to ensure that post-approval studies are conducted using design features that will be optimally useful for confirming the efficacy of the drug. ![]()
New research has revealed shortcomings of post-approval studies for drugs granted accelerated approval in the US.
Researchers found that, for drugs granted accelerated approval from 2009 to 2013, both pre-approval and post-approval trials had limitations in their design and the endpoints used.
“One might expect accelerated approval confirmatory trials to be much more rigorous than the pre-approval trials,” said study author Aaron S. Kesselheim, MD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“But we found that there were few differences in these key design features of the trials conducted before or after approval.”
Dr Kesselheim and his colleagues reported these findings in JAMA.
The researchers examined pre- and post-approval clinical trials of drugs granted accelerated approval by the US Food and Drug Administration (FDA) between 2009 and 2013.
During that time, the FDA granted 22 drugs accelerated approval for 24 indications (15 of them for hematologic disorders).
Fourteen of the indications were approved on the basis of single-intervention-group studies that enrolled a median of 132 patients.
The FDA ordered 38 post-approval studies to confirm the safety and efficacy of the drugs.
Three years after the last drug’s approval, half of those studies (n=19) were not complete. Eight (42%) of the incomplete studies were either terminated or delayed by more than 1 year.
For 14 of the 24 indications (58%), results from the post-approval studies were not available after a median of 5 years of follow-up.
Study comparison
Published reports were available for 18 of the 19 completed post-approval studies. The characteristics of these studies did not differ much from the 30 pre-approval studies.
There were no statistically significant differences with regard to median patient enrollment (P=0.17), the use of randomized (P=0.31) or double-blind trials (P=0.17), the use of placebo as a comparator (P=0.17), or the lack of a comparator (P=0.21).
However, there was a significant difference in the use of an active comparator (P=0.02), with more post-approval studies using an active comparator.
The researchers also found that 17 of the 18 post-approval trials still used surrogate measures of effect as primary endpoints.
There was no significant difference between pre- and post-approval trials when it came to the use of disease response (P=0.17) or most other surrogate measures (P=0.21) as the trials’ primary endpoint.
The same was true for overall survival (P=0.20), although significantly more post-approval studies used progression-free survival (P=0.001) as a primary endpoint.
“It is important to use clinical endpoints in testing investigational drugs whenever possible because there are numerous cases of drugs approved on the basis of a surrogate measure that turn out to later not effect actual clinical outcomes—or even make them worse,” Dr Kesselheim said.
To address these issues and improve the quality of confirmatory studies, Dr Kesselheim suggested the FDA clearly describe the limitations in the pre-approval data that will need to be addressed in post-approval studies.
He also suggested the agency work with manufacturers to ensure that post-approval studies are conducted using design features that will be optimally useful for confirming the efficacy of the drug. ![]()
FDA grants drug orphan designation for AML, CMML
The US Food and Drug Administration (FDA) has granted orphan drug designation to H3B-8800 as a treatment for patients with acute myelogenous leukemia (AML) or chronic myelomonocytic leukemia (CMML).
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
About H3B-8800
H3B-8800 is an orally bioavailable small-molecule modulator of wild-type and mutant SF3b complexes. The SF3b complex is a key component of the spliceosome that is found in the cell nucleus and is responsible for the removal of noncoding introns from a transcribed pre-messenger RNA.
Recurrent heterozygous mutations in several core members of the spliceosome (SF3B1, U2AF1, SRSF2, and ZRSR2) have been identified in solid tumor and hematologic malignancies. Mutations in the core spliceosome components lead to aberrant mRNA splicing that may contribute to disease pathogenesis.
Preclinical data have suggested that H3B-8800 modulates RNA splicing and shows preferential antitumor activity in spliceosome-mutant cancer models, including models of AML and CMML. H3B-8800 showed dose-dependent modulation of canonical and aberrant splicing when administered at tolerated doses.
Results from this research were presented at the 2017 AACR Annual Meeting (abstract 1185).
H3B-8800 is currently under investigation in a phase 1 trial of patients with AML, CMML, and myelodysplastic syndromes that may carry mutations in the core spliceosome genes.
H3B-8800 is being developed by H3 Biomedicine Inc. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to H3B-8800 as a treatment for patients with acute myelogenous leukemia (AML) or chronic myelomonocytic leukemia (CMML).
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
About H3B-8800
H3B-8800 is an orally bioavailable small-molecule modulator of wild-type and mutant SF3b complexes. The SF3b complex is a key component of the spliceosome that is found in the cell nucleus and is responsible for the removal of noncoding introns from a transcribed pre-messenger RNA.
Recurrent heterozygous mutations in several core members of the spliceosome (SF3B1, U2AF1, SRSF2, and ZRSR2) have been identified in solid tumor and hematologic malignancies. Mutations in the core spliceosome components lead to aberrant mRNA splicing that may contribute to disease pathogenesis.
Preclinical data have suggested that H3B-8800 modulates RNA splicing and shows preferential antitumor activity in spliceosome-mutant cancer models, including models of AML and CMML. H3B-8800 showed dose-dependent modulation of canonical and aberrant splicing when administered at tolerated doses.
Results from this research were presented at the 2017 AACR Annual Meeting (abstract 1185).
H3B-8800 is currently under investigation in a phase 1 trial of patients with AML, CMML, and myelodysplastic syndromes that may carry mutations in the core spliceosome genes.
H3B-8800 is being developed by H3 Biomedicine Inc. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to H3B-8800 as a treatment for patients with acute myelogenous leukemia (AML) or chronic myelomonocytic leukemia (CMML).
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
About H3B-8800
H3B-8800 is an orally bioavailable small-molecule modulator of wild-type and mutant SF3b complexes. The SF3b complex is a key component of the spliceosome that is found in the cell nucleus and is responsible for the removal of noncoding introns from a transcribed pre-messenger RNA.
Recurrent heterozygous mutations in several core members of the spliceosome (SF3B1, U2AF1, SRSF2, and ZRSR2) have been identified in solid tumor and hematologic malignancies. Mutations in the core spliceosome components lead to aberrant mRNA splicing that may contribute to disease pathogenesis.
Preclinical data have suggested that H3B-8800 modulates RNA splicing and shows preferential antitumor activity in spliceosome-mutant cancer models, including models of AML and CMML. H3B-8800 showed dose-dependent modulation of canonical and aberrant splicing when administered at tolerated doses.
Results from this research were presented at the 2017 AACR Annual Meeting (abstract 1185).
H3B-8800 is currently under investigation in a phase 1 trial of patients with AML, CMML, and myelodysplastic syndromes that may carry mutations in the core spliceosome genes.
H3B-8800 is being developed by H3 Biomedicine Inc. ![]()
FDA allows emergency use of multiplex Zika test
The US Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) for the CII-ArboViroPlex rRT-PCR Test.
It is the first multiplex assay that simultaneously tests for the presence of Zika virus, all serotypes of dengue virus, chikungunya virus, and West Nile virus, as well as a host gene that ensures the accuracy of results.
The EUA does not mean the CII-ArboViroPlex rRT-PCR Test is FDA cleared or approved.
An EUA allows for the use of unapproved medical products in an emergency. The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
The EUA for the CII-ArboViroPlex rRT-PCR Test means the test is only authorized as long as circumstances exist to justify the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner.
About the test
The CII-ArboViroPlex rRT-PCR Test is an assay that detects viral RNA matching Zika virus (ZIKV), dengue virus types 1-4 (DENV), chikungunya virus (CHIKV), and West Nile virus (WNV) with a human housekeeping gene, viral RNA controls, and extraction controls that ensure the integrity of the test from nucleic extraction to the final result.
Named for the 4 arboviruses it targets and the real-time reverse transcription polymerase chain reaction (rRT-PCR) technique it employs, the test can simultaneously detect ZIKV, DENV, CHIKV, and WNV in up to 88 samples of blood in less than 2 hours and ZIKV in urine (collected alongside a patient-matched serum specimen).
The CII-ArboViroPlex rRT-PCR Test was developed by scientists at the Center for Infection and Immunity (CII) at Columbia University’s Mailman School of Public Health in New York, New York. The manufacture of the test will be overseen by CII.
The CII-ArboViroPlex rRT-PCR Test is authorized to be used by laboratories in the US that are certified under the Clinical Laboratory Improvement Amendments of 1988, 42 U.S.C. § 263a, to perform high complexity tests, or by similarly qualified non-US laboratories.
The CII-ArboViroPlex rRT-PCR Test is authorized to be performed with the NucliSENS® easyMag® automated extraction platform (bioMérieux), the RNA UltraSense™ One-Step Quantitative RT-PCR System (Thermo Fisher), and CFX96 Real-Time PCR Detection System (Bio-Rad).
“The ArboViroPlex Test provides an easy and efficient means to simultaneously detect Zika and 3 other mosquito-borne viral infections that may present with similar clinical features,” said Nischay Mishra, of CII.
“The FDA decision to issue the EUA gives clinicians and researchers a powerful tool to diagnose and prevent the spread of Zika,” added W. Ian Lipkin, director of CII.
More information on the CII-ArboViroPlex rRT-PCR Test Virus Kit and other Zika tests granted EUAs can be found on the FDA’s EUA page. ![]()
The US Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) for the CII-ArboViroPlex rRT-PCR Test.
It is the first multiplex assay that simultaneously tests for the presence of Zika virus, all serotypes of dengue virus, chikungunya virus, and West Nile virus, as well as a host gene that ensures the accuracy of results.
The EUA does not mean the CII-ArboViroPlex rRT-PCR Test is FDA cleared or approved.
An EUA allows for the use of unapproved medical products in an emergency. The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
The EUA for the CII-ArboViroPlex rRT-PCR Test means the test is only authorized as long as circumstances exist to justify the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner.
About the test
The CII-ArboViroPlex rRT-PCR Test is an assay that detects viral RNA matching Zika virus (ZIKV), dengue virus types 1-4 (DENV), chikungunya virus (CHIKV), and West Nile virus (WNV) with a human housekeeping gene, viral RNA controls, and extraction controls that ensure the integrity of the test from nucleic extraction to the final result.
Named for the 4 arboviruses it targets and the real-time reverse transcription polymerase chain reaction (rRT-PCR) technique it employs, the test can simultaneously detect ZIKV, DENV, CHIKV, and WNV in up to 88 samples of blood in less than 2 hours and ZIKV in urine (collected alongside a patient-matched serum specimen).
The CII-ArboViroPlex rRT-PCR Test was developed by scientists at the Center for Infection and Immunity (CII) at Columbia University’s Mailman School of Public Health in New York, New York. The manufacture of the test will be overseen by CII.
The CII-ArboViroPlex rRT-PCR Test is authorized to be used by laboratories in the US that are certified under the Clinical Laboratory Improvement Amendments of 1988, 42 U.S.C. § 263a, to perform high complexity tests, or by similarly qualified non-US laboratories.
The CII-ArboViroPlex rRT-PCR Test is authorized to be performed with the NucliSENS® easyMag® automated extraction platform (bioMérieux), the RNA UltraSense™ One-Step Quantitative RT-PCR System (Thermo Fisher), and CFX96 Real-Time PCR Detection System (Bio-Rad).
“The ArboViroPlex Test provides an easy and efficient means to simultaneously detect Zika and 3 other mosquito-borne viral infections that may present with similar clinical features,” said Nischay Mishra, of CII.
“The FDA decision to issue the EUA gives clinicians and researchers a powerful tool to diagnose and prevent the spread of Zika,” added W. Ian Lipkin, director of CII.
More information on the CII-ArboViroPlex rRT-PCR Test Virus Kit and other Zika tests granted EUAs can be found on the FDA’s EUA page. ![]()
The US Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) for the CII-ArboViroPlex rRT-PCR Test.
It is the first multiplex assay that simultaneously tests for the presence of Zika virus, all serotypes of dengue virus, chikungunya virus, and West Nile virus, as well as a host gene that ensures the accuracy of results.
The EUA does not mean the CII-ArboViroPlex rRT-PCR Test is FDA cleared or approved.
An EUA allows for the use of unapproved medical products in an emergency. The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
The EUA for the CII-ArboViroPlex rRT-PCR Test means the test is only authorized as long as circumstances exist to justify the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner.
About the test
The CII-ArboViroPlex rRT-PCR Test is an assay that detects viral RNA matching Zika virus (ZIKV), dengue virus types 1-4 (DENV), chikungunya virus (CHIKV), and West Nile virus (WNV) with a human housekeeping gene, viral RNA controls, and extraction controls that ensure the integrity of the test from nucleic extraction to the final result.
Named for the 4 arboviruses it targets and the real-time reverse transcription polymerase chain reaction (rRT-PCR) technique it employs, the test can simultaneously detect ZIKV, DENV, CHIKV, and WNV in up to 88 samples of blood in less than 2 hours and ZIKV in urine (collected alongside a patient-matched serum specimen).
The CII-ArboViroPlex rRT-PCR Test was developed by scientists at the Center for Infection and Immunity (CII) at Columbia University’s Mailman School of Public Health in New York, New York. The manufacture of the test will be overseen by CII.
The CII-ArboViroPlex rRT-PCR Test is authorized to be used by laboratories in the US that are certified under the Clinical Laboratory Improvement Amendments of 1988, 42 U.S.C. § 263a, to perform high complexity tests, or by similarly qualified non-US laboratories.
The CII-ArboViroPlex rRT-PCR Test is authorized to be performed with the NucliSENS® easyMag® automated extraction platform (bioMérieux), the RNA UltraSense™ One-Step Quantitative RT-PCR System (Thermo Fisher), and CFX96 Real-Time PCR Detection System (Bio-Rad).
“The ArboViroPlex Test provides an easy and efficient means to simultaneously detect Zika and 3 other mosquito-borne viral infections that may present with similar clinical features,” said Nischay Mishra, of CII.
“The FDA decision to issue the EUA gives clinicians and researchers a powerful tool to diagnose and prevent the spread of Zika,” added W. Ian Lipkin, director of CII.
More information on the CII-ArboViroPlex rRT-PCR Test Virus Kit and other Zika tests granted EUAs can be found on the FDA’s EUA page.
New cancer diagnosis linked to arterial thromboembolism
Patients newly diagnosed with cancer may have a short-term increased risk of arterial thromboembolism, according to a new study.
The research showed that, within 6 months of their diagnosis, cancer patients had a rate of arterial thromboembolism that was more than double the rate in matched control patients without cancer.
However, the risk of arterial thromboembolism varied by cancer type.
Babak B. Navi, MD, of Weill Cornell Medicine in New York, New York, and his colleagues reported these findings in the Journal of the American College of Cardiology.
The researchers used the Surveillance Epidemiology and End Results–Medicare linked database to identify patients with a new primary diagnosis of breast, lung, prostate, colorectal, bladder, pancreatic, or gastric cancer or non-Hodgkin lymphoma from 2002 to 2011.
The team matched these patients (by demographics and comorbidities) to Medicare enrollees without cancer, collecting data on 279,719 pairs of subjects. The subjects were followed through 2012.
Arterial thromboembolism
The study’s primary outcome was the cumulative incidence of arterial thromboembolism, defined as any inpatient or outpatient diagnosis of myocardial infarction or ischemic stroke.
The incidence of arterial thromboembolism at 3 months was 3.4% in cancer patients and 1.1% in controls. At 6 months, it was 4.7% and 2.2%, respectively. At 1 year, it was 6.5% and 4.2%, respectively. And at 2 years, it was 9.1% and 8.1%, respectively.
The hazard ratios (HRs) for arterial thromboembolism among cancer patients were 5.2 at 0 to 1 month, 2.1 at 1 to 3 months, 1.4 at 3 to 6 months, 1.1 at 6 to 9 months, and 1.1 at 9 to 12 months.
The risk of arterial thromboembolism varied by cancer type, with the greatest excess risk observed in lung cancer. The 6-month cumulative incidence was 8.3% in lung cancer patients and 2.4% in matched controls (P<0.001).
In patients with non-Hodgkin lymphoma, the 6-month cumulative incidence of arterial thromboembolism was 5.4%, compared to 2.2% in matched controls (P<0.001).
Myocardial infarction
The cumulative incidence of myocardial infarction at 3 months was 1.4% in cancer patients and 0.3% in controls.
At 6 months, it was 2.0% and 0.7%, respectively. At 1 year, it was 2.6% and 1.4%, respectively. And at 2 years, it was 3.7% and 2.8%, respectively.
The HRs for myocardial infarction among cancer patients were 7.3 at 0 to 1 month, 3.0 at 1 to 3 months, 1.8 at 3 to 6 months, 1.3 at 6 to 9 months, and 1.0 at 9 to 12 months.
Ischemic stroke
The cumulative incidence of ischemic stroke at 3 months was 2.1% in cancer patients and 0.8% in controls.
At 6 months, it was 3.0% and 1.6%, respectively. At 1 year, it was 4.3% and 3.1%, respectively. And at 2 years, it was 6.1% and 5.8%, respectively.
The HRs for ischemic stroke among cancer patients were 4.5 at 0 to 1 month, 1.7 at 1 to 3 months, 1.3 at 3 to 6 months, 1.0 at 6 to 9 months, and 1.1 at 9 to 12 months.
The researchers said these findings raise the question of whether patients with newly diagnosed cancer should be considered for antithrombotic and statin medicines for primary prevention of cardiovascular disease.
The team stressed that because patients with cancer are also prone to bleeding due to frequent coagulopathy and invasive procedures, carefully designed clinical trials are needed to answer these questions.
Patients newly diagnosed with cancer may have a short-term increased risk of arterial thromboembolism, according to a new study.
The research showed that, within 6 months of their diagnosis, cancer patients had a rate of arterial thromboembolism that was more than double the rate in matched control patients without cancer.
However, the risk of arterial thromboembolism varied by cancer type.
Babak B. Navi, MD, of Weill Cornell Medicine in New York, New York, and his colleagues reported these findings in the Journal of the American College of Cardiology.
The researchers used the Surveillance Epidemiology and End Results–Medicare linked database to identify patients with a new primary diagnosis of breast, lung, prostate, colorectal, bladder, pancreatic, or gastric cancer or non-Hodgkin lymphoma from 2002 to 2011.
The team matched these patients (by demographics and comorbidities) to Medicare enrollees without cancer, collecting data on 279,719 pairs of subjects. The subjects were followed through 2012.
Arterial thromboembolism
The study’s primary outcome was the cumulative incidence of arterial thromboembolism, defined as any inpatient or outpatient diagnosis of myocardial infarction or ischemic stroke.
The incidence of arterial thromboembolism at 3 months was 3.4% in cancer patients and 1.1% in controls. At 6 months, it was 4.7% and 2.2%, respectively. At 1 year, it was 6.5% and 4.2%, respectively. And at 2 years, it was 9.1% and 8.1%, respectively.
The hazard ratios (HRs) for arterial thromboembolism among cancer patients were 5.2 at 0 to 1 month, 2.1 at 1 to 3 months, 1.4 at 3 to 6 months, 1.1 at 6 to 9 months, and 1.1 at 9 to 12 months.
The risk of arterial thromboembolism varied by cancer type, with the greatest excess risk observed in lung cancer. The 6-month cumulative incidence was 8.3% in lung cancer patients and 2.4% in matched controls (P<0.001).
In patients with non-Hodgkin lymphoma, the 6-month cumulative incidence of arterial thromboembolism was 5.4%, compared to 2.2% in matched controls (P<0.001).
Myocardial infarction
The cumulative incidence of myocardial infarction at 3 months was 1.4% in cancer patients and 0.3% in controls.
At 6 months, it was 2.0% and 0.7%, respectively. At 1 year, it was 2.6% and 1.4%, respectively. And at 2 years, it was 3.7% and 2.8%, respectively.
The HRs for myocardial infarction among cancer patients were 7.3 at 0 to 1 month, 3.0 at 1 to 3 months, 1.8 at 3 to 6 months, 1.3 at 6 to 9 months, and 1.0 at 9 to 12 months.
Ischemic stroke
The cumulative incidence of ischemic stroke at 3 months was 2.1% in cancer patients and 0.8% in controls.
At 6 months, it was 3.0% and 1.6%, respectively. At 1 year, it was 4.3% and 3.1%, respectively. And at 2 years, it was 6.1% and 5.8%, respectively.
The HRs for ischemic stroke among cancer patients were 4.5 at 0 to 1 month, 1.7 at 1 to 3 months, 1.3 at 3 to 6 months, 1.0 at 6 to 9 months, and 1.1 at 9 to 12 months.
The researchers said these findings raise the question of whether patients with newly diagnosed cancer should be considered for antithrombotic and statin medicines for primary prevention of cardiovascular disease.
The team stressed that because patients with cancer are also prone to bleeding due to frequent coagulopathy and invasive procedures, carefully designed clinical trials are needed to answer these questions.
Patients newly diagnosed with cancer may have a short-term increased risk of arterial thromboembolism, according to a new study.
The research showed that, within 6 months of their diagnosis, cancer patients had a rate of arterial thromboembolism that was more than double the rate in matched control patients without cancer.
However, the risk of arterial thromboembolism varied by cancer type.
Babak B. Navi, MD, of Weill Cornell Medicine in New York, New York, and his colleagues reported these findings in the Journal of the American College of Cardiology.
The researchers used the Surveillance Epidemiology and End Results–Medicare linked database to identify patients with a new primary diagnosis of breast, lung, prostate, colorectal, bladder, pancreatic, or gastric cancer or non-Hodgkin lymphoma from 2002 to 2011.
The team matched these patients (by demographics and comorbidities) to Medicare enrollees without cancer, collecting data on 279,719 pairs of subjects. The subjects were followed through 2012.
Arterial thromboembolism
The study’s primary outcome was the cumulative incidence of arterial thromboembolism, defined as any inpatient or outpatient diagnosis of myocardial infarction or ischemic stroke.
The incidence of arterial thromboembolism at 3 months was 3.4% in cancer patients and 1.1% in controls. At 6 months, it was 4.7% and 2.2%, respectively. At 1 year, it was 6.5% and 4.2%, respectively. And at 2 years, it was 9.1% and 8.1%, respectively.
The hazard ratios (HRs) for arterial thromboembolism among cancer patients were 5.2 at 0 to 1 month, 2.1 at 1 to 3 months, 1.4 at 3 to 6 months, 1.1 at 6 to 9 months, and 1.1 at 9 to 12 months.
The risk of arterial thromboembolism varied by cancer type, with the greatest excess risk observed in lung cancer. The 6-month cumulative incidence was 8.3% in lung cancer patients and 2.4% in matched controls (P<0.001).
In patients with non-Hodgkin lymphoma, the 6-month cumulative incidence of arterial thromboembolism was 5.4%, compared to 2.2% in matched controls (P<0.001).
Myocardial infarction
The cumulative incidence of myocardial infarction at 3 months was 1.4% in cancer patients and 0.3% in controls.
At 6 months, it was 2.0% and 0.7%, respectively. At 1 year, it was 2.6% and 1.4%, respectively. And at 2 years, it was 3.7% and 2.8%, respectively.
The HRs for myocardial infarction among cancer patients were 7.3 at 0 to 1 month, 3.0 at 1 to 3 months, 1.8 at 3 to 6 months, 1.3 at 6 to 9 months, and 1.0 at 9 to 12 months.
Ischemic stroke
The cumulative incidence of ischemic stroke at 3 months was 2.1% in cancer patients and 0.8% in controls.
At 6 months, it was 3.0% and 1.6%, respectively. At 1 year, it was 4.3% and 3.1%, respectively. And at 2 years, it was 6.1% and 5.8%, respectively.
The HRs for ischemic stroke among cancer patients were 4.5 at 0 to 1 month, 1.7 at 1 to 3 months, 1.3 at 3 to 6 months, 1.0 at 6 to 9 months, and 1.1 at 9 to 12 months.
The researchers said these findings raise the question of whether patients with newly diagnosed cancer should be considered for antithrombotic and statin medicines for primary prevention of cardiovascular disease.
The team stressed that because patients with cancer are also prone to bleeding due to frequent coagulopathy and invasive procedures, carefully designed clinical trials are needed to answer these questions.
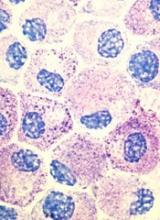
Popular theory of mast cell development is wrong, team says
Stem cell factor (SCF) and KIT signaling are not necessary for early mast cell development, according to research published in Blood.
It has been assumed that the differentiation of hematopoietic progenitors to mast cells requires SCF and KIT signaling.
However, researchers found that mast cell progenitors can survive, mature, and proliferate in the absence of SCF and KIT signaling.
The researchers began this work by analyzing mast cell progenitor populations in samples from healthy subjects, patients with chronic myeloid leukemia (CML) or gastrointestinal stromal tumors (GIST) who were treated with imatinib, and patients with systemic mastocytosis carrying the D816V KIT mutation.
Imatinib inhibits KIT signaling, and the D816V KIT mutation causes KIT signaling to be constitutively active.
The researchers found the imatinib-treated CML and GIST patients and the patients with systemic mastocytosis all had mast cell progenitor populations similar to those observed in healthy subjects.
The team therefore concluded that dysfunctional KIT signaling does not affect the frequency of circulating mast cell progenitors in vivo.
On the other hand, the researchers also found that circulating mast cells were sensitive to imatinib in patients with CML. The patients had higher numbers of peripheral blood mast cells at diagnosis than they did after treatment with imatinib.
“When the patients were treated with the drug imatinib, which blocks the effect of stem cell factor, the number of mature mast cells dropped, while the number of progenitor cells did not change,” said study author Gunnar Nilsson, PhD, of Karolinska Institutet in Stockholm, Sweden.
Subsequent experiments showed that mast cell progenitors can survive in vitro without KIT signaling and without SCF. In addition, mast cell progenitors were able to mature and proliferate in vitro without SCF.
In fact, the researchers said they found that interleukin 3 was sufficient to promote the survival of mast cell progenitors in vitro.
“The study increases our understanding of how mast cells are formed and could be important in the development of new therapies, for example, for mastocytosis . . . ,” said study author Joakim Dahlin, PhD, of the University of Cambridge in the UK.
“One hypothesis that we will now test is whether interleukin 3 can be a new target in the treatment of mast cell-driven diseases.”
Stem cell factor (SCF) and KIT signaling are not necessary for early mast cell development, according to research published in Blood.
It has been assumed that the differentiation of hematopoietic progenitors to mast cells requires SCF and KIT signaling.
However, researchers found that mast cell progenitors can survive, mature, and proliferate in the absence of SCF and KIT signaling.
The researchers began this work by analyzing mast cell progenitor populations in samples from healthy subjects, patients with chronic myeloid leukemia (CML) or gastrointestinal stromal tumors (GIST) who were treated with imatinib, and patients with systemic mastocytosis carrying the D816V KIT mutation.
Imatinib inhibits KIT signaling, and the D816V KIT mutation causes KIT signaling to be constitutively active.
The researchers found the imatinib-treated CML and GIST patients and the patients with systemic mastocytosis all had mast cell progenitor populations similar to those observed in healthy subjects.
The team therefore concluded that dysfunctional KIT signaling does not affect the frequency of circulating mast cell progenitors in vivo.
On the other hand, the researchers also found that circulating mast cells were sensitive to imatinib in patients with CML. The patients had higher numbers of peripheral blood mast cells at diagnosis than they did after treatment with imatinib.
“When the patients were treated with the drug imatinib, which blocks the effect of stem cell factor, the number of mature mast cells dropped, while the number of progenitor cells did not change,” said study author Gunnar Nilsson, PhD, of Karolinska Institutet in Stockholm, Sweden.
Subsequent experiments showed that mast cell progenitors can survive in vitro without KIT signaling and without SCF. In addition, mast cell progenitors were able to mature and proliferate in vitro without SCF.
In fact, the researchers said they found that interleukin 3 was sufficient to promote the survival of mast cell progenitors in vitro.
“The study increases our understanding of how mast cells are formed and could be important in the development of new therapies, for example, for mastocytosis . . . ,” said study author Joakim Dahlin, PhD, of the University of Cambridge in the UK.
“One hypothesis that we will now test is whether interleukin 3 can be a new target in the treatment of mast cell-driven diseases.”
Stem cell factor (SCF) and KIT signaling are not necessary for early mast cell development, according to research published in Blood.
It has been assumed that the differentiation of hematopoietic progenitors to mast cells requires SCF and KIT signaling.
However, researchers found that mast cell progenitors can survive, mature, and proliferate in the absence of SCF and KIT signaling.
The researchers began this work by analyzing mast cell progenitor populations in samples from healthy subjects, patients with chronic myeloid leukemia (CML) or gastrointestinal stromal tumors (GIST) who were treated with imatinib, and patients with systemic mastocytosis carrying the D816V KIT mutation.
Imatinib inhibits KIT signaling, and the D816V KIT mutation causes KIT signaling to be constitutively active.
The researchers found the imatinib-treated CML and GIST patients and the patients with systemic mastocytosis all had mast cell progenitor populations similar to those observed in healthy subjects.
The team therefore concluded that dysfunctional KIT signaling does not affect the frequency of circulating mast cell progenitors in vivo.
On the other hand, the researchers also found that circulating mast cells were sensitive to imatinib in patients with CML. The patients had higher numbers of peripheral blood mast cells at diagnosis than they did after treatment with imatinib.
“When the patients were treated with the drug imatinib, which blocks the effect of stem cell factor, the number of mature mast cells dropped, while the number of progenitor cells did not change,” said study author Gunnar Nilsson, PhD, of Karolinska Institutet in Stockholm, Sweden.
Subsequent experiments showed that mast cell progenitors can survive in vitro without KIT signaling and without SCF. In addition, mast cell progenitors were able to mature and proliferate in vitro without SCF.
In fact, the researchers said they found that interleukin 3 was sufficient to promote the survival of mast cell progenitors in vitro.
“The study increases our understanding of how mast cells are formed and could be important in the development of new therapies, for example, for mastocytosis . . . ,” said study author Joakim Dahlin, PhD, of the University of Cambridge in the UK.
“One hypothesis that we will now test is whether interleukin 3 can be a new target in the treatment of mast cell-driven diseases.”
Cancer patients perceive their abilities differently than caregivers do
New research suggests older cancer patients and their caregivers often differ in their assessment of the patients’ abilities.
In this study, patients generally rated their physical and mental function higher than caregivers did.
The study also showed the differences in assessment of patients’ physical abilities were associated with greater caregiver burden.
This research was published in The Oncologist.
“Caregivers are such an important part of our healthcare system, particularly for older adults with cancer,” said study author Arti Hurria, MD, of City of Hope National Medical Center in Duarte, California.
“We wanted to further understand the factors that are associated with caregiver burden.”
One factor Dr Hurria and her colleagues thought might be important is differences in assessments of patient health and physical abilities between patients and their caregivers.
“In daily practice, we sometimes see a disconnect between what the patient perceives their general health and abilities to be in comparison to what the caregiver thinks,” Dr Hurria said. “We wanted to see whether this disconnect impacted caregiver burden.”
To do this, Dr Hurria and her colleagues questioned 100 older cancer patients and their caregivers.
Subjects were asked about the patients’ general health and physical function, meaning their ability to perform everyday activities. The researchers then compared the answers given by the patients and their respective caregivers.
The researchers also assessed the level of caregiver burden (defined as a subjective feeling of stress caused by being overwhelmed by the demands of caring) by administering a standard questionnaire on topics such as sleep disturbance, physical effort, and patient behavior.
The 100 cancer patients, ages 65 to 91, were suffering from a variety of cancers. The most common were lymphoma (n=26), breast cancer (n=19), and gastrointestinal cancers (n=15). Twelve patients had leukemia, and 10 had myeloma.
The ages of the caregivers ranged from 28 to 85, and the majority were female (73%). They were mainly either the spouse of the patient (68%) or an adult child (18%).
Results
There was no significant difference in patient and caregiver accounts of the patients’ comorbidities (P=0.68), falls in the last 6 months (P=0.71), or percent weight change in the last 6 months (P=0.21).
However, caregivers consistently rated patients as having poorer physical function and mental health and requiring more social support than the patients themselves did.
There was a significant difference (P<0.05) in caregiver and patient accounts when it came to the following measures:
- Need for help with instrumental activities of daily living
- Karnofsky Performance Status
- Medical Outcomes Study-Physical Function
- Medical Outcomes Study-Social Support Survey
- Mental Health Inventory.
Only the disparity in the assessment of physical function was significantly associated with greater caregiver burden (P<0.001). What is still unclear is the cause of this disparity.
“I think there are 2 possible explanations,” said study author Tina Hsu, MD, of the University of Ottawa in Ontario, Canada.
“One is that older adults with cancer either don’t appreciate how much help they require or, more likely, they are able preserve their sense of independence and dignity through a perception that they feel they can do more than they really can.”
“Alternatively, it is possible that caregivers who are more stressed out perceive their loved one to require more help than they actually do need. Most likely, the truth of how much help the patient actually needs lies somewhere between what patients and caregivers report.”
Based on their findings, Drs Hsu and Hurria and their colleagues advise that clinicians consider assessing caregiver burden in those caregivers who report the patient as being more dependent than the patient does themselves.
“Caregivers play an essential role in supporting older adults with cancer,” Dr Hsu said. “We plan to further explore factors associated with caregiver burden in this population, particularly in those who are frailer and thus require even more hands-on support. We also hope to explore what resources caregivers of older adults with cancer feel they need to better help them with their role.”
New research suggests older cancer patients and their caregivers often differ in their assessment of the patients’ abilities.
In this study, patients generally rated their physical and mental function higher than caregivers did.
The study also showed the differences in assessment of patients’ physical abilities were associated with greater caregiver burden.
This research was published in The Oncologist.
“Caregivers are such an important part of our healthcare system, particularly for older adults with cancer,” said study author Arti Hurria, MD, of City of Hope National Medical Center in Duarte, California.
“We wanted to further understand the factors that are associated with caregiver burden.”
One factor Dr Hurria and her colleagues thought might be important is differences in assessments of patient health and physical abilities between patients and their caregivers.
“In daily practice, we sometimes see a disconnect between what the patient perceives their general health and abilities to be in comparison to what the caregiver thinks,” Dr Hurria said. “We wanted to see whether this disconnect impacted caregiver burden.”
To do this, Dr Hurria and her colleagues questioned 100 older cancer patients and their caregivers.
Subjects were asked about the patients’ general health and physical function, meaning their ability to perform everyday activities. The researchers then compared the answers given by the patients and their respective caregivers.
The researchers also assessed the level of caregiver burden (defined as a subjective feeling of stress caused by being overwhelmed by the demands of caring) by administering a standard questionnaire on topics such as sleep disturbance, physical effort, and patient behavior.
The 100 cancer patients, ages 65 to 91, were suffering from a variety of cancers. The most common were lymphoma (n=26), breast cancer (n=19), and gastrointestinal cancers (n=15). Twelve patients had leukemia, and 10 had myeloma.
The ages of the caregivers ranged from 28 to 85, and the majority were female (73%). They were mainly either the spouse of the patient (68%) or an adult child (18%).
Results
There was no significant difference in patient and caregiver accounts of the patients’ comorbidities (P=0.68), falls in the last 6 months (P=0.71), or percent weight change in the last 6 months (P=0.21).
However, caregivers consistently rated patients as having poorer physical function and mental health and requiring more social support than the patients themselves did.
There was a significant difference (P<0.05) in caregiver and patient accounts when it came to the following measures:
- Need for help with instrumental activities of daily living
- Karnofsky Performance Status
- Medical Outcomes Study-Physical Function
- Medical Outcomes Study-Social Support Survey
- Mental Health Inventory.
Only the disparity in the assessment of physical function was significantly associated with greater caregiver burden (P<0.001). What is still unclear is the cause of this disparity.
“I think there are 2 possible explanations,” said study author Tina Hsu, MD, of the University of Ottawa in Ontario, Canada.
“One is that older adults with cancer either don’t appreciate how much help they require or, more likely, they are able preserve their sense of independence and dignity through a perception that they feel they can do more than they really can.”
“Alternatively, it is possible that caregivers who are more stressed out perceive their loved one to require more help than they actually do need. Most likely, the truth of how much help the patient actually needs lies somewhere between what patients and caregivers report.”
Based on their findings, Drs Hsu and Hurria and their colleagues advise that clinicians consider assessing caregiver burden in those caregivers who report the patient as being more dependent than the patient does themselves.
“Caregivers play an essential role in supporting older adults with cancer,” Dr Hsu said. “We plan to further explore factors associated with caregiver burden in this population, particularly in those who are frailer and thus require even more hands-on support. We also hope to explore what resources caregivers of older adults with cancer feel they need to better help them with their role.”
New research suggests older cancer patients and their caregivers often differ in their assessment of the patients’ abilities.
In this study, patients generally rated their physical and mental function higher than caregivers did.
The study also showed the differences in assessment of patients’ physical abilities were associated with greater caregiver burden.
This research was published in The Oncologist.
“Caregivers are such an important part of our healthcare system, particularly for older adults with cancer,” said study author Arti Hurria, MD, of City of Hope National Medical Center in Duarte, California.
“We wanted to further understand the factors that are associated with caregiver burden.”
One factor Dr Hurria and her colleagues thought might be important is differences in assessments of patient health and physical abilities between patients and their caregivers.
“In daily practice, we sometimes see a disconnect between what the patient perceives their general health and abilities to be in comparison to what the caregiver thinks,” Dr Hurria said. “We wanted to see whether this disconnect impacted caregiver burden.”
To do this, Dr Hurria and her colleagues questioned 100 older cancer patients and their caregivers.
Subjects were asked about the patients’ general health and physical function, meaning their ability to perform everyday activities. The researchers then compared the answers given by the patients and their respective caregivers.
The researchers also assessed the level of caregiver burden (defined as a subjective feeling of stress caused by being overwhelmed by the demands of caring) by administering a standard questionnaire on topics such as sleep disturbance, physical effort, and patient behavior.
The 100 cancer patients, ages 65 to 91, were suffering from a variety of cancers. The most common were lymphoma (n=26), breast cancer (n=19), and gastrointestinal cancers (n=15). Twelve patients had leukemia, and 10 had myeloma.
The ages of the caregivers ranged from 28 to 85, and the majority were female (73%). They were mainly either the spouse of the patient (68%) or an adult child (18%).
Results
There was no significant difference in patient and caregiver accounts of the patients’ comorbidities (P=0.68), falls in the last 6 months (P=0.71), or percent weight change in the last 6 months (P=0.21).
However, caregivers consistently rated patients as having poorer physical function and mental health and requiring more social support than the patients themselves did.
There was a significant difference (P<0.05) in caregiver and patient accounts when it came to the following measures:
- Need for help with instrumental activities of daily living
- Karnofsky Performance Status
- Medical Outcomes Study-Physical Function
- Medical Outcomes Study-Social Support Survey
- Mental Health Inventory.
Only the disparity in the assessment of physical function was significantly associated with greater caregiver burden (P<0.001). What is still unclear is the cause of this disparity.
“I think there are 2 possible explanations,” said study author Tina Hsu, MD, of the University of Ottawa in Ontario, Canada.
“One is that older adults with cancer either don’t appreciate how much help they require or, more likely, they are able preserve their sense of independence and dignity through a perception that they feel they can do more than they really can.”
“Alternatively, it is possible that caregivers who are more stressed out perceive their loved one to require more help than they actually do need. Most likely, the truth of how much help the patient actually needs lies somewhere between what patients and caregivers report.”
Based on their findings, Drs Hsu and Hurria and their colleagues advise that clinicians consider assessing caregiver burden in those caregivers who report the patient as being more dependent than the patient does themselves.
“Caregivers play an essential role in supporting older adults with cancer,” Dr Hsu said. “We plan to further explore factors associated with caregiver burden in this population, particularly in those who are frailer and thus require even more hands-on support. We also hope to explore what resources caregivers of older adults with cancer feel they need to better help them with their role.”