User login
Development and Implementation of a Homeless Mobile Medical/Mental Veteran Intervention
Research has consistently identified remarkably high rates of addiction, mental illness, and health problems in the homeless population.1-9 Yet in spite of extensive service needs for these problems, abundant evidence exists of consistent underuse of health care services by homeless populations.10-12 Most of the homeless population reside in emergency shelters or in transitional or supportive housing, but many remain in places not meant for human habitation.
Homelessness is significantly overrepresented among military veterans.13 The January 2016 national point-in-time count identified 39,471 veterans experiencing homelessness.13 Iraq and Afghanistan veterans seem to have an especially high risk for homelessness.13-15 Disheartening statistics such as these prompted former VA Secretary Eric Shinseki to pledge to end veteran homelessness by December 2015.16 He argued in support of this mission that 85% of veteran homeless resources go to health care—implying that homelessness among veterans is primarily a health care issue, which is heavily burdened by substance abuse and other psychiatric and medical illnesses.17
Health care service use has been associated with improved health, mental health, and outcomes among homeless populations.12,18 Unfortunately, access to these services is limited by barriers associated with homelessness, such as transportation or lack of proper identification.19,20 Veterans experiencing homelessness also face these common barriers to health care, and unsheltered veterans especially underutilize VA health care services.21
Housing First—a successful model that places individuals into housing without prerequisites for sobriety, active participation in treatment, or other behavioral accomplishments, such as gainful employment—has not managed yet to place all the disengaged homeless veteran population into stable housing.22 However, the Housing First model, which is based on the individual’s priorities, is consistent with the approach of a new program at the VA North Texas Health Care System (VANTHCS).
The VHA, similar to other health care systems, is engaged in a cultural transformation to convert its health care approach from a traditional medical model to patient-centered care (PCC).23 In this priority area, a strategic objective is for the VHA to partner with each veteran to create a personalized, proactive strategy to optimize health and well-being and when needed provide state-of-the-art disease management. Patient-centered care is designed to address veterans’ specific needs in spiritual, environmental, physical, mental, and social domains and empower veterans to become active participants in their care. Patient-centered care differs from the traditional medical model in that patients are active participants in their treatment, partnering and collaborating with their providers on care that is quality-of-life centered instead of disease centered.23 This model is based on both respect for patients as unique individuals and on the obligation to care for them on their own terms, focused on their self-identified goals and aspirations.24
At VANTHCS, the Homeless Mobile Medical/Mental Veteran (HMMM-V) pilot program was designed to deliver effective health care services to a homeless subpopulation of veterans who historically have been the most difficult to serve—those living in unsheltered environments, such as under bridges and in encampments. The purpose of the HMMM-V program was to contact and serve veterans not currently being reached by the VA system of care, using a PCC model.
This pilot program was initially funded in January 2013 by a 2-year grant from the Office of Patient Centered Care and Cultural Transformation to apply the PCC approach to engage veteran participation. For this project, the VA Personal Health Inventory tool—originally designed for use with the general veteran population—was adapted for use with the homeless veteran population. The grant funding period covered the design, development, and implementation of the HMMM-V program; thereafter, VANTHCS provided resources through its Comprehensive Homeless Center Programs to assure its sustainability and continued use of the clinical assessment tool created for this project.
This article describes the development and implementation of this novel program with sufficient detail to inform the development of similar programs in other sites. Descriptions of the program and staffing, creation of community partnerships, and modification of an assessment instrument are provided. It also illustrates the original implementation period of the HMMM-V program through presentation of self-reported data on the first homeless veterans it served.
Equipment and Staffing
A custom 28-foot mobile outreach vehicle was assembled according to specifications identified by the HMMM-V team as necessary to conduct the program’s interventions. The van became fully operational on April 8, 2015, after it underwent all the required reviews and inspections (eg, safety, infection control, etc) and was accredited in 2015 by the Commission on Accreditation of Rehabilitation Facilities.
The HMMM-V van has a driver compartment that is separate from its services rooms, which include a patient registration area, a fully equipped examination room, a laboratory area, and a bathroom. The vehicle is equipped with a wheelchair lift and an awning to shade outdoor areas where tables and chairs are set up for patient/staff waiting and rest areas. The vehicle is stocked with essential equipment and supplies needed to conduct work in off-street locations, vacant lots, under bridges, fields, unpaved paths, etc. It also is equipped with telemedicine capabilities to provide clinical supervision and access to attending physicians and specialists at VANTHCS. Personnel carry cell phones and laptop computers with secure Internet connections using a commercially available mobile wireless Wi-Fi hotspot to facilitate documentation of medical records and communication from the field.
This reliable type of equipment is routine for use in VA field operations; the only hurdle using these technologies for the program was acquiring funding and purchasing the equipment. The vehicle is further equipped with a refrigerator solely for secure storage of pharmaceutical supplies, a second refrigerator for specimens, and wall-mounted blood pressure and otoscope/ophthalmoscope units. The vehicle is supplied with thermometers, scales, phlebotomy supplies, and first-aid kits and is stocked with vaccines and medications, including antibiotic, hypertensive, diabetic, allergy, and over-the-counter pain medications. A more comprehensive list of supplies for the vehicle is available from the authors on request.
Medication provisions supplied to the HMMM-V mobile clinic conform to the Texas State Board of Pharmacy compliance regulations. Because the vehicle is designated as federal property and has U.S. government license plates, it is considered an extension of VANTHCS Pharmacy Service and falls under its pharmacy license. A medication formulary was created with input from HMMM-V prescribers and Dallas VAMC Pharmacy Service pharmacists. To safeguard the integrity of these pharmaceutical agents, the HMMM-V physician assistant picks up the medications before field deployment and returns the unused medications to the Dallas VAMC at the end of the day. The medications are transported in locked containers and placed either in a locked medication refrigerator or cabinet on the mobile unit.
For medication prescriptions that need laboratory testing before prescribing them, HMMM-V prescribers can check the VA electronic medical record from the field to determine whether these tests have been completed recently. If not, then HMMM-V team has an agreement with Dallas VA Pathology and Laboratory Medicine Service for testing samples obtained in the field.
The program was designed for staffing of the vehicle by 2 professional teams, each includes medical (physician’s assistant or registered nurse), mental health (psychiatrist, residents), and social work providers (licensed social workers, clinical social workers); trainees of these disciplines; a peer support specialist; and an administrative clerk. The staffing varies daily, depending on available personnel. When personnel deploy to the field, they go in pairs or groups to address potential safety issues. Cell phones are available to summon police or ambulance services in an emergency. Systematic safety training was conducted with all field personnel before their first deployment to guard against vulnerability to danger in these settings.
Once in the field, personnel engage unsheltered homeless individuals to assess eligibility for VA services. Veterans found ineligible are assisted with application for military discharge upgrade, service-connected compensation, or appeal for health care coverage. Veterans eligible for VA care receive physical examinations, vital and glucose checks, influenza and pneumonia vaccinations, first-aid skin and wound care, medication management with limited medications provided at point of care, blood and urine testing, peer support services, suicide assessments, clinical mental health evaluations, and social work services through the HMMM-V program.
Social work assistance provided includes psychosocial assessment and care coordination for psychosocial needs such as mental health, substance abuse, vision, dental, housing, employment, legal aid, transportation, food, income, hygiene, and weather-appropriate provision needs.
Community Partnerships
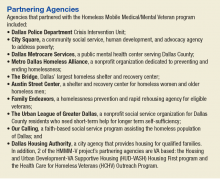
The HMMM-V program benefitted from a number of partnerships with community agencies. During development of the program, HMMM-V personnel accompanied the Dallas Police Department’s Crisis Intervention Unit on typical homeless crisis services deployments into the field to learn about the locations and nature of encampments and homeless peregrination patterns in the Dallas area.
To aid in the design and selection of features for the mobile outreach vehicle, team members toured Homeless Outreach Medical Service mobile clinics from 2 local county hospitals, Parkland Hospital and John Peter Smith Hospital. The staff for these mobile clinics were interviewed about their experience with various components of their programs and their recommendations for optimal design of the mobile medical clinic for service delivery.
Numerous agencies in the Dallas area that serve the homeless population assisted with locating and connecting homeless veterans to HMMM-V programs. These partnering agencies also serve homeless individuals who do not qualify for the HMMM-V program, such as veterans with other-than-honorable military discharges.
The HMMM-V mobile outreach vehicle travels to partnering agencies and provides services on a recurring basis. These agencies are the Dallas International Street Church, a church and faith-based agency aiding the recovery of people with “broken lives”; Cornerstone Ministries, a church-based ministry serving people with adverse circumstances; and City Square’s Opportunity Center, human services and community development programs for low-income city residents. The mobile clinic also travels regularly to other areas to serve homeless veterans residing in unsheltered locations, such as homeless encampments and under bridges.
Clinical Assessment
The project used a modification of the VA Personalized Health Inventory (PHI) for general veteran populations, which assesses 8 areas of self-identified needs to address the specific concerns of homeless veterans served by a mobile clinic.25 Version 19 of the PHI (revised September 18, 2012), the version of the instrument available to the team at the inception of the project, was deployed with the HMMM-V personnel into the field. It imposed a heavy interview time burden (several hours), and its content areas did not seem appropriate to address the immediate concerns of homeless populations (eg, sections pertaining to personal development through hobbies, recreation, or volunteering; healthy living spaces with plenty of lighting and color; “eating healthy, balanced meals with plenty of fruits and vegetables each day”).25
Based on HMMM-V personnel feedback, the team modified this tool and developed a patient-centered health inventory (P-CHI) for homeless veterans that was acceptable in length and applicable to the situational characteristics of homeless existence. The tool’s 10 “current and desired states” were revised to remove domains of exercise and flexibility, sleep and relaxation, and mind-body techniques. The intervention and prevention domains were combined. A material needs (clothing, furniture, transportation, financial benefits) domain was added, and a new domain on reducing alcohol/drug use was created by moving this material from the food and drink domain.
The remaining domains were modified to fit the homeless living situation (Food and Drink = Nutrition; Personal Development = Employment/Vocation; Family, Friends, and Co-Workers = Family/Social/Legal Support; Spirit and Soul = Personal/Spiritual Fulfillment; Surroundings = Housing). Current state ratings were revised to reflect level of satisfaction, and ratings of Desired State were replaced with level of importance.
The modifications resulted in 9 domains, which were assembled into a grid for efficient rating of both satisfaction and importance for each domain (rated 1 to 10, lowest to highest, respectively), followed by an instruction to mark an X in a designated space in all the domains with which the individual would like help (Table). The intent was to reduce the burden of the instrument by having the participant complete sections providing detailed information about only the domains selected by the participant.
The details of each domain in the original VA PHI tool were captured through open-ended questions in text responses provided by the veteran. Because open-ended text responses are not conducive for summarizing characteristics of the population served or for evaluating program activities, the detailed sections covering the domains were revised completely to capture data within categoric and numeric variables. Items from the validated Homeless Supplement Interview were added to collect information not provided in the Homeless Operations Management and Evaluation System interview that is routinely administered to all veterans accessing homeless VA services.26-28
The information collected in these domains cover duration of current homeless episode, lifetime number of homeless episodes, current living arrangements and dissatisfactions with these arrangements, frequency and source of meals, employment history and current work status, sources of income, special material needs, medical and dental problems and sources of care, current medications, mental health problems and sources of care, urgent mental health concerns, current amount and frequency of alcohol and drug use, substance abuse treatment history, relationships with family and intimate partners, legal assistance needs, and self-identified needs for spiritual and personal fulfillment. This instrument is available on request to the authors.
Veterans Served
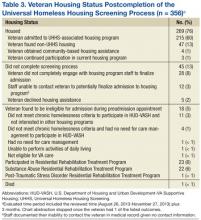
The project began with 1 team of professionals deploying with the HMMM-V vehicle while a second team was being assembled. Currently, the 2 HMMM-V teams deploy the mobile clinic 4 days per week. The mobile clinic visits agencies that serve the homeless, including emergency shelters and food ministries, as well as homeless encampments. To date, 195 homeless veterans have been served by the mobile clinic, 111 were currently enrolled with the VA, 8 were not enrolled but eligible for services, and 77 were not eligible for VA services. Of the unenrolled veterans, those eligible for services were offered VA enrollment assistance; those ineligible for VA services were offered a community referral.
For the veterans encountered in the field, the following interventions were provided: 49 housing placement referrals, 4 rental assistance referrals, 4 legal referrals, 27 medical care interventions, 13 dental referrals, 11 vision/hearing referrals, 12 mental health interventions, 9 substance abuse treatment referrals, 14 employment assistance referrals, 13 disability benefit applications, 18 transportation assists, 23 goods delivered, and 159 information assists. The HMMM-V mobile clinic also is deployed to participate in various educational and outreach events. At the time this article was written, the mobile clinic has reached nearly 2,000 veterans and community partners in at least 25 such events.
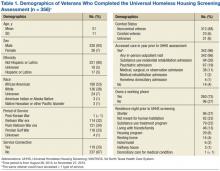
Of the veterans served to date, 73 completed the P-CHI. These veterans were predominantly male (77%), and the majority (60%) were black. The median age of the sample was 58 years, and typically they had a high school level of education (12.7; SD, 2.1 mean years of education). About half (49%) the sample were separated or divorced, and only a minority were currently married (8%). Half (50%) the sample served in the U.S. Army, with the post-Vietnam era being the era of service most represented (19%). Few (21%) veterans reported exposure to hostile or friendly fire during their service. More than three-fourths (80%) of the sample had experienced a homeless episode prior to their current one. On average, members of the sample had experienced a median of 3 lifetime homeless episodes. They had a mean 4.1 (SD, 5.8) lifetime number of years of homelessness, and 3.0 (SD, 5.2) years in their current homeless episode. Nearly one-third (31%) reported that they were currently staying in a homeless shelter, and nearly one-sixth (16%) were currently unsheltered in street settings, such as under bridges or in outdoor encampments at the time of the initial visit.
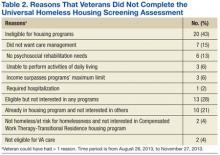
The mean number of minutes spent completing the P-CHI was 18.5 (SD, 9.4). The veterans indicated that they would like assistance with a mean 3.2 (SD, 2.2) number of domains. The domains with the highest average importance ratings were housing (mean, 9.4; SD, 1.7) and medical/dental care (mean, 8.9; SD, 2.2); the domains with the lowest average importance rating were reducing alcohol/drug use (mean, 6.4; SD, 4.1) and employment/vocation (mean, 6.3; SD, 4.2). The domains with the highest average satisfaction ratings were personal/spiritual fulfillment (mean, 7.3; SD, 2.9) and reducing substance use (mean, 5.9; SD, 4.0), and the domains with the lowest average satisfaction ratings were housing (mean, 2.9; SD, 2.9), material needs (mean, 4.2; SD, 3.3), and employment/vocation (mean, 4.2; SD, 3.2). The domain with the greatest indication of desire for help was housing, endorsed by more than four-fifths (84%) of the sample. This highly endorsed housing domain also was one of the lowest in satisfaction. The domains with the least expressed interest in obtaining help were reducing substance use (18%) and personal/spiritual fulfillment (15%).Reducing substance abuse also was one of the lowest domains of importance and the least for dissatisfaction.
Challenges and Barriers
As anticipated from its inception, this project encountered many challenges and barriers. The first was with the design, construction, and delivery of the mobile clinic unit. The vehicle took more than 2 years to be delivered. There were delays in progress necessitated by required selection of an approved vendor to build the vehicle, extensive specification of details and features, and stocking it with equipment and supplies. The weight of the unit had to be < 26,000 pounds to avoid the requirement of a commercial driver’s license, which limited the size of the vehicle to 28 feet. Stocking the unit with equipment and supplies required attention to a myriad of specifications and decisions. For example, separate refrigerators were needed for specimens, medications, and food; pharmaceutical regulations governing medications in mobile clinics required strict adherence; and difficulties were encountered in attempting to establish adequate and secure connectivity for communications devices in the field.
Once the mobile unit was delivered and prepared for deployment, the next set of challenges pertained to learning all of the instructions required to operate and drive the vehicle and learning how to maneuver the vehicle in the field. Specific challenges for driving the vehicle encountered included unexpectedly low overpasses that prohibited passage, narrow spaces for passage, rough and uneven terrain in off-road settings, and lateral and vertical tilt of roads creating potential for sideswipes and undercarriage scrapes. Maintenance schedules needed to be developed and implemented for cleaning the unit, inspection compliance, repairs, refueling, and emptying waste materials.
Staffing the vehicle required the development of unique job specifications addressing special expertise in accessing VA databases for veteran verification and registration and for driving the mobile clinic vehicle. Schedules and deployment plans for 2 teams that shared the same vehicle had to be established and followed. Locating veterans in unsheltered settings, such as under bridges and in encampments, required community intelligence facilitated through partnerships with knowledgeable members of the Dallas police crisis unit and by gaining field experience to locate where the usual homeless gathering places are, especially those inhabited by veterans. Safety of team members and equipment/supplies in the field was paramount from the start, and additional steps beyond safety training required extra measures, such as special care in navigating known dangerous areas. Provision of services necessitated completion of everything needed in a single visit due to the likelihood of loss to follow-up and acceptance of the limited types of service that could be provided in a mobile clinic. Special procedures were needed to provide referrals to sources of available care for non-VA-qualifying veterans.
Discussion
The HMMM-V program for delivery of PCC to homeless veterans is an innovative pilot program designed to connect with difficult-to-reach homeless veterans and engage them in care. The deliverables provided by this project are (1) A mobile outreach vehicle to deliver care to homeless veterans and outreach to other veterans and community agencies in North Texas; (2) The P-CHI assessment tool for homeless veterans modified and adapted for use with this special population; and (3) pilot data on its first cohort of homeless veterans served, describing their baseline characteristics and their stated satisfaction and preferences about their goals and aspirations for their physical, emotional, and mental health and well-being.
The HMMM-V program successfully identified homeless veterans in need of services, and more than one-third of these veterans were not previously engaged in VA services. Compared with the “typical” veterans served at VANTHCS homeless programs, veterans served by the HMMM-V comprised a greater proportion of minorities and a higher proportion who had been exposed to combat.29 Age and gender characteristics were similar.29 When compared with veterans who access care at VANTHCS and have not experienced homelessness, those served by the HMMM-V were younger and more likely to belong to a minority group; however, they were similar in combat exposure and gender.1 The veterans served by the HMMM-V program also were considerably older and had more homeless chronicity than did nonveteran homeless populations, consistent with other research.4,29,30
The veterans served by the HMMM-V program not surprisingly made housing their top priority in need of help, consistent with the Housing First model.22,31 They also indicated that employment/vocation and reducing substance use were of lower importance. Need for assistance with reducing substance use and social support were the domains least often identified as areas where help was needed, which seems inconsistent with the higher established rates of substance abuse problems among homeless veterans.1
With additional fieldwork, the HMMM-V program is expected to allow refinement of procedures for identifying and serving veterans from a patient-centered care perspective. The P-CHI will be further tested and developed, and the next step will be to create and pilot intervention templates for a Patient-Centered Health Improvement Plan, based on the P-CHI results. This process parallels the original development treatment plans for the VA’s Personalized Health Plan based on the PHI.25 Once the HMMM-V program is fully established in Dallas, the plans are for an expansion that will cover a broader geographic area in North Texas that includes rural areas.
The HMMM-V program was designed to address the barriers to health care that are encountered by homeless veterans. It is unique in homeless veteran care due to its patient-centered approach that partners with homeless veterans to prioritize their needs as determined by them rather than based solely on policies or provider conceptualizations of their needs. Access to services, engagement in care, and successful utilization of needed services may lead to measurable improvements in health care outcomes among homeless populations of veterans. Desired goals include remission of illness through appropriate medical intervention, preventing morbidity, achieving healthy lifestyles, recovery from addiction, stabilization of psychiatric illness, and attainment of stable housing.
The first hurdle for implementing this type of program in other settings is the identification of resources needed for these efforts. Need of additional staffing resources, however, may be circumvented by allowing employees working in other areas to rotate in community outreach shifts in the mobile unit. Another hurdle encountered in implementation of the HMMM-V initiative was the initial difficulty finding homeless veterans in community settings, especially those in unsheltered locations. The HMMM-V program addressed this issue by partnering with other agencies serving the homeless in the community. Therefore, a general recommendation for other entities seeking to implement this type of program is to reach out to these community partners from the outset.
Conclusion
The HMMM-V has the potential to engage the most difficult-to-reach homeless veterans in need of health services by delivering care and providing resources in challenging environments. Further work is needed to validate the P-CHI for use with this program and to conduct well-designed and implemented research to demonstrate effectiveness of this intervention on veteran outcomes, especially quality of life. Once this additional work is accomplished, this innovative program can potentially be implemented by VAMCs across the nation, and potentially in more general community care settings, to more effectively reach out and deliver services to homeless members of the community.
Acknowledgments
Grant support was received from the Department of Veterans Affairs, Office of Patient Centered Care. The authors would like to acknowledge all the clinicians, trainees, and support staff who have contributed to the success of the HMMM-V program: Tara Ayala, Jose Cabrera, Tony Castillo, Rachael Lynn David, Teresa DeShazo, Sylvia Figueroa, Steven Fisher, Eric Gary, Evelyn Gibbs, Kevin Hosey, JoAnn Joseph, Taly Drimer Kagan, Miranda Kelly, Michelle King-Thompson, Sharon Marcus, Shiji Mathew, Moneeza Matin, John Moreno, Joseph Neifert, Joel Price, Tiffany Price, Natalie Qualls, Reginald Robertson, Kristine Rodrigues, Jon Saffelder, Jill Stokes, Scott Stone, and John Smith.
1. LePage JP, Bradshaw LD, Cipher DJ, Crawford AM, Hooshyar D. The effects of homelessness on veterans’ health care service use: an evaluation of independence from comorbidities. Public Health. 2014;128(11):985-992.
2. Fischer PJ, Breakey WR. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol. 1991;46(11):1115-1128.
3. Robertson MJ, Zlotnick C, Westerfelt A. Drug use disorders and treatment contact among homeless adults in Alameda County, California. Am J Public Health. 1997;87(2):221-228.
4. North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? Am J Public Health. 2004;94(1):103-108.
5. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225.
6. Harpaz-Rotem I, Rosenheck RA, Desai R. The mental health of children exposed to maternal mental illness and homelessness. Community Ment Health J. 2006;42(5):437-448.
7. Pollio DE, Eyrich-Garg KM, North CS. The homeless. In: Johnson BA, ed. Addiction Medicine: Science and Practice. New York, NY: Springer; 2011:1487-1504.
8. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
9. Baggett TP, Singer DE, Rao SR, O’Connell JJ, Bharel M, Rigotti NA. Food insufficiency and health services utilization in a national sample of homeless adults. J Gen Intern Med. 2011;26(6):627-634.
10. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376.
11. Fuehrlein BS, Cowell AJ, Pollio D, Cupps L, Balfour ME, North CS. A prospective study of the associations among housing status and costs of services in a homeless population. Psychiatr Serv. 2015;66(1):27-32.
12. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
13. U.S. Department of Housing and Urban Development Office of Community Planning and Development. The 2016 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: point-in-time estimates of homelessness. https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Published 2016. Accessed August 7, 2017.
14. Tsai J, Rosenheck RA. Risk factors for homelessness among U.S. veterans. Epidemiol Rev. 2015;37:177-195.
15. Williamson V, Mulhall E. Coming home: the housing crisis and homelessness threaten new veterans. Iraq and Afghanistan Veterans of America, January, 2009. http://media.iava.org/IAVA_coming_home_2009%20The%20Housing%20Crisis%20and%20Homelessness%20Threaten%20New%20Veterans.pdf. Accessed August 10, 2017
16. Shinseki EK. Remarks by Secretary Eric K. Shinseki. National Summit on Homeless Veterans; November 3, 2009; Washington, DC. https://www.va.gov/opa/speeches/2009/09_1103.asp. Updated August 8, 2016. Accessed August 7, 2017.
17. Shinseki EK. Remarks by Secretary Eric K. Shinseki. 2014 National Coalition for Homeless Veterans Annual Meeting; May 30, 2014; Arlington, VA. https://www.va.gov/opa/speeches/2014/05_30_2014.asp. Updated April 21, 2015. Accessed August 7, 2017.
18. Pollio DE, Spitznagel EL, North CS, Thompson S, Foster DA. Service use over time and achievement of stable housing in a mentally ill homeless population. Psychiatr Serv. 2000;51(12):1536-1543.
19. Page J. Barriers to transferring care of homeless people with serious mental illnesses to community mental health organizations: perspectives of street-based programs. Best Practices in Mental Health: An International Journal. 2007;3(1):26.
20. Young AS, Chinman MJ, Cradock-O’Leary JA, et al. Characteristics of individuals with severe mental illness who use emergency services. Community Ment Health J. 2005;41(2):159-168.
21. Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461.
22. Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651-656.
23. U.S. Department of Veterans Affairs, Veterans Health Administration. VA Patient Centered Care. http://www.va.gov/patientcenteredcare. Updated July 24,2017. Accessed August 7, 2017.
24. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
25. U.S. Department of Veterans Affairs, Office of Patient Centered Care and Cultural Transformation. My story: personal health inventory. https://www.va.gov/PATIENTCENTEREDCARE/docs/VA-OPCC-Personal-Health-Inventory-final-508.pdf. Published October 7, 2013. Accessed August 7, 2017
26. North CS, Smith EM, Pollio DE. The Homeless Supplement to the Diagnostic Interview Schedule (DIS/HS). St. Louis: Washington University, 2004.
27. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The homeless supplement to the diagnostic interview schedule: test-retest analyses. Int J Methods Psychiatr Res. 2004;13(3):184-191.
28. LaSalle JL. Homeless Operations Management and Evaluation System (HOMES) user manual-phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed August 7, 2017.
29. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psychiatr Serv. 2014;65(6):751-757.
30. North CS, Smith EM. A comparison of homeless men and women: different populations, different needs. Community Ment Health J. 1993;29(5):423-431.
31. Kertesz SG, Austin EL, Holmes SK, et al. Making housing first happen: organizational leadership in VA’s expansion of permanent supportive housing. J Gen Intern Med. 2014;29(suppl 4):835-844.
Research has consistently identified remarkably high rates of addiction, mental illness, and health problems in the homeless population.1-9 Yet in spite of extensive service needs for these problems, abundant evidence exists of consistent underuse of health care services by homeless populations.10-12 Most of the homeless population reside in emergency shelters or in transitional or supportive housing, but many remain in places not meant for human habitation.
Homelessness is significantly overrepresented among military veterans.13 The January 2016 national point-in-time count identified 39,471 veterans experiencing homelessness.13 Iraq and Afghanistan veterans seem to have an especially high risk for homelessness.13-15 Disheartening statistics such as these prompted former VA Secretary Eric Shinseki to pledge to end veteran homelessness by December 2015.16 He argued in support of this mission that 85% of veteran homeless resources go to health care—implying that homelessness among veterans is primarily a health care issue, which is heavily burdened by substance abuse and other psychiatric and medical illnesses.17
Health care service use has been associated with improved health, mental health, and outcomes among homeless populations.12,18 Unfortunately, access to these services is limited by barriers associated with homelessness, such as transportation or lack of proper identification.19,20 Veterans experiencing homelessness also face these common barriers to health care, and unsheltered veterans especially underutilize VA health care services.21
Housing First—a successful model that places individuals into housing without prerequisites for sobriety, active participation in treatment, or other behavioral accomplishments, such as gainful employment—has not managed yet to place all the disengaged homeless veteran population into stable housing.22 However, the Housing First model, which is based on the individual’s priorities, is consistent with the approach of a new program at the VA North Texas Health Care System (VANTHCS).
The VHA, similar to other health care systems, is engaged in a cultural transformation to convert its health care approach from a traditional medical model to patient-centered care (PCC).23 In this priority area, a strategic objective is for the VHA to partner with each veteran to create a personalized, proactive strategy to optimize health and well-being and when needed provide state-of-the-art disease management. Patient-centered care is designed to address veterans’ specific needs in spiritual, environmental, physical, mental, and social domains and empower veterans to become active participants in their care. Patient-centered care differs from the traditional medical model in that patients are active participants in their treatment, partnering and collaborating with their providers on care that is quality-of-life centered instead of disease centered.23 This model is based on both respect for patients as unique individuals and on the obligation to care for them on their own terms, focused on their self-identified goals and aspirations.24
At VANTHCS, the Homeless Mobile Medical/Mental Veteran (HMMM-V) pilot program was designed to deliver effective health care services to a homeless subpopulation of veterans who historically have been the most difficult to serve—those living in unsheltered environments, such as under bridges and in encampments. The purpose of the HMMM-V program was to contact and serve veterans not currently being reached by the VA system of care, using a PCC model.
This pilot program was initially funded in January 2013 by a 2-year grant from the Office of Patient Centered Care and Cultural Transformation to apply the PCC approach to engage veteran participation. For this project, the VA Personal Health Inventory tool—originally designed for use with the general veteran population—was adapted for use with the homeless veteran population. The grant funding period covered the design, development, and implementation of the HMMM-V program; thereafter, VANTHCS provided resources through its Comprehensive Homeless Center Programs to assure its sustainability and continued use of the clinical assessment tool created for this project.
This article describes the development and implementation of this novel program with sufficient detail to inform the development of similar programs in other sites. Descriptions of the program and staffing, creation of community partnerships, and modification of an assessment instrument are provided. It also illustrates the original implementation period of the HMMM-V program through presentation of self-reported data on the first homeless veterans it served.
Equipment and Staffing
A custom 28-foot mobile outreach vehicle was assembled according to specifications identified by the HMMM-V team as necessary to conduct the program’s interventions. The van became fully operational on April 8, 2015, after it underwent all the required reviews and inspections (eg, safety, infection control, etc) and was accredited in 2015 by the Commission on Accreditation of Rehabilitation Facilities.
The HMMM-V van has a driver compartment that is separate from its services rooms, which include a patient registration area, a fully equipped examination room, a laboratory area, and a bathroom. The vehicle is equipped with a wheelchair lift and an awning to shade outdoor areas where tables and chairs are set up for patient/staff waiting and rest areas. The vehicle is stocked with essential equipment and supplies needed to conduct work in off-street locations, vacant lots, under bridges, fields, unpaved paths, etc. It also is equipped with telemedicine capabilities to provide clinical supervision and access to attending physicians and specialists at VANTHCS. Personnel carry cell phones and laptop computers with secure Internet connections using a commercially available mobile wireless Wi-Fi hotspot to facilitate documentation of medical records and communication from the field.
This reliable type of equipment is routine for use in VA field operations; the only hurdle using these technologies for the program was acquiring funding and purchasing the equipment. The vehicle is further equipped with a refrigerator solely for secure storage of pharmaceutical supplies, a second refrigerator for specimens, and wall-mounted blood pressure and otoscope/ophthalmoscope units. The vehicle is supplied with thermometers, scales, phlebotomy supplies, and first-aid kits and is stocked with vaccines and medications, including antibiotic, hypertensive, diabetic, allergy, and over-the-counter pain medications. A more comprehensive list of supplies for the vehicle is available from the authors on request.
Medication provisions supplied to the HMMM-V mobile clinic conform to the Texas State Board of Pharmacy compliance regulations. Because the vehicle is designated as federal property and has U.S. government license plates, it is considered an extension of VANTHCS Pharmacy Service and falls under its pharmacy license. A medication formulary was created with input from HMMM-V prescribers and Dallas VAMC Pharmacy Service pharmacists. To safeguard the integrity of these pharmaceutical agents, the HMMM-V physician assistant picks up the medications before field deployment and returns the unused medications to the Dallas VAMC at the end of the day. The medications are transported in locked containers and placed either in a locked medication refrigerator or cabinet on the mobile unit.
For medication prescriptions that need laboratory testing before prescribing them, HMMM-V prescribers can check the VA electronic medical record from the field to determine whether these tests have been completed recently. If not, then HMMM-V team has an agreement with Dallas VA Pathology and Laboratory Medicine Service for testing samples obtained in the field.
The program was designed for staffing of the vehicle by 2 professional teams, each includes medical (physician’s assistant or registered nurse), mental health (psychiatrist, residents), and social work providers (licensed social workers, clinical social workers); trainees of these disciplines; a peer support specialist; and an administrative clerk. The staffing varies daily, depending on available personnel. When personnel deploy to the field, they go in pairs or groups to address potential safety issues. Cell phones are available to summon police or ambulance services in an emergency. Systematic safety training was conducted with all field personnel before their first deployment to guard against vulnerability to danger in these settings.
Once in the field, personnel engage unsheltered homeless individuals to assess eligibility for VA services. Veterans found ineligible are assisted with application for military discharge upgrade, service-connected compensation, or appeal for health care coverage. Veterans eligible for VA care receive physical examinations, vital and glucose checks, influenza and pneumonia vaccinations, first-aid skin and wound care, medication management with limited medications provided at point of care, blood and urine testing, peer support services, suicide assessments, clinical mental health evaluations, and social work services through the HMMM-V program.
Social work assistance provided includes psychosocial assessment and care coordination for psychosocial needs such as mental health, substance abuse, vision, dental, housing, employment, legal aid, transportation, food, income, hygiene, and weather-appropriate provision needs.
Community Partnerships
The HMMM-V program benefitted from a number of partnerships with community agencies. During development of the program, HMMM-V personnel accompanied the Dallas Police Department’s Crisis Intervention Unit on typical homeless crisis services deployments into the field to learn about the locations and nature of encampments and homeless peregrination patterns in the Dallas area.
To aid in the design and selection of features for the mobile outreach vehicle, team members toured Homeless Outreach Medical Service mobile clinics from 2 local county hospitals, Parkland Hospital and John Peter Smith Hospital. The staff for these mobile clinics were interviewed about their experience with various components of their programs and their recommendations for optimal design of the mobile medical clinic for service delivery.
Numerous agencies in the Dallas area that serve the homeless population assisted with locating and connecting homeless veterans to HMMM-V programs. These partnering agencies also serve homeless individuals who do not qualify for the HMMM-V program, such as veterans with other-than-honorable military discharges.
The HMMM-V mobile outreach vehicle travels to partnering agencies and provides services on a recurring basis. These agencies are the Dallas International Street Church, a church and faith-based agency aiding the recovery of people with “broken lives”; Cornerstone Ministries, a church-based ministry serving people with adverse circumstances; and City Square’s Opportunity Center, human services and community development programs for low-income city residents. The mobile clinic also travels regularly to other areas to serve homeless veterans residing in unsheltered locations, such as homeless encampments and under bridges.
Clinical Assessment
The project used a modification of the VA Personalized Health Inventory (PHI) for general veteran populations, which assesses 8 areas of self-identified needs to address the specific concerns of homeless veterans served by a mobile clinic.25 Version 19 of the PHI (revised September 18, 2012), the version of the instrument available to the team at the inception of the project, was deployed with the HMMM-V personnel into the field. It imposed a heavy interview time burden (several hours), and its content areas did not seem appropriate to address the immediate concerns of homeless populations (eg, sections pertaining to personal development through hobbies, recreation, or volunteering; healthy living spaces with plenty of lighting and color; “eating healthy, balanced meals with plenty of fruits and vegetables each day”).25
Based on HMMM-V personnel feedback, the team modified this tool and developed a patient-centered health inventory (P-CHI) for homeless veterans that was acceptable in length and applicable to the situational characteristics of homeless existence. The tool’s 10 “current and desired states” were revised to remove domains of exercise and flexibility, sleep and relaxation, and mind-body techniques. The intervention and prevention domains were combined. A material needs (clothing, furniture, transportation, financial benefits) domain was added, and a new domain on reducing alcohol/drug use was created by moving this material from the food and drink domain.
The remaining domains were modified to fit the homeless living situation (Food and Drink = Nutrition; Personal Development = Employment/Vocation; Family, Friends, and Co-Workers = Family/Social/Legal Support; Spirit and Soul = Personal/Spiritual Fulfillment; Surroundings = Housing). Current state ratings were revised to reflect level of satisfaction, and ratings of Desired State were replaced with level of importance.
The modifications resulted in 9 domains, which were assembled into a grid for efficient rating of both satisfaction and importance for each domain (rated 1 to 10, lowest to highest, respectively), followed by an instruction to mark an X in a designated space in all the domains with which the individual would like help (Table). The intent was to reduce the burden of the instrument by having the participant complete sections providing detailed information about only the domains selected by the participant.
The details of each domain in the original VA PHI tool were captured through open-ended questions in text responses provided by the veteran. Because open-ended text responses are not conducive for summarizing characteristics of the population served or for evaluating program activities, the detailed sections covering the domains were revised completely to capture data within categoric and numeric variables. Items from the validated Homeless Supplement Interview were added to collect information not provided in the Homeless Operations Management and Evaluation System interview that is routinely administered to all veterans accessing homeless VA services.26-28
The information collected in these domains cover duration of current homeless episode, lifetime number of homeless episodes, current living arrangements and dissatisfactions with these arrangements, frequency and source of meals, employment history and current work status, sources of income, special material needs, medical and dental problems and sources of care, current medications, mental health problems and sources of care, urgent mental health concerns, current amount and frequency of alcohol and drug use, substance abuse treatment history, relationships with family and intimate partners, legal assistance needs, and self-identified needs for spiritual and personal fulfillment. This instrument is available on request to the authors.
Veterans Served
The project began with 1 team of professionals deploying with the HMMM-V vehicle while a second team was being assembled. Currently, the 2 HMMM-V teams deploy the mobile clinic 4 days per week. The mobile clinic visits agencies that serve the homeless, including emergency shelters and food ministries, as well as homeless encampments. To date, 195 homeless veterans have been served by the mobile clinic, 111 were currently enrolled with the VA, 8 were not enrolled but eligible for services, and 77 were not eligible for VA services. Of the unenrolled veterans, those eligible for services were offered VA enrollment assistance; those ineligible for VA services were offered a community referral.
For the veterans encountered in the field, the following interventions were provided: 49 housing placement referrals, 4 rental assistance referrals, 4 legal referrals, 27 medical care interventions, 13 dental referrals, 11 vision/hearing referrals, 12 mental health interventions, 9 substance abuse treatment referrals, 14 employment assistance referrals, 13 disability benefit applications, 18 transportation assists, 23 goods delivered, and 159 information assists. The HMMM-V mobile clinic also is deployed to participate in various educational and outreach events. At the time this article was written, the mobile clinic has reached nearly 2,000 veterans and community partners in at least 25 such events.
Of the veterans served to date, 73 completed the P-CHI. These veterans were predominantly male (77%), and the majority (60%) were black. The median age of the sample was 58 years, and typically they had a high school level of education (12.7; SD, 2.1 mean years of education). About half (49%) the sample were separated or divorced, and only a minority were currently married (8%). Half (50%) the sample served in the U.S. Army, with the post-Vietnam era being the era of service most represented (19%). Few (21%) veterans reported exposure to hostile or friendly fire during their service. More than three-fourths (80%) of the sample had experienced a homeless episode prior to their current one. On average, members of the sample had experienced a median of 3 lifetime homeless episodes. They had a mean 4.1 (SD, 5.8) lifetime number of years of homelessness, and 3.0 (SD, 5.2) years in their current homeless episode. Nearly one-third (31%) reported that they were currently staying in a homeless shelter, and nearly one-sixth (16%) were currently unsheltered in street settings, such as under bridges or in outdoor encampments at the time of the initial visit.
The mean number of minutes spent completing the P-CHI was 18.5 (SD, 9.4). The veterans indicated that they would like assistance with a mean 3.2 (SD, 2.2) number of domains. The domains with the highest average importance ratings were housing (mean, 9.4; SD, 1.7) and medical/dental care (mean, 8.9; SD, 2.2); the domains with the lowest average importance rating were reducing alcohol/drug use (mean, 6.4; SD, 4.1) and employment/vocation (mean, 6.3; SD, 4.2). The domains with the highest average satisfaction ratings were personal/spiritual fulfillment (mean, 7.3; SD, 2.9) and reducing substance use (mean, 5.9; SD, 4.0), and the domains with the lowest average satisfaction ratings were housing (mean, 2.9; SD, 2.9), material needs (mean, 4.2; SD, 3.3), and employment/vocation (mean, 4.2; SD, 3.2). The domain with the greatest indication of desire for help was housing, endorsed by more than four-fifths (84%) of the sample. This highly endorsed housing domain also was one of the lowest in satisfaction. The domains with the least expressed interest in obtaining help were reducing substance use (18%) and personal/spiritual fulfillment (15%).Reducing substance abuse also was one of the lowest domains of importance and the least for dissatisfaction.
Challenges and Barriers
As anticipated from its inception, this project encountered many challenges and barriers. The first was with the design, construction, and delivery of the mobile clinic unit. The vehicle took more than 2 years to be delivered. There were delays in progress necessitated by required selection of an approved vendor to build the vehicle, extensive specification of details and features, and stocking it with equipment and supplies. The weight of the unit had to be < 26,000 pounds to avoid the requirement of a commercial driver’s license, which limited the size of the vehicle to 28 feet. Stocking the unit with equipment and supplies required attention to a myriad of specifications and decisions. For example, separate refrigerators were needed for specimens, medications, and food; pharmaceutical regulations governing medications in mobile clinics required strict adherence; and difficulties were encountered in attempting to establish adequate and secure connectivity for communications devices in the field.
Once the mobile unit was delivered and prepared for deployment, the next set of challenges pertained to learning all of the instructions required to operate and drive the vehicle and learning how to maneuver the vehicle in the field. Specific challenges for driving the vehicle encountered included unexpectedly low overpasses that prohibited passage, narrow spaces for passage, rough and uneven terrain in off-road settings, and lateral and vertical tilt of roads creating potential for sideswipes and undercarriage scrapes. Maintenance schedules needed to be developed and implemented for cleaning the unit, inspection compliance, repairs, refueling, and emptying waste materials.
Staffing the vehicle required the development of unique job specifications addressing special expertise in accessing VA databases for veteran verification and registration and for driving the mobile clinic vehicle. Schedules and deployment plans for 2 teams that shared the same vehicle had to be established and followed. Locating veterans in unsheltered settings, such as under bridges and in encampments, required community intelligence facilitated through partnerships with knowledgeable members of the Dallas police crisis unit and by gaining field experience to locate where the usual homeless gathering places are, especially those inhabited by veterans. Safety of team members and equipment/supplies in the field was paramount from the start, and additional steps beyond safety training required extra measures, such as special care in navigating known dangerous areas. Provision of services necessitated completion of everything needed in a single visit due to the likelihood of loss to follow-up and acceptance of the limited types of service that could be provided in a mobile clinic. Special procedures were needed to provide referrals to sources of available care for non-VA-qualifying veterans.
Discussion
The HMMM-V program for delivery of PCC to homeless veterans is an innovative pilot program designed to connect with difficult-to-reach homeless veterans and engage them in care. The deliverables provided by this project are (1) A mobile outreach vehicle to deliver care to homeless veterans and outreach to other veterans and community agencies in North Texas; (2) The P-CHI assessment tool for homeless veterans modified and adapted for use with this special population; and (3) pilot data on its first cohort of homeless veterans served, describing their baseline characteristics and their stated satisfaction and preferences about their goals and aspirations for their physical, emotional, and mental health and well-being.
The HMMM-V program successfully identified homeless veterans in need of services, and more than one-third of these veterans were not previously engaged in VA services. Compared with the “typical” veterans served at VANTHCS homeless programs, veterans served by the HMMM-V comprised a greater proportion of minorities and a higher proportion who had been exposed to combat.29 Age and gender characteristics were similar.29 When compared with veterans who access care at VANTHCS and have not experienced homelessness, those served by the HMMM-V were younger and more likely to belong to a minority group; however, they were similar in combat exposure and gender.1 The veterans served by the HMMM-V program also were considerably older and had more homeless chronicity than did nonveteran homeless populations, consistent with other research.4,29,30
The veterans served by the HMMM-V program not surprisingly made housing their top priority in need of help, consistent with the Housing First model.22,31 They also indicated that employment/vocation and reducing substance use were of lower importance. Need for assistance with reducing substance use and social support were the domains least often identified as areas where help was needed, which seems inconsistent with the higher established rates of substance abuse problems among homeless veterans.1
With additional fieldwork, the HMMM-V program is expected to allow refinement of procedures for identifying and serving veterans from a patient-centered care perspective. The P-CHI will be further tested and developed, and the next step will be to create and pilot intervention templates for a Patient-Centered Health Improvement Plan, based on the P-CHI results. This process parallels the original development treatment plans for the VA’s Personalized Health Plan based on the PHI.25 Once the HMMM-V program is fully established in Dallas, the plans are for an expansion that will cover a broader geographic area in North Texas that includes rural areas.
The HMMM-V program was designed to address the barriers to health care that are encountered by homeless veterans. It is unique in homeless veteran care due to its patient-centered approach that partners with homeless veterans to prioritize their needs as determined by them rather than based solely on policies or provider conceptualizations of their needs. Access to services, engagement in care, and successful utilization of needed services may lead to measurable improvements in health care outcomes among homeless populations of veterans. Desired goals include remission of illness through appropriate medical intervention, preventing morbidity, achieving healthy lifestyles, recovery from addiction, stabilization of psychiatric illness, and attainment of stable housing.
The first hurdle for implementing this type of program in other settings is the identification of resources needed for these efforts. Need of additional staffing resources, however, may be circumvented by allowing employees working in other areas to rotate in community outreach shifts in the mobile unit. Another hurdle encountered in implementation of the HMMM-V initiative was the initial difficulty finding homeless veterans in community settings, especially those in unsheltered locations. The HMMM-V program addressed this issue by partnering with other agencies serving the homeless in the community. Therefore, a general recommendation for other entities seeking to implement this type of program is to reach out to these community partners from the outset.
Conclusion
The HMMM-V has the potential to engage the most difficult-to-reach homeless veterans in need of health services by delivering care and providing resources in challenging environments. Further work is needed to validate the P-CHI for use with this program and to conduct well-designed and implemented research to demonstrate effectiveness of this intervention on veteran outcomes, especially quality of life. Once this additional work is accomplished, this innovative program can potentially be implemented by VAMCs across the nation, and potentially in more general community care settings, to more effectively reach out and deliver services to homeless members of the community.
Acknowledgments
Grant support was received from the Department of Veterans Affairs, Office of Patient Centered Care. The authors would like to acknowledge all the clinicians, trainees, and support staff who have contributed to the success of the HMMM-V program: Tara Ayala, Jose Cabrera, Tony Castillo, Rachael Lynn David, Teresa DeShazo, Sylvia Figueroa, Steven Fisher, Eric Gary, Evelyn Gibbs, Kevin Hosey, JoAnn Joseph, Taly Drimer Kagan, Miranda Kelly, Michelle King-Thompson, Sharon Marcus, Shiji Mathew, Moneeza Matin, John Moreno, Joseph Neifert, Joel Price, Tiffany Price, Natalie Qualls, Reginald Robertson, Kristine Rodrigues, Jon Saffelder, Jill Stokes, Scott Stone, and John Smith.
Research has consistently identified remarkably high rates of addiction, mental illness, and health problems in the homeless population.1-9 Yet in spite of extensive service needs for these problems, abundant evidence exists of consistent underuse of health care services by homeless populations.10-12 Most of the homeless population reside in emergency shelters or in transitional or supportive housing, but many remain in places not meant for human habitation.
Homelessness is significantly overrepresented among military veterans.13 The January 2016 national point-in-time count identified 39,471 veterans experiencing homelessness.13 Iraq and Afghanistan veterans seem to have an especially high risk for homelessness.13-15 Disheartening statistics such as these prompted former VA Secretary Eric Shinseki to pledge to end veteran homelessness by December 2015.16 He argued in support of this mission that 85% of veteran homeless resources go to health care—implying that homelessness among veterans is primarily a health care issue, which is heavily burdened by substance abuse and other psychiatric and medical illnesses.17
Health care service use has been associated with improved health, mental health, and outcomes among homeless populations.12,18 Unfortunately, access to these services is limited by barriers associated with homelessness, such as transportation or lack of proper identification.19,20 Veterans experiencing homelessness also face these common barriers to health care, and unsheltered veterans especially underutilize VA health care services.21
Housing First—a successful model that places individuals into housing without prerequisites for sobriety, active participation in treatment, or other behavioral accomplishments, such as gainful employment—has not managed yet to place all the disengaged homeless veteran population into stable housing.22 However, the Housing First model, which is based on the individual’s priorities, is consistent with the approach of a new program at the VA North Texas Health Care System (VANTHCS).
The VHA, similar to other health care systems, is engaged in a cultural transformation to convert its health care approach from a traditional medical model to patient-centered care (PCC).23 In this priority area, a strategic objective is for the VHA to partner with each veteran to create a personalized, proactive strategy to optimize health and well-being and when needed provide state-of-the-art disease management. Patient-centered care is designed to address veterans’ specific needs in spiritual, environmental, physical, mental, and social domains and empower veterans to become active participants in their care. Patient-centered care differs from the traditional medical model in that patients are active participants in their treatment, partnering and collaborating with their providers on care that is quality-of-life centered instead of disease centered.23 This model is based on both respect for patients as unique individuals and on the obligation to care for them on their own terms, focused on their self-identified goals and aspirations.24
At VANTHCS, the Homeless Mobile Medical/Mental Veteran (HMMM-V) pilot program was designed to deliver effective health care services to a homeless subpopulation of veterans who historically have been the most difficult to serve—those living in unsheltered environments, such as under bridges and in encampments. The purpose of the HMMM-V program was to contact and serve veterans not currently being reached by the VA system of care, using a PCC model.
This pilot program was initially funded in January 2013 by a 2-year grant from the Office of Patient Centered Care and Cultural Transformation to apply the PCC approach to engage veteran participation. For this project, the VA Personal Health Inventory tool—originally designed for use with the general veteran population—was adapted for use with the homeless veteran population. The grant funding period covered the design, development, and implementation of the HMMM-V program; thereafter, VANTHCS provided resources through its Comprehensive Homeless Center Programs to assure its sustainability and continued use of the clinical assessment tool created for this project.
This article describes the development and implementation of this novel program with sufficient detail to inform the development of similar programs in other sites. Descriptions of the program and staffing, creation of community partnerships, and modification of an assessment instrument are provided. It also illustrates the original implementation period of the HMMM-V program through presentation of self-reported data on the first homeless veterans it served.
Equipment and Staffing
A custom 28-foot mobile outreach vehicle was assembled according to specifications identified by the HMMM-V team as necessary to conduct the program’s interventions. The van became fully operational on April 8, 2015, after it underwent all the required reviews and inspections (eg, safety, infection control, etc) and was accredited in 2015 by the Commission on Accreditation of Rehabilitation Facilities.
The HMMM-V van has a driver compartment that is separate from its services rooms, which include a patient registration area, a fully equipped examination room, a laboratory area, and a bathroom. The vehicle is equipped with a wheelchair lift and an awning to shade outdoor areas where tables and chairs are set up for patient/staff waiting and rest areas. The vehicle is stocked with essential equipment and supplies needed to conduct work in off-street locations, vacant lots, under bridges, fields, unpaved paths, etc. It also is equipped with telemedicine capabilities to provide clinical supervision and access to attending physicians and specialists at VANTHCS. Personnel carry cell phones and laptop computers with secure Internet connections using a commercially available mobile wireless Wi-Fi hotspot to facilitate documentation of medical records and communication from the field.
This reliable type of equipment is routine for use in VA field operations; the only hurdle using these technologies for the program was acquiring funding and purchasing the equipment. The vehicle is further equipped with a refrigerator solely for secure storage of pharmaceutical supplies, a second refrigerator for specimens, and wall-mounted blood pressure and otoscope/ophthalmoscope units. The vehicle is supplied with thermometers, scales, phlebotomy supplies, and first-aid kits and is stocked with vaccines and medications, including antibiotic, hypertensive, diabetic, allergy, and over-the-counter pain medications. A more comprehensive list of supplies for the vehicle is available from the authors on request.
Medication provisions supplied to the HMMM-V mobile clinic conform to the Texas State Board of Pharmacy compliance regulations. Because the vehicle is designated as federal property and has U.S. government license plates, it is considered an extension of VANTHCS Pharmacy Service and falls under its pharmacy license. A medication formulary was created with input from HMMM-V prescribers and Dallas VAMC Pharmacy Service pharmacists. To safeguard the integrity of these pharmaceutical agents, the HMMM-V physician assistant picks up the medications before field deployment and returns the unused medications to the Dallas VAMC at the end of the day. The medications are transported in locked containers and placed either in a locked medication refrigerator or cabinet on the mobile unit.
For medication prescriptions that need laboratory testing before prescribing them, HMMM-V prescribers can check the VA electronic medical record from the field to determine whether these tests have been completed recently. If not, then HMMM-V team has an agreement with Dallas VA Pathology and Laboratory Medicine Service for testing samples obtained in the field.
The program was designed for staffing of the vehicle by 2 professional teams, each includes medical (physician’s assistant or registered nurse), mental health (psychiatrist, residents), and social work providers (licensed social workers, clinical social workers); trainees of these disciplines; a peer support specialist; and an administrative clerk. The staffing varies daily, depending on available personnel. When personnel deploy to the field, they go in pairs or groups to address potential safety issues. Cell phones are available to summon police or ambulance services in an emergency. Systematic safety training was conducted with all field personnel before their first deployment to guard against vulnerability to danger in these settings.
Once in the field, personnel engage unsheltered homeless individuals to assess eligibility for VA services. Veterans found ineligible are assisted with application for military discharge upgrade, service-connected compensation, or appeal for health care coverage. Veterans eligible for VA care receive physical examinations, vital and glucose checks, influenza and pneumonia vaccinations, first-aid skin and wound care, medication management with limited medications provided at point of care, blood and urine testing, peer support services, suicide assessments, clinical mental health evaluations, and social work services through the HMMM-V program.
Social work assistance provided includes psychosocial assessment and care coordination for psychosocial needs such as mental health, substance abuse, vision, dental, housing, employment, legal aid, transportation, food, income, hygiene, and weather-appropriate provision needs.
Community Partnerships
The HMMM-V program benefitted from a number of partnerships with community agencies. During development of the program, HMMM-V personnel accompanied the Dallas Police Department’s Crisis Intervention Unit on typical homeless crisis services deployments into the field to learn about the locations and nature of encampments and homeless peregrination patterns in the Dallas area.
To aid in the design and selection of features for the mobile outreach vehicle, team members toured Homeless Outreach Medical Service mobile clinics from 2 local county hospitals, Parkland Hospital and John Peter Smith Hospital. The staff for these mobile clinics were interviewed about their experience with various components of their programs and their recommendations for optimal design of the mobile medical clinic for service delivery.
Numerous agencies in the Dallas area that serve the homeless population assisted with locating and connecting homeless veterans to HMMM-V programs. These partnering agencies also serve homeless individuals who do not qualify for the HMMM-V program, such as veterans with other-than-honorable military discharges.
The HMMM-V mobile outreach vehicle travels to partnering agencies and provides services on a recurring basis. These agencies are the Dallas International Street Church, a church and faith-based agency aiding the recovery of people with “broken lives”; Cornerstone Ministries, a church-based ministry serving people with adverse circumstances; and City Square’s Opportunity Center, human services and community development programs for low-income city residents. The mobile clinic also travels regularly to other areas to serve homeless veterans residing in unsheltered locations, such as homeless encampments and under bridges.
Clinical Assessment
The project used a modification of the VA Personalized Health Inventory (PHI) for general veteran populations, which assesses 8 areas of self-identified needs to address the specific concerns of homeless veterans served by a mobile clinic.25 Version 19 of the PHI (revised September 18, 2012), the version of the instrument available to the team at the inception of the project, was deployed with the HMMM-V personnel into the field. It imposed a heavy interview time burden (several hours), and its content areas did not seem appropriate to address the immediate concerns of homeless populations (eg, sections pertaining to personal development through hobbies, recreation, or volunteering; healthy living spaces with plenty of lighting and color; “eating healthy, balanced meals with plenty of fruits and vegetables each day”).25
Based on HMMM-V personnel feedback, the team modified this tool and developed a patient-centered health inventory (P-CHI) for homeless veterans that was acceptable in length and applicable to the situational characteristics of homeless existence. The tool’s 10 “current and desired states” were revised to remove domains of exercise and flexibility, sleep and relaxation, and mind-body techniques. The intervention and prevention domains were combined. A material needs (clothing, furniture, transportation, financial benefits) domain was added, and a new domain on reducing alcohol/drug use was created by moving this material from the food and drink domain.
The remaining domains were modified to fit the homeless living situation (Food and Drink = Nutrition; Personal Development = Employment/Vocation; Family, Friends, and Co-Workers = Family/Social/Legal Support; Spirit and Soul = Personal/Spiritual Fulfillment; Surroundings = Housing). Current state ratings were revised to reflect level of satisfaction, and ratings of Desired State were replaced with level of importance.
The modifications resulted in 9 domains, which were assembled into a grid for efficient rating of both satisfaction and importance for each domain (rated 1 to 10, lowest to highest, respectively), followed by an instruction to mark an X in a designated space in all the domains with which the individual would like help (Table). The intent was to reduce the burden of the instrument by having the participant complete sections providing detailed information about only the domains selected by the participant.
The details of each domain in the original VA PHI tool were captured through open-ended questions in text responses provided by the veteran. Because open-ended text responses are not conducive for summarizing characteristics of the population served or for evaluating program activities, the detailed sections covering the domains were revised completely to capture data within categoric and numeric variables. Items from the validated Homeless Supplement Interview were added to collect information not provided in the Homeless Operations Management and Evaluation System interview that is routinely administered to all veterans accessing homeless VA services.26-28
The information collected in these domains cover duration of current homeless episode, lifetime number of homeless episodes, current living arrangements and dissatisfactions with these arrangements, frequency and source of meals, employment history and current work status, sources of income, special material needs, medical and dental problems and sources of care, current medications, mental health problems and sources of care, urgent mental health concerns, current amount and frequency of alcohol and drug use, substance abuse treatment history, relationships with family and intimate partners, legal assistance needs, and self-identified needs for spiritual and personal fulfillment. This instrument is available on request to the authors.
Veterans Served
The project began with 1 team of professionals deploying with the HMMM-V vehicle while a second team was being assembled. Currently, the 2 HMMM-V teams deploy the mobile clinic 4 days per week. The mobile clinic visits agencies that serve the homeless, including emergency shelters and food ministries, as well as homeless encampments. To date, 195 homeless veterans have been served by the mobile clinic, 111 were currently enrolled with the VA, 8 were not enrolled but eligible for services, and 77 were not eligible for VA services. Of the unenrolled veterans, those eligible for services were offered VA enrollment assistance; those ineligible for VA services were offered a community referral.
For the veterans encountered in the field, the following interventions were provided: 49 housing placement referrals, 4 rental assistance referrals, 4 legal referrals, 27 medical care interventions, 13 dental referrals, 11 vision/hearing referrals, 12 mental health interventions, 9 substance abuse treatment referrals, 14 employment assistance referrals, 13 disability benefit applications, 18 transportation assists, 23 goods delivered, and 159 information assists. The HMMM-V mobile clinic also is deployed to participate in various educational and outreach events. At the time this article was written, the mobile clinic has reached nearly 2,000 veterans and community partners in at least 25 such events.
Of the veterans served to date, 73 completed the P-CHI. These veterans were predominantly male (77%), and the majority (60%) were black. The median age of the sample was 58 years, and typically they had a high school level of education (12.7; SD, 2.1 mean years of education). About half (49%) the sample were separated or divorced, and only a minority were currently married (8%). Half (50%) the sample served in the U.S. Army, with the post-Vietnam era being the era of service most represented (19%). Few (21%) veterans reported exposure to hostile or friendly fire during their service. More than three-fourths (80%) of the sample had experienced a homeless episode prior to their current one. On average, members of the sample had experienced a median of 3 lifetime homeless episodes. They had a mean 4.1 (SD, 5.8) lifetime number of years of homelessness, and 3.0 (SD, 5.2) years in their current homeless episode. Nearly one-third (31%) reported that they were currently staying in a homeless shelter, and nearly one-sixth (16%) were currently unsheltered in street settings, such as under bridges or in outdoor encampments at the time of the initial visit.
The mean number of minutes spent completing the P-CHI was 18.5 (SD, 9.4). The veterans indicated that they would like assistance with a mean 3.2 (SD, 2.2) number of domains. The domains with the highest average importance ratings were housing (mean, 9.4; SD, 1.7) and medical/dental care (mean, 8.9; SD, 2.2); the domains with the lowest average importance rating were reducing alcohol/drug use (mean, 6.4; SD, 4.1) and employment/vocation (mean, 6.3; SD, 4.2). The domains with the highest average satisfaction ratings were personal/spiritual fulfillment (mean, 7.3; SD, 2.9) and reducing substance use (mean, 5.9; SD, 4.0), and the domains with the lowest average satisfaction ratings were housing (mean, 2.9; SD, 2.9), material needs (mean, 4.2; SD, 3.3), and employment/vocation (mean, 4.2; SD, 3.2). The domain with the greatest indication of desire for help was housing, endorsed by more than four-fifths (84%) of the sample. This highly endorsed housing domain also was one of the lowest in satisfaction. The domains with the least expressed interest in obtaining help were reducing substance use (18%) and personal/spiritual fulfillment (15%).Reducing substance abuse also was one of the lowest domains of importance and the least for dissatisfaction.
Challenges and Barriers
As anticipated from its inception, this project encountered many challenges and barriers. The first was with the design, construction, and delivery of the mobile clinic unit. The vehicle took more than 2 years to be delivered. There were delays in progress necessitated by required selection of an approved vendor to build the vehicle, extensive specification of details and features, and stocking it with equipment and supplies. The weight of the unit had to be < 26,000 pounds to avoid the requirement of a commercial driver’s license, which limited the size of the vehicle to 28 feet. Stocking the unit with equipment and supplies required attention to a myriad of specifications and decisions. For example, separate refrigerators were needed for specimens, medications, and food; pharmaceutical regulations governing medications in mobile clinics required strict adherence; and difficulties were encountered in attempting to establish adequate and secure connectivity for communications devices in the field.
Once the mobile unit was delivered and prepared for deployment, the next set of challenges pertained to learning all of the instructions required to operate and drive the vehicle and learning how to maneuver the vehicle in the field. Specific challenges for driving the vehicle encountered included unexpectedly low overpasses that prohibited passage, narrow spaces for passage, rough and uneven terrain in off-road settings, and lateral and vertical tilt of roads creating potential for sideswipes and undercarriage scrapes. Maintenance schedules needed to be developed and implemented for cleaning the unit, inspection compliance, repairs, refueling, and emptying waste materials.
Staffing the vehicle required the development of unique job specifications addressing special expertise in accessing VA databases for veteran verification and registration and for driving the mobile clinic vehicle. Schedules and deployment plans for 2 teams that shared the same vehicle had to be established and followed. Locating veterans in unsheltered settings, such as under bridges and in encampments, required community intelligence facilitated through partnerships with knowledgeable members of the Dallas police crisis unit and by gaining field experience to locate where the usual homeless gathering places are, especially those inhabited by veterans. Safety of team members and equipment/supplies in the field was paramount from the start, and additional steps beyond safety training required extra measures, such as special care in navigating known dangerous areas. Provision of services necessitated completion of everything needed in a single visit due to the likelihood of loss to follow-up and acceptance of the limited types of service that could be provided in a mobile clinic. Special procedures were needed to provide referrals to sources of available care for non-VA-qualifying veterans.
Discussion
The HMMM-V program for delivery of PCC to homeless veterans is an innovative pilot program designed to connect with difficult-to-reach homeless veterans and engage them in care. The deliverables provided by this project are (1) A mobile outreach vehicle to deliver care to homeless veterans and outreach to other veterans and community agencies in North Texas; (2) The P-CHI assessment tool for homeless veterans modified and adapted for use with this special population; and (3) pilot data on its first cohort of homeless veterans served, describing their baseline characteristics and their stated satisfaction and preferences about their goals and aspirations for their physical, emotional, and mental health and well-being.
The HMMM-V program successfully identified homeless veterans in need of services, and more than one-third of these veterans were not previously engaged in VA services. Compared with the “typical” veterans served at VANTHCS homeless programs, veterans served by the HMMM-V comprised a greater proportion of minorities and a higher proportion who had been exposed to combat.29 Age and gender characteristics were similar.29 When compared with veterans who access care at VANTHCS and have not experienced homelessness, those served by the HMMM-V were younger and more likely to belong to a minority group; however, they were similar in combat exposure and gender.1 The veterans served by the HMMM-V program also were considerably older and had more homeless chronicity than did nonveteran homeless populations, consistent with other research.4,29,30
The veterans served by the HMMM-V program not surprisingly made housing their top priority in need of help, consistent with the Housing First model.22,31 They also indicated that employment/vocation and reducing substance use were of lower importance. Need for assistance with reducing substance use and social support were the domains least often identified as areas where help was needed, which seems inconsistent with the higher established rates of substance abuse problems among homeless veterans.1
With additional fieldwork, the HMMM-V program is expected to allow refinement of procedures for identifying and serving veterans from a patient-centered care perspective. The P-CHI will be further tested and developed, and the next step will be to create and pilot intervention templates for a Patient-Centered Health Improvement Plan, based on the P-CHI results. This process parallels the original development treatment plans for the VA’s Personalized Health Plan based on the PHI.25 Once the HMMM-V program is fully established in Dallas, the plans are for an expansion that will cover a broader geographic area in North Texas that includes rural areas.
The HMMM-V program was designed to address the barriers to health care that are encountered by homeless veterans. It is unique in homeless veteran care due to its patient-centered approach that partners with homeless veterans to prioritize their needs as determined by them rather than based solely on policies or provider conceptualizations of their needs. Access to services, engagement in care, and successful utilization of needed services may lead to measurable improvements in health care outcomes among homeless populations of veterans. Desired goals include remission of illness through appropriate medical intervention, preventing morbidity, achieving healthy lifestyles, recovery from addiction, stabilization of psychiatric illness, and attainment of stable housing.
The first hurdle for implementing this type of program in other settings is the identification of resources needed for these efforts. Need of additional staffing resources, however, may be circumvented by allowing employees working in other areas to rotate in community outreach shifts in the mobile unit. Another hurdle encountered in implementation of the HMMM-V initiative was the initial difficulty finding homeless veterans in community settings, especially those in unsheltered locations. The HMMM-V program addressed this issue by partnering with other agencies serving the homeless in the community. Therefore, a general recommendation for other entities seeking to implement this type of program is to reach out to these community partners from the outset.
Conclusion
The HMMM-V has the potential to engage the most difficult-to-reach homeless veterans in need of health services by delivering care and providing resources in challenging environments. Further work is needed to validate the P-CHI for use with this program and to conduct well-designed and implemented research to demonstrate effectiveness of this intervention on veteran outcomes, especially quality of life. Once this additional work is accomplished, this innovative program can potentially be implemented by VAMCs across the nation, and potentially in more general community care settings, to more effectively reach out and deliver services to homeless members of the community.
Acknowledgments
Grant support was received from the Department of Veterans Affairs, Office of Patient Centered Care. The authors would like to acknowledge all the clinicians, trainees, and support staff who have contributed to the success of the HMMM-V program: Tara Ayala, Jose Cabrera, Tony Castillo, Rachael Lynn David, Teresa DeShazo, Sylvia Figueroa, Steven Fisher, Eric Gary, Evelyn Gibbs, Kevin Hosey, JoAnn Joseph, Taly Drimer Kagan, Miranda Kelly, Michelle King-Thompson, Sharon Marcus, Shiji Mathew, Moneeza Matin, John Moreno, Joseph Neifert, Joel Price, Tiffany Price, Natalie Qualls, Reginald Robertson, Kristine Rodrigues, Jon Saffelder, Jill Stokes, Scott Stone, and John Smith.
1. LePage JP, Bradshaw LD, Cipher DJ, Crawford AM, Hooshyar D. The effects of homelessness on veterans’ health care service use: an evaluation of independence from comorbidities. Public Health. 2014;128(11):985-992.
2. Fischer PJ, Breakey WR. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol. 1991;46(11):1115-1128.
3. Robertson MJ, Zlotnick C, Westerfelt A. Drug use disorders and treatment contact among homeless adults in Alameda County, California. Am J Public Health. 1997;87(2):221-228.
4. North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? Am J Public Health. 2004;94(1):103-108.
5. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225.
6. Harpaz-Rotem I, Rosenheck RA, Desai R. The mental health of children exposed to maternal mental illness and homelessness. Community Ment Health J. 2006;42(5):437-448.
7. Pollio DE, Eyrich-Garg KM, North CS. The homeless. In: Johnson BA, ed. Addiction Medicine: Science and Practice. New York, NY: Springer; 2011:1487-1504.
8. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
9. Baggett TP, Singer DE, Rao SR, O’Connell JJ, Bharel M, Rigotti NA. Food insufficiency and health services utilization in a national sample of homeless adults. J Gen Intern Med. 2011;26(6):627-634.
10. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376.
11. Fuehrlein BS, Cowell AJ, Pollio D, Cupps L, Balfour ME, North CS. A prospective study of the associations among housing status and costs of services in a homeless population. Psychiatr Serv. 2015;66(1):27-32.
12. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
13. U.S. Department of Housing and Urban Development Office of Community Planning and Development. The 2016 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: point-in-time estimates of homelessness. https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Published 2016. Accessed August 7, 2017.
14. Tsai J, Rosenheck RA. Risk factors for homelessness among U.S. veterans. Epidemiol Rev. 2015;37:177-195.
15. Williamson V, Mulhall E. Coming home: the housing crisis and homelessness threaten new veterans. Iraq and Afghanistan Veterans of America, January, 2009. http://media.iava.org/IAVA_coming_home_2009%20The%20Housing%20Crisis%20and%20Homelessness%20Threaten%20New%20Veterans.pdf. Accessed August 10, 2017
16. Shinseki EK. Remarks by Secretary Eric K. Shinseki. National Summit on Homeless Veterans; November 3, 2009; Washington, DC. https://www.va.gov/opa/speeches/2009/09_1103.asp. Updated August 8, 2016. Accessed August 7, 2017.
17. Shinseki EK. Remarks by Secretary Eric K. Shinseki. 2014 National Coalition for Homeless Veterans Annual Meeting; May 30, 2014; Arlington, VA. https://www.va.gov/opa/speeches/2014/05_30_2014.asp. Updated April 21, 2015. Accessed August 7, 2017.
18. Pollio DE, Spitznagel EL, North CS, Thompson S, Foster DA. Service use over time and achievement of stable housing in a mentally ill homeless population. Psychiatr Serv. 2000;51(12):1536-1543.
19. Page J. Barriers to transferring care of homeless people with serious mental illnesses to community mental health organizations: perspectives of street-based programs. Best Practices in Mental Health: An International Journal. 2007;3(1):26.
20. Young AS, Chinman MJ, Cradock-O’Leary JA, et al. Characteristics of individuals with severe mental illness who use emergency services. Community Ment Health J. 2005;41(2):159-168.
21. Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461.
22. Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651-656.
23. U.S. Department of Veterans Affairs, Veterans Health Administration. VA Patient Centered Care. http://www.va.gov/patientcenteredcare. Updated July 24,2017. Accessed August 7, 2017.
24. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
25. U.S. Department of Veterans Affairs, Office of Patient Centered Care and Cultural Transformation. My story: personal health inventory. https://www.va.gov/PATIENTCENTEREDCARE/docs/VA-OPCC-Personal-Health-Inventory-final-508.pdf. Published October 7, 2013. Accessed August 7, 2017
26. North CS, Smith EM, Pollio DE. The Homeless Supplement to the Diagnostic Interview Schedule (DIS/HS). St. Louis: Washington University, 2004.
27. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The homeless supplement to the diagnostic interview schedule: test-retest analyses. Int J Methods Psychiatr Res. 2004;13(3):184-191.
28. LaSalle JL. Homeless Operations Management and Evaluation System (HOMES) user manual-phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed August 7, 2017.
29. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psychiatr Serv. 2014;65(6):751-757.
30. North CS, Smith EM. A comparison of homeless men and women: different populations, different needs. Community Ment Health J. 1993;29(5):423-431.
31. Kertesz SG, Austin EL, Holmes SK, et al. Making housing first happen: organizational leadership in VA’s expansion of permanent supportive housing. J Gen Intern Med. 2014;29(suppl 4):835-844.
1. LePage JP, Bradshaw LD, Cipher DJ, Crawford AM, Hooshyar D. The effects of homelessness on veterans’ health care service use: an evaluation of independence from comorbidities. Public Health. 2014;128(11):985-992.
2. Fischer PJ, Breakey WR. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol. 1991;46(11):1115-1128.
3. Robertson MJ, Zlotnick C, Westerfelt A. Drug use disorders and treatment contact among homeless adults in Alameda County, California. Am J Public Health. 1997;87(2):221-228.
4. North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? Am J Public Health. 2004;94(1):103-108.
5. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225.
6. Harpaz-Rotem I, Rosenheck RA, Desai R. The mental health of children exposed to maternal mental illness and homelessness. Community Ment Health J. 2006;42(5):437-448.
7. Pollio DE, Eyrich-Garg KM, North CS. The homeless. In: Johnson BA, ed. Addiction Medicine: Science and Practice. New York, NY: Springer; 2011:1487-1504.
8. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
9. Baggett TP, Singer DE, Rao SR, O’Connell JJ, Bharel M, Rigotti NA. Food insufficiency and health services utilization in a national sample of homeless adults. J Gen Intern Med. 2011;26(6):627-634.
10. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376.
11. Fuehrlein BS, Cowell AJ, Pollio D, Cupps L, Balfour ME, North CS. A prospective study of the associations among housing status and costs of services in a homeless population. Psychiatr Serv. 2015;66(1):27-32.
12. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
13. U.S. Department of Housing and Urban Development Office of Community Planning and Development. The 2016 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: point-in-time estimates of homelessness. https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Published 2016. Accessed August 7, 2017.
14. Tsai J, Rosenheck RA. Risk factors for homelessness among U.S. veterans. Epidemiol Rev. 2015;37:177-195.
15. Williamson V, Mulhall E. Coming home: the housing crisis and homelessness threaten new veterans. Iraq and Afghanistan Veterans of America, January, 2009. http://media.iava.org/IAVA_coming_home_2009%20The%20Housing%20Crisis%20and%20Homelessness%20Threaten%20New%20Veterans.pdf. Accessed August 10, 2017
16. Shinseki EK. Remarks by Secretary Eric K. Shinseki. National Summit on Homeless Veterans; November 3, 2009; Washington, DC. https://www.va.gov/opa/speeches/2009/09_1103.asp. Updated August 8, 2016. Accessed August 7, 2017.
17. Shinseki EK. Remarks by Secretary Eric K. Shinseki. 2014 National Coalition for Homeless Veterans Annual Meeting; May 30, 2014; Arlington, VA. https://www.va.gov/opa/speeches/2014/05_30_2014.asp. Updated April 21, 2015. Accessed August 7, 2017.
18. Pollio DE, Spitznagel EL, North CS, Thompson S, Foster DA. Service use over time and achievement of stable housing in a mentally ill homeless population. Psychiatr Serv. 2000;51(12):1536-1543.
19. Page J. Barriers to transferring care of homeless people with serious mental illnesses to community mental health organizations: perspectives of street-based programs. Best Practices in Mental Health: An International Journal. 2007;3(1):26.
20. Young AS, Chinman MJ, Cradock-O’Leary JA, et al. Characteristics of individuals with severe mental illness who use emergency services. Community Ment Health J. 2005;41(2):159-168.
21. Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461.
22. Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651-656.
23. U.S. Department of Veterans Affairs, Veterans Health Administration. VA Patient Centered Care. http://www.va.gov/patientcenteredcare. Updated July 24,2017. Accessed August 7, 2017.
24. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
25. U.S. Department of Veterans Affairs, Office of Patient Centered Care and Cultural Transformation. My story: personal health inventory. https://www.va.gov/PATIENTCENTEREDCARE/docs/VA-OPCC-Personal-Health-Inventory-final-508.pdf. Published October 7, 2013. Accessed August 7, 2017
26. North CS, Smith EM, Pollio DE. The Homeless Supplement to the Diagnostic Interview Schedule (DIS/HS). St. Louis: Washington University, 2004.
27. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The homeless supplement to the diagnostic interview schedule: test-retest analyses. Int J Methods Psychiatr Res. 2004;13(3):184-191.
28. LaSalle JL. Homeless Operations Management and Evaluation System (HOMES) user manual-phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed August 7, 2017.
29. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psychiatr Serv. 2014;65(6):751-757.
30. North CS, Smith EM. A comparison of homeless men and women: different populations, different needs. Community Ment Health J. 1993;29(5):423-431.
31. Kertesz SG, Austin EL, Holmes SK, et al. Making housing first happen: organizational leadership in VA’s expansion of permanent supportive housing. J Gen Intern Med. 2014;29(suppl 4):835-844.
Redesign of a Screening Process for VA Homeless Housing
Homelessness is associated with disproportionate medical morbidity and mortality and use of nonpreventive health services.1 In fiscal year 2010, veterans experiencing homelessness were 4 times more likely to use VA emergency departments and had a greater 10-year mortality risk than did veterans who were housed.1 Veterans experiencing homelessness were more likely to be diagnosed with substance use disorder, schizophrenia, liver disease, and/or HIV/AIDS than were their housed counterparts.
Ending veteran homelessness is a federal priority, exemplified by the goal of President Obama to end veteran homelessness by 2015.2 Since the goal’s articulation, veteran homelessness has declined nationally by 33% (24,117 veterans) from 2009 to 2014 however, 49,933 veterans were identified as being homeless on a given night in January 2014.3
Related: Landmark Initiative Signed for Homeless Veterans
A crucial element needed to end veteran homelessness is veteran and health care provider knowledge of existing homeless services and mechanisms of access. In 2012, VHA launched a homelessness screening clinical reminder in the Computerized Patient Record System (CPRS), which prompts a discussion of housing status between the veteran and provider.4 The staff of the VA North Texas Health Care System (VANTHCS) Comprehensive Homeless Center Programs (CHCP) realized that homeless housing programs at the facility could be more accessible if staff from each program could screen for all available programs and if a single phone number existed for scheduling appointments. Therefore, VANTHCS transformed its homeless housing screening process to a standardized process through which veterans are screened for all CHCP housing programs during a single screening assessment, Universal Homeless Housing Screening (UHHS).
This article describes the creation of the UHHS, the screening tool, 3-month postimplementation findings, and recommendations based on initial VANTHCS staff experiences with this process. During the redesign of screening process for homeless housing, VANTHCS staff found a paucity of guidance regarding best practices. This article attempts to fill this gap and provide guidance to institutions that are considering standardizing their screening process for homeless housing across multiple programs at different locations.
Background
Established in 1990, VANTHCS CHCP is VA’ s first comprehensive homeless center. The CHCP provides both housing and vocational rehabilitation programs, including 13 housing programs in 6 different cities and long-standing partnerships between CHCP and 3 community agencies whose programs have specific housing for veterans.5 Screenings performed in Dallas, Texas, for CHCP housing programs are completed at 4 separate locations.
Prior to the inception of the UHHS process, access to housing programs was limited by veteran awareness of the programs and transportation to various program locations. To participate in these programs, veterans needed to complete a form for the VA Northeast Program Evaluation Center (NEPEC), which staff at the Healthcare for Homeless Veterans (HCHV) CHCP program could administer. This process created an admission bottleneck, because HCHV staff needed to evaluate veterans even if they were being admitted to non-HCHV programs.
UHHS Creation Process
In 2011, NEPEC launched the electronic Homeless Operations Management and Evaluation System (HOMES) to replace paper-based reporting.6 This tool allowed non-HCHV CHCP staff to complete NEPEC evaluation and allowed CHCP to meet its goal of designing a system where all CHCP housing programs could complete a screening assessment. This goal originated from the desire of then CHCP Director Teresa House-Hatfield to create a more efficient housing screening process and from similar feedback from veterans.
Furthermore, in 2009, then Secretary of Veterans Affairs Eric K. Shinseki described a “no wrong door” philosophy for ending veteran homelessness, which CHCP operationalized by screening veterans for any CHCP housing program regardless of initial point of contact within the CHCP system.2 Subsequently, in 2010, the VA Office of Mental Health Services contracted with Mathematica Policy Research, Inc., to conduct a quality review of VA Mental Health Residential Rehabilitation Treatment Programs. Notable among their recommendations was to create a one-stop screening process for these programs.
Related: Primary Care Medical Services for Homeless Veterans
In 2010, CHCP embarked on a process to transform the facility’s screening procedure to a one-stop assessment with standardized screening questions and create a systematic process to track outcomes across all CHCP housing programs. The new process allowed for a standardized appeal procedure when eligibility for a program was not met. It also improved the ease of communication by having 1 phone number for making appointments or informing about screening times. These changes were enacted without the addition of any new staff positions. Instead, in October 2011, Ms. House-Hatfield tasked Dina Hooshyar of the VANTHCS to champion and spearhead this transformation.
The challenge associated with the UHHS creation process was to balance individual program autonomy with standardized processes. This balance was achieved through weekly calls where Ms. House- Hatfield, Dr. Hooshyar, and CHCP program managers discussed how to design UHHS. The management of the CHCP also actively sought input from CHCP frontline staff. During the preimplementation phase, Dr. Hooshyar gave multiple UHHS trainings to CHCP staff who would become involved in UHHS process, another feedback mechanism.
Program managers retained their programs’ autonomy by picking screeners and the number of employees in that position for their program, screening location and time, and screening type (appointment, walk-in, telephone, and/or combination). Managers and staff also assisted in the creation of the UHHS tool by providing their program’s eligibility criteria and customary psychosocial assessment questions. The UHHS tool not only brought consistency to the screening process, but also removed any perceived biases by asking all veterans the same questions across all UHHS screening locations. Implemented on August 26, 2013, UHHS continues to be used.
UHHS Screening Tool
The UHHS tool is an assessment composed of 4 sections: (1) History; (2) Decision Tree; (3) Specific Program Eligibility Criteria; and (4) Plan. The sections exist as templates in the CPRS.
The History section asks about demographic information, diagnoses, alcohol and illicit drug use history, dependent status, outstanding legal issues, housing status, functional limitations, income and employment status, and potential benefit from and interest in psychosocial rehabilitation and care management. If the veteran would not benefit from and/or is not interested in participating in psychosocial rehabilitation and care management, the screener concludes the assessment, as these factors are eligibility requirements for all CHCP programs. Veterans can appeal their case to the screener’s program manager.
The Decision Tree template consists of 6 core eligibility criteria across programs that can serve to narrow the list of eligible programs: (1) Is the veteran currently homeless; (2) Has the veteran been homeless continuously for ≥ 1 year, or has the veteran had ≥ 4 separate occasions of homelessness in the past 3 years; (3) Does the veteran have a mental health or substance use diagnosis; (4) Can the veteran pay a program fee (9 of 16 UHHS-associated programs have no fees); (5) Is the veteran capable of self-administering medications; and (6) Can the veteran perform activities of daily living and does not need acute hospitalization?
Related: Using H-PACT to Overcome Treatment Obstacles for Homeless Veterans (audio)
Veterans are then asked in which town(s) they want to reside. The questions for the Specific Program Eligibility Criteria section are asked only for those programs for which the veteran is found to be tentatively eligible by the Decision Tree and has interest in participating.
The Plan section gives veterans the opportunity to appeal a UHHS finding to the specific program’s manager whose program they are not eligible to participate. Veterans also rank their preference for the programs for which they are interested and eligible. A shared folder contains all program census information. Through the screening tool, veterans devise a plan to contact the potential admitting program. Veterans are informed about the importance of keeping in contact with these programs, because programs will not hold openings for an indefinite time.
Completion of this screening assessment, which includes HOMES and the UHHS tool, generally takes 1.5 hours. After a veteran undergoes this assessment, a preadmission appointment is made with the first open program for which they are eligible and interested in participating. The main goal of this appointment varies by program, such as finalizing referral processes with associated community partners, performing a preliminary medical clearance, determining whether veterans have already used their program’s maximum allotted time, coordinating a Therapeutic Supported Employment Services assessment, or obtaining the required documents from veterans. If at the preadmission appointment, either the veteran declines participation or the program declines admittance, the veteran can follow up with other programs for which they met eligibility criteria and were interested in participating during the initial UHHS assessment instead of undergoing another housing screening.
Notification of Screening Results
The CHCP staff member who performs the screening is responsible for documenting the veteran’s name, phone number or means of contact, current residence, and housing outcome in a secure shared Microsoft Excel document called Housing Outcome. The Excel IF and VLOOKUP function link the original document to each program’s acceptance and petition documents. This linkage auto populates information entered in the Housing Outcome document to each program’s acceptance and petition documents if the veteran has a housing outcome associated with the program. CHCP staff members then look at their individual program’s acceptance and/or petition documents to see the list of veterans who have a housing outcome involving their program instead of having to sort through the Housing Outcome document. As a backup to the Housing Outcome document, screeners add the point of contact for the programs that the veteran had an associated housing outcome as additional signers to their CPRS screening note.
When UHHS was first implemented, the screeners had a daily call to discuss the screened veterans’ housing outcomes and screener experiences with the new system. Dr. Hooshyar also participated in this call as a means to answer screener questions and to get feedback. Within a month of UHHS implementation, these calls were cancelled, because the screeners felt comfortable with the UHHS process and the majority of housing programs were operating at full capacity.
UHHS Appointment Line
The UHHS appointment phone number uses an automatic call distributor, a call-center technology. Thus, 1 phone number can be answered by multiple people working in separate locations. The challenge was how to connect phones associated with offices located offsite from the VANTHCS campus. The solution was to use Internet phones in addition to existing staff phones.
Results
During the review period from August 26, 2013, to November 27, 2013 (65 workdays), 392 unique veterans attended a UHHS assessment. Four veterans who were screened twice were included only once in the analysis; outcomes from only their initial screenings were evaluated. Three hundred fifty-six veterans completed a UHHS assessment; 36 had an assessment but did not complete it. Rates of veterans not presenting for their scheduled appointments increased over time, from 24% in August 2013 to 50% in November 2013. To address the no-show rate, program managers decreased the number of offered scheduled appointments and increased the number of walk-in visits. Overall, the schedule distribution consisted of about twice as much time allotted for walk-in appointments compared with scheduled appointments. The UHHS appointment line received 873 calls, where the number decreased over time.
The typical screened veteran who completed a UHHS assessment was a non-Hispanic, African American male aged 51 years with no service connection or history of combat who served either in the Vietnam War era, post-Vietnam War era, or Persian Gulf War. He had accessed VANTHCS care in the year prior to screening; owned a working phone; and was staying in a shelter, a place not meant for human habitation, or a substance use treatment program the night prior to screening (Table 1). Only 20 veterans (5%) were ineligible for participation in all programs, because they did not meet core eligibility criteria as defined by the UHHS Decision Tree, their income surpassed the program limit, or they were not eligible for VA care (Table 2).
To determine the housing outcome of the veterans screened during the reviewed period, a 3-month follow-up from the end of the review period was used. During this time, 269 veterans (76%) who completed the UHHS process were housed, with 215 (60%) veterans housed in a UHHS-associated housing program (Table 3). Of the veterans who completed a UHHS assessment, 45 veterans (13%) did not complete the screening process; admitting program staff documented in CPRS unsuccessful attempts at reaching 12 veterans (3%), among whom 4 had no working phone at the time of their UHHS assessment. Time to admission depended on the program mission, openings, and the veteran’s UHHS engagement. Admission date indicates the date that programs housed veterans except in the case of the U.S. Department of Housing and Urban Development-VA Supportive Housing (HUD-VASH), where admission date indicates the date the veteran gave all required documents to HUD-VASH staff.
Discussion
Prior to the inception of UHHS, the staff of the CHCP housing program did not have a standardized process for communication across programs about veterans’ housing status and outcomes. Veterans went to multiple locations for screening if they were interested in > 1 program or if they were not admitted to the first program they approached. The UHHS process improved communication across CHCP housing programs, resulting in increased veteran accessibility to these programs as suggested by 3 CHCP housing programs having fewer days with openings post-UHHS implementation. Furthermore, a new screener position did not need to be created, because existing CHCP social workers were all capable screeners due to process standardization.
Fifty-five percent of the screened veterans were interested in and eligible for participation in > 1 housing program. They were eligible for 3 programs on average and were usually admitted to the housing program with the earliest opening. The need for screenings across all the CHCP housing programs was potentially decreased by ≥ one-third. This increased available time for the screeners to accomplish their other clinical responsibilities.
Limitations
A limitation of the review period evaluation is little information on noncompleters. The available data are confined to information documented in CPRS regarding why 45 veterans (13% of those who completed UHHS assessment) did not complete the screening process. For 12, admitting staff of the housing program documented in CPRS that they had been unable to reach the veteran; 9 of these veterans attended subsequent non-UHHS VANTHCS visits. To further improve the homeless housing delivery service, the creation of a CPRS-related process that informs VA clinicians that a housing program is attempting to contact a veteran is needed.
Challenges and Recommendations
Because the Housing Outcome document is a shared document, only 1 person at a time can save information in it. Facility staff have been unable to create a simple macro that closes the document automatically. Instead, screeners who need to save information when a document is already opened elsewhere must use a group e-mail list to alert others to close the document.
Streamlining the communication channel between the screeners and management evolved from the daily call, to e-mailing and program managers discussing topics with their staff, to Dr. Hooshyar facilitating a weekly call for screeners and program managers.
Optimizing the ratio of walk-in to scheduled appointments took time. Prior to the UHHS process, some CHCP housing programs offered scheduled appointments, whereas others had walk-in appointments. The decision to offer in-person scheduled appointments for veterans who preferred scheduled appointments or who commuted from a distance was made. Universal Homeless Housing Screening staff also offered scheduled telephone appointments for veterans who lacked transportation.
At times, admitting program staff was unable to reach veterans eligible for and interested in their program, despite screeners recommending to veterans that they should provide these programs with any changes in their contact information.
Recommendations for designing a screening process for homeless housing include:
- Have periodic retreats instead of weekly conference calls to quicken the pre-implementation process.
- Start with a pilot that includes some potential screeners to test the implementation process. The screeners involved in the pilot would train future screeners to expand the screener pool.
- Invest time in electronic tracking tools despite upfront and maintenance time requirements.
- Offer more walk-in than scheduled screening appointments.
- Embrace the idea that the pro-cess is always under development.
Conclusion
To ameliorate anxiety associated with changing the system, UHHS- associated staff redesigned the housing screening process through openness to stakeholder feedback and building on consensus. The staff also nurtured a culture that could change newly revised processes, depending on quality assurance findings. Without this method, the unknown likely would have propagated continued status quo. Universal Homeless Housing Screening processes improved veteran access to CHCP housing programs through instituting a one-stop housing screening assessment that also reduced the potential number of screenings by ≥ one-third.
Acknowledgments
The authors greatly appreciate the input of the many people involved in the creation of the UHHS process, in particular Daniel Anderson, Heather Arredondo, Tara Ayala, TiieShaiyon Banton, Melody Boyet, Amelia Bradley, Timothy Brown, Carnisha Campbell, Donald Capps, Burnell Carden Jr, Pushpi Chaudhary, Howard Cunningham, Rachael David, Marianna Demko, Derrick Evans, Steven Fisher, Kimberly Fite, Fatina Ford, Christi Godfrey, Gerald Goodwin, Melvin Haley, Tony Hall, Jessica Hennessey, Teresa House-Hatfield, Don Hubbard, Kathryn Jacob, Tonja King, Cecelia Knight, Janine Lenger-Gvist, Vickie Linden, Julia Long, Kristin Manley, Peggy Martin, Treva McDaniel, William McNair, Tammy Miller, Jeffery Milligan, Anhloan Nguyen, Tywanna Nichols, Cheryl Paul, Catherine Orsak, Dustin Perkins, Claudette Phillips, Joan Prescott, John Purkey, Martin Roback, Catriska Robertson, Charles Ross, Shanna Ruppert, Stephanie Saldivar, Linda Saucedo, Inga Sinclair-Henderson, John Smith, Zaire Smith, Cheryl Stringer, Valetta Ward, Carolyn Washington, Tammra Wood, and Skylar Woods-Nunley. They would also like to thank the veterans for their service and feedback.
Author disclosures
Dr. North discloses research support from National Institute on Alcohol Abuse and Alcoholism, National Institute of Diabetes and Digestive and Kidney Diseases, and VA and consultant fees from the University of Missouri-Columbia. Dr. Surís is Local Site Investigator for VA CSP #589 VIPSTAR-Veterans Individual Placement and Support Towards Advancing Recovery (PI Lori Davis, MD). She is co- investigator for VISN 17 grant Association of Myocardial Viability to Symptom Improvement post-CTO PCI (PI-Shuaib Abdullah, MD) and co-investigator for National Institutes on Drug Abuse grant Lidocaine Infusion as a Treatment for Cocaine Relapse and Craving (PI-Bryon Adinoff, MD). In addition, Dr. Surís is co-site-PI for the upcoming VA CSP #590 Lithium for Suicidal Behavior in Mood Disorders.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: National comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(suppl 2):S225-S231.
2. Secretary Shinseki Details Plan to End Homelessness for Veterans [news release]. U.S. Department of Veterans Affairs: Office of Public and Intergovernmental Affairs. http://www.va.gov/opa/pressrel/pressrelease.cfm?id=1807. Published November 3, 2009. Accessed March 3, 2014.
3. U.S. Department of Housing and Urban Development: Office of Community Planning and Development. The 2014 Annual Homeless Assessment Report (AHAR) to Congress. Part 1 Point-In-Time Estimates of Homelessness. https://www.hudexchange.info/resources/documents /2014-AHAR-Part1.pdf. Published October 2014. Accessed March 18, 2015.
4. Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210-S211.
5. Berman S, Barilich JE, Rosenheck R, Koerber G. The VA’s first comprehensive homeless center: A catalyst for public and private partnerships. Hosp Community Psychiatry. 1993;44(12):1183-1184.
6. U.S. Department of Veterans Affairs. Homeless Operations Management and Evaluation System (HOMES) User Manual–Phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed March 3, 2014.
Homelessness is associated with disproportionate medical morbidity and mortality and use of nonpreventive health services.1 In fiscal year 2010, veterans experiencing homelessness were 4 times more likely to use VA emergency departments and had a greater 10-year mortality risk than did veterans who were housed.1 Veterans experiencing homelessness were more likely to be diagnosed with substance use disorder, schizophrenia, liver disease, and/or HIV/AIDS than were their housed counterparts.
Ending veteran homelessness is a federal priority, exemplified by the goal of President Obama to end veteran homelessness by 2015.2 Since the goal’s articulation, veteran homelessness has declined nationally by 33% (24,117 veterans) from 2009 to 2014 however, 49,933 veterans were identified as being homeless on a given night in January 2014.3
Related: Landmark Initiative Signed for Homeless Veterans
A crucial element needed to end veteran homelessness is veteran and health care provider knowledge of existing homeless services and mechanisms of access. In 2012, VHA launched a homelessness screening clinical reminder in the Computerized Patient Record System (CPRS), which prompts a discussion of housing status between the veteran and provider.4 The staff of the VA North Texas Health Care System (VANTHCS) Comprehensive Homeless Center Programs (CHCP) realized that homeless housing programs at the facility could be more accessible if staff from each program could screen for all available programs and if a single phone number existed for scheduling appointments. Therefore, VANTHCS transformed its homeless housing screening process to a standardized process through which veterans are screened for all CHCP housing programs during a single screening assessment, Universal Homeless Housing Screening (UHHS).
This article describes the creation of the UHHS, the screening tool, 3-month postimplementation findings, and recommendations based on initial VANTHCS staff experiences with this process. During the redesign of screening process for homeless housing, VANTHCS staff found a paucity of guidance regarding best practices. This article attempts to fill this gap and provide guidance to institutions that are considering standardizing their screening process for homeless housing across multiple programs at different locations.
Background
Established in 1990, VANTHCS CHCP is VA’ s first comprehensive homeless center. The CHCP provides both housing and vocational rehabilitation programs, including 13 housing programs in 6 different cities and long-standing partnerships between CHCP and 3 community agencies whose programs have specific housing for veterans.5 Screenings performed in Dallas, Texas, for CHCP housing programs are completed at 4 separate locations.
Prior to the inception of the UHHS process, access to housing programs was limited by veteran awareness of the programs and transportation to various program locations. To participate in these programs, veterans needed to complete a form for the VA Northeast Program Evaluation Center (NEPEC), which staff at the Healthcare for Homeless Veterans (HCHV) CHCP program could administer. This process created an admission bottleneck, because HCHV staff needed to evaluate veterans even if they were being admitted to non-HCHV programs.
UHHS Creation Process
In 2011, NEPEC launched the electronic Homeless Operations Management and Evaluation System (HOMES) to replace paper-based reporting.6 This tool allowed non-HCHV CHCP staff to complete NEPEC evaluation and allowed CHCP to meet its goal of designing a system where all CHCP housing programs could complete a screening assessment. This goal originated from the desire of then CHCP Director Teresa House-Hatfield to create a more efficient housing screening process and from similar feedback from veterans.
Furthermore, in 2009, then Secretary of Veterans Affairs Eric K. Shinseki described a “no wrong door” philosophy for ending veteran homelessness, which CHCP operationalized by screening veterans for any CHCP housing program regardless of initial point of contact within the CHCP system.2 Subsequently, in 2010, the VA Office of Mental Health Services contracted with Mathematica Policy Research, Inc., to conduct a quality review of VA Mental Health Residential Rehabilitation Treatment Programs. Notable among their recommendations was to create a one-stop screening process for these programs.
Related: Primary Care Medical Services for Homeless Veterans
In 2010, CHCP embarked on a process to transform the facility’s screening procedure to a one-stop assessment with standardized screening questions and create a systematic process to track outcomes across all CHCP housing programs. The new process allowed for a standardized appeal procedure when eligibility for a program was not met. It also improved the ease of communication by having 1 phone number for making appointments or informing about screening times. These changes were enacted without the addition of any new staff positions. Instead, in October 2011, Ms. House-Hatfield tasked Dina Hooshyar of the VANTHCS to champion and spearhead this transformation.
The challenge associated with the UHHS creation process was to balance individual program autonomy with standardized processes. This balance was achieved through weekly calls where Ms. House- Hatfield, Dr. Hooshyar, and CHCP program managers discussed how to design UHHS. The management of the CHCP also actively sought input from CHCP frontline staff. During the preimplementation phase, Dr. Hooshyar gave multiple UHHS trainings to CHCP staff who would become involved in UHHS process, another feedback mechanism.
Program managers retained their programs’ autonomy by picking screeners and the number of employees in that position for their program, screening location and time, and screening type (appointment, walk-in, telephone, and/or combination). Managers and staff also assisted in the creation of the UHHS tool by providing their program’s eligibility criteria and customary psychosocial assessment questions. The UHHS tool not only brought consistency to the screening process, but also removed any perceived biases by asking all veterans the same questions across all UHHS screening locations. Implemented on August 26, 2013, UHHS continues to be used.
UHHS Screening Tool
The UHHS tool is an assessment composed of 4 sections: (1) History; (2) Decision Tree; (3) Specific Program Eligibility Criteria; and (4) Plan. The sections exist as templates in the CPRS.
The History section asks about demographic information, diagnoses, alcohol and illicit drug use history, dependent status, outstanding legal issues, housing status, functional limitations, income and employment status, and potential benefit from and interest in psychosocial rehabilitation and care management. If the veteran would not benefit from and/or is not interested in participating in psychosocial rehabilitation and care management, the screener concludes the assessment, as these factors are eligibility requirements for all CHCP programs. Veterans can appeal their case to the screener’s program manager.
The Decision Tree template consists of 6 core eligibility criteria across programs that can serve to narrow the list of eligible programs: (1) Is the veteran currently homeless; (2) Has the veteran been homeless continuously for ≥ 1 year, or has the veteran had ≥ 4 separate occasions of homelessness in the past 3 years; (3) Does the veteran have a mental health or substance use diagnosis; (4) Can the veteran pay a program fee (9 of 16 UHHS-associated programs have no fees); (5) Is the veteran capable of self-administering medications; and (6) Can the veteran perform activities of daily living and does not need acute hospitalization?
Related: Using H-PACT to Overcome Treatment Obstacles for Homeless Veterans (audio)
Veterans are then asked in which town(s) they want to reside. The questions for the Specific Program Eligibility Criteria section are asked only for those programs for which the veteran is found to be tentatively eligible by the Decision Tree and has interest in participating.
The Plan section gives veterans the opportunity to appeal a UHHS finding to the specific program’s manager whose program they are not eligible to participate. Veterans also rank their preference for the programs for which they are interested and eligible. A shared folder contains all program census information. Through the screening tool, veterans devise a plan to contact the potential admitting program. Veterans are informed about the importance of keeping in contact with these programs, because programs will not hold openings for an indefinite time.
Completion of this screening assessment, which includes HOMES and the UHHS tool, generally takes 1.5 hours. After a veteran undergoes this assessment, a preadmission appointment is made with the first open program for which they are eligible and interested in participating. The main goal of this appointment varies by program, such as finalizing referral processes with associated community partners, performing a preliminary medical clearance, determining whether veterans have already used their program’s maximum allotted time, coordinating a Therapeutic Supported Employment Services assessment, or obtaining the required documents from veterans. If at the preadmission appointment, either the veteran declines participation or the program declines admittance, the veteran can follow up with other programs for which they met eligibility criteria and were interested in participating during the initial UHHS assessment instead of undergoing another housing screening.
Notification of Screening Results
The CHCP staff member who performs the screening is responsible for documenting the veteran’s name, phone number or means of contact, current residence, and housing outcome in a secure shared Microsoft Excel document called Housing Outcome. The Excel IF and VLOOKUP function link the original document to each program’s acceptance and petition documents. This linkage auto populates information entered in the Housing Outcome document to each program’s acceptance and petition documents if the veteran has a housing outcome associated with the program. CHCP staff members then look at their individual program’s acceptance and/or petition documents to see the list of veterans who have a housing outcome involving their program instead of having to sort through the Housing Outcome document. As a backup to the Housing Outcome document, screeners add the point of contact for the programs that the veteran had an associated housing outcome as additional signers to their CPRS screening note.
When UHHS was first implemented, the screeners had a daily call to discuss the screened veterans’ housing outcomes and screener experiences with the new system. Dr. Hooshyar also participated in this call as a means to answer screener questions and to get feedback. Within a month of UHHS implementation, these calls were cancelled, because the screeners felt comfortable with the UHHS process and the majority of housing programs were operating at full capacity.
UHHS Appointment Line
The UHHS appointment phone number uses an automatic call distributor, a call-center technology. Thus, 1 phone number can be answered by multiple people working in separate locations. The challenge was how to connect phones associated with offices located offsite from the VANTHCS campus. The solution was to use Internet phones in addition to existing staff phones.
Results
During the review period from August 26, 2013, to November 27, 2013 (65 workdays), 392 unique veterans attended a UHHS assessment. Four veterans who were screened twice were included only once in the analysis; outcomes from only their initial screenings were evaluated. Three hundred fifty-six veterans completed a UHHS assessment; 36 had an assessment but did not complete it. Rates of veterans not presenting for their scheduled appointments increased over time, from 24% in August 2013 to 50% in November 2013. To address the no-show rate, program managers decreased the number of offered scheduled appointments and increased the number of walk-in visits. Overall, the schedule distribution consisted of about twice as much time allotted for walk-in appointments compared with scheduled appointments. The UHHS appointment line received 873 calls, where the number decreased over time.
The typical screened veteran who completed a UHHS assessment was a non-Hispanic, African American male aged 51 years with no service connection or history of combat who served either in the Vietnam War era, post-Vietnam War era, or Persian Gulf War. He had accessed VANTHCS care in the year prior to screening; owned a working phone; and was staying in a shelter, a place not meant for human habitation, or a substance use treatment program the night prior to screening (Table 1). Only 20 veterans (5%) were ineligible for participation in all programs, because they did not meet core eligibility criteria as defined by the UHHS Decision Tree, their income surpassed the program limit, or they were not eligible for VA care (Table 2).
To determine the housing outcome of the veterans screened during the reviewed period, a 3-month follow-up from the end of the review period was used. During this time, 269 veterans (76%) who completed the UHHS process were housed, with 215 (60%) veterans housed in a UHHS-associated housing program (Table 3). Of the veterans who completed a UHHS assessment, 45 veterans (13%) did not complete the screening process; admitting program staff documented in CPRS unsuccessful attempts at reaching 12 veterans (3%), among whom 4 had no working phone at the time of their UHHS assessment. Time to admission depended on the program mission, openings, and the veteran’s UHHS engagement. Admission date indicates the date that programs housed veterans except in the case of the U.S. Department of Housing and Urban Development-VA Supportive Housing (HUD-VASH), where admission date indicates the date the veteran gave all required documents to HUD-VASH staff.
Discussion
Prior to the inception of UHHS, the staff of the CHCP housing program did not have a standardized process for communication across programs about veterans’ housing status and outcomes. Veterans went to multiple locations for screening if they were interested in > 1 program or if they were not admitted to the first program they approached. The UHHS process improved communication across CHCP housing programs, resulting in increased veteran accessibility to these programs as suggested by 3 CHCP housing programs having fewer days with openings post-UHHS implementation. Furthermore, a new screener position did not need to be created, because existing CHCP social workers were all capable screeners due to process standardization.
Fifty-five percent of the screened veterans were interested in and eligible for participation in > 1 housing program. They were eligible for 3 programs on average and were usually admitted to the housing program with the earliest opening. The need for screenings across all the CHCP housing programs was potentially decreased by ≥ one-third. This increased available time for the screeners to accomplish their other clinical responsibilities.
Limitations
A limitation of the review period evaluation is little information on noncompleters. The available data are confined to information documented in CPRS regarding why 45 veterans (13% of those who completed UHHS assessment) did not complete the screening process. For 12, admitting staff of the housing program documented in CPRS that they had been unable to reach the veteran; 9 of these veterans attended subsequent non-UHHS VANTHCS visits. To further improve the homeless housing delivery service, the creation of a CPRS-related process that informs VA clinicians that a housing program is attempting to contact a veteran is needed.
Challenges and Recommendations
Because the Housing Outcome document is a shared document, only 1 person at a time can save information in it. Facility staff have been unable to create a simple macro that closes the document automatically. Instead, screeners who need to save information when a document is already opened elsewhere must use a group e-mail list to alert others to close the document.
Streamlining the communication channel between the screeners and management evolved from the daily call, to e-mailing and program managers discussing topics with their staff, to Dr. Hooshyar facilitating a weekly call for screeners and program managers.
Optimizing the ratio of walk-in to scheduled appointments took time. Prior to the UHHS process, some CHCP housing programs offered scheduled appointments, whereas others had walk-in appointments. The decision to offer in-person scheduled appointments for veterans who preferred scheduled appointments or who commuted from a distance was made. Universal Homeless Housing Screening staff also offered scheduled telephone appointments for veterans who lacked transportation.
At times, admitting program staff was unable to reach veterans eligible for and interested in their program, despite screeners recommending to veterans that they should provide these programs with any changes in their contact information.
Recommendations for designing a screening process for homeless housing include:
- Have periodic retreats instead of weekly conference calls to quicken the pre-implementation process.
- Start with a pilot that includes some potential screeners to test the implementation process. The screeners involved in the pilot would train future screeners to expand the screener pool.
- Invest time in electronic tracking tools despite upfront and maintenance time requirements.
- Offer more walk-in than scheduled screening appointments.
- Embrace the idea that the pro-cess is always under development.
Conclusion
To ameliorate anxiety associated with changing the system, UHHS- associated staff redesigned the housing screening process through openness to stakeholder feedback and building on consensus. The staff also nurtured a culture that could change newly revised processes, depending on quality assurance findings. Without this method, the unknown likely would have propagated continued status quo. Universal Homeless Housing Screening processes improved veteran access to CHCP housing programs through instituting a one-stop housing screening assessment that also reduced the potential number of screenings by ≥ one-third.
Acknowledgments
The authors greatly appreciate the input of the many people involved in the creation of the UHHS process, in particular Daniel Anderson, Heather Arredondo, Tara Ayala, TiieShaiyon Banton, Melody Boyet, Amelia Bradley, Timothy Brown, Carnisha Campbell, Donald Capps, Burnell Carden Jr, Pushpi Chaudhary, Howard Cunningham, Rachael David, Marianna Demko, Derrick Evans, Steven Fisher, Kimberly Fite, Fatina Ford, Christi Godfrey, Gerald Goodwin, Melvin Haley, Tony Hall, Jessica Hennessey, Teresa House-Hatfield, Don Hubbard, Kathryn Jacob, Tonja King, Cecelia Knight, Janine Lenger-Gvist, Vickie Linden, Julia Long, Kristin Manley, Peggy Martin, Treva McDaniel, William McNair, Tammy Miller, Jeffery Milligan, Anhloan Nguyen, Tywanna Nichols, Cheryl Paul, Catherine Orsak, Dustin Perkins, Claudette Phillips, Joan Prescott, John Purkey, Martin Roback, Catriska Robertson, Charles Ross, Shanna Ruppert, Stephanie Saldivar, Linda Saucedo, Inga Sinclair-Henderson, John Smith, Zaire Smith, Cheryl Stringer, Valetta Ward, Carolyn Washington, Tammra Wood, and Skylar Woods-Nunley. They would also like to thank the veterans for their service and feedback.
Author disclosures
Dr. North discloses research support from National Institute on Alcohol Abuse and Alcoholism, National Institute of Diabetes and Digestive and Kidney Diseases, and VA and consultant fees from the University of Missouri-Columbia. Dr. Surís is Local Site Investigator for VA CSP #589 VIPSTAR-Veterans Individual Placement and Support Towards Advancing Recovery (PI Lori Davis, MD). She is co- investigator for VISN 17 grant Association of Myocardial Viability to Symptom Improvement post-CTO PCI (PI-Shuaib Abdullah, MD) and co-investigator for National Institutes on Drug Abuse grant Lidocaine Infusion as a Treatment for Cocaine Relapse and Craving (PI-Bryon Adinoff, MD). In addition, Dr. Surís is co-site-PI for the upcoming VA CSP #590 Lithium for Suicidal Behavior in Mood Disorders.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Homelessness is associated with disproportionate medical morbidity and mortality and use of nonpreventive health services.1 In fiscal year 2010, veterans experiencing homelessness were 4 times more likely to use VA emergency departments and had a greater 10-year mortality risk than did veterans who were housed.1 Veterans experiencing homelessness were more likely to be diagnosed with substance use disorder, schizophrenia, liver disease, and/or HIV/AIDS than were their housed counterparts.
Ending veteran homelessness is a federal priority, exemplified by the goal of President Obama to end veteran homelessness by 2015.2 Since the goal’s articulation, veteran homelessness has declined nationally by 33% (24,117 veterans) from 2009 to 2014 however, 49,933 veterans were identified as being homeless on a given night in January 2014.3
Related: Landmark Initiative Signed for Homeless Veterans
A crucial element needed to end veteran homelessness is veteran and health care provider knowledge of existing homeless services and mechanisms of access. In 2012, VHA launched a homelessness screening clinical reminder in the Computerized Patient Record System (CPRS), which prompts a discussion of housing status between the veteran and provider.4 The staff of the VA North Texas Health Care System (VANTHCS) Comprehensive Homeless Center Programs (CHCP) realized that homeless housing programs at the facility could be more accessible if staff from each program could screen for all available programs and if a single phone number existed for scheduling appointments. Therefore, VANTHCS transformed its homeless housing screening process to a standardized process through which veterans are screened for all CHCP housing programs during a single screening assessment, Universal Homeless Housing Screening (UHHS).
This article describes the creation of the UHHS, the screening tool, 3-month postimplementation findings, and recommendations based on initial VANTHCS staff experiences with this process. During the redesign of screening process for homeless housing, VANTHCS staff found a paucity of guidance regarding best practices. This article attempts to fill this gap and provide guidance to institutions that are considering standardizing their screening process for homeless housing across multiple programs at different locations.
Background
Established in 1990, VANTHCS CHCP is VA’ s first comprehensive homeless center. The CHCP provides both housing and vocational rehabilitation programs, including 13 housing programs in 6 different cities and long-standing partnerships between CHCP and 3 community agencies whose programs have specific housing for veterans.5 Screenings performed in Dallas, Texas, for CHCP housing programs are completed at 4 separate locations.
Prior to the inception of the UHHS process, access to housing programs was limited by veteran awareness of the programs and transportation to various program locations. To participate in these programs, veterans needed to complete a form for the VA Northeast Program Evaluation Center (NEPEC), which staff at the Healthcare for Homeless Veterans (HCHV) CHCP program could administer. This process created an admission bottleneck, because HCHV staff needed to evaluate veterans even if they were being admitted to non-HCHV programs.
UHHS Creation Process
In 2011, NEPEC launched the electronic Homeless Operations Management and Evaluation System (HOMES) to replace paper-based reporting.6 This tool allowed non-HCHV CHCP staff to complete NEPEC evaluation and allowed CHCP to meet its goal of designing a system where all CHCP housing programs could complete a screening assessment. This goal originated from the desire of then CHCP Director Teresa House-Hatfield to create a more efficient housing screening process and from similar feedback from veterans.
Furthermore, in 2009, then Secretary of Veterans Affairs Eric K. Shinseki described a “no wrong door” philosophy for ending veteran homelessness, which CHCP operationalized by screening veterans for any CHCP housing program regardless of initial point of contact within the CHCP system.2 Subsequently, in 2010, the VA Office of Mental Health Services contracted with Mathematica Policy Research, Inc., to conduct a quality review of VA Mental Health Residential Rehabilitation Treatment Programs. Notable among their recommendations was to create a one-stop screening process for these programs.
Related: Primary Care Medical Services for Homeless Veterans
In 2010, CHCP embarked on a process to transform the facility’s screening procedure to a one-stop assessment with standardized screening questions and create a systematic process to track outcomes across all CHCP housing programs. The new process allowed for a standardized appeal procedure when eligibility for a program was not met. It also improved the ease of communication by having 1 phone number for making appointments or informing about screening times. These changes were enacted without the addition of any new staff positions. Instead, in October 2011, Ms. House-Hatfield tasked Dina Hooshyar of the VANTHCS to champion and spearhead this transformation.
The challenge associated with the UHHS creation process was to balance individual program autonomy with standardized processes. This balance was achieved through weekly calls where Ms. House- Hatfield, Dr. Hooshyar, and CHCP program managers discussed how to design UHHS. The management of the CHCP also actively sought input from CHCP frontline staff. During the preimplementation phase, Dr. Hooshyar gave multiple UHHS trainings to CHCP staff who would become involved in UHHS process, another feedback mechanism.
Program managers retained their programs’ autonomy by picking screeners and the number of employees in that position for their program, screening location and time, and screening type (appointment, walk-in, telephone, and/or combination). Managers and staff also assisted in the creation of the UHHS tool by providing their program’s eligibility criteria and customary psychosocial assessment questions. The UHHS tool not only brought consistency to the screening process, but also removed any perceived biases by asking all veterans the same questions across all UHHS screening locations. Implemented on August 26, 2013, UHHS continues to be used.
UHHS Screening Tool
The UHHS tool is an assessment composed of 4 sections: (1) History; (2) Decision Tree; (3) Specific Program Eligibility Criteria; and (4) Plan. The sections exist as templates in the CPRS.
The History section asks about demographic information, diagnoses, alcohol and illicit drug use history, dependent status, outstanding legal issues, housing status, functional limitations, income and employment status, and potential benefit from and interest in psychosocial rehabilitation and care management. If the veteran would not benefit from and/or is not interested in participating in psychosocial rehabilitation and care management, the screener concludes the assessment, as these factors are eligibility requirements for all CHCP programs. Veterans can appeal their case to the screener’s program manager.
The Decision Tree template consists of 6 core eligibility criteria across programs that can serve to narrow the list of eligible programs: (1) Is the veteran currently homeless; (2) Has the veteran been homeless continuously for ≥ 1 year, or has the veteran had ≥ 4 separate occasions of homelessness in the past 3 years; (3) Does the veteran have a mental health or substance use diagnosis; (4) Can the veteran pay a program fee (9 of 16 UHHS-associated programs have no fees); (5) Is the veteran capable of self-administering medications; and (6) Can the veteran perform activities of daily living and does not need acute hospitalization?
Related: Using H-PACT to Overcome Treatment Obstacles for Homeless Veterans (audio)
Veterans are then asked in which town(s) they want to reside. The questions for the Specific Program Eligibility Criteria section are asked only for those programs for which the veteran is found to be tentatively eligible by the Decision Tree and has interest in participating.
The Plan section gives veterans the opportunity to appeal a UHHS finding to the specific program’s manager whose program they are not eligible to participate. Veterans also rank their preference for the programs for which they are interested and eligible. A shared folder contains all program census information. Through the screening tool, veterans devise a plan to contact the potential admitting program. Veterans are informed about the importance of keeping in contact with these programs, because programs will not hold openings for an indefinite time.
Completion of this screening assessment, which includes HOMES and the UHHS tool, generally takes 1.5 hours. After a veteran undergoes this assessment, a preadmission appointment is made with the first open program for which they are eligible and interested in participating. The main goal of this appointment varies by program, such as finalizing referral processes with associated community partners, performing a preliminary medical clearance, determining whether veterans have already used their program’s maximum allotted time, coordinating a Therapeutic Supported Employment Services assessment, or obtaining the required documents from veterans. If at the preadmission appointment, either the veteran declines participation or the program declines admittance, the veteran can follow up with other programs for which they met eligibility criteria and were interested in participating during the initial UHHS assessment instead of undergoing another housing screening.
Notification of Screening Results
The CHCP staff member who performs the screening is responsible for documenting the veteran’s name, phone number or means of contact, current residence, and housing outcome in a secure shared Microsoft Excel document called Housing Outcome. The Excel IF and VLOOKUP function link the original document to each program’s acceptance and petition documents. This linkage auto populates information entered in the Housing Outcome document to each program’s acceptance and petition documents if the veteran has a housing outcome associated with the program. CHCP staff members then look at their individual program’s acceptance and/or petition documents to see the list of veterans who have a housing outcome involving their program instead of having to sort through the Housing Outcome document. As a backup to the Housing Outcome document, screeners add the point of contact for the programs that the veteran had an associated housing outcome as additional signers to their CPRS screening note.
When UHHS was first implemented, the screeners had a daily call to discuss the screened veterans’ housing outcomes and screener experiences with the new system. Dr. Hooshyar also participated in this call as a means to answer screener questions and to get feedback. Within a month of UHHS implementation, these calls were cancelled, because the screeners felt comfortable with the UHHS process and the majority of housing programs were operating at full capacity.
UHHS Appointment Line
The UHHS appointment phone number uses an automatic call distributor, a call-center technology. Thus, 1 phone number can be answered by multiple people working in separate locations. The challenge was how to connect phones associated with offices located offsite from the VANTHCS campus. The solution was to use Internet phones in addition to existing staff phones.
Results
During the review period from August 26, 2013, to November 27, 2013 (65 workdays), 392 unique veterans attended a UHHS assessment. Four veterans who were screened twice were included only once in the analysis; outcomes from only their initial screenings were evaluated. Three hundred fifty-six veterans completed a UHHS assessment; 36 had an assessment but did not complete it. Rates of veterans not presenting for their scheduled appointments increased over time, from 24% in August 2013 to 50% in November 2013. To address the no-show rate, program managers decreased the number of offered scheduled appointments and increased the number of walk-in visits. Overall, the schedule distribution consisted of about twice as much time allotted for walk-in appointments compared with scheduled appointments. The UHHS appointment line received 873 calls, where the number decreased over time.
The typical screened veteran who completed a UHHS assessment was a non-Hispanic, African American male aged 51 years with no service connection or history of combat who served either in the Vietnam War era, post-Vietnam War era, or Persian Gulf War. He had accessed VANTHCS care in the year prior to screening; owned a working phone; and was staying in a shelter, a place not meant for human habitation, or a substance use treatment program the night prior to screening (Table 1). Only 20 veterans (5%) were ineligible for participation in all programs, because they did not meet core eligibility criteria as defined by the UHHS Decision Tree, their income surpassed the program limit, or they were not eligible for VA care (Table 2).
To determine the housing outcome of the veterans screened during the reviewed period, a 3-month follow-up from the end of the review period was used. During this time, 269 veterans (76%) who completed the UHHS process were housed, with 215 (60%) veterans housed in a UHHS-associated housing program (Table 3). Of the veterans who completed a UHHS assessment, 45 veterans (13%) did not complete the screening process; admitting program staff documented in CPRS unsuccessful attempts at reaching 12 veterans (3%), among whom 4 had no working phone at the time of their UHHS assessment. Time to admission depended on the program mission, openings, and the veteran’s UHHS engagement. Admission date indicates the date that programs housed veterans except in the case of the U.S. Department of Housing and Urban Development-VA Supportive Housing (HUD-VASH), where admission date indicates the date the veteran gave all required documents to HUD-VASH staff.
Discussion
Prior to the inception of UHHS, the staff of the CHCP housing program did not have a standardized process for communication across programs about veterans’ housing status and outcomes. Veterans went to multiple locations for screening if they were interested in > 1 program or if they were not admitted to the first program they approached. The UHHS process improved communication across CHCP housing programs, resulting in increased veteran accessibility to these programs as suggested by 3 CHCP housing programs having fewer days with openings post-UHHS implementation. Furthermore, a new screener position did not need to be created, because existing CHCP social workers were all capable screeners due to process standardization.
Fifty-five percent of the screened veterans were interested in and eligible for participation in > 1 housing program. They were eligible for 3 programs on average and were usually admitted to the housing program with the earliest opening. The need for screenings across all the CHCP housing programs was potentially decreased by ≥ one-third. This increased available time for the screeners to accomplish their other clinical responsibilities.
Limitations
A limitation of the review period evaluation is little information on noncompleters. The available data are confined to information documented in CPRS regarding why 45 veterans (13% of those who completed UHHS assessment) did not complete the screening process. For 12, admitting staff of the housing program documented in CPRS that they had been unable to reach the veteran; 9 of these veterans attended subsequent non-UHHS VANTHCS visits. To further improve the homeless housing delivery service, the creation of a CPRS-related process that informs VA clinicians that a housing program is attempting to contact a veteran is needed.
Challenges and Recommendations
Because the Housing Outcome document is a shared document, only 1 person at a time can save information in it. Facility staff have been unable to create a simple macro that closes the document automatically. Instead, screeners who need to save information when a document is already opened elsewhere must use a group e-mail list to alert others to close the document.
Streamlining the communication channel between the screeners and management evolved from the daily call, to e-mailing and program managers discussing topics with their staff, to Dr. Hooshyar facilitating a weekly call for screeners and program managers.
Optimizing the ratio of walk-in to scheduled appointments took time. Prior to the UHHS process, some CHCP housing programs offered scheduled appointments, whereas others had walk-in appointments. The decision to offer in-person scheduled appointments for veterans who preferred scheduled appointments or who commuted from a distance was made. Universal Homeless Housing Screening staff also offered scheduled telephone appointments for veterans who lacked transportation.
At times, admitting program staff was unable to reach veterans eligible for and interested in their program, despite screeners recommending to veterans that they should provide these programs with any changes in their contact information.
Recommendations for designing a screening process for homeless housing include:
- Have periodic retreats instead of weekly conference calls to quicken the pre-implementation process.
- Start with a pilot that includes some potential screeners to test the implementation process. The screeners involved in the pilot would train future screeners to expand the screener pool.
- Invest time in electronic tracking tools despite upfront and maintenance time requirements.
- Offer more walk-in than scheduled screening appointments.
- Embrace the idea that the pro-cess is always under development.
Conclusion
To ameliorate anxiety associated with changing the system, UHHS- associated staff redesigned the housing screening process through openness to stakeholder feedback and building on consensus. The staff also nurtured a culture that could change newly revised processes, depending on quality assurance findings. Without this method, the unknown likely would have propagated continued status quo. Universal Homeless Housing Screening processes improved veteran access to CHCP housing programs through instituting a one-stop housing screening assessment that also reduced the potential number of screenings by ≥ one-third.
Acknowledgments
The authors greatly appreciate the input of the many people involved in the creation of the UHHS process, in particular Daniel Anderson, Heather Arredondo, Tara Ayala, TiieShaiyon Banton, Melody Boyet, Amelia Bradley, Timothy Brown, Carnisha Campbell, Donald Capps, Burnell Carden Jr, Pushpi Chaudhary, Howard Cunningham, Rachael David, Marianna Demko, Derrick Evans, Steven Fisher, Kimberly Fite, Fatina Ford, Christi Godfrey, Gerald Goodwin, Melvin Haley, Tony Hall, Jessica Hennessey, Teresa House-Hatfield, Don Hubbard, Kathryn Jacob, Tonja King, Cecelia Knight, Janine Lenger-Gvist, Vickie Linden, Julia Long, Kristin Manley, Peggy Martin, Treva McDaniel, William McNair, Tammy Miller, Jeffery Milligan, Anhloan Nguyen, Tywanna Nichols, Cheryl Paul, Catherine Orsak, Dustin Perkins, Claudette Phillips, Joan Prescott, John Purkey, Martin Roback, Catriska Robertson, Charles Ross, Shanna Ruppert, Stephanie Saldivar, Linda Saucedo, Inga Sinclair-Henderson, John Smith, Zaire Smith, Cheryl Stringer, Valetta Ward, Carolyn Washington, Tammra Wood, and Skylar Woods-Nunley. They would also like to thank the veterans for their service and feedback.
Author disclosures
Dr. North discloses research support from National Institute on Alcohol Abuse and Alcoholism, National Institute of Diabetes and Digestive and Kidney Diseases, and VA and consultant fees from the University of Missouri-Columbia. Dr. Surís is Local Site Investigator for VA CSP #589 VIPSTAR-Veterans Individual Placement and Support Towards Advancing Recovery (PI Lori Davis, MD). She is co- investigator for VISN 17 grant Association of Myocardial Viability to Symptom Improvement post-CTO PCI (PI-Shuaib Abdullah, MD) and co-investigator for National Institutes on Drug Abuse grant Lidocaine Infusion as a Treatment for Cocaine Relapse and Craving (PI-Bryon Adinoff, MD). In addition, Dr. Surís is co-site-PI for the upcoming VA CSP #590 Lithium for Suicidal Behavior in Mood Disorders.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: National comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(suppl 2):S225-S231.
2. Secretary Shinseki Details Plan to End Homelessness for Veterans [news release]. U.S. Department of Veterans Affairs: Office of Public and Intergovernmental Affairs. http://www.va.gov/opa/pressrel/pressrelease.cfm?id=1807. Published November 3, 2009. Accessed March 3, 2014.
3. U.S. Department of Housing and Urban Development: Office of Community Planning and Development. The 2014 Annual Homeless Assessment Report (AHAR) to Congress. Part 1 Point-In-Time Estimates of Homelessness. https://www.hudexchange.info/resources/documents /2014-AHAR-Part1.pdf. Published October 2014. Accessed March 18, 2015.
4. Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210-S211.
5. Berman S, Barilich JE, Rosenheck R, Koerber G. The VA’s first comprehensive homeless center: A catalyst for public and private partnerships. Hosp Community Psychiatry. 1993;44(12):1183-1184.
6. U.S. Department of Veterans Affairs. Homeless Operations Management and Evaluation System (HOMES) User Manual–Phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed March 3, 2014.
1. Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: National comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(suppl 2):S225-S231.
2. Secretary Shinseki Details Plan to End Homelessness for Veterans [news release]. U.S. Department of Veterans Affairs: Office of Public and Intergovernmental Affairs. http://www.va.gov/opa/pressrel/pressrelease.cfm?id=1807. Published November 3, 2009. Accessed March 3, 2014.
3. U.S. Department of Housing and Urban Development: Office of Community Planning and Development. The 2014 Annual Homeless Assessment Report (AHAR) to Congress. Part 1 Point-In-Time Estimates of Homelessness. https://www.hudexchange.info/resources/documents /2014-AHAR-Part1.pdf. Published October 2014. Accessed March 18, 2015.
4. Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal screening for homelessness and risk for homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(suppl 2):S210-S211.
5. Berman S, Barilich JE, Rosenheck R, Koerber G. The VA’s first comprehensive homeless center: A catalyst for public and private partnerships. Hosp Community Psychiatry. 1993;44(12):1183-1184.
6. U.S. Department of Veterans Affairs. Homeless Operations Management and Evaluation System (HOMES) User Manual–Phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed March 3, 2014.