User login
PTSD: A systematic approach to diagnosis and treatment
Posttraumatic stress disorder (PTSD) has increasingly become a part of American culture since its introduction in the American Psychiatric Association’s third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) in 1980.1 Since then, a proliferation of material about this disorder—both academic and popular—has been generated, yet much confusion persists surrounding the definition of the disorder, its prevalence, and its management. This review addresses the essential elements for diagnosis and treatment of PTSD.
Diagnosis: A closer look at the criteria
Criteria for the diagnosis of PTSD have evolved since 1980, with changes in the definition of trauma and the addition of symptoms and symptom groups.2 Table 13 summarizes the current DSM-5 criteria for PTSD.
Trauma exposure. An essential first step in the diagnosis of PTSD is to determine whether the individual has experienced exposure to trauma. This concept is defined in Criterion A (trauma exposure).3 PTSD is nonconformist among the psychiatric diagnoses in that it requires a specific external event as part of its definition. Misapplication of the trauma exposure criterion by many clinicians and researchers has led to misdiagnosis and erroneously high prevalence estimates of PTSD.4,5
A traumatic event is one that represents a threat to life or limb, specifically defined as “actual or threatened death, serious injury, or sexual violence.”3 DSM-5 does not allow for just any stressful event to be considered trauma. For example, no matter how distressing, failing an important test at school or being served with divorce proceedings do not represent a requisite trauma6 because these examples do not entail a threat to life or limb.
DSM-5 PTSD Criterion A also requires a qualifying exposure to the traumatic event. There are 4 types of qualifying exposures:
- direct experience of immediate serious physical danger
- eyewitness of trauma to others
- indirect exposure via violent or accidental trauma experienced by a close family member or close friend
- repeated or extreme exposure to aversive details of trauma, such as first responders collecting human remains or law enforcement officers being repeatedly exposed to horrific details of child abuse.3
Witnessed trauma must be in person; thus, viewing trauma in media reports would not constitute a qualifying exposure. Indirect trauma exposure can occur through learning of the experience of a qualifying trauma exposure by a close family member or personal friend.
It is critical to differentiate exposure to trauma (an objective construct) from the subjective distress that may be associated with it. If trauma has not occurred or a qualifying exposure is not established, no amount of distress associated with it can establish the experience as meeting Criterion A for PTSD. This does not mean that nonqualifying experiences of stressful events are not distressing; in fact, such experiences can result in substantial psychological angst. Conversely, exposure to trauma is not tantamount to a diagnosis of PTSD, as most trauma exposures do not result in PTSD.7,8
Continue to: Symptom groups
Symptom groups. DSM-5 symptom criteria for PTSD include 4 symptom groups, Criteria B to E, respectively:
- intrusion
- avoidance
- negative cognitions and mood (numbing)
- hyperarousal/reactivity.
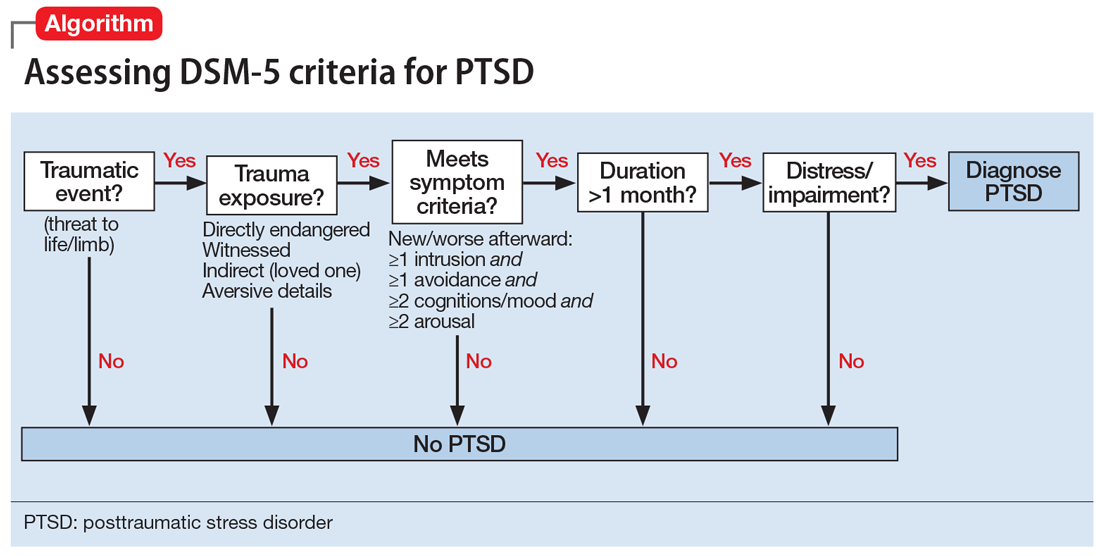
A specific number of symptoms must be present in all 4 of the symptom groups to fulfill diagnostic criteria. Importantly, these symptoms must be linked temporally and conceptually to the traumatic exposure to qualify as PTSD symptoms. Specifically, the symptoms must be new or substantially worsened after the event. For example, continuing sleep disturbance in someone who has had lifetime difficulty sleeping would not count as a trauma-related symptom. Most symptom checklists do not properly assess diagnostic criteria for PTSD because they do not anchor the symptoms in an exposure to a traumatic event; diagnosis requires an interview to fully assess all the diagnostic criteria. Finally, the symptoms must have been present for >1 month for the diagnosis, and the symptoms must have resulted in clinically significant distress or functional impairment to qualify.
The Algorithm provides a practical way to systematically assess all DSM-5 criteria for PTSD to arrive at a diagnosis. The clinician begins by determining whether a traumatic event has occurred and whether the individual had a qualifying exposure to it. If not, PTSD cannot be diagnosed. Alternative diagnoses to consider for new disorders that arise in the context of trauma among patients who are not exposed to trauma include major depressive disorder, adjustment disorder, and bereavement, as well as acute stress disorder (which is not validated but has potential utility as a billable diagnosis).
Avoidance and numbing symptoms (present in Criteria C and D) have been shown to represent markers of illness and can be useful in predicting PTSD.8-10 Unlike symptoms of intrusion and hyperarousal (Criteria B and E, respectively), which are very common and by themselves are nonpathological, avoidance/numbing symptoms occur much less commonly, are associated with functional impairment and other indicators of illness, and are strongly associated with PTSD.6 Prominent avoidance/numbing profiles have been demonstrated to predict PTSD in the first 1 to 2 weeks after trauma exposure, before PTSD can be formally diagnosed.11 Posttraumatic stress symptoms are nearly universal after trauma exposure, even in people who do not develop PTSD.5 Intrusion and hyperarousal symptoms constitute most of such symptoms,7 and these symptoms in the absence of prominent avoidance/numbing can be considered normative distress responses to trauma exposure.12
Some PTSD symptoms may seem quite similar to symptoms of depressive disorders and anxiety disorders. PTSD can be differentiated from these other disorders by linking the symptoms temporally and contextually to a qualifying exposure to a traumatic event. More often than not, PTSD presents with comorbid psychiatric disorders, especially depressive disorders, anxiety disorders, and/or substance use disorders.
Continue to: Treatment: Medication, psychotherapy, or both
Treatment: Medication, psychotherapy, or both
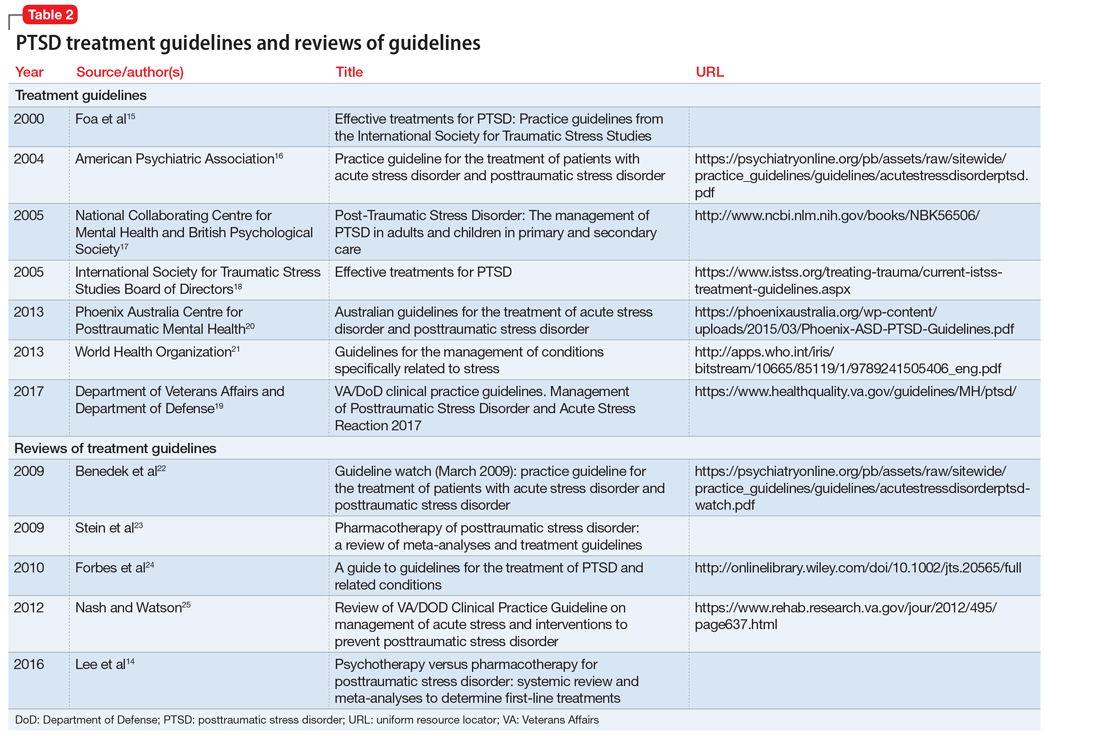
Both pharmacotherapy and psychotherapy—as monotherapy or in combination—are beneficial for treatment of PTSD. Research has not conclusively shown either treatment modality to be superior, because adequate head-to-head trials have not been conducted.4 Therefore, the choice of initial treatment is based on individual circumstances, such as patient preference for medication and/or psychotherapy, or the availability of therapists trained in evidence-based PTSD psychotherapy. Pharmacotherapeutic approaches are considered especially beneficial for depressive- and anxiety-like symptoms of PTSD, and trauma-focused psychotherapies are presumed to address the neuropathology of conditioned fear and anxiety responses involved in PTSD.14 Table 214-25 provides a list of published treatment guidelines and reviews to help clinicians seeking further detail beyond that provided in this article.
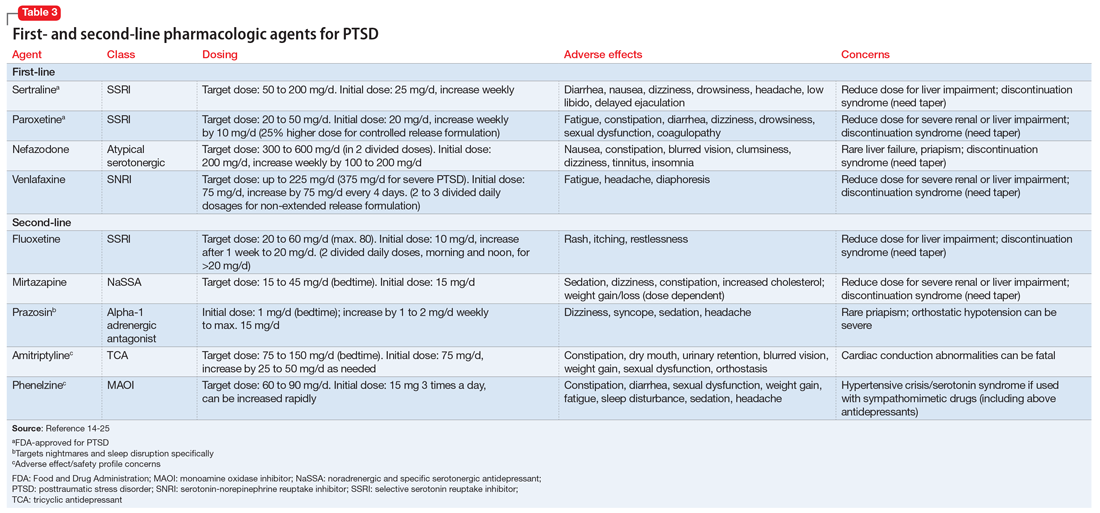
Antidepressants are the mainstay of pharmacotherapy for PTSD. These medications are effective for treating major depressive disorder, and have beneficial properties for PTSD independent of their antidepressant effects. The serotonin selective reuptake inhibitors (SSRIs) sertraline and paroxetine are FDA-approved for the treatment of PTSD.6 Other recommended medications include the serotonin-norepinephrine reuptake inhibitor (SNRI) venlafaxine, and nefazodone, an atypical serotoninergic agent.13 Other antidepressants with less published evidence of effectiveness are used as second-line pharmacotherapies for PTSD, including fluoxetine (SSRI), and mirtazapine, a noradrenergic and specific serotonergic antidepressant (NaSSA).4 Older medications, such as the tricyclic antidepressant amitriptyline and the monoamine oxidase inhibitor phenelzine, have also been used successfully as second-line treatments, but evidence of their benefit is less convincing than that supporting the first-line SSRIs/SNRIs. Additionally, their less favorable adverse effect and safety profiles make them less attractive treatment choices.13 Table 314-25 provides a list of first- and second-line medications for PTSD with recommended dosages and adverse effect profiles.
Other medications. Antiepileptics, antipsychotics, and benzodiazepines have not been demonstrated to have efficacy for primary treatment of PTSD, and none of the medications are considered first-line treatments, although sometimes they are used adjunctively in attempts to enhance the effectiveness of antidepressants. Benzodiazepines are sometimes used to target symptoms, such as sleep disturbance or hyperarousal, but only for very short periods. Several authoritative reviews strongly recommend against practices of polypharmacy that commonly involves use of these agents.4,14 Prazosin, an alpha-1 adrenergic antagonist, has been demonstrated to be an effective treatment for nightmares and sleep disturbances, and has grown increasingly popular for treating these symptoms in PTSD, especially in military veterans.13
A well-established barrier to effective pharmacotherapy of PTSD is medication nonadherence.13 Two common underlying sources of nonadherence are inconsistency with the patient’s treatment preference and intolerable adverse effects. Because SSRIs/SNRIs require 8 to 12 weeks of adequate dosing for symptom relief,13 medication adherence is vital. Explaining to patients that it takes many weeks of consistent dosing for clinical effects and reassuring them that the antidepressant agents used to treat PTSD are not habit-forming may help improve adherence.4
Psychotherapy. Prolonged exposure therapy and cognitive processing therapy—both trauma-focused therapies—have the best empirical evidence for efficacy for PTSD.4,14,26 Some patients are too anxious or avoidant to participate in trauma-focused psychotherapy and may benefit from a course of antidepressant treatment before initiating psychotherapy to reduce hyperarousal and avoidance symptoms enough to allow them to tolerate therapy that incorporates trauma memories.6 However, current PTSD treatment guidelines no longer recommend stabilization with medication or preparatory therapy as a routine prerequisite to trauma-focused psychotherapy.4
Continue to: Eye movement desensitization and reprocessing (EMDR) therapy...
Eye movement desensitization and reprocessing (EMDR) therapy has emerged as a popular trauma-focused therapy with documented effectiveness. During EMDR, the patient attends to emotionally disturbing material in brief sequential doses (which varies with individual patients) while simultaneously focusing on an external stimulus, typically therapist-directed lateral eye movements. Critics of EMDR point out that the theoretical concepts and therapeutic maneuvers (eg, finger movements to guide eye gaze) in EMDR are not consistent with current understanding of the neurobiological processes involved in PTSD. Further, studies testing separate components of the therapy have not established independent effectiveness of the therapeutic maneuvers beyond the therapeutic effects of the psychotherapy components of the procedure.4
Other psychotherapies might also be beneficial, but not enough research has been conducted to provide evidence for their effectiveness.4 Non-trauma–focused psychotherapies used for PTSD include supportive therapy, motivational interviewing, relaxation, and mindfulness. Because these therapies have less evidence of effectiveness, they are now widely considered second-line options. Psychological first aid is not a treatment for PTSD, but rather a nontreatment intervention for distress that is widely used by first responders and crisis counselors to provide compassion, support, and stabilization for people exposed to trauma, whether or not they have developed PTSD. Psychological first aid is supported by expert consensus, but it has not been studied enough to demonstrate how helpful it is as a treatment.6
Comorbidities require careful consideration
PTSD in the presence of other psychiatric disorders may require a unique and specialized approach to pharmacotherapy and psychotherapy. For instance, for a patient who has a comorbid substance use disorder, acute substance withdrawal can exacerbate PTSD symptoms. Sertraline is considered a medication of choice for these patients,13 and having a substance abuse specialist on the treatment team is desirable.4,13 A patient with comorbid traumatic brain injury (TBI) may have reduced tolerance to medications, and may require an individually-tailored and elongated titration strategy. Additionally, stimulants sometimes used to improve cognition for patients with comorbid TBI can exacerbate symptoms of hyperarousal, and these patients may need stabilization before beginning PTSD treatment. Antidepressant treatment for PTSD among patients with comorbid bipolar disorder has the potential to induce mania. Psychiatrists must consider these issues when formulating treatment plans for patients with PTSD and specific psychiatric comorbidities.4,6
PTSD symptoms can be chronic, sometimes lasting many years or even decades.27 In a longitudinal study of 716 survivors of 10 different disasters, 62% of those diagnosed with PTSD were still symptomatic 1 to 3 years after the disaster, demonstrating the enduring nature of PTSD symptoms.12 Similarly, a follow-up study of survivors of the Oklahoma City bombing found 58% of those with PTSD and 39% of those without PTSD were still reporting posttraumatic stress symptoms 7 years after the incident.28 Remarkably, these same individuals reported substantially improved functioning at work, with family and personal activities, and social interactions,28 and long-term employment disability specifically related to PTSD is highly unusual.29 Even individuals who continued to report active posttraumatic stress symptoms experienced a return of functioning equivalent to levels in individuals with no PTSD.28 These data suggest that treating psychiatrists and other mental health clinicians can be optimistic that functioning can improve remarkably over the long term, even if posttraumatic stress symptoms persist.
Bottom Line
A thorough understanding of the criteria for posttraumatic stress disorder (PTSD) is necessary for accurate diagnosis and treatment. Evidence-based treatment options for adults with PTSD include certain antidepressants and trauma-focused psychotherapies.
Related Resources
- Bernadino M, Nelson KJ. FIGHT to remember PTSD. Current Psychiatry. 2017;16(8):17.
- Koola MM. Prazosin and doxazosin for PTSD are underutilized and underdosed. Current Psychiatry. 2017;16(3):19-20,47,e1.
Drug Brand Names
Amitriptyline • Elavil, Endep
Fluoxetine • Prozac, Sarafem
Mirtazapine • Remeron
Nefazodone • Serzone
Paroxetine • Paxil
Phenelzine • Nardil
Prazosin • Minipress
Sertraline • Zoloft
Venlafaxine • Effexor
1. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. Washington, DC: American Psychiatric Association; 1980.
2. North CS, Surís AM, Smith RP, et al. The evolution of PTSD criteria across editions of the DSM. Ann Clin Psychiatry. 2016;28(3):197-208.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013
4. Downs DL, North CS. Trauma-related disorders. Overview of posttraumatic stress disorder. https://www.deckerip.com/products/scientific-american-psychiatry/table-of-contents/. Published July 2017. Accessed February 27, 2018.
5. North CS. Disaster mental health epidemiology: methodological review and interpretation of research findings. Psychiatry. 2016; 79(2):130-146.
6. North CS, Yutzy SH. Goodwin and Guze’s Psychiatric Diagnosis, 6th ed. New York, NY: Oxford University Press; 2010.
7. North CS, Nixon SJ, Shariat S, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. 1999;282(8):755-762.
8. North CS, Pfefferbaum B. Mental Health Response to Community Disasters: A Systematic Review. JAMA. 2013;310(5):507-518.
9. North CS, Pollio DE, Smith, RP, et al. Trauma exposure and posttraumatic stress disorder among employees of New York City companies affected by the September 11, 2001 attacks on the World Trade Center. Disaster Med Public Health Prep. 2011;5(suppl 2):S205-S213.
10. North CS, Oliver J, Pandya A. Examining a comprehensive model of disaster-related posttraumatic stress disorder in systematically studied survivors of 10 disasters. Am J Public Health. 2012;102(10):e40-e48.
11. Whitman JB, North CS, Downs DL, et al. A prospective study of the onset of PTSD symptoms in the first month after trauma exposure. Ann Clin Psychiatry. 2013;25(3):163-172.
12. North CS, Oliver J. Analysis of the longitudinal course of PTSD in 716 survivors of 10 disasters. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1189-1197.
13. Jeffreys M, Capehart B, Friedman MJ. Pharmacotherapy for posttraumatic stress disorder: review with clinical applications. J Rehabil Res Dev. 2012;49(5):703-715.
14. Lee DJ, Schnitzlein CW, Wolf JP, et al. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: systemic review and meta-analyses to determine first-line treatments. Depress Anxiety. 2016;33(9):792-806.
15. Foa EB, Keane T, Friedman MJ. Effective treatments for PTSD: practice guidelines from the International Society for traumatic stress studies. New York, NY: The Guilford Press; 2000.
16. Ursano RJ, Bell C, Eth S, et al; Work Group on ASD and PTSD. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Arlington, VA: American Psychiatric Association Publishing; 2004.
17. National Collaborating Centre for Mental Health. Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care. London, UK: Gaskell and the British Psychological Society; 2005.
18. Foa EB, Keane TM, Friedman MJ, eds; The Board of Directors of the International Society for Traumatic Stress Studies. Effective treatments for PTSD. 2nd ed. Oakbrook Terrace, IL: The Guilford Press; 2005.
19. Department of Veterans Affairs and Department of Defense. VA/DoD clinical practice guidelines. Management of Posttraumatic Stress Disorder and Acute Stress Reaction 2017. https://www.healthquality.va.gov/guidelines/MH/ptsd/. Published June 2017. Accessed February 26, 2018.
20. Phoenix Australia -Centre for Posttraumatic Mental Health. Australian guidelines for the treatment of acute stress disorder and posttraumatic stress disorder. Melbourne, Australia: Phoenix Australia Centre for Posttraumatic Mental Health; 2013.
21. World Health Organization. Guidelines for the management of conditions specifically related to stress. Geneva, Switzerland: World Health Organization Press; 2013.
22. Benedek DM, Friedman MJ, Zatzick D, et al. Guideline watch (March 2009): practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Focus. 2009;7(2):201-213.
23. Stein DJ, Ipser J, McAnda N. Pharmacotherapy of posttraumatic stress disorder: a review of meta-analyses and treatment guidelines. CNS Spectr. 2009;14(suppl 1):25-31.
24. Forbes D, Creamer M, Bisson JI, et al. A guide to guidelines for the treatment of PTSD and related conditions. J Trauma Stress. 2010;23(5):537-552.
25. Nash WP, Watson PJ. Review of VA/DOD clinical practice guideline on management of acute stress and interventions to prevent posttraumatic stress disorder. J Rehabil Res Dev. 2012;49(5):637-648.
26. Birur B, Moore NC, Davis LL. An evidence-based review of early intervention and prevention of posttraumatic stress disorder. Community Ment Health J. 2017;53(2):183-201.
27. Breslau N, Davis GC. Posttraumatic stress disorder in an urban population of young adults: Risk factors for chronicity. Am J Psychiatry. 1992;149(5):671-675.
28. North CS, Pfefferbaum B, Kawasaki A, et al. Psychosocial adjustment of directly exposed survivors seven years after the Oklahoma City bombing. Compr Psychiatry. 2011;52(1):1-8
29. Rasco SS, North CS. An empirical study of employment and disability over three years among survivors of major disasters. J Am Acad Psychiatry Law. 2010;38(1):80-86.
Posttraumatic stress disorder (PTSD) has increasingly become a part of American culture since its introduction in the American Psychiatric Association’s third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) in 1980.1 Since then, a proliferation of material about this disorder—both academic and popular—has been generated, yet much confusion persists surrounding the definition of the disorder, its prevalence, and its management. This review addresses the essential elements for diagnosis and treatment of PTSD.
Diagnosis: A closer look at the criteria
Criteria for the diagnosis of PTSD have evolved since 1980, with changes in the definition of trauma and the addition of symptoms and symptom groups.2 Table 13 summarizes the current DSM-5 criteria for PTSD.
Trauma exposure. An essential first step in the diagnosis of PTSD is to determine whether the individual has experienced exposure to trauma. This concept is defined in Criterion A (trauma exposure).3 PTSD is nonconformist among the psychiatric diagnoses in that it requires a specific external event as part of its definition. Misapplication of the trauma exposure criterion by many clinicians and researchers has led to misdiagnosis and erroneously high prevalence estimates of PTSD.4,5
A traumatic event is one that represents a threat to life or limb, specifically defined as “actual or threatened death, serious injury, or sexual violence.”3 DSM-5 does not allow for just any stressful event to be considered trauma. For example, no matter how distressing, failing an important test at school or being served with divorce proceedings do not represent a requisite trauma6 because these examples do not entail a threat to life or limb.
DSM-5 PTSD Criterion A also requires a qualifying exposure to the traumatic event. There are 4 types of qualifying exposures:
- direct experience of immediate serious physical danger
- eyewitness of trauma to others
- indirect exposure via violent or accidental trauma experienced by a close family member or close friend
- repeated or extreme exposure to aversive details of trauma, such as first responders collecting human remains or law enforcement officers being repeatedly exposed to horrific details of child abuse.3
Witnessed trauma must be in person; thus, viewing trauma in media reports would not constitute a qualifying exposure. Indirect trauma exposure can occur through learning of the experience of a qualifying trauma exposure by a close family member or personal friend.
It is critical to differentiate exposure to trauma (an objective construct) from the subjective distress that may be associated with it. If trauma has not occurred or a qualifying exposure is not established, no amount of distress associated with it can establish the experience as meeting Criterion A for PTSD. This does not mean that nonqualifying experiences of stressful events are not distressing; in fact, such experiences can result in substantial psychological angst. Conversely, exposure to trauma is not tantamount to a diagnosis of PTSD, as most trauma exposures do not result in PTSD.7,8
Continue to: Symptom groups
Symptom groups. DSM-5 symptom criteria for PTSD include 4 symptom groups, Criteria B to E, respectively:
- intrusion
- avoidance
- negative cognitions and mood (numbing)
- hyperarousal/reactivity.
A specific number of symptoms must be present in all 4 of the symptom groups to fulfill diagnostic criteria. Importantly, these symptoms must be linked temporally and conceptually to the traumatic exposure to qualify as PTSD symptoms. Specifically, the symptoms must be new or substantially worsened after the event. For example, continuing sleep disturbance in someone who has had lifetime difficulty sleeping would not count as a trauma-related symptom. Most symptom checklists do not properly assess diagnostic criteria for PTSD because they do not anchor the symptoms in an exposure to a traumatic event; diagnosis requires an interview to fully assess all the diagnostic criteria. Finally, the symptoms must have been present for >1 month for the diagnosis, and the symptoms must have resulted in clinically significant distress or functional impairment to qualify.
The Algorithm provides a practical way to systematically assess all DSM-5 criteria for PTSD to arrive at a diagnosis. The clinician begins by determining whether a traumatic event has occurred and whether the individual had a qualifying exposure to it. If not, PTSD cannot be diagnosed. Alternative diagnoses to consider for new disorders that arise in the context of trauma among patients who are not exposed to trauma include major depressive disorder, adjustment disorder, and bereavement, as well as acute stress disorder (which is not validated but has potential utility as a billable diagnosis).
Avoidance and numbing symptoms (present in Criteria C and D) have been shown to represent markers of illness and can be useful in predicting PTSD.8-10 Unlike symptoms of intrusion and hyperarousal (Criteria B and E, respectively), which are very common and by themselves are nonpathological, avoidance/numbing symptoms occur much less commonly, are associated with functional impairment and other indicators of illness, and are strongly associated with PTSD.6 Prominent avoidance/numbing profiles have been demonstrated to predict PTSD in the first 1 to 2 weeks after trauma exposure, before PTSD can be formally diagnosed.11 Posttraumatic stress symptoms are nearly universal after trauma exposure, even in people who do not develop PTSD.5 Intrusion and hyperarousal symptoms constitute most of such symptoms,7 and these symptoms in the absence of prominent avoidance/numbing can be considered normative distress responses to trauma exposure.12
Some PTSD symptoms may seem quite similar to symptoms of depressive disorders and anxiety disorders. PTSD can be differentiated from these other disorders by linking the symptoms temporally and contextually to a qualifying exposure to a traumatic event. More often than not, PTSD presents with comorbid psychiatric disorders, especially depressive disorders, anxiety disorders, and/or substance use disorders.
Continue to: Treatment: Medication, psychotherapy, or both
Treatment: Medication, psychotherapy, or both
Both pharmacotherapy and psychotherapy—as monotherapy or in combination—are beneficial for treatment of PTSD. Research has not conclusively shown either treatment modality to be superior, because adequate head-to-head trials have not been conducted.4 Therefore, the choice of initial treatment is based on individual circumstances, such as patient preference for medication and/or psychotherapy, or the availability of therapists trained in evidence-based PTSD psychotherapy. Pharmacotherapeutic approaches are considered especially beneficial for depressive- and anxiety-like symptoms of PTSD, and trauma-focused psychotherapies are presumed to address the neuropathology of conditioned fear and anxiety responses involved in PTSD.14 Table 214-25 provides a list of published treatment guidelines and reviews to help clinicians seeking further detail beyond that provided in this article.
Antidepressants are the mainstay of pharmacotherapy for PTSD. These medications are effective for treating major depressive disorder, and have beneficial properties for PTSD independent of their antidepressant effects. The serotonin selective reuptake inhibitors (SSRIs) sertraline and paroxetine are FDA-approved for the treatment of PTSD.6 Other recommended medications include the serotonin-norepinephrine reuptake inhibitor (SNRI) venlafaxine, and nefazodone, an atypical serotoninergic agent.13 Other antidepressants with less published evidence of effectiveness are used as second-line pharmacotherapies for PTSD, including fluoxetine (SSRI), and mirtazapine, a noradrenergic and specific serotonergic antidepressant (NaSSA).4 Older medications, such as the tricyclic antidepressant amitriptyline and the monoamine oxidase inhibitor phenelzine, have also been used successfully as second-line treatments, but evidence of their benefit is less convincing than that supporting the first-line SSRIs/SNRIs. Additionally, their less favorable adverse effect and safety profiles make them less attractive treatment choices.13 Table 314-25 provides a list of first- and second-line medications for PTSD with recommended dosages and adverse effect profiles.
Other medications. Antiepileptics, antipsychotics, and benzodiazepines have not been demonstrated to have efficacy for primary treatment of PTSD, and none of the medications are considered first-line treatments, although sometimes they are used adjunctively in attempts to enhance the effectiveness of antidepressants. Benzodiazepines are sometimes used to target symptoms, such as sleep disturbance or hyperarousal, but only for very short periods. Several authoritative reviews strongly recommend against practices of polypharmacy that commonly involves use of these agents.4,14 Prazosin, an alpha-1 adrenergic antagonist, has been demonstrated to be an effective treatment for nightmares and sleep disturbances, and has grown increasingly popular for treating these symptoms in PTSD, especially in military veterans.13
A well-established barrier to effective pharmacotherapy of PTSD is medication nonadherence.13 Two common underlying sources of nonadherence are inconsistency with the patient’s treatment preference and intolerable adverse effects. Because SSRIs/SNRIs require 8 to 12 weeks of adequate dosing for symptom relief,13 medication adherence is vital. Explaining to patients that it takes many weeks of consistent dosing for clinical effects and reassuring them that the antidepressant agents used to treat PTSD are not habit-forming may help improve adherence.4
Psychotherapy. Prolonged exposure therapy and cognitive processing therapy—both trauma-focused therapies—have the best empirical evidence for efficacy for PTSD.4,14,26 Some patients are too anxious or avoidant to participate in trauma-focused psychotherapy and may benefit from a course of antidepressant treatment before initiating psychotherapy to reduce hyperarousal and avoidance symptoms enough to allow them to tolerate therapy that incorporates trauma memories.6 However, current PTSD treatment guidelines no longer recommend stabilization with medication or preparatory therapy as a routine prerequisite to trauma-focused psychotherapy.4
Continue to: Eye movement desensitization and reprocessing (EMDR) therapy...
Eye movement desensitization and reprocessing (EMDR) therapy has emerged as a popular trauma-focused therapy with documented effectiveness. During EMDR, the patient attends to emotionally disturbing material in brief sequential doses (which varies with individual patients) while simultaneously focusing on an external stimulus, typically therapist-directed lateral eye movements. Critics of EMDR point out that the theoretical concepts and therapeutic maneuvers (eg, finger movements to guide eye gaze) in EMDR are not consistent with current understanding of the neurobiological processes involved in PTSD. Further, studies testing separate components of the therapy have not established independent effectiveness of the therapeutic maneuvers beyond the therapeutic effects of the psychotherapy components of the procedure.4
Other psychotherapies might also be beneficial, but not enough research has been conducted to provide evidence for their effectiveness.4 Non-trauma–focused psychotherapies used for PTSD include supportive therapy, motivational interviewing, relaxation, and mindfulness. Because these therapies have less evidence of effectiveness, they are now widely considered second-line options. Psychological first aid is not a treatment for PTSD, but rather a nontreatment intervention for distress that is widely used by first responders and crisis counselors to provide compassion, support, and stabilization for people exposed to trauma, whether or not they have developed PTSD. Psychological first aid is supported by expert consensus, but it has not been studied enough to demonstrate how helpful it is as a treatment.6
Comorbidities require careful consideration
PTSD in the presence of other psychiatric disorders may require a unique and specialized approach to pharmacotherapy and psychotherapy. For instance, for a patient who has a comorbid substance use disorder, acute substance withdrawal can exacerbate PTSD symptoms. Sertraline is considered a medication of choice for these patients,13 and having a substance abuse specialist on the treatment team is desirable.4,13 A patient with comorbid traumatic brain injury (TBI) may have reduced tolerance to medications, and may require an individually-tailored and elongated titration strategy. Additionally, stimulants sometimes used to improve cognition for patients with comorbid TBI can exacerbate symptoms of hyperarousal, and these patients may need stabilization before beginning PTSD treatment. Antidepressant treatment for PTSD among patients with comorbid bipolar disorder has the potential to induce mania. Psychiatrists must consider these issues when formulating treatment plans for patients with PTSD and specific psychiatric comorbidities.4,6
PTSD symptoms can be chronic, sometimes lasting many years or even decades.27 In a longitudinal study of 716 survivors of 10 different disasters, 62% of those diagnosed with PTSD were still symptomatic 1 to 3 years after the disaster, demonstrating the enduring nature of PTSD symptoms.12 Similarly, a follow-up study of survivors of the Oklahoma City bombing found 58% of those with PTSD and 39% of those without PTSD were still reporting posttraumatic stress symptoms 7 years after the incident.28 Remarkably, these same individuals reported substantially improved functioning at work, with family and personal activities, and social interactions,28 and long-term employment disability specifically related to PTSD is highly unusual.29 Even individuals who continued to report active posttraumatic stress symptoms experienced a return of functioning equivalent to levels in individuals with no PTSD.28 These data suggest that treating psychiatrists and other mental health clinicians can be optimistic that functioning can improve remarkably over the long term, even if posttraumatic stress symptoms persist.
Bottom Line
A thorough understanding of the criteria for posttraumatic stress disorder (PTSD) is necessary for accurate diagnosis and treatment. Evidence-based treatment options for adults with PTSD include certain antidepressants and trauma-focused psychotherapies.
Related Resources
- Bernadino M, Nelson KJ. FIGHT to remember PTSD. Current Psychiatry. 2017;16(8):17.
- Koola MM. Prazosin and doxazosin for PTSD are underutilized and underdosed. Current Psychiatry. 2017;16(3):19-20,47,e1.
Drug Brand Names
Amitriptyline • Elavil, Endep
Fluoxetine • Prozac, Sarafem
Mirtazapine • Remeron
Nefazodone • Serzone
Paroxetine • Paxil
Phenelzine • Nardil
Prazosin • Minipress
Sertraline • Zoloft
Venlafaxine • Effexor
Posttraumatic stress disorder (PTSD) has increasingly become a part of American culture since its introduction in the American Psychiatric Association’s third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) in 1980.1 Since then, a proliferation of material about this disorder—both academic and popular—has been generated, yet much confusion persists surrounding the definition of the disorder, its prevalence, and its management. This review addresses the essential elements for diagnosis and treatment of PTSD.
Diagnosis: A closer look at the criteria
Criteria for the diagnosis of PTSD have evolved since 1980, with changes in the definition of trauma and the addition of symptoms and symptom groups.2 Table 13 summarizes the current DSM-5 criteria for PTSD.
Trauma exposure. An essential first step in the diagnosis of PTSD is to determine whether the individual has experienced exposure to trauma. This concept is defined in Criterion A (trauma exposure).3 PTSD is nonconformist among the psychiatric diagnoses in that it requires a specific external event as part of its definition. Misapplication of the trauma exposure criterion by many clinicians and researchers has led to misdiagnosis and erroneously high prevalence estimates of PTSD.4,5
A traumatic event is one that represents a threat to life or limb, specifically defined as “actual or threatened death, serious injury, or sexual violence.”3 DSM-5 does not allow for just any stressful event to be considered trauma. For example, no matter how distressing, failing an important test at school or being served with divorce proceedings do not represent a requisite trauma6 because these examples do not entail a threat to life or limb.
DSM-5 PTSD Criterion A also requires a qualifying exposure to the traumatic event. There are 4 types of qualifying exposures:
- direct experience of immediate serious physical danger
- eyewitness of trauma to others
- indirect exposure via violent or accidental trauma experienced by a close family member or close friend
- repeated or extreme exposure to aversive details of trauma, such as first responders collecting human remains or law enforcement officers being repeatedly exposed to horrific details of child abuse.3
Witnessed trauma must be in person; thus, viewing trauma in media reports would not constitute a qualifying exposure. Indirect trauma exposure can occur through learning of the experience of a qualifying trauma exposure by a close family member or personal friend.
It is critical to differentiate exposure to trauma (an objective construct) from the subjective distress that may be associated with it. If trauma has not occurred or a qualifying exposure is not established, no amount of distress associated with it can establish the experience as meeting Criterion A for PTSD. This does not mean that nonqualifying experiences of stressful events are not distressing; in fact, such experiences can result in substantial psychological angst. Conversely, exposure to trauma is not tantamount to a diagnosis of PTSD, as most trauma exposures do not result in PTSD.7,8
Continue to: Symptom groups
Symptom groups. DSM-5 symptom criteria for PTSD include 4 symptom groups, Criteria B to E, respectively:
- intrusion
- avoidance
- negative cognitions and mood (numbing)
- hyperarousal/reactivity.
A specific number of symptoms must be present in all 4 of the symptom groups to fulfill diagnostic criteria. Importantly, these symptoms must be linked temporally and conceptually to the traumatic exposure to qualify as PTSD symptoms. Specifically, the symptoms must be new or substantially worsened after the event. For example, continuing sleep disturbance in someone who has had lifetime difficulty sleeping would not count as a trauma-related symptom. Most symptom checklists do not properly assess diagnostic criteria for PTSD because they do not anchor the symptoms in an exposure to a traumatic event; diagnosis requires an interview to fully assess all the diagnostic criteria. Finally, the symptoms must have been present for >1 month for the diagnosis, and the symptoms must have resulted in clinically significant distress or functional impairment to qualify.
The Algorithm provides a practical way to systematically assess all DSM-5 criteria for PTSD to arrive at a diagnosis. The clinician begins by determining whether a traumatic event has occurred and whether the individual had a qualifying exposure to it. If not, PTSD cannot be diagnosed. Alternative diagnoses to consider for new disorders that arise in the context of trauma among patients who are not exposed to trauma include major depressive disorder, adjustment disorder, and bereavement, as well as acute stress disorder (which is not validated but has potential utility as a billable diagnosis).
Avoidance and numbing symptoms (present in Criteria C and D) have been shown to represent markers of illness and can be useful in predicting PTSD.8-10 Unlike symptoms of intrusion and hyperarousal (Criteria B and E, respectively), which are very common and by themselves are nonpathological, avoidance/numbing symptoms occur much less commonly, are associated with functional impairment and other indicators of illness, and are strongly associated with PTSD.6 Prominent avoidance/numbing profiles have been demonstrated to predict PTSD in the first 1 to 2 weeks after trauma exposure, before PTSD can be formally diagnosed.11 Posttraumatic stress symptoms are nearly universal after trauma exposure, even in people who do not develop PTSD.5 Intrusion and hyperarousal symptoms constitute most of such symptoms,7 and these symptoms in the absence of prominent avoidance/numbing can be considered normative distress responses to trauma exposure.12
Some PTSD symptoms may seem quite similar to symptoms of depressive disorders and anxiety disorders. PTSD can be differentiated from these other disorders by linking the symptoms temporally and contextually to a qualifying exposure to a traumatic event. More often than not, PTSD presents with comorbid psychiatric disorders, especially depressive disorders, anxiety disorders, and/or substance use disorders.
Continue to: Treatment: Medication, psychotherapy, or both
Treatment: Medication, psychotherapy, or both
Both pharmacotherapy and psychotherapy—as monotherapy or in combination—are beneficial for treatment of PTSD. Research has not conclusively shown either treatment modality to be superior, because adequate head-to-head trials have not been conducted.4 Therefore, the choice of initial treatment is based on individual circumstances, such as patient preference for medication and/or psychotherapy, or the availability of therapists trained in evidence-based PTSD psychotherapy. Pharmacotherapeutic approaches are considered especially beneficial for depressive- and anxiety-like symptoms of PTSD, and trauma-focused psychotherapies are presumed to address the neuropathology of conditioned fear and anxiety responses involved in PTSD.14 Table 214-25 provides a list of published treatment guidelines and reviews to help clinicians seeking further detail beyond that provided in this article.
Antidepressants are the mainstay of pharmacotherapy for PTSD. These medications are effective for treating major depressive disorder, and have beneficial properties for PTSD independent of their antidepressant effects. The serotonin selective reuptake inhibitors (SSRIs) sertraline and paroxetine are FDA-approved for the treatment of PTSD.6 Other recommended medications include the serotonin-norepinephrine reuptake inhibitor (SNRI) venlafaxine, and nefazodone, an atypical serotoninergic agent.13 Other antidepressants with less published evidence of effectiveness are used as second-line pharmacotherapies for PTSD, including fluoxetine (SSRI), and mirtazapine, a noradrenergic and specific serotonergic antidepressant (NaSSA).4 Older medications, such as the tricyclic antidepressant amitriptyline and the monoamine oxidase inhibitor phenelzine, have also been used successfully as second-line treatments, but evidence of their benefit is less convincing than that supporting the first-line SSRIs/SNRIs. Additionally, their less favorable adverse effect and safety profiles make them less attractive treatment choices.13 Table 314-25 provides a list of first- and second-line medications for PTSD with recommended dosages and adverse effect profiles.
Other medications. Antiepileptics, antipsychotics, and benzodiazepines have not been demonstrated to have efficacy for primary treatment of PTSD, and none of the medications are considered first-line treatments, although sometimes they are used adjunctively in attempts to enhance the effectiveness of antidepressants. Benzodiazepines are sometimes used to target symptoms, such as sleep disturbance or hyperarousal, but only for very short periods. Several authoritative reviews strongly recommend against practices of polypharmacy that commonly involves use of these agents.4,14 Prazosin, an alpha-1 adrenergic antagonist, has been demonstrated to be an effective treatment for nightmares and sleep disturbances, and has grown increasingly popular for treating these symptoms in PTSD, especially in military veterans.13
A well-established barrier to effective pharmacotherapy of PTSD is medication nonadherence.13 Two common underlying sources of nonadherence are inconsistency with the patient’s treatment preference and intolerable adverse effects. Because SSRIs/SNRIs require 8 to 12 weeks of adequate dosing for symptom relief,13 medication adherence is vital. Explaining to patients that it takes many weeks of consistent dosing for clinical effects and reassuring them that the antidepressant agents used to treat PTSD are not habit-forming may help improve adherence.4
Psychotherapy. Prolonged exposure therapy and cognitive processing therapy—both trauma-focused therapies—have the best empirical evidence for efficacy for PTSD.4,14,26 Some patients are too anxious or avoidant to participate in trauma-focused psychotherapy and may benefit from a course of antidepressant treatment before initiating psychotherapy to reduce hyperarousal and avoidance symptoms enough to allow them to tolerate therapy that incorporates trauma memories.6 However, current PTSD treatment guidelines no longer recommend stabilization with medication or preparatory therapy as a routine prerequisite to trauma-focused psychotherapy.4
Continue to: Eye movement desensitization and reprocessing (EMDR) therapy...
Eye movement desensitization and reprocessing (EMDR) therapy has emerged as a popular trauma-focused therapy with documented effectiveness. During EMDR, the patient attends to emotionally disturbing material in brief sequential doses (which varies with individual patients) while simultaneously focusing on an external stimulus, typically therapist-directed lateral eye movements. Critics of EMDR point out that the theoretical concepts and therapeutic maneuvers (eg, finger movements to guide eye gaze) in EMDR are not consistent with current understanding of the neurobiological processes involved in PTSD. Further, studies testing separate components of the therapy have not established independent effectiveness of the therapeutic maneuvers beyond the therapeutic effects of the psychotherapy components of the procedure.4
Other psychotherapies might also be beneficial, but not enough research has been conducted to provide evidence for their effectiveness.4 Non-trauma–focused psychotherapies used for PTSD include supportive therapy, motivational interviewing, relaxation, and mindfulness. Because these therapies have less evidence of effectiveness, they are now widely considered second-line options. Psychological first aid is not a treatment for PTSD, but rather a nontreatment intervention for distress that is widely used by first responders and crisis counselors to provide compassion, support, and stabilization for people exposed to trauma, whether or not they have developed PTSD. Psychological first aid is supported by expert consensus, but it has not been studied enough to demonstrate how helpful it is as a treatment.6
Comorbidities require careful consideration
PTSD in the presence of other psychiatric disorders may require a unique and specialized approach to pharmacotherapy and psychotherapy. For instance, for a patient who has a comorbid substance use disorder, acute substance withdrawal can exacerbate PTSD symptoms. Sertraline is considered a medication of choice for these patients,13 and having a substance abuse specialist on the treatment team is desirable.4,13 A patient with comorbid traumatic brain injury (TBI) may have reduced tolerance to medications, and may require an individually-tailored and elongated titration strategy. Additionally, stimulants sometimes used to improve cognition for patients with comorbid TBI can exacerbate symptoms of hyperarousal, and these patients may need stabilization before beginning PTSD treatment. Antidepressant treatment for PTSD among patients with comorbid bipolar disorder has the potential to induce mania. Psychiatrists must consider these issues when formulating treatment plans for patients with PTSD and specific psychiatric comorbidities.4,6
PTSD symptoms can be chronic, sometimes lasting many years or even decades.27 In a longitudinal study of 716 survivors of 10 different disasters, 62% of those diagnosed with PTSD were still symptomatic 1 to 3 years after the disaster, demonstrating the enduring nature of PTSD symptoms.12 Similarly, a follow-up study of survivors of the Oklahoma City bombing found 58% of those with PTSD and 39% of those without PTSD were still reporting posttraumatic stress symptoms 7 years after the incident.28 Remarkably, these same individuals reported substantially improved functioning at work, with family and personal activities, and social interactions,28 and long-term employment disability specifically related to PTSD is highly unusual.29 Even individuals who continued to report active posttraumatic stress symptoms experienced a return of functioning equivalent to levels in individuals with no PTSD.28 These data suggest that treating psychiatrists and other mental health clinicians can be optimistic that functioning can improve remarkably over the long term, even if posttraumatic stress symptoms persist.
Bottom Line
A thorough understanding of the criteria for posttraumatic stress disorder (PTSD) is necessary for accurate diagnosis and treatment. Evidence-based treatment options for adults with PTSD include certain antidepressants and trauma-focused psychotherapies.
Related Resources
- Bernadino M, Nelson KJ. FIGHT to remember PTSD. Current Psychiatry. 2017;16(8):17.
- Koola MM. Prazosin and doxazosin for PTSD are underutilized and underdosed. Current Psychiatry. 2017;16(3):19-20,47,e1.
Drug Brand Names
Amitriptyline • Elavil, Endep
Fluoxetine • Prozac, Sarafem
Mirtazapine • Remeron
Nefazodone • Serzone
Paroxetine • Paxil
Phenelzine • Nardil
Prazosin • Minipress
Sertraline • Zoloft
Venlafaxine • Effexor
1. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. Washington, DC: American Psychiatric Association; 1980.
2. North CS, Surís AM, Smith RP, et al. The evolution of PTSD criteria across editions of the DSM. Ann Clin Psychiatry. 2016;28(3):197-208.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013
4. Downs DL, North CS. Trauma-related disorders. Overview of posttraumatic stress disorder. https://www.deckerip.com/products/scientific-american-psychiatry/table-of-contents/. Published July 2017. Accessed February 27, 2018.
5. North CS. Disaster mental health epidemiology: methodological review and interpretation of research findings. Psychiatry. 2016; 79(2):130-146.
6. North CS, Yutzy SH. Goodwin and Guze’s Psychiatric Diagnosis, 6th ed. New York, NY: Oxford University Press; 2010.
7. North CS, Nixon SJ, Shariat S, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. 1999;282(8):755-762.
8. North CS, Pfefferbaum B. Mental Health Response to Community Disasters: A Systematic Review. JAMA. 2013;310(5):507-518.
9. North CS, Pollio DE, Smith, RP, et al. Trauma exposure and posttraumatic stress disorder among employees of New York City companies affected by the September 11, 2001 attacks on the World Trade Center. Disaster Med Public Health Prep. 2011;5(suppl 2):S205-S213.
10. North CS, Oliver J, Pandya A. Examining a comprehensive model of disaster-related posttraumatic stress disorder in systematically studied survivors of 10 disasters. Am J Public Health. 2012;102(10):e40-e48.
11. Whitman JB, North CS, Downs DL, et al. A prospective study of the onset of PTSD symptoms in the first month after trauma exposure. Ann Clin Psychiatry. 2013;25(3):163-172.
12. North CS, Oliver J. Analysis of the longitudinal course of PTSD in 716 survivors of 10 disasters. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1189-1197.
13. Jeffreys M, Capehart B, Friedman MJ. Pharmacotherapy for posttraumatic stress disorder: review with clinical applications. J Rehabil Res Dev. 2012;49(5):703-715.
14. Lee DJ, Schnitzlein CW, Wolf JP, et al. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: systemic review and meta-analyses to determine first-line treatments. Depress Anxiety. 2016;33(9):792-806.
15. Foa EB, Keane T, Friedman MJ. Effective treatments for PTSD: practice guidelines from the International Society for traumatic stress studies. New York, NY: The Guilford Press; 2000.
16. Ursano RJ, Bell C, Eth S, et al; Work Group on ASD and PTSD. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Arlington, VA: American Psychiatric Association Publishing; 2004.
17. National Collaborating Centre for Mental Health. Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care. London, UK: Gaskell and the British Psychological Society; 2005.
18. Foa EB, Keane TM, Friedman MJ, eds; The Board of Directors of the International Society for Traumatic Stress Studies. Effective treatments for PTSD. 2nd ed. Oakbrook Terrace, IL: The Guilford Press; 2005.
19. Department of Veterans Affairs and Department of Defense. VA/DoD clinical practice guidelines. Management of Posttraumatic Stress Disorder and Acute Stress Reaction 2017. https://www.healthquality.va.gov/guidelines/MH/ptsd/. Published June 2017. Accessed February 26, 2018.
20. Phoenix Australia -Centre for Posttraumatic Mental Health. Australian guidelines for the treatment of acute stress disorder and posttraumatic stress disorder. Melbourne, Australia: Phoenix Australia Centre for Posttraumatic Mental Health; 2013.
21. World Health Organization. Guidelines for the management of conditions specifically related to stress. Geneva, Switzerland: World Health Organization Press; 2013.
22. Benedek DM, Friedman MJ, Zatzick D, et al. Guideline watch (March 2009): practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Focus. 2009;7(2):201-213.
23. Stein DJ, Ipser J, McAnda N. Pharmacotherapy of posttraumatic stress disorder: a review of meta-analyses and treatment guidelines. CNS Spectr. 2009;14(suppl 1):25-31.
24. Forbes D, Creamer M, Bisson JI, et al. A guide to guidelines for the treatment of PTSD and related conditions. J Trauma Stress. 2010;23(5):537-552.
25. Nash WP, Watson PJ. Review of VA/DOD clinical practice guideline on management of acute stress and interventions to prevent posttraumatic stress disorder. J Rehabil Res Dev. 2012;49(5):637-648.
26. Birur B, Moore NC, Davis LL. An evidence-based review of early intervention and prevention of posttraumatic stress disorder. Community Ment Health J. 2017;53(2):183-201.
27. Breslau N, Davis GC. Posttraumatic stress disorder in an urban population of young adults: Risk factors for chronicity. Am J Psychiatry. 1992;149(5):671-675.
28. North CS, Pfefferbaum B, Kawasaki A, et al. Psychosocial adjustment of directly exposed survivors seven years after the Oklahoma City bombing. Compr Psychiatry. 2011;52(1):1-8
29. Rasco SS, North CS. An empirical study of employment and disability over three years among survivors of major disasters. J Am Acad Psychiatry Law. 2010;38(1):80-86.
1. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. Washington, DC: American Psychiatric Association; 1980.
2. North CS, Surís AM, Smith RP, et al. The evolution of PTSD criteria across editions of the DSM. Ann Clin Psychiatry. 2016;28(3):197-208.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013
4. Downs DL, North CS. Trauma-related disorders. Overview of posttraumatic stress disorder. https://www.deckerip.com/products/scientific-american-psychiatry/table-of-contents/. Published July 2017. Accessed February 27, 2018.
5. North CS. Disaster mental health epidemiology: methodological review and interpretation of research findings. Psychiatry. 2016; 79(2):130-146.
6. North CS, Yutzy SH. Goodwin and Guze’s Psychiatric Diagnosis, 6th ed. New York, NY: Oxford University Press; 2010.
7. North CS, Nixon SJ, Shariat S, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. 1999;282(8):755-762.
8. North CS, Pfefferbaum B. Mental Health Response to Community Disasters: A Systematic Review. JAMA. 2013;310(5):507-518.
9. North CS, Pollio DE, Smith, RP, et al. Trauma exposure and posttraumatic stress disorder among employees of New York City companies affected by the September 11, 2001 attacks on the World Trade Center. Disaster Med Public Health Prep. 2011;5(suppl 2):S205-S213.
10. North CS, Oliver J, Pandya A. Examining a comprehensive model of disaster-related posttraumatic stress disorder in systematically studied survivors of 10 disasters. Am J Public Health. 2012;102(10):e40-e48.
11. Whitman JB, North CS, Downs DL, et al. A prospective study of the onset of PTSD symptoms in the first month after trauma exposure. Ann Clin Psychiatry. 2013;25(3):163-172.
12. North CS, Oliver J. Analysis of the longitudinal course of PTSD in 716 survivors of 10 disasters. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1189-1197.
13. Jeffreys M, Capehart B, Friedman MJ. Pharmacotherapy for posttraumatic stress disorder: review with clinical applications. J Rehabil Res Dev. 2012;49(5):703-715.
14. Lee DJ, Schnitzlein CW, Wolf JP, et al. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: systemic review and meta-analyses to determine first-line treatments. Depress Anxiety. 2016;33(9):792-806.
15. Foa EB, Keane T, Friedman MJ. Effective treatments for PTSD: practice guidelines from the International Society for traumatic stress studies. New York, NY: The Guilford Press; 2000.
16. Ursano RJ, Bell C, Eth S, et al; Work Group on ASD and PTSD. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Arlington, VA: American Psychiatric Association Publishing; 2004.
17. National Collaborating Centre for Mental Health. Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care. London, UK: Gaskell and the British Psychological Society; 2005.
18. Foa EB, Keane TM, Friedman MJ, eds; The Board of Directors of the International Society for Traumatic Stress Studies. Effective treatments for PTSD. 2nd ed. Oakbrook Terrace, IL: The Guilford Press; 2005.
19. Department of Veterans Affairs and Department of Defense. VA/DoD clinical practice guidelines. Management of Posttraumatic Stress Disorder and Acute Stress Reaction 2017. https://www.healthquality.va.gov/guidelines/MH/ptsd/. Published June 2017. Accessed February 26, 2018.
20. Phoenix Australia -Centre for Posttraumatic Mental Health. Australian guidelines for the treatment of acute stress disorder and posttraumatic stress disorder. Melbourne, Australia: Phoenix Australia Centre for Posttraumatic Mental Health; 2013.
21. World Health Organization. Guidelines for the management of conditions specifically related to stress. Geneva, Switzerland: World Health Organization Press; 2013.
22. Benedek DM, Friedman MJ, Zatzick D, et al. Guideline watch (March 2009): practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Focus. 2009;7(2):201-213.
23. Stein DJ, Ipser J, McAnda N. Pharmacotherapy of posttraumatic stress disorder: a review of meta-analyses and treatment guidelines. CNS Spectr. 2009;14(suppl 1):25-31.
24. Forbes D, Creamer M, Bisson JI, et al. A guide to guidelines for the treatment of PTSD and related conditions. J Trauma Stress. 2010;23(5):537-552.
25. Nash WP, Watson PJ. Review of VA/DOD clinical practice guideline on management of acute stress and interventions to prevent posttraumatic stress disorder. J Rehabil Res Dev. 2012;49(5):637-648.
26. Birur B, Moore NC, Davis LL. An evidence-based review of early intervention and prevention of posttraumatic stress disorder. Community Ment Health J. 2017;53(2):183-201.
27. Breslau N, Davis GC. Posttraumatic stress disorder in an urban population of young adults: Risk factors for chronicity. Am J Psychiatry. 1992;149(5):671-675.
28. North CS, Pfefferbaum B, Kawasaki A, et al. Psychosocial adjustment of directly exposed survivors seven years after the Oklahoma City bombing. Compr Psychiatry. 2011;52(1):1-8
29. Rasco SS, North CS. An empirical study of employment and disability over three years among survivors of major disasters. J Am Acad Psychiatry Law. 2010;38(1):80-86.
Development and Implementation of a Homeless Mobile Medical/Mental Veteran Intervention
Research has consistently identified remarkably high rates of addiction, mental illness, and health problems in the homeless population.1-9 Yet in spite of extensive service needs for these problems, abundant evidence exists of consistent underuse of health care services by homeless populations.10-12 Most of the homeless population reside in emergency shelters or in transitional or supportive housing, but many remain in places not meant for human habitation.
Homelessness is significantly overrepresented among military veterans.13 The January 2016 national point-in-time count identified 39,471 veterans experiencing homelessness.13 Iraq and Afghanistan veterans seem to have an especially high risk for homelessness.13-15 Disheartening statistics such as these prompted former VA Secretary Eric Shinseki to pledge to end veteran homelessness by December 2015.16 He argued in support of this mission that 85% of veteran homeless resources go to health care—implying that homelessness among veterans is primarily a health care issue, which is heavily burdened by substance abuse and other psychiatric and medical illnesses.17
Health care service use has been associated with improved health, mental health, and outcomes among homeless populations.12,18 Unfortunately, access to these services is limited by barriers associated with homelessness, such as transportation or lack of proper identification.19,20 Veterans experiencing homelessness also face these common barriers to health care, and unsheltered veterans especially underutilize VA health care services.21
Housing First—a successful model that places individuals into housing without prerequisites for sobriety, active participation in treatment, or other behavioral accomplishments, such as gainful employment—has not managed yet to place all the disengaged homeless veteran population into stable housing.22 However, the Housing First model, which is based on the individual’s priorities, is consistent with the approach of a new program at the VA North Texas Health Care System (VANTHCS).
The VHA, similar to other health care systems, is engaged in a cultural transformation to convert its health care approach from a traditional medical model to patient-centered care (PCC).23 In this priority area, a strategic objective is for the VHA to partner with each veteran to create a personalized, proactive strategy to optimize health and well-being and when needed provide state-of-the-art disease management. Patient-centered care is designed to address veterans’ specific needs in spiritual, environmental, physical, mental, and social domains and empower veterans to become active participants in their care. Patient-centered care differs from the traditional medical model in that patients are active participants in their treatment, partnering and collaborating with their providers on care that is quality-of-life centered instead of disease centered.23 This model is based on both respect for patients as unique individuals and on the obligation to care for them on their own terms, focused on their self-identified goals and aspirations.24
At VANTHCS, the Homeless Mobile Medical/Mental Veteran (HMMM-V) pilot program was designed to deliver effective health care services to a homeless subpopulation of veterans who historically have been the most difficult to serve—those living in unsheltered environments, such as under bridges and in encampments. The purpose of the HMMM-V program was to contact and serve veterans not currently being reached by the VA system of care, using a PCC model.
This pilot program was initially funded in January 2013 by a 2-year grant from the Office of Patient Centered Care and Cultural Transformation to apply the PCC approach to engage veteran participation. For this project, the VA Personal Health Inventory tool—originally designed for use with the general veteran population—was adapted for use with the homeless veteran population. The grant funding period covered the design, development, and implementation of the HMMM-V program; thereafter, VANTHCS provided resources through its Comprehensive Homeless Center Programs to assure its sustainability and continued use of the clinical assessment tool created for this project.
This article describes the development and implementation of this novel program with sufficient detail to inform the development of similar programs in other sites. Descriptions of the program and staffing, creation of community partnerships, and modification of an assessment instrument are provided. It also illustrates the original implementation period of the HMMM-V program through presentation of self-reported data on the first homeless veterans it served.
Equipment and Staffing
A custom 28-foot mobile outreach vehicle was assembled according to specifications identified by the HMMM-V team as necessary to conduct the program’s interventions. The van became fully operational on April 8, 2015, after it underwent all the required reviews and inspections (eg, safety, infection control, etc) and was accredited in 2015 by the Commission on Accreditation of Rehabilitation Facilities.
The HMMM-V van has a driver compartment that is separate from its services rooms, which include a patient registration area, a fully equipped examination room, a laboratory area, and a bathroom. The vehicle is equipped with a wheelchair lift and an awning to shade outdoor areas where tables and chairs are set up for patient/staff waiting and rest areas. The vehicle is stocked with essential equipment and supplies needed to conduct work in off-street locations, vacant lots, under bridges, fields, unpaved paths, etc. It also is equipped with telemedicine capabilities to provide clinical supervision and access to attending physicians and specialists at VANTHCS. Personnel carry cell phones and laptop computers with secure Internet connections using a commercially available mobile wireless Wi-Fi hotspot to facilitate documentation of medical records and communication from the field.
This reliable type of equipment is routine for use in VA field operations; the only hurdle using these technologies for the program was acquiring funding and purchasing the equipment. The vehicle is further equipped with a refrigerator solely for secure storage of pharmaceutical supplies, a second refrigerator for specimens, and wall-mounted blood pressure and otoscope/ophthalmoscope units. The vehicle is supplied with thermometers, scales, phlebotomy supplies, and first-aid kits and is stocked with vaccines and medications, including antibiotic, hypertensive, diabetic, allergy, and over-the-counter pain medications. A more comprehensive list of supplies for the vehicle is available from the authors on request.
Medication provisions supplied to the HMMM-V mobile clinic conform to the Texas State Board of Pharmacy compliance regulations. Because the vehicle is designated as federal property and has U.S. government license plates, it is considered an extension of VANTHCS Pharmacy Service and falls under its pharmacy license. A medication formulary was created with input from HMMM-V prescribers and Dallas VAMC Pharmacy Service pharmacists. To safeguard the integrity of these pharmaceutical agents, the HMMM-V physician assistant picks up the medications before field deployment and returns the unused medications to the Dallas VAMC at the end of the day. The medications are transported in locked containers and placed either in a locked medication refrigerator or cabinet on the mobile unit.
For medication prescriptions that need laboratory testing before prescribing them, HMMM-V prescribers can check the VA electronic medical record from the field to determine whether these tests have been completed recently. If not, then HMMM-V team has an agreement with Dallas VA Pathology and Laboratory Medicine Service for testing samples obtained in the field.
The program was designed for staffing of the vehicle by 2 professional teams, each includes medical (physician’s assistant or registered nurse), mental health (psychiatrist, residents), and social work providers (licensed social workers, clinical social workers); trainees of these disciplines; a peer support specialist; and an administrative clerk. The staffing varies daily, depending on available personnel. When personnel deploy to the field, they go in pairs or groups to address potential safety issues. Cell phones are available to summon police or ambulance services in an emergency. Systematic safety training was conducted with all field personnel before their first deployment to guard against vulnerability to danger in these settings.
Once in the field, personnel engage unsheltered homeless individuals to assess eligibility for VA services. Veterans found ineligible are assisted with application for military discharge upgrade, service-connected compensation, or appeal for health care coverage. Veterans eligible for VA care receive physical examinations, vital and glucose checks, influenza and pneumonia vaccinations, first-aid skin and wound care, medication management with limited medications provided at point of care, blood and urine testing, peer support services, suicide assessments, clinical mental health evaluations, and social work services through the HMMM-V program.
Social work assistance provided includes psychosocial assessment and care coordination for psychosocial needs such as mental health, substance abuse, vision, dental, housing, employment, legal aid, transportation, food, income, hygiene, and weather-appropriate provision needs.
Community Partnerships
The HMMM-V program benefitted from a number of partnerships with community agencies. During development of the program, HMMM-V personnel accompanied the Dallas Police Department’s Crisis Intervention Unit on typical homeless crisis services deployments into the field to learn about the locations and nature of encampments and homeless peregrination patterns in the Dallas area.
To aid in the design and selection of features for the mobile outreach vehicle, team members toured Homeless Outreach Medical Service mobile clinics from 2 local county hospitals, Parkland Hospital and John Peter Smith Hospital. The staff for these mobile clinics were interviewed about their experience with various components of their programs and their recommendations for optimal design of the mobile medical clinic for service delivery.
Numerous agencies in the Dallas area that serve the homeless population assisted with locating and connecting homeless veterans to HMMM-V programs. These partnering agencies also serve homeless individuals who do not qualify for the HMMM-V program, such as veterans with other-than-honorable military discharges.
The HMMM-V mobile outreach vehicle travels to partnering agencies and provides services on a recurring basis. These agencies are the Dallas International Street Church, a church and faith-based agency aiding the recovery of people with “broken lives”; Cornerstone Ministries, a church-based ministry serving people with adverse circumstances; and City Square’s Opportunity Center, human services and community development programs for low-income city residents. The mobile clinic also travels regularly to other areas to serve homeless veterans residing in unsheltered locations, such as homeless encampments and under bridges.
Clinical Assessment
The project used a modification of the VA Personalized Health Inventory (PHI) for general veteran populations, which assesses 8 areas of self-identified needs to address the specific concerns of homeless veterans served by a mobile clinic.25 Version 19 of the PHI (revised September 18, 2012), the version of the instrument available to the team at the inception of the project, was deployed with the HMMM-V personnel into the field. It imposed a heavy interview time burden (several hours), and its content areas did not seem appropriate to address the immediate concerns of homeless populations (eg, sections pertaining to personal development through hobbies, recreation, or volunteering; healthy living spaces with plenty of lighting and color; “eating healthy, balanced meals with plenty of fruits and vegetables each day”).25
Based on HMMM-V personnel feedback, the team modified this tool and developed a patient-centered health inventory (P-CHI) for homeless veterans that was acceptable in length and applicable to the situational characteristics of homeless existence. The tool’s 10 “current and desired states” were revised to remove domains of exercise and flexibility, sleep and relaxation, and mind-body techniques. The intervention and prevention domains were combined. A material needs (clothing, furniture, transportation, financial benefits) domain was added, and a new domain on reducing alcohol/drug use was created by moving this material from the food and drink domain.
The remaining domains were modified to fit the homeless living situation (Food and Drink = Nutrition; Personal Development = Employment/Vocation; Family, Friends, and Co-Workers = Family/Social/Legal Support; Spirit and Soul = Personal/Spiritual Fulfillment; Surroundings = Housing). Current state ratings were revised to reflect level of satisfaction, and ratings of Desired State were replaced with level of importance.
The modifications resulted in 9 domains, which were assembled into a grid for efficient rating of both satisfaction and importance for each domain (rated 1 to 10, lowest to highest, respectively), followed by an instruction to mark an X in a designated space in all the domains with which the individual would like help (Table). The intent was to reduce the burden of the instrument by having the participant complete sections providing detailed information about only the domains selected by the participant.
The details of each domain in the original VA PHI tool were captured through open-ended questions in text responses provided by the veteran. Because open-ended text responses are not conducive for summarizing characteristics of the population served or for evaluating program activities, the detailed sections covering the domains were revised completely to capture data within categoric and numeric variables. Items from the validated Homeless Supplement Interview were added to collect information not provided in the Homeless Operations Management and Evaluation System interview that is routinely administered to all veterans accessing homeless VA services.26-28
The information collected in these domains cover duration of current homeless episode, lifetime number of homeless episodes, current living arrangements and dissatisfactions with these arrangements, frequency and source of meals, employment history and current work status, sources of income, special material needs, medical and dental problems and sources of care, current medications, mental health problems and sources of care, urgent mental health concerns, current amount and frequency of alcohol and drug use, substance abuse treatment history, relationships with family and intimate partners, legal assistance needs, and self-identified needs for spiritual and personal fulfillment. This instrument is available on request to the authors.
Veterans Served
The project began with 1 team of professionals deploying with the HMMM-V vehicle while a second team was being assembled. Currently, the 2 HMMM-V teams deploy the mobile clinic 4 days per week. The mobile clinic visits agencies that serve the homeless, including emergency shelters and food ministries, as well as homeless encampments. To date, 195 homeless veterans have been served by the mobile clinic, 111 were currently enrolled with the VA, 8 were not enrolled but eligible for services, and 77 were not eligible for VA services. Of the unenrolled veterans, those eligible for services were offered VA enrollment assistance; those ineligible for VA services were offered a community referral.
For the veterans encountered in the field, the following interventions were provided: 49 housing placement referrals, 4 rental assistance referrals, 4 legal referrals, 27 medical care interventions, 13 dental referrals, 11 vision/hearing referrals, 12 mental health interventions, 9 substance abuse treatment referrals, 14 employment assistance referrals, 13 disability benefit applications, 18 transportation assists, 23 goods delivered, and 159 information assists. The HMMM-V mobile clinic also is deployed to participate in various educational and outreach events. At the time this article was written, the mobile clinic has reached nearly 2,000 veterans and community partners in at least 25 such events.
Of the veterans served to date, 73 completed the P-CHI. These veterans were predominantly male (77%), and the majority (60%) were black. The median age of the sample was 58 years, and typically they had a high school level of education (12.7; SD, 2.1 mean years of education). About half (49%) the sample were separated or divorced, and only a minority were currently married (8%). Half (50%) the sample served in the U.S. Army, with the post-Vietnam era being the era of service most represented (19%). Few (21%) veterans reported exposure to hostile or friendly fire during their service. More than three-fourths (80%) of the sample had experienced a homeless episode prior to their current one. On average, members of the sample had experienced a median of 3 lifetime homeless episodes. They had a mean 4.1 (SD, 5.8) lifetime number of years of homelessness, and 3.0 (SD, 5.2) years in their current homeless episode. Nearly one-third (31%) reported that they were currently staying in a homeless shelter, and nearly one-sixth (16%) were currently unsheltered in street settings, such as under bridges or in outdoor encampments at the time of the initial visit.
The mean number of minutes spent completing the P-CHI was 18.5 (SD, 9.4). The veterans indicated that they would like assistance with a mean 3.2 (SD, 2.2) number of domains. The domains with the highest average importance ratings were housing (mean, 9.4; SD, 1.7) and medical/dental care (mean, 8.9; SD, 2.2); the domains with the lowest average importance rating were reducing alcohol/drug use (mean, 6.4; SD, 4.1) and employment/vocation (mean, 6.3; SD, 4.2). The domains with the highest average satisfaction ratings were personal/spiritual fulfillment (mean, 7.3; SD, 2.9) and reducing substance use (mean, 5.9; SD, 4.0), and the domains with the lowest average satisfaction ratings were housing (mean, 2.9; SD, 2.9), material needs (mean, 4.2; SD, 3.3), and employment/vocation (mean, 4.2; SD, 3.2). The domain with the greatest indication of desire for help was housing, endorsed by more than four-fifths (84%) of the sample. This highly endorsed housing domain also was one of the lowest in satisfaction. The domains with the least expressed interest in obtaining help were reducing substance use (18%) and personal/spiritual fulfillment (15%).Reducing substance abuse also was one of the lowest domains of importance and the least for dissatisfaction.
Challenges and Barriers
As anticipated from its inception, this project encountered many challenges and barriers. The first was with the design, construction, and delivery of the mobile clinic unit. The vehicle took more than 2 years to be delivered. There were delays in progress necessitated by required selection of an approved vendor to build the vehicle, extensive specification of details and features, and stocking it with equipment and supplies. The weight of the unit had to be < 26,000 pounds to avoid the requirement of a commercial driver’s license, which limited the size of the vehicle to 28 feet. Stocking the unit with equipment and supplies required attention to a myriad of specifications and decisions. For example, separate refrigerators were needed for specimens, medications, and food; pharmaceutical regulations governing medications in mobile clinics required strict adherence; and difficulties were encountered in attempting to establish adequate and secure connectivity for communications devices in the field.
Once the mobile unit was delivered and prepared for deployment, the next set of challenges pertained to learning all of the instructions required to operate and drive the vehicle and learning how to maneuver the vehicle in the field. Specific challenges for driving the vehicle encountered included unexpectedly low overpasses that prohibited passage, narrow spaces for passage, rough and uneven terrain in off-road settings, and lateral and vertical tilt of roads creating potential for sideswipes and undercarriage scrapes. Maintenance schedules needed to be developed and implemented for cleaning the unit, inspection compliance, repairs, refueling, and emptying waste materials.
Staffing the vehicle required the development of unique job specifications addressing special expertise in accessing VA databases for veteran verification and registration and for driving the mobile clinic vehicle. Schedules and deployment plans for 2 teams that shared the same vehicle had to be established and followed. Locating veterans in unsheltered settings, such as under bridges and in encampments, required community intelligence facilitated through partnerships with knowledgeable members of the Dallas police crisis unit and by gaining field experience to locate where the usual homeless gathering places are, especially those inhabited by veterans. Safety of team members and equipment/supplies in the field was paramount from the start, and additional steps beyond safety training required extra measures, such as special care in navigating known dangerous areas. Provision of services necessitated completion of everything needed in a single visit due to the likelihood of loss to follow-up and acceptance of the limited types of service that could be provided in a mobile clinic. Special procedures were needed to provide referrals to sources of available care for non-VA-qualifying veterans.
Discussion
The HMMM-V program for delivery of PCC to homeless veterans is an innovative pilot program designed to connect with difficult-to-reach homeless veterans and engage them in care. The deliverables provided by this project are (1) A mobile outreach vehicle to deliver care to homeless veterans and outreach to other veterans and community agencies in North Texas; (2) The P-CHI assessment tool for homeless veterans modified and adapted for use with this special population; and (3) pilot data on its first cohort of homeless veterans served, describing their baseline characteristics and their stated satisfaction and preferences about their goals and aspirations for their physical, emotional, and mental health and well-being.
The HMMM-V program successfully identified homeless veterans in need of services, and more than one-third of these veterans were not previously engaged in VA services. Compared with the “typical” veterans served at VANTHCS homeless programs, veterans served by the HMMM-V comprised a greater proportion of minorities and a higher proportion who had been exposed to combat.29 Age and gender characteristics were similar.29 When compared with veterans who access care at VANTHCS and have not experienced homelessness, those served by the HMMM-V were younger and more likely to belong to a minority group; however, they were similar in combat exposure and gender.1 The veterans served by the HMMM-V program also were considerably older and had more homeless chronicity than did nonveteran homeless populations, consistent with other research.4,29,30
The veterans served by the HMMM-V program not surprisingly made housing their top priority in need of help, consistent with the Housing First model.22,31 They also indicated that employment/vocation and reducing substance use were of lower importance. Need for assistance with reducing substance use and social support were the domains least often identified as areas where help was needed, which seems inconsistent with the higher established rates of substance abuse problems among homeless veterans.1
With additional fieldwork, the HMMM-V program is expected to allow refinement of procedures for identifying and serving veterans from a patient-centered care perspective. The P-CHI will be further tested and developed, and the next step will be to create and pilot intervention templates for a Patient-Centered Health Improvement Plan, based on the P-CHI results. This process parallels the original development treatment plans for the VA’s Personalized Health Plan based on the PHI.25 Once the HMMM-V program is fully established in Dallas, the plans are for an expansion that will cover a broader geographic area in North Texas that includes rural areas.
The HMMM-V program was designed to address the barriers to health care that are encountered by homeless veterans. It is unique in homeless veteran care due to its patient-centered approach that partners with homeless veterans to prioritize their needs as determined by them rather than based solely on policies or provider conceptualizations of their needs. Access to services, engagement in care, and successful utilization of needed services may lead to measurable improvements in health care outcomes among homeless populations of veterans. Desired goals include remission of illness through appropriate medical intervention, preventing morbidity, achieving healthy lifestyles, recovery from addiction, stabilization of psychiatric illness, and attainment of stable housing.
The first hurdle for implementing this type of program in other settings is the identification of resources needed for these efforts. Need of additional staffing resources, however, may be circumvented by allowing employees working in other areas to rotate in community outreach shifts in the mobile unit. Another hurdle encountered in implementation of the HMMM-V initiative was the initial difficulty finding homeless veterans in community settings, especially those in unsheltered locations. The HMMM-V program addressed this issue by partnering with other agencies serving the homeless in the community. Therefore, a general recommendation for other entities seeking to implement this type of program is to reach out to these community partners from the outset.
Conclusion
The HMMM-V has the potential to engage the most difficult-to-reach homeless veterans in need of health services by delivering care and providing resources in challenging environments. Further work is needed to validate the P-CHI for use with this program and to conduct well-designed and implemented research to demonstrate effectiveness of this intervention on veteran outcomes, especially quality of life. Once this additional work is accomplished, this innovative program can potentially be implemented by VAMCs across the nation, and potentially in more general community care settings, to more effectively reach out and deliver services to homeless members of the community.
Acknowledgments
Grant support was received from the Department of Veterans Affairs, Office of Patient Centered Care. The authors would like to acknowledge all the clinicians, trainees, and support staff who have contributed to the success of the HMMM-V program: Tara Ayala, Jose Cabrera, Tony Castillo, Rachael Lynn David, Teresa DeShazo, Sylvia Figueroa, Steven Fisher, Eric Gary, Evelyn Gibbs, Kevin Hosey, JoAnn Joseph, Taly Drimer Kagan, Miranda Kelly, Michelle King-Thompson, Sharon Marcus, Shiji Mathew, Moneeza Matin, John Moreno, Joseph Neifert, Joel Price, Tiffany Price, Natalie Qualls, Reginald Robertson, Kristine Rodrigues, Jon Saffelder, Jill Stokes, Scott Stone, and John Smith.
1. LePage JP, Bradshaw LD, Cipher DJ, Crawford AM, Hooshyar D. The effects of homelessness on veterans’ health care service use: an evaluation of independence from comorbidities. Public Health. 2014;128(11):985-992.
2. Fischer PJ, Breakey WR. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol. 1991;46(11):1115-1128.
3. Robertson MJ, Zlotnick C, Westerfelt A. Drug use disorders and treatment contact among homeless adults in Alameda County, California. Am J Public Health. 1997;87(2):221-228.
4. North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? Am J Public Health. 2004;94(1):103-108.
5. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225.
6. Harpaz-Rotem I, Rosenheck RA, Desai R. The mental health of children exposed to maternal mental illness and homelessness. Community Ment Health J. 2006;42(5):437-448.
7. Pollio DE, Eyrich-Garg KM, North CS. The homeless. In: Johnson BA, ed. Addiction Medicine: Science and Practice. New York, NY: Springer; 2011:1487-1504.
8. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
9. Baggett TP, Singer DE, Rao SR, O’Connell JJ, Bharel M, Rigotti NA. Food insufficiency and health services utilization in a national sample of homeless adults. J Gen Intern Med. 2011;26(6):627-634.
10. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376.
11. Fuehrlein BS, Cowell AJ, Pollio D, Cupps L, Balfour ME, North CS. A prospective study of the associations among housing status and costs of services in a homeless population. Psychiatr Serv. 2015;66(1):27-32.
12. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
13. U.S. Department of Housing and Urban Development Office of Community Planning and Development. The 2016 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: point-in-time estimates of homelessness. https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Published 2016. Accessed August 7, 2017.
14. Tsai J, Rosenheck RA. Risk factors for homelessness among U.S. veterans. Epidemiol Rev. 2015;37:177-195.
15. Williamson V, Mulhall E. Coming home: the housing crisis and homelessness threaten new veterans. Iraq and Afghanistan Veterans of America, January, 2009. http://media.iava.org/IAVA_coming_home_2009%20The%20Housing%20Crisis%20and%20Homelessness%20Threaten%20New%20Veterans.pdf. Accessed August 10, 2017
16. Shinseki EK. Remarks by Secretary Eric K. Shinseki. National Summit on Homeless Veterans; November 3, 2009; Washington, DC. https://www.va.gov/opa/speeches/2009/09_1103.asp. Updated August 8, 2016. Accessed August 7, 2017.
17. Shinseki EK. Remarks by Secretary Eric K. Shinseki. 2014 National Coalition for Homeless Veterans Annual Meeting; May 30, 2014; Arlington, VA. https://www.va.gov/opa/speeches/2014/05_30_2014.asp. Updated April 21, 2015. Accessed August 7, 2017.
18. Pollio DE, Spitznagel EL, North CS, Thompson S, Foster DA. Service use over time and achievement of stable housing in a mentally ill homeless population. Psychiatr Serv. 2000;51(12):1536-1543.
19. Page J. Barriers to transferring care of homeless people with serious mental illnesses to community mental health organizations: perspectives of street-based programs. Best Practices in Mental Health: An International Journal. 2007;3(1):26.
20. Young AS, Chinman MJ, Cradock-O’Leary JA, et al. Characteristics of individuals with severe mental illness who use emergency services. Community Ment Health J. 2005;41(2):159-168.
21. Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461.
22. Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651-656.
23. U.S. Department of Veterans Affairs, Veterans Health Administration. VA Patient Centered Care. http://www.va.gov/patientcenteredcare. Updated July 24,2017. Accessed August 7, 2017.
24. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
25. U.S. Department of Veterans Affairs, Office of Patient Centered Care and Cultural Transformation. My story: personal health inventory. https://www.va.gov/PATIENTCENTEREDCARE/docs/VA-OPCC-Personal-Health-Inventory-final-508.pdf. Published October 7, 2013. Accessed August 7, 2017
26. North CS, Smith EM, Pollio DE. The Homeless Supplement to the Diagnostic Interview Schedule (DIS/HS). St. Louis: Washington University, 2004.
27. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The homeless supplement to the diagnostic interview schedule: test-retest analyses. Int J Methods Psychiatr Res. 2004;13(3):184-191.
28. LaSalle JL. Homeless Operations Management and Evaluation System (HOMES) user manual-phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed August 7, 2017.
29. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psychiatr Serv. 2014;65(6):751-757.
30. North CS, Smith EM. A comparison of homeless men and women: different populations, different needs. Community Ment Health J. 1993;29(5):423-431.
31. Kertesz SG, Austin EL, Holmes SK, et al. Making housing first happen: organizational leadership in VA’s expansion of permanent supportive housing. J Gen Intern Med. 2014;29(suppl 4):835-844.
Research has consistently identified remarkably high rates of addiction, mental illness, and health problems in the homeless population.1-9 Yet in spite of extensive service needs for these problems, abundant evidence exists of consistent underuse of health care services by homeless populations.10-12 Most of the homeless population reside in emergency shelters or in transitional or supportive housing, but many remain in places not meant for human habitation.
Homelessness is significantly overrepresented among military veterans.13 The January 2016 national point-in-time count identified 39,471 veterans experiencing homelessness.13 Iraq and Afghanistan veterans seem to have an especially high risk for homelessness.13-15 Disheartening statistics such as these prompted former VA Secretary Eric Shinseki to pledge to end veteran homelessness by December 2015.16 He argued in support of this mission that 85% of veteran homeless resources go to health care—implying that homelessness among veterans is primarily a health care issue, which is heavily burdened by substance abuse and other psychiatric and medical illnesses.17
Health care service use has been associated with improved health, mental health, and outcomes among homeless populations.12,18 Unfortunately, access to these services is limited by barriers associated with homelessness, such as transportation or lack of proper identification.19,20 Veterans experiencing homelessness also face these common barriers to health care, and unsheltered veterans especially underutilize VA health care services.21
Housing First—a successful model that places individuals into housing without prerequisites for sobriety, active participation in treatment, or other behavioral accomplishments, such as gainful employment—has not managed yet to place all the disengaged homeless veteran population into stable housing.22 However, the Housing First model, which is based on the individual’s priorities, is consistent with the approach of a new program at the VA North Texas Health Care System (VANTHCS).
The VHA, similar to other health care systems, is engaged in a cultural transformation to convert its health care approach from a traditional medical model to patient-centered care (PCC).23 In this priority area, a strategic objective is for the VHA to partner with each veteran to create a personalized, proactive strategy to optimize health and well-being and when needed provide state-of-the-art disease management. Patient-centered care is designed to address veterans’ specific needs in spiritual, environmental, physical, mental, and social domains and empower veterans to become active participants in their care. Patient-centered care differs from the traditional medical model in that patients are active participants in their treatment, partnering and collaborating with their providers on care that is quality-of-life centered instead of disease centered.23 This model is based on both respect for patients as unique individuals and on the obligation to care for them on their own terms, focused on their self-identified goals and aspirations.24
At VANTHCS, the Homeless Mobile Medical/Mental Veteran (HMMM-V) pilot program was designed to deliver effective health care services to a homeless subpopulation of veterans who historically have been the most difficult to serve—those living in unsheltered environments, such as under bridges and in encampments. The purpose of the HMMM-V program was to contact and serve veterans not currently being reached by the VA system of care, using a PCC model.
This pilot program was initially funded in January 2013 by a 2-year grant from the Office of Patient Centered Care and Cultural Transformation to apply the PCC approach to engage veteran participation. For this project, the VA Personal Health Inventory tool—originally designed for use with the general veteran population—was adapted for use with the homeless veteran population. The grant funding period covered the design, development, and implementation of the HMMM-V program; thereafter, VANTHCS provided resources through its Comprehensive Homeless Center Programs to assure its sustainability and continued use of the clinical assessment tool created for this project.
This article describes the development and implementation of this novel program with sufficient detail to inform the development of similar programs in other sites. Descriptions of the program and staffing, creation of community partnerships, and modification of an assessment instrument are provided. It also illustrates the original implementation period of the HMMM-V program through presentation of self-reported data on the first homeless veterans it served.
Equipment and Staffing
A custom 28-foot mobile outreach vehicle was assembled according to specifications identified by the HMMM-V team as necessary to conduct the program’s interventions. The van became fully operational on April 8, 2015, after it underwent all the required reviews and inspections (eg, safety, infection control, etc) and was accredited in 2015 by the Commission on Accreditation of Rehabilitation Facilities.
The HMMM-V van has a driver compartment that is separate from its services rooms, which include a patient registration area, a fully equipped examination room, a laboratory area, and a bathroom. The vehicle is equipped with a wheelchair lift and an awning to shade outdoor areas where tables and chairs are set up for patient/staff waiting and rest areas. The vehicle is stocked with essential equipment and supplies needed to conduct work in off-street locations, vacant lots, under bridges, fields, unpaved paths, etc. It also is equipped with telemedicine capabilities to provide clinical supervision and access to attending physicians and specialists at VANTHCS. Personnel carry cell phones and laptop computers with secure Internet connections using a commercially available mobile wireless Wi-Fi hotspot to facilitate documentation of medical records and communication from the field.
This reliable type of equipment is routine for use in VA field operations; the only hurdle using these technologies for the program was acquiring funding and purchasing the equipment. The vehicle is further equipped with a refrigerator solely for secure storage of pharmaceutical supplies, a second refrigerator for specimens, and wall-mounted blood pressure and otoscope/ophthalmoscope units. The vehicle is supplied with thermometers, scales, phlebotomy supplies, and first-aid kits and is stocked with vaccines and medications, including antibiotic, hypertensive, diabetic, allergy, and over-the-counter pain medications. A more comprehensive list of supplies for the vehicle is available from the authors on request.
Medication provisions supplied to the HMMM-V mobile clinic conform to the Texas State Board of Pharmacy compliance regulations. Because the vehicle is designated as federal property and has U.S. government license plates, it is considered an extension of VANTHCS Pharmacy Service and falls under its pharmacy license. A medication formulary was created with input from HMMM-V prescribers and Dallas VAMC Pharmacy Service pharmacists. To safeguard the integrity of these pharmaceutical agents, the HMMM-V physician assistant picks up the medications before field deployment and returns the unused medications to the Dallas VAMC at the end of the day. The medications are transported in locked containers and placed either in a locked medication refrigerator or cabinet on the mobile unit.
For medication prescriptions that need laboratory testing before prescribing them, HMMM-V prescribers can check the VA electronic medical record from the field to determine whether these tests have been completed recently. If not, then HMMM-V team has an agreement with Dallas VA Pathology and Laboratory Medicine Service for testing samples obtained in the field.
The program was designed for staffing of the vehicle by 2 professional teams, each includes medical (physician’s assistant or registered nurse), mental health (psychiatrist, residents), and social work providers (licensed social workers, clinical social workers); trainees of these disciplines; a peer support specialist; and an administrative clerk. The staffing varies daily, depending on available personnel. When personnel deploy to the field, they go in pairs or groups to address potential safety issues. Cell phones are available to summon police or ambulance services in an emergency. Systematic safety training was conducted with all field personnel before their first deployment to guard against vulnerability to danger in these settings.
Once in the field, personnel engage unsheltered homeless individuals to assess eligibility for VA services. Veterans found ineligible are assisted with application for military discharge upgrade, service-connected compensation, or appeal for health care coverage. Veterans eligible for VA care receive physical examinations, vital and glucose checks, influenza and pneumonia vaccinations, first-aid skin and wound care, medication management with limited medications provided at point of care, blood and urine testing, peer support services, suicide assessments, clinical mental health evaluations, and social work services through the HMMM-V program.
Social work assistance provided includes psychosocial assessment and care coordination for psychosocial needs such as mental health, substance abuse, vision, dental, housing, employment, legal aid, transportation, food, income, hygiene, and weather-appropriate provision needs.
Community Partnerships
The HMMM-V program benefitted from a number of partnerships with community agencies. During development of the program, HMMM-V personnel accompanied the Dallas Police Department’s Crisis Intervention Unit on typical homeless crisis services deployments into the field to learn about the locations and nature of encampments and homeless peregrination patterns in the Dallas area.
To aid in the design and selection of features for the mobile outreach vehicle, team members toured Homeless Outreach Medical Service mobile clinics from 2 local county hospitals, Parkland Hospital and John Peter Smith Hospital. The staff for these mobile clinics were interviewed about their experience with various components of their programs and their recommendations for optimal design of the mobile medical clinic for service delivery.
Numerous agencies in the Dallas area that serve the homeless population assisted with locating and connecting homeless veterans to HMMM-V programs. These partnering agencies also serve homeless individuals who do not qualify for the HMMM-V program, such as veterans with other-than-honorable military discharges.
The HMMM-V mobile outreach vehicle travels to partnering agencies and provides services on a recurring basis. These agencies are the Dallas International Street Church, a church and faith-based agency aiding the recovery of people with “broken lives”; Cornerstone Ministries, a church-based ministry serving people with adverse circumstances; and City Square’s Opportunity Center, human services and community development programs for low-income city residents. The mobile clinic also travels regularly to other areas to serve homeless veterans residing in unsheltered locations, such as homeless encampments and under bridges.
Clinical Assessment
The project used a modification of the VA Personalized Health Inventory (PHI) for general veteran populations, which assesses 8 areas of self-identified needs to address the specific concerns of homeless veterans served by a mobile clinic.25 Version 19 of the PHI (revised September 18, 2012), the version of the instrument available to the team at the inception of the project, was deployed with the HMMM-V personnel into the field. It imposed a heavy interview time burden (several hours), and its content areas did not seem appropriate to address the immediate concerns of homeless populations (eg, sections pertaining to personal development through hobbies, recreation, or volunteering; healthy living spaces with plenty of lighting and color; “eating healthy, balanced meals with plenty of fruits and vegetables each day”).25
Based on HMMM-V personnel feedback, the team modified this tool and developed a patient-centered health inventory (P-CHI) for homeless veterans that was acceptable in length and applicable to the situational characteristics of homeless existence. The tool’s 10 “current and desired states” were revised to remove domains of exercise and flexibility, sleep and relaxation, and mind-body techniques. The intervention and prevention domains were combined. A material needs (clothing, furniture, transportation, financial benefits) domain was added, and a new domain on reducing alcohol/drug use was created by moving this material from the food and drink domain.
The remaining domains were modified to fit the homeless living situation (Food and Drink = Nutrition; Personal Development = Employment/Vocation; Family, Friends, and Co-Workers = Family/Social/Legal Support; Spirit and Soul = Personal/Spiritual Fulfillment; Surroundings = Housing). Current state ratings were revised to reflect level of satisfaction, and ratings of Desired State were replaced with level of importance.
The modifications resulted in 9 domains, which were assembled into a grid for efficient rating of both satisfaction and importance for each domain (rated 1 to 10, lowest to highest, respectively), followed by an instruction to mark an X in a designated space in all the domains with which the individual would like help (Table). The intent was to reduce the burden of the instrument by having the participant complete sections providing detailed information about only the domains selected by the participant.
The details of each domain in the original VA PHI tool were captured through open-ended questions in text responses provided by the veteran. Because open-ended text responses are not conducive for summarizing characteristics of the population served or for evaluating program activities, the detailed sections covering the domains were revised completely to capture data within categoric and numeric variables. Items from the validated Homeless Supplement Interview were added to collect information not provided in the Homeless Operations Management and Evaluation System interview that is routinely administered to all veterans accessing homeless VA services.26-28
The information collected in these domains cover duration of current homeless episode, lifetime number of homeless episodes, current living arrangements and dissatisfactions with these arrangements, frequency and source of meals, employment history and current work status, sources of income, special material needs, medical and dental problems and sources of care, current medications, mental health problems and sources of care, urgent mental health concerns, current amount and frequency of alcohol and drug use, substance abuse treatment history, relationships with family and intimate partners, legal assistance needs, and self-identified needs for spiritual and personal fulfillment. This instrument is available on request to the authors.
Veterans Served
The project began with 1 team of professionals deploying with the HMMM-V vehicle while a second team was being assembled. Currently, the 2 HMMM-V teams deploy the mobile clinic 4 days per week. The mobile clinic visits agencies that serve the homeless, including emergency shelters and food ministries, as well as homeless encampments. To date, 195 homeless veterans have been served by the mobile clinic, 111 were currently enrolled with the VA, 8 were not enrolled but eligible for services, and 77 were not eligible for VA services. Of the unenrolled veterans, those eligible for services were offered VA enrollment assistance; those ineligible for VA services were offered a community referral.
For the veterans encountered in the field, the following interventions were provided: 49 housing placement referrals, 4 rental assistance referrals, 4 legal referrals, 27 medical care interventions, 13 dental referrals, 11 vision/hearing referrals, 12 mental health interventions, 9 substance abuse treatment referrals, 14 employment assistance referrals, 13 disability benefit applications, 18 transportation assists, 23 goods delivered, and 159 information assists. The HMMM-V mobile clinic also is deployed to participate in various educational and outreach events. At the time this article was written, the mobile clinic has reached nearly 2,000 veterans and community partners in at least 25 such events.
Of the veterans served to date, 73 completed the P-CHI. These veterans were predominantly male (77%), and the majority (60%) were black. The median age of the sample was 58 years, and typically they had a high school level of education (12.7; SD, 2.1 mean years of education). About half (49%) the sample were separated or divorced, and only a minority were currently married (8%). Half (50%) the sample served in the U.S. Army, with the post-Vietnam era being the era of service most represented (19%). Few (21%) veterans reported exposure to hostile or friendly fire during their service. More than three-fourths (80%) of the sample had experienced a homeless episode prior to their current one. On average, members of the sample had experienced a median of 3 lifetime homeless episodes. They had a mean 4.1 (SD, 5.8) lifetime number of years of homelessness, and 3.0 (SD, 5.2) years in their current homeless episode. Nearly one-third (31%) reported that they were currently staying in a homeless shelter, and nearly one-sixth (16%) were currently unsheltered in street settings, such as under bridges or in outdoor encampments at the time of the initial visit.
The mean number of minutes spent completing the P-CHI was 18.5 (SD, 9.4). The veterans indicated that they would like assistance with a mean 3.2 (SD, 2.2) number of domains. The domains with the highest average importance ratings were housing (mean, 9.4; SD, 1.7) and medical/dental care (mean, 8.9; SD, 2.2); the domains with the lowest average importance rating were reducing alcohol/drug use (mean, 6.4; SD, 4.1) and employment/vocation (mean, 6.3; SD, 4.2). The domains with the highest average satisfaction ratings were personal/spiritual fulfillment (mean, 7.3; SD, 2.9) and reducing substance use (mean, 5.9; SD, 4.0), and the domains with the lowest average satisfaction ratings were housing (mean, 2.9; SD, 2.9), material needs (mean, 4.2; SD, 3.3), and employment/vocation (mean, 4.2; SD, 3.2). The domain with the greatest indication of desire for help was housing, endorsed by more than four-fifths (84%) of the sample. This highly endorsed housing domain also was one of the lowest in satisfaction. The domains with the least expressed interest in obtaining help were reducing substance use (18%) and personal/spiritual fulfillment (15%).Reducing substance abuse also was one of the lowest domains of importance and the least for dissatisfaction.
Challenges and Barriers
As anticipated from its inception, this project encountered many challenges and barriers. The first was with the design, construction, and delivery of the mobile clinic unit. The vehicle took more than 2 years to be delivered. There were delays in progress necessitated by required selection of an approved vendor to build the vehicle, extensive specification of details and features, and stocking it with equipment and supplies. The weight of the unit had to be < 26,000 pounds to avoid the requirement of a commercial driver’s license, which limited the size of the vehicle to 28 feet. Stocking the unit with equipment and supplies required attention to a myriad of specifications and decisions. For example, separate refrigerators were needed for specimens, medications, and food; pharmaceutical regulations governing medications in mobile clinics required strict adherence; and difficulties were encountered in attempting to establish adequate and secure connectivity for communications devices in the field.
Once the mobile unit was delivered and prepared for deployment, the next set of challenges pertained to learning all of the instructions required to operate and drive the vehicle and learning how to maneuver the vehicle in the field. Specific challenges for driving the vehicle encountered included unexpectedly low overpasses that prohibited passage, narrow spaces for passage, rough and uneven terrain in off-road settings, and lateral and vertical tilt of roads creating potential for sideswipes and undercarriage scrapes. Maintenance schedules needed to be developed and implemented for cleaning the unit, inspection compliance, repairs, refueling, and emptying waste materials.
Staffing the vehicle required the development of unique job specifications addressing special expertise in accessing VA databases for veteran verification and registration and for driving the mobile clinic vehicle. Schedules and deployment plans for 2 teams that shared the same vehicle had to be established and followed. Locating veterans in unsheltered settings, such as under bridges and in encampments, required community intelligence facilitated through partnerships with knowledgeable members of the Dallas police crisis unit and by gaining field experience to locate where the usual homeless gathering places are, especially those inhabited by veterans. Safety of team members and equipment/supplies in the field was paramount from the start, and additional steps beyond safety training required extra measures, such as special care in navigating known dangerous areas. Provision of services necessitated completion of everything needed in a single visit due to the likelihood of loss to follow-up and acceptance of the limited types of service that could be provided in a mobile clinic. Special procedures were needed to provide referrals to sources of available care for non-VA-qualifying veterans.
Discussion
The HMMM-V program for delivery of PCC to homeless veterans is an innovative pilot program designed to connect with difficult-to-reach homeless veterans and engage them in care. The deliverables provided by this project are (1) A mobile outreach vehicle to deliver care to homeless veterans and outreach to other veterans and community agencies in North Texas; (2) The P-CHI assessment tool for homeless veterans modified and adapted for use with this special population; and (3) pilot data on its first cohort of homeless veterans served, describing their baseline characteristics and their stated satisfaction and preferences about their goals and aspirations for their physical, emotional, and mental health and well-being.
The HMMM-V program successfully identified homeless veterans in need of services, and more than one-third of these veterans were not previously engaged in VA services. Compared with the “typical” veterans served at VANTHCS homeless programs, veterans served by the HMMM-V comprised a greater proportion of minorities and a higher proportion who had been exposed to combat.29 Age and gender characteristics were similar.29 When compared with veterans who access care at VANTHCS and have not experienced homelessness, those served by the HMMM-V were younger and more likely to belong to a minority group; however, they were similar in combat exposure and gender.1 The veterans served by the HMMM-V program also were considerably older and had more homeless chronicity than did nonveteran homeless populations, consistent with other research.4,29,30
The veterans served by the HMMM-V program not surprisingly made housing their top priority in need of help, consistent with the Housing First model.22,31 They also indicated that employment/vocation and reducing substance use were of lower importance. Need for assistance with reducing substance use and social support were the domains least often identified as areas where help was needed, which seems inconsistent with the higher established rates of substance abuse problems among homeless veterans.1
With additional fieldwork, the HMMM-V program is expected to allow refinement of procedures for identifying and serving veterans from a patient-centered care perspective. The P-CHI will be further tested and developed, and the next step will be to create and pilot intervention templates for a Patient-Centered Health Improvement Plan, based on the P-CHI results. This process parallels the original development treatment plans for the VA’s Personalized Health Plan based on the PHI.25 Once the HMMM-V program is fully established in Dallas, the plans are for an expansion that will cover a broader geographic area in North Texas that includes rural areas.
The HMMM-V program was designed to address the barriers to health care that are encountered by homeless veterans. It is unique in homeless veteran care due to its patient-centered approach that partners with homeless veterans to prioritize their needs as determined by them rather than based solely on policies or provider conceptualizations of their needs. Access to services, engagement in care, and successful utilization of needed services may lead to measurable improvements in health care outcomes among homeless populations of veterans. Desired goals include remission of illness through appropriate medical intervention, preventing morbidity, achieving healthy lifestyles, recovery from addiction, stabilization of psychiatric illness, and attainment of stable housing.
The first hurdle for implementing this type of program in other settings is the identification of resources needed for these efforts. Need of additional staffing resources, however, may be circumvented by allowing employees working in other areas to rotate in community outreach shifts in the mobile unit. Another hurdle encountered in implementation of the HMMM-V initiative was the initial difficulty finding homeless veterans in community settings, especially those in unsheltered locations. The HMMM-V program addressed this issue by partnering with other agencies serving the homeless in the community. Therefore, a general recommendation for other entities seeking to implement this type of program is to reach out to these community partners from the outset.
Conclusion
The HMMM-V has the potential to engage the most difficult-to-reach homeless veterans in need of health services by delivering care and providing resources in challenging environments. Further work is needed to validate the P-CHI for use with this program and to conduct well-designed and implemented research to demonstrate effectiveness of this intervention on veteran outcomes, especially quality of life. Once this additional work is accomplished, this innovative program can potentially be implemented by VAMCs across the nation, and potentially in more general community care settings, to more effectively reach out and deliver services to homeless members of the community.
Acknowledgments
Grant support was received from the Department of Veterans Affairs, Office of Patient Centered Care. The authors would like to acknowledge all the clinicians, trainees, and support staff who have contributed to the success of the HMMM-V program: Tara Ayala, Jose Cabrera, Tony Castillo, Rachael Lynn David, Teresa DeShazo, Sylvia Figueroa, Steven Fisher, Eric Gary, Evelyn Gibbs, Kevin Hosey, JoAnn Joseph, Taly Drimer Kagan, Miranda Kelly, Michelle King-Thompson, Sharon Marcus, Shiji Mathew, Moneeza Matin, John Moreno, Joseph Neifert, Joel Price, Tiffany Price, Natalie Qualls, Reginald Robertson, Kristine Rodrigues, Jon Saffelder, Jill Stokes, Scott Stone, and John Smith.
Research has consistently identified remarkably high rates of addiction, mental illness, and health problems in the homeless population.1-9 Yet in spite of extensive service needs for these problems, abundant evidence exists of consistent underuse of health care services by homeless populations.10-12 Most of the homeless population reside in emergency shelters or in transitional or supportive housing, but many remain in places not meant for human habitation.
Homelessness is significantly overrepresented among military veterans.13 The January 2016 national point-in-time count identified 39,471 veterans experiencing homelessness.13 Iraq and Afghanistan veterans seem to have an especially high risk for homelessness.13-15 Disheartening statistics such as these prompted former VA Secretary Eric Shinseki to pledge to end veteran homelessness by December 2015.16 He argued in support of this mission that 85% of veteran homeless resources go to health care—implying that homelessness among veterans is primarily a health care issue, which is heavily burdened by substance abuse and other psychiatric and medical illnesses.17
Health care service use has been associated with improved health, mental health, and outcomes among homeless populations.12,18 Unfortunately, access to these services is limited by barriers associated with homelessness, such as transportation or lack of proper identification.19,20 Veterans experiencing homelessness also face these common barriers to health care, and unsheltered veterans especially underutilize VA health care services.21
Housing First—a successful model that places individuals into housing without prerequisites for sobriety, active participation in treatment, or other behavioral accomplishments, such as gainful employment—has not managed yet to place all the disengaged homeless veteran population into stable housing.22 However, the Housing First model, which is based on the individual’s priorities, is consistent with the approach of a new program at the VA North Texas Health Care System (VANTHCS).
The VHA, similar to other health care systems, is engaged in a cultural transformation to convert its health care approach from a traditional medical model to patient-centered care (PCC).23 In this priority area, a strategic objective is for the VHA to partner with each veteran to create a personalized, proactive strategy to optimize health and well-being and when needed provide state-of-the-art disease management. Patient-centered care is designed to address veterans’ specific needs in spiritual, environmental, physical, mental, and social domains and empower veterans to become active participants in their care. Patient-centered care differs from the traditional medical model in that patients are active participants in their treatment, partnering and collaborating with their providers on care that is quality-of-life centered instead of disease centered.23 This model is based on both respect for patients as unique individuals and on the obligation to care for them on their own terms, focused on their self-identified goals and aspirations.24
At VANTHCS, the Homeless Mobile Medical/Mental Veteran (HMMM-V) pilot program was designed to deliver effective health care services to a homeless subpopulation of veterans who historically have been the most difficult to serve—those living in unsheltered environments, such as under bridges and in encampments. The purpose of the HMMM-V program was to contact and serve veterans not currently being reached by the VA system of care, using a PCC model.
This pilot program was initially funded in January 2013 by a 2-year grant from the Office of Patient Centered Care and Cultural Transformation to apply the PCC approach to engage veteran participation. For this project, the VA Personal Health Inventory tool—originally designed for use with the general veteran population—was adapted for use with the homeless veteran population. The grant funding period covered the design, development, and implementation of the HMMM-V program; thereafter, VANTHCS provided resources through its Comprehensive Homeless Center Programs to assure its sustainability and continued use of the clinical assessment tool created for this project.
This article describes the development and implementation of this novel program with sufficient detail to inform the development of similar programs in other sites. Descriptions of the program and staffing, creation of community partnerships, and modification of an assessment instrument are provided. It also illustrates the original implementation period of the HMMM-V program through presentation of self-reported data on the first homeless veterans it served.
Equipment and Staffing
A custom 28-foot mobile outreach vehicle was assembled according to specifications identified by the HMMM-V team as necessary to conduct the program’s interventions. The van became fully operational on April 8, 2015, after it underwent all the required reviews and inspections (eg, safety, infection control, etc) and was accredited in 2015 by the Commission on Accreditation of Rehabilitation Facilities.
The HMMM-V van has a driver compartment that is separate from its services rooms, which include a patient registration area, a fully equipped examination room, a laboratory area, and a bathroom. The vehicle is equipped with a wheelchair lift and an awning to shade outdoor areas where tables and chairs are set up for patient/staff waiting and rest areas. The vehicle is stocked with essential equipment and supplies needed to conduct work in off-street locations, vacant lots, under bridges, fields, unpaved paths, etc. It also is equipped with telemedicine capabilities to provide clinical supervision and access to attending physicians and specialists at VANTHCS. Personnel carry cell phones and laptop computers with secure Internet connections using a commercially available mobile wireless Wi-Fi hotspot to facilitate documentation of medical records and communication from the field.
This reliable type of equipment is routine for use in VA field operations; the only hurdle using these technologies for the program was acquiring funding and purchasing the equipment. The vehicle is further equipped with a refrigerator solely for secure storage of pharmaceutical supplies, a second refrigerator for specimens, and wall-mounted blood pressure and otoscope/ophthalmoscope units. The vehicle is supplied with thermometers, scales, phlebotomy supplies, and first-aid kits and is stocked with vaccines and medications, including antibiotic, hypertensive, diabetic, allergy, and over-the-counter pain medications. A more comprehensive list of supplies for the vehicle is available from the authors on request.
Medication provisions supplied to the HMMM-V mobile clinic conform to the Texas State Board of Pharmacy compliance regulations. Because the vehicle is designated as federal property and has U.S. government license plates, it is considered an extension of VANTHCS Pharmacy Service and falls under its pharmacy license. A medication formulary was created with input from HMMM-V prescribers and Dallas VAMC Pharmacy Service pharmacists. To safeguard the integrity of these pharmaceutical agents, the HMMM-V physician assistant picks up the medications before field deployment and returns the unused medications to the Dallas VAMC at the end of the day. The medications are transported in locked containers and placed either in a locked medication refrigerator or cabinet on the mobile unit.
For medication prescriptions that need laboratory testing before prescribing them, HMMM-V prescribers can check the VA electronic medical record from the field to determine whether these tests have been completed recently. If not, then HMMM-V team has an agreement with Dallas VA Pathology and Laboratory Medicine Service for testing samples obtained in the field.
The program was designed for staffing of the vehicle by 2 professional teams, each includes medical (physician’s assistant or registered nurse), mental health (psychiatrist, residents), and social work providers (licensed social workers, clinical social workers); trainees of these disciplines; a peer support specialist; and an administrative clerk. The staffing varies daily, depending on available personnel. When personnel deploy to the field, they go in pairs or groups to address potential safety issues. Cell phones are available to summon police or ambulance services in an emergency. Systematic safety training was conducted with all field personnel before their first deployment to guard against vulnerability to danger in these settings.
Once in the field, personnel engage unsheltered homeless individuals to assess eligibility for VA services. Veterans found ineligible are assisted with application for military discharge upgrade, service-connected compensation, or appeal for health care coverage. Veterans eligible for VA care receive physical examinations, vital and glucose checks, influenza and pneumonia vaccinations, first-aid skin and wound care, medication management with limited medications provided at point of care, blood and urine testing, peer support services, suicide assessments, clinical mental health evaluations, and social work services through the HMMM-V program.
Social work assistance provided includes psychosocial assessment and care coordination for psychosocial needs such as mental health, substance abuse, vision, dental, housing, employment, legal aid, transportation, food, income, hygiene, and weather-appropriate provision needs.
Community Partnerships
The HMMM-V program benefitted from a number of partnerships with community agencies. During development of the program, HMMM-V personnel accompanied the Dallas Police Department’s Crisis Intervention Unit on typical homeless crisis services deployments into the field to learn about the locations and nature of encampments and homeless peregrination patterns in the Dallas area.
To aid in the design and selection of features for the mobile outreach vehicle, team members toured Homeless Outreach Medical Service mobile clinics from 2 local county hospitals, Parkland Hospital and John Peter Smith Hospital. The staff for these mobile clinics were interviewed about their experience with various components of their programs and their recommendations for optimal design of the mobile medical clinic for service delivery.
Numerous agencies in the Dallas area that serve the homeless population assisted with locating and connecting homeless veterans to HMMM-V programs. These partnering agencies also serve homeless individuals who do not qualify for the HMMM-V program, such as veterans with other-than-honorable military discharges.
The HMMM-V mobile outreach vehicle travels to partnering agencies and provides services on a recurring basis. These agencies are the Dallas International Street Church, a church and faith-based agency aiding the recovery of people with “broken lives”; Cornerstone Ministries, a church-based ministry serving people with adverse circumstances; and City Square’s Opportunity Center, human services and community development programs for low-income city residents. The mobile clinic also travels regularly to other areas to serve homeless veterans residing in unsheltered locations, such as homeless encampments and under bridges.
Clinical Assessment
The project used a modification of the VA Personalized Health Inventory (PHI) for general veteran populations, which assesses 8 areas of self-identified needs to address the specific concerns of homeless veterans served by a mobile clinic.25 Version 19 of the PHI (revised September 18, 2012), the version of the instrument available to the team at the inception of the project, was deployed with the HMMM-V personnel into the field. It imposed a heavy interview time burden (several hours), and its content areas did not seem appropriate to address the immediate concerns of homeless populations (eg, sections pertaining to personal development through hobbies, recreation, or volunteering; healthy living spaces with plenty of lighting and color; “eating healthy, balanced meals with plenty of fruits and vegetables each day”).25
Based on HMMM-V personnel feedback, the team modified this tool and developed a patient-centered health inventory (P-CHI) for homeless veterans that was acceptable in length and applicable to the situational characteristics of homeless existence. The tool’s 10 “current and desired states” were revised to remove domains of exercise and flexibility, sleep and relaxation, and mind-body techniques. The intervention and prevention domains were combined. A material needs (clothing, furniture, transportation, financial benefits) domain was added, and a new domain on reducing alcohol/drug use was created by moving this material from the food and drink domain.
The remaining domains were modified to fit the homeless living situation (Food and Drink = Nutrition; Personal Development = Employment/Vocation; Family, Friends, and Co-Workers = Family/Social/Legal Support; Spirit and Soul = Personal/Spiritual Fulfillment; Surroundings = Housing). Current state ratings were revised to reflect level of satisfaction, and ratings of Desired State were replaced with level of importance.
The modifications resulted in 9 domains, which were assembled into a grid for efficient rating of both satisfaction and importance for each domain (rated 1 to 10, lowest to highest, respectively), followed by an instruction to mark an X in a designated space in all the domains with which the individual would like help (Table). The intent was to reduce the burden of the instrument by having the participant complete sections providing detailed information about only the domains selected by the participant.
The details of each domain in the original VA PHI tool were captured through open-ended questions in text responses provided by the veteran. Because open-ended text responses are not conducive for summarizing characteristics of the population served or for evaluating program activities, the detailed sections covering the domains were revised completely to capture data within categoric and numeric variables. Items from the validated Homeless Supplement Interview were added to collect information not provided in the Homeless Operations Management and Evaluation System interview that is routinely administered to all veterans accessing homeless VA services.26-28
The information collected in these domains cover duration of current homeless episode, lifetime number of homeless episodes, current living arrangements and dissatisfactions with these arrangements, frequency and source of meals, employment history and current work status, sources of income, special material needs, medical and dental problems and sources of care, current medications, mental health problems and sources of care, urgent mental health concerns, current amount and frequency of alcohol and drug use, substance abuse treatment history, relationships with family and intimate partners, legal assistance needs, and self-identified needs for spiritual and personal fulfillment. This instrument is available on request to the authors.
Veterans Served
The project began with 1 team of professionals deploying with the HMMM-V vehicle while a second team was being assembled. Currently, the 2 HMMM-V teams deploy the mobile clinic 4 days per week. The mobile clinic visits agencies that serve the homeless, including emergency shelters and food ministries, as well as homeless encampments. To date, 195 homeless veterans have been served by the mobile clinic, 111 were currently enrolled with the VA, 8 were not enrolled but eligible for services, and 77 were not eligible for VA services. Of the unenrolled veterans, those eligible for services were offered VA enrollment assistance; those ineligible for VA services were offered a community referral.
For the veterans encountered in the field, the following interventions were provided: 49 housing placement referrals, 4 rental assistance referrals, 4 legal referrals, 27 medical care interventions, 13 dental referrals, 11 vision/hearing referrals, 12 mental health interventions, 9 substance abuse treatment referrals, 14 employment assistance referrals, 13 disability benefit applications, 18 transportation assists, 23 goods delivered, and 159 information assists. The HMMM-V mobile clinic also is deployed to participate in various educational and outreach events. At the time this article was written, the mobile clinic has reached nearly 2,000 veterans and community partners in at least 25 such events.
Of the veterans served to date, 73 completed the P-CHI. These veterans were predominantly male (77%), and the majority (60%) were black. The median age of the sample was 58 years, and typically they had a high school level of education (12.7; SD, 2.1 mean years of education). About half (49%) the sample were separated or divorced, and only a minority were currently married (8%). Half (50%) the sample served in the U.S. Army, with the post-Vietnam era being the era of service most represented (19%). Few (21%) veterans reported exposure to hostile or friendly fire during their service. More than three-fourths (80%) of the sample had experienced a homeless episode prior to their current one. On average, members of the sample had experienced a median of 3 lifetime homeless episodes. They had a mean 4.1 (SD, 5.8) lifetime number of years of homelessness, and 3.0 (SD, 5.2) years in their current homeless episode. Nearly one-third (31%) reported that they were currently staying in a homeless shelter, and nearly one-sixth (16%) were currently unsheltered in street settings, such as under bridges or in outdoor encampments at the time of the initial visit.
The mean number of minutes spent completing the P-CHI was 18.5 (SD, 9.4). The veterans indicated that they would like assistance with a mean 3.2 (SD, 2.2) number of domains. The domains with the highest average importance ratings were housing (mean, 9.4; SD, 1.7) and medical/dental care (mean, 8.9; SD, 2.2); the domains with the lowest average importance rating were reducing alcohol/drug use (mean, 6.4; SD, 4.1) and employment/vocation (mean, 6.3; SD, 4.2). The domains with the highest average satisfaction ratings were personal/spiritual fulfillment (mean, 7.3; SD, 2.9) and reducing substance use (mean, 5.9; SD, 4.0), and the domains with the lowest average satisfaction ratings were housing (mean, 2.9; SD, 2.9), material needs (mean, 4.2; SD, 3.3), and employment/vocation (mean, 4.2; SD, 3.2). The domain with the greatest indication of desire for help was housing, endorsed by more than four-fifths (84%) of the sample. This highly endorsed housing domain also was one of the lowest in satisfaction. The domains with the least expressed interest in obtaining help were reducing substance use (18%) and personal/spiritual fulfillment (15%).Reducing substance abuse also was one of the lowest domains of importance and the least for dissatisfaction.
Challenges and Barriers
As anticipated from its inception, this project encountered many challenges and barriers. The first was with the design, construction, and delivery of the mobile clinic unit. The vehicle took more than 2 years to be delivered. There were delays in progress necessitated by required selection of an approved vendor to build the vehicle, extensive specification of details and features, and stocking it with equipment and supplies. The weight of the unit had to be < 26,000 pounds to avoid the requirement of a commercial driver’s license, which limited the size of the vehicle to 28 feet. Stocking the unit with equipment and supplies required attention to a myriad of specifications and decisions. For example, separate refrigerators were needed for specimens, medications, and food; pharmaceutical regulations governing medications in mobile clinics required strict adherence; and difficulties were encountered in attempting to establish adequate and secure connectivity for communications devices in the field.
Once the mobile unit was delivered and prepared for deployment, the next set of challenges pertained to learning all of the instructions required to operate and drive the vehicle and learning how to maneuver the vehicle in the field. Specific challenges for driving the vehicle encountered included unexpectedly low overpasses that prohibited passage, narrow spaces for passage, rough and uneven terrain in off-road settings, and lateral and vertical tilt of roads creating potential for sideswipes and undercarriage scrapes. Maintenance schedules needed to be developed and implemented for cleaning the unit, inspection compliance, repairs, refueling, and emptying waste materials.
Staffing the vehicle required the development of unique job specifications addressing special expertise in accessing VA databases for veteran verification and registration and for driving the mobile clinic vehicle. Schedules and deployment plans for 2 teams that shared the same vehicle had to be established and followed. Locating veterans in unsheltered settings, such as under bridges and in encampments, required community intelligence facilitated through partnerships with knowledgeable members of the Dallas police crisis unit and by gaining field experience to locate where the usual homeless gathering places are, especially those inhabited by veterans. Safety of team members and equipment/supplies in the field was paramount from the start, and additional steps beyond safety training required extra measures, such as special care in navigating known dangerous areas. Provision of services necessitated completion of everything needed in a single visit due to the likelihood of loss to follow-up and acceptance of the limited types of service that could be provided in a mobile clinic. Special procedures were needed to provide referrals to sources of available care for non-VA-qualifying veterans.
Discussion
The HMMM-V program for delivery of PCC to homeless veterans is an innovative pilot program designed to connect with difficult-to-reach homeless veterans and engage them in care. The deliverables provided by this project are (1) A mobile outreach vehicle to deliver care to homeless veterans and outreach to other veterans and community agencies in North Texas; (2) The P-CHI assessment tool for homeless veterans modified and adapted for use with this special population; and (3) pilot data on its first cohort of homeless veterans served, describing their baseline characteristics and their stated satisfaction and preferences about their goals and aspirations for their physical, emotional, and mental health and well-being.
The HMMM-V program successfully identified homeless veterans in need of services, and more than one-third of these veterans were not previously engaged in VA services. Compared with the “typical” veterans served at VANTHCS homeless programs, veterans served by the HMMM-V comprised a greater proportion of minorities and a higher proportion who had been exposed to combat.29 Age and gender characteristics were similar.29 When compared with veterans who access care at VANTHCS and have not experienced homelessness, those served by the HMMM-V were younger and more likely to belong to a minority group; however, they were similar in combat exposure and gender.1 The veterans served by the HMMM-V program also were considerably older and had more homeless chronicity than did nonveteran homeless populations, consistent with other research.4,29,30
The veterans served by the HMMM-V program not surprisingly made housing their top priority in need of help, consistent with the Housing First model.22,31 They also indicated that employment/vocation and reducing substance use were of lower importance. Need for assistance with reducing substance use and social support were the domains least often identified as areas where help was needed, which seems inconsistent with the higher established rates of substance abuse problems among homeless veterans.1
With additional fieldwork, the HMMM-V program is expected to allow refinement of procedures for identifying and serving veterans from a patient-centered care perspective. The P-CHI will be further tested and developed, and the next step will be to create and pilot intervention templates for a Patient-Centered Health Improvement Plan, based on the P-CHI results. This process parallels the original development treatment plans for the VA’s Personalized Health Plan based on the PHI.25 Once the HMMM-V program is fully established in Dallas, the plans are for an expansion that will cover a broader geographic area in North Texas that includes rural areas.
The HMMM-V program was designed to address the barriers to health care that are encountered by homeless veterans. It is unique in homeless veteran care due to its patient-centered approach that partners with homeless veterans to prioritize their needs as determined by them rather than based solely on policies or provider conceptualizations of their needs. Access to services, engagement in care, and successful utilization of needed services may lead to measurable improvements in health care outcomes among homeless populations of veterans. Desired goals include remission of illness through appropriate medical intervention, preventing morbidity, achieving healthy lifestyles, recovery from addiction, stabilization of psychiatric illness, and attainment of stable housing.
The first hurdle for implementing this type of program in other settings is the identification of resources needed for these efforts. Need of additional staffing resources, however, may be circumvented by allowing employees working in other areas to rotate in community outreach shifts in the mobile unit. Another hurdle encountered in implementation of the HMMM-V initiative was the initial difficulty finding homeless veterans in community settings, especially those in unsheltered locations. The HMMM-V program addressed this issue by partnering with other agencies serving the homeless in the community. Therefore, a general recommendation for other entities seeking to implement this type of program is to reach out to these community partners from the outset.
Conclusion
The HMMM-V has the potential to engage the most difficult-to-reach homeless veterans in need of health services by delivering care and providing resources in challenging environments. Further work is needed to validate the P-CHI for use with this program and to conduct well-designed and implemented research to demonstrate effectiveness of this intervention on veteran outcomes, especially quality of life. Once this additional work is accomplished, this innovative program can potentially be implemented by VAMCs across the nation, and potentially in more general community care settings, to more effectively reach out and deliver services to homeless members of the community.
Acknowledgments
Grant support was received from the Department of Veterans Affairs, Office of Patient Centered Care. The authors would like to acknowledge all the clinicians, trainees, and support staff who have contributed to the success of the HMMM-V program: Tara Ayala, Jose Cabrera, Tony Castillo, Rachael Lynn David, Teresa DeShazo, Sylvia Figueroa, Steven Fisher, Eric Gary, Evelyn Gibbs, Kevin Hosey, JoAnn Joseph, Taly Drimer Kagan, Miranda Kelly, Michelle King-Thompson, Sharon Marcus, Shiji Mathew, Moneeza Matin, John Moreno, Joseph Neifert, Joel Price, Tiffany Price, Natalie Qualls, Reginald Robertson, Kristine Rodrigues, Jon Saffelder, Jill Stokes, Scott Stone, and John Smith.
1. LePage JP, Bradshaw LD, Cipher DJ, Crawford AM, Hooshyar D. The effects of homelessness on veterans’ health care service use: an evaluation of independence from comorbidities. Public Health. 2014;128(11):985-992.
2. Fischer PJ, Breakey WR. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol. 1991;46(11):1115-1128.
3. Robertson MJ, Zlotnick C, Westerfelt A. Drug use disorders and treatment contact among homeless adults in Alameda County, California. Am J Public Health. 1997;87(2):221-228.
4. North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? Am J Public Health. 2004;94(1):103-108.
5. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225.
6. Harpaz-Rotem I, Rosenheck RA, Desai R. The mental health of children exposed to maternal mental illness and homelessness. Community Ment Health J. 2006;42(5):437-448.
7. Pollio DE, Eyrich-Garg KM, North CS. The homeless. In: Johnson BA, ed. Addiction Medicine: Science and Practice. New York, NY: Springer; 2011:1487-1504.
8. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
9. Baggett TP, Singer DE, Rao SR, O’Connell JJ, Bharel M, Rigotti NA. Food insufficiency and health services utilization in a national sample of homeless adults. J Gen Intern Med. 2011;26(6):627-634.
10. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376.
11. Fuehrlein BS, Cowell AJ, Pollio D, Cupps L, Balfour ME, North CS. A prospective study of the associations among housing status and costs of services in a homeless population. Psychiatr Serv. 2015;66(1):27-32.
12. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
13. U.S. Department of Housing and Urban Development Office of Community Planning and Development. The 2016 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: point-in-time estimates of homelessness. https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Published 2016. Accessed August 7, 2017.
14. Tsai J, Rosenheck RA. Risk factors for homelessness among U.S. veterans. Epidemiol Rev. 2015;37:177-195.
15. Williamson V, Mulhall E. Coming home: the housing crisis and homelessness threaten new veterans. Iraq and Afghanistan Veterans of America, January, 2009. http://media.iava.org/IAVA_coming_home_2009%20The%20Housing%20Crisis%20and%20Homelessness%20Threaten%20New%20Veterans.pdf. Accessed August 10, 2017
16. Shinseki EK. Remarks by Secretary Eric K. Shinseki. National Summit on Homeless Veterans; November 3, 2009; Washington, DC. https://www.va.gov/opa/speeches/2009/09_1103.asp. Updated August 8, 2016. Accessed August 7, 2017.
17. Shinseki EK. Remarks by Secretary Eric K. Shinseki. 2014 National Coalition for Homeless Veterans Annual Meeting; May 30, 2014; Arlington, VA. https://www.va.gov/opa/speeches/2014/05_30_2014.asp. Updated April 21, 2015. Accessed August 7, 2017.
18. Pollio DE, Spitznagel EL, North CS, Thompson S, Foster DA. Service use over time and achievement of stable housing in a mentally ill homeless population. Psychiatr Serv. 2000;51(12):1536-1543.
19. Page J. Barriers to transferring care of homeless people with serious mental illnesses to community mental health organizations: perspectives of street-based programs. Best Practices in Mental Health: An International Journal. 2007;3(1):26.
20. Young AS, Chinman MJ, Cradock-O’Leary JA, et al. Characteristics of individuals with severe mental illness who use emergency services. Community Ment Health J. 2005;41(2):159-168.
21. Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461.
22. Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651-656.
23. U.S. Department of Veterans Affairs, Veterans Health Administration. VA Patient Centered Care. http://www.va.gov/patientcenteredcare. Updated July 24,2017. Accessed August 7, 2017.
24. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
25. U.S. Department of Veterans Affairs, Office of Patient Centered Care and Cultural Transformation. My story: personal health inventory. https://www.va.gov/PATIENTCENTEREDCARE/docs/VA-OPCC-Personal-Health-Inventory-final-508.pdf. Published October 7, 2013. Accessed August 7, 2017
26. North CS, Smith EM, Pollio DE. The Homeless Supplement to the Diagnostic Interview Schedule (DIS/HS). St. Louis: Washington University, 2004.
27. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The homeless supplement to the diagnostic interview schedule: test-retest analyses. Int J Methods Psychiatr Res. 2004;13(3):184-191.
28. LaSalle JL. Homeless Operations Management and Evaluation System (HOMES) user manual-phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed August 7, 2017.
29. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psychiatr Serv. 2014;65(6):751-757.
30. North CS, Smith EM. A comparison of homeless men and women: different populations, different needs. Community Ment Health J. 1993;29(5):423-431.
31. Kertesz SG, Austin EL, Holmes SK, et al. Making housing first happen: organizational leadership in VA’s expansion of permanent supportive housing. J Gen Intern Med. 2014;29(suppl 4):835-844.
1. LePage JP, Bradshaw LD, Cipher DJ, Crawford AM, Hooshyar D. The effects of homelessness on veterans’ health care service use: an evaluation of independence from comorbidities. Public Health. 2014;128(11):985-992.
2. Fischer PJ, Breakey WR. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol. 1991;46(11):1115-1128.
3. Robertson MJ, Zlotnick C, Westerfelt A. Drug use disorders and treatment contact among homeless adults in Alameda County, California. Am J Public Health. 1997;87(2):221-228.
4. North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? Am J Public Health. 2004;94(1):103-108.
5. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225.
6. Harpaz-Rotem I, Rosenheck RA, Desai R. The mental health of children exposed to maternal mental illness and homelessness. Community Ment Health J. 2006;42(5):437-448.
7. Pollio DE, Eyrich-Garg KM, North CS. The homeless. In: Johnson BA, ed. Addiction Medicine: Science and Practice. New York, NY: Springer; 2011:1487-1504.
8. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
9. Baggett TP, Singer DE, Rao SR, O’Connell JJ, Bharel M, Rigotti NA. Food insufficiency and health services utilization in a national sample of homeless adults. J Gen Intern Med. 2011;26(6):627-634.
10. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376.
11. Fuehrlein BS, Cowell AJ, Pollio D, Cupps L, Balfour ME, North CS. A prospective study of the associations among housing status and costs of services in a homeless population. Psychiatr Serv. 2015;66(1):27-32.
12. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
13. U.S. Department of Housing and Urban Development Office of Community Planning and Development. The 2016 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: point-in-time estimates of homelessness. https://www.hudexchange.info/resources/documents/2016-AHAR-Part-1.pdf. Published 2016. Accessed August 7, 2017.
14. Tsai J, Rosenheck RA. Risk factors for homelessness among U.S. veterans. Epidemiol Rev. 2015;37:177-195.
15. Williamson V, Mulhall E. Coming home: the housing crisis and homelessness threaten new veterans. Iraq and Afghanistan Veterans of America, January, 2009. http://media.iava.org/IAVA_coming_home_2009%20The%20Housing%20Crisis%20and%20Homelessness%20Threaten%20New%20Veterans.pdf. Accessed August 10, 2017
16. Shinseki EK. Remarks by Secretary Eric K. Shinseki. National Summit on Homeless Veterans; November 3, 2009; Washington, DC. https://www.va.gov/opa/speeches/2009/09_1103.asp. Updated August 8, 2016. Accessed August 7, 2017.
17. Shinseki EK. Remarks by Secretary Eric K. Shinseki. 2014 National Coalition for Homeless Veterans Annual Meeting; May 30, 2014; Arlington, VA. https://www.va.gov/opa/speeches/2014/05_30_2014.asp. Updated April 21, 2015. Accessed August 7, 2017.
18. Pollio DE, Spitznagel EL, North CS, Thompson S, Foster DA. Service use over time and achievement of stable housing in a mentally ill homeless population. Psychiatr Serv. 2000;51(12):1536-1543.
19. Page J. Barriers to transferring care of homeless people with serious mental illnesses to community mental health organizations: perspectives of street-based programs. Best Practices in Mental Health: An International Journal. 2007;3(1):26.
20. Young AS, Chinman MJ, Cradock-O’Leary JA, et al. Characteristics of individuals with severe mental illness who use emergency services. Community Ment Health J. 2005;41(2):159-168.
21. Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461.
22. Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651-656.
23. U.S. Department of Veterans Affairs, Veterans Health Administration. VA Patient Centered Care. http://www.va.gov/patientcenteredcare. Updated July 24,2017. Accessed August 7, 2017.
24. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
25. U.S. Department of Veterans Affairs, Office of Patient Centered Care and Cultural Transformation. My story: personal health inventory. https://www.va.gov/PATIENTCENTEREDCARE/docs/VA-OPCC-Personal-Health-Inventory-final-508.pdf. Published October 7, 2013. Accessed August 7, 2017
26. North CS, Smith EM, Pollio DE. The Homeless Supplement to the Diagnostic Interview Schedule (DIS/HS). St. Louis: Washington University, 2004.
27. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The homeless supplement to the diagnostic interview schedule: test-retest analyses. Int J Methods Psychiatr Res. 2004;13(3):184-191.
28. LaSalle JL. Homeless Operations Management and Evaluation System (HOMES) user manual-phase 1. http://www.vfwsc.org/homes.pdf. Published April 19, 2011. Accessed August 7, 2017.
29. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psychiatr Serv. 2014;65(6):751-757.
30. North CS, Smith EM. A comparison of homeless men and women: different populations, different needs. Community Ment Health J. 1993;29(5):423-431.
31. Kertesz SG, Austin EL, Holmes SK, et al. Making housing first happen: organizational leadership in VA’s expansion of permanent supportive housing. J Gen Intern Med. 2014;29(suppl 4):835-844.
Predictors of VA and Non-VA Health Care Service Use by Homeless Veterans Residing in a Low-Demand Emergency Shelter
In 2009, the VA announced a goal of ending veteran homelessness by 2015.1 The primary focus of this new policy has been housing veterans experiencing chronic homelessness, many of whom languish outside the VA housing system. Since that time, progress has been made with point-in-time enumerations indicating that veteran homelessness has decreased nationally. Despite this progress, however, more than 55,000 veterans are still estimated to experience homelessness each night.2
Historically, the VA has offered an array of services specifically meant to alleviate veteran homelessness (grant, per diem, and other transitional housing programs; vocational rehabilitation, etc).3 The majority of these programs require some period of veteran abstinence as a condition for providing housing services. The recent move toward permanent “housing first” programs with few conditions for enrollment and participation provides new opportunities for housing veterans experiencing chronic homelessness, who are the specific target of the goal of ending veteran homelessness.4
Because veterans experiencing chronic homelessness have additional, substantial need for medical, psychiatric, and substance-abuse services, the VA also offers these services to this population.5-7 Veterans experiencing homelessness also may access parallel non-VA services.8 Information about veterans outside of traditional VA housing services, specifically those housed in low-demand shelters, is needed to develop services for this population and will be critical to success in ending veteran homelessness.
The Behavioral Model of Health Services Use9-11 and its later refinement, the Behavioral Model for Vulnerable Persons,12 have been used to conceptualize health care service use (Figure). In these models, health service use is predicted by 3 types of factors: predisposing factors (eg, age, race, gender, residential history), enabling factors (eg, availability, accessibility, affordability, acceptability), and service need factors (eg, substance-use disorders, mental health problems, physical health problems).
Studies applying these models of health care service use to both general homeless populations and, specifically to populations of veterans experiencing homelessness have found that service use is most influenced by need-based factors (eg, drug abuse, poor health, mental health problems).6,12-20 These same studies indicate that predisposing factors (eg, age, race, and gender) and enabling factors (eg, insurance, use of other services, and usual place of care) are also associated with service use, though less consistently.
Studies focused on veterans experiencing homelessness, however, included only treatment-seeking populations, which are not necessarily representative of the broader population of veterans experiencing homelessness. Additionally, none of these prior studies focused on the unique subset of veterans residing in low-demand shelters (characterized by unlimited duration of stay, no government ID or fee required for entry, and no requirement for service participation). This is a population that seems to be less engaged in services but nevertheless is challenged.21 This study, therefore, is focused on nontreatment seeking veterans residing in a low-demand shelter. The study applied the Behavioral Model of Health Services Use and the Behavioral Model for Vulnerable Persons to examine use of VA and non-VA services.
Study Parameters
This study was conducted in Fort Worth, Texas, the 17th largest city in the U.S. with more than 810,000 residents.22 In 2013, a biennial point-in-time count identified about 2,300 individuals who were homeless in Fort Worth. Most were found in emergency shelters (n = 1,126, 50%) or transitional housing (n = 965, 40%). Slightly more than 10% (n = 281) were found to be unsheltered: sleeping on the streets or in encampments, automobiles, or abandoned buildings.23 Although national estimates identify 12% of all adults who are homeless as veterans,2 only 8% (n = 189) of people experiencing homelessness in Fort Worth reported military service.23
Access to the full array of VA emergency department (ED), inpatient, and outpatient medical, psychiatric, and substance-abuse services are available to veterans experiencing homelessness at the Dallas VA Medical Center (DVAMC), located 35 miles away. Only VA outpatient medical, psychiatric, and substance-related services are available in Fort Worth through the VA Outpatient Clinic and Health Care for the Homeless Veterans (HCHV) program. If veterans experiencing homelessness seek care outside of the VA system, a comprehensive network of emergency, inpatient and outpatient medical, psychiatric, and substance-related services is available in Fort Worth.
Sample
The study sample included 110 adult male veterans randomly recruited as they awaited admission to a private, low-demand emergency shelter. The study excluded veterans with a dishonorable discharge to ensure participants were eligible for VA services. Institutional review board approvals were obtained prior to the study from the University of Texas at Arlington and DVAMC. All participants provided informed consent and were given a $5 gift for their involvement.
Instruments
Through structured interviews, experienced research staff collected demographics, history of homelessness, military service, and substance abuse in the previous 30 days. Data on alcohol and drug problems in the past 12 months were obtained using the Short Michigan Alcohol Screening Test (SMAST) and the Drug Abuse Screening Test. The Veterans RAND 12-Item Health Survey (VR-12) was used to measure physical and mental health functioning in the previous 4 weeks. Finally, participants reported their use of VA or non-VA medical (ED, inpatient, and outpatient), psychiatric (ED, inpatient, and outpatient), and substance abuse-related (inpatient and outpatient) services in the 12 months prior to the interview. These measures have been shown to be valid and reliable with acceptable psychometrics.24-26
Data Analysis
Statistical analysis was completed using IBM SPSS Statistics version 19. Descriptive data were summarized using counts, percentages, means, and standard deviations. A dichotomous variable for alcohol abuse was defined as SMAST score ≥ 3. A variable representing participant’s VR-12 mental component summary scores was used as an indicator of mental health functioning.
McNemar’s test was used to compare the use of VA and non-VA medical, psychiatric, and substance-related services using dichotomous variables for each overall sector as well as respective sector subcomponent services (emergency, inpatient, and outpatient for medical and psychiatric sectors and inpatient and outpatient for the substance-related sector). Statistical significance level was set at α = .05.
Logistic regression was used to predict psychiatric and substance abuse-related service use with separate dependent variables for VA, non-VA, and both VA and non-VA services. Need-based factors included in all models as independent variables were mental health functioning, alcohol abuse, and a dichotomous variable representing cocaine use in the previous 30 days. Independent variables for the other service sectors were included as enabling factors (eg, medical and substance-related problems predicting psychiatric service use), aligning all service use variables in the model to the same provider system (eg, VA service sector independent variables with VA service sector dependent variables).
Results
The sample mean age was 49.2 years (SD = 9.2), and fewer than half (n = 45, 41%) were white. Three-fourths (n = 82, 75%) had ever been married, and few participants (n = 5, 5%) were currently married. Total mean lifetime experience of homelessness was 3.9 years (SD = 4.3). One-third of the samples participants (n = 36, 33%) reported that their current episode of homelessness had lasted 1 year or longer. Most had an adult felony conviction (n = 78, 71%) and a history of incarceration as an adult (n = 104, 95%). All military branches were represented, with 49% serving in the Army, 23% in the Marine Corps, 17% in the Navy, 10% in the Air Force, and 1% in the Coast Guard.
Most of the sample’s veterans served during the Vietnam era (n = 43, 43%) or the post-Vietnam era (n = 49, 45%), but 12 (11%) served during the Persian Gulf era (including Operation Iraqi Freedom and Operation Enduring Freedom). Few received a nonservice connected VA pension (n = 21, 19%) or service-connected disability benefits (n = 20, 18%). The mean income earned in the previous 30 days was $466 (SD = $431). None of these predisposing factors were associated with any service variables.
The sample’s mean VR-12 physical functioning score was 43.8 (SD = 9.1), which was significantly higher (t = 6.2, df = 109, P < .001) than the 38.4 (SD = 12.2) population norm used with the instrument. The sample’s mean mental health functioning score of 39.4 (SD = 14.3) was significantly lower (t = -8.6, df = 109, P < .001) than the population norm (51.1, SD = 11.4).27 Substance-related problems were prevalent, with an identified alcohol problem in 62% (n = 68) and a drug problem in 79% (n = 87) of participants. More than half reported illicit drug use in the past 30 days (n = 61, 56%), especially cocaine (n = 42, 38%) and marijuana (n = 37, 33%).
The majority of veterans (n = 96, 87%) reported using some type of service in the past 12 months (Table 1). Most survey respondents used medical services. About half used psychiatric services, and almost one-third used substance-related services. More veterans used non-VA ED services than used VA ED services. More veterans used VA outpatient medical services than used non-VA outpatient medical services. Examining service sectors indicated that more veterans used VA psychiatric services than used non-VA psychiatric services, especially VA outpatient psychiatric services. More veterans used non-VA substance abuse-related services, especially outpatient services, rather than similar services offered by the VA.
Separate logistic regression models predicted use of psychiatric and substance-abuse services with 3 models (VA, non-VA, or any service use) for each dependent variable from independent variables that reflected need and enabling factors (Tables 2 and 3). Demographic predisposing factors, which were not associated with service use, were not included as covariates in these models. For the model predicting the use of non-VA substance-abuse services, collinearity between the alcohol-abuse and cocaine-abuse variables required separate models for each of the 2 variables.
Medical sector service use predicted psychiatric sector service use in all models. In fact, VA medical service use was the only predictor of use of VA psychiatric services. Lower mental health functioning predicted the use of any (VA or non-VA) psychiatric service use. In addition to the use of medical services, 30-day cocaine use predicted non-VA psychiatric service use.
Any substance-related sector service use was predicted by lower mental health functioning, self-reported alcohol problem, and any medical services utilization. No independent variables included in the model predicted any VA substance-related service use. Non-VA substance abuse service use was predicted by non-VA psychiatric service use and alcohol abuse. In the separate analysis that replaced alcohol problems with 30-day cocaine use variable, only 30-day cocaine use predicted non-VA substance-related service utilization.
Discussion
This study examined the use of medical, psychiatric, and substance-abuse services by randomly sampled veterans from a low-demand emergency shelter. Random selection of the sample and its high (98%) participation rate virtually eliminated potential for bias within this sample. Another strength of this study is its focus on low-demand shelter users—a population that has not been well studied. This low-demand shelter-dwelling population of veterans experiencing homelessness is of interest because more substance-abuse problems and histories of incarceration seem to make them especially disadvantaged and challenged.
The limitation of the sample to users of a low-demand shelter at only 1 location may reduce generalizability to other veteran homeless populations and settings. The study also may not generalize to populations of female veterans experiencing homelessness. Another limitation of the study is that it did not use diagnostic assessments for psychiatric and substance use disorders and objective collateral information such as agency record data. Finally, although the limited size of the sample may have been insufficient to adequately test certain hypotheses, it was a relatively large sample of this population and was large enough to yield significant findings.
This study found that need-based factors predicted the use of some service sectors intended for those needs. For example, mental health functioning appropriately predicted any psychiatric service use, and presence of an alcohol problem appropriately predicted any substance abuse service use. Specifically for non-VA services, both cocaine use and presence of an alcohol problem in separate models predicted substance-abuse service use. However for VA substance-abuse services, neither cocaine use nor presence of an alcohol problem predicted service use. Despite the high need, very few veterans used substance-abuse services, and they rarely used VA substance-abuse services.
For 2 service sectors, need-based factors predicted the use of services intended for other needs. Cocaine use predicted non-VA psychiatric service use, and low mental health functioning predicted substance-abuse service use. One potential explanation for this finding could be that providers or patients incorrectly classified cocaine-related substance use problems as psychiatric. The VR-12 mental health functioning measure also may have incorrectly classified cocaine-related problems as psychiatric.
Three enabling factors predicted service use by sector and type. The first 2 are preference for VA-provided services and the geographic availability of services, which competed for veterans’ selection of service providers. When both VA and non-VA services were present in Fort Worth, a preference for VA-provided services was observed, with the exception of outpatient substance abuse services which were highly underutilized in general. No preference was observed for any non-VA services when both were present. When VA services were not present in Fort Worth, veterans used geographically available non-VA providers for some services, but for other services they used Dallas-based VA and Fort Worth-based non-VA providers equally (Table 3 and Table 4).
The third enabling factor influencing service use was through other service use as an enabling pathway. Those veterans who opted out of locally available services in favor of VA services in Dallas may have been prompted to do so by provider referrals, which were further facilitated by VA and public transportation between Fort Worth and Dallas. The most consistent enabling pathway was medical service use, which predicted all types of psychiatric service use (VA and non-VA combined, VA only, and non-VA only), and any substance-related service use. Psychiatric service use predicted substance abuse service use but only in non-VA settings; no pathways led from VA medical or psychiatric services to VA substance abuse services.
Conclusions
These findings suggest, in large part, the validity of the Andersen and Gelberg models of health care service use. Consistent with prior studies, need-based factors predicted the use of any psychiatric and substance-related sector services as well as the use of non-VA subcomponent services for both sectors. Also consistent with prior studies, enabling factors (medical sector service use) predicted service use, with the exception of VA or non-VA substance-abuse services. Unlike prior studies, however, predisposing factors (eg, age, race, marital status, and income) were not associated with service use.
This study could not determine why veterans underutilized substance-abuse services, even those available locally to them in Fort Worth. One possible barrier to care is that the services are designed or delivered in a manner that does not engage these veterans (eg, expectations regarding abstinence or service involvement). Another barrier could be that referral pathways between VA outpatient medical and psychiatric service providers and VA substance-related services are not sufficiently facilitative. Future investigations could build upon the findings of this study by collecting data that could help assess these potential barriers.
The data from this study suggest 3 opportunities to improve the utilization of services most needed by this population. The first opportunity would be to accurately differentiate between substance abuse and psychiatric problems in clinical assessment and identify the most appropriate type of care. Another opportunity, linked closely to the first, would be to facilitate more effective and efficient referral pathways among VA service sectors, especially from medical and psychiatric services to substance-abuse services. Another strategy to improve referral pathways would be for VA service networks to systematically examine local service systems for factors or processes that may disrupt integrated care and implement program improvements.28 For homeless veterans navigating an inherently complex VA health care system, peer-to-peer and patient navigator programs have helped improve service efficiency and service outcomes.29 The third opportunity to improve utilization of services would be to ensure geographic availability and accessibility by strategic placement of these services.
The results from this study, while informative, point directly to needed areas for further inquiry to inform public health response. Although the low-demand shelter users are a particularly challenging subgroup of veterans experiencing chronic homelessness, other equally challenging populations warrant additional study. For example, veterans outside of both VA and community services (eg, unsheltered populations) are likely to require different approaches to engage in appropriate services. Additionally, changes to the homeless policy implemented in the period after this sample was recruited suggest the need to revisit the service-using behaviors of this population. Finally, interventions developed as part of the national response need to be assessed for their ability to engage these difficult-to-reach veterans.
Acknowledgements
This study was funded by a U.S. Department of Veterans Affairs Office of Academic Affiliations Pre-Doctoral Social Work Research Fellowship award.
1. U.S. Department of Veterans Affairs. Homeless veterans: VA is working to end homelessness among veterans. U.S. Department of Veterans Affairs Website. www.va.gov/homeless/about_the_initiative.asp#one. Updated January 26, 2016. Accessed February 16, 2016.
2. Henry M, Cortes A, Morris S, Abt Associates; U. S. Department of Housing and Urban Development Office of Community Planning and Development. The 2013 Annual Homeless Assessment Report (AHAR) to Congress: Part 1 Point-in-Time Estimates of Homelessness. HUD Exchange Website. https://www.hudexchange.info/resources/documents/ahar-2013-part1.pdf. Published October 2014. Accessed February 16, 2016.
3. U.S. Department of Veterans Affairs. Homeless Veterans: Housing Assistance. U.S. Department of Veterans Affairs Web site. http://www.va.gov/homeless/housing.asp. Updated November 5, 2015. Accessed February 16, 2016.
4. Austin EL, Pollio DE, Holmes S, et al. VA's expansion of supportive housing: successes and challenges on the path to Housing First. Psychiatr Serv. 2014;65(5):641-647.
5. Tsai J, Kasprow WJ, Rosenheck RA. Alcohol and drug use disorders among homeless veterans: prevalence and association with supported housing outcomes. Addict Behav. 2014;39(2):455-460.
6. Wenzel SL, Bakhtiar L, Caskey NH, et al. Homeless veterans utilization of medical, psychiatric, and substance abuse services. Med Care. 1995;33(11):1132-1144.
7. McQuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental health illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255-264.
8. Tsai J, Mares AS, Rosenheck RA. Do homeless veterans have the same needs and outcomes as non-veterans? Mil Med. 2012;177(1):27-31.
9. Andersen RM. A behavioral model of families use of health services: Research Series No. 25. Chicago, IL: University of Chicago Center for Health Administrative Studies; 1968.
10. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10.
11. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
12. Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273-1302.
13. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
14. Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: a prospective analysis. J Health Care Poor Underserved. 2000;11(2):212-230.
15. Gamache G, Rosenheck RA, Tessler R. Factors predicting choice of provider among homeless veterans with mental illness. Psychiatr Serv. 2000;51(8):1024-1028.
16. Wenzel SL, Audrey Burnam, M, Koegel P, et al. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Med Care. 2001;39(11):1158-1169.
17. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
18. Solorio MR, Milburn NG, Andersen RM, Trifskin S, Rodríguez MA. Emotional distress and mental health service use among urban homeless adolescents. J Behav Health Serv Res. 2006;33(4):381-393.
19. Stein JA, Andersen RM, Robertson M, Gelberg L. Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Anderson Behavioral Model for Vulnerable Populations. Health Psychol. 2012;31(1):20-30.
20. Linton KF, Shafer MS. Factors associated with the health service use of unsheltered, chronically homeless adults. Soc Work Public Health. 2013;29(1):73-80.
21. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psych Serv. 2014;65(6):751-757.
22. U.S. Census Bureau. State & County Quick Facts: Fort Worth (city), Texas. U.S. Census Bureau Website. http://quickfacts.census.gov/qfd/states/48/4827000.html. Revised December 2, 2015. Accessed February 17, 2016.
23. Tarrant County Homeless Coalition. 2014 point in time count results. Tarrant County Homeless Coalition Website. http://www.ahomewithhope.org/staff/local-data-research/2014-homeless-count/. Accessed February 16, 2016.
24. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The Homeless Supplement to the Diagnostic Interview Schedule: test-retest analyses. Int J Method Psychiatr Res. 2004;13(3):184-191.
25. Iqbal SU, Rogers W, Selim A, et al. The Veterans RAND 12 Item Health Survey (VR-12): What it is and how it is Used. Washington, DC: Veterans Health Administration; 2009.
26. Fischer J, Corcoran K, eds. Measures for Clinical Practice and Research: A Sourcebook. 4th ed. New York, NY: Oxford University Press; 2013.
27. Selim AJ, Rogers W, Fleishman JA, Qian SX, Finke BG, Rothendler JA, Kazis LE. Updated U.S. population standard for the Veterans RAND 12-Item Health Survey (VR-12). Qual Life Res. 2009;18(1):43-52.
28. Blue-Howells J, McQuire J, Nakashima J. Co-location of health care services for homeless veterans: a case study of innovation in program implementation. Soc Work Health Care. 2008;47(3):219-231.
29. Piette JD, Holtz B, Beard AJ, et al; Ann Arbor PACT Steering Committee. Improving chronic illness care for veterans within the framework of the Patient-Centered Medical Home: experiences from the Ann Arbor Patient-Aligned Care Team Laboratory. Transl Behav Med. 2011;1(4):615-623.
In 2009, the VA announced a goal of ending veteran homelessness by 2015.1 The primary focus of this new policy has been housing veterans experiencing chronic homelessness, many of whom languish outside the VA housing system. Since that time, progress has been made with point-in-time enumerations indicating that veteran homelessness has decreased nationally. Despite this progress, however, more than 55,000 veterans are still estimated to experience homelessness each night.2
Historically, the VA has offered an array of services specifically meant to alleviate veteran homelessness (grant, per diem, and other transitional housing programs; vocational rehabilitation, etc).3 The majority of these programs require some period of veteran abstinence as a condition for providing housing services. The recent move toward permanent “housing first” programs with few conditions for enrollment and participation provides new opportunities for housing veterans experiencing chronic homelessness, who are the specific target of the goal of ending veteran homelessness.4
Because veterans experiencing chronic homelessness have additional, substantial need for medical, psychiatric, and substance-abuse services, the VA also offers these services to this population.5-7 Veterans experiencing homelessness also may access parallel non-VA services.8 Information about veterans outside of traditional VA housing services, specifically those housed in low-demand shelters, is needed to develop services for this population and will be critical to success in ending veteran homelessness.
The Behavioral Model of Health Services Use9-11 and its later refinement, the Behavioral Model for Vulnerable Persons,12 have been used to conceptualize health care service use (Figure). In these models, health service use is predicted by 3 types of factors: predisposing factors (eg, age, race, gender, residential history), enabling factors (eg, availability, accessibility, affordability, acceptability), and service need factors (eg, substance-use disorders, mental health problems, physical health problems).
Studies applying these models of health care service use to both general homeless populations and, specifically to populations of veterans experiencing homelessness have found that service use is most influenced by need-based factors (eg, drug abuse, poor health, mental health problems).6,12-20 These same studies indicate that predisposing factors (eg, age, race, and gender) and enabling factors (eg, insurance, use of other services, and usual place of care) are also associated with service use, though less consistently.
Studies focused on veterans experiencing homelessness, however, included only treatment-seeking populations, which are not necessarily representative of the broader population of veterans experiencing homelessness. Additionally, none of these prior studies focused on the unique subset of veterans residing in low-demand shelters (characterized by unlimited duration of stay, no government ID or fee required for entry, and no requirement for service participation). This is a population that seems to be less engaged in services but nevertheless is challenged.21 This study, therefore, is focused on nontreatment seeking veterans residing in a low-demand shelter. The study applied the Behavioral Model of Health Services Use and the Behavioral Model for Vulnerable Persons to examine use of VA and non-VA services.
Study Parameters
This study was conducted in Fort Worth, Texas, the 17th largest city in the U.S. with more than 810,000 residents.22 In 2013, a biennial point-in-time count identified about 2,300 individuals who were homeless in Fort Worth. Most were found in emergency shelters (n = 1,126, 50%) or transitional housing (n = 965, 40%). Slightly more than 10% (n = 281) were found to be unsheltered: sleeping on the streets or in encampments, automobiles, or abandoned buildings.23 Although national estimates identify 12% of all adults who are homeless as veterans,2 only 8% (n = 189) of people experiencing homelessness in Fort Worth reported military service.23
Access to the full array of VA emergency department (ED), inpatient, and outpatient medical, psychiatric, and substance-abuse services are available to veterans experiencing homelessness at the Dallas VA Medical Center (DVAMC), located 35 miles away. Only VA outpatient medical, psychiatric, and substance-related services are available in Fort Worth through the VA Outpatient Clinic and Health Care for the Homeless Veterans (HCHV) program. If veterans experiencing homelessness seek care outside of the VA system, a comprehensive network of emergency, inpatient and outpatient medical, psychiatric, and substance-related services is available in Fort Worth.
Sample
The study sample included 110 adult male veterans randomly recruited as they awaited admission to a private, low-demand emergency shelter. The study excluded veterans with a dishonorable discharge to ensure participants were eligible for VA services. Institutional review board approvals were obtained prior to the study from the University of Texas at Arlington and DVAMC. All participants provided informed consent and were given a $5 gift for their involvement.
Instruments
Through structured interviews, experienced research staff collected demographics, history of homelessness, military service, and substance abuse in the previous 30 days. Data on alcohol and drug problems in the past 12 months were obtained using the Short Michigan Alcohol Screening Test (SMAST) and the Drug Abuse Screening Test. The Veterans RAND 12-Item Health Survey (VR-12) was used to measure physical and mental health functioning in the previous 4 weeks. Finally, participants reported their use of VA or non-VA medical (ED, inpatient, and outpatient), psychiatric (ED, inpatient, and outpatient), and substance abuse-related (inpatient and outpatient) services in the 12 months prior to the interview. These measures have been shown to be valid and reliable with acceptable psychometrics.24-26
Data Analysis
Statistical analysis was completed using IBM SPSS Statistics version 19. Descriptive data were summarized using counts, percentages, means, and standard deviations. A dichotomous variable for alcohol abuse was defined as SMAST score ≥ 3. A variable representing participant’s VR-12 mental component summary scores was used as an indicator of mental health functioning.
McNemar’s test was used to compare the use of VA and non-VA medical, psychiatric, and substance-related services using dichotomous variables for each overall sector as well as respective sector subcomponent services (emergency, inpatient, and outpatient for medical and psychiatric sectors and inpatient and outpatient for the substance-related sector). Statistical significance level was set at α = .05.
Logistic regression was used to predict psychiatric and substance abuse-related service use with separate dependent variables for VA, non-VA, and both VA and non-VA services. Need-based factors included in all models as independent variables were mental health functioning, alcohol abuse, and a dichotomous variable representing cocaine use in the previous 30 days. Independent variables for the other service sectors were included as enabling factors (eg, medical and substance-related problems predicting psychiatric service use), aligning all service use variables in the model to the same provider system (eg, VA service sector independent variables with VA service sector dependent variables).
Results
The sample mean age was 49.2 years (SD = 9.2), and fewer than half (n = 45, 41%) were white. Three-fourths (n = 82, 75%) had ever been married, and few participants (n = 5, 5%) were currently married. Total mean lifetime experience of homelessness was 3.9 years (SD = 4.3). One-third of the samples participants (n = 36, 33%) reported that their current episode of homelessness had lasted 1 year or longer. Most had an adult felony conviction (n = 78, 71%) and a history of incarceration as an adult (n = 104, 95%). All military branches were represented, with 49% serving in the Army, 23% in the Marine Corps, 17% in the Navy, 10% in the Air Force, and 1% in the Coast Guard.
Most of the sample’s veterans served during the Vietnam era (n = 43, 43%) or the post-Vietnam era (n = 49, 45%), but 12 (11%) served during the Persian Gulf era (including Operation Iraqi Freedom and Operation Enduring Freedom). Few received a nonservice connected VA pension (n = 21, 19%) or service-connected disability benefits (n = 20, 18%). The mean income earned in the previous 30 days was $466 (SD = $431). None of these predisposing factors were associated with any service variables.
The sample’s mean VR-12 physical functioning score was 43.8 (SD = 9.1), which was significantly higher (t = 6.2, df = 109, P < .001) than the 38.4 (SD = 12.2) population norm used with the instrument. The sample’s mean mental health functioning score of 39.4 (SD = 14.3) was significantly lower (t = -8.6, df = 109, P < .001) than the population norm (51.1, SD = 11.4).27 Substance-related problems were prevalent, with an identified alcohol problem in 62% (n = 68) and a drug problem in 79% (n = 87) of participants. More than half reported illicit drug use in the past 30 days (n = 61, 56%), especially cocaine (n = 42, 38%) and marijuana (n = 37, 33%).
The majority of veterans (n = 96, 87%) reported using some type of service in the past 12 months (Table 1). Most survey respondents used medical services. About half used psychiatric services, and almost one-third used substance-related services. More veterans used non-VA ED services than used VA ED services. More veterans used VA outpatient medical services than used non-VA outpatient medical services. Examining service sectors indicated that more veterans used VA psychiatric services than used non-VA psychiatric services, especially VA outpatient psychiatric services. More veterans used non-VA substance abuse-related services, especially outpatient services, rather than similar services offered by the VA.
Separate logistic regression models predicted use of psychiatric and substance-abuse services with 3 models (VA, non-VA, or any service use) for each dependent variable from independent variables that reflected need and enabling factors (Tables 2 and 3). Demographic predisposing factors, which were not associated with service use, were not included as covariates in these models. For the model predicting the use of non-VA substance-abuse services, collinearity between the alcohol-abuse and cocaine-abuse variables required separate models for each of the 2 variables.
Medical sector service use predicted psychiatric sector service use in all models. In fact, VA medical service use was the only predictor of use of VA psychiatric services. Lower mental health functioning predicted the use of any (VA or non-VA) psychiatric service use. In addition to the use of medical services, 30-day cocaine use predicted non-VA psychiatric service use.
Any substance-related sector service use was predicted by lower mental health functioning, self-reported alcohol problem, and any medical services utilization. No independent variables included in the model predicted any VA substance-related service use. Non-VA substance abuse service use was predicted by non-VA psychiatric service use and alcohol abuse. In the separate analysis that replaced alcohol problems with 30-day cocaine use variable, only 30-day cocaine use predicted non-VA substance-related service utilization.
Discussion
This study examined the use of medical, psychiatric, and substance-abuse services by randomly sampled veterans from a low-demand emergency shelter. Random selection of the sample and its high (98%) participation rate virtually eliminated potential for bias within this sample. Another strength of this study is its focus on low-demand shelter users—a population that has not been well studied. This low-demand shelter-dwelling population of veterans experiencing homelessness is of interest because more substance-abuse problems and histories of incarceration seem to make them especially disadvantaged and challenged.
The limitation of the sample to users of a low-demand shelter at only 1 location may reduce generalizability to other veteran homeless populations and settings. The study also may not generalize to populations of female veterans experiencing homelessness. Another limitation of the study is that it did not use diagnostic assessments for psychiatric and substance use disorders and objective collateral information such as agency record data. Finally, although the limited size of the sample may have been insufficient to adequately test certain hypotheses, it was a relatively large sample of this population and was large enough to yield significant findings.
This study found that need-based factors predicted the use of some service sectors intended for those needs. For example, mental health functioning appropriately predicted any psychiatric service use, and presence of an alcohol problem appropriately predicted any substance abuse service use. Specifically for non-VA services, both cocaine use and presence of an alcohol problem in separate models predicted substance-abuse service use. However for VA substance-abuse services, neither cocaine use nor presence of an alcohol problem predicted service use. Despite the high need, very few veterans used substance-abuse services, and they rarely used VA substance-abuse services.
For 2 service sectors, need-based factors predicted the use of services intended for other needs. Cocaine use predicted non-VA psychiatric service use, and low mental health functioning predicted substance-abuse service use. One potential explanation for this finding could be that providers or patients incorrectly classified cocaine-related substance use problems as psychiatric. The VR-12 mental health functioning measure also may have incorrectly classified cocaine-related problems as psychiatric.
Three enabling factors predicted service use by sector and type. The first 2 are preference for VA-provided services and the geographic availability of services, which competed for veterans’ selection of service providers. When both VA and non-VA services were present in Fort Worth, a preference for VA-provided services was observed, with the exception of outpatient substance abuse services which were highly underutilized in general. No preference was observed for any non-VA services when both were present. When VA services were not present in Fort Worth, veterans used geographically available non-VA providers for some services, but for other services they used Dallas-based VA and Fort Worth-based non-VA providers equally (Table 3 and Table 4).
The third enabling factor influencing service use was through other service use as an enabling pathway. Those veterans who opted out of locally available services in favor of VA services in Dallas may have been prompted to do so by provider referrals, which were further facilitated by VA and public transportation between Fort Worth and Dallas. The most consistent enabling pathway was medical service use, which predicted all types of psychiatric service use (VA and non-VA combined, VA only, and non-VA only), and any substance-related service use. Psychiatric service use predicted substance abuse service use but only in non-VA settings; no pathways led from VA medical or psychiatric services to VA substance abuse services.
Conclusions
These findings suggest, in large part, the validity of the Andersen and Gelberg models of health care service use. Consistent with prior studies, need-based factors predicted the use of any psychiatric and substance-related sector services as well as the use of non-VA subcomponent services for both sectors. Also consistent with prior studies, enabling factors (medical sector service use) predicted service use, with the exception of VA or non-VA substance-abuse services. Unlike prior studies, however, predisposing factors (eg, age, race, marital status, and income) were not associated with service use.
This study could not determine why veterans underutilized substance-abuse services, even those available locally to them in Fort Worth. One possible barrier to care is that the services are designed or delivered in a manner that does not engage these veterans (eg, expectations regarding abstinence or service involvement). Another barrier could be that referral pathways between VA outpatient medical and psychiatric service providers and VA substance-related services are not sufficiently facilitative. Future investigations could build upon the findings of this study by collecting data that could help assess these potential barriers.
The data from this study suggest 3 opportunities to improve the utilization of services most needed by this population. The first opportunity would be to accurately differentiate between substance abuse and psychiatric problems in clinical assessment and identify the most appropriate type of care. Another opportunity, linked closely to the first, would be to facilitate more effective and efficient referral pathways among VA service sectors, especially from medical and psychiatric services to substance-abuse services. Another strategy to improve referral pathways would be for VA service networks to systematically examine local service systems for factors or processes that may disrupt integrated care and implement program improvements.28 For homeless veterans navigating an inherently complex VA health care system, peer-to-peer and patient navigator programs have helped improve service efficiency and service outcomes.29 The third opportunity to improve utilization of services would be to ensure geographic availability and accessibility by strategic placement of these services.
The results from this study, while informative, point directly to needed areas for further inquiry to inform public health response. Although the low-demand shelter users are a particularly challenging subgroup of veterans experiencing chronic homelessness, other equally challenging populations warrant additional study. For example, veterans outside of both VA and community services (eg, unsheltered populations) are likely to require different approaches to engage in appropriate services. Additionally, changes to the homeless policy implemented in the period after this sample was recruited suggest the need to revisit the service-using behaviors of this population. Finally, interventions developed as part of the national response need to be assessed for their ability to engage these difficult-to-reach veterans.
Acknowledgements
This study was funded by a U.S. Department of Veterans Affairs Office of Academic Affiliations Pre-Doctoral Social Work Research Fellowship award.
In 2009, the VA announced a goal of ending veteran homelessness by 2015.1 The primary focus of this new policy has been housing veterans experiencing chronic homelessness, many of whom languish outside the VA housing system. Since that time, progress has been made with point-in-time enumerations indicating that veteran homelessness has decreased nationally. Despite this progress, however, more than 55,000 veterans are still estimated to experience homelessness each night.2
Historically, the VA has offered an array of services specifically meant to alleviate veteran homelessness (grant, per diem, and other transitional housing programs; vocational rehabilitation, etc).3 The majority of these programs require some period of veteran abstinence as a condition for providing housing services. The recent move toward permanent “housing first” programs with few conditions for enrollment and participation provides new opportunities for housing veterans experiencing chronic homelessness, who are the specific target of the goal of ending veteran homelessness.4
Because veterans experiencing chronic homelessness have additional, substantial need for medical, psychiatric, and substance-abuse services, the VA also offers these services to this population.5-7 Veterans experiencing homelessness also may access parallel non-VA services.8 Information about veterans outside of traditional VA housing services, specifically those housed in low-demand shelters, is needed to develop services for this population and will be critical to success in ending veteran homelessness.
The Behavioral Model of Health Services Use9-11 and its later refinement, the Behavioral Model for Vulnerable Persons,12 have been used to conceptualize health care service use (Figure). In these models, health service use is predicted by 3 types of factors: predisposing factors (eg, age, race, gender, residential history), enabling factors (eg, availability, accessibility, affordability, acceptability), and service need factors (eg, substance-use disorders, mental health problems, physical health problems).
Studies applying these models of health care service use to both general homeless populations and, specifically to populations of veterans experiencing homelessness have found that service use is most influenced by need-based factors (eg, drug abuse, poor health, mental health problems).6,12-20 These same studies indicate that predisposing factors (eg, age, race, and gender) and enabling factors (eg, insurance, use of other services, and usual place of care) are also associated with service use, though less consistently.
Studies focused on veterans experiencing homelessness, however, included only treatment-seeking populations, which are not necessarily representative of the broader population of veterans experiencing homelessness. Additionally, none of these prior studies focused on the unique subset of veterans residing in low-demand shelters (characterized by unlimited duration of stay, no government ID or fee required for entry, and no requirement for service participation). This is a population that seems to be less engaged in services but nevertheless is challenged.21 This study, therefore, is focused on nontreatment seeking veterans residing in a low-demand shelter. The study applied the Behavioral Model of Health Services Use and the Behavioral Model for Vulnerable Persons to examine use of VA and non-VA services.
Study Parameters
This study was conducted in Fort Worth, Texas, the 17th largest city in the U.S. with more than 810,000 residents.22 In 2013, a biennial point-in-time count identified about 2,300 individuals who were homeless in Fort Worth. Most were found in emergency shelters (n = 1,126, 50%) or transitional housing (n = 965, 40%). Slightly more than 10% (n = 281) were found to be unsheltered: sleeping on the streets or in encampments, automobiles, or abandoned buildings.23 Although national estimates identify 12% of all adults who are homeless as veterans,2 only 8% (n = 189) of people experiencing homelessness in Fort Worth reported military service.23
Access to the full array of VA emergency department (ED), inpatient, and outpatient medical, psychiatric, and substance-abuse services are available to veterans experiencing homelessness at the Dallas VA Medical Center (DVAMC), located 35 miles away. Only VA outpatient medical, psychiatric, and substance-related services are available in Fort Worth through the VA Outpatient Clinic and Health Care for the Homeless Veterans (HCHV) program. If veterans experiencing homelessness seek care outside of the VA system, a comprehensive network of emergency, inpatient and outpatient medical, psychiatric, and substance-related services is available in Fort Worth.
Sample
The study sample included 110 adult male veterans randomly recruited as they awaited admission to a private, low-demand emergency shelter. The study excluded veterans with a dishonorable discharge to ensure participants were eligible for VA services. Institutional review board approvals were obtained prior to the study from the University of Texas at Arlington and DVAMC. All participants provided informed consent and were given a $5 gift for their involvement.
Instruments
Through structured interviews, experienced research staff collected demographics, history of homelessness, military service, and substance abuse in the previous 30 days. Data on alcohol and drug problems in the past 12 months were obtained using the Short Michigan Alcohol Screening Test (SMAST) and the Drug Abuse Screening Test. The Veterans RAND 12-Item Health Survey (VR-12) was used to measure physical and mental health functioning in the previous 4 weeks. Finally, participants reported their use of VA or non-VA medical (ED, inpatient, and outpatient), psychiatric (ED, inpatient, and outpatient), and substance abuse-related (inpatient and outpatient) services in the 12 months prior to the interview. These measures have been shown to be valid and reliable with acceptable psychometrics.24-26
Data Analysis
Statistical analysis was completed using IBM SPSS Statistics version 19. Descriptive data were summarized using counts, percentages, means, and standard deviations. A dichotomous variable for alcohol abuse was defined as SMAST score ≥ 3. A variable representing participant’s VR-12 mental component summary scores was used as an indicator of mental health functioning.
McNemar’s test was used to compare the use of VA and non-VA medical, psychiatric, and substance-related services using dichotomous variables for each overall sector as well as respective sector subcomponent services (emergency, inpatient, and outpatient for medical and psychiatric sectors and inpatient and outpatient for the substance-related sector). Statistical significance level was set at α = .05.
Logistic regression was used to predict psychiatric and substance abuse-related service use with separate dependent variables for VA, non-VA, and both VA and non-VA services. Need-based factors included in all models as independent variables were mental health functioning, alcohol abuse, and a dichotomous variable representing cocaine use in the previous 30 days. Independent variables for the other service sectors were included as enabling factors (eg, medical and substance-related problems predicting psychiatric service use), aligning all service use variables in the model to the same provider system (eg, VA service sector independent variables with VA service sector dependent variables).
Results
The sample mean age was 49.2 years (SD = 9.2), and fewer than half (n = 45, 41%) were white. Three-fourths (n = 82, 75%) had ever been married, and few participants (n = 5, 5%) were currently married. Total mean lifetime experience of homelessness was 3.9 years (SD = 4.3). One-third of the samples participants (n = 36, 33%) reported that their current episode of homelessness had lasted 1 year or longer. Most had an adult felony conviction (n = 78, 71%) and a history of incarceration as an adult (n = 104, 95%). All military branches were represented, with 49% serving in the Army, 23% in the Marine Corps, 17% in the Navy, 10% in the Air Force, and 1% in the Coast Guard.
Most of the sample’s veterans served during the Vietnam era (n = 43, 43%) or the post-Vietnam era (n = 49, 45%), but 12 (11%) served during the Persian Gulf era (including Operation Iraqi Freedom and Operation Enduring Freedom). Few received a nonservice connected VA pension (n = 21, 19%) or service-connected disability benefits (n = 20, 18%). The mean income earned in the previous 30 days was $466 (SD = $431). None of these predisposing factors were associated with any service variables.
The sample’s mean VR-12 physical functioning score was 43.8 (SD = 9.1), which was significantly higher (t = 6.2, df = 109, P < .001) than the 38.4 (SD = 12.2) population norm used with the instrument. The sample’s mean mental health functioning score of 39.4 (SD = 14.3) was significantly lower (t = -8.6, df = 109, P < .001) than the population norm (51.1, SD = 11.4).27 Substance-related problems were prevalent, with an identified alcohol problem in 62% (n = 68) and a drug problem in 79% (n = 87) of participants. More than half reported illicit drug use in the past 30 days (n = 61, 56%), especially cocaine (n = 42, 38%) and marijuana (n = 37, 33%).
The majority of veterans (n = 96, 87%) reported using some type of service in the past 12 months (Table 1). Most survey respondents used medical services. About half used psychiatric services, and almost one-third used substance-related services. More veterans used non-VA ED services than used VA ED services. More veterans used VA outpatient medical services than used non-VA outpatient medical services. Examining service sectors indicated that more veterans used VA psychiatric services than used non-VA psychiatric services, especially VA outpatient psychiatric services. More veterans used non-VA substance abuse-related services, especially outpatient services, rather than similar services offered by the VA.
Separate logistic regression models predicted use of psychiatric and substance-abuse services with 3 models (VA, non-VA, or any service use) for each dependent variable from independent variables that reflected need and enabling factors (Tables 2 and 3). Demographic predisposing factors, which were not associated with service use, were not included as covariates in these models. For the model predicting the use of non-VA substance-abuse services, collinearity between the alcohol-abuse and cocaine-abuse variables required separate models for each of the 2 variables.
Medical sector service use predicted psychiatric sector service use in all models. In fact, VA medical service use was the only predictor of use of VA psychiatric services. Lower mental health functioning predicted the use of any (VA or non-VA) psychiatric service use. In addition to the use of medical services, 30-day cocaine use predicted non-VA psychiatric service use.
Any substance-related sector service use was predicted by lower mental health functioning, self-reported alcohol problem, and any medical services utilization. No independent variables included in the model predicted any VA substance-related service use. Non-VA substance abuse service use was predicted by non-VA psychiatric service use and alcohol abuse. In the separate analysis that replaced alcohol problems with 30-day cocaine use variable, only 30-day cocaine use predicted non-VA substance-related service utilization.
Discussion
This study examined the use of medical, psychiatric, and substance-abuse services by randomly sampled veterans from a low-demand emergency shelter. Random selection of the sample and its high (98%) participation rate virtually eliminated potential for bias within this sample. Another strength of this study is its focus on low-demand shelter users—a population that has not been well studied. This low-demand shelter-dwelling population of veterans experiencing homelessness is of interest because more substance-abuse problems and histories of incarceration seem to make them especially disadvantaged and challenged.
The limitation of the sample to users of a low-demand shelter at only 1 location may reduce generalizability to other veteran homeless populations and settings. The study also may not generalize to populations of female veterans experiencing homelessness. Another limitation of the study is that it did not use diagnostic assessments for psychiatric and substance use disorders and objective collateral information such as agency record data. Finally, although the limited size of the sample may have been insufficient to adequately test certain hypotheses, it was a relatively large sample of this population and was large enough to yield significant findings.
This study found that need-based factors predicted the use of some service sectors intended for those needs. For example, mental health functioning appropriately predicted any psychiatric service use, and presence of an alcohol problem appropriately predicted any substance abuse service use. Specifically for non-VA services, both cocaine use and presence of an alcohol problem in separate models predicted substance-abuse service use. However for VA substance-abuse services, neither cocaine use nor presence of an alcohol problem predicted service use. Despite the high need, very few veterans used substance-abuse services, and they rarely used VA substance-abuse services.
For 2 service sectors, need-based factors predicted the use of services intended for other needs. Cocaine use predicted non-VA psychiatric service use, and low mental health functioning predicted substance-abuse service use. One potential explanation for this finding could be that providers or patients incorrectly classified cocaine-related substance use problems as psychiatric. The VR-12 mental health functioning measure also may have incorrectly classified cocaine-related problems as psychiatric.
Three enabling factors predicted service use by sector and type. The first 2 are preference for VA-provided services and the geographic availability of services, which competed for veterans’ selection of service providers. When both VA and non-VA services were present in Fort Worth, a preference for VA-provided services was observed, with the exception of outpatient substance abuse services which were highly underutilized in general. No preference was observed for any non-VA services when both were present. When VA services were not present in Fort Worth, veterans used geographically available non-VA providers for some services, but for other services they used Dallas-based VA and Fort Worth-based non-VA providers equally (Table 3 and Table 4).
The third enabling factor influencing service use was through other service use as an enabling pathway. Those veterans who opted out of locally available services in favor of VA services in Dallas may have been prompted to do so by provider referrals, which were further facilitated by VA and public transportation between Fort Worth and Dallas. The most consistent enabling pathway was medical service use, which predicted all types of psychiatric service use (VA and non-VA combined, VA only, and non-VA only), and any substance-related service use. Psychiatric service use predicted substance abuse service use but only in non-VA settings; no pathways led from VA medical or psychiatric services to VA substance abuse services.
Conclusions
These findings suggest, in large part, the validity of the Andersen and Gelberg models of health care service use. Consistent with prior studies, need-based factors predicted the use of any psychiatric and substance-related sector services as well as the use of non-VA subcomponent services for both sectors. Also consistent with prior studies, enabling factors (medical sector service use) predicted service use, with the exception of VA or non-VA substance-abuse services. Unlike prior studies, however, predisposing factors (eg, age, race, marital status, and income) were not associated with service use.
This study could not determine why veterans underutilized substance-abuse services, even those available locally to them in Fort Worth. One possible barrier to care is that the services are designed or delivered in a manner that does not engage these veterans (eg, expectations regarding abstinence or service involvement). Another barrier could be that referral pathways between VA outpatient medical and psychiatric service providers and VA substance-related services are not sufficiently facilitative. Future investigations could build upon the findings of this study by collecting data that could help assess these potential barriers.
The data from this study suggest 3 opportunities to improve the utilization of services most needed by this population. The first opportunity would be to accurately differentiate between substance abuse and psychiatric problems in clinical assessment and identify the most appropriate type of care. Another opportunity, linked closely to the first, would be to facilitate more effective and efficient referral pathways among VA service sectors, especially from medical and psychiatric services to substance-abuse services. Another strategy to improve referral pathways would be for VA service networks to systematically examine local service systems for factors or processes that may disrupt integrated care and implement program improvements.28 For homeless veterans navigating an inherently complex VA health care system, peer-to-peer and patient navigator programs have helped improve service efficiency and service outcomes.29 The third opportunity to improve utilization of services would be to ensure geographic availability and accessibility by strategic placement of these services.
The results from this study, while informative, point directly to needed areas for further inquiry to inform public health response. Although the low-demand shelter users are a particularly challenging subgroup of veterans experiencing chronic homelessness, other equally challenging populations warrant additional study. For example, veterans outside of both VA and community services (eg, unsheltered populations) are likely to require different approaches to engage in appropriate services. Additionally, changes to the homeless policy implemented in the period after this sample was recruited suggest the need to revisit the service-using behaviors of this population. Finally, interventions developed as part of the national response need to be assessed for their ability to engage these difficult-to-reach veterans.
Acknowledgements
This study was funded by a U.S. Department of Veterans Affairs Office of Academic Affiliations Pre-Doctoral Social Work Research Fellowship award.
1. U.S. Department of Veterans Affairs. Homeless veterans: VA is working to end homelessness among veterans. U.S. Department of Veterans Affairs Website. www.va.gov/homeless/about_the_initiative.asp#one. Updated January 26, 2016. Accessed February 16, 2016.
2. Henry M, Cortes A, Morris S, Abt Associates; U. S. Department of Housing and Urban Development Office of Community Planning and Development. The 2013 Annual Homeless Assessment Report (AHAR) to Congress: Part 1 Point-in-Time Estimates of Homelessness. HUD Exchange Website. https://www.hudexchange.info/resources/documents/ahar-2013-part1.pdf. Published October 2014. Accessed February 16, 2016.
3. U.S. Department of Veterans Affairs. Homeless Veterans: Housing Assistance. U.S. Department of Veterans Affairs Web site. http://www.va.gov/homeless/housing.asp. Updated November 5, 2015. Accessed February 16, 2016.
4. Austin EL, Pollio DE, Holmes S, et al. VA's expansion of supportive housing: successes and challenges on the path to Housing First. Psychiatr Serv. 2014;65(5):641-647.
5. Tsai J, Kasprow WJ, Rosenheck RA. Alcohol and drug use disorders among homeless veterans: prevalence and association with supported housing outcomes. Addict Behav. 2014;39(2):455-460.
6. Wenzel SL, Bakhtiar L, Caskey NH, et al. Homeless veterans utilization of medical, psychiatric, and substance abuse services. Med Care. 1995;33(11):1132-1144.
7. McQuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental health illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255-264.
8. Tsai J, Mares AS, Rosenheck RA. Do homeless veterans have the same needs and outcomes as non-veterans? Mil Med. 2012;177(1):27-31.
9. Andersen RM. A behavioral model of families use of health services: Research Series No. 25. Chicago, IL: University of Chicago Center for Health Administrative Studies; 1968.
10. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10.
11. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
12. Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273-1302.
13. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
14. Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: a prospective analysis. J Health Care Poor Underserved. 2000;11(2):212-230.
15. Gamache G, Rosenheck RA, Tessler R. Factors predicting choice of provider among homeless veterans with mental illness. Psychiatr Serv. 2000;51(8):1024-1028.
16. Wenzel SL, Audrey Burnam, M, Koegel P, et al. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Med Care. 2001;39(11):1158-1169.
17. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
18. Solorio MR, Milburn NG, Andersen RM, Trifskin S, Rodríguez MA. Emotional distress and mental health service use among urban homeless adolescents. J Behav Health Serv Res. 2006;33(4):381-393.
19. Stein JA, Andersen RM, Robertson M, Gelberg L. Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Anderson Behavioral Model for Vulnerable Populations. Health Psychol. 2012;31(1):20-30.
20. Linton KF, Shafer MS. Factors associated with the health service use of unsheltered, chronically homeless adults. Soc Work Public Health. 2013;29(1):73-80.
21. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psych Serv. 2014;65(6):751-757.
22. U.S. Census Bureau. State & County Quick Facts: Fort Worth (city), Texas. U.S. Census Bureau Website. http://quickfacts.census.gov/qfd/states/48/4827000.html. Revised December 2, 2015. Accessed February 17, 2016.
23. Tarrant County Homeless Coalition. 2014 point in time count results. Tarrant County Homeless Coalition Website. http://www.ahomewithhope.org/staff/local-data-research/2014-homeless-count/. Accessed February 16, 2016.
24. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The Homeless Supplement to the Diagnostic Interview Schedule: test-retest analyses. Int J Method Psychiatr Res. 2004;13(3):184-191.
25. Iqbal SU, Rogers W, Selim A, et al. The Veterans RAND 12 Item Health Survey (VR-12): What it is and how it is Used. Washington, DC: Veterans Health Administration; 2009.
26. Fischer J, Corcoran K, eds. Measures for Clinical Practice and Research: A Sourcebook. 4th ed. New York, NY: Oxford University Press; 2013.
27. Selim AJ, Rogers W, Fleishman JA, Qian SX, Finke BG, Rothendler JA, Kazis LE. Updated U.S. population standard for the Veterans RAND 12-Item Health Survey (VR-12). Qual Life Res. 2009;18(1):43-52.
28. Blue-Howells J, McQuire J, Nakashima J. Co-location of health care services for homeless veterans: a case study of innovation in program implementation. Soc Work Health Care. 2008;47(3):219-231.
29. Piette JD, Holtz B, Beard AJ, et al; Ann Arbor PACT Steering Committee. Improving chronic illness care for veterans within the framework of the Patient-Centered Medical Home: experiences from the Ann Arbor Patient-Aligned Care Team Laboratory. Transl Behav Med. 2011;1(4):615-623.
1. U.S. Department of Veterans Affairs. Homeless veterans: VA is working to end homelessness among veterans. U.S. Department of Veterans Affairs Website. www.va.gov/homeless/about_the_initiative.asp#one. Updated January 26, 2016. Accessed February 16, 2016.
2. Henry M, Cortes A, Morris S, Abt Associates; U. S. Department of Housing and Urban Development Office of Community Planning and Development. The 2013 Annual Homeless Assessment Report (AHAR) to Congress: Part 1 Point-in-Time Estimates of Homelessness. HUD Exchange Website. https://www.hudexchange.info/resources/documents/ahar-2013-part1.pdf. Published October 2014. Accessed February 16, 2016.
3. U.S. Department of Veterans Affairs. Homeless Veterans: Housing Assistance. U.S. Department of Veterans Affairs Web site. http://www.va.gov/homeless/housing.asp. Updated November 5, 2015. Accessed February 16, 2016.
4. Austin EL, Pollio DE, Holmes S, et al. VA's expansion of supportive housing: successes and challenges on the path to Housing First. Psychiatr Serv. 2014;65(5):641-647.
5. Tsai J, Kasprow WJ, Rosenheck RA. Alcohol and drug use disorders among homeless veterans: prevalence and association with supported housing outcomes. Addict Behav. 2014;39(2):455-460.
6. Wenzel SL, Bakhtiar L, Caskey NH, et al. Homeless veterans utilization of medical, psychiatric, and substance abuse services. Med Care. 1995;33(11):1132-1144.
7. McQuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental health illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255-264.
8. Tsai J, Mares AS, Rosenheck RA. Do homeless veterans have the same needs and outcomes as non-veterans? Mil Med. 2012;177(1):27-31.
9. Andersen RM. A behavioral model of families use of health services: Research Series No. 25. Chicago, IL: University of Chicago Center for Health Administrative Studies; 1968.
10. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10.
11. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
12. Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273-1302.
13. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
14. Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: a prospective analysis. J Health Care Poor Underserved. 2000;11(2):212-230.
15. Gamache G, Rosenheck RA, Tessler R. Factors predicting choice of provider among homeless veterans with mental illness. Psychiatr Serv. 2000;51(8):1024-1028.
16. Wenzel SL, Audrey Burnam, M, Koegel P, et al. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Med Care. 2001;39(11):1158-1169.
17. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
18. Solorio MR, Milburn NG, Andersen RM, Trifskin S, Rodríguez MA. Emotional distress and mental health service use among urban homeless adolescents. J Behav Health Serv Res. 2006;33(4):381-393.
19. Stein JA, Andersen RM, Robertson M, Gelberg L. Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Anderson Behavioral Model for Vulnerable Populations. Health Psychol. 2012;31(1):20-30.
20. Linton KF, Shafer MS. Factors associated with the health service use of unsheltered, chronically homeless adults. Soc Work Public Health. 2013;29(1):73-80.
21. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psych Serv. 2014;65(6):751-757.
22. U.S. Census Bureau. State & County Quick Facts: Fort Worth (city), Texas. U.S. Census Bureau Website. http://quickfacts.census.gov/qfd/states/48/4827000.html. Revised December 2, 2015. Accessed February 17, 2016.
23. Tarrant County Homeless Coalition. 2014 point in time count results. Tarrant County Homeless Coalition Website. http://www.ahomewithhope.org/staff/local-data-research/2014-homeless-count/. Accessed February 16, 2016.
24. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The Homeless Supplement to the Diagnostic Interview Schedule: test-retest analyses. Int J Method Psychiatr Res. 2004;13(3):184-191.
25. Iqbal SU, Rogers W, Selim A, et al. The Veterans RAND 12 Item Health Survey (VR-12): What it is and how it is Used. Washington, DC: Veterans Health Administration; 2009.
26. Fischer J, Corcoran K, eds. Measures for Clinical Practice and Research: A Sourcebook. 4th ed. New York, NY: Oxford University Press; 2013.
27. Selim AJ, Rogers W, Fleishman JA, Qian SX, Finke BG, Rothendler JA, Kazis LE. Updated U.S. population standard for the Veterans RAND 12-Item Health Survey (VR-12). Qual Life Res. 2009;18(1):43-52.
28. Blue-Howells J, McQuire J, Nakashima J. Co-location of health care services for homeless veterans: a case study of innovation in program implementation. Soc Work Health Care. 2008;47(3):219-231.
29. Piette JD, Holtz B, Beard AJ, et al; Ann Arbor PACT Steering Committee. Improving chronic illness care for veterans within the framework of the Patient-Centered Medical Home: experiences from the Ann Arbor Patient-Aligned Care Team Laboratory. Transl Behav Med. 2011;1(4):615-623.