User login
Clinical presentation and imaging of bone and soft-tissue sarcomas
Sarcomas are rare neoplasms arising from connective tissue elements of the body. Approximately 80% arise in soft tissue, while the remainder originate in bone.1 Soft-tissue sarcomas are tumors of the mesenchymal system, and about half develop in the extremities. Bone sarcomas are characterized by their location in bone and sometimes produce osteoid, or immature bone.
The most common types of soft-tissue sarcomas are malignant fibrous histiocytoma (although this term has lost favor with some pathologists) and liposarcoma.
The most common types of bone sarcomas are osteosarcoma (a sarcoma that makes osteoid or bone), Ewing sarcoma (composed of small round blue cells with a characteristic chromosomal translocation), and chondrosarcoma (a sarcoma that makes chondroid tissue, or cartilage).
EPIDEMIOLOGY AND PRIMARY BODY SITES
Approximately 10,600 new cases of soft-tissue sarcoma and 2,570 new cases of bone sarcoma were estimated to have been diagnosed in the United States in 2009.2,3 For perspective, the annual incidence of soft-tissue sarcoma is approximately 5.5% that of breast cancer and approximately 5% that of lung cancer.3
Most sarcomas develop in the lower extremities, although the age groups at greatest risk vary among sarcoma types.4
Soft-tissue sarcomas develop most commonly in the thigh and occur primarily in adults.2
Osteosarcomas are the most common bone sarcoma and develop most frequently in 10- to 20-year-olds; their most common location is the distal femur.5–8 Metastatic osteosarcoma is found in approximately 20% of patients at the time of osteosarcoma diagnosis. Osteosarcomas mainly spread hematogenously, and the lungs are the most common initial site of metastases, being affected in up to 90% of patients with metastatic disease.9
Ewing sarcomas develop most often in the long bones of the extremities or bones of the pelvis. The large majority of cases develop in patients aged 10 to 15 years. 5–8
Chondrosarcomas represent approximately 20% of all bone sarcomas and primarily affect older adults, with a peak incidence in the sixth decade of life.10
OVERVIEW OF PRESENTATION AND EVALUATION
Presentation is highly variable
The clinical presentation of patients with bone or soft-tissue sarcoma is highly variable. Patients often present with a mass, typically one that is increasing in size. In general, bone sarcomas are painful and soft-tissue sarcomas are not, but there are exceptions to this general rule. Constitutional symptoms are rare in patients with bone or soft-tissue sarcomas, but symptoms such as fever, malaise, and weight loss can be seen, especially in patients with Ewing sarcoma.11
Delayed presentation and diagnosis are common
Particularly when a sarcoma is painless, patients sometimes do not seek medical attention until a suspicious mass becomes quite large. Certain tumors, such as synovial sarcoma, a high-grade soft-tissue sarcoma often seen in young adults, may present as a slowly growing or stable-appearing mass over several years. In one study of 33 children with synovial sarcoma, the mean duration of symptoms was 98 weeks (range, 2–364), the mean patient delay before a doctor was seen was 43 weeks (0–156), the mean doctor delay before a correct diagnosis was made was 50 weeks (0–362), and the mean number of doctors seen before referral was 3 (1–6).12 For nearly half the patients in this study (15), the diagnosis was obtained only after unplanned excision, meaning that the surgeon did not expect a malignancy at the time of biopsy. Because delayed presentation is not uncommon in cases of bone or soft-tissue sarcoma, every patient with a mass with indeterminate imaging findings should be referred to or reviewed by an orthopedic or musculoskeletal oncologist.
Biopsy is gold standard for diagnosis
A comprehensive medical history and physical examination are essential at the initial presentation of patients with masses and/or pain suggestive of bone or soft-tissue sarcoma. Sarcoma simulators such as hematoma, metastatic disease, or infection can sometimes be ruled out by careful clinical examination, laboratory work-up, and appropriate imaging, but the gold standard for diagnosis is a biopsy. Moreover, an index of suspicion is required to rule out primary malignancy in any soft-tissue or bone lesion, and this index of suspicion will allow for referral or appropriate selection of the site for biopsy.
Biopsy considerations, as well as further detail on clinical presentation, are provided in the second and third articles in this supplement, which focus, respectively, on bone sarcoma and soft-tissue sarcoma. The remainder of this article reviews the use of imaging for the evaluation of suspected sarcomas, as imaging findings typically prompt or guide biopsy of a suspicious mass. Choosing the right imaging modality is critical to the diagnosis and management of patients with suspected sarcoma.
CONVENTIONAL IMAGING MODALITIES
Despite their utility for evaluating osseous lesions, radiographs have limited to no value in the evaluation of soft-tissue sarcomas but can demonstrate matrix mineralization and erosion or destruction of adjacent bone.
Angiography. In the past, angiography was frequently used to assess the vascularity of sarcomas preoperatively. Diagnostic angiography has been replaced by conventional MRI and magnetic resonance angiography, but some vascular sarcomas may require presurgical embolization to prevent excessive bleeding during surgery.
Radionuclide bone scans have long been a reliable tool for detecting multifocal or disseminated osseous lesions and remain the mainstay for evaluation of osseous metastases. They also are helpful in identifying skip lesions of osteosarcoma (ie, smaller discrete foci of osteosarcoma occurring in the same bone or on the opposing side of a joint).14 Advantages of this modality include whole-body scanning and low radiation at relatively low cost. Radionuclide bone scans demonstrate areas of bony repair and thus could be negative in purely lytic/destructive processes such as renal cell carcinoma metastases and multiple myeloma.
Chest radiographs are typically obtained in the initial stages of patient evaluation and are helpful in demonstrating large nodules or masses resulting from metastatic disease. In a patient with known sarcoma, a negative or equivocal chest radiograph should be followed by chest CT to definitively assess for metastasis.
CROSS-SECTIONAL IMAGING WITH MRI AND CT
MRI preferred for evaluation of most masses
MRI is the examination of choice in the evaluation of soft-tissue masses in light of its superior contrast resolution and ability to demonstrate subtle changes in soft tissues.
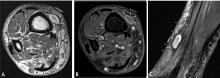
Predicting the histology of most soft-tissue masses is difficult, with the exception of some benign vascular lesions (eg, hemangioma), ganglia, neurogenic lesions, and well-differentiated lipomatous lesions. Aggressive features of a soft-tissue neoplasm include size greater than 5 cm,15 deep location, and absence of central enhancement, which is suggestive of necrosis (Figure 1). Yet one third of soft-tissue sarcomas are either superficial or smaller than 5 cm, which highlights the relative nonspecificity of these features.15
MRI is also the preferred modality in the evaluation of the majority of bone sarcomas, given its ability to accurately define the extent of marrow changes and soft-tissue involvement. MRI should be performed prior to a biopsy to prevent misinterpretation of biopsy-related signal changes in the surrounding tissues, which may negate the value of MRI in sarcoma staging.
Several distinct roles for CT
Chest CT should be obtained in all cases of known malignant neoplasms to evaluate for pulmonary nodules, masses, and lymphadenopathy. Despite the recent advances in MRI, CT remains the imaging modality of choice to evaluate the retroperitoneum, abdomen, and pelvis for masses, lymphadenopathy, or other signs of metastatic disease.
Post-treatment monitoring for recurrence
ULTRASONOGRAPHY
Ultrasonography has a limited role in the initial diagnosis and follow-up of musculoskeletal tumors. Its main advantages are a lack of ionizing radiation and dynamic imaging capabilities. Doppler ultrasonography allows direct visualization of tumor vascularity, which may be important for diagnosis and presurgical planning. Unfortunately, bone lesions cannot be evaluated with ultrasonography, owing to the inability of sound waves to penetrate the bony cortex. Poor sound wave penetration may prevent visualization of deep-seated lesions, such as retroperitoneal sarcomas.
Ultrasonography is best used for differentiating solid masses from cystic structures and can provide image guidance in solid tumor biopsy and cyst aspiration. It also may play a role in detecting suspected tumor recurrence in patients in whom artifact from implanted hardware precludes cross-sectional imaging, and it can be reliably used for following up unequivocal soft-tissue masses such as ganglia near joints.
POSITRON EMISSION TOMOGRAPHY
IMAGING-GUIDED INTERVENTIONS
Percutaneous imaging-guided procedures have increasingly replaced open surgical biopsies for bone and soft-tissue tumors. CT guidance is commonly used for percutaneous biopsy, whereas ultrasonographic guidance is sometimes used for superficial soft-tissue lesions. Although the shortest and most direct approach is desirable, this may not be possible in all cases due to the presence of nearby vital structures or the risk of contamination. Seeding of malignant cells along the biopsy tract is a well-known possible complication of image-guided biopsies, and en bloc resection of the needle tract is typically performed at the definitive surgery.
Knowledge of compartmental anatomy is paramount in planning the approach for these biopsies, and consultation with the referring orthopedic surgeon is recommended for optimal management. Expert histopathological interpretation of bone and soft-tissue specimens is essential for the efficacy and high success rates of percutaneous imaging-guided biopsies. Such expertise is integral to the broader interdisciplinary collaboration that is needed to arrive at the most plausible diagnosis, especially in the setting of uncommon or atypical neoplasms.
Currently, MRI-guided interventions are in the initial stage of evolution and could provide valuable guidance for subtle marrow or soft-tissue lesions visible on MRI but not well seen on CT.22 In the future, MRI could play an increasingly important role in imaging-guided procedures because of its lack of ionizing radiation and its ability to demonstrate subtle soft-tissue and bone marrow changes. Imaging-guided therapeutics are growing in their applications in musculoskeletal oncology. CT-guided radiofrequency ablation and cryoablation have been used in the treatment of a variety of tumors23 as well as in the palliation of metastatic bone pain.24
SUMMARY AND CONCLUSION
Bone and soft-tissue sarcomas are rare neoplasms with variable clinical presentations. A high index of suspicion is required for any unexplained mass with indeterminate imaging findings. Recent advances in imaging technology, including cross-sectional MRI and CT, have significantly refined the diagnosis and management of bone and soft-tissue sarcomas. When faced with a possible sarcoma, the clinician’s selection of imaging modalities has a direct impact on diagnosis, staging, and patient management.
- American Cancer Society. Cancer facts & figures 2009. Atlanta, GA: American Cancer Society; 2009.
- Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weiss’ Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin 2009; 59:225–249.
- Simon MA, Springfield DS, eds. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Dahlin DC, Unni KK. Bone Tumors: General Aspects and Data on 8,542 Cases. 4th ed. Springfield, IL: Thomas; 1986.
- Unni KK. Bone Tumors. New York, NY: Churchill Livingstone; 1988.
- Unni KK. Atlas of Bone Pathology. New York, NY: Chapman & Hall; 1996:1 computer optical disc.
- Unni KK, Dahlin DC. Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases. 5th ed. Philadelphia, PA: Lippincott-Raven; 1996.
- Kaste SC, Pratt CB, Cain AM, Jones-Wallace DJ, Rao BN. Metastases detected at the time of diagnosis of primary pediatric extremity osteosarcoma at diagnosis: imaging features. Cancer 1999; 86:1602–1608.
- Healey JH, Lane JM. Chondrosarcoma. Clin Orthop Relat Res 1986; 204:119–129.
- Kissane JM, Askin FB, Foulkes M, Stratton LB, Shirley SF. Ewing’s sarcoma of bone: clinicopathologic aspects of 303 cases from the Intergroup Ewing’s Sarcoma Study. Hum Pathol 1983; 14:773–779.
- Chotel F, Unnithan A, Chandrasekar CR, et al. Variability in the presentation of synovial sarcoma in children: a plea for greater awareness. J Bone Joint Surg Br 2008; 90:1090–1096.
- Miller TT. Bone tumors and tumorlike conditions: analysis with conventional radiography. Radiology 2008; 246:662–674.
- Richardson ML, Gillespy T. Magnetic resonance imaging. In: Kricun ME, ed. Imaging of Bone Tumors. Philadelphia, PA: WB Saunders; 1993:365.
- Fisher C. Soft tissue sarcomas: diagnosis, classification and prognostic factors. Br J Plast Surg 1996; 49:27–33.
- White LM, Wunder JS, Bell RS, et al. Histologic assessment of peritumoral edema in soft tissue sarcoma. Int J Radiat Oncol Biol Phys 2005; 61:1439–1445.
- White LM, Buckwalter KA. Technical considerations: CT and MR imaging in the postoperative orthopedic patient. Semin Musculoskelet Radiol 2002; 6:5–17.
- Blodgett TM, Casagranda B, Townsend DW, Meltzer CC. Issues, controversies, and clinical utility of combined PET/CT imaging: what is the interpreting physician facing? AJR Am J Roentgenol 2005; 184(suppl 5):S138–S145.
- Shin DS, Shon OJ, Han DS, Choi JH, Chun KA, Cho IH. The clinical efficacy of 18F-FDG-PET/CT in benign and malignant musculoskeletal tumors. Ann Nucl Med 2008; 22:603–609.
- Benz MR, Czernin J, Allen-Auerbach MS, et al. FDG-PET/CT imaging predicts histopathologic treatment responses after the initial cycle of neoadjuvant chemotherapy in high-grade soft-tissue sarcomas. Clin Cancer Res 2009; 15:2856–2863.
- Aoki J, Watanabe H, Shinozaki T, et al. FDG-PET for preoperative differential diagnosis between benign and malignant soft tissue masses. Skeletal Radiol 2003; 32:133–138.
- Blanco Sequeiros R, Klemola R, Ojala R, et al. MRI-guided trephine biopsy and fine-needle aspiration in the diagnosis of bone lesions in low-field (0.23 T) MRI system using optical instrument tracking. Eur Radiol 2002; 12:830–835.
- Rosenthal DI. Radiofrequency treatment. Orthop Clin North Am 2006; 37:475–484.
- Callstrom MR, Charboneau JW. Image-guided palliation of painful metastases using percutaneous ablation. Tech Vasc Interv Radiol 2007; 10:120–131.
Sarcomas are rare neoplasms arising from connective tissue elements of the body. Approximately 80% arise in soft tissue, while the remainder originate in bone.1 Soft-tissue sarcomas are tumors of the mesenchymal system, and about half develop in the extremities. Bone sarcomas are characterized by their location in bone and sometimes produce osteoid, or immature bone.
The most common types of soft-tissue sarcomas are malignant fibrous histiocytoma (although this term has lost favor with some pathologists) and liposarcoma.
The most common types of bone sarcomas are osteosarcoma (a sarcoma that makes osteoid or bone), Ewing sarcoma (composed of small round blue cells with a characteristic chromosomal translocation), and chondrosarcoma (a sarcoma that makes chondroid tissue, or cartilage).
EPIDEMIOLOGY AND PRIMARY BODY SITES
Approximately 10,600 new cases of soft-tissue sarcoma and 2,570 new cases of bone sarcoma were estimated to have been diagnosed in the United States in 2009.2,3 For perspective, the annual incidence of soft-tissue sarcoma is approximately 5.5% that of breast cancer and approximately 5% that of lung cancer.3
Most sarcomas develop in the lower extremities, although the age groups at greatest risk vary among sarcoma types.4
Soft-tissue sarcomas develop most commonly in the thigh and occur primarily in adults.2
Osteosarcomas are the most common bone sarcoma and develop most frequently in 10- to 20-year-olds; their most common location is the distal femur.5–8 Metastatic osteosarcoma is found in approximately 20% of patients at the time of osteosarcoma diagnosis. Osteosarcomas mainly spread hematogenously, and the lungs are the most common initial site of metastases, being affected in up to 90% of patients with metastatic disease.9
Ewing sarcomas develop most often in the long bones of the extremities or bones of the pelvis. The large majority of cases develop in patients aged 10 to 15 years. 5–8
Chondrosarcomas represent approximately 20% of all bone sarcomas and primarily affect older adults, with a peak incidence in the sixth decade of life.10
OVERVIEW OF PRESENTATION AND EVALUATION
Presentation is highly variable
The clinical presentation of patients with bone or soft-tissue sarcoma is highly variable. Patients often present with a mass, typically one that is increasing in size. In general, bone sarcomas are painful and soft-tissue sarcomas are not, but there are exceptions to this general rule. Constitutional symptoms are rare in patients with bone or soft-tissue sarcomas, but symptoms such as fever, malaise, and weight loss can be seen, especially in patients with Ewing sarcoma.11
Delayed presentation and diagnosis are common
Particularly when a sarcoma is painless, patients sometimes do not seek medical attention until a suspicious mass becomes quite large. Certain tumors, such as synovial sarcoma, a high-grade soft-tissue sarcoma often seen in young adults, may present as a slowly growing or stable-appearing mass over several years. In one study of 33 children with synovial sarcoma, the mean duration of symptoms was 98 weeks (range, 2–364), the mean patient delay before a doctor was seen was 43 weeks (0–156), the mean doctor delay before a correct diagnosis was made was 50 weeks (0–362), and the mean number of doctors seen before referral was 3 (1–6).12 For nearly half the patients in this study (15), the diagnosis was obtained only after unplanned excision, meaning that the surgeon did not expect a malignancy at the time of biopsy. Because delayed presentation is not uncommon in cases of bone or soft-tissue sarcoma, every patient with a mass with indeterminate imaging findings should be referred to or reviewed by an orthopedic or musculoskeletal oncologist.
Biopsy is gold standard for diagnosis
A comprehensive medical history and physical examination are essential at the initial presentation of patients with masses and/or pain suggestive of bone or soft-tissue sarcoma. Sarcoma simulators such as hematoma, metastatic disease, or infection can sometimes be ruled out by careful clinical examination, laboratory work-up, and appropriate imaging, but the gold standard for diagnosis is a biopsy. Moreover, an index of suspicion is required to rule out primary malignancy in any soft-tissue or bone lesion, and this index of suspicion will allow for referral or appropriate selection of the site for biopsy.
Biopsy considerations, as well as further detail on clinical presentation, are provided in the second and third articles in this supplement, which focus, respectively, on bone sarcoma and soft-tissue sarcoma. The remainder of this article reviews the use of imaging for the evaluation of suspected sarcomas, as imaging findings typically prompt or guide biopsy of a suspicious mass. Choosing the right imaging modality is critical to the diagnosis and management of patients with suspected sarcoma.
CONVENTIONAL IMAGING MODALITIES
Despite their utility for evaluating osseous lesions, radiographs have limited to no value in the evaluation of soft-tissue sarcomas but can demonstrate matrix mineralization and erosion or destruction of adjacent bone.
Angiography. In the past, angiography was frequently used to assess the vascularity of sarcomas preoperatively. Diagnostic angiography has been replaced by conventional MRI and magnetic resonance angiography, but some vascular sarcomas may require presurgical embolization to prevent excessive bleeding during surgery.
Radionuclide bone scans have long been a reliable tool for detecting multifocal or disseminated osseous lesions and remain the mainstay for evaluation of osseous metastases. They also are helpful in identifying skip lesions of osteosarcoma (ie, smaller discrete foci of osteosarcoma occurring in the same bone or on the opposing side of a joint).14 Advantages of this modality include whole-body scanning and low radiation at relatively low cost. Radionuclide bone scans demonstrate areas of bony repair and thus could be negative in purely lytic/destructive processes such as renal cell carcinoma metastases and multiple myeloma.
Chest radiographs are typically obtained in the initial stages of patient evaluation and are helpful in demonstrating large nodules or masses resulting from metastatic disease. In a patient with known sarcoma, a negative or equivocal chest radiograph should be followed by chest CT to definitively assess for metastasis.
CROSS-SECTIONAL IMAGING WITH MRI AND CT
MRI preferred for evaluation of most masses
MRI is the examination of choice in the evaluation of soft-tissue masses in light of its superior contrast resolution and ability to demonstrate subtle changes in soft tissues.
Predicting the histology of most soft-tissue masses is difficult, with the exception of some benign vascular lesions (eg, hemangioma), ganglia, neurogenic lesions, and well-differentiated lipomatous lesions. Aggressive features of a soft-tissue neoplasm include size greater than 5 cm,15 deep location, and absence of central enhancement, which is suggestive of necrosis (Figure 1). Yet one third of soft-tissue sarcomas are either superficial or smaller than 5 cm, which highlights the relative nonspecificity of these features.15
MRI is also the preferred modality in the evaluation of the majority of bone sarcomas, given its ability to accurately define the extent of marrow changes and soft-tissue involvement. MRI should be performed prior to a biopsy to prevent misinterpretation of biopsy-related signal changes in the surrounding tissues, which may negate the value of MRI in sarcoma staging.
Several distinct roles for CT
Chest CT should be obtained in all cases of known malignant neoplasms to evaluate for pulmonary nodules, masses, and lymphadenopathy. Despite the recent advances in MRI, CT remains the imaging modality of choice to evaluate the retroperitoneum, abdomen, and pelvis for masses, lymphadenopathy, or other signs of metastatic disease.
Post-treatment monitoring for recurrence
ULTRASONOGRAPHY
Ultrasonography has a limited role in the initial diagnosis and follow-up of musculoskeletal tumors. Its main advantages are a lack of ionizing radiation and dynamic imaging capabilities. Doppler ultrasonography allows direct visualization of tumor vascularity, which may be important for diagnosis and presurgical planning. Unfortunately, bone lesions cannot be evaluated with ultrasonography, owing to the inability of sound waves to penetrate the bony cortex. Poor sound wave penetration may prevent visualization of deep-seated lesions, such as retroperitoneal sarcomas.
Ultrasonography is best used for differentiating solid masses from cystic structures and can provide image guidance in solid tumor biopsy and cyst aspiration. It also may play a role in detecting suspected tumor recurrence in patients in whom artifact from implanted hardware precludes cross-sectional imaging, and it can be reliably used for following up unequivocal soft-tissue masses such as ganglia near joints.
POSITRON EMISSION TOMOGRAPHY
IMAGING-GUIDED INTERVENTIONS
Percutaneous imaging-guided procedures have increasingly replaced open surgical biopsies for bone and soft-tissue tumors. CT guidance is commonly used for percutaneous biopsy, whereas ultrasonographic guidance is sometimes used for superficial soft-tissue lesions. Although the shortest and most direct approach is desirable, this may not be possible in all cases due to the presence of nearby vital structures or the risk of contamination. Seeding of malignant cells along the biopsy tract is a well-known possible complication of image-guided biopsies, and en bloc resection of the needle tract is typically performed at the definitive surgery.
Knowledge of compartmental anatomy is paramount in planning the approach for these biopsies, and consultation with the referring orthopedic surgeon is recommended for optimal management. Expert histopathological interpretation of bone and soft-tissue specimens is essential for the efficacy and high success rates of percutaneous imaging-guided biopsies. Such expertise is integral to the broader interdisciplinary collaboration that is needed to arrive at the most plausible diagnosis, especially in the setting of uncommon or atypical neoplasms.
Currently, MRI-guided interventions are in the initial stage of evolution and could provide valuable guidance for subtle marrow or soft-tissue lesions visible on MRI but not well seen on CT.22 In the future, MRI could play an increasingly important role in imaging-guided procedures because of its lack of ionizing radiation and its ability to demonstrate subtle soft-tissue and bone marrow changes. Imaging-guided therapeutics are growing in their applications in musculoskeletal oncology. CT-guided radiofrequency ablation and cryoablation have been used in the treatment of a variety of tumors23 as well as in the palliation of metastatic bone pain.24
SUMMARY AND CONCLUSION
Bone and soft-tissue sarcomas are rare neoplasms with variable clinical presentations. A high index of suspicion is required for any unexplained mass with indeterminate imaging findings. Recent advances in imaging technology, including cross-sectional MRI and CT, have significantly refined the diagnosis and management of bone and soft-tissue sarcomas. When faced with a possible sarcoma, the clinician’s selection of imaging modalities has a direct impact on diagnosis, staging, and patient management.
Sarcomas are rare neoplasms arising from connective tissue elements of the body. Approximately 80% arise in soft tissue, while the remainder originate in bone.1 Soft-tissue sarcomas are tumors of the mesenchymal system, and about half develop in the extremities. Bone sarcomas are characterized by their location in bone and sometimes produce osteoid, or immature bone.
The most common types of soft-tissue sarcomas are malignant fibrous histiocytoma (although this term has lost favor with some pathologists) and liposarcoma.
The most common types of bone sarcomas are osteosarcoma (a sarcoma that makes osteoid or bone), Ewing sarcoma (composed of small round blue cells with a characteristic chromosomal translocation), and chondrosarcoma (a sarcoma that makes chondroid tissue, or cartilage).
EPIDEMIOLOGY AND PRIMARY BODY SITES
Approximately 10,600 new cases of soft-tissue sarcoma and 2,570 new cases of bone sarcoma were estimated to have been diagnosed in the United States in 2009.2,3 For perspective, the annual incidence of soft-tissue sarcoma is approximately 5.5% that of breast cancer and approximately 5% that of lung cancer.3
Most sarcomas develop in the lower extremities, although the age groups at greatest risk vary among sarcoma types.4
Soft-tissue sarcomas develop most commonly in the thigh and occur primarily in adults.2
Osteosarcomas are the most common bone sarcoma and develop most frequently in 10- to 20-year-olds; their most common location is the distal femur.5–8 Metastatic osteosarcoma is found in approximately 20% of patients at the time of osteosarcoma diagnosis. Osteosarcomas mainly spread hematogenously, and the lungs are the most common initial site of metastases, being affected in up to 90% of patients with metastatic disease.9
Ewing sarcomas develop most often in the long bones of the extremities or bones of the pelvis. The large majority of cases develop in patients aged 10 to 15 years. 5–8
Chondrosarcomas represent approximately 20% of all bone sarcomas and primarily affect older adults, with a peak incidence in the sixth decade of life.10
OVERVIEW OF PRESENTATION AND EVALUATION
Presentation is highly variable
The clinical presentation of patients with bone or soft-tissue sarcoma is highly variable. Patients often present with a mass, typically one that is increasing in size. In general, bone sarcomas are painful and soft-tissue sarcomas are not, but there are exceptions to this general rule. Constitutional symptoms are rare in patients with bone or soft-tissue sarcomas, but symptoms such as fever, malaise, and weight loss can be seen, especially in patients with Ewing sarcoma.11
Delayed presentation and diagnosis are common
Particularly when a sarcoma is painless, patients sometimes do not seek medical attention until a suspicious mass becomes quite large. Certain tumors, such as synovial sarcoma, a high-grade soft-tissue sarcoma often seen in young adults, may present as a slowly growing or stable-appearing mass over several years. In one study of 33 children with synovial sarcoma, the mean duration of symptoms was 98 weeks (range, 2–364), the mean patient delay before a doctor was seen was 43 weeks (0–156), the mean doctor delay before a correct diagnosis was made was 50 weeks (0–362), and the mean number of doctors seen before referral was 3 (1–6).12 For nearly half the patients in this study (15), the diagnosis was obtained only after unplanned excision, meaning that the surgeon did not expect a malignancy at the time of biopsy. Because delayed presentation is not uncommon in cases of bone or soft-tissue sarcoma, every patient with a mass with indeterminate imaging findings should be referred to or reviewed by an orthopedic or musculoskeletal oncologist.
Biopsy is gold standard for diagnosis
A comprehensive medical history and physical examination are essential at the initial presentation of patients with masses and/or pain suggestive of bone or soft-tissue sarcoma. Sarcoma simulators such as hematoma, metastatic disease, or infection can sometimes be ruled out by careful clinical examination, laboratory work-up, and appropriate imaging, but the gold standard for diagnosis is a biopsy. Moreover, an index of suspicion is required to rule out primary malignancy in any soft-tissue or bone lesion, and this index of suspicion will allow for referral or appropriate selection of the site for biopsy.
Biopsy considerations, as well as further detail on clinical presentation, are provided in the second and third articles in this supplement, which focus, respectively, on bone sarcoma and soft-tissue sarcoma. The remainder of this article reviews the use of imaging for the evaluation of suspected sarcomas, as imaging findings typically prompt or guide biopsy of a suspicious mass. Choosing the right imaging modality is critical to the diagnosis and management of patients with suspected sarcoma.
CONVENTIONAL IMAGING MODALITIES
Despite their utility for evaluating osseous lesions, radiographs have limited to no value in the evaluation of soft-tissue sarcomas but can demonstrate matrix mineralization and erosion or destruction of adjacent bone.
Angiography. In the past, angiography was frequently used to assess the vascularity of sarcomas preoperatively. Diagnostic angiography has been replaced by conventional MRI and magnetic resonance angiography, but some vascular sarcomas may require presurgical embolization to prevent excessive bleeding during surgery.
Radionuclide bone scans have long been a reliable tool for detecting multifocal or disseminated osseous lesions and remain the mainstay for evaluation of osseous metastases. They also are helpful in identifying skip lesions of osteosarcoma (ie, smaller discrete foci of osteosarcoma occurring in the same bone or on the opposing side of a joint).14 Advantages of this modality include whole-body scanning and low radiation at relatively low cost. Radionuclide bone scans demonstrate areas of bony repair and thus could be negative in purely lytic/destructive processes such as renal cell carcinoma metastases and multiple myeloma.
Chest radiographs are typically obtained in the initial stages of patient evaluation and are helpful in demonstrating large nodules or masses resulting from metastatic disease. In a patient with known sarcoma, a negative or equivocal chest radiograph should be followed by chest CT to definitively assess for metastasis.
CROSS-SECTIONAL IMAGING WITH MRI AND CT
MRI preferred for evaluation of most masses
MRI is the examination of choice in the evaluation of soft-tissue masses in light of its superior contrast resolution and ability to demonstrate subtle changes in soft tissues.
Predicting the histology of most soft-tissue masses is difficult, with the exception of some benign vascular lesions (eg, hemangioma), ganglia, neurogenic lesions, and well-differentiated lipomatous lesions. Aggressive features of a soft-tissue neoplasm include size greater than 5 cm,15 deep location, and absence of central enhancement, which is suggestive of necrosis (Figure 1). Yet one third of soft-tissue sarcomas are either superficial or smaller than 5 cm, which highlights the relative nonspecificity of these features.15
MRI is also the preferred modality in the evaluation of the majority of bone sarcomas, given its ability to accurately define the extent of marrow changes and soft-tissue involvement. MRI should be performed prior to a biopsy to prevent misinterpretation of biopsy-related signal changes in the surrounding tissues, which may negate the value of MRI in sarcoma staging.
Several distinct roles for CT
Chest CT should be obtained in all cases of known malignant neoplasms to evaluate for pulmonary nodules, masses, and lymphadenopathy. Despite the recent advances in MRI, CT remains the imaging modality of choice to evaluate the retroperitoneum, abdomen, and pelvis for masses, lymphadenopathy, or other signs of metastatic disease.
Post-treatment monitoring for recurrence
ULTRASONOGRAPHY
Ultrasonography has a limited role in the initial diagnosis and follow-up of musculoskeletal tumors. Its main advantages are a lack of ionizing radiation and dynamic imaging capabilities. Doppler ultrasonography allows direct visualization of tumor vascularity, which may be important for diagnosis and presurgical planning. Unfortunately, bone lesions cannot be evaluated with ultrasonography, owing to the inability of sound waves to penetrate the bony cortex. Poor sound wave penetration may prevent visualization of deep-seated lesions, such as retroperitoneal sarcomas.
Ultrasonography is best used for differentiating solid masses from cystic structures and can provide image guidance in solid tumor biopsy and cyst aspiration. It also may play a role in detecting suspected tumor recurrence in patients in whom artifact from implanted hardware precludes cross-sectional imaging, and it can be reliably used for following up unequivocal soft-tissue masses such as ganglia near joints.
POSITRON EMISSION TOMOGRAPHY
IMAGING-GUIDED INTERVENTIONS
Percutaneous imaging-guided procedures have increasingly replaced open surgical biopsies for bone and soft-tissue tumors. CT guidance is commonly used for percutaneous biopsy, whereas ultrasonographic guidance is sometimes used for superficial soft-tissue lesions. Although the shortest and most direct approach is desirable, this may not be possible in all cases due to the presence of nearby vital structures or the risk of contamination. Seeding of malignant cells along the biopsy tract is a well-known possible complication of image-guided biopsies, and en bloc resection of the needle tract is typically performed at the definitive surgery.
Knowledge of compartmental anatomy is paramount in planning the approach for these biopsies, and consultation with the referring orthopedic surgeon is recommended for optimal management. Expert histopathological interpretation of bone and soft-tissue specimens is essential for the efficacy and high success rates of percutaneous imaging-guided biopsies. Such expertise is integral to the broader interdisciplinary collaboration that is needed to arrive at the most plausible diagnosis, especially in the setting of uncommon or atypical neoplasms.
Currently, MRI-guided interventions are in the initial stage of evolution and could provide valuable guidance for subtle marrow or soft-tissue lesions visible on MRI but not well seen on CT.22 In the future, MRI could play an increasingly important role in imaging-guided procedures because of its lack of ionizing radiation and its ability to demonstrate subtle soft-tissue and bone marrow changes. Imaging-guided therapeutics are growing in their applications in musculoskeletal oncology. CT-guided radiofrequency ablation and cryoablation have been used in the treatment of a variety of tumors23 as well as in the palliation of metastatic bone pain.24
SUMMARY AND CONCLUSION
Bone and soft-tissue sarcomas are rare neoplasms with variable clinical presentations. A high index of suspicion is required for any unexplained mass with indeterminate imaging findings. Recent advances in imaging technology, including cross-sectional MRI and CT, have significantly refined the diagnosis and management of bone and soft-tissue sarcomas. When faced with a possible sarcoma, the clinician’s selection of imaging modalities has a direct impact on diagnosis, staging, and patient management.
- American Cancer Society. Cancer facts & figures 2009. Atlanta, GA: American Cancer Society; 2009.
- Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weiss’ Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin 2009; 59:225–249.
- Simon MA, Springfield DS, eds. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Dahlin DC, Unni KK. Bone Tumors: General Aspects and Data on 8,542 Cases. 4th ed. Springfield, IL: Thomas; 1986.
- Unni KK. Bone Tumors. New York, NY: Churchill Livingstone; 1988.
- Unni KK. Atlas of Bone Pathology. New York, NY: Chapman & Hall; 1996:1 computer optical disc.
- Unni KK, Dahlin DC. Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases. 5th ed. Philadelphia, PA: Lippincott-Raven; 1996.
- Kaste SC, Pratt CB, Cain AM, Jones-Wallace DJ, Rao BN. Metastases detected at the time of diagnosis of primary pediatric extremity osteosarcoma at diagnosis: imaging features. Cancer 1999; 86:1602–1608.
- Healey JH, Lane JM. Chondrosarcoma. Clin Orthop Relat Res 1986; 204:119–129.
- Kissane JM, Askin FB, Foulkes M, Stratton LB, Shirley SF. Ewing’s sarcoma of bone: clinicopathologic aspects of 303 cases from the Intergroup Ewing’s Sarcoma Study. Hum Pathol 1983; 14:773–779.
- Chotel F, Unnithan A, Chandrasekar CR, et al. Variability in the presentation of synovial sarcoma in children: a plea for greater awareness. J Bone Joint Surg Br 2008; 90:1090–1096.
- Miller TT. Bone tumors and tumorlike conditions: analysis with conventional radiography. Radiology 2008; 246:662–674.
- Richardson ML, Gillespy T. Magnetic resonance imaging. In: Kricun ME, ed. Imaging of Bone Tumors. Philadelphia, PA: WB Saunders; 1993:365.
- Fisher C. Soft tissue sarcomas: diagnosis, classification and prognostic factors. Br J Plast Surg 1996; 49:27–33.
- White LM, Wunder JS, Bell RS, et al. Histologic assessment of peritumoral edema in soft tissue sarcoma. Int J Radiat Oncol Biol Phys 2005; 61:1439–1445.
- White LM, Buckwalter KA. Technical considerations: CT and MR imaging in the postoperative orthopedic patient. Semin Musculoskelet Radiol 2002; 6:5–17.
- Blodgett TM, Casagranda B, Townsend DW, Meltzer CC. Issues, controversies, and clinical utility of combined PET/CT imaging: what is the interpreting physician facing? AJR Am J Roentgenol 2005; 184(suppl 5):S138–S145.
- Shin DS, Shon OJ, Han DS, Choi JH, Chun KA, Cho IH. The clinical efficacy of 18F-FDG-PET/CT in benign and malignant musculoskeletal tumors. Ann Nucl Med 2008; 22:603–609.
- Benz MR, Czernin J, Allen-Auerbach MS, et al. FDG-PET/CT imaging predicts histopathologic treatment responses after the initial cycle of neoadjuvant chemotherapy in high-grade soft-tissue sarcomas. Clin Cancer Res 2009; 15:2856–2863.
- Aoki J, Watanabe H, Shinozaki T, et al. FDG-PET for preoperative differential diagnosis between benign and malignant soft tissue masses. Skeletal Radiol 2003; 32:133–138.
- Blanco Sequeiros R, Klemola R, Ojala R, et al. MRI-guided trephine biopsy and fine-needle aspiration in the diagnosis of bone lesions in low-field (0.23 T) MRI system using optical instrument tracking. Eur Radiol 2002; 12:830–835.
- Rosenthal DI. Radiofrequency treatment. Orthop Clin North Am 2006; 37:475–484.
- Callstrom MR, Charboneau JW. Image-guided palliation of painful metastases using percutaneous ablation. Tech Vasc Interv Radiol 2007; 10:120–131.
- American Cancer Society. Cancer facts & figures 2009. Atlanta, GA: American Cancer Society; 2009.
- Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weiss’ Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin 2009; 59:225–249.
- Simon MA, Springfield DS, eds. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Dahlin DC, Unni KK. Bone Tumors: General Aspects and Data on 8,542 Cases. 4th ed. Springfield, IL: Thomas; 1986.
- Unni KK. Bone Tumors. New York, NY: Churchill Livingstone; 1988.
- Unni KK. Atlas of Bone Pathology. New York, NY: Chapman & Hall; 1996:1 computer optical disc.
- Unni KK, Dahlin DC. Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases. 5th ed. Philadelphia, PA: Lippincott-Raven; 1996.
- Kaste SC, Pratt CB, Cain AM, Jones-Wallace DJ, Rao BN. Metastases detected at the time of diagnosis of primary pediatric extremity osteosarcoma at diagnosis: imaging features. Cancer 1999; 86:1602–1608.
- Healey JH, Lane JM. Chondrosarcoma. Clin Orthop Relat Res 1986; 204:119–129.
- Kissane JM, Askin FB, Foulkes M, Stratton LB, Shirley SF. Ewing’s sarcoma of bone: clinicopathologic aspects of 303 cases from the Intergroup Ewing’s Sarcoma Study. Hum Pathol 1983; 14:773–779.
- Chotel F, Unnithan A, Chandrasekar CR, et al. Variability in the presentation of synovial sarcoma in children: a plea for greater awareness. J Bone Joint Surg Br 2008; 90:1090–1096.
- Miller TT. Bone tumors and tumorlike conditions: analysis with conventional radiography. Radiology 2008; 246:662–674.
- Richardson ML, Gillespy T. Magnetic resonance imaging. In: Kricun ME, ed. Imaging of Bone Tumors. Philadelphia, PA: WB Saunders; 1993:365.
- Fisher C. Soft tissue sarcomas: diagnosis, classification and prognostic factors. Br J Plast Surg 1996; 49:27–33.
- White LM, Wunder JS, Bell RS, et al. Histologic assessment of peritumoral edema in soft tissue sarcoma. Int J Radiat Oncol Biol Phys 2005; 61:1439–1445.
- White LM, Buckwalter KA. Technical considerations: CT and MR imaging in the postoperative orthopedic patient. Semin Musculoskelet Radiol 2002; 6:5–17.
- Blodgett TM, Casagranda B, Townsend DW, Meltzer CC. Issues, controversies, and clinical utility of combined PET/CT imaging: what is the interpreting physician facing? AJR Am J Roentgenol 2005; 184(suppl 5):S138–S145.
- Shin DS, Shon OJ, Han DS, Choi JH, Chun KA, Cho IH. The clinical efficacy of 18F-FDG-PET/CT in benign and malignant musculoskeletal tumors. Ann Nucl Med 2008; 22:603–609.
- Benz MR, Czernin J, Allen-Auerbach MS, et al. FDG-PET/CT imaging predicts histopathologic treatment responses after the initial cycle of neoadjuvant chemotherapy in high-grade soft-tissue sarcomas. Clin Cancer Res 2009; 15:2856–2863.
- Aoki J, Watanabe H, Shinozaki T, et al. FDG-PET for preoperative differential diagnosis between benign and malignant soft tissue masses. Skeletal Radiol 2003; 32:133–138.
- Blanco Sequeiros R, Klemola R, Ojala R, et al. MRI-guided trephine biopsy and fine-needle aspiration in the diagnosis of bone lesions in low-field (0.23 T) MRI system using optical instrument tracking. Eur Radiol 2002; 12:830–835.
- Rosenthal DI. Radiofrequency treatment. Orthop Clin North Am 2006; 37:475–484.
- Callstrom MR, Charboneau JW. Image-guided palliation of painful metastases using percutaneous ablation. Tech Vasc Interv Radiol 2007; 10:120–131.
The painful knee: Choosing the right imaging test
Radiography plays a key role in the initial evaluation of acute knee pain in adults. Yet conflicting studies and the absence of clear guidelines may leave the primary care physician uncertain as to which imaging test to order—ie, whether radiography is sufficient, and when computed tomography (CT) or magnetic resonance imaging (MRI) is needed. This article reviews the indications for radiologic examination of the knee and discusses indications for cross-sectional imaging studies. Imaging in oncology patients is not discussed here.
ACUTE KNEE PAIN: A TYPICAL SCENARIO
A 47-year-old woman presents to the emergency department with left knee pain after a motor vehicle accident that occurred the day before. The car she was driving hit a tree, and she hit her knee on the dashboard. She was wearing a seatbelt at the time of the accident. She says she was unable to walk immediately after the accident because of knee pain.
The initial examination in the emergency room reveals swelling and pain throughout the range of motion. The anterior drawer test and the Lachman test are negative (see below).
The patient is discharged home with a knee immobilizer, pain medication, and crutches, with instructions for a follow-up visit in the orthopedics clinic.
Five days later, she returns to the emergency department complaining of continuing knee pain. She says the knee gives way when she puts weight on it. The physical findings are unchanged, and she is discharged home with a follow-up appointment with orthopedics in 3 days.
At the follow-up visit, she complains of persistent knee pain in the medial aspect of the knee joint. Physical examination is difficult because of pain and swelling, and it reveals mild joint effusion with no gross instability. She has pain on the medial side with valgus stress, but there appears to be a hard end point. There is no posterior sag, and the Lachman test is negative.
Based on the physical examination and the patient’s complaints, she receives a diagnosis of medial collateral ligament strain and injury. She is given a hinged brace and is instructed to undergo a physical rehabilitation program.
Three weeks after the initial evaluation, she returns to the orthopedics clinic with continuing knee problems. Mild knee effusion persists, but she has less pain and swelling, allowing a more complete examination. The examination reveals less limitation of range of motion and a hint of positivity on the Lachman test. The knee is diffusely tender, and the pain seems out of proportion with the maneuvers used during the examination. She requests more pain medication. You suspect internal derangement of the knee. Which imaging test should you order to further evaluate this patient?
A SYSTEMATIC AND COST-EFFECTIVE APPROACH IS NEEDED
The case presented above represents a typical scenario for the presentation of acute knee pain and illustrates the diagnostic challenges.
Knee pain is a common reason for emergency room visits, and it accounts for approximately 1.9 million visits to primary care clinics annually.1 In the emergency department, most patients undergo plain radiography to assess for fracture, yet approximately 92% of radiographic studies do not show a fracture.2 Clearly, the evaluation of knee pain requires a systematic, accurate, and cost-effective approach.
Key elements of the physical examination
In acute knee pain, accurate diagnosis begins with a detailed history and physical examination.
The anterior drawer test is done to evaluate the anterior cruciate ligament. With the relaxed knee flexed to approximately 80° and the foot stabilized in a neutral position, the examiner grasps the proximal tibia in a firm yet gentle grip, and then applies anterior force, noting the degree of anterior displacement compared with the other knee.
The Lachman test, a variation of the anterior drawer test, is more definitive for the anterior cruciate ligament and is carried out with the knee in 15° of flexion and external rotation, in order to relax the iliotibial band. The upper hand grasps the distal thigh, and the lower hand, with the thumb on the tibial tubercle, pulls the tibia forward. The degree of anterior motion in millimeters is noted and compared with that on the other side, and the end point is graded as “soft” or “hard.” An end point is considered hard when a ligament abruptly halts the motion of the bone being tested against the stabilized bone. An end point is considered soft when the ligament is disrupted and the restraints are the more elastic secondary stabilizers.
Debate continues
Some authors contend that in skilled hands a thorough history, physical examination, and radiographic examination are sufficient to diagnose trauma-related intra-articular knee disorders.3 Others contend that MRI plays a key role in the initial evaluation. A number of studies4–8 have shown that using MRI in the initial evaluation not only identifies key lesions, but also may eliminate the need for an invasive diagnostic procedure (ie, arthroscopy).
For example, MRI can reveal fracture, stress fracture, insufficiency fracture, and transient patellar dislocation—conditions that may satisfactorily explain knee symptoms.
PLAIN RADIOGRAPHY STILL THE FIRST STEP IN KNEE EVALUATION
Radiography is the first step in the evaluation of knee pain. It is quick and inexpensive and can yield many diagnostic clues. It can readily reveal fractures, osteochondral defects, bony lesions, joint effusions, joint space narrowing, and bone misalignment.
In patients with knee trauma, supine anteroposterior and cross-table lateral radiographic images are generally obtained. In patients whose knee pain is not due to trauma, standing projections are done, as well as dedicated projection of the patellofemoral articulation. A standing series is most helpful for evaluating joint space and alignment.
Applying the Ottawa rules
When a patient presents to the emergency room with acute knee pain, the immediate concern is whether he or she has a fracture. The Ottawa knee rules9 for when to order radiography in adults with knee pain are highly sensitive for detecting a clinically important fracture. If any one of the five Ottawa criteria applies—ie, the patient is age 55 or older, has tenderness at the head of the fibula, has patellar tenderness, is unable to flex the knee to 90°, or is unable to bear weight—then radiography is indicated.
While studies have validated the ability of the Ottawa rules to detect important fractures in acute knee injury,2,10 fracture is the cause of only a small percentage of knee complaints in the primary care setting. More common causes include osteoarthritis, meniscal injury, ligamental injury, and crystal arthropathy, and these account for approximately half of all diagnoses. Sprain and strain account for most of the rest of knee injuries.1
Acute exacerbations of osteoarthritis
Osteoarthritis is a chronic problem, yet it is not unusual for a patient to present to the primary care physician with an acute exacerbation of joint pain. The clinical hallmarks include age over 50, stiffness lasting less than 30 minutes, bony enlargement and tenderness, and crepitus. The radiographic hallmarks, according to the Kellgren-Lawrence grading scale, are joint space narrowing, osteophytes, subchondral cysts, and sclerosis. These radiographic findings correlate well with clinical findings in these patients.11
Situations in which radiography is less helpful
In some cases the radiographic findings may not explain the patient’s clinical signs and symptoms. For example, in suspected crystalline and septic arthritis, the clinical presentation may include warmth, erythema, and effusion. Arthrocentesis would be indicated in such a patient. Indeed, in the case of suspected pseudogout, chondrocalcinosis may be radiographically evident. However, it is also present in many patients without symptoms or with osteoarthritis, so radiographic evidence does not provide a definite diagnosis.
While radiography may not always identify the cause of knee pain, it is useful in excluding serious problems such as fractures, advanced degenerative changes, and neoplasms, and it may help direct further management. Radiography is not useful in the evaluation of the cruciate and collateral ligaments, the menisci, and the hyaline cartilage of the knee and may fail to show an insufficiency or stress fracture. To evaluate these structures and associated soft tissues, MRI is preferable.
COMPUTED TOMOGRAPHY IN ACUTE KNEE PAIN
CURRENT USES OF MRI TO EVALUATE ACUTE KNEE PAIN
As mentioned above, MRI is useful in evaluating suspected meniscal and ligamentous injuries.
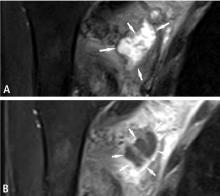
Figure 3 shows how T2-weighted MRI was used to evaluate for suspected meniscal injury in our 47-year-old female patient with left knee pain after a motor vehicle accident.
Still a matter of debate
MRI’s role in the diagnosis of knee pain is still a contentious issue.
Advantages of MRI are that it is noninvasive, it does not use ionizing radiation, it gives multiplanar images, and it provides images of soft-tissue structures, which other imaging methods cannot.12 It is a well-proven and widely accepted test. Its sensitivity for detecting meniscal and cruciate ligament injury ranges from 75% to 88%,1 and it can help in the evaluation of other injuries for which radiography is not useful, including synovitis, bone bruise, stress or insufficiency fracture, osteochondral defects, and osteonecrosis.
In addition, several studies show that using MRI to establish the diagnosis in acute knee pain can mean that 22% to 42% fewer arthroscopic procedures need to be performed.4–8 Authors of a prospective double-blind study8 recommended that MRI be used in patients with acute knee injury when the findings of the clinical history and examination by orthopedic surgeons prove equivocal.8 MRI evaluation is especially desirable for young, active patients who wish to resume activity as soon as possible.
A routine MRI examination consists of T1- and T2-weighted images in three planes, although the number of sequences and planes varies from hospital to hospital. The use of gadolinium contrast is indicated only when osteomyelitis, septic arthritis, or a mass is suspected.
Disadvantages of MRI include its cost: Medicare reimbursement for knee MRI is around $400, compared with $200 for knee CT and $50 for knee radiography with four views. Also, while studies have shown MRI to have a high sensitivity and specificity in the diagnosis of acute knee injury, some have reported a high false-positive rate for the detection of meniscal tear.13,14 MRI has also been shown to have a lower sensitivity than arthroscopy for lesions of the articular cartilage.13 Furthermore, MRI has been shown to reveal cartilage lesions, osteophytes, and meniscal abnormalities in asymptomatic study volunteers with no history of pain, trauma or knee disease.14 Therefore, findings on MRI must closely correlate with findings on the history and physical examination.
Additional indications for knee MRI
Cartilage can be assessed on routine MRI sequences of the knee. Since closed MRI systems have more powerful magnets than open systems, closed MRI systems provide greater anatomic detail.
MRI can identify other lesions, such as spontaneous osteonecrosis of the knee, usually seen in elderly women who may present with sudden knee pain. In such patients, MRI findings of focal replacement of the bone marrow and surrounding edema are specific for osteonecrosis.
Opinions vary as to whether bone marrow edema is always associated with pain. Sequential MRI studies have shown persistence of bone marrow edema for 2 years in patients with degenerative arthritis whose symptoms have waned. Bone marrow edema may be associated with pain but may be absent or inconsequential in the presence of pain.
Because fluid-sensitive T2-weighted MRI is exquisitely sensitive for mobile water protons (ie, in bone marrow edema), it is important that a cause for the edema-like signal be sought on the MRI scan, since this finding is nonspecific and may be associated with articular disease, trauma, osteonecrosis, infection, or bone tumors. Additionally, clinicians need to be aware that the findings on MRI depend on the quality of the study, and are influenced by technical factors such as magnet strength, imaging planes, and use of surface coils.
MRI should be used in patients in whom surgical treatment, ie, arthroscopy, is being considered. As discussed above, several studies have shown that a significant number of unnecessary arthroscopies may be prevented when preceded by an MRI examination.
Figure 5 shows the use of MRI in the evaluation of a 45-year-old man with left knee pain after a motorcycle accident.
ULTRASONOGRAPHY HAS ONLY A LIMITED ROLE
Ultrasonography does not play a major role in the evaluation of acute knee pain in the United States, in part because the accuracy of the results depend much on the technical skills and experience of the operator.
Ultrasonography can be useful in evaluating for rupture of the quadriceps and patellar tendon, or to assess a repaired tendon after surgery,15 and it is a quick and reliable way to determine the presence of joint effusion and popliteal cyst. It is also used to guide needle placement for joint aspiration and injection.
- Jackson JL, O’Malley PG, Kroenke K. Evaluation of acute knee pain in primary care. Ann Intern Med 2003; 139:575–588.
- Steill IG, Greenberg GH, Wells GA, et al. Prospective validation of a decision rule for the use of radiographs in acute knee injuries. JAMA 1996; 275:611–615.
- O’Shea KJ, Murphy DP, Heekin RD, Herzwurm PJ. The diagnostic accuracy of history, physical examination, and radiographs in the evaluation of traumatic knee disorders. Am J Sports Med 1996; 24:164–167.
- Spiers AS, Meagher T, Ostlere SJ, Wilson DJ, Dodd CA. Can MRI of the knee affect arthroscopic practice? J Bone Joint Surg 1993; 75:49–52.
- Bui-Mansfield LT, Youngberg RA, Warme W, Pitcher JD, Nguyen PL. Potential cost savings of MR imaging obtained before arthroscopy of the knee: evaluation of 50 consecutive patients. AJR Am J Roentgenol 1997; 168:913–918.
- Rangger C, Klestil T, Kathrein A, Inderster A, Hamid L. Influence of magnetic resonance imaging on indications for arthroscopy of the knee. Clin Orthop Rel Res 1996; 330:133–142.
- Mackenzie R, Dixon AK, Keene GS, Hollingsworth W, Lomas DJ, Villar RN. Magnetic resonance imaging of the knee: assessment of effectiveness. Clin Radiol 1996; 51:245–250.
- Munshi M, Davidson M, MacDonald PB, Froese W, Sutherland K. The efficacy of magnetic resonance imaging in acute knee injuries. Clin J Sport Med 2000; 10:34–39.
- Steill IG, Wells GA, Hoag RH, et al. Implementation of the Ottawa knee rule for the use of radiography in acute knee injuries. JAMA 1997; 278:2075–2079.
- Tigges S, Pitts S, Mukundan S, Morrison D, Olson M, Shahriara A. External validation of the Ottawa knee rules in an urban trauma center in the United States. AJR Am J Roentgenol 1999; 172:1069–1071.
- Claessens AA, Schouten JS, van den Ouweland FA, Valkenburg HA. Do clinical findings associate with radiographic osteoarthritis of the knee? Ann Rheum Dis 1990; 49:771–774.
- Gries PE, Bardana DE, Holmstrom MC, Burks RT. Meniscal injury: basic science and evaluation. J Am Acad Orthop Surg 2002; 10:168–176.
- Gelb HJ, Glasgow SG, Sapega AA, Torg JS. Magnetic resonance imaging of knee disorders. Clinical value and cost-effectiveness in a sports medicine practice. Am J Sports Med 1996; 24:99–103.
- Beattie KA, Boulos P, Pui M, et al. Abnormalities identified in the knees of asymptomatic volunteers using peripheral magnetic resonance imaging. Osteoarthritis Cartilage 2005; 13:181–186.
- Ilan DI, Tejwani N, Keschner M, Leibman M. Quadriceps tendon rupture. J Am Acad Orthop Surg 2003; 11:192–200.
Radiography plays a key role in the initial evaluation of acute knee pain in adults. Yet conflicting studies and the absence of clear guidelines may leave the primary care physician uncertain as to which imaging test to order—ie, whether radiography is sufficient, and when computed tomography (CT) or magnetic resonance imaging (MRI) is needed. This article reviews the indications for radiologic examination of the knee and discusses indications for cross-sectional imaging studies. Imaging in oncology patients is not discussed here.
ACUTE KNEE PAIN: A TYPICAL SCENARIO
A 47-year-old woman presents to the emergency department with left knee pain after a motor vehicle accident that occurred the day before. The car she was driving hit a tree, and she hit her knee on the dashboard. She was wearing a seatbelt at the time of the accident. She says she was unable to walk immediately after the accident because of knee pain.
The initial examination in the emergency room reveals swelling and pain throughout the range of motion. The anterior drawer test and the Lachman test are negative (see below).
The patient is discharged home with a knee immobilizer, pain medication, and crutches, with instructions for a follow-up visit in the orthopedics clinic.
Five days later, she returns to the emergency department complaining of continuing knee pain. She says the knee gives way when she puts weight on it. The physical findings are unchanged, and she is discharged home with a follow-up appointment with orthopedics in 3 days.
At the follow-up visit, she complains of persistent knee pain in the medial aspect of the knee joint. Physical examination is difficult because of pain and swelling, and it reveals mild joint effusion with no gross instability. She has pain on the medial side with valgus stress, but there appears to be a hard end point. There is no posterior sag, and the Lachman test is negative.
Based on the physical examination and the patient’s complaints, she receives a diagnosis of medial collateral ligament strain and injury. She is given a hinged brace and is instructed to undergo a physical rehabilitation program.
Three weeks after the initial evaluation, she returns to the orthopedics clinic with continuing knee problems. Mild knee effusion persists, but she has less pain and swelling, allowing a more complete examination. The examination reveals less limitation of range of motion and a hint of positivity on the Lachman test. The knee is diffusely tender, and the pain seems out of proportion with the maneuvers used during the examination. She requests more pain medication. You suspect internal derangement of the knee. Which imaging test should you order to further evaluate this patient?
A SYSTEMATIC AND COST-EFFECTIVE APPROACH IS NEEDED
The case presented above represents a typical scenario for the presentation of acute knee pain and illustrates the diagnostic challenges.
Knee pain is a common reason for emergency room visits, and it accounts for approximately 1.9 million visits to primary care clinics annually.1 In the emergency department, most patients undergo plain radiography to assess for fracture, yet approximately 92% of radiographic studies do not show a fracture.2 Clearly, the evaluation of knee pain requires a systematic, accurate, and cost-effective approach.
Key elements of the physical examination
In acute knee pain, accurate diagnosis begins with a detailed history and physical examination.
The anterior drawer test is done to evaluate the anterior cruciate ligament. With the relaxed knee flexed to approximately 80° and the foot stabilized in a neutral position, the examiner grasps the proximal tibia in a firm yet gentle grip, and then applies anterior force, noting the degree of anterior displacement compared with the other knee.
The Lachman test, a variation of the anterior drawer test, is more definitive for the anterior cruciate ligament and is carried out with the knee in 15° of flexion and external rotation, in order to relax the iliotibial band. The upper hand grasps the distal thigh, and the lower hand, with the thumb on the tibial tubercle, pulls the tibia forward. The degree of anterior motion in millimeters is noted and compared with that on the other side, and the end point is graded as “soft” or “hard.” An end point is considered hard when a ligament abruptly halts the motion of the bone being tested against the stabilized bone. An end point is considered soft when the ligament is disrupted and the restraints are the more elastic secondary stabilizers.
Debate continues
Some authors contend that in skilled hands a thorough history, physical examination, and radiographic examination are sufficient to diagnose trauma-related intra-articular knee disorders.3 Others contend that MRI plays a key role in the initial evaluation. A number of studies4–8 have shown that using MRI in the initial evaluation not only identifies key lesions, but also may eliminate the need for an invasive diagnostic procedure (ie, arthroscopy).
For example, MRI can reveal fracture, stress fracture, insufficiency fracture, and transient patellar dislocation—conditions that may satisfactorily explain knee symptoms.
PLAIN RADIOGRAPHY STILL THE FIRST STEP IN KNEE EVALUATION
Radiography is the first step in the evaluation of knee pain. It is quick and inexpensive and can yield many diagnostic clues. It can readily reveal fractures, osteochondral defects, bony lesions, joint effusions, joint space narrowing, and bone misalignment.
In patients with knee trauma, supine anteroposterior and cross-table lateral radiographic images are generally obtained. In patients whose knee pain is not due to trauma, standing projections are done, as well as dedicated projection of the patellofemoral articulation. A standing series is most helpful for evaluating joint space and alignment.
Applying the Ottawa rules
When a patient presents to the emergency room with acute knee pain, the immediate concern is whether he or she has a fracture. The Ottawa knee rules9 for when to order radiography in adults with knee pain are highly sensitive for detecting a clinically important fracture. If any one of the five Ottawa criteria applies—ie, the patient is age 55 or older, has tenderness at the head of the fibula, has patellar tenderness, is unable to flex the knee to 90°, or is unable to bear weight—then radiography is indicated.
While studies have validated the ability of the Ottawa rules to detect important fractures in acute knee injury,2,10 fracture is the cause of only a small percentage of knee complaints in the primary care setting. More common causes include osteoarthritis, meniscal injury, ligamental injury, and crystal arthropathy, and these account for approximately half of all diagnoses. Sprain and strain account for most of the rest of knee injuries.1
Acute exacerbations of osteoarthritis
Osteoarthritis is a chronic problem, yet it is not unusual for a patient to present to the primary care physician with an acute exacerbation of joint pain. The clinical hallmarks include age over 50, stiffness lasting less than 30 minutes, bony enlargement and tenderness, and crepitus. The radiographic hallmarks, according to the Kellgren-Lawrence grading scale, are joint space narrowing, osteophytes, subchondral cysts, and sclerosis. These radiographic findings correlate well with clinical findings in these patients.11
Situations in which radiography is less helpful
In some cases the radiographic findings may not explain the patient’s clinical signs and symptoms. For example, in suspected crystalline and septic arthritis, the clinical presentation may include warmth, erythema, and effusion. Arthrocentesis would be indicated in such a patient. Indeed, in the case of suspected pseudogout, chondrocalcinosis may be radiographically evident. However, it is also present in many patients without symptoms or with osteoarthritis, so radiographic evidence does not provide a definite diagnosis.
While radiography may not always identify the cause of knee pain, it is useful in excluding serious problems such as fractures, advanced degenerative changes, and neoplasms, and it may help direct further management. Radiography is not useful in the evaluation of the cruciate and collateral ligaments, the menisci, and the hyaline cartilage of the knee and may fail to show an insufficiency or stress fracture. To evaluate these structures and associated soft tissues, MRI is preferable.
COMPUTED TOMOGRAPHY IN ACUTE KNEE PAIN
CURRENT USES OF MRI TO EVALUATE ACUTE KNEE PAIN
As mentioned above, MRI is useful in evaluating suspected meniscal and ligamentous injuries.
Figure 3 shows how T2-weighted MRI was used to evaluate for suspected meniscal injury in our 47-year-old female patient with left knee pain after a motor vehicle accident.
Still a matter of debate
MRI’s role in the diagnosis of knee pain is still a contentious issue.
Advantages of MRI are that it is noninvasive, it does not use ionizing radiation, it gives multiplanar images, and it provides images of soft-tissue structures, which other imaging methods cannot.12 It is a well-proven and widely accepted test. Its sensitivity for detecting meniscal and cruciate ligament injury ranges from 75% to 88%,1 and it can help in the evaluation of other injuries for which radiography is not useful, including synovitis, bone bruise, stress or insufficiency fracture, osteochondral defects, and osteonecrosis.
In addition, several studies show that using MRI to establish the diagnosis in acute knee pain can mean that 22% to 42% fewer arthroscopic procedures need to be performed.4–8 Authors of a prospective double-blind study8 recommended that MRI be used in patients with acute knee injury when the findings of the clinical history and examination by orthopedic surgeons prove equivocal.8 MRI evaluation is especially desirable for young, active patients who wish to resume activity as soon as possible.
A routine MRI examination consists of T1- and T2-weighted images in three planes, although the number of sequences and planes varies from hospital to hospital. The use of gadolinium contrast is indicated only when osteomyelitis, septic arthritis, or a mass is suspected.
Disadvantages of MRI include its cost: Medicare reimbursement for knee MRI is around $400, compared with $200 for knee CT and $50 for knee radiography with four views. Also, while studies have shown MRI to have a high sensitivity and specificity in the diagnosis of acute knee injury, some have reported a high false-positive rate for the detection of meniscal tear.13,14 MRI has also been shown to have a lower sensitivity than arthroscopy for lesions of the articular cartilage.13 Furthermore, MRI has been shown to reveal cartilage lesions, osteophytes, and meniscal abnormalities in asymptomatic study volunteers with no history of pain, trauma or knee disease.14 Therefore, findings on MRI must closely correlate with findings on the history and physical examination.
Additional indications for knee MRI
Cartilage can be assessed on routine MRI sequences of the knee. Since closed MRI systems have more powerful magnets than open systems, closed MRI systems provide greater anatomic detail.
MRI can identify other lesions, such as spontaneous osteonecrosis of the knee, usually seen in elderly women who may present with sudden knee pain. In such patients, MRI findings of focal replacement of the bone marrow and surrounding edema are specific for osteonecrosis.
Opinions vary as to whether bone marrow edema is always associated with pain. Sequential MRI studies have shown persistence of bone marrow edema for 2 years in patients with degenerative arthritis whose symptoms have waned. Bone marrow edema may be associated with pain but may be absent or inconsequential in the presence of pain.
Because fluid-sensitive T2-weighted MRI is exquisitely sensitive for mobile water protons (ie, in bone marrow edema), it is important that a cause for the edema-like signal be sought on the MRI scan, since this finding is nonspecific and may be associated with articular disease, trauma, osteonecrosis, infection, or bone tumors. Additionally, clinicians need to be aware that the findings on MRI depend on the quality of the study, and are influenced by technical factors such as magnet strength, imaging planes, and use of surface coils.
MRI should be used in patients in whom surgical treatment, ie, arthroscopy, is being considered. As discussed above, several studies have shown that a significant number of unnecessary arthroscopies may be prevented when preceded by an MRI examination.
Figure 5 shows the use of MRI in the evaluation of a 45-year-old man with left knee pain after a motorcycle accident.
ULTRASONOGRAPHY HAS ONLY A LIMITED ROLE
Ultrasonography does not play a major role in the evaluation of acute knee pain in the United States, in part because the accuracy of the results depend much on the technical skills and experience of the operator.
Ultrasonography can be useful in evaluating for rupture of the quadriceps and patellar tendon, or to assess a repaired tendon after surgery,15 and it is a quick and reliable way to determine the presence of joint effusion and popliteal cyst. It is also used to guide needle placement for joint aspiration and injection.
Radiography plays a key role in the initial evaluation of acute knee pain in adults. Yet conflicting studies and the absence of clear guidelines may leave the primary care physician uncertain as to which imaging test to order—ie, whether radiography is sufficient, and when computed tomography (CT) or magnetic resonance imaging (MRI) is needed. This article reviews the indications for radiologic examination of the knee and discusses indications for cross-sectional imaging studies. Imaging in oncology patients is not discussed here.
ACUTE KNEE PAIN: A TYPICAL SCENARIO
A 47-year-old woman presents to the emergency department with left knee pain after a motor vehicle accident that occurred the day before. The car she was driving hit a tree, and she hit her knee on the dashboard. She was wearing a seatbelt at the time of the accident. She says she was unable to walk immediately after the accident because of knee pain.
The initial examination in the emergency room reveals swelling and pain throughout the range of motion. The anterior drawer test and the Lachman test are negative (see below).
The patient is discharged home with a knee immobilizer, pain medication, and crutches, with instructions for a follow-up visit in the orthopedics clinic.
Five days later, she returns to the emergency department complaining of continuing knee pain. She says the knee gives way when she puts weight on it. The physical findings are unchanged, and she is discharged home with a follow-up appointment with orthopedics in 3 days.
At the follow-up visit, she complains of persistent knee pain in the medial aspect of the knee joint. Physical examination is difficult because of pain and swelling, and it reveals mild joint effusion with no gross instability. She has pain on the medial side with valgus stress, but there appears to be a hard end point. There is no posterior sag, and the Lachman test is negative.
Based on the physical examination and the patient’s complaints, she receives a diagnosis of medial collateral ligament strain and injury. She is given a hinged brace and is instructed to undergo a physical rehabilitation program.
Three weeks after the initial evaluation, she returns to the orthopedics clinic with continuing knee problems. Mild knee effusion persists, but she has less pain and swelling, allowing a more complete examination. The examination reveals less limitation of range of motion and a hint of positivity on the Lachman test. The knee is diffusely tender, and the pain seems out of proportion with the maneuvers used during the examination. She requests more pain medication. You suspect internal derangement of the knee. Which imaging test should you order to further evaluate this patient?
A SYSTEMATIC AND COST-EFFECTIVE APPROACH IS NEEDED
The case presented above represents a typical scenario for the presentation of acute knee pain and illustrates the diagnostic challenges.
Knee pain is a common reason for emergency room visits, and it accounts for approximately 1.9 million visits to primary care clinics annually.1 In the emergency department, most patients undergo plain radiography to assess for fracture, yet approximately 92% of radiographic studies do not show a fracture.2 Clearly, the evaluation of knee pain requires a systematic, accurate, and cost-effective approach.
Key elements of the physical examination
In acute knee pain, accurate diagnosis begins with a detailed history and physical examination.
The anterior drawer test is done to evaluate the anterior cruciate ligament. With the relaxed knee flexed to approximately 80° and the foot stabilized in a neutral position, the examiner grasps the proximal tibia in a firm yet gentle grip, and then applies anterior force, noting the degree of anterior displacement compared with the other knee.
The Lachman test, a variation of the anterior drawer test, is more definitive for the anterior cruciate ligament and is carried out with the knee in 15° of flexion and external rotation, in order to relax the iliotibial band. The upper hand grasps the distal thigh, and the lower hand, with the thumb on the tibial tubercle, pulls the tibia forward. The degree of anterior motion in millimeters is noted and compared with that on the other side, and the end point is graded as “soft” or “hard.” An end point is considered hard when a ligament abruptly halts the motion of the bone being tested against the stabilized bone. An end point is considered soft when the ligament is disrupted and the restraints are the more elastic secondary stabilizers.
Debate continues
Some authors contend that in skilled hands a thorough history, physical examination, and radiographic examination are sufficient to diagnose trauma-related intra-articular knee disorders.3 Others contend that MRI plays a key role in the initial evaluation. A number of studies4–8 have shown that using MRI in the initial evaluation not only identifies key lesions, but also may eliminate the need for an invasive diagnostic procedure (ie, arthroscopy).
For example, MRI can reveal fracture, stress fracture, insufficiency fracture, and transient patellar dislocation—conditions that may satisfactorily explain knee symptoms.
PLAIN RADIOGRAPHY STILL THE FIRST STEP IN KNEE EVALUATION
Radiography is the first step in the evaluation of knee pain. It is quick and inexpensive and can yield many diagnostic clues. It can readily reveal fractures, osteochondral defects, bony lesions, joint effusions, joint space narrowing, and bone misalignment.
In patients with knee trauma, supine anteroposterior and cross-table lateral radiographic images are generally obtained. In patients whose knee pain is not due to trauma, standing projections are done, as well as dedicated projection of the patellofemoral articulation. A standing series is most helpful for evaluating joint space and alignment.
Applying the Ottawa rules
When a patient presents to the emergency room with acute knee pain, the immediate concern is whether he or she has a fracture. The Ottawa knee rules9 for when to order radiography in adults with knee pain are highly sensitive for detecting a clinically important fracture. If any one of the five Ottawa criteria applies—ie, the patient is age 55 or older, has tenderness at the head of the fibula, has patellar tenderness, is unable to flex the knee to 90°, or is unable to bear weight—then radiography is indicated.
While studies have validated the ability of the Ottawa rules to detect important fractures in acute knee injury,2,10 fracture is the cause of only a small percentage of knee complaints in the primary care setting. More common causes include osteoarthritis, meniscal injury, ligamental injury, and crystal arthropathy, and these account for approximately half of all diagnoses. Sprain and strain account for most of the rest of knee injuries.1
Acute exacerbations of osteoarthritis
Osteoarthritis is a chronic problem, yet it is not unusual for a patient to present to the primary care physician with an acute exacerbation of joint pain. The clinical hallmarks include age over 50, stiffness lasting less than 30 minutes, bony enlargement and tenderness, and crepitus. The radiographic hallmarks, according to the Kellgren-Lawrence grading scale, are joint space narrowing, osteophytes, subchondral cysts, and sclerosis. These radiographic findings correlate well with clinical findings in these patients.11
Situations in which radiography is less helpful
In some cases the radiographic findings may not explain the patient’s clinical signs and symptoms. For example, in suspected crystalline and septic arthritis, the clinical presentation may include warmth, erythema, and effusion. Arthrocentesis would be indicated in such a patient. Indeed, in the case of suspected pseudogout, chondrocalcinosis may be radiographically evident. However, it is also present in many patients without symptoms or with osteoarthritis, so radiographic evidence does not provide a definite diagnosis.
While radiography may not always identify the cause of knee pain, it is useful in excluding serious problems such as fractures, advanced degenerative changes, and neoplasms, and it may help direct further management. Radiography is not useful in the evaluation of the cruciate and collateral ligaments, the menisci, and the hyaline cartilage of the knee and may fail to show an insufficiency or stress fracture. To evaluate these structures and associated soft tissues, MRI is preferable.
COMPUTED TOMOGRAPHY IN ACUTE KNEE PAIN
CURRENT USES OF MRI TO EVALUATE ACUTE KNEE PAIN
As mentioned above, MRI is useful in evaluating suspected meniscal and ligamentous injuries.
Figure 3 shows how T2-weighted MRI was used to evaluate for suspected meniscal injury in our 47-year-old female patient with left knee pain after a motor vehicle accident.
Still a matter of debate
MRI’s role in the diagnosis of knee pain is still a contentious issue.
Advantages of MRI are that it is noninvasive, it does not use ionizing radiation, it gives multiplanar images, and it provides images of soft-tissue structures, which other imaging methods cannot.12 It is a well-proven and widely accepted test. Its sensitivity for detecting meniscal and cruciate ligament injury ranges from 75% to 88%,1 and it can help in the evaluation of other injuries for which radiography is not useful, including synovitis, bone bruise, stress or insufficiency fracture, osteochondral defects, and osteonecrosis.
In addition, several studies show that using MRI to establish the diagnosis in acute knee pain can mean that 22% to 42% fewer arthroscopic procedures need to be performed.4–8 Authors of a prospective double-blind study8 recommended that MRI be used in patients with acute knee injury when the findings of the clinical history and examination by orthopedic surgeons prove equivocal.8 MRI evaluation is especially desirable for young, active patients who wish to resume activity as soon as possible.
A routine MRI examination consists of T1- and T2-weighted images in three planes, although the number of sequences and planes varies from hospital to hospital. The use of gadolinium contrast is indicated only when osteomyelitis, septic arthritis, or a mass is suspected.
Disadvantages of MRI include its cost: Medicare reimbursement for knee MRI is around $400, compared with $200 for knee CT and $50 for knee radiography with four views. Also, while studies have shown MRI to have a high sensitivity and specificity in the diagnosis of acute knee injury, some have reported a high false-positive rate for the detection of meniscal tear.13,14 MRI has also been shown to have a lower sensitivity than arthroscopy for lesions of the articular cartilage.13 Furthermore, MRI has been shown to reveal cartilage lesions, osteophytes, and meniscal abnormalities in asymptomatic study volunteers with no history of pain, trauma or knee disease.14 Therefore, findings on MRI must closely correlate with findings on the history and physical examination.
Additional indications for knee MRI
Cartilage can be assessed on routine MRI sequences of the knee. Since closed MRI systems have more powerful magnets than open systems, closed MRI systems provide greater anatomic detail.
MRI can identify other lesions, such as spontaneous osteonecrosis of the knee, usually seen in elderly women who may present with sudden knee pain. In such patients, MRI findings of focal replacement of the bone marrow and surrounding edema are specific for osteonecrosis.
Opinions vary as to whether bone marrow edema is always associated with pain. Sequential MRI studies have shown persistence of bone marrow edema for 2 years in patients with degenerative arthritis whose symptoms have waned. Bone marrow edema may be associated with pain but may be absent or inconsequential in the presence of pain.
Because fluid-sensitive T2-weighted MRI is exquisitely sensitive for mobile water protons (ie, in bone marrow edema), it is important that a cause for the edema-like signal be sought on the MRI scan, since this finding is nonspecific and may be associated with articular disease, trauma, osteonecrosis, infection, or bone tumors. Additionally, clinicians need to be aware that the findings on MRI depend on the quality of the study, and are influenced by technical factors such as magnet strength, imaging planes, and use of surface coils.
MRI should be used in patients in whom surgical treatment, ie, arthroscopy, is being considered. As discussed above, several studies have shown that a significant number of unnecessary arthroscopies may be prevented when preceded by an MRI examination.
Figure 5 shows the use of MRI in the evaluation of a 45-year-old man with left knee pain after a motorcycle accident.
ULTRASONOGRAPHY HAS ONLY A LIMITED ROLE
Ultrasonography does not play a major role in the evaluation of acute knee pain in the United States, in part because the accuracy of the results depend much on the technical skills and experience of the operator.
Ultrasonography can be useful in evaluating for rupture of the quadriceps and patellar tendon, or to assess a repaired tendon after surgery,15 and it is a quick and reliable way to determine the presence of joint effusion and popliteal cyst. It is also used to guide needle placement for joint aspiration and injection.
- Jackson JL, O’Malley PG, Kroenke K. Evaluation of acute knee pain in primary care. Ann Intern Med 2003; 139:575–588.
- Steill IG, Greenberg GH, Wells GA, et al. Prospective validation of a decision rule for the use of radiographs in acute knee injuries. JAMA 1996; 275:611–615.
- O’Shea KJ, Murphy DP, Heekin RD, Herzwurm PJ. The diagnostic accuracy of history, physical examination, and radiographs in the evaluation of traumatic knee disorders. Am J Sports Med 1996; 24:164–167.
- Spiers AS, Meagher T, Ostlere SJ, Wilson DJ, Dodd CA. Can MRI of the knee affect arthroscopic practice? J Bone Joint Surg 1993; 75:49–52.
- Bui-Mansfield LT, Youngberg RA, Warme W, Pitcher JD, Nguyen PL. Potential cost savings of MR imaging obtained before arthroscopy of the knee: evaluation of 50 consecutive patients. AJR Am J Roentgenol 1997; 168:913–918.
- Rangger C, Klestil T, Kathrein A, Inderster A, Hamid L. Influence of magnetic resonance imaging on indications for arthroscopy of the knee. Clin Orthop Rel Res 1996; 330:133–142.
- Mackenzie R, Dixon AK, Keene GS, Hollingsworth W, Lomas DJ, Villar RN. Magnetic resonance imaging of the knee: assessment of effectiveness. Clin Radiol 1996; 51:245–250.
- Munshi M, Davidson M, MacDonald PB, Froese W, Sutherland K. The efficacy of magnetic resonance imaging in acute knee injuries. Clin J Sport Med 2000; 10:34–39.
- Steill IG, Wells GA, Hoag RH, et al. Implementation of the Ottawa knee rule for the use of radiography in acute knee injuries. JAMA 1997; 278:2075–2079.
- Tigges S, Pitts S, Mukundan S, Morrison D, Olson M, Shahriara A. External validation of the Ottawa knee rules in an urban trauma center in the United States. AJR Am J Roentgenol 1999; 172:1069–1071.
- Claessens AA, Schouten JS, van den Ouweland FA, Valkenburg HA. Do clinical findings associate with radiographic osteoarthritis of the knee? Ann Rheum Dis 1990; 49:771–774.
- Gries PE, Bardana DE, Holmstrom MC, Burks RT. Meniscal injury: basic science and evaluation. J Am Acad Orthop Surg 2002; 10:168–176.
- Gelb HJ, Glasgow SG, Sapega AA, Torg JS. Magnetic resonance imaging of knee disorders. Clinical value and cost-effectiveness in a sports medicine practice. Am J Sports Med 1996; 24:99–103.
- Beattie KA, Boulos P, Pui M, et al. Abnormalities identified in the knees of asymptomatic volunteers using peripheral magnetic resonance imaging. Osteoarthritis Cartilage 2005; 13:181–186.
- Ilan DI, Tejwani N, Keschner M, Leibman M. Quadriceps tendon rupture. J Am Acad Orthop Surg 2003; 11:192–200.
- Jackson JL, O’Malley PG, Kroenke K. Evaluation of acute knee pain in primary care. Ann Intern Med 2003; 139:575–588.
- Steill IG, Greenberg GH, Wells GA, et al. Prospective validation of a decision rule for the use of radiographs in acute knee injuries. JAMA 1996; 275:611–615.
- O’Shea KJ, Murphy DP, Heekin RD, Herzwurm PJ. The diagnostic accuracy of history, physical examination, and radiographs in the evaluation of traumatic knee disorders. Am J Sports Med 1996; 24:164–167.
- Spiers AS, Meagher T, Ostlere SJ, Wilson DJ, Dodd CA. Can MRI of the knee affect arthroscopic practice? J Bone Joint Surg 1993; 75:49–52.
- Bui-Mansfield LT, Youngberg RA, Warme W, Pitcher JD, Nguyen PL. Potential cost savings of MR imaging obtained before arthroscopy of the knee: evaluation of 50 consecutive patients. AJR Am J Roentgenol 1997; 168:913–918.
- Rangger C, Klestil T, Kathrein A, Inderster A, Hamid L. Influence of magnetic resonance imaging on indications for arthroscopy of the knee. Clin Orthop Rel Res 1996; 330:133–142.
- Mackenzie R, Dixon AK, Keene GS, Hollingsworth W, Lomas DJ, Villar RN. Magnetic resonance imaging of the knee: assessment of effectiveness. Clin Radiol 1996; 51:245–250.
- Munshi M, Davidson M, MacDonald PB, Froese W, Sutherland K. The efficacy of magnetic resonance imaging in acute knee injuries. Clin J Sport Med 2000; 10:34–39.
- Steill IG, Wells GA, Hoag RH, et al. Implementation of the Ottawa knee rule for the use of radiography in acute knee injuries. JAMA 1997; 278:2075–2079.
- Tigges S, Pitts S, Mukundan S, Morrison D, Olson M, Shahriara A. External validation of the Ottawa knee rules in an urban trauma center in the United States. AJR Am J Roentgenol 1999; 172:1069–1071.
- Claessens AA, Schouten JS, van den Ouweland FA, Valkenburg HA. Do clinical findings associate with radiographic osteoarthritis of the knee? Ann Rheum Dis 1990; 49:771–774.
- Gries PE, Bardana DE, Holmstrom MC, Burks RT. Meniscal injury: basic science and evaluation. J Am Acad Orthop Surg 2002; 10:168–176.
- Gelb HJ, Glasgow SG, Sapega AA, Torg JS. Magnetic resonance imaging of knee disorders. Clinical value and cost-effectiveness in a sports medicine practice. Am J Sports Med 1996; 24:99–103.
- Beattie KA, Boulos P, Pui M, et al. Abnormalities identified in the knees of asymptomatic volunteers using peripheral magnetic resonance imaging. Osteoarthritis Cartilage 2005; 13:181–186.
- Ilan DI, Tejwani N, Keschner M, Leibman M. Quadriceps tendon rupture. J Am Acad Orthop Surg 2003; 11:192–200.
KEY POINTS
- In the emergency department, most patients undergo plain radiography to assess for fracture, yet more than 90% of these studies do not show a fracture.
- CT is useful in patients with knee trauma but normal radiographs.
- MRI is the imaging modality for internal derangement of the knee.
- Ultrasonography’s role in the evaluation of acute knee pain is generally limited to assessment of the extensor mechanism, joint effusion, and popliteal cyst.