User login
What is the best choice for prophylaxis against VTE in medical inpatients?
Case
A 76-year-old gentleman is admitted for progressively worsening dyspnea, cough, and bilateral leg edema. Upon admission, his blood pressure is 150/90 mm/Hg, pulse 90 beats per minute, and respiration is 24 per minute.
Pertinent physical findings include jugular venous distension, bilateral crackles, S3 gallop, and 2+ bilateral lower extremity edema. The chest radiograph shows cardiomegaly and pulmonary edema. He is admitted to the hospital with a diagnosis of acute decompensated heart failure and starts aggressive medical therapy.
Overview
Approximately 2 million cases of deep-vein thrombosis (DVT) occur annually in the United States. Based on studies utilizing ventilation-perfusion scanning, half these patients likely have a silent pulmonary embolism (PE); of these, approximately 250,000 die.
The spectrum of venous thromboembolism (VTE), which includes DVT and PE, can vary from being asymptomatic to sudden death. Autopsy studies suggest a leading cause of sudden death in hospitalized medical patients is often a PE. There also are sequelae, such as chronic pulmonary hypertension, occurring in approximately 5% of PE cases, and post-thrombotic syndrome, occurring in approximately 40% of patients with DVT at two years.1
A recent study suggests DVT occurs three times more commonly in the outpatient setting. However, more than half of these patients were hospitalized in the three months prior.2 This is likely due to inadequate in-hospital prevention because of absence of prophylaxis, use of an unsuitable modality, insufficient dose of the drug, or ineffective duration of therapy. Inadequate and omitted VTE prophylaxis for medical patients was clearly demonstrated in the DVT Free Registry. This registry was created by 183 U.S. hospitals and included 5,451 patients, inpatients, and outpatients with ultrasound-confirmed DVT.
The number of medical inpatients who received prophylaxis in the 30 days prior to diagnosis was 28%—lower than the 48% of surgical patients.3 In a recent international registry, IMPROVE, only approximately 50% of hospitalized patients received prophylaxis.4
Virchow’s triad describes three underlying etiologic factors for thrombosis: stasis of blood flow, endothelial injury, and hypercoagulability. Established VTE risk factors reflect these underlying pathophysiologic processes. Important risk factors for VTE include increasing age, prolonged immobility, malignancy, major surgery, multiple trauma, prior VTE, and chronic heart failure.5
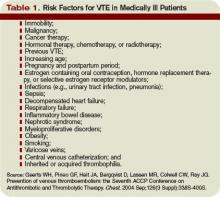
However, the magnitude of risk conferred by these and other risk factors varies (see Table 1, p. 35). It is not known how these factors interact to determine a patient’s individual VTE risk, but there is evidence it increases in proportion to the number of predisposing factors present.
In a recent systematic review of nine studies, including approximately 20,000 patients, prophylaxis reduced the rate of symptomatic VTE in at-risk hospitalized medical patients without increasing major bleeding.6
Multiple healthcare organizations, such as the National Quality Forum (NQF), Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and Agency for Healthcare Research and Quality (AHRQ) have identified VTE as a preventable condition in hospitalized patients. Formal risk assessment must be conducted as a first step, followed by the initiation of timely prophylaxis to improve patient safety.
Review of the Data
Mechanical forms of prophylaxis, such as graduated compression stockings, have been evaluated in patients with stroke and myocardial infarction. Intermittent pneumatic compression stockings and venous foot pumps have not been studied in randomized controlled trials (RCTs) in general medical patients.
Although there is data supporting the efficacy of these devices in surgical patients, the American College of Chest Physicians’ (ACCP) guidelines recommend against the use of mechanical forms of prophylaxis in medical patients unless there is a contraindication to pharmacologic prophylaxis.7
The ideal prophylactic agent is cost-effective and has no side effects. Available pharmacologic options for prevention of VTE in medical patients include unfractionated heparin (UFH), low molecular weight heparins (LMWHs), and the synthetic pentasaccharide, fondaparinux. Oral anticoagulants, (e.g., vitamin K antagonists [VKA]), have not been adequately studied in medical inpatients. Since VKA take several days to achieve therapeutic anticoagulation, we do not recommend using them de novo as VTE prophylaxis.
However, patients taking an oral VKA in the outpatient setting who have a therapeutic international normalized ratio (INR) during hospitalization probably are adequately protected from VTE and do not need additional pharmacologic prophylaxis. Newer anticoagulants in phase III testing for prevention of VTE in medically ill patients include oral direct thrombin inhibitors and anti-Xa inhibitors. ACCP guidelines recommend either low-dose UFH or LMWH as first-line agents for VTE prevention in medical inpatients.
Unfractionated heparin: UFH is a heterogeneous mixture of repeating polysaccharide chains of varying sizes, averaging about 15,000 Daltons. It binds anti-thrombin III (AT-III) and facilitates AT-III-mediated inactivation of factors IIa, IXa, Xa, and XIIa; of these, IIa and Xa are most responsive to inhibition.
Due to its large size, UFH only is partially absorbed from subcutaneous (SC) tissue, and it has a variable anticoagulant response due to interactions with plasma proteins, macrophages, and endothelial cells.8 However, in prophylactic SC doses (5,000 units two or three times daily), monitoring of the activated partial thromboplastin time (aPTT) is not required. In some cases, (e.g., frail or elderly patients), prophylactic SC doses may slightly prolong the aPTT.
UFH also binds to platelets and platelet factor 4 (PF4), and may precipitate heparin-induced thrombocytopenia (HIT). At least three clinical trials have compared the efficacy of SC UFH with a placebo and found prophylactic doses of UFH decrease the relative risk of DVT as detected by fibrinogen uptake test by about 70% without increasing the risk of bleeding.9-11
Low molecular weight heparins: LMWHs are derived from UFH through a chemical depolymerization, or fractionation, process. They are about one-third the size of UFH, with a molecular weight of approximately 5,000 Daltons.
These smaller molecules are readily absorbed from the SC tissue, eliciting a more predictable anticoagulant response than UFH. Unlike UFH, LMWHs have only minimal nonspecific binding to plasma proteins, endothelial cells, and monocytes, resulting in a predictable dose response. This obviates the need for lab monitoring, even when used in full, therapeutic dosing.
Compared with UFH, these agents have a longer plasma half-life, allowing them to be dosed SC once or twice daily. Also, they don’t bind platelets as readily as UFH resulting in a lower risk of HIT. Because they’re smaller, LMWHs tend to preferentially inhibit factor Xa, whereas UFH tends to inhibit factors Xa and IIa equally.
LMWHs have been evaluated in two large, placebo-controlled clinical trials for the prevention of VTE in medical inpatients.
In the first trial, MEDENOX, almost half the patients were older than 75 (mean age approximately 73). Inclusion criteria were NYHA class 3 or 4 heart failure, acute respiratory failure without mechanical ventilation, acute infection without septic shock, acute rheumatic disease, or inflammatory bowel disease. The primary outcome was assessed in 866 patients. Enoxaparin 40 mg SC once daily decreased the rate of VTE by two-thirds, from 15% to 5% (p=0.0002), without increased bleeding or thrombocytopenia compared with placebo.12 Enoxaparin 40 mg SC once daily is approved by the Food and Drug Administration (FDA) for VTE prophylaxis in medically ill patients.
PREVENT was an international, multicenter, randomized, double-blind, placebo-controlled trial evaluating dalteparin’s efficacy and safety. The inclusion criteria in this trial were acute congestive heart failure, non-ventilator-requiring acute respiratory failure, infection without septic shock, acute rheumatologic disorders, or inflammatory bowel disease. It studied 2,991 patients, and the primary outcome was VTE incidence and sudden death at day 21.
Dalteparin at 5,000 units decreased the rate of VTE, as detected by compression ultrasound, from 5% in the placebo group to 2.8%, a relative risk reduction of 45% (p=0.0015). The authors concluded the use of dalteparin reduced the incidence of VTE without increased risk of bleeding.13 Dalteparin is FDA approved for VTE prophylaxis in medical inpatients.
At least two meta-analyses have evaluated LMWHs compared with UFH. In the first, nine trials comparing LMWH to UFH (4,669 patients) were included. No significant effect was observed on DVT, clinical PE, or mortality. However, LMWH reduced the risk of major hemorrhage by 52% (p=0.049).14
In a more recent meta-analysis, 36 studies were included comparing placebos with UFH and LMWH. Both agents were associated with a reduced risk of VTE. A UFH dosage of 5,000 units three times daily was more effective in preventing DVT than a dosage of 5,000 units twice daily when compared with the control (risk ratio [RR], 0.27; 95% confidence interval [CI], 0.20-0.36; vs. RR, 0.52; 95% CI, 0.28-0.96). Neither UFH nor LMWH reduced mortality. When directly compared with UFH, LMWH was associated with a lower risk of DVT (RR, 0.68; 95% CI, 0.52-0.88) and injection-site hematoma (RR, 0.47; 95% CI, 0.36-0.62), but no difference was seen between the two agents in the risk of bleeding or thrombocytopenia.
This contemporary meta-analysis clearly illustrates that UFH and LMWH reduce VTE risk in hospitalized medical patients, but neither agent alters mortality. When directly compared, LMWH is more effective in preventing DVT.15
Despite the higher drug acquisition costs, LMWHs are more cost-effective than UFH for prophylaxis in medical patients because of their lower complication rates of HIT. LMWH reduces incremental costs by $13.88 per day compared with UFH.16, 17
Synthetic pentasaccharide: Fondaparinux is a synthetic analogue of the unique pentasaccharide sequence that mediates the interaction of heparin with antithrombin. It inhibits both free and platelet-bound factor Xa. It binds antithrombin with high affinity, has close to 100% bioavailability, and has a plasma half-life of 17 hours that permits once-daily administration.
The drug is excreted unchanged in the urine and therefore contraindicated in patients with severe renal impairment (e.g., creatinine clearance less than 30 mL/min). It does not bind PF4 in vitro and thus should not cause HIT.
Fondaparinux has been evaluated in medical inpatients in a randomized placebo controlled trial, ARTEMIS. Fondaparinux 2.5 mg SC once daily decreased the rate of venographically-confirmed DVT from 10.5% to 5.6% (p=0.029); there was also a decrease in fatal PE from 1.7% to 0.7% (p=0.029). A reduction in overall mortality from 6% to 3.3% (P=NS) was observed. Major bleeding occurred in 0.2% of patients in both groups. The drug is not FDA approved to prevent VTE in medical inpatients.18
Duration of therapy: Most clinical trials have used prophylaxis for seven to 14 days. The Extended Clinical Prophylaxis in Acutely Ill Medical Patients (EXCLAIM) trial evaluated duration of therapy, the results of which were presented recently at the 21st Congress of the International Society on Thrombosis and Haemostasis (ISTH).
Of the 5,105 patients who met inclusion criteria, 5,049, or 99%, received open-label prophylaxis with enoxaparin (10 ± four days); 2,013 patients subsequently received extended-duration enoxaparin; and 2,027 received placebo (each for 28 ± four days). Subjects were at least 40 years old, had been recently immobilized (for at least 3 days) and had a predefined acute medical illness. Mobility was defined as level 1 (total bed rest or sedentary) or level 2 (bathroom privileges). After a planned blinded interim analysis, the trial’s data safety monitoring board recommended an amendment to the inclusion criteria, changing level 2 mobility to include age >75 years, and/or prior VTE, and/or diagnosed cancer.
When compared with placebo, extended-duration enoxaparin following the open-label, standard-duration enoxaparin reduced the relative risk of VTE by 44% (2.8% vs. 4.9%; p=0.0011). There was major bleeding in 12 subjects who received extended-duration enoxaparin and three subjects receiving placebo (0.6% vs. 0.1%; p=0.0192).
There was no difference in all-cause mortality between the extended-duration enoxaparin and placebo groups at six months (10.1% vs. 8.9%, p=0.179). The authors concluded 38 days of enoxaparin 40 mg SC once daily significantly reduced the overall incidence of VTE compared with a 10-day regimen in acutely ill medical patients with reduced mobility. This reduction in overall risk for VTE was consistent with a reduction in risk for asymptomatic proximal DVT and symptomatic VTE.
Based on this trial, we would recommend five weeks of prophylaxis for those older than 75 years with prior history of VTE or with active cancer. In the absence of these criteria, we recommend up to 14 days of therapy.
For many patients, this will mean prophylaxis after discharge from the hospital. While this represents a change in practice for many and may significantly complicate some discharge care plans we believe the significant burden of post-hospital VTE mandates a more aggressive approach to peri-hospitalization prophylaxis.
Back to the Case
Our patient has acute decompensated heart failure and likely will be limited in his ability to ambulate. All the clinical trials discussed above included similar patients and support the use of pharmacological prophylaxis. All hospitalized medical patients should undergo VTE risk assessment and implementation of pharmacologic prophylaxis in the absence of contraindications. TH
Dr. Lenchus is an assistant professor of medicine at the University of Miami School of Medicine. Dr. Jaffer is an associate professor of medicine at the University of Miami School of Medicine, where he serves as the chief of the division of hospital medicine.
References
- Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism. A statement for healthcare professionals. Council on Thrombosis (in consultation with the Council on Cardiovascular Radiology), American Heart Association. Circulation. 1996 Jun 15;93(12):2212-2245.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007 Jul 23;167(14):1471-1475.
- Goldhaber SZ, Tapson VF. A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. Am J Cardiol. 2004 Jan 15;93(2):259-262.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest. Sep 2007;132(3):936-945.
- Anderson FA, Jr., Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003 Jun 17;107(23 Suppl 1):I9-16.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med. 2007 Feb 20;146(4):278-288.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):338S-400S.
- Hirsh J, Raschke R. Heparin and low-molecular-weight heparin: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):188S-203S.
- Cade JF, Andrews JT, Stubbs AE. Comparison of sodium and calcium heparin in prevention of venous thromboembolism. Aust N Z J Med. 1982 Oct;12(5):501-504.
- Gallus AS, Hirsh J, Tutle RJ, et al. Small subcutaneous doses of heparin in prevention of venous thrombosis. N Engl J Med. 1973 Mar 15;288(11):545-551.
- Belch JJ, Lowe GD, Ward AG, Forbes CD, Prentice CR. Prevention of deep vein thrombosis in medical patients by low-dose heparin. Scott Med J. 1981 Apr;26(2):115-117.
- Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med. 1999 Sep 9;341(11):793-800.
- Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Vaitkus PT, Goldhaber SZ. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004 Aug 17;110(7):874-879.
- Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost. Jan 2000;83(1):14-19.
- Wein L, Wein S, Haas SJ, Shaw J, Krum H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007 Jul 23;167(14):1476-1486.
- McGarry LJ, Thompson D, Weinstein MC, Goldhaber SZ. Cost effectiveness of thromboprophylaxis with a low-molecular-weight heparin versus unfractionated heparin in acutely ill medical inpatients. Am J Manag Care. 2004 Sep;10(9):632-642.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy. 2006 Oct;26(10):1438-1445.
- Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006 Feb 11;332(7537):325-329.
Case
A 76-year-old gentleman is admitted for progressively worsening dyspnea, cough, and bilateral leg edema. Upon admission, his blood pressure is 150/90 mm/Hg, pulse 90 beats per minute, and respiration is 24 per minute.
Pertinent physical findings include jugular venous distension, bilateral crackles, S3 gallop, and 2+ bilateral lower extremity edema. The chest radiograph shows cardiomegaly and pulmonary edema. He is admitted to the hospital with a diagnosis of acute decompensated heart failure and starts aggressive medical therapy.
Overview
Approximately 2 million cases of deep-vein thrombosis (DVT) occur annually in the United States. Based on studies utilizing ventilation-perfusion scanning, half these patients likely have a silent pulmonary embolism (PE); of these, approximately 250,000 die.
The spectrum of venous thromboembolism (VTE), which includes DVT and PE, can vary from being asymptomatic to sudden death. Autopsy studies suggest a leading cause of sudden death in hospitalized medical patients is often a PE. There also are sequelae, such as chronic pulmonary hypertension, occurring in approximately 5% of PE cases, and post-thrombotic syndrome, occurring in approximately 40% of patients with DVT at two years.1
A recent study suggests DVT occurs three times more commonly in the outpatient setting. However, more than half of these patients were hospitalized in the three months prior.2 This is likely due to inadequate in-hospital prevention because of absence of prophylaxis, use of an unsuitable modality, insufficient dose of the drug, or ineffective duration of therapy. Inadequate and omitted VTE prophylaxis for medical patients was clearly demonstrated in the DVT Free Registry. This registry was created by 183 U.S. hospitals and included 5,451 patients, inpatients, and outpatients with ultrasound-confirmed DVT.
The number of medical inpatients who received prophylaxis in the 30 days prior to diagnosis was 28%—lower than the 48% of surgical patients.3 In a recent international registry, IMPROVE, only approximately 50% of hospitalized patients received prophylaxis.4
Virchow’s triad describes three underlying etiologic factors for thrombosis: stasis of blood flow, endothelial injury, and hypercoagulability. Established VTE risk factors reflect these underlying pathophysiologic processes. Important risk factors for VTE include increasing age, prolonged immobility, malignancy, major surgery, multiple trauma, prior VTE, and chronic heart failure.5
However, the magnitude of risk conferred by these and other risk factors varies (see Table 1, p. 35). It is not known how these factors interact to determine a patient’s individual VTE risk, but there is evidence it increases in proportion to the number of predisposing factors present.
In a recent systematic review of nine studies, including approximately 20,000 patients, prophylaxis reduced the rate of symptomatic VTE in at-risk hospitalized medical patients without increasing major bleeding.6
Multiple healthcare organizations, such as the National Quality Forum (NQF), Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and Agency for Healthcare Research and Quality (AHRQ) have identified VTE as a preventable condition in hospitalized patients. Formal risk assessment must be conducted as a first step, followed by the initiation of timely prophylaxis to improve patient safety.
Review of the Data
Mechanical forms of prophylaxis, such as graduated compression stockings, have been evaluated in patients with stroke and myocardial infarction. Intermittent pneumatic compression stockings and venous foot pumps have not been studied in randomized controlled trials (RCTs) in general medical patients.
Although there is data supporting the efficacy of these devices in surgical patients, the American College of Chest Physicians’ (ACCP) guidelines recommend against the use of mechanical forms of prophylaxis in medical patients unless there is a contraindication to pharmacologic prophylaxis.7
The ideal prophylactic agent is cost-effective and has no side effects. Available pharmacologic options for prevention of VTE in medical patients include unfractionated heparin (UFH), low molecular weight heparins (LMWHs), and the synthetic pentasaccharide, fondaparinux. Oral anticoagulants, (e.g., vitamin K antagonists [VKA]), have not been adequately studied in medical inpatients. Since VKA take several days to achieve therapeutic anticoagulation, we do not recommend using them de novo as VTE prophylaxis.
However, patients taking an oral VKA in the outpatient setting who have a therapeutic international normalized ratio (INR) during hospitalization probably are adequately protected from VTE and do not need additional pharmacologic prophylaxis. Newer anticoagulants in phase III testing for prevention of VTE in medically ill patients include oral direct thrombin inhibitors and anti-Xa inhibitors. ACCP guidelines recommend either low-dose UFH or LMWH as first-line agents for VTE prevention in medical inpatients.
Unfractionated heparin: UFH is a heterogeneous mixture of repeating polysaccharide chains of varying sizes, averaging about 15,000 Daltons. It binds anti-thrombin III (AT-III) and facilitates AT-III-mediated inactivation of factors IIa, IXa, Xa, and XIIa; of these, IIa and Xa are most responsive to inhibition.
Due to its large size, UFH only is partially absorbed from subcutaneous (SC) tissue, and it has a variable anticoagulant response due to interactions with plasma proteins, macrophages, and endothelial cells.8 However, in prophylactic SC doses (5,000 units two or three times daily), monitoring of the activated partial thromboplastin time (aPTT) is not required. In some cases, (e.g., frail or elderly patients), prophylactic SC doses may slightly prolong the aPTT.
UFH also binds to platelets and platelet factor 4 (PF4), and may precipitate heparin-induced thrombocytopenia (HIT). At least three clinical trials have compared the efficacy of SC UFH with a placebo and found prophylactic doses of UFH decrease the relative risk of DVT as detected by fibrinogen uptake test by about 70% without increasing the risk of bleeding.9-11
Low molecular weight heparins: LMWHs are derived from UFH through a chemical depolymerization, or fractionation, process. They are about one-third the size of UFH, with a molecular weight of approximately 5,000 Daltons.
These smaller molecules are readily absorbed from the SC tissue, eliciting a more predictable anticoagulant response than UFH. Unlike UFH, LMWHs have only minimal nonspecific binding to plasma proteins, endothelial cells, and monocytes, resulting in a predictable dose response. This obviates the need for lab monitoring, even when used in full, therapeutic dosing.
Compared with UFH, these agents have a longer plasma half-life, allowing them to be dosed SC once or twice daily. Also, they don’t bind platelets as readily as UFH resulting in a lower risk of HIT. Because they’re smaller, LMWHs tend to preferentially inhibit factor Xa, whereas UFH tends to inhibit factors Xa and IIa equally.
LMWHs have been evaluated in two large, placebo-controlled clinical trials for the prevention of VTE in medical inpatients.
In the first trial, MEDENOX, almost half the patients were older than 75 (mean age approximately 73). Inclusion criteria were NYHA class 3 or 4 heart failure, acute respiratory failure without mechanical ventilation, acute infection without septic shock, acute rheumatic disease, or inflammatory bowel disease. The primary outcome was assessed in 866 patients. Enoxaparin 40 mg SC once daily decreased the rate of VTE by two-thirds, from 15% to 5% (p=0.0002), without increased bleeding or thrombocytopenia compared with placebo.12 Enoxaparin 40 mg SC once daily is approved by the Food and Drug Administration (FDA) for VTE prophylaxis in medically ill patients.
PREVENT was an international, multicenter, randomized, double-blind, placebo-controlled trial evaluating dalteparin’s efficacy and safety. The inclusion criteria in this trial were acute congestive heart failure, non-ventilator-requiring acute respiratory failure, infection without septic shock, acute rheumatologic disorders, or inflammatory bowel disease. It studied 2,991 patients, and the primary outcome was VTE incidence and sudden death at day 21.
Dalteparin at 5,000 units decreased the rate of VTE, as detected by compression ultrasound, from 5% in the placebo group to 2.8%, a relative risk reduction of 45% (p=0.0015). The authors concluded the use of dalteparin reduced the incidence of VTE without increased risk of bleeding.13 Dalteparin is FDA approved for VTE prophylaxis in medical inpatients.
At least two meta-analyses have evaluated LMWHs compared with UFH. In the first, nine trials comparing LMWH to UFH (4,669 patients) were included. No significant effect was observed on DVT, clinical PE, or mortality. However, LMWH reduced the risk of major hemorrhage by 52% (p=0.049).14
In a more recent meta-analysis, 36 studies were included comparing placebos with UFH and LMWH. Both agents were associated with a reduced risk of VTE. A UFH dosage of 5,000 units three times daily was more effective in preventing DVT than a dosage of 5,000 units twice daily when compared with the control (risk ratio [RR], 0.27; 95% confidence interval [CI], 0.20-0.36; vs. RR, 0.52; 95% CI, 0.28-0.96). Neither UFH nor LMWH reduced mortality. When directly compared with UFH, LMWH was associated with a lower risk of DVT (RR, 0.68; 95% CI, 0.52-0.88) and injection-site hematoma (RR, 0.47; 95% CI, 0.36-0.62), but no difference was seen between the two agents in the risk of bleeding or thrombocytopenia.
This contemporary meta-analysis clearly illustrates that UFH and LMWH reduce VTE risk in hospitalized medical patients, but neither agent alters mortality. When directly compared, LMWH is more effective in preventing DVT.15
Despite the higher drug acquisition costs, LMWHs are more cost-effective than UFH for prophylaxis in medical patients because of their lower complication rates of HIT. LMWH reduces incremental costs by $13.88 per day compared with UFH.16, 17
Synthetic pentasaccharide: Fondaparinux is a synthetic analogue of the unique pentasaccharide sequence that mediates the interaction of heparin with antithrombin. It inhibits both free and platelet-bound factor Xa. It binds antithrombin with high affinity, has close to 100% bioavailability, and has a plasma half-life of 17 hours that permits once-daily administration.
The drug is excreted unchanged in the urine and therefore contraindicated in patients with severe renal impairment (e.g., creatinine clearance less than 30 mL/min). It does not bind PF4 in vitro and thus should not cause HIT.
Fondaparinux has been evaluated in medical inpatients in a randomized placebo controlled trial, ARTEMIS. Fondaparinux 2.5 mg SC once daily decreased the rate of venographically-confirmed DVT from 10.5% to 5.6% (p=0.029); there was also a decrease in fatal PE from 1.7% to 0.7% (p=0.029). A reduction in overall mortality from 6% to 3.3% (P=NS) was observed. Major bleeding occurred in 0.2% of patients in both groups. The drug is not FDA approved to prevent VTE in medical inpatients.18
Duration of therapy: Most clinical trials have used prophylaxis for seven to 14 days. The Extended Clinical Prophylaxis in Acutely Ill Medical Patients (EXCLAIM) trial evaluated duration of therapy, the results of which were presented recently at the 21st Congress of the International Society on Thrombosis and Haemostasis (ISTH).
Of the 5,105 patients who met inclusion criteria, 5,049, or 99%, received open-label prophylaxis with enoxaparin (10 ± four days); 2,013 patients subsequently received extended-duration enoxaparin; and 2,027 received placebo (each for 28 ± four days). Subjects were at least 40 years old, had been recently immobilized (for at least 3 days) and had a predefined acute medical illness. Mobility was defined as level 1 (total bed rest or sedentary) or level 2 (bathroom privileges). After a planned blinded interim analysis, the trial’s data safety monitoring board recommended an amendment to the inclusion criteria, changing level 2 mobility to include age >75 years, and/or prior VTE, and/or diagnosed cancer.
When compared with placebo, extended-duration enoxaparin following the open-label, standard-duration enoxaparin reduced the relative risk of VTE by 44% (2.8% vs. 4.9%; p=0.0011). There was major bleeding in 12 subjects who received extended-duration enoxaparin and three subjects receiving placebo (0.6% vs. 0.1%; p=0.0192).
There was no difference in all-cause mortality between the extended-duration enoxaparin and placebo groups at six months (10.1% vs. 8.9%, p=0.179). The authors concluded 38 days of enoxaparin 40 mg SC once daily significantly reduced the overall incidence of VTE compared with a 10-day regimen in acutely ill medical patients with reduced mobility. This reduction in overall risk for VTE was consistent with a reduction in risk for asymptomatic proximal DVT and symptomatic VTE.
Based on this trial, we would recommend five weeks of prophylaxis for those older than 75 years with prior history of VTE or with active cancer. In the absence of these criteria, we recommend up to 14 days of therapy.
For many patients, this will mean prophylaxis after discharge from the hospital. While this represents a change in practice for many and may significantly complicate some discharge care plans we believe the significant burden of post-hospital VTE mandates a more aggressive approach to peri-hospitalization prophylaxis.
Back to the Case
Our patient has acute decompensated heart failure and likely will be limited in his ability to ambulate. All the clinical trials discussed above included similar patients and support the use of pharmacological prophylaxis. All hospitalized medical patients should undergo VTE risk assessment and implementation of pharmacologic prophylaxis in the absence of contraindications. TH
Dr. Lenchus is an assistant professor of medicine at the University of Miami School of Medicine. Dr. Jaffer is an associate professor of medicine at the University of Miami School of Medicine, where he serves as the chief of the division of hospital medicine.
References
- Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism. A statement for healthcare professionals. Council on Thrombosis (in consultation with the Council on Cardiovascular Radiology), American Heart Association. Circulation. 1996 Jun 15;93(12):2212-2245.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007 Jul 23;167(14):1471-1475.
- Goldhaber SZ, Tapson VF. A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. Am J Cardiol. 2004 Jan 15;93(2):259-262.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest. Sep 2007;132(3):936-945.
- Anderson FA, Jr., Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003 Jun 17;107(23 Suppl 1):I9-16.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med. 2007 Feb 20;146(4):278-288.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):338S-400S.
- Hirsh J, Raschke R. Heparin and low-molecular-weight heparin: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):188S-203S.
- Cade JF, Andrews JT, Stubbs AE. Comparison of sodium and calcium heparin in prevention of venous thromboembolism. Aust N Z J Med. 1982 Oct;12(5):501-504.
- Gallus AS, Hirsh J, Tutle RJ, et al. Small subcutaneous doses of heparin in prevention of venous thrombosis. N Engl J Med. 1973 Mar 15;288(11):545-551.
- Belch JJ, Lowe GD, Ward AG, Forbes CD, Prentice CR. Prevention of deep vein thrombosis in medical patients by low-dose heparin. Scott Med J. 1981 Apr;26(2):115-117.
- Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med. 1999 Sep 9;341(11):793-800.
- Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Vaitkus PT, Goldhaber SZ. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004 Aug 17;110(7):874-879.
- Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost. Jan 2000;83(1):14-19.
- Wein L, Wein S, Haas SJ, Shaw J, Krum H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007 Jul 23;167(14):1476-1486.
- McGarry LJ, Thompson D, Weinstein MC, Goldhaber SZ. Cost effectiveness of thromboprophylaxis with a low-molecular-weight heparin versus unfractionated heparin in acutely ill medical inpatients. Am J Manag Care. 2004 Sep;10(9):632-642.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy. 2006 Oct;26(10):1438-1445.
- Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006 Feb 11;332(7537):325-329.
Case
A 76-year-old gentleman is admitted for progressively worsening dyspnea, cough, and bilateral leg edema. Upon admission, his blood pressure is 150/90 mm/Hg, pulse 90 beats per minute, and respiration is 24 per minute.
Pertinent physical findings include jugular venous distension, bilateral crackles, S3 gallop, and 2+ bilateral lower extremity edema. The chest radiograph shows cardiomegaly and pulmonary edema. He is admitted to the hospital with a diagnosis of acute decompensated heart failure and starts aggressive medical therapy.
Overview
Approximately 2 million cases of deep-vein thrombosis (DVT) occur annually in the United States. Based on studies utilizing ventilation-perfusion scanning, half these patients likely have a silent pulmonary embolism (PE); of these, approximately 250,000 die.
The spectrum of venous thromboembolism (VTE), which includes DVT and PE, can vary from being asymptomatic to sudden death. Autopsy studies suggest a leading cause of sudden death in hospitalized medical patients is often a PE. There also are sequelae, such as chronic pulmonary hypertension, occurring in approximately 5% of PE cases, and post-thrombotic syndrome, occurring in approximately 40% of patients with DVT at two years.1
A recent study suggests DVT occurs three times more commonly in the outpatient setting. However, more than half of these patients were hospitalized in the three months prior.2 This is likely due to inadequate in-hospital prevention because of absence of prophylaxis, use of an unsuitable modality, insufficient dose of the drug, or ineffective duration of therapy. Inadequate and omitted VTE prophylaxis for medical patients was clearly demonstrated in the DVT Free Registry. This registry was created by 183 U.S. hospitals and included 5,451 patients, inpatients, and outpatients with ultrasound-confirmed DVT.
The number of medical inpatients who received prophylaxis in the 30 days prior to diagnosis was 28%—lower than the 48% of surgical patients.3 In a recent international registry, IMPROVE, only approximately 50% of hospitalized patients received prophylaxis.4
Virchow’s triad describes three underlying etiologic factors for thrombosis: stasis of blood flow, endothelial injury, and hypercoagulability. Established VTE risk factors reflect these underlying pathophysiologic processes. Important risk factors for VTE include increasing age, prolonged immobility, malignancy, major surgery, multiple trauma, prior VTE, and chronic heart failure.5
However, the magnitude of risk conferred by these and other risk factors varies (see Table 1, p. 35). It is not known how these factors interact to determine a patient’s individual VTE risk, but there is evidence it increases in proportion to the number of predisposing factors present.
In a recent systematic review of nine studies, including approximately 20,000 patients, prophylaxis reduced the rate of symptomatic VTE in at-risk hospitalized medical patients without increasing major bleeding.6
Multiple healthcare organizations, such as the National Quality Forum (NQF), Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and Agency for Healthcare Research and Quality (AHRQ) have identified VTE as a preventable condition in hospitalized patients. Formal risk assessment must be conducted as a first step, followed by the initiation of timely prophylaxis to improve patient safety.
Review of the Data
Mechanical forms of prophylaxis, such as graduated compression stockings, have been evaluated in patients with stroke and myocardial infarction. Intermittent pneumatic compression stockings and venous foot pumps have not been studied in randomized controlled trials (RCTs) in general medical patients.
Although there is data supporting the efficacy of these devices in surgical patients, the American College of Chest Physicians’ (ACCP) guidelines recommend against the use of mechanical forms of prophylaxis in medical patients unless there is a contraindication to pharmacologic prophylaxis.7
The ideal prophylactic agent is cost-effective and has no side effects. Available pharmacologic options for prevention of VTE in medical patients include unfractionated heparin (UFH), low molecular weight heparins (LMWHs), and the synthetic pentasaccharide, fondaparinux. Oral anticoagulants, (e.g., vitamin K antagonists [VKA]), have not been adequately studied in medical inpatients. Since VKA take several days to achieve therapeutic anticoagulation, we do not recommend using them de novo as VTE prophylaxis.
However, patients taking an oral VKA in the outpatient setting who have a therapeutic international normalized ratio (INR) during hospitalization probably are adequately protected from VTE and do not need additional pharmacologic prophylaxis. Newer anticoagulants in phase III testing for prevention of VTE in medically ill patients include oral direct thrombin inhibitors and anti-Xa inhibitors. ACCP guidelines recommend either low-dose UFH or LMWH as first-line agents for VTE prevention in medical inpatients.
Unfractionated heparin: UFH is a heterogeneous mixture of repeating polysaccharide chains of varying sizes, averaging about 15,000 Daltons. It binds anti-thrombin III (AT-III) and facilitates AT-III-mediated inactivation of factors IIa, IXa, Xa, and XIIa; of these, IIa and Xa are most responsive to inhibition.
Due to its large size, UFH only is partially absorbed from subcutaneous (SC) tissue, and it has a variable anticoagulant response due to interactions with plasma proteins, macrophages, and endothelial cells.8 However, in prophylactic SC doses (5,000 units two or three times daily), monitoring of the activated partial thromboplastin time (aPTT) is not required. In some cases, (e.g., frail or elderly patients), prophylactic SC doses may slightly prolong the aPTT.
UFH also binds to platelets and platelet factor 4 (PF4), and may precipitate heparin-induced thrombocytopenia (HIT). At least three clinical trials have compared the efficacy of SC UFH with a placebo and found prophylactic doses of UFH decrease the relative risk of DVT as detected by fibrinogen uptake test by about 70% without increasing the risk of bleeding.9-11
Low molecular weight heparins: LMWHs are derived from UFH through a chemical depolymerization, or fractionation, process. They are about one-third the size of UFH, with a molecular weight of approximately 5,000 Daltons.
These smaller molecules are readily absorbed from the SC tissue, eliciting a more predictable anticoagulant response than UFH. Unlike UFH, LMWHs have only minimal nonspecific binding to plasma proteins, endothelial cells, and monocytes, resulting in a predictable dose response. This obviates the need for lab monitoring, even when used in full, therapeutic dosing.
Compared with UFH, these agents have a longer plasma half-life, allowing them to be dosed SC once or twice daily. Also, they don’t bind platelets as readily as UFH resulting in a lower risk of HIT. Because they’re smaller, LMWHs tend to preferentially inhibit factor Xa, whereas UFH tends to inhibit factors Xa and IIa equally.
LMWHs have been evaluated in two large, placebo-controlled clinical trials for the prevention of VTE in medical inpatients.
In the first trial, MEDENOX, almost half the patients were older than 75 (mean age approximately 73). Inclusion criteria were NYHA class 3 or 4 heart failure, acute respiratory failure without mechanical ventilation, acute infection without septic shock, acute rheumatic disease, or inflammatory bowel disease. The primary outcome was assessed in 866 patients. Enoxaparin 40 mg SC once daily decreased the rate of VTE by two-thirds, from 15% to 5% (p=0.0002), without increased bleeding or thrombocytopenia compared with placebo.12 Enoxaparin 40 mg SC once daily is approved by the Food and Drug Administration (FDA) for VTE prophylaxis in medically ill patients.
PREVENT was an international, multicenter, randomized, double-blind, placebo-controlled trial evaluating dalteparin’s efficacy and safety. The inclusion criteria in this trial were acute congestive heart failure, non-ventilator-requiring acute respiratory failure, infection without septic shock, acute rheumatologic disorders, or inflammatory bowel disease. It studied 2,991 patients, and the primary outcome was VTE incidence and sudden death at day 21.
Dalteparin at 5,000 units decreased the rate of VTE, as detected by compression ultrasound, from 5% in the placebo group to 2.8%, a relative risk reduction of 45% (p=0.0015). The authors concluded the use of dalteparin reduced the incidence of VTE without increased risk of bleeding.13 Dalteparin is FDA approved for VTE prophylaxis in medical inpatients.
At least two meta-analyses have evaluated LMWHs compared with UFH. In the first, nine trials comparing LMWH to UFH (4,669 patients) were included. No significant effect was observed on DVT, clinical PE, or mortality. However, LMWH reduced the risk of major hemorrhage by 52% (p=0.049).14
In a more recent meta-analysis, 36 studies were included comparing placebos with UFH and LMWH. Both agents were associated with a reduced risk of VTE. A UFH dosage of 5,000 units three times daily was more effective in preventing DVT than a dosage of 5,000 units twice daily when compared with the control (risk ratio [RR], 0.27; 95% confidence interval [CI], 0.20-0.36; vs. RR, 0.52; 95% CI, 0.28-0.96). Neither UFH nor LMWH reduced mortality. When directly compared with UFH, LMWH was associated with a lower risk of DVT (RR, 0.68; 95% CI, 0.52-0.88) and injection-site hematoma (RR, 0.47; 95% CI, 0.36-0.62), but no difference was seen between the two agents in the risk of bleeding or thrombocytopenia.
This contemporary meta-analysis clearly illustrates that UFH and LMWH reduce VTE risk in hospitalized medical patients, but neither agent alters mortality. When directly compared, LMWH is more effective in preventing DVT.15
Despite the higher drug acquisition costs, LMWHs are more cost-effective than UFH for prophylaxis in medical patients because of their lower complication rates of HIT. LMWH reduces incremental costs by $13.88 per day compared with UFH.16, 17
Synthetic pentasaccharide: Fondaparinux is a synthetic analogue of the unique pentasaccharide sequence that mediates the interaction of heparin with antithrombin. It inhibits both free and platelet-bound factor Xa. It binds antithrombin with high affinity, has close to 100% bioavailability, and has a plasma half-life of 17 hours that permits once-daily administration.
The drug is excreted unchanged in the urine and therefore contraindicated in patients with severe renal impairment (e.g., creatinine clearance less than 30 mL/min). It does not bind PF4 in vitro and thus should not cause HIT.
Fondaparinux has been evaluated in medical inpatients in a randomized placebo controlled trial, ARTEMIS. Fondaparinux 2.5 mg SC once daily decreased the rate of venographically-confirmed DVT from 10.5% to 5.6% (p=0.029); there was also a decrease in fatal PE from 1.7% to 0.7% (p=0.029). A reduction in overall mortality from 6% to 3.3% (P=NS) was observed. Major bleeding occurred in 0.2% of patients in both groups. The drug is not FDA approved to prevent VTE in medical inpatients.18
Duration of therapy: Most clinical trials have used prophylaxis for seven to 14 days. The Extended Clinical Prophylaxis in Acutely Ill Medical Patients (EXCLAIM) trial evaluated duration of therapy, the results of which were presented recently at the 21st Congress of the International Society on Thrombosis and Haemostasis (ISTH).
Of the 5,105 patients who met inclusion criteria, 5,049, or 99%, received open-label prophylaxis with enoxaparin (10 ± four days); 2,013 patients subsequently received extended-duration enoxaparin; and 2,027 received placebo (each for 28 ± four days). Subjects were at least 40 years old, had been recently immobilized (for at least 3 days) and had a predefined acute medical illness. Mobility was defined as level 1 (total bed rest or sedentary) or level 2 (bathroom privileges). After a planned blinded interim analysis, the trial’s data safety monitoring board recommended an amendment to the inclusion criteria, changing level 2 mobility to include age >75 years, and/or prior VTE, and/or diagnosed cancer.
When compared with placebo, extended-duration enoxaparin following the open-label, standard-duration enoxaparin reduced the relative risk of VTE by 44% (2.8% vs. 4.9%; p=0.0011). There was major bleeding in 12 subjects who received extended-duration enoxaparin and three subjects receiving placebo (0.6% vs. 0.1%; p=0.0192).
There was no difference in all-cause mortality between the extended-duration enoxaparin and placebo groups at six months (10.1% vs. 8.9%, p=0.179). The authors concluded 38 days of enoxaparin 40 mg SC once daily significantly reduced the overall incidence of VTE compared with a 10-day regimen in acutely ill medical patients with reduced mobility. This reduction in overall risk for VTE was consistent with a reduction in risk for asymptomatic proximal DVT and symptomatic VTE.
Based on this trial, we would recommend five weeks of prophylaxis for those older than 75 years with prior history of VTE or with active cancer. In the absence of these criteria, we recommend up to 14 days of therapy.
For many patients, this will mean prophylaxis after discharge from the hospital. While this represents a change in practice for many and may significantly complicate some discharge care plans we believe the significant burden of post-hospital VTE mandates a more aggressive approach to peri-hospitalization prophylaxis.
Back to the Case
Our patient has acute decompensated heart failure and likely will be limited in his ability to ambulate. All the clinical trials discussed above included similar patients and support the use of pharmacological prophylaxis. All hospitalized medical patients should undergo VTE risk assessment and implementation of pharmacologic prophylaxis in the absence of contraindications. TH
Dr. Lenchus is an assistant professor of medicine at the University of Miami School of Medicine. Dr. Jaffer is an associate professor of medicine at the University of Miami School of Medicine, where he serves as the chief of the division of hospital medicine.
References
- Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism. A statement for healthcare professionals. Council on Thrombosis (in consultation with the Council on Cardiovascular Radiology), American Heart Association. Circulation. 1996 Jun 15;93(12):2212-2245.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007 Jul 23;167(14):1471-1475.
- Goldhaber SZ, Tapson VF. A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. Am J Cardiol. 2004 Jan 15;93(2):259-262.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest. Sep 2007;132(3):936-945.
- Anderson FA, Jr., Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003 Jun 17;107(23 Suppl 1):I9-16.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med. 2007 Feb 20;146(4):278-288.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):338S-400S.
- Hirsh J, Raschke R. Heparin and low-molecular-weight heparin: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):188S-203S.
- Cade JF, Andrews JT, Stubbs AE. Comparison of sodium and calcium heparin in prevention of venous thromboembolism. Aust N Z J Med. 1982 Oct;12(5):501-504.
- Gallus AS, Hirsh J, Tutle RJ, et al. Small subcutaneous doses of heparin in prevention of venous thrombosis. N Engl J Med. 1973 Mar 15;288(11):545-551.
- Belch JJ, Lowe GD, Ward AG, Forbes CD, Prentice CR. Prevention of deep vein thrombosis in medical patients by low-dose heparin. Scott Med J. 1981 Apr;26(2):115-117.
- Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med. 1999 Sep 9;341(11):793-800.
- Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Vaitkus PT, Goldhaber SZ. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004 Aug 17;110(7):874-879.
- Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost. Jan 2000;83(1):14-19.
- Wein L, Wein S, Haas SJ, Shaw J, Krum H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007 Jul 23;167(14):1476-1486.
- McGarry LJ, Thompson D, Weinstein MC, Goldhaber SZ. Cost effectiveness of thromboprophylaxis with a low-molecular-weight heparin versus unfractionated heparin in acutely ill medical inpatients. Am J Manag Care. 2004 Sep;10(9):632-642.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy. 2006 Oct;26(10):1438-1445.
- Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006 Feb 11;332(7537):325-329.