User login
ECHO-CT: An Interdisciplinary Videoconference Model for Identifying Potential Postdischarge Transition-of-Care Events
As the population of the United States continues to age, hospitals are seeing an increasing number of older patients with significant medical and social complexity. Medicare data have shown that an increasing number require post–acute care after a hospitalization.1 Discharges to post–acute care settings are often longer and more costly compared with discharges to other settings, which suggests that targeting quality improvement efforts at this transition period may improve the value of care.2
The transition from the hospital setting to a post–acute care facility can be dangerous and complicated due to lapses in communication, medication errors, and the complexity of medical treatment plans. Suboptimal transitions in care can result in adverse events for the patient, as well as confusion in medication regimens or incomplete plans for follow-up care.3
The Project ECHO (Extension for Community Healthcare Outcomes) model was first developed and launched by Sanjeev Arora, MD, in New Mexico in 2003 to expand access to subspecialist care using videoconferencing.4 We first applied this model in 2013 to evaluate the impact of this interdisciplinary videoconferencing tool on the care of patients discharged to post–acute settings.5 We found that patients participating in the Extension for Community Healthcare Outcomes–Care Transitions (ECHO-CT) model experienced decreased risk of rehospitalization, decreased skilled nursing facility (SNF) length of stay, and reduced 30-day healthcare costs, compared with those patients not enrolled in this program; these outcomes were likely due to identification and correction of medication-related errors, improved care coordination, improved disease management, and clarification of goals of care.6 Though these investigations did identify some issues arising during the care transition process, they did not fully describe the types of problems uncovered. We sought to better characterize the clinical and operational issues identified through the ECHO-CT conference, hereafter known as transition-of-care events (TCEs). These issues may include new or evolving medical concerns, an adverse event, or a “near miss.” Identification and classification of TCEs that may contribute to unsafe or fractured care transitions are critical in developing systematic solutions to improve transitions of care, which can ultimately improve patient safety and potentially avoid preventable errors.
METHODS
ECHO-CT Multidisciplinary Video Conference
We conducted ECHO-CT at a large, tertiary care academic medical center. The project design for the ECHO-CT program has been previously described.5 In brief, the program is a weekly, multidisciplinary videoconference between a hospital-based team and post–acute care providers to discuss patients discharged from inpatient services to post–acute care sites, including SNFs and long-term acute care hospitals (LTACHs), during the preceding week. All patients discharged from the tertiary care inpatient site to one of the eight participating SNFs or LTACHs, from either a medical or surgical service, are eligible to be discussed at this weekly interdisciplinary conference. Long-term care facilities were not included in this study. The ECHO-CT program used HIPAA (Health Insurance Portability and Accountability Act)-compliant videoconferencing technology to connect hospital and post–acute care providers.
During the videoconferences, each patient’s hospital course and discharge documentation are reviewed by a hospitalist, and a pharmacist performs a medication reconciliation of each patient’s admission, discharge, and post–acute care medication list. The discharging attending, primary care providers, residents, other trainees, and subspecialist providers are invited to attend. Typically, the interdisciplinary team at the post–acute care sites includes physicians, nurse practitioners, physical therapists, social workers, and case managers. Between 10 and 20 patients are discussed in a case-based format, which includes a summary of the patient’s hospital course, an update from the post–acute care team on the patient’s care, and an opportunity for a discussion regarding any concerns or questions raised by the post–acute care or inpatient care teams. The content and duration of discussion typically lasts approximately 3 to 10 minutes, depending on the needs of the patient and the care team. Each of the eight post–acute care sites participating in the project are assigned a 10- to 15-minute block. A copy of the ECHO-CT session process document is included in the Appendix.
Data Collection
At each interdisciplinary patient review, TCEs were identified and recorded. These events were categorized in real time by the ECHO-CT data collection team into the following categories: medication related, medical, discharge communication/coordination, or other, and recorded in a secured, deidentified database. For individuals whose TCEs could represent more than one category, authors reviewed the available information about the TCEs and determined the most appropriate category; if more than one category was felt to be applicable to a patient’s situation, the events were reclassified into all applicable categories. Data about individual patients, including gender, age at the time of discharge, and other demographic information, were obtained from hospital databases. Number of diagnoses included any diagnosis billed during the patient’s hospital stay, and these data were obtained from a hospital billing database. Average number of medications at discharge was obtained from a hospital pharmacy database.
RESULTS
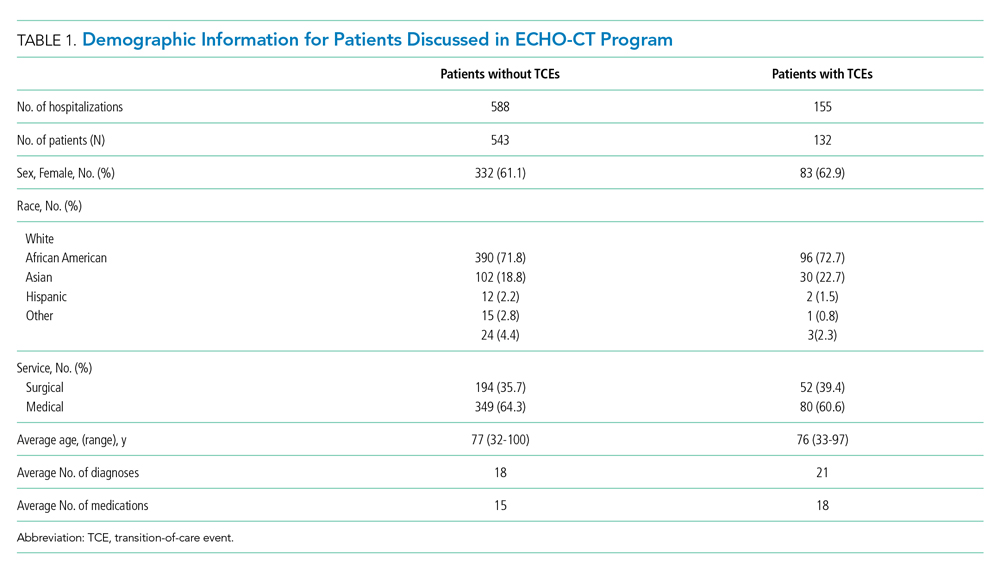
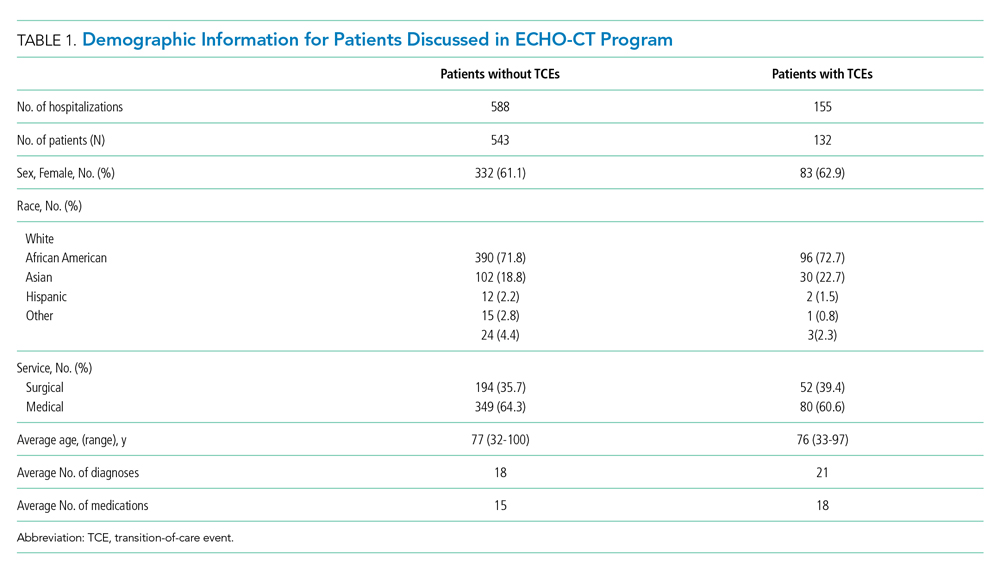
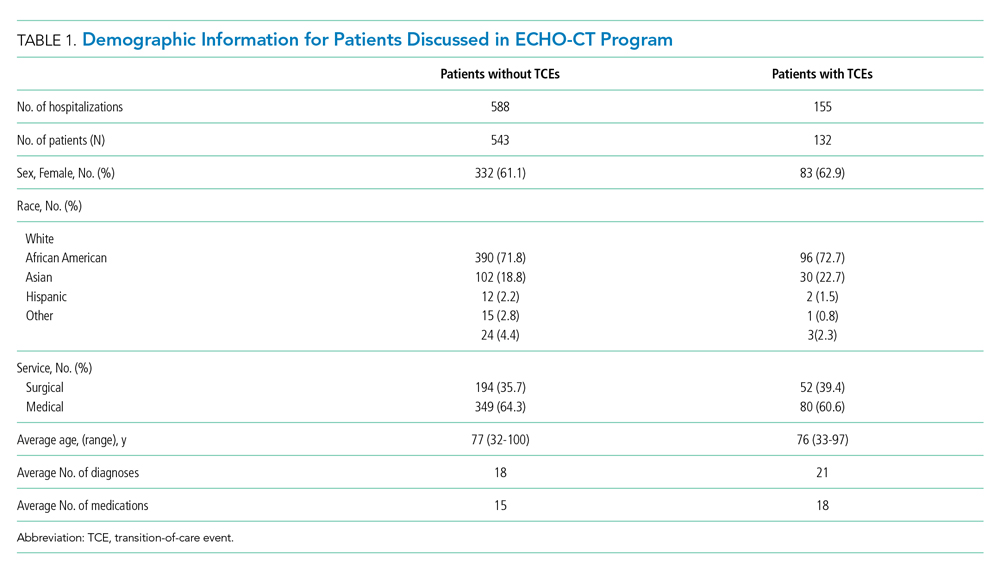
A total of 675 patients (experiencing 743 hospitalizations) were discharged from a medical or surgical service to one of the participating post–acute care sites from January 2016 to October 2018, and were discussed at the interdisciplinary conference. During that time, 139 TCEs were recorded for review, involving 132 patients (Table 1). Patients who experienced TCEs were noted to have a slightly higher average number of diagnoses than did those in the non-TCE group (21 vs 18, respectively) and number of medications (18 vs 15).
Representative examples of TCEs are provided in Table 2. Fifty-eight issues were identified as discharge communication or coordination issues (eg, discharge summary was late or missing at time of discharge to facility, transitional issues were unclear, follow-up appointments were not appropriately scheduled or documented). An additional 52 TCEs were identified as pharmacy or medication issues (eg, medications were inadvertently omitted from discharge medication list, prehospital medication list was incorrect). Medical issues accounted for an additional 27 concerns (eg, patient was hypoglycemic on arrival, inadequate pain control, discovery of new acute medical issues or medical diagnoses that were not clearly documented or communicated by the inpatient team). “Other” issues (two) included unaddressed social concerns, such as insurance issues.

DISCUSSION
The ECHO-CT model unites hospital and post–acute care providers to improve transitions of care and is unique in its focus on the transition from hospital to post–acute care rather than to home care. In 2 years of data collection, we identified several TCEs encompassing a range of concerns. Of the 675 patients discussed, 132 (20%) were noted to have a TCE. When these percentages are applied to the 140 million Medicare hospital discharges that took place during 2000 to 2015, we would estimate nearly 5.5 million TCEs, or 375,000 TCEs per year, that may have affected this population.
The majority of TCEs were communication and coordination errors. Missing or incomplete discharge paperwork, inadequate documentation of inpatient care, and confusion about medical devices or postoperative needs (eg, slings, braces, wound care, drains) were commonly reported. Follow-up appointments with specialists were often not appropriately scheduled or communicated. This may have resulted from unstandardized discharge documentation and a lower priority given to documentation in the setting of multiple clinical demands (eg, direct patient care, complex care coordination, and clinical paperwork and charting). Studies have demonstrated that fewer than one-third of discharge summaries are received by outpatient providers before postdischarge follow-up, and additionally that nearly 40% of patients did not undergo recommended workups for medical issues identified during their hospital stay.7,8 All of this is problematic because appropriate documentation in discharge summaries is associated with a decreased risk of hospital readmission.9
Pharmacy issues were the second most common TCE identified. One member of the post–acute care team noted that “omissions, additions, and replacements” relating to medications were common occurrences. Additionally, it was noted that medications were inadvertently continued for longer than planned or not adjusted appropriately with changing clinical parameters, such as renal function. The results of our analysis are consistent with current literature, which suggests that up to 60% of all medication errors occur during the period surrounding transitions of care.10
There were several limitations to this investigation. Though recording of identified TCEs occurred in real time, analysis of these identified events occurred retrospectively; therefore, investigators had limited ability to retroactively review or recategorize recorded issues, which potentially could have resulted in misclassification or misinterpretation. Additionally, the data were intended to be descriptive; therefore, outcomes such as hospital readmission and patient harm could not be linked to specific TCEs. Furthermore, it is possible that events were not detected by either the postdischarge team or the hospital-based team and, therefore, not captured in this analysis. Further work would be helpful to determine the root causes underlying the identified issues in care transitions, with the goal of improving patient safety and avoiding preventable errors during transitions of care. Although there is comprehensive literature related to errors and medication-related adverse events,11 there is not a consensus of how to classify and report, in a standardized fashion, events arising during the transition period. A validated structure for systematically identifying, monitoring, recording, and reporting issues arising during care transitions will be critical in preventing errors and ensuring patient safety during this high-risk period.
CONCLUSION
Our model is a unique intervention that uses the expertise and engagement of an interdisciplinary team and seeks to identify and remedy issues arising during transitions of care—in real time—to prevent direct harm to vulnerable patients. We have already implemented interventions to improve care based on our experiences with this videoconference-based program. For example, direct feedback was given to discharging teams to improve the discharge summary and associated documentation, and changes to the medication-ordering system were implemented to address specific medication errors discovered. The TCEs identified in this investigation highlight specific areas for improvement with the goal of providing high-quality care for patients and seamless transitions to post–acute care. As health systems and hospitals face new challenges in communication and care coordination, especially due to the recent COVID-19 pandemic, the technology and communication methods used in the ECHO-CT model may become even more relevant for promoting clear communication and patient safety during transitions of care.
Acknowledgment
The ECHO CT team thanks Sabrina Carretie for her contributions in data collection and analysis.
1. Werner RM, Konetzka RT. Trends in post-acute care use among medicare beneficiaries: 2000 to 2015. JAMA. 2018;319(15):1616–1617. https://doi.org/10.1001/jama.2018.2408
2. Tian W. An All-Payer View of Hospital Discharge to Postacute Care, 2013. Statistical Brief #205. Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality; May 2016. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb205-Hospital-Discharge-Postacute-Care.pdf
3. Kessler C, Williams MC, Moustoukas JN, Pappas C. Transitions of care for the geriatric patient in the emergency department. Clin Geriatr Med. 2013;29(1):49-69. https://doi.org/10.1016/j.cger.2012.10.005
4. Arora S, Thornton K, Jenkusky SM, Parish B, Scaletti JV. Project ECHO: linking university specialists with rural and prison-based clinicians to improve care for people with chronic hepatitis C in New Mexico. Public Health Rep. 2007;122(Suppl 2):74-77. https://doi.org/10.1177/00333549071220s214
5. Farris G, Sircar M, Bortinger J, et al. Extension for community healthcare outcomes–care transitions: enhancing geriatric care transitions through a multidisciplinary videoconference. J Am Geriatr Soc. 2017;65(3):598-602. https://doi.org/10.1111/jgs.14690
6. Moore AB, Krupp JE, Dufour AB, et al. Improving transitions to postacute care for elderly patients using a novel video-conferencing program: ECHO-Care transitions. Am J Med. 2017;130(10):1199-1204. https://doi.org/10.1016/j.amjmed.2017.04.041
7. Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. https://doi.org/10.1001/jama.297.8.831
8. Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305-1311. https://doi.org/10.1001/archinte.167.12.1305
9. van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186-192. https://doi.org/10.1046/j.1525-1497.2002.10741.x
10. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167. https://doi.org/10.7326/0003-4819-138-3-200302040-00007
11. Claeys C, Nève J, Tulkens PM, Spinewine A. Content validity and inter-rater reliability of an instrument to characterize unintentional medication discrepancies. Drugs Aging. 2012;29(7):577-591. https://doi.org/10.1007/bf03262275
As the population of the United States continues to age, hospitals are seeing an increasing number of older patients with significant medical and social complexity. Medicare data have shown that an increasing number require post–acute care after a hospitalization.1 Discharges to post–acute care settings are often longer and more costly compared with discharges to other settings, which suggests that targeting quality improvement efforts at this transition period may improve the value of care.2
The transition from the hospital setting to a post–acute care facility can be dangerous and complicated due to lapses in communication, medication errors, and the complexity of medical treatment plans. Suboptimal transitions in care can result in adverse events for the patient, as well as confusion in medication regimens or incomplete plans for follow-up care.3
The Project ECHO (Extension for Community Healthcare Outcomes) model was first developed and launched by Sanjeev Arora, MD, in New Mexico in 2003 to expand access to subspecialist care using videoconferencing.4 We first applied this model in 2013 to evaluate the impact of this interdisciplinary videoconferencing tool on the care of patients discharged to post–acute settings.5 We found that patients participating in the Extension for Community Healthcare Outcomes–Care Transitions (ECHO-CT) model experienced decreased risk of rehospitalization, decreased skilled nursing facility (SNF) length of stay, and reduced 30-day healthcare costs, compared with those patients not enrolled in this program; these outcomes were likely due to identification and correction of medication-related errors, improved care coordination, improved disease management, and clarification of goals of care.6 Though these investigations did identify some issues arising during the care transition process, they did not fully describe the types of problems uncovered. We sought to better characterize the clinical and operational issues identified through the ECHO-CT conference, hereafter known as transition-of-care events (TCEs). These issues may include new or evolving medical concerns, an adverse event, or a “near miss.” Identification and classification of TCEs that may contribute to unsafe or fractured care transitions are critical in developing systematic solutions to improve transitions of care, which can ultimately improve patient safety and potentially avoid preventable errors.
METHODS
ECHO-CT Multidisciplinary Video Conference
We conducted ECHO-CT at a large, tertiary care academic medical center. The project design for the ECHO-CT program has been previously described.5 In brief, the program is a weekly, multidisciplinary videoconference between a hospital-based team and post–acute care providers to discuss patients discharged from inpatient services to post–acute care sites, including SNFs and long-term acute care hospitals (LTACHs), during the preceding week. All patients discharged from the tertiary care inpatient site to one of the eight participating SNFs or LTACHs, from either a medical or surgical service, are eligible to be discussed at this weekly interdisciplinary conference. Long-term care facilities were not included in this study. The ECHO-CT program used HIPAA (Health Insurance Portability and Accountability Act)-compliant videoconferencing technology to connect hospital and post–acute care providers.
During the videoconferences, each patient’s hospital course and discharge documentation are reviewed by a hospitalist, and a pharmacist performs a medication reconciliation of each patient’s admission, discharge, and post–acute care medication list. The discharging attending, primary care providers, residents, other trainees, and subspecialist providers are invited to attend. Typically, the interdisciplinary team at the post–acute care sites includes physicians, nurse practitioners, physical therapists, social workers, and case managers. Between 10 and 20 patients are discussed in a case-based format, which includes a summary of the patient’s hospital course, an update from the post–acute care team on the patient’s care, and an opportunity for a discussion regarding any concerns or questions raised by the post–acute care or inpatient care teams. The content and duration of discussion typically lasts approximately 3 to 10 minutes, depending on the needs of the patient and the care team. Each of the eight post–acute care sites participating in the project are assigned a 10- to 15-minute block. A copy of the ECHO-CT session process document is included in the Appendix.
Data Collection
At each interdisciplinary patient review, TCEs were identified and recorded. These events were categorized in real time by the ECHO-CT data collection team into the following categories: medication related, medical, discharge communication/coordination, or other, and recorded in a secured, deidentified database. For individuals whose TCEs could represent more than one category, authors reviewed the available information about the TCEs and determined the most appropriate category; if more than one category was felt to be applicable to a patient’s situation, the events were reclassified into all applicable categories. Data about individual patients, including gender, age at the time of discharge, and other demographic information, were obtained from hospital databases. Number of diagnoses included any diagnosis billed during the patient’s hospital stay, and these data were obtained from a hospital billing database. Average number of medications at discharge was obtained from a hospital pharmacy database.
RESULTS
A total of 675 patients (experiencing 743 hospitalizations) were discharged from a medical or surgical service to one of the participating post–acute care sites from January 2016 to October 2018, and were discussed at the interdisciplinary conference. During that time, 139 TCEs were recorded for review, involving 132 patients (Table 1). Patients who experienced TCEs were noted to have a slightly higher average number of diagnoses than did those in the non-TCE group (21 vs 18, respectively) and number of medications (18 vs 15).
Representative examples of TCEs are provided in Table 2. Fifty-eight issues were identified as discharge communication or coordination issues (eg, discharge summary was late or missing at time of discharge to facility, transitional issues were unclear, follow-up appointments were not appropriately scheduled or documented). An additional 52 TCEs were identified as pharmacy or medication issues (eg, medications were inadvertently omitted from discharge medication list, prehospital medication list was incorrect). Medical issues accounted for an additional 27 concerns (eg, patient was hypoglycemic on arrival, inadequate pain control, discovery of new acute medical issues or medical diagnoses that were not clearly documented or communicated by the inpatient team). “Other” issues (two) included unaddressed social concerns, such as insurance issues.

DISCUSSION
The ECHO-CT model unites hospital and post–acute care providers to improve transitions of care and is unique in its focus on the transition from hospital to post–acute care rather than to home care. In 2 years of data collection, we identified several TCEs encompassing a range of concerns. Of the 675 patients discussed, 132 (20%) were noted to have a TCE. When these percentages are applied to the 140 million Medicare hospital discharges that took place during 2000 to 2015, we would estimate nearly 5.5 million TCEs, or 375,000 TCEs per year, that may have affected this population.
The majority of TCEs were communication and coordination errors. Missing or incomplete discharge paperwork, inadequate documentation of inpatient care, and confusion about medical devices or postoperative needs (eg, slings, braces, wound care, drains) were commonly reported. Follow-up appointments with specialists were often not appropriately scheduled or communicated. This may have resulted from unstandardized discharge documentation and a lower priority given to documentation in the setting of multiple clinical demands (eg, direct patient care, complex care coordination, and clinical paperwork and charting). Studies have demonstrated that fewer than one-third of discharge summaries are received by outpatient providers before postdischarge follow-up, and additionally that nearly 40% of patients did not undergo recommended workups for medical issues identified during their hospital stay.7,8 All of this is problematic because appropriate documentation in discharge summaries is associated with a decreased risk of hospital readmission.9
Pharmacy issues were the second most common TCE identified. One member of the post–acute care team noted that “omissions, additions, and replacements” relating to medications were common occurrences. Additionally, it was noted that medications were inadvertently continued for longer than planned or not adjusted appropriately with changing clinical parameters, such as renal function. The results of our analysis are consistent with current literature, which suggests that up to 60% of all medication errors occur during the period surrounding transitions of care.10
There were several limitations to this investigation. Though recording of identified TCEs occurred in real time, analysis of these identified events occurred retrospectively; therefore, investigators had limited ability to retroactively review or recategorize recorded issues, which potentially could have resulted in misclassification or misinterpretation. Additionally, the data were intended to be descriptive; therefore, outcomes such as hospital readmission and patient harm could not be linked to specific TCEs. Furthermore, it is possible that events were not detected by either the postdischarge team or the hospital-based team and, therefore, not captured in this analysis. Further work would be helpful to determine the root causes underlying the identified issues in care transitions, with the goal of improving patient safety and avoiding preventable errors during transitions of care. Although there is comprehensive literature related to errors and medication-related adverse events,11 there is not a consensus of how to classify and report, in a standardized fashion, events arising during the transition period. A validated structure for systematically identifying, monitoring, recording, and reporting issues arising during care transitions will be critical in preventing errors and ensuring patient safety during this high-risk period.
CONCLUSION
Our model is a unique intervention that uses the expertise and engagement of an interdisciplinary team and seeks to identify and remedy issues arising during transitions of care—in real time—to prevent direct harm to vulnerable patients. We have already implemented interventions to improve care based on our experiences with this videoconference-based program. For example, direct feedback was given to discharging teams to improve the discharge summary and associated documentation, and changes to the medication-ordering system were implemented to address specific medication errors discovered. The TCEs identified in this investigation highlight specific areas for improvement with the goal of providing high-quality care for patients and seamless transitions to post–acute care. As health systems and hospitals face new challenges in communication and care coordination, especially due to the recent COVID-19 pandemic, the technology and communication methods used in the ECHO-CT model may become even more relevant for promoting clear communication and patient safety during transitions of care.
Acknowledgment
The ECHO CT team thanks Sabrina Carretie for her contributions in data collection and analysis.
As the population of the United States continues to age, hospitals are seeing an increasing number of older patients with significant medical and social complexity. Medicare data have shown that an increasing number require post–acute care after a hospitalization.1 Discharges to post–acute care settings are often longer and more costly compared with discharges to other settings, which suggests that targeting quality improvement efforts at this transition period may improve the value of care.2
The transition from the hospital setting to a post–acute care facility can be dangerous and complicated due to lapses in communication, medication errors, and the complexity of medical treatment plans. Suboptimal transitions in care can result in adverse events for the patient, as well as confusion in medication regimens or incomplete plans for follow-up care.3
The Project ECHO (Extension for Community Healthcare Outcomes) model was first developed and launched by Sanjeev Arora, MD, in New Mexico in 2003 to expand access to subspecialist care using videoconferencing.4 We first applied this model in 2013 to evaluate the impact of this interdisciplinary videoconferencing tool on the care of patients discharged to post–acute settings.5 We found that patients participating in the Extension for Community Healthcare Outcomes–Care Transitions (ECHO-CT) model experienced decreased risk of rehospitalization, decreased skilled nursing facility (SNF) length of stay, and reduced 30-day healthcare costs, compared with those patients not enrolled in this program; these outcomes were likely due to identification and correction of medication-related errors, improved care coordination, improved disease management, and clarification of goals of care.6 Though these investigations did identify some issues arising during the care transition process, they did not fully describe the types of problems uncovered. We sought to better characterize the clinical and operational issues identified through the ECHO-CT conference, hereafter known as transition-of-care events (TCEs). These issues may include new or evolving medical concerns, an adverse event, or a “near miss.” Identification and classification of TCEs that may contribute to unsafe or fractured care transitions are critical in developing systematic solutions to improve transitions of care, which can ultimately improve patient safety and potentially avoid preventable errors.
METHODS
ECHO-CT Multidisciplinary Video Conference
We conducted ECHO-CT at a large, tertiary care academic medical center. The project design for the ECHO-CT program has been previously described.5 In brief, the program is a weekly, multidisciplinary videoconference between a hospital-based team and post–acute care providers to discuss patients discharged from inpatient services to post–acute care sites, including SNFs and long-term acute care hospitals (LTACHs), during the preceding week. All patients discharged from the tertiary care inpatient site to one of the eight participating SNFs or LTACHs, from either a medical or surgical service, are eligible to be discussed at this weekly interdisciplinary conference. Long-term care facilities were not included in this study. The ECHO-CT program used HIPAA (Health Insurance Portability and Accountability Act)-compliant videoconferencing technology to connect hospital and post–acute care providers.
During the videoconferences, each patient’s hospital course and discharge documentation are reviewed by a hospitalist, and a pharmacist performs a medication reconciliation of each patient’s admission, discharge, and post–acute care medication list. The discharging attending, primary care providers, residents, other trainees, and subspecialist providers are invited to attend. Typically, the interdisciplinary team at the post–acute care sites includes physicians, nurse practitioners, physical therapists, social workers, and case managers. Between 10 and 20 patients are discussed in a case-based format, which includes a summary of the patient’s hospital course, an update from the post–acute care team on the patient’s care, and an opportunity for a discussion regarding any concerns or questions raised by the post–acute care or inpatient care teams. The content and duration of discussion typically lasts approximately 3 to 10 minutes, depending on the needs of the patient and the care team. Each of the eight post–acute care sites participating in the project are assigned a 10- to 15-minute block. A copy of the ECHO-CT session process document is included in the Appendix.
Data Collection
At each interdisciplinary patient review, TCEs were identified and recorded. These events were categorized in real time by the ECHO-CT data collection team into the following categories: medication related, medical, discharge communication/coordination, or other, and recorded in a secured, deidentified database. For individuals whose TCEs could represent more than one category, authors reviewed the available information about the TCEs and determined the most appropriate category; if more than one category was felt to be applicable to a patient’s situation, the events were reclassified into all applicable categories. Data about individual patients, including gender, age at the time of discharge, and other demographic information, were obtained from hospital databases. Number of diagnoses included any diagnosis billed during the patient’s hospital stay, and these data were obtained from a hospital billing database. Average number of medications at discharge was obtained from a hospital pharmacy database.
RESULTS
A total of 675 patients (experiencing 743 hospitalizations) were discharged from a medical or surgical service to one of the participating post–acute care sites from January 2016 to October 2018, and were discussed at the interdisciplinary conference. During that time, 139 TCEs were recorded for review, involving 132 patients (Table 1). Patients who experienced TCEs were noted to have a slightly higher average number of diagnoses than did those in the non-TCE group (21 vs 18, respectively) and number of medications (18 vs 15).
Representative examples of TCEs are provided in Table 2. Fifty-eight issues were identified as discharge communication or coordination issues (eg, discharge summary was late or missing at time of discharge to facility, transitional issues were unclear, follow-up appointments were not appropriately scheduled or documented). An additional 52 TCEs were identified as pharmacy or medication issues (eg, medications were inadvertently omitted from discharge medication list, prehospital medication list was incorrect). Medical issues accounted for an additional 27 concerns (eg, patient was hypoglycemic on arrival, inadequate pain control, discovery of new acute medical issues or medical diagnoses that were not clearly documented or communicated by the inpatient team). “Other” issues (two) included unaddressed social concerns, such as insurance issues.

DISCUSSION
The ECHO-CT model unites hospital and post–acute care providers to improve transitions of care and is unique in its focus on the transition from hospital to post–acute care rather than to home care. In 2 years of data collection, we identified several TCEs encompassing a range of concerns. Of the 675 patients discussed, 132 (20%) were noted to have a TCE. When these percentages are applied to the 140 million Medicare hospital discharges that took place during 2000 to 2015, we would estimate nearly 5.5 million TCEs, or 375,000 TCEs per year, that may have affected this population.
The majority of TCEs were communication and coordination errors. Missing or incomplete discharge paperwork, inadequate documentation of inpatient care, and confusion about medical devices or postoperative needs (eg, slings, braces, wound care, drains) were commonly reported. Follow-up appointments with specialists were often not appropriately scheduled or communicated. This may have resulted from unstandardized discharge documentation and a lower priority given to documentation in the setting of multiple clinical demands (eg, direct patient care, complex care coordination, and clinical paperwork and charting). Studies have demonstrated that fewer than one-third of discharge summaries are received by outpatient providers before postdischarge follow-up, and additionally that nearly 40% of patients did not undergo recommended workups for medical issues identified during their hospital stay.7,8 All of this is problematic because appropriate documentation in discharge summaries is associated with a decreased risk of hospital readmission.9
Pharmacy issues were the second most common TCE identified. One member of the post–acute care team noted that “omissions, additions, and replacements” relating to medications were common occurrences. Additionally, it was noted that medications were inadvertently continued for longer than planned or not adjusted appropriately with changing clinical parameters, such as renal function. The results of our analysis are consistent with current literature, which suggests that up to 60% of all medication errors occur during the period surrounding transitions of care.10
There were several limitations to this investigation. Though recording of identified TCEs occurred in real time, analysis of these identified events occurred retrospectively; therefore, investigators had limited ability to retroactively review or recategorize recorded issues, which potentially could have resulted in misclassification or misinterpretation. Additionally, the data were intended to be descriptive; therefore, outcomes such as hospital readmission and patient harm could not be linked to specific TCEs. Furthermore, it is possible that events were not detected by either the postdischarge team or the hospital-based team and, therefore, not captured in this analysis. Further work would be helpful to determine the root causes underlying the identified issues in care transitions, with the goal of improving patient safety and avoiding preventable errors during transitions of care. Although there is comprehensive literature related to errors and medication-related adverse events,11 there is not a consensus of how to classify and report, in a standardized fashion, events arising during the transition period. A validated structure for systematically identifying, monitoring, recording, and reporting issues arising during care transitions will be critical in preventing errors and ensuring patient safety during this high-risk period.
CONCLUSION
Our model is a unique intervention that uses the expertise and engagement of an interdisciplinary team and seeks to identify and remedy issues arising during transitions of care—in real time—to prevent direct harm to vulnerable patients. We have already implemented interventions to improve care based on our experiences with this videoconference-based program. For example, direct feedback was given to discharging teams to improve the discharge summary and associated documentation, and changes to the medication-ordering system were implemented to address specific medication errors discovered. The TCEs identified in this investigation highlight specific areas for improvement with the goal of providing high-quality care for patients and seamless transitions to post–acute care. As health systems and hospitals face new challenges in communication and care coordination, especially due to the recent COVID-19 pandemic, the technology and communication methods used in the ECHO-CT model may become even more relevant for promoting clear communication and patient safety during transitions of care.
Acknowledgment
The ECHO CT team thanks Sabrina Carretie for her contributions in data collection and analysis.
1. Werner RM, Konetzka RT. Trends in post-acute care use among medicare beneficiaries: 2000 to 2015. JAMA. 2018;319(15):1616–1617. https://doi.org/10.1001/jama.2018.2408
2. Tian W. An All-Payer View of Hospital Discharge to Postacute Care, 2013. Statistical Brief #205. Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality; May 2016. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb205-Hospital-Discharge-Postacute-Care.pdf
3. Kessler C, Williams MC, Moustoukas JN, Pappas C. Transitions of care for the geriatric patient in the emergency department. Clin Geriatr Med. 2013;29(1):49-69. https://doi.org/10.1016/j.cger.2012.10.005
4. Arora S, Thornton K, Jenkusky SM, Parish B, Scaletti JV. Project ECHO: linking university specialists with rural and prison-based clinicians to improve care for people with chronic hepatitis C in New Mexico. Public Health Rep. 2007;122(Suppl 2):74-77. https://doi.org/10.1177/00333549071220s214
5. Farris G, Sircar M, Bortinger J, et al. Extension for community healthcare outcomes–care transitions: enhancing geriatric care transitions through a multidisciplinary videoconference. J Am Geriatr Soc. 2017;65(3):598-602. https://doi.org/10.1111/jgs.14690
6. Moore AB, Krupp JE, Dufour AB, et al. Improving transitions to postacute care for elderly patients using a novel video-conferencing program: ECHO-Care transitions. Am J Med. 2017;130(10):1199-1204. https://doi.org/10.1016/j.amjmed.2017.04.041
7. Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. https://doi.org/10.1001/jama.297.8.831
8. Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305-1311. https://doi.org/10.1001/archinte.167.12.1305
9. van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186-192. https://doi.org/10.1046/j.1525-1497.2002.10741.x
10. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167. https://doi.org/10.7326/0003-4819-138-3-200302040-00007
11. Claeys C, Nève J, Tulkens PM, Spinewine A. Content validity and inter-rater reliability of an instrument to characterize unintentional medication discrepancies. Drugs Aging. 2012;29(7):577-591. https://doi.org/10.1007/bf03262275
1. Werner RM, Konetzka RT. Trends in post-acute care use among medicare beneficiaries: 2000 to 2015. JAMA. 2018;319(15):1616–1617. https://doi.org/10.1001/jama.2018.2408
2. Tian W. An All-Payer View of Hospital Discharge to Postacute Care, 2013. Statistical Brief #205. Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality; May 2016. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb205-Hospital-Discharge-Postacute-Care.pdf
3. Kessler C, Williams MC, Moustoukas JN, Pappas C. Transitions of care for the geriatric patient in the emergency department. Clin Geriatr Med. 2013;29(1):49-69. https://doi.org/10.1016/j.cger.2012.10.005
4. Arora S, Thornton K, Jenkusky SM, Parish B, Scaletti JV. Project ECHO: linking university specialists with rural and prison-based clinicians to improve care for people with chronic hepatitis C in New Mexico. Public Health Rep. 2007;122(Suppl 2):74-77. https://doi.org/10.1177/00333549071220s214
5. Farris G, Sircar M, Bortinger J, et al. Extension for community healthcare outcomes–care transitions: enhancing geriatric care transitions through a multidisciplinary videoconference. J Am Geriatr Soc. 2017;65(3):598-602. https://doi.org/10.1111/jgs.14690
6. Moore AB, Krupp JE, Dufour AB, et al. Improving transitions to postacute care for elderly patients using a novel video-conferencing program: ECHO-Care transitions. Am J Med. 2017;130(10):1199-1204. https://doi.org/10.1016/j.amjmed.2017.04.041
7. Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. https://doi.org/10.1001/jama.297.8.831
8. Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305-1311. https://doi.org/10.1001/archinte.167.12.1305
9. van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186-192. https://doi.org/10.1046/j.1525-1497.2002.10741.x
10. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167. https://doi.org/10.7326/0003-4819-138-3-200302040-00007
11. Claeys C, Nève J, Tulkens PM, Spinewine A. Content validity and inter-rater reliability of an instrument to characterize unintentional medication discrepancies. Drugs Aging. 2012;29(7):577-591. https://doi.org/10.1007/bf03262275
© 2021 Society of Hospital Medicine