User login
Acne severity shows negative impact on women’s self esteem
The severity of acne has a substantial negative impact on patients’ self-esteem in different age groups and cultures, with the greatest impact on women and in those with more severe acne, according to the authors of a review of studies that evaluated self-esteem in patients with acne.
Dermatologists Stephanie M. Gallitano, MD, of Columbia University, and Diane S. Berson, MD, of Cornell University, both in New York City, conducted a literature search of studies using the terms “acne vulgaris” and “self-esteem.” They identified 13 studies in 11 countries, including India, Singapore, Brazil, Greece, the United Kingdom, Egypt, South Korea, and Australia.
In the review, published in the International Journal of Women’s Dermatology, they wrote that most of the study authors determined that women with acne were more likely to have a greater degree of feelings that involved self-consciousness, lower self-esteem, and self-worth. In four studies, though, “men and women were equally affected by their disease,” and in one study in Egypt, self-esteem was significantly lower in males with acne than in women with acne, they wrote.
In all the studies, “self-esteem became lower as severity of acne increased,” they observed. There was evidence that subjective perceptions of acne severity affected self-esteem, with a few studies associating subjective evaluations of acne severity, but not objective evaluations, with lower self-esteem. They included a study of 550 students in Turkey, which found “a significant relationship between subjective acne severity and self-esteem but no relationship between objective acne severity and self-esteem.”
Most – between 70% and 80% – of patients used self-prescribed treatments, and 5% to almost 30% had seen a dermatologist. But patients with more severe acne were more likely to have seen a dermatologist, with 61% of those with moderate to severe acne having seen a dermatologist in a Greek study, for example. In addition, in an adult study and in an adolescent study, patients who felt that they had benefited from treatment also had improved self-esteem, improved quality of life, and less anxiety compared with those who did not feel they had benefited from treatment, the authors wrote.
Their review shows that acne “has a substantial negative impact on patients’ self-esteem” and that more severe acne and acne in women “tend to have the greatest impact across cultures,” they concluded.
Read the full study in the International Journal of Women’s Dermatology.
SOURCE: Gallitano S.M, et al. Int J Womens Dermatol 2017 Oct. doi: 10.1016/j.ijwd.2017.10.004
The severity of acne has a substantial negative impact on patients’ self-esteem in different age groups and cultures, with the greatest impact on women and in those with more severe acne, according to the authors of a review of studies that evaluated self-esteem in patients with acne.
Dermatologists Stephanie M. Gallitano, MD, of Columbia University, and Diane S. Berson, MD, of Cornell University, both in New York City, conducted a literature search of studies using the terms “acne vulgaris” and “self-esteem.” They identified 13 studies in 11 countries, including India, Singapore, Brazil, Greece, the United Kingdom, Egypt, South Korea, and Australia.
In the review, published in the International Journal of Women’s Dermatology, they wrote that most of the study authors determined that women with acne were more likely to have a greater degree of feelings that involved self-consciousness, lower self-esteem, and self-worth. In four studies, though, “men and women were equally affected by their disease,” and in one study in Egypt, self-esteem was significantly lower in males with acne than in women with acne, they wrote.
In all the studies, “self-esteem became lower as severity of acne increased,” they observed. There was evidence that subjective perceptions of acne severity affected self-esteem, with a few studies associating subjective evaluations of acne severity, but not objective evaluations, with lower self-esteem. They included a study of 550 students in Turkey, which found “a significant relationship between subjective acne severity and self-esteem but no relationship between objective acne severity and self-esteem.”
Most – between 70% and 80% – of patients used self-prescribed treatments, and 5% to almost 30% had seen a dermatologist. But patients with more severe acne were more likely to have seen a dermatologist, with 61% of those with moderate to severe acne having seen a dermatologist in a Greek study, for example. In addition, in an adult study and in an adolescent study, patients who felt that they had benefited from treatment also had improved self-esteem, improved quality of life, and less anxiety compared with those who did not feel they had benefited from treatment, the authors wrote.
Their review shows that acne “has a substantial negative impact on patients’ self-esteem” and that more severe acne and acne in women “tend to have the greatest impact across cultures,” they concluded.
Read the full study in the International Journal of Women’s Dermatology.
SOURCE: Gallitano S.M, et al. Int J Womens Dermatol 2017 Oct. doi: 10.1016/j.ijwd.2017.10.004
The severity of acne has a substantial negative impact on patients’ self-esteem in different age groups and cultures, with the greatest impact on women and in those with more severe acne, according to the authors of a review of studies that evaluated self-esteem in patients with acne.
Dermatologists Stephanie M. Gallitano, MD, of Columbia University, and Diane S. Berson, MD, of Cornell University, both in New York City, conducted a literature search of studies using the terms “acne vulgaris” and “self-esteem.” They identified 13 studies in 11 countries, including India, Singapore, Brazil, Greece, the United Kingdom, Egypt, South Korea, and Australia.
In the review, published in the International Journal of Women’s Dermatology, they wrote that most of the study authors determined that women with acne were more likely to have a greater degree of feelings that involved self-consciousness, lower self-esteem, and self-worth. In four studies, though, “men and women were equally affected by their disease,” and in one study in Egypt, self-esteem was significantly lower in males with acne than in women with acne, they wrote.
In all the studies, “self-esteem became lower as severity of acne increased,” they observed. There was evidence that subjective perceptions of acne severity affected self-esteem, with a few studies associating subjective evaluations of acne severity, but not objective evaluations, with lower self-esteem. They included a study of 550 students in Turkey, which found “a significant relationship between subjective acne severity and self-esteem but no relationship between objective acne severity and self-esteem.”
Most – between 70% and 80% – of patients used self-prescribed treatments, and 5% to almost 30% had seen a dermatologist. But patients with more severe acne were more likely to have seen a dermatologist, with 61% of those with moderate to severe acne having seen a dermatologist in a Greek study, for example. In addition, in an adult study and in an adolescent study, patients who felt that they had benefited from treatment also had improved self-esteem, improved quality of life, and less anxiety compared with those who did not feel they had benefited from treatment, the authors wrote.
Their review shows that acne “has a substantial negative impact on patients’ self-esteem” and that more severe acne and acne in women “tend to have the greatest impact across cultures,” they concluded.
Read the full study in the International Journal of Women’s Dermatology.
SOURCE: Gallitano S.M, et al. Int J Womens Dermatol 2017 Oct. doi: 10.1016/j.ijwd.2017.10.004
FROM THE INTERNATIONAL JOURNAL OF WOMEN’S DERMATOLOGY
FDA approves first therapy treatment for EGPA
The Food and Drug Administration announced Dec. 12 the approval of mepolizumab (Nucala) to treat adult patients with eosinophilic granulomatosis with polyangiitis (EGPA), making it the first FDA-approved therapy intended to treat this rare disease.
Approval was based on data from a 52-week clinical trial that compared mepolizumab with placebo, according to the FDA. Patients received 300 mg of mepolizumab once every 4 weeks while continuing stable daily oral corticosteroid therapy. Those patients receiving mepolizumab “achieved a significantly greater accrued time in remission compared with placebo,” and a significantly higher proportion of patients receiving 300 mg of mepolizumab had achieved remission at week 36 and week 48, the statement said. Additionally, significantly more patients treated with mepolizumab achieved remission within the first 24 weeks and remained in remission for the remainder of the 52-week study treatment period.
“The expanded indication of Nucala meets a critical, unmet need for EGPA patients. It’s notable that patients taking Nucala in clinical trials reported a significant improvement in their symptoms,” said Badrul Chowdhury, MD, PhD, director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research in the press release announcing the approval. EGPA was formerly known as Churg-Strauss syndrome, the statement pointed out.
Read the full press release on the FDA’s website.
SOURCE: FDA.gov
The Food and Drug Administration announced Dec. 12 the approval of mepolizumab (Nucala) to treat adult patients with eosinophilic granulomatosis with polyangiitis (EGPA), making it the first FDA-approved therapy intended to treat this rare disease.
Approval was based on data from a 52-week clinical trial that compared mepolizumab with placebo, according to the FDA. Patients received 300 mg of mepolizumab once every 4 weeks while continuing stable daily oral corticosteroid therapy. Those patients receiving mepolizumab “achieved a significantly greater accrued time in remission compared with placebo,” and a significantly higher proportion of patients receiving 300 mg of mepolizumab had achieved remission at week 36 and week 48, the statement said. Additionally, significantly more patients treated with mepolizumab achieved remission within the first 24 weeks and remained in remission for the remainder of the 52-week study treatment period.
“The expanded indication of Nucala meets a critical, unmet need for EGPA patients. It’s notable that patients taking Nucala in clinical trials reported a significant improvement in their symptoms,” said Badrul Chowdhury, MD, PhD, director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research in the press release announcing the approval. EGPA was formerly known as Churg-Strauss syndrome, the statement pointed out.
Read the full press release on the FDA’s website.
SOURCE: FDA.gov
The Food and Drug Administration announced Dec. 12 the approval of mepolizumab (Nucala) to treat adult patients with eosinophilic granulomatosis with polyangiitis (EGPA), making it the first FDA-approved therapy intended to treat this rare disease.
Approval was based on data from a 52-week clinical trial that compared mepolizumab with placebo, according to the FDA. Patients received 300 mg of mepolizumab once every 4 weeks while continuing stable daily oral corticosteroid therapy. Those patients receiving mepolizumab “achieved a significantly greater accrued time in remission compared with placebo,” and a significantly higher proportion of patients receiving 300 mg of mepolizumab had achieved remission at week 36 and week 48, the statement said. Additionally, significantly more patients treated with mepolizumab achieved remission within the first 24 weeks and remained in remission for the remainder of the 52-week study treatment period.
“The expanded indication of Nucala meets a critical, unmet need for EGPA patients. It’s notable that patients taking Nucala in clinical trials reported a significant improvement in their symptoms,” said Badrul Chowdhury, MD, PhD, director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research in the press release announcing the approval. EGPA was formerly known as Churg-Strauss syndrome, the statement pointed out.
Read the full press release on the FDA’s website.
SOURCE: FDA.gov
Device-based treatments improved acne in small study, with good safety profile
with a reasonable safety profile, in a small prospective split-face study that compared the two treatments.
Both treatments resulted in similar – and steady – improvements during treatment, but FMR was more effective in long-term maintenance, according to H. H. Kwon, MD, of the Oaro Dermatology Clinic, Seoul, South Korea, and associates.
In the 20-week prospective, randomized, split-face study, published in the Journal of the European Academy of Dermatology and Venereology, 25 Korean patients (Fitzpatrick skin types III or IV), aged 19-37 years, with mild to moderate facial acne, were treated with nonablative 1,450-nm DL and FMR on different sides of their faces every 4 weeks, for a total of three treatments, and were followed up 12 weeks after the third treatment.
During treatment, there were significant improvements in inflammatory acne lesion counts on both sides. At the 12-week follow-up, counts had decreased by 39.3% (from 14.5 at baseline to 9.5) on the DL-treated side and by 58.2% (from 15.6 to 6.0) on the FMR-treated side, a significant difference between the two (P less than .05).
In addition, “both sides demonstrated gradual decreases in sebum output with significant reductions after the second session, and notable difference between the two sides was observed at the follow-up visit,” the authors wrote. Patient self-assessments indicated that they were more satisfied with the degree of improvements in acne, skin texture/enlarged pores, and acne scars on the FMR-treated side.
There was no significant difference in posttreatment erythema and edema associated with the two treatments; mild postinflammatory hyperpigmentation was seen on the DL-treated side in two patients, but not on the FMR-treated side. There were no cases of secondary scarring or infection.
The authors wrote that, as far as they know, this was the first study to compare these two treatments in patients with acne. Based on the results, they concluded, “a few sessions of these devices, as monotherapy or as an element of component of combination therapy, would be a viable option for acne treatment.”
Limitations of the study included the same ethnic background of all the patients, they noted, adding that studies combining treatment with these devices and acne medications in patients with severe acne “would provide clinically interesting data.”
The authors had no disclosures; there was no funding source disclosed.
SOURCE: Kwon HH et al. J Eur Acad Dermatol Venereol. 2017 Nov 24. doi: 10.1111/jdv.14714).
with a reasonable safety profile, in a small prospective split-face study that compared the two treatments.
Both treatments resulted in similar – and steady – improvements during treatment, but FMR was more effective in long-term maintenance, according to H. H. Kwon, MD, of the Oaro Dermatology Clinic, Seoul, South Korea, and associates.
In the 20-week prospective, randomized, split-face study, published in the Journal of the European Academy of Dermatology and Venereology, 25 Korean patients (Fitzpatrick skin types III or IV), aged 19-37 years, with mild to moderate facial acne, were treated with nonablative 1,450-nm DL and FMR on different sides of their faces every 4 weeks, for a total of three treatments, and were followed up 12 weeks after the third treatment.
During treatment, there were significant improvements in inflammatory acne lesion counts on both sides. At the 12-week follow-up, counts had decreased by 39.3% (from 14.5 at baseline to 9.5) on the DL-treated side and by 58.2% (from 15.6 to 6.0) on the FMR-treated side, a significant difference between the two (P less than .05).
In addition, “both sides demonstrated gradual decreases in sebum output with significant reductions after the second session, and notable difference between the two sides was observed at the follow-up visit,” the authors wrote. Patient self-assessments indicated that they were more satisfied with the degree of improvements in acne, skin texture/enlarged pores, and acne scars on the FMR-treated side.
There was no significant difference in posttreatment erythema and edema associated with the two treatments; mild postinflammatory hyperpigmentation was seen on the DL-treated side in two patients, but not on the FMR-treated side. There were no cases of secondary scarring or infection.
The authors wrote that, as far as they know, this was the first study to compare these two treatments in patients with acne. Based on the results, they concluded, “a few sessions of these devices, as monotherapy or as an element of component of combination therapy, would be a viable option for acne treatment.”
Limitations of the study included the same ethnic background of all the patients, they noted, adding that studies combining treatment with these devices and acne medications in patients with severe acne “would provide clinically interesting data.”
The authors had no disclosures; there was no funding source disclosed.
SOURCE: Kwon HH et al. J Eur Acad Dermatol Venereol. 2017 Nov 24. doi: 10.1111/jdv.14714).
with a reasonable safety profile, in a small prospective split-face study that compared the two treatments.
Both treatments resulted in similar – and steady – improvements during treatment, but FMR was more effective in long-term maintenance, according to H. H. Kwon, MD, of the Oaro Dermatology Clinic, Seoul, South Korea, and associates.
In the 20-week prospective, randomized, split-face study, published in the Journal of the European Academy of Dermatology and Venereology, 25 Korean patients (Fitzpatrick skin types III or IV), aged 19-37 years, with mild to moderate facial acne, were treated with nonablative 1,450-nm DL and FMR on different sides of their faces every 4 weeks, for a total of three treatments, and were followed up 12 weeks after the third treatment.
During treatment, there were significant improvements in inflammatory acne lesion counts on both sides. At the 12-week follow-up, counts had decreased by 39.3% (from 14.5 at baseline to 9.5) on the DL-treated side and by 58.2% (from 15.6 to 6.0) on the FMR-treated side, a significant difference between the two (P less than .05).
In addition, “both sides demonstrated gradual decreases in sebum output with significant reductions after the second session, and notable difference between the two sides was observed at the follow-up visit,” the authors wrote. Patient self-assessments indicated that they were more satisfied with the degree of improvements in acne, skin texture/enlarged pores, and acne scars on the FMR-treated side.
There was no significant difference in posttreatment erythema and edema associated with the two treatments; mild postinflammatory hyperpigmentation was seen on the DL-treated side in two patients, but not on the FMR-treated side. There were no cases of secondary scarring or infection.
The authors wrote that, as far as they know, this was the first study to compare these two treatments in patients with acne. Based on the results, they concluded, “a few sessions of these devices, as monotherapy or as an element of component of combination therapy, would be a viable option for acne treatment.”
Limitations of the study included the same ethnic background of all the patients, they noted, adding that studies combining treatment with these devices and acne medications in patients with severe acne “would provide clinically interesting data.”
The authors had no disclosures; there was no funding source disclosed.
SOURCE: Kwon HH et al. J Eur Acad Dermatol Venereol. 2017 Nov 24. doi: 10.1111/jdv.14714).
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Key clinical point: Device-based treatments could be a promising for acne, alone or in combination with other treatments.
Major finding: At follow-up, acne lesion counts had decreased by 39.3% on the DL-treated side and 58.2% on the FMR-treated side (P less than.05).
Study details: A 20-week prospective, randomized, split-face study in 25 Korean patients with mild to moderate facial acne.
Disclosures: The authors had no disclosures; there was no funding source disclosed.
Source: Kwon HH et al. J Eur Acad Dermatol Venereol. 2017 Nov 24. doi: 10.1111/jdv.14714.
Robotic Nissen fundoplication has teaching advantages
Training level affected operative time for laparoscopic Nissen fundoplication, but not for the robotic procedure, according to Maureen D. Moore, MD, and her associates.
Further, in laparoscopic and robotic procedures, junior and senior assistant cohorts had similar outcome measures for estimated blood loss, length of stay, postoperative complications, and 30-day readmission rate.
“The robotic technique offers unique advantages as an educational platform and potentially allows for increased trainee participation without compromising perioperative outcomes,” researchers concluded.
They evaluated surgical times and outcomes for 105 patients; junior assistants (postgraduate year-3 surgery residents) were present in 29 laparoscopic and 44 robotic procedures and senior assistants (minimally invasive surgery fellows) assisted in 18 laparoscopic and 14 robotic procedures.
Median operative time was significantly shorter for the laparoscopic procedures, 112 minutes vs. 157 minutes for the robotic procedures (P less than 0.001). Plus, the median operative time was significantly lower when senior assistants were involved in the laparoscopic procedures, 85 minutes vs. 129 minutes for the junior assistants (P = 0.02).
For the robotic procedures, the median operative times were not significantly different based on the assistant’s level of training, 154 minutes vs. 158 minutes.
Read the full study in the Journal of Surgical Research (doi: 10.1016/j.jss.2017.05.127).
Training level affected operative time for laparoscopic Nissen fundoplication, but not for the robotic procedure, according to Maureen D. Moore, MD, and her associates.
Further, in laparoscopic and robotic procedures, junior and senior assistant cohorts had similar outcome measures for estimated blood loss, length of stay, postoperative complications, and 30-day readmission rate.
“The robotic technique offers unique advantages as an educational platform and potentially allows for increased trainee participation without compromising perioperative outcomes,” researchers concluded.
They evaluated surgical times and outcomes for 105 patients; junior assistants (postgraduate year-3 surgery residents) were present in 29 laparoscopic and 44 robotic procedures and senior assistants (minimally invasive surgery fellows) assisted in 18 laparoscopic and 14 robotic procedures.
Median operative time was significantly shorter for the laparoscopic procedures, 112 minutes vs. 157 minutes for the robotic procedures (P less than 0.001). Plus, the median operative time was significantly lower when senior assistants were involved in the laparoscopic procedures, 85 minutes vs. 129 minutes for the junior assistants (P = 0.02).
For the robotic procedures, the median operative times were not significantly different based on the assistant’s level of training, 154 minutes vs. 158 minutes.
Read the full study in the Journal of Surgical Research (doi: 10.1016/j.jss.2017.05.127).
Training level affected operative time for laparoscopic Nissen fundoplication, but not for the robotic procedure, according to Maureen D. Moore, MD, and her associates.
Further, in laparoscopic and robotic procedures, junior and senior assistant cohorts had similar outcome measures for estimated blood loss, length of stay, postoperative complications, and 30-day readmission rate.
“The robotic technique offers unique advantages as an educational platform and potentially allows for increased trainee participation without compromising perioperative outcomes,” researchers concluded.
They evaluated surgical times and outcomes for 105 patients; junior assistants (postgraduate year-3 surgery residents) were present in 29 laparoscopic and 44 robotic procedures and senior assistants (minimally invasive surgery fellows) assisted in 18 laparoscopic and 14 robotic procedures.
Median operative time was significantly shorter for the laparoscopic procedures, 112 minutes vs. 157 minutes for the robotic procedures (P less than 0.001). Plus, the median operative time was significantly lower when senior assistants were involved in the laparoscopic procedures, 85 minutes vs. 129 minutes for the junior assistants (P = 0.02).
For the robotic procedures, the median operative times were not significantly different based on the assistant’s level of training, 154 minutes vs. 158 minutes.
Read the full study in the Journal of Surgical Research (doi: 10.1016/j.jss.2017.05.127).
FROM THE JOURNAL OF SURGICAL RESEARCH
FDA grants 510k clearance for glucose monitoring system
OptiScan Biomedical Corporation announced Oct. 18 that the Food and Drug Administration has granted 510(k) clearance for the OptiScanner 5000 Glucose Monitoring System.
The clearance allows the device to be used for monitoring plasma glucose levels and determining dysglycemia in surgical intensive care unit (SICU) patients. It is a bedside glucose monitoring system that provides physicians with critical trending and tracking information to manage patient glucose levels in the ICU.
It is estimated that roughly 20% of ICU patients have pre-existing diabetes and an additional 40- to- 60% of ICU patients suffer from “stress hyperglycemia” or a temporary elevation of glucose levels, with all of these patients requiring accurate glucose monitoring to maintain glycemic control.
“There is a broad consensus in the medical community regarding the need for automated, continuous and highly accurate glucose monitoring in the ICU and my experience with the OptiScanner 5000 indicates that this device will play a critical role in delivering this enhanced level of care. I look forward to implementing this technology as soon as possible,” said Grant V. Bochicchio, MD, MPH, FACS, chief of acute and critical care surgery, and Harry Edison Professor of Surgery, Washington University School of Medicine, in a press release.
Read the full press release here.
OptiScan Biomedical Corporation announced Oct. 18 that the Food and Drug Administration has granted 510(k) clearance for the OptiScanner 5000 Glucose Monitoring System.
The clearance allows the device to be used for monitoring plasma glucose levels and determining dysglycemia in surgical intensive care unit (SICU) patients. It is a bedside glucose monitoring system that provides physicians with critical trending and tracking information to manage patient glucose levels in the ICU.
It is estimated that roughly 20% of ICU patients have pre-existing diabetes and an additional 40- to- 60% of ICU patients suffer from “stress hyperglycemia” or a temporary elevation of glucose levels, with all of these patients requiring accurate glucose monitoring to maintain glycemic control.
“There is a broad consensus in the medical community regarding the need for automated, continuous and highly accurate glucose monitoring in the ICU and my experience with the OptiScanner 5000 indicates that this device will play a critical role in delivering this enhanced level of care. I look forward to implementing this technology as soon as possible,” said Grant V. Bochicchio, MD, MPH, FACS, chief of acute and critical care surgery, and Harry Edison Professor of Surgery, Washington University School of Medicine, in a press release.
Read the full press release here.
OptiScan Biomedical Corporation announced Oct. 18 that the Food and Drug Administration has granted 510(k) clearance for the OptiScanner 5000 Glucose Monitoring System.
The clearance allows the device to be used for monitoring plasma glucose levels and determining dysglycemia in surgical intensive care unit (SICU) patients. It is a bedside glucose monitoring system that provides physicians with critical trending and tracking information to manage patient glucose levels in the ICU.
It is estimated that roughly 20% of ICU patients have pre-existing diabetes and an additional 40- to- 60% of ICU patients suffer from “stress hyperglycemia” or a temporary elevation of glucose levels, with all of these patients requiring accurate glucose monitoring to maintain glycemic control.
“There is a broad consensus in the medical community regarding the need for automated, continuous and highly accurate glucose monitoring in the ICU and my experience with the OptiScanner 5000 indicates that this device will play a critical role in delivering this enhanced level of care. I look forward to implementing this technology as soon as possible,” said Grant V. Bochicchio, MD, MPH, FACS, chief of acute and critical care surgery, and Harry Edison Professor of Surgery, Washington University School of Medicine, in a press release.
Read the full press release here.
Multipart collaboration brings data-driven care management tools to patients
One Drop announced on Oct. 31 a multipart collaboration with Fitbit to bring enhanced data-driven care management tools to the diabetes community.
One Drop users will now be able to sync Fitbit intraday data to their One Drop accounts. The first initiative will be to help users better understand the impact of physical activity on blood glucose management. The app software also will analyze user-generated health data points with the goal of gaining deeper insights and improving health outcomes for all people with diabetes worldwide. It can potentially allow users to see how their physical activity impacts blood glucose levels. Users can review these data with their very own Certified Diabetes Educator as they work together to meet personalized health goals.
In a study published in JMIR Diabetes in August 2017, results showed a 1.1%-1.3% absolute reduction in hemoglobin A1C in just 4 months in patients using One Drop. It is noted that this was a more significant reduction than other published research suggested was possible using a mobile care management app.
“By integrating Fitbit data and creating an app for Fitbit Ionic, we will be able to provide our users and their health care providers with more data and deeper insights to better manage their diabetes,” said Jeff Dachis, CEO and founder of One Drop, in a press release.
Read the full press release here.
One Drop announced on Oct. 31 a multipart collaboration with Fitbit to bring enhanced data-driven care management tools to the diabetes community.
One Drop users will now be able to sync Fitbit intraday data to their One Drop accounts. The first initiative will be to help users better understand the impact of physical activity on blood glucose management. The app software also will analyze user-generated health data points with the goal of gaining deeper insights and improving health outcomes for all people with diabetes worldwide. It can potentially allow users to see how their physical activity impacts blood glucose levels. Users can review these data with their very own Certified Diabetes Educator as they work together to meet personalized health goals.
In a study published in JMIR Diabetes in August 2017, results showed a 1.1%-1.3% absolute reduction in hemoglobin A1C in just 4 months in patients using One Drop. It is noted that this was a more significant reduction than other published research suggested was possible using a mobile care management app.
“By integrating Fitbit data and creating an app for Fitbit Ionic, we will be able to provide our users and their health care providers with more data and deeper insights to better manage their diabetes,” said Jeff Dachis, CEO and founder of One Drop, in a press release.
Read the full press release here.
One Drop announced on Oct. 31 a multipart collaboration with Fitbit to bring enhanced data-driven care management tools to the diabetes community.
One Drop users will now be able to sync Fitbit intraday data to their One Drop accounts. The first initiative will be to help users better understand the impact of physical activity on blood glucose management. The app software also will analyze user-generated health data points with the goal of gaining deeper insights and improving health outcomes for all people with diabetes worldwide. It can potentially allow users to see how their physical activity impacts blood glucose levels. Users can review these data with their very own Certified Diabetes Educator as they work together to meet personalized health goals.
In a study published in JMIR Diabetes in August 2017, results showed a 1.1%-1.3% absolute reduction in hemoglobin A1C in just 4 months in patients using One Drop. It is noted that this was a more significant reduction than other published research suggested was possible using a mobile care management app.
“By integrating Fitbit data and creating an app for Fitbit Ionic, we will be able to provide our users and their health care providers with more data and deeper insights to better manage their diabetes,” said Jeff Dachis, CEO and founder of One Drop, in a press release.
Read the full press release here.
FDA approves first extended-release steroid injection for OA knee pain
Flexion Therapeutics announced Oct. 6 the approval of Zilretta (triamcinolone acetonide extended-release injectable suspension) as the first and only extended-release, intra-articular injection for osteoarthritis knee pain.
Zilretta uses a proprietary microsphere-based formulation of triamcinolone acetonide to provide pain relief over 12 weeks by prolonging the release of triamcinolone acetonide inside the synovial fluid. The approval is based on data from a phase 3 clinical trial. The randomized, double-blind study enrolled 484 patients at 37 centers worldwide. The label also includes the results from a double-blind, randomized, parallel-group trial, which examined blood glucose concentrations in patients with type 2 diabetes to show how Zilretta can avoid blood glucose spikes observed with corticosteroid use.
Zilretta is expected to be available in the United States by the end of October.
Flexion Therapeutics announced Oct. 6 the approval of Zilretta (triamcinolone acetonide extended-release injectable suspension) as the first and only extended-release, intra-articular injection for osteoarthritis knee pain.
Zilretta uses a proprietary microsphere-based formulation of triamcinolone acetonide to provide pain relief over 12 weeks by prolonging the release of triamcinolone acetonide inside the synovial fluid. The approval is based on data from a phase 3 clinical trial. The randomized, double-blind study enrolled 484 patients at 37 centers worldwide. The label also includes the results from a double-blind, randomized, parallel-group trial, which examined blood glucose concentrations in patients with type 2 diabetes to show how Zilretta can avoid blood glucose spikes observed with corticosteroid use.
Zilretta is expected to be available in the United States by the end of October.
Flexion Therapeutics announced Oct. 6 the approval of Zilretta (triamcinolone acetonide extended-release injectable suspension) as the first and only extended-release, intra-articular injection for osteoarthritis knee pain.
Zilretta uses a proprietary microsphere-based formulation of triamcinolone acetonide to provide pain relief over 12 weeks by prolonging the release of triamcinolone acetonide inside the synovial fluid. The approval is based on data from a phase 3 clinical trial. The randomized, double-blind study enrolled 484 patients at 37 centers worldwide. The label also includes the results from a double-blind, randomized, parallel-group trial, which examined blood glucose concentrations in patients with type 2 diabetes to show how Zilretta can avoid blood glucose spikes observed with corticosteroid use.
Zilretta is expected to be available in the United States by the end of October.
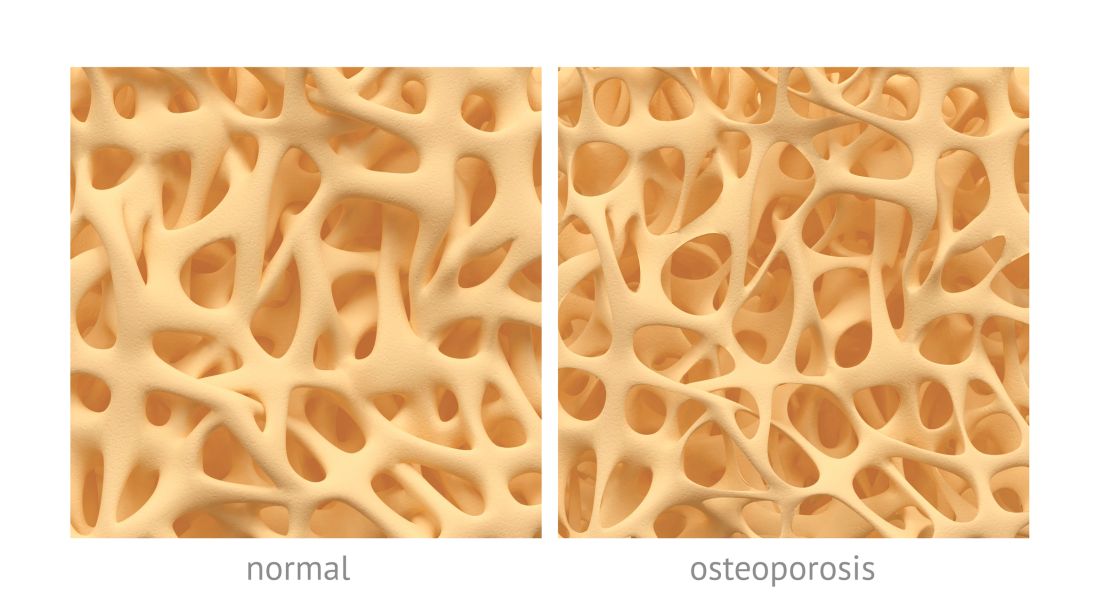
PBC linked to low BMD, increased risk of osteoporosis
Patients with primary biliary cholangitis (PBC) have lower lumbar spine and hip bone mineral density (BMD) and are at an increased risk of osteoporosis and fracture, according to Junyu Fan, MD, and associates.
In a meta-analysis of 210 potentially relevant articles, only 8 met the study’s criteria. Of those, five studies were pooled and the overall relationship between PBC and osteoporosis risk was assessed. Results found a significant association between PBC (n = 504) and the prevalence of osteoporosis (P = .01), compared with the control group (n = 2,052).
The study additionally examined possible connection between PBC and bone fractures; more fracture events were reported in PBC patients (n = 929) than in controls (n = 8,699; P less than .00001). It is noted that there was no publication bias (P = .476).
“Further clinical management, follow-up, and surveillance issues should be addressed with caution,” researchers concluded. “Given the limited number of studies included, more high-quality studies will be required to determine the mechanisms underpinning the relationship between PBC and osteoporosis risk.”
Find the full study in Clinical Rheumatology (2017. doi: 10.1007/s10067-017-3844-x).
Patients with primary biliary cholangitis (PBC) have lower lumbar spine and hip bone mineral density (BMD) and are at an increased risk of osteoporosis and fracture, according to Junyu Fan, MD, and associates.
In a meta-analysis of 210 potentially relevant articles, only 8 met the study’s criteria. Of those, five studies were pooled and the overall relationship between PBC and osteoporosis risk was assessed. Results found a significant association between PBC (n = 504) and the prevalence of osteoporosis (P = .01), compared with the control group (n = 2,052).
The study additionally examined possible connection between PBC and bone fractures; more fracture events were reported in PBC patients (n = 929) than in controls (n = 8,699; P less than .00001). It is noted that there was no publication bias (P = .476).
“Further clinical management, follow-up, and surveillance issues should be addressed with caution,” researchers concluded. “Given the limited number of studies included, more high-quality studies will be required to determine the mechanisms underpinning the relationship between PBC and osteoporosis risk.”
Find the full study in Clinical Rheumatology (2017. doi: 10.1007/s10067-017-3844-x).
Patients with primary biliary cholangitis (PBC) have lower lumbar spine and hip bone mineral density (BMD) and are at an increased risk of osteoporosis and fracture, according to Junyu Fan, MD, and associates.
In a meta-analysis of 210 potentially relevant articles, only 8 met the study’s criteria. Of those, five studies were pooled and the overall relationship between PBC and osteoporosis risk was assessed. Results found a significant association between PBC (n = 504) and the prevalence of osteoporosis (P = .01), compared with the control group (n = 2,052).
The study additionally examined possible connection between PBC and bone fractures; more fracture events were reported in PBC patients (n = 929) than in controls (n = 8,699; P less than .00001). It is noted that there was no publication bias (P = .476).
“Further clinical management, follow-up, and surveillance issues should be addressed with caution,” researchers concluded. “Given the limited number of studies included, more high-quality studies will be required to determine the mechanisms underpinning the relationship between PBC and osteoporosis risk.”
Find the full study in Clinical Rheumatology (2017. doi: 10.1007/s10067-017-3844-x).
FROM CLINICAL RHEUMATOLOGY
Clinical trial: Mesh weights compared for ventral hernia repair
A clinical trial comparing heavy- and medium-weight surgical mesh for ventral hernia repairs is recruiting patients.
The Long-term Results of Heavy Weight Versus Medium Weight Mesh in Ventral Hernia Repair trial will determine if mesh weight has an impact on postoperative pain, ventral hernia recurrence, incidence of deep wound infection, and overall quality of life following ventral hernia repair with mesh.
Patients will be included if they have a ventral hernia, are 18 years of age or older, have a defect classified as CDC wound class 1, are able to achieve midline fascial closure, have a hernia defect width less than or equal to 20 cm, can tolerate general anesthesia, and can give informed consent. Patients will be excluded if they have undergone emergent ventral hernia repair, undergone laparoscopic or robotic ventral hernia repair, undergone staged repair of their ventral hernia, or are pregnant at the time of the surgery.
The primary outcome of this trial is pain that will be measured via the NIH Promis 3A Pain instrument in 1 year postoperatively. Other outcomes include hernia recurrence, to be determined via the Ventral Hernia Recurrence Inventory; the occurrence of a deep wound infection, to be determined by physical examination and/or computed tomography scanning; and quality of life measured by the HerQLes questionnaire.
Find more information at clinicaltrials.gov.
A clinical trial comparing heavy- and medium-weight surgical mesh for ventral hernia repairs is recruiting patients.
The Long-term Results of Heavy Weight Versus Medium Weight Mesh in Ventral Hernia Repair trial will determine if mesh weight has an impact on postoperative pain, ventral hernia recurrence, incidence of deep wound infection, and overall quality of life following ventral hernia repair with mesh.
Patients will be included if they have a ventral hernia, are 18 years of age or older, have a defect classified as CDC wound class 1, are able to achieve midline fascial closure, have a hernia defect width less than or equal to 20 cm, can tolerate general anesthesia, and can give informed consent. Patients will be excluded if they have undergone emergent ventral hernia repair, undergone laparoscopic or robotic ventral hernia repair, undergone staged repair of their ventral hernia, or are pregnant at the time of the surgery.
The primary outcome of this trial is pain that will be measured via the NIH Promis 3A Pain instrument in 1 year postoperatively. Other outcomes include hernia recurrence, to be determined via the Ventral Hernia Recurrence Inventory; the occurrence of a deep wound infection, to be determined by physical examination and/or computed tomography scanning; and quality of life measured by the HerQLes questionnaire.
Find more information at clinicaltrials.gov.
A clinical trial comparing heavy- and medium-weight surgical mesh for ventral hernia repairs is recruiting patients.
The Long-term Results of Heavy Weight Versus Medium Weight Mesh in Ventral Hernia Repair trial will determine if mesh weight has an impact on postoperative pain, ventral hernia recurrence, incidence of deep wound infection, and overall quality of life following ventral hernia repair with mesh.
Patients will be included if they have a ventral hernia, are 18 years of age or older, have a defect classified as CDC wound class 1, are able to achieve midline fascial closure, have a hernia defect width less than or equal to 20 cm, can tolerate general anesthesia, and can give informed consent. Patients will be excluded if they have undergone emergent ventral hernia repair, undergone laparoscopic or robotic ventral hernia repair, undergone staged repair of their ventral hernia, or are pregnant at the time of the surgery.
The primary outcome of this trial is pain that will be measured via the NIH Promis 3A Pain instrument in 1 year postoperatively. Other outcomes include hernia recurrence, to be determined via the Ventral Hernia Recurrence Inventory; the occurrence of a deep wound infection, to be determined by physical examination and/or computed tomography scanning; and quality of life measured by the HerQLes questionnaire.
Find more information at clinicaltrials.gov.
FROM CLINICALTRIALS.GOV
Patients with severe obesity may have difficulty grading pain
Patients with severe obesity may have greater difficulty perceiving and grading pain than do average-weight patients. Those with severe obesity display hypoalgesia when exposed to random noxious stimuli, according to Bart Torensma and his associates.
In the study, 43 patients with severe obesity and 38 controls were enrolled, of whom 41 and 35 participated. Results found the penalty scores, a tool developed to assess perception and grading of pain, differed significantly with higher penalty scores in patients with obesity for both nociceptive assays (heat pain; P = .01, electrical pain; P = .03). “We observed that participants with severe obesity had higher electrical pain threshold and tolerance values, compared with control patients, an indication of lower sensitivity to electrical pain,” the investigators wrote.
In patients with obesity the penalty scores ranged from 1.5 to 13.5 (heat pain) and from 1.0 to 12.5 (electrical pain). But penalty score distribution differed significantly between study groups for electrical pain, with penalty scores greater than 3.5 in 47.3% in patients with obesity versus 22.9% of controls (P = .049). For heat pain, 46.2% of patients with obesity versus 28.6% of control participants had penalty scores greater than 3.5 (P = .15).
“Compared with patients without obesity, patients with obesity displayed hypoalgesia to noxious electrical stimuli together with difficulty in grading experimental noxious thermal and electrical stimuli in between pain threshold and tolerance,” researchers concluded. “We argue that the latter may have a significant effect on pain treatment and consequently needs to be taken into account when treating patients with obesity for acute or chronic pain.”
Read the full study in Surgery for Obesity and Related Diseases (doi: 10.1016/j.soard.2017.01.015).
Patients with severe obesity may have greater difficulty perceiving and grading pain than do average-weight patients. Those with severe obesity display hypoalgesia when exposed to random noxious stimuli, according to Bart Torensma and his associates.
In the study, 43 patients with severe obesity and 38 controls were enrolled, of whom 41 and 35 participated. Results found the penalty scores, a tool developed to assess perception and grading of pain, differed significantly with higher penalty scores in patients with obesity for both nociceptive assays (heat pain; P = .01, electrical pain; P = .03). “We observed that participants with severe obesity had higher electrical pain threshold and tolerance values, compared with control patients, an indication of lower sensitivity to electrical pain,” the investigators wrote.
In patients with obesity the penalty scores ranged from 1.5 to 13.5 (heat pain) and from 1.0 to 12.5 (electrical pain). But penalty score distribution differed significantly between study groups for electrical pain, with penalty scores greater than 3.5 in 47.3% in patients with obesity versus 22.9% of controls (P = .049). For heat pain, 46.2% of patients with obesity versus 28.6% of control participants had penalty scores greater than 3.5 (P = .15).
“Compared with patients without obesity, patients with obesity displayed hypoalgesia to noxious electrical stimuli together with difficulty in grading experimental noxious thermal and electrical stimuli in between pain threshold and tolerance,” researchers concluded. “We argue that the latter may have a significant effect on pain treatment and consequently needs to be taken into account when treating patients with obesity for acute or chronic pain.”
Read the full study in Surgery for Obesity and Related Diseases (doi: 10.1016/j.soard.2017.01.015).
Patients with severe obesity may have greater difficulty perceiving and grading pain than do average-weight patients. Those with severe obesity display hypoalgesia when exposed to random noxious stimuli, according to Bart Torensma and his associates.
In the study, 43 patients with severe obesity and 38 controls were enrolled, of whom 41 and 35 participated. Results found the penalty scores, a tool developed to assess perception and grading of pain, differed significantly with higher penalty scores in patients with obesity for both nociceptive assays (heat pain; P = .01, electrical pain; P = .03). “We observed that participants with severe obesity had higher electrical pain threshold and tolerance values, compared with control patients, an indication of lower sensitivity to electrical pain,” the investigators wrote.
In patients with obesity the penalty scores ranged from 1.5 to 13.5 (heat pain) and from 1.0 to 12.5 (electrical pain). But penalty score distribution differed significantly between study groups for electrical pain, with penalty scores greater than 3.5 in 47.3% in patients with obesity versus 22.9% of controls (P = .049). For heat pain, 46.2% of patients with obesity versus 28.6% of control participants had penalty scores greater than 3.5 (P = .15).
“Compared with patients without obesity, patients with obesity displayed hypoalgesia to noxious electrical stimuli together with difficulty in grading experimental noxious thermal and electrical stimuli in between pain threshold and tolerance,” researchers concluded. “We argue that the latter may have a significant effect on pain treatment and consequently needs to be taken into account when treating patients with obesity for acute or chronic pain.”
Read the full study in Surgery for Obesity and Related Diseases (doi: 10.1016/j.soard.2017.01.015).
FROM SURGERY FOR OBESITY AND RELATED DISEASES