User login
Rash Judgement
A 38-year-old, healthy, incarcerated, African-American man presented with a one-and-a-half year history of an eruption in his axillae. The patient stated that the “rash” worsened with sweating but the lesions were otherwise asymptomatic.
Corticosteroid creams, antifungal creams, and oral antibiotics had not led to any improvement. The eruption progressed to involve his trunk, arms, and face. The skin exam showed hyperpigmented, firm plaques with erythematous papules in the axillae. The plaques were also present on the chest, back, and upper extremities. Verrucous papules were noted on the flexural areas of upper extremities as well as tan colored plaques at the lateral canthi of eyes. (See Figures 1-3 this page.)
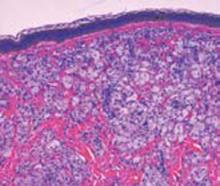
CBC and serum electrolytes were normal. Lipid panel showed a cholesterol of 593 mg/dL, triglycerides 106 mg/dL, high density lipoprotein of 37 g/dL, low density lipoprotein of 535 mg/dL, and very low density lipoprotein of 21 mg/dL. A biopsy from the axilla and the umbilical area were sent for histologic examination. (See Figure 4 this page.)
What is this patient’s most likely diagnosis?
- Sarcoidosis
- Disseminated xanthomas
- Xanthoma disseminatum
- Erythema elevatum diutinum
- Necrobiosis lipoidica
Discussion
The answer is B: disseminated xanthomas. Punch biopsy from the axilla and shave biopsy from the periumbilical area both revealed localized infiltrates of lipid containing macrophages.
Xanthomas develop due to accumulation of lipid-filled macrophages and suggest an underlying disorder of lipid metabolism. Morbidity and mortality are primarily related to atherosclerosis (e.g., coronary artery disease) and pancreatitis, which occur secondarily to the increased lipid levels rather than the xanthoma itself.
In general, four clinical types of xanthomas exist: tendinous, planar, tuberous, and eruptive. A particular diagnosis cannot necessarily be made on the basis of clinical signs; however, certain types of xanthomas are more characteristic of specific hyperlipidemias. Eruptive xanthomas are found in the setting of primary or secondary hypertriglyeridemia. Tuberous xanthomas have both elevated serum cholesterol and triglycerides. This patient had plane xanthomas and xanthelasma and was especially notable for intertriginous plane xanthomas, which can be pathognomonic for homozygous familial hypercholesterolemia.
This patient’s histology from both the periumbilical area and the axilla depict the characteristic presence of vacuolated macrophages (foamy macrophages) to confirm the diagnosis as disseminated xanthoma.1-3 Sarcoidosis is a chronic idiopathic disorder characterized by noncaseating granulomas that can affect any organ system. Cutaneous sarcoidosis typically presents as asymptomatic, red-brown macules and papules affecting the face, periorbital areas, nasolabial folds, and/or extensor surfaces. Typical sarcoid lesions are characterized by the presence of circumscribed granulomas of epithelioid cells with little or no necrosis. The granulomas are characteristically referred to as “naked” due to the sparse lymphocytic infiltrate at the margins.
This patient’s histologic exam did not reveal any granulomas and localized infiltrates of lipid containing macrophages make the diagnosis of cutaneous sarcoidosis unlikely.4,5
Necrobiosis lipoidica (NL) is a cutaneous disorder that is often, but not always, associated with diabetes mellitus. NL is a disorder of collagen degeneration with a granulomatous response, thickening of blood vessel walls, and fat deposition. Patients usually present with asymptomatic shiny patches that slowly enlarge over months to years. The patient’s main complaint is the unsightly cosmetic appearance of the lesions.
Skin lesions of classic NL begin as 1- to 3-mm well-circumscribed papules or nodules that expand with an active border to become waxy, atrophic, round plaques centrally. Initially, these plaques are red-brown in color but progressively become more yellow and atrophic in appearance. Most cases of NL occur on the pretibial area, but cases have been reported on the face, scalp, trunk, and upper extremities where the diagnosis is more likely to be missed.
Although this patient’s mother had diabetes, his fasting blood glucose was well within normal limits (71 mg/dL). Histologically NL displays sclerotic collagen and obliteration of the bundle pattern, with interstitial and palisaded granulomas that involve the subcutaneous tissue and dermis. Fat containing foam cells are often present.
Although our patient’s biopsy showed fat containing foam cells, it did not have the interstitial granulomas or the sclerotic collagen. In addition, the lack of diabetes makes this diagnosis less likely.6,7
Erythema elevatum diutinum (EED) is a rare type of leukocytoclastic vasculitis characterized by red, purple, brown, or yellow papules, plaques, or nodules. These lesions are usually distributed on the extensor surfaces of the body. The lesions are usually asymptomatic but can be associated occasionally with joint pain. Clinical studies show a preference for the extensor surfaces of the hands, the wrists, the elbows, the ankles, the Achilles’ tendons, the fingers, and the toes. The buttocks, the face, and the ears as well as the palms, the soles, the legs, the forearms, and the genitals may be involved; however, the trunk is usually spared. EED is a type of necrotizing vasculitis.
In its early stages, there are no specific histologic findings that can be used to single out the diagnosis of EED from other leukocytoclastic diseases. Although the distribution and lack of symptomatology in EED is reminiscent of our patient, this patient’s lesions were more often found in the flexural areas rather than extensors. In addition, there was no necrotizing vasculitis on histology, which precludes this rare diagnosis of EED.8
Xanthoma disseminatum (XD) is a rare, benign, proliferative disorder in children and young adults characterized by xanthomatous lesions especially in the flexural folds and eyelids. Although it sounds like a disorder of lipid metabolism, it is actually a histiocytic disorder that is not associated with lipoprotein abnormalities and patients are normolipemic. Histologically, it shows mononuclear phagocyte proliferation with Touton giant cells and CD68 positivity on immunophenotyping. It is unlikely that this patient has XD despite the appropriate clinical presentation because histologically all that is found are foam cells. In addition, the patient had a definite lipoprotein abnormality while XD patients are normolipemic.9 TH
References
- Cruz PD, East C, Bergstresser P. Dermal, subcutaneous, and tendon xanthomas: diagnostic markers for specific lipoprotein disorders. J Am Acad Dermatol 1988 Jul;19(1 pt 1):95-111.
- Massengale WT, Nesbitt LT. Xanthomas. In: Bolognia JL, Jorrizo JL, Rapini RP, eds. Dermatology. Vol. 2. London: Mosby; 2003:1447-1454.
- Parker F. Xanthomas and hyperlipidemias. J Am Acad Dermatol. 1985 Jul;13 (1):1-30.
- Young RJ, 3rd, Gilson RT, Yanase D, et al. Cutaneous sarcoidosis. Int J Dermatol. 2001;40:249-253.
- English JC, Patel PJ, Greer KE. Sarcoidosis. J Am Acad Dermatol. 2001;44:725-743: quiz 744-746.
- Fitzpatrick TB, Johnson R, Wolff K, et al. Genetic, metabolic, endocrine and nutritional diseases. Color Atlas and Synopsis of Clinical Dermatology, Common and Serious Diseases. New York: McGraw-Hill; 2001:415-416.
- Lowitt MH, Dover JS. Necrobiosis lipoidica. J Am Acad Dermatol. 1991; 25:735-748.
- Yiannias JA, el-Azhary RA, Gibson LE. Erythema elevatum diutinum: a clinical and histopathologic study of 13 patients. J Am Acad Dermatol 1992 Jan;26(1):38-44.
- Alexander AS, Turner R, Uniate L, et al. Xanthoma disseminatum: a case report and literature review. Br J Radiol 2005 Feb;78(926):153-157.
A 38-year-old, healthy, incarcerated, African-American man presented with a one-and-a-half year history of an eruption in his axillae. The patient stated that the “rash” worsened with sweating but the lesions were otherwise asymptomatic.
Corticosteroid creams, antifungal creams, and oral antibiotics had not led to any improvement. The eruption progressed to involve his trunk, arms, and face. The skin exam showed hyperpigmented, firm plaques with erythematous papules in the axillae. The plaques were also present on the chest, back, and upper extremities. Verrucous papules were noted on the flexural areas of upper extremities as well as tan colored plaques at the lateral canthi of eyes. (See Figures 1-3 this page.)
CBC and serum electrolytes were normal. Lipid panel showed a cholesterol of 593 mg/dL, triglycerides 106 mg/dL, high density lipoprotein of 37 g/dL, low density lipoprotein of 535 mg/dL, and very low density lipoprotein of 21 mg/dL. A biopsy from the axilla and the umbilical area were sent for histologic examination. (See Figure 4 this page.)
What is this patient’s most likely diagnosis?
- Sarcoidosis
- Disseminated xanthomas
- Xanthoma disseminatum
- Erythema elevatum diutinum
- Necrobiosis lipoidica
Discussion
The answer is B: disseminated xanthomas. Punch biopsy from the axilla and shave biopsy from the periumbilical area both revealed localized infiltrates of lipid containing macrophages.
Xanthomas develop due to accumulation of lipid-filled macrophages and suggest an underlying disorder of lipid metabolism. Morbidity and mortality are primarily related to atherosclerosis (e.g., coronary artery disease) and pancreatitis, which occur secondarily to the increased lipid levels rather than the xanthoma itself.
In general, four clinical types of xanthomas exist: tendinous, planar, tuberous, and eruptive. A particular diagnosis cannot necessarily be made on the basis of clinical signs; however, certain types of xanthomas are more characteristic of specific hyperlipidemias. Eruptive xanthomas are found in the setting of primary or secondary hypertriglyeridemia. Tuberous xanthomas have both elevated serum cholesterol and triglycerides. This patient had plane xanthomas and xanthelasma and was especially notable for intertriginous plane xanthomas, which can be pathognomonic for homozygous familial hypercholesterolemia.
This patient’s histology from both the periumbilical area and the axilla depict the characteristic presence of vacuolated macrophages (foamy macrophages) to confirm the diagnosis as disseminated xanthoma.1-3 Sarcoidosis is a chronic idiopathic disorder characterized by noncaseating granulomas that can affect any organ system. Cutaneous sarcoidosis typically presents as asymptomatic, red-brown macules and papules affecting the face, periorbital areas, nasolabial folds, and/or extensor surfaces. Typical sarcoid lesions are characterized by the presence of circumscribed granulomas of epithelioid cells with little or no necrosis. The granulomas are characteristically referred to as “naked” due to the sparse lymphocytic infiltrate at the margins.
This patient’s histologic exam did not reveal any granulomas and localized infiltrates of lipid containing macrophages make the diagnosis of cutaneous sarcoidosis unlikely.4,5
Necrobiosis lipoidica (NL) is a cutaneous disorder that is often, but not always, associated with diabetes mellitus. NL is a disorder of collagen degeneration with a granulomatous response, thickening of blood vessel walls, and fat deposition. Patients usually present with asymptomatic shiny patches that slowly enlarge over months to years. The patient’s main complaint is the unsightly cosmetic appearance of the lesions.
Skin lesions of classic NL begin as 1- to 3-mm well-circumscribed papules or nodules that expand with an active border to become waxy, atrophic, round plaques centrally. Initially, these plaques are red-brown in color but progressively become more yellow and atrophic in appearance. Most cases of NL occur on the pretibial area, but cases have been reported on the face, scalp, trunk, and upper extremities where the diagnosis is more likely to be missed.
Although this patient’s mother had diabetes, his fasting blood glucose was well within normal limits (71 mg/dL). Histologically NL displays sclerotic collagen and obliteration of the bundle pattern, with interstitial and palisaded granulomas that involve the subcutaneous tissue and dermis. Fat containing foam cells are often present.
Although our patient’s biopsy showed fat containing foam cells, it did not have the interstitial granulomas or the sclerotic collagen. In addition, the lack of diabetes makes this diagnosis less likely.6,7
Erythema elevatum diutinum (EED) is a rare type of leukocytoclastic vasculitis characterized by red, purple, brown, or yellow papules, plaques, or nodules. These lesions are usually distributed on the extensor surfaces of the body. The lesions are usually asymptomatic but can be associated occasionally with joint pain. Clinical studies show a preference for the extensor surfaces of the hands, the wrists, the elbows, the ankles, the Achilles’ tendons, the fingers, and the toes. The buttocks, the face, and the ears as well as the palms, the soles, the legs, the forearms, and the genitals may be involved; however, the trunk is usually spared. EED is a type of necrotizing vasculitis.
In its early stages, there are no specific histologic findings that can be used to single out the diagnosis of EED from other leukocytoclastic diseases. Although the distribution and lack of symptomatology in EED is reminiscent of our patient, this patient’s lesions were more often found in the flexural areas rather than extensors. In addition, there was no necrotizing vasculitis on histology, which precludes this rare diagnosis of EED.8
Xanthoma disseminatum (XD) is a rare, benign, proliferative disorder in children and young adults characterized by xanthomatous lesions especially in the flexural folds and eyelids. Although it sounds like a disorder of lipid metabolism, it is actually a histiocytic disorder that is not associated with lipoprotein abnormalities and patients are normolipemic. Histologically, it shows mononuclear phagocyte proliferation with Touton giant cells and CD68 positivity on immunophenotyping. It is unlikely that this patient has XD despite the appropriate clinical presentation because histologically all that is found are foam cells. In addition, the patient had a definite lipoprotein abnormality while XD patients are normolipemic.9 TH
References
- Cruz PD, East C, Bergstresser P. Dermal, subcutaneous, and tendon xanthomas: diagnostic markers for specific lipoprotein disorders. J Am Acad Dermatol 1988 Jul;19(1 pt 1):95-111.
- Massengale WT, Nesbitt LT. Xanthomas. In: Bolognia JL, Jorrizo JL, Rapini RP, eds. Dermatology. Vol. 2. London: Mosby; 2003:1447-1454.
- Parker F. Xanthomas and hyperlipidemias. J Am Acad Dermatol. 1985 Jul;13 (1):1-30.
- Young RJ, 3rd, Gilson RT, Yanase D, et al. Cutaneous sarcoidosis. Int J Dermatol. 2001;40:249-253.
- English JC, Patel PJ, Greer KE. Sarcoidosis. J Am Acad Dermatol. 2001;44:725-743: quiz 744-746.
- Fitzpatrick TB, Johnson R, Wolff K, et al. Genetic, metabolic, endocrine and nutritional diseases. Color Atlas and Synopsis of Clinical Dermatology, Common and Serious Diseases. New York: McGraw-Hill; 2001:415-416.
- Lowitt MH, Dover JS. Necrobiosis lipoidica. J Am Acad Dermatol. 1991; 25:735-748.
- Yiannias JA, el-Azhary RA, Gibson LE. Erythema elevatum diutinum: a clinical and histopathologic study of 13 patients. J Am Acad Dermatol 1992 Jan;26(1):38-44.
- Alexander AS, Turner R, Uniate L, et al. Xanthoma disseminatum: a case report and literature review. Br J Radiol 2005 Feb;78(926):153-157.
A 38-year-old, healthy, incarcerated, African-American man presented with a one-and-a-half year history of an eruption in his axillae. The patient stated that the “rash” worsened with sweating but the lesions were otherwise asymptomatic.
Corticosteroid creams, antifungal creams, and oral antibiotics had not led to any improvement. The eruption progressed to involve his trunk, arms, and face. The skin exam showed hyperpigmented, firm plaques with erythematous papules in the axillae. The plaques were also present on the chest, back, and upper extremities. Verrucous papules were noted on the flexural areas of upper extremities as well as tan colored plaques at the lateral canthi of eyes. (See Figures 1-3 this page.)
CBC and serum electrolytes were normal. Lipid panel showed a cholesterol of 593 mg/dL, triglycerides 106 mg/dL, high density lipoprotein of 37 g/dL, low density lipoprotein of 535 mg/dL, and very low density lipoprotein of 21 mg/dL. A biopsy from the axilla and the umbilical area were sent for histologic examination. (See Figure 4 this page.)
What is this patient’s most likely diagnosis?
- Sarcoidosis
- Disseminated xanthomas
- Xanthoma disseminatum
- Erythema elevatum diutinum
- Necrobiosis lipoidica
Discussion
The answer is B: disseminated xanthomas. Punch biopsy from the axilla and shave biopsy from the periumbilical area both revealed localized infiltrates of lipid containing macrophages.
Xanthomas develop due to accumulation of lipid-filled macrophages and suggest an underlying disorder of lipid metabolism. Morbidity and mortality are primarily related to atherosclerosis (e.g., coronary artery disease) and pancreatitis, which occur secondarily to the increased lipid levels rather than the xanthoma itself.
In general, four clinical types of xanthomas exist: tendinous, planar, tuberous, and eruptive. A particular diagnosis cannot necessarily be made on the basis of clinical signs; however, certain types of xanthomas are more characteristic of specific hyperlipidemias. Eruptive xanthomas are found in the setting of primary or secondary hypertriglyeridemia. Tuberous xanthomas have both elevated serum cholesterol and triglycerides. This patient had plane xanthomas and xanthelasma and was especially notable for intertriginous plane xanthomas, which can be pathognomonic for homozygous familial hypercholesterolemia.
This patient’s histology from both the periumbilical area and the axilla depict the characteristic presence of vacuolated macrophages (foamy macrophages) to confirm the diagnosis as disseminated xanthoma.1-3 Sarcoidosis is a chronic idiopathic disorder characterized by noncaseating granulomas that can affect any organ system. Cutaneous sarcoidosis typically presents as asymptomatic, red-brown macules and papules affecting the face, periorbital areas, nasolabial folds, and/or extensor surfaces. Typical sarcoid lesions are characterized by the presence of circumscribed granulomas of epithelioid cells with little or no necrosis. The granulomas are characteristically referred to as “naked” due to the sparse lymphocytic infiltrate at the margins.
This patient’s histologic exam did not reveal any granulomas and localized infiltrates of lipid containing macrophages make the diagnosis of cutaneous sarcoidosis unlikely.4,5
Necrobiosis lipoidica (NL) is a cutaneous disorder that is often, but not always, associated with diabetes mellitus. NL is a disorder of collagen degeneration with a granulomatous response, thickening of blood vessel walls, and fat deposition. Patients usually present with asymptomatic shiny patches that slowly enlarge over months to years. The patient’s main complaint is the unsightly cosmetic appearance of the lesions.
Skin lesions of classic NL begin as 1- to 3-mm well-circumscribed papules or nodules that expand with an active border to become waxy, atrophic, round plaques centrally. Initially, these plaques are red-brown in color but progressively become more yellow and atrophic in appearance. Most cases of NL occur on the pretibial area, but cases have been reported on the face, scalp, trunk, and upper extremities where the diagnosis is more likely to be missed.
Although this patient’s mother had diabetes, his fasting blood glucose was well within normal limits (71 mg/dL). Histologically NL displays sclerotic collagen and obliteration of the bundle pattern, with interstitial and palisaded granulomas that involve the subcutaneous tissue and dermis. Fat containing foam cells are often present.
Although our patient’s biopsy showed fat containing foam cells, it did not have the interstitial granulomas or the sclerotic collagen. In addition, the lack of diabetes makes this diagnosis less likely.6,7
Erythema elevatum diutinum (EED) is a rare type of leukocytoclastic vasculitis characterized by red, purple, brown, or yellow papules, plaques, or nodules. These lesions are usually distributed on the extensor surfaces of the body. The lesions are usually asymptomatic but can be associated occasionally with joint pain. Clinical studies show a preference for the extensor surfaces of the hands, the wrists, the elbows, the ankles, the Achilles’ tendons, the fingers, and the toes. The buttocks, the face, and the ears as well as the palms, the soles, the legs, the forearms, and the genitals may be involved; however, the trunk is usually spared. EED is a type of necrotizing vasculitis.
In its early stages, there are no specific histologic findings that can be used to single out the diagnosis of EED from other leukocytoclastic diseases. Although the distribution and lack of symptomatology in EED is reminiscent of our patient, this patient’s lesions were more often found in the flexural areas rather than extensors. In addition, there was no necrotizing vasculitis on histology, which precludes this rare diagnosis of EED.8
Xanthoma disseminatum (XD) is a rare, benign, proliferative disorder in children and young adults characterized by xanthomatous lesions especially in the flexural folds and eyelids. Although it sounds like a disorder of lipid metabolism, it is actually a histiocytic disorder that is not associated with lipoprotein abnormalities and patients are normolipemic. Histologically, it shows mononuclear phagocyte proliferation with Touton giant cells and CD68 positivity on immunophenotyping. It is unlikely that this patient has XD despite the appropriate clinical presentation because histologically all that is found are foam cells. In addition, the patient had a definite lipoprotein abnormality while XD patients are normolipemic.9 TH
References
- Cruz PD, East C, Bergstresser P. Dermal, subcutaneous, and tendon xanthomas: diagnostic markers for specific lipoprotein disorders. J Am Acad Dermatol 1988 Jul;19(1 pt 1):95-111.
- Massengale WT, Nesbitt LT. Xanthomas. In: Bolognia JL, Jorrizo JL, Rapini RP, eds. Dermatology. Vol. 2. London: Mosby; 2003:1447-1454.
- Parker F. Xanthomas and hyperlipidemias. J Am Acad Dermatol. 1985 Jul;13 (1):1-30.
- Young RJ, 3rd, Gilson RT, Yanase D, et al. Cutaneous sarcoidosis. Int J Dermatol. 2001;40:249-253.
- English JC, Patel PJ, Greer KE. Sarcoidosis. J Am Acad Dermatol. 2001;44:725-743: quiz 744-746.
- Fitzpatrick TB, Johnson R, Wolff K, et al. Genetic, metabolic, endocrine and nutritional diseases. Color Atlas and Synopsis of Clinical Dermatology, Common and Serious Diseases. New York: McGraw-Hill; 2001:415-416.
- Lowitt MH, Dover JS. Necrobiosis lipoidica. J Am Acad Dermatol. 1991; 25:735-748.
- Yiannias JA, el-Azhary RA, Gibson LE. Erythema elevatum diutinum: a clinical and histopathologic study of 13 patients. J Am Acad Dermatol 1992 Jan;26(1):38-44.
- Alexander AS, Turner R, Uniate L, et al. Xanthoma disseminatum: a case report and literature review. Br J Radiol 2005 Feb;78(926):153-157.