User login
Driving-Related Coping Thoughts in Post-9/11 Combat Veterans With and Without Comorbid PTSD and TBI
Combat veterans who have served in Iraq and Afghanistan in the post-9/11 era face unique reintegration challenges, one being the transition from driving in combat zones to driving at home.1 Relative to previous conflicts, post-9/11 combat involves increased participation in road patrols and convoys along with more prevalent threats of improvised explosive devices (IEDs).1,2 Roadside ambushes designed to destroy or stop vehicles became a common warfare strategy, meaning that driving became an inherently dangerous combat maneuver.3
The modern combat driving framework includes cognitive tools (eg, targeted aggression and tactical awareness) combined with specific behaviors (eg, driving unpredictably fast, using rapid lane changes, and keeping other vehicles at a distance to avoid IEDs).4 This framework is adaptive and lifesaving in combat zones, but it can be maladaptive and dangerous in civilian environments. Service members face difficulty in updating this cognitive framework after leaving combat zones and may continue to experience specific cognitions (eg, “the world is dangerous”; “that car holds an IED”) while driving on civilian roads.3,5-8
The high prevalence of posttraumatic stress disorder (PTSD) and traumatic brain injury (TBI) in post-9/11 veterans may complicate reintegration. Both PTSD and TBI are considered signature wounds of these conflicts.8-11 Traumatic brain injury may be sustained as a result of blast injury or other mechanism, including a closed head injury or penetrating brain injury.10 Previous literature indicated that both PTSD and TBI across all severities are related to deficits in executive functioning, attention, and memory.12-16
In addition to cognitive deficits, veterans with PTSD also may experience cognitive misappraisal, in which they are more likely to perceive ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations.5,17,18 Examples of roadside-specific trauma triggers include busy highways, traffic, loud or distracting noises, and vehicles of similar make and model as those commonly rigged with IEDs in Iraq or Afghanistan.2,7
Blast injury
Prior research suggests that veterans with PTSD and/or TBI experience significantly higher levels of anxiety in response to common roadside stimuli (ie, an overpass or stop sign) while driving than do veterans without either PTSD or TBI.3 Cognitive behavioral therapy (CBT) interventions have been developed and systematically evaluated for treating anxiety.21 The goal of CBT is to identify and change dysfunctional cognitions that result in biased information processing. Cognitive restructuring, the process by which problematic cognitions (negative automatic thoughts) are identified and examined for distortions, is one method of accomplishing this goal. Distortions then are disputed and rebutted with assistance from the clinician.22 A strategy for restructuring negative automatic thoughts is coping self-instruction, which centers on identifying when negative automatic thoughts are focused on others’ behavior, accepting that their behavior cannot be changed, and using positive coping behaviors to minimize negative automatic thoughts.23
The link between history of comorbid PTSD and TBI and combat driving, current driving anxiety, and coping strategies has not yet been extensively studied in veterans. Thus, the aim of the current study is to determine whether veterans with comorbid PTSD and TBI utilize coping self-instruction behind the wheel. Driving-specific coping self-instruction involves generating thoughts that are adaptive and accepting of others’ driving behaviors (eg, “Just turn up the radio and tune them out”). It was hypothesized that veterans with comorbid PTSD and TBI would endorse fewer coping self-instruction thoughts than would veterans without either PTSD or TBI.
Methods
The current project is part of a larger study that examines driving behaviors of post-9/11 combat veterans at the Michael J. Crescenz Veterans Affairs Medical Center in Philadelphia, Pennsylvania. Thirty-two male veterans aged between 22 and 48 years (M = 31.6, SD = 6.9) were included in the sample. Twenty-three were diagnosed with comorbid PTSD and TBI and 9 veterans with no major psychiatric or physical
Assessment
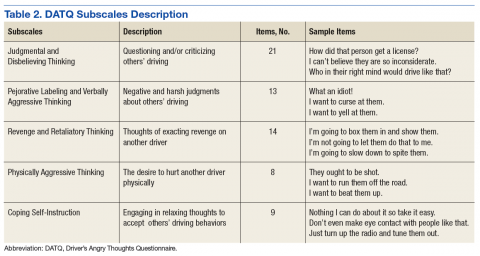
All participants completed a battery of questionnaires, including the Driver’s Angry Thoughts Questionnaire (DATQ).23 The DATQ was used to investigate the specific thoughts that veterans experienced while driving.23 Participants indicated on a Likert scale from 1 (not at all) to 5 (all the time) how often they experienced any of 65 thoughts while driving. Each item was categorized into 1 of 5 distinct subscales (Table 2). A frequency score was generated for each of the 5 subscales. Each subscale had good internal consistency and convergent, divergent, and predictive validity. The Coping Self-Instruction subscale, which is defined as engaging in relaxing thoughts to accept others’ driving behaviors, was of primary interest. It is a 9-item scale (frequency score can range from 9 to 45) with good reliability (α = .83).23
Given the small and unequal sample sizes, nonparametric independent samples Mann-Whitney U-tests were selected to compare frequency of driving-related thoughts across veterans with comorbid PTSD and TBI and those of veterans without either PTSD or TBI.
Results
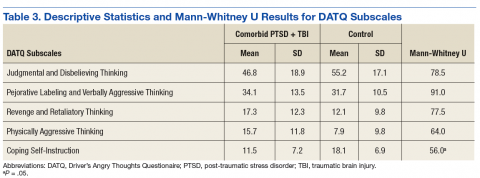
Descriptive statistics and results for each DATQ subscale are reported in Table 3. Group comparisons revealed that veterans with comorbid PTSD and TBI endorsed statistically significantly fewer coping self-instruction thoughts while driving (M = 11.5, SD = 7.2) than did combat veterans without either PTSD or TBI (M = 18.1, SD = 6.9; U = 56.0, P = .05). Conversely, frequency of angry thoughts were statistically significant in their difference as a function of PTSD or TBI diagnostic status.
Discussion
While driving, veterans with PTSD or TBI endorsed statistically significantly fewer coping self-instruction thoughts than did veterans without either PTSD or TBI. Prior research suggests that veterans with PTSD or TBI experience greater anxiety than do veterans without either condition while driving.2,3 Taken together, this suggests that veterans with PTSD or TBI may lack efficient cognitive coping strategies related to the anxiety they experience while driving. Furthermore, the groups did not significantly differ in frequency of angry thoughts behind the wheel. This result was expected based on prior analyses that suggested that veterans with and without PTSD or TBI endorsed feelings of aggression, impatience, and frustration while driving at similar frequencies.3
Because all veterans in the current sample were exposed to combat, these results help to parse out the unique contribution of PTSD and TBI diagnoses on driving in civilian environments. Exposure to combat plus diagnoses of PTSD or TBI may be related to veterans’ ability to cope with typical driving situations at home. In the context of prior literature, results suggest that veterans with PTSD or TBI automatically may perceive neutral roadside stimuli as threatening, feel anxious in response to this perceived threat, and be ill-equipped to cope with this anxiety.3,5,17,18 According to CBT models, negative automatic thoughts play a critical role in maintaining anxiety.24 Particular cognitive distortions associated with PTSD symptomatology and combat driving experiences, such as misperceiving ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations, may therefore maintain driving anxiety following military separation.
Research on CBT interventions suggests that cognitive restructuring, including coping self-instruction, are effective treatments to reduce anxiety.22,24 The current findings suggest that combat veterans with PTSD and TBI who experience driving anxiety endorse significantly fewer coping self-instruction thoughts than do controls in response to anxiety-provoking driving situations. In fact, prior research suggests that a majority of veterans experiencing driving-related anxiety do not seek help for their symptoms, and many of those who do prefer to reach out to friends rather than mental health professionals.2 However, due to their high levels of anxiety, these veterans likely would benefit from CBT interventions specifically targeted to coping strategies for civilian driving. These coping strategies should focus on recognizing that common roadside stimuli are not necessarily threatening in civilian environments. This type of cognitive restructuring may help veterans better manage anxiety while driving.
Limitations
The current study is limited by its small and unequal sample sizes and lack of a noncombat exposure comparison group. Additionally, while this study highlights a potential relationship between reduced cognitive coping strategies and behind-the-wheel anxiety in veterans with PTSD or TBI, causal inferences cannot be made. It is possible that individuals without coping strategies who are deployed to combat are more likely to develop PTSD or TBI. Being equipped with few coping strategies may then lead these veterans to experience greater anxiety while driving. Conversely, PTSD and TBI symptoms may prevent veterans from developing coping strategies over time.
Furthermore, the comorbid PTSD and TBI group was separated from the military for significantly longer than was the control group. Future studies using a longitudinal design could better examine the potential causal relationship between comorbid PTSD and TBI and coping and determine whether endorsement of coping self-instruction changes as a function of time since military separation.
Veterans in the current study report a variety of deployment experiences and locations. Methods of combat, type of vehicle, driving terrain, and prevalence of IEDs changed over the multiple post-9/11 military campaigns. Veterans who were deployed to Iraq in the mid-2000s were instructed to drive quickly and erratically to avoid IEDs and mortars, whereas veterans deployed in later years were taught to drive slowly and carefully to hunt for IEDs in heavily armored vehicles.3 Seventy-five percent of the veterans with PTSD or TBI in the current sample were deployed to Iraq in the early to mid-2000s, compared with 33% of the veterans without PTSD or TBI. Thus, the 2 groups in the current sample may have experienced different combat environments, which could impact how they perceived roadside stimuli. Future studies should recruit a larger and more balanced sample to better determine whether specific combat experiences impact coping strategies while driving.
Conclusion
To the best of the authors’ knowledge, the current study is the first to examine specific types of thoughts that veterans with and without PTSD or TBI experience while driving on civilian roads. Veterans with PTSD or TBI are not engaging in as many coping self-instruction thoughts behind the wheel, despite experiencing greater anxiety than that of veterans without either PTSD or TBI. Cognitive behavioral therapy interventions for anxiety include engaging in coping self-instruction during anxiety-provoking situations.22 Therefore, veterans with PTSD or TBI may benefit from learning targeted coping self-instruction thoughts that they can utilize when anxiety-provoking situations arise behind the wheel. Results suggest that clinicians should work with veterans with comorbid PTSD and TBI to develop specific coping self-instruction statements that they can utilize internally when faced with anxiety-provoking driving situations.
Acknowledgments
This study is the result of work supported by the Council on Brain Injury (grant #260472). The authors thank Dr. Rosette Biester for her guidance.
1. Belmont PJ, Schoenfeld AJ, Goodman G. Epidemiology of combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom: orthopaedic burden of disease. J Surg Orthop Adv. 2010;19(1):2-7.
2. Zinzow HM, Brooks J, Stern EB. Driving-related anxiety in recently deployed service members: cues, mental health correlates, and help-seeking behavior. Mil Med. 2013;178(3):e357-e361.
3. Whipple EK, Schultheis MT, Robinson KM. Preliminary findings of a novel measure of driving behaviors in veterans with comorbid TBI and PTSD. J Rehabil Res Dev. 2016;53(6):827-838.
4. Adler AB, Bliese PD, McGurk D, Hoge CW, Castro CA. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: randomization by platoon. J Consult Clin Psychol. 2009;77(5):928-940.
5. Amick MM, Kraft M, McGlinchey R. Driving simulator performance of veterans from the Iraq and Afghanistan wars. J Rehabil Res Dev. 2013;50(4):463-470.
6. Classen S, Cormack NL, Winter SM, et al. Efficacy of an occupational therapy driving intervention for returning combat veterans. OTJR (Thorofare NJ). 2014;34(4):177-182.
7. Hannold EM, Classen S, Winter S, Lanford DN, Levy CE. Exploratory pilot study of driving perceptions among OIF/OEF veterans with mTBI and PTSD. J Rehabil Res Dev. 2013;50(10):1315-1330.
8. Lew HL, Kraft M, Pogoda TK, Amick MM, Woods P, Cifu DX. Prevalence and characteristics of driving difficulties in Operation Iraqi Freedom/Operation Enduring Freedom combat returnees. J Rehabil Res Dev. 2011;48(8):913-925.
9. Arthur DC, MacDermid S, Kiley KC; Defense Health Board Task Force on Mental Health. An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: Defense Health Board; 2007.
10. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008.
11. Independent Review Group. Rebuilding the Trust: Independent Review Group Report on Rehabilitation Care and Administrative Processes at Walter Reed Army Medical Center and National Naval Medical Center. Arlington, VA: Independent Review Group; 2007
12. Bailie JM, Cole WR, Ivins B, et al. The experience, expression, and control of anger following traumatic brain injury in a military sample. J Head Trauma Rehabil. 2015;30(1):12-20.
13. Campbell TA, Nelson LA, Lumpkin R, Yoash-Gantz RE, Pickett TC, McCormick CL. Neuropsychological measures of processing speed and executive functioning in combat veterans with PTSD, TBI, and comorbid TBI/PTSD. Psychiatr Ann. 2009;39(8):796-803.
14. Classen S, Levy C, Meyer DL, Bewernitz M, Lanford DN, Mann WC. Simulated driving performance of combat veterans with mild tramatic brain injury and posttraumatic stress disorder: a pilot study. Am J Occup Ther. 2011;65(4):419-427.
15. Lew HL, Amick MM, Kraft M, Stein MB, Cifu DX. Potential driving issues in combat returnees. NeuroRehabilitation. 2010;26(3):271-278.
16. Vasterling JL, Brailey K, Allain AN, Duke LM, Constans JI, Sutker PB. Attention, learning, and memory performances and intellectual resources in Vietnam veterans: PTSD and no disorder comparisons. Neuropsychology. 2002;16(1):5-14.
17. Kimble MO, Kaufman ML, Leonard LL, et al. Sentence completion test in veterans with and without PTSD: preliminary findings. Psychiatry Res. 2002;113(3):303-307.
18. Kuhn E, Drescher K, Ruzek J, Rosen C. Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. J Trauma Stress. 2010;23(3):399-402.
19. Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. Am J Psychiatry. 2009;166(7):768-776.
20. Hill JJ III, Mobo BH Jr, Cullen MR. Separating deployment-related traumatic brain injury and posttraumatic stress disorder in veterans: preliminary findings from the Veterans Affairs traumatic brain injury screening program. Am J Phys Med Rehabil. 2009;88(8):605-614.
21. Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
22. Hope DA, Burns JA, Hayes SA, Herbert JD, Warner MD. Automatic thoughts and cognitive restructuring in cognitive behavioral group therapy for social anxiety disorder. Cognit Ther Res. 2010;34(1):1-12.
23. Deffenbacher JL, Petrilli RT, Lynch RS, Oetting ER, Swaim RC. The driver’s angry thoughts questionnaire: a measure of angry cognitions when driving. Cognit Ther Res. 2003;27(4):383-402.
24. Beck AT, Emery G, Greenberg RL. Anxiety Disorders and Phobias: A Cognitive Perspective. Rev. paperback ed. New York, NY: Basic Books; 2005.
Combat veterans who have served in Iraq and Afghanistan in the post-9/11 era face unique reintegration challenges, one being the transition from driving in combat zones to driving at home.1 Relative to previous conflicts, post-9/11 combat involves increased participation in road patrols and convoys along with more prevalent threats of improvised explosive devices (IEDs).1,2 Roadside ambushes designed to destroy or stop vehicles became a common warfare strategy, meaning that driving became an inherently dangerous combat maneuver.3
The modern combat driving framework includes cognitive tools (eg, targeted aggression and tactical awareness) combined with specific behaviors (eg, driving unpredictably fast, using rapid lane changes, and keeping other vehicles at a distance to avoid IEDs).4 This framework is adaptive and lifesaving in combat zones, but it can be maladaptive and dangerous in civilian environments. Service members face difficulty in updating this cognitive framework after leaving combat zones and may continue to experience specific cognitions (eg, “the world is dangerous”; “that car holds an IED”) while driving on civilian roads.3,5-8
The high prevalence of posttraumatic stress disorder (PTSD) and traumatic brain injury (TBI) in post-9/11 veterans may complicate reintegration. Both PTSD and TBI are considered signature wounds of these conflicts.8-11 Traumatic brain injury may be sustained as a result of blast injury or other mechanism, including a closed head injury or penetrating brain injury.10 Previous literature indicated that both PTSD and TBI across all severities are related to deficits in executive functioning, attention, and memory.12-16
In addition to cognitive deficits, veterans with PTSD also may experience cognitive misappraisal, in which they are more likely to perceive ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations.5,17,18 Examples of roadside-specific trauma triggers include busy highways, traffic, loud or distracting noises, and vehicles of similar make and model as those commonly rigged with IEDs in Iraq or Afghanistan.2,7
Blast injury
Prior research suggests that veterans with PTSD and/or TBI experience significantly higher levels of anxiety in response to common roadside stimuli (ie, an overpass or stop sign) while driving than do veterans without either PTSD or TBI.3 Cognitive behavioral therapy (CBT) interventions have been developed and systematically evaluated for treating anxiety.21 The goal of CBT is to identify and change dysfunctional cognitions that result in biased information processing. Cognitive restructuring, the process by which problematic cognitions (negative automatic thoughts) are identified and examined for distortions, is one method of accomplishing this goal. Distortions then are disputed and rebutted with assistance from the clinician.22 A strategy for restructuring negative automatic thoughts is coping self-instruction, which centers on identifying when negative automatic thoughts are focused on others’ behavior, accepting that their behavior cannot be changed, and using positive coping behaviors to minimize negative automatic thoughts.23
The link between history of comorbid PTSD and TBI and combat driving, current driving anxiety, and coping strategies has not yet been extensively studied in veterans. Thus, the aim of the current study is to determine whether veterans with comorbid PTSD and TBI utilize coping self-instruction behind the wheel. Driving-specific coping self-instruction involves generating thoughts that are adaptive and accepting of others’ driving behaviors (eg, “Just turn up the radio and tune them out”). It was hypothesized that veterans with comorbid PTSD and TBI would endorse fewer coping self-instruction thoughts than would veterans without either PTSD or TBI.
Methods
The current project is part of a larger study that examines driving behaviors of post-9/11 combat veterans at the Michael J. Crescenz Veterans Affairs Medical Center in Philadelphia, Pennsylvania. Thirty-two male veterans aged between 22 and 48 years (M = 31.6, SD = 6.9) were included in the sample. Twenty-three were diagnosed with comorbid PTSD and TBI and 9 veterans with no major psychiatric or physical
Assessment
All participants completed a battery of questionnaires, including the Driver’s Angry Thoughts Questionnaire (DATQ).23 The DATQ was used to investigate the specific thoughts that veterans experienced while driving.23 Participants indicated on a Likert scale from 1 (not at all) to 5 (all the time) how often they experienced any of 65 thoughts while driving. Each item was categorized into 1 of 5 distinct subscales (Table 2). A frequency score was generated for each of the 5 subscales. Each subscale had good internal consistency and convergent, divergent, and predictive validity. The Coping Self-Instruction subscale, which is defined as engaging in relaxing thoughts to accept others’ driving behaviors, was of primary interest. It is a 9-item scale (frequency score can range from 9 to 45) with good reliability (α = .83).23
Given the small and unequal sample sizes, nonparametric independent samples Mann-Whitney U-tests were selected to compare frequency of driving-related thoughts across veterans with comorbid PTSD and TBI and those of veterans without either PTSD or TBI.
Results
Descriptive statistics and results for each DATQ subscale are reported in Table 3. Group comparisons revealed that veterans with comorbid PTSD and TBI endorsed statistically significantly fewer coping self-instruction thoughts while driving (M = 11.5, SD = 7.2) than did combat veterans without either PTSD or TBI (M = 18.1, SD = 6.9; U = 56.0, P = .05). Conversely, frequency of angry thoughts were statistically significant in their difference as a function of PTSD or TBI diagnostic status.
Discussion
While driving, veterans with PTSD or TBI endorsed statistically significantly fewer coping self-instruction thoughts than did veterans without either PTSD or TBI. Prior research suggests that veterans with PTSD or TBI experience greater anxiety than do veterans without either condition while driving.2,3 Taken together, this suggests that veterans with PTSD or TBI may lack efficient cognitive coping strategies related to the anxiety they experience while driving. Furthermore, the groups did not significantly differ in frequency of angry thoughts behind the wheel. This result was expected based on prior analyses that suggested that veterans with and without PTSD or TBI endorsed feelings of aggression, impatience, and frustration while driving at similar frequencies.3
Because all veterans in the current sample were exposed to combat, these results help to parse out the unique contribution of PTSD and TBI diagnoses on driving in civilian environments. Exposure to combat plus diagnoses of PTSD or TBI may be related to veterans’ ability to cope with typical driving situations at home. In the context of prior literature, results suggest that veterans with PTSD or TBI automatically may perceive neutral roadside stimuli as threatening, feel anxious in response to this perceived threat, and be ill-equipped to cope with this anxiety.3,5,17,18 According to CBT models, negative automatic thoughts play a critical role in maintaining anxiety.24 Particular cognitive distortions associated with PTSD symptomatology and combat driving experiences, such as misperceiving ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations, may therefore maintain driving anxiety following military separation.
Research on CBT interventions suggests that cognitive restructuring, including coping self-instruction, are effective treatments to reduce anxiety.22,24 The current findings suggest that combat veterans with PTSD and TBI who experience driving anxiety endorse significantly fewer coping self-instruction thoughts than do controls in response to anxiety-provoking driving situations. In fact, prior research suggests that a majority of veterans experiencing driving-related anxiety do not seek help for their symptoms, and many of those who do prefer to reach out to friends rather than mental health professionals.2 However, due to their high levels of anxiety, these veterans likely would benefit from CBT interventions specifically targeted to coping strategies for civilian driving. These coping strategies should focus on recognizing that common roadside stimuli are not necessarily threatening in civilian environments. This type of cognitive restructuring may help veterans better manage anxiety while driving.
Limitations
The current study is limited by its small and unequal sample sizes and lack of a noncombat exposure comparison group. Additionally, while this study highlights a potential relationship between reduced cognitive coping strategies and behind-the-wheel anxiety in veterans with PTSD or TBI, causal inferences cannot be made. It is possible that individuals without coping strategies who are deployed to combat are more likely to develop PTSD or TBI. Being equipped with few coping strategies may then lead these veterans to experience greater anxiety while driving. Conversely, PTSD and TBI symptoms may prevent veterans from developing coping strategies over time.
Furthermore, the comorbid PTSD and TBI group was separated from the military for significantly longer than was the control group. Future studies using a longitudinal design could better examine the potential causal relationship between comorbid PTSD and TBI and coping and determine whether endorsement of coping self-instruction changes as a function of time since military separation.
Veterans in the current study report a variety of deployment experiences and locations. Methods of combat, type of vehicle, driving terrain, and prevalence of IEDs changed over the multiple post-9/11 military campaigns. Veterans who were deployed to Iraq in the mid-2000s were instructed to drive quickly and erratically to avoid IEDs and mortars, whereas veterans deployed in later years were taught to drive slowly and carefully to hunt for IEDs in heavily armored vehicles.3 Seventy-five percent of the veterans with PTSD or TBI in the current sample were deployed to Iraq in the early to mid-2000s, compared with 33% of the veterans without PTSD or TBI. Thus, the 2 groups in the current sample may have experienced different combat environments, which could impact how they perceived roadside stimuli. Future studies should recruit a larger and more balanced sample to better determine whether specific combat experiences impact coping strategies while driving.
Conclusion
To the best of the authors’ knowledge, the current study is the first to examine specific types of thoughts that veterans with and without PTSD or TBI experience while driving on civilian roads. Veterans with PTSD or TBI are not engaging in as many coping self-instruction thoughts behind the wheel, despite experiencing greater anxiety than that of veterans without either PTSD or TBI. Cognitive behavioral therapy interventions for anxiety include engaging in coping self-instruction during anxiety-provoking situations.22 Therefore, veterans with PTSD or TBI may benefit from learning targeted coping self-instruction thoughts that they can utilize when anxiety-provoking situations arise behind the wheel. Results suggest that clinicians should work with veterans with comorbid PTSD and TBI to develop specific coping self-instruction statements that they can utilize internally when faced with anxiety-provoking driving situations.
Acknowledgments
This study is the result of work supported by the Council on Brain Injury (grant #260472). The authors thank Dr. Rosette Biester for her guidance.
Combat veterans who have served in Iraq and Afghanistan in the post-9/11 era face unique reintegration challenges, one being the transition from driving in combat zones to driving at home.1 Relative to previous conflicts, post-9/11 combat involves increased participation in road patrols and convoys along with more prevalent threats of improvised explosive devices (IEDs).1,2 Roadside ambushes designed to destroy or stop vehicles became a common warfare strategy, meaning that driving became an inherently dangerous combat maneuver.3
The modern combat driving framework includes cognitive tools (eg, targeted aggression and tactical awareness) combined with specific behaviors (eg, driving unpredictably fast, using rapid lane changes, and keeping other vehicles at a distance to avoid IEDs).4 This framework is adaptive and lifesaving in combat zones, but it can be maladaptive and dangerous in civilian environments. Service members face difficulty in updating this cognitive framework after leaving combat zones and may continue to experience specific cognitions (eg, “the world is dangerous”; “that car holds an IED”) while driving on civilian roads.3,5-8
The high prevalence of posttraumatic stress disorder (PTSD) and traumatic brain injury (TBI) in post-9/11 veterans may complicate reintegration. Both PTSD and TBI are considered signature wounds of these conflicts.8-11 Traumatic brain injury may be sustained as a result of blast injury or other mechanism, including a closed head injury or penetrating brain injury.10 Previous literature indicated that both PTSD and TBI across all severities are related to deficits in executive functioning, attention, and memory.12-16
In addition to cognitive deficits, veterans with PTSD also may experience cognitive misappraisal, in which they are more likely to perceive ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations.5,17,18 Examples of roadside-specific trauma triggers include busy highways, traffic, loud or distracting noises, and vehicles of similar make and model as those commonly rigged with IEDs in Iraq or Afghanistan.2,7
Blast injury
Prior research suggests that veterans with PTSD and/or TBI experience significantly higher levels of anxiety in response to common roadside stimuli (ie, an overpass or stop sign) while driving than do veterans without either PTSD or TBI.3 Cognitive behavioral therapy (CBT) interventions have been developed and systematically evaluated for treating anxiety.21 The goal of CBT is to identify and change dysfunctional cognitions that result in biased information processing. Cognitive restructuring, the process by which problematic cognitions (negative automatic thoughts) are identified and examined for distortions, is one method of accomplishing this goal. Distortions then are disputed and rebutted with assistance from the clinician.22 A strategy for restructuring negative automatic thoughts is coping self-instruction, which centers on identifying when negative automatic thoughts are focused on others’ behavior, accepting that their behavior cannot be changed, and using positive coping behaviors to minimize negative automatic thoughts.23
The link between history of comorbid PTSD and TBI and combat driving, current driving anxiety, and coping strategies has not yet been extensively studied in veterans. Thus, the aim of the current study is to determine whether veterans with comorbid PTSD and TBI utilize coping self-instruction behind the wheel. Driving-specific coping self-instruction involves generating thoughts that are adaptive and accepting of others’ driving behaviors (eg, “Just turn up the radio and tune them out”). It was hypothesized that veterans with comorbid PTSD and TBI would endorse fewer coping self-instruction thoughts than would veterans without either PTSD or TBI.
Methods
The current project is part of a larger study that examines driving behaviors of post-9/11 combat veterans at the Michael J. Crescenz Veterans Affairs Medical Center in Philadelphia, Pennsylvania. Thirty-two male veterans aged between 22 and 48 years (M = 31.6, SD = 6.9) were included in the sample. Twenty-three were diagnosed with comorbid PTSD and TBI and 9 veterans with no major psychiatric or physical
Assessment
All participants completed a battery of questionnaires, including the Driver’s Angry Thoughts Questionnaire (DATQ).23 The DATQ was used to investigate the specific thoughts that veterans experienced while driving.23 Participants indicated on a Likert scale from 1 (not at all) to 5 (all the time) how often they experienced any of 65 thoughts while driving. Each item was categorized into 1 of 5 distinct subscales (Table 2). A frequency score was generated for each of the 5 subscales. Each subscale had good internal consistency and convergent, divergent, and predictive validity. The Coping Self-Instruction subscale, which is defined as engaging in relaxing thoughts to accept others’ driving behaviors, was of primary interest. It is a 9-item scale (frequency score can range from 9 to 45) with good reliability (α = .83).23
Given the small and unequal sample sizes, nonparametric independent samples Mann-Whitney U-tests were selected to compare frequency of driving-related thoughts across veterans with comorbid PTSD and TBI and those of veterans without either PTSD or TBI.
Results
Descriptive statistics and results for each DATQ subscale are reported in Table 3. Group comparisons revealed that veterans with comorbid PTSD and TBI endorsed statistically significantly fewer coping self-instruction thoughts while driving (M = 11.5, SD = 7.2) than did combat veterans without either PTSD or TBI (M = 18.1, SD = 6.9; U = 56.0, P = .05). Conversely, frequency of angry thoughts were statistically significant in their difference as a function of PTSD or TBI diagnostic status.
Discussion
While driving, veterans with PTSD or TBI endorsed statistically significantly fewer coping self-instruction thoughts than did veterans without either PTSD or TBI. Prior research suggests that veterans with PTSD or TBI experience greater anxiety than do veterans without either condition while driving.2,3 Taken together, this suggests that veterans with PTSD or TBI may lack efficient cognitive coping strategies related to the anxiety they experience while driving. Furthermore, the groups did not significantly differ in frequency of angry thoughts behind the wheel. This result was expected based on prior analyses that suggested that veterans with and without PTSD or TBI endorsed feelings of aggression, impatience, and frustration while driving at similar frequencies.3
Because all veterans in the current sample were exposed to combat, these results help to parse out the unique contribution of PTSD and TBI diagnoses on driving in civilian environments. Exposure to combat plus diagnoses of PTSD or TBI may be related to veterans’ ability to cope with typical driving situations at home. In the context of prior literature, results suggest that veterans with PTSD or TBI automatically may perceive neutral roadside stimuli as threatening, feel anxious in response to this perceived threat, and be ill-equipped to cope with this anxiety.3,5,17,18 According to CBT models, negative automatic thoughts play a critical role in maintaining anxiety.24 Particular cognitive distortions associated with PTSD symptomatology and combat driving experiences, such as misperceiving ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations, may therefore maintain driving anxiety following military separation.
Research on CBT interventions suggests that cognitive restructuring, including coping self-instruction, are effective treatments to reduce anxiety.22,24 The current findings suggest that combat veterans with PTSD and TBI who experience driving anxiety endorse significantly fewer coping self-instruction thoughts than do controls in response to anxiety-provoking driving situations. In fact, prior research suggests that a majority of veterans experiencing driving-related anxiety do not seek help for their symptoms, and many of those who do prefer to reach out to friends rather than mental health professionals.2 However, due to their high levels of anxiety, these veterans likely would benefit from CBT interventions specifically targeted to coping strategies for civilian driving. These coping strategies should focus on recognizing that common roadside stimuli are not necessarily threatening in civilian environments. This type of cognitive restructuring may help veterans better manage anxiety while driving.
Limitations
The current study is limited by its small and unequal sample sizes and lack of a noncombat exposure comparison group. Additionally, while this study highlights a potential relationship between reduced cognitive coping strategies and behind-the-wheel anxiety in veterans with PTSD or TBI, causal inferences cannot be made. It is possible that individuals without coping strategies who are deployed to combat are more likely to develop PTSD or TBI. Being equipped with few coping strategies may then lead these veterans to experience greater anxiety while driving. Conversely, PTSD and TBI symptoms may prevent veterans from developing coping strategies over time.
Furthermore, the comorbid PTSD and TBI group was separated from the military for significantly longer than was the control group. Future studies using a longitudinal design could better examine the potential causal relationship between comorbid PTSD and TBI and coping and determine whether endorsement of coping self-instruction changes as a function of time since military separation.
Veterans in the current study report a variety of deployment experiences and locations. Methods of combat, type of vehicle, driving terrain, and prevalence of IEDs changed over the multiple post-9/11 military campaigns. Veterans who were deployed to Iraq in the mid-2000s were instructed to drive quickly and erratically to avoid IEDs and mortars, whereas veterans deployed in later years were taught to drive slowly and carefully to hunt for IEDs in heavily armored vehicles.3 Seventy-five percent of the veterans with PTSD or TBI in the current sample were deployed to Iraq in the early to mid-2000s, compared with 33% of the veterans without PTSD or TBI. Thus, the 2 groups in the current sample may have experienced different combat environments, which could impact how they perceived roadside stimuli. Future studies should recruit a larger and more balanced sample to better determine whether specific combat experiences impact coping strategies while driving.
Conclusion
To the best of the authors’ knowledge, the current study is the first to examine specific types of thoughts that veterans with and without PTSD or TBI experience while driving on civilian roads. Veterans with PTSD or TBI are not engaging in as many coping self-instruction thoughts behind the wheel, despite experiencing greater anxiety than that of veterans without either PTSD or TBI. Cognitive behavioral therapy interventions for anxiety include engaging in coping self-instruction during anxiety-provoking situations.22 Therefore, veterans with PTSD or TBI may benefit from learning targeted coping self-instruction thoughts that they can utilize when anxiety-provoking situations arise behind the wheel. Results suggest that clinicians should work with veterans with comorbid PTSD and TBI to develop specific coping self-instruction statements that they can utilize internally when faced with anxiety-provoking driving situations.
Acknowledgments
This study is the result of work supported by the Council on Brain Injury (grant #260472). The authors thank Dr. Rosette Biester for her guidance.
1. Belmont PJ, Schoenfeld AJ, Goodman G. Epidemiology of combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom: orthopaedic burden of disease. J Surg Orthop Adv. 2010;19(1):2-7.
2. Zinzow HM, Brooks J, Stern EB. Driving-related anxiety in recently deployed service members: cues, mental health correlates, and help-seeking behavior. Mil Med. 2013;178(3):e357-e361.
3. Whipple EK, Schultheis MT, Robinson KM. Preliminary findings of a novel measure of driving behaviors in veterans with comorbid TBI and PTSD. J Rehabil Res Dev. 2016;53(6):827-838.
4. Adler AB, Bliese PD, McGurk D, Hoge CW, Castro CA. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: randomization by platoon. J Consult Clin Psychol. 2009;77(5):928-940.
5. Amick MM, Kraft M, McGlinchey R. Driving simulator performance of veterans from the Iraq and Afghanistan wars. J Rehabil Res Dev. 2013;50(4):463-470.
6. Classen S, Cormack NL, Winter SM, et al. Efficacy of an occupational therapy driving intervention for returning combat veterans. OTJR (Thorofare NJ). 2014;34(4):177-182.
7. Hannold EM, Classen S, Winter S, Lanford DN, Levy CE. Exploratory pilot study of driving perceptions among OIF/OEF veterans with mTBI and PTSD. J Rehabil Res Dev. 2013;50(10):1315-1330.
8. Lew HL, Kraft M, Pogoda TK, Amick MM, Woods P, Cifu DX. Prevalence and characteristics of driving difficulties in Operation Iraqi Freedom/Operation Enduring Freedom combat returnees. J Rehabil Res Dev. 2011;48(8):913-925.
9. Arthur DC, MacDermid S, Kiley KC; Defense Health Board Task Force on Mental Health. An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: Defense Health Board; 2007.
10. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008.
11. Independent Review Group. Rebuilding the Trust: Independent Review Group Report on Rehabilitation Care and Administrative Processes at Walter Reed Army Medical Center and National Naval Medical Center. Arlington, VA: Independent Review Group; 2007
12. Bailie JM, Cole WR, Ivins B, et al. The experience, expression, and control of anger following traumatic brain injury in a military sample. J Head Trauma Rehabil. 2015;30(1):12-20.
13. Campbell TA, Nelson LA, Lumpkin R, Yoash-Gantz RE, Pickett TC, McCormick CL. Neuropsychological measures of processing speed and executive functioning in combat veterans with PTSD, TBI, and comorbid TBI/PTSD. Psychiatr Ann. 2009;39(8):796-803.
14. Classen S, Levy C, Meyer DL, Bewernitz M, Lanford DN, Mann WC. Simulated driving performance of combat veterans with mild tramatic brain injury and posttraumatic stress disorder: a pilot study. Am J Occup Ther. 2011;65(4):419-427.
15. Lew HL, Amick MM, Kraft M, Stein MB, Cifu DX. Potential driving issues in combat returnees. NeuroRehabilitation. 2010;26(3):271-278.
16. Vasterling JL, Brailey K, Allain AN, Duke LM, Constans JI, Sutker PB. Attention, learning, and memory performances and intellectual resources in Vietnam veterans: PTSD and no disorder comparisons. Neuropsychology. 2002;16(1):5-14.
17. Kimble MO, Kaufman ML, Leonard LL, et al. Sentence completion test in veterans with and without PTSD: preliminary findings. Psychiatry Res. 2002;113(3):303-307.
18. Kuhn E, Drescher K, Ruzek J, Rosen C. Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. J Trauma Stress. 2010;23(3):399-402.
19. Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. Am J Psychiatry. 2009;166(7):768-776.
20. Hill JJ III, Mobo BH Jr, Cullen MR. Separating deployment-related traumatic brain injury and posttraumatic stress disorder in veterans: preliminary findings from the Veterans Affairs traumatic brain injury screening program. Am J Phys Med Rehabil. 2009;88(8):605-614.
21. Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
22. Hope DA, Burns JA, Hayes SA, Herbert JD, Warner MD. Automatic thoughts and cognitive restructuring in cognitive behavioral group therapy for social anxiety disorder. Cognit Ther Res. 2010;34(1):1-12.
23. Deffenbacher JL, Petrilli RT, Lynch RS, Oetting ER, Swaim RC. The driver’s angry thoughts questionnaire: a measure of angry cognitions when driving. Cognit Ther Res. 2003;27(4):383-402.
24. Beck AT, Emery G, Greenberg RL. Anxiety Disorders and Phobias: A Cognitive Perspective. Rev. paperback ed. New York, NY: Basic Books; 2005.
1. Belmont PJ, Schoenfeld AJ, Goodman G. Epidemiology of combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom: orthopaedic burden of disease. J Surg Orthop Adv. 2010;19(1):2-7.
2. Zinzow HM, Brooks J, Stern EB. Driving-related anxiety in recently deployed service members: cues, mental health correlates, and help-seeking behavior. Mil Med. 2013;178(3):e357-e361.
3. Whipple EK, Schultheis MT, Robinson KM. Preliminary findings of a novel measure of driving behaviors in veterans with comorbid TBI and PTSD. J Rehabil Res Dev. 2016;53(6):827-838.
4. Adler AB, Bliese PD, McGurk D, Hoge CW, Castro CA. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: randomization by platoon. J Consult Clin Psychol. 2009;77(5):928-940.
5. Amick MM, Kraft M, McGlinchey R. Driving simulator performance of veterans from the Iraq and Afghanistan wars. J Rehabil Res Dev. 2013;50(4):463-470.
6. Classen S, Cormack NL, Winter SM, et al. Efficacy of an occupational therapy driving intervention for returning combat veterans. OTJR (Thorofare NJ). 2014;34(4):177-182.
7. Hannold EM, Classen S, Winter S, Lanford DN, Levy CE. Exploratory pilot study of driving perceptions among OIF/OEF veterans with mTBI and PTSD. J Rehabil Res Dev. 2013;50(10):1315-1330.
8. Lew HL, Kraft M, Pogoda TK, Amick MM, Woods P, Cifu DX. Prevalence and characteristics of driving difficulties in Operation Iraqi Freedom/Operation Enduring Freedom combat returnees. J Rehabil Res Dev. 2011;48(8):913-925.
9. Arthur DC, MacDermid S, Kiley KC; Defense Health Board Task Force on Mental Health. An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: Defense Health Board; 2007.
10. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008.
11. Independent Review Group. Rebuilding the Trust: Independent Review Group Report on Rehabilitation Care and Administrative Processes at Walter Reed Army Medical Center and National Naval Medical Center. Arlington, VA: Independent Review Group; 2007
12. Bailie JM, Cole WR, Ivins B, et al. The experience, expression, and control of anger following traumatic brain injury in a military sample. J Head Trauma Rehabil. 2015;30(1):12-20.
13. Campbell TA, Nelson LA, Lumpkin R, Yoash-Gantz RE, Pickett TC, McCormick CL. Neuropsychological measures of processing speed and executive functioning in combat veterans with PTSD, TBI, and comorbid TBI/PTSD. Psychiatr Ann. 2009;39(8):796-803.
14. Classen S, Levy C, Meyer DL, Bewernitz M, Lanford DN, Mann WC. Simulated driving performance of combat veterans with mild tramatic brain injury and posttraumatic stress disorder: a pilot study. Am J Occup Ther. 2011;65(4):419-427.
15. Lew HL, Amick MM, Kraft M, Stein MB, Cifu DX. Potential driving issues in combat returnees. NeuroRehabilitation. 2010;26(3):271-278.
16. Vasterling JL, Brailey K, Allain AN, Duke LM, Constans JI, Sutker PB. Attention, learning, and memory performances and intellectual resources in Vietnam veterans: PTSD and no disorder comparisons. Neuropsychology. 2002;16(1):5-14.
17. Kimble MO, Kaufman ML, Leonard LL, et al. Sentence completion test in veterans with and without PTSD: preliminary findings. Psychiatry Res. 2002;113(3):303-307.
18. Kuhn E, Drescher K, Ruzek J, Rosen C. Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. J Trauma Stress. 2010;23(3):399-402.
19. Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. Am J Psychiatry. 2009;166(7):768-776.
20. Hill JJ III, Mobo BH Jr, Cullen MR. Separating deployment-related traumatic brain injury and posttraumatic stress disorder in veterans: preliminary findings from the Veterans Affairs traumatic brain injury screening program. Am J Phys Med Rehabil. 2009;88(8):605-614.
21. Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
22. Hope DA, Burns JA, Hayes SA, Herbert JD, Warner MD. Automatic thoughts and cognitive restructuring in cognitive behavioral group therapy for social anxiety disorder. Cognit Ther Res. 2010;34(1):1-12.
23. Deffenbacher JL, Petrilli RT, Lynch RS, Oetting ER, Swaim RC. The driver’s angry thoughts questionnaire: a measure of angry cognitions when driving. Cognit Ther Res. 2003;27(4):383-402.
24. Beck AT, Emery G, Greenberg RL. Anxiety Disorders and Phobias: A Cognitive Perspective. Rev. paperback ed. New York, NY: Basic Books; 2005.