User login
Driving-Related Coping Thoughts in Post-9/11 Combat Veterans With and Without Comorbid PTSD and TBI
Combat veterans who have served in Iraq and Afghanistan in the post-9/11 era face unique reintegration challenges, one being the transition from driving in combat zones to driving at home.1 Relative to previous conflicts, post-9/11 combat involves increased participation in road patrols and convoys along with more prevalent threats of improvised explosive devices (IEDs).1,2 Roadside ambushes designed to destroy or stop vehicles became a common warfare strategy, meaning that driving became an inherently dangerous combat maneuver.3
The modern combat driving framework includes cognitive tools (eg, targeted aggression and tactical awareness) combined with specific behaviors (eg, driving unpredictably fast, using rapid lane changes, and keeping other vehicles at a distance to avoid IEDs).4 This framework is adaptive and lifesaving in combat zones, but it can be maladaptive and dangerous in civilian environments. Service members face difficulty in updating this cognitive framework after leaving combat zones and may continue to experience specific cognitions (eg, “the world is dangerous”; “that car holds an IED”) while driving on civilian roads.3,5-8
The high prevalence of posttraumatic stress disorder (PTSD) and traumatic brain injury (TBI) in post-9/11 veterans may complicate reintegration. Both PTSD and TBI are considered signature wounds of these conflicts.8-11 Traumatic brain injury may be sustained as a result of blast injury or other mechanism, including a closed head injury or penetrating brain injury.10 Previous literature indicated that both PTSD and TBI across all severities are related to deficits in executive functioning, attention, and memory.12-16
In addition to cognitive deficits, veterans with PTSD also may experience cognitive misappraisal, in which they are more likely to perceive ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations.5,17,18 Examples of roadside-specific trauma triggers include busy highways, traffic, loud or distracting noises, and vehicles of similar make and model as those commonly rigged with IEDs in Iraq or Afghanistan.2,7
Blast injury
Prior research suggests that veterans with PTSD and/or TBI experience significantly higher levels of anxiety in response to common roadside stimuli (ie, an overpass or stop sign) while driving than do veterans without either PTSD or TBI.3 Cognitive behavioral therapy (CBT) interventions have been developed and systematically evaluated for treating anxiety.21 The goal of CBT is to identify and change dysfunctional cognitions that result in biased information processing. Cognitive restructuring, the process by which problematic cognitions (negative automatic thoughts) are identified and examined for distortions, is one method of accomplishing this goal. Distortions then are disputed and rebutted with assistance from the clinician.22 A strategy for restructuring negative automatic thoughts is coping self-instruction, which centers on identifying when negative automatic thoughts are focused on others’ behavior, accepting that their behavior cannot be changed, and using positive coping behaviors to minimize negative automatic thoughts.23
The link between history of comorbid PTSD and TBI and combat driving, current driving anxiety, and coping strategies has not yet been extensively studied in veterans. Thus, the aim of the current study is to determine whether veterans with comorbid PTSD and TBI utilize coping self-instruction behind the wheel. Driving-specific coping self-instruction involves generating thoughts that are adaptive and accepting of others’ driving behaviors (eg, “Just turn up the radio and tune them out”). It was hypothesized that veterans with comorbid PTSD and TBI would endorse fewer coping self-instruction thoughts than would veterans without either PTSD or TBI.
Methods
The current project is part of a larger study that examines driving behaviors of post-9/11 combat veterans at the Michael J. Crescenz Veterans Affairs Medical Center in Philadelphia, Pennsylvania. Thirty-two male veterans aged between 22 and 48 years (M = 31.6, SD = 6.9) were included in the sample. Twenty-three were diagnosed with comorbid PTSD and TBI and 9 veterans with no major psychiatric or physical
Assessment
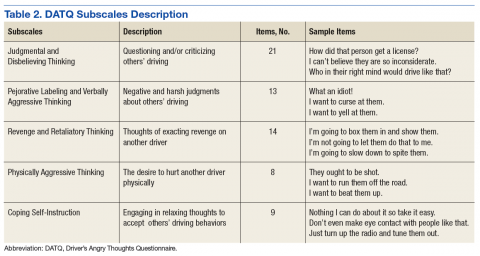
All participants completed a battery of questionnaires, including the Driver’s Angry Thoughts Questionnaire (DATQ).23 The DATQ was used to investigate the specific thoughts that veterans experienced while driving.23 Participants indicated on a Likert scale from 1 (not at all) to 5 (all the time) how often they experienced any of 65 thoughts while driving. Each item was categorized into 1 of 5 distinct subscales (Table 2). A frequency score was generated for each of the 5 subscales. Each subscale had good internal consistency and convergent, divergent, and predictive validity. The Coping Self-Instruction subscale, which is defined as engaging in relaxing thoughts to accept others’ driving behaviors, was of primary interest. It is a 9-item scale (frequency score can range from 9 to 45) with good reliability (α = .83).23
Given the small and unequal sample sizes, nonparametric independent samples Mann-Whitney U-tests were selected to compare frequency of driving-related thoughts across veterans with comorbid PTSD and TBI and those of veterans without either PTSD or TBI.
Results
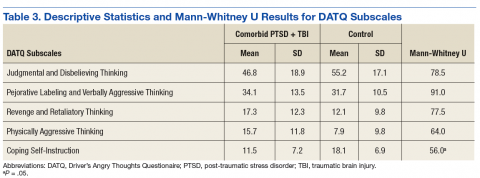
Descriptive statistics and results for each DATQ subscale are reported in Table 3. Group comparisons revealed that veterans with comorbid PTSD and TBI endorsed statistically significantly fewer coping self-instruction thoughts while driving (M = 11.5, SD = 7.2) than did combat veterans without either PTSD or TBI (M = 18.1, SD = 6.9; U = 56.0, P = .05). Conversely, frequency of angry thoughts were statistically significant in their difference as a function of PTSD or TBI diagnostic status.
Discussion
While driving, veterans with PTSD or TBI endorsed statistically significantly fewer coping self-instruction thoughts than did veterans without either PTSD or TBI. Prior research suggests that veterans with PTSD or TBI experience greater anxiety than do veterans without either condition while driving.2,3 Taken together, this suggests that veterans with PTSD or TBI may lack efficient cognitive coping strategies related to the anxiety they experience while driving. Furthermore, the groups did not significantly differ in frequency of angry thoughts behind the wheel. This result was expected based on prior analyses that suggested that veterans with and without PTSD or TBI endorsed feelings of aggression, impatience, and frustration while driving at similar frequencies.3
Because all veterans in the current sample were exposed to combat, these results help to parse out the unique contribution of PTSD and TBI diagnoses on driving in civilian environments. Exposure to combat plus diagnoses of PTSD or TBI may be related to veterans’ ability to cope with typical driving situations at home. In the context of prior literature, results suggest that veterans with PTSD or TBI automatically may perceive neutral roadside stimuli as threatening, feel anxious in response to this perceived threat, and be ill-equipped to cope with this anxiety.3,5,17,18 According to CBT models, negative automatic thoughts play a critical role in maintaining anxiety.24 Particular cognitive distortions associated with PTSD symptomatology and combat driving experiences, such as misperceiving ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations, may therefore maintain driving anxiety following military separation.
Research on CBT interventions suggests that cognitive restructuring, including coping self-instruction, are effective treatments to reduce anxiety.22,24 The current findings suggest that combat veterans with PTSD and TBI who experience driving anxiety endorse significantly fewer coping self-instruction thoughts than do controls in response to anxiety-provoking driving situations. In fact, prior research suggests that a majority of veterans experiencing driving-related anxiety do not seek help for their symptoms, and many of those who do prefer to reach out to friends rather than mental health professionals.2 However, due to their high levels of anxiety, these veterans likely would benefit from CBT interventions specifically targeted to coping strategies for civilian driving. These coping strategies should focus on recognizing that common roadside stimuli are not necessarily threatening in civilian environments. This type of cognitive restructuring may help veterans better manage anxiety while driving.
Limitations
The current study is limited by its small and unequal sample sizes and lack of a noncombat exposure comparison group. Additionally, while this study highlights a potential relationship between reduced cognitive coping strategies and behind-the-wheel anxiety in veterans with PTSD or TBI, causal inferences cannot be made. It is possible that individuals without coping strategies who are deployed to combat are more likely to develop PTSD or TBI. Being equipped with few coping strategies may then lead these veterans to experience greater anxiety while driving. Conversely, PTSD and TBI symptoms may prevent veterans from developing coping strategies over time.
Furthermore, the comorbid PTSD and TBI group was separated from the military for significantly longer than was the control group. Future studies using a longitudinal design could better examine the potential causal relationship between comorbid PTSD and TBI and coping and determine whether endorsement of coping self-instruction changes as a function of time since military separation.
Veterans in the current study report a variety of deployment experiences and locations. Methods of combat, type of vehicle, driving terrain, and prevalence of IEDs changed over the multiple post-9/11 military campaigns. Veterans who were deployed to Iraq in the mid-2000s were instructed to drive quickly and erratically to avoid IEDs and mortars, whereas veterans deployed in later years were taught to drive slowly and carefully to hunt for IEDs in heavily armored vehicles.3 Seventy-five percent of the veterans with PTSD or TBI in the current sample were deployed to Iraq in the early to mid-2000s, compared with 33% of the veterans without PTSD or TBI. Thus, the 2 groups in the current sample may have experienced different combat environments, which could impact how they perceived roadside stimuli. Future studies should recruit a larger and more balanced sample to better determine whether specific combat experiences impact coping strategies while driving.
Conclusion
To the best of the authors’ knowledge, the current study is the first to examine specific types of thoughts that veterans with and without PTSD or TBI experience while driving on civilian roads. Veterans with PTSD or TBI are not engaging in as many coping self-instruction thoughts behind the wheel, despite experiencing greater anxiety than that of veterans without either PTSD or TBI. Cognitive behavioral therapy interventions for anxiety include engaging in coping self-instruction during anxiety-provoking situations.22 Therefore, veterans with PTSD or TBI may benefit from learning targeted coping self-instruction thoughts that they can utilize when anxiety-provoking situations arise behind the wheel. Results suggest that clinicians should work with veterans with comorbid PTSD and TBI to develop specific coping self-instruction statements that they can utilize internally when faced with anxiety-provoking driving situations.
Acknowledgments
This study is the result of work supported by the Council on Brain Injury (grant #260472). The authors thank Dr. Rosette Biester for her guidance.
1. Belmont PJ, Schoenfeld AJ, Goodman G. Epidemiology of combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom: orthopaedic burden of disease. J Surg Orthop Adv. 2010;19(1):2-7.
2. Zinzow HM, Brooks J, Stern EB. Driving-related anxiety in recently deployed service members: cues, mental health correlates, and help-seeking behavior. Mil Med. 2013;178(3):e357-e361.
3. Whipple EK, Schultheis MT, Robinson KM. Preliminary findings of a novel measure of driving behaviors in veterans with comorbid TBI and PTSD. J Rehabil Res Dev. 2016;53(6):827-838.
4. Adler AB, Bliese PD, McGurk D, Hoge CW, Castro CA. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: randomization by platoon. J Consult Clin Psychol. 2009;77(5):928-940.
5. Amick MM, Kraft M, McGlinchey R. Driving simulator performance of veterans from the Iraq and Afghanistan wars. J Rehabil Res Dev. 2013;50(4):463-470.
6. Classen S, Cormack NL, Winter SM, et al. Efficacy of an occupational therapy driving intervention for returning combat veterans. OTJR (Thorofare NJ). 2014;34(4):177-182.
7. Hannold EM, Classen S, Winter S, Lanford DN, Levy CE. Exploratory pilot study of driving perceptions among OIF/OEF veterans with mTBI and PTSD. J Rehabil Res Dev. 2013;50(10):1315-1330.
8. Lew HL, Kraft M, Pogoda TK, Amick MM, Woods P, Cifu DX. Prevalence and characteristics of driving difficulties in Operation Iraqi Freedom/Operation Enduring Freedom combat returnees. J Rehabil Res Dev. 2011;48(8):913-925.
9. Arthur DC, MacDermid S, Kiley KC; Defense Health Board Task Force on Mental Health. An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: Defense Health Board; 2007.
10. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008.
11. Independent Review Group. Rebuilding the Trust: Independent Review Group Report on Rehabilitation Care and Administrative Processes at Walter Reed Army Medical Center and National Naval Medical Center. Arlington, VA: Independent Review Group; 2007
12. Bailie JM, Cole WR, Ivins B, et al. The experience, expression, and control of anger following traumatic brain injury in a military sample. J Head Trauma Rehabil. 2015;30(1):12-20.
13. Campbell TA, Nelson LA, Lumpkin R, Yoash-Gantz RE, Pickett TC, McCormick CL. Neuropsychological measures of processing speed and executive functioning in combat veterans with PTSD, TBI, and comorbid TBI/PTSD. Psychiatr Ann. 2009;39(8):796-803.
14. Classen S, Levy C, Meyer DL, Bewernitz M, Lanford DN, Mann WC. Simulated driving performance of combat veterans with mild tramatic brain injury and posttraumatic stress disorder: a pilot study. Am J Occup Ther. 2011;65(4):419-427.
15. Lew HL, Amick MM, Kraft M, Stein MB, Cifu DX. Potential driving issues in combat returnees. NeuroRehabilitation. 2010;26(3):271-278.
16. Vasterling JL, Brailey K, Allain AN, Duke LM, Constans JI, Sutker PB. Attention, learning, and memory performances and intellectual resources in Vietnam veterans: PTSD and no disorder comparisons. Neuropsychology. 2002;16(1):5-14.
17. Kimble MO, Kaufman ML, Leonard LL, et al. Sentence completion test in veterans with and without PTSD: preliminary findings. Psychiatry Res. 2002;113(3):303-307.
18. Kuhn E, Drescher K, Ruzek J, Rosen C. Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. J Trauma Stress. 2010;23(3):399-402.
19. Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. Am J Psychiatry. 2009;166(7):768-776.
20. Hill JJ III, Mobo BH Jr, Cullen MR. Separating deployment-related traumatic brain injury and posttraumatic stress disorder in veterans: preliminary findings from the Veterans Affairs traumatic brain injury screening program. Am J Phys Med Rehabil. 2009;88(8):605-614.
21. Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
22. Hope DA, Burns JA, Hayes SA, Herbert JD, Warner MD. Automatic thoughts and cognitive restructuring in cognitive behavioral group therapy for social anxiety disorder. Cognit Ther Res. 2010;34(1):1-12.
23. Deffenbacher JL, Petrilli RT, Lynch RS, Oetting ER, Swaim RC. The driver’s angry thoughts questionnaire: a measure of angry cognitions when driving. Cognit Ther Res. 2003;27(4):383-402.
24. Beck AT, Emery G, Greenberg RL. Anxiety Disorders and Phobias: A Cognitive Perspective. Rev. paperback ed. New York, NY: Basic Books; 2005.
Combat veterans who have served in Iraq and Afghanistan in the post-9/11 era face unique reintegration challenges, one being the transition from driving in combat zones to driving at home.1 Relative to previous conflicts, post-9/11 combat involves increased participation in road patrols and convoys along with more prevalent threats of improvised explosive devices (IEDs).1,2 Roadside ambushes designed to destroy or stop vehicles became a common warfare strategy, meaning that driving became an inherently dangerous combat maneuver.3
The modern combat driving framework includes cognitive tools (eg, targeted aggression and tactical awareness) combined with specific behaviors (eg, driving unpredictably fast, using rapid lane changes, and keeping other vehicles at a distance to avoid IEDs).4 This framework is adaptive and lifesaving in combat zones, but it can be maladaptive and dangerous in civilian environments. Service members face difficulty in updating this cognitive framework after leaving combat zones and may continue to experience specific cognitions (eg, “the world is dangerous”; “that car holds an IED”) while driving on civilian roads.3,5-8
The high prevalence of posttraumatic stress disorder (PTSD) and traumatic brain injury (TBI) in post-9/11 veterans may complicate reintegration. Both PTSD and TBI are considered signature wounds of these conflicts.8-11 Traumatic brain injury may be sustained as a result of blast injury or other mechanism, including a closed head injury or penetrating brain injury.10 Previous literature indicated that both PTSD and TBI across all severities are related to deficits in executive functioning, attention, and memory.12-16
In addition to cognitive deficits, veterans with PTSD also may experience cognitive misappraisal, in which they are more likely to perceive ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations.5,17,18 Examples of roadside-specific trauma triggers include busy highways, traffic, loud or distracting noises, and vehicles of similar make and model as those commonly rigged with IEDs in Iraq or Afghanistan.2,7
Blast injury
Prior research suggests that veterans with PTSD and/or TBI experience significantly higher levels of anxiety in response to common roadside stimuli (ie, an overpass or stop sign) while driving than do veterans without either PTSD or TBI.3 Cognitive behavioral therapy (CBT) interventions have been developed and systematically evaluated for treating anxiety.21 The goal of CBT is to identify and change dysfunctional cognitions that result in biased information processing. Cognitive restructuring, the process by which problematic cognitions (negative automatic thoughts) are identified and examined for distortions, is one method of accomplishing this goal. Distortions then are disputed and rebutted with assistance from the clinician.22 A strategy for restructuring negative automatic thoughts is coping self-instruction, which centers on identifying when negative automatic thoughts are focused on others’ behavior, accepting that their behavior cannot be changed, and using positive coping behaviors to minimize negative automatic thoughts.23
The link between history of comorbid PTSD and TBI and combat driving, current driving anxiety, and coping strategies has not yet been extensively studied in veterans. Thus, the aim of the current study is to determine whether veterans with comorbid PTSD and TBI utilize coping self-instruction behind the wheel. Driving-specific coping self-instruction involves generating thoughts that are adaptive and accepting of others’ driving behaviors (eg, “Just turn up the radio and tune them out”). It was hypothesized that veterans with comorbid PTSD and TBI would endorse fewer coping self-instruction thoughts than would veterans without either PTSD or TBI.
Methods
The current project is part of a larger study that examines driving behaviors of post-9/11 combat veterans at the Michael J. Crescenz Veterans Affairs Medical Center in Philadelphia, Pennsylvania. Thirty-two male veterans aged between 22 and 48 years (M = 31.6, SD = 6.9) were included in the sample. Twenty-three were diagnosed with comorbid PTSD and TBI and 9 veterans with no major psychiatric or physical
Assessment
All participants completed a battery of questionnaires, including the Driver’s Angry Thoughts Questionnaire (DATQ).23 The DATQ was used to investigate the specific thoughts that veterans experienced while driving.23 Participants indicated on a Likert scale from 1 (not at all) to 5 (all the time) how often they experienced any of 65 thoughts while driving. Each item was categorized into 1 of 5 distinct subscales (Table 2). A frequency score was generated for each of the 5 subscales. Each subscale had good internal consistency and convergent, divergent, and predictive validity. The Coping Self-Instruction subscale, which is defined as engaging in relaxing thoughts to accept others’ driving behaviors, was of primary interest. It is a 9-item scale (frequency score can range from 9 to 45) with good reliability (α = .83).23
Given the small and unequal sample sizes, nonparametric independent samples Mann-Whitney U-tests were selected to compare frequency of driving-related thoughts across veterans with comorbid PTSD and TBI and those of veterans without either PTSD or TBI.
Results
Descriptive statistics and results for each DATQ subscale are reported in Table 3. Group comparisons revealed that veterans with comorbid PTSD and TBI endorsed statistically significantly fewer coping self-instruction thoughts while driving (M = 11.5, SD = 7.2) than did combat veterans without either PTSD or TBI (M = 18.1, SD = 6.9; U = 56.0, P = .05). Conversely, frequency of angry thoughts were statistically significant in their difference as a function of PTSD or TBI diagnostic status.
Discussion
While driving, veterans with PTSD or TBI endorsed statistically significantly fewer coping self-instruction thoughts than did veterans without either PTSD or TBI. Prior research suggests that veterans with PTSD or TBI experience greater anxiety than do veterans without either condition while driving.2,3 Taken together, this suggests that veterans with PTSD or TBI may lack efficient cognitive coping strategies related to the anxiety they experience while driving. Furthermore, the groups did not significantly differ in frequency of angry thoughts behind the wheel. This result was expected based on prior analyses that suggested that veterans with and without PTSD or TBI endorsed feelings of aggression, impatience, and frustration while driving at similar frequencies.3
Because all veterans in the current sample were exposed to combat, these results help to parse out the unique contribution of PTSD and TBI diagnoses on driving in civilian environments. Exposure to combat plus diagnoses of PTSD or TBI may be related to veterans’ ability to cope with typical driving situations at home. In the context of prior literature, results suggest that veterans with PTSD or TBI automatically may perceive neutral roadside stimuli as threatening, feel anxious in response to this perceived threat, and be ill-equipped to cope with this anxiety.3,5,17,18 According to CBT models, negative automatic thoughts play a critical role in maintaining anxiety.24 Particular cognitive distortions associated with PTSD symptomatology and combat driving experiences, such as misperceiving ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations, may therefore maintain driving anxiety following military separation.
Research on CBT interventions suggests that cognitive restructuring, including coping self-instruction, are effective treatments to reduce anxiety.22,24 The current findings suggest that combat veterans with PTSD and TBI who experience driving anxiety endorse significantly fewer coping self-instruction thoughts than do controls in response to anxiety-provoking driving situations. In fact, prior research suggests that a majority of veterans experiencing driving-related anxiety do not seek help for their symptoms, and many of those who do prefer to reach out to friends rather than mental health professionals.2 However, due to their high levels of anxiety, these veterans likely would benefit from CBT interventions specifically targeted to coping strategies for civilian driving. These coping strategies should focus on recognizing that common roadside stimuli are not necessarily threatening in civilian environments. This type of cognitive restructuring may help veterans better manage anxiety while driving.
Limitations
The current study is limited by its small and unequal sample sizes and lack of a noncombat exposure comparison group. Additionally, while this study highlights a potential relationship between reduced cognitive coping strategies and behind-the-wheel anxiety in veterans with PTSD or TBI, causal inferences cannot be made. It is possible that individuals without coping strategies who are deployed to combat are more likely to develop PTSD or TBI. Being equipped with few coping strategies may then lead these veterans to experience greater anxiety while driving. Conversely, PTSD and TBI symptoms may prevent veterans from developing coping strategies over time.
Furthermore, the comorbid PTSD and TBI group was separated from the military for significantly longer than was the control group. Future studies using a longitudinal design could better examine the potential causal relationship between comorbid PTSD and TBI and coping and determine whether endorsement of coping self-instruction changes as a function of time since military separation.
Veterans in the current study report a variety of deployment experiences and locations. Methods of combat, type of vehicle, driving terrain, and prevalence of IEDs changed over the multiple post-9/11 military campaigns. Veterans who were deployed to Iraq in the mid-2000s were instructed to drive quickly and erratically to avoid IEDs and mortars, whereas veterans deployed in later years were taught to drive slowly and carefully to hunt for IEDs in heavily armored vehicles.3 Seventy-five percent of the veterans with PTSD or TBI in the current sample were deployed to Iraq in the early to mid-2000s, compared with 33% of the veterans without PTSD or TBI. Thus, the 2 groups in the current sample may have experienced different combat environments, which could impact how they perceived roadside stimuli. Future studies should recruit a larger and more balanced sample to better determine whether specific combat experiences impact coping strategies while driving.
Conclusion
To the best of the authors’ knowledge, the current study is the first to examine specific types of thoughts that veterans with and without PTSD or TBI experience while driving on civilian roads. Veterans with PTSD or TBI are not engaging in as many coping self-instruction thoughts behind the wheel, despite experiencing greater anxiety than that of veterans without either PTSD or TBI. Cognitive behavioral therapy interventions for anxiety include engaging in coping self-instruction during anxiety-provoking situations.22 Therefore, veterans with PTSD or TBI may benefit from learning targeted coping self-instruction thoughts that they can utilize when anxiety-provoking situations arise behind the wheel. Results suggest that clinicians should work with veterans with comorbid PTSD and TBI to develop specific coping self-instruction statements that they can utilize internally when faced with anxiety-provoking driving situations.
Acknowledgments
This study is the result of work supported by the Council on Brain Injury (grant #260472). The authors thank Dr. Rosette Biester for her guidance.
Combat veterans who have served in Iraq and Afghanistan in the post-9/11 era face unique reintegration challenges, one being the transition from driving in combat zones to driving at home.1 Relative to previous conflicts, post-9/11 combat involves increased participation in road patrols and convoys along with more prevalent threats of improvised explosive devices (IEDs).1,2 Roadside ambushes designed to destroy or stop vehicles became a common warfare strategy, meaning that driving became an inherently dangerous combat maneuver.3
The modern combat driving framework includes cognitive tools (eg, targeted aggression and tactical awareness) combined with specific behaviors (eg, driving unpredictably fast, using rapid lane changes, and keeping other vehicles at a distance to avoid IEDs).4 This framework is adaptive and lifesaving in combat zones, but it can be maladaptive and dangerous in civilian environments. Service members face difficulty in updating this cognitive framework after leaving combat zones and may continue to experience specific cognitions (eg, “the world is dangerous”; “that car holds an IED”) while driving on civilian roads.3,5-8
The high prevalence of posttraumatic stress disorder (PTSD) and traumatic brain injury (TBI) in post-9/11 veterans may complicate reintegration. Both PTSD and TBI are considered signature wounds of these conflicts.8-11 Traumatic brain injury may be sustained as a result of blast injury or other mechanism, including a closed head injury or penetrating brain injury.10 Previous literature indicated that both PTSD and TBI across all severities are related to deficits in executive functioning, attention, and memory.12-16
In addition to cognitive deficits, veterans with PTSD also may experience cognitive misappraisal, in which they are more likely to perceive ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations.5,17,18 Examples of roadside-specific trauma triggers include busy highways, traffic, loud or distracting noises, and vehicles of similar make and model as those commonly rigged with IEDs in Iraq or Afghanistan.2,7
Blast injury
Prior research suggests that veterans with PTSD and/or TBI experience significantly higher levels of anxiety in response to common roadside stimuli (ie, an overpass or stop sign) while driving than do veterans without either PTSD or TBI.3 Cognitive behavioral therapy (CBT) interventions have been developed and systematically evaluated for treating anxiety.21 The goal of CBT is to identify and change dysfunctional cognitions that result in biased information processing. Cognitive restructuring, the process by which problematic cognitions (negative automatic thoughts) are identified and examined for distortions, is one method of accomplishing this goal. Distortions then are disputed and rebutted with assistance from the clinician.22 A strategy for restructuring negative automatic thoughts is coping self-instruction, which centers on identifying when negative automatic thoughts are focused on others’ behavior, accepting that their behavior cannot be changed, and using positive coping behaviors to minimize negative automatic thoughts.23
The link between history of comorbid PTSD and TBI and combat driving, current driving anxiety, and coping strategies has not yet been extensively studied in veterans. Thus, the aim of the current study is to determine whether veterans with comorbid PTSD and TBI utilize coping self-instruction behind the wheel. Driving-specific coping self-instruction involves generating thoughts that are adaptive and accepting of others’ driving behaviors (eg, “Just turn up the radio and tune them out”). It was hypothesized that veterans with comorbid PTSD and TBI would endorse fewer coping self-instruction thoughts than would veterans without either PTSD or TBI.
Methods
The current project is part of a larger study that examines driving behaviors of post-9/11 combat veterans at the Michael J. Crescenz Veterans Affairs Medical Center in Philadelphia, Pennsylvania. Thirty-two male veterans aged between 22 and 48 years (M = 31.6, SD = 6.9) were included in the sample. Twenty-three were diagnosed with comorbid PTSD and TBI and 9 veterans with no major psychiatric or physical
Assessment
All participants completed a battery of questionnaires, including the Driver’s Angry Thoughts Questionnaire (DATQ).23 The DATQ was used to investigate the specific thoughts that veterans experienced while driving.23 Participants indicated on a Likert scale from 1 (not at all) to 5 (all the time) how often they experienced any of 65 thoughts while driving. Each item was categorized into 1 of 5 distinct subscales (Table 2). A frequency score was generated for each of the 5 subscales. Each subscale had good internal consistency and convergent, divergent, and predictive validity. The Coping Self-Instruction subscale, which is defined as engaging in relaxing thoughts to accept others’ driving behaviors, was of primary interest. It is a 9-item scale (frequency score can range from 9 to 45) with good reliability (α = .83).23
Given the small and unequal sample sizes, nonparametric independent samples Mann-Whitney U-tests were selected to compare frequency of driving-related thoughts across veterans with comorbid PTSD and TBI and those of veterans without either PTSD or TBI.
Results
Descriptive statistics and results for each DATQ subscale are reported in Table 3. Group comparisons revealed that veterans with comorbid PTSD and TBI endorsed statistically significantly fewer coping self-instruction thoughts while driving (M = 11.5, SD = 7.2) than did combat veterans without either PTSD or TBI (M = 18.1, SD = 6.9; U = 56.0, P = .05). Conversely, frequency of angry thoughts were statistically significant in their difference as a function of PTSD or TBI diagnostic status.
Discussion
While driving, veterans with PTSD or TBI endorsed statistically significantly fewer coping self-instruction thoughts than did veterans without either PTSD or TBI. Prior research suggests that veterans with PTSD or TBI experience greater anxiety than do veterans without either condition while driving.2,3 Taken together, this suggests that veterans with PTSD or TBI may lack efficient cognitive coping strategies related to the anxiety they experience while driving. Furthermore, the groups did not significantly differ in frequency of angry thoughts behind the wheel. This result was expected based on prior analyses that suggested that veterans with and without PTSD or TBI endorsed feelings of aggression, impatience, and frustration while driving at similar frequencies.3
Because all veterans in the current sample were exposed to combat, these results help to parse out the unique contribution of PTSD and TBI diagnoses on driving in civilian environments. Exposure to combat plus diagnoses of PTSD or TBI may be related to veterans’ ability to cope with typical driving situations at home. In the context of prior literature, results suggest that veterans with PTSD or TBI automatically may perceive neutral roadside stimuli as threatening, feel anxious in response to this perceived threat, and be ill-equipped to cope with this anxiety.3,5,17,18 According to CBT models, negative automatic thoughts play a critical role in maintaining anxiety.24 Particular cognitive distortions associated with PTSD symptomatology and combat driving experiences, such as misperceiving ambiguous stimuli as threatening because of an inability to suppress trauma-related schema and associations, may therefore maintain driving anxiety following military separation.
Research on CBT interventions suggests that cognitive restructuring, including coping self-instruction, are effective treatments to reduce anxiety.22,24 The current findings suggest that combat veterans with PTSD and TBI who experience driving anxiety endorse significantly fewer coping self-instruction thoughts than do controls in response to anxiety-provoking driving situations. In fact, prior research suggests that a majority of veterans experiencing driving-related anxiety do not seek help for their symptoms, and many of those who do prefer to reach out to friends rather than mental health professionals.2 However, due to their high levels of anxiety, these veterans likely would benefit from CBT interventions specifically targeted to coping strategies for civilian driving. These coping strategies should focus on recognizing that common roadside stimuli are not necessarily threatening in civilian environments. This type of cognitive restructuring may help veterans better manage anxiety while driving.
Limitations
The current study is limited by its small and unequal sample sizes and lack of a noncombat exposure comparison group. Additionally, while this study highlights a potential relationship between reduced cognitive coping strategies and behind-the-wheel anxiety in veterans with PTSD or TBI, causal inferences cannot be made. It is possible that individuals without coping strategies who are deployed to combat are more likely to develop PTSD or TBI. Being equipped with few coping strategies may then lead these veterans to experience greater anxiety while driving. Conversely, PTSD and TBI symptoms may prevent veterans from developing coping strategies over time.
Furthermore, the comorbid PTSD and TBI group was separated from the military for significantly longer than was the control group. Future studies using a longitudinal design could better examine the potential causal relationship between comorbid PTSD and TBI and coping and determine whether endorsement of coping self-instruction changes as a function of time since military separation.
Veterans in the current study report a variety of deployment experiences and locations. Methods of combat, type of vehicle, driving terrain, and prevalence of IEDs changed over the multiple post-9/11 military campaigns. Veterans who were deployed to Iraq in the mid-2000s were instructed to drive quickly and erratically to avoid IEDs and mortars, whereas veterans deployed in later years were taught to drive slowly and carefully to hunt for IEDs in heavily armored vehicles.3 Seventy-five percent of the veterans with PTSD or TBI in the current sample were deployed to Iraq in the early to mid-2000s, compared with 33% of the veterans without PTSD or TBI. Thus, the 2 groups in the current sample may have experienced different combat environments, which could impact how they perceived roadside stimuli. Future studies should recruit a larger and more balanced sample to better determine whether specific combat experiences impact coping strategies while driving.
Conclusion
To the best of the authors’ knowledge, the current study is the first to examine specific types of thoughts that veterans with and without PTSD or TBI experience while driving on civilian roads. Veterans with PTSD or TBI are not engaging in as many coping self-instruction thoughts behind the wheel, despite experiencing greater anxiety than that of veterans without either PTSD or TBI. Cognitive behavioral therapy interventions for anxiety include engaging in coping self-instruction during anxiety-provoking situations.22 Therefore, veterans with PTSD or TBI may benefit from learning targeted coping self-instruction thoughts that they can utilize when anxiety-provoking situations arise behind the wheel. Results suggest that clinicians should work with veterans with comorbid PTSD and TBI to develop specific coping self-instruction statements that they can utilize internally when faced with anxiety-provoking driving situations.
Acknowledgments
This study is the result of work supported by the Council on Brain Injury (grant #260472). The authors thank Dr. Rosette Biester for her guidance.
1. Belmont PJ, Schoenfeld AJ, Goodman G. Epidemiology of combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom: orthopaedic burden of disease. J Surg Orthop Adv. 2010;19(1):2-7.
2. Zinzow HM, Brooks J, Stern EB. Driving-related anxiety in recently deployed service members: cues, mental health correlates, and help-seeking behavior. Mil Med. 2013;178(3):e357-e361.
3. Whipple EK, Schultheis MT, Robinson KM. Preliminary findings of a novel measure of driving behaviors in veterans with comorbid TBI and PTSD. J Rehabil Res Dev. 2016;53(6):827-838.
4. Adler AB, Bliese PD, McGurk D, Hoge CW, Castro CA. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: randomization by platoon. J Consult Clin Psychol. 2009;77(5):928-940.
5. Amick MM, Kraft M, McGlinchey R. Driving simulator performance of veterans from the Iraq and Afghanistan wars. J Rehabil Res Dev. 2013;50(4):463-470.
6. Classen S, Cormack NL, Winter SM, et al. Efficacy of an occupational therapy driving intervention for returning combat veterans. OTJR (Thorofare NJ). 2014;34(4):177-182.
7. Hannold EM, Classen S, Winter S, Lanford DN, Levy CE. Exploratory pilot study of driving perceptions among OIF/OEF veterans with mTBI and PTSD. J Rehabil Res Dev. 2013;50(10):1315-1330.
8. Lew HL, Kraft M, Pogoda TK, Amick MM, Woods P, Cifu DX. Prevalence and characteristics of driving difficulties in Operation Iraqi Freedom/Operation Enduring Freedom combat returnees. J Rehabil Res Dev. 2011;48(8):913-925.
9. Arthur DC, MacDermid S, Kiley KC; Defense Health Board Task Force on Mental Health. An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: Defense Health Board; 2007.
10. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008.
11. Independent Review Group. Rebuilding the Trust: Independent Review Group Report on Rehabilitation Care and Administrative Processes at Walter Reed Army Medical Center and National Naval Medical Center. Arlington, VA: Independent Review Group; 2007
12. Bailie JM, Cole WR, Ivins B, et al. The experience, expression, and control of anger following traumatic brain injury in a military sample. J Head Trauma Rehabil. 2015;30(1):12-20.
13. Campbell TA, Nelson LA, Lumpkin R, Yoash-Gantz RE, Pickett TC, McCormick CL. Neuropsychological measures of processing speed and executive functioning in combat veterans with PTSD, TBI, and comorbid TBI/PTSD. Psychiatr Ann. 2009;39(8):796-803.
14. Classen S, Levy C, Meyer DL, Bewernitz M, Lanford DN, Mann WC. Simulated driving performance of combat veterans with mild tramatic brain injury and posttraumatic stress disorder: a pilot study. Am J Occup Ther. 2011;65(4):419-427.
15. Lew HL, Amick MM, Kraft M, Stein MB, Cifu DX. Potential driving issues in combat returnees. NeuroRehabilitation. 2010;26(3):271-278.
16. Vasterling JL, Brailey K, Allain AN, Duke LM, Constans JI, Sutker PB. Attention, learning, and memory performances and intellectual resources in Vietnam veterans: PTSD and no disorder comparisons. Neuropsychology. 2002;16(1):5-14.
17. Kimble MO, Kaufman ML, Leonard LL, et al. Sentence completion test in veterans with and without PTSD: preliminary findings. Psychiatry Res. 2002;113(3):303-307.
18. Kuhn E, Drescher K, Ruzek J, Rosen C. Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. J Trauma Stress. 2010;23(3):399-402.
19. Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. Am J Psychiatry. 2009;166(7):768-776.
20. Hill JJ III, Mobo BH Jr, Cullen MR. Separating deployment-related traumatic brain injury and posttraumatic stress disorder in veterans: preliminary findings from the Veterans Affairs traumatic brain injury screening program. Am J Phys Med Rehabil. 2009;88(8):605-614.
21. Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
22. Hope DA, Burns JA, Hayes SA, Herbert JD, Warner MD. Automatic thoughts and cognitive restructuring in cognitive behavioral group therapy for social anxiety disorder. Cognit Ther Res. 2010;34(1):1-12.
23. Deffenbacher JL, Petrilli RT, Lynch RS, Oetting ER, Swaim RC. The driver’s angry thoughts questionnaire: a measure of angry cognitions when driving. Cognit Ther Res. 2003;27(4):383-402.
24. Beck AT, Emery G, Greenberg RL. Anxiety Disorders and Phobias: A Cognitive Perspective. Rev. paperback ed. New York, NY: Basic Books; 2005.
1. Belmont PJ, Schoenfeld AJ, Goodman G. Epidemiology of combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom: orthopaedic burden of disease. J Surg Orthop Adv. 2010;19(1):2-7.
2. Zinzow HM, Brooks J, Stern EB. Driving-related anxiety in recently deployed service members: cues, mental health correlates, and help-seeking behavior. Mil Med. 2013;178(3):e357-e361.
3. Whipple EK, Schultheis MT, Robinson KM. Preliminary findings of a novel measure of driving behaviors in veterans with comorbid TBI and PTSD. J Rehabil Res Dev. 2016;53(6):827-838.
4. Adler AB, Bliese PD, McGurk D, Hoge CW, Castro CA. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: randomization by platoon. J Consult Clin Psychol. 2009;77(5):928-940.
5. Amick MM, Kraft M, McGlinchey R. Driving simulator performance of veterans from the Iraq and Afghanistan wars. J Rehabil Res Dev. 2013;50(4):463-470.
6. Classen S, Cormack NL, Winter SM, et al. Efficacy of an occupational therapy driving intervention for returning combat veterans. OTJR (Thorofare NJ). 2014;34(4):177-182.
7. Hannold EM, Classen S, Winter S, Lanford DN, Levy CE. Exploratory pilot study of driving perceptions among OIF/OEF veterans with mTBI and PTSD. J Rehabil Res Dev. 2013;50(10):1315-1330.
8. Lew HL, Kraft M, Pogoda TK, Amick MM, Woods P, Cifu DX. Prevalence and characteristics of driving difficulties in Operation Iraqi Freedom/Operation Enduring Freedom combat returnees. J Rehabil Res Dev. 2011;48(8):913-925.
9. Arthur DC, MacDermid S, Kiley KC; Defense Health Board Task Force on Mental Health. An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: Defense Health Board; 2007.
10. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008.
11. Independent Review Group. Rebuilding the Trust: Independent Review Group Report on Rehabilitation Care and Administrative Processes at Walter Reed Army Medical Center and National Naval Medical Center. Arlington, VA: Independent Review Group; 2007
12. Bailie JM, Cole WR, Ivins B, et al. The experience, expression, and control of anger following traumatic brain injury in a military sample. J Head Trauma Rehabil. 2015;30(1):12-20.
13. Campbell TA, Nelson LA, Lumpkin R, Yoash-Gantz RE, Pickett TC, McCormick CL. Neuropsychological measures of processing speed and executive functioning in combat veterans with PTSD, TBI, and comorbid TBI/PTSD. Psychiatr Ann. 2009;39(8):796-803.
14. Classen S, Levy C, Meyer DL, Bewernitz M, Lanford DN, Mann WC. Simulated driving performance of combat veterans with mild tramatic brain injury and posttraumatic stress disorder: a pilot study. Am J Occup Ther. 2011;65(4):419-427.
15. Lew HL, Amick MM, Kraft M, Stein MB, Cifu DX. Potential driving issues in combat returnees. NeuroRehabilitation. 2010;26(3):271-278.
16. Vasterling JL, Brailey K, Allain AN, Duke LM, Constans JI, Sutker PB. Attention, learning, and memory performances and intellectual resources in Vietnam veterans: PTSD and no disorder comparisons. Neuropsychology. 2002;16(1):5-14.
17. Kimble MO, Kaufman ML, Leonard LL, et al. Sentence completion test in veterans with and without PTSD: preliminary findings. Psychiatry Res. 2002;113(3):303-307.
18. Kuhn E, Drescher K, Ruzek J, Rosen C. Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. J Trauma Stress. 2010;23(3):399-402.
19. Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. Am J Psychiatry. 2009;166(7):768-776.
20. Hill JJ III, Mobo BH Jr, Cullen MR. Separating deployment-related traumatic brain injury and posttraumatic stress disorder in veterans: preliminary findings from the Veterans Affairs traumatic brain injury screening program. Am J Phys Med Rehabil. 2009;88(8):605-614.
21. Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
22. Hope DA, Burns JA, Hayes SA, Herbert JD, Warner MD. Automatic thoughts and cognitive restructuring in cognitive behavioral group therapy for social anxiety disorder. Cognit Ther Res. 2010;34(1):1-12.
23. Deffenbacher JL, Petrilli RT, Lynch RS, Oetting ER, Swaim RC. The driver’s angry thoughts questionnaire: a measure of angry cognitions when driving. Cognit Ther Res. 2003;27(4):383-402.
24. Beck AT, Emery G, Greenberg RL. Anxiety Disorders and Phobias: A Cognitive Perspective. Rev. paperback ed. New York, NY: Basic Books; 2005.
Yoga-Based Classes for Veterans With Severe Mental Illness: Development, Dissemination, and Assessment
There is growing interest in developing a holistic and integrative approach for the treatment of severe mental illnesses (SMI), such as schizophrenia, major depression, posttraumatic stress disorder (PTSD), and anxiety disorders. Western medicine has traditionally focused on the direct treatment of symptoms and separated the management of physical and mental health, but increasing attention is being given to complementary and alternative medicine (CAM) for patients with SMI.
Recognizing the connectedness of the mind and body, these complementary or alternative approaches incorporate nontraditional therapeutic techniques with mainstream treatment methods, including psychopharmacology and psychotherapy.1 Patients with SMI may particularly benefit from a mind-body therapeutic approach, because they often experience psychological symptoms such as stress, anxiety, depression and psychosis, as well as a preponderance of medical comorbidities, including obesity, diabetes mellitus, and cardiovascular disease, some of which are compounded by adverse effects (AEs) of essential pharmacologic treatments.2-4 Mind-body interventions might also be particularly advantageous for veterans, who often experience a range of interconnected physical and psychological difficulties due to trauma exposure and challenges transitioning from military to civilian life.5
Related: Complementary and Alternative Medicine for Chronic Musculoskeletal Pain
In 2002, the White House Commission on Complementary and Alternative Medicine Policy issued a report supporting CAM research and integration into existing medical systems.6 The DoD later established Total Force Fitness, a holistic health care program for active-duty military personnel.7 The VA has also incorporated mind-body and holistic strategies into veteran care.8 One such mind-body intervention, yoga, is becoming increasingly popular within the health care field.
Recent research has documented the effectiveness of yoga, underscoring its utility as a mind-body therapeutic approach. Yoga is associated with improvement in balance and flexibility,9 fatigue,10 blood pressure,11 sleep,12 strength,13 and pain14 in both healthy individuals and patients with medical and psychiatric disorders.15 The literature also illustrates that yoga has led to significant improvements in stress and psychiatric symptoms in individuals with PTSD, schizophrenia, depression, and anxiety.16-22 A previous meta-analysis conducted by the authors, which considered studies of the effectiveness of yoga as an adjunctive treatment for patients with mental illness, found that 212 studies with null results would need to be located and incorporated to negate the positive effects of yoga found in the literature.17
Because yoga emphasizes the practice of mindfulness and timing movement with breath awareness, it is a calming practice that may decrease stress and relieve psychiatric symptoms not treated through psychopharmacology and psychotherapy.17,21 Recent research has postulated that the physiological mechanisms by which this occurs may include (a) reduction in sympathetic and increase in parasympathetic activity23,24; (b) increases in heart-rate variability and respiratory sinus arrhythmia, low levels of which are associated with anxiety, panic disorder, and depression23,24; (c) increases in melatonin and serotonin 25-27; and (d) decrease in cortisol.28,29
Related: Enhancing Patient Satisfaction Through the Use of Complementary Therapies
As yoga may calm the autonomic nervous system and reduce stress, it may benefit patients with SMI, whose symptoms are often aggravated by stress.30 In addition, veterans experience both acute stressors and high levels of chronic stress.5 Therefore, because they experience mind-body comorbid illnesses as well as high levels of stress, the authors believe that veterans with SMI could benefit greatly from a tailored yoga-based program as part of a holistic approach that includes necessary medication and evidence-based therapies.
In order to evaluate the effects of a yoga program on veterans receiving mental health treatment across the VA Greater Los Angeles Healthcare System (VAGLAHS), the authors developed a set of yoga-based wellness classes called Breathing, Stretching, Relaxation (BSR) classes. This article describes the process of developing these classes and outlines the procedures and results of a study to assess their effects.
BSR Classes
The development of BSR classes took place at the West Los Angeles VA Medical Center (WLAVAMC), within the Psychosocial Rehabilitation and Recovery Center (PRRC) program. The PRRC is a psychoeducational program that focuses on the biological, psychological, social, and spiritual aspects of life in order to help veterans with SMI rehabilitate and reintegrate into the community. The program allows veterans to create their own recovery curriculum by selecting from diverse classes led by program staff members, including physicians, psychologists, nurses, social workers, nutritionists, and recreational therapists.
Development of BSR Protocols
The primary goal of this project was to develop a yoga-based program tailored to the specific needs of veterans with SMI. To the authors’ knowledge, BSR is the first yoga-based program customized for SMI. The BSR classes were developed within interdisciplinary focus groups that included professional yoga teachers, the director of the PRRC, psychiatrists, psychologists, nurses, occupational therapists, and physical therapists. Drawing on their experience with SMI and yoga, members of the focus groups identified 3 aspects of yoga that would be most beneficial to veterans with SMI, and the program was designed to optimize these effects. Because SMI can both create and be exacerbated by stress, BSR classes were designed to reduce stress and provide veterans with the tools to monitor and manage their stress.
Breathing and meditative techniques were adapted from yoga in order to facilitate stress reduction. In addition, aerobic elements of yoga have the potential to help veterans manage their incidence of medical diseases, such as cardiovascular disease, obesity, and diabetes. Patients with SMI are at a greater risk for developing these diseases, so classes were designed to incorporate physical stretching elements to promote overall health.4,31-33 Finally BSR was designed to improve veteran self- efficacy and self-esteem, and to place veterans at the center of their care by equipping them with skills to practice BSR independently.
Related: Mindfulness to Reduce Stress
The focus groups also identified the logistic requirements when implementing a yoga-based program for veterans with SMI, including (a) obtaining participant or conservator consent; (b) obtaining medical clearance from care providers, given the high prevalence of medical comorbidities; (c) removing the traditional yoga terms, taking a secular approach, and naming the class “Breathing, Stretching, Relaxation” without directly referencing yoga; (d) asking veterans’ permission before incorporating physical contact into demonstrations, because veterans with SMI, especially those with PTSD, might be uncomfortable with touching from instructors; (e) creating protocols of varying duration and intensity so that BSR was approachable for veterans with diverse levels of physical ability; and (f) ensuring that a clinician who regularly works with SMI patients be present to supervise classes for the safety of patients and instructors.
Yoga instructors and clinicians collaborated to create adaptable 30- and 50-minute protocols that reflected best practices for an SMI population. The 30-minute seated BSR class protocol is included in eAppendix A. Once protocols were finalized, a Train the Trainer program was established to facilitate dissemination of BSR to clinicians working with veterans with SMI throughout the VAGLAHS.
Interested clinicians were given protocols and trained to lead BSR classes on their own. Subsequently, clinician-led BSR classes of various lengths (depending on clinician preference and program scheduling) were established at PRRCs and other mental health programs, such as Mental Health Recovery and Intensive Treatment and Dual Diagnosis Treatment Program, throughout the VAGLAHS. These programs were selected, because they are centered on recovery and improvements in symptoms of SMI. The adoption of a Train the Trainer model, through which VA clinicians were trained by professional yoga instructors, allowed for seamless integration of BSR into VA usual care for veterans with SMI.
Assessment of Classes
The authors conducted a study to assess the quality and effectiveness of BSR classes. This survey research was approved by the VAGLAHS institutional review board for human subjects. The authors hypothesized that there would be significant improvements in veterans’ stress, pain, well-being, and perception of the benefits of BSR over 8 weeks of participation in classes. Also hypothesized was that there would be greater benefits in veterans who participated in longer classes and who attended classes more frequently.
Methods
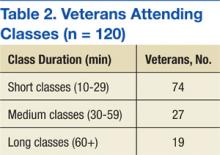
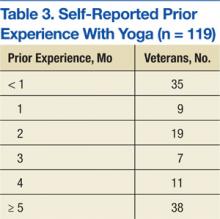
A total of 120 veterans completed surveys after participating in clinician- and yoga instructor-led BSR classes at the 3 sites within the VAGLAHS: WLAVAMC, Los Angeles Ambulatory Care Center (LAACC), and Sepulveda Ambulatory Care Center (SACC). At the WLAVAMC, surveys were collected at 10-, 30-, 60-, and 90-minute classes. At LAACC, surveys were collected at 30- and 60-minute classes. At SACC, surveys were collected at 20- and 45-minute classes. A researcher noted the duration of the class and was available to assist with comprehension. Veterans completed identical surveys after classes at a designated week 0 (baseline), week 4, and week 8. Of the 120 patients with an initial survey, 82 completed at least 1 follow-up survey and 49 completed both follow-up surveys.
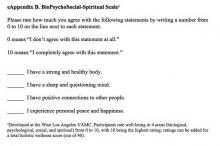
Survey packets included (a) demographic questions, including age, gender, and ethnicity; (b) class participation questions, including frequency of class attendance, patients’ favorite aspect of class, and dura tion of class attendance (in months of prior participation); (c) a pain rating from 0 (no pain) to 10 (the worst pain imaginable); (d) the BioPsychoSocial-Spiritual (BPSS) Scale (eAppendix B), developed at the WLAVAMC, which provides wellness scores from 0 (low) to 10 (high) in 4 areas as well as a holistic wellness score from 0 (low) to 40 (high); (e) the Perceived Stress Scale (PSS), developed by Cohen and colleagues, which generates a stress score for the past month from 0 (low) to 40 (high)34; and (f) the Perceived Benefits of Yoga Questionnaire (PBYQ) (eAppendix C), which rates participants’ opinions about the benefits of yoga from 12 (low) to 60 (high) and is based on the Perceived Benefits of Dance Questionnaire.35
Statistical Analysis
Pearson’s r correlation coefficients were calculated between PBYQ scores and quantitative survey items at each time point (weeks 0, 4, and 8). Linear mixed-effects models were used to test for effects of multiple predictor variables on individual outcomes. Each model had a random intercept by participant, and regressors included main effects for the following: survey week (0, 4, or 8), class duration (in minutes), age, sex, ethnicity, frequency of attendance (in days per week), and duration of attendance (in months). For all statistical analyses, a 2-tailed significance criterion of α = .05 was used.
Results
Veterans who completed surveys were predominantly male (90.8%) and averaged 61.4 years of age. Table 1 shows demographic information. Table 2 displays the number of participants who were involved in short (< 30 min), medium (30-59 min), and long (> 60 min) classes. Veteran participants also had a wide range of prior BSR experience (Table 3).
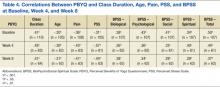
At all time points, PBYQ scores were significantly positively correlated with class duration and biological, psychological, social, spiritual, and total well-being as measured by the BPSS. The PBYQ scores at all time points were also significantly negatively correlated with age, pain ratings, and PSS scores. Table 4 includes specific Pearson’s r values.
Survey week was not significantly associated with any individual outcome measures. There were no significant regressors for total PSS score or total BPSS score within the linear models. However, participants’ PBYQ scores were significantly associated with age (t(98) = -2.13, P = .036), frequency of attendance (t(103) = 2.10, P = .038), and class duration (t(98) = 4.35, P < .001). Additionally, class duration was significantly associated with pain (t(98) = -3.01, P = .003), with longer duration associated with less pain. Ethnicity was also associated with pain, with African American veterans reporting less pain than did white (t(98) = -2.41, P = .017) and Hispanic (t(98) = -2.31, P = .023) veterans. Because ethnicity was significantly associated with class duration (F(5,339) = 3.81, P = .002), the authors used an analysis of covariance to test for a mediating effect of ethnicity on the relationship between class duration and pain. Although there was a partial mediation (F(5,203) = 2.57, P = .028), the main effect of class duration remained significant.
Discussion and Limitations
The goals of this project were to develop a yoga-based program tailored for veterans with SMI and assess the program in a sample of veterans with SMI on subjective reports of stress, pain, well-being, and benefits of yoga. The authors hypothesized that significant improvements in these measures in veterans with SMI would be observed over 8 weeks of participation in BSR classes and that there would be greater benefits in veterans who participated in longer classes and who attended classes more frequently.
The authors succeeded in developing an adaptable yoga-based wellness program for veterans with SMI that can be both practiced in structured classes and incorporated into veterans’ everyday routines. The BSR classes were well tolerated by veterans with SMI, caused no discernible AEs, and are readily available for dissemination across other mental health programs. Veterans described integrating the tools they learned within BSR classes into their daily lives, helping them to manage pain; feel more flexible; reduce stress, anxiety, depression, and PTSD symptoms; and increase relaxation and feelings of self-control and confidence. Table 5 shows qualitative feedback collected from veterans. In addition, the Train the Trainer model optimized clinical applicability and flexibility, demonstrating that clinicians can seamlessly integrate BSR classes into a health care plan for veterans with SMI.
In assessing quantitative measures of stress, pain, well-being, and perceived benefits of a yoga-based program, veterans who reported BSR classes as beneficial experienced lower levels of pain and stress and higher levels of biological, psychological, social, spiritual, and overall well-being. Those veterans who perceived BSR as more beneficial tended to be younger and attend longer classes with greater frequency. Veterans who attended longer classes also reported experiencing less pain. This may be because the more rigorous stretching and posing involved in longer BSR classes made them more effective at reducing pain; however, it is also possible that veterans who were experiencing more pain avoided these longer classes due to their rigor and length.
Results suggest that longer classes attended with greater regularity may be more beneficial to veterans than short and infrequent classes, particularly in regards to their pain. Despite the relationships between class and outcome variables, the authors did not find significant improvements in measures of wellness, pain, stress, or perceived benefits of BSR over time, as was hypothesized. This may be because the data collection for this study began after classes had been established for some time. In fact, only 35 of 120 veterans included in this study reported having < 1 month of BSR experience at week 0, suggesting that results collected from week 0 did not represent a true baseline measurement. Although no relationship was found between prior duration of attendance and any outcome measures, the fact that most veterans in the sample had attended classes for several months prior to completing surveys may have biased the results by favoring the responses of veterans who were more invested in the classes. Improvements may have been better captured in a BSR-naïve sample.
The finding that the PBYQ score was significantly correlated with all other outcome measures (pain, BPSS score, and PSS score) raises some questions about the ways in which these classes were beneficial to veterans. It may be that veterans who experienced more positive outcomes from classes saw BSR as more beneficial, but it is also possible that veterans who entered classes with greater expectations experienced better outcomes due to a placebo effect—that is, outcomes may have been influenced more by the expectation than by the content of the classes. In the case of well-being (BPSS scores) and stress (PSS score), this could explain why these outcomes were significantly correlated with perceived benefits of BSR but were not significantly related to any class-related variables such as duration and frequency of attendance. Pain ratings, however, were related to class variables and perceived benefits of BSR.
In a post hoc analysis, the main effect of the PBYQ score as a regressor was added to the linear model for pain, resulting in the PBYQ score having a significant main effect (t(100) = -2.98, P = .004). The main effect of class duration remained significant (t(97) = -1.99, P = .050) but was less substantial when the PBYQ score was added, suggesting some correlation between class duration and pain, independent of BSR’s perceived benefits. Future research should consider the possible mediating effect of perceptions of the effectiveness of a yoga-based program a priori or control for placebo effects in order to address the degree to which outcomes are influenced by participant expectations.
This study had a few other notable limitations. Because it was an observational study administered within a clinical mental health program, a control group was not included. Measurement began after BSR classes were established, so veterans had varying levels of prior experience. Specific SMI and medical diagnosis information was not collected from individual veterans. Data were collected from classes of varying length and intensity. The BSR classes often took place within larger programs at the VA, which offered comprehensive care, so some effects of the BSR classes might have been confounded with concurrent evidenced-based treatments or other holistic care programs. Due to these limitations, particularly the absence of a control group, the relationships between BSR participation and health outcomes cannot be assumed to be causal, because a multitude of other variables, such as patient contact and expectancy effects, may have influenced outcomes.
Future Directions
Future research should aim to utilize a control group and collect data from classes of the same intensity and length to better examine whether BSR can be causally linked with improvements in measures of stress, pain, and well-being and to attempt to control for expectancy and contact effects. In addition, future research should aim to recruit a BSR-naïve sample to account for prior experience. Future studies should also aim to parse out whether BSR is differentially effective for each SMI or medical diagnosis, whether there is a relationship between class time and outcomes (as these results suggest that longer class times might be more beneficial for pain), and whether any pain-management benefits from BSR influence other measures of functionality and well-being. Finally, future research can further divide BSR into its active components, such as meditative breathing and aerobic stretching, in order to examine which aspect leads to the greatest effect on each measure; the current results imply that the more rigorous components of BSR classes have the greatest effects on pain.
Conclusion
A yoga-based class affects the mind and body, making it particularly useful for veterans with SMI who experience a range of physical and psychological symptoms and comorbidities.4 Other studies have demonstrated that when practiced alone, yoga leads to improvements in both physical and psychological symptoms.15,17 Looking forward, yoga-based classes may be implemented as part of a larger biopsychosocial-spiritual care plan that is being embraced both within and outside of the VA.7,8,36,37 This integrative health care model suggests that psychosocial and CAM modalities are additive and should be practiced concurrently.37
Although little research has assessed the effects of comprehensive psychosocial and CAM treatment programs, initial research indicates that these programs are associated with reductions in symptoms of medical and mental illness.37-40 Participants in BSR classes may derive further benefits if classes are incorporated into a larger holistic health care plan that includes both traditional psychiatric treatment modalities and CAM therapies that integrate biopsychosocial-spiritual components.
Acknowledgements
The authors would like to thank Nancy Mohler, Anne Platt, and Matthew Crowder, all professional yoga instructors, for their integral role in developing classes, providing classes to veterans, and assisting VA staff with training. The authors also acknowledge Rosie Dominguez, LCSW, for expertly leading BSR classes at LAACC. The authors also thank Irina Arnold, MS, MD, and Vanessa Streiff, MA, for their vital assistance with data collection at SACC.
Funding for the development of BSR protocols, quality improvement research, and expenses associated with classes was provided by the Disabled American Veterans Charitable Service Trust. Support for dissemination of classes to multiple VA programs was provided by a grant from the VA Center of Innovation for Patient Centered Care, headed by Sandra Robertson, RN, MSN, PH-CNS.
The authors are very grateful to the veterans and staff of the Mental Health Intensive Case Management, Psychosocial Rehabilitation and Recovery Centers, Mental Health Clinics, and Domiciliary throughout Greater Los Angeles for their support of the BSR classes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. National Center for Complementary and Integrative Health. Complementary, alternative, or integrative health: what's in a name? U.S. Department of Health and Human Services, National Institutes of Health Website. http://nccam.nih.gov/health/whatiscam. Updated March 2015. Accessed August 27, 2015.
2. Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Fleischhacker WW, Cetkovich-Bakmas M, De Hert M, et al. Comorbid somatic illnesses in patients with severe mental disorders: clinical, policy, and research challenges. J Clin Psychiatry. 2008;69(4):514-519.
4. Wirshing DA, Boyd JA, Meng LR, Ballon JS, Marder SR, Wirshing WC. The effects of novel antipsychotics on glucose and lipid levels. J Clin Psychiatry. 2002;63(10):856-865.
5. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008.
6. White House Commission on Complementary and Alternative Medicine Policy. Final Report. Washington, DC: White House Commission on Complementary and Alternative Medicine Policy; 2002.
7. Land BC. Current Department of Defense guidance for total force fitness. Mil Med. 2010;175(suppl 8):3-5.
8. U.S. Department of Veterans Affairs, Veterans Health Administration. Pain Management. VHA Directive 2009-053. Washington, DC: U.S. Department of Veterans Affairs, Veterans Health Administration; 2009.
9. Oken BS, Zajdel D, Kishiyama S, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med. 2006;12(1):40-47.
10. Bower JE, Garet D, Sternlieb B, et al. Yoga for persistent fatigue in breast cancer survivors: a randomized controlled trial. Cancer. 2012;118(15):3766-3775.
11. Cade WT, Reeds DN, Mondy KE, et al. Yoga lifestyle intervention reduces blood pressure in HIV-infected adults with cardiovascular disease risk factors. HIV Med. 2010;11(6):379-388.
12. Innes KE, Selfe TK. The effects of a gentle yoga program on sleep, mood, and blood pressure in older women with restless leg syndrome (RLS): a preliminary randomized controlled trial. Evid Based Complement Alternat Med. 2012;2012:294058.
13. Van Puymbroeck M, Payne LL, Hsieh PC. A phase I feasibility study of yoga on the physical health and coping of informal caregivers. Evid Based Complement Alternat Med. 2007;4(4):519-529.
14. Rani K, Tiwari SC, Singh U, Agrawal GG, Srivastava N. Six-month trial of Yoga Nidra in menstrual disorder patients: effects on somatoform symptoms. Ind Psychiatry J. 2011;20(2):97-102.
15. Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J Altern Complement Med. 2010;16(1):3-12.
16. Banerjee B, Vadiraj HS, Ram A, et al. Effects of an integrated yoga program in modulating psychological stress and radiation-induced genotoxic stress in breast cancer patients undergoing radiotherapy. Integr Cancer Ther. 2007;6(3):242-250.
17. Cabral P, Meyer HB, Ames D. Effectiveness of yoga therapy as a complementary treatment for major psychiatric disorders: a meta-analysis. Prim Care Companion CNS Disord. 2011;13(4):doi:10.4088/PCC.10r01068.
18. Katzman MA, Vermani M, Gerbarg PL, et al. A multicomponent yoga-based, breath intervention program as an adjunctive treatment in patients suffering from generalized anxiety disorder with or without comorbidities. Int J Yoga. 2012;5(1):57-65.
19. Köhn M, Persson Lundholm U, Bryngelsson IL, Anderzén-Carlsson A, Westerdahl E. Medical yoga for patients with stress-related symptoms and diagnoses in primary health care: a randomized controlled trial. Evid Based Complement Alternat Med. 2013;2013:215348.
20. Krishnamurthy MN, Telles S. Assessing depression following two ancient Indian interventions: effects of yoga and ayurveda on older adults in a residential home. J Gerontol Nurs. 2007;33(2):17-23.
21. Meyer HB, Katsman A, Sones AC, Auerbach DE, Ames D, Rubin RT. Yoga as an ancillary treatment for neurological and psychiatric disorders: a review. J Neuropsychiatry Clin Neurosci. 2012;24(2):152-164.
22. Visceglia E, Lewis S. Yoga therapy as an adjunctive treatment for schizophrenia: a randomized, controlled pilot study. J Altern Complement Med. 2011;17(7):601-607.
23. Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression, part I-neurophysiologic model. J Altern Complement Med. 2005;11(1):189-201.
24. Brown RP, Gerbarg PL. Yoga breathing, meditation, and longevity. Ann N Y Acad Sci. 2009;1172:54-62.
25. Harinath K, Malhotra AS, Pal K, et al. Effects of hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004;10(2):261-268.
26. Tooley GA, Armstrong SM, Norman TR, Sali A. Acute increases in night-time plasma melatonin levels following a period of meditation. Biol Psychol. 2000;53(1):69-78.
27. Walton KG, Pugh ND, Gelderloos P, Macrae P. Stress reduction and preventing hypertension: preliminary support of a psychoneuroendocrine mechanism. J Altern Complement Med. 1995;1(3):263-283.
28. Banasik J, Williams H, Haberman M, Blank SE, Bendel R. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23(3):135-142.
29. Vadiraja HS, Raghavendra RM, Nagarathna R, et al. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Integr Cancer Ther. 2009;8(1):37-46.
30. Esch T, Stefano GB, Fricchione GL, Benson H. The role of stress in neurodegenerative diseases and mental disorders. Neuro Endocrinol Lett. 2002;23(3):199-208.
31. Lingjaerde O, Ahlfors UG, Bech P, Dencker SJ, Elgen K. The UKU side effect rating scale. A new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatr Scand Suppl. 1987;334:1-100.
32. Schwartz TL, Nihalani N, Jindal S, Virk S, Jones N. Psychiatric medication-induced obesity: a review. Obes Rev. 2004;5(2):115-121.
33. Wirshing DA, Spellberg BJ, Erhart SM, Marder SR, Wirshing WC. Novel antipsychotics and new onset diabetes. Biol Psychiatry. 1998;44(8):778-783.
34. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396.
35. Quiroga Murcia C, Kreutz G, Clift S, Bongard S. Shall we dance? An exploration of the perceived benefits of dancing on well-being. Arts Health. 2010;2(2):149-163.
36. The Duke Center for Integrative Medicine; Liebowitz R, Smith L. The Duke Encyclopedia of New Medicine: Conventional and Alternative Medicine for All Ages. London, UK: Rodale Books International; 2006.
37. Walsh R. Lifestyle and mental health. Am Psychol. 2011;66(7):579-592.
38. Frattaroli J, Weidner G, Dnistrian AM, et al. Clinical events in prostate cancer lifestyle trial: results from two years of follow-up. Urology. 2008;72(6):1319-1323.
39. Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med. 2008;5(1):e12.
40. Sidhu KS, Vandana P, Balon R. Exercise prescription: a practical, effective therapy for depression. Curr Psychiatr. 2009;8(6):38-51.
There is growing interest in developing a holistic and integrative approach for the treatment of severe mental illnesses (SMI), such as schizophrenia, major depression, posttraumatic stress disorder (PTSD), and anxiety disorders. Western medicine has traditionally focused on the direct treatment of symptoms and separated the management of physical and mental health, but increasing attention is being given to complementary and alternative medicine (CAM) for patients with SMI.
Recognizing the connectedness of the mind and body, these complementary or alternative approaches incorporate nontraditional therapeutic techniques with mainstream treatment methods, including psychopharmacology and psychotherapy.1 Patients with SMI may particularly benefit from a mind-body therapeutic approach, because they often experience psychological symptoms such as stress, anxiety, depression and psychosis, as well as a preponderance of medical comorbidities, including obesity, diabetes mellitus, and cardiovascular disease, some of which are compounded by adverse effects (AEs) of essential pharmacologic treatments.2-4 Mind-body interventions might also be particularly advantageous for veterans, who often experience a range of interconnected physical and psychological difficulties due to trauma exposure and challenges transitioning from military to civilian life.5
Related: Complementary and Alternative Medicine for Chronic Musculoskeletal Pain
In 2002, the White House Commission on Complementary and Alternative Medicine Policy issued a report supporting CAM research and integration into existing medical systems.6 The DoD later established Total Force Fitness, a holistic health care program for active-duty military personnel.7 The VA has also incorporated mind-body and holistic strategies into veteran care.8 One such mind-body intervention, yoga, is becoming increasingly popular within the health care field.
Recent research has documented the effectiveness of yoga, underscoring its utility as a mind-body therapeutic approach. Yoga is associated with improvement in balance and flexibility,9 fatigue,10 blood pressure,11 sleep,12 strength,13 and pain14 in both healthy individuals and patients with medical and psychiatric disorders.15 The literature also illustrates that yoga has led to significant improvements in stress and psychiatric symptoms in individuals with PTSD, schizophrenia, depression, and anxiety.16-22 A previous meta-analysis conducted by the authors, which considered studies of the effectiveness of yoga as an adjunctive treatment for patients with mental illness, found that 212 studies with null results would need to be located and incorporated to negate the positive effects of yoga found in the literature.17
Because yoga emphasizes the practice of mindfulness and timing movement with breath awareness, it is a calming practice that may decrease stress and relieve psychiatric symptoms not treated through psychopharmacology and psychotherapy.17,21 Recent research has postulated that the physiological mechanisms by which this occurs may include (a) reduction in sympathetic and increase in parasympathetic activity23,24; (b) increases in heart-rate variability and respiratory sinus arrhythmia, low levels of which are associated with anxiety, panic disorder, and depression23,24; (c) increases in melatonin and serotonin 25-27; and (d) decrease in cortisol.28,29
Related: Enhancing Patient Satisfaction Through the Use of Complementary Therapies
As yoga may calm the autonomic nervous system and reduce stress, it may benefit patients with SMI, whose symptoms are often aggravated by stress.30 In addition, veterans experience both acute stressors and high levels of chronic stress.5 Therefore, because they experience mind-body comorbid illnesses as well as high levels of stress, the authors believe that veterans with SMI could benefit greatly from a tailored yoga-based program as part of a holistic approach that includes necessary medication and evidence-based therapies.
In order to evaluate the effects of a yoga program on veterans receiving mental health treatment across the VA Greater Los Angeles Healthcare System (VAGLAHS), the authors developed a set of yoga-based wellness classes called Breathing, Stretching, Relaxation (BSR) classes. This article describes the process of developing these classes and outlines the procedures and results of a study to assess their effects.
BSR Classes
The development of BSR classes took place at the West Los Angeles VA Medical Center (WLAVAMC), within the Psychosocial Rehabilitation and Recovery Center (PRRC) program. The PRRC is a psychoeducational program that focuses on the biological, psychological, social, and spiritual aspects of life in order to help veterans with SMI rehabilitate and reintegrate into the community. The program allows veterans to create their own recovery curriculum by selecting from diverse classes led by program staff members, including physicians, psychologists, nurses, social workers, nutritionists, and recreational therapists.
Development of BSR Protocols
The primary goal of this project was to develop a yoga-based program tailored to the specific needs of veterans with SMI. To the authors’ knowledge, BSR is the first yoga-based program customized for SMI. The BSR classes were developed within interdisciplinary focus groups that included professional yoga teachers, the director of the PRRC, psychiatrists, psychologists, nurses, occupational therapists, and physical therapists. Drawing on their experience with SMI and yoga, members of the focus groups identified 3 aspects of yoga that would be most beneficial to veterans with SMI, and the program was designed to optimize these effects. Because SMI can both create and be exacerbated by stress, BSR classes were designed to reduce stress and provide veterans with the tools to monitor and manage their stress.
Breathing and meditative techniques were adapted from yoga in order to facilitate stress reduction. In addition, aerobic elements of yoga have the potential to help veterans manage their incidence of medical diseases, such as cardiovascular disease, obesity, and diabetes. Patients with SMI are at a greater risk for developing these diseases, so classes were designed to incorporate physical stretching elements to promote overall health.4,31-33 Finally BSR was designed to improve veteran self- efficacy and self-esteem, and to place veterans at the center of their care by equipping them with skills to practice BSR independently.
Related: Mindfulness to Reduce Stress
The focus groups also identified the logistic requirements when implementing a yoga-based program for veterans with SMI, including (a) obtaining participant or conservator consent; (b) obtaining medical clearance from care providers, given the high prevalence of medical comorbidities; (c) removing the traditional yoga terms, taking a secular approach, and naming the class “Breathing, Stretching, Relaxation” without directly referencing yoga; (d) asking veterans’ permission before incorporating physical contact into demonstrations, because veterans with SMI, especially those with PTSD, might be uncomfortable with touching from instructors; (e) creating protocols of varying duration and intensity so that BSR was approachable for veterans with diverse levels of physical ability; and (f) ensuring that a clinician who regularly works with SMI patients be present to supervise classes for the safety of patients and instructors.
Yoga instructors and clinicians collaborated to create adaptable 30- and 50-minute protocols that reflected best practices for an SMI population. The 30-minute seated BSR class protocol is included in eAppendix A. Once protocols were finalized, a Train the Trainer program was established to facilitate dissemination of BSR to clinicians working with veterans with SMI throughout the VAGLAHS.
Interested clinicians were given protocols and trained to lead BSR classes on their own. Subsequently, clinician-led BSR classes of various lengths (depending on clinician preference and program scheduling) were established at PRRCs and other mental health programs, such as Mental Health Recovery and Intensive Treatment and Dual Diagnosis Treatment Program, throughout the VAGLAHS. These programs were selected, because they are centered on recovery and improvements in symptoms of SMI. The adoption of a Train the Trainer model, through which VA clinicians were trained by professional yoga instructors, allowed for seamless integration of BSR into VA usual care for veterans with SMI.
Assessment of Classes
The authors conducted a study to assess the quality and effectiveness of BSR classes. This survey research was approved by the VAGLAHS institutional review board for human subjects. The authors hypothesized that there would be significant improvements in veterans’ stress, pain, well-being, and perception of the benefits of BSR over 8 weeks of participation in classes. Also hypothesized was that there would be greater benefits in veterans who participated in longer classes and who attended classes more frequently.
Methods
A total of 120 veterans completed surveys after participating in clinician- and yoga instructor-led BSR classes at the 3 sites within the VAGLAHS: WLAVAMC, Los Angeles Ambulatory Care Center (LAACC), and Sepulveda Ambulatory Care Center (SACC). At the WLAVAMC, surveys were collected at 10-, 30-, 60-, and 90-minute classes. At LAACC, surveys were collected at 30- and 60-minute classes. At SACC, surveys were collected at 20- and 45-minute classes. A researcher noted the duration of the class and was available to assist with comprehension. Veterans completed identical surveys after classes at a designated week 0 (baseline), week 4, and week 8. Of the 120 patients with an initial survey, 82 completed at least 1 follow-up survey and 49 completed both follow-up surveys.
Survey packets included (a) demographic questions, including age, gender, and ethnicity; (b) class participation questions, including frequency of class attendance, patients’ favorite aspect of class, and dura tion of class attendance (in months of prior participation); (c) a pain rating from 0 (no pain) to 10 (the worst pain imaginable); (d) the BioPsychoSocial-Spiritual (BPSS) Scale (eAppendix B), developed at the WLAVAMC, which provides wellness scores from 0 (low) to 10 (high) in 4 areas as well as a holistic wellness score from 0 (low) to 40 (high); (e) the Perceived Stress Scale (PSS), developed by Cohen and colleagues, which generates a stress score for the past month from 0 (low) to 40 (high)34; and (f) the Perceived Benefits of Yoga Questionnaire (PBYQ) (eAppendix C), which rates participants’ opinions about the benefits of yoga from 12 (low) to 60 (high) and is based on the Perceived Benefits of Dance Questionnaire.35
Statistical Analysis
Pearson’s r correlation coefficients were calculated between PBYQ scores and quantitative survey items at each time point (weeks 0, 4, and 8). Linear mixed-effects models were used to test for effects of multiple predictor variables on individual outcomes. Each model had a random intercept by participant, and regressors included main effects for the following: survey week (0, 4, or 8), class duration (in minutes), age, sex, ethnicity, frequency of attendance (in days per week), and duration of attendance (in months). For all statistical analyses, a 2-tailed significance criterion of α = .05 was used.
Results
Veterans who completed surveys were predominantly male (90.8%) and averaged 61.4 years of age. Table 1 shows demographic information. Table 2 displays the number of participants who were involved in short (< 30 min), medium (30-59 min), and long (> 60 min) classes. Veteran participants also had a wide range of prior BSR experience (Table 3).
At all time points, PBYQ scores were significantly positively correlated with class duration and biological, psychological, social, spiritual, and total well-being as measured by the BPSS. The PBYQ scores at all time points were also significantly negatively correlated with age, pain ratings, and PSS scores. Table 4 includes specific Pearson’s r values.
Survey week was not significantly associated with any individual outcome measures. There were no significant regressors for total PSS score or total BPSS score within the linear models. However, participants’ PBYQ scores were significantly associated with age (t(98) = -2.13, P = .036), frequency of attendance (t(103) = 2.10, P = .038), and class duration (t(98) = 4.35, P < .001). Additionally, class duration was significantly associated with pain (t(98) = -3.01, P = .003), with longer duration associated with less pain. Ethnicity was also associated with pain, with African American veterans reporting less pain than did white (t(98) = -2.41, P = .017) and Hispanic (t(98) = -2.31, P = .023) veterans. Because ethnicity was significantly associated with class duration (F(5,339) = 3.81, P = .002), the authors used an analysis of covariance to test for a mediating effect of ethnicity on the relationship between class duration and pain. Although there was a partial mediation (F(5,203) = 2.57, P = .028), the main effect of class duration remained significant.
Discussion and Limitations
The goals of this project were to develop a yoga-based program tailored for veterans with SMI and assess the program in a sample of veterans with SMI on subjective reports of stress, pain, well-being, and benefits of yoga. The authors hypothesized that significant improvements in these measures in veterans with SMI would be observed over 8 weeks of participation in BSR classes and that there would be greater benefits in veterans who participated in longer classes and who attended classes more frequently.
The authors succeeded in developing an adaptable yoga-based wellness program for veterans with SMI that can be both practiced in structured classes and incorporated into veterans’ everyday routines. The BSR classes were well tolerated by veterans with SMI, caused no discernible AEs, and are readily available for dissemination across other mental health programs. Veterans described integrating the tools they learned within BSR classes into their daily lives, helping them to manage pain; feel more flexible; reduce stress, anxiety, depression, and PTSD symptoms; and increase relaxation and feelings of self-control and confidence. Table 5 shows qualitative feedback collected from veterans. In addition, the Train the Trainer model optimized clinical applicability and flexibility, demonstrating that clinicians can seamlessly integrate BSR classes into a health care plan for veterans with SMI.
In assessing quantitative measures of stress, pain, well-being, and perceived benefits of a yoga-based program, veterans who reported BSR classes as beneficial experienced lower levels of pain and stress and higher levels of biological, psychological, social, spiritual, and overall well-being. Those veterans who perceived BSR as more beneficial tended to be younger and attend longer classes with greater frequency. Veterans who attended longer classes also reported experiencing less pain. This may be because the more rigorous stretching and posing involved in longer BSR classes made them more effective at reducing pain; however, it is also possible that veterans who were experiencing more pain avoided these longer classes due to their rigor and length.
Results suggest that longer classes attended with greater regularity may be more beneficial to veterans than short and infrequent classes, particularly in regards to their pain. Despite the relationships between class and outcome variables, the authors did not find significant improvements in measures of wellness, pain, stress, or perceived benefits of BSR over time, as was hypothesized. This may be because the data collection for this study began after classes had been established for some time. In fact, only 35 of 120 veterans included in this study reported having < 1 month of BSR experience at week 0, suggesting that results collected from week 0 did not represent a true baseline measurement. Although no relationship was found between prior duration of attendance and any outcome measures, the fact that most veterans in the sample had attended classes for several months prior to completing surveys may have biased the results by favoring the responses of veterans who were more invested in the classes. Improvements may have been better captured in a BSR-naïve sample.
The finding that the PBYQ score was significantly correlated with all other outcome measures (pain, BPSS score, and PSS score) raises some questions about the ways in which these classes were beneficial to veterans. It may be that veterans who experienced more positive outcomes from classes saw BSR as more beneficial, but it is also possible that veterans who entered classes with greater expectations experienced better outcomes due to a placebo effect—that is, outcomes may have been influenced more by the expectation than by the content of the classes. In the case of well-being (BPSS scores) and stress (PSS score), this could explain why these outcomes were significantly correlated with perceived benefits of BSR but were not significantly related to any class-related variables such as duration and frequency of attendance. Pain ratings, however, were related to class variables and perceived benefits of BSR.
In a post hoc analysis, the main effect of the PBYQ score as a regressor was added to the linear model for pain, resulting in the PBYQ score having a significant main effect (t(100) = -2.98, P = .004). The main effect of class duration remained significant (t(97) = -1.99, P = .050) but was less substantial when the PBYQ score was added, suggesting some correlation between class duration and pain, independent of BSR’s perceived benefits. Future research should consider the possible mediating effect of perceptions of the effectiveness of a yoga-based program a priori or control for placebo effects in order to address the degree to which outcomes are influenced by participant expectations.
This study had a few other notable limitations. Because it was an observational study administered within a clinical mental health program, a control group was not included. Measurement began after BSR classes were established, so veterans had varying levels of prior experience. Specific SMI and medical diagnosis information was not collected from individual veterans. Data were collected from classes of varying length and intensity. The BSR classes often took place within larger programs at the VA, which offered comprehensive care, so some effects of the BSR classes might have been confounded with concurrent evidenced-based treatments or other holistic care programs. Due to these limitations, particularly the absence of a control group, the relationships between BSR participation and health outcomes cannot be assumed to be causal, because a multitude of other variables, such as patient contact and expectancy effects, may have influenced outcomes.
Future Directions
Future research should aim to utilize a control group and collect data from classes of the same intensity and length to better examine whether BSR can be causally linked with improvements in measures of stress, pain, and well-being and to attempt to control for expectancy and contact effects. In addition, future research should aim to recruit a BSR-naïve sample to account for prior experience. Future studies should also aim to parse out whether BSR is differentially effective for each SMI or medical diagnosis, whether there is a relationship between class time and outcomes (as these results suggest that longer class times might be more beneficial for pain), and whether any pain-management benefits from BSR influence other measures of functionality and well-being. Finally, future research can further divide BSR into its active components, such as meditative breathing and aerobic stretching, in order to examine which aspect leads to the greatest effect on each measure; the current results imply that the more rigorous components of BSR classes have the greatest effects on pain.
Conclusion
A yoga-based class affects the mind and body, making it particularly useful for veterans with SMI who experience a range of physical and psychological symptoms and comorbidities.4 Other studies have demonstrated that when practiced alone, yoga leads to improvements in both physical and psychological symptoms.15,17 Looking forward, yoga-based classes may be implemented as part of a larger biopsychosocial-spiritual care plan that is being embraced both within and outside of the VA.7,8,36,37 This integrative health care model suggests that psychosocial and CAM modalities are additive and should be practiced concurrently.37
Although little research has assessed the effects of comprehensive psychosocial and CAM treatment programs, initial research indicates that these programs are associated with reductions in symptoms of medical and mental illness.37-40 Participants in BSR classes may derive further benefits if classes are incorporated into a larger holistic health care plan that includes both traditional psychiatric treatment modalities and CAM therapies that integrate biopsychosocial-spiritual components.
Acknowledgements
The authors would like to thank Nancy Mohler, Anne Platt, and Matthew Crowder, all professional yoga instructors, for their integral role in developing classes, providing classes to veterans, and assisting VA staff with training. The authors also acknowledge Rosie Dominguez, LCSW, for expertly leading BSR classes at LAACC. The authors also thank Irina Arnold, MS, MD, and Vanessa Streiff, MA, for their vital assistance with data collection at SACC.
Funding for the development of BSR protocols, quality improvement research, and expenses associated with classes was provided by the Disabled American Veterans Charitable Service Trust. Support for dissemination of classes to multiple VA programs was provided by a grant from the VA Center of Innovation for Patient Centered Care, headed by Sandra Robertson, RN, MSN, PH-CNS.
The authors are very grateful to the veterans and staff of the Mental Health Intensive Case Management, Psychosocial Rehabilitation and Recovery Centers, Mental Health Clinics, and Domiciliary throughout Greater Los Angeles for their support of the BSR classes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
There is growing interest in developing a holistic and integrative approach for the treatment of severe mental illnesses (SMI), such as schizophrenia, major depression, posttraumatic stress disorder (PTSD), and anxiety disorders. Western medicine has traditionally focused on the direct treatment of symptoms and separated the management of physical and mental health, but increasing attention is being given to complementary and alternative medicine (CAM) for patients with SMI.
Recognizing the connectedness of the mind and body, these complementary or alternative approaches incorporate nontraditional therapeutic techniques with mainstream treatment methods, including psychopharmacology and psychotherapy.1 Patients with SMI may particularly benefit from a mind-body therapeutic approach, because they often experience psychological symptoms such as stress, anxiety, depression and psychosis, as well as a preponderance of medical comorbidities, including obesity, diabetes mellitus, and cardiovascular disease, some of which are compounded by adverse effects (AEs) of essential pharmacologic treatments.2-4 Mind-body interventions might also be particularly advantageous for veterans, who often experience a range of interconnected physical and psychological difficulties due to trauma exposure and challenges transitioning from military to civilian life.5
Related: Complementary and Alternative Medicine for Chronic Musculoskeletal Pain
In 2002, the White House Commission on Complementary and Alternative Medicine Policy issued a report supporting CAM research and integration into existing medical systems.6 The DoD later established Total Force Fitness, a holistic health care program for active-duty military personnel.7 The VA has also incorporated mind-body and holistic strategies into veteran care.8 One such mind-body intervention, yoga, is becoming increasingly popular within the health care field.
Recent research has documented the effectiveness of yoga, underscoring its utility as a mind-body therapeutic approach. Yoga is associated with improvement in balance and flexibility,9 fatigue,10 blood pressure,11 sleep,12 strength,13 and pain14 in both healthy individuals and patients with medical and psychiatric disorders.15 The literature also illustrates that yoga has led to significant improvements in stress and psychiatric symptoms in individuals with PTSD, schizophrenia, depression, and anxiety.16-22 A previous meta-analysis conducted by the authors, which considered studies of the effectiveness of yoga as an adjunctive treatment for patients with mental illness, found that 212 studies with null results would need to be located and incorporated to negate the positive effects of yoga found in the literature.17
Because yoga emphasizes the practice of mindfulness and timing movement with breath awareness, it is a calming practice that may decrease stress and relieve psychiatric symptoms not treated through psychopharmacology and psychotherapy.17,21 Recent research has postulated that the physiological mechanisms by which this occurs may include (a) reduction in sympathetic and increase in parasympathetic activity23,24; (b) increases in heart-rate variability and respiratory sinus arrhythmia, low levels of which are associated with anxiety, panic disorder, and depression23,24; (c) increases in melatonin and serotonin 25-27; and (d) decrease in cortisol.28,29
Related: Enhancing Patient Satisfaction Through the Use of Complementary Therapies
As yoga may calm the autonomic nervous system and reduce stress, it may benefit patients with SMI, whose symptoms are often aggravated by stress.30 In addition, veterans experience both acute stressors and high levels of chronic stress.5 Therefore, because they experience mind-body comorbid illnesses as well as high levels of stress, the authors believe that veterans with SMI could benefit greatly from a tailored yoga-based program as part of a holistic approach that includes necessary medication and evidence-based therapies.
In order to evaluate the effects of a yoga program on veterans receiving mental health treatment across the VA Greater Los Angeles Healthcare System (VAGLAHS), the authors developed a set of yoga-based wellness classes called Breathing, Stretching, Relaxation (BSR) classes. This article describes the process of developing these classes and outlines the procedures and results of a study to assess their effects.
BSR Classes
The development of BSR classes took place at the West Los Angeles VA Medical Center (WLAVAMC), within the Psychosocial Rehabilitation and Recovery Center (PRRC) program. The PRRC is a psychoeducational program that focuses on the biological, psychological, social, and spiritual aspects of life in order to help veterans with SMI rehabilitate and reintegrate into the community. The program allows veterans to create their own recovery curriculum by selecting from diverse classes led by program staff members, including physicians, psychologists, nurses, social workers, nutritionists, and recreational therapists.
Development of BSR Protocols
The primary goal of this project was to develop a yoga-based program tailored to the specific needs of veterans with SMI. To the authors’ knowledge, BSR is the first yoga-based program customized for SMI. The BSR classes were developed within interdisciplinary focus groups that included professional yoga teachers, the director of the PRRC, psychiatrists, psychologists, nurses, occupational therapists, and physical therapists. Drawing on their experience with SMI and yoga, members of the focus groups identified 3 aspects of yoga that would be most beneficial to veterans with SMI, and the program was designed to optimize these effects. Because SMI can both create and be exacerbated by stress, BSR classes were designed to reduce stress and provide veterans with the tools to monitor and manage their stress.
Breathing and meditative techniques were adapted from yoga in order to facilitate stress reduction. In addition, aerobic elements of yoga have the potential to help veterans manage their incidence of medical diseases, such as cardiovascular disease, obesity, and diabetes. Patients with SMI are at a greater risk for developing these diseases, so classes were designed to incorporate physical stretching elements to promote overall health.4,31-33 Finally BSR was designed to improve veteran self- efficacy and self-esteem, and to place veterans at the center of their care by equipping them with skills to practice BSR independently.
Related: Mindfulness to Reduce Stress
The focus groups also identified the logistic requirements when implementing a yoga-based program for veterans with SMI, including (a) obtaining participant or conservator consent; (b) obtaining medical clearance from care providers, given the high prevalence of medical comorbidities; (c) removing the traditional yoga terms, taking a secular approach, and naming the class “Breathing, Stretching, Relaxation” without directly referencing yoga; (d) asking veterans’ permission before incorporating physical contact into demonstrations, because veterans with SMI, especially those with PTSD, might be uncomfortable with touching from instructors; (e) creating protocols of varying duration and intensity so that BSR was approachable for veterans with diverse levels of physical ability; and (f) ensuring that a clinician who regularly works with SMI patients be present to supervise classes for the safety of patients and instructors.
Yoga instructors and clinicians collaborated to create adaptable 30- and 50-minute protocols that reflected best practices for an SMI population. The 30-minute seated BSR class protocol is included in eAppendix A. Once protocols were finalized, a Train the Trainer program was established to facilitate dissemination of BSR to clinicians working with veterans with SMI throughout the VAGLAHS.
Interested clinicians were given protocols and trained to lead BSR classes on their own. Subsequently, clinician-led BSR classes of various lengths (depending on clinician preference and program scheduling) were established at PRRCs and other mental health programs, such as Mental Health Recovery and Intensive Treatment and Dual Diagnosis Treatment Program, throughout the VAGLAHS. These programs were selected, because they are centered on recovery and improvements in symptoms of SMI. The adoption of a Train the Trainer model, through which VA clinicians were trained by professional yoga instructors, allowed for seamless integration of BSR into VA usual care for veterans with SMI.
Assessment of Classes
The authors conducted a study to assess the quality and effectiveness of BSR classes. This survey research was approved by the VAGLAHS institutional review board for human subjects. The authors hypothesized that there would be significant improvements in veterans’ stress, pain, well-being, and perception of the benefits of BSR over 8 weeks of participation in classes. Also hypothesized was that there would be greater benefits in veterans who participated in longer classes and who attended classes more frequently.
Methods
A total of 120 veterans completed surveys after participating in clinician- and yoga instructor-led BSR classes at the 3 sites within the VAGLAHS: WLAVAMC, Los Angeles Ambulatory Care Center (LAACC), and Sepulveda Ambulatory Care Center (SACC). At the WLAVAMC, surveys were collected at 10-, 30-, 60-, and 90-minute classes. At LAACC, surveys were collected at 30- and 60-minute classes. At SACC, surveys were collected at 20- and 45-minute classes. A researcher noted the duration of the class and was available to assist with comprehension. Veterans completed identical surveys after classes at a designated week 0 (baseline), week 4, and week 8. Of the 120 patients with an initial survey, 82 completed at least 1 follow-up survey and 49 completed both follow-up surveys.
Survey packets included (a) demographic questions, including age, gender, and ethnicity; (b) class participation questions, including frequency of class attendance, patients’ favorite aspect of class, and dura tion of class attendance (in months of prior participation); (c) a pain rating from 0 (no pain) to 10 (the worst pain imaginable); (d) the BioPsychoSocial-Spiritual (BPSS) Scale (eAppendix B), developed at the WLAVAMC, which provides wellness scores from 0 (low) to 10 (high) in 4 areas as well as a holistic wellness score from 0 (low) to 40 (high); (e) the Perceived Stress Scale (PSS), developed by Cohen and colleagues, which generates a stress score for the past month from 0 (low) to 40 (high)34; and (f) the Perceived Benefits of Yoga Questionnaire (PBYQ) (eAppendix C), which rates participants’ opinions about the benefits of yoga from 12 (low) to 60 (high) and is based on the Perceived Benefits of Dance Questionnaire.35
Statistical Analysis
Pearson’s r correlation coefficients were calculated between PBYQ scores and quantitative survey items at each time point (weeks 0, 4, and 8). Linear mixed-effects models were used to test for effects of multiple predictor variables on individual outcomes. Each model had a random intercept by participant, and regressors included main effects for the following: survey week (0, 4, or 8), class duration (in minutes), age, sex, ethnicity, frequency of attendance (in days per week), and duration of attendance (in months). For all statistical analyses, a 2-tailed significance criterion of α = .05 was used.
Results
Veterans who completed surveys were predominantly male (90.8%) and averaged 61.4 years of age. Table 1 shows demographic information. Table 2 displays the number of participants who were involved in short (< 30 min), medium (30-59 min), and long (> 60 min) classes. Veteran participants also had a wide range of prior BSR experience (Table 3).
At all time points, PBYQ scores were significantly positively correlated with class duration and biological, psychological, social, spiritual, and total well-being as measured by the BPSS. The PBYQ scores at all time points were also significantly negatively correlated with age, pain ratings, and PSS scores. Table 4 includes specific Pearson’s r values.
Survey week was not significantly associated with any individual outcome measures. There were no significant regressors for total PSS score or total BPSS score within the linear models. However, participants’ PBYQ scores were significantly associated with age (t(98) = -2.13, P = .036), frequency of attendance (t(103) = 2.10, P = .038), and class duration (t(98) = 4.35, P < .001). Additionally, class duration was significantly associated with pain (t(98) = -3.01, P = .003), with longer duration associated with less pain. Ethnicity was also associated with pain, with African American veterans reporting less pain than did white (t(98) = -2.41, P = .017) and Hispanic (t(98) = -2.31, P = .023) veterans. Because ethnicity was significantly associated with class duration (F(5,339) = 3.81, P = .002), the authors used an analysis of covariance to test for a mediating effect of ethnicity on the relationship between class duration and pain. Although there was a partial mediation (F(5,203) = 2.57, P = .028), the main effect of class duration remained significant.
Discussion and Limitations
The goals of this project were to develop a yoga-based program tailored for veterans with SMI and assess the program in a sample of veterans with SMI on subjective reports of stress, pain, well-being, and benefits of yoga. The authors hypothesized that significant improvements in these measures in veterans with SMI would be observed over 8 weeks of participation in BSR classes and that there would be greater benefits in veterans who participated in longer classes and who attended classes more frequently.
The authors succeeded in developing an adaptable yoga-based wellness program for veterans with SMI that can be both practiced in structured classes and incorporated into veterans’ everyday routines. The BSR classes were well tolerated by veterans with SMI, caused no discernible AEs, and are readily available for dissemination across other mental health programs. Veterans described integrating the tools they learned within BSR classes into their daily lives, helping them to manage pain; feel more flexible; reduce stress, anxiety, depression, and PTSD symptoms; and increase relaxation and feelings of self-control and confidence. Table 5 shows qualitative feedback collected from veterans. In addition, the Train the Trainer model optimized clinical applicability and flexibility, demonstrating that clinicians can seamlessly integrate BSR classes into a health care plan for veterans with SMI.
In assessing quantitative measures of stress, pain, well-being, and perceived benefits of a yoga-based program, veterans who reported BSR classes as beneficial experienced lower levels of pain and stress and higher levels of biological, psychological, social, spiritual, and overall well-being. Those veterans who perceived BSR as more beneficial tended to be younger and attend longer classes with greater frequency. Veterans who attended longer classes also reported experiencing less pain. This may be because the more rigorous stretching and posing involved in longer BSR classes made them more effective at reducing pain; however, it is also possible that veterans who were experiencing more pain avoided these longer classes due to their rigor and length.
Results suggest that longer classes attended with greater regularity may be more beneficial to veterans than short and infrequent classes, particularly in regards to their pain. Despite the relationships between class and outcome variables, the authors did not find significant improvements in measures of wellness, pain, stress, or perceived benefits of BSR over time, as was hypothesized. This may be because the data collection for this study began after classes had been established for some time. In fact, only 35 of 120 veterans included in this study reported having < 1 month of BSR experience at week 0, suggesting that results collected from week 0 did not represent a true baseline measurement. Although no relationship was found between prior duration of attendance and any outcome measures, the fact that most veterans in the sample had attended classes for several months prior to completing surveys may have biased the results by favoring the responses of veterans who were more invested in the classes. Improvements may have been better captured in a BSR-naïve sample.
The finding that the PBYQ score was significantly correlated with all other outcome measures (pain, BPSS score, and PSS score) raises some questions about the ways in which these classes were beneficial to veterans. It may be that veterans who experienced more positive outcomes from classes saw BSR as more beneficial, but it is also possible that veterans who entered classes with greater expectations experienced better outcomes due to a placebo effect—that is, outcomes may have been influenced more by the expectation than by the content of the classes. In the case of well-being (BPSS scores) and stress (PSS score), this could explain why these outcomes were significantly correlated with perceived benefits of BSR but were not significantly related to any class-related variables such as duration and frequency of attendance. Pain ratings, however, were related to class variables and perceived benefits of BSR.
In a post hoc analysis, the main effect of the PBYQ score as a regressor was added to the linear model for pain, resulting in the PBYQ score having a significant main effect (t(100) = -2.98, P = .004). The main effect of class duration remained significant (t(97) = -1.99, P = .050) but was less substantial when the PBYQ score was added, suggesting some correlation between class duration and pain, independent of BSR’s perceived benefits. Future research should consider the possible mediating effect of perceptions of the effectiveness of a yoga-based program a priori or control for placebo effects in order to address the degree to which outcomes are influenced by participant expectations.
This study had a few other notable limitations. Because it was an observational study administered within a clinical mental health program, a control group was not included. Measurement began after BSR classes were established, so veterans had varying levels of prior experience. Specific SMI and medical diagnosis information was not collected from individual veterans. Data were collected from classes of varying length and intensity. The BSR classes often took place within larger programs at the VA, which offered comprehensive care, so some effects of the BSR classes might have been confounded with concurrent evidenced-based treatments or other holistic care programs. Due to these limitations, particularly the absence of a control group, the relationships between BSR participation and health outcomes cannot be assumed to be causal, because a multitude of other variables, such as patient contact and expectancy effects, may have influenced outcomes.
Future Directions
Future research should aim to utilize a control group and collect data from classes of the same intensity and length to better examine whether BSR can be causally linked with improvements in measures of stress, pain, and well-being and to attempt to control for expectancy and contact effects. In addition, future research should aim to recruit a BSR-naïve sample to account for prior experience. Future studies should also aim to parse out whether BSR is differentially effective for each SMI or medical diagnosis, whether there is a relationship between class time and outcomes (as these results suggest that longer class times might be more beneficial for pain), and whether any pain-management benefits from BSR influence other measures of functionality and well-being. Finally, future research can further divide BSR into its active components, such as meditative breathing and aerobic stretching, in order to examine which aspect leads to the greatest effect on each measure; the current results imply that the more rigorous components of BSR classes have the greatest effects on pain.
Conclusion
A yoga-based class affects the mind and body, making it particularly useful for veterans with SMI who experience a range of physical and psychological symptoms and comorbidities.4 Other studies have demonstrated that when practiced alone, yoga leads to improvements in both physical and psychological symptoms.15,17 Looking forward, yoga-based classes may be implemented as part of a larger biopsychosocial-spiritual care plan that is being embraced both within and outside of the VA.7,8,36,37 This integrative health care model suggests that psychosocial and CAM modalities are additive and should be practiced concurrently.37
Although little research has assessed the effects of comprehensive psychosocial and CAM treatment programs, initial research indicates that these programs are associated with reductions in symptoms of medical and mental illness.37-40 Participants in BSR classes may derive further benefits if classes are incorporated into a larger holistic health care plan that includes both traditional psychiatric treatment modalities and CAM therapies that integrate biopsychosocial-spiritual components.
Acknowledgements
The authors would like to thank Nancy Mohler, Anne Platt, and Matthew Crowder, all professional yoga instructors, for their integral role in developing classes, providing classes to veterans, and assisting VA staff with training. The authors also acknowledge Rosie Dominguez, LCSW, for expertly leading BSR classes at LAACC. The authors also thank Irina Arnold, MS, MD, and Vanessa Streiff, MA, for their vital assistance with data collection at SACC.
Funding for the development of BSR protocols, quality improvement research, and expenses associated with classes was provided by the Disabled American Veterans Charitable Service Trust. Support for dissemination of classes to multiple VA programs was provided by a grant from the VA Center of Innovation for Patient Centered Care, headed by Sandra Robertson, RN, MSN, PH-CNS.
The authors are very grateful to the veterans and staff of the Mental Health Intensive Case Management, Psychosocial Rehabilitation and Recovery Centers, Mental Health Clinics, and Domiciliary throughout Greater Los Angeles for their support of the BSR classes.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. National Center for Complementary and Integrative Health. Complementary, alternative, or integrative health: what's in a name? U.S. Department of Health and Human Services, National Institutes of Health Website. http://nccam.nih.gov/health/whatiscam. Updated March 2015. Accessed August 27, 2015.
2. Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Fleischhacker WW, Cetkovich-Bakmas M, De Hert M, et al. Comorbid somatic illnesses in patients with severe mental disorders: clinical, policy, and research challenges. J Clin Psychiatry. 2008;69(4):514-519.
4. Wirshing DA, Boyd JA, Meng LR, Ballon JS, Marder SR, Wirshing WC. The effects of novel antipsychotics on glucose and lipid levels. J Clin Psychiatry. 2002;63(10):856-865.
5. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008.
6. White House Commission on Complementary and Alternative Medicine Policy. Final Report. Washington, DC: White House Commission on Complementary and Alternative Medicine Policy; 2002.
7. Land BC. Current Department of Defense guidance for total force fitness. Mil Med. 2010;175(suppl 8):3-5.
8. U.S. Department of Veterans Affairs, Veterans Health Administration. Pain Management. VHA Directive 2009-053. Washington, DC: U.S. Department of Veterans Affairs, Veterans Health Administration; 2009.
9. Oken BS, Zajdel D, Kishiyama S, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med. 2006;12(1):40-47.
10. Bower JE, Garet D, Sternlieb B, et al. Yoga for persistent fatigue in breast cancer survivors: a randomized controlled trial. Cancer. 2012;118(15):3766-3775.
11. Cade WT, Reeds DN, Mondy KE, et al. Yoga lifestyle intervention reduces blood pressure in HIV-infected adults with cardiovascular disease risk factors. HIV Med. 2010;11(6):379-388.
12. Innes KE, Selfe TK. The effects of a gentle yoga program on sleep, mood, and blood pressure in older women with restless leg syndrome (RLS): a preliminary randomized controlled trial. Evid Based Complement Alternat Med. 2012;2012:294058.
13. Van Puymbroeck M, Payne LL, Hsieh PC. A phase I feasibility study of yoga on the physical health and coping of informal caregivers. Evid Based Complement Alternat Med. 2007;4(4):519-529.
14. Rani K, Tiwari SC, Singh U, Agrawal GG, Srivastava N. Six-month trial of Yoga Nidra in menstrual disorder patients: effects on somatoform symptoms. Ind Psychiatry J. 2011;20(2):97-102.
15. Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J Altern Complement Med. 2010;16(1):3-12.
16. Banerjee B, Vadiraj HS, Ram A, et al. Effects of an integrated yoga program in modulating psychological stress and radiation-induced genotoxic stress in breast cancer patients undergoing radiotherapy. Integr Cancer Ther. 2007;6(3):242-250.
17. Cabral P, Meyer HB, Ames D. Effectiveness of yoga therapy as a complementary treatment for major psychiatric disorders: a meta-analysis. Prim Care Companion CNS Disord. 2011;13(4):doi:10.4088/PCC.10r01068.
18. Katzman MA, Vermani M, Gerbarg PL, et al. A multicomponent yoga-based, breath intervention program as an adjunctive treatment in patients suffering from generalized anxiety disorder with or without comorbidities. Int J Yoga. 2012;5(1):57-65.
19. Köhn M, Persson Lundholm U, Bryngelsson IL, Anderzén-Carlsson A, Westerdahl E. Medical yoga for patients with stress-related symptoms and diagnoses in primary health care: a randomized controlled trial. Evid Based Complement Alternat Med. 2013;2013:215348.
20. Krishnamurthy MN, Telles S. Assessing depression following two ancient Indian interventions: effects of yoga and ayurveda on older adults in a residential home. J Gerontol Nurs. 2007;33(2):17-23.
21. Meyer HB, Katsman A, Sones AC, Auerbach DE, Ames D, Rubin RT. Yoga as an ancillary treatment for neurological and psychiatric disorders: a review. J Neuropsychiatry Clin Neurosci. 2012;24(2):152-164.
22. Visceglia E, Lewis S. Yoga therapy as an adjunctive treatment for schizophrenia: a randomized, controlled pilot study. J Altern Complement Med. 2011;17(7):601-607.
23. Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression, part I-neurophysiologic model. J Altern Complement Med. 2005;11(1):189-201.
24. Brown RP, Gerbarg PL. Yoga breathing, meditation, and longevity. Ann N Y Acad Sci. 2009;1172:54-62.
25. Harinath K, Malhotra AS, Pal K, et al. Effects of hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004;10(2):261-268.
26. Tooley GA, Armstrong SM, Norman TR, Sali A. Acute increases in night-time plasma melatonin levels following a period of meditation. Biol Psychol. 2000;53(1):69-78.
27. Walton KG, Pugh ND, Gelderloos P, Macrae P. Stress reduction and preventing hypertension: preliminary support of a psychoneuroendocrine mechanism. J Altern Complement Med. 1995;1(3):263-283.
28. Banasik J, Williams H, Haberman M, Blank SE, Bendel R. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23(3):135-142.
29. Vadiraja HS, Raghavendra RM, Nagarathna R, et al. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Integr Cancer Ther. 2009;8(1):37-46.
30. Esch T, Stefano GB, Fricchione GL, Benson H. The role of stress in neurodegenerative diseases and mental disorders. Neuro Endocrinol Lett. 2002;23(3):199-208.
31. Lingjaerde O, Ahlfors UG, Bech P, Dencker SJ, Elgen K. The UKU side effect rating scale. A new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatr Scand Suppl. 1987;334:1-100.
32. Schwartz TL, Nihalani N, Jindal S, Virk S, Jones N. Psychiatric medication-induced obesity: a review. Obes Rev. 2004;5(2):115-121.
33. Wirshing DA, Spellberg BJ, Erhart SM, Marder SR, Wirshing WC. Novel antipsychotics and new onset diabetes. Biol Psychiatry. 1998;44(8):778-783.
34. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396.
35. Quiroga Murcia C, Kreutz G, Clift S, Bongard S. Shall we dance? An exploration of the perceived benefits of dancing on well-being. Arts Health. 2010;2(2):149-163.
36. The Duke Center for Integrative Medicine; Liebowitz R, Smith L. The Duke Encyclopedia of New Medicine: Conventional and Alternative Medicine for All Ages. London, UK: Rodale Books International; 2006.
37. Walsh R. Lifestyle and mental health. Am Psychol. 2011;66(7):579-592.
38. Frattaroli J, Weidner G, Dnistrian AM, et al. Clinical events in prostate cancer lifestyle trial: results from two years of follow-up. Urology. 2008;72(6):1319-1323.
39. Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med. 2008;5(1):e12.
40. Sidhu KS, Vandana P, Balon R. Exercise prescription: a practical, effective therapy for depression. Curr Psychiatr. 2009;8(6):38-51.
1. National Center for Complementary and Integrative Health. Complementary, alternative, or integrative health: what's in a name? U.S. Department of Health and Human Services, National Institutes of Health Website. http://nccam.nih.gov/health/whatiscam. Updated March 2015. Accessed August 27, 2015.
2. Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Fleischhacker WW, Cetkovich-Bakmas M, De Hert M, et al. Comorbid somatic illnesses in patients with severe mental disorders: clinical, policy, and research challenges. J Clin Psychiatry. 2008;69(4):514-519.
4. Wirshing DA, Boyd JA, Meng LR, Ballon JS, Marder SR, Wirshing WC. The effects of novel antipsychotics on glucose and lipid levels. J Clin Psychiatry. 2002;63(10):856-865.
5. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008.
6. White House Commission on Complementary and Alternative Medicine Policy. Final Report. Washington, DC: White House Commission on Complementary and Alternative Medicine Policy; 2002.
7. Land BC. Current Department of Defense guidance for total force fitness. Mil Med. 2010;175(suppl 8):3-5.
8. U.S. Department of Veterans Affairs, Veterans Health Administration. Pain Management. VHA Directive 2009-053. Washington, DC: U.S. Department of Veterans Affairs, Veterans Health Administration; 2009.
9. Oken BS, Zajdel D, Kishiyama S, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med. 2006;12(1):40-47.
10. Bower JE, Garet D, Sternlieb B, et al. Yoga for persistent fatigue in breast cancer survivors: a randomized controlled trial. Cancer. 2012;118(15):3766-3775.
11. Cade WT, Reeds DN, Mondy KE, et al. Yoga lifestyle intervention reduces blood pressure in HIV-infected adults with cardiovascular disease risk factors. HIV Med. 2010;11(6):379-388.
12. Innes KE, Selfe TK. The effects of a gentle yoga program on sleep, mood, and blood pressure in older women with restless leg syndrome (RLS): a preliminary randomized controlled trial. Evid Based Complement Alternat Med. 2012;2012:294058.
13. Van Puymbroeck M, Payne LL, Hsieh PC. A phase I feasibility study of yoga on the physical health and coping of informal caregivers. Evid Based Complement Alternat Med. 2007;4(4):519-529.
14. Rani K, Tiwari SC, Singh U, Agrawal GG, Srivastava N. Six-month trial of Yoga Nidra in menstrual disorder patients: effects on somatoform symptoms. Ind Psychiatry J. 2011;20(2):97-102.
15. Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J Altern Complement Med. 2010;16(1):3-12.
16. Banerjee B, Vadiraj HS, Ram A, et al. Effects of an integrated yoga program in modulating psychological stress and radiation-induced genotoxic stress in breast cancer patients undergoing radiotherapy. Integr Cancer Ther. 2007;6(3):242-250.
17. Cabral P, Meyer HB, Ames D. Effectiveness of yoga therapy as a complementary treatment for major psychiatric disorders: a meta-analysis. Prim Care Companion CNS Disord. 2011;13(4):doi:10.4088/PCC.10r01068.
18. Katzman MA, Vermani M, Gerbarg PL, et al. A multicomponent yoga-based, breath intervention program as an adjunctive treatment in patients suffering from generalized anxiety disorder with or without comorbidities. Int J Yoga. 2012;5(1):57-65.
19. Köhn M, Persson Lundholm U, Bryngelsson IL, Anderzén-Carlsson A, Westerdahl E. Medical yoga for patients with stress-related symptoms and diagnoses in primary health care: a randomized controlled trial. Evid Based Complement Alternat Med. 2013;2013:215348.
20. Krishnamurthy MN, Telles S. Assessing depression following two ancient Indian interventions: effects of yoga and ayurveda on older adults in a residential home. J Gerontol Nurs. 2007;33(2):17-23.
21. Meyer HB, Katsman A, Sones AC, Auerbach DE, Ames D, Rubin RT. Yoga as an ancillary treatment for neurological and psychiatric disorders: a review. J Neuropsychiatry Clin Neurosci. 2012;24(2):152-164.
22. Visceglia E, Lewis S. Yoga therapy as an adjunctive treatment for schizophrenia: a randomized, controlled pilot study. J Altern Complement Med. 2011;17(7):601-607.
23. Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression, part I-neurophysiologic model. J Altern Complement Med. 2005;11(1):189-201.
24. Brown RP, Gerbarg PL. Yoga breathing, meditation, and longevity. Ann N Y Acad Sci. 2009;1172:54-62.
25. Harinath K, Malhotra AS, Pal K, et al. Effects of hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004;10(2):261-268.
26. Tooley GA, Armstrong SM, Norman TR, Sali A. Acute increases in night-time plasma melatonin levels following a period of meditation. Biol Psychol. 2000;53(1):69-78.
27. Walton KG, Pugh ND, Gelderloos P, Macrae P. Stress reduction and preventing hypertension: preliminary support of a psychoneuroendocrine mechanism. J Altern Complement Med. 1995;1(3):263-283.
28. Banasik J, Williams H, Haberman M, Blank SE, Bendel R. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23(3):135-142.
29. Vadiraja HS, Raghavendra RM, Nagarathna R, et al. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Integr Cancer Ther. 2009;8(1):37-46.
30. Esch T, Stefano GB, Fricchione GL, Benson H. The role of stress in neurodegenerative diseases and mental disorders. Neuro Endocrinol Lett. 2002;23(3):199-208.
31. Lingjaerde O, Ahlfors UG, Bech P, Dencker SJ, Elgen K. The UKU side effect rating scale. A new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatr Scand Suppl. 1987;334:1-100.
32. Schwartz TL, Nihalani N, Jindal S, Virk S, Jones N. Psychiatric medication-induced obesity: a review. Obes Rev. 2004;5(2):115-121.
33. Wirshing DA, Spellberg BJ, Erhart SM, Marder SR, Wirshing WC. Novel antipsychotics and new onset diabetes. Biol Psychiatry. 1998;44(8):778-783.
34. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396.
35. Quiroga Murcia C, Kreutz G, Clift S, Bongard S. Shall we dance? An exploration of the perceived benefits of dancing on well-being. Arts Health. 2010;2(2):149-163.
36. The Duke Center for Integrative Medicine; Liebowitz R, Smith L. The Duke Encyclopedia of New Medicine: Conventional and Alternative Medicine for All Ages. London, UK: Rodale Books International; 2006.
37. Walsh R. Lifestyle and mental health. Am Psychol. 2011;66(7):579-592.
38. Frattaroli J, Weidner G, Dnistrian AM, et al. Clinical events in prostate cancer lifestyle trial: results from two years of follow-up. Urology. 2008;72(6):1319-1323.
39. Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med. 2008;5(1):e12.
40. Sidhu KS, Vandana P, Balon R. Exercise prescription: a practical, effective therapy for depression. Curr Psychiatr. 2009;8(6):38-51.