User login
New ACOG president puts focus on smoking, obesity
SAN FRANCISCO – The new president of the American College of Obstetricians and Gynecologists wants ob.gyns. to step up their efforts to help patients with their overall wellness, including smoking cessation, help with weight control, and cardiac screening.
For many women, the ob.gyn. is their primary physician and if that physician isn’t counseling and screening for these health issues, it won’t be done at all, Dr. Mark S. DeFrancesco, the incoming president of ACOG, said during a press briefing at the organization’s annual meeting.
Dr. DeFrancesco, an ob.gyn. in Waterbury, Conn., and assistant clinical professor at the University of Connecticut, was installed as the new ACOG president on May 6. He also will serve as president of the American Congress of Obstetricians and Gynecologists.
He said that he plans to focus on population health, specifically encouraging ob.gyns. to do more to address significant preventable causes of death such as smoking and obesity, during his year-long term in office.
The idea isn’t that ob.gyns. should be treating hypertension in their offices but that they should be looking for it during the well woman visit and making appropriate referrals.
“These things should not happen on our watch,” Dr. DeFrancesco said.
He said that he plans to work with the ACOG staff to develop a toolkit for ob.gyns. that will make it easier to address these population health issues. He also plans to work with insurers to convince them to pay physicians for the time spent on this counseling.
Dr. John C. Jennings, the outgoing president of ACOG, said that Dr. DeFrancesco’s focus on population health will complement the work that ACOG has been doing over the past year in encouraging a team approach to women’s health care. For instance, if a patient needs help losing weight, physicians could partner with a dietitian. Physicians shouldn’t be expected to conquer complex health issues such as smoking and obesity on their own, he said.
“You can’t tackle those [issues] with just one physician,” Dr. Jennings said.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
SAN FRANCISCO – The new president of the American College of Obstetricians and Gynecologists wants ob.gyns. to step up their efforts to help patients with their overall wellness, including smoking cessation, help with weight control, and cardiac screening.
For many women, the ob.gyn. is their primary physician and if that physician isn’t counseling and screening for these health issues, it won’t be done at all, Dr. Mark S. DeFrancesco, the incoming president of ACOG, said during a press briefing at the organization’s annual meeting.
Dr. DeFrancesco, an ob.gyn. in Waterbury, Conn., and assistant clinical professor at the University of Connecticut, was installed as the new ACOG president on May 6. He also will serve as president of the American Congress of Obstetricians and Gynecologists.
He said that he plans to focus on population health, specifically encouraging ob.gyns. to do more to address significant preventable causes of death such as smoking and obesity, during his year-long term in office.
The idea isn’t that ob.gyns. should be treating hypertension in their offices but that they should be looking for it during the well woman visit and making appropriate referrals.
“These things should not happen on our watch,” Dr. DeFrancesco said.
He said that he plans to work with the ACOG staff to develop a toolkit for ob.gyns. that will make it easier to address these population health issues. He also plans to work with insurers to convince them to pay physicians for the time spent on this counseling.
Dr. John C. Jennings, the outgoing president of ACOG, said that Dr. DeFrancesco’s focus on population health will complement the work that ACOG has been doing over the past year in encouraging a team approach to women’s health care. For instance, if a patient needs help losing weight, physicians could partner with a dietitian. Physicians shouldn’t be expected to conquer complex health issues such as smoking and obesity on their own, he said.
“You can’t tackle those [issues] with just one physician,” Dr. Jennings said.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
SAN FRANCISCO – The new president of the American College of Obstetricians and Gynecologists wants ob.gyns. to step up their efforts to help patients with their overall wellness, including smoking cessation, help with weight control, and cardiac screening.
For many women, the ob.gyn. is their primary physician and if that physician isn’t counseling and screening for these health issues, it won’t be done at all, Dr. Mark S. DeFrancesco, the incoming president of ACOG, said during a press briefing at the organization’s annual meeting.
Dr. DeFrancesco, an ob.gyn. in Waterbury, Conn., and assistant clinical professor at the University of Connecticut, was installed as the new ACOG president on May 6. He also will serve as president of the American Congress of Obstetricians and Gynecologists.
He said that he plans to focus on population health, specifically encouraging ob.gyns. to do more to address significant preventable causes of death such as smoking and obesity, during his year-long term in office.
The idea isn’t that ob.gyns. should be treating hypertension in their offices but that they should be looking for it during the well woman visit and making appropriate referrals.
“These things should not happen on our watch,” Dr. DeFrancesco said.
He said that he plans to work with the ACOG staff to develop a toolkit for ob.gyns. that will make it easier to address these population health issues. He also plans to work with insurers to convince them to pay physicians for the time spent on this counseling.
Dr. John C. Jennings, the outgoing president of ACOG, said that Dr. DeFrancesco’s focus on population health will complement the work that ACOG has been doing over the past year in encouraging a team approach to women’s health care. For instance, if a patient needs help losing weight, physicians could partner with a dietitian. Physicians shouldn’t be expected to conquer complex health issues such as smoking and obesity on their own, he said.
“You can’t tackle those [issues] with just one physician,” Dr. Jennings said.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
AT THE ACOG ANNUAL CLINICAL MEETING
VIDEO: Cervicovaginal microbiome holds promise in preventing preterm birth
SAN FRANCISCO– Predicting and preventing preterm birth continues to be a challenge for clinicians, but new research into the cervicovaginal microbiome could help explain the premature cervical remodeling that precedes preterm birth and ultimately lead to the development of novel therapeutics.
Researchers at the University of Pennsylvania recently found that there is a distinct molecular profile in the cervix that is associated with preterm birth and can be assessed noninvasively using RNA Pap testing.
In a video interview at the annual meeting of the American Congress of Obstetricians and Gynecologists, Dr. Michal Elovitz, director of the maternal and child health research program and the prematurity prevention program at the University of Pennsylvania, Philadelphia, said that the findings represent a “fork in the road” that could change how clinicians treat preterm birth, provided the findings can be validated in other studies.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mschneider@frontlinemedcom.com
On Twitter @maryellenny
SAN FRANCISCO– Predicting and preventing preterm birth continues to be a challenge for clinicians, but new research into the cervicovaginal microbiome could help explain the premature cervical remodeling that precedes preterm birth and ultimately lead to the development of novel therapeutics.
Researchers at the University of Pennsylvania recently found that there is a distinct molecular profile in the cervix that is associated with preterm birth and can be assessed noninvasively using RNA Pap testing.
In a video interview at the annual meeting of the American Congress of Obstetricians and Gynecologists, Dr. Michal Elovitz, director of the maternal and child health research program and the prematurity prevention program at the University of Pennsylvania, Philadelphia, said that the findings represent a “fork in the road” that could change how clinicians treat preterm birth, provided the findings can be validated in other studies.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mschneider@frontlinemedcom.com
On Twitter @maryellenny
SAN FRANCISCO– Predicting and preventing preterm birth continues to be a challenge for clinicians, but new research into the cervicovaginal microbiome could help explain the premature cervical remodeling that precedes preterm birth and ultimately lead to the development of novel therapeutics.
Researchers at the University of Pennsylvania recently found that there is a distinct molecular profile in the cervix that is associated with preterm birth and can be assessed noninvasively using RNA Pap testing.
In a video interview at the annual meeting of the American Congress of Obstetricians and Gynecologists, Dr. Michal Elovitz, director of the maternal and child health research program and the prematurity prevention program at the University of Pennsylvania, Philadelphia, said that the findings represent a “fork in the road” that could change how clinicians treat preterm birth, provided the findings can be validated in other studies.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mschneider@frontlinemedcom.com
On Twitter @maryellenny
AT THE ACOG ANNUAL CLINICAL MEETING
VIDEO: Are birthing centers a safe choice for women?
SAN FRANCISCO – The number of babies delivered at birthing centers in the United States is still very low, but freestanding birthing facilities are growing rapidly. Are these centers, many of which are not accredited, safe choices for women who are looking for a noninstitutional birth experience?
At the annual meeting of the American Congress of Obstetricians and Gynecologists, Dr. Edward R. Yeomans, chair of the department of ob.gyn. at Texas Tech University, Lubbock, faced off against Ginger Breedlove, Ph.D., president of the American College of Nurse-Midwives, in a debate about the preferred site for delivery.
Dr. Yeomans, who favors hospital-based deliveries, said that safety is the major issue. Birthing centers are not equipped to deal with emergencies that can arise even in low-risk pregnancies and may require immediate access to surgery or a blood bank.
Dr. Breedlove countered that accredited birthing centers have strict standards for the cases they accept and have transport plans in place for emergencies. She added that she supports accreditation for all freestanding birthing centers.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
SAN FRANCISCO – The number of babies delivered at birthing centers in the United States is still very low, but freestanding birthing facilities are growing rapidly. Are these centers, many of which are not accredited, safe choices for women who are looking for a noninstitutional birth experience?
At the annual meeting of the American Congress of Obstetricians and Gynecologists, Dr. Edward R. Yeomans, chair of the department of ob.gyn. at Texas Tech University, Lubbock, faced off against Ginger Breedlove, Ph.D., president of the American College of Nurse-Midwives, in a debate about the preferred site for delivery.
Dr. Yeomans, who favors hospital-based deliveries, said that safety is the major issue. Birthing centers are not equipped to deal with emergencies that can arise even in low-risk pregnancies and may require immediate access to surgery or a blood bank.
Dr. Breedlove countered that accredited birthing centers have strict standards for the cases they accept and have transport plans in place for emergencies. She added that she supports accreditation for all freestanding birthing centers.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
SAN FRANCISCO – The number of babies delivered at birthing centers in the United States is still very low, but freestanding birthing facilities are growing rapidly. Are these centers, many of which are not accredited, safe choices for women who are looking for a noninstitutional birth experience?
At the annual meeting of the American Congress of Obstetricians and Gynecologists, Dr. Edward R. Yeomans, chair of the department of ob.gyn. at Texas Tech University, Lubbock, faced off against Ginger Breedlove, Ph.D., president of the American College of Nurse-Midwives, in a debate about the preferred site for delivery.
Dr. Yeomans, who favors hospital-based deliveries, said that safety is the major issue. Birthing centers are not equipped to deal with emergencies that can arise even in low-risk pregnancies and may require immediate access to surgery or a blood bank.
Dr. Breedlove countered that accredited birthing centers have strict standards for the cases they accept and have transport plans in place for emergencies. She added that she supports accreditation for all freestanding birthing centers.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
AT THE ACOG ANNUAL CLINICAL MEETING
Coalition decries legislative interference in medicine
A coalition of physician, consumer, and other advocacy groups is asking politicians to stop trying to regulate the physician-patient relationship.
The Coalition to Protect the Patient-Provider Relationship – which includes the American College of Obstetricians and Gynecologists, the American Academy of Family Physicians, the American College of Physicians, and 13 other organizations – issued a statement expressing “serious concern” about the increasing number of government actions that “inappropriately interfere” in the relationship between patients and their health care providers by asking providers to violate their medical training and their ethical obligations to patients.
The statement points to laws recently enacted in Arizona and Arkansas that require abortion providers to inform patients that medication abortion may be reversible, a claim that is not supported by science, the coalition wrote.
“The mandate is emblematic of a larger trend of lawmakers abusing their responsibilities by imposing ideological views on licensed and highly trained health care professionals,” the coalition said in its statement.
The coalition urged lawmakers to follow four principles to protect the patient-provider relationship:
The coalition’s statement comes as physician organizations are increasingly pushing back against lawmakers for attempts to legislate their interactions with patients, including a Florida law that bars physicians from asking families about the presence of guns in the home and requirements in other states that women have ultrasonography before an abortion.
In 2012, the ACP, AAFP, ACOG, American Academy of Pediatrics, and American College of Surgeons wrote a joint editorial in the New England Journal of Medicine condemning these laws (2012;367:1557-9).
“Physicians must have the ability and freedom to speak to their patients freely and confidentially, to provide patients with factual information relevant to their health, to fully answer their patients’ questions, and to advise them on the course of best care without the fear of penalty,” the groups wrote in the editorial.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
A coalition of physician, consumer, and other advocacy groups is asking politicians to stop trying to regulate the physician-patient relationship.
The Coalition to Protect the Patient-Provider Relationship – which includes the American College of Obstetricians and Gynecologists, the American Academy of Family Physicians, the American College of Physicians, and 13 other organizations – issued a statement expressing “serious concern” about the increasing number of government actions that “inappropriately interfere” in the relationship between patients and their health care providers by asking providers to violate their medical training and their ethical obligations to patients.
The statement points to laws recently enacted in Arizona and Arkansas that require abortion providers to inform patients that medication abortion may be reversible, a claim that is not supported by science, the coalition wrote.
“The mandate is emblematic of a larger trend of lawmakers abusing their responsibilities by imposing ideological views on licensed and highly trained health care professionals,” the coalition said in its statement.
The coalition urged lawmakers to follow four principles to protect the patient-provider relationship:
The coalition’s statement comes as physician organizations are increasingly pushing back against lawmakers for attempts to legislate their interactions with patients, including a Florida law that bars physicians from asking families about the presence of guns in the home and requirements in other states that women have ultrasonography before an abortion.
In 2012, the ACP, AAFP, ACOG, American Academy of Pediatrics, and American College of Surgeons wrote a joint editorial in the New England Journal of Medicine condemning these laws (2012;367:1557-9).
“Physicians must have the ability and freedom to speak to their patients freely and confidentially, to provide patients with factual information relevant to their health, to fully answer their patients’ questions, and to advise them on the course of best care without the fear of penalty,” the groups wrote in the editorial.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
A coalition of physician, consumer, and other advocacy groups is asking politicians to stop trying to regulate the physician-patient relationship.
The Coalition to Protect the Patient-Provider Relationship – which includes the American College of Obstetricians and Gynecologists, the American Academy of Family Physicians, the American College of Physicians, and 13 other organizations – issued a statement expressing “serious concern” about the increasing number of government actions that “inappropriately interfere” in the relationship between patients and their health care providers by asking providers to violate their medical training and their ethical obligations to patients.
The statement points to laws recently enacted in Arizona and Arkansas that require abortion providers to inform patients that medication abortion may be reversible, a claim that is not supported by science, the coalition wrote.
“The mandate is emblematic of a larger trend of lawmakers abusing their responsibilities by imposing ideological views on licensed and highly trained health care professionals,” the coalition said in its statement.
The coalition urged lawmakers to follow four principles to protect the patient-provider relationship:
The coalition’s statement comes as physician organizations are increasingly pushing back against lawmakers for attempts to legislate their interactions with patients, including a Florida law that bars physicians from asking families about the presence of guns in the home and requirements in other states that women have ultrasonography before an abortion.
In 2012, the ACP, AAFP, ACOG, American Academy of Pediatrics, and American College of Surgeons wrote a joint editorial in the New England Journal of Medicine condemning these laws (2012;367:1557-9).
“Physicians must have the ability and freedom to speak to their patients freely and confidentially, to provide patients with factual information relevant to their health, to fully answer their patients’ questions, and to advise them on the course of best care without the fear of penalty,” the groups wrote in the editorial.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Match Day 2015: Ob.gyn. remains desirable for U.S. grads
Obstetrics and gynecology was a popular choice for medical students in the 2015 Main Residency Match, filling all of the 1,255 positions available.
Ob.gyn. joined dermatology, medicine-psychiatry, orthopedic surgery, thoracic surgery, pediatric-primary care, and physical medicine/rehabilitation as the only first-year programs offering at least 20 positions in the Match that filled all of their residency spots, according to data from the National Resident Matching Program.
Of the 1,255 residency positions offered in ob.gyn., 79.8% were filled by U.S. medical graduates. Over the past 5 years, both the overall fill rate and the percentage of residency positions filled by U.S. graduates have gradually increased: In 2011, 99.1% of the 1,200 positions were filled, with 74.3% filled by U.S. graduates.
The appeal of the specialty is easy to see, according to Dr. Todd Griffin, chair of the department of obstetrics, gynecology and reproductive medicine at Stony Brook University School of Medicine (N.Y.).
“Ob.gyn. is becoming a more popular field again,” Dr. Griffin said. “I think people are really understanding what the field is and all the different opportunities within it.”
Advances in surgery, from robotics to advanced laparoscopy, have made ob.gyn. more appealing for students with an interest in surgery, he said, and changing attitude about lifestyle has also made the specialty more attractive.
“When you graduate, there’s more focus on work-life balance,” he said. “That’s made it much more attractive for candidates.”
The rising interest in ob.gyn. means that residency directors have their pick of the top candidates. Dr. Melissa Henretta, the director of the ob.gyn. residency program at Stony Brook University, said that her program accepts five new residents each year. This year they received approximately 400 applications and interviewed about 80 students.
“We’ve got a great group of really strong people,” she said.
Dr. Griffin said he’s hearing the same thing from ob.gyn. department chairs around the country.
“It seems that more and more of the top students are choosing ob.gyn., which I think it is great,” he said. “I think it’s great for women’s health going forward. Hopefully that’s because we’re giving them the right experience in medical school.”
Workforce concerns remain
Despite the high fill rate, leaders in obstetrics and gynecology are still concerned about shortages, especially in rural and underserved areas.
“There’s a tremendous geographic maldistribution of our graduates,” said Dr. John C. Jennings, president of the American Congress of Obstetricians and Gynecologists. “We’ve got to do something to correct that.”
A 2011 workforce report commissioned by ACOG cited a shortage of ob.gyns. of somewhere between 18% (about 9,000 physicians) and 25% (about 15,000 physicians) by 2030, depending on the number of years a physician spends in practice. Already nearly half of the 3,107 counties in the U.S. are without an ob.gyn. The shortages are predominantly in rural areas in the Midwest and the Mountain West, though shortages exist in all states, according to the report.
One of the problems, Dr. Jennings said, is that the number of ob.gyn. residency positions has been “stagnant” since Congress restricted Medicare funding for graduate medical education in the Balanced Budget Act of 1997. That means that teaching hospitals must fund the high-cost of training ob.gyns. on their own if they want to increase the positions they offer.
In ob.gyn., though there have been small fluctuations from year to year, the overall number of residency slots has remained around 1,200 for the last 30 years, according to the report.
“This year, we were unable to accommodate a large number of medical students who applied to ob.gyn. programs,” Dr. Jennings said. “The number of unmatched ob.gyn. applicants shows the need for more ob.gyn. residencies in the U.S. More ob.gyn. residencies would allow us to better meet the growing needs of American women.”
Another issue is that about a quarter of residents will enter subspecialty training programs, taking them out of the pool of physicians addressing general women’s health issues and providing prenatal care, Dr. Jennings said. And another 20% to 25% will “self-specialize” by restricting their practice to outpatient gynecology or becoming laborists, he added.
One possible solution comes in the form of new federal legislation, the Improving Access to Maternity Care Act (H.R. 1209), which would designate maternity care shortage areas under the Public Health Service Act, allowing providers in the National Health Service Corps to serve in medical facilities in these shortage areas. These shortage designations already exist for primary care, dental care, and mental health.
But Dr. Jennings said more work is needed, including designing programs so that ob.gyn. residents are allowed to rotate into community clinics in these shortage areas, rather than being tied to their training hospital. Switching up the traditional training paradigm would make it more likely that these residents would choose to practice in these high-need communities after they finish their training, he said.
ACOG has assembled task forces of experts to look for solutions to the looming shortage, including team approaches to women’s health care as well as ways to preserve ob.gyns. in the workforce as more physicians sell their practices to multispecialty groups or go to work for hospitals.
Why Ob. Gyn.?
At Stony Brook University School of Medicine in New York, the medical students who matched to ob.gyn. residencies expressed a variety of reasons for choosing their future career paths, but they all cited the connection to patients as the deciding factor.
Stephanie Miller, who matched to the State University of New York Upstate Medical University in Syracuse, said she had her “a-ha moment” when she helped deliver a baby for the first time. “This was the only place where I felt like I really connected with my patients,” she said. Her future plans aren’t set but she said she’s considering a fellowship training in maternal-fetal medicine with the goal of a career in academics.
Joan Rosario, who heads to the Bronx (N.Y.) for her ob.gyn. residency at Einstein/Montefiore Medical Center, also chose ob.gyn. during her clinical clerkship. She said the connection between ob.gyn. physicians and their patients was unique. “They were the most caring, compassionate physicians,” she said. Ms. Rosario said that she was also drawn the variety of career opportunities within the field, including the surgical aspects. Right now, she’s considering subspecializing in gynecologic oncology after residency.
Andrew Rivara matched to his first choice: Duke University Medical Center in Durham, N.C. He said he was drawn to ob.gyn. because it combines his love of surgery with the deep physician-patient relationship he wants to experience. He also wants to pursue a fellowship in gynecologic oncology, he said, because it offers the potential to “change somebody’s life.”
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Obstetrics and gynecology was a popular choice for medical students in the 2015 Main Residency Match, filling all of the 1,255 positions available.
Ob.gyn. joined dermatology, medicine-psychiatry, orthopedic surgery, thoracic surgery, pediatric-primary care, and physical medicine/rehabilitation as the only first-year programs offering at least 20 positions in the Match that filled all of their residency spots, according to data from the National Resident Matching Program.
Of the 1,255 residency positions offered in ob.gyn., 79.8% were filled by U.S. medical graduates. Over the past 5 years, both the overall fill rate and the percentage of residency positions filled by U.S. graduates have gradually increased: In 2011, 99.1% of the 1,200 positions were filled, with 74.3% filled by U.S. graduates.
The appeal of the specialty is easy to see, according to Dr. Todd Griffin, chair of the department of obstetrics, gynecology and reproductive medicine at Stony Brook University School of Medicine (N.Y.).
“Ob.gyn. is becoming a more popular field again,” Dr. Griffin said. “I think people are really understanding what the field is and all the different opportunities within it.”
Advances in surgery, from robotics to advanced laparoscopy, have made ob.gyn. more appealing for students with an interest in surgery, he said, and changing attitude about lifestyle has also made the specialty more attractive.
“When you graduate, there’s more focus on work-life balance,” he said. “That’s made it much more attractive for candidates.”
The rising interest in ob.gyn. means that residency directors have their pick of the top candidates. Dr. Melissa Henretta, the director of the ob.gyn. residency program at Stony Brook University, said that her program accepts five new residents each year. This year they received approximately 400 applications and interviewed about 80 students.
“We’ve got a great group of really strong people,” she said.
Dr. Griffin said he’s hearing the same thing from ob.gyn. department chairs around the country.
“It seems that more and more of the top students are choosing ob.gyn., which I think it is great,” he said. “I think it’s great for women’s health going forward. Hopefully that’s because we’re giving them the right experience in medical school.”
Workforce concerns remain
Despite the high fill rate, leaders in obstetrics and gynecology are still concerned about shortages, especially in rural and underserved areas.
“There’s a tremendous geographic maldistribution of our graduates,” said Dr. John C. Jennings, president of the American Congress of Obstetricians and Gynecologists. “We’ve got to do something to correct that.”
A 2011 workforce report commissioned by ACOG cited a shortage of ob.gyns. of somewhere between 18% (about 9,000 physicians) and 25% (about 15,000 physicians) by 2030, depending on the number of years a physician spends in practice. Already nearly half of the 3,107 counties in the U.S. are without an ob.gyn. The shortages are predominantly in rural areas in the Midwest and the Mountain West, though shortages exist in all states, according to the report.
One of the problems, Dr. Jennings said, is that the number of ob.gyn. residency positions has been “stagnant” since Congress restricted Medicare funding for graduate medical education in the Balanced Budget Act of 1997. That means that teaching hospitals must fund the high-cost of training ob.gyns. on their own if they want to increase the positions they offer.
In ob.gyn., though there have been small fluctuations from year to year, the overall number of residency slots has remained around 1,200 for the last 30 years, according to the report.
“This year, we were unable to accommodate a large number of medical students who applied to ob.gyn. programs,” Dr. Jennings said. “The number of unmatched ob.gyn. applicants shows the need for more ob.gyn. residencies in the U.S. More ob.gyn. residencies would allow us to better meet the growing needs of American women.”
Another issue is that about a quarter of residents will enter subspecialty training programs, taking them out of the pool of physicians addressing general women’s health issues and providing prenatal care, Dr. Jennings said. And another 20% to 25% will “self-specialize” by restricting their practice to outpatient gynecology or becoming laborists, he added.
One possible solution comes in the form of new federal legislation, the Improving Access to Maternity Care Act (H.R. 1209), which would designate maternity care shortage areas under the Public Health Service Act, allowing providers in the National Health Service Corps to serve in medical facilities in these shortage areas. These shortage designations already exist for primary care, dental care, and mental health.
But Dr. Jennings said more work is needed, including designing programs so that ob.gyn. residents are allowed to rotate into community clinics in these shortage areas, rather than being tied to their training hospital. Switching up the traditional training paradigm would make it more likely that these residents would choose to practice in these high-need communities after they finish their training, he said.
ACOG has assembled task forces of experts to look for solutions to the looming shortage, including team approaches to women’s health care as well as ways to preserve ob.gyns. in the workforce as more physicians sell their practices to multispecialty groups or go to work for hospitals.
Why Ob. Gyn.?
At Stony Brook University School of Medicine in New York, the medical students who matched to ob.gyn. residencies expressed a variety of reasons for choosing their future career paths, but they all cited the connection to patients as the deciding factor.
Stephanie Miller, who matched to the State University of New York Upstate Medical University in Syracuse, said she had her “a-ha moment” when she helped deliver a baby for the first time. “This was the only place where I felt like I really connected with my patients,” she said. Her future plans aren’t set but she said she’s considering a fellowship training in maternal-fetal medicine with the goal of a career in academics.
Joan Rosario, who heads to the Bronx (N.Y.) for her ob.gyn. residency at Einstein/Montefiore Medical Center, also chose ob.gyn. during her clinical clerkship. She said the connection between ob.gyn. physicians and their patients was unique. “They were the most caring, compassionate physicians,” she said. Ms. Rosario said that she was also drawn the variety of career opportunities within the field, including the surgical aspects. Right now, she’s considering subspecializing in gynecologic oncology after residency.
Andrew Rivara matched to his first choice: Duke University Medical Center in Durham, N.C. He said he was drawn to ob.gyn. because it combines his love of surgery with the deep physician-patient relationship he wants to experience. He also wants to pursue a fellowship in gynecologic oncology, he said, because it offers the potential to “change somebody’s life.”
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Obstetrics and gynecology was a popular choice for medical students in the 2015 Main Residency Match, filling all of the 1,255 positions available.
Ob.gyn. joined dermatology, medicine-psychiatry, orthopedic surgery, thoracic surgery, pediatric-primary care, and physical medicine/rehabilitation as the only first-year programs offering at least 20 positions in the Match that filled all of their residency spots, according to data from the National Resident Matching Program.
Of the 1,255 residency positions offered in ob.gyn., 79.8% were filled by U.S. medical graduates. Over the past 5 years, both the overall fill rate and the percentage of residency positions filled by U.S. graduates have gradually increased: In 2011, 99.1% of the 1,200 positions were filled, with 74.3% filled by U.S. graduates.
The appeal of the specialty is easy to see, according to Dr. Todd Griffin, chair of the department of obstetrics, gynecology and reproductive medicine at Stony Brook University School of Medicine (N.Y.).
“Ob.gyn. is becoming a more popular field again,” Dr. Griffin said. “I think people are really understanding what the field is and all the different opportunities within it.”
Advances in surgery, from robotics to advanced laparoscopy, have made ob.gyn. more appealing for students with an interest in surgery, he said, and changing attitude about lifestyle has also made the specialty more attractive.
“When you graduate, there’s more focus on work-life balance,” he said. “That’s made it much more attractive for candidates.”
The rising interest in ob.gyn. means that residency directors have their pick of the top candidates. Dr. Melissa Henretta, the director of the ob.gyn. residency program at Stony Brook University, said that her program accepts five new residents each year. This year they received approximately 400 applications and interviewed about 80 students.
“We’ve got a great group of really strong people,” she said.
Dr. Griffin said he’s hearing the same thing from ob.gyn. department chairs around the country.
“It seems that more and more of the top students are choosing ob.gyn., which I think it is great,” he said. “I think it’s great for women’s health going forward. Hopefully that’s because we’re giving them the right experience in medical school.”
Workforce concerns remain
Despite the high fill rate, leaders in obstetrics and gynecology are still concerned about shortages, especially in rural and underserved areas.
“There’s a tremendous geographic maldistribution of our graduates,” said Dr. John C. Jennings, president of the American Congress of Obstetricians and Gynecologists. “We’ve got to do something to correct that.”
A 2011 workforce report commissioned by ACOG cited a shortage of ob.gyns. of somewhere between 18% (about 9,000 physicians) and 25% (about 15,000 physicians) by 2030, depending on the number of years a physician spends in practice. Already nearly half of the 3,107 counties in the U.S. are without an ob.gyn. The shortages are predominantly in rural areas in the Midwest and the Mountain West, though shortages exist in all states, according to the report.
One of the problems, Dr. Jennings said, is that the number of ob.gyn. residency positions has been “stagnant” since Congress restricted Medicare funding for graduate medical education in the Balanced Budget Act of 1997. That means that teaching hospitals must fund the high-cost of training ob.gyns. on their own if they want to increase the positions they offer.
In ob.gyn., though there have been small fluctuations from year to year, the overall number of residency slots has remained around 1,200 for the last 30 years, according to the report.
“This year, we were unable to accommodate a large number of medical students who applied to ob.gyn. programs,” Dr. Jennings said. “The number of unmatched ob.gyn. applicants shows the need for more ob.gyn. residencies in the U.S. More ob.gyn. residencies would allow us to better meet the growing needs of American women.”
Another issue is that about a quarter of residents will enter subspecialty training programs, taking them out of the pool of physicians addressing general women’s health issues and providing prenatal care, Dr. Jennings said. And another 20% to 25% will “self-specialize” by restricting their practice to outpatient gynecology or becoming laborists, he added.
One possible solution comes in the form of new federal legislation, the Improving Access to Maternity Care Act (H.R. 1209), which would designate maternity care shortage areas under the Public Health Service Act, allowing providers in the National Health Service Corps to serve in medical facilities in these shortage areas. These shortage designations already exist for primary care, dental care, and mental health.
But Dr. Jennings said more work is needed, including designing programs so that ob.gyn. residents are allowed to rotate into community clinics in these shortage areas, rather than being tied to their training hospital. Switching up the traditional training paradigm would make it more likely that these residents would choose to practice in these high-need communities after they finish their training, he said.
ACOG has assembled task forces of experts to look for solutions to the looming shortage, including team approaches to women’s health care as well as ways to preserve ob.gyns. in the workforce as more physicians sell their practices to multispecialty groups or go to work for hospitals.
Why Ob. Gyn.?
At Stony Brook University School of Medicine in New York, the medical students who matched to ob.gyn. residencies expressed a variety of reasons for choosing their future career paths, but they all cited the connection to patients as the deciding factor.
Stephanie Miller, who matched to the State University of New York Upstate Medical University in Syracuse, said she had her “a-ha moment” when she helped deliver a baby for the first time. “This was the only place where I felt like I really connected with my patients,” she said. Her future plans aren’t set but she said she’s considering a fellowship training in maternal-fetal medicine with the goal of a career in academics.
Joan Rosario, who heads to the Bronx (N.Y.) for her ob.gyn. residency at Einstein/Montefiore Medical Center, also chose ob.gyn. during her clinical clerkship. She said the connection between ob.gyn. physicians and their patients was unique. “They were the most caring, compassionate physicians,” she said. Ms. Rosario said that she was also drawn the variety of career opportunities within the field, including the surgical aspects. Right now, she’s considering subspecializing in gynecologic oncology after residency.
Andrew Rivara matched to his first choice: Duke University Medical Center in Durham, N.C. He said he was drawn to ob.gyn. because it combines his love of surgery with the deep physician-patient relationship he wants to experience. He also wants to pursue a fellowship in gynecologic oncology, he said, because it offers the potential to “change somebody’s life.”
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Leapfrog: Early elective deliveries down nationally, but rates vary
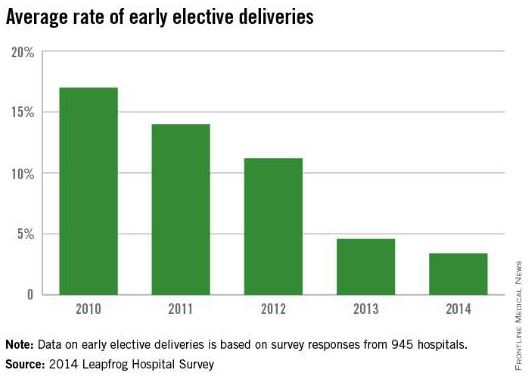
The practice of early elective deliveries is down across the country, but there is still wide variation in meeting maternal quality indicators at U.S. hospitals, according to a new report from the Leapfrog Group.
Among 945 hospitals that voluntarily reported quality data to the Leapfrog Group, 78% performed early elective deliveries less than 5% of the time in 2014. The current data shows a steady decline in the early elective deliveries – scheduled cesarean deliveries or elective inductions that occur prior to 39 weeks’ gestation without a medical indication. Between 2010 and 2014, the national average rate of early elective deliveries dropped from 17% to 3.4%.
But variation remains. Among 82 hospitals that reported data in 2014, the rate of early elective deliveries was more than 10%. The rate was higher in rural areas than at hospitals in urban areas, the report found.
The Leapfrog Group report also shows some small gains in decreasing the use of episiotomy at U.S. hospitals. The national average rate of episiotomies decreased from 13% in 2012 to 11.3% in 2014.
However, there was also wide variation in this measure. Of the 990 hospitals that reported episiotomy data, 65% met the Leapfrog goal of performing the procedure 12% of the time or less. In 25 hospitals, the rate was 1% or less, while it was 40% or more in 12 hospitals.
U.S. hospitals have made virtually no progress in ensuring that high-risk deliveries are performed at hospitals with experienced, on-site neonatal intensive care units, according to the report.
Hospitals met the Leapfrog standard for high-risk deliveries if they delivered at least 50 very-low-birth-weight babies per year and ensured that at least 80% of mothers received antenatal steroids prior to delivery, or if they maintained a lower-than-average morbidity/mortality rate for very-low-birth-weight babies and provided antenatal steroids prior to delivery for at least 80% of mothers.
In 2014, the number of high-risk deliveries that occurred in hospitals meeting the Leapfrog standard was 24.4% of 435 hospitals, compared with 24% of 451 hospitals during the previous year.
The Leapfrog Group report relies on voluntary reporting from adult general acute care and freestanding pediatric hospitals across the United States. The report was prepared by Castlight Health.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
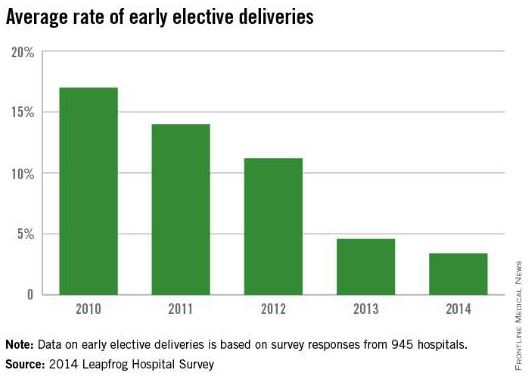
The practice of early elective deliveries is down across the country, but there is still wide variation in meeting maternal quality indicators at U.S. hospitals, according to a new report from the Leapfrog Group.
Among 945 hospitals that voluntarily reported quality data to the Leapfrog Group, 78% performed early elective deliveries less than 5% of the time in 2014. The current data shows a steady decline in the early elective deliveries – scheduled cesarean deliveries or elective inductions that occur prior to 39 weeks’ gestation without a medical indication. Between 2010 and 2014, the national average rate of early elective deliveries dropped from 17% to 3.4%.
But variation remains. Among 82 hospitals that reported data in 2014, the rate of early elective deliveries was more than 10%. The rate was higher in rural areas than at hospitals in urban areas, the report found.
The Leapfrog Group report also shows some small gains in decreasing the use of episiotomy at U.S. hospitals. The national average rate of episiotomies decreased from 13% in 2012 to 11.3% in 2014.
However, there was also wide variation in this measure. Of the 990 hospitals that reported episiotomy data, 65% met the Leapfrog goal of performing the procedure 12% of the time or less. In 25 hospitals, the rate was 1% or less, while it was 40% or more in 12 hospitals.
U.S. hospitals have made virtually no progress in ensuring that high-risk deliveries are performed at hospitals with experienced, on-site neonatal intensive care units, according to the report.
Hospitals met the Leapfrog standard for high-risk deliveries if they delivered at least 50 very-low-birth-weight babies per year and ensured that at least 80% of mothers received antenatal steroids prior to delivery, or if they maintained a lower-than-average morbidity/mortality rate for very-low-birth-weight babies and provided antenatal steroids prior to delivery for at least 80% of mothers.
In 2014, the number of high-risk deliveries that occurred in hospitals meeting the Leapfrog standard was 24.4% of 435 hospitals, compared with 24% of 451 hospitals during the previous year.
The Leapfrog Group report relies on voluntary reporting from adult general acute care and freestanding pediatric hospitals across the United States. The report was prepared by Castlight Health.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
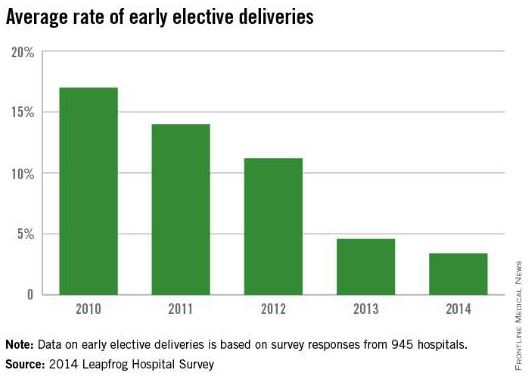
The practice of early elective deliveries is down across the country, but there is still wide variation in meeting maternal quality indicators at U.S. hospitals, according to a new report from the Leapfrog Group.
Among 945 hospitals that voluntarily reported quality data to the Leapfrog Group, 78% performed early elective deliveries less than 5% of the time in 2014. The current data shows a steady decline in the early elective deliveries – scheduled cesarean deliveries or elective inductions that occur prior to 39 weeks’ gestation without a medical indication. Between 2010 and 2014, the national average rate of early elective deliveries dropped from 17% to 3.4%.
But variation remains. Among 82 hospitals that reported data in 2014, the rate of early elective deliveries was more than 10%. The rate was higher in rural areas than at hospitals in urban areas, the report found.
The Leapfrog Group report also shows some small gains in decreasing the use of episiotomy at U.S. hospitals. The national average rate of episiotomies decreased from 13% in 2012 to 11.3% in 2014.
However, there was also wide variation in this measure. Of the 990 hospitals that reported episiotomy data, 65% met the Leapfrog goal of performing the procedure 12% of the time or less. In 25 hospitals, the rate was 1% or less, while it was 40% or more in 12 hospitals.
U.S. hospitals have made virtually no progress in ensuring that high-risk deliveries are performed at hospitals with experienced, on-site neonatal intensive care units, according to the report.
Hospitals met the Leapfrog standard for high-risk deliveries if they delivered at least 50 very-low-birth-weight babies per year and ensured that at least 80% of mothers received antenatal steroids prior to delivery, or if they maintained a lower-than-average morbidity/mortality rate for very-low-birth-weight babies and provided antenatal steroids prior to delivery for at least 80% of mothers.
In 2014, the number of high-risk deliveries that occurred in hospitals meeting the Leapfrog standard was 24.4% of 435 hospitals, compared with 24% of 451 hospitals during the previous year.
The Leapfrog Group report relies on voluntary reporting from adult general acute care and freestanding pediatric hospitals across the United States. The report was prepared by Castlight Health.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Senators propose development of maternal care quality measures
A small group of senators is pushing legislation that would establish a set of maternal care quality measures under the Medicaid and the Children’s Health Insurance programs.
The Quality Care for Moms and Babies Act (S. 466), introduced Feb. 11, instructs the Health & Human Services secretary to develop a set of measures to assess the quality of care provided during pregnancy and the postpartum period. The measures would apply to clinicians and group practices, hospitals, health plans, and accountable care organizations.
The bill was introduced by Sen. Debbie Stabenow (D-Mich.) and Sen. Chuck Grassley (R-Iowa) and cosponsored by a handful of Democrats in the Senate. A companion bill is expected to be introduced in the House.
Sen. Stabenow introduced the same bill in 2013, but it stalled in committee.
The bill would require HHS to seek public comments on a set of proposed measures by Jan. 1, 2018, with the publication of an initial measure set by Jan. 1, 2019. Measures would be evidence based and risk adjusted.
Debra L. Ness, president of the National Partnership for Women & Families, praised the introduction of the bill.
“Our country’s infant and maternal mortality rates are too high, and our performance on prematurity, low-birth-weight babies, cesareans, early elective deliveries, and exclusive breastfeeding lags behind that of many other nations,” she said in a statement. “We simply must improve the quality of care for both mothers and babies – and this legislation can do that.”
mschneider@frontlinemedcom.com
On Twitter @maryellenny
A small group of senators is pushing legislation that would establish a set of maternal care quality measures under the Medicaid and the Children’s Health Insurance programs.
The Quality Care for Moms and Babies Act (S. 466), introduced Feb. 11, instructs the Health & Human Services secretary to develop a set of measures to assess the quality of care provided during pregnancy and the postpartum period. The measures would apply to clinicians and group practices, hospitals, health plans, and accountable care organizations.
The bill was introduced by Sen. Debbie Stabenow (D-Mich.) and Sen. Chuck Grassley (R-Iowa) and cosponsored by a handful of Democrats in the Senate. A companion bill is expected to be introduced in the House.
Sen. Stabenow introduced the same bill in 2013, but it stalled in committee.
The bill would require HHS to seek public comments on a set of proposed measures by Jan. 1, 2018, with the publication of an initial measure set by Jan. 1, 2019. Measures would be evidence based and risk adjusted.
Debra L. Ness, president of the National Partnership for Women & Families, praised the introduction of the bill.
“Our country’s infant and maternal mortality rates are too high, and our performance on prematurity, low-birth-weight babies, cesareans, early elective deliveries, and exclusive breastfeeding lags behind that of many other nations,” she said in a statement. “We simply must improve the quality of care for both mothers and babies – and this legislation can do that.”
mschneider@frontlinemedcom.com
On Twitter @maryellenny
A small group of senators is pushing legislation that would establish a set of maternal care quality measures under the Medicaid and the Children’s Health Insurance programs.
The Quality Care for Moms and Babies Act (S. 466), introduced Feb. 11, instructs the Health & Human Services secretary to develop a set of measures to assess the quality of care provided during pregnancy and the postpartum period. The measures would apply to clinicians and group practices, hospitals, health plans, and accountable care organizations.
The bill was introduced by Sen. Debbie Stabenow (D-Mich.) and Sen. Chuck Grassley (R-Iowa) and cosponsored by a handful of Democrats in the Senate. A companion bill is expected to be introduced in the House.
Sen. Stabenow introduced the same bill in 2013, but it stalled in committee.
The bill would require HHS to seek public comments on a set of proposed measures by Jan. 1, 2018, with the publication of an initial measure set by Jan. 1, 2019. Measures would be evidence based and risk adjusted.
Debra L. Ness, president of the National Partnership for Women & Families, praised the introduction of the bill.
“Our country’s infant and maternal mortality rates are too high, and our performance on prematurity, low-birth-weight babies, cesareans, early elective deliveries, and exclusive breastfeeding lags behind that of many other nations,” she said in a statement. “We simply must improve the quality of care for both mothers and babies – and this legislation can do that.”
mschneider@frontlinemedcom.com
On Twitter @maryellenny
GOP lawmakers offer ACA alternative that includes tort reform
Three Republican lawmakers are proposing an alternative to the Affordable Care Act that would undo the controversial individual and employer mandates, cap medical liability damages, and offer a slimmed-down set of consumer insurance protections.
Sen. Orrin Hatch (R-Utah), chairman of the Senate Finance Committee; Rep. Fred Upton (R-Mich.), chairman of the House Energy and Commerce Committee; and Sen. Richard Burr (R-N.C.), a member of the Senate Finance Committee, proposed on Feb. 5 the Patient Choice, Affordability, Responsibility, and Empowerment (CARE) Act to repeal and replace the current health law.
“Our nation’s health care system was broken before Obamacare, and the President’s health care debacle has only made things worse,” Sen. Burr said in a statement. “The Patient CARE Act repeals Obamacare and addresses the fundamental cost drivers that Obamacare failed to address. We can lower costs and expand access to quality coverage and care by empowering individuals and their families to make their own health care decisions, rather than having the federal government make those decisions for them.”
The proposal – which came in the form of a 9-page outline – was unveiled just days after the House passed a bill to repeal the ACA by a vote of 239 to 186. While the House has voted numerous times to repeal the health law, this is the first time that the bill might actually be considered in the Senate, since control of that chamber has shifted to the Republicans.
Sen. Hatch and other GOP lawmakers offered a similar replacement proposal last year.
The Patient CARE Act outlines some federal medical liability reforms, including a cap on noneconomic damages and limits on attorneys’ fees. It also seeks to encourage new models for resolving disputes on the state level, such as expert panels to evaluate injury claims and administrative health courts.
The proposal offers a more limited range of consumer insurance protections than does the ACA, including:
• Adopting an age rating ratio of 5-1 for premiums, which would limit plans from charging older individuals any more than five times what a younger person pays. Under the ACA, the age rating ratio is 3-1.
• Banning the use of lifetime dollar limits on health coverage.
• Allowing states to opt out of the ACA’s dependent coverage provision, which lets younger adults stay on their parents’ health plans up to age 26.
• Providing guaranteed renewability of health plans regardless of an individual’s health status. Health plans would be able to cancel coverage only in cases of fraud, misrepresentation by a consumer, or failure to pay premiums.
• Banning denials of coverage based on preexisting medical conditions as long as the individual has been continuously covered with at least a catastrophic plan for 18 months. The proposal includes a one-time open enrollment for people currently uninsured.
The Patient CARE Act would provide federal tax subsidies to purchase insurance to individuals with annual incomes of up to 300% of the federal poverty level. The amount of the tax credit would decrease between 200% and 300% percent of poverty and would be age-adjusted with older individuals receiving a larger subsidy.
The proposal would change the tax treatment of employer-sponsored health insurance by capping the tax exclusion for health benefits at $12,000 for individuals and $30,000 for families. That means that workers would pay federal income taxes on benefits above those thresholds.
Within the Medicaid program, the Patient CARE Act seeks to provide states with a capped amount of federal funds that would “follow the patient” based on health status, age, and life circumstances. Some Medicaid participants would also have the option of using their federal tax credits to purchase private coverage.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Dr. Michael Nelson, FCCP, comments: With a new Congress controlled by Republicans, and given the prior attempts to overturn the Patient Protection and Affordable Care Act (a.k.a. "Obamacare"), it is not surprising that early in this legislative session an alternative plan has been proposed. One could argue some of the points of the proposal but not the accuracy of the statement made by one of the bills authors that "our nation's health care system was broken before Obamacare."
While this bill does address some issues of importance to physicians, it is certainly disappointing that this bill does not address the Sustainable Growth Rate formula (SGR). This looming threat of a 20% or more cut in physician reimbursement will do more harm to patient access and care than any other aspect addressed in this bill. Unfortunately, physicians rarely advocate at the federal level for themselves or their patients. Perhaps, with the introduction of this bill, it is the time to start.
Dr. Michael Nelson, FCCP, comments: With a new Congress controlled by Republicans, and given the prior attempts to overturn the Patient Protection and Affordable Care Act (a.k.a. "Obamacare"), it is not surprising that early in this legislative session an alternative plan has been proposed. One could argue some of the points of the proposal but not the accuracy of the statement made by one of the bills authors that "our nation's health care system was broken before Obamacare."
While this bill does address some issues of importance to physicians, it is certainly disappointing that this bill does not address the Sustainable Growth Rate formula (SGR). This looming threat of a 20% or more cut in physician reimbursement will do more harm to patient access and care than any other aspect addressed in this bill. Unfortunately, physicians rarely advocate at the federal level for themselves or their patients. Perhaps, with the introduction of this bill, it is the time to start.
Dr. Michael Nelson, FCCP, comments: With a new Congress controlled by Republicans, and given the prior attempts to overturn the Patient Protection and Affordable Care Act (a.k.a. "Obamacare"), it is not surprising that early in this legislative session an alternative plan has been proposed. One could argue some of the points of the proposal but not the accuracy of the statement made by one of the bills authors that "our nation's health care system was broken before Obamacare."
While this bill does address some issues of importance to physicians, it is certainly disappointing that this bill does not address the Sustainable Growth Rate formula (SGR). This looming threat of a 20% or more cut in physician reimbursement will do more harm to patient access and care than any other aspect addressed in this bill. Unfortunately, physicians rarely advocate at the federal level for themselves or their patients. Perhaps, with the introduction of this bill, it is the time to start.
Three Republican lawmakers are proposing an alternative to the Affordable Care Act that would undo the controversial individual and employer mandates, cap medical liability damages, and offer a slimmed-down set of consumer insurance protections.
Sen. Orrin Hatch (R-Utah), chairman of the Senate Finance Committee; Rep. Fred Upton (R-Mich.), chairman of the House Energy and Commerce Committee; and Sen. Richard Burr (R-N.C.), a member of the Senate Finance Committee, proposed on Feb. 5 the Patient Choice, Affordability, Responsibility, and Empowerment (CARE) Act to repeal and replace the current health law.
“Our nation’s health care system was broken before Obamacare, and the President’s health care debacle has only made things worse,” Sen. Burr said in a statement. “The Patient CARE Act repeals Obamacare and addresses the fundamental cost drivers that Obamacare failed to address. We can lower costs and expand access to quality coverage and care by empowering individuals and their families to make their own health care decisions, rather than having the federal government make those decisions for them.”
The proposal – which came in the form of a 9-page outline – was unveiled just days after the House passed a bill to repeal the ACA by a vote of 239 to 186. While the House has voted numerous times to repeal the health law, this is the first time that the bill might actually be considered in the Senate, since control of that chamber has shifted to the Republicans.
Sen. Hatch and other GOP lawmakers offered a similar replacement proposal last year.
The Patient CARE Act outlines some federal medical liability reforms, including a cap on noneconomic damages and limits on attorneys’ fees. It also seeks to encourage new models for resolving disputes on the state level, such as expert panels to evaluate injury claims and administrative health courts.
The proposal offers a more limited range of consumer insurance protections than does the ACA, including:
• Adopting an age rating ratio of 5-1 for premiums, which would limit plans from charging older individuals any more than five times what a younger person pays. Under the ACA, the age rating ratio is 3-1.
• Banning the use of lifetime dollar limits on health coverage.
• Allowing states to opt out of the ACA’s dependent coverage provision, which lets younger adults stay on their parents’ health plans up to age 26.
• Providing guaranteed renewability of health plans regardless of an individual’s health status. Health plans would be able to cancel coverage only in cases of fraud, misrepresentation by a consumer, or failure to pay premiums.
• Banning denials of coverage based on preexisting medical conditions as long as the individual has been continuously covered with at least a catastrophic plan for 18 months. The proposal includes a one-time open enrollment for people currently uninsured.
The Patient CARE Act would provide federal tax subsidies to purchase insurance to individuals with annual incomes of up to 300% of the federal poverty level. The amount of the tax credit would decrease between 200% and 300% percent of poverty and would be age-adjusted with older individuals receiving a larger subsidy.
The proposal would change the tax treatment of employer-sponsored health insurance by capping the tax exclusion for health benefits at $12,000 for individuals and $30,000 for families. That means that workers would pay federal income taxes on benefits above those thresholds.
Within the Medicaid program, the Patient CARE Act seeks to provide states with a capped amount of federal funds that would “follow the patient” based on health status, age, and life circumstances. Some Medicaid participants would also have the option of using their federal tax credits to purchase private coverage.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Three Republican lawmakers are proposing an alternative to the Affordable Care Act that would undo the controversial individual and employer mandates, cap medical liability damages, and offer a slimmed-down set of consumer insurance protections.
Sen. Orrin Hatch (R-Utah), chairman of the Senate Finance Committee; Rep. Fred Upton (R-Mich.), chairman of the House Energy and Commerce Committee; and Sen. Richard Burr (R-N.C.), a member of the Senate Finance Committee, proposed on Feb. 5 the Patient Choice, Affordability, Responsibility, and Empowerment (CARE) Act to repeal and replace the current health law.
“Our nation’s health care system was broken before Obamacare, and the President’s health care debacle has only made things worse,” Sen. Burr said in a statement. “The Patient CARE Act repeals Obamacare and addresses the fundamental cost drivers that Obamacare failed to address. We can lower costs and expand access to quality coverage and care by empowering individuals and their families to make their own health care decisions, rather than having the federal government make those decisions for them.”
The proposal – which came in the form of a 9-page outline – was unveiled just days after the House passed a bill to repeal the ACA by a vote of 239 to 186. While the House has voted numerous times to repeal the health law, this is the first time that the bill might actually be considered in the Senate, since control of that chamber has shifted to the Republicans.
Sen. Hatch and other GOP lawmakers offered a similar replacement proposal last year.
The Patient CARE Act outlines some federal medical liability reforms, including a cap on noneconomic damages and limits on attorneys’ fees. It also seeks to encourage new models for resolving disputes on the state level, such as expert panels to evaluate injury claims and administrative health courts.
The proposal offers a more limited range of consumer insurance protections than does the ACA, including:
• Adopting an age rating ratio of 5-1 for premiums, which would limit plans from charging older individuals any more than five times what a younger person pays. Under the ACA, the age rating ratio is 3-1.
• Banning the use of lifetime dollar limits on health coverage.
• Allowing states to opt out of the ACA’s dependent coverage provision, which lets younger adults stay on their parents’ health plans up to age 26.
• Providing guaranteed renewability of health plans regardless of an individual’s health status. Health plans would be able to cancel coverage only in cases of fraud, misrepresentation by a consumer, or failure to pay premiums.
• Banning denials of coverage based on preexisting medical conditions as long as the individual has been continuously covered with at least a catastrophic plan for 18 months. The proposal includes a one-time open enrollment for people currently uninsured.
The Patient CARE Act would provide federal tax subsidies to purchase insurance to individuals with annual incomes of up to 300% of the federal poverty level. The amount of the tax credit would decrease between 200% and 300% percent of poverty and would be age-adjusted with older individuals receiving a larger subsidy.
The proposal would change the tax treatment of employer-sponsored health insurance by capping the tax exclusion for health benefits at $12,000 for individuals and $30,000 for families. That means that workers would pay federal income taxes on benefits above those thresholds.
Within the Medicaid program, the Patient CARE Act seeks to provide states with a capped amount of federal funds that would “follow the patient” based on health status, age, and life circumstances. Some Medicaid participants would also have the option of using their federal tax credits to purchase private coverage.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Feds award $2.4 million to fund pregnancy exposure hotline, counseling
The MotherToBaby network, which provides free education and counseling about drug exposure during pregnancy, is getting a funding infusion, thanks to a $2.4-million federal grant.
The money is part of a 2-year cooperative agreement between the Health Resources and Services Administration’s Maternal and Child Health Bureau and the Organization of Teratology Information Specialists, which operates the MotherToBaby network.
The new money will allow the nonprofit group to expand access to a number of its services, including its toll-free hotline, website, and in-person counseling program.
The MotherToBaby network includes 14 sites at universities and hospitals around the United States where women can receive free, evidence-based, personalized risk assessments related to their exposure to a number of prescription and over-the-counter drugs during pregnancy and breastfeeding. The toll-free hotline (1-866-626-6847) connects women and health care providers to teratogen information specialists, while the website includes fact sheets on medications and other exposures.
“Before this funding opportunity, we were in danger of closing some of the services providing critical exposure counseling to health care providers and the general public,” Dr. Kenneth Lyons Jones, a past president of MotherToBaby, said in an interview. “Not only does the funding from HRSA make it possible for our 14 services to continue providing free and in-depth personalized risk assessments, but also to conduct even more outreach efforts across all 50 states.”
The group plans to use the funding specifically to reach out to women in Spanish-speaking communities. They estimate that more than 100,000 women and their health care providers seek information about birth-defect prevention from MotherToBaby each year. With the new federal support, they are hoping to increase that number two-fold over the next 2 years, Dr. Jones said.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
The MotherToBaby network, which provides free education and counseling about drug exposure during pregnancy, is getting a funding infusion, thanks to a $2.4-million federal grant.
The money is part of a 2-year cooperative agreement between the Health Resources and Services Administration’s Maternal and Child Health Bureau and the Organization of Teratology Information Specialists, which operates the MotherToBaby network.
The new money will allow the nonprofit group to expand access to a number of its services, including its toll-free hotline, website, and in-person counseling program.
The MotherToBaby network includes 14 sites at universities and hospitals around the United States where women can receive free, evidence-based, personalized risk assessments related to their exposure to a number of prescription and over-the-counter drugs during pregnancy and breastfeeding. The toll-free hotline (1-866-626-6847) connects women and health care providers to teratogen information specialists, while the website includes fact sheets on medications and other exposures.
“Before this funding opportunity, we were in danger of closing some of the services providing critical exposure counseling to health care providers and the general public,” Dr. Kenneth Lyons Jones, a past president of MotherToBaby, said in an interview. “Not only does the funding from HRSA make it possible for our 14 services to continue providing free and in-depth personalized risk assessments, but also to conduct even more outreach efforts across all 50 states.”
The group plans to use the funding specifically to reach out to women in Spanish-speaking communities. They estimate that more than 100,000 women and their health care providers seek information about birth-defect prevention from MotherToBaby each year. With the new federal support, they are hoping to increase that number two-fold over the next 2 years, Dr. Jones said.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
The MotherToBaby network, which provides free education and counseling about drug exposure during pregnancy, is getting a funding infusion, thanks to a $2.4-million federal grant.
The money is part of a 2-year cooperative agreement between the Health Resources and Services Administration’s Maternal and Child Health Bureau and the Organization of Teratology Information Specialists, which operates the MotherToBaby network.
The new money will allow the nonprofit group to expand access to a number of its services, including its toll-free hotline, website, and in-person counseling program.
The MotherToBaby network includes 14 sites at universities and hospitals around the United States where women can receive free, evidence-based, personalized risk assessments related to their exposure to a number of prescription and over-the-counter drugs during pregnancy and breastfeeding. The toll-free hotline (1-866-626-6847) connects women and health care providers to teratogen information specialists, while the website includes fact sheets on medications and other exposures.
“Before this funding opportunity, we were in danger of closing some of the services providing critical exposure counseling to health care providers and the general public,” Dr. Kenneth Lyons Jones, a past president of MotherToBaby, said in an interview. “Not only does the funding from HRSA make it possible for our 14 services to continue providing free and in-depth personalized risk assessments, but also to conduct even more outreach efforts across all 50 states.”
The group plans to use the funding specifically to reach out to women in Spanish-speaking communities. They estimate that more than 100,000 women and their health care providers seek information about birth-defect prevention from MotherToBaby each year. With the new federal support, they are hoping to increase that number two-fold over the next 2 years, Dr. Jones said.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Few ACA marketplaces offer plans with abortion coverage
More than half of reproductive-age women who are eligible for tax credits through the Affordable Care Act marketplaces can’t buy a health plan that covers abortion, either because that coverage is banned in their state or it’s simply not offered.
In a new analysis of ACA health plans available in 2015, the Kaiser Family Foundation found that 1.76 million reproductive-age women live in states that have enacted laws banning abortion coverage through health plans sold on the marketplace. Another 123,000 women live in states where there is no ban, but no health plans offer the coverage. That leaves about 1.26 million reproductive-age women whose incomes are low enough to qualify for insurance subsidies with access to health plans that offer abortion.
Overall, 24 states have enacted bans or restrictions on abortion coverage within ACA marketplace plans, and 7 states have no restrictions but the coverage is still not available.
Researchers with the Kaiser Family Foundation said that it is unclear why some ACA health plans do not offer abortion coverage even in states where there are no restrictions. However, they speculated that the complexity of the ACA’s abortion rules could be a factor.
Under the 2010 health law, federal funds are not allowed to be used to pay for abortions, and states have the authority to enact additional bans and restrictions on whether plans can offer the coverage. For those states where bans are not in place, the health plans must collect an additional fee for abortion coverage and keep this funding separate from federal dollars. Aside from the extra administrative work, these plans must also meet additional reporting requirements and undergo audits.
More than half of reproductive-age women who are eligible for tax credits through the Affordable Care Act marketplaces can’t buy a health plan that covers abortion, either because that coverage is banned in their state or it’s simply not offered.
In a new analysis of ACA health plans available in 2015, the Kaiser Family Foundation found that 1.76 million reproductive-age women live in states that have enacted laws banning abortion coverage through health plans sold on the marketplace. Another 123,000 women live in states where there is no ban, but no health plans offer the coverage. That leaves about 1.26 million reproductive-age women whose incomes are low enough to qualify for insurance subsidies with access to health plans that offer abortion.
Overall, 24 states have enacted bans or restrictions on abortion coverage within ACA marketplace plans, and 7 states have no restrictions but the coverage is still not available.
Researchers with the Kaiser Family Foundation said that it is unclear why some ACA health plans do not offer abortion coverage even in states where there are no restrictions. However, they speculated that the complexity of the ACA’s abortion rules could be a factor.
Under the 2010 health law, federal funds are not allowed to be used to pay for abortions, and states have the authority to enact additional bans and restrictions on whether plans can offer the coverage. For those states where bans are not in place, the health plans must collect an additional fee for abortion coverage and keep this funding separate from federal dollars. Aside from the extra administrative work, these plans must also meet additional reporting requirements and undergo audits.
More than half of reproductive-age women who are eligible for tax credits through the Affordable Care Act marketplaces can’t buy a health plan that covers abortion, either because that coverage is banned in their state or it’s simply not offered.
In a new analysis of ACA health plans available in 2015, the Kaiser Family Foundation found that 1.76 million reproductive-age women live in states that have enacted laws banning abortion coverage through health plans sold on the marketplace. Another 123,000 women live in states where there is no ban, but no health plans offer the coverage. That leaves about 1.26 million reproductive-age women whose incomes are low enough to qualify for insurance subsidies with access to health plans that offer abortion.
Overall, 24 states have enacted bans or restrictions on abortion coverage within ACA marketplace plans, and 7 states have no restrictions but the coverage is still not available.
Researchers with the Kaiser Family Foundation said that it is unclear why some ACA health plans do not offer abortion coverage even in states where there are no restrictions. However, they speculated that the complexity of the ACA’s abortion rules could be a factor.
Under the 2010 health law, federal funds are not allowed to be used to pay for abortions, and states have the authority to enact additional bans and restrictions on whether plans can offer the coverage. For those states where bans are not in place, the health plans must collect an additional fee for abortion coverage and keep this funding separate from federal dollars. Aside from the extra administrative work, these plans must also meet additional reporting requirements and undergo audits.




















