User login
Feds Release Quality Data on Diabetes, Heart Disease, Infections
Medicare officials have released a slew of new data demonstrating clinicians’ and hospitals’ performance on quality measures related to diabetes, cardiovascular care, and hospital-acquired infections and injuries.
The quality data were posted on Medicare’s Physician Compare and Hospital Compare websites, which aim to provide consumers with the information they need to help them select physicians and other health care providers. The information is also available on data.medicare.gov.
“The Compare sites empower consumers with information to help with health care decisions, encourage providers to strive for higher levels of quality, drive overall health system improvement,” Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Center for Medicare & Medicaid Services, wrote in a blog post.
For physicians, CMS is posting four measures related to diabetes and heart disease: controlling hemoglobin A1c (less than 8%); controlling blood pressure; prescribing aspirin to patients with diabetes and ischemic vascular disease; and prescribing ACE inhibitors or angiotensin receptor blockers for patients with coronary artery disease and diabetes or left ventricular systolic dysfunction.
The data come from 139 physician group practices, 214 shared savings program accountable care organizations, and 23 Pioneer ACOs.
To make the data more user-friendly, CMS uses stars, followed by a percentage score, to show group performance on individual measures. For instance, if a practice scored 80% on a measure, four stars would be shown along with the 80% score.
This is the second time that CMS officials have added quality data to Physician Compare – the first posting was in February 2014. CMS plans to expand the number of quality measures and the number of providers who are listed on the website. By late 2015, CMS plans to post quality data for group practices of all sizes and some data on individual physicians.
For hospitals, CMS posted performance on reducing hospital-acquired conditions, including central line–associated bloodstream infections, catheter-associated urinary tract infections, pressure ulcers, and accidental punctures and lacerations.
The agency also added data from its Hospital Readmissions Reduction Program, including 30-day readmission rates following elective and primary total hip and/or total knee replacement and the 30-day rate of unplanned readmission for chronic obstructive pulmonary disease.
CMS also released data on payment adjustments made as part of the 2015 Hospital Value-Based Purchasing Program, which ties payment to performance on certain quality measures. In fiscal year 2015 – the third year of the program – 1,714 hospitals will see their payments go up as a result of bonus payments from the program, compared with 1,375 that will see their payments decline, according to CMS.
Medicare officials have released a slew of new data demonstrating clinicians’ and hospitals’ performance on quality measures related to diabetes, cardiovascular care, and hospital-acquired infections and injuries.
The quality data were posted on Medicare’s Physician Compare and Hospital Compare websites, which aim to provide consumers with the information they need to help them select physicians and other health care providers. The information is also available on data.medicare.gov.
“The Compare sites empower consumers with information to help with health care decisions, encourage providers to strive for higher levels of quality, drive overall health system improvement,” Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Center for Medicare & Medicaid Services, wrote in a blog post.
For physicians, CMS is posting four measures related to diabetes and heart disease: controlling hemoglobin A1c (less than 8%); controlling blood pressure; prescribing aspirin to patients with diabetes and ischemic vascular disease; and prescribing ACE inhibitors or angiotensin receptor blockers for patients with coronary artery disease and diabetes or left ventricular systolic dysfunction.
The data come from 139 physician group practices, 214 shared savings program accountable care organizations, and 23 Pioneer ACOs.
To make the data more user-friendly, CMS uses stars, followed by a percentage score, to show group performance on individual measures. For instance, if a practice scored 80% on a measure, four stars would be shown along with the 80% score.
This is the second time that CMS officials have added quality data to Physician Compare – the first posting was in February 2014. CMS plans to expand the number of quality measures and the number of providers who are listed on the website. By late 2015, CMS plans to post quality data for group practices of all sizes and some data on individual physicians.
For hospitals, CMS posted performance on reducing hospital-acquired conditions, including central line–associated bloodstream infections, catheter-associated urinary tract infections, pressure ulcers, and accidental punctures and lacerations.
The agency also added data from its Hospital Readmissions Reduction Program, including 30-day readmission rates following elective and primary total hip and/or total knee replacement and the 30-day rate of unplanned readmission for chronic obstructive pulmonary disease.
CMS also released data on payment adjustments made as part of the 2015 Hospital Value-Based Purchasing Program, which ties payment to performance on certain quality measures. In fiscal year 2015 – the third year of the program – 1,714 hospitals will see their payments go up as a result of bonus payments from the program, compared with 1,375 that will see their payments decline, according to CMS.
Medicare officials have released a slew of new data demonstrating clinicians’ and hospitals’ performance on quality measures related to diabetes, cardiovascular care, and hospital-acquired infections and injuries.
The quality data were posted on Medicare’s Physician Compare and Hospital Compare websites, which aim to provide consumers with the information they need to help them select physicians and other health care providers. The information is also available on data.medicare.gov.
“The Compare sites empower consumers with information to help with health care decisions, encourage providers to strive for higher levels of quality, drive overall health system improvement,” Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Center for Medicare & Medicaid Services, wrote in a blog post.
For physicians, CMS is posting four measures related to diabetes and heart disease: controlling hemoglobin A1c (less than 8%); controlling blood pressure; prescribing aspirin to patients with diabetes and ischemic vascular disease; and prescribing ACE inhibitors or angiotensin receptor blockers for patients with coronary artery disease and diabetes or left ventricular systolic dysfunction.
The data come from 139 physician group practices, 214 shared savings program accountable care organizations, and 23 Pioneer ACOs.
To make the data more user-friendly, CMS uses stars, followed by a percentage score, to show group performance on individual measures. For instance, if a practice scored 80% on a measure, four stars would be shown along with the 80% score.
This is the second time that CMS officials have added quality data to Physician Compare – the first posting was in February 2014. CMS plans to expand the number of quality measures and the number of providers who are listed on the website. By late 2015, CMS plans to post quality data for group practices of all sizes and some data on individual physicians.
For hospitals, CMS posted performance on reducing hospital-acquired conditions, including central line–associated bloodstream infections, catheter-associated urinary tract infections, pressure ulcers, and accidental punctures and lacerations.
The agency also added data from its Hospital Readmissions Reduction Program, including 30-day readmission rates following elective and primary total hip and/or total knee replacement and the 30-day rate of unplanned readmission for chronic obstructive pulmonary disease.
CMS also released data on payment adjustments made as part of the 2015 Hospital Value-Based Purchasing Program, which ties payment to performance on certain quality measures. In fiscal year 2015 – the third year of the program – 1,714 hospitals will see their payments go up as a result of bonus payments from the program, compared with 1,375 that will see their payments decline, according to CMS.
Legislative battles over abortion put doctors in the middle
Legislative battles over abortion could intensify this year, with both state and federal lawmakers eyeing additional restrictions on access to the procedure.
And ob.gyns. are finding themselves in the middle once again, with some opposing legislative interference in the physician-patient relationship and others supporting increased regulation of abortion providers.
Just days after the start of the 114th Congress, lawmakers introduced H.R. 36, the Pain-Capable Unborn Child Protection Act, a bill to ban abortion after 20 weeks’ gestation, citing the existence of fetal pain at that point in development. The bill includes exceptions when an abortion is necessary to save the life of a pregnant woman, or in cases of rape or incest.
And while most state legislatures are just gearing up, experts expect to see significant activity on abortion again this year.
Over the last 4 years, state governments have enacted 231 laws limiting access to abortion, with 26 new laws being passed in 2014, according to an analysis by the Guttmacher Institute.
In 2014, Oklahoma added a requirement that abortion counseling include information on the availability of perinatal hospice when a woman is seeking an abortion because of a fetal abnormality. In Alabama, lawmakers extended the waiting period between counseling and obtaining an abortion from 24 to 48 hours. Meanwhile, Mississippi lawmakers banned abortion at 18 weeks post fertilization.
his year will likely be more active than 2014, said Elizabeth Nash, the senior state issues associate at the Guttmacher Institute, since some state legislatures that had been actively targeting abortion access, such as Texas, did not meet last year, and others had shortened sessions.
In addition, more Republican governors and state legislators are taking office in 2015. Republicans now control both legislative chambers and the governor’s office in 23 states. Debate around H.R. 36 also could spur activity at the state level, she said.
For those states that do pursue abortion legislation in 2015, Ms. Nash said she expects them to build on existing restrictions, such as extending the waiting period between mandated counseling and an abortion.
“States will look at existing restrictions and try to make them more burdensome,” she said.
The movement toward increasing barriers to abortion access has some physicians crying foul.
Dr. Nancy L. Stanwood, the section chief for family planning at Yale University in New Haven, Conn., and the board chair of Physicians for Reproductive Health, said many of these proposals claim to be aimed at making abortion safer, but are really a “wolf in sheep’s clothing” because they delay necessary care, jeopardizing safety.
“As a general rule, all of these restrictions do interfere with the doctor-patient relationship,” she said. “I think it has chilling effects on the entire profession.”
Further, some proposals, such as mandates that physicians use outdated protocols for medical abortions, are contrary to medical evidence, Dr. Stanwood said.
H.R. 36 is one proposal that’s not evidence based, according to Dr. Hal C. Lawrence, executive vice president and CEO of the American Congress of Obstetricians and Gynecologists. There’s no evidence, despite a fair amount of literature, to indicate that a fetus can feel pain at that time, he said.
And the actual number of abortions performed after 20 weeks is very low – less than 1% nationally. These typically involve serious medical complications where the termination of the pregnancy is necessary to save the mother’s life, Dr. Lawrence said. “I don’t think we want to take that therapeutic option away from physicians.”
ACOG has been campaigning against the idea of “legislative interference” for the past few years and enlisting physicians from other specialties in the effort. The American Medical Association, for one, has been vocal about its opposition to “governmental intrusions” into the patient-physician relationship and has called on lawmakers to stay out of decisions about what constitutes medically necessary treatment.
“The ability of physicians to provide appropriate treatment options and have open, honest, confidential communications with their patients is an essential value that must be protected,” said Dr. Robert M. Wah, an ob.gyn. and AMA president.
Dr. Lisa M. Hollier, an ob.gyn. in Houston, said she feels the impact of that intrusion firsthand when she’s with a patient.
“My patients come to me, trusting that I will be completely honest with them, open with them, and counsel them fairly regardless of my personal beliefs on a particular topic,” Dr. Hollier said. “When we have legislatures intruding into that very personal moment between a woman and me, it brings in a third party, and she no longer has the complete confidence that I can tell her everything.”
Texas, in particular, has been a battleground when it comes to abortion access. A 2013 Texas law that requires the state’s abortion clinics to adhere to construction, equipment, and staffing standards similar to those of ambulatory surgery centers is currently being challenged in federal appeals court.
The stakes are high in this case, Dr. Hollier said, because if the law is upheld, many facilities won’t be able to meet the new standards, forcing women to travel longer and spend money on lodging, child care, and missed time at work.
“Functionally, what it does is really limit the patient’s opportunity to get access to the full range of reproductive health services,” she said.
But not all physicians see the increasing regulation of abortion services as a problem. Dr. Gene Rudd, an ob.gyn. and senior vice president of the Christian Medical & Dental Associations, said it’s part of the necessary regulation of medical practice, in the same way that the government ensures that only competent surgeons can perform an appendectomy, he said.
“The claim that there’s interference is a smoke screen,” he said.
What makes the abortion situation unusual and different, he said, is that lawmakers and physicians aren’t dealing with an appendix, but an “early life,” Dr. Rudd said. The issue of how early in that life the government should offer legal protections is a societal issue, he added, and lawmakers have every right to define it, with input from experts on all sides.
Dr. Rudd, who supports H.R. 36, said he expects that the abortion battle will continue in state houses and courthouses around the country until there is some cultural consensus around the issue.
“I think it’s going to be an ongoing issue,” he said.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Legislative battles over abortion could intensify this year, with both state and federal lawmakers eyeing additional restrictions on access to the procedure.
And ob.gyns. are finding themselves in the middle once again, with some opposing legislative interference in the physician-patient relationship and others supporting increased regulation of abortion providers.
Just days after the start of the 114th Congress, lawmakers introduced H.R. 36, the Pain-Capable Unborn Child Protection Act, a bill to ban abortion after 20 weeks’ gestation, citing the existence of fetal pain at that point in development. The bill includes exceptions when an abortion is necessary to save the life of a pregnant woman, or in cases of rape or incest.
And while most state legislatures are just gearing up, experts expect to see significant activity on abortion again this year.
Over the last 4 years, state governments have enacted 231 laws limiting access to abortion, with 26 new laws being passed in 2014, according to an analysis by the Guttmacher Institute.
In 2014, Oklahoma added a requirement that abortion counseling include information on the availability of perinatal hospice when a woman is seeking an abortion because of a fetal abnormality. In Alabama, lawmakers extended the waiting period between counseling and obtaining an abortion from 24 to 48 hours. Meanwhile, Mississippi lawmakers banned abortion at 18 weeks post fertilization.
his year will likely be more active than 2014, said Elizabeth Nash, the senior state issues associate at the Guttmacher Institute, since some state legislatures that had been actively targeting abortion access, such as Texas, did not meet last year, and others had shortened sessions.
In addition, more Republican governors and state legislators are taking office in 2015. Republicans now control both legislative chambers and the governor’s office in 23 states. Debate around H.R. 36 also could spur activity at the state level, she said.
For those states that do pursue abortion legislation in 2015, Ms. Nash said she expects them to build on existing restrictions, such as extending the waiting period between mandated counseling and an abortion.
“States will look at existing restrictions and try to make them more burdensome,” she said.
The movement toward increasing barriers to abortion access has some physicians crying foul.
Dr. Nancy L. Stanwood, the section chief for family planning at Yale University in New Haven, Conn., and the board chair of Physicians for Reproductive Health, said many of these proposals claim to be aimed at making abortion safer, but are really a “wolf in sheep’s clothing” because they delay necessary care, jeopardizing safety.
“As a general rule, all of these restrictions do interfere with the doctor-patient relationship,” she said. “I think it has chilling effects on the entire profession.”
Further, some proposals, such as mandates that physicians use outdated protocols for medical abortions, are contrary to medical evidence, Dr. Stanwood said.
H.R. 36 is one proposal that’s not evidence based, according to Dr. Hal C. Lawrence, executive vice president and CEO of the American Congress of Obstetricians and Gynecologists. There’s no evidence, despite a fair amount of literature, to indicate that a fetus can feel pain at that time, he said.
And the actual number of abortions performed after 20 weeks is very low – less than 1% nationally. These typically involve serious medical complications where the termination of the pregnancy is necessary to save the mother’s life, Dr. Lawrence said. “I don’t think we want to take that therapeutic option away from physicians.”
ACOG has been campaigning against the idea of “legislative interference” for the past few years and enlisting physicians from other specialties in the effort. The American Medical Association, for one, has been vocal about its opposition to “governmental intrusions” into the patient-physician relationship and has called on lawmakers to stay out of decisions about what constitutes medically necessary treatment.
“The ability of physicians to provide appropriate treatment options and have open, honest, confidential communications with their patients is an essential value that must be protected,” said Dr. Robert M. Wah, an ob.gyn. and AMA president.
Dr. Lisa M. Hollier, an ob.gyn. in Houston, said she feels the impact of that intrusion firsthand when she’s with a patient.
“My patients come to me, trusting that I will be completely honest with them, open with them, and counsel them fairly regardless of my personal beliefs on a particular topic,” Dr. Hollier said. “When we have legislatures intruding into that very personal moment between a woman and me, it brings in a third party, and she no longer has the complete confidence that I can tell her everything.”
Texas, in particular, has been a battleground when it comes to abortion access. A 2013 Texas law that requires the state’s abortion clinics to adhere to construction, equipment, and staffing standards similar to those of ambulatory surgery centers is currently being challenged in federal appeals court.
The stakes are high in this case, Dr. Hollier said, because if the law is upheld, many facilities won’t be able to meet the new standards, forcing women to travel longer and spend money on lodging, child care, and missed time at work.
“Functionally, what it does is really limit the patient’s opportunity to get access to the full range of reproductive health services,” she said.
But not all physicians see the increasing regulation of abortion services as a problem. Dr. Gene Rudd, an ob.gyn. and senior vice president of the Christian Medical & Dental Associations, said it’s part of the necessary regulation of medical practice, in the same way that the government ensures that only competent surgeons can perform an appendectomy, he said.
“The claim that there’s interference is a smoke screen,” he said.
What makes the abortion situation unusual and different, he said, is that lawmakers and physicians aren’t dealing with an appendix, but an “early life,” Dr. Rudd said. The issue of how early in that life the government should offer legal protections is a societal issue, he added, and lawmakers have every right to define it, with input from experts on all sides.
Dr. Rudd, who supports H.R. 36, said he expects that the abortion battle will continue in state houses and courthouses around the country until there is some cultural consensus around the issue.
“I think it’s going to be an ongoing issue,” he said.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Legislative battles over abortion could intensify this year, with both state and federal lawmakers eyeing additional restrictions on access to the procedure.
And ob.gyns. are finding themselves in the middle once again, with some opposing legislative interference in the physician-patient relationship and others supporting increased regulation of abortion providers.
Just days after the start of the 114th Congress, lawmakers introduced H.R. 36, the Pain-Capable Unborn Child Protection Act, a bill to ban abortion after 20 weeks’ gestation, citing the existence of fetal pain at that point in development. The bill includes exceptions when an abortion is necessary to save the life of a pregnant woman, or in cases of rape or incest.
And while most state legislatures are just gearing up, experts expect to see significant activity on abortion again this year.
Over the last 4 years, state governments have enacted 231 laws limiting access to abortion, with 26 new laws being passed in 2014, according to an analysis by the Guttmacher Institute.
In 2014, Oklahoma added a requirement that abortion counseling include information on the availability of perinatal hospice when a woman is seeking an abortion because of a fetal abnormality. In Alabama, lawmakers extended the waiting period between counseling and obtaining an abortion from 24 to 48 hours. Meanwhile, Mississippi lawmakers banned abortion at 18 weeks post fertilization.
his year will likely be more active than 2014, said Elizabeth Nash, the senior state issues associate at the Guttmacher Institute, since some state legislatures that had been actively targeting abortion access, such as Texas, did not meet last year, and others had shortened sessions.
In addition, more Republican governors and state legislators are taking office in 2015. Republicans now control both legislative chambers and the governor’s office in 23 states. Debate around H.R. 36 also could spur activity at the state level, she said.
For those states that do pursue abortion legislation in 2015, Ms. Nash said she expects them to build on existing restrictions, such as extending the waiting period between mandated counseling and an abortion.
“States will look at existing restrictions and try to make them more burdensome,” she said.
The movement toward increasing barriers to abortion access has some physicians crying foul.
Dr. Nancy L. Stanwood, the section chief for family planning at Yale University in New Haven, Conn., and the board chair of Physicians for Reproductive Health, said many of these proposals claim to be aimed at making abortion safer, but are really a “wolf in sheep’s clothing” because they delay necessary care, jeopardizing safety.
“As a general rule, all of these restrictions do interfere with the doctor-patient relationship,” she said. “I think it has chilling effects on the entire profession.”
Further, some proposals, such as mandates that physicians use outdated protocols for medical abortions, are contrary to medical evidence, Dr. Stanwood said.
H.R. 36 is one proposal that’s not evidence based, according to Dr. Hal C. Lawrence, executive vice president and CEO of the American Congress of Obstetricians and Gynecologists. There’s no evidence, despite a fair amount of literature, to indicate that a fetus can feel pain at that time, he said.
And the actual number of abortions performed after 20 weeks is very low – less than 1% nationally. These typically involve serious medical complications where the termination of the pregnancy is necessary to save the mother’s life, Dr. Lawrence said. “I don’t think we want to take that therapeutic option away from physicians.”
ACOG has been campaigning against the idea of “legislative interference” for the past few years and enlisting physicians from other specialties in the effort. The American Medical Association, for one, has been vocal about its opposition to “governmental intrusions” into the patient-physician relationship and has called on lawmakers to stay out of decisions about what constitutes medically necessary treatment.
“The ability of physicians to provide appropriate treatment options and have open, honest, confidential communications with their patients is an essential value that must be protected,” said Dr. Robert M. Wah, an ob.gyn. and AMA president.
Dr. Lisa M. Hollier, an ob.gyn. in Houston, said she feels the impact of that intrusion firsthand when she’s with a patient.
“My patients come to me, trusting that I will be completely honest with them, open with them, and counsel them fairly regardless of my personal beliefs on a particular topic,” Dr. Hollier said. “When we have legislatures intruding into that very personal moment between a woman and me, it brings in a third party, and she no longer has the complete confidence that I can tell her everything.”
Texas, in particular, has been a battleground when it comes to abortion access. A 2013 Texas law that requires the state’s abortion clinics to adhere to construction, equipment, and staffing standards similar to those of ambulatory surgery centers is currently being challenged in federal appeals court.
The stakes are high in this case, Dr. Hollier said, because if the law is upheld, many facilities won’t be able to meet the new standards, forcing women to travel longer and spend money on lodging, child care, and missed time at work.
“Functionally, what it does is really limit the patient’s opportunity to get access to the full range of reproductive health services,” she said.
But not all physicians see the increasing regulation of abortion services as a problem. Dr. Gene Rudd, an ob.gyn. and senior vice president of the Christian Medical & Dental Associations, said it’s part of the necessary regulation of medical practice, in the same way that the government ensures that only competent surgeons can perform an appendectomy, he said.
“The claim that there’s interference is a smoke screen,” he said.
What makes the abortion situation unusual and different, he said, is that lawmakers and physicians aren’t dealing with an appendix, but an “early life,” Dr. Rudd said. The issue of how early in that life the government should offer legal protections is a societal issue, he added, and lawmakers have every right to define it, with input from experts on all sides.
Dr. Rudd, who supports H.R. 36, said he expects that the abortion battle will continue in state houses and courthouses around the country until there is some cultural consensus around the issue.
“I think it’s going to be an ongoing issue,” he said.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
FDA: No new recommendations for pain meds in pregnancy
Physicians seeking greater clarity about the safe prescribing of pain medications during pregnancy won’t get it from the Food and Drug Administration.
In a safety announcement issued Jan. 9, the FDA informed physicians and patients that it was unable to make any new recommendations about the use of nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and acetaminophen in pregnant women because the existing medical literature is “too limited.”
FDA officials advised physicians to continue to talk with patients about the risks and benefits of analgesics during pregnancy and to follow recommendations in current drug labels for use during pregnancy. For example, current labeling states that NSAIDs should not be used in the third trimester because of the risk of premature closure of the ductus arteriosus in the fetus.
The agency reviewed the medical literature following safety concerns about the use of both over-the-counter and prescription pain medication by pregnant women. The FDA specifically considered prescription NSAIDs and the risk of miscarriage in the first half of pregnancy; opioids and the risk of birth defects following first trimester use; and over-the-counter and prescription acetaminophen use and the risk of attention deficit hyperactivity disorder.
Some of the studies had potential limitations in their designs, while in other cases the accumulated studies on a topic had conflicting results, according to the FDA. “As a result, our recommendations on how pain medications are used during pregnancy will remain the same at this time,” FDA officials wrote in the safety announcement.
Agency officials said they plan to continue to monitor the use of pain medication in pregnant women and will update the public as new safety data becomes available.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Physicians seeking greater clarity about the safe prescribing of pain medications during pregnancy won’t get it from the Food and Drug Administration.
In a safety announcement issued Jan. 9, the FDA informed physicians and patients that it was unable to make any new recommendations about the use of nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and acetaminophen in pregnant women because the existing medical literature is “too limited.”
FDA officials advised physicians to continue to talk with patients about the risks and benefits of analgesics during pregnancy and to follow recommendations in current drug labels for use during pregnancy. For example, current labeling states that NSAIDs should not be used in the third trimester because of the risk of premature closure of the ductus arteriosus in the fetus.
The agency reviewed the medical literature following safety concerns about the use of both over-the-counter and prescription pain medication by pregnant women. The FDA specifically considered prescription NSAIDs and the risk of miscarriage in the first half of pregnancy; opioids and the risk of birth defects following first trimester use; and over-the-counter and prescription acetaminophen use and the risk of attention deficit hyperactivity disorder.
Some of the studies had potential limitations in their designs, while in other cases the accumulated studies on a topic had conflicting results, according to the FDA. “As a result, our recommendations on how pain medications are used during pregnancy will remain the same at this time,” FDA officials wrote in the safety announcement.
Agency officials said they plan to continue to monitor the use of pain medication in pregnant women and will update the public as new safety data becomes available.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Physicians seeking greater clarity about the safe prescribing of pain medications during pregnancy won’t get it from the Food and Drug Administration.
In a safety announcement issued Jan. 9, the FDA informed physicians and patients that it was unable to make any new recommendations about the use of nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and acetaminophen in pregnant women because the existing medical literature is “too limited.”
FDA officials advised physicians to continue to talk with patients about the risks and benefits of analgesics during pregnancy and to follow recommendations in current drug labels for use during pregnancy. For example, current labeling states that NSAIDs should not be used in the third trimester because of the risk of premature closure of the ductus arteriosus in the fetus.
The agency reviewed the medical literature following safety concerns about the use of both over-the-counter and prescription pain medication by pregnant women. The FDA specifically considered prescription NSAIDs and the risk of miscarriage in the first half of pregnancy; opioids and the risk of birth defects following first trimester use; and over-the-counter and prescription acetaminophen use and the risk of attention deficit hyperactivity disorder.
Some of the studies had potential limitations in their designs, while in other cases the accumulated studies on a topic had conflicting results, according to the FDA. “As a result, our recommendations on how pain medications are used during pregnancy will remain the same at this time,” FDA officials wrote in the safety announcement.
Agency officials said they plan to continue to monitor the use of pain medication in pregnant women and will update the public as new safety data becomes available.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
States passed fewer abortion restrictions in 2014
State legislatures enacted fewer restrictions on abortion during 2014 than in the previous year, but that downward trend is unlikely to continue in the new year, according to an analysis from the Guttmacher Institute.
In 2014, state legislatures enacted only 26 of the 341 abortion restrictions introduced. And the total number of laws was down sharply from the 70 provisions enacted in 2013. The new laws included new counseling requirements before an abortion, longer waiting periods, second trimester abortion bans, and parental consent requirements.
But Elizabeth Nash, the senior state issues associate at the Guttmacher Institute, said the number of restrictive laws only looks small in comparision to the spike in legislative activity over the last 4 years, during which states enacted 231 laws limiting access to abortion.
“The scale has changed somewhat,” she said.
Some state legislatures that have been actively targeting abortion access, such as Texas, did not meet in 2014, and others had shortened sessions.
This year could bring more abortion restrictions, Ms. Nash said, as more Republican governors and state legislators take office. In 23 states, Republicans now control both legislative chambers and the governor’s office. An expected debate at the federal level on a 20-week abortion ban could also drive activity at the state level, she said.
For those states that do pursue abortion legislation in 2015, Ms. Nash said she expects them to build on existing restrictions, such as extending the waiting period between mandated counseling and an abortion.
“States will look at existing restrictions and try to make them more burdensome,” she said.
In 2014, Oklahoma enacted a requirement that abortion counseling include information on the availability perinatal hospice when a woman is seeking an abortion because of a fetal abnormality. In Alabama, lawmakers extended the waiting period between counseling and obtaining an abortion from 24 to 48 hours. Meanwhile, Mississippi lawmakers banned abortion at 18 weeks post-fertilization, citing fetal pain.
But other states took action to protect access to abortion in 2014. Following a U.S. Supreme Court ruling striking down a Massachusetts law providing a 35-foot buffer zone around abortion clinics, that state’s lawmakers enacted a new law establishing a 25-foot buffer zone for up to 8 hours after a police officer issues a dispersal order. Similarly, New Hampshire set a 25-foot buffer zone around abortion clinics. And in Utah, the legislature waived some counseling requirements in cases in which a woman is obtaining an abortion because of a diagnosed fetal impairment.
mschneider@frontlinemedcom.com
Twitter @maryellenny
State legislatures enacted fewer restrictions on abortion during 2014 than in the previous year, but that downward trend is unlikely to continue in the new year, according to an analysis from the Guttmacher Institute.
In 2014, state legislatures enacted only 26 of the 341 abortion restrictions introduced. And the total number of laws was down sharply from the 70 provisions enacted in 2013. The new laws included new counseling requirements before an abortion, longer waiting periods, second trimester abortion bans, and parental consent requirements.
But Elizabeth Nash, the senior state issues associate at the Guttmacher Institute, said the number of restrictive laws only looks small in comparision to the spike in legislative activity over the last 4 years, during which states enacted 231 laws limiting access to abortion.
“The scale has changed somewhat,” she said.
Some state legislatures that have been actively targeting abortion access, such as Texas, did not meet in 2014, and others had shortened sessions.
This year could bring more abortion restrictions, Ms. Nash said, as more Republican governors and state legislators take office. In 23 states, Republicans now control both legislative chambers and the governor’s office. An expected debate at the federal level on a 20-week abortion ban could also drive activity at the state level, she said.
For those states that do pursue abortion legislation in 2015, Ms. Nash said she expects them to build on existing restrictions, such as extending the waiting period between mandated counseling and an abortion.
“States will look at existing restrictions and try to make them more burdensome,” she said.
In 2014, Oklahoma enacted a requirement that abortion counseling include information on the availability perinatal hospice when a woman is seeking an abortion because of a fetal abnormality. In Alabama, lawmakers extended the waiting period between counseling and obtaining an abortion from 24 to 48 hours. Meanwhile, Mississippi lawmakers banned abortion at 18 weeks post-fertilization, citing fetal pain.
But other states took action to protect access to abortion in 2014. Following a U.S. Supreme Court ruling striking down a Massachusetts law providing a 35-foot buffer zone around abortion clinics, that state’s lawmakers enacted a new law establishing a 25-foot buffer zone for up to 8 hours after a police officer issues a dispersal order. Similarly, New Hampshire set a 25-foot buffer zone around abortion clinics. And in Utah, the legislature waived some counseling requirements in cases in which a woman is obtaining an abortion because of a diagnosed fetal impairment.
mschneider@frontlinemedcom.com
Twitter @maryellenny
State legislatures enacted fewer restrictions on abortion during 2014 than in the previous year, but that downward trend is unlikely to continue in the new year, according to an analysis from the Guttmacher Institute.
In 2014, state legislatures enacted only 26 of the 341 abortion restrictions introduced. And the total number of laws was down sharply from the 70 provisions enacted in 2013. The new laws included new counseling requirements before an abortion, longer waiting periods, second trimester abortion bans, and parental consent requirements.
But Elizabeth Nash, the senior state issues associate at the Guttmacher Institute, said the number of restrictive laws only looks small in comparision to the spike in legislative activity over the last 4 years, during which states enacted 231 laws limiting access to abortion.
“The scale has changed somewhat,” she said.
Some state legislatures that have been actively targeting abortion access, such as Texas, did not meet in 2014, and others had shortened sessions.
This year could bring more abortion restrictions, Ms. Nash said, as more Republican governors and state legislators take office. In 23 states, Republicans now control both legislative chambers and the governor’s office. An expected debate at the federal level on a 20-week abortion ban could also drive activity at the state level, she said.
For those states that do pursue abortion legislation in 2015, Ms. Nash said she expects them to build on existing restrictions, such as extending the waiting period between mandated counseling and an abortion.
“States will look at existing restrictions and try to make them more burdensome,” she said.
In 2014, Oklahoma enacted a requirement that abortion counseling include information on the availability perinatal hospice when a woman is seeking an abortion because of a fetal abnormality. In Alabama, lawmakers extended the waiting period between counseling and obtaining an abortion from 24 to 48 hours. Meanwhile, Mississippi lawmakers banned abortion at 18 weeks post-fertilization, citing fetal pain.
But other states took action to protect access to abortion in 2014. Following a U.S. Supreme Court ruling striking down a Massachusetts law providing a 35-foot buffer zone around abortion clinics, that state’s lawmakers enacted a new law establishing a 25-foot buffer zone for up to 8 hours after a police officer issues a dispersal order. Similarly, New Hampshire set a 25-foot buffer zone around abortion clinics. And in Utah, the legislature waived some counseling requirements in cases in which a woman is obtaining an abortion because of a diagnosed fetal impairment.
mschneider@frontlinemedcom.com
Twitter @maryellenny
Medicare @ 50: Popular with patients; problematic for physicians
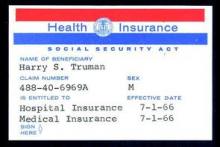
When President Lyndon B. Johnson signed Medicare into law on July 30, 1965, he vowed that the program would give seniors access to the “healing miracle of modern medicine” and save them from exhausting their savings when they became ill.
For the most part, the program has delivered on those bold promises. Americans over age 65 years are living longer, healthier lives, and they are doing so without fear that a trip to the hospital will lead to bankruptcy. That security has only increased over time, as Congress added prescription drug coverage and most recently, free preventive care. In 1972, the Medicare program was extended to the long-term disabled and those with end stage renal disease.
Medicare “fundamentally changed the way we thought about health in our nation for our seniors,” said Dr. Georges C. Benjamin, executive director of the American Public Health Association. “This probably was the most important tool to lift seniors out of poverty. The economic benefit of this, in addition to the health benefit, was enormous.”
Along with coverage of hospital stays and physician services for seniors under Medicare, the Social Security Act Amendments of 1965 also created Medicaid, a voluntary federal-state partnership to provide medical care and long-term care services to low-income Americans.
Changing medical practice
When combined with the Civil Rights Act of 1964, Medicare desegregated all hospitals that participated in the program. Prior to the start of Medicare on July 1, 1966, a large number of hospitals around the country were still racially segregated in some manner. In many areas of the South, a separate hospital system served the black community and were the only places where black physicians could train and practice (Milbank Q. 2005; 83: 247-69). But in a matter of months, hospitals across the country integrated their facilities and staff in a relative peaceful manner, according to a study conducted by the Commonwealth Fund.
“Now, physicians of color could not be kept out of hospitals as a matter of policy,” Dr. Benjamin said. “It dramatically improved practice opportunities for physicians and access to care opportunities for patients.”
Stuart Guterman, Ph.D., vice president for Medicare and cost control at the Commonwealth Fund, said it’s one of the lesser-known elements of Medicare’s history that the law became an impetus to overcoming racial barriers for both patients and physicians.
Changing payment incentives
Medicare payments opened up a significant new stream of revenue for hospitals that made desegregation more palatable. But hospitals weren’t the only ones who benefited financially from the new program.
Despite the American Medical Association’s fight against the creation of Medicare, during which officials famously decried the program as “socialized medicine,” physicians were financial winners under the new law, at least at first.
Much like hospitals, doctors got paid for the first time for treating patients who they had previously seen as charity care. And, in those early years of the Medicare program, the government paid on a charge basis. The result was that Medicare spending was quickly out of control.
Cost controls were added first for hospital care. In 1983, Medicare adopted the inpatient hospital prospective payment system, which replaced hospitals’ cost-based payments with the diagnosis-related group (DRG) system.
“Changing the notion of what hospitals did from each individual service or each individual day to the hospital stay, really changed the way hospital care was looked at,” Dr. Guterman said.
It took somewhat longer for federal health officials to tackle payment on the physician side. Throughout the 1980s, Congress froze physician payment rates in an effort to address rising costs. In 1984, Congress established the Participating Physicians’ Program, which required physicians to accept assignment for all Medicare patients and services rather than on a service-by-service basis. It also barred balance billing of Medicare beneficiaries.
In 1989, Congress made the most significant change yet to physician payment, creating the Resource-Based Relative Value Scale (RBRVS) under the Omnibus Budget Reconciliation Act. Medicare officials used the new RBRVS to establish a standardized physician payment schedule in 1992. Under the new system, payments were determined by calculating the costs of physician work, practice expenses, and professional liability insurance. Payments are then adjusted by a conversion factor and geographic cost differences.
“The impact of the fee schedule all depends on where you sit,” said Paul B. Ginsburg, Ph.D., director of health policy at the Schaeffer Center for Health Policy and Economics at the University of Southern California.
The fee schedule was positive for primary care physicians at first, but a flawed updating process over the decades led to differences in Medicare payments by specialty, largely favoring procedural specialists over those who billed for evaluation and management services.
But Dr. Ginsburg said Medicare is now on the cusp of an even more important payment change as federal officials begin to move away from fee-for-service and toward payment approaches that emphasize quality and value.
While some new payment model experiments have been promising, the attempts by the Centers for Medicare & Medicaid Services have been “fumbling,” Dr. Ginsburg said.
Changing physician satisfaction
Medicare beneficiaries are typically happier with their health coverage than individuals enrolled in private, employer-sponsored insurance and are less worried about financial barriers to care, Dr. Guterman said.
“I think it’s fair to say that it’s one of the more popular federal programs ever,” he said. “You hear people frequently talking about how touchy it is to make any changes to the program because people are very wary of having that benefit diluted.”
That’s not the case for physicians.
“The physicians I’ve talked to over the last 2 years feel like they’re drowning in red tape,” said Dr. Austin King, president of the Texas Medical Association and a head and neck surgeon in Abilene.
The result is that physicians are becoming employees in large physician practices or hospitals, or they are moving to set up boutique practices, Dr. King said. “Right now, the physicians are not real happy with the program.”
Dr. King predicted that physicians will continue to move out of the program, creating patient access issues, unless Congress gives them a way to recoup their costs, such as through the practice of balance billing.
Resolving issues like the looming annual cuts from the Sustainable Growth Rate formula and eliminating the Affordable Care Act’s Independent Payment Advisory Board would put some predictability back into the system, Dr. King said, adding that it’s not enough because it would still leave the numerous regulatory requirements, which many physicians “agonize” over.
It’s that kind of agony that keeps Dr. Jane Orient, a general internist in Tucson, Ariz., from participating in Medicare. Dr. Orient opted out of the program in 1990, around the time that Medicare began requiring that physicians file claims for payment. Previously, patients could pay her directly for services and be reimbursed by Medicare.
“I decided I just could not do that,” said Dr. Orient, executive director of the Association of American Physicians and Surgeons. “For me to file the claim and figure out what all those E&M guidelines meant, was just impossible. I certainly couldn’t do it with the staff I had.”
The fundamental problem, said Rep. Michael C. Burgess (R-Texas), cochair of the Congressional Health Caucus and an ob.gyn., is that patients get their care covered at a price they can afford, while Medicare’s payment to physicians doesn’t cover the cost of care.
“What has always been a bad situation is getting worse and worse with every passing year,” Rep. Burgess said.
Rep. Phil Roe (R-Tenn.), cochair of the GOP Doctors Caucus, said the problem for lawmakers is that they must fix the physician payment system before patient access is significantly affected. How much time do they have?
Rep. Roe, an ob.gyn., said physicians will hang on for as long as they can. But if Medicare continues to cut payments, an access crisis is coming.
If Medicare’s solution to their financing problem is to cut providers, he said, physicians will look for a way out of the program, and that will start with large-scale retirements of older physicians.
“They are all looking for the exit signs now,” Rep. Roe said. 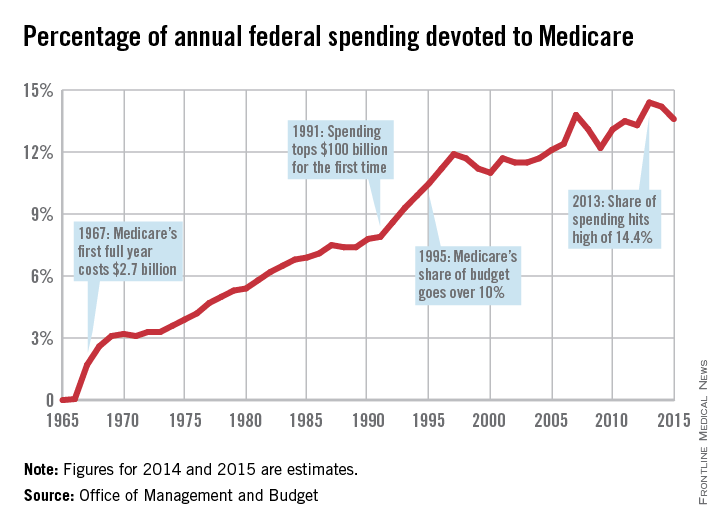
|
This is the first in a series of articles tracing the 50-year history of Medicare and its impact on physicians and patients. Future articles will focus on the public health impact of Medicare, the origins of the Sustainable Growth Rate formula, and the long-term financial viability of the program.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
When President Lyndon B. Johnson signed Medicare into law on July 30, 1965, he vowed that the program would give seniors access to the “healing miracle of modern medicine” and save them from exhausting their savings when they became ill.
For the most part, the program has delivered on those bold promises. Americans over age 65 years are living longer, healthier lives, and they are doing so without fear that a trip to the hospital will lead to bankruptcy. That security has only increased over time, as Congress added prescription drug coverage and most recently, free preventive care. In 1972, the Medicare program was extended to the long-term disabled and those with end stage renal disease.
Medicare “fundamentally changed the way we thought about health in our nation for our seniors,” said Dr. Georges C. Benjamin, executive director of the American Public Health Association. “This probably was the most important tool to lift seniors out of poverty. The economic benefit of this, in addition to the health benefit, was enormous.”
Along with coverage of hospital stays and physician services for seniors under Medicare, the Social Security Act Amendments of 1965 also created Medicaid, a voluntary federal-state partnership to provide medical care and long-term care services to low-income Americans.
Changing medical practice
When combined with the Civil Rights Act of 1964, Medicare desegregated all hospitals that participated in the program. Prior to the start of Medicare on July 1, 1966, a large number of hospitals around the country were still racially segregated in some manner. In many areas of the South, a separate hospital system served the black community and were the only places where black physicians could train and practice (Milbank Q. 2005; 83: 247-69). But in a matter of months, hospitals across the country integrated their facilities and staff in a relative peaceful manner, according to a study conducted by the Commonwealth Fund.
“Now, physicians of color could not be kept out of hospitals as a matter of policy,” Dr. Benjamin said. “It dramatically improved practice opportunities for physicians and access to care opportunities for patients.”
Stuart Guterman, Ph.D., vice president for Medicare and cost control at the Commonwealth Fund, said it’s one of the lesser-known elements of Medicare’s history that the law became an impetus to overcoming racial barriers for both patients and physicians.
Changing payment incentives
Medicare payments opened up a significant new stream of revenue for hospitals that made desegregation more palatable. But hospitals weren’t the only ones who benefited financially from the new program.
Despite the American Medical Association’s fight against the creation of Medicare, during which officials famously decried the program as “socialized medicine,” physicians were financial winners under the new law, at least at first.
Much like hospitals, doctors got paid for the first time for treating patients who they had previously seen as charity care. And, in those early years of the Medicare program, the government paid on a charge basis. The result was that Medicare spending was quickly out of control.
Cost controls were added first for hospital care. In 1983, Medicare adopted the inpatient hospital prospective payment system, which replaced hospitals’ cost-based payments with the diagnosis-related group (DRG) system.
“Changing the notion of what hospitals did from each individual service or each individual day to the hospital stay, really changed the way hospital care was looked at,” Dr. Guterman said.
It took somewhat longer for federal health officials to tackle payment on the physician side. Throughout the 1980s, Congress froze physician payment rates in an effort to address rising costs. In 1984, Congress established the Participating Physicians’ Program, which required physicians to accept assignment for all Medicare patients and services rather than on a service-by-service basis. It also barred balance billing of Medicare beneficiaries.
In 1989, Congress made the most significant change yet to physician payment, creating the Resource-Based Relative Value Scale (RBRVS) under the Omnibus Budget Reconciliation Act. Medicare officials used the new RBRVS to establish a standardized physician payment schedule in 1992. Under the new system, payments were determined by calculating the costs of physician work, practice expenses, and professional liability insurance. Payments are then adjusted by a conversion factor and geographic cost differences.
“The impact of the fee schedule all depends on where you sit,” said Paul B. Ginsburg, Ph.D., director of health policy at the Schaeffer Center for Health Policy and Economics at the University of Southern California.
The fee schedule was positive for primary care physicians at first, but a flawed updating process over the decades led to differences in Medicare payments by specialty, largely favoring procedural specialists over those who billed for evaluation and management services.
But Dr. Ginsburg said Medicare is now on the cusp of an even more important payment change as federal officials begin to move away from fee-for-service and toward payment approaches that emphasize quality and value.
While some new payment model experiments have been promising, the attempts by the Centers for Medicare & Medicaid Services have been “fumbling,” Dr. Ginsburg said.
Changing physician satisfaction
Medicare beneficiaries are typically happier with their health coverage than individuals enrolled in private, employer-sponsored insurance and are less worried about financial barriers to care, Dr. Guterman said.
“I think it’s fair to say that it’s one of the more popular federal programs ever,” he said. “You hear people frequently talking about how touchy it is to make any changes to the program because people are very wary of having that benefit diluted.”
That’s not the case for physicians.
“The physicians I’ve talked to over the last 2 years feel like they’re drowning in red tape,” said Dr. Austin King, president of the Texas Medical Association and a head and neck surgeon in Abilene.
The result is that physicians are becoming employees in large physician practices or hospitals, or they are moving to set up boutique practices, Dr. King said. “Right now, the physicians are not real happy with the program.”
Dr. King predicted that physicians will continue to move out of the program, creating patient access issues, unless Congress gives them a way to recoup their costs, such as through the practice of balance billing.
Resolving issues like the looming annual cuts from the Sustainable Growth Rate formula and eliminating the Affordable Care Act’s Independent Payment Advisory Board would put some predictability back into the system, Dr. King said, adding that it’s not enough because it would still leave the numerous regulatory requirements, which many physicians “agonize” over.
It’s that kind of agony that keeps Dr. Jane Orient, a general internist in Tucson, Ariz., from participating in Medicare. Dr. Orient opted out of the program in 1990, around the time that Medicare began requiring that physicians file claims for payment. Previously, patients could pay her directly for services and be reimbursed by Medicare.
“I decided I just could not do that,” said Dr. Orient, executive director of the Association of American Physicians and Surgeons. “For me to file the claim and figure out what all those E&M guidelines meant, was just impossible. I certainly couldn’t do it with the staff I had.”
The fundamental problem, said Rep. Michael C. Burgess (R-Texas), cochair of the Congressional Health Caucus and an ob.gyn., is that patients get their care covered at a price they can afford, while Medicare’s payment to physicians doesn’t cover the cost of care.
“What has always been a bad situation is getting worse and worse with every passing year,” Rep. Burgess said.
Rep. Phil Roe (R-Tenn.), cochair of the GOP Doctors Caucus, said the problem for lawmakers is that they must fix the physician payment system before patient access is significantly affected. How much time do they have?
Rep. Roe, an ob.gyn., said physicians will hang on for as long as they can. But if Medicare continues to cut payments, an access crisis is coming.
If Medicare’s solution to their financing problem is to cut providers, he said, physicians will look for a way out of the program, and that will start with large-scale retirements of older physicians.
“They are all looking for the exit signs now,” Rep. Roe said. 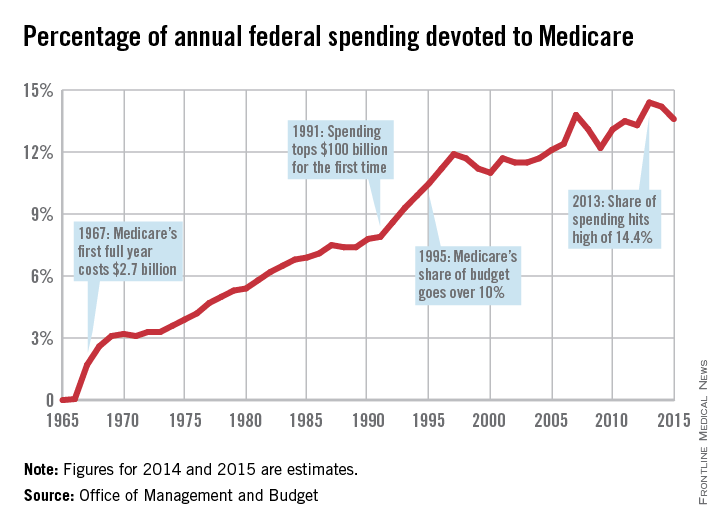
|
This is the first in a series of articles tracing the 50-year history of Medicare and its impact on physicians and patients. Future articles will focus on the public health impact of Medicare, the origins of the Sustainable Growth Rate formula, and the long-term financial viability of the program.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
When President Lyndon B. Johnson signed Medicare into law on July 30, 1965, he vowed that the program would give seniors access to the “healing miracle of modern medicine” and save them from exhausting their savings when they became ill.
For the most part, the program has delivered on those bold promises. Americans over age 65 years are living longer, healthier lives, and they are doing so without fear that a trip to the hospital will lead to bankruptcy. That security has only increased over time, as Congress added prescription drug coverage and most recently, free preventive care. In 1972, the Medicare program was extended to the long-term disabled and those with end stage renal disease.
Medicare “fundamentally changed the way we thought about health in our nation for our seniors,” said Dr. Georges C. Benjamin, executive director of the American Public Health Association. “This probably was the most important tool to lift seniors out of poverty. The economic benefit of this, in addition to the health benefit, was enormous.”
Along with coverage of hospital stays and physician services for seniors under Medicare, the Social Security Act Amendments of 1965 also created Medicaid, a voluntary federal-state partnership to provide medical care and long-term care services to low-income Americans.
Changing medical practice
When combined with the Civil Rights Act of 1964, Medicare desegregated all hospitals that participated in the program. Prior to the start of Medicare on July 1, 1966, a large number of hospitals around the country were still racially segregated in some manner. In many areas of the South, a separate hospital system served the black community and were the only places where black physicians could train and practice (Milbank Q. 2005; 83: 247-69). But in a matter of months, hospitals across the country integrated their facilities and staff in a relative peaceful manner, according to a study conducted by the Commonwealth Fund.
“Now, physicians of color could not be kept out of hospitals as a matter of policy,” Dr. Benjamin said. “It dramatically improved practice opportunities for physicians and access to care opportunities for patients.”
Stuart Guterman, Ph.D., vice president for Medicare and cost control at the Commonwealth Fund, said it’s one of the lesser-known elements of Medicare’s history that the law became an impetus to overcoming racial barriers for both patients and physicians.
Changing payment incentives
Medicare payments opened up a significant new stream of revenue for hospitals that made desegregation more palatable. But hospitals weren’t the only ones who benefited financially from the new program.
Despite the American Medical Association’s fight against the creation of Medicare, during which officials famously decried the program as “socialized medicine,” physicians were financial winners under the new law, at least at first.
Much like hospitals, doctors got paid for the first time for treating patients who they had previously seen as charity care. And, in those early years of the Medicare program, the government paid on a charge basis. The result was that Medicare spending was quickly out of control.
Cost controls were added first for hospital care. In 1983, Medicare adopted the inpatient hospital prospective payment system, which replaced hospitals’ cost-based payments with the diagnosis-related group (DRG) system.
“Changing the notion of what hospitals did from each individual service or each individual day to the hospital stay, really changed the way hospital care was looked at,” Dr. Guterman said.
It took somewhat longer for federal health officials to tackle payment on the physician side. Throughout the 1980s, Congress froze physician payment rates in an effort to address rising costs. In 1984, Congress established the Participating Physicians’ Program, which required physicians to accept assignment for all Medicare patients and services rather than on a service-by-service basis. It also barred balance billing of Medicare beneficiaries.
In 1989, Congress made the most significant change yet to physician payment, creating the Resource-Based Relative Value Scale (RBRVS) under the Omnibus Budget Reconciliation Act. Medicare officials used the new RBRVS to establish a standardized physician payment schedule in 1992. Under the new system, payments were determined by calculating the costs of physician work, practice expenses, and professional liability insurance. Payments are then adjusted by a conversion factor and geographic cost differences.
“The impact of the fee schedule all depends on where you sit,” said Paul B. Ginsburg, Ph.D., director of health policy at the Schaeffer Center for Health Policy and Economics at the University of Southern California.
The fee schedule was positive for primary care physicians at first, but a flawed updating process over the decades led to differences in Medicare payments by specialty, largely favoring procedural specialists over those who billed for evaluation and management services.
But Dr. Ginsburg said Medicare is now on the cusp of an even more important payment change as federal officials begin to move away from fee-for-service and toward payment approaches that emphasize quality and value.
While some new payment model experiments have been promising, the attempts by the Centers for Medicare & Medicaid Services have been “fumbling,” Dr. Ginsburg said.
Changing physician satisfaction
Medicare beneficiaries are typically happier with their health coverage than individuals enrolled in private, employer-sponsored insurance and are less worried about financial barriers to care, Dr. Guterman said.
“I think it’s fair to say that it’s one of the more popular federal programs ever,” he said. “You hear people frequently talking about how touchy it is to make any changes to the program because people are very wary of having that benefit diluted.”
That’s not the case for physicians.
“The physicians I’ve talked to over the last 2 years feel like they’re drowning in red tape,” said Dr. Austin King, president of the Texas Medical Association and a head and neck surgeon in Abilene.
The result is that physicians are becoming employees in large physician practices or hospitals, or they are moving to set up boutique practices, Dr. King said. “Right now, the physicians are not real happy with the program.”
Dr. King predicted that physicians will continue to move out of the program, creating patient access issues, unless Congress gives them a way to recoup their costs, such as through the practice of balance billing.
Resolving issues like the looming annual cuts from the Sustainable Growth Rate formula and eliminating the Affordable Care Act’s Independent Payment Advisory Board would put some predictability back into the system, Dr. King said, adding that it’s not enough because it would still leave the numerous regulatory requirements, which many physicians “agonize” over.
It’s that kind of agony that keeps Dr. Jane Orient, a general internist in Tucson, Ariz., from participating in Medicare. Dr. Orient opted out of the program in 1990, around the time that Medicare began requiring that physicians file claims for payment. Previously, patients could pay her directly for services and be reimbursed by Medicare.
“I decided I just could not do that,” said Dr. Orient, executive director of the Association of American Physicians and Surgeons. “For me to file the claim and figure out what all those E&M guidelines meant, was just impossible. I certainly couldn’t do it with the staff I had.”
The fundamental problem, said Rep. Michael C. Burgess (R-Texas), cochair of the Congressional Health Caucus and an ob.gyn., is that patients get their care covered at a price they can afford, while Medicare’s payment to physicians doesn’t cover the cost of care.
“What has always been a bad situation is getting worse and worse with every passing year,” Rep. Burgess said.
Rep. Phil Roe (R-Tenn.), cochair of the GOP Doctors Caucus, said the problem for lawmakers is that they must fix the physician payment system before patient access is significantly affected. How much time do they have?
Rep. Roe, an ob.gyn., said physicians will hang on for as long as they can. But if Medicare continues to cut payments, an access crisis is coming.
If Medicare’s solution to their financing problem is to cut providers, he said, physicians will look for a way out of the program, and that will start with large-scale retirements of older physicians.
“They are all looking for the exit signs now,” Rep. Roe said. 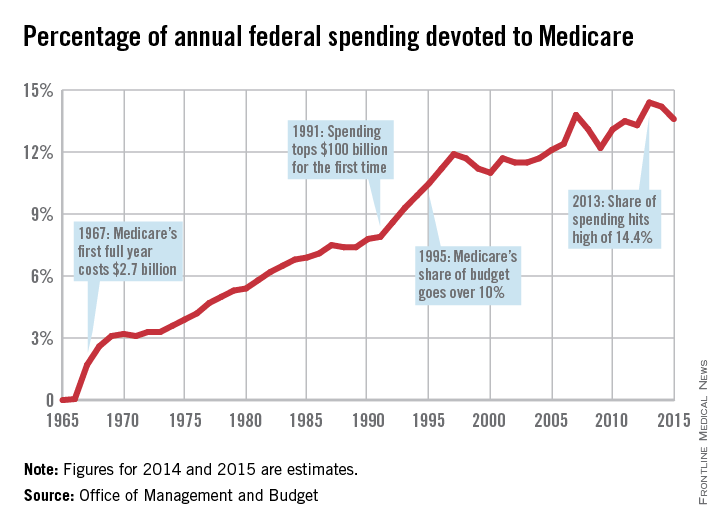
|
This is the first in a series of articles tracing the 50-year history of Medicare and its impact on physicians and patients. Future articles will focus on the public health impact of Medicare, the origins of the Sustainable Growth Rate formula, and the long-term financial viability of the program.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Feds release quality data on diabetes, heart disease, infections
Medicare officials have released a slew of new data demonstrating physicians’ and hospitals’ performance on quality measures related to diabetes, cardiovascular care, and hospital-acquired infections and injuries.
The quality data were posted on Medicare’s Physician Compare and Hospital Compare websites, which aim to provide consumers with the information they need to help them select physicians and other health care providers. The information is also available on data.medicare.gov.
“The Compare sites empower consumers with information to help with health care decisions, encourage providers to strive for higher levels of quality, drive overall health system improvement,” Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Center for Medicare & Medicaid Services, wrote in a blog post.
For physicians, CMS is posting four measures related to diabetes and heart disease: controlling hemoglobin A1c (less than 8%); controlling blood pressure; prescribing aspirin to patients with diabetes and ischemic vascular disease; and prescribing ACE inhibitors or angiotensin receptor blockers for patients with coronary artery disease and diabetes or left ventricular systolic dysfunction.
The data come from 139 physician group practices, 214 shared savings program accountable care organizations, and 23 Pioneer ACOs.
To make the data more user-friendly, CMS uses stars, followed by a percentage score, to show group performance on individual measures. For instance, if a practice scored 80% on a measure, four stars would be shown along with the 80% score.
This is the second time that CMS officials have added quality data to Physician Compare – the first posting was in February 2014. CMS plans to expand the number of quality measures and the number of providers who are listed on the website. By late 2015, CMS plans to post quality data for group practices of all sizes and some data on individual physicians.
For hospitals, CMS posted performance on reducing hospital-acquired conditions, including central line–associated bloodstream infections, catheter-associated urinary tract infections, pressure ulcers, and accidental punctures and lacerations.
The agency also added data from its Hospital Readmissions Reduction Program, including 30-day readmission rates following elective and primary total hip and/or total knee replacement and the 30-day rate of unplanned readmission for chronic obstructive pulmonary disease.
CMS also released data on payment adjustments made as part of the 2015 Hospital Value-Based Purchasing Program, which ties payment to performance on certain quality measures. In fiscal year 2015 – the third year of the program – 1,714 hospitals will see their payments go up as a result of bonus payments from the program, compared with 1,375 that will see their payments decline, according to CMS.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Medicare officials have released a slew of new data demonstrating physicians’ and hospitals’ performance on quality measures related to diabetes, cardiovascular care, and hospital-acquired infections and injuries.
The quality data were posted on Medicare’s Physician Compare and Hospital Compare websites, which aim to provide consumers with the information they need to help them select physicians and other health care providers. The information is also available on data.medicare.gov.
“The Compare sites empower consumers with information to help with health care decisions, encourage providers to strive for higher levels of quality, drive overall health system improvement,” Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Center for Medicare & Medicaid Services, wrote in a blog post.
For physicians, CMS is posting four measures related to diabetes and heart disease: controlling hemoglobin A1c (less than 8%); controlling blood pressure; prescribing aspirin to patients with diabetes and ischemic vascular disease; and prescribing ACE inhibitors or angiotensin receptor blockers for patients with coronary artery disease and diabetes or left ventricular systolic dysfunction.
The data come from 139 physician group practices, 214 shared savings program accountable care organizations, and 23 Pioneer ACOs.
To make the data more user-friendly, CMS uses stars, followed by a percentage score, to show group performance on individual measures. For instance, if a practice scored 80% on a measure, four stars would be shown along with the 80% score.
This is the second time that CMS officials have added quality data to Physician Compare – the first posting was in February 2014. CMS plans to expand the number of quality measures and the number of providers who are listed on the website. By late 2015, CMS plans to post quality data for group practices of all sizes and some data on individual physicians.
For hospitals, CMS posted performance on reducing hospital-acquired conditions, including central line–associated bloodstream infections, catheter-associated urinary tract infections, pressure ulcers, and accidental punctures and lacerations.
The agency also added data from its Hospital Readmissions Reduction Program, including 30-day readmission rates following elective and primary total hip and/or total knee replacement and the 30-day rate of unplanned readmission for chronic obstructive pulmonary disease.
CMS also released data on payment adjustments made as part of the 2015 Hospital Value-Based Purchasing Program, which ties payment to performance on certain quality measures. In fiscal year 2015 – the third year of the program – 1,714 hospitals will see their payments go up as a result of bonus payments from the program, compared with 1,375 that will see their payments decline, according to CMS.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Medicare officials have released a slew of new data demonstrating physicians’ and hospitals’ performance on quality measures related to diabetes, cardiovascular care, and hospital-acquired infections and injuries.
The quality data were posted on Medicare’s Physician Compare and Hospital Compare websites, which aim to provide consumers with the information they need to help them select physicians and other health care providers. The information is also available on data.medicare.gov.
“The Compare sites empower consumers with information to help with health care decisions, encourage providers to strive for higher levels of quality, drive overall health system improvement,” Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Center for Medicare & Medicaid Services, wrote in a blog post.
For physicians, CMS is posting four measures related to diabetes and heart disease: controlling hemoglobin A1c (less than 8%); controlling blood pressure; prescribing aspirin to patients with diabetes and ischemic vascular disease; and prescribing ACE inhibitors or angiotensin receptor blockers for patients with coronary artery disease and diabetes or left ventricular systolic dysfunction.
The data come from 139 physician group practices, 214 shared savings program accountable care organizations, and 23 Pioneer ACOs.
To make the data more user-friendly, CMS uses stars, followed by a percentage score, to show group performance on individual measures. For instance, if a practice scored 80% on a measure, four stars would be shown along with the 80% score.
This is the second time that CMS officials have added quality data to Physician Compare – the first posting was in February 2014. CMS plans to expand the number of quality measures and the number of providers who are listed on the website. By late 2015, CMS plans to post quality data for group practices of all sizes and some data on individual physicians.
For hospitals, CMS posted performance on reducing hospital-acquired conditions, including central line–associated bloodstream infections, catheter-associated urinary tract infections, pressure ulcers, and accidental punctures and lacerations.
The agency also added data from its Hospital Readmissions Reduction Program, including 30-day readmission rates following elective and primary total hip and/or total knee replacement and the 30-day rate of unplanned readmission for chronic obstructive pulmonary disease.
CMS also released data on payment adjustments made as part of the 2015 Hospital Value-Based Purchasing Program, which ties payment to performance on certain quality measures. In fiscal year 2015 – the third year of the program – 1,714 hospitals will see their payments go up as a result of bonus payments from the program, compared with 1,375 that will see their payments decline, according to CMS.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Nearly 9% of Medicaid-financed births are early elective deliveries
Early elective deliveries – inductions and cesarean deliveries before 39 weeks’ gestation – account for nearly 9% of the singleton births paid for under the Medicaid program, according to an analysis published in the December issue of Health Affairs.*
The rate of early elective deliveries has improved over the last few years, falling by nearly a third among Medicaid-financed births between 2007 and 2011 (Health Aff. 2014;33:2170-8).
Medicaid medical directors in Ohio and Minnesota, working with staff members of AcademyHealth, compared birth certificate data and hospital records from 22 states to determine the rate of early elective deliveries from 2010-2012. Twelve states also provided trend data or 2007-2011.
Of the more than 800,000 singleton births paid for by the Medicaid program across the 22 states, about 32% were elective deliveries and nearly 9% were early-term elective deliveries.
Elective cesarean deliveries were more common than were elective labor inductions before 39 weeks’ gestation. And early elective deliveries increased with maternal age. Mothers older than 34 years had the highest rate at 12.7%. Mothers younger than 20 years had the lowest rate at 6.6%. Early elective deliveries were also higher among women with a history of cesarean delivery.
Over the last few years, there has been a steady push to reduce nonmedically indicated early deliveries. Both the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine say that early elective deliveries are not appropriate.
The federal government is also getting involved. In 2012, the Centers for Medicare & Medicaid Services joined other federal health agencies to launch the Strong Start for Mothers and Newborns Initiative, aimed at reducing early elective deliveries. And decreasing the rate of early elective deliveries is a priority measure in the CMS initial Core Set of Health Care Quality Measures for Adults Enrolled in Medicaid.
More than 20 state Medicaid programs have also implemented policies that discourage early elective deliveries, ranging from clinical education to partnering with hospitals on “hard stop” policies that bar scheduling of deliveries before 39 weeks without documentation of medical necessity.
While the rate of early elective deliveries has been falling since 2007, the researchers could not pinpoint which strategy is most effective, since most of the efforts are new.
*Correction, 1/30/2015: An earlier version of this story misstated the definition of early elective deliveries.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Early elective deliveries – inductions and cesarean deliveries before 39 weeks’ gestation – account for nearly 9% of the singleton births paid for under the Medicaid program, according to an analysis published in the December issue of Health Affairs.*
The rate of early elective deliveries has improved over the last few years, falling by nearly a third among Medicaid-financed births between 2007 and 2011 (Health Aff. 2014;33:2170-8).
Medicaid medical directors in Ohio and Minnesota, working with staff members of AcademyHealth, compared birth certificate data and hospital records from 22 states to determine the rate of early elective deliveries from 2010-2012. Twelve states also provided trend data or 2007-2011.
Of the more than 800,000 singleton births paid for by the Medicaid program across the 22 states, about 32% were elective deliveries and nearly 9% were early-term elective deliveries.
Elective cesarean deliveries were more common than were elective labor inductions before 39 weeks’ gestation. And early elective deliveries increased with maternal age. Mothers older than 34 years had the highest rate at 12.7%. Mothers younger than 20 years had the lowest rate at 6.6%. Early elective deliveries were also higher among women with a history of cesarean delivery.
Over the last few years, there has been a steady push to reduce nonmedically indicated early deliveries. Both the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine say that early elective deliveries are not appropriate.
The federal government is also getting involved. In 2012, the Centers for Medicare & Medicaid Services joined other federal health agencies to launch the Strong Start for Mothers and Newborns Initiative, aimed at reducing early elective deliveries. And decreasing the rate of early elective deliveries is a priority measure in the CMS initial Core Set of Health Care Quality Measures for Adults Enrolled in Medicaid.
More than 20 state Medicaid programs have also implemented policies that discourage early elective deliveries, ranging from clinical education to partnering with hospitals on “hard stop” policies that bar scheduling of deliveries before 39 weeks without documentation of medical necessity.
While the rate of early elective deliveries has been falling since 2007, the researchers could not pinpoint which strategy is most effective, since most of the efforts are new.
*Correction, 1/30/2015: An earlier version of this story misstated the definition of early elective deliveries.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Early elective deliveries – inductions and cesarean deliveries before 39 weeks’ gestation – account for nearly 9% of the singleton births paid for under the Medicaid program, according to an analysis published in the December issue of Health Affairs.*
The rate of early elective deliveries has improved over the last few years, falling by nearly a third among Medicaid-financed births between 2007 and 2011 (Health Aff. 2014;33:2170-8).
Medicaid medical directors in Ohio and Minnesota, working with staff members of AcademyHealth, compared birth certificate data and hospital records from 22 states to determine the rate of early elective deliveries from 2010-2012. Twelve states also provided trend data or 2007-2011.
Of the more than 800,000 singleton births paid for by the Medicaid program across the 22 states, about 32% were elective deliveries and nearly 9% were early-term elective deliveries.
Elective cesarean deliveries were more common than were elective labor inductions before 39 weeks’ gestation. And early elective deliveries increased with maternal age. Mothers older than 34 years had the highest rate at 12.7%. Mothers younger than 20 years had the lowest rate at 6.6%. Early elective deliveries were also higher among women with a history of cesarean delivery.
Over the last few years, there has been a steady push to reduce nonmedically indicated early deliveries. Both the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine say that early elective deliveries are not appropriate.
The federal government is also getting involved. In 2012, the Centers for Medicare & Medicaid Services joined other federal health agencies to launch the Strong Start for Mothers and Newborns Initiative, aimed at reducing early elective deliveries. And decreasing the rate of early elective deliveries is a priority measure in the CMS initial Core Set of Health Care Quality Measures for Adults Enrolled in Medicaid.
More than 20 state Medicaid programs have also implemented policies that discourage early elective deliveries, ranging from clinical education to partnering with hospitals on “hard stop” policies that bar scheduling of deliveries before 39 weeks without documentation of medical necessity.
While the rate of early elective deliveries has been falling since 2007, the researchers could not pinpoint which strategy is most effective, since most of the efforts are new.
*Correction, 1/30/2015: An earlier version of this story misstated the definition of early elective deliveries.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
FROM HEALTH AFFAIRS
Key clinical point: Clinicians need to do more to curb early elective deliveries.
Major finding: Between 2007 and 2011, early elective deliveries in Medicaid fell 32%, but still account for nearly 9% of births.
Data source: Retrospective descriptive study covering 839,688 Medicaid-covered singleton births during 2010-2012.
Disclosures: The study was funded by the Agency for Healthcare Research and Quality, the Centers for Medicare & Medicaid Services, and the Health Resources and Services Administration. The study authors reported having no financial disclosures.
Audit: Children in Medicaid Missing Key Screenings
More than a third of children enrolled in the Medicaid program aren’t receiving recommended screenings and other preventive care, according to a government audit.
A new report from the Health & Human Services Office of Inspector General found that in 2013 only about 63% of eligible children in the Medicaid program were receiving required screenings under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program. That figure increased from 56% in 2006, but is still significantly below the federal participation goal of 80% in each state annually.
Some children are missing out on well-child visits, while others are not receiving hearing and vision screenings. Even among children who had recommended well-child visits, the exams may not have been complete, according to the report.
For instance, 40% of children had not received the recommended six or more well-child visits by 15 months of age, and 34% had not received one or more visits between ages 3-6 years.
The findings are both surprising and discouraging, said Dr. Stuart Cohen, a San Diego pediatrician and the chairperson of the American Academy of Pediatrics’ California district.
“It raises a red flag,” Dr. Cohen said. “Why aren’t they doing it?”
It’s not because the EPSDT screenings are too onerous, he said, since in many states the schedules are less demanding than what the American Academy of Pediatrics recommends as part of their Bright Futures initiative. And lack of payment isn’t the issue either, he said, because Medicaid payment for EPSDT screenings is higher than Medicaid payments for other pediatric services.
“I think we have to align the incentives and disincentives more closely,” Dr. Cohen said. “Just like we report HEDIS [Healthcare Effectiveness Data and Information Set] measures for the rate of immunizations, Medicaid plans that measure the completeness of a screening and the frequency of screening should be sending more patients to the offices that are high performers.”
Payers also should encourage the greater use of patient reminder and recall modules as part of an electronic health record, Dr. Cohen said.
But there are also drivers of the underutilization of screening that are out of the hands of physicians, said Dr. Michael McManus, a pediatrician at Boston Children’s Hospital and a member of the AAP’s committee on state government affairs. Patients may have difficulty finding transportation to the office, or there may be language barriers that interfere with providing care on the recommended schedule.
These barriers are compounded for small practices working in underserved areas who may not have access to health information technology that allows them to more easily track patients and reach out to them, Dr. McManus said.
This is a vulnerable patient population, and they often have many barriers to care, said Dr. Robert Wergin, a family physician in Milford, Neb., and the president of the American Academy of Family Physicians. “You have to be understanding as a provider and break down the barriers.”
While physicians may not be able to help with issues like lack of transportation, they can make visits more convenient by offering extended hours.
Talking to parents about the importance of preventive screening also can go a long way, Dr. Wergin said. “We get better compliance when we tell them why it’s important.”
More than a third of children enrolled in the Medicaid program aren’t receiving recommended screenings and other preventive care, according to a government audit.
A new report from the Health & Human Services Office of Inspector General found that in 2013 only about 63% of eligible children in the Medicaid program were receiving required screenings under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program. That figure increased from 56% in 2006, but is still significantly below the federal participation goal of 80% in each state annually.
Some children are missing out on well-child visits, while others are not receiving hearing and vision screenings. Even among children who had recommended well-child visits, the exams may not have been complete, according to the report.
For instance, 40% of children had not received the recommended six or more well-child visits by 15 months of age, and 34% had not received one or more visits between ages 3-6 years.
The findings are both surprising and discouraging, said Dr. Stuart Cohen, a San Diego pediatrician and the chairperson of the American Academy of Pediatrics’ California district.
“It raises a red flag,” Dr. Cohen said. “Why aren’t they doing it?”
It’s not because the EPSDT screenings are too onerous, he said, since in many states the schedules are less demanding than what the American Academy of Pediatrics recommends as part of their Bright Futures initiative. And lack of payment isn’t the issue either, he said, because Medicaid payment for EPSDT screenings is higher than Medicaid payments for other pediatric services.
“I think we have to align the incentives and disincentives more closely,” Dr. Cohen said. “Just like we report HEDIS [Healthcare Effectiveness Data and Information Set] measures for the rate of immunizations, Medicaid plans that measure the completeness of a screening and the frequency of screening should be sending more patients to the offices that are high performers.”
Payers also should encourage the greater use of patient reminder and recall modules as part of an electronic health record, Dr. Cohen said.
But there are also drivers of the underutilization of screening that are out of the hands of physicians, said Dr. Michael McManus, a pediatrician at Boston Children’s Hospital and a member of the AAP’s committee on state government affairs. Patients may have difficulty finding transportation to the office, or there may be language barriers that interfere with providing care on the recommended schedule.
These barriers are compounded for small practices working in underserved areas who may not have access to health information technology that allows them to more easily track patients and reach out to them, Dr. McManus said.
This is a vulnerable patient population, and they often have many barriers to care, said Dr. Robert Wergin, a family physician in Milford, Neb., and the president of the American Academy of Family Physicians. “You have to be understanding as a provider and break down the barriers.”
While physicians may not be able to help with issues like lack of transportation, they can make visits more convenient by offering extended hours.
Talking to parents about the importance of preventive screening also can go a long way, Dr. Wergin said. “We get better compliance when we tell them why it’s important.”
More than a third of children enrolled in the Medicaid program aren’t receiving recommended screenings and other preventive care, according to a government audit.
A new report from the Health & Human Services Office of Inspector General found that in 2013 only about 63% of eligible children in the Medicaid program were receiving required screenings under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program. That figure increased from 56% in 2006, but is still significantly below the federal participation goal of 80% in each state annually.
Some children are missing out on well-child visits, while others are not receiving hearing and vision screenings. Even among children who had recommended well-child visits, the exams may not have been complete, according to the report.
For instance, 40% of children had not received the recommended six or more well-child visits by 15 months of age, and 34% had not received one or more visits between ages 3-6 years.
The findings are both surprising and discouraging, said Dr. Stuart Cohen, a San Diego pediatrician and the chairperson of the American Academy of Pediatrics’ California district.
“It raises a red flag,” Dr. Cohen said. “Why aren’t they doing it?”
It’s not because the EPSDT screenings are too onerous, he said, since in many states the schedules are less demanding than what the American Academy of Pediatrics recommends as part of their Bright Futures initiative. And lack of payment isn’t the issue either, he said, because Medicaid payment for EPSDT screenings is higher than Medicaid payments for other pediatric services.
“I think we have to align the incentives and disincentives more closely,” Dr. Cohen said. “Just like we report HEDIS [Healthcare Effectiveness Data and Information Set] measures for the rate of immunizations, Medicaid plans that measure the completeness of a screening and the frequency of screening should be sending more patients to the offices that are high performers.”
Payers also should encourage the greater use of patient reminder and recall modules as part of an electronic health record, Dr. Cohen said.
But there are also drivers of the underutilization of screening that are out of the hands of physicians, said Dr. Michael McManus, a pediatrician at Boston Children’s Hospital and a member of the AAP’s committee on state government affairs. Patients may have difficulty finding transportation to the office, or there may be language barriers that interfere with providing care on the recommended schedule.
These barriers are compounded for small practices working in underserved areas who may not have access to health information technology that allows them to more easily track patients and reach out to them, Dr. McManus said.
This is a vulnerable patient population, and they often have many barriers to care, said Dr. Robert Wergin, a family physician in Milford, Neb., and the president of the American Academy of Family Physicians. “You have to be understanding as a provider and break down the barriers.”
While physicians may not be able to help with issues like lack of transportation, they can make visits more convenient by offering extended hours.
Talking to parents about the importance of preventive screening also can go a long way, Dr. Wergin said. “We get better compliance when we tell them why it’s important.”
Audit: Children in Medicaid missing key screenings
More than a third of children enrolled in the Medicaid program aren’t receiving recommended screenings and other preventive care, according to a government audit.
A new report from the Health & Human Services Office of Inspector General found that in 2013 only about 63% of eligible children in the Medicaid program were receiving required screenings under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program. That figure increased from 56% in 2006, but is still significantly below the federal participation goal of 80% in each state annually.
Some children are missing out on well-child visits, while others are not receiving hearing and vision screenings. Even among children who had recommended well-child visits, the exams may not have been complete, according to the report.
For instance, 40% of children had not received the recommended six or more well-child visits by 15 months of age, and 34% had not received one or more visits between ages 3-6 years.
The findings are both surprising and discouraging, said Dr. Stuart Cohen, a San Diego pediatrician and the chairperson of the American Academy of Pediatrics’ California district.
“It raises a red flag,” Dr. Cohen said. “Why aren’t they doing it?”
It’s not because the EPSDT screenings are too onerous, he said, since in many states the schedules are less demanding than what the American Academy of Pediatrics recommends as part of their Bright Futures initiative. And lack of payment isn’t the issue either, he said, because Medicaid payment for EPSDT screenings is higher than Medicaid payments for other pediatric services.
“I think we have to align the incentives and disincentives more closely,” Dr. Cohen said. “Just like we report HEDIS [Healthcare Effectiveness Data and Information Set] measures for the rate of immunizations, Medicaid plans that measure the completeness of a screening and the frequency of screening should be sending more patients to the offices that are high performers.”
Payers also should encourage the greater use of patient reminder and recall modules as part of an electronic health record, Dr. Cohen said.
But there are also drivers of the underutilization of screening that are out of the hands of physicians, said Dr. Michael McManus, a pediatrician at Boston Children’s Hospital and a member of the AAP’s committee on state government affairs. Patients may have difficulty finding transportation to the office, or there may be language barriers that interfere with providing care on the recommended schedule.
These barriers are compounded for small practices working in underserved areas who may not have access to health information technology that allows them to more easily track patients and reach out to them, Dr. McManus said.
This is a vulnerable patient population, and they often have many barriers to care, said Dr. Robert Wergin, a family physician in Milford, Neb., and the president of the American Academy of Family Physicians. “You have to be understanding as a provider and break down the barriers.”
While physicians may not be able to help with issues like lack of transportation, they can make visits more convenient by offering extended hours.
Talking to parents about the importance of preventive screening also can go a long way, Dr. Wergin said. “We get better compliance when we tell them why it’s important.”
mschneider@frontlinemedcom.com
On Twitter @maryellenny
More than a third of children enrolled in the Medicaid program aren’t receiving recommended screenings and other preventive care, according to a government audit.
A new report from the Health & Human Services Office of Inspector General found that in 2013 only about 63% of eligible children in the Medicaid program were receiving required screenings under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program. That figure increased from 56% in 2006, but is still significantly below the federal participation goal of 80% in each state annually.
Some children are missing out on well-child visits, while others are not receiving hearing and vision screenings. Even among children who had recommended well-child visits, the exams may not have been complete, according to the report.
For instance, 40% of children had not received the recommended six or more well-child visits by 15 months of age, and 34% had not received one or more visits between ages 3-6 years.
The findings are both surprising and discouraging, said Dr. Stuart Cohen, a San Diego pediatrician and the chairperson of the American Academy of Pediatrics’ California district.
“It raises a red flag,” Dr. Cohen said. “Why aren’t they doing it?”
It’s not because the EPSDT screenings are too onerous, he said, since in many states the schedules are less demanding than what the American Academy of Pediatrics recommends as part of their Bright Futures initiative. And lack of payment isn’t the issue either, he said, because Medicaid payment for EPSDT screenings is higher than Medicaid payments for other pediatric services.
“I think we have to align the incentives and disincentives more closely,” Dr. Cohen said. “Just like we report HEDIS [Healthcare Effectiveness Data and Information Set] measures for the rate of immunizations, Medicaid plans that measure the completeness of a screening and the frequency of screening should be sending more patients to the offices that are high performers.”
Payers also should encourage the greater use of patient reminder and recall modules as part of an electronic health record, Dr. Cohen said.
But there are also drivers of the underutilization of screening that are out of the hands of physicians, said Dr. Michael McManus, a pediatrician at Boston Children’s Hospital and a member of the AAP’s committee on state government affairs. Patients may have difficulty finding transportation to the office, or there may be language barriers that interfere with providing care on the recommended schedule.
These barriers are compounded for small practices working in underserved areas who may not have access to health information technology that allows them to more easily track patients and reach out to them, Dr. McManus said.
This is a vulnerable patient population, and they often have many barriers to care, said Dr. Robert Wergin, a family physician in Milford, Neb., and the president of the American Academy of Family Physicians. “You have to be understanding as a provider and break down the barriers.”
While physicians may not be able to help with issues like lack of transportation, they can make visits more convenient by offering extended hours.
Talking to parents about the importance of preventive screening also can go a long way, Dr. Wergin said. “We get better compliance when we tell them why it’s important.”
mschneider@frontlinemedcom.com
On Twitter @maryellenny
More than a third of children enrolled in the Medicaid program aren’t receiving recommended screenings and other preventive care, according to a government audit.
A new report from the Health & Human Services Office of Inspector General found that in 2013 only about 63% of eligible children in the Medicaid program were receiving required screenings under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program. That figure increased from 56% in 2006, but is still significantly below the federal participation goal of 80% in each state annually.
Some children are missing out on well-child visits, while others are not receiving hearing and vision screenings. Even among children who had recommended well-child visits, the exams may not have been complete, according to the report.
For instance, 40% of children had not received the recommended six or more well-child visits by 15 months of age, and 34% had not received one or more visits between ages 3-6 years.
The findings are both surprising and discouraging, said Dr. Stuart Cohen, a San Diego pediatrician and the chairperson of the American Academy of Pediatrics’ California district.
“It raises a red flag,” Dr. Cohen said. “Why aren’t they doing it?”
It’s not because the EPSDT screenings are too onerous, he said, since in many states the schedules are less demanding than what the American Academy of Pediatrics recommends as part of their Bright Futures initiative. And lack of payment isn’t the issue either, he said, because Medicaid payment for EPSDT screenings is higher than Medicaid payments for other pediatric services.
“I think we have to align the incentives and disincentives more closely,” Dr. Cohen said. “Just like we report HEDIS [Healthcare Effectiveness Data and Information Set] measures for the rate of immunizations, Medicaid plans that measure the completeness of a screening and the frequency of screening should be sending more patients to the offices that are high performers.”
Payers also should encourage the greater use of patient reminder and recall modules as part of an electronic health record, Dr. Cohen said.
But there are also drivers of the underutilization of screening that are out of the hands of physicians, said Dr. Michael McManus, a pediatrician at Boston Children’s Hospital and a member of the AAP’s committee on state government affairs. Patients may have difficulty finding transportation to the office, or there may be language barriers that interfere with providing care on the recommended schedule.
These barriers are compounded for small practices working in underserved areas who may not have access to health information technology that allows them to more easily track patients and reach out to them, Dr. McManus said.
This is a vulnerable patient population, and they often have many barriers to care, said Dr. Robert Wergin, a family physician in Milford, Neb., and the president of the American Academy of Family Physicians. “You have to be understanding as a provider and break down the barriers.”
While physicians may not be able to help with issues like lack of transportation, they can make visits more convenient by offering extended hours.
Talking to parents about the importance of preventive screening also can go a long way, Dr. Wergin said. “We get better compliance when we tell them why it’s important.”
mschneider@frontlinemedcom.com
On Twitter @maryellenny
CMS rules on bundled payments, fee schedule
After a year-long delay, Medicare officials are implementing bundled payments for a number of services performed in hospital outpatient departments.
The new payments, which were finalized in the 2015 Medicare Hospital Outpatient Prospective Payment System rule, take effect on Jan. 1, 2015.
The Centers for Medicare & Medicaid Services (CMS) selected 25 primary services and their adjunctive services and supplies as comprehensive ambulatory payment classifications (C-APCs) and will provide a single payment under Medicare Part B. Medicare beneficiaries will pay a single copayment for the C-APC services.
The 25 C-APCs fall within 12 clinical families and include gastrointestinal procedures.
Overall, the HOPPS payment codes for GI services were given a positive update for 2015. For example, endoscopic retrograde cholangiopancreatography stent procedure (43274, 43276) payments increased by 64%; esophagoscopy and EGD with endoscopic mucosal resection (43211, 43254) were reassigned, resulting in a payment increase of about 60%; and drainage of pseudocyst (43240) also benefited from reassigment and netted an increase in payment of about 90%. Nearly all of the APCs containing GI procedures saw payment increases, anywhere from 1% for ERCP (0151), to 152% for level II noninvasive physiologic studies (0096).
Medicare Physician Fee Schedule
In the final rule, CMS outlined a new review process that will allow new and revised codes to be published in the proposed rule for public comment. Previously, the values for new and revised codes were not released until the final rule, leaving physicians with little time to prepare for changes in payment.
CMS delayed its valuation of lower GI codes, including colonoscopy, until 2016, as requested by the presidents of the American Gastroenterological Association, the American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy. The three societies have been advocating on GI reimbursement issues, with some success (http://www.gastro.org/journals-publications/news/2015-Medicare-Pay-Rules-Delay-Cuts-To-Lower-GI-Codes).
“AGA believes that CMS acted in response to an intensive educational effort coordinated among multiple medical and surgical societies,” said AGA President Dr. John I. Allen, AGAF.
The final rule, which was released by CMS on Oct. 31, also reversed the CMS policy of requiring physician certification for all Medicare Part A hospital admissions.
Starting Jan. 1, a formal physician certification is required only for long-stay cases of 20 days or more, or in costly outlier cases. For most patients, the admission order, medical record, and progress notes will contain “sufficient information to support the medical necessity of an inpatient admission without a separate requirement of an additional, formal, physician certification,” according to the final rule.
The revision of the physician certification policy does not remove any of the requirements associated with Medicare’s controversial 2-midnight policy, which governs short-stay hospitalizations.
The final rule was published in the Federal Register on Nov. 10.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
After a year-long delay, Medicare officials are implementing bundled payments for a number of services performed in hospital outpatient departments.
The new payments, which were finalized in the 2015 Medicare Hospital Outpatient Prospective Payment System rule, take effect on Jan. 1, 2015.
The Centers for Medicare & Medicaid Services (CMS) selected 25 primary services and their adjunctive services and supplies as comprehensive ambulatory payment classifications (C-APCs) and will provide a single payment under Medicare Part B. Medicare beneficiaries will pay a single copayment for the C-APC services.
The 25 C-APCs fall within 12 clinical families and include gastrointestinal procedures.
Overall, the HOPPS payment codes for GI services were given a positive update for 2015. For example, endoscopic retrograde cholangiopancreatography stent procedure (43274, 43276) payments increased by 64%; esophagoscopy and EGD with endoscopic mucosal resection (43211, 43254) were reassigned, resulting in a payment increase of about 60%; and drainage of pseudocyst (43240) also benefited from reassigment and netted an increase in payment of about 90%. Nearly all of the APCs containing GI procedures saw payment increases, anywhere from 1% for ERCP (0151), to 152% for level II noninvasive physiologic studies (0096).
Medicare Physician Fee Schedule
In the final rule, CMS outlined a new review process that will allow new and revised codes to be published in the proposed rule for public comment. Previously, the values for new and revised codes were not released until the final rule, leaving physicians with little time to prepare for changes in payment.
CMS delayed its valuation of lower GI codes, including colonoscopy, until 2016, as requested by the presidents of the American Gastroenterological Association, the American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy. The three societies have been advocating on GI reimbursement issues, with some success (http://www.gastro.org/journals-publications/news/2015-Medicare-Pay-Rules-Delay-Cuts-To-Lower-GI-Codes).
“AGA believes that CMS acted in response to an intensive educational effort coordinated among multiple medical and surgical societies,” said AGA President Dr. John I. Allen, AGAF.
The final rule, which was released by CMS on Oct. 31, also reversed the CMS policy of requiring physician certification for all Medicare Part A hospital admissions.
Starting Jan. 1, a formal physician certification is required only for long-stay cases of 20 days or more, or in costly outlier cases. For most patients, the admission order, medical record, and progress notes will contain “sufficient information to support the medical necessity of an inpatient admission without a separate requirement of an additional, formal, physician certification,” according to the final rule.
The revision of the physician certification policy does not remove any of the requirements associated with Medicare’s controversial 2-midnight policy, which governs short-stay hospitalizations.
The final rule was published in the Federal Register on Nov. 10.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
After a year-long delay, Medicare officials are implementing bundled payments for a number of services performed in hospital outpatient departments.
The new payments, which were finalized in the 2015 Medicare Hospital Outpatient Prospective Payment System rule, take effect on Jan. 1, 2015.
The Centers for Medicare & Medicaid Services (CMS) selected 25 primary services and their adjunctive services and supplies as comprehensive ambulatory payment classifications (C-APCs) and will provide a single payment under Medicare Part B. Medicare beneficiaries will pay a single copayment for the C-APC services.
The 25 C-APCs fall within 12 clinical families and include gastrointestinal procedures.
Overall, the HOPPS payment codes for GI services were given a positive update for 2015. For example, endoscopic retrograde cholangiopancreatography stent procedure (43274, 43276) payments increased by 64%; esophagoscopy and EGD with endoscopic mucosal resection (43211, 43254) were reassigned, resulting in a payment increase of about 60%; and drainage of pseudocyst (43240) also benefited from reassigment and netted an increase in payment of about 90%. Nearly all of the APCs containing GI procedures saw payment increases, anywhere from 1% for ERCP (0151), to 152% for level II noninvasive physiologic studies (0096).
Medicare Physician Fee Schedule
In the final rule, CMS outlined a new review process that will allow new and revised codes to be published in the proposed rule for public comment. Previously, the values for new and revised codes were not released until the final rule, leaving physicians with little time to prepare for changes in payment.
CMS delayed its valuation of lower GI codes, including colonoscopy, until 2016, as requested by the presidents of the American Gastroenterological Association, the American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy. The three societies have been advocating on GI reimbursement issues, with some success (http://www.gastro.org/journals-publications/news/2015-Medicare-Pay-Rules-Delay-Cuts-To-Lower-GI-Codes).
“AGA believes that CMS acted in response to an intensive educational effort coordinated among multiple medical and surgical societies,” said AGA President Dr. John I. Allen, AGAF.
The final rule, which was released by CMS on Oct. 31, also reversed the CMS policy of requiring physician certification for all Medicare Part A hospital admissions.
Starting Jan. 1, a formal physician certification is required only for long-stay cases of 20 days or more, or in costly outlier cases. For most patients, the admission order, medical record, and progress notes will contain “sufficient information to support the medical necessity of an inpatient admission without a separate requirement of an additional, formal, physician certification,” according to the final rule.
The revision of the physician certification policy does not remove any of the requirements associated with Medicare’s controversial 2-midnight policy, which governs short-stay hospitalizations.
The final rule was published in the Federal Register on Nov. 10.
mschneider@frontlinemedcom.com
On Twitter @maryellenny