User login
Screening database shows ABI can be cost-effective
PALM BEACH, FLA. – The ankle-brachial index value is directly associated with the prevalence of carotid artery stenosis and with a history of coronary artery disease and cerebrovascular disease, according to analysis of more than 3.6 million records obtained from the private health screening company, Life Line Screening.
But what makes the study interesting is the database itself, and not so much the findings, which have been previously shown, commented Dr. Spence M. Taylor, president of the Greenville (S.C.) Health System Clinical University.
Life Line Screening has mobile units, which travel to various locations and for a fee of more than $100, screen individuals, collecting nearly 300 data points per person. Meanwhile, the ankle-brachial index (ABI) costs less than $30 approximately. Yet, the test hasn’t become widely used, despite the evidence. Not much has changed since the 2001 PARTNERS study, which showed that the primary care physicians’ awareness of PAD diagnosis was "relatively low" (JAMA 2001;286:1317-24).
Results using the Life Line Screening’s large database may show the federal government that ABI can be cost effective, and getting them on board would popularize the screening tool, said Dr. Mark A. Adelman of the New York University Langone Medical Center, who presented his study at the Southern Association for Vascular Surgery annual meeting.
"Life Line is a huge paradox," said Dr. Taylor, senior associate dean of academic affairs at University of South Carolina, Greenville. It’s an operation that "we love to hate and hate to love," he added.
Dr. Adelman, the Frank J. Veith, M.D. Professor of Vascular and Endovascular Surgery and chief of vascular surgery at NYU Langone, and his colleagues analyzed data obtained from Life Line Screening, and found that individuals with an ABI between 0.41 and 0.60 had a 26.4% incidence of carotid artery stenosis (CAS), compared with individuals who had a normal ABI. The incidence increased to 35% for patients with ABI of 0.4 or less.
The majority of the abnormal ABI cases were between 0.81 and 0.90.
The analysis by Dr. Adelman and his colleagues also showed that individuals with PAD were more likely to be aged 70 years or older, male, and have modifiable risk factors, such as a history of smoking, hypertension, diabetes, and hypercholesterolemia, compared with non–PAD persons (P less than .001). (A comparison of Life Line’s database to one from the general population showed that the risk factors such as hypertension, hyperlipidemia, diabetes, and smoking were comparable.)
PAD subjects were also more likely to have CAS, prior stroke, prior transient ischemic attack, prior MI, and prior coronary revascularization, compared with those who didn’t have PAD (P less than .001). There was a significant correlation between decreasing ABI value and an increase in the prevalence of CAS, CAD, and cardiovascular disease (P less than .001).
In a separate study analyzing the same database, Dr. Adelman and his colleagues found that modifiable risk factors, such as hypertension and smoking, are associated with increased prevalence of peripheral vascular disease (J. Vasc. Surg. 2013;58:673-81).
Dr. Adelman said that screening for ABI could trigger other screening and lead to modification of risk factors that could affect better patient outcomes, changes in lifestyle, or changes in pharmacological management.
Dr. Adelman and Dr. Taylor had no disclosures.
On Twitter @naseemsmiller
 |
| Dr. R. Eugene Zierler |
This presentation confirms what we already know in a population consisting mostly of the "worried well" who are motivated to pay out-of-pocket for screening. I think it could be used to support selective screening of patients above a certain age threshold with risk factors. However, it suggests that most of the screening subjects with low ABIs also had other signs or symptoms of cardiovascular disease, so ABI screening alone probably did not add much new information. The article mentions cost-effectiveness, but that is big leap given the data and low prevalence of abnormal ABIs in the screened population.
Dr. R. Eugene Zierler is a professor of surgery at the University of Washington, Seattle, and an associate medical editor of Vascular Specialist.
 |
| Dr. R. Eugene Zierler |
This presentation confirms what we already know in a population consisting mostly of the "worried well" who are motivated to pay out-of-pocket for screening. I think it could be used to support selective screening of patients above a certain age threshold with risk factors. However, it suggests that most of the screening subjects with low ABIs also had other signs or symptoms of cardiovascular disease, so ABI screening alone probably did not add much new information. The article mentions cost-effectiveness, but that is big leap given the data and low prevalence of abnormal ABIs in the screened population.
Dr. R. Eugene Zierler is a professor of surgery at the University of Washington, Seattle, and an associate medical editor of Vascular Specialist.
 |
| Dr. R. Eugene Zierler |
This presentation confirms what we already know in a population consisting mostly of the "worried well" who are motivated to pay out-of-pocket for screening. I think it could be used to support selective screening of patients above a certain age threshold with risk factors. However, it suggests that most of the screening subjects with low ABIs also had other signs or symptoms of cardiovascular disease, so ABI screening alone probably did not add much new information. The article mentions cost-effectiveness, but that is big leap given the data and low prevalence of abnormal ABIs in the screened population.
Dr. R. Eugene Zierler is a professor of surgery at the University of Washington, Seattle, and an associate medical editor of Vascular Specialist.
PALM BEACH, FLA. – The ankle-brachial index value is directly associated with the prevalence of carotid artery stenosis and with a history of coronary artery disease and cerebrovascular disease, according to analysis of more than 3.6 million records obtained from the private health screening company, Life Line Screening.
But what makes the study interesting is the database itself, and not so much the findings, which have been previously shown, commented Dr. Spence M. Taylor, president of the Greenville (S.C.) Health System Clinical University.
Life Line Screening has mobile units, which travel to various locations and for a fee of more than $100, screen individuals, collecting nearly 300 data points per person. Meanwhile, the ankle-brachial index (ABI) costs less than $30 approximately. Yet, the test hasn’t become widely used, despite the evidence. Not much has changed since the 2001 PARTNERS study, which showed that the primary care physicians’ awareness of PAD diagnosis was "relatively low" (JAMA 2001;286:1317-24).
Results using the Life Line Screening’s large database may show the federal government that ABI can be cost effective, and getting them on board would popularize the screening tool, said Dr. Mark A. Adelman of the New York University Langone Medical Center, who presented his study at the Southern Association for Vascular Surgery annual meeting.
"Life Line is a huge paradox," said Dr. Taylor, senior associate dean of academic affairs at University of South Carolina, Greenville. It’s an operation that "we love to hate and hate to love," he added.
Dr. Adelman, the Frank J. Veith, M.D. Professor of Vascular and Endovascular Surgery and chief of vascular surgery at NYU Langone, and his colleagues analyzed data obtained from Life Line Screening, and found that individuals with an ABI between 0.41 and 0.60 had a 26.4% incidence of carotid artery stenosis (CAS), compared with individuals who had a normal ABI. The incidence increased to 35% for patients with ABI of 0.4 or less.
The majority of the abnormal ABI cases were between 0.81 and 0.90.
The analysis by Dr. Adelman and his colleagues also showed that individuals with PAD were more likely to be aged 70 years or older, male, and have modifiable risk factors, such as a history of smoking, hypertension, diabetes, and hypercholesterolemia, compared with non–PAD persons (P less than .001). (A comparison of Life Line’s database to one from the general population showed that the risk factors such as hypertension, hyperlipidemia, diabetes, and smoking were comparable.)
PAD subjects were also more likely to have CAS, prior stroke, prior transient ischemic attack, prior MI, and prior coronary revascularization, compared with those who didn’t have PAD (P less than .001). There was a significant correlation between decreasing ABI value and an increase in the prevalence of CAS, CAD, and cardiovascular disease (P less than .001).
In a separate study analyzing the same database, Dr. Adelman and his colleagues found that modifiable risk factors, such as hypertension and smoking, are associated with increased prevalence of peripheral vascular disease (J. Vasc. Surg. 2013;58:673-81).
Dr. Adelman said that screening for ABI could trigger other screening and lead to modification of risk factors that could affect better patient outcomes, changes in lifestyle, or changes in pharmacological management.
Dr. Adelman and Dr. Taylor had no disclosures.
On Twitter @naseemsmiller
PALM BEACH, FLA. – The ankle-brachial index value is directly associated with the prevalence of carotid artery stenosis and with a history of coronary artery disease and cerebrovascular disease, according to analysis of more than 3.6 million records obtained from the private health screening company, Life Line Screening.
But what makes the study interesting is the database itself, and not so much the findings, which have been previously shown, commented Dr. Spence M. Taylor, president of the Greenville (S.C.) Health System Clinical University.
Life Line Screening has mobile units, which travel to various locations and for a fee of more than $100, screen individuals, collecting nearly 300 data points per person. Meanwhile, the ankle-brachial index (ABI) costs less than $30 approximately. Yet, the test hasn’t become widely used, despite the evidence. Not much has changed since the 2001 PARTNERS study, which showed that the primary care physicians’ awareness of PAD diagnosis was "relatively low" (JAMA 2001;286:1317-24).
Results using the Life Line Screening’s large database may show the federal government that ABI can be cost effective, and getting them on board would popularize the screening tool, said Dr. Mark A. Adelman of the New York University Langone Medical Center, who presented his study at the Southern Association for Vascular Surgery annual meeting.
"Life Line is a huge paradox," said Dr. Taylor, senior associate dean of academic affairs at University of South Carolina, Greenville. It’s an operation that "we love to hate and hate to love," he added.
Dr. Adelman, the Frank J. Veith, M.D. Professor of Vascular and Endovascular Surgery and chief of vascular surgery at NYU Langone, and his colleagues analyzed data obtained from Life Line Screening, and found that individuals with an ABI between 0.41 and 0.60 had a 26.4% incidence of carotid artery stenosis (CAS), compared with individuals who had a normal ABI. The incidence increased to 35% for patients with ABI of 0.4 or less.
The majority of the abnormal ABI cases were between 0.81 and 0.90.
The analysis by Dr. Adelman and his colleagues also showed that individuals with PAD were more likely to be aged 70 years or older, male, and have modifiable risk factors, such as a history of smoking, hypertension, diabetes, and hypercholesterolemia, compared with non–PAD persons (P less than .001). (A comparison of Life Line’s database to one from the general population showed that the risk factors such as hypertension, hyperlipidemia, diabetes, and smoking were comparable.)
PAD subjects were also more likely to have CAS, prior stroke, prior transient ischemic attack, prior MI, and prior coronary revascularization, compared with those who didn’t have PAD (P less than .001). There was a significant correlation between decreasing ABI value and an increase in the prevalence of CAS, CAD, and cardiovascular disease (P less than .001).
In a separate study analyzing the same database, Dr. Adelman and his colleagues found that modifiable risk factors, such as hypertension and smoking, are associated with increased prevalence of peripheral vascular disease (J. Vasc. Surg. 2013;58:673-81).
Dr. Adelman said that screening for ABI could trigger other screening and lead to modification of risk factors that could affect better patient outcomes, changes in lifestyle, or changes in pharmacological management.
Dr. Adelman and Dr. Taylor had no disclosures.
On Twitter @naseemsmiller
AT THE SAVS ANNUAL MEETING
Major finding: Individuals with an ABI between 0.41 and 0.60 had a 26.4% incidence of CAS, compared with individuals who had a normal ABI. The incidence increased to 35% for patients with ABI of 0.4 or less.
Data source: 3.6 million records collected by Life Line Screening.
Disclosures: Dr. Adelman and Dr. Taylor had no disclosures.
Bedside IVC filter placement safe in critically ill
PALM BEACH, FLA. – Bedside vena cava filter placement using intravascular ultrasound was a safe and effective option in critically ill patients, according to a retrospective study at the University of Alabama at Birmingham.
During a 5-year period, 98% of the filter placements were successful. Technical success also improved significantly, and the complication rates dropped, reported Dr. Roan J. Glocker during a presentation at the annual meeting of the Southern Association for Vascular Surgery.
Vena cava filters have been used for nearly 4 decades for the prevention of pulmonary embolism. Dr. Glocker said that the bedside methods of filter placement often eliminate the need to transport patients, who are often critically ill or injured. It also eliminates the need for an operating room or angiography usage and reduces the risk that may result from contrast administration and radiation.
In 2010, researchers at the University of Alabama first reported successful outcomes of an algorithm for bedside intravascular ultrasound (IVUS) guided inferior vena cava (IVC) filter placement. Dr. Glocker said that the team wanted to evaluate their experience over a longer period of time, and to determine whether the safety and efficacy of the procedure was sustainable and evaluate the complication rates.
Researchers conducted a retrospective review of 398 patients undergoing bedside IVUS-guided IVC filter placement from 2008 to 2012. Seventy-percent of the patients were male, with a mean age of 77 years old, ranging from 14 to 91 years old. Close to 80% were multitrauma patients. The most common indication for filter placement was VTE prophylaxis in multisystem injury.
Outcomes were analyzed at 30 days. The study had no control groups.
Results showed that the technical success was 98%. The optional filters – Gunther Tulip or Cook Celect – were used in 94% of the patients, and the Greenfield permanent filter was used in the rest.
In 97% of the cases, a single puncture technique was performed. Periprocedural complications occurred only 3% of the time. Thirty patients died within 30 days of filter placement; however, there were no deaths related to pulmonary embolism or filter-related problems, Dr. Glocker reported.
When researchers compared the first and last 100 procedures, the complication rates dropped from 7% to 2 % (P = .08), and the technical success improved significantly from 96% in the first 100 procedures to 100% in the last 100.
Although there has been little change in the basic design of the filters, there have been remarkable improvements in placement techniques, going from the operating room to the radiology suites, to the patient bedside, said Dr. Lazar J. Greenfield Sr., professor emeritus of surgery at the University of Michigan, Ann Arbor, and the inventor of the filter.
But a 2013 study showed that the use of vena cava filters varies widely among hospitals, and some experts say that there’s still not enough evidence about its effectiveness.
In 2010, the Food and Drug Administration issued safety concerns about leaving the filters in place for a long period of time. Currently, the PRESERVE (Predicting the Safety and Effectiveness of Inferior Vena Cava Filters) study, a 5-year, multispecialty, prospective trial, is examining the use of IVC filters by focusing on safety endpoints.
The procedure has a learning curve. The surgeon has to be familiar with the IVUS modality and should have a thorough understanding of deployment of each filter, Dr. Glocker said. He guesstimated that physicians should perform approximately 20-50 procedures to reach competency and start performing the procedure on their own.
Dr. Glocker and Dr. Greenfield had no disclosures.
On Twitter @naseemsmiller
PALM BEACH, FLA. – Bedside vena cava filter placement using intravascular ultrasound was a safe and effective option in critically ill patients, according to a retrospective study at the University of Alabama at Birmingham.
During a 5-year period, 98% of the filter placements were successful. Technical success also improved significantly, and the complication rates dropped, reported Dr. Roan J. Glocker during a presentation at the annual meeting of the Southern Association for Vascular Surgery.
Vena cava filters have been used for nearly 4 decades for the prevention of pulmonary embolism. Dr. Glocker said that the bedside methods of filter placement often eliminate the need to transport patients, who are often critically ill or injured. It also eliminates the need for an operating room or angiography usage and reduces the risk that may result from contrast administration and radiation.
In 2010, researchers at the University of Alabama first reported successful outcomes of an algorithm for bedside intravascular ultrasound (IVUS) guided inferior vena cava (IVC) filter placement. Dr. Glocker said that the team wanted to evaluate their experience over a longer period of time, and to determine whether the safety and efficacy of the procedure was sustainable and evaluate the complication rates.
Researchers conducted a retrospective review of 398 patients undergoing bedside IVUS-guided IVC filter placement from 2008 to 2012. Seventy-percent of the patients were male, with a mean age of 77 years old, ranging from 14 to 91 years old. Close to 80% were multitrauma patients. The most common indication for filter placement was VTE prophylaxis in multisystem injury.
Outcomes were analyzed at 30 days. The study had no control groups.
Results showed that the technical success was 98%. The optional filters – Gunther Tulip or Cook Celect – were used in 94% of the patients, and the Greenfield permanent filter was used in the rest.
In 97% of the cases, a single puncture technique was performed. Periprocedural complications occurred only 3% of the time. Thirty patients died within 30 days of filter placement; however, there were no deaths related to pulmonary embolism or filter-related problems, Dr. Glocker reported.
When researchers compared the first and last 100 procedures, the complication rates dropped from 7% to 2 % (P = .08), and the technical success improved significantly from 96% in the first 100 procedures to 100% in the last 100.
Although there has been little change in the basic design of the filters, there have been remarkable improvements in placement techniques, going from the operating room to the radiology suites, to the patient bedside, said Dr. Lazar J. Greenfield Sr., professor emeritus of surgery at the University of Michigan, Ann Arbor, and the inventor of the filter.
But a 2013 study showed that the use of vena cava filters varies widely among hospitals, and some experts say that there’s still not enough evidence about its effectiveness.
In 2010, the Food and Drug Administration issued safety concerns about leaving the filters in place for a long period of time. Currently, the PRESERVE (Predicting the Safety and Effectiveness of Inferior Vena Cava Filters) study, a 5-year, multispecialty, prospective trial, is examining the use of IVC filters by focusing on safety endpoints.
The procedure has a learning curve. The surgeon has to be familiar with the IVUS modality and should have a thorough understanding of deployment of each filter, Dr. Glocker said. He guesstimated that physicians should perform approximately 20-50 procedures to reach competency and start performing the procedure on their own.
Dr. Glocker and Dr. Greenfield had no disclosures.
On Twitter @naseemsmiller
PALM BEACH, FLA. – Bedside vena cava filter placement using intravascular ultrasound was a safe and effective option in critically ill patients, according to a retrospective study at the University of Alabama at Birmingham.
During a 5-year period, 98% of the filter placements were successful. Technical success also improved significantly, and the complication rates dropped, reported Dr. Roan J. Glocker during a presentation at the annual meeting of the Southern Association for Vascular Surgery.
Vena cava filters have been used for nearly 4 decades for the prevention of pulmonary embolism. Dr. Glocker said that the bedside methods of filter placement often eliminate the need to transport patients, who are often critically ill or injured. It also eliminates the need for an operating room or angiography usage and reduces the risk that may result from contrast administration and radiation.
In 2010, researchers at the University of Alabama first reported successful outcomes of an algorithm for bedside intravascular ultrasound (IVUS) guided inferior vena cava (IVC) filter placement. Dr. Glocker said that the team wanted to evaluate their experience over a longer period of time, and to determine whether the safety and efficacy of the procedure was sustainable and evaluate the complication rates.
Researchers conducted a retrospective review of 398 patients undergoing bedside IVUS-guided IVC filter placement from 2008 to 2012. Seventy-percent of the patients were male, with a mean age of 77 years old, ranging from 14 to 91 years old. Close to 80% were multitrauma patients. The most common indication for filter placement was VTE prophylaxis in multisystem injury.
Outcomes were analyzed at 30 days. The study had no control groups.
Results showed that the technical success was 98%. The optional filters – Gunther Tulip or Cook Celect – were used in 94% of the patients, and the Greenfield permanent filter was used in the rest.
In 97% of the cases, a single puncture technique was performed. Periprocedural complications occurred only 3% of the time. Thirty patients died within 30 days of filter placement; however, there were no deaths related to pulmonary embolism or filter-related problems, Dr. Glocker reported.
When researchers compared the first and last 100 procedures, the complication rates dropped from 7% to 2 % (P = .08), and the technical success improved significantly from 96% in the first 100 procedures to 100% in the last 100.
Although there has been little change in the basic design of the filters, there have been remarkable improvements in placement techniques, going from the operating room to the radiology suites, to the patient bedside, said Dr. Lazar J. Greenfield Sr., professor emeritus of surgery at the University of Michigan, Ann Arbor, and the inventor of the filter.
But a 2013 study showed that the use of vena cava filters varies widely among hospitals, and some experts say that there’s still not enough evidence about its effectiveness.
In 2010, the Food and Drug Administration issued safety concerns about leaving the filters in place for a long period of time. Currently, the PRESERVE (Predicting the Safety and Effectiveness of Inferior Vena Cava Filters) study, a 5-year, multispecialty, prospective trial, is examining the use of IVC filters by focusing on safety endpoints.
The procedure has a learning curve. The surgeon has to be familiar with the IVUS modality and should have a thorough understanding of deployment of each filter, Dr. Glocker said. He guesstimated that physicians should perform approximately 20-50 procedures to reach competency and start performing the procedure on their own.
Dr. Glocker and Dr. Greenfield had no disclosures.
On Twitter @naseemsmiller
AT THE SAVS ANNUAL MEETING
Major finding: When researchers compared the first and last 100 procedures, the complication rates dropped from 7% to 2 % (P = .08), and the technical success improved significantly from 96% in the first 100 procedures to 100% in the last 100.
Data source: A retrospective review of 398 patients undergoing bedside IVUS-guided IVC filter placement from 2008 to 2012
Disclosures: Dr. Glocker had no disclosures.
Screening database shows ABI can be cost effective
PALM BEACH, FLA. – The ankle-brachial index value is directly associated with the prevalence of carotid artery stenosis and with a history of coronary artery disease and cerebrovascular disease, according to analysis of more than 3.6 million records obtained from the private health screening company, Life Line Screening.
But what makes the study interesting is the database itself, and not so much the findings, which have been previously shown, commented Dr. Spence M. Taylor, president of the Greenville Health System Clinical University, Greenville, South Carolina.
Life Line Screening has mobile units, which travel to various locations and for a fee of more than $100, screen individuals, collecting nearly 300 data points per person. Meanwhile, the ankle-brachial index (ABI) costs less than $30 approximately. Yet, the test hasn’t become widely used, despite the evidence. Not much has changed since the 2001 PARTNERS study, which showed that the primary care physicians’ awareness of PAD diagnosis was "relatively low" (JAMA 2001;286:1317-24).
Results using the Life Line Screening’s large database may show the federal government that ABI can be cost effective, and getting them on board would popularize the screening tool, said Dr. Mark A. Adelman of the NYU Langone Medical Center, who presented his study at the Southern Association for Vascular Surgery annual meeting.
"Life Line is a huge paradox," said Dr. Taylor, senior associate dean of academic affairs at University of South Carolina, Greenville. It’s an operation that "we love to hate and hate to love," he added.
Dr. Adelman, the Frank J. Veith, M.D. Professor of Vascular and Endovascular Surgery and chief of vascular surgery at NYU Langone, and his colleagues analyzed data obtained from Life Line Screening, and found that individuals with an ABI between 0.41 and 0.60 had a 26.4% incidence of carotid artery stenosis (CAS), compared with individuals who had a normal ABI. The incidence increased to 35% for patients with ABI of 0.4 or less.
The majority of the abnormal ABI cases were between 0.81 and 0.90.
The analysis by Dr. Adelman and his colleagues also showed that individuals with PAD were more likely to be aged 70 years or older, male, and have modifiable risk factors, such as a history of smoking, hypertension, diabetes, and hypercholesterolemia, compared with non–PAD persons (P less than .001). (A comparison of Life Line’s database to one from the general population showed that the risk factors such as hypertension, hyperlipidemia, diabetes, and smoking were comparable.)
PAD subjects were also more likely to have CAS, prior stroke, prior transient ischemic attack, prior MI, and prior coronary revascularization, compared with those who didn’t have PAD (P less than .001). There was a significant correlation between decreasing ABI value and an increase in the prevalence of CAS, CAD, and cardiovascular disease (P less than .001).
In a separate study analyzing the same database, Dr. Adelman and his colleagues found that modifiable risk factors, such as hypertension and smoking, are associated with increased prevalence of peripheral vascular disease (J. Vasc. Surg. 2013;58:673-81).
Dr. Adelman said that screening for ABI could trigger other screening and lead to modification of risk factors that could affect better patient outcomes, changes in lifestyle, or changes in pharmacological management.
Dr. Adelman and Dr. Taylor had no disclosures.
On Twitter @naseemsmiller
PALM BEACH, FLA. – The ankle-brachial index value is directly associated with the prevalence of carotid artery stenosis and with a history of coronary artery disease and cerebrovascular disease, according to analysis of more than 3.6 million records obtained from the private health screening company, Life Line Screening.
But what makes the study interesting is the database itself, and not so much the findings, which have been previously shown, commented Dr. Spence M. Taylor, president of the Greenville Health System Clinical University, Greenville, South Carolina.
Life Line Screening has mobile units, which travel to various locations and for a fee of more than $100, screen individuals, collecting nearly 300 data points per person. Meanwhile, the ankle-brachial index (ABI) costs less than $30 approximately. Yet, the test hasn’t become widely used, despite the evidence. Not much has changed since the 2001 PARTNERS study, which showed that the primary care physicians’ awareness of PAD diagnosis was "relatively low" (JAMA 2001;286:1317-24).
Results using the Life Line Screening’s large database may show the federal government that ABI can be cost effective, and getting them on board would popularize the screening tool, said Dr. Mark A. Adelman of the NYU Langone Medical Center, who presented his study at the Southern Association for Vascular Surgery annual meeting.
"Life Line is a huge paradox," said Dr. Taylor, senior associate dean of academic affairs at University of South Carolina, Greenville. It’s an operation that "we love to hate and hate to love," he added.
Dr. Adelman, the Frank J. Veith, M.D. Professor of Vascular and Endovascular Surgery and chief of vascular surgery at NYU Langone, and his colleagues analyzed data obtained from Life Line Screening, and found that individuals with an ABI between 0.41 and 0.60 had a 26.4% incidence of carotid artery stenosis (CAS), compared with individuals who had a normal ABI. The incidence increased to 35% for patients with ABI of 0.4 or less.
The majority of the abnormal ABI cases were between 0.81 and 0.90.
The analysis by Dr. Adelman and his colleagues also showed that individuals with PAD were more likely to be aged 70 years or older, male, and have modifiable risk factors, such as a history of smoking, hypertension, diabetes, and hypercholesterolemia, compared with non–PAD persons (P less than .001). (A comparison of Life Line’s database to one from the general population showed that the risk factors such as hypertension, hyperlipidemia, diabetes, and smoking were comparable.)
PAD subjects were also more likely to have CAS, prior stroke, prior transient ischemic attack, prior MI, and prior coronary revascularization, compared with those who didn’t have PAD (P less than .001). There was a significant correlation between decreasing ABI value and an increase in the prevalence of CAS, CAD, and cardiovascular disease (P less than .001).
In a separate study analyzing the same database, Dr. Adelman and his colleagues found that modifiable risk factors, such as hypertension and smoking, are associated with increased prevalence of peripheral vascular disease (J. Vasc. Surg. 2013;58:673-81).
Dr. Adelman said that screening for ABI could trigger other screening and lead to modification of risk factors that could affect better patient outcomes, changes in lifestyle, or changes in pharmacological management.
Dr. Adelman and Dr. Taylor had no disclosures.
On Twitter @naseemsmiller
PALM BEACH, FLA. – The ankle-brachial index value is directly associated with the prevalence of carotid artery stenosis and with a history of coronary artery disease and cerebrovascular disease, according to analysis of more than 3.6 million records obtained from the private health screening company, Life Line Screening.
But what makes the study interesting is the database itself, and not so much the findings, which have been previously shown, commented Dr. Spence M. Taylor, president of the Greenville Health System Clinical University, Greenville, South Carolina.
Life Line Screening has mobile units, which travel to various locations and for a fee of more than $100, screen individuals, collecting nearly 300 data points per person. Meanwhile, the ankle-brachial index (ABI) costs less than $30 approximately. Yet, the test hasn’t become widely used, despite the evidence. Not much has changed since the 2001 PARTNERS study, which showed that the primary care physicians’ awareness of PAD diagnosis was "relatively low" (JAMA 2001;286:1317-24).
Results using the Life Line Screening’s large database may show the federal government that ABI can be cost effective, and getting them on board would popularize the screening tool, said Dr. Mark A. Adelman of the NYU Langone Medical Center, who presented his study at the Southern Association for Vascular Surgery annual meeting.
"Life Line is a huge paradox," said Dr. Taylor, senior associate dean of academic affairs at University of South Carolina, Greenville. It’s an operation that "we love to hate and hate to love," he added.
Dr. Adelman, the Frank J. Veith, M.D. Professor of Vascular and Endovascular Surgery and chief of vascular surgery at NYU Langone, and his colleagues analyzed data obtained from Life Line Screening, and found that individuals with an ABI between 0.41 and 0.60 had a 26.4% incidence of carotid artery stenosis (CAS), compared with individuals who had a normal ABI. The incidence increased to 35% for patients with ABI of 0.4 or less.
The majority of the abnormal ABI cases were between 0.81 and 0.90.
The analysis by Dr. Adelman and his colleagues also showed that individuals with PAD were more likely to be aged 70 years or older, male, and have modifiable risk factors, such as a history of smoking, hypertension, diabetes, and hypercholesterolemia, compared with non–PAD persons (P less than .001). (A comparison of Life Line’s database to one from the general population showed that the risk factors such as hypertension, hyperlipidemia, diabetes, and smoking were comparable.)
PAD subjects were also more likely to have CAS, prior stroke, prior transient ischemic attack, prior MI, and prior coronary revascularization, compared with those who didn’t have PAD (P less than .001). There was a significant correlation between decreasing ABI value and an increase in the prevalence of CAS, CAD, and cardiovascular disease (P less than .001).
In a separate study analyzing the same database, Dr. Adelman and his colleagues found that modifiable risk factors, such as hypertension and smoking, are associated with increased prevalence of peripheral vascular disease (J. Vasc. Surg. 2013;58:673-81).
Dr. Adelman said that screening for ABI could trigger other screening and lead to modification of risk factors that could affect better patient outcomes, changes in lifestyle, or changes in pharmacological management.
Dr. Adelman and Dr. Taylor had no disclosures.
On Twitter @naseemsmiller
AT THE SAVS ANNUAL MEETING
Major finding: Individuals with an ABI between 0.41 and 0.60 had a 26.4% incidence of CAS, compared with individuals who had a normal ABI. The incidence increased to 35% for patients with ABI of 0.4 or less.
Data source: 3.6 million records collected by Life Line Screening.
Disclosures: Dr. Adelman and Dr. Taylor had no disclosures.
Telepsychiatry effective for ADHD treatment in rural areas
ORLANDO – Telepsychiatry in rural areas is beneficial for children with attention-deficit/hyperactivity disorder and their parents, according to one of the largest randomized controlled trials of its kind.
During the 22 weeks of the study, children who received telemental health (TMH) improved significantly in ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning, based on the ratings provided by their parents.
The study is yet another piece of evidence that telemedicine can play a role in closing the mental health gap.
"Our study shows that with modern technology, we have the opportunity to reach out to underserved areas and provide care," said Dr. William P. French of the University of Washington, Seattle. "And the care is good care and can improve the health of the patients at least as well as the local providers."
Dr. French and his colleagues used the Children’s ADHD Telemental Health Treatment Study, or CATTS, to assess the impact of telemental health on children’s inattention, hyperactivity, opposition, school performance, and impairment. They also evaluated the telepsychiatrists’ and therapists’ adherence to evidence-based treatment protocols implemented within the TMH model.
CATTS includes 223 English-speaking children aged 5.5-12 years with ADHD, along with their parents. The children were recruited from several local primary care practices in seven rural areas in Washington and Oregon between November 2009 and August 2012.
The children were randomly assigned to two groups. Group A, or the intervention group, received six teleconferencing sessions over a 22-week period. Their medication and education were delivered via videoconferencing by a child and adolescent psychiatrist. Their parents’ behavior training, which also occurred in six sessions, was provided in person by a community therapist. The local therapists already had been trained in treatment protocols and were supervised remotely.
Group B, or the active control group, received one video conferencing session with the child and adolescent psychiatrist, who gave the primary care providers treatment recommendations. For the rest of the trial period, this group received the standard of care, which was mainly treatment by their primary care provider.
The primary outcome included the Vanderbilt ADHD Rating Scales (VADRS) and the Columbia Impairment Scale–Parent Version (CIS-P), both of which were filled out by parents. Teachers assessed the ADHD and oppositional defiant disorder symptoms using VADRS.
Assessments were conducted at baseline, 4, 10, and 19 weeks, and at 25 weeks post randomization.
Results showed that during the 22 weeks, children receiving TMH had significantly better responses than the control group, the researchers found. Their parent-rated ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning improved, as did their teacher-rated ADHD inattention and school performance.
However, no effect was shown in the teacher-rated hyperactivity or oppositional defiant disorder. Dr. French said this could be attributable to the contextual demands of school versus home, or a change in teacher with kids moved to the next grade during the study period.
The study also showed that telepsychiatrists and therapists adhered to the evidence-based treatment protocols more than 90% of the time. Researchers said that TMH can be effective in training community therapists in evidence-based treatment behavioral management.
Barriers still exist to widespread implementation and adoption of telepsychiatry– with privacy concerns and lack of reimbursement just to name two – but advancement in technology is making the service more readily available, said Dr. French, who presented his findings in a poster at the American Academy of Child and Adolescent Psychiatry meeting.
"Telemedicine is going to be mostly Internet based," he said, "and this opens the potential to anyone with Internet access and a mobile device that has a camera and audio capabilities."
The study was supported by the National Institute of Mental Health. Researchers reported no relevant financial disclosures.
On Twitter @naseemsmiller
ORLANDO – Telepsychiatry in rural areas is beneficial for children with attention-deficit/hyperactivity disorder and their parents, according to one of the largest randomized controlled trials of its kind.
During the 22 weeks of the study, children who received telemental health (TMH) improved significantly in ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning, based on the ratings provided by their parents.
The study is yet another piece of evidence that telemedicine can play a role in closing the mental health gap.
"Our study shows that with modern technology, we have the opportunity to reach out to underserved areas and provide care," said Dr. William P. French of the University of Washington, Seattle. "And the care is good care and can improve the health of the patients at least as well as the local providers."
Dr. French and his colleagues used the Children’s ADHD Telemental Health Treatment Study, or CATTS, to assess the impact of telemental health on children’s inattention, hyperactivity, opposition, school performance, and impairment. They also evaluated the telepsychiatrists’ and therapists’ adherence to evidence-based treatment protocols implemented within the TMH model.
CATTS includes 223 English-speaking children aged 5.5-12 years with ADHD, along with their parents. The children were recruited from several local primary care practices in seven rural areas in Washington and Oregon between November 2009 and August 2012.
The children were randomly assigned to two groups. Group A, or the intervention group, received six teleconferencing sessions over a 22-week period. Their medication and education were delivered via videoconferencing by a child and adolescent psychiatrist. Their parents’ behavior training, which also occurred in six sessions, was provided in person by a community therapist. The local therapists already had been trained in treatment protocols and were supervised remotely.
Group B, or the active control group, received one video conferencing session with the child and adolescent psychiatrist, who gave the primary care providers treatment recommendations. For the rest of the trial period, this group received the standard of care, which was mainly treatment by their primary care provider.
The primary outcome included the Vanderbilt ADHD Rating Scales (VADRS) and the Columbia Impairment Scale–Parent Version (CIS-P), both of which were filled out by parents. Teachers assessed the ADHD and oppositional defiant disorder symptoms using VADRS.
Assessments were conducted at baseline, 4, 10, and 19 weeks, and at 25 weeks post randomization.
Results showed that during the 22 weeks, children receiving TMH had significantly better responses than the control group, the researchers found. Their parent-rated ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning improved, as did their teacher-rated ADHD inattention and school performance.
However, no effect was shown in the teacher-rated hyperactivity or oppositional defiant disorder. Dr. French said this could be attributable to the contextual demands of school versus home, or a change in teacher with kids moved to the next grade during the study period.
The study also showed that telepsychiatrists and therapists adhered to the evidence-based treatment protocols more than 90% of the time. Researchers said that TMH can be effective in training community therapists in evidence-based treatment behavioral management.
Barriers still exist to widespread implementation and adoption of telepsychiatry– with privacy concerns and lack of reimbursement just to name two – but advancement in technology is making the service more readily available, said Dr. French, who presented his findings in a poster at the American Academy of Child and Adolescent Psychiatry meeting.
"Telemedicine is going to be mostly Internet based," he said, "and this opens the potential to anyone with Internet access and a mobile device that has a camera and audio capabilities."
The study was supported by the National Institute of Mental Health. Researchers reported no relevant financial disclosures.
On Twitter @naseemsmiller
ORLANDO – Telepsychiatry in rural areas is beneficial for children with attention-deficit/hyperactivity disorder and their parents, according to one of the largest randomized controlled trials of its kind.
During the 22 weeks of the study, children who received telemental health (TMH) improved significantly in ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning, based on the ratings provided by their parents.
The study is yet another piece of evidence that telemedicine can play a role in closing the mental health gap.
"Our study shows that with modern technology, we have the opportunity to reach out to underserved areas and provide care," said Dr. William P. French of the University of Washington, Seattle. "And the care is good care and can improve the health of the patients at least as well as the local providers."
Dr. French and his colleagues used the Children’s ADHD Telemental Health Treatment Study, or CATTS, to assess the impact of telemental health on children’s inattention, hyperactivity, opposition, school performance, and impairment. They also evaluated the telepsychiatrists’ and therapists’ adherence to evidence-based treatment protocols implemented within the TMH model.
CATTS includes 223 English-speaking children aged 5.5-12 years with ADHD, along with their parents. The children were recruited from several local primary care practices in seven rural areas in Washington and Oregon between November 2009 and August 2012.
The children were randomly assigned to two groups. Group A, or the intervention group, received six teleconferencing sessions over a 22-week period. Their medication and education were delivered via videoconferencing by a child and adolescent psychiatrist. Their parents’ behavior training, which also occurred in six sessions, was provided in person by a community therapist. The local therapists already had been trained in treatment protocols and were supervised remotely.
Group B, or the active control group, received one video conferencing session with the child and adolescent psychiatrist, who gave the primary care providers treatment recommendations. For the rest of the trial period, this group received the standard of care, which was mainly treatment by their primary care provider.
The primary outcome included the Vanderbilt ADHD Rating Scales (VADRS) and the Columbia Impairment Scale–Parent Version (CIS-P), both of which were filled out by parents. Teachers assessed the ADHD and oppositional defiant disorder symptoms using VADRS.
Assessments were conducted at baseline, 4, 10, and 19 weeks, and at 25 weeks post randomization.
Results showed that during the 22 weeks, children receiving TMH had significantly better responses than the control group, the researchers found. Their parent-rated ADHD inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning improved, as did their teacher-rated ADHD inattention and school performance.
However, no effect was shown in the teacher-rated hyperactivity or oppositional defiant disorder. Dr. French said this could be attributable to the contextual demands of school versus home, or a change in teacher with kids moved to the next grade during the study period.
The study also showed that telepsychiatrists and therapists adhered to the evidence-based treatment protocols more than 90% of the time. Researchers said that TMH can be effective in training community therapists in evidence-based treatment behavioral management.
Barriers still exist to widespread implementation and adoption of telepsychiatry– with privacy concerns and lack of reimbursement just to name two – but advancement in technology is making the service more readily available, said Dr. French, who presented his findings in a poster at the American Academy of Child and Adolescent Psychiatry meeting.
"Telemedicine is going to be mostly Internet based," he said, "and this opens the potential to anyone with Internet access and a mobile device that has a camera and audio capabilities."
The study was supported by the National Institute of Mental Health. Researchers reported no relevant financial disclosures.
On Twitter @naseemsmiller
AT THE AACAP ANNUAL MEETING
Major finding: During the 22 weeks of the study, children who received telemental health improved significantly in attention-deficit/hyperactivity disorder inattention and hyperactivity, oppositional defiant disorder, school performance, and adaptive functioning.
Data source: The results are based on 223 English-speaking children aged 5.5-12 years with ADHD, along with their parents, who were recruited from local primary care practices in seven rural areas in Washington and Oregon between November 2009 and August 2012.
Disclosures: The study was supported by the National Institute of Mental Health. The researchers said they had no relevant financial disclosures.
CV risk in former light smokers reduced sooner than in heavy smokers
DALLAS – Older people who quit their moderate smoking habit reduced their cigarette-associated cardiovascular risks to the level seen people who had never smoked in as little as 8 years, according to a prospective population study.
This risk reversal occurred much sooner than the 15 years predicted in a 2004 report by the U.S. Surgeon General. This is yet another study to highlight the cardiovascular benefits of smoking cessation, and the message remains the same: "If you’re not a smoker, don’t start. And if you’re a smoker, quit, and quit early," said Dr. Ali Ahmed, professor of cardiovascular disease and gerontology, geriatrics, and palliative care at the University of Alabama at Birmingham and professor of epidemiology at the School of Public Health there. He presented his study at the American Heart Association’s annual scientific sessions.
They narrowed down the Cardiovascular Health Study population to 3,409 adults, 65 years and older, who were free of baseline heart failure. Of the 850 former smokers, roughly 320 had smoked less than 32 pack-years. They had quit within the past 15 years, with the median of 8 years.
Adjusted and age-sex-race adjusted findings during 13 years of follow-up showed that the risk of incident heart failure and cardiovascular mortality were similar between former light smokers and never-smokers.
The light smokers, defined as individuals smoking less than 32 pack-years, who quit smoking less than 15 years ago, had an 18% risk of incident heart failure, compared with 21% in never-smoker; and 14% risk of cardiovascular mortality, compared with 17% in never-smokers. However, their risk of all-cause and noncardiovascular mortality remained significantly higher than in never-smokers.
In previous studies, Dr. Ahmed and his associates had shown that former heavy smokers (32 or more pack-years) may be at increased risk of cardiovascular disease, even after 15 years. (Circulation 2010;122:A17788; Circulation 2011;124:A18263). The team wanted to find out whether smoking less than 32 pack-years would mean earlier reversal of cardiovascular risk.
Dr. Ahmed said that the cardiovascular benefits of quitting smoking, which – unlike mutations or damage to alveolar lining – is reversible, begins within 24 hours after cessation, unless the damage has reached a threshold of no return from heavy smoking.
Dr. Ahmed had no disclosures.
On Twitter @NaseemSMiller
DALLAS – Older people who quit their moderate smoking habit reduced their cigarette-associated cardiovascular risks to the level seen people who had never smoked in as little as 8 years, according to a prospective population study.
This risk reversal occurred much sooner than the 15 years predicted in a 2004 report by the U.S. Surgeon General. This is yet another study to highlight the cardiovascular benefits of smoking cessation, and the message remains the same: "If you’re not a smoker, don’t start. And if you’re a smoker, quit, and quit early," said Dr. Ali Ahmed, professor of cardiovascular disease and gerontology, geriatrics, and palliative care at the University of Alabama at Birmingham and professor of epidemiology at the School of Public Health there. He presented his study at the American Heart Association’s annual scientific sessions.
They narrowed down the Cardiovascular Health Study population to 3,409 adults, 65 years and older, who were free of baseline heart failure. Of the 850 former smokers, roughly 320 had smoked less than 32 pack-years. They had quit within the past 15 years, with the median of 8 years.
Adjusted and age-sex-race adjusted findings during 13 years of follow-up showed that the risk of incident heart failure and cardiovascular mortality were similar between former light smokers and never-smokers.
The light smokers, defined as individuals smoking less than 32 pack-years, who quit smoking less than 15 years ago, had an 18% risk of incident heart failure, compared with 21% in never-smoker; and 14% risk of cardiovascular mortality, compared with 17% in never-smokers. However, their risk of all-cause and noncardiovascular mortality remained significantly higher than in never-smokers.
In previous studies, Dr. Ahmed and his associates had shown that former heavy smokers (32 or more pack-years) may be at increased risk of cardiovascular disease, even after 15 years. (Circulation 2010;122:A17788; Circulation 2011;124:A18263). The team wanted to find out whether smoking less than 32 pack-years would mean earlier reversal of cardiovascular risk.
Dr. Ahmed said that the cardiovascular benefits of quitting smoking, which – unlike mutations or damage to alveolar lining – is reversible, begins within 24 hours after cessation, unless the damage has reached a threshold of no return from heavy smoking.
Dr. Ahmed had no disclosures.
On Twitter @NaseemSMiller
DALLAS – Older people who quit their moderate smoking habit reduced their cigarette-associated cardiovascular risks to the level seen people who had never smoked in as little as 8 years, according to a prospective population study.
This risk reversal occurred much sooner than the 15 years predicted in a 2004 report by the U.S. Surgeon General. This is yet another study to highlight the cardiovascular benefits of smoking cessation, and the message remains the same: "If you’re not a smoker, don’t start. And if you’re a smoker, quit, and quit early," said Dr. Ali Ahmed, professor of cardiovascular disease and gerontology, geriatrics, and palliative care at the University of Alabama at Birmingham and professor of epidemiology at the School of Public Health there. He presented his study at the American Heart Association’s annual scientific sessions.
They narrowed down the Cardiovascular Health Study population to 3,409 adults, 65 years and older, who were free of baseline heart failure. Of the 850 former smokers, roughly 320 had smoked less than 32 pack-years. They had quit within the past 15 years, with the median of 8 years.
Adjusted and age-sex-race adjusted findings during 13 years of follow-up showed that the risk of incident heart failure and cardiovascular mortality were similar between former light smokers and never-smokers.
The light smokers, defined as individuals smoking less than 32 pack-years, who quit smoking less than 15 years ago, had an 18% risk of incident heart failure, compared with 21% in never-smoker; and 14% risk of cardiovascular mortality, compared with 17% in never-smokers. However, their risk of all-cause and noncardiovascular mortality remained significantly higher than in never-smokers.
In previous studies, Dr. Ahmed and his associates had shown that former heavy smokers (32 or more pack-years) may be at increased risk of cardiovascular disease, even after 15 years. (Circulation 2010;122:A17788; Circulation 2011;124:A18263). The team wanted to find out whether smoking less than 32 pack-years would mean earlier reversal of cardiovascular risk.
Dr. Ahmed said that the cardiovascular benefits of quitting smoking, which – unlike mutations or damage to alveolar lining – is reversible, begins within 24 hours after cessation, unless the damage has reached a threshold of no return from heavy smoking.
Dr. Ahmed had no disclosures.
On Twitter @NaseemSMiller
AT THE 2013 AHA SCIENTIFIC SESSIONS
Major finding: Former smokers with less than 32 pack-years had a 14% risk of CV death, compared with 17% in never-smokers. (P = .691)
Data source: Prospective analysis of data from the Cardiovascular Health Study.
Disclosures: Dr. Ahmed had no disclosures.
Mohs surgery site, not type, predicts risk of suture contamination
CHICAGO – Bacterial contamination of sutures is surprisingly common, and periorificial sites have a suture contamination rate of nearly 100%, according to a study of sutures collected during Mohs micrographic surgeries in 182 patients.
There’s no direct correlation between suture contamination and surgery site infection, said Dr. Jeremy Sunseri of Brown University, Providence, R.I., who presented the unpublished study at the annual meeting of the American Society of Dermatologic Surgery. However, knowing the risk factors for suture contamination can help reduce the risk of infections and potential antibiotic overuse, he noted.
"For instance, the use of antibiotic-coated sutures in high-risk contamination sites, or variations on draping techniques in these areas, may prove beneficial," Dr. Sunseri noted.
The investigators removed 338 sutures directly from their sterile surgery sites, and placed them in Petri dishes with a growth medium used for the isolation of gram-positive organisms.
They further classified the sutures based on anatomic locations (17), type of surgical closure (5), and suture type (7).
More than 57% of all sutures had bacterial growth, and almost all of those collected from the nose, mouth/lip, eye/orbit were contaminated.
Sutures collected from the scalp, neck, trunk, and upper and lower extremities had significantly lower risk of contamination, ranging from 0% to 20%, with the exception of the groin, which showed a 100% contamination rate.
Sutures from flap repairs were the most frequently contaminated (71%). Sutures collected from complex closures also had a relatively high rate of contamination (68%).
Sutures from intermediate repairs had a contamination rate of 47%, while grafts, purse string closures, and incomplete closures had a 44% rate.
Staphylococci were the most commonly identified bacteria, notably isolates of of Propionibacterium acnes, Corynebacterium sp., and Rothia dentocariosa.
There were no significant differences in the contamination rates of the seven different types of sutures studied.
"The take-home message is that the suture is long and patients are dirty, so be careful where you put that suture," Dr. Sunseri said during his presentation.
Dr. Sunseri had no financial conflicts to disclose.
On Twitter @NaseemSMiller
CHICAGO – Bacterial contamination of sutures is surprisingly common, and periorificial sites have a suture contamination rate of nearly 100%, according to a study of sutures collected during Mohs micrographic surgeries in 182 patients.
There’s no direct correlation between suture contamination and surgery site infection, said Dr. Jeremy Sunseri of Brown University, Providence, R.I., who presented the unpublished study at the annual meeting of the American Society of Dermatologic Surgery. However, knowing the risk factors for suture contamination can help reduce the risk of infections and potential antibiotic overuse, he noted.
"For instance, the use of antibiotic-coated sutures in high-risk contamination sites, or variations on draping techniques in these areas, may prove beneficial," Dr. Sunseri noted.
The investigators removed 338 sutures directly from their sterile surgery sites, and placed them in Petri dishes with a growth medium used for the isolation of gram-positive organisms.
They further classified the sutures based on anatomic locations (17), type of surgical closure (5), and suture type (7).
More than 57% of all sutures had bacterial growth, and almost all of those collected from the nose, mouth/lip, eye/orbit were contaminated.
Sutures collected from the scalp, neck, trunk, and upper and lower extremities had significantly lower risk of contamination, ranging from 0% to 20%, with the exception of the groin, which showed a 100% contamination rate.
Sutures from flap repairs were the most frequently contaminated (71%). Sutures collected from complex closures also had a relatively high rate of contamination (68%).
Sutures from intermediate repairs had a contamination rate of 47%, while grafts, purse string closures, and incomplete closures had a 44% rate.
Staphylococci were the most commonly identified bacteria, notably isolates of of Propionibacterium acnes, Corynebacterium sp., and Rothia dentocariosa.
There were no significant differences in the contamination rates of the seven different types of sutures studied.
"The take-home message is that the suture is long and patients are dirty, so be careful where you put that suture," Dr. Sunseri said during his presentation.
Dr. Sunseri had no financial conflicts to disclose.
On Twitter @NaseemSMiller
CHICAGO – Bacterial contamination of sutures is surprisingly common, and periorificial sites have a suture contamination rate of nearly 100%, according to a study of sutures collected during Mohs micrographic surgeries in 182 patients.
There’s no direct correlation between suture contamination and surgery site infection, said Dr. Jeremy Sunseri of Brown University, Providence, R.I., who presented the unpublished study at the annual meeting of the American Society of Dermatologic Surgery. However, knowing the risk factors for suture contamination can help reduce the risk of infections and potential antibiotic overuse, he noted.
"For instance, the use of antibiotic-coated sutures in high-risk contamination sites, or variations on draping techniques in these areas, may prove beneficial," Dr. Sunseri noted.
The investigators removed 338 sutures directly from their sterile surgery sites, and placed them in Petri dishes with a growth medium used for the isolation of gram-positive organisms.
They further classified the sutures based on anatomic locations (17), type of surgical closure (5), and suture type (7).
More than 57% of all sutures had bacterial growth, and almost all of those collected from the nose, mouth/lip, eye/orbit were contaminated.
Sutures collected from the scalp, neck, trunk, and upper and lower extremities had significantly lower risk of contamination, ranging from 0% to 20%, with the exception of the groin, which showed a 100% contamination rate.
Sutures from flap repairs were the most frequently contaminated (71%). Sutures collected from complex closures also had a relatively high rate of contamination (68%).
Sutures from intermediate repairs had a contamination rate of 47%, while grafts, purse string closures, and incomplete closures had a 44% rate.
Staphylococci were the most commonly identified bacteria, notably isolates of of Propionibacterium acnes, Corynebacterium sp., and Rothia dentocariosa.
There were no significant differences in the contamination rates of the seven different types of sutures studied.
"The take-home message is that the suture is long and patients are dirty, so be careful where you put that suture," Dr. Sunseri said during his presentation.
Dr. Sunseri had no financial conflicts to disclose.
On Twitter @NaseemSMiller
AT THE ASDS ANNUAL MEETING
Major finding: Nearly 100% of sutures removed from periorificial surfaces showed bacterial contamination.
Data source: Analysis of bacterial growth from 338 sutures removed directly from the sterile surgery site in 182 patients.
Disclosures: Dr. Sunseri had no financial conflicts to disclose.
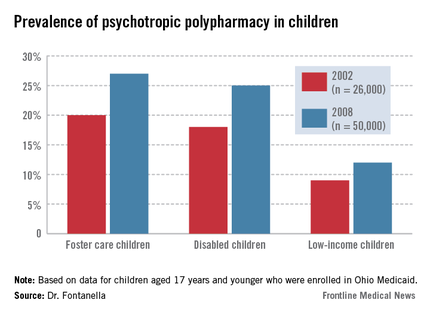
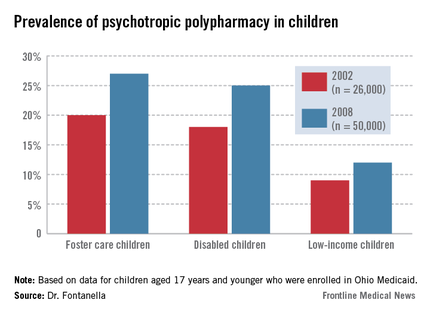
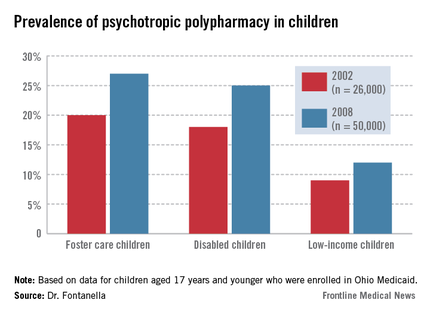
Ohio Medicaid data document rising polypharmacy in foster children
ORLANDO – Prescribing of three or more psychotropic medications has increased among foster children enrolled in Medicaid, based on an analysis of claims data in Ohio. The findings of polypharmacy are raising red flags about oversight and monitoring of psychotropic medication use among high-risk youth.
By 2008, nearly a quarter of foster care and disabled children in the Ohio Medicaid program were prescribed three or more psychiatric medications. Nearly one-fifth of them were prescribed medications from three or more drug classes, with the most common combination being stimulants, antipsychotics, and alpha-agonists.
The findings make a powerful case for system-wide oversight and monitoring of psychotropic prescribing practices in the Medicaid population, especially for children in foster care, said Cynthia A. Fontanella, Ph.D., of the Ohio State University, Columbus, who led the study and presented her findings at the annual meeting of the American Academy of Child and Adolescent Psychiatry. "We don’t know if these kids are doing better ... The increase has "occurred despite lack of data on safety and efficacy of multiple drug combination and existing concerns about adverse effects of drug-drug interactions."
A 2012 report by the Government Accountability Office that showed 18% of foster children were taking psychotropic medications. That report additionally noted, however, that 30% of the children who may have needed mental health services hadn't received them.
The rising rates of polypharmacy, especially in children enrolled in Medicaid, have been documented in other studies. But the accumulating data implies polypharmacy is pervasive in at-risk children. "It’s a growing trend," said Susan dosReis, Ph.D., associate professor at the University of Maryland School of Pharmacy, Baltimore, who has studied psychiatric prescription patterns among youth. She was not involved in the study.
Dr. dosReis acknowledged that the issue is complex, especially in the cases of children with severe conditions. Clinicians face families who are looking for a way to manage their child or to keep them in school. "And once you have a child on a combination, and there’s improvement, the thought of taking away the medications is hard to accept, because [the family is] afraid that the condition will worsen again."
Also, follow-up has been problematic, with data that don’t clearly indicate whether the children were on several medications for a short period of time until they were stabilized, or the whether the polypharmacy lasted longer. Data for children enrolled in private insurance are lacking, and prescribing is difficult to track for children in foster care because they move frequently.
Dr. Fontanella and her colleagues compared polypharmacy patterns and rates in foster care, disabled, and low-income youth aged 17 years and younger enrolled in Ohio Medicaid between 2002 (n = 26,000) and 2008 (n = 50,000).
The two outcome measures — any polypharmacy (three or more medications) — and multiclass polypharmacy (three or more medications from different drug classes) increased over time across all three groups. Polypharmacy increased from 9% to 12% for low-income youth; from 18% to 25% in disabled youth; and from 20% to 27% in foster care youth.
Combination therapies that increased the most during the time of the study were prescriptions of two or more antipsychotics, two or more stimulants, and antipsychotics with stimulants and other psychotropic medications excluding antidepressants.
The percentage of foster children who were prescribed two or more antipsychotics increased from 5% in 2002 to 10% in 2008, compared with 6% to 9% among children with disabilities, and 3% to 5% among low-income children.
The percentage of foster children who were prescribed two or more stimulants also showed a bigger jump – from 1.5% in 2002 to 8% in 2008 – compared with 1.5% to 6% among children with disabilities, and 3% to 7% among low-income children.
Meanwhile, multiclass polypharmacy has been increasing over the years, from 14% during 1996-1999 to 20% during 2004-2007. Even when it’s indicated, polypharmacy increases the risk for adverse events and drug-drug interactions, creates a complicated drug regimen and the need for more medication, and leads to higher costs, the researchers said.
Researchers also found some within class and between-class prescribing trends.
While the prescription rates for two or more antipsychotics and stimulants increased, the rate of combination antidepressant prescribing decreased.
It’s not clear if the findings can be generalized to other states and to non-Medicaid populations, the researchers noted. Also, a 30-day window as a measure of prevalence may lead to overestimation of polypharmacy, and, prescriptions don’t necessarily translate to adherence.
Dr. Fontanella and Dr. dosReis had no disclosures.
On Twitter @NaseemSMiller
ORLANDO – Prescribing of three or more psychotropic medications has increased among foster children enrolled in Medicaid, based on an analysis of claims data in Ohio. The findings of polypharmacy are raising red flags about oversight and monitoring of psychotropic medication use among high-risk youth.
By 2008, nearly a quarter of foster care and disabled children in the Ohio Medicaid program were prescribed three or more psychiatric medications. Nearly one-fifth of them were prescribed medications from three or more drug classes, with the most common combination being stimulants, antipsychotics, and alpha-agonists.
The findings make a powerful case for system-wide oversight and monitoring of psychotropic prescribing practices in the Medicaid population, especially for children in foster care, said Cynthia A. Fontanella, Ph.D., of the Ohio State University, Columbus, who led the study and presented her findings at the annual meeting of the American Academy of Child and Adolescent Psychiatry. "We don’t know if these kids are doing better ... The increase has "occurred despite lack of data on safety and efficacy of multiple drug combination and existing concerns about adverse effects of drug-drug interactions."
A 2012 report by the Government Accountability Office that showed 18% of foster children were taking psychotropic medications. That report additionally noted, however, that 30% of the children who may have needed mental health services hadn't received them.
The rising rates of polypharmacy, especially in children enrolled in Medicaid, have been documented in other studies. But the accumulating data implies polypharmacy is pervasive in at-risk children. "It’s a growing trend," said Susan dosReis, Ph.D., associate professor at the University of Maryland School of Pharmacy, Baltimore, who has studied psychiatric prescription patterns among youth. She was not involved in the study.
Dr. dosReis acknowledged that the issue is complex, especially in the cases of children with severe conditions. Clinicians face families who are looking for a way to manage their child or to keep them in school. "And once you have a child on a combination, and there’s improvement, the thought of taking away the medications is hard to accept, because [the family is] afraid that the condition will worsen again."
Also, follow-up has been problematic, with data that don’t clearly indicate whether the children were on several medications for a short period of time until they were stabilized, or the whether the polypharmacy lasted longer. Data for children enrolled in private insurance are lacking, and prescribing is difficult to track for children in foster care because they move frequently.
Dr. Fontanella and her colleagues compared polypharmacy patterns and rates in foster care, disabled, and low-income youth aged 17 years and younger enrolled in Ohio Medicaid between 2002 (n = 26,000) and 2008 (n = 50,000).
The two outcome measures — any polypharmacy (three or more medications) — and multiclass polypharmacy (three or more medications from different drug classes) increased over time across all three groups. Polypharmacy increased from 9% to 12% for low-income youth; from 18% to 25% in disabled youth; and from 20% to 27% in foster care youth.
Combination therapies that increased the most during the time of the study were prescriptions of two or more antipsychotics, two or more stimulants, and antipsychotics with stimulants and other psychotropic medications excluding antidepressants.
The percentage of foster children who were prescribed two or more antipsychotics increased from 5% in 2002 to 10% in 2008, compared with 6% to 9% among children with disabilities, and 3% to 5% among low-income children.
The percentage of foster children who were prescribed two or more stimulants also showed a bigger jump – from 1.5% in 2002 to 8% in 2008 – compared with 1.5% to 6% among children with disabilities, and 3% to 7% among low-income children.
Meanwhile, multiclass polypharmacy has been increasing over the years, from 14% during 1996-1999 to 20% during 2004-2007. Even when it’s indicated, polypharmacy increases the risk for adverse events and drug-drug interactions, creates a complicated drug regimen and the need for more medication, and leads to higher costs, the researchers said.
Researchers also found some within class and between-class prescribing trends.
While the prescription rates for two or more antipsychotics and stimulants increased, the rate of combination antidepressant prescribing decreased.
It’s not clear if the findings can be generalized to other states and to non-Medicaid populations, the researchers noted. Also, a 30-day window as a measure of prevalence may lead to overestimation of polypharmacy, and, prescriptions don’t necessarily translate to adherence.
Dr. Fontanella and Dr. dosReis had no disclosures.
On Twitter @NaseemSMiller
ORLANDO – Prescribing of three or more psychotropic medications has increased among foster children enrolled in Medicaid, based on an analysis of claims data in Ohio. The findings of polypharmacy are raising red flags about oversight and monitoring of psychotropic medication use among high-risk youth.
By 2008, nearly a quarter of foster care and disabled children in the Ohio Medicaid program were prescribed three or more psychiatric medications. Nearly one-fifth of them were prescribed medications from three or more drug classes, with the most common combination being stimulants, antipsychotics, and alpha-agonists.
The findings make a powerful case for system-wide oversight and monitoring of psychotropic prescribing practices in the Medicaid population, especially for children in foster care, said Cynthia A. Fontanella, Ph.D., of the Ohio State University, Columbus, who led the study and presented her findings at the annual meeting of the American Academy of Child and Adolescent Psychiatry. "We don’t know if these kids are doing better ... The increase has "occurred despite lack of data on safety and efficacy of multiple drug combination and existing concerns about adverse effects of drug-drug interactions."
A 2012 report by the Government Accountability Office that showed 18% of foster children were taking psychotropic medications. That report additionally noted, however, that 30% of the children who may have needed mental health services hadn't received them.
The rising rates of polypharmacy, especially in children enrolled in Medicaid, have been documented in other studies. But the accumulating data implies polypharmacy is pervasive in at-risk children. "It’s a growing trend," said Susan dosReis, Ph.D., associate professor at the University of Maryland School of Pharmacy, Baltimore, who has studied psychiatric prescription patterns among youth. She was not involved in the study.
Dr. dosReis acknowledged that the issue is complex, especially in the cases of children with severe conditions. Clinicians face families who are looking for a way to manage their child or to keep them in school. "And once you have a child on a combination, and there’s improvement, the thought of taking away the medications is hard to accept, because [the family is] afraid that the condition will worsen again."
Also, follow-up has been problematic, with data that don’t clearly indicate whether the children were on several medications for a short period of time until they were stabilized, or the whether the polypharmacy lasted longer. Data for children enrolled in private insurance are lacking, and prescribing is difficult to track for children in foster care because they move frequently.
Dr. Fontanella and her colleagues compared polypharmacy patterns and rates in foster care, disabled, and low-income youth aged 17 years and younger enrolled in Ohio Medicaid between 2002 (n = 26,000) and 2008 (n = 50,000).
The two outcome measures — any polypharmacy (three or more medications) — and multiclass polypharmacy (three or more medications from different drug classes) increased over time across all three groups. Polypharmacy increased from 9% to 12% for low-income youth; from 18% to 25% in disabled youth; and from 20% to 27% in foster care youth.
Combination therapies that increased the most during the time of the study were prescriptions of two or more antipsychotics, two or more stimulants, and antipsychotics with stimulants and other psychotropic medications excluding antidepressants.
The percentage of foster children who were prescribed two or more antipsychotics increased from 5% in 2002 to 10% in 2008, compared with 6% to 9% among children with disabilities, and 3% to 5% among low-income children.
The percentage of foster children who were prescribed two or more stimulants also showed a bigger jump – from 1.5% in 2002 to 8% in 2008 – compared with 1.5% to 6% among children with disabilities, and 3% to 7% among low-income children.
Meanwhile, multiclass polypharmacy has been increasing over the years, from 14% during 1996-1999 to 20% during 2004-2007. Even when it’s indicated, polypharmacy increases the risk for adverse events and drug-drug interactions, creates a complicated drug regimen and the need for more medication, and leads to higher costs, the researchers said.
Researchers also found some within class and between-class prescribing trends.
While the prescription rates for two or more antipsychotics and stimulants increased, the rate of combination antidepressant prescribing decreased.
It’s not clear if the findings can be generalized to other states and to non-Medicaid populations, the researchers noted. Also, a 30-day window as a measure of prevalence may lead to overestimation of polypharmacy, and, prescriptions don’t necessarily translate to adherence.
Dr. Fontanella and Dr. dosReis had no disclosures.
On Twitter @NaseemSMiller
AT THE AACAP ANNUAL MEETING
Major finding: Based on 2008 Medicaid data, the rate of polypharmacy was 27% in foster children.
Data source: Foster care, disabled, and low income youth aged 17 years and younger enrolled in Ohio Medicaid between 2002 (n = 26,000) and 2008 (n = 50,000).
Disclosures: Dr. Fontanella and Dr. dosReis had no disclosures.
Endocrinology association rejects new ACC/AHA obesity, cholesterol guidelines
One of the nation’s leading clinical endocrinology associations is rejecting the new cholesterol and obesity guidelines issued by the American Heart Association and the American College of Cardiology in November, saying that the already-controversial new risk calculator is outdated and that the guidelines are incompatible with the association’s existing guidelines.
"Additionally, there are questions and concerns regarding the scientific basis for these new guidelines and the populations of patients at risk from disease who are underserved or ill-considered in these new strategies," the American Association of Clinical Endocrinologists (AACE) said in a statement to the press issued Dec. 23, nearly a month after it was released to its members.
The ACC and AHA released new cardiovascular disease prevention guidelines focused on cholesterol treatment, assessment of cardiovascular risk, lifestyle management, and management of overweight and obesity.
The cholesterol management guidelines quickly became controversial, especially after two Harvard researchers questioned the validity of the new Cardiovascular Risk Calculator.
AACE too has taken issue with the risk calculator, saying that it’s "already outdated," and that "it is based upon outmoded data, does not model the totality of the U.S. population, has not been validated, and therefore has only limited applicability."
The association said in its statement that it agreed with the use of full-dose statins, but disagreed with removing low-density lipoprotein (LDL) goals and the notion that statin therapy alone is sufficient for all at-risk patients.
AACE is not alone in declining to endorse the new cholesterol guidelines. In a separate statement earlier, the National Lipid Association took issue with removing LDL goals, saying it did “not find evidence-based support for the Panel’s recommendation for removing LDL-C (and non-HDL-C) treatment targets.”
ACC and AHA leaders called a last-minute press conference during the AHA’s annual meeting in Dallas in November, defending the cholesterol guidelines and the new risk calculator.
AACE also says that the new obesity guidelines are limited in their scope and do not include data after 2011. “These new guidelines fail to classify obesity as a disease and continue the paradigm of BMI-centric risk stratification, both of which are contrary to recently stated AACE positions.”
AACE said that the new ACC/AHA guidelines “are now among many available guidelines, including the AACE lipid guidelines, to which clinicians can refer.”
nmiller@frontlinemedcom.com
On Twitter @naseemsmiller
One of the nation’s leading clinical endocrinology associations is rejecting the new cholesterol and obesity guidelines issued by the American Heart Association and the American College of Cardiology in November, saying that the already-controversial new risk calculator is outdated and that the guidelines are incompatible with the association’s existing guidelines.
"Additionally, there are questions and concerns regarding the scientific basis for these new guidelines and the populations of patients at risk from disease who are underserved or ill-considered in these new strategies," the American Association of Clinical Endocrinologists (AACE) said in a statement to the press issued Dec. 23, nearly a month after it was released to its members.
The ACC and AHA released new cardiovascular disease prevention guidelines focused on cholesterol treatment, assessment of cardiovascular risk, lifestyle management, and management of overweight and obesity.
The cholesterol management guidelines quickly became controversial, especially after two Harvard researchers questioned the validity of the new Cardiovascular Risk Calculator.
AACE too has taken issue with the risk calculator, saying that it’s "already outdated," and that "it is based upon outmoded data, does not model the totality of the U.S. population, has not been validated, and therefore has only limited applicability."
The association said in its statement that it agreed with the use of full-dose statins, but disagreed with removing low-density lipoprotein (LDL) goals and the notion that statin therapy alone is sufficient for all at-risk patients.
AACE is not alone in declining to endorse the new cholesterol guidelines. In a separate statement earlier, the National Lipid Association took issue with removing LDL goals, saying it did “not find evidence-based support for the Panel’s recommendation for removing LDL-C (and non-HDL-C) treatment targets.”
ACC and AHA leaders called a last-minute press conference during the AHA’s annual meeting in Dallas in November, defending the cholesterol guidelines and the new risk calculator.
AACE also says that the new obesity guidelines are limited in their scope and do not include data after 2011. “These new guidelines fail to classify obesity as a disease and continue the paradigm of BMI-centric risk stratification, both of which are contrary to recently stated AACE positions.”
AACE said that the new ACC/AHA guidelines “are now among many available guidelines, including the AACE lipid guidelines, to which clinicians can refer.”
nmiller@frontlinemedcom.com
On Twitter @naseemsmiller
One of the nation’s leading clinical endocrinology associations is rejecting the new cholesterol and obesity guidelines issued by the American Heart Association and the American College of Cardiology in November, saying that the already-controversial new risk calculator is outdated and that the guidelines are incompatible with the association’s existing guidelines.
"Additionally, there are questions and concerns regarding the scientific basis for these new guidelines and the populations of patients at risk from disease who are underserved or ill-considered in these new strategies," the American Association of Clinical Endocrinologists (AACE) said in a statement to the press issued Dec. 23, nearly a month after it was released to its members.
The ACC and AHA released new cardiovascular disease prevention guidelines focused on cholesterol treatment, assessment of cardiovascular risk, lifestyle management, and management of overweight and obesity.
The cholesterol management guidelines quickly became controversial, especially after two Harvard researchers questioned the validity of the new Cardiovascular Risk Calculator.
AACE too has taken issue with the risk calculator, saying that it’s "already outdated," and that "it is based upon outmoded data, does not model the totality of the U.S. population, has not been validated, and therefore has only limited applicability."
The association said in its statement that it agreed with the use of full-dose statins, but disagreed with removing low-density lipoprotein (LDL) goals and the notion that statin therapy alone is sufficient for all at-risk patients.
AACE is not alone in declining to endorse the new cholesterol guidelines. In a separate statement earlier, the National Lipid Association took issue with removing LDL goals, saying it did “not find evidence-based support for the Panel’s recommendation for removing LDL-C (and non-HDL-C) treatment targets.”
ACC and AHA leaders called a last-minute press conference during the AHA’s annual meeting in Dallas in November, defending the cholesterol guidelines and the new risk calculator.
AACE also says that the new obesity guidelines are limited in their scope and do not include data after 2011. “These new guidelines fail to classify obesity as a disease and continue the paradigm of BMI-centric risk stratification, both of which are contrary to recently stated AACE positions.”
AACE said that the new ACC/AHA guidelines “are now among many available guidelines, including the AACE lipid guidelines, to which clinicians can refer.”
nmiller@frontlinemedcom.com
On Twitter @naseemsmiller
Mechanical device as effective as manual chest compressions
AMSTERDAM – LUCAS, a mechanical chest compression device, could be as effective as manual chest compressions, based on results from a multicenter, randomized controlled trial of 5,000 cardiac arrest patients.
The LINC (LUCAS in Cardiac Arrest) study showed that the device was no better than manual chest compression at improving the 4-hour survivals of cardiac arrest patients. Patients exposed to the device were not harmed, however, and their 6-month survival rates and neurologic outcomes were similar to those of patients who received manual compressions, said Dr. Sten Rubertsson, the principle investigator of the study and a consultant for the device’s manufacturer, Physio-Control.
One of several mechanical chest compression devices available in the market, LUCAS has a piston and suction cup mechanism that performs chest compressions at guideline recommended rates. The device also permits simultaneous use of a defibrillator.
In a study was conducted between 2008 and 2013, about 2,600 of 5,000 cardiac arrest patients were randomized to either LUCAS or manual compression. The other patients were excluded from the study because they had traumatic cardiac arrest, were pregnant, were defibrillated before LUCAS was on scene, or had a return of spontaneous circulation.
Patients were on average 69 years old and most were men.
The primary endpoint of the study, 4-hour survival, was comparable for both groups at 23.6% for LUCAS and 23.7% for manual compressions.
The study’s secondary endpoint – survival up to 6 months with good neurologic outcome – similarly was comparable at 8.5% for LUCAS and 7.6% for manual compressions.
Conducting a study for several years in a pre-hospital setting is rather difficult, said Dr. Patrick Goldstein of Lille University Hospital France, who commented on the study at the meeting. The results of the trial could be considered neutral, but "I think it is positive for many reasons."
Mechanical chest compressions can be useful in several subgroups, including those patients who need long-term CPR and for those in the non–heart-beating donors programs, for example.
Dr. Rubertsson said that in the future, the device could be used to individualize care, by considering the compressions and EKG, and deciding when to do the interventions.
The LINC study was initiated by Uppsala (Sweden) University and sponsored by Physio-Control/Jolife AB. Dr. Rubertsson has received consultation fee from Physio-Control/Jolife AB. Dr. Goldstein had no relevant conflicts of interest.
On Twitter @NaseemSMiller
AMSTERDAM – LUCAS, a mechanical chest compression device, could be as effective as manual chest compressions, based on results from a multicenter, randomized controlled trial of 5,000 cardiac arrest patients.
The LINC (LUCAS in Cardiac Arrest) study showed that the device was no better than manual chest compression at improving the 4-hour survivals of cardiac arrest patients. Patients exposed to the device were not harmed, however, and their 6-month survival rates and neurologic outcomes were similar to those of patients who received manual compressions, said Dr. Sten Rubertsson, the principle investigator of the study and a consultant for the device’s manufacturer, Physio-Control.
One of several mechanical chest compression devices available in the market, LUCAS has a piston and suction cup mechanism that performs chest compressions at guideline recommended rates. The device also permits simultaneous use of a defibrillator.
In a study was conducted between 2008 and 2013, about 2,600 of 5,000 cardiac arrest patients were randomized to either LUCAS or manual compression. The other patients were excluded from the study because they had traumatic cardiac arrest, were pregnant, were defibrillated before LUCAS was on scene, or had a return of spontaneous circulation.
Patients were on average 69 years old and most were men.
The primary endpoint of the study, 4-hour survival, was comparable for both groups at 23.6% for LUCAS and 23.7% for manual compressions.
The study’s secondary endpoint – survival up to 6 months with good neurologic outcome – similarly was comparable at 8.5% for LUCAS and 7.6% for manual compressions.
Conducting a study for several years in a pre-hospital setting is rather difficult, said Dr. Patrick Goldstein of Lille University Hospital France, who commented on the study at the meeting. The results of the trial could be considered neutral, but "I think it is positive for many reasons."
Mechanical chest compressions can be useful in several subgroups, including those patients who need long-term CPR and for those in the non–heart-beating donors programs, for example.
Dr. Rubertsson said that in the future, the device could be used to individualize care, by considering the compressions and EKG, and deciding when to do the interventions.
The LINC study was initiated by Uppsala (Sweden) University and sponsored by Physio-Control/Jolife AB. Dr. Rubertsson has received consultation fee from Physio-Control/Jolife AB. Dr. Goldstein had no relevant conflicts of interest.
On Twitter @NaseemSMiller
AMSTERDAM – LUCAS, a mechanical chest compression device, could be as effective as manual chest compressions, based on results from a multicenter, randomized controlled trial of 5,000 cardiac arrest patients.
The LINC (LUCAS in Cardiac Arrest) study showed that the device was no better than manual chest compression at improving the 4-hour survivals of cardiac arrest patients. Patients exposed to the device were not harmed, however, and their 6-month survival rates and neurologic outcomes were similar to those of patients who received manual compressions, said Dr. Sten Rubertsson, the principle investigator of the study and a consultant for the device’s manufacturer, Physio-Control.
One of several mechanical chest compression devices available in the market, LUCAS has a piston and suction cup mechanism that performs chest compressions at guideline recommended rates. The device also permits simultaneous use of a defibrillator.
In a study was conducted between 2008 and 2013, about 2,600 of 5,000 cardiac arrest patients were randomized to either LUCAS or manual compression. The other patients were excluded from the study because they had traumatic cardiac arrest, were pregnant, were defibrillated before LUCAS was on scene, or had a return of spontaneous circulation.
Patients were on average 69 years old and most were men.
The primary endpoint of the study, 4-hour survival, was comparable for both groups at 23.6% for LUCAS and 23.7% for manual compressions.
The study’s secondary endpoint – survival up to 6 months with good neurologic outcome – similarly was comparable at 8.5% for LUCAS and 7.6% for manual compressions.
Conducting a study for several years in a pre-hospital setting is rather difficult, said Dr. Patrick Goldstein of Lille University Hospital France, who commented on the study at the meeting. The results of the trial could be considered neutral, but "I think it is positive for many reasons."
Mechanical chest compressions can be useful in several subgroups, including those patients who need long-term CPR and for those in the non–heart-beating donors programs, for example.
Dr. Rubertsson said that in the future, the device could be used to individualize care, by considering the compressions and EKG, and deciding when to do the interventions.
The LINC study was initiated by Uppsala (Sweden) University and sponsored by Physio-Control/Jolife AB. Dr. Rubertsson has received consultation fee from Physio-Control/Jolife AB. Dr. Goldstein had no relevant conflicts of interest.
On Twitter @NaseemSMiller
AT THE ESC CONGRESS 2013
Major finding: LUCAS did not improve patients’ 4-hour survival, compared with manual CPR (23.6% in LUCAS vs. 23.7%; P = 1.00)
Data source: A multicenter, randomized controlled trial of 5,000 cardiac arrest patients.
Disclosures: The study was initiated by Uppsala (Sweden) University and sponsored by Physio-Control/Jolife AB. Dr. Rubertsson has received consultation fee from Physio-Control/Jolife AB. Dr. Goldstein had no relevant conflicts of interest.
VIDEO: What's ahead for chronic myelogenous leukemia?
NEW ORLEANS – Available medications to treat CML are giving rise to new questions. For instance, why do some patients respond to some medications better than others? How can side effects best be managed? And how can treatment be stopped safely?
In an exclusive interview at the American Society of Hematology's annual meeting, Dr. Richard E. Clark of Royal Liverpool University Hospital, Liverpool, United Kingdom, provides an overview of the field and its future.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Available medications to treat CML are giving rise to new questions. For instance, why do some patients respond to some medications better than others? How can side effects best be managed? And how can treatment be stopped safely?
In an exclusive interview at the American Society of Hematology's annual meeting, Dr. Richard E. Clark of Royal Liverpool University Hospital, Liverpool, United Kingdom, provides an overview of the field and its future.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Available medications to treat CML are giving rise to new questions. For instance, why do some patients respond to some medications better than others? How can side effects best be managed? And how can treatment be stopped safely?
In an exclusive interview at the American Society of Hematology's annual meeting, Dr. Richard E. Clark of Royal Liverpool University Hospital, Liverpool, United Kingdom, provides an overview of the field and its future.