User login
PHM Strategic Planning Roundtable
Hospitalists are the fastest growing segment of physicians in the United States.1 Given the growing field of Pediatric Hospital Medicine (PHM) and the need to define strategic direction, the Society of Hospital Medicine (SHM), the American Academy of Pediatrics (AAP), and the Academic Pediatric Association (APA) sponsored a strategic planning meeting in February 2009 that brought together 22 PHM leaders to discuss the future of the field.
PHM is at a critical juncture in terms of clinical practice, research, workforce issues, and quality improvement. The field has developed sufficiently to produce leaders capable of setting an agenda and moving forward. A discussion with the American Board of Pediatrics (ABP) by PHM leaders from the AAP, APA, and SHM at the Pediatric Hospital Medicine 2007 Conference regarding subspecialty designation stimulated convening the PHM Strategic Planning Roundtable to address the task of coordinating further development of PHM (Table 1).
|
| Develop a strategic vision for the role of PHM in the future of children's health care |
| Describe the current gaps between the vision and today's reality |
| Develop a common understanding regarding current initiatives in PHM domains of clinical practice, quality, research, and workforce |
| Determine the method(s) by which participants can be organized to accomplish additional initiatives to implement the vision |
| Identify and prioritize key strategic initiatives |
| Assign accountability and determine next steps and timeline to implement the selected initiatives |
The objective of this article is to describe: (1) the Strategic Planning Roundtable's vision for the field of pediatric hospital medicine; (2) the generation and progress on specific initiatives in clinical practice, quality, research, and workforce identified by the Strategic Planning Roundtable; and (3) issues in the designation of PHM as a subspecialty.
METHODS
The PHM Strategic Planning Roundtable was conducted by a facilitator (S.M.) during a 2‐day retreat using established healthcare strategic planning methods.2
Participants were the existing PHM leaders from the AAP, APA, and SHM, as well as other national leaders in clinical practice, quality, research, and workforce. Development of the vision statement was a key step in which the participants developed a consensus‐based aspirational view of the future. The draft version of the vision statement was initially developed after extensive interviews with key stakeholders and experts in PHM, and was revised by the participants in the course of a facilitated group discussion during the retreat. Following creation of the vision statement, the group then defined the elements of transformation pertaining to PHM and detailed the components of the vision.
Analysis of internal and external environmental factors was critical in the strategic planning process. This type of analysis, detailing the current state of PHM practice, permitted the strategic planners to understand the gaps that existed between the aspirational vision statement and today's reality, and set the stage to identify and implement initiatives to achieve the vision. Several months before the meeting, 4 expert panels comprised of PHM specialists representing a variety of academic and clinical practice settings were brought together via e‐mail and conference calls to focus on 4 domains of PHM: clinical practice, quality of care, research, and workforce. These groups were asked to describe the current status, challenges, and opportunities in these areas. Combining literature review and key stakeholder interviews, their findings and recommendations were distilled into brief summaries that were presented at the Roundtable meeting. Following the presentations, the participants, working in small groups representing all areas of focus,provided additional feedback.
Following the creation of a consensus vision statement and review of internal and external factors, the participants worked to identify specific initiatives in the 4 domains that would advance the field towards the goals contained in the vision statement. These initiatives were grouped into categories. Initiatives by category were scored and prioritized according to predetermined criteria including potential impact, cost, operational complexity, and achievability.
For each initiative selected, the group developed targets and metrics that would be used to track progress. Assigning leadership, accountability, and a timeline to each of the selected projects completed the implementation plan. In addition, the group developed an organizational structure to provide oversight for the overall process, and designated individuals representing the sponsoring organizations into those roles. In conclusion, the group discussed potential structures to guide the future of PHM.
CLINICAL PRACTICE
The Roundtable defined clinical practice for PHM as the general medical care of the hospitalized child, including direct patient care and leadership of the inpatient service. Clinical practice is affected by a number of current national trends including: fewer primary care providers interested in, or with the time to provide, inpatient care; resident work hour restrictions; increasing complexity of clinical issues; and increasing availability of pediatric hospitalists. At the hospital level, clinical practice is affected by increasing need for quality and safety measures, electronic health records and computerized physician order entry, and mounting financial pressures on the hospital system. Hospitalists are assuming more roles in leading quality and safety initiatives, creating computerized systems that address children's needs, and creating financially viable systems of quality pediatric care.3 Hospitalists' clinical care and leadership roles are emerging, and therefore the field faces training and mentorship issues.
Progress to date in this area includes 2 textbooks that define a scope of knowledge and practice, and a newly developed journal in PHM. Core competencies in PHM have been published and provide further refinement of scope and a template for future training.4
Multiple opportunities exist for hospitalists to establish themselves as clinical leaders. Hospitalists can become the preferred providers for hospitalized chronically ill children, with specific initiatives to improve care coordination and multidisciplinary communication. In addition to care coordination and decreasing length of stay, hospitalists, with their intimate knowledge of hospital operations, can be leaders in hospital capacity management and patient flow to increase operational efficiency. Hospitalists can expand evidence‐based guidelines for, and data about, inpatient conditions, and explore the effect of workload and hours on patient care. In addition, there is an expanding role into administrative areas, as well as alternate care arenas, such as: intensive care support (pediatric and neonatal), transport, sedation, palliative care, and pain management. Activities in administrative and alternate care areas have profound direct affects on patient care, as well as providing value added services and additional revenue streams which can further support clinical needs. Finally, achieving quality targets will likely be increasingly linked to payment, so hospitalists may play a key role in the incentives paid to their hospitals. Meeting these challenges will further solidify the standing of hospitalists in the clinical realm.
QUALITY
National and governmental agencies have influenced quality and performance improvement measurements in adult healthcare, resulting in improvements in adult healthcare quality measurement.5 There is limited similar influence or measure development in pediatric medicine, so the quality chasm between adult and child healthcare has widened. Few resources are invested in improving quality and safety of pediatric inpatient care. Of the 18 private health insurance plans' quality and pay for performance programs identified by Leapfrog, only 17% developed pediatric‐specific inpatient measures.6 Only 5 of 40 controlled trials of quality improvement efforts for children published between 1980 and 1998 addressed inpatient problems.7
There have been recent efforts at the national level addressing these issues, highlighted by the introduction of The Children's Health Care Quality Act, in 2007. Early studies in PHM systems focused on overall operational efficiency, documenting 9% to 16% decreases in length of stay and cost compared to traditional models of care.8 Conway et al. identified higher reported adherence to evidence‐based care for hospitalists compared to community pediatricians.9 However, Landrigan et al. demonstrated that there is still large variation in care that exists in the management of common inpatient diagnoses, lacking strong evidence‐based guidelines even among pediatric hospitalists.10 Moreover, there have been no significant studies reviewing the impact of pediatric hospitalists on safety of inpatient care. Magnifying these challenges is the reality that our healthcare system is fragmented with various entities scrambling to define, measure, and compare the effectiveness and safety of pediatric healthcare.
These challenges create an opportunity for PHM to develop a model of how to deliver the highest quality and safest care to our patients. The solution is complex and will take cooperation at many levels of our healthcare system. Improving the safety and quality of care for children in all settings of inpatient care in the United States may best be accomplished via an effective collaborative. This collaborative should be comprehensive and inclusive, and focused on demonstrating and disseminating how standardized, evidence‐based care in both clinical and safety domains can lead to high‐value and high‐quality outcomes. The success of PHM will be measured by its ability to deliver a clear value proposition to all consumers and payers of healthcare. The creation of a robust national collaborative network is a first step towards meeting this goal and will take an extraordinary effort. A PHM Quality Improvement (QI) Collaborative workgroup was created in August 2009. Three collaboratives have been commissioned: (1) Reduction of patient identification errors; (2) Improving discharge communication to referring primary care providers for pediatric hospitalist programs, and (3) Reducing the misuse and overuse of bronchodilators for bronchiolitis. All the collaborative groups have effectively engaged key groups of stakeholders and utilized standard QI tools, demonstrating improvement by the fall of 2010 (unpublished data, S.N.).
RESEARCH
Despite being a relatively young field, there is a critical mass of pediatric hospitalist‐investigators who are establishing research career paths for themselves by securing external grant funding for their work, publishing, and receiving mentorship from largely non‐hospitalist mentors. Some hospitalists are now in a position to mentor junior investigators. These hospitalist‐investigators identified a collective goal of working together across multiple sites in a clinical research network. The goal is to conduct high‐quality studies and provide the necessary clinical information to allow practicing hospitalists to make better decisions regarding patient care. This new inpatient evidence‐base will have the added advantage of helping further define the field of PHM.
The Pediatric Research in Inpatient Settings Network (PRIS) was identified as the vehicle to accomplish these goals. A series of objectives were identified to redesign PRIS in order to accommodate and organize this new influx of hospitalist‐investigators. These objectives included having hospitalist‐investigators commit their time to the prioritization, design, and execution of multicenter studies, drafting new governance documents for PRIS, securing external funding, redefining the relationships of the 3 existing organizations that formed PRIS (AAP, APA, SHM), defining how new clinical sites could be added to PRIS, creating a pipeline for junior hospitalist‐investigators to transition to leadership roles, securing a data coordinating center with established expertise in conducting multicenter studies, and establishing an external research advisory committee of leaders in pediatric clinical research and QI.
Several critical issues were identified, but funding remained a priority for the sustainability of PRIS. Comparative effectiveness (CE) was recognized as a potential important source of future funding. Pediatric studies on CE (eg, surgery vs medical management) conducted by PRIS would provide important new data to allow hospitalists to practice evidence‐based medicine and to improve quality.
A Research Leadership Task Force was created with 4 members of the PHM Strategic Planning Roundtable to work on the identified issues. The APA leadership worked with PRIS to establish a new Executive Council (comprised of additional qualified hospitalist‐investigators). The Executive Council was charged with accomplishing the tasks outlined from the Strategic Planning Roundtable. They have created the governance documents and standard operating procedures necessary for PRIS to conduct multicenter studies, defined a strategic framework for PRIS including the mission, vision and values, and funding strategy. In February 2010, PRIS received a 3‐year award for over $1 million from the Child Health Corporation of America to both fund the infrastructure of PRIS and to conduct a Prioritization Project. The Prioritization Project seeks to identify the conditions that are costly, prevalent, and demonstrate high inter‐hospital variation in resource utilization, which signals either lack of high‐quality data upon which to base medical decisions, and/or an opportunity to standardize care across hospitals. Some of these conditions will warrant further investigation to define the evidence base, whereas other conditions may require implementation studies to reliably introduce evidence into practice. Members of the Executive Council received additional funding to investigate community settings, as most children are hospitalized outside of large children's hospitals. PRIS also reengaged all 3 societies (APA, AAP, and SHM) for support for the first face‐to‐face meeting of the Executive Council. PRIS applied for 2 Recovery Act stimulus grants, and received funding for both of approximately $12 million. The processes used to design, provide feedback, and shepherd these initial studies formed the basis for the standard operating procedures for the Network. PRIS is now reengaging its membership to establish how sites may be able to conduct research, and receive new ideas to be considered for study in PRIS.
Although much work remains to be done, the Executive Council is continuing the charge with quarterly face‐to‐face meetings, hiring of a full‐time PRIS Coordinator, and carrying out these initial projects, while maintaining the goal of meeting the needs of the membership and PHM. If PRIS is to accomplish its mission of improving the health of, and healthcare delivery to, hospitalized children and their families, then the types of studies undertaken will include not only original research questions, but also comparative implementation methods to better understand how hospitalists in a variety of settings can best translate research findings into clinical practice and ultimately improve patient outcomes.
WORKFORCE
The current number of pediatric hospitalists is difficult to gauge11; estimates range from 1500 to 3000 physicians. There are groups of pediatric hospitalists within several national organizations including the AAP, APA, and SHM, in addition to a very active listserve community. It is likely that only a portion of pediatric hospitalists are represented by membership in these organizations.
Most physicians entering the field of PHM come directly out of residency. A recent survey by Freed et al.12 reported that 3% of current pediatric residents are interested in PHM as a career. In another survey by Freed et al., about 6% of recent pediatric residency graduates reported currently practicing as pediatric hospitalists.13 This difference may indicate a number of pediatricians practicing transiently as pediatric hospitalists.
There are numerous issues that will affect the growth and sustainability of PHM. A large number of pediatric residents entering the field will be needed to maintain current numbers. With 45% of hospitalists in practice less than 3 years,11 the growth of PHM in both numbers and influence will require an increasing number of hospitalists with sustained careers in the field. Recognition as experts in inpatient care, as well as expansion of the role of hospitalists beyond the clinical realm to education, research, and hospital leadership, will foster long‐term career satisfaction. The increasingly common stature of hospital medicine as an independent division, equivalent to general pediatrics and subspecialty divisions within a department, may further bolster the perception of hospital medicine as a career.
The majority of pediatric hospitalists believe that current pediatric residency training does not provide all of the skills necessary to practice as a pediatric hospitalist,14 though there is disagreement regarding how additional training in pediatric hospital medicine should be achieved: a dedicated fellowship versus continuing medical education (CME). There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified. The Residency Review and Redesign Project indicates that pediatric residency is likely to be reformed to better meet the training demands of the individual resident's chosen career path. Changing residency to better prepare pediatric residents to take positions in pediatric hospital medicine will certainly affect the workforce emerging from residency programs and their subsequent training needs.15 The American Board of Internal Medicine and the American Board of Family Medicine have approved a Recognition of Focused Practice in Hospital Medicine. This recognition is gained through the Maintenance of Certification (MOC) Program of the respective boards after a minimum of 3 years of practice. SHM is offering fellow recognition in tiered designations of Fellow of Hospital Medicine (FHM), Senior Fellow of Hospital Medicine, and Master of Hospital Medicine. Five hundred hospitalists, including many pediatric hospitalists, received the inaugural FHM designation in 2009. Organizational recognition is a common process in many other medical fields, although previously limited in pediatrics to Fellow of the AAP. FHM is an important step, but cannot substitute for specific training and certification.
Academic fellowships in PHM will aid in the training of hospitalists with scholarly skills and will help produce more pediatric hospitalists with clinical, quality, administrative, and leadership skills. A model of subspecialty fellowship training and certification of all PHM physicians would require a several‐fold increase in available fellowships, currently approximately 15.
Ongoing CME offerings are also critical to sustaining and developing the workforce. The annual national meetings of the APA, AAP, and SHM all offer PHM‐dedicated content, and there is an annual PHM conference sponsored by these 3 organizations. There are now multiple additional national and regional meetings focused on PHM, reflecting the growing audience for PHM CME content. The AAP offers a PHM study guide and an Education in quality improvement for pediatric practice (eQIPP) module on inpatient asthma, specifically designed to facilitate the MOC process for pediatric hospitalists.
Some form of ABP recognition may be necessary to provide the status for PHM to be widely recognized as a viable academic career in the larger pediatric community. This would entail standardized fellowships that will ensure graduates have demonstrated proficiency in the core competencies. PHM leaders have engaged the ABP to better understand the subspecialty approval process and thoughtfully examine the ramifications of subspecialty status, specifically what subspecialty certification would mean for PHM providers and hospitals. Achieving ABP certification may create a new standard of care meaning that noncertified PHM providers will be at a disadvantage. It is unknown what the impact on pediatric inpatient care would be if a PHM standard was set without the supply of practitioners to provide that care.
STRUCTURE
The efforts of the Roundtable demonstrate the potential effectiveness of the current structure that guides the field: that of the cooperative interchange between the PHM leaders within the APA, AAP, and SHM. It may be that, similar to Pediatric Emergency Medicine (PEM), no formal, unifying structure is necessary. Alternatively, both Adolescent Medicine and Behavioral and Developmental Pediatrics (BDP) have their own organizations that guide their respective fields. A hybrid model is that of Pediatric Cardiology which has the Joint Council on Congenital Heart Disease. This structure assures that the leaders of the various organizations concerned with congenital heart disease meet at least annually to report on their activities and coordinate future efforts. Its makeup is similar to how the planning committee of the annual national PHM conference is constructed. Although PHM has largely succeeded with the current organizational structure, it is possible that a more formal structure is needed to continue forward.
CONCLUSION
The Roundtable members developed the following vision for PHM: Pediatric hospitalists will transform the delivery of hospital care for children. This will be done by achieving 7 goals (Table 2).
|
| We will ensure that care for hospitalized children is fully integrated and includes the medical home |
| We will design and support systems for children that eliminate harm associated with hospital care |
| We will develop a skilled and stable workforce that is the preferred provider of care for most hospitalized children |
| We will use collaborative research models to answer questions of clinical efficacy, comparative effectiveness, and quality improvement, and we will deliver care based on that knowledge |
| We will provide the expertise that supports continuing education in the care of the hospitalized child for pediatric hospitalists, trainees, midlevel providers, and hospital staff |
| We will create value for our patients and organizations in which we work based on our unique expertise in PHM clinical care, research, and education |
| We will be leaders and influential agents in national health care policies that impact hospital care |
Attaining this vision will take tremendous dedication, effort, and collaboration. As a starting point, the following initiatives were proposed and implemented as noted:
Clinical
-
Develop an educational plan supporting the PHM Core Competencies, addressing both hospitalist training needs and the role as formal educators.
-
Create a clinical practice monitoring dashboard template for use at PHM hospitals and practices (implemented July 2010).
Quality
-
Undertake environmental assessment of PHM participation on key quality and safety committees, societies, and agencies to ensure appropriate PHM representation in liaison and/or leadership positions.
-
Create a plan for a QI collaborative by assessing the needs and resources available; draft plans for 2 projects (1 safety and 1 quality) which will improve care for children hospitalized with common conditions (started July 2009).
Research
-
Create a collaborative research entity by restructuring the existing research network and formalizing relationships with affiliated networks.
-
Create a pipeline/mentorship system to increase the number of PHM researchers.
Workforce
-
Develop a descriptive statement that can be used by any PHM physician that defines the field of PHM and answers the question who are we?
-
Develop a communications tool describing value added of PHM.
-
Develop a tool to assess career satisfaction among PHM physicians, with links to current SHM work in this area.
Structure
-
Formalize an organizational infrastructure for oversight and guidance of PHM Strategic Planning Roundtable efforts, with clear delineation of the relationships with the AAP, APA, and SHM.
This review demonstrates the work that needs to be done to close the gaps between the current state of affairs and the full vision of the potential impact of PHM. Harm is still common in hospitalized children, and, as a group of physicians, we do not consistently provide evidence‐based care. Quality and safety activities are currently dispersed throughout multiple national entities often working in silos. Much of our PHM research is fragmented, with a lack of effective research networks and collaborative efforts. We also found that while our workforce has many strengths, it is not yet stable.
We believe the Roundtable was successful in describing the current state of PHM and laying a course for the future. We developed a series of deliverable products that have already seen success on many fronts, and that will serve as the foundation for further maturation of the field. We hope to engage the pediatric community, within and without PHM, to comment, advise, and foster PHM so that these efforts are not static but ongoing and evolving. Already, new challenges have arisen not addressed at the Roundtable, such as further resident work restrictions, and healthcare reform with its potential effects on hospital finances. This is truly an exciting and dynamic time, and we know that this is just the beginning.
Acknowledgements
The authors acknowledge the contribution of all members of the roundtable: Douglas Carlson, Vincent Chiang, Patrick Conway, Jennifer Daru, Matthew Garber, Christopher Landrigan, Patricia Lye, Sanjay Mahant, Jennifer Maniscalco, Sanford Melzer, Stephen Muething, Steve Narang, Mary Ottolini, Jack Percelay, Daniel Rauch, Mario Reyes, Beth Robbins, Jeff Sperring, Rajendu Srivastava, Erin Stucky, Lisa Zaoutis, and David Zipes. The authors thank David Zipes for his help in reviewing the manuscript.
- ,.The hospitalist movement 5 years later.JAMA.2002;287(4):487–494.
- ,,.The Physician Strategist: Setting Strategic Direction for Your Practice; Chicago, Irwin Professional Pub,1996.
- ,.Pediatric hospitalists: training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- The Pediatric Core Competencies Supplement.J Hosp Med.2010;5(suppl 2):1–114.
- ,,,.Reauthorizing SCHIP: Opportunities for Promoting Effective Health Coverage and High Quality Care for Children and Adolescents. Publication 1051.New York, NY:The Commonwealth Fund; August2007:4.
- ,.National Association of Children's Hospitals. Quality Performance Measurement in Medicaid and SCHIP: Result of a 2006 National Survey of State Officials.Lansing, MI:Health Management Associates; August2006.
- ,,,.A report card on quality improvement for children's health care.Pediatrics.2001;107:143–155.
- ,,, et al.Impact of a hospitalist system on length of stay and cost for children with common conditions.Pediatrics.2007;120(2):267–274.
- ,,,,,.Variations in management of common inpatient pediatric illnesses: hospitalists and community pediatricians.Pediatrics.2006;118:441–447.
- ,,,,.Variation in pediatric hospitalists' use of unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- ,,,.Characteristics of the pediatric hospitalist workforce: its roles and work environment.Pediatrics.2007;120(1):33–39.
- ,,,,.General pediatrics resident perspectives on training decisions and career choice.Pediatrics.2009;123(suppl 1):S26–S30.
- ,,,,.Recently trained general pediatricians: perspectives on residency training and scope of practice.Pediatrics.2009;123(suppl 1):S38–S43.
- ,,,.PRIS survey: pediatric hospitalist roles and training needs [abstract].Pediatr Res.2004(55):1.
- ,,.The Residency Review and Redesign in Pediatrics (R3P) Project: roots and branches.Pediatrics.2009;123(suppl 1):S8–S11.
Hospitalists are the fastest growing segment of physicians in the United States.1 Given the growing field of Pediatric Hospital Medicine (PHM) and the need to define strategic direction, the Society of Hospital Medicine (SHM), the American Academy of Pediatrics (AAP), and the Academic Pediatric Association (APA) sponsored a strategic planning meeting in February 2009 that brought together 22 PHM leaders to discuss the future of the field.
PHM is at a critical juncture in terms of clinical practice, research, workforce issues, and quality improvement. The field has developed sufficiently to produce leaders capable of setting an agenda and moving forward. A discussion with the American Board of Pediatrics (ABP) by PHM leaders from the AAP, APA, and SHM at the Pediatric Hospital Medicine 2007 Conference regarding subspecialty designation stimulated convening the PHM Strategic Planning Roundtable to address the task of coordinating further development of PHM (Table 1).
|
| Develop a strategic vision for the role of PHM in the future of children's health care |
| Describe the current gaps between the vision and today's reality |
| Develop a common understanding regarding current initiatives in PHM domains of clinical practice, quality, research, and workforce |
| Determine the method(s) by which participants can be organized to accomplish additional initiatives to implement the vision |
| Identify and prioritize key strategic initiatives |
| Assign accountability and determine next steps and timeline to implement the selected initiatives |
The objective of this article is to describe: (1) the Strategic Planning Roundtable's vision for the field of pediatric hospital medicine; (2) the generation and progress on specific initiatives in clinical practice, quality, research, and workforce identified by the Strategic Planning Roundtable; and (3) issues in the designation of PHM as a subspecialty.
METHODS
The PHM Strategic Planning Roundtable was conducted by a facilitator (S.M.) during a 2‐day retreat using established healthcare strategic planning methods.2
Participants were the existing PHM leaders from the AAP, APA, and SHM, as well as other national leaders in clinical practice, quality, research, and workforce. Development of the vision statement was a key step in which the participants developed a consensus‐based aspirational view of the future. The draft version of the vision statement was initially developed after extensive interviews with key stakeholders and experts in PHM, and was revised by the participants in the course of a facilitated group discussion during the retreat. Following creation of the vision statement, the group then defined the elements of transformation pertaining to PHM and detailed the components of the vision.
Analysis of internal and external environmental factors was critical in the strategic planning process. This type of analysis, detailing the current state of PHM practice, permitted the strategic planners to understand the gaps that existed between the aspirational vision statement and today's reality, and set the stage to identify and implement initiatives to achieve the vision. Several months before the meeting, 4 expert panels comprised of PHM specialists representing a variety of academic and clinical practice settings were brought together via e‐mail and conference calls to focus on 4 domains of PHM: clinical practice, quality of care, research, and workforce. These groups were asked to describe the current status, challenges, and opportunities in these areas. Combining literature review and key stakeholder interviews, their findings and recommendations were distilled into brief summaries that were presented at the Roundtable meeting. Following the presentations, the participants, working in small groups representing all areas of focus,provided additional feedback.
Following the creation of a consensus vision statement and review of internal and external factors, the participants worked to identify specific initiatives in the 4 domains that would advance the field towards the goals contained in the vision statement. These initiatives were grouped into categories. Initiatives by category were scored and prioritized according to predetermined criteria including potential impact, cost, operational complexity, and achievability.
For each initiative selected, the group developed targets and metrics that would be used to track progress. Assigning leadership, accountability, and a timeline to each of the selected projects completed the implementation plan. In addition, the group developed an organizational structure to provide oversight for the overall process, and designated individuals representing the sponsoring organizations into those roles. In conclusion, the group discussed potential structures to guide the future of PHM.
CLINICAL PRACTICE
The Roundtable defined clinical practice for PHM as the general medical care of the hospitalized child, including direct patient care and leadership of the inpatient service. Clinical practice is affected by a number of current national trends including: fewer primary care providers interested in, or with the time to provide, inpatient care; resident work hour restrictions; increasing complexity of clinical issues; and increasing availability of pediatric hospitalists. At the hospital level, clinical practice is affected by increasing need for quality and safety measures, electronic health records and computerized physician order entry, and mounting financial pressures on the hospital system. Hospitalists are assuming more roles in leading quality and safety initiatives, creating computerized systems that address children's needs, and creating financially viable systems of quality pediatric care.3 Hospitalists' clinical care and leadership roles are emerging, and therefore the field faces training and mentorship issues.
Progress to date in this area includes 2 textbooks that define a scope of knowledge and practice, and a newly developed journal in PHM. Core competencies in PHM have been published and provide further refinement of scope and a template for future training.4
Multiple opportunities exist for hospitalists to establish themselves as clinical leaders. Hospitalists can become the preferred providers for hospitalized chronically ill children, with specific initiatives to improve care coordination and multidisciplinary communication. In addition to care coordination and decreasing length of stay, hospitalists, with their intimate knowledge of hospital operations, can be leaders in hospital capacity management and patient flow to increase operational efficiency. Hospitalists can expand evidence‐based guidelines for, and data about, inpatient conditions, and explore the effect of workload and hours on patient care. In addition, there is an expanding role into administrative areas, as well as alternate care arenas, such as: intensive care support (pediatric and neonatal), transport, sedation, palliative care, and pain management. Activities in administrative and alternate care areas have profound direct affects on patient care, as well as providing value added services and additional revenue streams which can further support clinical needs. Finally, achieving quality targets will likely be increasingly linked to payment, so hospitalists may play a key role in the incentives paid to their hospitals. Meeting these challenges will further solidify the standing of hospitalists in the clinical realm.
QUALITY
National and governmental agencies have influenced quality and performance improvement measurements in adult healthcare, resulting in improvements in adult healthcare quality measurement.5 There is limited similar influence or measure development in pediatric medicine, so the quality chasm between adult and child healthcare has widened. Few resources are invested in improving quality and safety of pediatric inpatient care. Of the 18 private health insurance plans' quality and pay for performance programs identified by Leapfrog, only 17% developed pediatric‐specific inpatient measures.6 Only 5 of 40 controlled trials of quality improvement efforts for children published between 1980 and 1998 addressed inpatient problems.7
There have been recent efforts at the national level addressing these issues, highlighted by the introduction of The Children's Health Care Quality Act, in 2007. Early studies in PHM systems focused on overall operational efficiency, documenting 9% to 16% decreases in length of stay and cost compared to traditional models of care.8 Conway et al. identified higher reported adherence to evidence‐based care for hospitalists compared to community pediatricians.9 However, Landrigan et al. demonstrated that there is still large variation in care that exists in the management of common inpatient diagnoses, lacking strong evidence‐based guidelines even among pediatric hospitalists.10 Moreover, there have been no significant studies reviewing the impact of pediatric hospitalists on safety of inpatient care. Magnifying these challenges is the reality that our healthcare system is fragmented with various entities scrambling to define, measure, and compare the effectiveness and safety of pediatric healthcare.
These challenges create an opportunity for PHM to develop a model of how to deliver the highest quality and safest care to our patients. The solution is complex and will take cooperation at many levels of our healthcare system. Improving the safety and quality of care for children in all settings of inpatient care in the United States may best be accomplished via an effective collaborative. This collaborative should be comprehensive and inclusive, and focused on demonstrating and disseminating how standardized, evidence‐based care in both clinical and safety domains can lead to high‐value and high‐quality outcomes. The success of PHM will be measured by its ability to deliver a clear value proposition to all consumers and payers of healthcare. The creation of a robust national collaborative network is a first step towards meeting this goal and will take an extraordinary effort. A PHM Quality Improvement (QI) Collaborative workgroup was created in August 2009. Three collaboratives have been commissioned: (1) Reduction of patient identification errors; (2) Improving discharge communication to referring primary care providers for pediatric hospitalist programs, and (3) Reducing the misuse and overuse of bronchodilators for bronchiolitis. All the collaborative groups have effectively engaged key groups of stakeholders and utilized standard QI tools, demonstrating improvement by the fall of 2010 (unpublished data, S.N.).
RESEARCH
Despite being a relatively young field, there is a critical mass of pediatric hospitalist‐investigators who are establishing research career paths for themselves by securing external grant funding for their work, publishing, and receiving mentorship from largely non‐hospitalist mentors. Some hospitalists are now in a position to mentor junior investigators. These hospitalist‐investigators identified a collective goal of working together across multiple sites in a clinical research network. The goal is to conduct high‐quality studies and provide the necessary clinical information to allow practicing hospitalists to make better decisions regarding patient care. This new inpatient evidence‐base will have the added advantage of helping further define the field of PHM.
The Pediatric Research in Inpatient Settings Network (PRIS) was identified as the vehicle to accomplish these goals. A series of objectives were identified to redesign PRIS in order to accommodate and organize this new influx of hospitalist‐investigators. These objectives included having hospitalist‐investigators commit their time to the prioritization, design, and execution of multicenter studies, drafting new governance documents for PRIS, securing external funding, redefining the relationships of the 3 existing organizations that formed PRIS (AAP, APA, SHM), defining how new clinical sites could be added to PRIS, creating a pipeline for junior hospitalist‐investigators to transition to leadership roles, securing a data coordinating center with established expertise in conducting multicenter studies, and establishing an external research advisory committee of leaders in pediatric clinical research and QI.
Several critical issues were identified, but funding remained a priority for the sustainability of PRIS. Comparative effectiveness (CE) was recognized as a potential important source of future funding. Pediatric studies on CE (eg, surgery vs medical management) conducted by PRIS would provide important new data to allow hospitalists to practice evidence‐based medicine and to improve quality.
A Research Leadership Task Force was created with 4 members of the PHM Strategic Planning Roundtable to work on the identified issues. The APA leadership worked with PRIS to establish a new Executive Council (comprised of additional qualified hospitalist‐investigators). The Executive Council was charged with accomplishing the tasks outlined from the Strategic Planning Roundtable. They have created the governance documents and standard operating procedures necessary for PRIS to conduct multicenter studies, defined a strategic framework for PRIS including the mission, vision and values, and funding strategy. In February 2010, PRIS received a 3‐year award for over $1 million from the Child Health Corporation of America to both fund the infrastructure of PRIS and to conduct a Prioritization Project. The Prioritization Project seeks to identify the conditions that are costly, prevalent, and demonstrate high inter‐hospital variation in resource utilization, which signals either lack of high‐quality data upon which to base medical decisions, and/or an opportunity to standardize care across hospitals. Some of these conditions will warrant further investigation to define the evidence base, whereas other conditions may require implementation studies to reliably introduce evidence into practice. Members of the Executive Council received additional funding to investigate community settings, as most children are hospitalized outside of large children's hospitals. PRIS also reengaged all 3 societies (APA, AAP, and SHM) for support for the first face‐to‐face meeting of the Executive Council. PRIS applied for 2 Recovery Act stimulus grants, and received funding for both of approximately $12 million. The processes used to design, provide feedback, and shepherd these initial studies formed the basis for the standard operating procedures for the Network. PRIS is now reengaging its membership to establish how sites may be able to conduct research, and receive new ideas to be considered for study in PRIS.
Although much work remains to be done, the Executive Council is continuing the charge with quarterly face‐to‐face meetings, hiring of a full‐time PRIS Coordinator, and carrying out these initial projects, while maintaining the goal of meeting the needs of the membership and PHM. If PRIS is to accomplish its mission of improving the health of, and healthcare delivery to, hospitalized children and their families, then the types of studies undertaken will include not only original research questions, but also comparative implementation methods to better understand how hospitalists in a variety of settings can best translate research findings into clinical practice and ultimately improve patient outcomes.
WORKFORCE
The current number of pediatric hospitalists is difficult to gauge11; estimates range from 1500 to 3000 physicians. There are groups of pediatric hospitalists within several national organizations including the AAP, APA, and SHM, in addition to a very active listserve community. It is likely that only a portion of pediatric hospitalists are represented by membership in these organizations.
Most physicians entering the field of PHM come directly out of residency. A recent survey by Freed et al.12 reported that 3% of current pediatric residents are interested in PHM as a career. In another survey by Freed et al., about 6% of recent pediatric residency graduates reported currently practicing as pediatric hospitalists.13 This difference may indicate a number of pediatricians practicing transiently as pediatric hospitalists.
There are numerous issues that will affect the growth and sustainability of PHM. A large number of pediatric residents entering the field will be needed to maintain current numbers. With 45% of hospitalists in practice less than 3 years,11 the growth of PHM in both numbers and influence will require an increasing number of hospitalists with sustained careers in the field. Recognition as experts in inpatient care, as well as expansion of the role of hospitalists beyond the clinical realm to education, research, and hospital leadership, will foster long‐term career satisfaction. The increasingly common stature of hospital medicine as an independent division, equivalent to general pediatrics and subspecialty divisions within a department, may further bolster the perception of hospital medicine as a career.
The majority of pediatric hospitalists believe that current pediatric residency training does not provide all of the skills necessary to practice as a pediatric hospitalist,14 though there is disagreement regarding how additional training in pediatric hospital medicine should be achieved: a dedicated fellowship versus continuing medical education (CME). There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified. The Residency Review and Redesign Project indicates that pediatric residency is likely to be reformed to better meet the training demands of the individual resident's chosen career path. Changing residency to better prepare pediatric residents to take positions in pediatric hospital medicine will certainly affect the workforce emerging from residency programs and their subsequent training needs.15 The American Board of Internal Medicine and the American Board of Family Medicine have approved a Recognition of Focused Practice in Hospital Medicine. This recognition is gained through the Maintenance of Certification (MOC) Program of the respective boards after a minimum of 3 years of practice. SHM is offering fellow recognition in tiered designations of Fellow of Hospital Medicine (FHM), Senior Fellow of Hospital Medicine, and Master of Hospital Medicine. Five hundred hospitalists, including many pediatric hospitalists, received the inaugural FHM designation in 2009. Organizational recognition is a common process in many other medical fields, although previously limited in pediatrics to Fellow of the AAP. FHM is an important step, but cannot substitute for specific training and certification.
Academic fellowships in PHM will aid in the training of hospitalists with scholarly skills and will help produce more pediatric hospitalists with clinical, quality, administrative, and leadership skills. A model of subspecialty fellowship training and certification of all PHM physicians would require a several‐fold increase in available fellowships, currently approximately 15.
Ongoing CME offerings are also critical to sustaining and developing the workforce. The annual national meetings of the APA, AAP, and SHM all offer PHM‐dedicated content, and there is an annual PHM conference sponsored by these 3 organizations. There are now multiple additional national and regional meetings focused on PHM, reflecting the growing audience for PHM CME content. The AAP offers a PHM study guide and an Education in quality improvement for pediatric practice (eQIPP) module on inpatient asthma, specifically designed to facilitate the MOC process for pediatric hospitalists.
Some form of ABP recognition may be necessary to provide the status for PHM to be widely recognized as a viable academic career in the larger pediatric community. This would entail standardized fellowships that will ensure graduates have demonstrated proficiency in the core competencies. PHM leaders have engaged the ABP to better understand the subspecialty approval process and thoughtfully examine the ramifications of subspecialty status, specifically what subspecialty certification would mean for PHM providers and hospitals. Achieving ABP certification may create a new standard of care meaning that noncertified PHM providers will be at a disadvantage. It is unknown what the impact on pediatric inpatient care would be if a PHM standard was set without the supply of practitioners to provide that care.
STRUCTURE
The efforts of the Roundtable demonstrate the potential effectiveness of the current structure that guides the field: that of the cooperative interchange between the PHM leaders within the APA, AAP, and SHM. It may be that, similar to Pediatric Emergency Medicine (PEM), no formal, unifying structure is necessary. Alternatively, both Adolescent Medicine and Behavioral and Developmental Pediatrics (BDP) have their own organizations that guide their respective fields. A hybrid model is that of Pediatric Cardiology which has the Joint Council on Congenital Heart Disease. This structure assures that the leaders of the various organizations concerned with congenital heart disease meet at least annually to report on their activities and coordinate future efforts. Its makeup is similar to how the planning committee of the annual national PHM conference is constructed. Although PHM has largely succeeded with the current organizational structure, it is possible that a more formal structure is needed to continue forward.
CONCLUSION
The Roundtable members developed the following vision for PHM: Pediatric hospitalists will transform the delivery of hospital care for children. This will be done by achieving 7 goals (Table 2).
|
| We will ensure that care for hospitalized children is fully integrated and includes the medical home |
| We will design and support systems for children that eliminate harm associated with hospital care |
| We will develop a skilled and stable workforce that is the preferred provider of care for most hospitalized children |
| We will use collaborative research models to answer questions of clinical efficacy, comparative effectiveness, and quality improvement, and we will deliver care based on that knowledge |
| We will provide the expertise that supports continuing education in the care of the hospitalized child for pediatric hospitalists, trainees, midlevel providers, and hospital staff |
| We will create value for our patients and organizations in which we work based on our unique expertise in PHM clinical care, research, and education |
| We will be leaders and influential agents in national health care policies that impact hospital care |
Attaining this vision will take tremendous dedication, effort, and collaboration. As a starting point, the following initiatives were proposed and implemented as noted:
Clinical
-
Develop an educational plan supporting the PHM Core Competencies, addressing both hospitalist training needs and the role as formal educators.
-
Create a clinical practice monitoring dashboard template for use at PHM hospitals and practices (implemented July 2010).
Quality
-
Undertake environmental assessment of PHM participation on key quality and safety committees, societies, and agencies to ensure appropriate PHM representation in liaison and/or leadership positions.
-
Create a plan for a QI collaborative by assessing the needs and resources available; draft plans for 2 projects (1 safety and 1 quality) which will improve care for children hospitalized with common conditions (started July 2009).
Research
-
Create a collaborative research entity by restructuring the existing research network and formalizing relationships with affiliated networks.
-
Create a pipeline/mentorship system to increase the number of PHM researchers.
Workforce
-
Develop a descriptive statement that can be used by any PHM physician that defines the field of PHM and answers the question who are we?
-
Develop a communications tool describing value added of PHM.
-
Develop a tool to assess career satisfaction among PHM physicians, with links to current SHM work in this area.
Structure
-
Formalize an organizational infrastructure for oversight and guidance of PHM Strategic Planning Roundtable efforts, with clear delineation of the relationships with the AAP, APA, and SHM.
This review demonstrates the work that needs to be done to close the gaps between the current state of affairs and the full vision of the potential impact of PHM. Harm is still common in hospitalized children, and, as a group of physicians, we do not consistently provide evidence‐based care. Quality and safety activities are currently dispersed throughout multiple national entities often working in silos. Much of our PHM research is fragmented, with a lack of effective research networks and collaborative efforts. We also found that while our workforce has many strengths, it is not yet stable.
We believe the Roundtable was successful in describing the current state of PHM and laying a course for the future. We developed a series of deliverable products that have already seen success on many fronts, and that will serve as the foundation for further maturation of the field. We hope to engage the pediatric community, within and without PHM, to comment, advise, and foster PHM so that these efforts are not static but ongoing and evolving. Already, new challenges have arisen not addressed at the Roundtable, such as further resident work restrictions, and healthcare reform with its potential effects on hospital finances. This is truly an exciting and dynamic time, and we know that this is just the beginning.
Acknowledgements
The authors acknowledge the contribution of all members of the roundtable: Douglas Carlson, Vincent Chiang, Patrick Conway, Jennifer Daru, Matthew Garber, Christopher Landrigan, Patricia Lye, Sanjay Mahant, Jennifer Maniscalco, Sanford Melzer, Stephen Muething, Steve Narang, Mary Ottolini, Jack Percelay, Daniel Rauch, Mario Reyes, Beth Robbins, Jeff Sperring, Rajendu Srivastava, Erin Stucky, Lisa Zaoutis, and David Zipes. The authors thank David Zipes for his help in reviewing the manuscript.
Hospitalists are the fastest growing segment of physicians in the United States.1 Given the growing field of Pediatric Hospital Medicine (PHM) and the need to define strategic direction, the Society of Hospital Medicine (SHM), the American Academy of Pediatrics (AAP), and the Academic Pediatric Association (APA) sponsored a strategic planning meeting in February 2009 that brought together 22 PHM leaders to discuss the future of the field.
PHM is at a critical juncture in terms of clinical practice, research, workforce issues, and quality improvement. The field has developed sufficiently to produce leaders capable of setting an agenda and moving forward. A discussion with the American Board of Pediatrics (ABP) by PHM leaders from the AAP, APA, and SHM at the Pediatric Hospital Medicine 2007 Conference regarding subspecialty designation stimulated convening the PHM Strategic Planning Roundtable to address the task of coordinating further development of PHM (Table 1).
|
| Develop a strategic vision for the role of PHM in the future of children's health care |
| Describe the current gaps between the vision and today's reality |
| Develop a common understanding regarding current initiatives in PHM domains of clinical practice, quality, research, and workforce |
| Determine the method(s) by which participants can be organized to accomplish additional initiatives to implement the vision |
| Identify and prioritize key strategic initiatives |
| Assign accountability and determine next steps and timeline to implement the selected initiatives |
The objective of this article is to describe: (1) the Strategic Planning Roundtable's vision for the field of pediatric hospital medicine; (2) the generation and progress on specific initiatives in clinical practice, quality, research, and workforce identified by the Strategic Planning Roundtable; and (3) issues in the designation of PHM as a subspecialty.
METHODS
The PHM Strategic Planning Roundtable was conducted by a facilitator (S.M.) during a 2‐day retreat using established healthcare strategic planning methods.2
Participants were the existing PHM leaders from the AAP, APA, and SHM, as well as other national leaders in clinical practice, quality, research, and workforce. Development of the vision statement was a key step in which the participants developed a consensus‐based aspirational view of the future. The draft version of the vision statement was initially developed after extensive interviews with key stakeholders and experts in PHM, and was revised by the participants in the course of a facilitated group discussion during the retreat. Following creation of the vision statement, the group then defined the elements of transformation pertaining to PHM and detailed the components of the vision.
Analysis of internal and external environmental factors was critical in the strategic planning process. This type of analysis, detailing the current state of PHM practice, permitted the strategic planners to understand the gaps that existed between the aspirational vision statement and today's reality, and set the stage to identify and implement initiatives to achieve the vision. Several months before the meeting, 4 expert panels comprised of PHM specialists representing a variety of academic and clinical practice settings were brought together via e‐mail and conference calls to focus on 4 domains of PHM: clinical practice, quality of care, research, and workforce. These groups were asked to describe the current status, challenges, and opportunities in these areas. Combining literature review and key stakeholder interviews, their findings and recommendations were distilled into brief summaries that were presented at the Roundtable meeting. Following the presentations, the participants, working in small groups representing all areas of focus,provided additional feedback.
Following the creation of a consensus vision statement and review of internal and external factors, the participants worked to identify specific initiatives in the 4 domains that would advance the field towards the goals contained in the vision statement. These initiatives were grouped into categories. Initiatives by category were scored and prioritized according to predetermined criteria including potential impact, cost, operational complexity, and achievability.
For each initiative selected, the group developed targets and metrics that would be used to track progress. Assigning leadership, accountability, and a timeline to each of the selected projects completed the implementation plan. In addition, the group developed an organizational structure to provide oversight for the overall process, and designated individuals representing the sponsoring organizations into those roles. In conclusion, the group discussed potential structures to guide the future of PHM.
CLINICAL PRACTICE
The Roundtable defined clinical practice for PHM as the general medical care of the hospitalized child, including direct patient care and leadership of the inpatient service. Clinical practice is affected by a number of current national trends including: fewer primary care providers interested in, or with the time to provide, inpatient care; resident work hour restrictions; increasing complexity of clinical issues; and increasing availability of pediatric hospitalists. At the hospital level, clinical practice is affected by increasing need for quality and safety measures, electronic health records and computerized physician order entry, and mounting financial pressures on the hospital system. Hospitalists are assuming more roles in leading quality and safety initiatives, creating computerized systems that address children's needs, and creating financially viable systems of quality pediatric care.3 Hospitalists' clinical care and leadership roles are emerging, and therefore the field faces training and mentorship issues.
Progress to date in this area includes 2 textbooks that define a scope of knowledge and practice, and a newly developed journal in PHM. Core competencies in PHM have been published and provide further refinement of scope and a template for future training.4
Multiple opportunities exist for hospitalists to establish themselves as clinical leaders. Hospitalists can become the preferred providers for hospitalized chronically ill children, with specific initiatives to improve care coordination and multidisciplinary communication. In addition to care coordination and decreasing length of stay, hospitalists, with their intimate knowledge of hospital operations, can be leaders in hospital capacity management and patient flow to increase operational efficiency. Hospitalists can expand evidence‐based guidelines for, and data about, inpatient conditions, and explore the effect of workload and hours on patient care. In addition, there is an expanding role into administrative areas, as well as alternate care arenas, such as: intensive care support (pediatric and neonatal), transport, sedation, palliative care, and pain management. Activities in administrative and alternate care areas have profound direct affects on patient care, as well as providing value added services and additional revenue streams which can further support clinical needs. Finally, achieving quality targets will likely be increasingly linked to payment, so hospitalists may play a key role in the incentives paid to their hospitals. Meeting these challenges will further solidify the standing of hospitalists in the clinical realm.
QUALITY
National and governmental agencies have influenced quality and performance improvement measurements in adult healthcare, resulting in improvements in adult healthcare quality measurement.5 There is limited similar influence or measure development in pediatric medicine, so the quality chasm between adult and child healthcare has widened. Few resources are invested in improving quality and safety of pediatric inpatient care. Of the 18 private health insurance plans' quality and pay for performance programs identified by Leapfrog, only 17% developed pediatric‐specific inpatient measures.6 Only 5 of 40 controlled trials of quality improvement efforts for children published between 1980 and 1998 addressed inpatient problems.7
There have been recent efforts at the national level addressing these issues, highlighted by the introduction of The Children's Health Care Quality Act, in 2007. Early studies in PHM systems focused on overall operational efficiency, documenting 9% to 16% decreases in length of stay and cost compared to traditional models of care.8 Conway et al. identified higher reported adherence to evidence‐based care for hospitalists compared to community pediatricians.9 However, Landrigan et al. demonstrated that there is still large variation in care that exists in the management of common inpatient diagnoses, lacking strong evidence‐based guidelines even among pediatric hospitalists.10 Moreover, there have been no significant studies reviewing the impact of pediatric hospitalists on safety of inpatient care. Magnifying these challenges is the reality that our healthcare system is fragmented with various entities scrambling to define, measure, and compare the effectiveness and safety of pediatric healthcare.
These challenges create an opportunity for PHM to develop a model of how to deliver the highest quality and safest care to our patients. The solution is complex and will take cooperation at many levels of our healthcare system. Improving the safety and quality of care for children in all settings of inpatient care in the United States may best be accomplished via an effective collaborative. This collaborative should be comprehensive and inclusive, and focused on demonstrating and disseminating how standardized, evidence‐based care in both clinical and safety domains can lead to high‐value and high‐quality outcomes. The success of PHM will be measured by its ability to deliver a clear value proposition to all consumers and payers of healthcare. The creation of a robust national collaborative network is a first step towards meeting this goal and will take an extraordinary effort. A PHM Quality Improvement (QI) Collaborative workgroup was created in August 2009. Three collaboratives have been commissioned: (1) Reduction of patient identification errors; (2) Improving discharge communication to referring primary care providers for pediatric hospitalist programs, and (3) Reducing the misuse and overuse of bronchodilators for bronchiolitis. All the collaborative groups have effectively engaged key groups of stakeholders and utilized standard QI tools, demonstrating improvement by the fall of 2010 (unpublished data, S.N.).
RESEARCH
Despite being a relatively young field, there is a critical mass of pediatric hospitalist‐investigators who are establishing research career paths for themselves by securing external grant funding for their work, publishing, and receiving mentorship from largely non‐hospitalist mentors. Some hospitalists are now in a position to mentor junior investigators. These hospitalist‐investigators identified a collective goal of working together across multiple sites in a clinical research network. The goal is to conduct high‐quality studies and provide the necessary clinical information to allow practicing hospitalists to make better decisions regarding patient care. This new inpatient evidence‐base will have the added advantage of helping further define the field of PHM.
The Pediatric Research in Inpatient Settings Network (PRIS) was identified as the vehicle to accomplish these goals. A series of objectives were identified to redesign PRIS in order to accommodate and organize this new influx of hospitalist‐investigators. These objectives included having hospitalist‐investigators commit their time to the prioritization, design, and execution of multicenter studies, drafting new governance documents for PRIS, securing external funding, redefining the relationships of the 3 existing organizations that formed PRIS (AAP, APA, SHM), defining how new clinical sites could be added to PRIS, creating a pipeline for junior hospitalist‐investigators to transition to leadership roles, securing a data coordinating center with established expertise in conducting multicenter studies, and establishing an external research advisory committee of leaders in pediatric clinical research and QI.
Several critical issues were identified, but funding remained a priority for the sustainability of PRIS. Comparative effectiveness (CE) was recognized as a potential important source of future funding. Pediatric studies on CE (eg, surgery vs medical management) conducted by PRIS would provide important new data to allow hospitalists to practice evidence‐based medicine and to improve quality.
A Research Leadership Task Force was created with 4 members of the PHM Strategic Planning Roundtable to work on the identified issues. The APA leadership worked with PRIS to establish a new Executive Council (comprised of additional qualified hospitalist‐investigators). The Executive Council was charged with accomplishing the tasks outlined from the Strategic Planning Roundtable. They have created the governance documents and standard operating procedures necessary for PRIS to conduct multicenter studies, defined a strategic framework for PRIS including the mission, vision and values, and funding strategy. In February 2010, PRIS received a 3‐year award for over $1 million from the Child Health Corporation of America to both fund the infrastructure of PRIS and to conduct a Prioritization Project. The Prioritization Project seeks to identify the conditions that are costly, prevalent, and demonstrate high inter‐hospital variation in resource utilization, which signals either lack of high‐quality data upon which to base medical decisions, and/or an opportunity to standardize care across hospitals. Some of these conditions will warrant further investigation to define the evidence base, whereas other conditions may require implementation studies to reliably introduce evidence into practice. Members of the Executive Council received additional funding to investigate community settings, as most children are hospitalized outside of large children's hospitals. PRIS also reengaged all 3 societies (APA, AAP, and SHM) for support for the first face‐to‐face meeting of the Executive Council. PRIS applied for 2 Recovery Act stimulus grants, and received funding for both of approximately $12 million. The processes used to design, provide feedback, and shepherd these initial studies formed the basis for the standard operating procedures for the Network. PRIS is now reengaging its membership to establish how sites may be able to conduct research, and receive new ideas to be considered for study in PRIS.
Although much work remains to be done, the Executive Council is continuing the charge with quarterly face‐to‐face meetings, hiring of a full‐time PRIS Coordinator, and carrying out these initial projects, while maintaining the goal of meeting the needs of the membership and PHM. If PRIS is to accomplish its mission of improving the health of, and healthcare delivery to, hospitalized children and their families, then the types of studies undertaken will include not only original research questions, but also comparative implementation methods to better understand how hospitalists in a variety of settings can best translate research findings into clinical practice and ultimately improve patient outcomes.
WORKFORCE
The current number of pediatric hospitalists is difficult to gauge11; estimates range from 1500 to 3000 physicians. There are groups of pediatric hospitalists within several national organizations including the AAP, APA, and SHM, in addition to a very active listserve community. It is likely that only a portion of pediatric hospitalists are represented by membership in these organizations.
Most physicians entering the field of PHM come directly out of residency. A recent survey by Freed et al.12 reported that 3% of current pediatric residents are interested in PHM as a career. In another survey by Freed et al., about 6% of recent pediatric residency graduates reported currently practicing as pediatric hospitalists.13 This difference may indicate a number of pediatricians practicing transiently as pediatric hospitalists.
There are numerous issues that will affect the growth and sustainability of PHM. A large number of pediatric residents entering the field will be needed to maintain current numbers. With 45% of hospitalists in practice less than 3 years,11 the growth of PHM in both numbers and influence will require an increasing number of hospitalists with sustained careers in the field. Recognition as experts in inpatient care, as well as expansion of the role of hospitalists beyond the clinical realm to education, research, and hospital leadership, will foster long‐term career satisfaction. The increasingly common stature of hospital medicine as an independent division, equivalent to general pediatrics and subspecialty divisions within a department, may further bolster the perception of hospital medicine as a career.
The majority of pediatric hospitalists believe that current pediatric residency training does not provide all of the skills necessary to practice as a pediatric hospitalist,14 though there is disagreement regarding how additional training in pediatric hospital medicine should be achieved: a dedicated fellowship versus continuing medical education (CME). There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified. The Residency Review and Redesign Project indicates that pediatric residency is likely to be reformed to better meet the training demands of the individual resident's chosen career path. Changing residency to better prepare pediatric residents to take positions in pediatric hospital medicine will certainly affect the workforce emerging from residency programs and their subsequent training needs.15 The American Board of Internal Medicine and the American Board of Family Medicine have approved a Recognition of Focused Practice in Hospital Medicine. This recognition is gained through the Maintenance of Certification (MOC) Program of the respective boards after a minimum of 3 years of practice. SHM is offering fellow recognition in tiered designations of Fellow of Hospital Medicine (FHM), Senior Fellow of Hospital Medicine, and Master of Hospital Medicine. Five hundred hospitalists, including many pediatric hospitalists, received the inaugural FHM designation in 2009. Organizational recognition is a common process in many other medical fields, although previously limited in pediatrics to Fellow of the AAP. FHM is an important step, but cannot substitute for specific training and certification.
Academic fellowships in PHM will aid in the training of hospitalists with scholarly skills and will help produce more pediatric hospitalists with clinical, quality, administrative, and leadership skills. A model of subspecialty fellowship training and certification of all PHM physicians would require a several‐fold increase in available fellowships, currently approximately 15.
Ongoing CME offerings are also critical to sustaining and developing the workforce. The annual national meetings of the APA, AAP, and SHM all offer PHM‐dedicated content, and there is an annual PHM conference sponsored by these 3 organizations. There are now multiple additional national and regional meetings focused on PHM, reflecting the growing audience for PHM CME content. The AAP offers a PHM study guide and an Education in quality improvement for pediatric practice (eQIPP) module on inpatient asthma, specifically designed to facilitate the MOC process for pediatric hospitalists.
Some form of ABP recognition may be necessary to provide the status for PHM to be widely recognized as a viable academic career in the larger pediatric community. This would entail standardized fellowships that will ensure graduates have demonstrated proficiency in the core competencies. PHM leaders have engaged the ABP to better understand the subspecialty approval process and thoughtfully examine the ramifications of subspecialty status, specifically what subspecialty certification would mean for PHM providers and hospitals. Achieving ABP certification may create a new standard of care meaning that noncertified PHM providers will be at a disadvantage. It is unknown what the impact on pediatric inpatient care would be if a PHM standard was set without the supply of practitioners to provide that care.
STRUCTURE
The efforts of the Roundtable demonstrate the potential effectiveness of the current structure that guides the field: that of the cooperative interchange between the PHM leaders within the APA, AAP, and SHM. It may be that, similar to Pediatric Emergency Medicine (PEM), no formal, unifying structure is necessary. Alternatively, both Adolescent Medicine and Behavioral and Developmental Pediatrics (BDP) have their own organizations that guide their respective fields. A hybrid model is that of Pediatric Cardiology which has the Joint Council on Congenital Heart Disease. This structure assures that the leaders of the various organizations concerned with congenital heart disease meet at least annually to report on their activities and coordinate future efforts. Its makeup is similar to how the planning committee of the annual national PHM conference is constructed. Although PHM has largely succeeded with the current organizational structure, it is possible that a more formal structure is needed to continue forward.
CONCLUSION
The Roundtable members developed the following vision for PHM: Pediatric hospitalists will transform the delivery of hospital care for children. This will be done by achieving 7 goals (Table 2).
|
| We will ensure that care for hospitalized children is fully integrated and includes the medical home |
| We will design and support systems for children that eliminate harm associated with hospital care |
| We will develop a skilled and stable workforce that is the preferred provider of care for most hospitalized children |
| We will use collaborative research models to answer questions of clinical efficacy, comparative effectiveness, and quality improvement, and we will deliver care based on that knowledge |
| We will provide the expertise that supports continuing education in the care of the hospitalized child for pediatric hospitalists, trainees, midlevel providers, and hospital staff |
| We will create value for our patients and organizations in which we work based on our unique expertise in PHM clinical care, research, and education |
| We will be leaders and influential agents in national health care policies that impact hospital care |
Attaining this vision will take tremendous dedication, effort, and collaboration. As a starting point, the following initiatives were proposed and implemented as noted:
Clinical
-
Develop an educational plan supporting the PHM Core Competencies, addressing both hospitalist training needs and the role as formal educators.
-
Create a clinical practice monitoring dashboard template for use at PHM hospitals and practices (implemented July 2010).
Quality
-
Undertake environmental assessment of PHM participation on key quality and safety committees, societies, and agencies to ensure appropriate PHM representation in liaison and/or leadership positions.
-
Create a plan for a QI collaborative by assessing the needs and resources available; draft plans for 2 projects (1 safety and 1 quality) which will improve care for children hospitalized with common conditions (started July 2009).
Research
-
Create a collaborative research entity by restructuring the existing research network and formalizing relationships with affiliated networks.
-
Create a pipeline/mentorship system to increase the number of PHM researchers.
Workforce
-
Develop a descriptive statement that can be used by any PHM physician that defines the field of PHM and answers the question who are we?
-
Develop a communications tool describing value added of PHM.
-
Develop a tool to assess career satisfaction among PHM physicians, with links to current SHM work in this area.
Structure
-
Formalize an organizational infrastructure for oversight and guidance of PHM Strategic Planning Roundtable efforts, with clear delineation of the relationships with the AAP, APA, and SHM.
This review demonstrates the work that needs to be done to close the gaps between the current state of affairs and the full vision of the potential impact of PHM. Harm is still common in hospitalized children, and, as a group of physicians, we do not consistently provide evidence‐based care. Quality and safety activities are currently dispersed throughout multiple national entities often working in silos. Much of our PHM research is fragmented, with a lack of effective research networks and collaborative efforts. We also found that while our workforce has many strengths, it is not yet stable.
We believe the Roundtable was successful in describing the current state of PHM and laying a course for the future. We developed a series of deliverable products that have already seen success on many fronts, and that will serve as the foundation for further maturation of the field. We hope to engage the pediatric community, within and without PHM, to comment, advise, and foster PHM so that these efforts are not static but ongoing and evolving. Already, new challenges have arisen not addressed at the Roundtable, such as further resident work restrictions, and healthcare reform with its potential effects on hospital finances. This is truly an exciting and dynamic time, and we know that this is just the beginning.
Acknowledgements
The authors acknowledge the contribution of all members of the roundtable: Douglas Carlson, Vincent Chiang, Patrick Conway, Jennifer Daru, Matthew Garber, Christopher Landrigan, Patricia Lye, Sanjay Mahant, Jennifer Maniscalco, Sanford Melzer, Stephen Muething, Steve Narang, Mary Ottolini, Jack Percelay, Daniel Rauch, Mario Reyes, Beth Robbins, Jeff Sperring, Rajendu Srivastava, Erin Stucky, Lisa Zaoutis, and David Zipes. The authors thank David Zipes for his help in reviewing the manuscript.
- ,.The hospitalist movement 5 years later.JAMA.2002;287(4):487–494.
- ,,.The Physician Strategist: Setting Strategic Direction for Your Practice; Chicago, Irwin Professional Pub,1996.
- ,.Pediatric hospitalists: training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- The Pediatric Core Competencies Supplement.J Hosp Med.2010;5(suppl 2):1–114.
- ,,,.Reauthorizing SCHIP: Opportunities for Promoting Effective Health Coverage and High Quality Care for Children and Adolescents. Publication 1051.New York, NY:The Commonwealth Fund; August2007:4.
- ,.National Association of Children's Hospitals. Quality Performance Measurement in Medicaid and SCHIP: Result of a 2006 National Survey of State Officials.Lansing, MI:Health Management Associates; August2006.
- ,,,.A report card on quality improvement for children's health care.Pediatrics.2001;107:143–155.
- ,,, et al.Impact of a hospitalist system on length of stay and cost for children with common conditions.Pediatrics.2007;120(2):267–274.
- ,,,,,.Variations in management of common inpatient pediatric illnesses: hospitalists and community pediatricians.Pediatrics.2006;118:441–447.
- ,,,,.Variation in pediatric hospitalists' use of unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- ,,,.Characteristics of the pediatric hospitalist workforce: its roles and work environment.Pediatrics.2007;120(1):33–39.
- ,,,,.General pediatrics resident perspectives on training decisions and career choice.Pediatrics.2009;123(suppl 1):S26–S30.
- ,,,,.Recently trained general pediatricians: perspectives on residency training and scope of practice.Pediatrics.2009;123(suppl 1):S38–S43.
- ,,,.PRIS survey: pediatric hospitalist roles and training needs [abstract].Pediatr Res.2004(55):1.
- ,,.The Residency Review and Redesign in Pediatrics (R3P) Project: roots and branches.Pediatrics.2009;123(suppl 1):S8–S11.
- ,.The hospitalist movement 5 years later.JAMA.2002;287(4):487–494.
- ,,.The Physician Strategist: Setting Strategic Direction for Your Practice; Chicago, Irwin Professional Pub,1996.
- ,.Pediatric hospitalists: training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- The Pediatric Core Competencies Supplement.J Hosp Med.2010;5(suppl 2):1–114.
- ,,,.Reauthorizing SCHIP: Opportunities for Promoting Effective Health Coverage and High Quality Care for Children and Adolescents. Publication 1051.New York, NY:The Commonwealth Fund; August2007:4.
- ,.National Association of Children's Hospitals. Quality Performance Measurement in Medicaid and SCHIP: Result of a 2006 National Survey of State Officials.Lansing, MI:Health Management Associates; August2006.
- ,,,.A report card on quality improvement for children's health care.Pediatrics.2001;107:143–155.
- ,,, et al.Impact of a hospitalist system on length of stay and cost for children with common conditions.Pediatrics.2007;120(2):267–274.
- ,,,,,.Variations in management of common inpatient pediatric illnesses: hospitalists and community pediatricians.Pediatrics.2006;118:441–447.
- ,,,,.Variation in pediatric hospitalists' use of unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- ,,,.Characteristics of the pediatric hospitalist workforce: its roles and work environment.Pediatrics.2007;120(1):33–39.
- ,,,,.General pediatrics resident perspectives on training decisions and career choice.Pediatrics.2009;123(suppl 1):S26–S30.
- ,,,,.Recently trained general pediatricians: perspectives on residency training and scope of practice.Pediatrics.2009;123(suppl 1):S38–S43.
- ,,,.PRIS survey: pediatric hospitalist roles and training needs [abstract].Pediatr Res.2004(55):1.
- ,,.The Residency Review and Redesign in Pediatrics (R3P) Project: roots and branches.Pediatrics.2009;123(suppl 1):S8–S11.
Prolonged Stay Factors in Bronchiolitis
Prior studies have identified risk factors for increased severity of illness, readmission, or prolonged length of stay (LOS) in infants admitted with bronchiolitis.123 These risk factors include birth‐related factors (prematurity, birth within six months of respiratory syncytial virus [RSV] season, discharge from the neonatal intensive care unit during winter, multiple birth infant), environmental factors (day care attendance, school‐age siblings, smoke exposure), and underlying diseases (chronic lung disease and other pulmonary conditions, failure to thrive (FTT), congenital heart disease, immunologic disorders, and neuromuscular disease).123 Additional risk factors occurring during the bronchiolitis course that have been associated with prolonged hospital course are mechanical ventilation, intensive care unit (ICU) admission, hypoxia on admission, apnea, feeding problems, and duration of supplemental oxygen.2123
Having a reliable model to identify infants at high risk for prolonged LOS early in the course of an admission would be helpful, both for clinical care and for studies of interventions designed to reduce LOS. Prior attempts at developing a model have yielded mixed results. The Michigan Logistic Regression Model displayed excellent predictive ability with an area under the receiver‐operator curve (ROC) of 0.88 using variables including prematurity, FTT, pulmonary disease, other comorbid diseases, and early mechanical ventilation.21 However, when applied to another patient population it did not perform as well. The Rotterdam Model using the variables of weight and supplemental oxygen had an ROC of 0.65.24
Prior prediction models have focused more on birth‐ and disease‐related risk factors than on hospital course factors, particularly common clinical assessments including respiratory status and caloric intake. An additional limitation of prior models is some loss of ability to study the interaction between various predictor variables when using multivariate regression methods.
Our aims were: 1) to study the associations of various clinical markers identifiable during the first two days of the hospital admission with LOS; and 2) to develop a LOS prediction model, using both previously identified risk factors and more detailed clinical data from the first two days of the hospital admission.
MATERIALS AND METHODS
Study Population and Setting
We conducted a retrospective cohort study during a single bronchiolitis season to identify factors predictive of a prolonged length of stay.
Children's Hospital of Wisconsin (CHW) is a 242‐bed tertiary care academic center. The charts of all infants discharged from CHW who met the following criteria were reviewed:
Age <365 days;
Admitted between November 1, 2004 and April 15, 2005;
Bronchiolitis diagnosis using the International Classification of Diseases, 9th edition (ICD‐9) discharge codes 466.11 (RSV bronchiolitis) or 466.19 (bronchiolitis from other organisms);
Placement on the CHW bronchiolitis treatment protocol. Major elements of this protocol include:
respiratory therapists (RT) assessments three times daily providing a standard means of evaluating severity of illness throughout the admission;
pre‐ and post‐intervention assessments.
Infants in this protocol differ from those not on the protocol; their average LOS is one day shorter and their care is more closely aligned with practices established in the Child Health Accountability Initiative (CHAI)25 and the American Academy of Pediatrics Guidelines,26 including: emphasis on clinical diagnosis rather than using laboratory and radiologic testing; avoiding routine bronchodilator use; and decreasing continuous pulse oximetry use. Only patients placed on the bronchiolitis treatment protocol were studied because these infants have a consistent model of care proven to be effective at CHW and other institutions25, 27; 70% of infants admitted to CHW with bronchiolitis were placed on the protocol. Common reasons for not placing infants on the protocol include: 1) the diagnosis of bronchiolitis was initially unclear; 2) the infant had chronic respiratory problems; and 3) physician preference.
Infants with events occurring during the admission not related to bronchiolitis and impacting LOS were excluded. Infants admitted or transferred to the ICU were included if placed on the bronchiolitis protocol; however, few ICU patients were placed on the protocol, as its intent is mainly for the general units.
Data Collected
Five trained abstractors (two were study authors) abstracted the following information from patient records: 1) baseline patient characteristics; 2) initial evaluation: respiratory rate, oxygen saturation, supplemental oxygen use, presence of increased work of breathing, weight, height, Waterlow percentile (percent of ideal body weight);28 3) fluid and nutritional information on hospital days 15; 4) respiratory assessments and treatments on hospital days 15 (clinical respiratory scores, respiratory rates, oxygen saturation, use of supplemental oxygen, medications received; 5) laboratory and imaging results; and 6) diagnoses. Each hospital day was defined as 0600 to 0559 the following day.
Clinical Respiratory Scores
The Children's Hospital of Wisconsin Respiratory Score (CHWRS) is a marker of overall respiratory status (not yet validated.) It contains six variables scored 03 based on degree: breath sounds, dyspnea, retractions, respiratory rate, heart rate, and supplemental oxygen. Scores range from 0 to 18, with lower scores representing less respiratory distress.
Outcomes and Analysis
The primary outcome was LOS, defined as the number of hours from the time a subject arrived on the hospital unit to time of last nursing documentation at time of discharge. The average LOS at CHW of 2.5 days is comparable to the lower end of that reported in the literature (2.85 days21, 22, 29, 30). LOS was dichotomized as short or prolonged, with prolonged LOS defined as 108 hours. We chose this length as it represents the 80th percentile LOS at our institution. Most physicians caring for infants with bronchiolitis at CHW use discharge criteria aligned with those in the hospitalist group's bronchiolitis clinical practice guideline,31 the SOFFFAR criteria: Sno longer dependent on nasopharyngeal suctioning; Ooff oxygen, or to baseline oxygen requirement; Ffamily agreeable to discharge; F follow‐up plan in place; FFeeding well enough to maintain hydration; Aif albuterol responsive, requiring treatments no more frequently than every six hours, Rrespiratory status acceptable (not too tachypneic or in respiratory distress).
Univariate Analysis
We examined the association between selected variables and LOS group (short or prolonged). Three groups of variables were studied: 1) variables identifiable upon admission (Table 1); 2) variables identifiable on hospital days 1 and 2 (Table 2); and 3) variables identifiable later in the admission. The variables evaluated were all non‐normally distributed and, therefore, the MannWhitney test was used to examine differences between groups with continuous or categorical variables. Dichotomous variables were compared using chi‐square or Fisher's exact test. SPSS (Chicago, IL) was used for these analyses. Because of multiple comparisons, 90% power and an alpha of 0.01 were used.
| Variable | Median (IQR), N [% of subjects] | P Value | |
|---|---|---|---|
| Short (N = 225) | Long (N = 47) | ||
| |||
| Age (days) | 134 (63‐225.5) | 139 (63‐240) | 0.86 |
| Gestation (weeks) | 40 (37‐40) | 39 (35‐40) | 0.07 |
| Race | |||
| White | 108 [48] | 23 [49] | 0.91 |
| Other | 117 [52] | 24 [51] | |
| Gender | |||
| Male | 121 [54] | 25 [53] | 0.94 |
| Respiratory support at birth | 22 [10] | 12 [26] | 0.003* |
| Chronic respiratory disease | 21 [9] | 8 [17] | 0.12 |
| Respiratory rate on admission | 56 (44‐64) | 56 (46‐66) | 0.58 |
| Cardiac conditions | 4 [2] | 3 [6] | 0.10 |
| Waterlow percent | 100 (92‐109) {n =203} | 96 (88‐107) {n =46} | 0.16 |
| Days of cough prior to admission | 4 (2‐6) {n =202} | 4 (2‐5) {n = 40} | 0.78 |
| Days of congestion prior to admission | 3 (1‐5) {n =183} | 3 (1‐5) {n =35} | 0.98 |
| Days of fever prior to admission | 1 (0‐3) {n =206} | 1 (0‐2) {n =43} | 0.50 |
| Days of decreased oral intake prior to admission | 1 (0‐2) {n =181} | 1 (0‐1) {n =36} | 0.44 |
| Variable | Median (IQR) or N [%] | P | Median (IQR) or N [%] | P | ||
|---|---|---|---|---|---|---|
| Short | Long | Short | Long | |||
| Hospital Day 1 | Hospital Day 2 | |||||
| ||||||
| Hours of supplemental oxygen | 3 (0‐10) | 11 (5‐17) | <0.001* | 3 (0‐19) | 24 (17‐24) | <0.001* |
| Minimum supplemental oxygen use (liters) | 0 (0‐0.1) | 0.25 (0‐0.5) | <0.001* | 0 (0‐0) | 0.2 (0‐0.5) | <0.001* |
| Maximum supplemental oxygen use (liters) | 0.5 (0‐1) | 0.75 (0.5‐1.5) | <0.001* | 0.2 (0‐0.5) | 1 (0.5‐1.5) | <0.001* |
| Minimum oxygen saturation (percent) | 94 (92‐96) | 94 (92‐96) | 0.89 | 94 (92‐95) | 93 (91‐94) | 0.001* |
| Maximum oxygen saturation (percent) | 99 (98‐100) | 100 (99‐100) | 0.23 | 100 (98‐100) | 100 (99‐100) | 0.37 |
| Minimum respiratory rate | 36 (32‐46) | 36 (32‐46) | 0.92 | 34 (30‐40) | 36 (32‐41) | 0.11 |
| Maximum respiratory rate | 53 (45‐62) | 56 (48‐64) | 0.14 | 55 (48‐64) | 63 (52‐75) | <0.001* |
| Mean respiratory score | 4 (3‐5.5) | 5 (4‐6.7) | 0.008* | 3.4 (2.7‐4.5) | 4.8 (3.7‐7) | <0.001* |
| Change in respiratory score | 0 (0‐1) | 0 (1‐1.5) | 0.3 | 1 (0‐2) | 0 (‐2‐2) | 0.022 |
| Number of times nasopharyngeal suctioned | 1 (0‐2) | 2 (1‐3) | 0.012 | 1 (0‐3) | 4 (2‐5) | <0.001* |
| Calories consumed (Kcal/kg/day) | 53 (22‐82) | 54 (33‐79) | 0.801 | 66 (47‐90) | 54 (21‐72) | 0.001* |
| ICU (% of subjects) | 4 (1.8%) | 2 (4.3%) | 0.28 | 4 (1.8%) | 5 (10.6%) | 0.009* |
Recursive Partitioning Analysis
We chose recursive partitioning as the method for model creation instead of multivariate linear regression in order to: 1) study multiple possible variable interactions without having to create multiple interaction terms; and 2) generate an easy‐to‐use flow diagram to identify infants at risk for prolonged LOS without having to use a complex formula generated by multivariate regression. In recursive partitioning methodology, the statistical program selects the variable among the set of candidate variables that best separates the first parent node with all subjects into short and prolonged stay intermediate nodes. The process is repeated with additional variables selected that further separate the intermediate nodes into short and prolonged stay nodes, until finally a flow diagram is generated, resulting in terminal nodes of predicted short and prolonged stay subjects. Recursive partitioning was performed using Salford Systems' CART software San Diego, CA. The minimum number of cases required in parent/emntermediate nodes was 20, and in terminal nodes was 5. Eighty percent of cases were randomly selected for the learning tree, and 20% in the test tree for cross‐validation.
Sixteen variables were considered a priori as potentially important in affecting LOS and were candidates for inclusion. These included five baseline variables (age, gestation, Waterlow percentile, presence of chronic respiratory disease, and a marker for missing Waterlow percentile) and 11 variables from hospital day 2 (kcal/kg/day consumed, hours of supplemental oxygen, maximum supplemental oxygen use, maximum oxygen saturation, maximum respiratory rate, minimum supplemental oxygen use, minimum oxygen saturation, minimum respiratory rate, mean clinical respiratory score, change in respiratory score, and nasopharyngeal suctioning frequency). Hospital day 2 variables were chosen rather than hospital day 1, because hospital day 1 was only a partial day in the hospital for the majority of subjects. Several aspects of oxygenation were studied because oxygen need has been consistently found to be an important predictor of LOS. We sought to discover which particular aspect of oxygen need was most important. For comparison, recursive partitioning was performed on the variable sets taken from the Michigan (weight, congenital heart disease, failure to thrive, gestational age, chronic pulmonary diseases, and early mechanical ventilation)21 and Rotterdam (weight and need for supplemental oxygen)24 Models.
This study was approved by the CHW Institutional Review Board.
RESULTS
Three hundred forty‐seven infants were admitted during the 20042005 bronchiolitis season, with 273 placed in the bronchiolitis treatment protocol. The charts of these 273 patients were reviewed. One was excluded because of gastrostomy tube placement during the admission. Of the remaining 272 patients, 47 (17.3%) had a LOS 108 hours. The median LOS was 59 hours (range 10334 hours). Two patients had missing data for caloric intake on days 1 and 2; and 23 patients did not have height obtained, therefore their Waterlow classification could not be determined. Historical details concerning fever, congestion, cough, and diminished caloric intake preceding admission were variably reported, resulting in a smaller sample size for these baseline characteristics as described in Table 1.
Univariate Analysis
Baseline characteristics of infants having short and prolonged LOS are described in Table 1. Groups were statistically similar except that the long stay group contained a significantly larger proportion of infants requiring respiratory support at birth (defined as needing intubation, continuous positive airway pressure [CPAP], or oxygen).
Table 2 describes selected variables on hospital days 1 and 2 in infants having short and prolonged LOS. On hospital day 1, infants in the prolonged LOS group had a significantly greater need for supplemental oxygen, and mean respiratory score. On hospital day 2, infants in the prolonged LOS group had a significantly greater need for supplemental oxygen maximum respiratory rate, mean respiratory score, and number of times they were suctioned. They had a significantly lower minimum oxygen saturation and caloric intake. On hospital day 2, the prolonged LOS group had a greater proportion of subjects in the ICU, on CPAP, and on the ventilator.
We examined two characteristics identifiable after the second hospital day. There was a significant difference in: a) the median number of discharge diagnoses in the short LOS group (two) vs the prolonged LOS group (three) (P < 0.001); and b) the presence of apnea during the admission in the short LOS group (0.1%) vs the prolonged LOS group (9%) (P = 0.009).
Recursive Partitioning Model
Figure 1 depicts the recursive partitioning model that best predicted LOS. Five variables were selected by the recursive partitioning model. Selected variables, in order of appearance (variable importance is related to order of appearance, ie, most important variable is first), were: hours of supplemental oxygen, maximum respiratory rate, minimum supplemental oxygen use, gestation, and kilocalories (kcal)/kilogram (kg)/day consumed. The characteristics of this model were: ROC 0.89 and 0.72 for the learning and test trees, respectively; sensitivity, 0.85; and specificity, 0.82
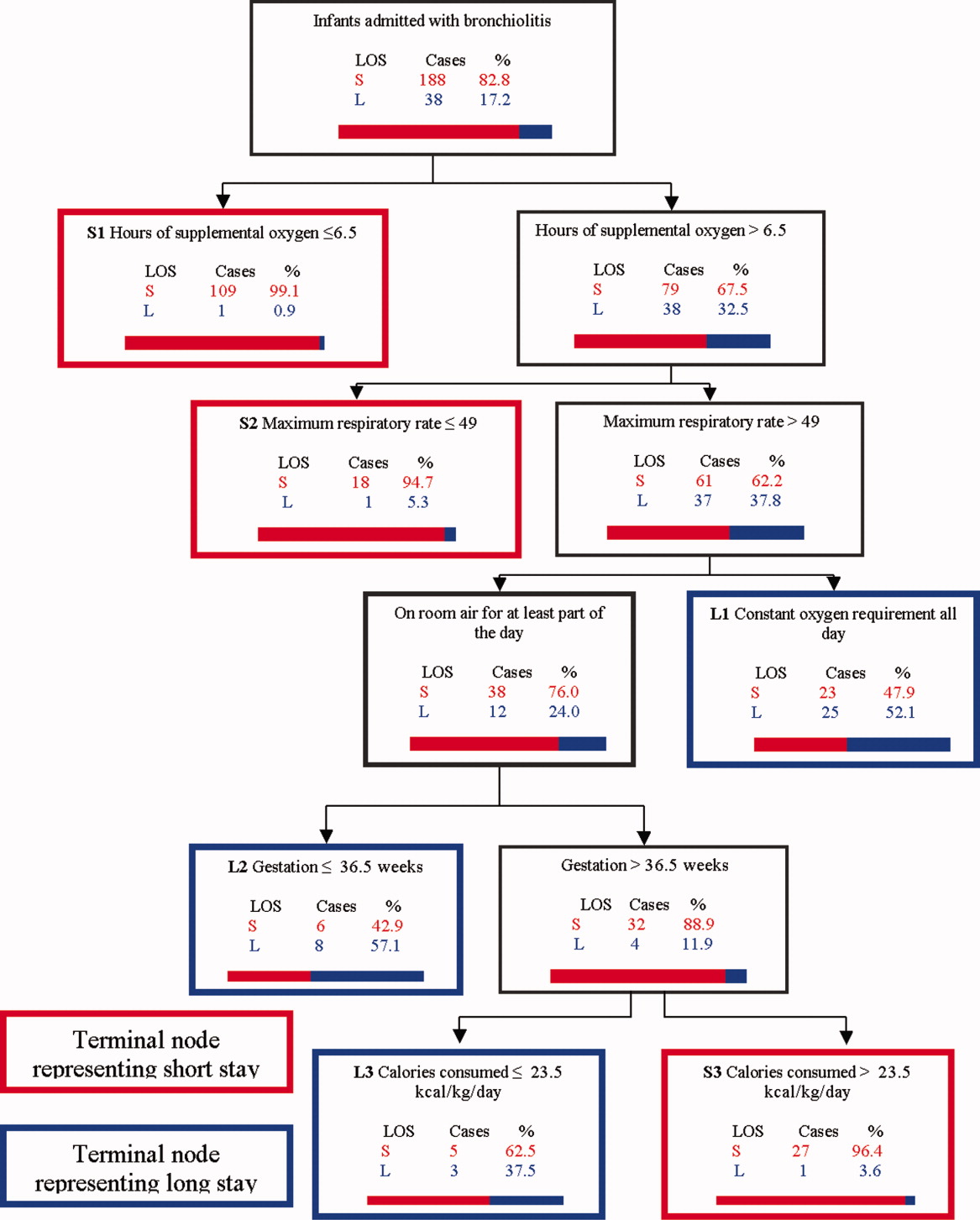
Infants predicted as having a short LOS had three distinct profiles labeled S1, S2, and S3 in Figure 1. The S1 group required 6.5 hours of oxygen. The S2 group required >6.5 hours of oxygen, but had a maximum respiratory rate 49. The S3 group required >6.5 hours of oxygen, had a maximum respiratory rate >49, but were >36.5 week gestation, and consumed >23.5 kcal/kg/day.
Infants predicted as having a long LOS had three distinct profiles labeled L1, L2, and L3 in Figure 1. The L1 group required >6.5 hours of supplemental oxygen, had a maximum respiratory rate >49, and required some level of oxygen support the entire day. The L2 group required >6.5 hours of supplemental oxygen, had a maximum respiratory rate >49, were on room air some portion of the day, but had a gestation 36.5 weeks. The L3 group required >6.5 hours of supplemental oxygen, had a maximum respiratory rate >49, were on room air for some portion of the day, had a gestation >36.5 weeks, but consumed 23.5 kcal/kg/day.
Table 3 compares the performance of our model (the Milwaukee Model), the Michigan Model, and the Rotterdam Model in predicting LOS group. Overall, the Milwaukee Model had the highest ROC 0.89/0.72 for the learning and test trees. All three models had good sensitivity (Milwaukee, 85%; Michigan, 85%), with the Rotterdam Model having the highest (98%). The Milwaukee Model also had good specificity (82%), while the Michigan and Rotterdam Models were less specific (46% and 44%).
| Model | Priors* | Sensitivity | Specificity | Learning Tree ROC | Test Tree ROC | |
|---|---|---|---|---|---|---|
| Long LOS | Short LOS | |||||
| ||||||
| Michigan | 0.5 | 0.5 | 0.85 | 0.46 | 0.69 | 0.56 |
| Rotterdam | 0.5 | 0.5 | 0.98 | 0.44 | 0.73 | 0.61 |
| Milwaukee | 0.5 | 0.5 | 0.85 | 0.82 | 0.89 | 0.72 |
DISCUSSION
We confirmed several previously recognized risk factors for prolonged LOS, including: apnea, at least part of the hospital stay in ICU, use of CPAP, mechanical ventilation, and prematurity. However, most patients admitted with bronchiolitis do not have these risk factors. The major contribution of this study is the evaluation of factors applicable to all patients admitted with bronchiolitis, and a more in‐depth analysis of clinical assessments performed on hospital days 1 and 2 than had been previously reported.
We did find strong associations between a number of clinical assessments and LOS. While some were apparent on day 1 of the admission, the number and degree of clinical differences between infants destined for a short vs prolonged stay were more apparent on hospital day 2. On this day, there were significant differences between the groups in the length and amount of oxygen received, oxygen saturation, maximum respiratory rate, respiratory scores, nasopharyngeal suctioning need, and caloric intake. Interestingly, it was noted the prolonged stay group had overall worsening or a lack of improvement in several clinical markers from day 1 to day 2, in areas where the short stay group showed improvements.
To our knowledge, the Milwaukee Model is the first bronchiolitis LOS prediction model to incorporate several clinical markers occurring early in the hospital stay. These clinical markers were found to be more effective predictors of LOS group in our study population than some of the traditional birth‐ and disease‐related risk factors previously reported. The model highlighted some important interactions among variables, and identified specific profiles of patients likely to have a short or prolonged LOS based on their day 2 clinical status.
The short LOS groups all shared one of the following three features: 1) low duration of oxygen use; 2) absence of tachypnea (tachypnea defined as a respiratory rate >60 in infants <2 months old and >50 for infants between 2 and 12 months old.3234); or 3) absence of severely diminished caloric intake. The prolonged LOS groups shared the common characteristics of higher duration of oxygen use and higher maximum respiratory rates. In addition to these two elements, each long stay group had either a constant oxygen requirement, prematurity (36.5 weeks), or very low caloric intake (<23.5 kcal/kg/day).
While all three models shared good sensitivity, the increased specificity of the Milwaukee Model limits the number of false positives (infants screening as destined for a prolonged LOS who actually will have a short LOS). For clinicians or researchers planning interventions for high‐risk infants, this greater specificity would reduce the number of infants who might unnecessarily receive those interventions. While there are limited proven therapies to hasten the recovery of patients with bronchiolits,35 many treatments and combinations of treatments are currently being used and studied. Nebulized hypertonic saline,36 airway secretion clearance modalities,37 and nutritional supplementation22, 38 are some examples of interventions that could be used and evaluated in infants screened as high risk for prolonged LOS. While it may have been better to identify short vs long stay immediately upon admission or after hospital day 1, it was the more clear separation between the short and long stay groups that occurred on day 2 that allowed us to develop an accurate predictive model. We believe that for infants destined to be in the hospital for at least three more days, a model based on hospital day 2 variables is worthwhile.
When evaluating the characteristics of the three models, it is important to note that they were initially studied in populations with some important differences. Only 11% of Milwaukee patients had chronic respiratory diseases, whereas the previously developed models were generated from a sample with a higher prevalence of chronic respiratory diseases (Michigan, 20%; Rotterdam, 23%). Only 3% of subjects needed placement in the ICU compared to higher rates in prior studies (Michigan, 15%; Rotterdam, 43.5%). In a population of patients with a lower prevalence of chronic respiratory diseases and need for ICU, early clinical markers may become more important in predicting LOS. While our model may generalize well in such a cohort of patients, it might not generalize as well to a cohort with a high prevalence of chronic lung disease and higher need for ICU. It is also important to note that the area under the ROC was lower in the test tree than the learning tree. This variation demonstrates the need for evaluating the performance of this model in additional populations.
This study has several limitations. First, it is a retrospective study of a single bronchiolitis season at a single institution. Second, the authors served as data abstractors and could have been biased, as they were not blinded. Third, four out of the five markers in our model are clinical markers that could vary based on clinical assessment skills and institutional practice. For example, oxygen use is dependent on the practice of nurses and respiratory therapists charged with regulating the oxygen delivery. However, the practice of initiating and weaning oxygen is fairly standardized at our institution. Fourth, environmental and social risk factors, such as day care attendance, school‐age siblings, and smoke exposure, can impact LOS but were not included in our model. Fifth, we do not have data on those infants not included in the bronchiolitis protocol. It is possible that they differed from those in protocol. Finally, six infants were either placed or transferred to the ICU on day 1, which may make them inherently different than the other infants in the model. However, four out of these six infants did go on to have a short stay, highlighting the fact that many other factors affect LOS.
We believe this model may be useful because the clinical markers it uses represent some of the key problems seen in bronchiolitis (poor oxygenation, tachypnea, and poor feeding). Careful assessment of these clinical markers can allow effective prediction of those infants likely to have a prolonged LOS. This early risk assessment could allow more effective targeting of interventions to help high‐risk infants.
CONCLUSIONS
There are important differences between infants with bronchiolitis having short and prolonged hospital stays, including several clinical markers identifiable on hospital day 2, such as the length and amount of oxygen received, minimum oxygen saturation, maximum respiratory rate, clinical respiratory scores, deep suctioning need, and caloric intake. The Milwaukee Model uses the number of hours of supplemental oxygen, respiratory rate, minimum supplemental oxygen use, gestation, and caloric intake to predict short or prolonged LOS. It performed well with a good ROC, sensitivity, and specificity in one population of infants with a low prevalence of chronic respiratory disease.
- ,.Clinical significance of respiratory syncytial virus.Postgrad Med.1964;35:460–465.
- ,,,,.Respiratory syncytial virus infection in young hospitalized children. Identification of risk patients and prevention of nosocomial spread by rapid diagnosis.Acta Paediatr Scand.1983;72(1):47–51.
- .Pathogenesis of bronchiolitis—epidemiologic considerations.Pediatr Res.1977;11(3 pt 2):239–243.
- ,,.Respiratory syncytial virus infection in children with bronchopulmonary dysplasia.Pediatrics.1988;82(2):199–203.
- ,,, et al.Respiratory syncytial viral infection in children with compromised immune function.N Engl J Med.1986;315(2):77–81.
- ,,,,.Risk of secondary bacterial infection in infants hospitalized with respiratory syncytial viral infection.J Pediatr.1988;113(2):266–271.
- ,,,,,.Respiratory syncytial viral infection in infants with congenital heart disease.N Engl J Med.1982;307(7):397–400.
- ,,, et al.Hospitalized children with respiratory syncytial virus infection and neuromuscular impairment face an increased risk of a complicated course.Pediatr Infect Dis J.2007;26(6):485–491.
- ,,.Rehospitalization for respiratory illness in infants of less than 32 weeks' gestation.Pediatrics.1991;88(3):527–532.
- ,,, et al.Respiratory syncytial virus (RSV) immune globulin intravenous therapy for RSV lower respiratory tract infection in infants and young children at high risk for severe RSV infections: Respiratory Syncytial Virus Immune Globulin Study Group.Pediatrics.1997;99(3):454–461.
- ,,,,.Risk factors for bronchiolitis‐associated deaths among infants in the United States.Pediatr Infect Dis J.2003;22(6):483–490.
- ,.Risk factors for severe respiratory syncytial virus infection in infants.Respir Med.2002;96(suppl B):S9–S14.
- ,,,,.Rehospitalization for respiratory syncytial virus among premature infants.Pediatrics.1999;104(4 pt 1):894–899.
- ,,,,.Risk of respiratory syncytial virus infection for infants from low‐income families in relationship to age, sex, ethnic group, and maternal antibody level.J Pediatr.1981;98(5):708–715.
- ,,,.Preterm twins and triplets. A high‐risk group for severe respiratory syncytial virus infection.Am J Dis Child.1993;147(3):303–306.
- ,,, et al.Rehospitalization because of respiratory syncytial virus infection in premature infants younger than 33 weeks of gestation: a prospective study. IRIS Study Group.Pediatr Infect Dis J.2000;19(7):592–597.
- ,.Parental smoking, presence of older siblings, and family history of asthma increase risk of bronchiolitis.Am J Dis Child.1986;140(8):806–812.
- ,,,,.Role of respiratory syncytial virus in early hospitalizations for respiratory distress of young infants with cystic fibrosis.J Pediatr.1988;113(5):826–830.
- ,,, et al.Variable morbidity of respiratory syncytial virus infection in patients with underlying lung disease: a review of the PICNIC RSV database. Pediatric Investigators Collaborative Network on Infections in Canada.Pediatr Infect Dis J.1999;18(10):866–869.
- ,,,,.Rates of hospitalization for respiratory syncytial virus infection among children in Medicaid.J Pediatr.2000;137(6):865–870.
- ,.Severity of illness models for respiratory syncytial virus‐associated hospitalization.Am J Respir Crit Care Med.1999;159(4 pt 1):1234–1240.
- ,.Effect of oxygen supplementation on length of stay for infants hospitalized with acute viral bronchiolitis.Pediatrics.2008;121(3):470–475.
- ,,.Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) prospective study of risk factors and outcomes in patients hospitalized with respiratory syncytial viral lower respiratory tract infection.J Pediatr.1995;126(2):212–219.
- ,,,.Prediction of duration of hospitalization in respiratory syncytial virus infection.Pediatr Pulmonol.2002;33(6):453–457.
- ,,,,,.Impact of a bronchiolitis guideline: a multisite demonstration project.Chest.2002;121(6):1789–1797.
- , , , , , , , , , Diagnosis and management of bronchiolitis.Pediatrics.2006;118(4):1774–1793.
- ,,, et al.Evaluation of an evidence‐based guideline for bronchiolitis.Pediatrics.1999;104(6):1334–1341.
- .Classification and definition of protein‐calorie malnutrition.Br Med J.1972;3(5826):566–569.
- ,,,,.Inpatient care for uncomplicated bronchiolitis: comparison with Milliman and Robertson guidelines.Arch Pediatr Adolesc Med.2001;155(12):1323–1327.
- ,,,.Impact of pulse oximetry and oxygen therapy on length of stay in bronchiolitis hospitalizations.Arch Pediatr Adolesc Med.2004;158(6):527–530.
- .Bronchiolitis clinical practice guideline.Children's Hospital of Wisconsin Intranet;2007. http://clinicalpractice.chw.org/display/displayFile.asp?docid=393185(2):319–336.
- ,.The rational clinical examination. Does this infant have pneumonia?JAMA.1998;279(4):308–313.
- ,.Focused ethnographic studies in the WHO Programme for the Control of Acute Respiratory Infections.Med Anthropol.1994;15(4):409–424.
- ,.Bronchiolitis: recent evidence on diagnosis and management.Pediatrics.125(2):342–349.
- ,,,.Nebulized hypertonic saline solution for acute bronchiolitis in infants.Cochrane Database Syst Rev.2008(4):CD006458.
- .Airway clearance applications in infants and children.Respir Care.2007;52(10):1382–1391.
- ,.Immunonutrition in critically ill patients: a systematic review and analysis of the literature.Intensive Care Med.2008;34(11):1980–1990.
Prior studies have identified risk factors for increased severity of illness, readmission, or prolonged length of stay (LOS) in infants admitted with bronchiolitis.123 These risk factors include birth‐related factors (prematurity, birth within six months of respiratory syncytial virus [RSV] season, discharge from the neonatal intensive care unit during winter, multiple birth infant), environmental factors (day care attendance, school‐age siblings, smoke exposure), and underlying diseases (chronic lung disease and other pulmonary conditions, failure to thrive (FTT), congenital heart disease, immunologic disorders, and neuromuscular disease).123 Additional risk factors occurring during the bronchiolitis course that have been associated with prolonged hospital course are mechanical ventilation, intensive care unit (ICU) admission, hypoxia on admission, apnea, feeding problems, and duration of supplemental oxygen.2123
Having a reliable model to identify infants at high risk for prolonged LOS early in the course of an admission would be helpful, both for clinical care and for studies of interventions designed to reduce LOS. Prior attempts at developing a model have yielded mixed results. The Michigan Logistic Regression Model displayed excellent predictive ability with an area under the receiver‐operator curve (ROC) of 0.88 using variables including prematurity, FTT, pulmonary disease, other comorbid diseases, and early mechanical ventilation.21 However, when applied to another patient population it did not perform as well. The Rotterdam Model using the variables of weight and supplemental oxygen had an ROC of 0.65.24
Prior prediction models have focused more on birth‐ and disease‐related risk factors than on hospital course factors, particularly common clinical assessments including respiratory status and caloric intake. An additional limitation of prior models is some loss of ability to study the interaction between various predictor variables when using multivariate regression methods.
Our aims were: 1) to study the associations of various clinical markers identifiable during the first two days of the hospital admission with LOS; and 2) to develop a LOS prediction model, using both previously identified risk factors and more detailed clinical data from the first two days of the hospital admission.
MATERIALS AND METHODS
Study Population and Setting
We conducted a retrospective cohort study during a single bronchiolitis season to identify factors predictive of a prolonged length of stay.
Children's Hospital of Wisconsin (CHW) is a 242‐bed tertiary care academic center. The charts of all infants discharged from CHW who met the following criteria were reviewed:
Age <365 days;
Admitted between November 1, 2004 and April 15, 2005;
Bronchiolitis diagnosis using the International Classification of Diseases, 9th edition (ICD‐9) discharge codes 466.11 (RSV bronchiolitis) or 466.19 (bronchiolitis from other organisms);
Placement on the CHW bronchiolitis treatment protocol. Major elements of this protocol include:
respiratory therapists (RT) assessments three times daily providing a standard means of evaluating severity of illness throughout the admission;
pre‐ and post‐intervention assessments.
Infants in this protocol differ from those not on the protocol; their average LOS is one day shorter and their care is more closely aligned with practices established in the Child Health Accountability Initiative (CHAI)25 and the American Academy of Pediatrics Guidelines,26 including: emphasis on clinical diagnosis rather than using laboratory and radiologic testing; avoiding routine bronchodilator use; and decreasing continuous pulse oximetry use. Only patients placed on the bronchiolitis treatment protocol were studied because these infants have a consistent model of care proven to be effective at CHW and other institutions25, 27; 70% of infants admitted to CHW with bronchiolitis were placed on the protocol. Common reasons for not placing infants on the protocol include: 1) the diagnosis of bronchiolitis was initially unclear; 2) the infant had chronic respiratory problems; and 3) physician preference.
Infants with events occurring during the admission not related to bronchiolitis and impacting LOS were excluded. Infants admitted or transferred to the ICU were included if placed on the bronchiolitis protocol; however, few ICU patients were placed on the protocol, as its intent is mainly for the general units.
Data Collected
Five trained abstractors (two were study authors) abstracted the following information from patient records: 1) baseline patient characteristics; 2) initial evaluation: respiratory rate, oxygen saturation, supplemental oxygen use, presence of increased work of breathing, weight, height, Waterlow percentile (percent of ideal body weight);28 3) fluid and nutritional information on hospital days 15; 4) respiratory assessments and treatments on hospital days 15 (clinical respiratory scores, respiratory rates, oxygen saturation, use of supplemental oxygen, medications received; 5) laboratory and imaging results; and 6) diagnoses. Each hospital day was defined as 0600 to 0559 the following day.
Clinical Respiratory Scores
The Children's Hospital of Wisconsin Respiratory Score (CHWRS) is a marker of overall respiratory status (not yet validated.) It contains six variables scored 03 based on degree: breath sounds, dyspnea, retractions, respiratory rate, heart rate, and supplemental oxygen. Scores range from 0 to 18, with lower scores representing less respiratory distress.
Outcomes and Analysis
The primary outcome was LOS, defined as the number of hours from the time a subject arrived on the hospital unit to time of last nursing documentation at time of discharge. The average LOS at CHW of 2.5 days is comparable to the lower end of that reported in the literature (2.85 days21, 22, 29, 30). LOS was dichotomized as short or prolonged, with prolonged LOS defined as 108 hours. We chose this length as it represents the 80th percentile LOS at our institution. Most physicians caring for infants with bronchiolitis at CHW use discharge criteria aligned with those in the hospitalist group's bronchiolitis clinical practice guideline,31 the SOFFFAR criteria: Sno longer dependent on nasopharyngeal suctioning; Ooff oxygen, or to baseline oxygen requirement; Ffamily agreeable to discharge; F follow‐up plan in place; FFeeding well enough to maintain hydration; Aif albuterol responsive, requiring treatments no more frequently than every six hours, Rrespiratory status acceptable (not too tachypneic or in respiratory distress).
Univariate Analysis
We examined the association between selected variables and LOS group (short or prolonged). Three groups of variables were studied: 1) variables identifiable upon admission (Table 1); 2) variables identifiable on hospital days 1 and 2 (Table 2); and 3) variables identifiable later in the admission. The variables evaluated were all non‐normally distributed and, therefore, the MannWhitney test was used to examine differences between groups with continuous or categorical variables. Dichotomous variables were compared using chi‐square or Fisher's exact test. SPSS (Chicago, IL) was used for these analyses. Because of multiple comparisons, 90% power and an alpha of 0.01 were used.
| Variable | Median (IQR), N [% of subjects] | P Value | |
|---|---|---|---|
| Short (N = 225) | Long (N = 47) | ||
| |||
| Age (days) | 134 (63‐225.5) | 139 (63‐240) | 0.86 |
| Gestation (weeks) | 40 (37‐40) | 39 (35‐40) | 0.07 |
| Race | |||
| White | 108 [48] | 23 [49] | 0.91 |
| Other | 117 [52] | 24 [51] | |
| Gender | |||
| Male | 121 [54] | 25 [53] | 0.94 |
| Respiratory support at birth | 22 [10] | 12 [26] | 0.003* |
| Chronic respiratory disease | 21 [9] | 8 [17] | 0.12 |
| Respiratory rate on admission | 56 (44‐64) | 56 (46‐66) | 0.58 |
| Cardiac conditions | 4 [2] | 3 [6] | 0.10 |
| Waterlow percent | 100 (92‐109) {n =203} | 96 (88‐107) {n =46} | 0.16 |
| Days of cough prior to admission | 4 (2‐6) {n =202} | 4 (2‐5) {n = 40} | 0.78 |
| Days of congestion prior to admission | 3 (1‐5) {n =183} | 3 (1‐5) {n =35} | 0.98 |
| Days of fever prior to admission | 1 (0‐3) {n =206} | 1 (0‐2) {n =43} | 0.50 |
| Days of decreased oral intake prior to admission | 1 (0‐2) {n =181} | 1 (0‐1) {n =36} | 0.44 |
| Variable | Median (IQR) or N [%] | P | Median (IQR) or N [%] | P | ||
|---|---|---|---|---|---|---|
| Short | Long | Short | Long | |||
| Hospital Day 1 | Hospital Day 2 | |||||
| ||||||
| Hours of supplemental oxygen | 3 (0‐10) | 11 (5‐17) | <0.001* | 3 (0‐19) | 24 (17‐24) | <0.001* |
| Minimum supplemental oxygen use (liters) | 0 (0‐0.1) | 0.25 (0‐0.5) | <0.001* | 0 (0‐0) | 0.2 (0‐0.5) | <0.001* |
| Maximum supplemental oxygen use (liters) | 0.5 (0‐1) | 0.75 (0.5‐1.5) | <0.001* | 0.2 (0‐0.5) | 1 (0.5‐1.5) | <0.001* |
| Minimum oxygen saturation (percent) | 94 (92‐96) | 94 (92‐96) | 0.89 | 94 (92‐95) | 93 (91‐94) | 0.001* |
| Maximum oxygen saturation (percent) | 99 (98‐100) | 100 (99‐100) | 0.23 | 100 (98‐100) | 100 (99‐100) | 0.37 |
| Minimum respiratory rate | 36 (32‐46) | 36 (32‐46) | 0.92 | 34 (30‐40) | 36 (32‐41) | 0.11 |
| Maximum respiratory rate | 53 (45‐62) | 56 (48‐64) | 0.14 | 55 (48‐64) | 63 (52‐75) | <0.001* |
| Mean respiratory score | 4 (3‐5.5) | 5 (4‐6.7) | 0.008* | 3.4 (2.7‐4.5) | 4.8 (3.7‐7) | <0.001* |
| Change in respiratory score | 0 (0‐1) | 0 (1‐1.5) | 0.3 | 1 (0‐2) | 0 (‐2‐2) | 0.022 |
| Number of times nasopharyngeal suctioned | 1 (0‐2) | 2 (1‐3) | 0.012 | 1 (0‐3) | 4 (2‐5) | <0.001* |
| Calories consumed (Kcal/kg/day) | 53 (22‐82) | 54 (33‐79) | 0.801 | 66 (47‐90) | 54 (21‐72) | 0.001* |
| ICU (% of subjects) | 4 (1.8%) | 2 (4.3%) | 0.28 | 4 (1.8%) | 5 (10.6%) | 0.009* |
Recursive Partitioning Analysis
We chose recursive partitioning as the method for model creation instead of multivariate linear regression in order to: 1) study multiple possible variable interactions without having to create multiple interaction terms; and 2) generate an easy‐to‐use flow diagram to identify infants at risk for prolonged LOS without having to use a complex formula generated by multivariate regression. In recursive partitioning methodology, the statistical program selects the variable among the set of candidate variables that best separates the first parent node with all subjects into short and prolonged stay intermediate nodes. The process is repeated with additional variables selected that further separate the intermediate nodes into short and prolonged stay nodes, until finally a flow diagram is generated, resulting in terminal nodes of predicted short and prolonged stay subjects. Recursive partitioning was performed using Salford Systems' CART software San Diego, CA. The minimum number of cases required in parent/emntermediate nodes was 20, and in terminal nodes was 5. Eighty percent of cases were randomly selected for the learning tree, and 20% in the test tree for cross‐validation.
Sixteen variables were considered a priori as potentially important in affecting LOS and were candidates for inclusion. These included five baseline variables (age, gestation, Waterlow percentile, presence of chronic respiratory disease, and a marker for missing Waterlow percentile) and 11 variables from hospital day 2 (kcal/kg/day consumed, hours of supplemental oxygen, maximum supplemental oxygen use, maximum oxygen saturation, maximum respiratory rate, minimum supplemental oxygen use, minimum oxygen saturation, minimum respiratory rate, mean clinical respiratory score, change in respiratory score, and nasopharyngeal suctioning frequency). Hospital day 2 variables were chosen rather than hospital day 1, because hospital day 1 was only a partial day in the hospital for the majority of subjects. Several aspects of oxygenation were studied because oxygen need has been consistently found to be an important predictor of LOS. We sought to discover which particular aspect of oxygen need was most important. For comparison, recursive partitioning was performed on the variable sets taken from the Michigan (weight, congenital heart disease, failure to thrive, gestational age, chronic pulmonary diseases, and early mechanical ventilation)21 and Rotterdam (weight and need for supplemental oxygen)24 Models.
This study was approved by the CHW Institutional Review Board.
RESULTS
Three hundred forty‐seven infants were admitted during the 20042005 bronchiolitis season, with 273 placed in the bronchiolitis treatment protocol. The charts of these 273 patients were reviewed. One was excluded because of gastrostomy tube placement during the admission. Of the remaining 272 patients, 47 (17.3%) had a LOS 108 hours. The median LOS was 59 hours (range 10334 hours). Two patients had missing data for caloric intake on days 1 and 2; and 23 patients did not have height obtained, therefore their Waterlow classification could not be determined. Historical details concerning fever, congestion, cough, and diminished caloric intake preceding admission were variably reported, resulting in a smaller sample size for these baseline characteristics as described in Table 1.
Univariate Analysis
Baseline characteristics of infants having short and prolonged LOS are described in Table 1. Groups were statistically similar except that the long stay group contained a significantly larger proportion of infants requiring respiratory support at birth (defined as needing intubation, continuous positive airway pressure [CPAP], or oxygen).
Table 2 describes selected variables on hospital days 1 and 2 in infants having short and prolonged LOS. On hospital day 1, infants in the prolonged LOS group had a significantly greater need for supplemental oxygen, and mean respiratory score. On hospital day 2, infants in the prolonged LOS group had a significantly greater need for supplemental oxygen maximum respiratory rate, mean respiratory score, and number of times they were suctioned. They had a significantly lower minimum oxygen saturation and caloric intake. On hospital day 2, the prolonged LOS group had a greater proportion of subjects in the ICU, on CPAP, and on the ventilator.
We examined two characteristics identifiable after the second hospital day. There was a significant difference in: a) the median number of discharge diagnoses in the short LOS group (two) vs the prolonged LOS group (three) (P < 0.001); and b) the presence of apnea during the admission in the short LOS group (0.1%) vs the prolonged LOS group (9%) (P = 0.009).
Recursive Partitioning Model
Figure 1 depicts the recursive partitioning model that best predicted LOS. Five variables were selected by the recursive partitioning model. Selected variables, in order of appearance (variable importance is related to order of appearance, ie, most important variable is first), were: hours of supplemental oxygen, maximum respiratory rate, minimum supplemental oxygen use, gestation, and kilocalories (kcal)/kilogram (kg)/day consumed. The characteristics of this model were: ROC 0.89 and 0.72 for the learning and test trees, respectively; sensitivity, 0.85; and specificity, 0.82
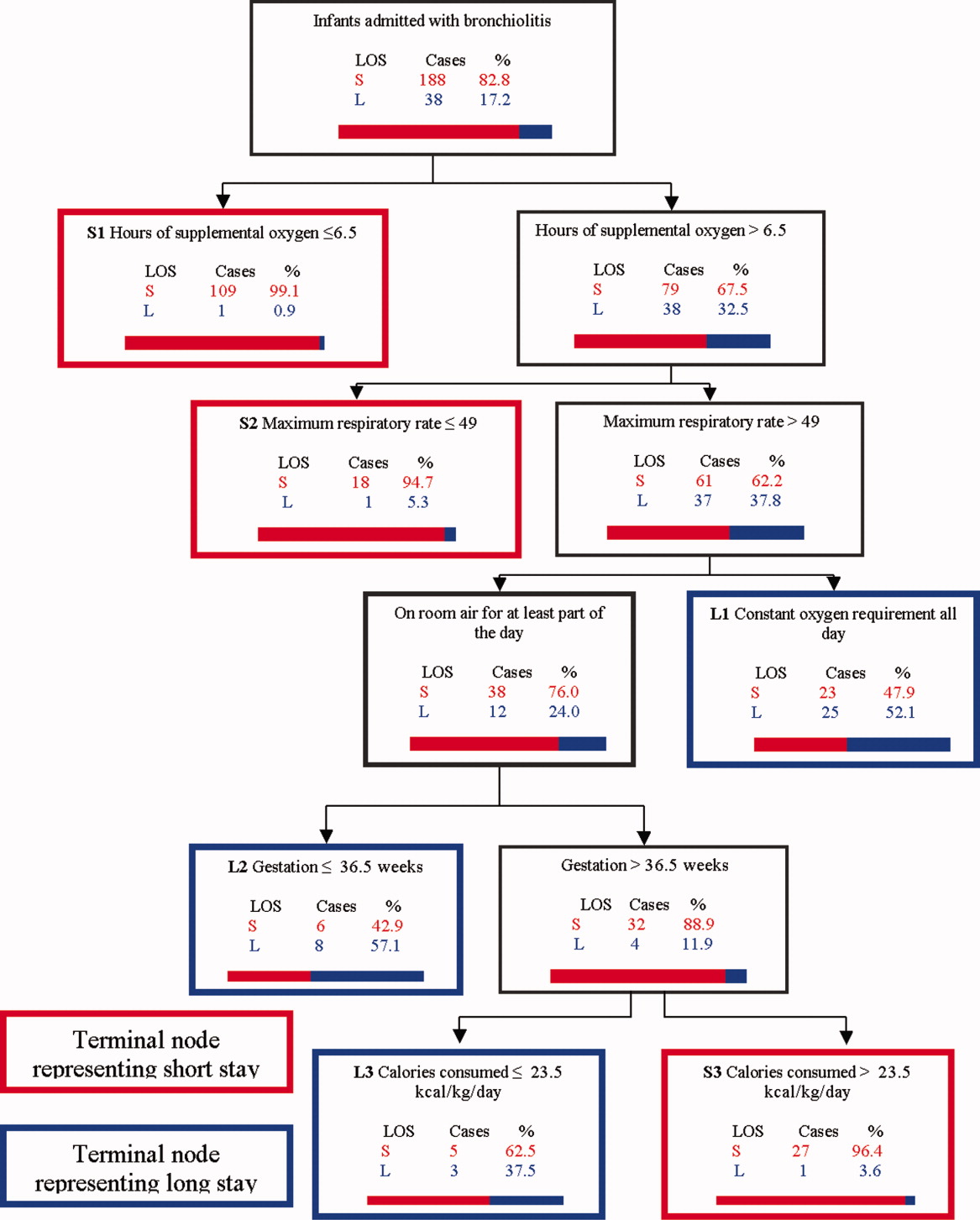
Infants predicted as having a short LOS had three distinct profiles labeled S1, S2, and S3 in Figure 1. The S1 group required 6.5 hours of oxygen. The S2 group required >6.5 hours of oxygen, but had a maximum respiratory rate 49. The S3 group required >6.5 hours of oxygen, had a maximum respiratory rate >49, but were >36.5 week gestation, and consumed >23.5 kcal/kg/day.
Infants predicted as having a long LOS had three distinct profiles labeled L1, L2, and L3 in Figure 1. The L1 group required >6.5 hours of supplemental oxygen, had a maximum respiratory rate >49, and required some level of oxygen support the entire day. The L2 group required >6.5 hours of supplemental oxygen, had a maximum respiratory rate >49, were on room air some portion of the day, but had a gestation 36.5 weeks. The L3 group required >6.5 hours of supplemental oxygen, had a maximum respiratory rate >49, were on room air for some portion of the day, had a gestation >36.5 weeks, but consumed 23.5 kcal/kg/day.
Table 3 compares the performance of our model (the Milwaukee Model), the Michigan Model, and the Rotterdam Model in predicting LOS group. Overall, the Milwaukee Model had the highest ROC 0.89/0.72 for the learning and test trees. All three models had good sensitivity (Milwaukee, 85%; Michigan, 85%), with the Rotterdam Model having the highest (98%). The Milwaukee Model also had good specificity (82%), while the Michigan and Rotterdam Models were less specific (46% and 44%).
| Model | Priors* | Sensitivity | Specificity | Learning Tree ROC | Test Tree ROC | |
|---|---|---|---|---|---|---|
| Long LOS | Short LOS | |||||
| ||||||
| Michigan | 0.5 | 0.5 | 0.85 | 0.46 | 0.69 | 0.56 |
| Rotterdam | 0.5 | 0.5 | 0.98 | 0.44 | 0.73 | 0.61 |
| Milwaukee | 0.5 | 0.5 | 0.85 | 0.82 | 0.89 | 0.72 |
DISCUSSION
We confirmed several previously recognized risk factors for prolonged LOS, including: apnea, at least part of the hospital stay in ICU, use of CPAP, mechanical ventilation, and prematurity. However, most patients admitted with bronchiolitis do not have these risk factors. The major contribution of this study is the evaluation of factors applicable to all patients admitted with bronchiolitis, and a more in‐depth analysis of clinical assessments performed on hospital days 1 and 2 than had been previously reported.
We did find strong associations between a number of clinical assessments and LOS. While some were apparent on day 1 of the admission, the number and degree of clinical differences between infants destined for a short vs prolonged stay were more apparent on hospital day 2. On this day, there were significant differences between the groups in the length and amount of oxygen received, oxygen saturation, maximum respiratory rate, respiratory scores, nasopharyngeal suctioning need, and caloric intake. Interestingly, it was noted the prolonged stay group had overall worsening or a lack of improvement in several clinical markers from day 1 to day 2, in areas where the short stay group showed improvements.
To our knowledge, the Milwaukee Model is the first bronchiolitis LOS prediction model to incorporate several clinical markers occurring early in the hospital stay. These clinical markers were found to be more effective predictors of LOS group in our study population than some of the traditional birth‐ and disease‐related risk factors previously reported. The model highlighted some important interactions among variables, and identified specific profiles of patients likely to have a short or prolonged LOS based on their day 2 clinical status.
The short LOS groups all shared one of the following three features: 1) low duration of oxygen use; 2) absence of tachypnea (tachypnea defined as a respiratory rate >60 in infants <2 months old and >50 for infants between 2 and 12 months old.3234); or 3) absence of severely diminished caloric intake. The prolonged LOS groups shared the common characteristics of higher duration of oxygen use and higher maximum respiratory rates. In addition to these two elements, each long stay group had either a constant oxygen requirement, prematurity (36.5 weeks), or very low caloric intake (<23.5 kcal/kg/day).
While all three models shared good sensitivity, the increased specificity of the Milwaukee Model limits the number of false positives (infants screening as destined for a prolonged LOS who actually will have a short LOS). For clinicians or researchers planning interventions for high‐risk infants, this greater specificity would reduce the number of infants who might unnecessarily receive those interventions. While there are limited proven therapies to hasten the recovery of patients with bronchiolits,35 many treatments and combinations of treatments are currently being used and studied. Nebulized hypertonic saline,36 airway secretion clearance modalities,37 and nutritional supplementation22, 38 are some examples of interventions that could be used and evaluated in infants screened as high risk for prolonged LOS. While it may have been better to identify short vs long stay immediately upon admission or after hospital day 1, it was the more clear separation between the short and long stay groups that occurred on day 2 that allowed us to develop an accurate predictive model. We believe that for infants destined to be in the hospital for at least three more days, a model based on hospital day 2 variables is worthwhile.
When evaluating the characteristics of the three models, it is important to note that they were initially studied in populations with some important differences. Only 11% of Milwaukee patients had chronic respiratory diseases, whereas the previously developed models were generated from a sample with a higher prevalence of chronic respiratory diseases (Michigan, 20%; Rotterdam, 23%). Only 3% of subjects needed placement in the ICU compared to higher rates in prior studies (Michigan, 15%; Rotterdam, 43.5%). In a population of patients with a lower prevalence of chronic respiratory diseases and need for ICU, early clinical markers may become more important in predicting LOS. While our model may generalize well in such a cohort of patients, it might not generalize as well to a cohort with a high prevalence of chronic lung disease and higher need for ICU. It is also important to note that the area under the ROC was lower in the test tree than the learning tree. This variation demonstrates the need for evaluating the performance of this model in additional populations.
This study has several limitations. First, it is a retrospective study of a single bronchiolitis season at a single institution. Second, the authors served as data abstractors and could have been biased, as they were not blinded. Third, four out of the five markers in our model are clinical markers that could vary based on clinical assessment skills and institutional practice. For example, oxygen use is dependent on the practice of nurses and respiratory therapists charged with regulating the oxygen delivery. However, the practice of initiating and weaning oxygen is fairly standardized at our institution. Fourth, environmental and social risk factors, such as day care attendance, school‐age siblings, and smoke exposure, can impact LOS but were not included in our model. Fifth, we do not have data on those infants not included in the bronchiolitis protocol. It is possible that they differed from those in protocol. Finally, six infants were either placed or transferred to the ICU on day 1, which may make them inherently different than the other infants in the model. However, four out of these six infants did go on to have a short stay, highlighting the fact that many other factors affect LOS.
We believe this model may be useful because the clinical markers it uses represent some of the key problems seen in bronchiolitis (poor oxygenation, tachypnea, and poor feeding). Careful assessment of these clinical markers can allow effective prediction of those infants likely to have a prolonged LOS. This early risk assessment could allow more effective targeting of interventions to help high‐risk infants.
CONCLUSIONS
There are important differences between infants with bronchiolitis having short and prolonged hospital stays, including several clinical markers identifiable on hospital day 2, such as the length and amount of oxygen received, minimum oxygen saturation, maximum respiratory rate, clinical respiratory scores, deep suctioning need, and caloric intake. The Milwaukee Model uses the number of hours of supplemental oxygen, respiratory rate, minimum supplemental oxygen use, gestation, and caloric intake to predict short or prolonged LOS. It performed well with a good ROC, sensitivity, and specificity in one population of infants with a low prevalence of chronic respiratory disease.
Prior studies have identified risk factors for increased severity of illness, readmission, or prolonged length of stay (LOS) in infants admitted with bronchiolitis.123 These risk factors include birth‐related factors (prematurity, birth within six months of respiratory syncytial virus [RSV] season, discharge from the neonatal intensive care unit during winter, multiple birth infant), environmental factors (day care attendance, school‐age siblings, smoke exposure), and underlying diseases (chronic lung disease and other pulmonary conditions, failure to thrive (FTT), congenital heart disease, immunologic disorders, and neuromuscular disease).123 Additional risk factors occurring during the bronchiolitis course that have been associated with prolonged hospital course are mechanical ventilation, intensive care unit (ICU) admission, hypoxia on admission, apnea, feeding problems, and duration of supplemental oxygen.2123
Having a reliable model to identify infants at high risk for prolonged LOS early in the course of an admission would be helpful, both for clinical care and for studies of interventions designed to reduce LOS. Prior attempts at developing a model have yielded mixed results. The Michigan Logistic Regression Model displayed excellent predictive ability with an area under the receiver‐operator curve (ROC) of 0.88 using variables including prematurity, FTT, pulmonary disease, other comorbid diseases, and early mechanical ventilation.21 However, when applied to another patient population it did not perform as well. The Rotterdam Model using the variables of weight and supplemental oxygen had an ROC of 0.65.24
Prior prediction models have focused more on birth‐ and disease‐related risk factors than on hospital course factors, particularly common clinical assessments including respiratory status and caloric intake. An additional limitation of prior models is some loss of ability to study the interaction between various predictor variables when using multivariate regression methods.
Our aims were: 1) to study the associations of various clinical markers identifiable during the first two days of the hospital admission with LOS; and 2) to develop a LOS prediction model, using both previously identified risk factors and more detailed clinical data from the first two days of the hospital admission.
MATERIALS AND METHODS
Study Population and Setting
We conducted a retrospective cohort study during a single bronchiolitis season to identify factors predictive of a prolonged length of stay.
Children's Hospital of Wisconsin (CHW) is a 242‐bed tertiary care academic center. The charts of all infants discharged from CHW who met the following criteria were reviewed:
Age <365 days;
Admitted between November 1, 2004 and April 15, 2005;
Bronchiolitis diagnosis using the International Classification of Diseases, 9th edition (ICD‐9) discharge codes 466.11 (RSV bronchiolitis) or 466.19 (bronchiolitis from other organisms);
Placement on the CHW bronchiolitis treatment protocol. Major elements of this protocol include:
respiratory therapists (RT) assessments three times daily providing a standard means of evaluating severity of illness throughout the admission;
pre‐ and post‐intervention assessments.
Infants in this protocol differ from those not on the protocol; their average LOS is one day shorter and their care is more closely aligned with practices established in the Child Health Accountability Initiative (CHAI)25 and the American Academy of Pediatrics Guidelines,26 including: emphasis on clinical diagnosis rather than using laboratory and radiologic testing; avoiding routine bronchodilator use; and decreasing continuous pulse oximetry use. Only patients placed on the bronchiolitis treatment protocol were studied because these infants have a consistent model of care proven to be effective at CHW and other institutions25, 27; 70% of infants admitted to CHW with bronchiolitis were placed on the protocol. Common reasons for not placing infants on the protocol include: 1) the diagnosis of bronchiolitis was initially unclear; 2) the infant had chronic respiratory problems; and 3) physician preference.
Infants with events occurring during the admission not related to bronchiolitis and impacting LOS were excluded. Infants admitted or transferred to the ICU were included if placed on the bronchiolitis protocol; however, few ICU patients were placed on the protocol, as its intent is mainly for the general units.
Data Collected
Five trained abstractors (two were study authors) abstracted the following information from patient records: 1) baseline patient characteristics; 2) initial evaluation: respiratory rate, oxygen saturation, supplemental oxygen use, presence of increased work of breathing, weight, height, Waterlow percentile (percent of ideal body weight);28 3) fluid and nutritional information on hospital days 15; 4) respiratory assessments and treatments on hospital days 15 (clinical respiratory scores, respiratory rates, oxygen saturation, use of supplemental oxygen, medications received; 5) laboratory and imaging results; and 6) diagnoses. Each hospital day was defined as 0600 to 0559 the following day.
Clinical Respiratory Scores
The Children's Hospital of Wisconsin Respiratory Score (CHWRS) is a marker of overall respiratory status (not yet validated.) It contains six variables scored 03 based on degree: breath sounds, dyspnea, retractions, respiratory rate, heart rate, and supplemental oxygen. Scores range from 0 to 18, with lower scores representing less respiratory distress.
Outcomes and Analysis
The primary outcome was LOS, defined as the number of hours from the time a subject arrived on the hospital unit to time of last nursing documentation at time of discharge. The average LOS at CHW of 2.5 days is comparable to the lower end of that reported in the literature (2.85 days21, 22, 29, 30). LOS was dichotomized as short or prolonged, with prolonged LOS defined as 108 hours. We chose this length as it represents the 80th percentile LOS at our institution. Most physicians caring for infants with bronchiolitis at CHW use discharge criteria aligned with those in the hospitalist group's bronchiolitis clinical practice guideline,31 the SOFFFAR criteria: Sno longer dependent on nasopharyngeal suctioning; Ooff oxygen, or to baseline oxygen requirement; Ffamily agreeable to discharge; F follow‐up plan in place; FFeeding well enough to maintain hydration; Aif albuterol responsive, requiring treatments no more frequently than every six hours, Rrespiratory status acceptable (not too tachypneic or in respiratory distress).
Univariate Analysis
We examined the association between selected variables and LOS group (short or prolonged). Three groups of variables were studied: 1) variables identifiable upon admission (Table 1); 2) variables identifiable on hospital days 1 and 2 (Table 2); and 3) variables identifiable later in the admission. The variables evaluated were all non‐normally distributed and, therefore, the MannWhitney test was used to examine differences between groups with continuous or categorical variables. Dichotomous variables were compared using chi‐square or Fisher's exact test. SPSS (Chicago, IL) was used for these analyses. Because of multiple comparisons, 90% power and an alpha of 0.01 were used.
| Variable | Median (IQR), N [% of subjects] | P Value | |
|---|---|---|---|
| Short (N = 225) | Long (N = 47) | ||
| |||
| Age (days) | 134 (63‐225.5) | 139 (63‐240) | 0.86 |
| Gestation (weeks) | 40 (37‐40) | 39 (35‐40) | 0.07 |
| Race | |||
| White | 108 [48] | 23 [49] | 0.91 |
| Other | 117 [52] | 24 [51] | |
| Gender | |||
| Male | 121 [54] | 25 [53] | 0.94 |
| Respiratory support at birth | 22 [10] | 12 [26] | 0.003* |
| Chronic respiratory disease | 21 [9] | 8 [17] | 0.12 |
| Respiratory rate on admission | 56 (44‐64) | 56 (46‐66) | 0.58 |
| Cardiac conditions | 4 [2] | 3 [6] | 0.10 |
| Waterlow percent | 100 (92‐109) {n =203} | 96 (88‐107) {n =46} | 0.16 |
| Days of cough prior to admission | 4 (2‐6) {n =202} | 4 (2‐5) {n = 40} | 0.78 |
| Days of congestion prior to admission | 3 (1‐5) {n =183} | 3 (1‐5) {n =35} | 0.98 |
| Days of fever prior to admission | 1 (0‐3) {n =206} | 1 (0‐2) {n =43} | 0.50 |
| Days of decreased oral intake prior to admission | 1 (0‐2) {n =181} | 1 (0‐1) {n =36} | 0.44 |
| Variable | Median (IQR) or N [%] | P | Median (IQR) or N [%] | P | ||
|---|---|---|---|---|---|---|
| Short | Long | Short | Long | |||
| Hospital Day 1 | Hospital Day 2 | |||||
| ||||||
| Hours of supplemental oxygen | 3 (0‐10) | 11 (5‐17) | <0.001* | 3 (0‐19) | 24 (17‐24) | <0.001* |
| Minimum supplemental oxygen use (liters) | 0 (0‐0.1) | 0.25 (0‐0.5) | <0.001* | 0 (0‐0) | 0.2 (0‐0.5) | <0.001* |
| Maximum supplemental oxygen use (liters) | 0.5 (0‐1) | 0.75 (0.5‐1.5) | <0.001* | 0.2 (0‐0.5) | 1 (0.5‐1.5) | <0.001* |
| Minimum oxygen saturation (percent) | 94 (92‐96) | 94 (92‐96) | 0.89 | 94 (92‐95) | 93 (91‐94) | 0.001* |
| Maximum oxygen saturation (percent) | 99 (98‐100) | 100 (99‐100) | 0.23 | 100 (98‐100) | 100 (99‐100) | 0.37 |
| Minimum respiratory rate | 36 (32‐46) | 36 (32‐46) | 0.92 | 34 (30‐40) | 36 (32‐41) | 0.11 |
| Maximum respiratory rate | 53 (45‐62) | 56 (48‐64) | 0.14 | 55 (48‐64) | 63 (52‐75) | <0.001* |
| Mean respiratory score | 4 (3‐5.5) | 5 (4‐6.7) | 0.008* | 3.4 (2.7‐4.5) | 4.8 (3.7‐7) | <0.001* |
| Change in respiratory score | 0 (0‐1) | 0 (1‐1.5) | 0.3 | 1 (0‐2) | 0 (‐2‐2) | 0.022 |
| Number of times nasopharyngeal suctioned | 1 (0‐2) | 2 (1‐3) | 0.012 | 1 (0‐3) | 4 (2‐5) | <0.001* |
| Calories consumed (Kcal/kg/day) | 53 (22‐82) | 54 (33‐79) | 0.801 | 66 (47‐90) | 54 (21‐72) | 0.001* |
| ICU (% of subjects) | 4 (1.8%) | 2 (4.3%) | 0.28 | 4 (1.8%) | 5 (10.6%) | 0.009* |
Recursive Partitioning Analysis
We chose recursive partitioning as the method for model creation instead of multivariate linear regression in order to: 1) study multiple possible variable interactions without having to create multiple interaction terms; and 2) generate an easy‐to‐use flow diagram to identify infants at risk for prolonged LOS without having to use a complex formula generated by multivariate regression. In recursive partitioning methodology, the statistical program selects the variable among the set of candidate variables that best separates the first parent node with all subjects into short and prolonged stay intermediate nodes. The process is repeated with additional variables selected that further separate the intermediate nodes into short and prolonged stay nodes, until finally a flow diagram is generated, resulting in terminal nodes of predicted short and prolonged stay subjects. Recursive partitioning was performed using Salford Systems' CART software San Diego, CA. The minimum number of cases required in parent/emntermediate nodes was 20, and in terminal nodes was 5. Eighty percent of cases were randomly selected for the learning tree, and 20% in the test tree for cross‐validation.
Sixteen variables were considered a priori as potentially important in affecting LOS and were candidates for inclusion. These included five baseline variables (age, gestation, Waterlow percentile, presence of chronic respiratory disease, and a marker for missing Waterlow percentile) and 11 variables from hospital day 2 (kcal/kg/day consumed, hours of supplemental oxygen, maximum supplemental oxygen use, maximum oxygen saturation, maximum respiratory rate, minimum supplemental oxygen use, minimum oxygen saturation, minimum respiratory rate, mean clinical respiratory score, change in respiratory score, and nasopharyngeal suctioning frequency). Hospital day 2 variables were chosen rather than hospital day 1, because hospital day 1 was only a partial day in the hospital for the majority of subjects. Several aspects of oxygenation were studied because oxygen need has been consistently found to be an important predictor of LOS. We sought to discover which particular aspect of oxygen need was most important. For comparison, recursive partitioning was performed on the variable sets taken from the Michigan (weight, congenital heart disease, failure to thrive, gestational age, chronic pulmonary diseases, and early mechanical ventilation)21 and Rotterdam (weight and need for supplemental oxygen)24 Models.
This study was approved by the CHW Institutional Review Board.
RESULTS
Three hundred forty‐seven infants were admitted during the 20042005 bronchiolitis season, with 273 placed in the bronchiolitis treatment protocol. The charts of these 273 patients were reviewed. One was excluded because of gastrostomy tube placement during the admission. Of the remaining 272 patients, 47 (17.3%) had a LOS 108 hours. The median LOS was 59 hours (range 10334 hours). Two patients had missing data for caloric intake on days 1 and 2; and 23 patients did not have height obtained, therefore their Waterlow classification could not be determined. Historical details concerning fever, congestion, cough, and diminished caloric intake preceding admission were variably reported, resulting in a smaller sample size for these baseline characteristics as described in Table 1.
Univariate Analysis
Baseline characteristics of infants having short and prolonged LOS are described in Table 1. Groups were statistically similar except that the long stay group contained a significantly larger proportion of infants requiring respiratory support at birth (defined as needing intubation, continuous positive airway pressure [CPAP], or oxygen).
Table 2 describes selected variables on hospital days 1 and 2 in infants having short and prolonged LOS. On hospital day 1, infants in the prolonged LOS group had a significantly greater need for supplemental oxygen, and mean respiratory score. On hospital day 2, infants in the prolonged LOS group had a significantly greater need for supplemental oxygen maximum respiratory rate, mean respiratory score, and number of times they were suctioned. They had a significantly lower minimum oxygen saturation and caloric intake. On hospital day 2, the prolonged LOS group had a greater proportion of subjects in the ICU, on CPAP, and on the ventilator.
We examined two characteristics identifiable after the second hospital day. There was a significant difference in: a) the median number of discharge diagnoses in the short LOS group (two) vs the prolonged LOS group (three) (P < 0.001); and b) the presence of apnea during the admission in the short LOS group (0.1%) vs the prolonged LOS group (9%) (P = 0.009).
Recursive Partitioning Model
Figure 1 depicts the recursive partitioning model that best predicted LOS. Five variables were selected by the recursive partitioning model. Selected variables, in order of appearance (variable importance is related to order of appearance, ie, most important variable is first), were: hours of supplemental oxygen, maximum respiratory rate, minimum supplemental oxygen use, gestation, and kilocalories (kcal)/kilogram (kg)/day consumed. The characteristics of this model were: ROC 0.89 and 0.72 for the learning and test trees, respectively; sensitivity, 0.85; and specificity, 0.82
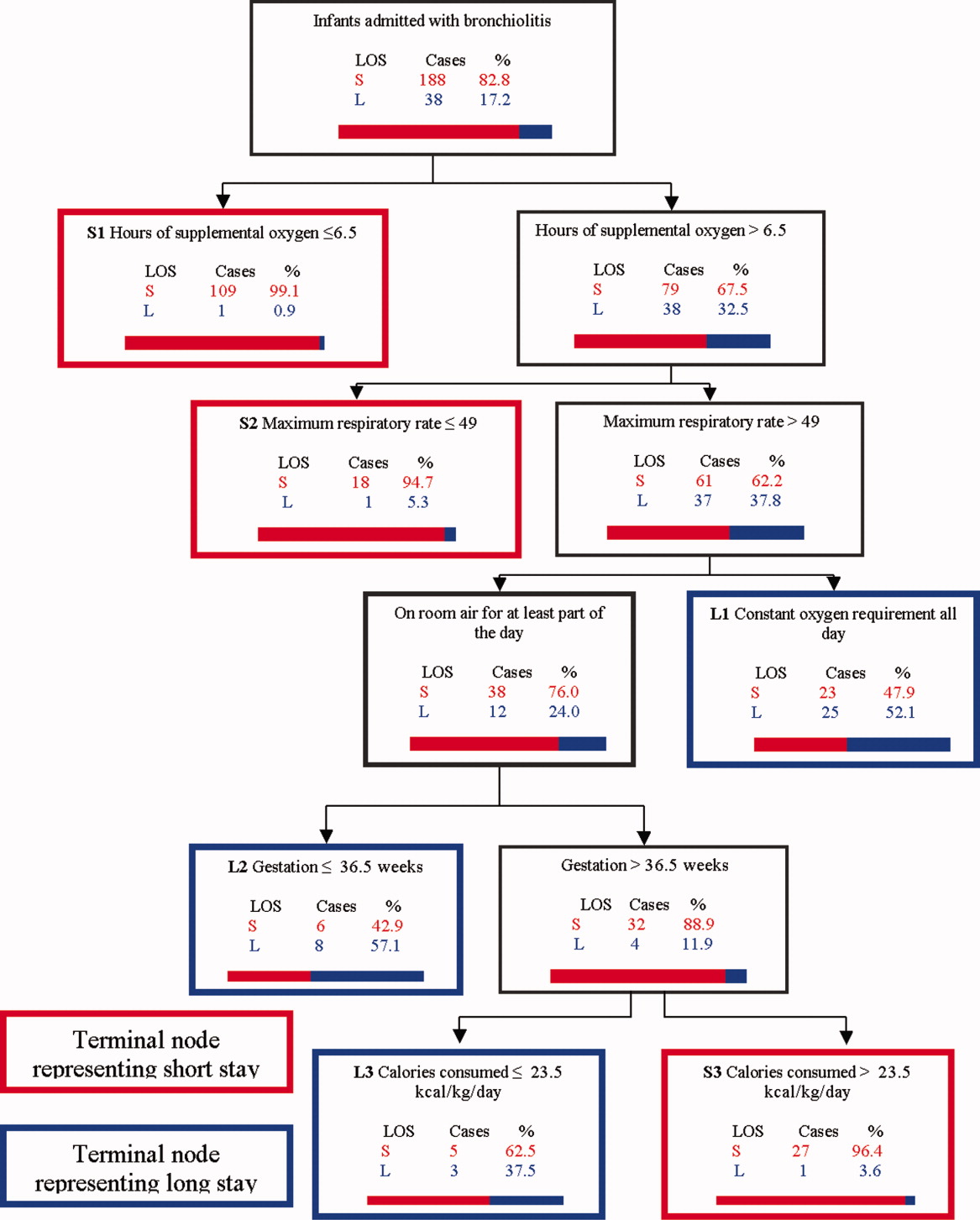
Infants predicted as having a short LOS had three distinct profiles labeled S1, S2, and S3 in Figure 1. The S1 group required 6.5 hours of oxygen. The S2 group required >6.5 hours of oxygen, but had a maximum respiratory rate 49. The S3 group required >6.5 hours of oxygen, had a maximum respiratory rate >49, but were >36.5 week gestation, and consumed >23.5 kcal/kg/day.
Infants predicted as having a long LOS had three distinct profiles labeled L1, L2, and L3 in Figure 1. The L1 group required >6.5 hours of supplemental oxygen, had a maximum respiratory rate >49, and required some level of oxygen support the entire day. The L2 group required >6.5 hours of supplemental oxygen, had a maximum respiratory rate >49, were on room air some portion of the day, but had a gestation 36.5 weeks. The L3 group required >6.5 hours of supplemental oxygen, had a maximum respiratory rate >49, were on room air for some portion of the day, had a gestation >36.5 weeks, but consumed 23.5 kcal/kg/day.
Table 3 compares the performance of our model (the Milwaukee Model), the Michigan Model, and the Rotterdam Model in predicting LOS group. Overall, the Milwaukee Model had the highest ROC 0.89/0.72 for the learning and test trees. All three models had good sensitivity (Milwaukee, 85%; Michigan, 85%), with the Rotterdam Model having the highest (98%). The Milwaukee Model also had good specificity (82%), while the Michigan and Rotterdam Models were less specific (46% and 44%).
| Model | Priors* | Sensitivity | Specificity | Learning Tree ROC | Test Tree ROC | |
|---|---|---|---|---|---|---|
| Long LOS | Short LOS | |||||
| ||||||
| Michigan | 0.5 | 0.5 | 0.85 | 0.46 | 0.69 | 0.56 |
| Rotterdam | 0.5 | 0.5 | 0.98 | 0.44 | 0.73 | 0.61 |
| Milwaukee | 0.5 | 0.5 | 0.85 | 0.82 | 0.89 | 0.72 |
DISCUSSION
We confirmed several previously recognized risk factors for prolonged LOS, including: apnea, at least part of the hospital stay in ICU, use of CPAP, mechanical ventilation, and prematurity. However, most patients admitted with bronchiolitis do not have these risk factors. The major contribution of this study is the evaluation of factors applicable to all patients admitted with bronchiolitis, and a more in‐depth analysis of clinical assessments performed on hospital days 1 and 2 than had been previously reported.
We did find strong associations between a number of clinical assessments and LOS. While some were apparent on day 1 of the admission, the number and degree of clinical differences between infants destined for a short vs prolonged stay were more apparent on hospital day 2. On this day, there were significant differences between the groups in the length and amount of oxygen received, oxygen saturation, maximum respiratory rate, respiratory scores, nasopharyngeal suctioning need, and caloric intake. Interestingly, it was noted the prolonged stay group had overall worsening or a lack of improvement in several clinical markers from day 1 to day 2, in areas where the short stay group showed improvements.
To our knowledge, the Milwaukee Model is the first bronchiolitis LOS prediction model to incorporate several clinical markers occurring early in the hospital stay. These clinical markers were found to be more effective predictors of LOS group in our study population than some of the traditional birth‐ and disease‐related risk factors previously reported. The model highlighted some important interactions among variables, and identified specific profiles of patients likely to have a short or prolonged LOS based on their day 2 clinical status.
The short LOS groups all shared one of the following three features: 1) low duration of oxygen use; 2) absence of tachypnea (tachypnea defined as a respiratory rate >60 in infants <2 months old and >50 for infants between 2 and 12 months old.3234); or 3) absence of severely diminished caloric intake. The prolonged LOS groups shared the common characteristics of higher duration of oxygen use and higher maximum respiratory rates. In addition to these two elements, each long stay group had either a constant oxygen requirement, prematurity (36.5 weeks), or very low caloric intake (<23.5 kcal/kg/day).
While all three models shared good sensitivity, the increased specificity of the Milwaukee Model limits the number of false positives (infants screening as destined for a prolonged LOS who actually will have a short LOS). For clinicians or researchers planning interventions for high‐risk infants, this greater specificity would reduce the number of infants who might unnecessarily receive those interventions. While there are limited proven therapies to hasten the recovery of patients with bronchiolits,35 many treatments and combinations of treatments are currently being used and studied. Nebulized hypertonic saline,36 airway secretion clearance modalities,37 and nutritional supplementation22, 38 are some examples of interventions that could be used and evaluated in infants screened as high risk for prolonged LOS. While it may have been better to identify short vs long stay immediately upon admission or after hospital day 1, it was the more clear separation between the short and long stay groups that occurred on day 2 that allowed us to develop an accurate predictive model. We believe that for infants destined to be in the hospital for at least three more days, a model based on hospital day 2 variables is worthwhile.
When evaluating the characteristics of the three models, it is important to note that they were initially studied in populations with some important differences. Only 11% of Milwaukee patients had chronic respiratory diseases, whereas the previously developed models were generated from a sample with a higher prevalence of chronic respiratory diseases (Michigan, 20%; Rotterdam, 23%). Only 3% of subjects needed placement in the ICU compared to higher rates in prior studies (Michigan, 15%; Rotterdam, 43.5%). In a population of patients with a lower prevalence of chronic respiratory diseases and need for ICU, early clinical markers may become more important in predicting LOS. While our model may generalize well in such a cohort of patients, it might not generalize as well to a cohort with a high prevalence of chronic lung disease and higher need for ICU. It is also important to note that the area under the ROC was lower in the test tree than the learning tree. This variation demonstrates the need for evaluating the performance of this model in additional populations.
This study has several limitations. First, it is a retrospective study of a single bronchiolitis season at a single institution. Second, the authors served as data abstractors and could have been biased, as they were not blinded. Third, four out of the five markers in our model are clinical markers that could vary based on clinical assessment skills and institutional practice. For example, oxygen use is dependent on the practice of nurses and respiratory therapists charged with regulating the oxygen delivery. However, the practice of initiating and weaning oxygen is fairly standardized at our institution. Fourth, environmental and social risk factors, such as day care attendance, school‐age siblings, and smoke exposure, can impact LOS but were not included in our model. Fifth, we do not have data on those infants not included in the bronchiolitis protocol. It is possible that they differed from those in protocol. Finally, six infants were either placed or transferred to the ICU on day 1, which may make them inherently different than the other infants in the model. However, four out of these six infants did go on to have a short stay, highlighting the fact that many other factors affect LOS.
We believe this model may be useful because the clinical markers it uses represent some of the key problems seen in bronchiolitis (poor oxygenation, tachypnea, and poor feeding). Careful assessment of these clinical markers can allow effective prediction of those infants likely to have a prolonged LOS. This early risk assessment could allow more effective targeting of interventions to help high‐risk infants.
CONCLUSIONS
There are important differences between infants with bronchiolitis having short and prolonged hospital stays, including several clinical markers identifiable on hospital day 2, such as the length and amount of oxygen received, minimum oxygen saturation, maximum respiratory rate, clinical respiratory scores, deep suctioning need, and caloric intake. The Milwaukee Model uses the number of hours of supplemental oxygen, respiratory rate, minimum supplemental oxygen use, gestation, and caloric intake to predict short or prolonged LOS. It performed well with a good ROC, sensitivity, and specificity in one population of infants with a low prevalence of chronic respiratory disease.
- ,.Clinical significance of respiratory syncytial virus.Postgrad Med.1964;35:460–465.
- ,,,,.Respiratory syncytial virus infection in young hospitalized children. Identification of risk patients and prevention of nosocomial spread by rapid diagnosis.Acta Paediatr Scand.1983;72(1):47–51.
- .Pathogenesis of bronchiolitis—epidemiologic considerations.Pediatr Res.1977;11(3 pt 2):239–243.
- ,,.Respiratory syncytial virus infection in children with bronchopulmonary dysplasia.Pediatrics.1988;82(2):199–203.
- ,,, et al.Respiratory syncytial viral infection in children with compromised immune function.N Engl J Med.1986;315(2):77–81.
- ,,,,.Risk of secondary bacterial infection in infants hospitalized with respiratory syncytial viral infection.J Pediatr.1988;113(2):266–271.
- ,,,,,.Respiratory syncytial viral infection in infants with congenital heart disease.N Engl J Med.1982;307(7):397–400.
- ,,, et al.Hospitalized children with respiratory syncytial virus infection and neuromuscular impairment face an increased risk of a complicated course.Pediatr Infect Dis J.2007;26(6):485–491.
- ,,.Rehospitalization for respiratory illness in infants of less than 32 weeks' gestation.Pediatrics.1991;88(3):527–532.
- ,,, et al.Respiratory syncytial virus (RSV) immune globulin intravenous therapy for RSV lower respiratory tract infection in infants and young children at high risk for severe RSV infections: Respiratory Syncytial Virus Immune Globulin Study Group.Pediatrics.1997;99(3):454–461.
- ,,,,.Risk factors for bronchiolitis‐associated deaths among infants in the United States.Pediatr Infect Dis J.2003;22(6):483–490.
- ,.Risk factors for severe respiratory syncytial virus infection in infants.Respir Med.2002;96(suppl B):S9–S14.
- ,,,,.Rehospitalization for respiratory syncytial virus among premature infants.Pediatrics.1999;104(4 pt 1):894–899.
- ,,,,.Risk of respiratory syncytial virus infection for infants from low‐income families in relationship to age, sex, ethnic group, and maternal antibody level.J Pediatr.1981;98(5):708–715.
- ,,,.Preterm twins and triplets. A high‐risk group for severe respiratory syncytial virus infection.Am J Dis Child.1993;147(3):303–306.
- ,,, et al.Rehospitalization because of respiratory syncytial virus infection in premature infants younger than 33 weeks of gestation: a prospective study. IRIS Study Group.Pediatr Infect Dis J.2000;19(7):592–597.
- ,.Parental smoking, presence of older siblings, and family history of asthma increase risk of bronchiolitis.Am J Dis Child.1986;140(8):806–812.
- ,,,,.Role of respiratory syncytial virus in early hospitalizations for respiratory distress of young infants with cystic fibrosis.J Pediatr.1988;113(5):826–830.
- ,,, et al.Variable morbidity of respiratory syncytial virus infection in patients with underlying lung disease: a review of the PICNIC RSV database. Pediatric Investigators Collaborative Network on Infections in Canada.Pediatr Infect Dis J.1999;18(10):866–869.
- ,,,,.Rates of hospitalization for respiratory syncytial virus infection among children in Medicaid.J Pediatr.2000;137(6):865–870.
- ,.Severity of illness models for respiratory syncytial virus‐associated hospitalization.Am J Respir Crit Care Med.1999;159(4 pt 1):1234–1240.
- ,.Effect of oxygen supplementation on length of stay for infants hospitalized with acute viral bronchiolitis.Pediatrics.2008;121(3):470–475.
- ,,.Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) prospective study of risk factors and outcomes in patients hospitalized with respiratory syncytial viral lower respiratory tract infection.J Pediatr.1995;126(2):212–219.
- ,,,.Prediction of duration of hospitalization in respiratory syncytial virus infection.Pediatr Pulmonol.2002;33(6):453–457.
- ,,,,,.Impact of a bronchiolitis guideline: a multisite demonstration project.Chest.2002;121(6):1789–1797.
- , , , , , , , , , Diagnosis and management of bronchiolitis.Pediatrics.2006;118(4):1774–1793.
- ,,, et al.Evaluation of an evidence‐based guideline for bronchiolitis.Pediatrics.1999;104(6):1334–1341.
- .Classification and definition of protein‐calorie malnutrition.Br Med J.1972;3(5826):566–569.
- ,,,,.Inpatient care for uncomplicated bronchiolitis: comparison with Milliman and Robertson guidelines.Arch Pediatr Adolesc Med.2001;155(12):1323–1327.
- ,,,.Impact of pulse oximetry and oxygen therapy on length of stay in bronchiolitis hospitalizations.Arch Pediatr Adolesc Med.2004;158(6):527–530.
- .Bronchiolitis clinical practice guideline.Children's Hospital of Wisconsin Intranet;2007. http://clinicalpractice.chw.org/display/displayFile.asp?docid=393185(2):319–336.
- ,.The rational clinical examination. Does this infant have pneumonia?JAMA.1998;279(4):308–313.
- ,.Focused ethnographic studies in the WHO Programme for the Control of Acute Respiratory Infections.Med Anthropol.1994;15(4):409–424.
- ,.Bronchiolitis: recent evidence on diagnosis and management.Pediatrics.125(2):342–349.
- ,,,.Nebulized hypertonic saline solution for acute bronchiolitis in infants.Cochrane Database Syst Rev.2008(4):CD006458.
- .Airway clearance applications in infants and children.Respir Care.2007;52(10):1382–1391.
- ,.Immunonutrition in critically ill patients: a systematic review and analysis of the literature.Intensive Care Med.2008;34(11):1980–1990.
- ,.Clinical significance of respiratory syncytial virus.Postgrad Med.1964;35:460–465.
- ,,,,.Respiratory syncytial virus infection in young hospitalized children. Identification of risk patients and prevention of nosocomial spread by rapid diagnosis.Acta Paediatr Scand.1983;72(1):47–51.
- .Pathogenesis of bronchiolitis—epidemiologic considerations.Pediatr Res.1977;11(3 pt 2):239–243.
- ,,.Respiratory syncytial virus infection in children with bronchopulmonary dysplasia.Pediatrics.1988;82(2):199–203.
- ,,, et al.Respiratory syncytial viral infection in children with compromised immune function.N Engl J Med.1986;315(2):77–81.
- ,,,,.Risk of secondary bacterial infection in infants hospitalized with respiratory syncytial viral infection.J Pediatr.1988;113(2):266–271.
- ,,,,,.Respiratory syncytial viral infection in infants with congenital heart disease.N Engl J Med.1982;307(7):397–400.
- ,,, et al.Hospitalized children with respiratory syncytial virus infection and neuromuscular impairment face an increased risk of a complicated course.Pediatr Infect Dis J.2007;26(6):485–491.
- ,,.Rehospitalization for respiratory illness in infants of less than 32 weeks' gestation.Pediatrics.1991;88(3):527–532.
- ,,, et al.Respiratory syncytial virus (RSV) immune globulin intravenous therapy for RSV lower respiratory tract infection in infants and young children at high risk for severe RSV infections: Respiratory Syncytial Virus Immune Globulin Study Group.Pediatrics.1997;99(3):454–461.
- ,,,,.Risk factors for bronchiolitis‐associated deaths among infants in the United States.Pediatr Infect Dis J.2003;22(6):483–490.
- ,.Risk factors for severe respiratory syncytial virus infection in infants.Respir Med.2002;96(suppl B):S9–S14.
- ,,,,.Rehospitalization for respiratory syncytial virus among premature infants.Pediatrics.1999;104(4 pt 1):894–899.
- ,,,,.Risk of respiratory syncytial virus infection for infants from low‐income families in relationship to age, sex, ethnic group, and maternal antibody level.J Pediatr.1981;98(5):708–715.
- ,,,.Preterm twins and triplets. A high‐risk group for severe respiratory syncytial virus infection.Am J Dis Child.1993;147(3):303–306.
- ,,, et al.Rehospitalization because of respiratory syncytial virus infection in premature infants younger than 33 weeks of gestation: a prospective study. IRIS Study Group.Pediatr Infect Dis J.2000;19(7):592–597.
- ,.Parental smoking, presence of older siblings, and family history of asthma increase risk of bronchiolitis.Am J Dis Child.1986;140(8):806–812.
- ,,,,.Role of respiratory syncytial virus in early hospitalizations for respiratory distress of young infants with cystic fibrosis.J Pediatr.1988;113(5):826–830.
- ,,, et al.Variable morbidity of respiratory syncytial virus infection in patients with underlying lung disease: a review of the PICNIC RSV database. Pediatric Investigators Collaborative Network on Infections in Canada.Pediatr Infect Dis J.1999;18(10):866–869.
- ,,,,.Rates of hospitalization for respiratory syncytial virus infection among children in Medicaid.J Pediatr.2000;137(6):865–870.
- ,.Severity of illness models for respiratory syncytial virus‐associated hospitalization.Am J Respir Crit Care Med.1999;159(4 pt 1):1234–1240.
- ,.Effect of oxygen supplementation on length of stay for infants hospitalized with acute viral bronchiolitis.Pediatrics.2008;121(3):470–475.
- ,,.Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) prospective study of risk factors and outcomes in patients hospitalized with respiratory syncytial viral lower respiratory tract infection.J Pediatr.1995;126(2):212–219.
- ,,,.Prediction of duration of hospitalization in respiratory syncytial virus infection.Pediatr Pulmonol.2002;33(6):453–457.
- ,,,,,.Impact of a bronchiolitis guideline: a multisite demonstration project.Chest.2002;121(6):1789–1797.
- , , , , , , , , , Diagnosis and management of bronchiolitis.Pediatrics.2006;118(4):1774–1793.
- ,,, et al.Evaluation of an evidence‐based guideline for bronchiolitis.Pediatrics.1999;104(6):1334–1341.
- .Classification and definition of protein‐calorie malnutrition.Br Med J.1972;3(5826):566–569.
- ,,,,.Inpatient care for uncomplicated bronchiolitis: comparison with Milliman and Robertson guidelines.Arch Pediatr Adolesc Med.2001;155(12):1323–1327.
- ,,,.Impact of pulse oximetry and oxygen therapy on length of stay in bronchiolitis hospitalizations.Arch Pediatr Adolesc Med.2004;158(6):527–530.
- .Bronchiolitis clinical practice guideline.Children's Hospital of Wisconsin Intranet;2007. http://clinicalpractice.chw.org/display/displayFile.asp?docid=393185(2):319–336.
- ,.The rational clinical examination. Does this infant have pneumonia?JAMA.1998;279(4):308–313.
- ,.Focused ethnographic studies in the WHO Programme for the Control of Acute Respiratory Infections.Med Anthropol.1994;15(4):409–424.
- ,.Bronchiolitis: recent evidence on diagnosis and management.Pediatrics.125(2):342–349.
- ,,,.Nebulized hypertonic saline solution for acute bronchiolitis in infants.Cochrane Database Syst Rev.2008(4):CD006458.
- .Airway clearance applications in infants and children.Respir Care.2007;52(10):1382–1391.
- ,.Immunonutrition in critically ill patients: a systematic review and analysis of the literature.Intensive Care Med.2008;34(11):1980–1990.
Copyright © 2011 Society of Hospital Medicine