User login
Pilot Inpatient Pain Pharmacist Consult Service at the West Palm Beach VA Medical Center
The term pain refers to unpleasant sensory, emotional experiences associated with actual or potential tissue damage and is described in terms of such damage.1 Acute pain from neurophysiologic responses to noxious stimuli resolves upon tissue healing or stimuli removal (eg, 3-6 months); however, chronic pain lingers beyond the expected time course of the acute injury and repair process.1,2 Despite pain management advances, the under- or overtreatment of pain for different patient populations (eg, cancer and noncancer) remains an important concern.3,4
Hospitals have focused on optimizing inpatient pain management, because uncontrolled pain remains the most common reason for readmissions the first week postsurgery.5 The safe use of opioids (prescription, illicit synthetic, or heroin) poses major challenges and raises significant concerns. Rates of opioid-related hospital admissions have increased by 42% since 2009, and total overdose deaths reached a new high of 47,055 in 2014, including 28,647 (61%) from opioids.6
Opioids rank among the medications most often associated with serious adverse events (AEs), including respiratory depression and death.7 In response, the Joint Commission recommends patient assessments for opioid-related AEs, technology to monitor opioid prescribing, pharmacist consultation for opioid conversions and route of administration changes, provider education about risks of opioids, and risk screening tools for opioid-related oversedation and respiratory depression.7 Treatment guidelines strive to minimize the impact of acute pain by offering a scientific basis for practice, but evidence suggests a lack of suitable pain programs.7 Increases in opioid prescribing along with clinical guidelines and state laws recommending specialty pain service referrals for patients on high-dose opioids, have increased demand for competent pain clinicians.8
The expertise of a clinical pharmacy specialists (CPS) can help refine ineffective and potentially harmful pain medication therapy in complex patient cases. Existing literature outlines the various benefits of pharmacist participation in collaborative pain services for cancer and noncancer pain, as well as cases involving substance abuse.9-13 Various articles support pharmacists’ role as an educator and team member who can add valuable, trustworthy clinical knowledge that enhances clinical encounters and guides protocol/policy development.12,13 These efforts have improved patient satisfaction and encouraged physicians and nurses to proactively seek pharmacists’ advice for difficult cases.9
Frequent communication with interdisciplinary teams have helped considerably in establishing clinical pharmacy services that benefit patient care and offer sources of professional accomplishment.10,11 For example, pharmacists at Kaweah Delta Medical Center in Visalia, CA launched an innovative pain program that encompassed consultations and opioid stewardship, which demonstrated that pharmacists can improve patient outcomes in the front lines of pain management.14 Pain CPSs have advanced knowledge of pharmacokinetics, pharmacodynamics, and therapeutics to promote safe and effective analgesic use, as well as to identify opioid use disorders. Evidence suggests that pharmacists’ presence on interdisciplinary pain teams improves outcomes by optimizing medication selection, improving adherence, and preventing AEs.8
Following the plan-do-study-act model for quality improvement (QI), this project hoped to expand current pain programs at the West Palm Beach VAMC (WPBVAMC) by evaluating the feasibility of an inpatient pain pharmacist consult service (IPPCS) at the 301-bed teaching facility, which includes 130 acute/intensive care and 120 nursing/domiciliary beds.15 Staff provide primary- and secondary-level care to veterans in 7 counties along Florida’s southeastern coast.
In 2009, the WPBVAMC PGY-2 Pain Management and Palliative Care Program became the VA’s first accredited pain pharmacy residency. Residents train with the Physical Medicine & Rehabilitation (PMR) and Chronic Pain Management departments, which provide outpatient services from 7 pain physicians, a pain psychologist, registered nurse, chiropractor, acupuncturist, physical/occupational therapy (PT/OT), and 3 pain/palliative care CPSs.
The WPBVAMC had established interdisciplinary outpatient chronic pain clinic (OCPC) physician- and pharmacist-run services along with a pain CPS electronic consult (e-consult) program. However, no formal mechanisms for inpatient pain consultations existed. Prior to the IPPCS outlined in this study, OCPC practitioners, including 2 pain CPSs, managed impromptu inpatient pain issues as “curbside consultations” along with usual day-to-day clinic duties.
The OCPC, PMR, and Clinical Pharmacy administration recognized the need for more clinical support to manage complex analgesic issues in inpatient veterans, as these patients often have acute pain with underlying chronic pain syndromes. In a national survey, veterans were significantly more likely than were nonveterans to report painful health conditions (65.5% vs 56.4%) and to classify their pain as severe (9.1% vs 6.3%).16 The WPBVAMC administration concluded that an IPPCS would offer a more efficient means of handling such cases. The IPPCS would formally streamline inpatient pain consults, enabling CPSs to thoroughly evaluate pain-related issues to propose evidence-based recommendations.
The primary objective of this QI project was to assess the IPPCS implementation as part of multimodal care to satisfy unmet patient care needs at the WPBVAMC. Secondary objectives for program feasibility included identifying the volume and type of pain consults, categorizing pharmacist interventions, classifying providers’ satisfaction, and determining types of responses to pharmacists’ medication recommendations.
Methods
This QI project ascertained the feasibility of the IPPCS by evaluating all consults obtained during the pilot period from November 2, 2015 through May 6, 2016. The IPPCS was accessible Monday through Friday during normal business hours. Goal turnaround time for consult completion was 24 to 72 hours, given the lack of coverage on holidays and weekends. The target population included veterans hospitalized at the WPBVAMC inpatient ward or nursing home with uncontrolled pain on IV and/or oral analgesic medications. All IPPCS consults submitted during the pilot period were included in the sample.
The WPBVAMC Scientific Advisory Committee (SAC) approved this QI program prior to initiation. Following supervisory support from the OCPC, PMR, and Clinical Pharmacy departments, hospital technologists assisted in creating a consult link in the Computerized Patient Record System (CPRS), which allowed providers to submit IPPCS requests for specific patients efficiently. Consults were categorized as postoperative pain, acute or chronic pain, malignant pain, or end-of-life pain. Inpatient providers could enter requests for assistance with 1 or more of the following: opioid dose conversions, opioid taper/titration schedules, general opioid treatment recommendations, or nonopioid/adjuvant recommendations.
The Medical Records Committee approved a customized CPRS subjective-objective-assessment-recommendations (SOAR) note template, which helped standardize the pain CPS documentation. To promote consult requests and interdisciplinary collaboration, inpatient clinicians received education about the IPPCS at respective meetings (eg, General Medicine staff and Clinical Pharmacy meetings).
All CPSs involved in this project were residency-trained in direct patient care, including pain and palliative care, and maintained national board certification as pharmacotherapy specialists. Their role included reviewing patients’ electronic medical records, conducting face-to-face pain assessments, completing opioid risk assessments, evaluating analgesic regimen appropriateness, reviewing medication adherence, completing pain medication reconciliation, querying the Florida Prescription Drug Monitoring Program (PDMP), interpreting urine drug testing (UDT), and delivering provider/patient/caregiver education. Parameters used to determine the appropriateness of analgesic regimens included, but were not limited to:
- Use of oral instead of IV medications if oral dosing was feasible/possible/appropriate;
- Dose and adjustments per renal/hepatic function;
- Adequate treatment duration and titration;
- No therapeutic drug class duplications;
- Medication tolerability (eg, allergies, AEs, drug interactions); and
- Opioid risk assessment per Opioid Risk Tool (ORT) score and medical history.
Consulting providers clarified patients’ pain diagnoses prior to pharmacy consultations.
After face-to-face patient interviews, the inpatient pain CPS prepared pain management recommendations, including nonopioid/adjuvant pain medications and/or opioid dose adjustments. The IPPCS also collaborated with pain physicians for intervention procedures, nonpharmacologic recommendations, and for more complex patients who may have required additional imaging or detailed physical evaluations. Pain CPSs documented CPRS notes with the SOAR template and discussed all recommendations with appropriate inpatient teams.
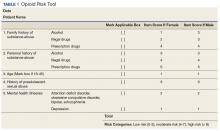
Respective providers received questionnaires hosted on SurveyMonkey.com (San Mateo, CA) to gauge their satisfaction with the IPPCS at the end of the pilot period, which helped determine program utility. Data collected for the pilot included patient demographics; patient admission diagnosis; consulting inpatient service; type of pain and reason for IPPCS request; total morphine equivalent daily dose (MEDD); pertinent past medical history (ie, sleep apnea, psychiatric comorbidities, or substance use disorder [SUD]); ORT score; patients’ reported average pain severity on the 10-point Numeric Pain Rating Scale (NPRS); number of requests submitted; medications discontinued, initiated, or dose increased/decreased; and number of pharmacist recommendations, including number accepted by providers. The ORT is a 5-item questionnaire used to determine risk of opioid-related aberrant behaviors in adults to help discriminate between low-risk and high-risk individuals (Table 1).17
Descriptive statistics were used to evaluate the results, and a Likert scale was used to evaluate responses the from provider satisfaction questionnaires. The IPPCS collected and organized the data using Microsoft Excel (Redmond, WA).
Results
By the end of the pilot period in May 2016, the IPPCS had received 100 consult requests and completed 81% (Figure). The remaining consults included 11% forwarded to other disciplines. The service discontinued 8% of the requests, given patients’ hospital discharge prior to IPPCS review.
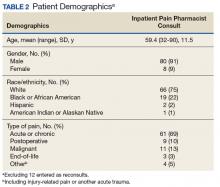
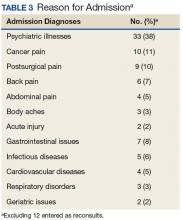
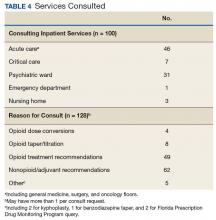
Baseline patient data are outlined in Tables 2, 3, 4, and 5. For each of the 100 consults, providers could select more than 1 reason for the request. The nonopioid/adjuvant treatment recommendations were the most common at 49% (62/128). Patients could have more than 1 pertinent medical comorbidity, with psychiatric illnesses the most prevalent at 68% (133/197). A mean ORT score of 8.1 indicated a high risk for opioid-related aberrant behavior. Overall, half the patients (37/73) were high risk, 25% (18/73) were medium risk (ORT 4-7), and 25% (18/73) were low risk (ORT 0-3). Patients’ reported average pain was often severe (NPRS 7-10) at 54% (40/74) or moderate (NPRS 4-6) at 39% (29/74).
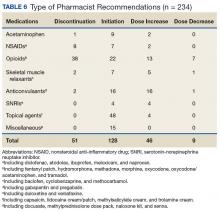
The IPPCS recommended various medications for initiation, discontinuation, or dosage changes (Table 6). For example, the IPPCS recommended initiation of topical agents in 38% (48/128) of cases. The inpatient pain CPS offered opioid initiation in 17% (22/128) of cases, with immediate-release oral morphine as the most predominant. Notably, opioids remained the most common medications suggested for discontinuation at 74% (38/51), including 47% (18/38) for IV hydromorphone. Dose titration recommendations mainly included anticonvulsants at 33% (16/48), and most dose reductions involved opioids at 78% (7/9), namely, oxycodone/acetaminophen and IV hydromorphone.
Providers accepted 76% (179/234) of IPPCS pharmacist medication recommendations. The most common included initiation/optimization of adjuvant therapy (eg, anticonvulsants, serotonin-norepinephrine reuptake inhibitors [SNRIs], and topical agents) at 46% (83/179), followed by opioid discontinuation (eg, IV hydromorphone) at 22% (40/179). Although this project primarily tracked medication interventions, examples of accepted nonpharmacologic recommendations included UDT and referrals to other programs (eg, pain psychology, substance abuse, mental health, acupuncture, chiropractor, PT/OT/PMR, and interventional pain management), which received support from each respective discipline. Declined pharmacologic recommendations mostly included topicals (eg, lidocaine, trolamine, and capsaicin cream) at 35% (19/55). However, findings also show that providers implemented 100% of medication recommendations in whole for 58% (47/81) of consults.
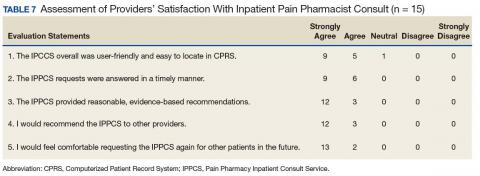
Likert scale satisfaction questionnaires offered insight into providers’ perception of the IPPCS (Table 7). One provider felt “neutral” about the consult submission process, given the time needed to complete the CPRS requests, but all other providers “agreed” or “strongly agreed” that the IPPCS was user-friendly. More importantly, 100% (15/15) “agreed” or “strongly agreed” that the inpatient pain CPS answered consults promptly with reasonable, evidence-based recommendations. All respondents declared that they would recommend the IPPCS to other practitioners and felt comfortable entering requests for future patients.
Discussion
The IPPCS achieved a total of 100 consults, which served as the sample for the pilot program. With support from the OCPC, PMR, and Clinical Pharmacy Department Administration, the IPPCS operated from November 2, 2015 through May 6, 2016. Results suggested that this new service could assist in managing inpatient pain issues in collaboration with inpatient multidisciplinary teams.
The most popular reason for IPPCS consults was acute on chronic pain. Given national efforts to improve opioid prescribing through the VA Opioid Safety Initiative (OSI) and the 2016 CDC Guideline for Opioid Prescribing, most pain consults requested nonopioid/adjuvant recommendations.18,19 Despite the wide MEDD range in this sample, the median/mean generally remained below recommended limits per current guidelines.18,19 However, the small sample size and lack of patient diversity (mostly white male veterans) limited the generalizability to non-VA medical facilities. Veterans often experienced both chronic pain and psychiatric disturbances, which explained the significant number of underlying mental health comorbidities observed. This affirmed the close interrelationship between pain and psychiatric issues described in the literature.20
Providers’ acceptance of pharmacologic and nonpharmacologic treatment modalities supported a comprehensive, multidisciplinary, and biopsychosocial approach to effective analgesic management. During this pilot, the most common pharmacy medication recommendations, namely, discontinuation of inappropriate opioids (eg, IV hydromorphone in patients who are controlled on and/or able to tolerate oral medications) and dose titration of adjuvant medications (eg, anticonvulsants for neuropathic pain), revealed that the IPPCS provided needed expertise and alternatives for complex pain patients. The IPPCS was well received, as inpatient providers accepted and implemented a large proportion of pharmacist recommendations. Despite risks of bias with a nonvalidated questionnaire, providers offered positive feedback. In the future, distributing satisfaction evaluations to patients also would provide more insight into how others perceived the IPPCS.
Limitations
Reasons for unaccepted recommendations included perceived limited effectiveness and/or feasibility of topical agents for acute pain, as providers seemed to favor systemic therapy for supposedly more immediate analgesia. Prescriber preference may explain why inpatient teams sometimes declined adjuvant therapy recommendations. However, the 2016 American Pain Society Guidelines on the Management of Postoperative Pain support a multimodal approach and confirm that adjuvants can reduce patients’ opioid requirements.21
Consulting teams did not execute some opioid recommendations, which may be due to various factors, including patient-related or provider-related factors in the inpatient vs outpatient setting. Lack of retrospective analysis for comparison of results pre- and post-IPPCS implementation also limited the outcomes. However, this project was piloted as a QI initiative after providers identified significant needs for inpatient pain management at the WPBVAMC. No retrospective analysis was undertaken, as this project analyzed only responses during the pilot program.
Other obstacles of the IPPCS included request appropriateness and triaging. The inpatient pain CPS deferred management of some consults to other disciplines (eg, gastroenterology) for more appropriate care. The IPPCS deferred certain cases of acute pancreatic pain or generalized abdominal pain for further workup to address patients’ underlying issues. The inpatient pain CPS relayed pertinent information regarding appropriate consults to inpatient teams. In the future, developing more specific inclusion/exclusion criteria and delivering provider education about proper IPPCS requests may resolve this issue.
Challenges with pain consults from inpatient psychiatry stemmed from patients’ skepticism and unwillingness to accept nonopioid/adjuvant therapies. Additionally, comorbid psychiatric disorders are often associated with SUDs and potentially opioid-related aberrant behavior. More than 40% of opioid-dependent individuals have comorbid psychiatric disorders, especially depression, anxiety, and bipolar disorder.22 Poorly-managed pain also drives SUD, as 80% of these patients illegally obtain prescription opioids. Thus, undertreatment of pain may push individuals to secure pain medications from illegal/illicit sources to achieve analgesia.23 Following pain physician consultation, the IPPCS continued inpatient opioids for 12% (10/81) of patients with a SUD history, including 5 with postoperative pain or other acute processes, since patients were kept in a monitored health care environment. The remaining included 4 with malignant pain and 1 with end-of-life pain. Overall, the IPPCS recommended that inpatient teams discharge these patients on as little opioids as possible, as well as to make referrals to substance abuse programs when necessary. Effective pain management of patients with aberrant behavior requires a comprehensive interdisciplinary team approach. To mitigate risk, effectively treat pain, and maintain patient safety, clinicians must recognize biologic, chemical, social, and psychiatric aspects of substance abuse.21
Another limitation during this pilot was an inability to promptly assess the impact of recommendations, given limited opportunities to reevaluate patients. In the future, more dedicated time for the inpatient pain CPSs to respond to consults may allow for better follow-up rather than initial consults only. Providers sometimes discharged patients within 24 hours of submitting consults as well, which left no time for the inpatient pain CPS consultation. However, the IPPCS forwarded appropriate requests to pain CPS e-consult services for chart review recommendations. Encouraging providers to submit consults earlier in patients’ hospital admissions may help reduce the number of incomplete IPPCS requests. Although expanding service hours would require more dedicated CPS staffing resources, it is another option for quicker consult completion and prompt follow-up.
Future Directions
Future efforts to expand this project include ensuring patient safety through judicious opioid use. Smooth transitions of care will particularly help to improve the quality of pain management. Current WPBVAMC policies stated that the primary care provider (PCP) alone must agree to continue prescribing outpatient analgesic medications, including opioids, prescribed from the OCPC once patients return to Primary Care. Continued provider education would ideally promote efficient utilization of the IPPCS and OCPC.
The pain pharmacy SOAR note template also could undergo additional edits/revisions, including the addition of opioid overdose risk assessments. For improved documentation and standardization, the template could autopopulate patient-specific information when the inpatient pain CPS chooses the designated note title. The IPPCS also hoped to streamline the CPRS consult link for more convenience and ease of use. Ultimately, the IPPCS wished to provide ongoing provider education, inpatient opioid therapy, and other topics upon request.
Conclusion
The IPPCS received positive provider feedback and collected 100 consults (averaging 4 per week) during the 6-month pilot QI project. Most consults were for acute or chronic pain and requested nonopioid/adjuvant recommendations. The new service intended to fulfill unmet needs at the WPBVAMC by expanding the facility’s current pain programs. Prescribers reported a high level of satisfaction and a willingness to not only refer other clinicians to the program, but also continue using the consult. Providers unanimously agreed that the pain CPS provided reasonable, evidence-based recommendations. This project demonstrated that the IPPCS can aid in meeting new demands amid the challenging landscape of pain practice.
1. D’Arcy Y. Treating acute pain in the hospitalized patient. Nurse Pract. 2012;37(8):22-30.
2. Marks AD, Rodgers PE. Diagnosis and management of acute pain in the hospitalized patient. Am J Med. 2014;3(3):e396-e408.
3. Paice JA, Von Roenn JH. Under- or overtreatment of pain in the patient with cancer: how to achieve proper balance. J Clin Oncol. 2014;32(16):1721-1726.
4. Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573-1581.
5. Palomano RC, Rathmell JP, Krenzischek DA, Dunwoody CJ. Emerging trends and new approaches to acute pain management. J Perianesth Nurs. 2008;23(suppl 1):S43-S53.
6. U.S. Department of Health & Human Services, Office of the Surgeon General. Facing addiction in America: the surgeon general’s report on alcohol, drugs, and health, executive summary. https://addiction.surgeongeneral.gov/executive-summary.pdf. Published November 2016. Accessed November 1, 2017.
7. Bagian JP, Cohen M, Barnsteiner JH, et al. Safe use of opioids in hospitals. Sentinel Event Alert. 2012;49:1-5.
8. Atkinson TJ, Gulum AH, Forkum WG. The future of pain pharmacy: directed by need. Integrated Pharm Res Pract. 2016;2016(5):33-42.
9. Lothian ST, Fotis MA, Von Gutten CF, et al. Cancer pain management through a pharmacist-based analgesic dosing service. Am J Health Syst Pharm. 1999;56:1119-1125.
10. Lynn MA. Pharmacist interventions in pain management. Am J Health Syst Pharm. 2004;61(14):1487-1489.
11. Strickland JM, Huskey A, Brushwood DB. Pharmacist-physician collaboration in pain management practice. J Opioid Manag. 2007;3(6):295-301.
12. Fan T and Elgourt T. Pain management pharmacy service in a community hospital. Am J Health Syst Pharm. 2008;65(16):1560-1565.
13. Andrews LB, Bridgeman MB, Dalal KS, et al. Implementation of a pharmacist-directed pain management consultation service for hospitalised adults with a history of substance abuse. Int J Clin Pract. 2013;67(12):1342-1349.
14. Poirier RH, Brown CS, Garcia YT, Gann NY, Sandoval RA, McNulty JR. Implementation of a pharmacist directed pain management service in the inpatient setting. http://www.ashpadvantage.com/bestpractices/2014_papers/Kaweah-Delta.htm. Published 2014. Accessed November 1, 2017.
15. Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nded. San Francisco, CA: Jossey-Bass; 2009.
16. Nahin, RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254.
17. Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the opioid risk tool. Pain Med. 2005;6(6):432-442.
18. Nazario M. Opioid therapy risk management: the VA opioid safety and naloxone distribution initiatives. http://jfpsmeeting.pharmacist.com/sites/default/files/slides/Opioid%20Therapy%20Risk%20Management.pdf. Published October 15, 2015. Accessed November 1, 2017.
19. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain – United States, 2016. MMWR Rep. 2016;65(1):1-49.
20. Outcalt SD, Kroenke K, Krebs EE, et al. Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. J Behav Med. 2015;38:535.
21. Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-157.
22. NIDA/SAMHSA Blending Initiative. https://www.drugabuse.gov/nidasamhsa-blending-initiative. Updated November 2015. Accessed November 1, 2017.
23. Alford DP, German JS, Samet JH, Cheng DM, Lloyd-Travaglini CA, Saitz R. Primary care patients with drug use report chronic pain and self-medicate with alcohol and other drugs. J Gen Intern Med. 2016;31(5):486-491.
The term pain refers to unpleasant sensory, emotional experiences associated with actual or potential tissue damage and is described in terms of such damage.1 Acute pain from neurophysiologic responses to noxious stimuli resolves upon tissue healing or stimuli removal (eg, 3-6 months); however, chronic pain lingers beyond the expected time course of the acute injury and repair process.1,2 Despite pain management advances, the under- or overtreatment of pain for different patient populations (eg, cancer and noncancer) remains an important concern.3,4
Hospitals have focused on optimizing inpatient pain management, because uncontrolled pain remains the most common reason for readmissions the first week postsurgery.5 The safe use of opioids (prescription, illicit synthetic, or heroin) poses major challenges and raises significant concerns. Rates of opioid-related hospital admissions have increased by 42% since 2009, and total overdose deaths reached a new high of 47,055 in 2014, including 28,647 (61%) from opioids.6
Opioids rank among the medications most often associated with serious adverse events (AEs), including respiratory depression and death.7 In response, the Joint Commission recommends patient assessments for opioid-related AEs, technology to monitor opioid prescribing, pharmacist consultation for opioid conversions and route of administration changes, provider education about risks of opioids, and risk screening tools for opioid-related oversedation and respiratory depression.7 Treatment guidelines strive to minimize the impact of acute pain by offering a scientific basis for practice, but evidence suggests a lack of suitable pain programs.7 Increases in opioid prescribing along with clinical guidelines and state laws recommending specialty pain service referrals for patients on high-dose opioids, have increased demand for competent pain clinicians.8
The expertise of a clinical pharmacy specialists (CPS) can help refine ineffective and potentially harmful pain medication therapy in complex patient cases. Existing literature outlines the various benefits of pharmacist participation in collaborative pain services for cancer and noncancer pain, as well as cases involving substance abuse.9-13 Various articles support pharmacists’ role as an educator and team member who can add valuable, trustworthy clinical knowledge that enhances clinical encounters and guides protocol/policy development.12,13 These efforts have improved patient satisfaction and encouraged physicians and nurses to proactively seek pharmacists’ advice for difficult cases.9
Frequent communication with interdisciplinary teams have helped considerably in establishing clinical pharmacy services that benefit patient care and offer sources of professional accomplishment.10,11 For example, pharmacists at Kaweah Delta Medical Center in Visalia, CA launched an innovative pain program that encompassed consultations and opioid stewardship, which demonstrated that pharmacists can improve patient outcomes in the front lines of pain management.14 Pain CPSs have advanced knowledge of pharmacokinetics, pharmacodynamics, and therapeutics to promote safe and effective analgesic use, as well as to identify opioid use disorders. Evidence suggests that pharmacists’ presence on interdisciplinary pain teams improves outcomes by optimizing medication selection, improving adherence, and preventing AEs.8
Following the plan-do-study-act model for quality improvement (QI), this project hoped to expand current pain programs at the West Palm Beach VAMC (WPBVAMC) by evaluating the feasibility of an inpatient pain pharmacist consult service (IPPCS) at the 301-bed teaching facility, which includes 130 acute/intensive care and 120 nursing/domiciliary beds.15 Staff provide primary- and secondary-level care to veterans in 7 counties along Florida’s southeastern coast.
In 2009, the WPBVAMC PGY-2 Pain Management and Palliative Care Program became the VA’s first accredited pain pharmacy residency. Residents train with the Physical Medicine & Rehabilitation (PMR) and Chronic Pain Management departments, which provide outpatient services from 7 pain physicians, a pain psychologist, registered nurse, chiropractor, acupuncturist, physical/occupational therapy (PT/OT), and 3 pain/palliative care CPSs.
The WPBVAMC had established interdisciplinary outpatient chronic pain clinic (OCPC) physician- and pharmacist-run services along with a pain CPS electronic consult (e-consult) program. However, no formal mechanisms for inpatient pain consultations existed. Prior to the IPPCS outlined in this study, OCPC practitioners, including 2 pain CPSs, managed impromptu inpatient pain issues as “curbside consultations” along with usual day-to-day clinic duties.
The OCPC, PMR, and Clinical Pharmacy administration recognized the need for more clinical support to manage complex analgesic issues in inpatient veterans, as these patients often have acute pain with underlying chronic pain syndromes. In a national survey, veterans were significantly more likely than were nonveterans to report painful health conditions (65.5% vs 56.4%) and to classify their pain as severe (9.1% vs 6.3%).16 The WPBVAMC administration concluded that an IPPCS would offer a more efficient means of handling such cases. The IPPCS would formally streamline inpatient pain consults, enabling CPSs to thoroughly evaluate pain-related issues to propose evidence-based recommendations.
The primary objective of this QI project was to assess the IPPCS implementation as part of multimodal care to satisfy unmet patient care needs at the WPBVAMC. Secondary objectives for program feasibility included identifying the volume and type of pain consults, categorizing pharmacist interventions, classifying providers’ satisfaction, and determining types of responses to pharmacists’ medication recommendations.
Methods
This QI project ascertained the feasibility of the IPPCS by evaluating all consults obtained during the pilot period from November 2, 2015 through May 6, 2016. The IPPCS was accessible Monday through Friday during normal business hours. Goal turnaround time for consult completion was 24 to 72 hours, given the lack of coverage on holidays and weekends. The target population included veterans hospitalized at the WPBVAMC inpatient ward or nursing home with uncontrolled pain on IV and/or oral analgesic medications. All IPPCS consults submitted during the pilot period were included in the sample.
The WPBVAMC Scientific Advisory Committee (SAC) approved this QI program prior to initiation. Following supervisory support from the OCPC, PMR, and Clinical Pharmacy departments, hospital technologists assisted in creating a consult link in the Computerized Patient Record System (CPRS), which allowed providers to submit IPPCS requests for specific patients efficiently. Consults were categorized as postoperative pain, acute or chronic pain, malignant pain, or end-of-life pain. Inpatient providers could enter requests for assistance with 1 or more of the following: opioid dose conversions, opioid taper/titration schedules, general opioid treatment recommendations, or nonopioid/adjuvant recommendations.
The Medical Records Committee approved a customized CPRS subjective-objective-assessment-recommendations (SOAR) note template, which helped standardize the pain CPS documentation. To promote consult requests and interdisciplinary collaboration, inpatient clinicians received education about the IPPCS at respective meetings (eg, General Medicine staff and Clinical Pharmacy meetings).
All CPSs involved in this project were residency-trained in direct patient care, including pain and palliative care, and maintained national board certification as pharmacotherapy specialists. Their role included reviewing patients’ electronic medical records, conducting face-to-face pain assessments, completing opioid risk assessments, evaluating analgesic regimen appropriateness, reviewing medication adherence, completing pain medication reconciliation, querying the Florida Prescription Drug Monitoring Program (PDMP), interpreting urine drug testing (UDT), and delivering provider/patient/caregiver education. Parameters used to determine the appropriateness of analgesic regimens included, but were not limited to:
- Use of oral instead of IV medications if oral dosing was feasible/possible/appropriate;
- Dose and adjustments per renal/hepatic function;
- Adequate treatment duration and titration;
- No therapeutic drug class duplications;
- Medication tolerability (eg, allergies, AEs, drug interactions); and
- Opioid risk assessment per Opioid Risk Tool (ORT) score and medical history.
Consulting providers clarified patients’ pain diagnoses prior to pharmacy consultations.
After face-to-face patient interviews, the inpatient pain CPS prepared pain management recommendations, including nonopioid/adjuvant pain medications and/or opioid dose adjustments. The IPPCS also collaborated with pain physicians for intervention procedures, nonpharmacologic recommendations, and for more complex patients who may have required additional imaging or detailed physical evaluations. Pain CPSs documented CPRS notes with the SOAR template and discussed all recommendations with appropriate inpatient teams.
Respective providers received questionnaires hosted on SurveyMonkey.com (San Mateo, CA) to gauge their satisfaction with the IPPCS at the end of the pilot period, which helped determine program utility. Data collected for the pilot included patient demographics; patient admission diagnosis; consulting inpatient service; type of pain and reason for IPPCS request; total morphine equivalent daily dose (MEDD); pertinent past medical history (ie, sleep apnea, psychiatric comorbidities, or substance use disorder [SUD]); ORT score; patients’ reported average pain severity on the 10-point Numeric Pain Rating Scale (NPRS); number of requests submitted; medications discontinued, initiated, or dose increased/decreased; and number of pharmacist recommendations, including number accepted by providers. The ORT is a 5-item questionnaire used to determine risk of opioid-related aberrant behaviors in adults to help discriminate between low-risk and high-risk individuals (Table 1).17
Descriptive statistics were used to evaluate the results, and a Likert scale was used to evaluate responses the from provider satisfaction questionnaires. The IPPCS collected and organized the data using Microsoft Excel (Redmond, WA).
Results
By the end of the pilot period in May 2016, the IPPCS had received 100 consult requests and completed 81% (Figure). The remaining consults included 11% forwarded to other disciplines. The service discontinued 8% of the requests, given patients’ hospital discharge prior to IPPCS review.
Baseline patient data are outlined in Tables 2, 3, 4, and 5. For each of the 100 consults, providers could select more than 1 reason for the request. The nonopioid/adjuvant treatment recommendations were the most common at 49% (62/128). Patients could have more than 1 pertinent medical comorbidity, with psychiatric illnesses the most prevalent at 68% (133/197). A mean ORT score of 8.1 indicated a high risk for opioid-related aberrant behavior. Overall, half the patients (37/73) were high risk, 25% (18/73) were medium risk (ORT 4-7), and 25% (18/73) were low risk (ORT 0-3). Patients’ reported average pain was often severe (NPRS 7-10) at 54% (40/74) or moderate (NPRS 4-6) at 39% (29/74).
The IPPCS recommended various medications for initiation, discontinuation, or dosage changes (Table 6). For example, the IPPCS recommended initiation of topical agents in 38% (48/128) of cases. The inpatient pain CPS offered opioid initiation in 17% (22/128) of cases, with immediate-release oral morphine as the most predominant. Notably, opioids remained the most common medications suggested for discontinuation at 74% (38/51), including 47% (18/38) for IV hydromorphone. Dose titration recommendations mainly included anticonvulsants at 33% (16/48), and most dose reductions involved opioids at 78% (7/9), namely, oxycodone/acetaminophen and IV hydromorphone.
Providers accepted 76% (179/234) of IPPCS pharmacist medication recommendations. The most common included initiation/optimization of adjuvant therapy (eg, anticonvulsants, serotonin-norepinephrine reuptake inhibitors [SNRIs], and topical agents) at 46% (83/179), followed by opioid discontinuation (eg, IV hydromorphone) at 22% (40/179). Although this project primarily tracked medication interventions, examples of accepted nonpharmacologic recommendations included UDT and referrals to other programs (eg, pain psychology, substance abuse, mental health, acupuncture, chiropractor, PT/OT/PMR, and interventional pain management), which received support from each respective discipline. Declined pharmacologic recommendations mostly included topicals (eg, lidocaine, trolamine, and capsaicin cream) at 35% (19/55). However, findings also show that providers implemented 100% of medication recommendations in whole for 58% (47/81) of consults.
Likert scale satisfaction questionnaires offered insight into providers’ perception of the IPPCS (Table 7). One provider felt “neutral” about the consult submission process, given the time needed to complete the CPRS requests, but all other providers “agreed” or “strongly agreed” that the IPPCS was user-friendly. More importantly, 100% (15/15) “agreed” or “strongly agreed” that the inpatient pain CPS answered consults promptly with reasonable, evidence-based recommendations. All respondents declared that they would recommend the IPPCS to other practitioners and felt comfortable entering requests for future patients.
Discussion
The IPPCS achieved a total of 100 consults, which served as the sample for the pilot program. With support from the OCPC, PMR, and Clinical Pharmacy Department Administration, the IPPCS operated from November 2, 2015 through May 6, 2016. Results suggested that this new service could assist in managing inpatient pain issues in collaboration with inpatient multidisciplinary teams.
The most popular reason for IPPCS consults was acute on chronic pain. Given national efforts to improve opioid prescribing through the VA Opioid Safety Initiative (OSI) and the 2016 CDC Guideline for Opioid Prescribing, most pain consults requested nonopioid/adjuvant recommendations.18,19 Despite the wide MEDD range in this sample, the median/mean generally remained below recommended limits per current guidelines.18,19 However, the small sample size and lack of patient diversity (mostly white male veterans) limited the generalizability to non-VA medical facilities. Veterans often experienced both chronic pain and psychiatric disturbances, which explained the significant number of underlying mental health comorbidities observed. This affirmed the close interrelationship between pain and psychiatric issues described in the literature.20
Providers’ acceptance of pharmacologic and nonpharmacologic treatment modalities supported a comprehensive, multidisciplinary, and biopsychosocial approach to effective analgesic management. During this pilot, the most common pharmacy medication recommendations, namely, discontinuation of inappropriate opioids (eg, IV hydromorphone in patients who are controlled on and/or able to tolerate oral medications) and dose titration of adjuvant medications (eg, anticonvulsants for neuropathic pain), revealed that the IPPCS provided needed expertise and alternatives for complex pain patients. The IPPCS was well received, as inpatient providers accepted and implemented a large proportion of pharmacist recommendations. Despite risks of bias with a nonvalidated questionnaire, providers offered positive feedback. In the future, distributing satisfaction evaluations to patients also would provide more insight into how others perceived the IPPCS.
Limitations
Reasons for unaccepted recommendations included perceived limited effectiveness and/or feasibility of topical agents for acute pain, as providers seemed to favor systemic therapy for supposedly more immediate analgesia. Prescriber preference may explain why inpatient teams sometimes declined adjuvant therapy recommendations. However, the 2016 American Pain Society Guidelines on the Management of Postoperative Pain support a multimodal approach and confirm that adjuvants can reduce patients’ opioid requirements.21
Consulting teams did not execute some opioid recommendations, which may be due to various factors, including patient-related or provider-related factors in the inpatient vs outpatient setting. Lack of retrospective analysis for comparison of results pre- and post-IPPCS implementation also limited the outcomes. However, this project was piloted as a QI initiative after providers identified significant needs for inpatient pain management at the WPBVAMC. No retrospective analysis was undertaken, as this project analyzed only responses during the pilot program.
Other obstacles of the IPPCS included request appropriateness and triaging. The inpatient pain CPS deferred management of some consults to other disciplines (eg, gastroenterology) for more appropriate care. The IPPCS deferred certain cases of acute pancreatic pain or generalized abdominal pain for further workup to address patients’ underlying issues. The inpatient pain CPS relayed pertinent information regarding appropriate consults to inpatient teams. In the future, developing more specific inclusion/exclusion criteria and delivering provider education about proper IPPCS requests may resolve this issue.
Challenges with pain consults from inpatient psychiatry stemmed from patients’ skepticism and unwillingness to accept nonopioid/adjuvant therapies. Additionally, comorbid psychiatric disorders are often associated with SUDs and potentially opioid-related aberrant behavior. More than 40% of opioid-dependent individuals have comorbid psychiatric disorders, especially depression, anxiety, and bipolar disorder.22 Poorly-managed pain also drives SUD, as 80% of these patients illegally obtain prescription opioids. Thus, undertreatment of pain may push individuals to secure pain medications from illegal/illicit sources to achieve analgesia.23 Following pain physician consultation, the IPPCS continued inpatient opioids for 12% (10/81) of patients with a SUD history, including 5 with postoperative pain or other acute processes, since patients were kept in a monitored health care environment. The remaining included 4 with malignant pain and 1 with end-of-life pain. Overall, the IPPCS recommended that inpatient teams discharge these patients on as little opioids as possible, as well as to make referrals to substance abuse programs when necessary. Effective pain management of patients with aberrant behavior requires a comprehensive interdisciplinary team approach. To mitigate risk, effectively treat pain, and maintain patient safety, clinicians must recognize biologic, chemical, social, and psychiatric aspects of substance abuse.21
Another limitation during this pilot was an inability to promptly assess the impact of recommendations, given limited opportunities to reevaluate patients. In the future, more dedicated time for the inpatient pain CPSs to respond to consults may allow for better follow-up rather than initial consults only. Providers sometimes discharged patients within 24 hours of submitting consults as well, which left no time for the inpatient pain CPS consultation. However, the IPPCS forwarded appropriate requests to pain CPS e-consult services for chart review recommendations. Encouraging providers to submit consults earlier in patients’ hospital admissions may help reduce the number of incomplete IPPCS requests. Although expanding service hours would require more dedicated CPS staffing resources, it is another option for quicker consult completion and prompt follow-up.
Future Directions
Future efforts to expand this project include ensuring patient safety through judicious opioid use. Smooth transitions of care will particularly help to improve the quality of pain management. Current WPBVAMC policies stated that the primary care provider (PCP) alone must agree to continue prescribing outpatient analgesic medications, including opioids, prescribed from the OCPC once patients return to Primary Care. Continued provider education would ideally promote efficient utilization of the IPPCS and OCPC.
The pain pharmacy SOAR note template also could undergo additional edits/revisions, including the addition of opioid overdose risk assessments. For improved documentation and standardization, the template could autopopulate patient-specific information when the inpatient pain CPS chooses the designated note title. The IPPCS also hoped to streamline the CPRS consult link for more convenience and ease of use. Ultimately, the IPPCS wished to provide ongoing provider education, inpatient opioid therapy, and other topics upon request.
Conclusion
The IPPCS received positive provider feedback and collected 100 consults (averaging 4 per week) during the 6-month pilot QI project. Most consults were for acute or chronic pain and requested nonopioid/adjuvant recommendations. The new service intended to fulfill unmet needs at the WPBVAMC by expanding the facility’s current pain programs. Prescribers reported a high level of satisfaction and a willingness to not only refer other clinicians to the program, but also continue using the consult. Providers unanimously agreed that the pain CPS provided reasonable, evidence-based recommendations. This project demonstrated that the IPPCS can aid in meeting new demands amid the challenging landscape of pain practice.
The term pain refers to unpleasant sensory, emotional experiences associated with actual or potential tissue damage and is described in terms of such damage.1 Acute pain from neurophysiologic responses to noxious stimuli resolves upon tissue healing or stimuli removal (eg, 3-6 months); however, chronic pain lingers beyond the expected time course of the acute injury and repair process.1,2 Despite pain management advances, the under- or overtreatment of pain for different patient populations (eg, cancer and noncancer) remains an important concern.3,4
Hospitals have focused on optimizing inpatient pain management, because uncontrolled pain remains the most common reason for readmissions the first week postsurgery.5 The safe use of opioids (prescription, illicit synthetic, or heroin) poses major challenges and raises significant concerns. Rates of opioid-related hospital admissions have increased by 42% since 2009, and total overdose deaths reached a new high of 47,055 in 2014, including 28,647 (61%) from opioids.6
Opioids rank among the medications most often associated with serious adverse events (AEs), including respiratory depression and death.7 In response, the Joint Commission recommends patient assessments for opioid-related AEs, technology to monitor opioid prescribing, pharmacist consultation for opioid conversions and route of administration changes, provider education about risks of opioids, and risk screening tools for opioid-related oversedation and respiratory depression.7 Treatment guidelines strive to minimize the impact of acute pain by offering a scientific basis for practice, but evidence suggests a lack of suitable pain programs.7 Increases in opioid prescribing along with clinical guidelines and state laws recommending specialty pain service referrals for patients on high-dose opioids, have increased demand for competent pain clinicians.8
The expertise of a clinical pharmacy specialists (CPS) can help refine ineffective and potentially harmful pain medication therapy in complex patient cases. Existing literature outlines the various benefits of pharmacist participation in collaborative pain services for cancer and noncancer pain, as well as cases involving substance abuse.9-13 Various articles support pharmacists’ role as an educator and team member who can add valuable, trustworthy clinical knowledge that enhances clinical encounters and guides protocol/policy development.12,13 These efforts have improved patient satisfaction and encouraged physicians and nurses to proactively seek pharmacists’ advice for difficult cases.9
Frequent communication with interdisciplinary teams have helped considerably in establishing clinical pharmacy services that benefit patient care and offer sources of professional accomplishment.10,11 For example, pharmacists at Kaweah Delta Medical Center in Visalia, CA launched an innovative pain program that encompassed consultations and opioid stewardship, which demonstrated that pharmacists can improve patient outcomes in the front lines of pain management.14 Pain CPSs have advanced knowledge of pharmacokinetics, pharmacodynamics, and therapeutics to promote safe and effective analgesic use, as well as to identify opioid use disorders. Evidence suggests that pharmacists’ presence on interdisciplinary pain teams improves outcomes by optimizing medication selection, improving adherence, and preventing AEs.8
Following the plan-do-study-act model for quality improvement (QI), this project hoped to expand current pain programs at the West Palm Beach VAMC (WPBVAMC) by evaluating the feasibility of an inpatient pain pharmacist consult service (IPPCS) at the 301-bed teaching facility, which includes 130 acute/intensive care and 120 nursing/domiciliary beds.15 Staff provide primary- and secondary-level care to veterans in 7 counties along Florida’s southeastern coast.
In 2009, the WPBVAMC PGY-2 Pain Management and Palliative Care Program became the VA’s first accredited pain pharmacy residency. Residents train with the Physical Medicine & Rehabilitation (PMR) and Chronic Pain Management departments, which provide outpatient services from 7 pain physicians, a pain psychologist, registered nurse, chiropractor, acupuncturist, physical/occupational therapy (PT/OT), and 3 pain/palliative care CPSs.
The WPBVAMC had established interdisciplinary outpatient chronic pain clinic (OCPC) physician- and pharmacist-run services along with a pain CPS electronic consult (e-consult) program. However, no formal mechanisms for inpatient pain consultations existed. Prior to the IPPCS outlined in this study, OCPC practitioners, including 2 pain CPSs, managed impromptu inpatient pain issues as “curbside consultations” along with usual day-to-day clinic duties.
The OCPC, PMR, and Clinical Pharmacy administration recognized the need for more clinical support to manage complex analgesic issues in inpatient veterans, as these patients often have acute pain with underlying chronic pain syndromes. In a national survey, veterans were significantly more likely than were nonveterans to report painful health conditions (65.5% vs 56.4%) and to classify their pain as severe (9.1% vs 6.3%).16 The WPBVAMC administration concluded that an IPPCS would offer a more efficient means of handling such cases. The IPPCS would formally streamline inpatient pain consults, enabling CPSs to thoroughly evaluate pain-related issues to propose evidence-based recommendations.
The primary objective of this QI project was to assess the IPPCS implementation as part of multimodal care to satisfy unmet patient care needs at the WPBVAMC. Secondary objectives for program feasibility included identifying the volume and type of pain consults, categorizing pharmacist interventions, classifying providers’ satisfaction, and determining types of responses to pharmacists’ medication recommendations.
Methods
This QI project ascertained the feasibility of the IPPCS by evaluating all consults obtained during the pilot period from November 2, 2015 through May 6, 2016. The IPPCS was accessible Monday through Friday during normal business hours. Goal turnaround time for consult completion was 24 to 72 hours, given the lack of coverage on holidays and weekends. The target population included veterans hospitalized at the WPBVAMC inpatient ward or nursing home with uncontrolled pain on IV and/or oral analgesic medications. All IPPCS consults submitted during the pilot period were included in the sample.
The WPBVAMC Scientific Advisory Committee (SAC) approved this QI program prior to initiation. Following supervisory support from the OCPC, PMR, and Clinical Pharmacy departments, hospital technologists assisted in creating a consult link in the Computerized Patient Record System (CPRS), which allowed providers to submit IPPCS requests for specific patients efficiently. Consults were categorized as postoperative pain, acute or chronic pain, malignant pain, or end-of-life pain. Inpatient providers could enter requests for assistance with 1 or more of the following: opioid dose conversions, opioid taper/titration schedules, general opioid treatment recommendations, or nonopioid/adjuvant recommendations.
The Medical Records Committee approved a customized CPRS subjective-objective-assessment-recommendations (SOAR) note template, which helped standardize the pain CPS documentation. To promote consult requests and interdisciplinary collaboration, inpatient clinicians received education about the IPPCS at respective meetings (eg, General Medicine staff and Clinical Pharmacy meetings).
All CPSs involved in this project were residency-trained in direct patient care, including pain and palliative care, and maintained national board certification as pharmacotherapy specialists. Their role included reviewing patients’ electronic medical records, conducting face-to-face pain assessments, completing opioid risk assessments, evaluating analgesic regimen appropriateness, reviewing medication adherence, completing pain medication reconciliation, querying the Florida Prescription Drug Monitoring Program (PDMP), interpreting urine drug testing (UDT), and delivering provider/patient/caregiver education. Parameters used to determine the appropriateness of analgesic regimens included, but were not limited to:
- Use of oral instead of IV medications if oral dosing was feasible/possible/appropriate;
- Dose and adjustments per renal/hepatic function;
- Adequate treatment duration and titration;
- No therapeutic drug class duplications;
- Medication tolerability (eg, allergies, AEs, drug interactions); and
- Opioid risk assessment per Opioid Risk Tool (ORT) score and medical history.
Consulting providers clarified patients’ pain diagnoses prior to pharmacy consultations.
After face-to-face patient interviews, the inpatient pain CPS prepared pain management recommendations, including nonopioid/adjuvant pain medications and/or opioid dose adjustments. The IPPCS also collaborated with pain physicians for intervention procedures, nonpharmacologic recommendations, and for more complex patients who may have required additional imaging or detailed physical evaluations. Pain CPSs documented CPRS notes with the SOAR template and discussed all recommendations with appropriate inpatient teams.
Respective providers received questionnaires hosted on SurveyMonkey.com (San Mateo, CA) to gauge their satisfaction with the IPPCS at the end of the pilot period, which helped determine program utility. Data collected for the pilot included patient demographics; patient admission diagnosis; consulting inpatient service; type of pain and reason for IPPCS request; total morphine equivalent daily dose (MEDD); pertinent past medical history (ie, sleep apnea, psychiatric comorbidities, or substance use disorder [SUD]); ORT score; patients’ reported average pain severity on the 10-point Numeric Pain Rating Scale (NPRS); number of requests submitted; medications discontinued, initiated, or dose increased/decreased; and number of pharmacist recommendations, including number accepted by providers. The ORT is a 5-item questionnaire used to determine risk of opioid-related aberrant behaviors in adults to help discriminate between low-risk and high-risk individuals (Table 1).17
Descriptive statistics were used to evaluate the results, and a Likert scale was used to evaluate responses the from provider satisfaction questionnaires. The IPPCS collected and organized the data using Microsoft Excel (Redmond, WA).
Results
By the end of the pilot period in May 2016, the IPPCS had received 100 consult requests and completed 81% (Figure). The remaining consults included 11% forwarded to other disciplines. The service discontinued 8% of the requests, given patients’ hospital discharge prior to IPPCS review.
Baseline patient data are outlined in Tables 2, 3, 4, and 5. For each of the 100 consults, providers could select more than 1 reason for the request. The nonopioid/adjuvant treatment recommendations were the most common at 49% (62/128). Patients could have more than 1 pertinent medical comorbidity, with psychiatric illnesses the most prevalent at 68% (133/197). A mean ORT score of 8.1 indicated a high risk for opioid-related aberrant behavior. Overall, half the patients (37/73) were high risk, 25% (18/73) were medium risk (ORT 4-7), and 25% (18/73) were low risk (ORT 0-3). Patients’ reported average pain was often severe (NPRS 7-10) at 54% (40/74) or moderate (NPRS 4-6) at 39% (29/74).
The IPPCS recommended various medications for initiation, discontinuation, or dosage changes (Table 6). For example, the IPPCS recommended initiation of topical agents in 38% (48/128) of cases. The inpatient pain CPS offered opioid initiation in 17% (22/128) of cases, with immediate-release oral morphine as the most predominant. Notably, opioids remained the most common medications suggested for discontinuation at 74% (38/51), including 47% (18/38) for IV hydromorphone. Dose titration recommendations mainly included anticonvulsants at 33% (16/48), and most dose reductions involved opioids at 78% (7/9), namely, oxycodone/acetaminophen and IV hydromorphone.
Providers accepted 76% (179/234) of IPPCS pharmacist medication recommendations. The most common included initiation/optimization of adjuvant therapy (eg, anticonvulsants, serotonin-norepinephrine reuptake inhibitors [SNRIs], and topical agents) at 46% (83/179), followed by opioid discontinuation (eg, IV hydromorphone) at 22% (40/179). Although this project primarily tracked medication interventions, examples of accepted nonpharmacologic recommendations included UDT and referrals to other programs (eg, pain psychology, substance abuse, mental health, acupuncture, chiropractor, PT/OT/PMR, and interventional pain management), which received support from each respective discipline. Declined pharmacologic recommendations mostly included topicals (eg, lidocaine, trolamine, and capsaicin cream) at 35% (19/55). However, findings also show that providers implemented 100% of medication recommendations in whole for 58% (47/81) of consults.
Likert scale satisfaction questionnaires offered insight into providers’ perception of the IPPCS (Table 7). One provider felt “neutral” about the consult submission process, given the time needed to complete the CPRS requests, but all other providers “agreed” or “strongly agreed” that the IPPCS was user-friendly. More importantly, 100% (15/15) “agreed” or “strongly agreed” that the inpatient pain CPS answered consults promptly with reasonable, evidence-based recommendations. All respondents declared that they would recommend the IPPCS to other practitioners and felt comfortable entering requests for future patients.
Discussion
The IPPCS achieved a total of 100 consults, which served as the sample for the pilot program. With support from the OCPC, PMR, and Clinical Pharmacy Department Administration, the IPPCS operated from November 2, 2015 through May 6, 2016. Results suggested that this new service could assist in managing inpatient pain issues in collaboration with inpatient multidisciplinary teams.
The most popular reason for IPPCS consults was acute on chronic pain. Given national efforts to improve opioid prescribing through the VA Opioid Safety Initiative (OSI) and the 2016 CDC Guideline for Opioid Prescribing, most pain consults requested nonopioid/adjuvant recommendations.18,19 Despite the wide MEDD range in this sample, the median/mean generally remained below recommended limits per current guidelines.18,19 However, the small sample size and lack of patient diversity (mostly white male veterans) limited the generalizability to non-VA medical facilities. Veterans often experienced both chronic pain and psychiatric disturbances, which explained the significant number of underlying mental health comorbidities observed. This affirmed the close interrelationship between pain and psychiatric issues described in the literature.20
Providers’ acceptance of pharmacologic and nonpharmacologic treatment modalities supported a comprehensive, multidisciplinary, and biopsychosocial approach to effective analgesic management. During this pilot, the most common pharmacy medication recommendations, namely, discontinuation of inappropriate opioids (eg, IV hydromorphone in patients who are controlled on and/or able to tolerate oral medications) and dose titration of adjuvant medications (eg, anticonvulsants for neuropathic pain), revealed that the IPPCS provided needed expertise and alternatives for complex pain patients. The IPPCS was well received, as inpatient providers accepted and implemented a large proportion of pharmacist recommendations. Despite risks of bias with a nonvalidated questionnaire, providers offered positive feedback. In the future, distributing satisfaction evaluations to patients also would provide more insight into how others perceived the IPPCS.
Limitations
Reasons for unaccepted recommendations included perceived limited effectiveness and/or feasibility of topical agents for acute pain, as providers seemed to favor systemic therapy for supposedly more immediate analgesia. Prescriber preference may explain why inpatient teams sometimes declined adjuvant therapy recommendations. However, the 2016 American Pain Society Guidelines on the Management of Postoperative Pain support a multimodal approach and confirm that adjuvants can reduce patients’ opioid requirements.21
Consulting teams did not execute some opioid recommendations, which may be due to various factors, including patient-related or provider-related factors in the inpatient vs outpatient setting. Lack of retrospective analysis for comparison of results pre- and post-IPPCS implementation also limited the outcomes. However, this project was piloted as a QI initiative after providers identified significant needs for inpatient pain management at the WPBVAMC. No retrospective analysis was undertaken, as this project analyzed only responses during the pilot program.
Other obstacles of the IPPCS included request appropriateness and triaging. The inpatient pain CPS deferred management of some consults to other disciplines (eg, gastroenterology) for more appropriate care. The IPPCS deferred certain cases of acute pancreatic pain or generalized abdominal pain for further workup to address patients’ underlying issues. The inpatient pain CPS relayed pertinent information regarding appropriate consults to inpatient teams. In the future, developing more specific inclusion/exclusion criteria and delivering provider education about proper IPPCS requests may resolve this issue.
Challenges with pain consults from inpatient psychiatry stemmed from patients’ skepticism and unwillingness to accept nonopioid/adjuvant therapies. Additionally, comorbid psychiatric disorders are often associated with SUDs and potentially opioid-related aberrant behavior. More than 40% of opioid-dependent individuals have comorbid psychiatric disorders, especially depression, anxiety, and bipolar disorder.22 Poorly-managed pain also drives SUD, as 80% of these patients illegally obtain prescription opioids. Thus, undertreatment of pain may push individuals to secure pain medications from illegal/illicit sources to achieve analgesia.23 Following pain physician consultation, the IPPCS continued inpatient opioids for 12% (10/81) of patients with a SUD history, including 5 with postoperative pain or other acute processes, since patients were kept in a monitored health care environment. The remaining included 4 with malignant pain and 1 with end-of-life pain. Overall, the IPPCS recommended that inpatient teams discharge these patients on as little opioids as possible, as well as to make referrals to substance abuse programs when necessary. Effective pain management of patients with aberrant behavior requires a comprehensive interdisciplinary team approach. To mitigate risk, effectively treat pain, and maintain patient safety, clinicians must recognize biologic, chemical, social, and psychiatric aspects of substance abuse.21
Another limitation during this pilot was an inability to promptly assess the impact of recommendations, given limited opportunities to reevaluate patients. In the future, more dedicated time for the inpatient pain CPSs to respond to consults may allow for better follow-up rather than initial consults only. Providers sometimes discharged patients within 24 hours of submitting consults as well, which left no time for the inpatient pain CPS consultation. However, the IPPCS forwarded appropriate requests to pain CPS e-consult services for chart review recommendations. Encouraging providers to submit consults earlier in patients’ hospital admissions may help reduce the number of incomplete IPPCS requests. Although expanding service hours would require more dedicated CPS staffing resources, it is another option for quicker consult completion and prompt follow-up.
Future Directions
Future efforts to expand this project include ensuring patient safety through judicious opioid use. Smooth transitions of care will particularly help to improve the quality of pain management. Current WPBVAMC policies stated that the primary care provider (PCP) alone must agree to continue prescribing outpatient analgesic medications, including opioids, prescribed from the OCPC once patients return to Primary Care. Continued provider education would ideally promote efficient utilization of the IPPCS and OCPC.
The pain pharmacy SOAR note template also could undergo additional edits/revisions, including the addition of opioid overdose risk assessments. For improved documentation and standardization, the template could autopopulate patient-specific information when the inpatient pain CPS chooses the designated note title. The IPPCS also hoped to streamline the CPRS consult link for more convenience and ease of use. Ultimately, the IPPCS wished to provide ongoing provider education, inpatient opioid therapy, and other topics upon request.
Conclusion
The IPPCS received positive provider feedback and collected 100 consults (averaging 4 per week) during the 6-month pilot QI project. Most consults were for acute or chronic pain and requested nonopioid/adjuvant recommendations. The new service intended to fulfill unmet needs at the WPBVAMC by expanding the facility’s current pain programs. Prescribers reported a high level of satisfaction and a willingness to not only refer other clinicians to the program, but also continue using the consult. Providers unanimously agreed that the pain CPS provided reasonable, evidence-based recommendations. This project demonstrated that the IPPCS can aid in meeting new demands amid the challenging landscape of pain practice.
1. D’Arcy Y. Treating acute pain in the hospitalized patient. Nurse Pract. 2012;37(8):22-30.
2. Marks AD, Rodgers PE. Diagnosis and management of acute pain in the hospitalized patient. Am J Med. 2014;3(3):e396-e408.
3. Paice JA, Von Roenn JH. Under- or overtreatment of pain in the patient with cancer: how to achieve proper balance. J Clin Oncol. 2014;32(16):1721-1726.
4. Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573-1581.
5. Palomano RC, Rathmell JP, Krenzischek DA, Dunwoody CJ. Emerging trends and new approaches to acute pain management. J Perianesth Nurs. 2008;23(suppl 1):S43-S53.
6. U.S. Department of Health & Human Services, Office of the Surgeon General. Facing addiction in America: the surgeon general’s report on alcohol, drugs, and health, executive summary. https://addiction.surgeongeneral.gov/executive-summary.pdf. Published November 2016. Accessed November 1, 2017.
7. Bagian JP, Cohen M, Barnsteiner JH, et al. Safe use of opioids in hospitals. Sentinel Event Alert. 2012;49:1-5.
8. Atkinson TJ, Gulum AH, Forkum WG. The future of pain pharmacy: directed by need. Integrated Pharm Res Pract. 2016;2016(5):33-42.
9. Lothian ST, Fotis MA, Von Gutten CF, et al. Cancer pain management through a pharmacist-based analgesic dosing service. Am J Health Syst Pharm. 1999;56:1119-1125.
10. Lynn MA. Pharmacist interventions in pain management. Am J Health Syst Pharm. 2004;61(14):1487-1489.
11. Strickland JM, Huskey A, Brushwood DB. Pharmacist-physician collaboration in pain management practice. J Opioid Manag. 2007;3(6):295-301.
12. Fan T and Elgourt T. Pain management pharmacy service in a community hospital. Am J Health Syst Pharm. 2008;65(16):1560-1565.
13. Andrews LB, Bridgeman MB, Dalal KS, et al. Implementation of a pharmacist-directed pain management consultation service for hospitalised adults with a history of substance abuse. Int J Clin Pract. 2013;67(12):1342-1349.
14. Poirier RH, Brown CS, Garcia YT, Gann NY, Sandoval RA, McNulty JR. Implementation of a pharmacist directed pain management service in the inpatient setting. http://www.ashpadvantage.com/bestpractices/2014_papers/Kaweah-Delta.htm. Published 2014. Accessed November 1, 2017.
15. Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nded. San Francisco, CA: Jossey-Bass; 2009.
16. Nahin, RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254.
17. Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the opioid risk tool. Pain Med. 2005;6(6):432-442.
18. Nazario M. Opioid therapy risk management: the VA opioid safety and naloxone distribution initiatives. http://jfpsmeeting.pharmacist.com/sites/default/files/slides/Opioid%20Therapy%20Risk%20Management.pdf. Published October 15, 2015. Accessed November 1, 2017.
19. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain – United States, 2016. MMWR Rep. 2016;65(1):1-49.
20. Outcalt SD, Kroenke K, Krebs EE, et al. Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. J Behav Med. 2015;38:535.
21. Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-157.
22. NIDA/SAMHSA Blending Initiative. https://www.drugabuse.gov/nidasamhsa-blending-initiative. Updated November 2015. Accessed November 1, 2017.
23. Alford DP, German JS, Samet JH, Cheng DM, Lloyd-Travaglini CA, Saitz R. Primary care patients with drug use report chronic pain and self-medicate with alcohol and other drugs. J Gen Intern Med. 2016;31(5):486-491.
1. D’Arcy Y. Treating acute pain in the hospitalized patient. Nurse Pract. 2012;37(8):22-30.
2. Marks AD, Rodgers PE. Diagnosis and management of acute pain in the hospitalized patient. Am J Med. 2014;3(3):e396-e408.
3. Paice JA, Von Roenn JH. Under- or overtreatment of pain in the patient with cancer: how to achieve proper balance. J Clin Oncol. 2014;32(16):1721-1726.
4. Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573-1581.
5. Palomano RC, Rathmell JP, Krenzischek DA, Dunwoody CJ. Emerging trends and new approaches to acute pain management. J Perianesth Nurs. 2008;23(suppl 1):S43-S53.
6. U.S. Department of Health & Human Services, Office of the Surgeon General. Facing addiction in America: the surgeon general’s report on alcohol, drugs, and health, executive summary. https://addiction.surgeongeneral.gov/executive-summary.pdf. Published November 2016. Accessed November 1, 2017.
7. Bagian JP, Cohen M, Barnsteiner JH, et al. Safe use of opioids in hospitals. Sentinel Event Alert. 2012;49:1-5.
8. Atkinson TJ, Gulum AH, Forkum WG. The future of pain pharmacy: directed by need. Integrated Pharm Res Pract. 2016;2016(5):33-42.
9. Lothian ST, Fotis MA, Von Gutten CF, et al. Cancer pain management through a pharmacist-based analgesic dosing service. Am J Health Syst Pharm. 1999;56:1119-1125.
10. Lynn MA. Pharmacist interventions in pain management. Am J Health Syst Pharm. 2004;61(14):1487-1489.
11. Strickland JM, Huskey A, Brushwood DB. Pharmacist-physician collaboration in pain management practice. J Opioid Manag. 2007;3(6):295-301.
12. Fan T and Elgourt T. Pain management pharmacy service in a community hospital. Am J Health Syst Pharm. 2008;65(16):1560-1565.
13. Andrews LB, Bridgeman MB, Dalal KS, et al. Implementation of a pharmacist-directed pain management consultation service for hospitalised adults with a history of substance abuse. Int J Clin Pract. 2013;67(12):1342-1349.
14. Poirier RH, Brown CS, Garcia YT, Gann NY, Sandoval RA, McNulty JR. Implementation of a pharmacist directed pain management service in the inpatient setting. http://www.ashpadvantage.com/bestpractices/2014_papers/Kaweah-Delta.htm. Published 2014. Accessed November 1, 2017.
15. Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nded. San Francisco, CA: Jossey-Bass; 2009.
16. Nahin, RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254.
17. Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the opioid risk tool. Pain Med. 2005;6(6):432-442.
18. Nazario M. Opioid therapy risk management: the VA opioid safety and naloxone distribution initiatives. http://jfpsmeeting.pharmacist.com/sites/default/files/slides/Opioid%20Therapy%20Risk%20Management.pdf. Published October 15, 2015. Accessed November 1, 2017.
19. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain – United States, 2016. MMWR Rep. 2016;65(1):1-49.
20. Outcalt SD, Kroenke K, Krebs EE, et al. Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. J Behav Med. 2015;38:535.
21. Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-157.
22. NIDA/SAMHSA Blending Initiative. https://www.drugabuse.gov/nidasamhsa-blending-initiative. Updated November 2015. Accessed November 1, 2017.
23. Alford DP, German JS, Samet JH, Cheng DM, Lloyd-Travaglini CA, Saitz R. Primary care patients with drug use report chronic pain and self-medicate with alcohol and other drugs. J Gen Intern Med. 2016;31(5):486-491.
Opioid-Induced Androgen Deficiency in Veterans With Chronic Nonmalignant Pain
According to the CDC, the medical use of opioid painkillers has increased at least 10-fold during the past 20 years, “because of a movement toward more aggressive management of pain.”1 Although opioid therapy is generally considered effective for the treatment of pain, long-term use (both orally and intrathecally) is associated with adverse effects (AEs) such as constipation, fatigue, nausea, sleep disturbances, depression, sexual dysfunction, and hypogonadism.2,3Opioid-induced androgen deficiency (OPIAD), as defined by Smith and Elliot, is a clinical syndrome characterized by inappropriately low concentrations of gonadotropins (specifically, follicle-stimulating hormone [FSH] and luteinizing hormone [LH]), which leads to inadequate production of sex hormones, including estradiol and testosterone.4
Related: Testosterone Replacement Therapy: Playing Catch-up With Patients
The mechanism behind this phenomenon is initiated by either endogenous or exogenous opioids acting on opioid receptors in the hypothalamus, which causes a decrease in the release of gonadotropin- releasing hormone (GnRH). This decrease in GnRH causes a reduction in the release of LH and FSH from the pituitary gland as well as testosterone or estradiol from the gonads.4,5 Various guidelines report different cutoffs for the lower limit of normal total testosterone: The Endocrine Society recommends 300 ng/dL, the American Association of Clinical Endocrinologists suggests 200 ng/dL, and various other organizations suggest 230 ng/dL.6-8 Hypotestosteronism can result in patients presenting with a broad spectrum of clinical symptoms, including reduced libido, erectile dysfunction (ED), fatigue, hot flashes, depression, anemia, decreased muscle mass, weight gain, and osteopenia or osteoporosis.4 Women with low testosterone levels can experience irregular menstrual periods, oligomenorrhea, or amenorrhea.9 Opioid-induced androgen deficiency often goes unrecognized and untreated. The reported prevalence of opioid-induced hypogonadism ranges from 21% to 86%.4,9 Given the growing number of patients on chronic opioid therapy, OPIAD warrants further investigation to identify the prevalence in the veteran population to appropriately monitor and manage this deficiency.
The objective of this retrospective review was to identify the presence of secondary hypogonadism in chronic opioid users among a cohort of veterans receiving chronic opioids for nonmalignant pain. In addition to identifying the presence of secondary hypogonadism, the relationship between testosterone concentrations and total daily morphine equivalent doses (MEDs) was reviewed. These data along with the new information recently published on testosterone replacement therapy (TRT) and cardiovascular (CV) risk were then used to evaluate current practices at the West Palm Beach VAMC for OPIAD monitoring and management and to modify and update the local Criteria for Use (CFU) for TRT.
Methods
Patient data from the West Palm Beach VAMC in Florida from January 2013 to December 2013 were reviewed to identify patients who had a total testosterone (TT) level measured. All patient appointments for evaluation and treatment by the clinical pharmacy specialist in pain management were reviewed for data collection. This retrospective review was approved by the scientific advisory committee as part of the facility’s ongoing performance improvement efforts as defined by VHA Handbook 1058.05 and did not require written patient consent.10
Several distinct TT level data were collected. The descriptive data included patient age; gender; type of treated pain; testosterone level(s) drawn, including TT level before opioid therapy, TT level before/during/after TRT, and current total testosterone level; total daily MED of opioid therapy; duration of chronic opioid therapy; symptoms of exhibited hypogonadism; TRT formulation, dose, and duration; TRT prescriber; symptom change (if any); and laboratory tests ordered for TRT monitoring (lipid profile, liver profile, complete blood count, LH/FSH, and prostate specific antigen [PSA] panel).5,11,12
Related: Combination Treatment Relieves Opioid-Induced Constipation
Daily MED of opioid therapy was calculated using the VA/DoD opioid conversion table for patients on oxycodone, hydromorphone, or hydrocodone.13 For those on the fentanyl patch or methadone, conversion factors of 1:2 (fentanyl [µg/h]:morphine [mg/d]) and 1:3 (methadone:morphine) were used to convert to the MED.14 For patients on the buprenorphine patch, the package insert was used to convert to the corresponding MED.15 Combination therapies used the applicable conversions to calculate the total daily MED.
Once the data were collected, descriptive statistics were used to analyze the data. In addition, 4 graphs were generated to review potential relationships. The correlation coefficient was calculated using the Alcula Online Statistics Calculator (http://www.alcula.com; Correlation Coefficient Calculator).
Results
A total of 316 unique veteran patients were seen by the clinical pharmacy specialist in pain management from January 1, 2013, through December 31, 2013. Of these, 73 patients (23.1%) had at least 1 TT level drawn in 2013. Three patients with testosterone levels drawn (4.1%) were excluded from the data analysis for the following reasons: 1 patient did not have testosterone levels on file before receiving testosterone replacement from a non-VA source, 1 patient received opioids from a non-VA source (MED and duration of opioid therapy could not be calculated), and 1 patient inconsistently received opioids and MED used at the time of testosterone level draw. Per the local TRT CFU, a TT level > 350 ng/dL does not require treatment, whereas levels < 230 ng/dL (with symptoms) may require TRT, and < 200 ng/dL should be treated as hypogonadal (interpretation based on local laboratory’s reference range for TT).16 Of the 70 patients included in the analysis, 34 (48.6%) had a TT level < 230 ng/dL and would be considered eligible for TRT if they presented with symptoms of low testosterone. Of these 34 patients with a low testosterone level, 28 (40%) were being treated or had been treated with TRT (Figure 1).
The average age of the male patients with a testosterone level drawn was 58.3 years, which was not significantly different from the calculated median age of 60 years. No female patients had a testosterone level drawn. On average, the TT level was normal before starting opioids (reference range per local laboratory: 175-781 ng/dL). Once opioids were initiated, patients were treated for an average duration of 52.5 months (calculated through December 2013) with an average daily dose of 126.8 MED (Table). Fifty of the 70 patients (71.4%) with testosterone levels drawn in 2013 received TRT. The most common symptoms reported by patients related to low testosterone included ED, decreased libido, depression, chronic fatigue, generalized weakness, and hot flashes or night sweats.
The average TT level prior to TRT was 145.3, and the average testosterone level after initiation of or during treatment with TRT was 292.4, which is within the normal TT level range. Most patients receiving TRT were treated with testosterone cypionate injections, and this was also the formulation used for the longest periods, likely due to the local CFU. In addition to testosterone cypionate injections, patients were also treated with testosterone enanthate injections, testosterone patches, and testosterone gel.
Figure 1 compares current testosterone level and testosterone level before TRT with total daily MEDs. Figure 2 compares current testosterone level and testosterone level before TRT with length of opioid therapy. The 2 figures use data from all patients included in the analysis and indicate a potential inverse relationship between the total daily MED and duration of therapy with the testosterone level, although none of the calculated correlation coefficients indicate that a strong relationship was present.
Figures 3 and 4 include data only for patients who had both a testosterone level collected before opioids (baseline testosterone level) and a current testosterone level. Figure 3 trends the data using total daily MED, and Figure 4 uses the duration of opioid therapy. The correlation for Figure 4 is slightly stronger; the strongest negative correlations were identified between total daily MED and testosterone level before opioid therapy (r = -0.273) and duration of opioid therapy and testosterone level prior to opioid therapy (r = -0.396). The trends indicate that most patients had a normal TT level before opioid treatment and that patients treated with higher MEDs and for longer durations of time were more likely to have lower total testosterone levels.
Discussion
Low testosterone levels can adversely affect patients’ quality of life (QOL) and add to patients’ medication burden with the initiation of TRT. Given new data analyzing the potential effects of TRT on CV event risk, the use of TRT should be carefully considered, as it may carry significant risks and may not be suitable for all patients.
In November 2013, a study was published regarding TRT and increased CV risk.17 This was a retrospective cohort study of men with low testosterone levels (< 300 ng/dL) who had undergone coronary angiography in the VA system between 2005 and 2011 (average age in testosterone group was 60.6 years). The results were significant for an absolute rate of events (all-cause mortality, myocardial infarction [MI], and ischemic stroke) of 19.9% in the no testosterone group and 25.7% in the TRT group, an absolute risk difference of 5.8% at 3 years after coronary angiography. Kaplan-Meier survival curves demonstrated that testosterone use was associated with increased risk of death, MI, and stroke. This result was unchanged when adjusted for the presence of coronary artery disease (CAD). In addition, no significant difference was found between the groups in terms of systolic blood pressure, low- density lipoprotein cholesterol level, or in the use of beta-blocker and statin medications. What is important to note is that in this cohort, 20% had a prior history of MI and heart failure, and more than 50% had confirmed obstructive CAD on angiography. In addition, as this was an observational study, confounding or bias may exist, and given the study population, generalizability may be limited to a veteran population.
Related: A Multidisciplinary Chronic Pain Management Clinic in an Indian Health Service Facility
Another retrospective cohort study assessed the risk of acute nonfatal MI following an initial TRT prescription in a large health care database (average age based on TRT prescription was 54.4 years).18 In men aged ≥ 65 years, a 2-fold increase in the risk of MI in the immediate 90 days after filling an initial TRT prescription declined to baseline after 91 to 180 days among those who did not refill their prescription. Younger men with a history of heart disease had a 2- to 3-fold increased risk of MI in the 90 days following initial TRT prescription. No excess risk was observed in the younger men without such a history. Again, this study has its limitations related to the retrospective design and use of a health care database as opposed to a randomized controlled trial.
In February 2014, a VA National Pharmacy Benefits Management (PBM) bulletin addressed 2 recent studies that had identified a possible risk of increased CV events in men receiving TRT. The bulletin noted that these studies had prompted the FDA to reassess the CV safety of TRT.19 The TRT CFU was updated by VISN 8 to ensure that the patients receive appropriate treatment and are monitored accordingly.
One of the major changes to the CFU was defining the reference ranges for TRT (interpretation based on a local laboratory’s reference range for total testosterone): serum TT < 200 ng/dL be “treated as hypogonadal, those with TT > 400 ng/dL be considered normal and those with TT 200-400 ng/dL be treated based on their clinical presentation if symptomatic; TT levels > 350 ng/dL do not require treatment, and levels below 230 ng/dL (with symptoms) may require testosterone replacement therapy.”16 Other important updates included revision of the exclusion criteria as well as highlighting special considerations related to TRT, including the use of free testosterone levels rather than TT levels in patients with suspected protein-binding issues, role in fertility treatments, limited use in patients on spironolactone therapy (due to spironolactone’s anti-androgen effects), and potential association with mood and behavior.16
As chronic opioid therapy is associated with OPIAD, the renewed interest in TRT and its potential AEs provides yet another reason to reconsider opioid therapy. This is especially valid when opioids are the potential cause of hypogonadism and the reaction is treating the AEs of opioids (as opposed to considering elimination of the causative agent) with a therapy that can potentially increase the risk for CV events so that opioids can be continued. Outside the potential CV risk with TRT, opioids carry the innate risk for substance abuse and addiction.
The Opioid Safety Initiative Requirements was released as a memorandum in April 2014 and is the VHA’s effort to “reduce harm from unsafe medications and/or excessive doses while adequately controlling pain in Veterans.”20 Although it does not discuss the risk of OPIAD, it does highlight the need to identify and mitigate high-risk patients as well as high-risk opioid regimens. All these factors, including the possibility of hypogonadism, should be considered before starting opioid therapy and at the time of opioid renewal, as it is known that opioid therapy is not without risks.
At the West Palm Beach VAMC, the primary care providers (PCPs) are responsible for the management of TRT, including the workup, renewal, and monitoring. The Chronic Nonmalignant Pain Management Clinic (CNMPMC) orders testosterone levels on patients who report symptoms of low testosterone, such as hot flashes, depression, and low energy level and refers them to their PCP as indicated. The authors believe that this is most appropriate for a number of reasons: (1) the CNMPMC is a consult service, and patients are not followed indefinitely; (2) patients should be fully evaluated for appropriateness of TRT (including assessment of CV risk) before starting therapy; and (3) the necessary monitoring parameters (laboratory testing, digital rectal exam, and osteoporosis screening) are not typically within the VA pain clinic provider’s scope of practice or expertise. A consideration for future practice would be to incorporate the use of a standardized questionnaire for OPIAD monitoring in patients receiving ≥ 100 mg of morphine daily (eg, the Aging Males’ Symptoms scale).21 It should, however, be at the forefront of the pain specialist’s and PCP’s minds that all patients on chronic opioid therapy or considering chronic opioid therapy should be counseled on the risk for OPIAD. If OPIAD is identified, the patient should be carefully considered for an opioid dose reduction as an initial management strategy.
Limitations
A limitation of this review is the lack of consistency or adequacy of serum testosterone sampling, noting that valid testosterone levels need to be drawn in the morning and not obtained during a time of acute illness. In addition, testosterone levels need to be drawn at an appropriate interval while on TRT (eg, at the midpoint between testosterone injections).16 Although the time of the sample collection is documented in the Computerized Patient Record System (CPRS), it is unknown whether the patient was acutely ill on the day of the sampling unless a progress note is entered, and it is difficult to determine whether the level timing was accurate based on the testosterone replacement formulation. Another limitation is that the average decline in serum testosterone levels with aging in men is 1% to 2% per year. A significant fraction of older men have levels below the lower limit of the normal range for healthy young men, so in older men it can be more difficult to determine whether low testosterone is related to chronic opioid use or to older age.5,16
As this was a retrospective review, additional limitations included the inability to measure subclinical OPIAD, and the data collection related to symptoms of hypogonadism was restricted by documentation in the CPRS progress notes. The lack of data for females does not contribute to the literature on OPIAD in women. Finally, as the total daily MED does not distinguish between short-acting and long-acting opioid therapy, no differences between the impacts of short-acting vs long- acting opioid therapy on risk for hypogonadism can be inferred. There is evidence to suggest that long-acting opioids are associated with a significantly higher risk for OPIAD compared with short-acting opioids, although the mechanism behind this is not well established.22,23
Conclusions
The average age of the patients on chronic opioid therapy with a testosterone level drawn in this cohort was 58.3 years, which is younger than originally anticipated. The median age of 60 years is not significantly different from the average age, indicating that outliers did not impact this calculation. On average, the TT level was normal before starting opioids. Once opioids were started, patients were treated for an average duration of 52.5 months with an average daily dose of 126.8 mg MED. In this veteran cohort, 48.6% of patients met the criteria for TRT based on TT level alone, which is within the reported prevalence range of opioid-induced hypogonadism already published.4,9 These results are in line with the original hypothesis that chronic opioid use can adversely impact testosterone levels and can have a poor effect on a patient’s QOL due to symptoms of low testosterone. In addition to TRT, possible and suggested (but not proven) treatment options for OPIAD include discontinuation of opioid therapy, opioid rotation, or conversion to buprenorphine.21 The approach used should account for multiple patient-specific factors and should be individualized.
Based on the data, there is a trend toward lower testosterone levels in veterans treated with higher MED and for longer periods with chronic opioids. Given recent data that infer that TRT carries increased CV risk as well as the VHA’s Opioid Safety Initiative, it is imperative that providers closely evaluate the appropriateness of starting TRT and/or continuing chronic opioid therapy. All patients generally should have failed non- opioid management prior to opioid therapy for chronic nonmalignant pain, and this should be documented accordingly. It is also crucial to have the “opioid talk” with patients from time to time and discuss the risks vs benefits, the potential for addiction, overdose, dependence, tolerance, constipation, and OPIAD so patients can continue to be an active and informed participants in their care.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Unintentional drug poisoning in the United States, 2010. Atlanta, GA: Centers for Disease Control and Prevention Website. http://www.cdc.gov /HomeandRecreationalSafety/pdf/poison-issue-brief .pdf. Published July 2010. Accessed August 28, 2015.
2. American Academy of Family Physicians. Using opioids in the management of chronic pain patients: challenges and future options. University of Kentucky Medical Center Website. http://www .mc.uky.edu/equip-4-pcps/documents/CRx%20Literature/Opioids%20for%20chronic%20pain.pdf. Published 2010. Accessed August 28, 2015.
3. Duarte RV, Raphael JH, Labib M, Southall JL, Ashford RL. Prevalence and influence of diagnostic criteria in the assessment of hypogonadism in intrathecal opioid therapy patients. Pain Physician. 2013;16(1):9-14.
4. Smith HS, Elliott JA. Opioid-induced androgen deficiency (OPIAD). Pain Physician. 2012;15(suppl 3):ES145-ES156.
5. De Maddalena C, Bellini M, Berra M, Meriggiola MC, Aloisi AM. Opioid-induced hypogonadism: why and how to treat it. Pain Physician. 2012;15(suppl 3):ES111-ES118.
6. Bhasin S, Cunningham GR, Hayes FJ, et al; VM Endocrine Society Task Force. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536-2559.
7. Petak SM, Nankin HR, Spark RF, Swerdloff RS, Rodriguez-Rigau LJ; American Association of Clinical Endocrinologists. American Association of Clinical Endocrinologists Medical Guidelines for clinical practice for the evaluation and treatment of hypogonadism in adult male patients–2002 update. Endocr Pract. 2002;8(6):440-456.
8. Wang C, Nieschlag E, Swerdloff R, et al. Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. J Androl. 2009;30(1):1-9.
9. Reddy RG, Aung T, Karavitaki N, Wass JA. Opioid induced hypogonadism. BMJ. 2010;341:c4462.
10. U.S. Department of Veterans Affairs, Veterans Health Administration. VHA Handbook 1058.05: VHA operations activities that may constitute research. U.S. Department of Veterans Affairs Website. http://www.va.gov/vhapublications /ViewPublication.asp?pub_ID=2456. Published October 28, 2011. Accessed August 28, 2015.
11. AndroGel [package insert]. North Chicago, IL: AbbVie Inc; 2013.
12. Axiron [package insert]. Indianapolis, IL: Lilly USA, LLC; 2011.
13. U.S. Department of Veterans Affairs. Opioid therapy for chronic pain pocket guide. U.S. Department of Veterans Affairs. http://www.healthquality .va.gov/guidelines/pain/cot/opioidpocketguide23may2013v1.pdf. Published May 2013 Accessed August 28, 2015.
14. McPherson ML. Demystifying Opioid Conversion Calculations: A Guide for Effective Dosing. Bethesda, MD: American Society of Health-System Pharmacists; 2009.
15. Butrans [package insert]. Stamford, CT: Purdue Pharma LP; 2014.
16. Testosterone Replacement Therapy Criteria for Use. VISN 8: VISN Pharmacist Executives, Veterans Health Administration, Department of Veterans Affairs; 2014. [Internal document.]
17. Vigen R, O’Donnell CI, Barón AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013;310(17):1829-1836.
18. Finkle WD, Greenland S, Ridgeway GK, et al. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One. 2014;9(1):e85805.
19. U.S. Department of Veterans Affairs. Testosterone products and cardiovascular safety. U.S. Department of Veterans Affairs Website. http://www.pbm .va.gov/PBM/vacenterformedicationsafety /nationalpbmbulletin/Testosterone_Products_and _Cardiovascular_Safety_NATIONAL_PBM _BULLETIN_02.pdf. Published February 7, 2014. Accessed August 28, 2015.
20. U.S. Department of Veterans Affairs Veterans Health Administration (VHA) Pharmacy Benefits Management Services (PBM), Medical Advisory Panel (MAP) and Center for Medication Safety (VA MEDSAFE). Memorandum: Opioid Safety Initiative Requirements. U.S. Department of Veterans Affairs Website. http://www.veterans.senate.gov/imo /media/doc/VA%20Testimony%20-%20April%2030%20SVAC%20Overmedication%20hearing.pdf. Published April 30, 2014. Accessed August 28, 2015.
21. Brennan MJ. The effect of opioid therapy on endocrine function. Am J Med. 2013;126(3)(suppl 1):S12-S18.
22. Rubinstein AL, Carpenter DM, Minkoff JR. Hypogonadism in men with chronic pain linked to the use of long-acting rather than short-acting opioids. Clin J Pain. 2013;29(10):840-845.
23. Rubinstein A, Carpenter DM. Elucidating risk factors for androgen deficiency associated with daily opioid use. Am J Med. 2014;127(12):1195-1201.
According to the CDC, the medical use of opioid painkillers has increased at least 10-fold during the past 20 years, “because of a movement toward more aggressive management of pain.”1 Although opioid therapy is generally considered effective for the treatment of pain, long-term use (both orally and intrathecally) is associated with adverse effects (AEs) such as constipation, fatigue, nausea, sleep disturbances, depression, sexual dysfunction, and hypogonadism.2,3Opioid-induced androgen deficiency (OPIAD), as defined by Smith and Elliot, is a clinical syndrome characterized by inappropriately low concentrations of gonadotropins (specifically, follicle-stimulating hormone [FSH] and luteinizing hormone [LH]), which leads to inadequate production of sex hormones, including estradiol and testosterone.4
Related: Testosterone Replacement Therapy: Playing Catch-up With Patients
The mechanism behind this phenomenon is initiated by either endogenous or exogenous opioids acting on opioid receptors in the hypothalamus, which causes a decrease in the release of gonadotropin- releasing hormone (GnRH). This decrease in GnRH causes a reduction in the release of LH and FSH from the pituitary gland as well as testosterone or estradiol from the gonads.4,5 Various guidelines report different cutoffs for the lower limit of normal total testosterone: The Endocrine Society recommends 300 ng/dL, the American Association of Clinical Endocrinologists suggests 200 ng/dL, and various other organizations suggest 230 ng/dL.6-8 Hypotestosteronism can result in patients presenting with a broad spectrum of clinical symptoms, including reduced libido, erectile dysfunction (ED), fatigue, hot flashes, depression, anemia, decreased muscle mass, weight gain, and osteopenia or osteoporosis.4 Women with low testosterone levels can experience irregular menstrual periods, oligomenorrhea, or amenorrhea.9 Opioid-induced androgen deficiency often goes unrecognized and untreated. The reported prevalence of opioid-induced hypogonadism ranges from 21% to 86%.4,9 Given the growing number of patients on chronic opioid therapy, OPIAD warrants further investigation to identify the prevalence in the veteran population to appropriately monitor and manage this deficiency.
The objective of this retrospective review was to identify the presence of secondary hypogonadism in chronic opioid users among a cohort of veterans receiving chronic opioids for nonmalignant pain. In addition to identifying the presence of secondary hypogonadism, the relationship between testosterone concentrations and total daily morphine equivalent doses (MEDs) was reviewed. These data along with the new information recently published on testosterone replacement therapy (TRT) and cardiovascular (CV) risk were then used to evaluate current practices at the West Palm Beach VAMC for OPIAD monitoring and management and to modify and update the local Criteria for Use (CFU) for TRT.
Methods
Patient data from the West Palm Beach VAMC in Florida from January 2013 to December 2013 were reviewed to identify patients who had a total testosterone (TT) level measured. All patient appointments for evaluation and treatment by the clinical pharmacy specialist in pain management were reviewed for data collection. This retrospective review was approved by the scientific advisory committee as part of the facility’s ongoing performance improvement efforts as defined by VHA Handbook 1058.05 and did not require written patient consent.10
Several distinct TT level data were collected. The descriptive data included patient age; gender; type of treated pain; testosterone level(s) drawn, including TT level before opioid therapy, TT level before/during/after TRT, and current total testosterone level; total daily MED of opioid therapy; duration of chronic opioid therapy; symptoms of exhibited hypogonadism; TRT formulation, dose, and duration; TRT prescriber; symptom change (if any); and laboratory tests ordered for TRT monitoring (lipid profile, liver profile, complete blood count, LH/FSH, and prostate specific antigen [PSA] panel).5,11,12
Related: Combination Treatment Relieves Opioid-Induced Constipation
Daily MED of opioid therapy was calculated using the VA/DoD opioid conversion table for patients on oxycodone, hydromorphone, or hydrocodone.13 For those on the fentanyl patch or methadone, conversion factors of 1:2 (fentanyl [µg/h]:morphine [mg/d]) and 1:3 (methadone:morphine) were used to convert to the MED.14 For patients on the buprenorphine patch, the package insert was used to convert to the corresponding MED.15 Combination therapies used the applicable conversions to calculate the total daily MED.
Once the data were collected, descriptive statistics were used to analyze the data. In addition, 4 graphs were generated to review potential relationships. The correlation coefficient was calculated using the Alcula Online Statistics Calculator (http://www.alcula.com; Correlation Coefficient Calculator).
Results
A total of 316 unique veteran patients were seen by the clinical pharmacy specialist in pain management from January 1, 2013, through December 31, 2013. Of these, 73 patients (23.1%) had at least 1 TT level drawn in 2013. Three patients with testosterone levels drawn (4.1%) were excluded from the data analysis for the following reasons: 1 patient did not have testosterone levels on file before receiving testosterone replacement from a non-VA source, 1 patient received opioids from a non-VA source (MED and duration of opioid therapy could not be calculated), and 1 patient inconsistently received opioids and MED used at the time of testosterone level draw. Per the local TRT CFU, a TT level > 350 ng/dL does not require treatment, whereas levels < 230 ng/dL (with symptoms) may require TRT, and < 200 ng/dL should be treated as hypogonadal (interpretation based on local laboratory’s reference range for TT).16 Of the 70 patients included in the analysis, 34 (48.6%) had a TT level < 230 ng/dL and would be considered eligible for TRT if they presented with symptoms of low testosterone. Of these 34 patients with a low testosterone level, 28 (40%) were being treated or had been treated with TRT (Figure 1).
The average age of the male patients with a testosterone level drawn was 58.3 years, which was not significantly different from the calculated median age of 60 years. No female patients had a testosterone level drawn. On average, the TT level was normal before starting opioids (reference range per local laboratory: 175-781 ng/dL). Once opioids were initiated, patients were treated for an average duration of 52.5 months (calculated through December 2013) with an average daily dose of 126.8 MED (Table). Fifty of the 70 patients (71.4%) with testosterone levels drawn in 2013 received TRT. The most common symptoms reported by patients related to low testosterone included ED, decreased libido, depression, chronic fatigue, generalized weakness, and hot flashes or night sweats.
The average TT level prior to TRT was 145.3, and the average testosterone level after initiation of or during treatment with TRT was 292.4, which is within the normal TT level range. Most patients receiving TRT were treated with testosterone cypionate injections, and this was also the formulation used for the longest periods, likely due to the local CFU. In addition to testosterone cypionate injections, patients were also treated with testosterone enanthate injections, testosterone patches, and testosterone gel.
Figure 1 compares current testosterone level and testosterone level before TRT with total daily MEDs. Figure 2 compares current testosterone level and testosterone level before TRT with length of opioid therapy. The 2 figures use data from all patients included in the analysis and indicate a potential inverse relationship between the total daily MED and duration of therapy with the testosterone level, although none of the calculated correlation coefficients indicate that a strong relationship was present.
Figures 3 and 4 include data only for patients who had both a testosterone level collected before opioids (baseline testosterone level) and a current testosterone level. Figure 3 trends the data using total daily MED, and Figure 4 uses the duration of opioid therapy. The correlation for Figure 4 is slightly stronger; the strongest negative correlations were identified between total daily MED and testosterone level before opioid therapy (r = -0.273) and duration of opioid therapy and testosterone level prior to opioid therapy (r = -0.396). The trends indicate that most patients had a normal TT level before opioid treatment and that patients treated with higher MEDs and for longer durations of time were more likely to have lower total testosterone levels.
Discussion
Low testosterone levels can adversely affect patients’ quality of life (QOL) and add to patients’ medication burden with the initiation of TRT. Given new data analyzing the potential effects of TRT on CV event risk, the use of TRT should be carefully considered, as it may carry significant risks and may not be suitable for all patients.
In November 2013, a study was published regarding TRT and increased CV risk.17 This was a retrospective cohort study of men with low testosterone levels (< 300 ng/dL) who had undergone coronary angiography in the VA system between 2005 and 2011 (average age in testosterone group was 60.6 years). The results were significant for an absolute rate of events (all-cause mortality, myocardial infarction [MI], and ischemic stroke) of 19.9% in the no testosterone group and 25.7% in the TRT group, an absolute risk difference of 5.8% at 3 years after coronary angiography. Kaplan-Meier survival curves demonstrated that testosterone use was associated with increased risk of death, MI, and stroke. This result was unchanged when adjusted for the presence of coronary artery disease (CAD). In addition, no significant difference was found between the groups in terms of systolic blood pressure, low- density lipoprotein cholesterol level, or in the use of beta-blocker and statin medications. What is important to note is that in this cohort, 20% had a prior history of MI and heart failure, and more than 50% had confirmed obstructive CAD on angiography. In addition, as this was an observational study, confounding or bias may exist, and given the study population, generalizability may be limited to a veteran population.
Related: A Multidisciplinary Chronic Pain Management Clinic in an Indian Health Service Facility
Another retrospective cohort study assessed the risk of acute nonfatal MI following an initial TRT prescription in a large health care database (average age based on TRT prescription was 54.4 years).18 In men aged ≥ 65 years, a 2-fold increase in the risk of MI in the immediate 90 days after filling an initial TRT prescription declined to baseline after 91 to 180 days among those who did not refill their prescription. Younger men with a history of heart disease had a 2- to 3-fold increased risk of MI in the 90 days following initial TRT prescription. No excess risk was observed in the younger men without such a history. Again, this study has its limitations related to the retrospective design and use of a health care database as opposed to a randomized controlled trial.
In February 2014, a VA National Pharmacy Benefits Management (PBM) bulletin addressed 2 recent studies that had identified a possible risk of increased CV events in men receiving TRT. The bulletin noted that these studies had prompted the FDA to reassess the CV safety of TRT.19 The TRT CFU was updated by VISN 8 to ensure that the patients receive appropriate treatment and are monitored accordingly.
One of the major changes to the CFU was defining the reference ranges for TRT (interpretation based on a local laboratory’s reference range for total testosterone): serum TT < 200 ng/dL be “treated as hypogonadal, those with TT > 400 ng/dL be considered normal and those with TT 200-400 ng/dL be treated based on their clinical presentation if symptomatic; TT levels > 350 ng/dL do not require treatment, and levels below 230 ng/dL (with symptoms) may require testosterone replacement therapy.”16 Other important updates included revision of the exclusion criteria as well as highlighting special considerations related to TRT, including the use of free testosterone levels rather than TT levels in patients with suspected protein-binding issues, role in fertility treatments, limited use in patients on spironolactone therapy (due to spironolactone’s anti-androgen effects), and potential association with mood and behavior.16
As chronic opioid therapy is associated with OPIAD, the renewed interest in TRT and its potential AEs provides yet another reason to reconsider opioid therapy. This is especially valid when opioids are the potential cause of hypogonadism and the reaction is treating the AEs of opioids (as opposed to considering elimination of the causative agent) with a therapy that can potentially increase the risk for CV events so that opioids can be continued. Outside the potential CV risk with TRT, opioids carry the innate risk for substance abuse and addiction.
The Opioid Safety Initiative Requirements was released as a memorandum in April 2014 and is the VHA’s effort to “reduce harm from unsafe medications and/or excessive doses while adequately controlling pain in Veterans.”20 Although it does not discuss the risk of OPIAD, it does highlight the need to identify and mitigate high-risk patients as well as high-risk opioid regimens. All these factors, including the possibility of hypogonadism, should be considered before starting opioid therapy and at the time of opioid renewal, as it is known that opioid therapy is not without risks.
At the West Palm Beach VAMC, the primary care providers (PCPs) are responsible for the management of TRT, including the workup, renewal, and monitoring. The Chronic Nonmalignant Pain Management Clinic (CNMPMC) orders testosterone levels on patients who report symptoms of low testosterone, such as hot flashes, depression, and low energy level and refers them to their PCP as indicated. The authors believe that this is most appropriate for a number of reasons: (1) the CNMPMC is a consult service, and patients are not followed indefinitely; (2) patients should be fully evaluated for appropriateness of TRT (including assessment of CV risk) before starting therapy; and (3) the necessary monitoring parameters (laboratory testing, digital rectal exam, and osteoporosis screening) are not typically within the VA pain clinic provider’s scope of practice or expertise. A consideration for future practice would be to incorporate the use of a standardized questionnaire for OPIAD monitoring in patients receiving ≥ 100 mg of morphine daily (eg, the Aging Males’ Symptoms scale).21 It should, however, be at the forefront of the pain specialist’s and PCP’s minds that all patients on chronic opioid therapy or considering chronic opioid therapy should be counseled on the risk for OPIAD. If OPIAD is identified, the patient should be carefully considered for an opioid dose reduction as an initial management strategy.
Limitations
A limitation of this review is the lack of consistency or adequacy of serum testosterone sampling, noting that valid testosterone levels need to be drawn in the morning and not obtained during a time of acute illness. In addition, testosterone levels need to be drawn at an appropriate interval while on TRT (eg, at the midpoint between testosterone injections).16 Although the time of the sample collection is documented in the Computerized Patient Record System (CPRS), it is unknown whether the patient was acutely ill on the day of the sampling unless a progress note is entered, and it is difficult to determine whether the level timing was accurate based on the testosterone replacement formulation. Another limitation is that the average decline in serum testosterone levels with aging in men is 1% to 2% per year. A significant fraction of older men have levels below the lower limit of the normal range for healthy young men, so in older men it can be more difficult to determine whether low testosterone is related to chronic opioid use or to older age.5,16
As this was a retrospective review, additional limitations included the inability to measure subclinical OPIAD, and the data collection related to symptoms of hypogonadism was restricted by documentation in the CPRS progress notes. The lack of data for females does not contribute to the literature on OPIAD in women. Finally, as the total daily MED does not distinguish between short-acting and long-acting opioid therapy, no differences between the impacts of short-acting vs long- acting opioid therapy on risk for hypogonadism can be inferred. There is evidence to suggest that long-acting opioids are associated with a significantly higher risk for OPIAD compared with short-acting opioids, although the mechanism behind this is not well established.22,23
Conclusions
The average age of the patients on chronic opioid therapy with a testosterone level drawn in this cohort was 58.3 years, which is younger than originally anticipated. The median age of 60 years is not significantly different from the average age, indicating that outliers did not impact this calculation. On average, the TT level was normal before starting opioids. Once opioids were started, patients were treated for an average duration of 52.5 months with an average daily dose of 126.8 mg MED. In this veteran cohort, 48.6% of patients met the criteria for TRT based on TT level alone, which is within the reported prevalence range of opioid-induced hypogonadism already published.4,9 These results are in line with the original hypothesis that chronic opioid use can adversely impact testosterone levels and can have a poor effect on a patient’s QOL due to symptoms of low testosterone. In addition to TRT, possible and suggested (but not proven) treatment options for OPIAD include discontinuation of opioid therapy, opioid rotation, or conversion to buprenorphine.21 The approach used should account for multiple patient-specific factors and should be individualized.
Based on the data, there is a trend toward lower testosterone levels in veterans treated with higher MED and for longer periods with chronic opioids. Given recent data that infer that TRT carries increased CV risk as well as the VHA’s Opioid Safety Initiative, it is imperative that providers closely evaluate the appropriateness of starting TRT and/or continuing chronic opioid therapy. All patients generally should have failed non- opioid management prior to opioid therapy for chronic nonmalignant pain, and this should be documented accordingly. It is also crucial to have the “opioid talk” with patients from time to time and discuss the risks vs benefits, the potential for addiction, overdose, dependence, tolerance, constipation, and OPIAD so patients can continue to be an active and informed participants in their care.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
According to the CDC, the medical use of opioid painkillers has increased at least 10-fold during the past 20 years, “because of a movement toward more aggressive management of pain.”1 Although opioid therapy is generally considered effective for the treatment of pain, long-term use (both orally and intrathecally) is associated with adverse effects (AEs) such as constipation, fatigue, nausea, sleep disturbances, depression, sexual dysfunction, and hypogonadism.2,3Opioid-induced androgen deficiency (OPIAD), as defined by Smith and Elliot, is a clinical syndrome characterized by inappropriately low concentrations of gonadotropins (specifically, follicle-stimulating hormone [FSH] and luteinizing hormone [LH]), which leads to inadequate production of sex hormones, including estradiol and testosterone.4
Related: Testosterone Replacement Therapy: Playing Catch-up With Patients
The mechanism behind this phenomenon is initiated by either endogenous or exogenous opioids acting on opioid receptors in the hypothalamus, which causes a decrease in the release of gonadotropin- releasing hormone (GnRH). This decrease in GnRH causes a reduction in the release of LH and FSH from the pituitary gland as well as testosterone or estradiol from the gonads.4,5 Various guidelines report different cutoffs for the lower limit of normal total testosterone: The Endocrine Society recommends 300 ng/dL, the American Association of Clinical Endocrinologists suggests 200 ng/dL, and various other organizations suggest 230 ng/dL.6-8 Hypotestosteronism can result in patients presenting with a broad spectrum of clinical symptoms, including reduced libido, erectile dysfunction (ED), fatigue, hot flashes, depression, anemia, decreased muscle mass, weight gain, and osteopenia or osteoporosis.4 Women with low testosterone levels can experience irregular menstrual periods, oligomenorrhea, or amenorrhea.9 Opioid-induced androgen deficiency often goes unrecognized and untreated. The reported prevalence of opioid-induced hypogonadism ranges from 21% to 86%.4,9 Given the growing number of patients on chronic opioid therapy, OPIAD warrants further investigation to identify the prevalence in the veteran population to appropriately monitor and manage this deficiency.
The objective of this retrospective review was to identify the presence of secondary hypogonadism in chronic opioid users among a cohort of veterans receiving chronic opioids for nonmalignant pain. In addition to identifying the presence of secondary hypogonadism, the relationship between testosterone concentrations and total daily morphine equivalent doses (MEDs) was reviewed. These data along with the new information recently published on testosterone replacement therapy (TRT) and cardiovascular (CV) risk were then used to evaluate current practices at the West Palm Beach VAMC for OPIAD monitoring and management and to modify and update the local Criteria for Use (CFU) for TRT.
Methods
Patient data from the West Palm Beach VAMC in Florida from January 2013 to December 2013 were reviewed to identify patients who had a total testosterone (TT) level measured. All patient appointments for evaluation and treatment by the clinical pharmacy specialist in pain management were reviewed for data collection. This retrospective review was approved by the scientific advisory committee as part of the facility’s ongoing performance improvement efforts as defined by VHA Handbook 1058.05 and did not require written patient consent.10
Several distinct TT level data were collected. The descriptive data included patient age; gender; type of treated pain; testosterone level(s) drawn, including TT level before opioid therapy, TT level before/during/after TRT, and current total testosterone level; total daily MED of opioid therapy; duration of chronic opioid therapy; symptoms of exhibited hypogonadism; TRT formulation, dose, and duration; TRT prescriber; symptom change (if any); and laboratory tests ordered for TRT monitoring (lipid profile, liver profile, complete blood count, LH/FSH, and prostate specific antigen [PSA] panel).5,11,12
Related: Combination Treatment Relieves Opioid-Induced Constipation
Daily MED of opioid therapy was calculated using the VA/DoD opioid conversion table for patients on oxycodone, hydromorphone, or hydrocodone.13 For those on the fentanyl patch or methadone, conversion factors of 1:2 (fentanyl [µg/h]:morphine [mg/d]) and 1:3 (methadone:morphine) were used to convert to the MED.14 For patients on the buprenorphine patch, the package insert was used to convert to the corresponding MED.15 Combination therapies used the applicable conversions to calculate the total daily MED.
Once the data were collected, descriptive statistics were used to analyze the data. In addition, 4 graphs were generated to review potential relationships. The correlation coefficient was calculated using the Alcula Online Statistics Calculator (http://www.alcula.com; Correlation Coefficient Calculator).
Results
A total of 316 unique veteran patients were seen by the clinical pharmacy specialist in pain management from January 1, 2013, through December 31, 2013. Of these, 73 patients (23.1%) had at least 1 TT level drawn in 2013. Three patients with testosterone levels drawn (4.1%) were excluded from the data analysis for the following reasons: 1 patient did not have testosterone levels on file before receiving testosterone replacement from a non-VA source, 1 patient received opioids from a non-VA source (MED and duration of opioid therapy could not be calculated), and 1 patient inconsistently received opioids and MED used at the time of testosterone level draw. Per the local TRT CFU, a TT level > 350 ng/dL does not require treatment, whereas levels < 230 ng/dL (with symptoms) may require TRT, and < 200 ng/dL should be treated as hypogonadal (interpretation based on local laboratory’s reference range for TT).16 Of the 70 patients included in the analysis, 34 (48.6%) had a TT level < 230 ng/dL and would be considered eligible for TRT if they presented with symptoms of low testosterone. Of these 34 patients with a low testosterone level, 28 (40%) were being treated or had been treated with TRT (Figure 1).
The average age of the male patients with a testosterone level drawn was 58.3 years, which was not significantly different from the calculated median age of 60 years. No female patients had a testosterone level drawn. On average, the TT level was normal before starting opioids (reference range per local laboratory: 175-781 ng/dL). Once opioids were initiated, patients were treated for an average duration of 52.5 months (calculated through December 2013) with an average daily dose of 126.8 MED (Table). Fifty of the 70 patients (71.4%) with testosterone levels drawn in 2013 received TRT. The most common symptoms reported by patients related to low testosterone included ED, decreased libido, depression, chronic fatigue, generalized weakness, and hot flashes or night sweats.
The average TT level prior to TRT was 145.3, and the average testosterone level after initiation of or during treatment with TRT was 292.4, which is within the normal TT level range. Most patients receiving TRT were treated with testosterone cypionate injections, and this was also the formulation used for the longest periods, likely due to the local CFU. In addition to testosterone cypionate injections, patients were also treated with testosterone enanthate injections, testosterone patches, and testosterone gel.
Figure 1 compares current testosterone level and testosterone level before TRT with total daily MEDs. Figure 2 compares current testosterone level and testosterone level before TRT with length of opioid therapy. The 2 figures use data from all patients included in the analysis and indicate a potential inverse relationship between the total daily MED and duration of therapy with the testosterone level, although none of the calculated correlation coefficients indicate that a strong relationship was present.
Figures 3 and 4 include data only for patients who had both a testosterone level collected before opioids (baseline testosterone level) and a current testosterone level. Figure 3 trends the data using total daily MED, and Figure 4 uses the duration of opioid therapy. The correlation for Figure 4 is slightly stronger; the strongest negative correlations were identified between total daily MED and testosterone level before opioid therapy (r = -0.273) and duration of opioid therapy and testosterone level prior to opioid therapy (r = -0.396). The trends indicate that most patients had a normal TT level before opioid treatment and that patients treated with higher MEDs and for longer durations of time were more likely to have lower total testosterone levels.
Discussion
Low testosterone levels can adversely affect patients’ quality of life (QOL) and add to patients’ medication burden with the initiation of TRT. Given new data analyzing the potential effects of TRT on CV event risk, the use of TRT should be carefully considered, as it may carry significant risks and may not be suitable for all patients.
In November 2013, a study was published regarding TRT and increased CV risk.17 This was a retrospective cohort study of men with low testosterone levels (< 300 ng/dL) who had undergone coronary angiography in the VA system between 2005 and 2011 (average age in testosterone group was 60.6 years). The results were significant for an absolute rate of events (all-cause mortality, myocardial infarction [MI], and ischemic stroke) of 19.9% in the no testosterone group and 25.7% in the TRT group, an absolute risk difference of 5.8% at 3 years after coronary angiography. Kaplan-Meier survival curves demonstrated that testosterone use was associated with increased risk of death, MI, and stroke. This result was unchanged when adjusted for the presence of coronary artery disease (CAD). In addition, no significant difference was found between the groups in terms of systolic blood pressure, low- density lipoprotein cholesterol level, or in the use of beta-blocker and statin medications. What is important to note is that in this cohort, 20% had a prior history of MI and heart failure, and more than 50% had confirmed obstructive CAD on angiography. In addition, as this was an observational study, confounding or bias may exist, and given the study population, generalizability may be limited to a veteran population.
Related: A Multidisciplinary Chronic Pain Management Clinic in an Indian Health Service Facility
Another retrospective cohort study assessed the risk of acute nonfatal MI following an initial TRT prescription in a large health care database (average age based on TRT prescription was 54.4 years).18 In men aged ≥ 65 years, a 2-fold increase in the risk of MI in the immediate 90 days after filling an initial TRT prescription declined to baseline after 91 to 180 days among those who did not refill their prescription. Younger men with a history of heart disease had a 2- to 3-fold increased risk of MI in the 90 days following initial TRT prescription. No excess risk was observed in the younger men without such a history. Again, this study has its limitations related to the retrospective design and use of a health care database as opposed to a randomized controlled trial.
In February 2014, a VA National Pharmacy Benefits Management (PBM) bulletin addressed 2 recent studies that had identified a possible risk of increased CV events in men receiving TRT. The bulletin noted that these studies had prompted the FDA to reassess the CV safety of TRT.19 The TRT CFU was updated by VISN 8 to ensure that the patients receive appropriate treatment and are monitored accordingly.
One of the major changes to the CFU was defining the reference ranges for TRT (interpretation based on a local laboratory’s reference range for total testosterone): serum TT < 200 ng/dL be “treated as hypogonadal, those with TT > 400 ng/dL be considered normal and those with TT 200-400 ng/dL be treated based on their clinical presentation if symptomatic; TT levels > 350 ng/dL do not require treatment, and levels below 230 ng/dL (with symptoms) may require testosterone replacement therapy.”16 Other important updates included revision of the exclusion criteria as well as highlighting special considerations related to TRT, including the use of free testosterone levels rather than TT levels in patients with suspected protein-binding issues, role in fertility treatments, limited use in patients on spironolactone therapy (due to spironolactone’s anti-androgen effects), and potential association with mood and behavior.16
As chronic opioid therapy is associated with OPIAD, the renewed interest in TRT and its potential AEs provides yet another reason to reconsider opioid therapy. This is especially valid when opioids are the potential cause of hypogonadism and the reaction is treating the AEs of opioids (as opposed to considering elimination of the causative agent) with a therapy that can potentially increase the risk for CV events so that opioids can be continued. Outside the potential CV risk with TRT, opioids carry the innate risk for substance abuse and addiction.
The Opioid Safety Initiative Requirements was released as a memorandum in April 2014 and is the VHA’s effort to “reduce harm from unsafe medications and/or excessive doses while adequately controlling pain in Veterans.”20 Although it does not discuss the risk of OPIAD, it does highlight the need to identify and mitigate high-risk patients as well as high-risk opioid regimens. All these factors, including the possibility of hypogonadism, should be considered before starting opioid therapy and at the time of opioid renewal, as it is known that opioid therapy is not without risks.
At the West Palm Beach VAMC, the primary care providers (PCPs) are responsible for the management of TRT, including the workup, renewal, and monitoring. The Chronic Nonmalignant Pain Management Clinic (CNMPMC) orders testosterone levels on patients who report symptoms of low testosterone, such as hot flashes, depression, and low energy level and refers them to their PCP as indicated. The authors believe that this is most appropriate for a number of reasons: (1) the CNMPMC is a consult service, and patients are not followed indefinitely; (2) patients should be fully evaluated for appropriateness of TRT (including assessment of CV risk) before starting therapy; and (3) the necessary monitoring parameters (laboratory testing, digital rectal exam, and osteoporosis screening) are not typically within the VA pain clinic provider’s scope of practice or expertise. A consideration for future practice would be to incorporate the use of a standardized questionnaire for OPIAD monitoring in patients receiving ≥ 100 mg of morphine daily (eg, the Aging Males’ Symptoms scale).21 It should, however, be at the forefront of the pain specialist’s and PCP’s minds that all patients on chronic opioid therapy or considering chronic opioid therapy should be counseled on the risk for OPIAD. If OPIAD is identified, the patient should be carefully considered for an opioid dose reduction as an initial management strategy.
Limitations
A limitation of this review is the lack of consistency or adequacy of serum testosterone sampling, noting that valid testosterone levels need to be drawn in the morning and not obtained during a time of acute illness. In addition, testosterone levels need to be drawn at an appropriate interval while on TRT (eg, at the midpoint between testosterone injections).16 Although the time of the sample collection is documented in the Computerized Patient Record System (CPRS), it is unknown whether the patient was acutely ill on the day of the sampling unless a progress note is entered, and it is difficult to determine whether the level timing was accurate based on the testosterone replacement formulation. Another limitation is that the average decline in serum testosterone levels with aging in men is 1% to 2% per year. A significant fraction of older men have levels below the lower limit of the normal range for healthy young men, so in older men it can be more difficult to determine whether low testosterone is related to chronic opioid use or to older age.5,16
As this was a retrospective review, additional limitations included the inability to measure subclinical OPIAD, and the data collection related to symptoms of hypogonadism was restricted by documentation in the CPRS progress notes. The lack of data for females does not contribute to the literature on OPIAD in women. Finally, as the total daily MED does not distinguish between short-acting and long-acting opioid therapy, no differences between the impacts of short-acting vs long- acting opioid therapy on risk for hypogonadism can be inferred. There is evidence to suggest that long-acting opioids are associated with a significantly higher risk for OPIAD compared with short-acting opioids, although the mechanism behind this is not well established.22,23
Conclusions
The average age of the patients on chronic opioid therapy with a testosterone level drawn in this cohort was 58.3 years, which is younger than originally anticipated. The median age of 60 years is not significantly different from the average age, indicating that outliers did not impact this calculation. On average, the TT level was normal before starting opioids. Once opioids were started, patients were treated for an average duration of 52.5 months with an average daily dose of 126.8 mg MED. In this veteran cohort, 48.6% of patients met the criteria for TRT based on TT level alone, which is within the reported prevalence range of opioid-induced hypogonadism already published.4,9 These results are in line with the original hypothesis that chronic opioid use can adversely impact testosterone levels and can have a poor effect on a patient’s QOL due to symptoms of low testosterone. In addition to TRT, possible and suggested (but not proven) treatment options for OPIAD include discontinuation of opioid therapy, opioid rotation, or conversion to buprenorphine.21 The approach used should account for multiple patient-specific factors and should be individualized.
Based on the data, there is a trend toward lower testosterone levels in veterans treated with higher MED and for longer periods with chronic opioids. Given recent data that infer that TRT carries increased CV risk as well as the VHA’s Opioid Safety Initiative, it is imperative that providers closely evaluate the appropriateness of starting TRT and/or continuing chronic opioid therapy. All patients generally should have failed non- opioid management prior to opioid therapy for chronic nonmalignant pain, and this should be documented accordingly. It is also crucial to have the “opioid talk” with patients from time to time and discuss the risks vs benefits, the potential for addiction, overdose, dependence, tolerance, constipation, and OPIAD so patients can continue to be an active and informed participants in their care.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Unintentional drug poisoning in the United States, 2010. Atlanta, GA: Centers for Disease Control and Prevention Website. http://www.cdc.gov /HomeandRecreationalSafety/pdf/poison-issue-brief .pdf. Published July 2010. Accessed August 28, 2015.
2. American Academy of Family Physicians. Using opioids in the management of chronic pain patients: challenges and future options. University of Kentucky Medical Center Website. http://www .mc.uky.edu/equip-4-pcps/documents/CRx%20Literature/Opioids%20for%20chronic%20pain.pdf. Published 2010. Accessed August 28, 2015.
3. Duarte RV, Raphael JH, Labib M, Southall JL, Ashford RL. Prevalence and influence of diagnostic criteria in the assessment of hypogonadism in intrathecal opioid therapy patients. Pain Physician. 2013;16(1):9-14.
4. Smith HS, Elliott JA. Opioid-induced androgen deficiency (OPIAD). Pain Physician. 2012;15(suppl 3):ES145-ES156.
5. De Maddalena C, Bellini M, Berra M, Meriggiola MC, Aloisi AM. Opioid-induced hypogonadism: why and how to treat it. Pain Physician. 2012;15(suppl 3):ES111-ES118.
6. Bhasin S, Cunningham GR, Hayes FJ, et al; VM Endocrine Society Task Force. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536-2559.
7. Petak SM, Nankin HR, Spark RF, Swerdloff RS, Rodriguez-Rigau LJ; American Association of Clinical Endocrinologists. American Association of Clinical Endocrinologists Medical Guidelines for clinical practice for the evaluation and treatment of hypogonadism in adult male patients–2002 update. Endocr Pract. 2002;8(6):440-456.
8. Wang C, Nieschlag E, Swerdloff R, et al. Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. J Androl. 2009;30(1):1-9.
9. Reddy RG, Aung T, Karavitaki N, Wass JA. Opioid induced hypogonadism. BMJ. 2010;341:c4462.
10. U.S. Department of Veterans Affairs, Veterans Health Administration. VHA Handbook 1058.05: VHA operations activities that may constitute research. U.S. Department of Veterans Affairs Website. http://www.va.gov/vhapublications /ViewPublication.asp?pub_ID=2456. Published October 28, 2011. Accessed August 28, 2015.
11. AndroGel [package insert]. North Chicago, IL: AbbVie Inc; 2013.
12. Axiron [package insert]. Indianapolis, IL: Lilly USA, LLC; 2011.
13. U.S. Department of Veterans Affairs. Opioid therapy for chronic pain pocket guide. U.S. Department of Veterans Affairs. http://www.healthquality .va.gov/guidelines/pain/cot/opioidpocketguide23may2013v1.pdf. Published May 2013 Accessed August 28, 2015.
14. McPherson ML. Demystifying Opioid Conversion Calculations: A Guide for Effective Dosing. Bethesda, MD: American Society of Health-System Pharmacists; 2009.
15. Butrans [package insert]. Stamford, CT: Purdue Pharma LP; 2014.
16. Testosterone Replacement Therapy Criteria for Use. VISN 8: VISN Pharmacist Executives, Veterans Health Administration, Department of Veterans Affairs; 2014. [Internal document.]
17. Vigen R, O’Donnell CI, Barón AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013;310(17):1829-1836.
18. Finkle WD, Greenland S, Ridgeway GK, et al. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One. 2014;9(1):e85805.
19. U.S. Department of Veterans Affairs. Testosterone products and cardiovascular safety. U.S. Department of Veterans Affairs Website. http://www.pbm .va.gov/PBM/vacenterformedicationsafety /nationalpbmbulletin/Testosterone_Products_and _Cardiovascular_Safety_NATIONAL_PBM _BULLETIN_02.pdf. Published February 7, 2014. Accessed August 28, 2015.
20. U.S. Department of Veterans Affairs Veterans Health Administration (VHA) Pharmacy Benefits Management Services (PBM), Medical Advisory Panel (MAP) and Center for Medication Safety (VA MEDSAFE). Memorandum: Opioid Safety Initiative Requirements. U.S. Department of Veterans Affairs Website. http://www.veterans.senate.gov/imo /media/doc/VA%20Testimony%20-%20April%2030%20SVAC%20Overmedication%20hearing.pdf. Published April 30, 2014. Accessed August 28, 2015.
21. Brennan MJ. The effect of opioid therapy on endocrine function. Am J Med. 2013;126(3)(suppl 1):S12-S18.
22. Rubinstein AL, Carpenter DM, Minkoff JR. Hypogonadism in men with chronic pain linked to the use of long-acting rather than short-acting opioids. Clin J Pain. 2013;29(10):840-845.
23. Rubinstein A, Carpenter DM. Elucidating risk factors for androgen deficiency associated with daily opioid use. Am J Med. 2014;127(12):1195-1201.
1. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Unintentional drug poisoning in the United States, 2010. Atlanta, GA: Centers for Disease Control and Prevention Website. http://www.cdc.gov /HomeandRecreationalSafety/pdf/poison-issue-brief .pdf. Published July 2010. Accessed August 28, 2015.
2. American Academy of Family Physicians. Using opioids in the management of chronic pain patients: challenges and future options. University of Kentucky Medical Center Website. http://www .mc.uky.edu/equip-4-pcps/documents/CRx%20Literature/Opioids%20for%20chronic%20pain.pdf. Published 2010. Accessed August 28, 2015.
3. Duarte RV, Raphael JH, Labib M, Southall JL, Ashford RL. Prevalence and influence of diagnostic criteria in the assessment of hypogonadism in intrathecal opioid therapy patients. Pain Physician. 2013;16(1):9-14.
4. Smith HS, Elliott JA. Opioid-induced androgen deficiency (OPIAD). Pain Physician. 2012;15(suppl 3):ES145-ES156.
5. De Maddalena C, Bellini M, Berra M, Meriggiola MC, Aloisi AM. Opioid-induced hypogonadism: why and how to treat it. Pain Physician. 2012;15(suppl 3):ES111-ES118.
6. Bhasin S, Cunningham GR, Hayes FJ, et al; VM Endocrine Society Task Force. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536-2559.
7. Petak SM, Nankin HR, Spark RF, Swerdloff RS, Rodriguez-Rigau LJ; American Association of Clinical Endocrinologists. American Association of Clinical Endocrinologists Medical Guidelines for clinical practice for the evaluation and treatment of hypogonadism in adult male patients–2002 update. Endocr Pract. 2002;8(6):440-456.
8. Wang C, Nieschlag E, Swerdloff R, et al. Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. J Androl. 2009;30(1):1-9.
9. Reddy RG, Aung T, Karavitaki N, Wass JA. Opioid induced hypogonadism. BMJ. 2010;341:c4462.
10. U.S. Department of Veterans Affairs, Veterans Health Administration. VHA Handbook 1058.05: VHA operations activities that may constitute research. U.S. Department of Veterans Affairs Website. http://www.va.gov/vhapublications /ViewPublication.asp?pub_ID=2456. Published October 28, 2011. Accessed August 28, 2015.
11. AndroGel [package insert]. North Chicago, IL: AbbVie Inc; 2013.
12. Axiron [package insert]. Indianapolis, IL: Lilly USA, LLC; 2011.
13. U.S. Department of Veterans Affairs. Opioid therapy for chronic pain pocket guide. U.S. Department of Veterans Affairs. http://www.healthquality .va.gov/guidelines/pain/cot/opioidpocketguide23may2013v1.pdf. Published May 2013 Accessed August 28, 2015.
14. McPherson ML. Demystifying Opioid Conversion Calculations: A Guide for Effective Dosing. Bethesda, MD: American Society of Health-System Pharmacists; 2009.
15. Butrans [package insert]. Stamford, CT: Purdue Pharma LP; 2014.
16. Testosterone Replacement Therapy Criteria for Use. VISN 8: VISN Pharmacist Executives, Veterans Health Administration, Department of Veterans Affairs; 2014. [Internal document.]
17. Vigen R, O’Donnell CI, Barón AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013;310(17):1829-1836.
18. Finkle WD, Greenland S, Ridgeway GK, et al. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One. 2014;9(1):e85805.
19. U.S. Department of Veterans Affairs. Testosterone products and cardiovascular safety. U.S. Department of Veterans Affairs Website. http://www.pbm .va.gov/PBM/vacenterformedicationsafety /nationalpbmbulletin/Testosterone_Products_and _Cardiovascular_Safety_NATIONAL_PBM _BULLETIN_02.pdf. Published February 7, 2014. Accessed August 28, 2015.
20. U.S. Department of Veterans Affairs Veterans Health Administration (VHA) Pharmacy Benefits Management Services (PBM), Medical Advisory Panel (MAP) and Center for Medication Safety (VA MEDSAFE). Memorandum: Opioid Safety Initiative Requirements. U.S. Department of Veterans Affairs Website. http://www.veterans.senate.gov/imo /media/doc/VA%20Testimony%20-%20April%2030%20SVAC%20Overmedication%20hearing.pdf. Published April 30, 2014. Accessed August 28, 2015.
21. Brennan MJ. The effect of opioid therapy on endocrine function. Am J Med. 2013;126(3)(suppl 1):S12-S18.
22. Rubinstein AL, Carpenter DM, Minkoff JR. Hypogonadism in men with chronic pain linked to the use of long-acting rather than short-acting opioids. Clin J Pain. 2013;29(10):840-845.
23. Rubinstein A, Carpenter DM. Elucidating risk factors for androgen deficiency associated with daily opioid use. Am J Med. 2014;127(12):1195-1201.