User login
Leaders Outline DHA “Market” Transition
One theme emerged from multiple military healthy system (MHS) leaders at the recent AMSUS annual conference: Significant change is coming to the MHS, and military health care providers can either embrace and shape that change or somebody else will. “If we don’t shape our future, others will step in and do it for us,” Tom McCaffrey, Assistant Secretary of Defense for Health Affairs; Defense Health Agency (DHA), and the Uniformed Service University for the Health Sciences (USU) told the audience.
The “historic” changes are underway, as the DHA has already begun to take over control of many military treatment facilities (MTFs) that were formerly operated by the separate services. In the next step of the transition, nearly 250 individual MTFs will be combined—along with TRICARE providers—in 21 geographically based “markets” in order to streamline management and avoid redundancies.
The exact details of the changes in store have not been released. McCaffrey noted that US Department of Defense (DoD) leadership will submit the “framework” for their assessment of the MHS to Congress “very soon, and at that point we will begin the hard work of detailed implementation of the results of that assessment and recommendations from the department.” Changes are expected to continue through fiscal year 2021, and some sources have estimated that as many as 18,000 jobs could be eliminated in the process.
Although Congress drove these changes in the National Defense Authorization Act of 2017, MHS leaders insist they are determining how to make the transformation without hurting medical readiness. “We the senior leadership of the MHS must continue to work together to shape our system to meet the challenges of the new environment,” McCaffrey insisted.
It seems as though all elements of the MHS are on the table. One report has suggested that the USU budget could be cut by a third. “Given the USU’s track record of excellence, we were alarmed to learn that the department is considering cuts as high as 30% to the university’s budget for research, development, testing, and evaluation, and 34% to university operations and maintenance... includ[ing] the cancellation of a $445 million military construction project and closure of the USU medical school,” US senators Chris Van Hollen (D-MD), Ben Cardin (D-MD.), Jack Reed (D-RI), and Congressman Jamie Raskin (D-MD) wrote in a November 21, 2019, letter to US Department of Defense Secretary Mark Esper. “These cuts, even if only partially implemented or scaled back, will adversely impact the enterprise across recruitment, retention, access to research funding, and severely impact medical readiness at a time when demand is increasing.”
The medical readiness of military health care providers remains one of the thorniest challenges revolving around the DHA transition. “As an infantryman, from my perspective if you can't maintain effectiveness on the trauma side than it is not worth getting more efficient,” argued LTG (Ret) Jeffrey S. Buchannon, who formerly served as senior commander of Fort Sam Houston, which includes Brooke Army Medical Center, the military’s only level 1 trauma center and 1 of only 2 trauma centers in San Antonio. “We need the home game in order to prepare for the away game,”
In its review, DoD is looking at how the MTFs support inpatient and/or outpatient services to maintain medical force readiness. “We need to identify those areas where we can expand capacity at MTFs that offer potential for sustaining the skills and knowledge of our members,” said McCaffrey. “But we also must examine those areas where facilities do not offer now and likely will not be able to offer in the future a platform for maximizing capabilities to support medical readiness. In those situations, we must be open to right sizing MTF services and capabilities so as to ensure that we are using finite resources most efficiently while not compromising our ability to meet the mission.”
“Our military healthy system is the envy of the world. Any great power competitor would trade its health care and battlefield medicine capabilities for the system you have built,” McCaffrey said. “But just as America’s combat supremacy is not guaranteed nor is the supremacy of the MHS.” The US faces new global security challenges, McCaffrey argued, and “we must adapt and evolve if we are to successfully meet these challenges.”
One theme emerged from multiple military healthy system (MHS) leaders at the recent AMSUS annual conference: Significant change is coming to the MHS, and military health care providers can either embrace and shape that change or somebody else will. “If we don’t shape our future, others will step in and do it for us,” Tom McCaffrey, Assistant Secretary of Defense for Health Affairs; Defense Health Agency (DHA), and the Uniformed Service University for the Health Sciences (USU) told the audience.
The “historic” changes are underway, as the DHA has already begun to take over control of many military treatment facilities (MTFs) that were formerly operated by the separate services. In the next step of the transition, nearly 250 individual MTFs will be combined—along with TRICARE providers—in 21 geographically based “markets” in order to streamline management and avoid redundancies.
The exact details of the changes in store have not been released. McCaffrey noted that US Department of Defense (DoD) leadership will submit the “framework” for their assessment of the MHS to Congress “very soon, and at that point we will begin the hard work of detailed implementation of the results of that assessment and recommendations from the department.” Changes are expected to continue through fiscal year 2021, and some sources have estimated that as many as 18,000 jobs could be eliminated in the process.
Although Congress drove these changes in the National Defense Authorization Act of 2017, MHS leaders insist they are determining how to make the transformation without hurting medical readiness. “We the senior leadership of the MHS must continue to work together to shape our system to meet the challenges of the new environment,” McCaffrey insisted.
It seems as though all elements of the MHS are on the table. One report has suggested that the USU budget could be cut by a third. “Given the USU’s track record of excellence, we were alarmed to learn that the department is considering cuts as high as 30% to the university’s budget for research, development, testing, and evaluation, and 34% to university operations and maintenance... includ[ing] the cancellation of a $445 million military construction project and closure of the USU medical school,” US senators Chris Van Hollen (D-MD), Ben Cardin (D-MD.), Jack Reed (D-RI), and Congressman Jamie Raskin (D-MD) wrote in a November 21, 2019, letter to US Department of Defense Secretary Mark Esper. “These cuts, even if only partially implemented or scaled back, will adversely impact the enterprise across recruitment, retention, access to research funding, and severely impact medical readiness at a time when demand is increasing.”
The medical readiness of military health care providers remains one of the thorniest challenges revolving around the DHA transition. “As an infantryman, from my perspective if you can't maintain effectiveness on the trauma side than it is not worth getting more efficient,” argued LTG (Ret) Jeffrey S. Buchannon, who formerly served as senior commander of Fort Sam Houston, which includes Brooke Army Medical Center, the military’s only level 1 trauma center and 1 of only 2 trauma centers in San Antonio. “We need the home game in order to prepare for the away game,”
In its review, DoD is looking at how the MTFs support inpatient and/or outpatient services to maintain medical force readiness. “We need to identify those areas where we can expand capacity at MTFs that offer potential for sustaining the skills and knowledge of our members,” said McCaffrey. “But we also must examine those areas where facilities do not offer now and likely will not be able to offer in the future a platform for maximizing capabilities to support medical readiness. In those situations, we must be open to right sizing MTF services and capabilities so as to ensure that we are using finite resources most efficiently while not compromising our ability to meet the mission.”
“Our military healthy system is the envy of the world. Any great power competitor would trade its health care and battlefield medicine capabilities for the system you have built,” McCaffrey said. “But just as America’s combat supremacy is not guaranteed nor is the supremacy of the MHS.” The US faces new global security challenges, McCaffrey argued, and “we must adapt and evolve if we are to successfully meet these challenges.”
One theme emerged from multiple military healthy system (MHS) leaders at the recent AMSUS annual conference: Significant change is coming to the MHS, and military health care providers can either embrace and shape that change or somebody else will. “If we don’t shape our future, others will step in and do it for us,” Tom McCaffrey, Assistant Secretary of Defense for Health Affairs; Defense Health Agency (DHA), and the Uniformed Service University for the Health Sciences (USU) told the audience.
The “historic” changes are underway, as the DHA has already begun to take over control of many military treatment facilities (MTFs) that were formerly operated by the separate services. In the next step of the transition, nearly 250 individual MTFs will be combined—along with TRICARE providers—in 21 geographically based “markets” in order to streamline management and avoid redundancies.
The exact details of the changes in store have not been released. McCaffrey noted that US Department of Defense (DoD) leadership will submit the “framework” for their assessment of the MHS to Congress “very soon, and at that point we will begin the hard work of detailed implementation of the results of that assessment and recommendations from the department.” Changes are expected to continue through fiscal year 2021, and some sources have estimated that as many as 18,000 jobs could be eliminated in the process.
Although Congress drove these changes in the National Defense Authorization Act of 2017, MHS leaders insist they are determining how to make the transformation without hurting medical readiness. “We the senior leadership of the MHS must continue to work together to shape our system to meet the challenges of the new environment,” McCaffrey insisted.
It seems as though all elements of the MHS are on the table. One report has suggested that the USU budget could be cut by a third. “Given the USU’s track record of excellence, we were alarmed to learn that the department is considering cuts as high as 30% to the university’s budget for research, development, testing, and evaluation, and 34% to university operations and maintenance... includ[ing] the cancellation of a $445 million military construction project and closure of the USU medical school,” US senators Chris Van Hollen (D-MD), Ben Cardin (D-MD.), Jack Reed (D-RI), and Congressman Jamie Raskin (D-MD) wrote in a November 21, 2019, letter to US Department of Defense Secretary Mark Esper. “These cuts, even if only partially implemented or scaled back, will adversely impact the enterprise across recruitment, retention, access to research funding, and severely impact medical readiness at a time when demand is increasing.”
The medical readiness of military health care providers remains one of the thorniest challenges revolving around the DHA transition. “As an infantryman, from my perspective if you can't maintain effectiveness on the trauma side than it is not worth getting more efficient,” argued LTG (Ret) Jeffrey S. Buchannon, who formerly served as senior commander of Fort Sam Houston, which includes Brooke Army Medical Center, the military’s only level 1 trauma center and 1 of only 2 trauma centers in San Antonio. “We need the home game in order to prepare for the away game,”
In its review, DoD is looking at how the MTFs support inpatient and/or outpatient services to maintain medical force readiness. “We need to identify those areas where we can expand capacity at MTFs that offer potential for sustaining the skills and knowledge of our members,” said McCaffrey. “But we also must examine those areas where facilities do not offer now and likely will not be able to offer in the future a platform for maximizing capabilities to support medical readiness. In those situations, we must be open to right sizing MTF services and capabilities so as to ensure that we are using finite resources most efficiently while not compromising our ability to meet the mission.”
“Our military healthy system is the envy of the world. Any great power competitor would trade its health care and battlefield medicine capabilities for the system you have built,” McCaffrey said. “But just as America’s combat supremacy is not guaranteed nor is the supremacy of the MHS.” The US faces new global security challenges, McCaffrey argued, and “we must adapt and evolve if we are to successfully meet these challenges.”
Peer-Review Transparency
Federal health care providers live under a microscope, so it seems only fair that we at Fed Pract honor that reality and open ourselves up to scrutiny as well.1 We hope that by shedding light on our peer-review process and manuscript acceptance rate, we will not only highlight our accomplishments, but identify areas for improvement.
Free access to Fed Pract content has always been our priority. While many journals charge authors or readers, Fed Pract has been and will remain free for readers and authors.2 Advertising enables the journal to support this free model of publishing, but we take care to ensure that advertisements do not influence content in any way. Our advertising policy can be found at www.mdedge.com/fedprac/page/advertising.
In January 2019, Fed Pract placed > 400 peer-reviewed articles published since January 2015 in the PubMed Central (PMC) database (ncbi.nlm.nih.gov/pmc). The full text of these and all future Fed Pract peer-reviewed articles will be available at PMC (no registration required), and the citations also will be included in PubMed. We hope that this process will make it even easier for anyone to access our authors’ works.
In 2018 about 36,000 federal health care providers (HCPs) received hard copies of this journal. The print journal is free, but circulation is limited to HCPs who work at the US Department of Veterans Affairs (VA), US Department of Defense (DoD), and the US Public Health Service (PHS). The mdedge.com/fedprac website, which includes every article published since 2003, had 1.4 million page views in 2018. After reading 3 online articles, readers in the US are asked to complete a simple registration form to help us better customize the reader experience. In some cases, international readers may be asked to pay for access to articles online; however, any VA, DoD, or PHS officer stationed overseas can contact the editorial staff (fedprac@mdedge.com) to ensure that they can access the articles for free.
In 2018 the journal received 164 manuscripts and published 94 articles written by 357 different federal HCPs. The 164 manuscript submissions represented a 45% growth over previous years. Not surprisingly, the increased rate of submissions began shortly after the May 2018 announcement that journal articles would be included in PMC. Most of those articles (83%) were submitted unsolicited.
Fed Pract has always prided itself on being an early promoter of interdisciplinary health care professional publications. Nearly half of its listed authors were physicians (48%), while pharmacists made up the next largest cohort (18%). There were smaller numbers of PhDs, nurses, social workers, and physical therapists. The majority were written by HCPs affiliated with the VA (95% of articles and 93% of authors), and no articles in 2018 were written by PHS officers. Physicians comprise about two-thirds of the audience, while pharmacists make up 17% and nurses 9%. PHS and DoD HCPs make up 19% of the Fed Pract audience, suggesting that the journal needs to do more work to encourage these HCPs to contribute articles to the journal.3
Articles published in 2018 covered a broad range of topics from “Anesthesia Care Practice Models in the VHA” and “Army Behavioral Health System” to “Vitreous Hemorrhage in the Setting of a Vascular Loop” and “A Workforce Assessment of VA Home-Based Primary Care Pharmacists.” Categorizing the articles is a challenge. Few health care topics fit neatly into a single topic or specialty. This is especially true in federal health care where much of the care is delivered by multidisciplinary patient-centered medical homes or patient aligned care teams. Nevertheless, a few broad outlines can be discerned. Articles were roughly split between primary care and hospital-based and/or specialty care topics; one-quarter of the articles were case studies or case series articles, and about 20% were editorials or opinion columns. Nineteen articles dealt explicitly with chronic conditions, and 10 articles focused on mental health care.
Peer reviewers are an essential part of the process. Reviewers are blinded to the identityof the authors, ensuring fairness and reducing potential conflicts of interest. We are extremely grateful to each and every reviewer for the time and energy they contribute to the journal. Peer reviewers do not get nearly enough recognition for their important work. In 2018 Fed Pract invited 1,205 reviewers for 164 manuscript submissions and 94 manuscript revisions. More than 200 different reviewers submitted 487 reviews with a median (SD) of 2 reviews (1.8) and a range of 1 to 10. The top 20 reviewers completed 134 reviews with a median (SD) of 6 reviews (1.2). The results stand in contrast to some journals that must offer many invitations per review and depend on a small number of reviewers.1,4-6
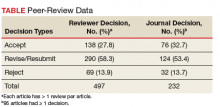
The reviewers recommended to reject 14% and to revise 26% of the articles, which is a much lower rejection rate than many other journals (Table).4
These data suggest that Fed Pract and its peer-review process is on a sound foundation but needs to make improvements. Moving into 2019, the journal expects that an increasing number of submissions will require a higher rejection rate. Moreover, we will need to do a better job reaching out to underrepresented portions of our audience. To decrease the time to publication for accepted manuscripts, in 2019 we will publish more articles online ahead of the print publication as we strive to improve the experience for authors, reviewers, readers, and the entire Fed Pract audience.
None of this work can be done without our small and dedicated staff. I would like to thank Managing Editor Joyce Brody who sent out each and every one of those reviewer invitations, Deputy Editor Robert Fee, who manages the special issues, Web Editor Teraya Smith, who runs our entire digital operation, and of course, Editor in Chief Cynthia Geppert, who oversees it all. Finally, it is important that you let us know how we are doing and whether we are meeting your needs. Visit mdedge.com/fedprac to take the readership survey or reach out to me at rpaul@mdedge.com.
1. Geppert CMA. Caring under a microscope. Fed Pract. 2018;35(7):6-7.
2. Smith R. Peer review: a flawed process at the heart of science and journals. J R Soc Med. 2006;99(4):178-182.
3. BPA Worldwide. Federal Practitioner brand report for the 6 month period ending June 2018. https://www.frontlinemedcom.com/wp-content/uploads/FEDPRAC_BPA.pdf. Updated June 2018. Accessed March 5, 2019.
4. Fontanarosa PB, Bauchner H, Golub RM. Thank you to JAMA authors, peer reviewers, and readers. JAMA. 2017;317(8):812-813.
5. Publons, Clarivate Analytics. 2018 global state of peer review. https://publons.com/static/Publons-Global-State-Of-Peer-Review-2018.pdf. Published September 2018. Accessed March 5, 2019.
6. Malcom D. It’s time we fix the peer review system. Am J Pharm Educ. 2018;82(5):7144.
Federal health care providers live under a microscope, so it seems only fair that we at Fed Pract honor that reality and open ourselves up to scrutiny as well.1 We hope that by shedding light on our peer-review process and manuscript acceptance rate, we will not only highlight our accomplishments, but identify areas for improvement.
Free access to Fed Pract content has always been our priority. While many journals charge authors or readers, Fed Pract has been and will remain free for readers and authors.2 Advertising enables the journal to support this free model of publishing, but we take care to ensure that advertisements do not influence content in any way. Our advertising policy can be found at www.mdedge.com/fedprac/page/advertising.
In January 2019, Fed Pract placed > 400 peer-reviewed articles published since January 2015 in the PubMed Central (PMC) database (ncbi.nlm.nih.gov/pmc). The full text of these and all future Fed Pract peer-reviewed articles will be available at PMC (no registration required), and the citations also will be included in PubMed. We hope that this process will make it even easier for anyone to access our authors’ works.
In 2018 about 36,000 federal health care providers (HCPs) received hard copies of this journal. The print journal is free, but circulation is limited to HCPs who work at the US Department of Veterans Affairs (VA), US Department of Defense (DoD), and the US Public Health Service (PHS). The mdedge.com/fedprac website, which includes every article published since 2003, had 1.4 million page views in 2018. After reading 3 online articles, readers in the US are asked to complete a simple registration form to help us better customize the reader experience. In some cases, international readers may be asked to pay for access to articles online; however, any VA, DoD, or PHS officer stationed overseas can contact the editorial staff (fedprac@mdedge.com) to ensure that they can access the articles for free.
In 2018 the journal received 164 manuscripts and published 94 articles written by 357 different federal HCPs. The 164 manuscript submissions represented a 45% growth over previous years. Not surprisingly, the increased rate of submissions began shortly after the May 2018 announcement that journal articles would be included in PMC. Most of those articles (83%) were submitted unsolicited.
Fed Pract has always prided itself on being an early promoter of interdisciplinary health care professional publications. Nearly half of its listed authors were physicians (48%), while pharmacists made up the next largest cohort (18%). There were smaller numbers of PhDs, nurses, social workers, and physical therapists. The majority were written by HCPs affiliated with the VA (95% of articles and 93% of authors), and no articles in 2018 were written by PHS officers. Physicians comprise about two-thirds of the audience, while pharmacists make up 17% and nurses 9%. PHS and DoD HCPs make up 19% of the Fed Pract audience, suggesting that the journal needs to do more work to encourage these HCPs to contribute articles to the journal.3
Articles published in 2018 covered a broad range of topics from “Anesthesia Care Practice Models in the VHA” and “Army Behavioral Health System” to “Vitreous Hemorrhage in the Setting of a Vascular Loop” and “A Workforce Assessment of VA Home-Based Primary Care Pharmacists.” Categorizing the articles is a challenge. Few health care topics fit neatly into a single topic or specialty. This is especially true in federal health care where much of the care is delivered by multidisciplinary patient-centered medical homes or patient aligned care teams. Nevertheless, a few broad outlines can be discerned. Articles were roughly split between primary care and hospital-based and/or specialty care topics; one-quarter of the articles were case studies or case series articles, and about 20% were editorials or opinion columns. Nineteen articles dealt explicitly with chronic conditions, and 10 articles focused on mental health care.
Peer reviewers are an essential part of the process. Reviewers are blinded to the identityof the authors, ensuring fairness and reducing potential conflicts of interest. We are extremely grateful to each and every reviewer for the time and energy they contribute to the journal. Peer reviewers do not get nearly enough recognition for their important work. In 2018 Fed Pract invited 1,205 reviewers for 164 manuscript submissions and 94 manuscript revisions. More than 200 different reviewers submitted 487 reviews with a median (SD) of 2 reviews (1.8) and a range of 1 to 10. The top 20 reviewers completed 134 reviews with a median (SD) of 6 reviews (1.2). The results stand in contrast to some journals that must offer many invitations per review and depend on a small number of reviewers.1,4-6
The reviewers recommended to reject 14% and to revise 26% of the articles, which is a much lower rejection rate than many other journals (Table).4
These data suggest that Fed Pract and its peer-review process is on a sound foundation but needs to make improvements. Moving into 2019, the journal expects that an increasing number of submissions will require a higher rejection rate. Moreover, we will need to do a better job reaching out to underrepresented portions of our audience. To decrease the time to publication for accepted manuscripts, in 2019 we will publish more articles online ahead of the print publication as we strive to improve the experience for authors, reviewers, readers, and the entire Fed Pract audience.
None of this work can be done without our small and dedicated staff. I would like to thank Managing Editor Joyce Brody who sent out each and every one of those reviewer invitations, Deputy Editor Robert Fee, who manages the special issues, Web Editor Teraya Smith, who runs our entire digital operation, and of course, Editor in Chief Cynthia Geppert, who oversees it all. Finally, it is important that you let us know how we are doing and whether we are meeting your needs. Visit mdedge.com/fedprac to take the readership survey or reach out to me at rpaul@mdedge.com.
Federal health care providers live under a microscope, so it seems only fair that we at Fed Pract honor that reality and open ourselves up to scrutiny as well.1 We hope that by shedding light on our peer-review process and manuscript acceptance rate, we will not only highlight our accomplishments, but identify areas for improvement.
Free access to Fed Pract content has always been our priority. While many journals charge authors or readers, Fed Pract has been and will remain free for readers and authors.2 Advertising enables the journal to support this free model of publishing, but we take care to ensure that advertisements do not influence content in any way. Our advertising policy can be found at www.mdedge.com/fedprac/page/advertising.
In January 2019, Fed Pract placed > 400 peer-reviewed articles published since January 2015 in the PubMed Central (PMC) database (ncbi.nlm.nih.gov/pmc). The full text of these and all future Fed Pract peer-reviewed articles will be available at PMC (no registration required), and the citations also will be included in PubMed. We hope that this process will make it even easier for anyone to access our authors’ works.
In 2018 about 36,000 federal health care providers (HCPs) received hard copies of this journal. The print journal is free, but circulation is limited to HCPs who work at the US Department of Veterans Affairs (VA), US Department of Defense (DoD), and the US Public Health Service (PHS). The mdedge.com/fedprac website, which includes every article published since 2003, had 1.4 million page views in 2018. After reading 3 online articles, readers in the US are asked to complete a simple registration form to help us better customize the reader experience. In some cases, international readers may be asked to pay for access to articles online; however, any VA, DoD, or PHS officer stationed overseas can contact the editorial staff (fedprac@mdedge.com) to ensure that they can access the articles for free.
In 2018 the journal received 164 manuscripts and published 94 articles written by 357 different federal HCPs. The 164 manuscript submissions represented a 45% growth over previous years. Not surprisingly, the increased rate of submissions began shortly after the May 2018 announcement that journal articles would be included in PMC. Most of those articles (83%) were submitted unsolicited.
Fed Pract has always prided itself on being an early promoter of interdisciplinary health care professional publications. Nearly half of its listed authors were physicians (48%), while pharmacists made up the next largest cohort (18%). There were smaller numbers of PhDs, nurses, social workers, and physical therapists. The majority were written by HCPs affiliated with the VA (95% of articles and 93% of authors), and no articles in 2018 were written by PHS officers. Physicians comprise about two-thirds of the audience, while pharmacists make up 17% and nurses 9%. PHS and DoD HCPs make up 19% of the Fed Pract audience, suggesting that the journal needs to do more work to encourage these HCPs to contribute articles to the journal.3
Articles published in 2018 covered a broad range of topics from “Anesthesia Care Practice Models in the VHA” and “Army Behavioral Health System” to “Vitreous Hemorrhage in the Setting of a Vascular Loop” and “A Workforce Assessment of VA Home-Based Primary Care Pharmacists.” Categorizing the articles is a challenge. Few health care topics fit neatly into a single topic or specialty. This is especially true in federal health care where much of the care is delivered by multidisciplinary patient-centered medical homes or patient aligned care teams. Nevertheless, a few broad outlines can be discerned. Articles were roughly split between primary care and hospital-based and/or specialty care topics; one-quarter of the articles were case studies or case series articles, and about 20% were editorials or opinion columns. Nineteen articles dealt explicitly with chronic conditions, and 10 articles focused on mental health care.
Peer reviewers are an essential part of the process. Reviewers are blinded to the identityof the authors, ensuring fairness and reducing potential conflicts of interest. We are extremely grateful to each and every reviewer for the time and energy they contribute to the journal. Peer reviewers do not get nearly enough recognition for their important work. In 2018 Fed Pract invited 1,205 reviewers for 164 manuscript submissions and 94 manuscript revisions. More than 200 different reviewers submitted 487 reviews with a median (SD) of 2 reviews (1.8) and a range of 1 to 10. The top 20 reviewers completed 134 reviews with a median (SD) of 6 reviews (1.2). The results stand in contrast to some journals that must offer many invitations per review and depend on a small number of reviewers.1,4-6
The reviewers recommended to reject 14% and to revise 26% of the articles, which is a much lower rejection rate than many other journals (Table).4
These data suggest that Fed Pract and its peer-review process is on a sound foundation but needs to make improvements. Moving into 2019, the journal expects that an increasing number of submissions will require a higher rejection rate. Moreover, we will need to do a better job reaching out to underrepresented portions of our audience. To decrease the time to publication for accepted manuscripts, in 2019 we will publish more articles online ahead of the print publication as we strive to improve the experience for authors, reviewers, readers, and the entire Fed Pract audience.
None of this work can be done without our small and dedicated staff. I would like to thank Managing Editor Joyce Brody who sent out each and every one of those reviewer invitations, Deputy Editor Robert Fee, who manages the special issues, Web Editor Teraya Smith, who runs our entire digital operation, and of course, Editor in Chief Cynthia Geppert, who oversees it all. Finally, it is important that you let us know how we are doing and whether we are meeting your needs. Visit mdedge.com/fedprac to take the readership survey or reach out to me at rpaul@mdedge.com.
1. Geppert CMA. Caring under a microscope. Fed Pract. 2018;35(7):6-7.
2. Smith R. Peer review: a flawed process at the heart of science and journals. J R Soc Med. 2006;99(4):178-182.
3. BPA Worldwide. Federal Practitioner brand report for the 6 month period ending June 2018. https://www.frontlinemedcom.com/wp-content/uploads/FEDPRAC_BPA.pdf. Updated June 2018. Accessed March 5, 2019.
4. Fontanarosa PB, Bauchner H, Golub RM. Thank you to JAMA authors, peer reviewers, and readers. JAMA. 2017;317(8):812-813.
5. Publons, Clarivate Analytics. 2018 global state of peer review. https://publons.com/static/Publons-Global-State-Of-Peer-Review-2018.pdf. Published September 2018. Accessed March 5, 2019.
6. Malcom D. It’s time we fix the peer review system. Am J Pharm Educ. 2018;82(5):7144.
1. Geppert CMA. Caring under a microscope. Fed Pract. 2018;35(7):6-7.
2. Smith R. Peer review: a flawed process at the heart of science and journals. J R Soc Med. 2006;99(4):178-182.
3. BPA Worldwide. Federal Practitioner brand report for the 6 month period ending June 2018. https://www.frontlinemedcom.com/wp-content/uploads/FEDPRAC_BPA.pdf. Updated June 2018. Accessed March 5, 2019.
4. Fontanarosa PB, Bauchner H, Golub RM. Thank you to JAMA authors, peer reviewers, and readers. JAMA. 2017;317(8):812-813.
5. Publons, Clarivate Analytics. 2018 global state of peer review. https://publons.com/static/Publons-Global-State-Of-Peer-Review-2018.pdf. Published September 2018. Accessed March 5, 2019.
6. Malcom D. It’s time we fix the peer review system. Am J Pharm Educ. 2018;82(5):7144.
Breaking News: Trump Upends Federal Pay for 2019
In a letter to Congressional leaders, President Trump has announced a pay freeze for all civilian federal employees in 2019. The decision will not impact active duty service members who are still are expected to receive a 2.6% pay raise next year.
The decision aims to circumvent a 2.1% across the board increase and additional locality pay increases that would average 25.7%. "We must maintain efforts to put our Nation on a fiscally sustainable course, and Federal agency budgets cannot sustain such increases. Accordingly, I have determined that it is appropriate to exercise my authority to set alternative across-the-board and locality pay adjustments for 2019."
In the letter, the President disputed the notion that locality pay was important for keeping and attracting quality applicants for positions. Currently, the Veterans Health Administration has more than 40,000 job openings.
"I have determined that for 2019, both across‑the‑board pay increases and locality pay increases will be set at zero. These alternative pay plan decisions will not materially affect our ability to attract and retain a well‑qualified Federal workforce.
President Trump had already included the pay freeze in his budget proposal. While Congress can override the President's decision, congressional action is not expected.
In a letter to Congressional leaders, President Trump has announced a pay freeze for all civilian federal employees in 2019. The decision will not impact active duty service members who are still are expected to receive a 2.6% pay raise next year.
The decision aims to circumvent a 2.1% across the board increase and additional locality pay increases that would average 25.7%. "We must maintain efforts to put our Nation on a fiscally sustainable course, and Federal agency budgets cannot sustain such increases. Accordingly, I have determined that it is appropriate to exercise my authority to set alternative across-the-board and locality pay adjustments for 2019."
In the letter, the President disputed the notion that locality pay was important for keeping and attracting quality applicants for positions. Currently, the Veterans Health Administration has more than 40,000 job openings.
"I have determined that for 2019, both across‑the‑board pay increases and locality pay increases will be set at zero. These alternative pay plan decisions will not materially affect our ability to attract and retain a well‑qualified Federal workforce.
President Trump had already included the pay freeze in his budget proposal. While Congress can override the President's decision, congressional action is not expected.
In a letter to Congressional leaders, President Trump has announced a pay freeze for all civilian federal employees in 2019. The decision will not impact active duty service members who are still are expected to receive a 2.6% pay raise next year.
The decision aims to circumvent a 2.1% across the board increase and additional locality pay increases that would average 25.7%. "We must maintain efforts to put our Nation on a fiscally sustainable course, and Federal agency budgets cannot sustain such increases. Accordingly, I have determined that it is appropriate to exercise my authority to set alternative across-the-board and locality pay adjustments for 2019."
In the letter, the President disputed the notion that locality pay was important for keeping and attracting quality applicants for positions. Currently, the Veterans Health Administration has more than 40,000 job openings.
"I have determined that for 2019, both across‑the‑board pay increases and locality pay increases will be set at zero. These alternative pay plan decisions will not materially affect our ability to attract and retain a well‑qualified Federal workforce.
President Trump had already included the pay freeze in his budget proposal. While Congress can override the President's decision, congressional action is not expected.
Singing Praises, Naming Names
Being a peer-reviewed journal, Federal Practitioner relies on the dedicated efforts of a great number of unsung (and uncompensated) people, and we would like to recognize these efforts. This journal exists because of the large body of federal health care providers who devote their time and energy to sharing best practices, case studies, literature reviews, and original research. An even larger number of men and women review the many submissions, check the research, and provide essential feedback to our authors. By design, this army of reviewers remains anonymous, but that does not diminish their importance.
Although it would be impossible to adequately thank our reviewers, authors, and other contributors, sufficiently, we are trying. We are delighted to induct some of the most engaged members of the Federal Practitioner community to the Editorial Advisory Association (EAA). The EAA helps guide the journal to ensure it remains focused on the essential issues that confront federal health care providers. Federal Practitioner strives for continuous improvement and is focused on enhancing the breadth, depth, and quality of the online and print content. The EAA plays an important role in that process, and we thank all the current EAA and new members for their guidance.
New EAA Members
Susanne G. Barnett, PharmD, BCPS, has directed the Pharmacy Notes column for Federal Practitioner since 2015. Dr. Barnett is an associate professor at the University of Wisconsin-Madison School of Pharmacy and a clinical pharmacist at the William S. Middleton Memorial Veterans Hospital. She has focused on antimicrobial stewardship and infectious diseases.
Anthony Breu, MD, conceived and directs the VA Boston Medical Forum series
Maggie Chartier, PsyD, MPH, has authored multiple articles for Federal Practitioner and provided guidance and direction for the 2017 and (forthcoming) 2018 editions of the public pathogens/infectious diseases special issues. Dr. Chartier is the deputy director for the HIV, Hepatitis, and Related Conditions Program in the VHA Office of Specialty Care Services and an assistant clinical professor at the University of California, San Francisco.
Marcia Johnson, DNP, FNP-BC, has been a highly active author and peer reviewer. Dr. Johnson has been a nurse practitioner at the VA for 18 years, and currently provides primary care at the Clermont CBOC in Florida. She previously served as the hepatitis C research coordinator at Philadelphia VAMC and practiced at the Orlando VAMC spinal cord injury clinic.
William Rodríguez-Cintrón, MD, is another active peer reviewer and a prolific contributor. Dr. Rodríguez-Cintrón is chief of the pulmonary, critical care and sleep medicine departments at the VA Caribbean Healthcare System in Puerto Rico.
Col. (Ret) Mona Pearl Treyball, PhD, MS, RN, USAF, also has been a dedicated peer reviewer. Col. Treyball is professor and specialty director of the
Federal Practitioner would like to thank all of the current and new members of the EAA for their continued support. All of the journal’s successes are built on their dedication and commitment. Federal Practitioner encourages all the members of the federal health care community to become more involved, whether as a peer reviewer, author, or by responding to our content in print, online, or via social media. Your feedback and involvement makes this journal better.
Being a peer-reviewed journal, Federal Practitioner relies on the dedicated efforts of a great number of unsung (and uncompensated) people, and we would like to recognize these efforts. This journal exists because of the large body of federal health care providers who devote their time and energy to sharing best practices, case studies, literature reviews, and original research. An even larger number of men and women review the many submissions, check the research, and provide essential feedback to our authors. By design, this army of reviewers remains anonymous, but that does not diminish their importance.
Although it would be impossible to adequately thank our reviewers, authors, and other contributors, sufficiently, we are trying. We are delighted to induct some of the most engaged members of the Federal Practitioner community to the Editorial Advisory Association (EAA). The EAA helps guide the journal to ensure it remains focused on the essential issues that confront federal health care providers. Federal Practitioner strives for continuous improvement and is focused on enhancing the breadth, depth, and quality of the online and print content. The EAA plays an important role in that process, and we thank all the current EAA and new members for their guidance.
New EAA Members
Susanne G. Barnett, PharmD, BCPS, has directed the Pharmacy Notes column for Federal Practitioner since 2015. Dr. Barnett is an associate professor at the University of Wisconsin-Madison School of Pharmacy and a clinical pharmacist at the William S. Middleton Memorial Veterans Hospital. She has focused on antimicrobial stewardship and infectious diseases.
Anthony Breu, MD, conceived and directs the VA Boston Medical Forum series
Maggie Chartier, PsyD, MPH, has authored multiple articles for Federal Practitioner and provided guidance and direction for the 2017 and (forthcoming) 2018 editions of the public pathogens/infectious diseases special issues. Dr. Chartier is the deputy director for the HIV, Hepatitis, and Related Conditions Program in the VHA Office of Specialty Care Services and an assistant clinical professor at the University of California, San Francisco.
Marcia Johnson, DNP, FNP-BC, has been a highly active author and peer reviewer. Dr. Johnson has been a nurse practitioner at the VA for 18 years, and currently provides primary care at the Clermont CBOC in Florida. She previously served as the hepatitis C research coordinator at Philadelphia VAMC and practiced at the Orlando VAMC spinal cord injury clinic.
William Rodríguez-Cintrón, MD, is another active peer reviewer and a prolific contributor. Dr. Rodríguez-Cintrón is chief of the pulmonary, critical care and sleep medicine departments at the VA Caribbean Healthcare System in Puerto Rico.
Col. (Ret) Mona Pearl Treyball, PhD, MS, RN, USAF, also has been a dedicated peer reviewer. Col. Treyball is professor and specialty director of the
Federal Practitioner would like to thank all of the current and new members of the EAA for their continued support. All of the journal’s successes are built on their dedication and commitment. Federal Practitioner encourages all the members of the federal health care community to become more involved, whether as a peer reviewer, author, or by responding to our content in print, online, or via social media. Your feedback and involvement makes this journal better.
Being a peer-reviewed journal, Federal Practitioner relies on the dedicated efforts of a great number of unsung (and uncompensated) people, and we would like to recognize these efforts. This journal exists because of the large body of federal health care providers who devote their time and energy to sharing best practices, case studies, literature reviews, and original research. An even larger number of men and women review the many submissions, check the research, and provide essential feedback to our authors. By design, this army of reviewers remains anonymous, but that does not diminish their importance.
Although it would be impossible to adequately thank our reviewers, authors, and other contributors, sufficiently, we are trying. We are delighted to induct some of the most engaged members of the Federal Practitioner community to the Editorial Advisory Association (EAA). The EAA helps guide the journal to ensure it remains focused on the essential issues that confront federal health care providers. Federal Practitioner strives for continuous improvement and is focused on enhancing the breadth, depth, and quality of the online and print content. The EAA plays an important role in that process, and we thank all the current EAA and new members for their guidance.
New EAA Members
Susanne G. Barnett, PharmD, BCPS, has directed the Pharmacy Notes column for Federal Practitioner since 2015. Dr. Barnett is an associate professor at the University of Wisconsin-Madison School of Pharmacy and a clinical pharmacist at the William S. Middleton Memorial Veterans Hospital. She has focused on antimicrobial stewardship and infectious diseases.
Anthony Breu, MD, conceived and directs the VA Boston Medical Forum series
Maggie Chartier, PsyD, MPH, has authored multiple articles for Federal Practitioner and provided guidance and direction for the 2017 and (forthcoming) 2018 editions of the public pathogens/infectious diseases special issues. Dr. Chartier is the deputy director for the HIV, Hepatitis, and Related Conditions Program in the VHA Office of Specialty Care Services and an assistant clinical professor at the University of California, San Francisco.
Marcia Johnson, DNP, FNP-BC, has been a highly active author and peer reviewer. Dr. Johnson has been a nurse practitioner at the VA for 18 years, and currently provides primary care at the Clermont CBOC in Florida. She previously served as the hepatitis C research coordinator at Philadelphia VAMC and practiced at the Orlando VAMC spinal cord injury clinic.
William Rodríguez-Cintrón, MD, is another active peer reviewer and a prolific contributor. Dr. Rodríguez-Cintrón is chief of the pulmonary, critical care and sleep medicine departments at the VA Caribbean Healthcare System in Puerto Rico.
Col. (Ret) Mona Pearl Treyball, PhD, MS, RN, USAF, also has been a dedicated peer reviewer. Col. Treyball is professor and specialty director of the
Federal Practitioner would like to thank all of the current and new members of the EAA for their continued support. All of the journal’s successes are built on their dedication and commitment. Federal Practitioner encourages all the members of the federal health care community to become more involved, whether as a peer reviewer, author, or by responding to our content in print, online, or via social media. Your feedback and involvement makes this journal better.
The Challenges of Malaria Prevention for Women at War
Remington L. Nevin, MD, MPH, of the Johns Hopkins Bloomberg School of Public Health and author of “Issues in the Prevention of Malaria Among Women at War” in the new book Women at War discusses the challenges in preventing malaria in deployed women, the lack of clinical trial data on the impact of antimalarial drugs on women, and the recent success in avoiding malaria in Liberia.
[Scroll down to hear the full interview.]
Women currently make up about 15% of the military population, and more than 300,000 women have deployed since September 11, 2001. Women at War includes 19 chapters covering a host of topics, including deployment, issues at home, psychological challenges, and the veteran experience, reviewing epidemiology, changes in policy and demographics, factors affecting health, issues related to reproductive and urogenital health, and suggestions for health care providers treating women service members and veterans.
For a limited time, a discount is being offered to Federal Practitioner readers. Click here and use the promo code AMPROMD9 at checkout.
Remington L. Nevin, MD, MPH, of the Johns Hopkins Bloomberg School of Public Health and author of “Issues in the Prevention of Malaria Among Women at War” in the new book Women at War discusses the challenges in preventing malaria in deployed women, the lack of clinical trial data on the impact of antimalarial drugs on women, and the recent success in avoiding malaria in Liberia.
[Scroll down to hear the full interview.]
Women currently make up about 15% of the military population, and more than 300,000 women have deployed since September 11, 2001. Women at War includes 19 chapters covering a host of topics, including deployment, issues at home, psychological challenges, and the veteran experience, reviewing epidemiology, changes in policy and demographics, factors affecting health, issues related to reproductive and urogenital health, and suggestions for health care providers treating women service members and veterans.
For a limited time, a discount is being offered to Federal Practitioner readers. Click here and use the promo code AMPROMD9 at checkout.
Remington L. Nevin, MD, MPH, of the Johns Hopkins Bloomberg School of Public Health and author of “Issues in the Prevention of Malaria Among Women at War” in the new book Women at War discusses the challenges in preventing malaria in deployed women, the lack of clinical trial data on the impact of antimalarial drugs on women, and the recent success in avoiding malaria in Liberia.
[Scroll down to hear the full interview.]
Women currently make up about 15% of the military population, and more than 300,000 women have deployed since September 11, 2001. Women at War includes 19 chapters covering a host of topics, including deployment, issues at home, psychological challenges, and the veteran experience, reviewing epidemiology, changes in policy and demographics, factors affecting health, issues related to reproductive and urogenital health, and suggestions for health care providers treating women service members and veterans.
For a limited time, a discount is being offered to Federal Practitioner readers. Click here and use the promo code AMPROMD9 at checkout.
Women at War: A Growing Body of Evidence-Based Research
[Scroll down to hear the full interview.]
Women currently make up about 15% of the military population, and more than 300,000 women have deployed since September 11, 2001. Women at War includes 19 chapters covering a host of topics, including deployment, issues at home, psychological challenges, and the veteran experience, reviewing epidemiology, changes in policy and demographics, factors affecting health, issues related to reproductive and urogenital health, and suggestions for health care providers treating women service members and veterans.
For a limited time, a discount is being offered to Federal Practitioner readers. Click here and use the promo code AMPROMD9 at checkout.
[Scroll down to hear the full interview.]
Women currently make up about 15% of the military population, and more than 300,000 women have deployed since September 11, 2001. Women at War includes 19 chapters covering a host of topics, including deployment, issues at home, psychological challenges, and the veteran experience, reviewing epidemiology, changes in policy and demographics, factors affecting health, issues related to reproductive and urogenital health, and suggestions for health care providers treating women service members and veterans.
For a limited time, a discount is being offered to Federal Practitioner readers. Click here and use the promo code AMPROMD9 at checkout.
[Scroll down to hear the full interview.]
Women currently make up about 15% of the military population, and more than 300,000 women have deployed since September 11, 2001. Women at War includes 19 chapters covering a host of topics, including deployment, issues at home, psychological challenges, and the veteran experience, reviewing epidemiology, changes in policy and demographics, factors affecting health, issues related to reproductive and urogenital health, and suggestions for health care providers treating women service members and veterans.
For a limited time, a discount is being offered to Federal Practitioner readers. Click here and use the promo code AMPROMD9 at checkout.
AMSUS Federal Health in Transition Wrap-Up
Dr. Clancy Outlines VA Blueprint for Change
Carolyn M. Clancy, MD, Interim Under Secretary for Health at the VA outlined strategic aims for reshaping and restructuring into a more unified veteran-focused health care system. The ultimate goal for the plan is to put the veteran in control of his or her health care by providing a single phone number, a website, and well-trained VA employees who understand all the VA’s offerings. According to Dr. Clancy, “[this restructuring's] success will be defined from the veteran’s perspective."
- Operate a health care network that anticipates and meets the needs of veterans;
- Deliver high-quality, veteran-centered care that compares favorably to private sector health care;
- Leverage information technology, analytics, and models of delivery to optimize health care;
- Grow an organizational culture rooted in the VA’s core values and mission and prioritize veterans;
- Foster an environment of continuous learning, responsible risk taking, and personal accountability;
- Advance a model of health care that is personalized, proactive, and patient-driven;
- Lead the nation in research and treatment of military service-related conditions;
- Support innovation in health services through academic affiliations;
- Operate and communicate with integrity, transparency, and accountability; and
- Modernize VA management, including human resources, accounting, and other support services.
An Update on the Defense Health Agency
The Assistant Secretary of Defense for Health Affairs Jonathan Woodson, MD, outlined the strategic challenges and plans for changes at the $50 billion Defense Health Agency (DHA). “Get ready, this train is going to move very fast and you are part of it,” he challenged active service health care providers. "We understand this is a complicated world, and we need to get energized to find the solutions.”
Dr. Woodson also promised to develop better telehealth capabilities. “Telehealth is going to be an important tool, because it gives us the capability to reach forward and reach back,” he said, “We are a highly distributed system, and we need to develop it as a system, not just as a technology.”
PHS Officials Discuss 50-Year Battle Against Tobacco Use
RADM Lushniak noted that the PHS became the first uniformed service to go tobacco-free while in uniform. Joining the Acting Surgeon General in the presentation was RADM David L. Ashley who discussed how the PHS eliminated tobacco use within its ranks. RADM Ashley outlined 10 guidelines for clinicians to support patients in battling a tobacco addiction.
CAPT Kimberly Elenberg also outlined the steps PHS is taking to help the other uniformed services in their efforts to reduce and eliminate tobacco use. According to CAPT Elenberg, it is essential to recognize the specific and unique deployment challenges that active service members face and the rationales behind tobacco use before being able to reduce its use.
For more information on the 2014 AMSUS Annual Continuing Education Meeting, visit http://amsusmeetings.org/annual-meeting.
Dr. Clancy Outlines VA Blueprint for Change
Carolyn M. Clancy, MD, Interim Under Secretary for Health at the VA outlined strategic aims for reshaping and restructuring into a more unified veteran-focused health care system. The ultimate goal for the plan is to put the veteran in control of his or her health care by providing a single phone number, a website, and well-trained VA employees who understand all the VA’s offerings. According to Dr. Clancy, “[this restructuring's] success will be defined from the veteran’s perspective."
- Operate a health care network that anticipates and meets the needs of veterans;
- Deliver high-quality, veteran-centered care that compares favorably to private sector health care;
- Leverage information technology, analytics, and models of delivery to optimize health care;
- Grow an organizational culture rooted in the VA’s core values and mission and prioritize veterans;
- Foster an environment of continuous learning, responsible risk taking, and personal accountability;
- Advance a model of health care that is personalized, proactive, and patient-driven;
- Lead the nation in research and treatment of military service-related conditions;
- Support innovation in health services through academic affiliations;
- Operate and communicate with integrity, transparency, and accountability; and
- Modernize VA management, including human resources, accounting, and other support services.
An Update on the Defense Health Agency
The Assistant Secretary of Defense for Health Affairs Jonathan Woodson, MD, outlined the strategic challenges and plans for changes at the $50 billion Defense Health Agency (DHA). “Get ready, this train is going to move very fast and you are part of it,” he challenged active service health care providers. "We understand this is a complicated world, and we need to get energized to find the solutions.”
Dr. Woodson also promised to develop better telehealth capabilities. “Telehealth is going to be an important tool, because it gives us the capability to reach forward and reach back,” he said, “We are a highly distributed system, and we need to develop it as a system, not just as a technology.”
PHS Officials Discuss 50-Year Battle Against Tobacco Use
RADM Lushniak noted that the PHS became the first uniformed service to go tobacco-free while in uniform. Joining the Acting Surgeon General in the presentation was RADM David L. Ashley who discussed how the PHS eliminated tobacco use within its ranks. RADM Ashley outlined 10 guidelines for clinicians to support patients in battling a tobacco addiction.
CAPT Kimberly Elenberg also outlined the steps PHS is taking to help the other uniformed services in their efforts to reduce and eliminate tobacco use. According to CAPT Elenberg, it is essential to recognize the specific and unique deployment challenges that active service members face and the rationales behind tobacco use before being able to reduce its use.
For more information on the 2014 AMSUS Annual Continuing Education Meeting, visit http://amsusmeetings.org/annual-meeting.
Dr. Clancy Outlines VA Blueprint for Change
Carolyn M. Clancy, MD, Interim Under Secretary for Health at the VA outlined strategic aims for reshaping and restructuring into a more unified veteran-focused health care system. The ultimate goal for the plan is to put the veteran in control of his or her health care by providing a single phone number, a website, and well-trained VA employees who understand all the VA’s offerings. According to Dr. Clancy, “[this restructuring's] success will be defined from the veteran’s perspective."
- Operate a health care network that anticipates and meets the needs of veterans;
- Deliver high-quality, veteran-centered care that compares favorably to private sector health care;
- Leverage information technology, analytics, and models of delivery to optimize health care;
- Grow an organizational culture rooted in the VA’s core values and mission and prioritize veterans;
- Foster an environment of continuous learning, responsible risk taking, and personal accountability;
- Advance a model of health care that is personalized, proactive, and patient-driven;
- Lead the nation in research and treatment of military service-related conditions;
- Support innovation in health services through academic affiliations;
- Operate and communicate with integrity, transparency, and accountability; and
- Modernize VA management, including human resources, accounting, and other support services.
An Update on the Defense Health Agency
The Assistant Secretary of Defense for Health Affairs Jonathan Woodson, MD, outlined the strategic challenges and plans for changes at the $50 billion Defense Health Agency (DHA). “Get ready, this train is going to move very fast and you are part of it,” he challenged active service health care providers. "We understand this is a complicated world, and we need to get energized to find the solutions.”
Dr. Woodson also promised to develop better telehealth capabilities. “Telehealth is going to be an important tool, because it gives us the capability to reach forward and reach back,” he said, “We are a highly distributed system, and we need to develop it as a system, not just as a technology.”
PHS Officials Discuss 50-Year Battle Against Tobacco Use
RADM Lushniak noted that the PHS became the first uniformed service to go tobacco-free while in uniform. Joining the Acting Surgeon General in the presentation was RADM David L. Ashley who discussed how the PHS eliminated tobacco use within its ranks. RADM Ashley outlined 10 guidelines for clinicians to support patients in battling a tobacco addiction.
CAPT Kimberly Elenberg also outlined the steps PHS is taking to help the other uniformed services in their efforts to reduce and eliminate tobacco use. According to CAPT Elenberg, it is essential to recognize the specific and unique deployment challenges that active service members face and the rationales behind tobacco use before being able to reduce its use.
For more information on the 2014 AMSUS Annual Continuing Education Meeting, visit http://amsusmeetings.org/annual-meeting.
Acting Surgeon General RADM Boris D. Lushniak on Zeroing Out Tobacco Use
For more information on the 2014 AMSUS Annual Continuing Education Meeting, visit http://amsusmeetings.org/annual-meeting.
Part II: Ebola and the Public Health Service
Part III: National Prevention Strategy
Rear Admiral (RADM) Boris D. Lushniak, MD, MPH, is the Acting United States Surgeon General and oversees the operations of the U.S. Public Health Service Commissioned Corps. He served as Deputy Surgeon General from November 2010 until July 17, 2013, when he assumed the duties of Acting Surgeon General. RADM Lushniak brings 26 years of experience in the PHS to the position. He has served with the Epidemic Intelligence Service and the National Institute for Occupational Safety and Health, both at the CDC. He also served at the FDA as the Chief Medical Officer of the Office of Counterterrorism and later the Assistant Commissioner, Counterterrorism Policy and Director of the Office of Counterterrorism and emerging Threats within the Office of the Commissioner. After Hurricane Katrina, RADM Lushniak served as the HHS representative in San Antonio, Texas.
For more information on the 2014 AMSUS Annual Continuing Education Meeting, visit http://amsusmeetings.org/annual-meeting.
Part II: Ebola and the Public Health Service
Part III: National Prevention Strategy
For more information on the 2014 AMSUS Annual Continuing Education Meeting, visit http://amsusmeetings.org/annual-meeting.
Part II: Ebola and the Public Health Service
Part III: National Prevention Strategy
Rear Admiral (RADM) Boris D. Lushniak, MD, MPH, is the Acting United States Surgeon General and oversees the operations of the U.S. Public Health Service Commissioned Corps. He served as Deputy Surgeon General from November 2010 until July 17, 2013, when he assumed the duties of Acting Surgeon General. RADM Lushniak brings 26 years of experience in the PHS to the position. He has served with the Epidemic Intelligence Service and the National Institute for Occupational Safety and Health, both at the CDC. He also served at the FDA as the Chief Medical Officer of the Office of Counterterrorism and later the Assistant Commissioner, Counterterrorism Policy and Director of the Office of Counterterrorism and emerging Threats within the Office of the Commissioner. After Hurricane Katrina, RADM Lushniak served as the HHS representative in San Antonio, Texas.
Rear Admiral (RADM) Boris D. Lushniak, MD, MPH, is the Acting United States Surgeon General and oversees the operations of the U.S. Public Health Service Commissioned Corps. He served as Deputy Surgeon General from November 2010 until July 17, 2013, when he assumed the duties of Acting Surgeon General. RADM Lushniak brings 26 years of experience in the PHS to the position. He has served with the Epidemic Intelligence Service and the National Institute for Occupational Safety and Health, both at the CDC. He also served at the FDA as the Chief Medical Officer of the Office of Counterterrorism and later the Assistant Commissioner, Counterterrorism Policy and Director of the Office of Counterterrorism and emerging Threats within the Office of the Commissioner. After Hurricane Katrina, RADM Lushniak served as the HHS representative in San Antonio, Texas.
Ebola, Surgeon General Top AMSUS Meeting Agenda
For more information on the 2014 AMSUS Annual Continuing Education Meeting, visit http://amsusmeetings.org/annual-meeting.
For more information on the 2014 AMSUS Annual Continuing Education Meeting, visit http://amsusmeetings.org/annual-meeting.
For more information on the 2014 AMSUS Annual Continuing Education Meeting, visit http://amsusmeetings.org/annual-meeting.
The Challenges of Treating the Military’s “Young Invincibles”
By Reid A. Paul
Providing health care to special operations personnel can pose unique challenges. On one hand, health care providers are tasked with much of the routine care that is the bread and butter of primary care; on the other hand, they need to work with patients who are especially averse to getting the care they need. The term “young invincibles” takes on a whole new meaning with this group.
That way of thinking was abundantly clear in “Special Operations Training: An Atypical Presentation of Aspiration Pneumonia.” Federal Practitioner recently spoke with one of the authors, Capt. Riley J. Burke, DO, USAF, MC (the other author was Michael C. Ott, MD), to better understand the challenges of working with this patient population and to get the story behind this fascinating case study. The audio of the entire conversation is below.
Federal Practitioner will bring you more of these conversations with the authors of original research, program profiles, case studies, and more. Sometimes the article is only the beginning of the story, so listen and let us know what you think. Join the conversation on Facebook and Twitter anytime.
By Reid A. Paul
Providing health care to special operations personnel can pose unique challenges. On one hand, health care providers are tasked with much of the routine care that is the bread and butter of primary care; on the other hand, they need to work with patients who are especially averse to getting the care they need. The term “young invincibles” takes on a whole new meaning with this group.
That way of thinking was abundantly clear in “Special Operations Training: An Atypical Presentation of Aspiration Pneumonia.” Federal Practitioner recently spoke with one of the authors, Capt. Riley J. Burke, DO, USAF, MC (the other author was Michael C. Ott, MD), to better understand the challenges of working with this patient population and to get the story behind this fascinating case study. The audio of the entire conversation is below.
Federal Practitioner will bring you more of these conversations with the authors of original research, program profiles, case studies, and more. Sometimes the article is only the beginning of the story, so listen and let us know what you think. Join the conversation on Facebook and Twitter anytime.
By Reid A. Paul
Providing health care to special operations personnel can pose unique challenges. On one hand, health care providers are tasked with much of the routine care that is the bread and butter of primary care; on the other hand, they need to work with patients who are especially averse to getting the care they need. The term “young invincibles” takes on a whole new meaning with this group.
That way of thinking was abundantly clear in “Special Operations Training: An Atypical Presentation of Aspiration Pneumonia.” Federal Practitioner recently spoke with one of the authors, Capt. Riley J. Burke, DO, USAF, MC (the other author was Michael C. Ott, MD), to better understand the challenges of working with this patient population and to get the story behind this fascinating case study. The audio of the entire conversation is below.
Federal Practitioner will bring you more of these conversations with the authors of original research, program profiles, case studies, and more. Sometimes the article is only the beginning of the story, so listen and let us know what you think. Join the conversation on Facebook and Twitter anytime.