User login
Newborn Screening Programs: What Do Clinicians Need to Know?
Newborn screening programs are public health services aimed at ensuring that the close to 4 million infants born each year in the United States are screened for certain serious disorders at birth. These disorders, albeit rare, are detected in roughly 12,500 newborn babies every year.
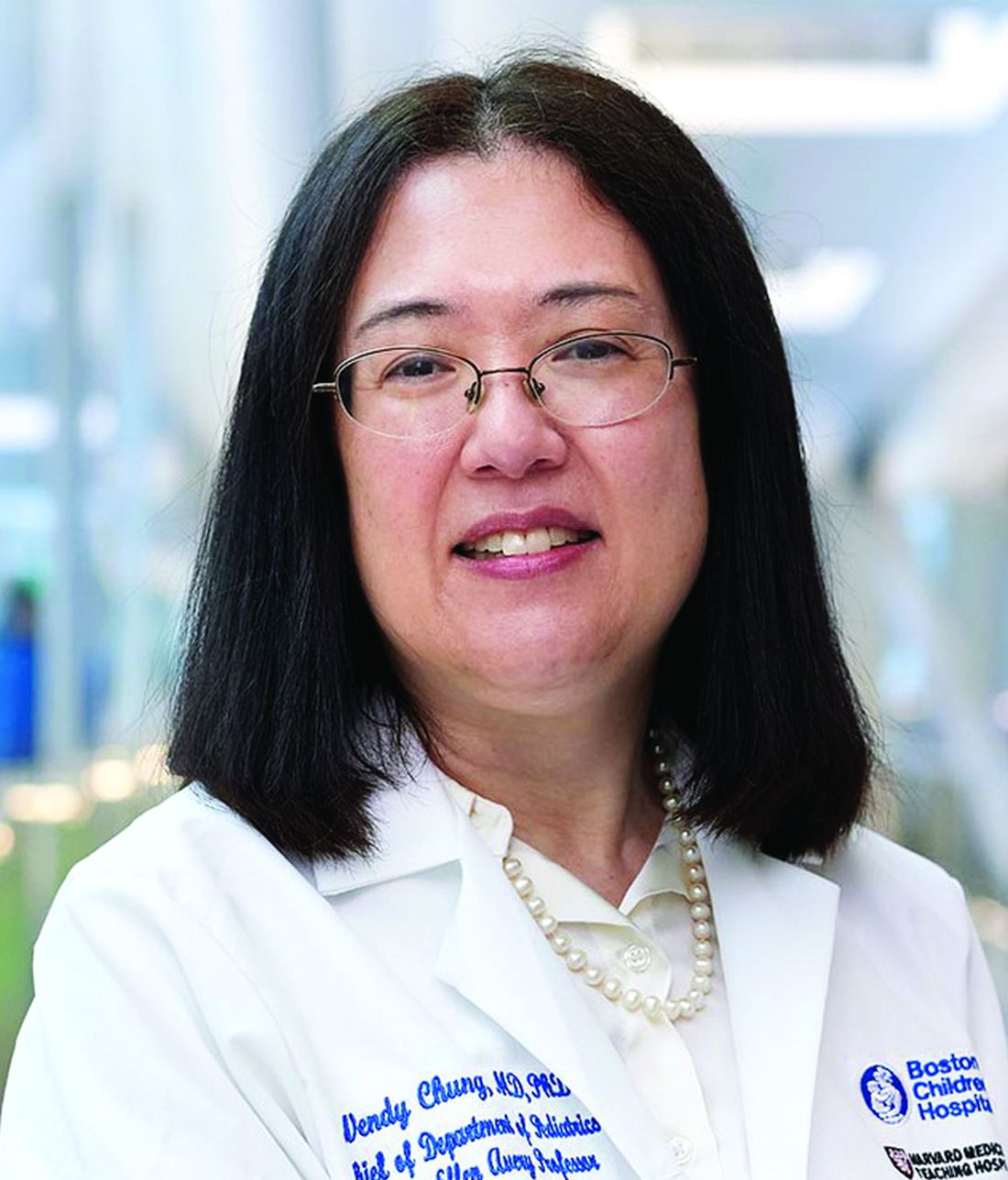
Newborn screening isn’t new, although it has expanded and transformed over the decades. The first newborn screening test was developed in the 1960s to detect phenylketonuria (PKU).1 Since then, the number of conditions screened for has increased, with programs in every US state and territory. “Newborn screening is well established now, not experimental or newfangled,” Wendy Chung, MD, PhD, professor of pediatrics, Harvard Medical School, Boston, Massachusetts, told Neurology Reviews.
In newborn screening, blood drawn from the baby’s heel is applied to specialized filter paper, which is then subjected to several analytical methods, including tandem mass spectrometry and molecular analyses to detect biomarkers for the diseases.2 More recently, genomic sequencing is being piloted as part of consented research studies.3
Newborn screening includes not only biochemical and genetic testing, but also includes noninvasive screening for hearing loss or for critical congenital heart disease using pulse oximetry. And newborn screening goes beyond analysis of a single drop of blood. Rather, “it’s an entire system, with the goal of identifying babies with genetic disorders who otherwise have no obvious symptoms,” said Dr. Chung. Left undetected and untreated, these conditions can be associated with serious adverse outcomes and even death.
Dr. Chung described newborn screening as a “one of the most successful public health programs, supporting health equity by screening almost every US baby after birth and then bringing timely treatments when relevant even before the baby develops symptoms of a disorder.” In this way, newborn screening has “saved lives and decreased disease burdens.”
There are at present 38 core conditions that the Department of Health and Human Services (HHS) regards as the most critical to screen for and 26 secondary conditions associated with these core disorders. This is called the Recommended Uniform Screening Panel (RUSP). Guidance regarding the most appropriate application of newborn screening tests, technologies and standards are provided by the Advisory Committee on Heritable Disorders in Newborns and Children (ACHDNC).
Each state “independently determines which screening tests are performed and what follow-up is provided.”4 Information about which tests are provided by which states can be found on the “Report Card” of the National Organization for Rare Diseases (NORD).
Challenges in Expanding the Current Newborn Screening
One of the major drawbacks in the current system is that “we don’t screen for enough diseases,” according to Zhanzhi Hu, PhD, of the Department of Systems Biology and the Department of Biomedical Information, Columbia University, New York City. “There are over 10,000 rare genetic diseases, but we’re currently screening for fewer than 100,” he told Neurology Reviews. Although in the United States, there are about 700-800 drugs approved for genetic diseases, “we can’t identify patients with these diseases early enough for the ideal window when treatments are most effective.”
Moreover, it’s a “lengthy process” to add new diseases to RUSP. “New conditions are added at the pace of less than one per year, on average — even for the hundreds of diseases for which there are treatments,” he said. “If we keep going at the current pace, we won’t be able to screen for those diseases for another few hundred years.”
Speeding up the pace of including new diseases in newborn screening is challenging because “we have more diseases than we have development dollars for,” Dr. Hu said. “Big pharmaceutical companies are reluctant to invest in rare diseases because the population is so small and it’s hard and expensive to develop such drugs. So if we can identify patients first, there will be more interest in developing treatments down the road.”
On the other hand, for trials to take place, these babies have to be identified in a timely manner — which requires testing. “Right now, we have a deadlock,” Dr. Hu said. “To nominate a disease, you need an approved treatment. But to get a treatment developed, you need to identify patients suitable for a clinical trial. If you have to wait for the symptoms to show up, the damage has already manifested and is irreversible. Our chance is to recognize the disease before symptom onset and then start treatment. I would call this a ‘chicken-and-egg’ problem.”
Dr. Hu is passionate about expanding newborn screening, and he has a very personal reason. Two of his children have a rare genetic disease. “My younger son, now 13 years old, was diagnosed at a much earlier age than my older son, although he had very few symptoms at the time, because his older brother was known to have the disease. As a result of this, his outcome was much better.” By contrast, Dr. Hu’s oldest son — now age 16 — wasn’t diagnosed until he became symptomatic.
His quest led him to join forces with Dr. Chung in conducting the Genomic Uniform-screening Against Rare Disease in All Newborns (Guardian) study, which screens newborns for more than 450 genetic conditions not currently screened as part of the standard newborn screening. To date, the study — which focuses on babies born in New York City — has screened about 11,000 infants.
“To accumulate enough evidence requires screening at least 100,000 babies because one requirement for nominating a disease for national inclusion in RUSP is an ‘N of 1’ study — meaning, to identify at least one positive patient using the proposed screening method in a prospective study,” Dr. Hu explained. “Most are rare diseases with an incidence rate of around one in 100,000. So getting to that magic number of 100,000 participants should enable us to hit that ‘N of 1’ for most diseases.”
The most challenging part, according to Dr. Hu, is the requirement of a prospective study, which means that you have to conduct a large-scale study enrolling tens of thousands of families and babies. If done for individual diseases (as has been the case in the past), “this is a huge cost and very inefficient.”
In reality, he added, the true incidence of these diseases is unclear. “Incidence rates are based on historical data rather than prospective studies. We’ve already seen some diseases show up more frequently than previously recorded, while others have shown up less frequently.”
For example, in the 11,000 babies screened to date, at least three girls with Rett syndrome have been identified, which is “quite a bit higher” than what has previously been identified in the literature (ie, one in 10,000-12,000 births). “This is a highly unmet need for these families because if you can initiate early treatment — at age 1, or even younger — the outcome will be better.”
He noted that there is at least one clinical trial underway for treating Rett syndrome, which has yielded “promising” data.5 “We’re hoping that by screening for diseases like Rett and identifying patients early, this will go hand-in-hand with clinical drug development. It can speed both the approval of the treatment and the addition to the newborn screening list,” Dr. Hu stated.
Screening and Drug Development Working in Tandem
Sequencing technologies have advanced and become more sophisticated as well as less costly, so interest in expanding newborn screening through newborn genome sequencing has increased. In fact, many states currently have incorporated genetic testing into newborn screening for conditions without biochemical markers. Additionally, newborn genomic sequencing is also used for further testing in infants with abnormal biochemical screening results.6
Genomic sequencing “identifies nucleotide changes that are the underlying etiology of monogenic disorders.”6 Its use could potentially enable identification of over 500 genetic disorders for which an newborn screening assay is not currently available, said Dr. Hu.
“Molecular DNA analysis has been integrated into newborn testing either as a first- or second-tier test for several conditions, including cystic fibrosis, severe combined immunodeficiency, and spinal muscular atrophy (SMA),” Dr. Hu said.
Dr. Hu pointed to SMA to illustrate the power and potential of newborn screening working hand-in-hand with the development of new treatments. SMA is a neurodegenerative disorder caused by mutations in SMN1, which encodes survival motor neuron protein (SMN).7 Deficiencies in SMN results in loss of motor neurons with muscle weakness and, often, early death.7A pilot study, on which Dr. Chung was the senior author, used both biochemical and genetic testing of close to 4000 newborns and found an SMA carrier frequency of 1.5%. One newborn was identified who had a homozygous SMN1 gene deletion and two copies of SMN2, strongly suggesting the presence of a severe type 1 SMA phenotype.8
At age 15 days, the baby was treated with nusinersen, an injection administered into the fluid surrounding the spinal cord, and the first FDA-approved genetic treatment for SMA. At the time of study publication, the baby was 12 months old, “meeting all developmental milestones and free of any respiratory issues,” the authors report.
“Screening for SMA — which was added to the RUSP in 2018 — has dramatically transformed what used to be the most common genetic cause of death in children under the age of 2,” Dr. Chung said. “Now, a once-and-done IV infusion of genetic therapy right after screening has transformed everything, taking what used to be a lethal condition and allowing children to grow up healthy.”
Advocating for Inclusion of Diseases With No Current Treatment
At present, any condition included in the RUSP is required to have a treatment, which can be dietary, surgical/procedural, or an FDA-approved drug-based agent. Unfortunately, a wide range of neurodevelopmental diseases still have no known treatments. But lack of availability of treatment shouldn’t invalidate a disease from being included in the RUSP, because even if there is no specific treatment for the condition itself, early intervention can still be initiated to prevent some of the manifestations of the condition, said Dr. Hu.
“For example, most patients with these diseases will sooner or later undergo seizures,” Dr. Hu remarked. “We know that repeated seizures can cause brain damage. If we can diagnose the disease before the seizures start to take place, we can put preventive seizure control interventions in place, even if there is no direct ‘treatment’ for the condition itself.”
Early identification can lead to early intervention, which can have other benefits, Dr. Hu noted. “If we train the brain at a young age, when the brain is most receptive, even though a disease may be progressive and will worsen, those abilities acquired earlier will last longer and remain in place longer. When these skills are acquired later, they’re forgotten sooner. This isn’t a ‘cure,’ but it will help with functional improvement.”
Moreover, parents are “interested in knowing that their child has a condition, even if no treatment is currently available for that disorder, according to our research,” Dr. Chung said. “We found that the parents we interviewed endorsed the nonmedical utility of having access to information, even in the absence of a ‘cure,’ so they could prepare for medical issues that might arise down the road and make informed choices.”9
Nina Gold, MD, director of Prenatal Medical Genetics and associate director for Research for Massachusetts General Brigham Personalized Medicine, Boston, obtained similar findings in her own research, which is currently under review for publication. “We conducted focus groups and one-on-one interviews with parents from diverse racial and socioeconomic backgrounds. At least one parent said they didn’t want to compare their child to other children if their child might have a different developmental trajectory. They stressed that the information would be helpful, even if there was no immediate clinical utility.”
Additionally, there are an “increasing number of fetal therapies for rare disorders, so information about a genetic disease in an older child can be helpful for parents who may go on to have another pregnancy,” Dr. Gold noted.
Dr. Hu detailed several other reasons for including a wider range of disorders in the RUSP. Doing so helps families avoid a “stressful and expensive diagnostic odyssey and also provides equitable access to a diagnosis.” And if these patients are identified early, “we can connect the family with clinical trials already underway or connect them to an organization such as the Accelerating Medicines Partnership (AMP) Program Bespoke Gene Therapy Consortium (AMP BGTC). Bespoke “brings together partners from the public, private, and nonprofit sectors to foster development of gene therapies intended to treat rare genetic diseases, which affect populations too small for viable commercial development.”
Next Steps Following Screening
Rebecca Sponberg, NP, of the Children’s Hospital of Orange County, UC Irvine School of Medicine, California, is part of a broader multidisciplinary team that interfaces with parents whose newborns have screened positive for a genetic disorder. The team also includes a biochemical geneticist, a pediatric neurologist, a pediatric endocrinologist, a genetic counselor, and a social worker.
Different states and locations have different procedures for receiving test results, said Dr. Chung. In some, pediatricians are the ones who receive the results, and they are tasked with the responsibility of making sure the children can start getting appropriate care. In particular, these pediatricians are associated with centers of excellence that specialize in working with families around these conditions. Other facilities have multidisciplinary teams.
Ms. Sponberg gave an example of how the process unfolded with X-linked adrenoleukodystrophy, a rare genetic disorder that affects the white matter of the nervous system and the adrenal cortex.10 “This is the most common peroxisomal disorder, affecting one in 20,000 males,” she said. “There are several different forms of the disorder, but males are most at risk for having the cerebral form, which can lead to neurological regression and hasten death. But the regression does not appear until 4 to 12 years of age.”
A baby who screens positive on the initial newborn screening has repeat testing; and if it’s confirmed, the family meets the entire team to help them understand what the disorder is, what to expect, and how it’s monitored and managed. “Children have to be followed closely with a brain MRI every 6 months to detect brain abnormalities quickly,” Ms. Sponberg explained “And we do regular bloodwork to look for adrenocortical insufficiency.”
A child who shows concerning changes on the MRI or abnormal blood test findings is immediately seen by the relevant specialist. “So far, our center has had one patient who had MRI changes consistent with the cerebral form of the disease and the patient was immediately able to receive a bone marrow transplant,” she reported. “We don’t think this child’s condition would have been picked up so quickly or treatment initiated so rapidly if we hadn’t known about it through newborn screening.”
Educating and Involving Families
Part of the role of clinicians is to provide education regarding newborn screening to families, according to Ms. Sponberg. “In my role, I have to call parents to tell them their child screened positive for a genetic condition and that we need to proceed with confirmatory testing,” she said. “We let them know if there’s a high concern that this might be a true positive for the condition, and we offer them information so they know what to expect.”
Unfortunately, Ms. Sponberg said, in the absence of education, some families are skeptical. “When I call families directly, some think it’s a scam and it can be hard to earn their trust. We need to do a better job educating families, especially our pregnant individuals, that testing will occur and if anything is abnormal, they will receive a call.”
References
1. Levy HL. Robert Guthrie and the Trials and Tribulations of Newborn Screening. Int J Neonatal Screen. 2021 Jan 19;7(1):5. doi: 10.3390/ijns7010005.
2. Chace DH et al. Clinical Chemistry and Dried Blood Spots: Increasing Laboratory Utilization by Improved Understanding of Quantitative Challenges. Bioanalysis. 2014;6(21):2791-2794. doi: 10.4155/bio.14.237.
3. Gold NB et al. Perspectives of Rare Disease Experts on Newborn Genome Sequencing. JAMA Netw Open. 2023 May 1;6(5):e2312231. doi: 10.1001/jamanetworkopen.2023.12231.
4. Weismiller DG. Expanded Newborn Screening: Information and Resources for the Family Physician. Am Fam Physician. 2017 Jun 1;95(11):703-709. https://www.aafp.org/pubs/afp/issues/2017/0601/p703.html.
5. Neul JL et al. Trofinetide for the Treatment of Rett Syndrome: A Randomized Phase 3 Study. Nat Med. 2023 Jun;29(6):1468-1475. doi: 10.1038/s41591-023-02398-1.
6. Chen T et al. Genomic Sequencing as a First-Tier Screening Test and Outcomes of Newborn Screening. JAMA Netw Open. 2023 Sep 5;6(9):e2331162. doi: 10.1001/jamanetworkopen.2023.31162.
7. Mercuri E et al. Spinal Muscular Atrophy. Nat Rev Dis Primers. 2022 Aug 4;8(1):52. doi: 10.1038/s41572-022-00380-8.
8. Kraszewski JN et al. Pilot Study of Population-Based Newborn Screening for Spinal Muscular Atrophy in New York State. Genet Med. 2018 Jun;20(6):608-613. doi: 10.1038/gim.2017.152.
9. Timmins GT et al. Diverse Parental Perspectives of the Social and Educational Needs for Expanding Newborn Screening Through Genomic Sequencing. Public Health Genomics. 2022 Sep 15:1-8. doi: 10.1159/000526382.
10. Turk BR et al. X-linked Adrenoleukodystrophy: Pathology, Pathophysiology, Diagnostic Testing, Newborn Screening and Therapies. Int J Dev Neurosci. 2020 Feb;80(1):52-72. doi: 10.1002/jdn.10003.
Newborn screening programs are public health services aimed at ensuring that the close to 4 million infants born each year in the United States are screened for certain serious disorders at birth. These disorders, albeit rare, are detected in roughly 12,500 newborn babies every year.
Newborn screening isn’t new, although it has expanded and transformed over the decades. The first newborn screening test was developed in the 1960s to detect phenylketonuria (PKU).1 Since then, the number of conditions screened for has increased, with programs in every US state and territory. “Newborn screening is well established now, not experimental or newfangled,” Wendy Chung, MD, PhD, professor of pediatrics, Harvard Medical School, Boston, Massachusetts, told Neurology Reviews.
In newborn screening, blood drawn from the baby’s heel is applied to specialized filter paper, which is then subjected to several analytical methods, including tandem mass spectrometry and molecular analyses to detect biomarkers for the diseases.2 More recently, genomic sequencing is being piloted as part of consented research studies.3
Newborn screening includes not only biochemical and genetic testing, but also includes noninvasive screening for hearing loss or for critical congenital heart disease using pulse oximetry. And newborn screening goes beyond analysis of a single drop of blood. Rather, “it’s an entire system, with the goal of identifying babies with genetic disorders who otherwise have no obvious symptoms,” said Dr. Chung. Left undetected and untreated, these conditions can be associated with serious adverse outcomes and even death.
Dr. Chung described newborn screening as a “one of the most successful public health programs, supporting health equity by screening almost every US baby after birth and then bringing timely treatments when relevant even before the baby develops symptoms of a disorder.” In this way, newborn screening has “saved lives and decreased disease burdens.”
There are at present 38 core conditions that the Department of Health and Human Services (HHS) regards as the most critical to screen for and 26 secondary conditions associated with these core disorders. This is called the Recommended Uniform Screening Panel (RUSP). Guidance regarding the most appropriate application of newborn screening tests, technologies and standards are provided by the Advisory Committee on Heritable Disorders in Newborns and Children (ACHDNC).
Each state “independently determines which screening tests are performed and what follow-up is provided.”4 Information about which tests are provided by which states can be found on the “Report Card” of the National Organization for Rare Diseases (NORD).
Challenges in Expanding the Current Newborn Screening
One of the major drawbacks in the current system is that “we don’t screen for enough diseases,” according to Zhanzhi Hu, PhD, of the Department of Systems Biology and the Department of Biomedical Information, Columbia University, New York City. “There are over 10,000 rare genetic diseases, but we’re currently screening for fewer than 100,” he told Neurology Reviews. Although in the United States, there are about 700-800 drugs approved for genetic diseases, “we can’t identify patients with these diseases early enough for the ideal window when treatments are most effective.”
Moreover, it’s a “lengthy process” to add new diseases to RUSP. “New conditions are added at the pace of less than one per year, on average — even for the hundreds of diseases for which there are treatments,” he said. “If we keep going at the current pace, we won’t be able to screen for those diseases for another few hundred years.”
Speeding up the pace of including new diseases in newborn screening is challenging because “we have more diseases than we have development dollars for,” Dr. Hu said. “Big pharmaceutical companies are reluctant to invest in rare diseases because the population is so small and it’s hard and expensive to develop such drugs. So if we can identify patients first, there will be more interest in developing treatments down the road.”
On the other hand, for trials to take place, these babies have to be identified in a timely manner — which requires testing. “Right now, we have a deadlock,” Dr. Hu said. “To nominate a disease, you need an approved treatment. But to get a treatment developed, you need to identify patients suitable for a clinical trial. If you have to wait for the symptoms to show up, the damage has already manifested and is irreversible. Our chance is to recognize the disease before symptom onset and then start treatment. I would call this a ‘chicken-and-egg’ problem.”
Dr. Hu is passionate about expanding newborn screening, and he has a very personal reason. Two of his children have a rare genetic disease. “My younger son, now 13 years old, was diagnosed at a much earlier age than my older son, although he had very few symptoms at the time, because his older brother was known to have the disease. As a result of this, his outcome was much better.” By contrast, Dr. Hu’s oldest son — now age 16 — wasn’t diagnosed until he became symptomatic.
His quest led him to join forces with Dr. Chung in conducting the Genomic Uniform-screening Against Rare Disease in All Newborns (Guardian) study, which screens newborns for more than 450 genetic conditions not currently screened as part of the standard newborn screening. To date, the study — which focuses on babies born in New York City — has screened about 11,000 infants.
“To accumulate enough evidence requires screening at least 100,000 babies because one requirement for nominating a disease for national inclusion in RUSP is an ‘N of 1’ study — meaning, to identify at least one positive patient using the proposed screening method in a prospective study,” Dr. Hu explained. “Most are rare diseases with an incidence rate of around one in 100,000. So getting to that magic number of 100,000 participants should enable us to hit that ‘N of 1’ for most diseases.”
The most challenging part, according to Dr. Hu, is the requirement of a prospective study, which means that you have to conduct a large-scale study enrolling tens of thousands of families and babies. If done for individual diseases (as has been the case in the past), “this is a huge cost and very inefficient.”
In reality, he added, the true incidence of these diseases is unclear. “Incidence rates are based on historical data rather than prospective studies. We’ve already seen some diseases show up more frequently than previously recorded, while others have shown up less frequently.”
For example, in the 11,000 babies screened to date, at least three girls with Rett syndrome have been identified, which is “quite a bit higher” than what has previously been identified in the literature (ie, one in 10,000-12,000 births). “This is a highly unmet need for these families because if you can initiate early treatment — at age 1, or even younger — the outcome will be better.”
He noted that there is at least one clinical trial underway for treating Rett syndrome, which has yielded “promising” data.5 “We’re hoping that by screening for diseases like Rett and identifying patients early, this will go hand-in-hand with clinical drug development. It can speed both the approval of the treatment and the addition to the newborn screening list,” Dr. Hu stated.
Screening and Drug Development Working in Tandem
Sequencing technologies have advanced and become more sophisticated as well as less costly, so interest in expanding newborn screening through newborn genome sequencing has increased. In fact, many states currently have incorporated genetic testing into newborn screening for conditions without biochemical markers. Additionally, newborn genomic sequencing is also used for further testing in infants with abnormal biochemical screening results.6
Genomic sequencing “identifies nucleotide changes that are the underlying etiology of monogenic disorders.”6 Its use could potentially enable identification of over 500 genetic disorders for which an newborn screening assay is not currently available, said Dr. Hu.
“Molecular DNA analysis has been integrated into newborn testing either as a first- or second-tier test for several conditions, including cystic fibrosis, severe combined immunodeficiency, and spinal muscular atrophy (SMA),” Dr. Hu said.
Dr. Hu pointed to SMA to illustrate the power and potential of newborn screening working hand-in-hand with the development of new treatments. SMA is a neurodegenerative disorder caused by mutations in SMN1, which encodes survival motor neuron protein (SMN).7 Deficiencies in SMN results in loss of motor neurons with muscle weakness and, often, early death.7A pilot study, on which Dr. Chung was the senior author, used both biochemical and genetic testing of close to 4000 newborns and found an SMA carrier frequency of 1.5%. One newborn was identified who had a homozygous SMN1 gene deletion and two copies of SMN2, strongly suggesting the presence of a severe type 1 SMA phenotype.8
At age 15 days, the baby was treated with nusinersen, an injection administered into the fluid surrounding the spinal cord, and the first FDA-approved genetic treatment for SMA. At the time of study publication, the baby was 12 months old, “meeting all developmental milestones and free of any respiratory issues,” the authors report.
“Screening for SMA — which was added to the RUSP in 2018 — has dramatically transformed what used to be the most common genetic cause of death in children under the age of 2,” Dr. Chung said. “Now, a once-and-done IV infusion of genetic therapy right after screening has transformed everything, taking what used to be a lethal condition and allowing children to grow up healthy.”
Advocating for Inclusion of Diseases With No Current Treatment
At present, any condition included in the RUSP is required to have a treatment, which can be dietary, surgical/procedural, or an FDA-approved drug-based agent. Unfortunately, a wide range of neurodevelopmental diseases still have no known treatments. But lack of availability of treatment shouldn’t invalidate a disease from being included in the RUSP, because even if there is no specific treatment for the condition itself, early intervention can still be initiated to prevent some of the manifestations of the condition, said Dr. Hu.
“For example, most patients with these diseases will sooner or later undergo seizures,” Dr. Hu remarked. “We know that repeated seizures can cause brain damage. If we can diagnose the disease before the seizures start to take place, we can put preventive seizure control interventions in place, even if there is no direct ‘treatment’ for the condition itself.”
Early identification can lead to early intervention, which can have other benefits, Dr. Hu noted. “If we train the brain at a young age, when the brain is most receptive, even though a disease may be progressive and will worsen, those abilities acquired earlier will last longer and remain in place longer. When these skills are acquired later, they’re forgotten sooner. This isn’t a ‘cure,’ but it will help with functional improvement.”
Moreover, parents are “interested in knowing that their child has a condition, even if no treatment is currently available for that disorder, according to our research,” Dr. Chung said. “We found that the parents we interviewed endorsed the nonmedical utility of having access to information, even in the absence of a ‘cure,’ so they could prepare for medical issues that might arise down the road and make informed choices.”9
Nina Gold, MD, director of Prenatal Medical Genetics and associate director for Research for Massachusetts General Brigham Personalized Medicine, Boston, obtained similar findings in her own research, which is currently under review for publication. “We conducted focus groups and one-on-one interviews with parents from diverse racial and socioeconomic backgrounds. At least one parent said they didn’t want to compare their child to other children if their child might have a different developmental trajectory. They stressed that the information would be helpful, even if there was no immediate clinical utility.”
Additionally, there are an “increasing number of fetal therapies for rare disorders, so information about a genetic disease in an older child can be helpful for parents who may go on to have another pregnancy,” Dr. Gold noted.
Dr. Hu detailed several other reasons for including a wider range of disorders in the RUSP. Doing so helps families avoid a “stressful and expensive diagnostic odyssey and also provides equitable access to a diagnosis.” And if these patients are identified early, “we can connect the family with clinical trials already underway or connect them to an organization such as the Accelerating Medicines Partnership (AMP) Program Bespoke Gene Therapy Consortium (AMP BGTC). Bespoke “brings together partners from the public, private, and nonprofit sectors to foster development of gene therapies intended to treat rare genetic diseases, which affect populations too small for viable commercial development.”
Next Steps Following Screening
Rebecca Sponberg, NP, of the Children’s Hospital of Orange County, UC Irvine School of Medicine, California, is part of a broader multidisciplinary team that interfaces with parents whose newborns have screened positive for a genetic disorder. The team also includes a biochemical geneticist, a pediatric neurologist, a pediatric endocrinologist, a genetic counselor, and a social worker.
Different states and locations have different procedures for receiving test results, said Dr. Chung. In some, pediatricians are the ones who receive the results, and they are tasked with the responsibility of making sure the children can start getting appropriate care. In particular, these pediatricians are associated with centers of excellence that specialize in working with families around these conditions. Other facilities have multidisciplinary teams.
Ms. Sponberg gave an example of how the process unfolded with X-linked adrenoleukodystrophy, a rare genetic disorder that affects the white matter of the nervous system and the adrenal cortex.10 “This is the most common peroxisomal disorder, affecting one in 20,000 males,” she said. “There are several different forms of the disorder, but males are most at risk for having the cerebral form, which can lead to neurological regression and hasten death. But the regression does not appear until 4 to 12 years of age.”
A baby who screens positive on the initial newborn screening has repeat testing; and if it’s confirmed, the family meets the entire team to help them understand what the disorder is, what to expect, and how it’s monitored and managed. “Children have to be followed closely with a brain MRI every 6 months to detect brain abnormalities quickly,” Ms. Sponberg explained “And we do regular bloodwork to look for adrenocortical insufficiency.”
A child who shows concerning changes on the MRI or abnormal blood test findings is immediately seen by the relevant specialist. “So far, our center has had one patient who had MRI changes consistent with the cerebral form of the disease and the patient was immediately able to receive a bone marrow transplant,” she reported. “We don’t think this child’s condition would have been picked up so quickly or treatment initiated so rapidly if we hadn’t known about it through newborn screening.”
Educating and Involving Families
Part of the role of clinicians is to provide education regarding newborn screening to families, according to Ms. Sponberg. “In my role, I have to call parents to tell them their child screened positive for a genetic condition and that we need to proceed with confirmatory testing,” she said. “We let them know if there’s a high concern that this might be a true positive for the condition, and we offer them information so they know what to expect.”
Unfortunately, Ms. Sponberg said, in the absence of education, some families are skeptical. “When I call families directly, some think it’s a scam and it can be hard to earn their trust. We need to do a better job educating families, especially our pregnant individuals, that testing will occur and if anything is abnormal, they will receive a call.”
References
1. Levy HL. Robert Guthrie and the Trials and Tribulations of Newborn Screening. Int J Neonatal Screen. 2021 Jan 19;7(1):5. doi: 10.3390/ijns7010005.
2. Chace DH et al. Clinical Chemistry and Dried Blood Spots: Increasing Laboratory Utilization by Improved Understanding of Quantitative Challenges. Bioanalysis. 2014;6(21):2791-2794. doi: 10.4155/bio.14.237.
3. Gold NB et al. Perspectives of Rare Disease Experts on Newborn Genome Sequencing. JAMA Netw Open. 2023 May 1;6(5):e2312231. doi: 10.1001/jamanetworkopen.2023.12231.
4. Weismiller DG. Expanded Newborn Screening: Information and Resources for the Family Physician. Am Fam Physician. 2017 Jun 1;95(11):703-709. https://www.aafp.org/pubs/afp/issues/2017/0601/p703.html.
5. Neul JL et al. Trofinetide for the Treatment of Rett Syndrome: A Randomized Phase 3 Study. Nat Med. 2023 Jun;29(6):1468-1475. doi: 10.1038/s41591-023-02398-1.
6. Chen T et al. Genomic Sequencing as a First-Tier Screening Test and Outcomes of Newborn Screening. JAMA Netw Open. 2023 Sep 5;6(9):e2331162. doi: 10.1001/jamanetworkopen.2023.31162.
7. Mercuri E et al. Spinal Muscular Atrophy. Nat Rev Dis Primers. 2022 Aug 4;8(1):52. doi: 10.1038/s41572-022-00380-8.
8. Kraszewski JN et al. Pilot Study of Population-Based Newborn Screening for Spinal Muscular Atrophy in New York State. Genet Med. 2018 Jun;20(6):608-613. doi: 10.1038/gim.2017.152.
9. Timmins GT et al. Diverse Parental Perspectives of the Social and Educational Needs for Expanding Newborn Screening Through Genomic Sequencing. Public Health Genomics. 2022 Sep 15:1-8. doi: 10.1159/000526382.
10. Turk BR et al. X-linked Adrenoleukodystrophy: Pathology, Pathophysiology, Diagnostic Testing, Newborn Screening and Therapies. Int J Dev Neurosci. 2020 Feb;80(1):52-72. doi: 10.1002/jdn.10003.
Newborn screening programs are public health services aimed at ensuring that the close to 4 million infants born each year in the United States are screened for certain serious disorders at birth. These disorders, albeit rare, are detected in roughly 12,500 newborn babies every year.
Newborn screening isn’t new, although it has expanded and transformed over the decades. The first newborn screening test was developed in the 1960s to detect phenylketonuria (PKU).1 Since then, the number of conditions screened for has increased, with programs in every US state and territory. “Newborn screening is well established now, not experimental or newfangled,” Wendy Chung, MD, PhD, professor of pediatrics, Harvard Medical School, Boston, Massachusetts, told Neurology Reviews.
In newborn screening, blood drawn from the baby’s heel is applied to specialized filter paper, which is then subjected to several analytical methods, including tandem mass spectrometry and molecular analyses to detect biomarkers for the diseases.2 More recently, genomic sequencing is being piloted as part of consented research studies.3
Newborn screening includes not only biochemical and genetic testing, but also includes noninvasive screening for hearing loss or for critical congenital heart disease using pulse oximetry. And newborn screening goes beyond analysis of a single drop of blood. Rather, “it’s an entire system, with the goal of identifying babies with genetic disorders who otherwise have no obvious symptoms,” said Dr. Chung. Left undetected and untreated, these conditions can be associated with serious adverse outcomes and even death.
Dr. Chung described newborn screening as a “one of the most successful public health programs, supporting health equity by screening almost every US baby after birth and then bringing timely treatments when relevant even before the baby develops symptoms of a disorder.” In this way, newborn screening has “saved lives and decreased disease burdens.”
There are at present 38 core conditions that the Department of Health and Human Services (HHS) regards as the most critical to screen for and 26 secondary conditions associated with these core disorders. This is called the Recommended Uniform Screening Panel (RUSP). Guidance regarding the most appropriate application of newborn screening tests, technologies and standards are provided by the Advisory Committee on Heritable Disorders in Newborns and Children (ACHDNC).
Each state “independently determines which screening tests are performed and what follow-up is provided.”4 Information about which tests are provided by which states can be found on the “Report Card” of the National Organization for Rare Diseases (NORD).
Challenges in Expanding the Current Newborn Screening
One of the major drawbacks in the current system is that “we don’t screen for enough diseases,” according to Zhanzhi Hu, PhD, of the Department of Systems Biology and the Department of Biomedical Information, Columbia University, New York City. “There are over 10,000 rare genetic diseases, but we’re currently screening for fewer than 100,” he told Neurology Reviews. Although in the United States, there are about 700-800 drugs approved for genetic diseases, “we can’t identify patients with these diseases early enough for the ideal window when treatments are most effective.”
Moreover, it’s a “lengthy process” to add new diseases to RUSP. “New conditions are added at the pace of less than one per year, on average — even for the hundreds of diseases for which there are treatments,” he said. “If we keep going at the current pace, we won’t be able to screen for those diseases for another few hundred years.”
Speeding up the pace of including new diseases in newborn screening is challenging because “we have more diseases than we have development dollars for,” Dr. Hu said. “Big pharmaceutical companies are reluctant to invest in rare diseases because the population is so small and it’s hard and expensive to develop such drugs. So if we can identify patients first, there will be more interest in developing treatments down the road.”
On the other hand, for trials to take place, these babies have to be identified in a timely manner — which requires testing. “Right now, we have a deadlock,” Dr. Hu said. “To nominate a disease, you need an approved treatment. But to get a treatment developed, you need to identify patients suitable for a clinical trial. If you have to wait for the symptoms to show up, the damage has already manifested and is irreversible. Our chance is to recognize the disease before symptom onset and then start treatment. I would call this a ‘chicken-and-egg’ problem.”
Dr. Hu is passionate about expanding newborn screening, and he has a very personal reason. Two of his children have a rare genetic disease. “My younger son, now 13 years old, was diagnosed at a much earlier age than my older son, although he had very few symptoms at the time, because his older brother was known to have the disease. As a result of this, his outcome was much better.” By contrast, Dr. Hu’s oldest son — now age 16 — wasn’t diagnosed until he became symptomatic.
His quest led him to join forces with Dr. Chung in conducting the Genomic Uniform-screening Against Rare Disease in All Newborns (Guardian) study, which screens newborns for more than 450 genetic conditions not currently screened as part of the standard newborn screening. To date, the study — which focuses on babies born in New York City — has screened about 11,000 infants.
“To accumulate enough evidence requires screening at least 100,000 babies because one requirement for nominating a disease for national inclusion in RUSP is an ‘N of 1’ study — meaning, to identify at least one positive patient using the proposed screening method in a prospective study,” Dr. Hu explained. “Most are rare diseases with an incidence rate of around one in 100,000. So getting to that magic number of 100,000 participants should enable us to hit that ‘N of 1’ for most diseases.”
The most challenging part, according to Dr. Hu, is the requirement of a prospective study, which means that you have to conduct a large-scale study enrolling tens of thousands of families and babies. If done for individual diseases (as has been the case in the past), “this is a huge cost and very inefficient.”
In reality, he added, the true incidence of these diseases is unclear. “Incidence rates are based on historical data rather than prospective studies. We’ve already seen some diseases show up more frequently than previously recorded, while others have shown up less frequently.”
For example, in the 11,000 babies screened to date, at least three girls with Rett syndrome have been identified, which is “quite a bit higher” than what has previously been identified in the literature (ie, one in 10,000-12,000 births). “This is a highly unmet need for these families because if you can initiate early treatment — at age 1, or even younger — the outcome will be better.”
He noted that there is at least one clinical trial underway for treating Rett syndrome, which has yielded “promising” data.5 “We’re hoping that by screening for diseases like Rett and identifying patients early, this will go hand-in-hand with clinical drug development. It can speed both the approval of the treatment and the addition to the newborn screening list,” Dr. Hu stated.
Screening and Drug Development Working in Tandem
Sequencing technologies have advanced and become more sophisticated as well as less costly, so interest in expanding newborn screening through newborn genome sequencing has increased. In fact, many states currently have incorporated genetic testing into newborn screening for conditions without biochemical markers. Additionally, newborn genomic sequencing is also used for further testing in infants with abnormal biochemical screening results.6
Genomic sequencing “identifies nucleotide changes that are the underlying etiology of monogenic disorders.”6 Its use could potentially enable identification of over 500 genetic disorders for which an newborn screening assay is not currently available, said Dr. Hu.
“Molecular DNA analysis has been integrated into newborn testing either as a first- or second-tier test for several conditions, including cystic fibrosis, severe combined immunodeficiency, and spinal muscular atrophy (SMA),” Dr. Hu said.
Dr. Hu pointed to SMA to illustrate the power and potential of newborn screening working hand-in-hand with the development of new treatments. SMA is a neurodegenerative disorder caused by mutations in SMN1, which encodes survival motor neuron protein (SMN).7 Deficiencies in SMN results in loss of motor neurons with muscle weakness and, often, early death.7A pilot study, on which Dr. Chung was the senior author, used both biochemical and genetic testing of close to 4000 newborns and found an SMA carrier frequency of 1.5%. One newborn was identified who had a homozygous SMN1 gene deletion and two copies of SMN2, strongly suggesting the presence of a severe type 1 SMA phenotype.8
At age 15 days, the baby was treated with nusinersen, an injection administered into the fluid surrounding the spinal cord, and the first FDA-approved genetic treatment for SMA. At the time of study publication, the baby was 12 months old, “meeting all developmental milestones and free of any respiratory issues,” the authors report.
“Screening for SMA — which was added to the RUSP in 2018 — has dramatically transformed what used to be the most common genetic cause of death in children under the age of 2,” Dr. Chung said. “Now, a once-and-done IV infusion of genetic therapy right after screening has transformed everything, taking what used to be a lethal condition and allowing children to grow up healthy.”
Advocating for Inclusion of Diseases With No Current Treatment
At present, any condition included in the RUSP is required to have a treatment, which can be dietary, surgical/procedural, or an FDA-approved drug-based agent. Unfortunately, a wide range of neurodevelopmental diseases still have no known treatments. But lack of availability of treatment shouldn’t invalidate a disease from being included in the RUSP, because even if there is no specific treatment for the condition itself, early intervention can still be initiated to prevent some of the manifestations of the condition, said Dr. Hu.
“For example, most patients with these diseases will sooner or later undergo seizures,” Dr. Hu remarked. “We know that repeated seizures can cause brain damage. If we can diagnose the disease before the seizures start to take place, we can put preventive seizure control interventions in place, even if there is no direct ‘treatment’ for the condition itself.”
Early identification can lead to early intervention, which can have other benefits, Dr. Hu noted. “If we train the brain at a young age, when the brain is most receptive, even though a disease may be progressive and will worsen, those abilities acquired earlier will last longer and remain in place longer. When these skills are acquired later, they’re forgotten sooner. This isn’t a ‘cure,’ but it will help with functional improvement.”
Moreover, parents are “interested in knowing that their child has a condition, even if no treatment is currently available for that disorder, according to our research,” Dr. Chung said. “We found that the parents we interviewed endorsed the nonmedical utility of having access to information, even in the absence of a ‘cure,’ so they could prepare for medical issues that might arise down the road and make informed choices.”9
Nina Gold, MD, director of Prenatal Medical Genetics and associate director for Research for Massachusetts General Brigham Personalized Medicine, Boston, obtained similar findings in her own research, which is currently under review for publication. “We conducted focus groups and one-on-one interviews with parents from diverse racial and socioeconomic backgrounds. At least one parent said they didn’t want to compare their child to other children if their child might have a different developmental trajectory. They stressed that the information would be helpful, even if there was no immediate clinical utility.”
Additionally, there are an “increasing number of fetal therapies for rare disorders, so information about a genetic disease in an older child can be helpful for parents who may go on to have another pregnancy,” Dr. Gold noted.
Dr. Hu detailed several other reasons for including a wider range of disorders in the RUSP. Doing so helps families avoid a “stressful and expensive diagnostic odyssey and also provides equitable access to a diagnosis.” And if these patients are identified early, “we can connect the family with clinical trials already underway or connect them to an organization such as the Accelerating Medicines Partnership (AMP) Program Bespoke Gene Therapy Consortium (AMP BGTC). Bespoke “brings together partners from the public, private, and nonprofit sectors to foster development of gene therapies intended to treat rare genetic diseases, which affect populations too small for viable commercial development.”
Next Steps Following Screening
Rebecca Sponberg, NP, of the Children’s Hospital of Orange County, UC Irvine School of Medicine, California, is part of a broader multidisciplinary team that interfaces with parents whose newborns have screened positive for a genetic disorder. The team also includes a biochemical geneticist, a pediatric neurologist, a pediatric endocrinologist, a genetic counselor, and a social worker.
Different states and locations have different procedures for receiving test results, said Dr. Chung. In some, pediatricians are the ones who receive the results, and they are tasked with the responsibility of making sure the children can start getting appropriate care. In particular, these pediatricians are associated with centers of excellence that specialize in working with families around these conditions. Other facilities have multidisciplinary teams.
Ms. Sponberg gave an example of how the process unfolded with X-linked adrenoleukodystrophy, a rare genetic disorder that affects the white matter of the nervous system and the adrenal cortex.10 “This is the most common peroxisomal disorder, affecting one in 20,000 males,” she said. “There are several different forms of the disorder, but males are most at risk for having the cerebral form, which can lead to neurological regression and hasten death. But the regression does not appear until 4 to 12 years of age.”
A baby who screens positive on the initial newborn screening has repeat testing; and if it’s confirmed, the family meets the entire team to help them understand what the disorder is, what to expect, and how it’s monitored and managed. “Children have to be followed closely with a brain MRI every 6 months to detect brain abnormalities quickly,” Ms. Sponberg explained “And we do regular bloodwork to look for adrenocortical insufficiency.”
A child who shows concerning changes on the MRI or abnormal blood test findings is immediately seen by the relevant specialist. “So far, our center has had one patient who had MRI changes consistent with the cerebral form of the disease and the patient was immediately able to receive a bone marrow transplant,” she reported. “We don’t think this child’s condition would have been picked up so quickly or treatment initiated so rapidly if we hadn’t known about it through newborn screening.”
Educating and Involving Families
Part of the role of clinicians is to provide education regarding newborn screening to families, according to Ms. Sponberg. “In my role, I have to call parents to tell them their child screened positive for a genetic condition and that we need to proceed with confirmatory testing,” she said. “We let them know if there’s a high concern that this might be a true positive for the condition, and we offer them information so they know what to expect.”
Unfortunately, Ms. Sponberg said, in the absence of education, some families are skeptical. “When I call families directly, some think it’s a scam and it can be hard to earn their trust. We need to do a better job educating families, especially our pregnant individuals, that testing will occur and if anything is abnormal, they will receive a call.”
References
1. Levy HL. Robert Guthrie and the Trials and Tribulations of Newborn Screening. Int J Neonatal Screen. 2021 Jan 19;7(1):5. doi: 10.3390/ijns7010005.
2. Chace DH et al. Clinical Chemistry and Dried Blood Spots: Increasing Laboratory Utilization by Improved Understanding of Quantitative Challenges. Bioanalysis. 2014;6(21):2791-2794. doi: 10.4155/bio.14.237.
3. Gold NB et al. Perspectives of Rare Disease Experts on Newborn Genome Sequencing. JAMA Netw Open. 2023 May 1;6(5):e2312231. doi: 10.1001/jamanetworkopen.2023.12231.
4. Weismiller DG. Expanded Newborn Screening: Information and Resources for the Family Physician. Am Fam Physician. 2017 Jun 1;95(11):703-709. https://www.aafp.org/pubs/afp/issues/2017/0601/p703.html.
5. Neul JL et al. Trofinetide for the Treatment of Rett Syndrome: A Randomized Phase 3 Study. Nat Med. 2023 Jun;29(6):1468-1475. doi: 10.1038/s41591-023-02398-1.
6. Chen T et al. Genomic Sequencing as a First-Tier Screening Test and Outcomes of Newborn Screening. JAMA Netw Open. 2023 Sep 5;6(9):e2331162. doi: 10.1001/jamanetworkopen.2023.31162.
7. Mercuri E et al. Spinal Muscular Atrophy. Nat Rev Dis Primers. 2022 Aug 4;8(1):52. doi: 10.1038/s41572-022-00380-8.
8. Kraszewski JN et al. Pilot Study of Population-Based Newborn Screening for Spinal Muscular Atrophy in New York State. Genet Med. 2018 Jun;20(6):608-613. doi: 10.1038/gim.2017.152.
9. Timmins GT et al. Diverse Parental Perspectives of the Social and Educational Needs for Expanding Newborn Screening Through Genomic Sequencing. Public Health Genomics. 2022 Sep 15:1-8. doi: 10.1159/000526382.
10. Turk BR et al. X-linked Adrenoleukodystrophy: Pathology, Pathophysiology, Diagnostic Testing, Newborn Screening and Therapies. Int J Dev Neurosci. 2020 Feb;80(1):52-72. doi: 10.1002/jdn.10003.
Measles Control So Far in 2024: ‘Not Off to a Great Start’
Just over 2 months into 2024, measles cases in the United States aren’t looking great.
The recent rise in cases across the U.S. is linked to unvaccinated travelers, lower than ideal vaccination rates, and misinformation, experts said.
The Centers for Disease Control and Prevention has identified 45 cases of measles in 17 jurisdictions across the U.S. As of March 7, the federal health agency reported measles cases in Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, New Jersey, New York City, Ohio, Pennsylvania, Virginia, and Washington.
As for the 45 cases, “that’s almost as many as we had for the entire calendar year of 2023,” said Sarah Lim, MD, a medical specialist at the Minnesota Department of Health. “So we’re really not off to a great start.” (For context, there were 58 officially reported measles cases last year.)
Chicago is having a measles outbreak — with eight cases reported so far. All but one case has been linked to a migrant child at a city shelter. Given the potential for rapid spread — measles is relatively rare here but potentially very serious — the CDC sent a team of experts to investigate and to help keep this outbreak from growing further.
Sometimes Deadly
About 30% of children have measles symptoms and about 25% end up hospitalized. Complications include diarrhea, a whole-body rash, ear infections that can lead to permanent deafness, and pneumonia. Pneumonia with measles can be so serious that 1 in 20 affected children die. Measles can also cause inflammation of the brain called encephalitis in about 1 in 1,000 children, sometimes causing epilepsy or permanent brain damage.
As with long COVID, some effects can last beyond the early infection. For example, measles “can wipe out immune memory that protects you against other bacterial and viral pathogens,” Dr. Lim said at a media briefing sponsored by the Infectious Diseases Society of America. This vulnerability to other infections can last up to 3 years after the early infection, she noted.
Overall, measles kills between 1 and 3 people infected per thousand, mostly children.
Vaccine Misinformation Playing a Role
Vaccine misinformation is partly behind the uptick, and while many cases are mild, “this can be a devastating disease,” said Joshua Barocas, MD, associate professor of medicine in the divisions of General Internal Medicine and Infectious Diseases at the University of Colorado School of Medicine.
“I’m a parent myself. Parents are flooded with tons of information, some of that time being misinformation,” he said at the media briefing. “If you are a parent who’s been on the fence [about vaccination], now is the time, given the outbreak potential and the outbreaks that we’re seeing.”
Vaccine misinformation “is about as old as vaccines themselves,” Dr. Lim said. Concerns about the MMR vaccine, which includes measles protection, are not new.
“It does seem to change periodically — new things bubble up, new ideas bubble up, and the problem is that it is like the old saying that ‘a lie can get halfway around the world before the truth can get its boots on.’ ” Social media helps to amplify vaccine misinformation, she said.
“You don’t want to scare people unnecessarily — but reminding people what these childhood diseases really look like and what they do is incredibly important,” Dr. Lim said. “It’s so much easier to see stories about potential side effects of vaccines than it is to see stories about parents whose children were in intensive care for 2 weeks with pneumonia because of a severe case of measles.”
Dr. Barocas said misinformation is sometimes deliberate, sometimes not. Regardless, “our job as infectious disease physicians and public health professionals is not necessarily to put the counternarrative out there, but to continue to advocate for what we know works based on the best science and the best evidence.”
“And there is no reason to believe that vaccines are anything but helpful when it comes to preventing measles,” he noted.
Lifelong Protection in Most Cases
The MMR vaccine, typically given as two doses in childhood, offers 93% and then 97% protection against the highly contagious virus. During the 2022-to-2023 school year, the measles vaccination rate among kindergarten children nationwide was 92%. That sounds like a high rate, Dr. Lim said, “but because measles is so contagious, vaccination rates need to be 95% or higher to contain transmission.”
One person with measles can infect anywhere from 12 to 18 other people, she said. When an infected person coughs or sneezes, tiny droplets spread through the air. “And if someone is unvaccinated and exposed, 9 times out of 10, that person will go on to develop the disease.” She said given the high transmission rate, measles often spreads within families to infect multiple children.
If you know you’re not vaccinated but exposed, the advice is to get the measles shot as quickly as possible. “There is a recommendation to receive the MMR vaccine within 72 hours as post-exposure prophylaxis,” Dr. Lim said. “That’s a tight time window, but if you can do that, it reduces the risk of developing measles significantly.”
If you’re unsure or do not remember getting vaccinated against measles as a young child, your health care provider may be able to search state registries for an answer. If that doesn’t work, getting revaccinated with the MMR vaccine as an adult is an option. “There is no shame in getting caught up now,” Dr. Barocas said.
Dr. Lim agreed. “There is really no downside to getting additional doses.”
A version of this article appeared on WebMD.com.
Just over 2 months into 2024, measles cases in the United States aren’t looking great.
The recent rise in cases across the U.S. is linked to unvaccinated travelers, lower than ideal vaccination rates, and misinformation, experts said.
The Centers for Disease Control and Prevention has identified 45 cases of measles in 17 jurisdictions across the U.S. As of March 7, the federal health agency reported measles cases in Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, New Jersey, New York City, Ohio, Pennsylvania, Virginia, and Washington.
As for the 45 cases, “that’s almost as many as we had for the entire calendar year of 2023,” said Sarah Lim, MD, a medical specialist at the Minnesota Department of Health. “So we’re really not off to a great start.” (For context, there were 58 officially reported measles cases last year.)
Chicago is having a measles outbreak — with eight cases reported so far. All but one case has been linked to a migrant child at a city shelter. Given the potential for rapid spread — measles is relatively rare here but potentially very serious — the CDC sent a team of experts to investigate and to help keep this outbreak from growing further.
Sometimes Deadly
About 30% of children have measles symptoms and about 25% end up hospitalized. Complications include diarrhea, a whole-body rash, ear infections that can lead to permanent deafness, and pneumonia. Pneumonia with measles can be so serious that 1 in 20 affected children die. Measles can also cause inflammation of the brain called encephalitis in about 1 in 1,000 children, sometimes causing epilepsy or permanent brain damage.
As with long COVID, some effects can last beyond the early infection. For example, measles “can wipe out immune memory that protects you against other bacterial and viral pathogens,” Dr. Lim said at a media briefing sponsored by the Infectious Diseases Society of America. This vulnerability to other infections can last up to 3 years after the early infection, she noted.
Overall, measles kills between 1 and 3 people infected per thousand, mostly children.
Vaccine Misinformation Playing a Role
Vaccine misinformation is partly behind the uptick, and while many cases are mild, “this can be a devastating disease,” said Joshua Barocas, MD, associate professor of medicine in the divisions of General Internal Medicine and Infectious Diseases at the University of Colorado School of Medicine.
“I’m a parent myself. Parents are flooded with tons of information, some of that time being misinformation,” he said at the media briefing. “If you are a parent who’s been on the fence [about vaccination], now is the time, given the outbreak potential and the outbreaks that we’re seeing.”
Vaccine misinformation “is about as old as vaccines themselves,” Dr. Lim said. Concerns about the MMR vaccine, which includes measles protection, are not new.
“It does seem to change periodically — new things bubble up, new ideas bubble up, and the problem is that it is like the old saying that ‘a lie can get halfway around the world before the truth can get its boots on.’ ” Social media helps to amplify vaccine misinformation, she said.
“You don’t want to scare people unnecessarily — but reminding people what these childhood diseases really look like and what they do is incredibly important,” Dr. Lim said. “It’s so much easier to see stories about potential side effects of vaccines than it is to see stories about parents whose children were in intensive care for 2 weeks with pneumonia because of a severe case of measles.”
Dr. Barocas said misinformation is sometimes deliberate, sometimes not. Regardless, “our job as infectious disease physicians and public health professionals is not necessarily to put the counternarrative out there, but to continue to advocate for what we know works based on the best science and the best evidence.”
“And there is no reason to believe that vaccines are anything but helpful when it comes to preventing measles,” he noted.
Lifelong Protection in Most Cases
The MMR vaccine, typically given as two doses in childhood, offers 93% and then 97% protection against the highly contagious virus. During the 2022-to-2023 school year, the measles vaccination rate among kindergarten children nationwide was 92%. That sounds like a high rate, Dr. Lim said, “but because measles is so contagious, vaccination rates need to be 95% or higher to contain transmission.”
One person with measles can infect anywhere from 12 to 18 other people, she said. When an infected person coughs or sneezes, tiny droplets spread through the air. “And if someone is unvaccinated and exposed, 9 times out of 10, that person will go on to develop the disease.” She said given the high transmission rate, measles often spreads within families to infect multiple children.
If you know you’re not vaccinated but exposed, the advice is to get the measles shot as quickly as possible. “There is a recommendation to receive the MMR vaccine within 72 hours as post-exposure prophylaxis,” Dr. Lim said. “That’s a tight time window, but if you can do that, it reduces the risk of developing measles significantly.”
If you’re unsure or do not remember getting vaccinated against measles as a young child, your health care provider may be able to search state registries for an answer. If that doesn’t work, getting revaccinated with the MMR vaccine as an adult is an option. “There is no shame in getting caught up now,” Dr. Barocas said.
Dr. Lim agreed. “There is really no downside to getting additional doses.”
A version of this article appeared on WebMD.com.
Just over 2 months into 2024, measles cases in the United States aren’t looking great.
The recent rise in cases across the U.S. is linked to unvaccinated travelers, lower than ideal vaccination rates, and misinformation, experts said.
The Centers for Disease Control and Prevention has identified 45 cases of measles in 17 jurisdictions across the U.S. As of March 7, the federal health agency reported measles cases in Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, New Jersey, New York City, Ohio, Pennsylvania, Virginia, and Washington.
As for the 45 cases, “that’s almost as many as we had for the entire calendar year of 2023,” said Sarah Lim, MD, a medical specialist at the Minnesota Department of Health. “So we’re really not off to a great start.” (For context, there were 58 officially reported measles cases last year.)
Chicago is having a measles outbreak — with eight cases reported so far. All but one case has been linked to a migrant child at a city shelter. Given the potential for rapid spread — measles is relatively rare here but potentially very serious — the CDC sent a team of experts to investigate and to help keep this outbreak from growing further.
Sometimes Deadly
About 30% of children have measles symptoms and about 25% end up hospitalized. Complications include diarrhea, a whole-body rash, ear infections that can lead to permanent deafness, and pneumonia. Pneumonia with measles can be so serious that 1 in 20 affected children die. Measles can also cause inflammation of the brain called encephalitis in about 1 in 1,000 children, sometimes causing epilepsy or permanent brain damage.
As with long COVID, some effects can last beyond the early infection. For example, measles “can wipe out immune memory that protects you against other bacterial and viral pathogens,” Dr. Lim said at a media briefing sponsored by the Infectious Diseases Society of America. This vulnerability to other infections can last up to 3 years after the early infection, she noted.
Overall, measles kills between 1 and 3 people infected per thousand, mostly children.
Vaccine Misinformation Playing a Role
Vaccine misinformation is partly behind the uptick, and while many cases are mild, “this can be a devastating disease,” said Joshua Barocas, MD, associate professor of medicine in the divisions of General Internal Medicine and Infectious Diseases at the University of Colorado School of Medicine.
“I’m a parent myself. Parents are flooded with tons of information, some of that time being misinformation,” he said at the media briefing. “If you are a parent who’s been on the fence [about vaccination], now is the time, given the outbreak potential and the outbreaks that we’re seeing.”
Vaccine misinformation “is about as old as vaccines themselves,” Dr. Lim said. Concerns about the MMR vaccine, which includes measles protection, are not new.
“It does seem to change periodically — new things bubble up, new ideas bubble up, and the problem is that it is like the old saying that ‘a lie can get halfway around the world before the truth can get its boots on.’ ” Social media helps to amplify vaccine misinformation, she said.
“You don’t want to scare people unnecessarily — but reminding people what these childhood diseases really look like and what they do is incredibly important,” Dr. Lim said. “It’s so much easier to see stories about potential side effects of vaccines than it is to see stories about parents whose children were in intensive care for 2 weeks with pneumonia because of a severe case of measles.”
Dr. Barocas said misinformation is sometimes deliberate, sometimes not. Regardless, “our job as infectious disease physicians and public health professionals is not necessarily to put the counternarrative out there, but to continue to advocate for what we know works based on the best science and the best evidence.”
“And there is no reason to believe that vaccines are anything but helpful when it comes to preventing measles,” he noted.
Lifelong Protection in Most Cases
The MMR vaccine, typically given as two doses in childhood, offers 93% and then 97% protection against the highly contagious virus. During the 2022-to-2023 school year, the measles vaccination rate among kindergarten children nationwide was 92%. That sounds like a high rate, Dr. Lim said, “but because measles is so contagious, vaccination rates need to be 95% or higher to contain transmission.”
One person with measles can infect anywhere from 12 to 18 other people, she said. When an infected person coughs or sneezes, tiny droplets spread through the air. “And if someone is unvaccinated and exposed, 9 times out of 10, that person will go on to develop the disease.” She said given the high transmission rate, measles often spreads within families to infect multiple children.
If you know you’re not vaccinated but exposed, the advice is to get the measles shot as quickly as possible. “There is a recommendation to receive the MMR vaccine within 72 hours as post-exposure prophylaxis,” Dr. Lim said. “That’s a tight time window, but if you can do that, it reduces the risk of developing measles significantly.”
If you’re unsure or do not remember getting vaccinated against measles as a young child, your health care provider may be able to search state registries for an answer. If that doesn’t work, getting revaccinated with the MMR vaccine as an adult is an option. “There is no shame in getting caught up now,” Dr. Barocas said.
Dr. Lim agreed. “There is really no downside to getting additional doses.”
A version of this article appeared on WebMD.com.
COVID vaccine is safe, effective for children aged 5-11, Pfizer says
With record numbers of COVID-19 cases being reported in kids, Pfizer and its partner BioNTech have announced that their mRNA vaccine for COVID-19 is safe and appears to generate a protective immune response in children as young as 5.
The companies have been testing a lower dose of the vaccine -- just 10 milligrams -- in children between the ages of 5 and 11. That’s one-third the dose given to adults.
In a clinical trial that included more than 2,200 children, Pfizer says two doses of the vaccines given 3 weeks apart generated a high level of neutralizing antibodies, comparable to the level seen in older children who get a higher dose of the vaccine.
On the advice of its vaccine advisory committee, the Food and Drug Administration asked vaccine makers to include more children in these studies earlier this year.
Rather than testing whether the vaccines are preventing COVID-19 illness in children, as they did in adults, the pharmaceutical companies that make the COVID-19 vaccines are looking at the antibody levels generated by the vaccines instead. The FDA has approved the approach in hopes of speeding vaccines to children, who are now back in school full time in most parts of the United States.
With that in mind, Evan Anderson, MD, a doctor with Children’s Healthcare of Atlanta who is an investigator for the trial — and is therefore kept in the dark about its results — said it’s important to keep in mind that the company didn’t share any efficacy data today.
“We don’t know whether there were cases of COVID-19 among children that were enrolled in the study and how those compared in those who received placebo versus those that received vaccine,” he said.
The company says side effects seen in the trial are comparable to those seen in older children. The company said there were no cases of heart inflammation called myocarditis observed. Pfizer says they plan to send their data to the FDA as soon as possible.
The company says side effects seen in the trial are comparable to those seen in older children. Pfizer says they plan to send their data to the FDA as soon as possible.
“We are pleased to be able to submit data to regulatory authorities for this group of school-aged children before the start of the winter season,” Ugur Sahin, MD, CEO and co-founder of BioNTech, said in a news release. “The safety profile and immunogenicity data in children aged 5 to 11 years vaccinated at a lower dose are consistent with those we have observed with our vaccine in other older populations at a higher dose.”
When asked how soon the FDA might act on Pfizer’s application, Anderson said others had speculated about timelines of 4 to 6 weeks, but he also noted that the FDA could still exercise its authority to ask the company for more information, which could slow the process down.
“As a parent myself, I would love to see that timeline occurring quickly. However, I do want the FDA to fully review the data and ask the necessary questions,” he said. “It’s a little speculative to get too definitive with timelines.”
A version of this article first appeared on WebMD.com.
With record numbers of COVID-19 cases being reported in kids, Pfizer and its partner BioNTech have announced that their mRNA vaccine for COVID-19 is safe and appears to generate a protective immune response in children as young as 5.
The companies have been testing a lower dose of the vaccine -- just 10 milligrams -- in children between the ages of 5 and 11. That’s one-third the dose given to adults.
In a clinical trial that included more than 2,200 children, Pfizer says two doses of the vaccines given 3 weeks apart generated a high level of neutralizing antibodies, comparable to the level seen in older children who get a higher dose of the vaccine.
On the advice of its vaccine advisory committee, the Food and Drug Administration asked vaccine makers to include more children in these studies earlier this year.
Rather than testing whether the vaccines are preventing COVID-19 illness in children, as they did in adults, the pharmaceutical companies that make the COVID-19 vaccines are looking at the antibody levels generated by the vaccines instead. The FDA has approved the approach in hopes of speeding vaccines to children, who are now back in school full time in most parts of the United States.
With that in mind, Evan Anderson, MD, a doctor with Children’s Healthcare of Atlanta who is an investigator for the trial — and is therefore kept in the dark about its results — said it’s important to keep in mind that the company didn’t share any efficacy data today.
“We don’t know whether there were cases of COVID-19 among children that were enrolled in the study and how those compared in those who received placebo versus those that received vaccine,” he said.
The company says side effects seen in the trial are comparable to those seen in older children. The company said there were no cases of heart inflammation called myocarditis observed. Pfizer says they plan to send their data to the FDA as soon as possible.
The company says side effects seen in the trial are comparable to those seen in older children. Pfizer says they plan to send their data to the FDA as soon as possible.
“We are pleased to be able to submit data to regulatory authorities for this group of school-aged children before the start of the winter season,” Ugur Sahin, MD, CEO and co-founder of BioNTech, said in a news release. “The safety profile and immunogenicity data in children aged 5 to 11 years vaccinated at a lower dose are consistent with those we have observed with our vaccine in other older populations at a higher dose.”
When asked how soon the FDA might act on Pfizer’s application, Anderson said others had speculated about timelines of 4 to 6 weeks, but he also noted that the FDA could still exercise its authority to ask the company for more information, which could slow the process down.
“As a parent myself, I would love to see that timeline occurring quickly. However, I do want the FDA to fully review the data and ask the necessary questions,” he said. “It’s a little speculative to get too definitive with timelines.”
A version of this article first appeared on WebMD.com.
With record numbers of COVID-19 cases being reported in kids, Pfizer and its partner BioNTech have announced that their mRNA vaccine for COVID-19 is safe and appears to generate a protective immune response in children as young as 5.
The companies have been testing a lower dose of the vaccine -- just 10 milligrams -- in children between the ages of 5 and 11. That’s one-third the dose given to adults.
In a clinical trial that included more than 2,200 children, Pfizer says two doses of the vaccines given 3 weeks apart generated a high level of neutralizing antibodies, comparable to the level seen in older children who get a higher dose of the vaccine.
On the advice of its vaccine advisory committee, the Food and Drug Administration asked vaccine makers to include more children in these studies earlier this year.
Rather than testing whether the vaccines are preventing COVID-19 illness in children, as they did in adults, the pharmaceutical companies that make the COVID-19 vaccines are looking at the antibody levels generated by the vaccines instead. The FDA has approved the approach in hopes of speeding vaccines to children, who are now back in school full time in most parts of the United States.
With that in mind, Evan Anderson, MD, a doctor with Children’s Healthcare of Atlanta who is an investigator for the trial — and is therefore kept in the dark about its results — said it’s important to keep in mind that the company didn’t share any efficacy data today.
“We don’t know whether there were cases of COVID-19 among children that were enrolled in the study and how those compared in those who received placebo versus those that received vaccine,” he said.
The company says side effects seen in the trial are comparable to those seen in older children. The company said there were no cases of heart inflammation called myocarditis observed. Pfizer says they plan to send their data to the FDA as soon as possible.
The company says side effects seen in the trial are comparable to those seen in older children. Pfizer says they plan to send their data to the FDA as soon as possible.
“We are pleased to be able to submit data to regulatory authorities for this group of school-aged children before the start of the winter season,” Ugur Sahin, MD, CEO and co-founder of BioNTech, said in a news release. “The safety profile and immunogenicity data in children aged 5 to 11 years vaccinated at a lower dose are consistent with those we have observed with our vaccine in other older populations at a higher dose.”
When asked how soon the FDA might act on Pfizer’s application, Anderson said others had speculated about timelines of 4 to 6 weeks, but he also noted that the FDA could still exercise its authority to ask the company for more information, which could slow the process down.
“As a parent myself, I would love to see that timeline occurring quickly. However, I do want the FDA to fully review the data and ask the necessary questions,” he said. “It’s a little speculative to get too definitive with timelines.”
A version of this article first appeared on WebMD.com.
New data on worldwide mental health impact of COVID-19
A new survey that assessed the mental health impact of COVID-19 across the globe shows high rates of trauma and clinical mood disorders related to the pandemic.
The survey, carried out by Sapien Labs, was conducted in eight English-speaking countries and included 49,000 adults. It showed that 57% of respondents experienced some COVID-19–related adversity or trauma.
Roughly one-quarter showed clinical signs of or were at risk for a mood disorder, and 40% described themselves as “succeeding or thriving.”
Those who reported the poorest mental health were young adults and individuals who experienced financial adversity or were unable to receive care for other medical conditions. Nonbinary gender and not getting enough sleep, exercise, or face-to-face socialization also increased the risk for poorer mental well-being.
“The data suggest that there will be long-term fallout from the pandemic on the mental health front,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, said in a press release.
Novel initiative
Dr. Thiagarajan said in an interview that she was running a company that provided microloans to 30,000 villages in India. The company included a research group the goal of which was to understand what predicts success in an individual and in a particular ecosystem, she said – “Why did some villages succeed and others didn’t?”
Dr. Thiagarajan and associates thought that “something big is happening in our life circumstances that causes changes in our brain and felt that we need to understand what they are and how they affect humanity. This was the impetus for founding Sapien Labs. “
The survey, which is part of the company’s Mental Health Million project, is an ongoing research initiative that makes data freely available to other researchers.
The investigators developed a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability,” said Dr. Thiagarajan.
The MHQ consists of 47 “elements of mental well-being.” Respondents’ MHQ scores ranged from –100 to +200. Negative scores indicate poorer mental well-being. Respondents were categorized as clinical, at risk, enduring, managing, succeeding, and thriving.
MHQ scores were computed for six “broad dimensions” of mental health: Core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
Participants were recruited through advertising on Google and Facebook in eight English-speaking countries – Canada, the United States, the United Kingdom, South Africa, Singapore, Australia, New Zealand, and India. The researchers collected demographic information, including age, education, and gender.
First step
The assessment was completed by 48,808 respondents between April 8 and Dec. 31, 2020.
A smaller sample of 2,000 people from the same countries who were polled by the investigators in 2019 was used as a comparator.
Taken together, the overall mental well-being score for 2020 was 8% lower than the score obtained in 2019 from the same countries, and the percentage of respondents who fell into the “clinical” category increased from 14% in 2009 to 26% in 2020.
Residents of Singapore had the highest MHQ score, followed by residents of the United States. At the other extreme, respondents from the United Kingdom and South Africa had the poorest MHQ scores.
“It is important to keep in mind that the English-speaking, Internet-enabled populace is not necessarily representative of each country as a whole,” the authors noted.
Youth hardest hit
whose average MHQ score was 29% lower than those aged at least 65 years.
Worldwide, 70% of respondents aged at least 65 years fell into the categories of “succeeding” or “thriving,” compared with just 17% of those aged 18-24 years.
“We saw a massive trend of diminishing mental well-being in younger individuals, suggesting that some societal force is at play that we need to get to the bottom of,” said Dr. Thiagarajan.
“Young people are still learning how to calibrate themselves in the world, and with age comes maturity, leading to a difference in emotional resilience,” she said.
Highest risk group
Mental well-being was poorest among nonbinary/third-gender respondents. Among those persons, more than 50% were classified as being at clinical risk, in comparison with males and females combined, and their MHQ scores were about 47 points lower.
Nonbinary individuals “are universally doing very poorly, relative to males or females,” said Dr. Thiagarajan. “This is a demographic at very high risk with a lot of suicidal thoughts.”
Respondents who had insufficient sleep, who lacked social interaction, and whose level of exercise was insufficient had lower MHQ scores of an “unexpected magnitude,” compared with their counterparts who had sufficient sleep, more social interaction, and more exercise (a discrepancy of 82, 66, and 46 points, respectively).
Only 3.9% of respondents reported having had COVID-19; 0.7% reported having had a severe case. Yet 57% of respondents reported that the pandemic had had negative consequences with regard to their health or their finances or social situation.
Those who were unable to get care for their other health conditions because of the pandemic (2% of all respondents) reported the worst mental well-being, followed by those who struggled for basic necessities (1.4%).
Reduced household income was associated with a 4% lower score but affected a higher percentage of people (17%). Social isolation was associated with a score of about 20 less. Higher rates of lifetime traumas and adversities were likewise associated with lower scores for mental well-being.
Creative, generous approach
Commenting on the survey results, Ken Duckworth, MD, clinical professor at Harvard Medical School, Boston, and chief medical officer of the National Alliance of Mental Illness, noted that the findings were similar to findings from studies in the United States, which showed disproportionately higher rates of mental health problems in younger individuals. Dr. Duckworth was not involved with the survey.
“The idea that this is an international phenomenon and the broad-stroke finding that younger people are suffering across nations is compelling and important for policymakers to look at,” he said.
Dr. Duckworth noted that although the findings are not “representative” of entire populations in a given country, the report is a “first step in a long journey.”
He described the report as “extremely brilliant, creative, and generous, allowing any academician to get access to the data.”
He saw it “less as a definitive report and more as a directionally informative survey that will yield great fruit over time.”
In a comment, Joshua Morganstein, MD, chair of the American Psychiatric Association’s Committee on the Psychiatric Dimensions of Disaster, said: “One of the important things a document like this highlights is the importance of understanding more where risk [for mental health disorders] is concentrated and what things have occurred or might occur that can buffer against that risk or protect us from it. We see that each nation has similar but also different challenges.”
Dr. Thiagarajan is the founder and chief scientist of Sapien Labs. Her coauthors are employees of Sapien Labs. Dr. Duckworth and Dr. Morganstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new survey that assessed the mental health impact of COVID-19 across the globe shows high rates of trauma and clinical mood disorders related to the pandemic.
The survey, carried out by Sapien Labs, was conducted in eight English-speaking countries and included 49,000 adults. It showed that 57% of respondents experienced some COVID-19–related adversity or trauma.
Roughly one-quarter showed clinical signs of or were at risk for a mood disorder, and 40% described themselves as “succeeding or thriving.”
Those who reported the poorest mental health were young adults and individuals who experienced financial adversity or were unable to receive care for other medical conditions. Nonbinary gender and not getting enough sleep, exercise, or face-to-face socialization also increased the risk for poorer mental well-being.
“The data suggest that there will be long-term fallout from the pandemic on the mental health front,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, said in a press release.
Novel initiative
Dr. Thiagarajan said in an interview that she was running a company that provided microloans to 30,000 villages in India. The company included a research group the goal of which was to understand what predicts success in an individual and in a particular ecosystem, she said – “Why did some villages succeed and others didn’t?”
Dr. Thiagarajan and associates thought that “something big is happening in our life circumstances that causes changes in our brain and felt that we need to understand what they are and how they affect humanity. This was the impetus for founding Sapien Labs. “
The survey, which is part of the company’s Mental Health Million project, is an ongoing research initiative that makes data freely available to other researchers.
The investigators developed a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability,” said Dr. Thiagarajan.
The MHQ consists of 47 “elements of mental well-being.” Respondents’ MHQ scores ranged from –100 to +200. Negative scores indicate poorer mental well-being. Respondents were categorized as clinical, at risk, enduring, managing, succeeding, and thriving.
MHQ scores were computed for six “broad dimensions” of mental health: Core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
Participants were recruited through advertising on Google and Facebook in eight English-speaking countries – Canada, the United States, the United Kingdom, South Africa, Singapore, Australia, New Zealand, and India. The researchers collected demographic information, including age, education, and gender.
First step
The assessment was completed by 48,808 respondents between April 8 and Dec. 31, 2020.
A smaller sample of 2,000 people from the same countries who were polled by the investigators in 2019 was used as a comparator.
Taken together, the overall mental well-being score for 2020 was 8% lower than the score obtained in 2019 from the same countries, and the percentage of respondents who fell into the “clinical” category increased from 14% in 2009 to 26% in 2020.
Residents of Singapore had the highest MHQ score, followed by residents of the United States. At the other extreme, respondents from the United Kingdom and South Africa had the poorest MHQ scores.
“It is important to keep in mind that the English-speaking, Internet-enabled populace is not necessarily representative of each country as a whole,” the authors noted.
Youth hardest hit
whose average MHQ score was 29% lower than those aged at least 65 years.
Worldwide, 70% of respondents aged at least 65 years fell into the categories of “succeeding” or “thriving,” compared with just 17% of those aged 18-24 years.
“We saw a massive trend of diminishing mental well-being in younger individuals, suggesting that some societal force is at play that we need to get to the bottom of,” said Dr. Thiagarajan.
“Young people are still learning how to calibrate themselves in the world, and with age comes maturity, leading to a difference in emotional resilience,” she said.
Highest risk group
Mental well-being was poorest among nonbinary/third-gender respondents. Among those persons, more than 50% were classified as being at clinical risk, in comparison with males and females combined, and their MHQ scores were about 47 points lower.
Nonbinary individuals “are universally doing very poorly, relative to males or females,” said Dr. Thiagarajan. “This is a demographic at very high risk with a lot of suicidal thoughts.”
Respondents who had insufficient sleep, who lacked social interaction, and whose level of exercise was insufficient had lower MHQ scores of an “unexpected magnitude,” compared with their counterparts who had sufficient sleep, more social interaction, and more exercise (a discrepancy of 82, 66, and 46 points, respectively).
Only 3.9% of respondents reported having had COVID-19; 0.7% reported having had a severe case. Yet 57% of respondents reported that the pandemic had had negative consequences with regard to their health or their finances or social situation.
Those who were unable to get care for their other health conditions because of the pandemic (2% of all respondents) reported the worst mental well-being, followed by those who struggled for basic necessities (1.4%).
Reduced household income was associated with a 4% lower score but affected a higher percentage of people (17%). Social isolation was associated with a score of about 20 less. Higher rates of lifetime traumas and adversities were likewise associated with lower scores for mental well-being.
Creative, generous approach
Commenting on the survey results, Ken Duckworth, MD, clinical professor at Harvard Medical School, Boston, and chief medical officer of the National Alliance of Mental Illness, noted that the findings were similar to findings from studies in the United States, which showed disproportionately higher rates of mental health problems in younger individuals. Dr. Duckworth was not involved with the survey.
“The idea that this is an international phenomenon and the broad-stroke finding that younger people are suffering across nations is compelling and important for policymakers to look at,” he said.
Dr. Duckworth noted that although the findings are not “representative” of entire populations in a given country, the report is a “first step in a long journey.”
He described the report as “extremely brilliant, creative, and generous, allowing any academician to get access to the data.”
He saw it “less as a definitive report and more as a directionally informative survey that will yield great fruit over time.”
In a comment, Joshua Morganstein, MD, chair of the American Psychiatric Association’s Committee on the Psychiatric Dimensions of Disaster, said: “One of the important things a document like this highlights is the importance of understanding more where risk [for mental health disorders] is concentrated and what things have occurred or might occur that can buffer against that risk or protect us from it. We see that each nation has similar but also different challenges.”
Dr. Thiagarajan is the founder and chief scientist of Sapien Labs. Her coauthors are employees of Sapien Labs. Dr. Duckworth and Dr. Morganstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new survey that assessed the mental health impact of COVID-19 across the globe shows high rates of trauma and clinical mood disorders related to the pandemic.
The survey, carried out by Sapien Labs, was conducted in eight English-speaking countries and included 49,000 adults. It showed that 57% of respondents experienced some COVID-19–related adversity or trauma.
Roughly one-quarter showed clinical signs of or were at risk for a mood disorder, and 40% described themselves as “succeeding or thriving.”
Those who reported the poorest mental health were young adults and individuals who experienced financial adversity or were unable to receive care for other medical conditions. Nonbinary gender and not getting enough sleep, exercise, or face-to-face socialization also increased the risk for poorer mental well-being.
“The data suggest that there will be long-term fallout from the pandemic on the mental health front,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, said in a press release.
Novel initiative
Dr. Thiagarajan said in an interview that she was running a company that provided microloans to 30,000 villages in India. The company included a research group the goal of which was to understand what predicts success in an individual and in a particular ecosystem, she said – “Why did some villages succeed and others didn’t?”
Dr. Thiagarajan and associates thought that “something big is happening in our life circumstances that causes changes in our brain and felt that we need to understand what they are and how they affect humanity. This was the impetus for founding Sapien Labs. “
The survey, which is part of the company’s Mental Health Million project, is an ongoing research initiative that makes data freely available to other researchers.
The investigators developed a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability,” said Dr. Thiagarajan.
The MHQ consists of 47 “elements of mental well-being.” Respondents’ MHQ scores ranged from –100 to +200. Negative scores indicate poorer mental well-being. Respondents were categorized as clinical, at risk, enduring, managing, succeeding, and thriving.
MHQ scores were computed for six “broad dimensions” of mental health: Core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
Participants were recruited through advertising on Google and Facebook in eight English-speaking countries – Canada, the United States, the United Kingdom, South Africa, Singapore, Australia, New Zealand, and India. The researchers collected demographic information, including age, education, and gender.
First step
The assessment was completed by 48,808 respondents between April 8 and Dec. 31, 2020.
A smaller sample of 2,000 people from the same countries who were polled by the investigators in 2019 was used as a comparator.
Taken together, the overall mental well-being score for 2020 was 8% lower than the score obtained in 2019 from the same countries, and the percentage of respondents who fell into the “clinical” category increased from 14% in 2009 to 26% in 2020.
Residents of Singapore had the highest MHQ score, followed by residents of the United States. At the other extreme, respondents from the United Kingdom and South Africa had the poorest MHQ scores.
“It is important to keep in mind that the English-speaking, Internet-enabled populace is not necessarily representative of each country as a whole,” the authors noted.
Youth hardest hit
whose average MHQ score was 29% lower than those aged at least 65 years.
Worldwide, 70% of respondents aged at least 65 years fell into the categories of “succeeding” or “thriving,” compared with just 17% of those aged 18-24 years.
“We saw a massive trend of diminishing mental well-being in younger individuals, suggesting that some societal force is at play that we need to get to the bottom of,” said Dr. Thiagarajan.
“Young people are still learning how to calibrate themselves in the world, and with age comes maturity, leading to a difference in emotional resilience,” she said.
Highest risk group
Mental well-being was poorest among nonbinary/third-gender respondents. Among those persons, more than 50% were classified as being at clinical risk, in comparison with males and females combined, and their MHQ scores were about 47 points lower.
Nonbinary individuals “are universally doing very poorly, relative to males or females,” said Dr. Thiagarajan. “This is a demographic at very high risk with a lot of suicidal thoughts.”
Respondents who had insufficient sleep, who lacked social interaction, and whose level of exercise was insufficient had lower MHQ scores of an “unexpected magnitude,” compared with their counterparts who had sufficient sleep, more social interaction, and more exercise (a discrepancy of 82, 66, and 46 points, respectively).
Only 3.9% of respondents reported having had COVID-19; 0.7% reported having had a severe case. Yet 57% of respondents reported that the pandemic had had negative consequences with regard to their health or their finances or social situation.
Those who were unable to get care for their other health conditions because of the pandemic (2% of all respondents) reported the worst mental well-being, followed by those who struggled for basic necessities (1.4%).
Reduced household income was associated with a 4% lower score but affected a higher percentage of people (17%). Social isolation was associated with a score of about 20 less. Higher rates of lifetime traumas and adversities were likewise associated with lower scores for mental well-being.
Creative, generous approach
Commenting on the survey results, Ken Duckworth, MD, clinical professor at Harvard Medical School, Boston, and chief medical officer of the National Alliance of Mental Illness, noted that the findings were similar to findings from studies in the United States, which showed disproportionately higher rates of mental health problems in younger individuals. Dr. Duckworth was not involved with the survey.
“The idea that this is an international phenomenon and the broad-stroke finding that younger people are suffering across nations is compelling and important for policymakers to look at,” he said.
Dr. Duckworth noted that although the findings are not “representative” of entire populations in a given country, the report is a “first step in a long journey.”
He described the report as “extremely brilliant, creative, and generous, allowing any academician to get access to the data.”
He saw it “less as a definitive report and more as a directionally informative survey that will yield great fruit over time.”
In a comment, Joshua Morganstein, MD, chair of the American Psychiatric Association’s Committee on the Psychiatric Dimensions of Disaster, said: “One of the important things a document like this highlights is the importance of understanding more where risk [for mental health disorders] is concentrated and what things have occurred or might occur that can buffer against that risk or protect us from it. We see that each nation has similar but also different challenges.”
Dr. Thiagarajan is the founder and chief scientist of Sapien Labs. Her coauthors are employees of Sapien Labs. Dr. Duckworth and Dr. Morganstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Peer-Review Transparency
Federal health care providers live under a microscope, so it seems only fair that we at Fed Pract honor that reality and open ourselves up to scrutiny as well.1 We hope that by shedding light on our peer-review process and manuscript acceptance rate, we will not only highlight our accomplishments, but identify areas for improvement.
Free access to Fed Pract content has always been our priority. While many journals charge authors or readers, Fed Pract has been and will remain free for readers and authors.2 Advertising enables the journal to support this free model of publishing, but we take care to ensure that advertisements do not influence content in any way. Our advertising policy can be found at www.mdedge.com/fedprac/page/advertising.
In January 2019, Fed Pract placed > 400 peer-reviewed articles published since January 2015 in the PubMed Central (PMC) database (ncbi.nlm.nih.gov/pmc). The full text of these and all future Fed Pract peer-reviewed articles will be available at PMC (no registration required), and the citations also will be included in PubMed. We hope that this process will make it even easier for anyone to access our authors’ works.
In 2018 about 36,000 federal health care providers (HCPs) received hard copies of this journal. The print journal is free, but circulation is limited to HCPs who work at the US Department of Veterans Affairs (VA), US Department of Defense (DoD), and the US Public Health Service (PHS). The mdedge.com/fedprac website, which includes every article published since 2003, had 1.4 million page views in 2018. After reading 3 online articles, readers in the US are asked to complete a simple registration form to help us better customize the reader experience. In some cases, international readers may be asked to pay for access to articles online; however, any VA, DoD, or PHS officer stationed overseas can contact the editorial staff (fedprac@mdedge.com) to ensure that they can access the articles for free.
In 2018 the journal received 164 manuscripts and published 94 articles written by 357 different federal HCPs. The 164 manuscript submissions represented a 45% growth over previous years. Not surprisingly, the increased rate of submissions began shortly after the May 2018 announcement that journal articles would be included in PMC. Most of those articles (83%) were submitted unsolicited.
Fed Pract has always prided itself on being an early promoter of interdisciplinary health care professional publications. Nearly half of its listed authors were physicians (48%), while pharmacists made up the next largest cohort (18%). There were smaller numbers of PhDs, nurses, social workers, and physical therapists. The majority were written by HCPs affiliated with the VA (95% of articles and 93% of authors), and no articles in 2018 were written by PHS officers. Physicians comprise about two-thirds of the audience, while pharmacists make up 17% and nurses 9%. PHS and DoD HCPs make up 19% of the Fed Pract audience, suggesting that the journal needs to do more work to encourage these HCPs to contribute articles to the journal.3
Articles published in 2018 covered a broad range of topics from “Anesthesia Care Practice Models in the VHA” and “Army Behavioral Health System” to “Vitreous Hemorrhage in the Setting of a Vascular Loop” and “A Workforce Assessment of VA Home-Based Primary Care Pharmacists.” Categorizing the articles is a challenge. Few health care topics fit neatly into a single topic or specialty. This is especially true in federal health care where much of the care is delivered by multidisciplinary patient-centered medical homes or patient aligned care teams. Nevertheless, a few broad outlines can be discerned. Articles were roughly split between primary care and hospital-based and/or specialty care topics; one-quarter of the articles were case studies or case series articles, and about 20% were editorials or opinion columns. Nineteen articles dealt explicitly with chronic conditions, and 10 articles focused on mental health care.
Peer reviewers are an essential part of the process. Reviewers are blinded to the identityof the authors, ensuring fairness and reducing potential conflicts of interest. We are extremely grateful to each and every reviewer for the time and energy they contribute to the journal. Peer reviewers do not get nearly enough recognition for their important work. In 2018 Fed Pract invited 1,205 reviewers for 164 manuscript submissions and 94 manuscript revisions. More than 200 different reviewers submitted 487 reviews with a median (SD) of 2 reviews (1.8) and a range of 1 to 10. The top 20 reviewers completed 134 reviews with a median (SD) of 6 reviews (1.2). The results stand in contrast to some journals that must offer many invitations per review and depend on a small number of reviewers.1,4-6
The reviewers recommended to reject 14% and to revise 26% of the articles, which is a much lower rejection rate than many other journals (Table).4
These data suggest that Fed Pract and its peer-review process is on a sound foundation but needs to make improvements. Moving into 2019, the journal expects that an increasing number of submissions will require a higher rejection rate. Moreover, we will need to do a better job reaching out to underrepresented portions of our audience. To decrease the time to publication for accepted manuscripts, in 2019 we will publish more articles online ahead of the print publication as we strive to improve the experience for authors, reviewers, readers, and the entire Fed Pract audience.
None of this work can be done without our small and dedicated staff. I would like to thank Managing Editor Joyce Brody who sent out each and every one of those reviewer invitations, Deputy Editor Robert Fee, who manages the special issues, Web Editor Teraya Smith, who runs our entire digital operation, and of course, Editor in Chief Cynthia Geppert, who oversees it all. Finally, it is important that you let us know how we are doing and whether we are meeting your needs. Visit mdedge.com/fedprac to take the readership survey or reach out to me at rpaul@mdedge.com.
1. Geppert CMA. Caring under a microscope. Fed Pract. 2018;35(7):6-7.
2. Smith R. Peer review: a flawed process at the heart of science and journals. J R Soc Med. 2006;99(4):178-182.
3. BPA Worldwide. Federal Practitioner brand report for the 6 month period ending June 2018. https://www.frontlinemedcom.com/wp-content/uploads/FEDPRAC_BPA.pdf. Updated June 2018. Accessed March 5, 2019.
4. Fontanarosa PB, Bauchner H, Golub RM. Thank you to JAMA authors, peer reviewers, and readers. JAMA. 2017;317(8):812-813.
5. Publons, Clarivate Analytics. 2018 global state of peer review. https://publons.com/static/Publons-Global-State-Of-Peer-Review-2018.pdf. Published September 2018. Accessed March 5, 2019.
6. Malcom D. It’s time we fix the peer review system. Am J Pharm Educ. 2018;82(5):7144.
Federal health care providers live under a microscope, so it seems only fair that we at Fed Pract honor that reality and open ourselves up to scrutiny as well.1 We hope that by shedding light on our peer-review process and manuscript acceptance rate, we will not only highlight our accomplishments, but identify areas for improvement.
Free access to Fed Pract content has always been our priority. While many journals charge authors or readers, Fed Pract has been and will remain free for readers and authors.2 Advertising enables the journal to support this free model of publishing, but we take care to ensure that advertisements do not influence content in any way. Our advertising policy can be found at www.mdedge.com/fedprac/page/advertising.
In January 2019, Fed Pract placed > 400 peer-reviewed articles published since January 2015 in the PubMed Central (PMC) database (ncbi.nlm.nih.gov/pmc). The full text of these and all future Fed Pract peer-reviewed articles will be available at PMC (no registration required), and the citations also will be included in PubMed. We hope that this process will make it even easier for anyone to access our authors’ works.
In 2018 about 36,000 federal health care providers (HCPs) received hard copies of this journal. The print journal is free, but circulation is limited to HCPs who work at the US Department of Veterans Affairs (VA), US Department of Defense (DoD), and the US Public Health Service (PHS). The mdedge.com/fedprac website, which includes every article published since 2003, had 1.4 million page views in 2018. After reading 3 online articles, readers in the US are asked to complete a simple registration form to help us better customize the reader experience. In some cases, international readers may be asked to pay for access to articles online; however, any VA, DoD, or PHS officer stationed overseas can contact the editorial staff (fedprac@mdedge.com) to ensure that they can access the articles for free.
In 2018 the journal received 164 manuscripts and published 94 articles written by 357 different federal HCPs. The 164 manuscript submissions represented a 45% growth over previous years. Not surprisingly, the increased rate of submissions began shortly after the May 2018 announcement that journal articles would be included in PMC. Most of those articles (83%) were submitted unsolicited.
Fed Pract has always prided itself on being an early promoter of interdisciplinary health care professional publications. Nearly half of its listed authors were physicians (48%), while pharmacists made up the next largest cohort (18%). There were smaller numbers of PhDs, nurses, social workers, and physical therapists. The majority were written by HCPs affiliated with the VA (95% of articles and 93% of authors), and no articles in 2018 were written by PHS officers. Physicians comprise about two-thirds of the audience, while pharmacists make up 17% and nurses 9%. PHS and DoD HCPs make up 19% of the Fed Pract audience, suggesting that the journal needs to do more work to encourage these HCPs to contribute articles to the journal.3
Articles published in 2018 covered a broad range of topics from “Anesthesia Care Practice Models in the VHA” and “Army Behavioral Health System” to “Vitreous Hemorrhage in the Setting of a Vascular Loop” and “A Workforce Assessment of VA Home-Based Primary Care Pharmacists.” Categorizing the articles is a challenge. Few health care topics fit neatly into a single topic or specialty. This is especially true in federal health care where much of the care is delivered by multidisciplinary patient-centered medical homes or patient aligned care teams. Nevertheless, a few broad outlines can be discerned. Articles were roughly split between primary care and hospital-based and/or specialty care topics; one-quarter of the articles were case studies or case series articles, and about 20% were editorials or opinion columns. Nineteen articles dealt explicitly with chronic conditions, and 10 articles focused on mental health care.
Peer reviewers are an essential part of the process. Reviewers are blinded to the identityof the authors, ensuring fairness and reducing potential conflicts of interest. We are extremely grateful to each and every reviewer for the time and energy they contribute to the journal. Peer reviewers do not get nearly enough recognition for their important work. In 2018 Fed Pract invited 1,205 reviewers for 164 manuscript submissions and 94 manuscript revisions. More than 200 different reviewers submitted 487 reviews with a median (SD) of 2 reviews (1.8) and a range of 1 to 10. The top 20 reviewers completed 134 reviews with a median (SD) of 6 reviews (1.2). The results stand in contrast to some journals that must offer many invitations per review and depend on a small number of reviewers.1,4-6
The reviewers recommended to reject 14% and to revise 26% of the articles, which is a much lower rejection rate than many other journals (Table).4
These data suggest that Fed Pract and its peer-review process is on a sound foundation but needs to make improvements. Moving into 2019, the journal expects that an increasing number of submissions will require a higher rejection rate. Moreover, we will need to do a better job reaching out to underrepresented portions of our audience. To decrease the time to publication for accepted manuscripts, in 2019 we will publish more articles online ahead of the print publication as we strive to improve the experience for authors, reviewers, readers, and the entire Fed Pract audience.
None of this work can be done without our small and dedicated staff. I would like to thank Managing Editor Joyce Brody who sent out each and every one of those reviewer invitations, Deputy Editor Robert Fee, who manages the special issues, Web Editor Teraya Smith, who runs our entire digital operation, and of course, Editor in Chief Cynthia Geppert, who oversees it all. Finally, it is important that you let us know how we are doing and whether we are meeting your needs. Visit mdedge.com/fedprac to take the readership survey or reach out to me at rpaul@mdedge.com.
Federal health care providers live under a microscope, so it seems only fair that we at Fed Pract honor that reality and open ourselves up to scrutiny as well.1 We hope that by shedding light on our peer-review process and manuscript acceptance rate, we will not only highlight our accomplishments, but identify areas for improvement.
Free access to Fed Pract content has always been our priority. While many journals charge authors or readers, Fed Pract has been and will remain free for readers and authors.2 Advertising enables the journal to support this free model of publishing, but we take care to ensure that advertisements do not influence content in any way. Our advertising policy can be found at www.mdedge.com/fedprac/page/advertising.
In January 2019, Fed Pract placed > 400 peer-reviewed articles published since January 2015 in the PubMed Central (PMC) database (ncbi.nlm.nih.gov/pmc). The full text of these and all future Fed Pract peer-reviewed articles will be available at PMC (no registration required), and the citations also will be included in PubMed. We hope that this process will make it even easier for anyone to access our authors’ works.
In 2018 about 36,000 federal health care providers (HCPs) received hard copies of this journal. The print journal is free, but circulation is limited to HCPs who work at the US Department of Veterans Affairs (VA), US Department of Defense (DoD), and the US Public Health Service (PHS). The mdedge.com/fedprac website, which includes every article published since 2003, had 1.4 million page views in 2018. After reading 3 online articles, readers in the US are asked to complete a simple registration form to help us better customize the reader experience. In some cases, international readers may be asked to pay for access to articles online; however, any VA, DoD, or PHS officer stationed overseas can contact the editorial staff (fedprac@mdedge.com) to ensure that they can access the articles for free.
In 2018 the journal received 164 manuscripts and published 94 articles written by 357 different federal HCPs. The 164 manuscript submissions represented a 45% growth over previous years. Not surprisingly, the increased rate of submissions began shortly after the May 2018 announcement that journal articles would be included in PMC. Most of those articles (83%) were submitted unsolicited.
Fed Pract has always prided itself on being an early promoter of interdisciplinary health care professional publications. Nearly half of its listed authors were physicians (48%), while pharmacists made up the next largest cohort (18%). There were smaller numbers of PhDs, nurses, social workers, and physical therapists. The majority were written by HCPs affiliated with the VA (95% of articles and 93% of authors), and no articles in 2018 were written by PHS officers. Physicians comprise about two-thirds of the audience, while pharmacists make up 17% and nurses 9%. PHS and DoD HCPs make up 19% of the Fed Pract audience, suggesting that the journal needs to do more work to encourage these HCPs to contribute articles to the journal.3
Articles published in 2018 covered a broad range of topics from “Anesthesia Care Practice Models in the VHA” and “Army Behavioral Health System” to “Vitreous Hemorrhage in the Setting of a Vascular Loop” and “A Workforce Assessment of VA Home-Based Primary Care Pharmacists.” Categorizing the articles is a challenge. Few health care topics fit neatly into a single topic or specialty. This is especially true in federal health care where much of the care is delivered by multidisciplinary patient-centered medical homes or patient aligned care teams. Nevertheless, a few broad outlines can be discerned. Articles were roughly split between primary care and hospital-based and/or specialty care topics; one-quarter of the articles were case studies or case series articles, and about 20% were editorials or opinion columns. Nineteen articles dealt explicitly with chronic conditions, and 10 articles focused on mental health care.
Peer reviewers are an essential part of the process. Reviewers are blinded to the identityof the authors, ensuring fairness and reducing potential conflicts of interest. We are extremely grateful to each and every reviewer for the time and energy they contribute to the journal. Peer reviewers do not get nearly enough recognition for their important work. In 2018 Fed Pract invited 1,205 reviewers for 164 manuscript submissions and 94 manuscript revisions. More than 200 different reviewers submitted 487 reviews with a median (SD) of 2 reviews (1.8) and a range of 1 to 10. The top 20 reviewers completed 134 reviews with a median (SD) of 6 reviews (1.2). The results stand in contrast to some journals that must offer many invitations per review and depend on a small number of reviewers.1,4-6
The reviewers recommended to reject 14% and to revise 26% of the articles, which is a much lower rejection rate than many other journals (Table).4
These data suggest that Fed Pract and its peer-review process is on a sound foundation but needs to make improvements. Moving into 2019, the journal expects that an increasing number of submissions will require a higher rejection rate. Moreover, we will need to do a better job reaching out to underrepresented portions of our audience. To decrease the time to publication for accepted manuscripts, in 2019 we will publish more articles online ahead of the print publication as we strive to improve the experience for authors, reviewers, readers, and the entire Fed Pract audience.
None of this work can be done without our small and dedicated staff. I would like to thank Managing Editor Joyce Brody who sent out each and every one of those reviewer invitations, Deputy Editor Robert Fee, who manages the special issues, Web Editor Teraya Smith, who runs our entire digital operation, and of course, Editor in Chief Cynthia Geppert, who oversees it all. Finally, it is important that you let us know how we are doing and whether we are meeting your needs. Visit mdedge.com/fedprac to take the readership survey or reach out to me at rpaul@mdedge.com.
1. Geppert CMA. Caring under a microscope. Fed Pract. 2018;35(7):6-7.
2. Smith R. Peer review: a flawed process at the heart of science and journals. J R Soc Med. 2006;99(4):178-182.
3. BPA Worldwide. Federal Practitioner brand report for the 6 month period ending June 2018. https://www.frontlinemedcom.com/wp-content/uploads/FEDPRAC_BPA.pdf. Updated June 2018. Accessed March 5, 2019.
4. Fontanarosa PB, Bauchner H, Golub RM. Thank you to JAMA authors, peer reviewers, and readers. JAMA. 2017;317(8):812-813.
5. Publons, Clarivate Analytics. 2018 global state of peer review. https://publons.com/static/Publons-Global-State-Of-Peer-Review-2018.pdf. Published September 2018. Accessed March 5, 2019.
6. Malcom D. It’s time we fix the peer review system. Am J Pharm Educ. 2018;82(5):7144.
1. Geppert CMA. Caring under a microscope. Fed Pract. 2018;35(7):6-7.
2. Smith R. Peer review: a flawed process at the heart of science and journals. J R Soc Med. 2006;99(4):178-182.
3. BPA Worldwide. Federal Practitioner brand report for the 6 month period ending June 2018. https://www.frontlinemedcom.com/wp-content/uploads/FEDPRAC_BPA.pdf. Updated June 2018. Accessed March 5, 2019.
4. Fontanarosa PB, Bauchner H, Golub RM. Thank you to JAMA authors, peer reviewers, and readers. JAMA. 2017;317(8):812-813.
5. Publons, Clarivate Analytics. 2018 global state of peer review. https://publons.com/static/Publons-Global-State-Of-Peer-Review-2018.pdf. Published September 2018. Accessed March 5, 2019.
6. Malcom D. It’s time we fix the peer review system. Am J Pharm Educ. 2018;82(5):7144.
Patient Knowledge of and Barriers to Breast, Colon, and Cervical Cancer Screenings: A Cross-Sectional Survey of TRICARE Beneficiaries (FULL)
The National Defense Appropriations Act for fiscal year 2009, Subtitle B, waived copayments for preventive cancer screening services for all TRICARE beneficiaries, excluding Medicare-eligible beneficiaries.1 These preventive services include screening for colorectal cancer (CRC), breast cancer, and cervical cancer based on current guidelines (eAppendix1).
Despite having unrestricted access to these cancer screenings, TRICARE Prime beneficiaries report overall screening completion rates that are below the national commercial benchmarks established by the Healthcare Effectiveness Data and Information Set (HEDIS) for all 3 cancer types.2 Specifically, among TRICARE Prime beneficiaries enrolled in the western region of the U.S. in October 2013, the reported breast cancer screening rate was 61.6% (43,138/69,976) for women aged 42 to 69 years, which is well below the HEDIS 75th percentile of 76%. Similarly, the reported rate of cervical cancer screening among women aged 24 to 64 years was 68.3% (63,523/92,946), well below the HEDIS 75th percentile of 79%. Last, the reported rate of CRC screening among male and female TRICARE Prime members aged 51 to 75 years was 61.6% (52,860/85,827), also below the 2013 HEDIS 75th percentile of 63% based on internal review of TRICARE data used for HEDIS reporting.
Given the reported low screening rates, the Defense Health Agency (DHA) performed a cross-sectional survey to assess TRICARE Prime West region beneficiaries’ knowledge and understanding of preventive health screening, specifically for breast cancer, cervical cancer, and CRC, and to identify any potential barriers to access for these screenings.
Methods
A mostly closed-ended, 42-item telephone survey was designed and conducted (eAppendix2)
All women participating in the survey, regardless of age, were asked questions regarding cervical cancer screening. Women aged ≥ 42 years additionally were asked a second set of survey questions specific to breast cancer screening, and women aged between 51 and 64 years were asked a third set of questions related to CRC screening. The ages selected were 1 to 2 years after the recommended age for the respective screening to ensure adequate follow-up time for the member to obtain the screening. Men included in the survey were asked questions related only to CRC screening.
The target survey sample was 3,500 beneficiaries, separated into the following 4 strata: women aged 21 to 64 years of age enrolled in the direct care system (n = 1,250); women aged 21 to 64 years enrolled in the purchased (commercial) care network (n = 1,250); men aged 51 to 64 years enrolled in the direct care system (n = 500); and men aged 51 to 64 years enrolled in the purchased care network (n = 500). The random sample was drawn from an overall population of about 35,000 members. Sampling was performed without replacement until the target number of surveys was achieved. Survey completion was defined as the respondent having reached the end of the survey questionnaire but not necessarily having answered every question.
Data Elements
The preventive health survey collected information on beneficiaries’ knowledge of and satisfaction with their PCM, the primary location where they sought health care in the previous 12 months, preference for scheduling cancer screening tests, and general knowledge about the frequency and type of screening for breast, cervical, and colorectal cancers. Responses were scored based on guidelines effective as of 2009. In addition, the survey collected information on the beneficiary’s overall health status, current age, highest level of education achieved, current employment status, place of residence (on or off a military installation), race, and whether the beneficiary carried other health insurance aside from TRICARE.
Survey Mode and Fielding
A sampling population of eligible beneficiaries was created from a database of all TRICARE Prime beneficiaries. An automated system was used to randomly draw potential participants from the sample. Survey interviewers were given the beneficiary’s name and telephone number but no other identifiable information. Phone numbers from the sample were dialed up to 6 times before the number was classified as a “no answer.” Interviewers read to each beneficiary a statement describing the survey and participation risk and benefits and explained that participation was voluntary and the participant could end the survey at any time without penalty or prejudice. The survey commenced only after verbal consent was obtained.
Sample Weighting and Statistical Analysis
Each survey record was weighted to control for potential bias associated with unequal rates of noncoverage and nonresponse in the sampled population. A design weight was calculated as the ratio of the frame size and the sample size in each stratum. For each stratum, an adjusted response rate (RR) was calculated as the number of completed surveys divided by the number of eligible respondents. Since all respondents were eligible, the RR was not adjusted. The ratio of the design weight to the adjusted RR was calculated and assigned to each survey.
Frequency distributions and descriptive statistics were calculated for all close-ended survey items. Open-ended survey items were summarized and assessed qualitatively. When appropriate, open-ended responses were categorized and included in descriptive analyses. No formal statistical testing was performed.
Results
A total of 6,563 beneficiaries were contacted, and 3,688 agreed to participate (56%), resulting in 3,500 TRICARE beneficiaries completing the survey (95% completion rate), of whom 71% (2,500) were female. The overall cooperation rates were similar across the 4 strata. Interviews ceased once 3,500 surveys were completed. The largest distribution of respondents was aged between 55 and 64 years (37%) (Table 1). Respondents aged 21 to 24 years comprised the smallest percentage of the sample (7%). Nearly a third of respondents were dependents of ADSMs (30%), another 30% were retirees, and most respondents self-identified as white (Table 1).
Barriers to Screening
A series of survey questions was asked about specific barriers to cancer screening, including the convenience of appointment times for the respondent’s last cancer screening. The majority (69%, 2,415 of 3,500) responded that the appointment times were convenient. Among those who stated that times were not convenient and those who had not scheduled an examination, 66% responded that they did not know or were not sure how to schedule a cancer screening test.
Screening Preferences
Less than half of survey respondents (48%) reported that they received screening guideline information from their physician or provider; 24% reported that they performed their own research. Only 9% reported that they learned about the guidelines through TRICARE materials, and 7% of respondents indicated that media, family, or friends were their source of screening information.
The survey respondents who indicated that they had not scheduled a screening examination were asked when (time of day) they preferred to have a screening. Less than half (47%) reported that varying available appointment times would not affect their ability to obtain screening. One-quarter preferred times for screening during working hours, 20% preferred times after working hours, 6% preferred times before working hours, and 2% responded that they were unsure or did not know. The majority (89%) reported that they would prefer to receive all available screenings on the same day if possible.
Breast Cancer Screening
Nearly all (98%) of the 1,100 women aged between 42 and 64 years reported having received a mammogram. These women were asked a specific subset of questions related to breast cancer screening. Respondents were asked to state the recommended age at which women should begin receiving mammogram screenings. More than half (55%) provided the correct response (40 years old, per the U.S. Preventive Services Task Force guidelines).3,4 About three-quarters of respondents (789) correctly responded annually to the question regarding how often women should receive mammograms.
The survey also sought to identify barriers that prevented women from obtaining necessary breast cancer screening. However, the majority surveyed (85%) noted that the question was not applicable because they typically scheduled screening appointments. Only a few (3%) reported factors such as either themselves or someone they know having had a negative experience, discomfort, pain, or concerns of a falsepositive result as reasons for not obtaining breast cancer screening. Of the 112 respondents to the open-ended question, 25% reported that their schedules prevented them from scheduling a mammogram in the past; 12% reported that an inconvenient clinic location, appointment time, or process prevented them from receiving a screening; and 13% reported forgetting to schedule the screening (Table 2).
Cervical Cancer Screening
Female respondents aged between 21 and 64 years (n = 2,432) were asked about the recommended age at which women should begin receiving cervical cancer screening. Only 1% of respondents provided the correct response (that screening begins at 21 years of age per the U.S. Preventive Services Task Force Report guidelines), while 88% provided an incorrect response, and 11% were unsure or did not provide any response.5 Among all respondents, 98% reported having had a cervical cancer screening.
Respondents were asked how frequently women should have a Papanicolaou (Pap) test. Responses such as “2 to 3 years,” “2 years,” or “every other year” were labeled as correct, whereas responses such as “every 6 months” or “greater than 3 years” were labeled as incorrect. Just 12% of respondents provided a correct response, whereas 86% answered incorrectly, and 2% did not answer or did not know. Of those who answered incorrectly, the most common response was “annually” or “every year,” with no notable differences according to race, age, or beneficiary category.
To better understand barriers to screening, respondents were asked to identify reasons they might not have sought cervical cancer screening. The majority (84%) reported that they typically scheduled appointments and that the question was not applicable. However, among 228 respondents who provided an open-ended response and who had not previously undergone a hysterectomy, 8% stated that they had received no reminder or that they lacked sufficient information to schedule the appointment, 21% forgot to schedule, 18% reported a scheduling conflict or difficulty in receiving care, and 13% noted that they did not believe in annual screening (Table 2).
Colorectal Cancer Screening
Eighty-seven percent of eligible respondents (n = 1,734) reported having ever had a sigmoidoscopy and/or colonoscopy. Respondents were asked for their understanding of the recommended age for men and women to begin CRC screening.6 Nearly three-quarters of respondents provided a correct response (n = 1,225), compared with 23% of respondents (n = 407) who answered incorrectly and 6% (n = 102) who did not provide a response or stated they did not know. Correct responses were numerically higher among white respondents (73%) compared with black (62%) and other (62%) respondents as well as among persons aged < 60 years (73%) vs those aged > 60 years (67%).
Respondents aged between 51 and 64 years were asked how often the average person should receive colon cancer screenings. The most common response was that screening should occur every 5 years (33%) followed by every 10 years (26%). This aligns with the U.S. Preventive Services Task Force’s recommendations for flexible sigmoidoscopy every 5 years or colonoscopy every 10 years.
Eligible respondents were asked to identify reasons they did not seek CRC screening. Eighty-six percent of respondents indicated that they typically scheduled CRC screening and that the question was not applicable. Among respondents who provided an open-ended response, 26% cited feeling uncomfortable with the procedure, 15% cited forgetting to schedule a screening, 15% noted a lack of information on screening, and 11% reported no need for screening (Table 2). Among the 1,734 respondents, 80% reported that they would prefer a fecal occult blood test (FOBT) over either a colonoscopy or a sigmoidoscopy. Only 51% reported that their PCM had previously discussed the different types of CRC screenings at some point.
Discussion
The purpose of this large, representative survey was to obtain information on beneficiaries’ knowledge, perceived barriers, and beliefs regarding breast, cervical, and colorectal cancer screenings to identify factors contributing to low completion rates. As far as is known, this is the first study to address these questions in a TRICARE population. Overall, the findings suggest that beneficiaries consider cancer screening important, largely relying on their PCM or their research to better understand how and when to obtain such screenings. The majority received 1 or more screenings prior to the survey, but there were some common knowledge gaps about how to schedule screening appointments, relevant TRICARE medical benefits, and the current recommendations regarding screening timing and frequency. A commonly reported issue across all surveyed groups was inconvenient screening times.
More than half (55%) of respondents correctly noted that breast cancer screening begins at age 40 years (based on recommendations at the time the survey was conducted), and 72% understood when screening should occur. Despite access to care, inconvenient schedules and testing locations were considered the biggest barriers to regularly obtaining a mammogram. There are few studies on knowledge of breast cancer screening in an insured population available for comparison.7-10 One study of medically insured black and non-Hispanic women aged 43 to 49 years showed that lack of reminders or knowledge about the need for mammograms, cost, being too busy, and forgetting to schedule appointments were all factors associated with nonadherence to repeat mammography examinations.8 In an integrative review published in 2000, authors cited that among 8 of 13 relevant studies, the major barrier to receiving a recommended mammogram was lack of physician recommendation.7
For cervical cancer screening, few respondents (1%) correctly identified the age for initiation of screening, and just 12% correctly identified the frequency of screening. These findings are consistent with those of other studies, suggesting a general misunderstanding
about Pap tests in the U.S. and among low-income women.11,12 Reported barriers to screening were uncommon but included scheduling conflicts and lack of reminders or information and were consistent with barriers cited in prior studies.13,14 A few respondents (13%) noted that they did not believe in annual screening, which is similar to the findings of Decker and colleagues who cited lack of knowledge about the test and belief that screening is of no benefit as reasons for failure to get a recommended Pap test.13 These findings suggest a need to improve patientprovider communication and to provide more patient educational materials about the importance of cervical cancer screening.
A large proportion (71%) gave the correct response regarding the appropriate age to initiate CRC screening. Discomfort with the procedure, belief that the screening is unnecessary, or lack of physician’s recommendation were noted barriers to CRC screening. These findings are similar to those reported elsewhere in non-TRICARE populations.15-20 Two focus groups included participants with little knowledge about CRC screening, such as risk factors and symptoms, and expressed fear and embarrassment about CRC and screening. Few of the focus group participants were aware of the available options for screening, and some were confused about the purpose and benefits of the various screening modalities.16
A Health Information National Trends survey reported that 24% participants had not received a colonoscopy or a sigmoidoscopy because their PCM did not order it or say that it was necessary.15 The reported perceived barriers included fear of an adverse finding, injury to the colon from screening, and embarrassment. A study performed in 1,901 Medicare-insured individuals with no history of CRC cited lack of knowledge/awareness and no physician order as the most common reasons for not undergoing CRC screening.18
Strengths and Limitations
A major strength of the current survey is the 56% completion rate, which far exceeds other survey participation rates that were as low as 9%.21 A second strength is the scope of the survey to capture information on not 1 but 3 different cancer screening practices in a unique population who receive preventive screenings at low to no cost.
There are a few study limitations. The majority of respondents identified as white (80%), which does not fully align with the racial distribution of the TRICARE Prime population in the West Region, which is about 68% white. This higher proportion of white respondents may affect the ability to generalize findings to other populations. However, given the open access to care, race should not be a major factor contributing to screening decisions. Another potential limitation to the generalizability of the study is that the age of the respondents was capped at 64 years. Considering that some of the reported barriers to screening were “too busy” or “scheduling conflict,” a study population that included respondents aged ≥ 65 years (who might be more likely to be retired) might report lower rates of these schedule-related barriers.
A third limitation is that most questions about prior screenings pertained to any time in the past, and, therefore, limited the ability to identify current factors leading to lower screening rates. Last, the survey was developed prior to the 2012 changes in cervical and breast cancer screening recommendations and was therefore scored based on prior recommendations. Given that the goal was to assess knowledge and barriers, results are not expected to differ greatly if they are scored using the newer guidelines.
Conclusion
Findings from this cross-sectional survey indicate high levels of knowledge among TRICARE West Region beneficiaries regarding when and how often screening for breast cancer, cervical cancer, and CRC should occur. To encourage TRICARE beneficiaries to seek and obtain recommended and covered cancer screenings, further efforts are needed, including more education about the importance of screening and how to obtain screening. The survey results suggest that TRICARE Prime beneficiaries view cancer screening as important for overall health but they require (and also may desire) more frequent scheduling reminders, education, and more options for scheduling. Newer modalities for communicating with beneficiaries, such as automated telephone appointment reminders, reminder texts, online appointment scheduling, educational blogs, podcasts on cancer screening, extended appointment hours, or unconventional strategies to bundle screening services, are tools that could be used by providers to achieve greater compliance with cancer screening recommendations.
Author Disclosure
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Click here to read the digital edition.
1. TRICARE. TRICARE policy manual 6010.57-M. http://manuals.tricare.osd.mil/pages/DisplayManualaspx?SeriesId=POLICY. Published February 1, 2008. Accessed March 9, 2017.
2. National Committee for Quality Assurance. 2013 accreditation benchmarks and thresholds—mid-year update. http://www.ncqa.org/Portals/0/PolicyUpdates/Trending %20and%20Benchmarks/archives/2013_BENCHMARKS ANDTHRESHOLDS_for%20MidYear%20Update_Final.pdf. Published July 24, 2013. Accessed March 9, 2017.
3. U.S. Preventative Services Task Force. Archived final recommendation statement: breast cancer: screening, 2002. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening-2002. Published December 30, 2013. Accessed March 9, 2017.
4. Smith RA, Saslow D, Sawyer KA, et al; American Cancer Society High-Risk Work Group; American Cancer Society Screening Older Women Work Group; American Cancer Society Mammography Work Group; American Cancer Society Physical Examination Work Group; American Cancer Society New Technologies Work Group; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast cancer screening: update 2003. CA Cancer J Clin. 2003;53(3):141-169.
5. Moyer VA; U.S. Preventive Services Task Force. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;156(12):880-891, W312.
6. U.S. Preventive Services Task Force. Archived: colorectal cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/colorectal-cancer-screening. Published October 2008. Accessed March 9, 2017.
7. George SA. Barriers to breast cancer screening: an integrative review. Health Care Women Int. 2000;21(1):53-65.
8. Gierisch JM, O’Neill SC, Rimer BK, DeFrank JT, Bowling JM, Skinner CS. Factors associated with annual-interval mammography for women in their 40s. Cancer Epidemiol. 2009;33(1):72-78.
9. Peppercorn J, Houck K, Beri N, et al. Breast cancer screening utilization and understanding of current guidelines among rural U.S. women with private insurance. Breast Cancer Res Treat. 2015;153(3):659-667.
10. Sarma EA. Barriers to screening mammography. Health Psychol Rev. 2015;9(1):42-62.
11. Hawkins NA, Benard VB, Greek A, Roland KB, Manninen D, Saraiya M. Patient knowledge and beliefs as barriers to extending cervical cancer screening intervals in federally qualified health centers. Prev Med. 2013;57(5):641-645.
12. Hawkins NA, Cooper CP, Saraiya M, Gelb CA, Polonec L. Why the Pap test? Awareness and use of the Pap test among women in the United States. J Womens Health (Larchmt). 2011;20(4):511-515.
13. Decker KM, Turner D, Demers AA, Martens PJ, Lambert P, Chateau D. Evaluating the effectiveness of cervical cancer screening invitation letters. J Womens Health (Larchmt). 2013;22(8):687-693.
14. Yao X, Dembe AE, Wickizer T, Lu B. Does time pressure create barriers for people to receive preventive health services? Prev Med. 2015;74:55-58.
15. Geiger TM, Miedema BW, Geana MV, Thaler K, Rangnekar NJ, Cameron GT. Improving rates for screening colonoscopy: analysis of the Health Information National Trends Survey (HINTS I) data. Surgical Endoscopy. 2008;22(2):527-533.
16. Greisinger A, Hawley ST, Bettencourt JL, Perz CA, Vernon SW. Primary care patients’ understanding of colorectal cancer screening. Cancer Detect Prev. 2006;30(1):67-74.
17. Janz NK, Wren PA, Schottenfeld D, Guire KE. Colorectal cancer screening attitudes and behavior: a populationbased study. Prev Med. 2003;37(6, pt 1):627-634.
18. Klabunde CN, Schenck AP, Davis WW. Barriers to colorectal cancer screening among Medicare consumers. Am J Prev Med. 2006;30(4):313-319.
19. Klabunde CN, Vernon SW, Nadel MR, Breen N, Seeff LC, Brown ML. Barriers to colorectal cancer screening: a comparison of reports from primary care physicians and average-risk adults. Med Care. 2005;43(9):939-944.
20. Berkowitz Z, Hawkins NA, Peipins LA, White MC, Nadel MR. Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. J Am Geriatr Soc. 2008;56(2):307-314.
21. Pew Research Center. Assessing the representativeness of public opinion surveys. http://www.people-press.org/2012/05/15/assessing-the-representativeness-of-public-opinion-surveys/. Published May 15, 2012. Accessed March 9, 2017.
The National Defense Appropriations Act for fiscal year 2009, Subtitle B, waived copayments for preventive cancer screening services for all TRICARE beneficiaries, excluding Medicare-eligible beneficiaries.1 These preventive services include screening for colorectal cancer (CRC), breast cancer, and cervical cancer based on current guidelines (eAppendix1).
Despite having unrestricted access to these cancer screenings, TRICARE Prime beneficiaries report overall screening completion rates that are below the national commercial benchmarks established by the Healthcare Effectiveness Data and Information Set (HEDIS) for all 3 cancer types.2 Specifically, among TRICARE Prime beneficiaries enrolled in the western region of the U.S. in October 2013, the reported breast cancer screening rate was 61.6% (43,138/69,976) for women aged 42 to 69 years, which is well below the HEDIS 75th percentile of 76%. Similarly, the reported rate of cervical cancer screening among women aged 24 to 64 years was 68.3% (63,523/92,946), well below the HEDIS 75th percentile of 79%. Last, the reported rate of CRC screening among male and female TRICARE Prime members aged 51 to 75 years was 61.6% (52,860/85,827), also below the 2013 HEDIS 75th percentile of 63% based on internal review of TRICARE data used for HEDIS reporting.
Given the reported low screening rates, the Defense Health Agency (DHA) performed a cross-sectional survey to assess TRICARE Prime West region beneficiaries’ knowledge and understanding of preventive health screening, specifically for breast cancer, cervical cancer, and CRC, and to identify any potential barriers to access for these screenings.
Methods
A mostly closed-ended, 42-item telephone survey was designed and conducted (eAppendix2)
All women participating in the survey, regardless of age, were asked questions regarding cervical cancer screening. Women aged ≥ 42 years additionally were asked a second set of survey questions specific to breast cancer screening, and women aged between 51 and 64 years were asked a third set of questions related to CRC screening. The ages selected were 1 to 2 years after the recommended age for the respective screening to ensure adequate follow-up time for the member to obtain the screening. Men included in the survey were asked questions related only to CRC screening.
The target survey sample was 3,500 beneficiaries, separated into the following 4 strata: women aged 21 to 64 years of age enrolled in the direct care system (n = 1,250); women aged 21 to 64 years enrolled in the purchased (commercial) care network (n = 1,250); men aged 51 to 64 years enrolled in the direct care system (n = 500); and men aged 51 to 64 years enrolled in the purchased care network (n = 500). The random sample was drawn from an overall population of about 35,000 members. Sampling was performed without replacement until the target number of surveys was achieved. Survey completion was defined as the respondent having reached the end of the survey questionnaire but not necessarily having answered every question.
Data Elements
The preventive health survey collected information on beneficiaries’ knowledge of and satisfaction with their PCM, the primary location where they sought health care in the previous 12 months, preference for scheduling cancer screening tests, and general knowledge about the frequency and type of screening for breast, cervical, and colorectal cancers. Responses were scored based on guidelines effective as of 2009. In addition, the survey collected information on the beneficiary’s overall health status, current age, highest level of education achieved, current employment status, place of residence (on or off a military installation), race, and whether the beneficiary carried other health insurance aside from TRICARE.
Survey Mode and Fielding
A sampling population of eligible beneficiaries was created from a database of all TRICARE Prime beneficiaries. An automated system was used to randomly draw potential participants from the sample. Survey interviewers were given the beneficiary’s name and telephone number but no other identifiable information. Phone numbers from the sample were dialed up to 6 times before the number was classified as a “no answer.” Interviewers read to each beneficiary a statement describing the survey and participation risk and benefits and explained that participation was voluntary and the participant could end the survey at any time without penalty or prejudice. The survey commenced only after verbal consent was obtained.
Sample Weighting and Statistical Analysis
Each survey record was weighted to control for potential bias associated with unequal rates of noncoverage and nonresponse in the sampled population. A design weight was calculated as the ratio of the frame size and the sample size in each stratum. For each stratum, an adjusted response rate (RR) was calculated as the number of completed surveys divided by the number of eligible respondents. Since all respondents were eligible, the RR was not adjusted. The ratio of the design weight to the adjusted RR was calculated and assigned to each survey.
Frequency distributions and descriptive statistics were calculated for all close-ended survey items. Open-ended survey items were summarized and assessed qualitatively. When appropriate, open-ended responses were categorized and included in descriptive analyses. No formal statistical testing was performed.
Results
A total of 6,563 beneficiaries were contacted, and 3,688 agreed to participate (56%), resulting in 3,500 TRICARE beneficiaries completing the survey (95% completion rate), of whom 71% (2,500) were female. The overall cooperation rates were similar across the 4 strata. Interviews ceased once 3,500 surveys were completed. The largest distribution of respondents was aged between 55 and 64 years (37%) (Table 1). Respondents aged 21 to 24 years comprised the smallest percentage of the sample (7%). Nearly a third of respondents were dependents of ADSMs (30%), another 30% were retirees, and most respondents self-identified as white (Table 1).
Barriers to Screening
A series of survey questions was asked about specific barriers to cancer screening, including the convenience of appointment times for the respondent’s last cancer screening. The majority (69%, 2,415 of 3,500) responded that the appointment times were convenient. Among those who stated that times were not convenient and those who had not scheduled an examination, 66% responded that they did not know or were not sure how to schedule a cancer screening test.
Screening Preferences
Less than half of survey respondents (48%) reported that they received screening guideline information from their physician or provider; 24% reported that they performed their own research. Only 9% reported that they learned about the guidelines through TRICARE materials, and 7% of respondents indicated that media, family, or friends were their source of screening information.
The survey respondents who indicated that they had not scheduled a screening examination were asked when (time of day) they preferred to have a screening. Less than half (47%) reported that varying available appointment times would not affect their ability to obtain screening. One-quarter preferred times for screening during working hours, 20% preferred times after working hours, 6% preferred times before working hours, and 2% responded that they were unsure or did not know. The majority (89%) reported that they would prefer to receive all available screenings on the same day if possible.
Breast Cancer Screening
Nearly all (98%) of the 1,100 women aged between 42 and 64 years reported having received a mammogram. These women were asked a specific subset of questions related to breast cancer screening. Respondents were asked to state the recommended age at which women should begin receiving mammogram screenings. More than half (55%) provided the correct response (40 years old, per the U.S. Preventive Services Task Force guidelines).3,4 About three-quarters of respondents (789) correctly responded annually to the question regarding how often women should receive mammograms.
The survey also sought to identify barriers that prevented women from obtaining necessary breast cancer screening. However, the majority surveyed (85%) noted that the question was not applicable because they typically scheduled screening appointments. Only a few (3%) reported factors such as either themselves or someone they know having had a negative experience, discomfort, pain, or concerns of a falsepositive result as reasons for not obtaining breast cancer screening. Of the 112 respondents to the open-ended question, 25% reported that their schedules prevented them from scheduling a mammogram in the past; 12% reported that an inconvenient clinic location, appointment time, or process prevented them from receiving a screening; and 13% reported forgetting to schedule the screening (Table 2).
Cervical Cancer Screening
Female respondents aged between 21 and 64 years (n = 2,432) were asked about the recommended age at which women should begin receiving cervical cancer screening. Only 1% of respondents provided the correct response (that screening begins at 21 years of age per the U.S. Preventive Services Task Force Report guidelines), while 88% provided an incorrect response, and 11% were unsure or did not provide any response.5 Among all respondents, 98% reported having had a cervical cancer screening.
Respondents were asked how frequently women should have a Papanicolaou (Pap) test. Responses such as “2 to 3 years,” “2 years,” or “every other year” were labeled as correct, whereas responses such as “every 6 months” or “greater than 3 years” were labeled as incorrect. Just 12% of respondents provided a correct response, whereas 86% answered incorrectly, and 2% did not answer or did not know. Of those who answered incorrectly, the most common response was “annually” or “every year,” with no notable differences according to race, age, or beneficiary category.
To better understand barriers to screening, respondents were asked to identify reasons they might not have sought cervical cancer screening. The majority (84%) reported that they typically scheduled appointments and that the question was not applicable. However, among 228 respondents who provided an open-ended response and who had not previously undergone a hysterectomy, 8% stated that they had received no reminder or that they lacked sufficient information to schedule the appointment, 21% forgot to schedule, 18% reported a scheduling conflict or difficulty in receiving care, and 13% noted that they did not believe in annual screening (Table 2).
Colorectal Cancer Screening
Eighty-seven percent of eligible respondents (n = 1,734) reported having ever had a sigmoidoscopy and/or colonoscopy. Respondents were asked for their understanding of the recommended age for men and women to begin CRC screening.6 Nearly three-quarters of respondents provided a correct response (n = 1,225), compared with 23% of respondents (n = 407) who answered incorrectly and 6% (n = 102) who did not provide a response or stated they did not know. Correct responses were numerically higher among white respondents (73%) compared with black (62%) and other (62%) respondents as well as among persons aged < 60 years (73%) vs those aged > 60 years (67%).
Respondents aged between 51 and 64 years were asked how often the average person should receive colon cancer screenings. The most common response was that screening should occur every 5 years (33%) followed by every 10 years (26%). This aligns with the U.S. Preventive Services Task Force’s recommendations for flexible sigmoidoscopy every 5 years or colonoscopy every 10 years.
Eligible respondents were asked to identify reasons they did not seek CRC screening. Eighty-six percent of respondents indicated that they typically scheduled CRC screening and that the question was not applicable. Among respondents who provided an open-ended response, 26% cited feeling uncomfortable with the procedure, 15% cited forgetting to schedule a screening, 15% noted a lack of information on screening, and 11% reported no need for screening (Table 2). Among the 1,734 respondents, 80% reported that they would prefer a fecal occult blood test (FOBT) over either a colonoscopy or a sigmoidoscopy. Only 51% reported that their PCM had previously discussed the different types of CRC screenings at some point.
Discussion
The purpose of this large, representative survey was to obtain information on beneficiaries’ knowledge, perceived barriers, and beliefs regarding breast, cervical, and colorectal cancer screenings to identify factors contributing to low completion rates. As far as is known, this is the first study to address these questions in a TRICARE population. Overall, the findings suggest that beneficiaries consider cancer screening important, largely relying on their PCM or their research to better understand how and when to obtain such screenings. The majority received 1 or more screenings prior to the survey, but there were some common knowledge gaps about how to schedule screening appointments, relevant TRICARE medical benefits, and the current recommendations regarding screening timing and frequency. A commonly reported issue across all surveyed groups was inconvenient screening times.
More than half (55%) of respondents correctly noted that breast cancer screening begins at age 40 years (based on recommendations at the time the survey was conducted), and 72% understood when screening should occur. Despite access to care, inconvenient schedules and testing locations were considered the biggest barriers to regularly obtaining a mammogram. There are few studies on knowledge of breast cancer screening in an insured population available for comparison.7-10 One study of medically insured black and non-Hispanic women aged 43 to 49 years showed that lack of reminders or knowledge about the need for mammograms, cost, being too busy, and forgetting to schedule appointments were all factors associated with nonadherence to repeat mammography examinations.8 In an integrative review published in 2000, authors cited that among 8 of 13 relevant studies, the major barrier to receiving a recommended mammogram was lack of physician recommendation.7
For cervical cancer screening, few respondents (1%) correctly identified the age for initiation of screening, and just 12% correctly identified the frequency of screening. These findings are consistent with those of other studies, suggesting a general misunderstanding
about Pap tests in the U.S. and among low-income women.11,12 Reported barriers to screening were uncommon but included scheduling conflicts and lack of reminders or information and were consistent with barriers cited in prior studies.13,14 A few respondents (13%) noted that they did not believe in annual screening, which is similar to the findings of Decker and colleagues who cited lack of knowledge about the test and belief that screening is of no benefit as reasons for failure to get a recommended Pap test.13 These findings suggest a need to improve patientprovider communication and to provide more patient educational materials about the importance of cervical cancer screening.
A large proportion (71%) gave the correct response regarding the appropriate age to initiate CRC screening. Discomfort with the procedure, belief that the screening is unnecessary, or lack of physician’s recommendation were noted barriers to CRC screening. These findings are similar to those reported elsewhere in non-TRICARE populations.15-20 Two focus groups included participants with little knowledge about CRC screening, such as risk factors and symptoms, and expressed fear and embarrassment about CRC and screening. Few of the focus group participants were aware of the available options for screening, and some were confused about the purpose and benefits of the various screening modalities.16
A Health Information National Trends survey reported that 24% participants had not received a colonoscopy or a sigmoidoscopy because their PCM did not order it or say that it was necessary.15 The reported perceived barriers included fear of an adverse finding, injury to the colon from screening, and embarrassment. A study performed in 1,901 Medicare-insured individuals with no history of CRC cited lack of knowledge/awareness and no physician order as the most common reasons for not undergoing CRC screening.18
Strengths and Limitations
A major strength of the current survey is the 56% completion rate, which far exceeds other survey participation rates that were as low as 9%.21 A second strength is the scope of the survey to capture information on not 1 but 3 different cancer screening practices in a unique population who receive preventive screenings at low to no cost.
There are a few study limitations. The majority of respondents identified as white (80%), which does not fully align with the racial distribution of the TRICARE Prime population in the West Region, which is about 68% white. This higher proportion of white respondents may affect the ability to generalize findings to other populations. However, given the open access to care, race should not be a major factor contributing to screening decisions. Another potential limitation to the generalizability of the study is that the age of the respondents was capped at 64 years. Considering that some of the reported barriers to screening were “too busy” or “scheduling conflict,” a study population that included respondents aged ≥ 65 years (who might be more likely to be retired) might report lower rates of these schedule-related barriers.
A third limitation is that most questions about prior screenings pertained to any time in the past, and, therefore, limited the ability to identify current factors leading to lower screening rates. Last, the survey was developed prior to the 2012 changes in cervical and breast cancer screening recommendations and was therefore scored based on prior recommendations. Given that the goal was to assess knowledge and barriers, results are not expected to differ greatly if they are scored using the newer guidelines.
Conclusion
Findings from this cross-sectional survey indicate high levels of knowledge among TRICARE West Region beneficiaries regarding when and how often screening for breast cancer, cervical cancer, and CRC should occur. To encourage TRICARE beneficiaries to seek and obtain recommended and covered cancer screenings, further efforts are needed, including more education about the importance of screening and how to obtain screening. The survey results suggest that TRICARE Prime beneficiaries view cancer screening as important for overall health but they require (and also may desire) more frequent scheduling reminders, education, and more options for scheduling. Newer modalities for communicating with beneficiaries, such as automated telephone appointment reminders, reminder texts, online appointment scheduling, educational blogs, podcasts on cancer screening, extended appointment hours, or unconventional strategies to bundle screening services, are tools that could be used by providers to achieve greater compliance with cancer screening recommendations.
Author Disclosure
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Click here to read the digital edition.
The National Defense Appropriations Act for fiscal year 2009, Subtitle B, waived copayments for preventive cancer screening services for all TRICARE beneficiaries, excluding Medicare-eligible beneficiaries.1 These preventive services include screening for colorectal cancer (CRC), breast cancer, and cervical cancer based on current guidelines (eAppendix1).
Despite having unrestricted access to these cancer screenings, TRICARE Prime beneficiaries report overall screening completion rates that are below the national commercial benchmarks established by the Healthcare Effectiveness Data and Information Set (HEDIS) for all 3 cancer types.2 Specifically, among TRICARE Prime beneficiaries enrolled in the western region of the U.S. in October 2013, the reported breast cancer screening rate was 61.6% (43,138/69,976) for women aged 42 to 69 years, which is well below the HEDIS 75th percentile of 76%. Similarly, the reported rate of cervical cancer screening among women aged 24 to 64 years was 68.3% (63,523/92,946), well below the HEDIS 75th percentile of 79%. Last, the reported rate of CRC screening among male and female TRICARE Prime members aged 51 to 75 years was 61.6% (52,860/85,827), also below the 2013 HEDIS 75th percentile of 63% based on internal review of TRICARE data used for HEDIS reporting.
Given the reported low screening rates, the Defense Health Agency (DHA) performed a cross-sectional survey to assess TRICARE Prime West region beneficiaries’ knowledge and understanding of preventive health screening, specifically for breast cancer, cervical cancer, and CRC, and to identify any potential barriers to access for these screenings.
Methods
A mostly closed-ended, 42-item telephone survey was designed and conducted (eAppendix2)
All women participating in the survey, regardless of age, were asked questions regarding cervical cancer screening. Women aged ≥ 42 years additionally were asked a second set of survey questions specific to breast cancer screening, and women aged between 51 and 64 years were asked a third set of questions related to CRC screening. The ages selected were 1 to 2 years after the recommended age for the respective screening to ensure adequate follow-up time for the member to obtain the screening. Men included in the survey were asked questions related only to CRC screening.
The target survey sample was 3,500 beneficiaries, separated into the following 4 strata: women aged 21 to 64 years of age enrolled in the direct care system (n = 1,250); women aged 21 to 64 years enrolled in the purchased (commercial) care network (n = 1,250); men aged 51 to 64 years enrolled in the direct care system (n = 500); and men aged 51 to 64 years enrolled in the purchased care network (n = 500). The random sample was drawn from an overall population of about 35,000 members. Sampling was performed without replacement until the target number of surveys was achieved. Survey completion was defined as the respondent having reached the end of the survey questionnaire but not necessarily having answered every question.
Data Elements
The preventive health survey collected information on beneficiaries’ knowledge of and satisfaction with their PCM, the primary location where they sought health care in the previous 12 months, preference for scheduling cancer screening tests, and general knowledge about the frequency and type of screening for breast, cervical, and colorectal cancers. Responses were scored based on guidelines effective as of 2009. In addition, the survey collected information on the beneficiary’s overall health status, current age, highest level of education achieved, current employment status, place of residence (on or off a military installation), race, and whether the beneficiary carried other health insurance aside from TRICARE.
Survey Mode and Fielding
A sampling population of eligible beneficiaries was created from a database of all TRICARE Prime beneficiaries. An automated system was used to randomly draw potential participants from the sample. Survey interviewers were given the beneficiary’s name and telephone number but no other identifiable information. Phone numbers from the sample were dialed up to 6 times before the number was classified as a “no answer.” Interviewers read to each beneficiary a statement describing the survey and participation risk and benefits and explained that participation was voluntary and the participant could end the survey at any time without penalty or prejudice. The survey commenced only after verbal consent was obtained.
Sample Weighting and Statistical Analysis
Each survey record was weighted to control for potential bias associated with unequal rates of noncoverage and nonresponse in the sampled population. A design weight was calculated as the ratio of the frame size and the sample size in each stratum. For each stratum, an adjusted response rate (RR) was calculated as the number of completed surveys divided by the number of eligible respondents. Since all respondents were eligible, the RR was not adjusted. The ratio of the design weight to the adjusted RR was calculated and assigned to each survey.
Frequency distributions and descriptive statistics were calculated for all close-ended survey items. Open-ended survey items were summarized and assessed qualitatively. When appropriate, open-ended responses were categorized and included in descriptive analyses. No formal statistical testing was performed.
Results
A total of 6,563 beneficiaries were contacted, and 3,688 agreed to participate (56%), resulting in 3,500 TRICARE beneficiaries completing the survey (95% completion rate), of whom 71% (2,500) were female. The overall cooperation rates were similar across the 4 strata. Interviews ceased once 3,500 surveys were completed. The largest distribution of respondents was aged between 55 and 64 years (37%) (Table 1). Respondents aged 21 to 24 years comprised the smallest percentage of the sample (7%). Nearly a third of respondents were dependents of ADSMs (30%), another 30% were retirees, and most respondents self-identified as white (Table 1).
Barriers to Screening
A series of survey questions was asked about specific barriers to cancer screening, including the convenience of appointment times for the respondent’s last cancer screening. The majority (69%, 2,415 of 3,500) responded that the appointment times were convenient. Among those who stated that times were not convenient and those who had not scheduled an examination, 66% responded that they did not know or were not sure how to schedule a cancer screening test.
Screening Preferences
Less than half of survey respondents (48%) reported that they received screening guideline information from their physician or provider; 24% reported that they performed their own research. Only 9% reported that they learned about the guidelines through TRICARE materials, and 7% of respondents indicated that media, family, or friends were their source of screening information.
The survey respondents who indicated that they had not scheduled a screening examination were asked when (time of day) they preferred to have a screening. Less than half (47%) reported that varying available appointment times would not affect their ability to obtain screening. One-quarter preferred times for screening during working hours, 20% preferred times after working hours, 6% preferred times before working hours, and 2% responded that they were unsure or did not know. The majority (89%) reported that they would prefer to receive all available screenings on the same day if possible.
Breast Cancer Screening
Nearly all (98%) of the 1,100 women aged between 42 and 64 years reported having received a mammogram. These women were asked a specific subset of questions related to breast cancer screening. Respondents were asked to state the recommended age at which women should begin receiving mammogram screenings. More than half (55%) provided the correct response (40 years old, per the U.S. Preventive Services Task Force guidelines).3,4 About three-quarters of respondents (789) correctly responded annually to the question regarding how often women should receive mammograms.
The survey also sought to identify barriers that prevented women from obtaining necessary breast cancer screening. However, the majority surveyed (85%) noted that the question was not applicable because they typically scheduled screening appointments. Only a few (3%) reported factors such as either themselves or someone they know having had a negative experience, discomfort, pain, or concerns of a falsepositive result as reasons for not obtaining breast cancer screening. Of the 112 respondents to the open-ended question, 25% reported that their schedules prevented them from scheduling a mammogram in the past; 12% reported that an inconvenient clinic location, appointment time, or process prevented them from receiving a screening; and 13% reported forgetting to schedule the screening (Table 2).
Cervical Cancer Screening
Female respondents aged between 21 and 64 years (n = 2,432) were asked about the recommended age at which women should begin receiving cervical cancer screening. Only 1% of respondents provided the correct response (that screening begins at 21 years of age per the U.S. Preventive Services Task Force Report guidelines), while 88% provided an incorrect response, and 11% were unsure or did not provide any response.5 Among all respondents, 98% reported having had a cervical cancer screening.
Respondents were asked how frequently women should have a Papanicolaou (Pap) test. Responses such as “2 to 3 years,” “2 years,” or “every other year” were labeled as correct, whereas responses such as “every 6 months” or “greater than 3 years” were labeled as incorrect. Just 12% of respondents provided a correct response, whereas 86% answered incorrectly, and 2% did not answer or did not know. Of those who answered incorrectly, the most common response was “annually” or “every year,” with no notable differences according to race, age, or beneficiary category.
To better understand barriers to screening, respondents were asked to identify reasons they might not have sought cervical cancer screening. The majority (84%) reported that they typically scheduled appointments and that the question was not applicable. However, among 228 respondents who provided an open-ended response and who had not previously undergone a hysterectomy, 8% stated that they had received no reminder or that they lacked sufficient information to schedule the appointment, 21% forgot to schedule, 18% reported a scheduling conflict or difficulty in receiving care, and 13% noted that they did not believe in annual screening (Table 2).
Colorectal Cancer Screening
Eighty-seven percent of eligible respondents (n = 1,734) reported having ever had a sigmoidoscopy and/or colonoscopy. Respondents were asked for their understanding of the recommended age for men and women to begin CRC screening.6 Nearly three-quarters of respondents provided a correct response (n = 1,225), compared with 23% of respondents (n = 407) who answered incorrectly and 6% (n = 102) who did not provide a response or stated they did not know. Correct responses were numerically higher among white respondents (73%) compared with black (62%) and other (62%) respondents as well as among persons aged < 60 years (73%) vs those aged > 60 years (67%).
Respondents aged between 51 and 64 years were asked how often the average person should receive colon cancer screenings. The most common response was that screening should occur every 5 years (33%) followed by every 10 years (26%). This aligns with the U.S. Preventive Services Task Force’s recommendations for flexible sigmoidoscopy every 5 years or colonoscopy every 10 years.
Eligible respondents were asked to identify reasons they did not seek CRC screening. Eighty-six percent of respondents indicated that they typically scheduled CRC screening and that the question was not applicable. Among respondents who provided an open-ended response, 26% cited feeling uncomfortable with the procedure, 15% cited forgetting to schedule a screening, 15% noted a lack of information on screening, and 11% reported no need for screening (Table 2). Among the 1,734 respondents, 80% reported that they would prefer a fecal occult blood test (FOBT) over either a colonoscopy or a sigmoidoscopy. Only 51% reported that their PCM had previously discussed the different types of CRC screenings at some point.
Discussion
The purpose of this large, representative survey was to obtain information on beneficiaries’ knowledge, perceived barriers, and beliefs regarding breast, cervical, and colorectal cancer screenings to identify factors contributing to low completion rates. As far as is known, this is the first study to address these questions in a TRICARE population. Overall, the findings suggest that beneficiaries consider cancer screening important, largely relying on their PCM or their research to better understand how and when to obtain such screenings. The majority received 1 or more screenings prior to the survey, but there were some common knowledge gaps about how to schedule screening appointments, relevant TRICARE medical benefits, and the current recommendations regarding screening timing and frequency. A commonly reported issue across all surveyed groups was inconvenient screening times.
More than half (55%) of respondents correctly noted that breast cancer screening begins at age 40 years (based on recommendations at the time the survey was conducted), and 72% understood when screening should occur. Despite access to care, inconvenient schedules and testing locations were considered the biggest barriers to regularly obtaining a mammogram. There are few studies on knowledge of breast cancer screening in an insured population available for comparison.7-10 One study of medically insured black and non-Hispanic women aged 43 to 49 years showed that lack of reminders or knowledge about the need for mammograms, cost, being too busy, and forgetting to schedule appointments were all factors associated with nonadherence to repeat mammography examinations.8 In an integrative review published in 2000, authors cited that among 8 of 13 relevant studies, the major barrier to receiving a recommended mammogram was lack of physician recommendation.7
For cervical cancer screening, few respondents (1%) correctly identified the age for initiation of screening, and just 12% correctly identified the frequency of screening. These findings are consistent with those of other studies, suggesting a general misunderstanding
about Pap tests in the U.S. and among low-income women.11,12 Reported barriers to screening were uncommon but included scheduling conflicts and lack of reminders or information and were consistent with barriers cited in prior studies.13,14 A few respondents (13%) noted that they did not believe in annual screening, which is similar to the findings of Decker and colleagues who cited lack of knowledge about the test and belief that screening is of no benefit as reasons for failure to get a recommended Pap test.13 These findings suggest a need to improve patientprovider communication and to provide more patient educational materials about the importance of cervical cancer screening.
A large proportion (71%) gave the correct response regarding the appropriate age to initiate CRC screening. Discomfort with the procedure, belief that the screening is unnecessary, or lack of physician’s recommendation were noted barriers to CRC screening. These findings are similar to those reported elsewhere in non-TRICARE populations.15-20 Two focus groups included participants with little knowledge about CRC screening, such as risk factors and symptoms, and expressed fear and embarrassment about CRC and screening. Few of the focus group participants were aware of the available options for screening, and some were confused about the purpose and benefits of the various screening modalities.16
A Health Information National Trends survey reported that 24% participants had not received a colonoscopy or a sigmoidoscopy because their PCM did not order it or say that it was necessary.15 The reported perceived barriers included fear of an adverse finding, injury to the colon from screening, and embarrassment. A study performed in 1,901 Medicare-insured individuals with no history of CRC cited lack of knowledge/awareness and no physician order as the most common reasons for not undergoing CRC screening.18
Strengths and Limitations
A major strength of the current survey is the 56% completion rate, which far exceeds other survey participation rates that were as low as 9%.21 A second strength is the scope of the survey to capture information on not 1 but 3 different cancer screening practices in a unique population who receive preventive screenings at low to no cost.
There are a few study limitations. The majority of respondents identified as white (80%), which does not fully align with the racial distribution of the TRICARE Prime population in the West Region, which is about 68% white. This higher proportion of white respondents may affect the ability to generalize findings to other populations. However, given the open access to care, race should not be a major factor contributing to screening decisions. Another potential limitation to the generalizability of the study is that the age of the respondents was capped at 64 years. Considering that some of the reported barriers to screening were “too busy” or “scheduling conflict,” a study population that included respondents aged ≥ 65 years (who might be more likely to be retired) might report lower rates of these schedule-related barriers.
A third limitation is that most questions about prior screenings pertained to any time in the past, and, therefore, limited the ability to identify current factors leading to lower screening rates. Last, the survey was developed prior to the 2012 changes in cervical and breast cancer screening recommendations and was therefore scored based on prior recommendations. Given that the goal was to assess knowledge and barriers, results are not expected to differ greatly if they are scored using the newer guidelines.
Conclusion
Findings from this cross-sectional survey indicate high levels of knowledge among TRICARE West Region beneficiaries regarding when and how often screening for breast cancer, cervical cancer, and CRC should occur. To encourage TRICARE beneficiaries to seek and obtain recommended and covered cancer screenings, further efforts are needed, including more education about the importance of screening and how to obtain screening. The survey results suggest that TRICARE Prime beneficiaries view cancer screening as important for overall health but they require (and also may desire) more frequent scheduling reminders, education, and more options for scheduling. Newer modalities for communicating with beneficiaries, such as automated telephone appointment reminders, reminder texts, online appointment scheduling, educational blogs, podcasts on cancer screening, extended appointment hours, or unconventional strategies to bundle screening services, are tools that could be used by providers to achieve greater compliance with cancer screening recommendations.
Author Disclosure
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Click here to read the digital edition.
1. TRICARE. TRICARE policy manual 6010.57-M. http://manuals.tricare.osd.mil/pages/DisplayManualaspx?SeriesId=POLICY. Published February 1, 2008. Accessed March 9, 2017.
2. National Committee for Quality Assurance. 2013 accreditation benchmarks and thresholds—mid-year update. http://www.ncqa.org/Portals/0/PolicyUpdates/Trending %20and%20Benchmarks/archives/2013_BENCHMARKS ANDTHRESHOLDS_for%20MidYear%20Update_Final.pdf. Published July 24, 2013. Accessed March 9, 2017.
3. U.S. Preventative Services Task Force. Archived final recommendation statement: breast cancer: screening, 2002. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening-2002. Published December 30, 2013. Accessed March 9, 2017.
4. Smith RA, Saslow D, Sawyer KA, et al; American Cancer Society High-Risk Work Group; American Cancer Society Screening Older Women Work Group; American Cancer Society Mammography Work Group; American Cancer Society Physical Examination Work Group; American Cancer Society New Technologies Work Group; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast cancer screening: update 2003. CA Cancer J Clin. 2003;53(3):141-169.
5. Moyer VA; U.S. Preventive Services Task Force. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;156(12):880-891, W312.
6. U.S. Preventive Services Task Force. Archived: colorectal cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/colorectal-cancer-screening. Published October 2008. Accessed March 9, 2017.
7. George SA. Barriers to breast cancer screening: an integrative review. Health Care Women Int. 2000;21(1):53-65.
8. Gierisch JM, O’Neill SC, Rimer BK, DeFrank JT, Bowling JM, Skinner CS. Factors associated with annual-interval mammography for women in their 40s. Cancer Epidemiol. 2009;33(1):72-78.
9. Peppercorn J, Houck K, Beri N, et al. Breast cancer screening utilization and understanding of current guidelines among rural U.S. women with private insurance. Breast Cancer Res Treat. 2015;153(3):659-667.
10. Sarma EA. Barriers to screening mammography. Health Psychol Rev. 2015;9(1):42-62.
11. Hawkins NA, Benard VB, Greek A, Roland KB, Manninen D, Saraiya M. Patient knowledge and beliefs as barriers to extending cervical cancer screening intervals in federally qualified health centers. Prev Med. 2013;57(5):641-645.
12. Hawkins NA, Cooper CP, Saraiya M, Gelb CA, Polonec L. Why the Pap test? Awareness and use of the Pap test among women in the United States. J Womens Health (Larchmt). 2011;20(4):511-515.
13. Decker KM, Turner D, Demers AA, Martens PJ, Lambert P, Chateau D. Evaluating the effectiveness of cervical cancer screening invitation letters. J Womens Health (Larchmt). 2013;22(8):687-693.
14. Yao X, Dembe AE, Wickizer T, Lu B. Does time pressure create barriers for people to receive preventive health services? Prev Med. 2015;74:55-58.
15. Geiger TM, Miedema BW, Geana MV, Thaler K, Rangnekar NJ, Cameron GT. Improving rates for screening colonoscopy: analysis of the Health Information National Trends Survey (HINTS I) data. Surgical Endoscopy. 2008;22(2):527-533.
16. Greisinger A, Hawley ST, Bettencourt JL, Perz CA, Vernon SW. Primary care patients’ understanding of colorectal cancer screening. Cancer Detect Prev. 2006;30(1):67-74.
17. Janz NK, Wren PA, Schottenfeld D, Guire KE. Colorectal cancer screening attitudes and behavior: a populationbased study. Prev Med. 2003;37(6, pt 1):627-634.
18. Klabunde CN, Schenck AP, Davis WW. Barriers to colorectal cancer screening among Medicare consumers. Am J Prev Med. 2006;30(4):313-319.
19. Klabunde CN, Vernon SW, Nadel MR, Breen N, Seeff LC, Brown ML. Barriers to colorectal cancer screening: a comparison of reports from primary care physicians and average-risk adults. Med Care. 2005;43(9):939-944.
20. Berkowitz Z, Hawkins NA, Peipins LA, White MC, Nadel MR. Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. J Am Geriatr Soc. 2008;56(2):307-314.
21. Pew Research Center. Assessing the representativeness of public opinion surveys. http://www.people-press.org/2012/05/15/assessing-the-representativeness-of-public-opinion-surveys/. Published May 15, 2012. Accessed March 9, 2017.
1. TRICARE. TRICARE policy manual 6010.57-M. http://manuals.tricare.osd.mil/pages/DisplayManualaspx?SeriesId=POLICY. Published February 1, 2008. Accessed March 9, 2017.
2. National Committee for Quality Assurance. 2013 accreditation benchmarks and thresholds—mid-year update. http://www.ncqa.org/Portals/0/PolicyUpdates/Trending %20and%20Benchmarks/archives/2013_BENCHMARKS ANDTHRESHOLDS_for%20MidYear%20Update_Final.pdf. Published July 24, 2013. Accessed March 9, 2017.
3. U.S. Preventative Services Task Force. Archived final recommendation statement: breast cancer: screening, 2002. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening-2002. Published December 30, 2013. Accessed March 9, 2017.
4. Smith RA, Saslow D, Sawyer KA, et al; American Cancer Society High-Risk Work Group; American Cancer Society Screening Older Women Work Group; American Cancer Society Mammography Work Group; American Cancer Society Physical Examination Work Group; American Cancer Society New Technologies Work Group; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast cancer screening: update 2003. CA Cancer J Clin. 2003;53(3):141-169.
5. Moyer VA; U.S. Preventive Services Task Force. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;156(12):880-891, W312.
6. U.S. Preventive Services Task Force. Archived: colorectal cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/colorectal-cancer-screening. Published October 2008. Accessed March 9, 2017.
7. George SA. Barriers to breast cancer screening: an integrative review. Health Care Women Int. 2000;21(1):53-65.
8. Gierisch JM, O’Neill SC, Rimer BK, DeFrank JT, Bowling JM, Skinner CS. Factors associated with annual-interval mammography for women in their 40s. Cancer Epidemiol. 2009;33(1):72-78.
9. Peppercorn J, Houck K, Beri N, et al. Breast cancer screening utilization and understanding of current guidelines among rural U.S. women with private insurance. Breast Cancer Res Treat. 2015;153(3):659-667.
10. Sarma EA. Barriers to screening mammography. Health Psychol Rev. 2015;9(1):42-62.
11. Hawkins NA, Benard VB, Greek A, Roland KB, Manninen D, Saraiya M. Patient knowledge and beliefs as barriers to extending cervical cancer screening intervals in federally qualified health centers. Prev Med. 2013;57(5):641-645.
12. Hawkins NA, Cooper CP, Saraiya M, Gelb CA, Polonec L. Why the Pap test? Awareness and use of the Pap test among women in the United States. J Womens Health (Larchmt). 2011;20(4):511-515.
13. Decker KM, Turner D, Demers AA, Martens PJ, Lambert P, Chateau D. Evaluating the effectiveness of cervical cancer screening invitation letters. J Womens Health (Larchmt). 2013;22(8):687-693.
14. Yao X, Dembe AE, Wickizer T, Lu B. Does time pressure create barriers for people to receive preventive health services? Prev Med. 2015;74:55-58.
15. Geiger TM, Miedema BW, Geana MV, Thaler K, Rangnekar NJ, Cameron GT. Improving rates for screening colonoscopy: analysis of the Health Information National Trends Survey (HINTS I) data. Surgical Endoscopy. 2008;22(2):527-533.
16. Greisinger A, Hawley ST, Bettencourt JL, Perz CA, Vernon SW. Primary care patients’ understanding of colorectal cancer screening. Cancer Detect Prev. 2006;30(1):67-74.
17. Janz NK, Wren PA, Schottenfeld D, Guire KE. Colorectal cancer screening attitudes and behavior: a populationbased study. Prev Med. 2003;37(6, pt 1):627-634.
18. Klabunde CN, Schenck AP, Davis WW. Barriers to colorectal cancer screening among Medicare consumers. Am J Prev Med. 2006;30(4):313-319.
19. Klabunde CN, Vernon SW, Nadel MR, Breen N, Seeff LC, Brown ML. Barriers to colorectal cancer screening: a comparison of reports from primary care physicians and average-risk adults. Med Care. 2005;43(9):939-944.
20. Berkowitz Z, Hawkins NA, Peipins LA, White MC, Nadel MR. Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. J Am Geriatr Soc. 2008;56(2):307-314.
21. Pew Research Center. Assessing the representativeness of public opinion surveys. http://www.people-press.org/2012/05/15/assessing-the-representativeness-of-public-opinion-surveys/. Published May 15, 2012. Accessed March 9, 2017.