User login
Preventing postoperative neuropathies: Patient positioning for minimally invasive procedures
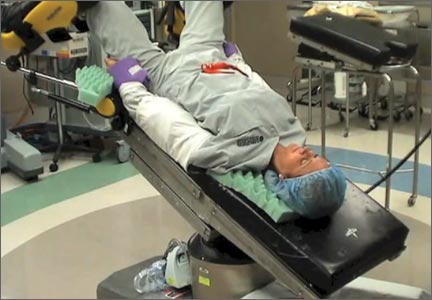
In this comprehensive educational video we review appropriate patient positioning for laparoscopic and robotic surgery to prevent postoperative neuropathies that can be experienced with gynecologic surgery. We also include a case-based review of injuries specific to the brachial plexus, ulnar nerve, and femoral nerve.
Our technique involves the use of a bed sheet, an egg crate foam mattress pad, and boot-type stirrups. We recommend setting up the operating room table to facilitate tucking of the patient’s arms and to prevent slippage of the patient when she is placed in steep Trendelenburg. For all steps involved, see the video.
Tips for setting up the operating room bed include:
- Use of a single bed sheet placed across the head of a bare table with an egg crate foam mattress pad over the sheet to prevent the need for strapping the patient to the bed or the use of shoulder braces to prevent slippage.
- For low dorsal lithotomy positioning, flex the patient’s hips with a trunk-to-thigh angle of approximately 170°, and never more than 180°.
- For arm tucking, remove the arm boards and excess egg crate foam from the patient’s side and placecushioning over the elbow and the wrist. Keep the patient’s hand pronated when tucking and do not allow the arm to hang over the side of the bed.
- If the patient is obese, support the tucked arm by placing the arm boards beneath the arm parallel to the bed.
Next month we continue our series on surgical techniques with a video on why choosing the proper colpotomy cup is critical for successful minimally invasive hysterectomy.

Will you be joining me at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver this November? Safe patient positioning for minimally invasive surgery and other exciting topics will be discussed. Visit www.aagl.org/globalcongress for more information.
—Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In this comprehensive educational video we review appropriate patient positioning for laparoscopic and robotic surgery to prevent postoperative neuropathies that can be experienced with gynecologic surgery. We also include a case-based review of injuries specific to the brachial plexus, ulnar nerve, and femoral nerve.
Our technique involves the use of a bed sheet, an egg crate foam mattress pad, and boot-type stirrups. We recommend setting up the operating room table to facilitate tucking of the patient’s arms and to prevent slippage of the patient when she is placed in steep Trendelenburg. For all steps involved, see the video.
Tips for setting up the operating room bed include:
- Use of a single bed sheet placed across the head of a bare table with an egg crate foam mattress pad over the sheet to prevent the need for strapping the patient to the bed or the use of shoulder braces to prevent slippage.
- For low dorsal lithotomy positioning, flex the patient’s hips with a trunk-to-thigh angle of approximately 170°, and never more than 180°.
- For arm tucking, remove the arm boards and excess egg crate foam from the patient’s side and placecushioning over the elbow and the wrist. Keep the patient’s hand pronated when tucking and do not allow the arm to hang over the side of the bed.
- If the patient is obese, support the tucked arm by placing the arm boards beneath the arm parallel to the bed.
Next month we continue our series on surgical techniques with a video on why choosing the proper colpotomy cup is critical for successful minimally invasive hysterectomy.

Will you be joining me at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver this November? Safe patient positioning for minimally invasive surgery and other exciting topics will be discussed. Visit www.aagl.org/globalcongress for more information.
—Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In this comprehensive educational video we review appropriate patient positioning for laparoscopic and robotic surgery to prevent postoperative neuropathies that can be experienced with gynecologic surgery. We also include a case-based review of injuries specific to the brachial plexus, ulnar nerve, and femoral nerve.
Our technique involves the use of a bed sheet, an egg crate foam mattress pad, and boot-type stirrups. We recommend setting up the operating room table to facilitate tucking of the patient’s arms and to prevent slippage of the patient when she is placed in steep Trendelenburg. For all steps involved, see the video.
Tips for setting up the operating room bed include:
- Use of a single bed sheet placed across the head of a bare table with an egg crate foam mattress pad over the sheet to prevent the need for strapping the patient to the bed or the use of shoulder braces to prevent slippage.
- For low dorsal lithotomy positioning, flex the patient’s hips with a trunk-to-thigh angle of approximately 170°, and never more than 180°.
- For arm tucking, remove the arm boards and excess egg crate foam from the patient’s side and placecushioning over the elbow and the wrist. Keep the patient’s hand pronated when tucking and do not allow the arm to hang over the side of the bed.
- If the patient is obese, support the tucked arm by placing the arm boards beneath the arm parallel to the bed.
Next month we continue our series on surgical techniques with a video on why choosing the proper colpotomy cup is critical for successful minimally invasive hysterectomy.

Will you be joining me at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver this November? Safe patient positioning for minimally invasive surgery and other exciting topics will be discussed. Visit www.aagl.org/globalcongress for more information.
—Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Doctor Nurse? What Is That?
“Doctor nurse?” If you want to be a doctor, go to medical school, right? That’s what I and many of my medical and nursing colleagues have concluded since advanced nursing education has evolved into the Doctor of Nursing Practice (DNP) as the terminal degree for the profession.
School has always come fairly easily to me. Thus, I tend to turn to education for self-fulfillment. So, I researched the DNP. Nurse practitioners have been around since 1965, and myriad studies have determined the NP to be an effective (even superior, according to some studies) provider of health care. Despite this, the concept of NPs as care providers remains controversial, and the thought that nurses would aspire to an even more advanced station has become fodder for heated discussion.
Early concerns regarding the safety and quality of care provided by NPs have been deemed largely irrelevant by “bipartisan” study, but the value of a DNP continues to be debated. Much study and contemplation have led me to 3 rationales for the nursing doctorate: (1) The highest level of research-based education is needed to help develop the practice of professional nursing within a dynamic health care environment; (2) Nursing models of care are distinct from medical models of care, and DNPs will be well prepared to articulate these complementary distinctions; (3) The nursing profession needs to develop leaders who are prepared to work alongside other doctorate-prepared professionals to be able to contribute to the continued evaluation and improvement of a multifaceted health care system.
In order to contribute to the evolution of the health care system, the nursing profession must be able to define and refine its practices. The Affordable Care Act requires cost-effective ways to serve more patients. Nurse practitioners as independent providers will serve as gatekeepers of the health care needs for these patients, responsible for collaborating with other members of the health care team and consulting with specialists as needed. The actions of the NP must provide value: Models of care must be continually evaluated and modified to ensure that best practices are determined and maintained. Doctors of nursing practice will be in key positions to guide these processes and optimize outcomes.
As a profession, nursing focuses on the human’s response(s) to disruptions in health and on optimizing the state of wellness. We apply some of the same concepts when we interact with our health care organizations and strive to improve them. We embrace the concept of the wholeness of the individual (and the system!) rather than on isolating the separate parts. Doctors of nursing practice are able to articulate this model as distinct from medicine while recognizing areas of overlap. Such understanding is imperative as we develop the most cost-effective models of patient care.
The American Academy of Colleges of Nursing has endorsed the proposal that the doctorate will be the entry level of education for nurse practitioners by 2015. The Institute of Medicine recommends doubling the number of nurses with doctorates by 2020. Our peers in pharmacy, psychology, occupational therapy, etc, have already recognized the value of higher academic and clinical preparation for leaders in their fields. Competence and leadership are gained not only through experience, but also through formal research-based learning. The doctorate in any profession or field of study has traditionally represented the most advanced level of practice and education.
As the largest of the health care–related fields, nursing is long overdue for being recognized as a profession that is on par with our colleagues. The DNP provides the avenue for such recognition.
The DNP is a doctorate in areas relating to clinical practice and health care organizational leadership. The degree is becoming a necessary pursuit, because health care is changing at an incredibly fast pace. As NPs, we are ready to earn the distinction as a recognized professional leader with the attainment of doctorate education.
Thus, though I have not come to terms with my new role of widow yet, I eagerly embrace the opportunity to one day introduce myself as “Dr. Brennan, your nurse practitioner.”
“Doctor nurse?” If you want to be a doctor, go to medical school, right? That’s what I and many of my medical and nursing colleagues have concluded since advanced nursing education has evolved into the Doctor of Nursing Practice (DNP) as the terminal degree for the profession.
School has always come fairly easily to me. Thus, I tend to turn to education for self-fulfillment. So, I researched the DNP. Nurse practitioners have been around since 1965, and myriad studies have determined the NP to be an effective (even superior, according to some studies) provider of health care. Despite this, the concept of NPs as care providers remains controversial, and the thought that nurses would aspire to an even more advanced station has become fodder for heated discussion.
Early concerns regarding the safety and quality of care provided by NPs have been deemed largely irrelevant by “bipartisan” study, but the value of a DNP continues to be debated. Much study and contemplation have led me to 3 rationales for the nursing doctorate: (1) The highest level of research-based education is needed to help develop the practice of professional nursing within a dynamic health care environment; (2) Nursing models of care are distinct from medical models of care, and DNPs will be well prepared to articulate these complementary distinctions; (3) The nursing profession needs to develop leaders who are prepared to work alongside other doctorate-prepared professionals to be able to contribute to the continued evaluation and improvement of a multifaceted health care system.
In order to contribute to the evolution of the health care system, the nursing profession must be able to define and refine its practices. The Affordable Care Act requires cost-effective ways to serve more patients. Nurse practitioners as independent providers will serve as gatekeepers of the health care needs for these patients, responsible for collaborating with other members of the health care team and consulting with specialists as needed. The actions of the NP must provide value: Models of care must be continually evaluated and modified to ensure that best practices are determined and maintained. Doctors of nursing practice will be in key positions to guide these processes and optimize outcomes.
As a profession, nursing focuses on the human’s response(s) to disruptions in health and on optimizing the state of wellness. We apply some of the same concepts when we interact with our health care organizations and strive to improve them. We embrace the concept of the wholeness of the individual (and the system!) rather than on isolating the separate parts. Doctors of nursing practice are able to articulate this model as distinct from medicine while recognizing areas of overlap. Such understanding is imperative as we develop the most cost-effective models of patient care.
The American Academy of Colleges of Nursing has endorsed the proposal that the doctorate will be the entry level of education for nurse practitioners by 2015. The Institute of Medicine recommends doubling the number of nurses with doctorates by 2020. Our peers in pharmacy, psychology, occupational therapy, etc, have already recognized the value of higher academic and clinical preparation for leaders in their fields. Competence and leadership are gained not only through experience, but also through formal research-based learning. The doctorate in any profession or field of study has traditionally represented the most advanced level of practice and education.
As the largest of the health care–related fields, nursing is long overdue for being recognized as a profession that is on par with our colleagues. The DNP provides the avenue for such recognition.
The DNP is a doctorate in areas relating to clinical practice and health care organizational leadership. The degree is becoming a necessary pursuit, because health care is changing at an incredibly fast pace. As NPs, we are ready to earn the distinction as a recognized professional leader with the attainment of doctorate education.
Thus, though I have not come to terms with my new role of widow yet, I eagerly embrace the opportunity to one day introduce myself as “Dr. Brennan, your nurse practitioner.”
“Doctor nurse?” If you want to be a doctor, go to medical school, right? That’s what I and many of my medical and nursing colleagues have concluded since advanced nursing education has evolved into the Doctor of Nursing Practice (DNP) as the terminal degree for the profession.
School has always come fairly easily to me. Thus, I tend to turn to education for self-fulfillment. So, I researched the DNP. Nurse practitioners have been around since 1965, and myriad studies have determined the NP to be an effective (even superior, according to some studies) provider of health care. Despite this, the concept of NPs as care providers remains controversial, and the thought that nurses would aspire to an even more advanced station has become fodder for heated discussion.
Early concerns regarding the safety and quality of care provided by NPs have been deemed largely irrelevant by “bipartisan” study, but the value of a DNP continues to be debated. Much study and contemplation have led me to 3 rationales for the nursing doctorate: (1) The highest level of research-based education is needed to help develop the practice of professional nursing within a dynamic health care environment; (2) Nursing models of care are distinct from medical models of care, and DNPs will be well prepared to articulate these complementary distinctions; (3) The nursing profession needs to develop leaders who are prepared to work alongside other doctorate-prepared professionals to be able to contribute to the continued evaluation and improvement of a multifaceted health care system.
In order to contribute to the evolution of the health care system, the nursing profession must be able to define and refine its practices. The Affordable Care Act requires cost-effective ways to serve more patients. Nurse practitioners as independent providers will serve as gatekeepers of the health care needs for these patients, responsible for collaborating with other members of the health care team and consulting with specialists as needed. The actions of the NP must provide value: Models of care must be continually evaluated and modified to ensure that best practices are determined and maintained. Doctors of nursing practice will be in key positions to guide these processes and optimize outcomes.
As a profession, nursing focuses on the human’s response(s) to disruptions in health and on optimizing the state of wellness. We apply some of the same concepts when we interact with our health care organizations and strive to improve them. We embrace the concept of the wholeness of the individual (and the system!) rather than on isolating the separate parts. Doctors of nursing practice are able to articulate this model as distinct from medicine while recognizing areas of overlap. Such understanding is imperative as we develop the most cost-effective models of patient care.
The American Academy of Colleges of Nursing has endorsed the proposal that the doctorate will be the entry level of education for nurse practitioners by 2015. The Institute of Medicine recommends doubling the number of nurses with doctorates by 2020. Our peers in pharmacy, psychology, occupational therapy, etc, have already recognized the value of higher academic and clinical preparation for leaders in their fields. Competence and leadership are gained not only through experience, but also through formal research-based learning. The doctorate in any profession or field of study has traditionally represented the most advanced level of practice and education.
As the largest of the health care–related fields, nursing is long overdue for being recognized as a profession that is on par with our colleagues. The DNP provides the avenue for such recognition.
The DNP is a doctorate in areas relating to clinical practice and health care organizational leadership. The degree is becoming a necessary pursuit, because health care is changing at an incredibly fast pace. As NPs, we are ready to earn the distinction as a recognized professional leader with the attainment of doctorate education.
Thus, though I have not come to terms with my new role of widow yet, I eagerly embrace the opportunity to one day introduce myself as “Dr. Brennan, your nurse practitioner.”
Management of dermatological toxicities in patients receiving EGFR inhibitors
Patients receiving treatment with epidermal growth factor receptor inhibitors often experience dermatological toxicities. The majority of patients develop skin rash, and may also experience adverse nail and periungual alterations. EGFR inhibitors have become part of the standard of care for several solid tumors, including metastatic colorectal cancer, cancers of the head and neck, and non small-cell lung cancer, thus adequate management of these side effects is necessary to ensure patient compliance to therapy, as well as to maximize patient comfort and quality of life. This review presents a protocol our center optimized to successfully manage cetuximab-associated acneiform rash and nail toxicities.
Click on the PDF icon at the top of this introduction to read the full article.
Patients receiving treatment with epidermal growth factor receptor inhibitors often experience dermatological toxicities. The majority of patients develop skin rash, and may also experience adverse nail and periungual alterations. EGFR inhibitors have become part of the standard of care for several solid tumors, including metastatic colorectal cancer, cancers of the head and neck, and non small-cell lung cancer, thus adequate management of these side effects is necessary to ensure patient compliance to therapy, as well as to maximize patient comfort and quality of life. This review presents a protocol our center optimized to successfully manage cetuximab-associated acneiform rash and nail toxicities.
Click on the PDF icon at the top of this introduction to read the full article.
Patients receiving treatment with epidermal growth factor receptor inhibitors often experience dermatological toxicities. The majority of patients develop skin rash, and may also experience adverse nail and periungual alterations. EGFR inhibitors have become part of the standard of care for several solid tumors, including metastatic colorectal cancer, cancers of the head and neck, and non small-cell lung cancer, thus adequate management of these side effects is necessary to ensure patient compliance to therapy, as well as to maximize patient comfort and quality of life. This review presents a protocol our center optimized to successfully manage cetuximab-associated acneiform rash and nail toxicities.
Click on the PDF icon at the top of this introduction to read the full article.