User login
CDC targets West Africa Ebola outbreak
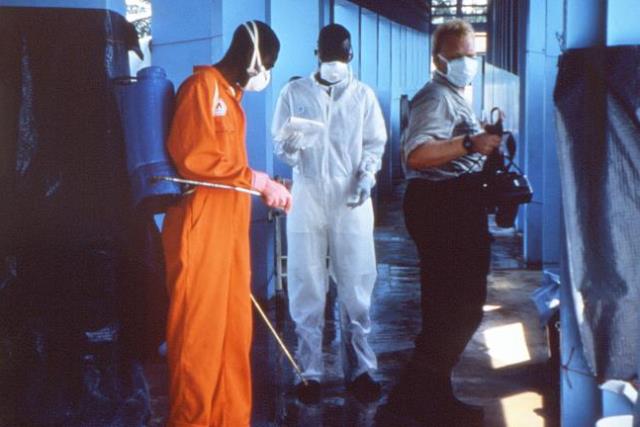
ATLANTA – The U.S. Centers for Disease Control and Prevention warned against nonessential travel to three West African countries facing the largest outbreak of Ebola virus in history and announced that it will send 50 more CDC personnel to assist those countries in the next 30 days.
The Ebola outbreak along the borders shared by Guinea, Liberia, and Sierra Leone is worsening, prompting the CDC to upgrade its response 4 days after it advised the public to take sensible, enhanced precautions when considering travel to that region.
The current outbreak is "the largest, most complex outbreak [of Ebola virus] that we know of in history," said Dr. Tom Frieden, director of the CDC. There is no known effective treatment for Ebola or vaccine against it.
The U.S. population is not at risk of an Ebola outbreak, however, because it has quarantine stations at all major ports of entry and isolation facilities in every hospital that has an intensive care unit, he said. The United States has a health care infrastructure better equipped to identify people who might have Ebola, rapidly test for the virus, monitor patients for signs of illness, and provide supportive care with infection control, Dr. Frieden added.
If health care workers see a patient who has a fever or other serious illness and has traveled to any of the three African countries recently, they should contact the CDC to arrange rapid testing and appropriate follow-up. An estimated 10,000 people travel between the United States and the three countries during a normal 3- or 4-month period, he said.
It’s important to note that Ebola is not spread by airborne routes, food, or water. People infected with Ebola are not contagious unless they are sick and someone comes in close contact with their infected bodily fluids. Anyone who may have been exposed to Ebolavirus (and all of their contacts) should be watched daily for 21 days to see if fever develops, Dr. Frieden said.
Many of the people who have died in the West African outbreak have been health care workers or people attending traditional funerals that include contact with the deceased person’s body.
The travel warning grew out of concern that people traveling to the West African countries might need medical attention for reasons unrelated to Ebola (such as appendicitis, a broken bone, or injuries sustained in a car accident), further stressing the local medical facilities and potentially exposing the travelers to Ebola when seeking care.
The surge in CDC infection control specialists headed to West Africa will help those countries develop the capacity to rapidly identify and isolate infected people and to screen travelers who are thinking of flying out of the country.
The CDC has worked with other African countries in the past to quell Ebola outbreaks through boots-on-the-ground infection control procedures. In Uganda, for example, working with traditional healers to recognize signs of Ebola and to make burial practices safer changed the environment so that "where there used to be large outbreaks, there are now single cases," Dr. Frieden said.
Quelling the West African outbreak would take at least 3-6 months under ideal conditions, but surely will take longer in West Africa, facing its first Ebola outbreak, he noted. The medical and public health infrastructures are limited and not used to dealing with Ebola, and public misconceptions about the virus have led to violence against some infection control workers.
"We already had one team that was confronted by an angry group of people and had to retreat across border to a safe country," Dr. Frieden said.
On Twitter @sherryboschert
ATLANTA – The U.S. Centers for Disease Control and Prevention warned against nonessential travel to three West African countries facing the largest outbreak of Ebola virus in history and announced that it will send 50 more CDC personnel to assist those countries in the next 30 days.
The Ebola outbreak along the borders shared by Guinea, Liberia, and Sierra Leone is worsening, prompting the CDC to upgrade its response 4 days after it advised the public to take sensible, enhanced precautions when considering travel to that region.
The current outbreak is "the largest, most complex outbreak [of Ebola virus] that we know of in history," said Dr. Tom Frieden, director of the CDC. There is no known effective treatment for Ebola or vaccine against it.
The U.S. population is not at risk of an Ebola outbreak, however, because it has quarantine stations at all major ports of entry and isolation facilities in every hospital that has an intensive care unit, he said. The United States has a health care infrastructure better equipped to identify people who might have Ebola, rapidly test for the virus, monitor patients for signs of illness, and provide supportive care with infection control, Dr. Frieden added.
If health care workers see a patient who has a fever or other serious illness and has traveled to any of the three African countries recently, they should contact the CDC to arrange rapid testing and appropriate follow-up. An estimated 10,000 people travel between the United States and the three countries during a normal 3- or 4-month period, he said.
It’s important to note that Ebola is not spread by airborne routes, food, or water. People infected with Ebola are not contagious unless they are sick and someone comes in close contact with their infected bodily fluids. Anyone who may have been exposed to Ebolavirus (and all of their contacts) should be watched daily for 21 days to see if fever develops, Dr. Frieden said.
Many of the people who have died in the West African outbreak have been health care workers or people attending traditional funerals that include contact with the deceased person’s body.
The travel warning grew out of concern that people traveling to the West African countries might need medical attention for reasons unrelated to Ebola (such as appendicitis, a broken bone, or injuries sustained in a car accident), further stressing the local medical facilities and potentially exposing the travelers to Ebola when seeking care.
The surge in CDC infection control specialists headed to West Africa will help those countries develop the capacity to rapidly identify and isolate infected people and to screen travelers who are thinking of flying out of the country.
The CDC has worked with other African countries in the past to quell Ebola outbreaks through boots-on-the-ground infection control procedures. In Uganda, for example, working with traditional healers to recognize signs of Ebola and to make burial practices safer changed the environment so that "where there used to be large outbreaks, there are now single cases," Dr. Frieden said.
Quelling the West African outbreak would take at least 3-6 months under ideal conditions, but surely will take longer in West Africa, facing its first Ebola outbreak, he noted. The medical and public health infrastructures are limited and not used to dealing with Ebola, and public misconceptions about the virus have led to violence against some infection control workers.
"We already had one team that was confronted by an angry group of people and had to retreat across border to a safe country," Dr. Frieden said.
On Twitter @sherryboschert
ATLANTA – The U.S. Centers for Disease Control and Prevention warned against nonessential travel to three West African countries facing the largest outbreak of Ebola virus in history and announced that it will send 50 more CDC personnel to assist those countries in the next 30 days.
The Ebola outbreak along the borders shared by Guinea, Liberia, and Sierra Leone is worsening, prompting the CDC to upgrade its response 4 days after it advised the public to take sensible, enhanced precautions when considering travel to that region.
The current outbreak is "the largest, most complex outbreak [of Ebola virus] that we know of in history," said Dr. Tom Frieden, director of the CDC. There is no known effective treatment for Ebola or vaccine against it.
The U.S. population is not at risk of an Ebola outbreak, however, because it has quarantine stations at all major ports of entry and isolation facilities in every hospital that has an intensive care unit, he said. The United States has a health care infrastructure better equipped to identify people who might have Ebola, rapidly test for the virus, monitor patients for signs of illness, and provide supportive care with infection control, Dr. Frieden added.
If health care workers see a patient who has a fever or other serious illness and has traveled to any of the three African countries recently, they should contact the CDC to arrange rapid testing and appropriate follow-up. An estimated 10,000 people travel between the United States and the three countries during a normal 3- or 4-month period, he said.
It’s important to note that Ebola is not spread by airborne routes, food, or water. People infected with Ebola are not contagious unless they are sick and someone comes in close contact with their infected bodily fluids. Anyone who may have been exposed to Ebolavirus (and all of their contacts) should be watched daily for 21 days to see if fever develops, Dr. Frieden said.
Many of the people who have died in the West African outbreak have been health care workers or people attending traditional funerals that include contact with the deceased person’s body.
The travel warning grew out of concern that people traveling to the West African countries might need medical attention for reasons unrelated to Ebola (such as appendicitis, a broken bone, or injuries sustained in a car accident), further stressing the local medical facilities and potentially exposing the travelers to Ebola when seeking care.
The surge in CDC infection control specialists headed to West Africa will help those countries develop the capacity to rapidly identify and isolate infected people and to screen travelers who are thinking of flying out of the country.
The CDC has worked with other African countries in the past to quell Ebola outbreaks through boots-on-the-ground infection control procedures. In Uganda, for example, working with traditional healers to recognize signs of Ebola and to make burial practices safer changed the environment so that "where there used to be large outbreaks, there are now single cases," Dr. Frieden said.
Quelling the West African outbreak would take at least 3-6 months under ideal conditions, but surely will take longer in West Africa, facing its first Ebola outbreak, he noted. The medical and public health infrastructures are limited and not used to dealing with Ebola, and public misconceptions about the virus have led to violence against some infection control workers.
"We already had one team that was confronted by an angry group of people and had to retreat across border to a safe country," Dr. Frieden said.
On Twitter @sherryboschert
FROM A CDC PRESS CONFERENCE
United States Diabetes Epidemic may be Slowing
SAN FRANCISCO – The U.S. incidence of adult diabetes doubled between 1980 and 2008 but has fallen a bit since then, which may be a sign that the diabetes epidemic is abating, according to Linda S. Geiss a health statistician with the Centers for Disease Control and Prevention.
This potentially good news does not apply to everyone, however. Both the incidence and prevalence of diabetes continue to increase in Hispanics, non-Hispanic blacks, and adults with less than a high school education, Ms. Geiss and her associates reported at the annual scientific session of the American Diabetes Association.
They studied annual data from the 1980-2012 National Health Interview Surveys to identify diabetes trends in U.S. residents aged 20-79 years. The age-adjusted prevalence and incidence of diagnosed diabetes changed little in the 1980s but each doubled between 1990 and 2008, she said.
During that time period, the U.S. population became older, less white, and better educated, she noted.
The age-adjusted incidence of diabetes increased from approximately 4/1,000 people in 1980 to more than 9/1,000 in 2008 and then declined to less than 8/1,000 in 2012, a statistically insignificant decrease after 2008. The age-adjusted prevalence of diabetes increased from approximately 4/100 people in 1980 to approximately 8/100 in 2008, with a slight increase after that, "although at a slower rate of pace," Ms. Geiss said.
Even when incidence declines, prevalence can continue to rise if the number of deaths among people with diabetes is smaller than the number of new diagnoses.
"Overall and for some subpopulations, incidence and/or prevalence slowed or plateaued around 2008. Some groups slowed earlier in the 2000s," she said. "After a steady 15- to 20-year increase in prevalence and incidence, we are seeing the first signs that the growth may be slowing or abating. However, given the uncertainty about the reasons behind these changes, future trends are uncertain. Given the large burden of diabetes in the United States, we need to sustain efforts to prevent diabetes and its complications," especially among population groups whose incidence and prevalence rates continue to climb.
Throughout the time period studied, the incidence and prevalence of diabetes were lowest among people aged 20-44 years and highest among people aged 65-79 years. For those two age groups, the incidence of diabetes increased throughout the time period. For middle-aged people of 45-64 years, the incidence plateaued in 2002. The prevalence of diabetes plateaued in 2008 for the middle-aged group and in 2003 for the oldest age group.
Incidence rates for men started to exceed those for women around 1997, continued increasing until 2008, and then declined, though not significantly. The incidence for women increased throughout the time period studied. The prevalence of diabetes plateaued for men in 2001 and for women in 2008.
For adults with a high school education, the incidence of diabetes increased until 2008 and then decreased insignificantly. For other educational levels (more than or less than a high school education), the incidence increased throughout the period. The prevalence slowed among people with more than a high school education in 2000, but increased throughout the time period for the other educational levels.
The incidence and prevalence of diabetes were higher among Hispanics and non-Hispanic blacks than among whites between 1997 and 2012. For whites, the incidence increased from approximately 5/1,000 people in 1997 to 8/1,000 in 2008, then decreased insignificantly to 6/1,000 in 2012. The prevalence of diabetes in whites slowed its rate of increase starting in 2005, Ms. Geiss reported.
"With these cross-sectional data, you can’t determine the reasons behind trend changes," she said. The nationally representative data spanning 3 decades give strength to the findings, but the surveys did not include institutionalized residents or people with undiagnosed diabetes. The study could not distinguish trends for type 1 vs. type 2 diabetes.
One physician in the audience asked if the global financial crisis in 2008 may have been a factor in slowing the diabetes epidemic.
Ms. Geiss said she hadn’t considered that possible explanation. Other factors that may have affected the incidence of diabetes include the adoption of hemoglobin A1c (HbA1c) for the diagnosis of diabetes, she speculated. "We know that HbA1c tends to identify fewer people who have hyperglycemia," she said. Also, U.S. obesity rates have not increased since 2003-2004, and a couple of separate studies have reported declining caloric intake by the U.S. population. Each of these factors may be "prominent drivers" of the slowing incidence of diabetes, she said.
Ms. Geiss reported having no financial disclosures.
On Twitter @sherryboschert
This was an interesting study. One thing to consider is whether the CDC has changed the way it defines diabetes, which the speaker hinted that they sort of have. She hinted that the HbA1c is less sensitive to diabetes. So, if you changed the way you diagnose diabetes, and you get a different number of people diagnosed with diabetes, it may be that there are truly fewer cases of diabetes or it may just be that the new test didn’t pick up all of the people the old tests did.
I think the public health messages shouldn’t change: Be active. Don’t gain weight. And all the other diabetes prevention messages. If primary care doctors have been encouraging people to do that, maybe this is evidence that their work is paying off. That would be a positive message.
Dr. Amanda Adler is consultant physician at Cambridge (England) University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence, England. She gave these comments in an interview at the meeting.
This was an interesting study. One thing to consider is whether the CDC has changed the way it defines diabetes, which the speaker hinted that they sort of have. She hinted that the HbA1c is less sensitive to diabetes. So, if you changed the way you diagnose diabetes, and you get a different number of people diagnosed with diabetes, it may be that there are truly fewer cases of diabetes or it may just be that the new test didn’t pick up all of the people the old tests did.
I think the public health messages shouldn’t change: Be active. Don’t gain weight. And all the other diabetes prevention messages. If primary care doctors have been encouraging people to do that, maybe this is evidence that their work is paying off. That would be a positive message.
Dr. Amanda Adler is consultant physician at Cambridge (England) University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence, England. She gave these comments in an interview at the meeting.
This was an interesting study. One thing to consider is whether the CDC has changed the way it defines diabetes, which the speaker hinted that they sort of have. She hinted that the HbA1c is less sensitive to diabetes. So, if you changed the way you diagnose diabetes, and you get a different number of people diagnosed with diabetes, it may be that there are truly fewer cases of diabetes or it may just be that the new test didn’t pick up all of the people the old tests did.
I think the public health messages shouldn’t change: Be active. Don’t gain weight. And all the other diabetes prevention messages. If primary care doctors have been encouraging people to do that, maybe this is evidence that their work is paying off. That would be a positive message.
Dr. Amanda Adler is consultant physician at Cambridge (England) University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence, England. She gave these comments in an interview at the meeting.
SAN FRANCISCO – The U.S. incidence of adult diabetes doubled between 1980 and 2008 but has fallen a bit since then, which may be a sign that the diabetes epidemic is abating, according to Linda S. Geiss a health statistician with the Centers for Disease Control and Prevention.
This potentially good news does not apply to everyone, however. Both the incidence and prevalence of diabetes continue to increase in Hispanics, non-Hispanic blacks, and adults with less than a high school education, Ms. Geiss and her associates reported at the annual scientific session of the American Diabetes Association.
They studied annual data from the 1980-2012 National Health Interview Surveys to identify diabetes trends in U.S. residents aged 20-79 years. The age-adjusted prevalence and incidence of diagnosed diabetes changed little in the 1980s but each doubled between 1990 and 2008, she said.
During that time period, the U.S. population became older, less white, and better educated, she noted.
The age-adjusted incidence of diabetes increased from approximately 4/1,000 people in 1980 to more than 9/1,000 in 2008 and then declined to less than 8/1,000 in 2012, a statistically insignificant decrease after 2008. The age-adjusted prevalence of diabetes increased from approximately 4/100 people in 1980 to approximately 8/100 in 2008, with a slight increase after that, "although at a slower rate of pace," Ms. Geiss said.
Even when incidence declines, prevalence can continue to rise if the number of deaths among people with diabetes is smaller than the number of new diagnoses.
"Overall and for some subpopulations, incidence and/or prevalence slowed or plateaued around 2008. Some groups slowed earlier in the 2000s," she said. "After a steady 15- to 20-year increase in prevalence and incidence, we are seeing the first signs that the growth may be slowing or abating. However, given the uncertainty about the reasons behind these changes, future trends are uncertain. Given the large burden of diabetes in the United States, we need to sustain efforts to prevent diabetes and its complications," especially among population groups whose incidence and prevalence rates continue to climb.
Throughout the time period studied, the incidence and prevalence of diabetes were lowest among people aged 20-44 years and highest among people aged 65-79 years. For those two age groups, the incidence of diabetes increased throughout the time period. For middle-aged people of 45-64 years, the incidence plateaued in 2002. The prevalence of diabetes plateaued in 2008 for the middle-aged group and in 2003 for the oldest age group.
Incidence rates for men started to exceed those for women around 1997, continued increasing until 2008, and then declined, though not significantly. The incidence for women increased throughout the time period studied. The prevalence of diabetes plateaued for men in 2001 and for women in 2008.
For adults with a high school education, the incidence of diabetes increased until 2008 and then decreased insignificantly. For other educational levels (more than or less than a high school education), the incidence increased throughout the period. The prevalence slowed among people with more than a high school education in 2000, but increased throughout the time period for the other educational levels.
The incidence and prevalence of diabetes were higher among Hispanics and non-Hispanic blacks than among whites between 1997 and 2012. For whites, the incidence increased from approximately 5/1,000 people in 1997 to 8/1,000 in 2008, then decreased insignificantly to 6/1,000 in 2012. The prevalence of diabetes in whites slowed its rate of increase starting in 2005, Ms. Geiss reported.
"With these cross-sectional data, you can’t determine the reasons behind trend changes," she said. The nationally representative data spanning 3 decades give strength to the findings, but the surveys did not include institutionalized residents or people with undiagnosed diabetes. The study could not distinguish trends for type 1 vs. type 2 diabetes.
One physician in the audience asked if the global financial crisis in 2008 may have been a factor in slowing the diabetes epidemic.
Ms. Geiss said she hadn’t considered that possible explanation. Other factors that may have affected the incidence of diabetes include the adoption of hemoglobin A1c (HbA1c) for the diagnosis of diabetes, she speculated. "We know that HbA1c tends to identify fewer people who have hyperglycemia," she said. Also, U.S. obesity rates have not increased since 2003-2004, and a couple of separate studies have reported declining caloric intake by the U.S. population. Each of these factors may be "prominent drivers" of the slowing incidence of diabetes, she said.
Ms. Geiss reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – The U.S. incidence of adult diabetes doubled between 1980 and 2008 but has fallen a bit since then, which may be a sign that the diabetes epidemic is abating, according to Linda S. Geiss a health statistician with the Centers for Disease Control and Prevention.
This potentially good news does not apply to everyone, however. Both the incidence and prevalence of diabetes continue to increase in Hispanics, non-Hispanic blacks, and adults with less than a high school education, Ms. Geiss and her associates reported at the annual scientific session of the American Diabetes Association.
They studied annual data from the 1980-2012 National Health Interview Surveys to identify diabetes trends in U.S. residents aged 20-79 years. The age-adjusted prevalence and incidence of diagnosed diabetes changed little in the 1980s but each doubled between 1990 and 2008, she said.
During that time period, the U.S. population became older, less white, and better educated, she noted.
The age-adjusted incidence of diabetes increased from approximately 4/1,000 people in 1980 to more than 9/1,000 in 2008 and then declined to less than 8/1,000 in 2012, a statistically insignificant decrease after 2008. The age-adjusted prevalence of diabetes increased from approximately 4/100 people in 1980 to approximately 8/100 in 2008, with a slight increase after that, "although at a slower rate of pace," Ms. Geiss said.
Even when incidence declines, prevalence can continue to rise if the number of deaths among people with diabetes is smaller than the number of new diagnoses.
"Overall and for some subpopulations, incidence and/or prevalence slowed or plateaued around 2008. Some groups slowed earlier in the 2000s," she said. "After a steady 15- to 20-year increase in prevalence and incidence, we are seeing the first signs that the growth may be slowing or abating. However, given the uncertainty about the reasons behind these changes, future trends are uncertain. Given the large burden of diabetes in the United States, we need to sustain efforts to prevent diabetes and its complications," especially among population groups whose incidence and prevalence rates continue to climb.
Throughout the time period studied, the incidence and prevalence of diabetes were lowest among people aged 20-44 years and highest among people aged 65-79 years. For those two age groups, the incidence of diabetes increased throughout the time period. For middle-aged people of 45-64 years, the incidence plateaued in 2002. The prevalence of diabetes plateaued in 2008 for the middle-aged group and in 2003 for the oldest age group.
Incidence rates for men started to exceed those for women around 1997, continued increasing until 2008, and then declined, though not significantly. The incidence for women increased throughout the time period studied. The prevalence of diabetes plateaued for men in 2001 and for women in 2008.
For adults with a high school education, the incidence of diabetes increased until 2008 and then decreased insignificantly. For other educational levels (more than or less than a high school education), the incidence increased throughout the period. The prevalence slowed among people with more than a high school education in 2000, but increased throughout the time period for the other educational levels.
The incidence and prevalence of diabetes were higher among Hispanics and non-Hispanic blacks than among whites between 1997 and 2012. For whites, the incidence increased from approximately 5/1,000 people in 1997 to 8/1,000 in 2008, then decreased insignificantly to 6/1,000 in 2012. The prevalence of diabetes in whites slowed its rate of increase starting in 2005, Ms. Geiss reported.
"With these cross-sectional data, you can’t determine the reasons behind trend changes," she said. The nationally representative data spanning 3 decades give strength to the findings, but the surveys did not include institutionalized residents or people with undiagnosed diabetes. The study could not distinguish trends for type 1 vs. type 2 diabetes.
One physician in the audience asked if the global financial crisis in 2008 may have been a factor in slowing the diabetes epidemic.
Ms. Geiss said she hadn’t considered that possible explanation. Other factors that may have affected the incidence of diabetes include the adoption of hemoglobin A1c (HbA1c) for the diagnosis of diabetes, she speculated. "We know that HbA1c tends to identify fewer people who have hyperglycemia," she said. Also, U.S. obesity rates have not increased since 2003-2004, and a couple of separate studies have reported declining caloric intake by the U.S. population. Each of these factors may be "prominent drivers" of the slowing incidence of diabetes, she said.
Ms. Geiss reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSION
Markers predict hypoglycemia on intensive glycemic therapy
SAN FRANCISCO – Patients with type 2 diabetes who were insulin deficient were 36 times more likely to develop severe hypoglycemia on treatment and to fail to get hemoglobin A1c levels below 6% after starting intensive therapy in a retrospective analysis of data on 1,401 patients.
In addition, patients with any of four antibodies against islet cells at baseline were 4-12 times more likely to develop severe hypoglycemia and fail to reach the glycemic target on intensive therapy, compared with patients without those biomarkers, Dr. Lisa Chow reported at the annual scientific sessions of the American Diabetes Association.
The study defined insulin deficiency as a fasting C-peptide level no higher than 0.45 ng/mL. Investigators measured levels of three of the autoantibodies and considered the fourth – insulin autoantibody (IAA) – to be present if the patient used insulin at baseline.
In unadjusted analyses, the likelihood of severe hypoglycemia and failure to reach the glycemic target was four times higher in patients with IAA or antibodies against glutamic acid decarboxylase (GAD) or zinc transporter 8 (ZnT8), compared with patients without those autoantibodies. Severe hypoglycemia and failure to get hemoglobin A1c (HbA1c) below 6% were 11 times more likely in patients with antibodies against tyrosine phosphatase–related islet antigen 2 (IA-2), reported Dr. Chow, an endocrinologist at the University of Minnesota, Minneapolis.
She and her associates studied data on 1,401 patients who were randomized to the intensive glycemic control arm of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. They compared 326 patients ("cases") who developed severe hypoglycemia and whose HbA1c levels did not reach the target of less than 6% with 1,075 control patients (matched 4:1 by age, race, and body mass index) who did not have severe hypoglycemia and who reached the HbA1c target.
Overall, 17% of cases and 1% of controls were insulin deficient. Excluding IAA (present in 62% of cases and 26% of controls), the most common islet antibody was GAD, in 17% of cases and 6% of controls. IA-2 was present in 4% of cases and 0.4% of controls, and ZnT8 was present in 2% of cases and 0.7% of controls.
"We propose that measuring C-peptide and GAD antibodies in patients with type 2 diabetes may serve as a biomarker to help tailor and individualize therapy" by predicting which patients are more likely to have adverse outcomes on intensive glycemic treatment, Dr. Chow said.
At baseline, the case group was significantly more likely to use insulin, compared with controls (89% and 24%, respectively) and less likely to be male (50% vs. 59%). The case patients had a higher HbA1c at baseline, compared with controls (8.54% vs. 8.08%, respectively) and a longer duration of diabetes (15 vs. 9 years).
After adjusting for the effects of age and body mass index, the combined outcome of severe hypoglycemia and failure to reach the glycemic target was 32 times more likely in patients with insulin deficiency at baseline, 3 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 9 times more likely in patients with IA-2, compared with patients without those markers, Dr. Chow said.
A third analysis removed data for any case patients who died and their associated controls and found that severe hypoglycemia and failure to reach the glycemic target was 30 times more likely in patients with insulin deficiency at baseline, 4 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 12 times more likely in patients with IA-2, compared with patients without those markers.
The study defined severe hypoglycemia as any hypoglycemia requiring assistance. Patients who developed severe hypoglycemia were four times less likely to get their HbA1c levels below 6%.
Dr. Chow reported having no financial disclosures. The National Institutes of Health funded the study.
On Twitter @sherryboschert
I don’t think this study means that we automatically should test everybody with type 2 diabetes for their insulin levels and their autoantibodies because we would need a study to show that if you did that, versus not doing that, people actually do better.
 |
|
I think what this study tells us is that there is a fair amount of slow-burn type 1 diabetes amongst people who we think have type 2 diabetes. Perhaps unsurprisingly, those people tend to have more hypoglycemia and trouble.
The study defined poor glycemic control as not being able to get an HbA1c of less than 6%. To be fair, that’s what the ACCORD trial said. Clinically, nobody would consider someone with an HbA1c of 6.2% to have poor glycemic control.
One take-home message might be that if your patient has poor glycemic control and severe hypoglycemia, consider checking for autoantibodies.
Dr. Amanda Adler is consultant physician at Cambridge University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence, England. She gave these comments in an interview at the meeting.
I don’t think this study means that we automatically should test everybody with type 2 diabetes for their insulin levels and their autoantibodies because we would need a study to show that if you did that, versus not doing that, people actually do better.
 |
|
I think what this study tells us is that there is a fair amount of slow-burn type 1 diabetes amongst people who we think have type 2 diabetes. Perhaps unsurprisingly, those people tend to have more hypoglycemia and trouble.
The study defined poor glycemic control as not being able to get an HbA1c of less than 6%. To be fair, that’s what the ACCORD trial said. Clinically, nobody would consider someone with an HbA1c of 6.2% to have poor glycemic control.
One take-home message might be that if your patient has poor glycemic control and severe hypoglycemia, consider checking for autoantibodies.
Dr. Amanda Adler is consultant physician at Cambridge University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence, England. She gave these comments in an interview at the meeting.
I don’t think this study means that we automatically should test everybody with type 2 diabetes for their insulin levels and their autoantibodies because we would need a study to show that if you did that, versus not doing that, people actually do better.
 |
|
I think what this study tells us is that there is a fair amount of slow-burn type 1 diabetes amongst people who we think have type 2 diabetes. Perhaps unsurprisingly, those people tend to have more hypoglycemia and trouble.
The study defined poor glycemic control as not being able to get an HbA1c of less than 6%. To be fair, that’s what the ACCORD trial said. Clinically, nobody would consider someone with an HbA1c of 6.2% to have poor glycemic control.
One take-home message might be that if your patient has poor glycemic control and severe hypoglycemia, consider checking for autoantibodies.
Dr. Amanda Adler is consultant physician at Cambridge University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence, England. She gave these comments in an interview at the meeting.
SAN FRANCISCO – Patients with type 2 diabetes who were insulin deficient were 36 times more likely to develop severe hypoglycemia on treatment and to fail to get hemoglobin A1c levels below 6% after starting intensive therapy in a retrospective analysis of data on 1,401 patients.
In addition, patients with any of four antibodies against islet cells at baseline were 4-12 times more likely to develop severe hypoglycemia and fail to reach the glycemic target on intensive therapy, compared with patients without those biomarkers, Dr. Lisa Chow reported at the annual scientific sessions of the American Diabetes Association.
The study defined insulin deficiency as a fasting C-peptide level no higher than 0.45 ng/mL. Investigators measured levels of three of the autoantibodies and considered the fourth – insulin autoantibody (IAA) – to be present if the patient used insulin at baseline.
In unadjusted analyses, the likelihood of severe hypoglycemia and failure to reach the glycemic target was four times higher in patients with IAA or antibodies against glutamic acid decarboxylase (GAD) or zinc transporter 8 (ZnT8), compared with patients without those autoantibodies. Severe hypoglycemia and failure to get hemoglobin A1c (HbA1c) below 6% were 11 times more likely in patients with antibodies against tyrosine phosphatase–related islet antigen 2 (IA-2), reported Dr. Chow, an endocrinologist at the University of Minnesota, Minneapolis.
She and her associates studied data on 1,401 patients who were randomized to the intensive glycemic control arm of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. They compared 326 patients ("cases") who developed severe hypoglycemia and whose HbA1c levels did not reach the target of less than 6% with 1,075 control patients (matched 4:1 by age, race, and body mass index) who did not have severe hypoglycemia and who reached the HbA1c target.
Overall, 17% of cases and 1% of controls were insulin deficient. Excluding IAA (present in 62% of cases and 26% of controls), the most common islet antibody was GAD, in 17% of cases and 6% of controls. IA-2 was present in 4% of cases and 0.4% of controls, and ZnT8 was present in 2% of cases and 0.7% of controls.
"We propose that measuring C-peptide and GAD antibodies in patients with type 2 diabetes may serve as a biomarker to help tailor and individualize therapy" by predicting which patients are more likely to have adverse outcomes on intensive glycemic treatment, Dr. Chow said.
At baseline, the case group was significantly more likely to use insulin, compared with controls (89% and 24%, respectively) and less likely to be male (50% vs. 59%). The case patients had a higher HbA1c at baseline, compared with controls (8.54% vs. 8.08%, respectively) and a longer duration of diabetes (15 vs. 9 years).
After adjusting for the effects of age and body mass index, the combined outcome of severe hypoglycemia and failure to reach the glycemic target was 32 times more likely in patients with insulin deficiency at baseline, 3 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 9 times more likely in patients with IA-2, compared with patients without those markers, Dr. Chow said.
A third analysis removed data for any case patients who died and their associated controls and found that severe hypoglycemia and failure to reach the glycemic target was 30 times more likely in patients with insulin deficiency at baseline, 4 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 12 times more likely in patients with IA-2, compared with patients without those markers.
The study defined severe hypoglycemia as any hypoglycemia requiring assistance. Patients who developed severe hypoglycemia were four times less likely to get their HbA1c levels below 6%.
Dr. Chow reported having no financial disclosures. The National Institutes of Health funded the study.
On Twitter @sherryboschert
SAN FRANCISCO – Patients with type 2 diabetes who were insulin deficient were 36 times more likely to develop severe hypoglycemia on treatment and to fail to get hemoglobin A1c levels below 6% after starting intensive therapy in a retrospective analysis of data on 1,401 patients.
In addition, patients with any of four antibodies against islet cells at baseline were 4-12 times more likely to develop severe hypoglycemia and fail to reach the glycemic target on intensive therapy, compared with patients without those biomarkers, Dr. Lisa Chow reported at the annual scientific sessions of the American Diabetes Association.
The study defined insulin deficiency as a fasting C-peptide level no higher than 0.45 ng/mL. Investigators measured levels of three of the autoantibodies and considered the fourth – insulin autoantibody (IAA) – to be present if the patient used insulin at baseline.
In unadjusted analyses, the likelihood of severe hypoglycemia and failure to reach the glycemic target was four times higher in patients with IAA or antibodies against glutamic acid decarboxylase (GAD) or zinc transporter 8 (ZnT8), compared with patients without those autoantibodies. Severe hypoglycemia and failure to get hemoglobin A1c (HbA1c) below 6% were 11 times more likely in patients with antibodies against tyrosine phosphatase–related islet antigen 2 (IA-2), reported Dr. Chow, an endocrinologist at the University of Minnesota, Minneapolis.
She and her associates studied data on 1,401 patients who were randomized to the intensive glycemic control arm of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. They compared 326 patients ("cases") who developed severe hypoglycemia and whose HbA1c levels did not reach the target of less than 6% with 1,075 control patients (matched 4:1 by age, race, and body mass index) who did not have severe hypoglycemia and who reached the HbA1c target.
Overall, 17% of cases and 1% of controls were insulin deficient. Excluding IAA (present in 62% of cases and 26% of controls), the most common islet antibody was GAD, in 17% of cases and 6% of controls. IA-2 was present in 4% of cases and 0.4% of controls, and ZnT8 was present in 2% of cases and 0.7% of controls.
"We propose that measuring C-peptide and GAD antibodies in patients with type 2 diabetes may serve as a biomarker to help tailor and individualize therapy" by predicting which patients are more likely to have adverse outcomes on intensive glycemic treatment, Dr. Chow said.
At baseline, the case group was significantly more likely to use insulin, compared with controls (89% and 24%, respectively) and less likely to be male (50% vs. 59%). The case patients had a higher HbA1c at baseline, compared with controls (8.54% vs. 8.08%, respectively) and a longer duration of diabetes (15 vs. 9 years).
After adjusting for the effects of age and body mass index, the combined outcome of severe hypoglycemia and failure to reach the glycemic target was 32 times more likely in patients with insulin deficiency at baseline, 3 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 9 times more likely in patients with IA-2, compared with patients without those markers, Dr. Chow said.
A third analysis removed data for any case patients who died and their associated controls and found that severe hypoglycemia and failure to reach the glycemic target was 30 times more likely in patients with insulin deficiency at baseline, 4 times more likely in patients with GAD or ZnT8, 5 times more likely in patients with IAA, and 12 times more likely in patients with IA-2, compared with patients without those markers.
The study defined severe hypoglycemia as any hypoglycemia requiring assistance. Patients who developed severe hypoglycemia were four times less likely to get their HbA1c levels below 6%.
Dr. Chow reported having no financial disclosures. The National Institutes of Health funded the study.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSION
Key clinical point: Consider measuring fasting C-peptide levels and testing for GAD autoantibodies before starting intensive therapy for type 2 diabetes.
Major finding: Severe hypoglycemia and failure to get HbA1c below 6% were 36 times more likely in patients with insulin deficiency and 4 times more likely in those with antibodies against GAD, compared with patients without those markers.
Data source: A retrospective, nested, case-control study of data on 1,401 patients from the intensive-therapy arm of the ACCORD trial.
Disclosures: Dr. Chow reported having no financial disclosures. The National Institutes of Health funded the study.
Inaccuracy plagues mobile blood pressure devices, videos
Separate studies related to hypertension send cautionary messages about smartphone-connected blood pressure cuffs and the quality of videos that patients see online about hypertension.
In one study, readings from three smartphone-connected blood pressure cuffs produced a wide range of measurements in an individual patient, raising questions about the apps’ accuracy even though those brands of devices previously had been validated. A separate survey of videos about hypertension posted on YouTube found lots of misleading information, often in the most popular videos.
Investigators presented the studies at the annual meeting of the American Society of Hypertension in New York.
Dr. Clarence E. Grim, an endocrinologist and former professor of medicine at the Medical College of Wisconsin, Milwaukee, tested three devices that connect to iPhones to enable patients to measure their blood pressure, store the results, and send the readings to others. Quality validation studies have been published for all three using international hypertension protocols, he said, and each passed muster with the Food and Drug Administration.
In multiple sessions over a 3-month period, Dr. Grim took his own blood pressure five times per session after being seated for 5 minutes, using the iHealth BP3 upper arm cuff, the iHealth BP7 wrist cuff, or the Withings upper arm blood pressure monitor. For reference measurements, he used a Tycos TR-2 Home Aneroid with an attached stethoscope for auscultatory measurements, validated against a mercury manometer.
In comparison with a reference systolic pressure of 138 using the auscultatory method, measurements using the iHealth arm device ranged from 127 to 158 mm Hg, with an average error of 8 mm Hg higher than the reference pressure. Measurements using the iHealth wrist device ranged from 123 to 164 mm Hg, with an average error of 13 mm Hg higher than the reference. Measurements using the Withings device ranged from 126 to 159 mm Hg. Although the average pressure with the Withings device did not differ significantly from the reference pressure, when there were errors, they tended to be large, he reported in an interview.
Diastolic pressure readings similarly were "not acceptable" due to wide variation, Dr. Grim said. With a reference diastolic pressure of 88 mm Hg, readings from either the iHealth arm device or the Withings device ranged from 80 to 100 mm Hg. With a reference diastolic pressure of 92 mm Hg, the iHealth wrist device readings ranged from 92 to 110 mm Hg.
No one should rely on a single blood pressure reading whether using a home device or the auscultatory method, Dr. Grim said. He’d prefer that automated devices be set to take three to five readings at a session. Anyone who chooses to use one of the three devices he tested should have a clinician check that the device is accurate on them, but the best way to test this is not clear, he added.
"I still have not found an automatic blood pressure device that is as accurate as auscultatory readings on me," he said.
Dr. Nilay Kumar, a hospitalist for Cambridge (Mass.) Health Alliance, separately reported at the meeting that he searched the popular video-sharing website YouTube using the terms "hypertension" and "high blood pressure." He and his associates analyzed English-language videos from the first 10 pages of search results for each term, comprising 209 videos of the 361,200 possible search results, and designated each video as useful, misleading, or a video of personal experiences.
While most were deemed useful (63%), 33% were misleading, and 4% represented patients’ personal experiences with hypertension (J. Am. Soc. Hypertens. 2014;8:e14-e15).
Cumulatively, the videos had been viewed more than 5.6 million times. Their usefulness did not correlate with the number of views per day, the number of "likes" or "dislikes" indicated by viewers, or comments left on the sites, he said in an e-mail interview. In fact, misleading videos had the highest numbers of views per day. Misleading videos were more likely to include advertisements for products for sale (52%), and 70% of misleading videos contained coverage of alternative treatments, often for products that are not recommended by American Heart Association guidelines.
The source of the video, however, did predict its usefulness. "Patients should trust videos from authoritative sources such as universities, professional organizations, and health information websites," Dr. Kumar said.
Dr. Grim and Dr. Kumar reported having no financial disclosures.
On Twitter @sherryboschert
Separate studies related to hypertension send cautionary messages about smartphone-connected blood pressure cuffs and the quality of videos that patients see online about hypertension.
In one study, readings from three smartphone-connected blood pressure cuffs produced a wide range of measurements in an individual patient, raising questions about the apps’ accuracy even though those brands of devices previously had been validated. A separate survey of videos about hypertension posted on YouTube found lots of misleading information, often in the most popular videos.
Investigators presented the studies at the annual meeting of the American Society of Hypertension in New York.
Dr. Clarence E. Grim, an endocrinologist and former professor of medicine at the Medical College of Wisconsin, Milwaukee, tested three devices that connect to iPhones to enable patients to measure their blood pressure, store the results, and send the readings to others. Quality validation studies have been published for all three using international hypertension protocols, he said, and each passed muster with the Food and Drug Administration.
In multiple sessions over a 3-month period, Dr. Grim took his own blood pressure five times per session after being seated for 5 minutes, using the iHealth BP3 upper arm cuff, the iHealth BP7 wrist cuff, or the Withings upper arm blood pressure monitor. For reference measurements, he used a Tycos TR-2 Home Aneroid with an attached stethoscope for auscultatory measurements, validated against a mercury manometer.
In comparison with a reference systolic pressure of 138 using the auscultatory method, measurements using the iHealth arm device ranged from 127 to 158 mm Hg, with an average error of 8 mm Hg higher than the reference pressure. Measurements using the iHealth wrist device ranged from 123 to 164 mm Hg, with an average error of 13 mm Hg higher than the reference. Measurements using the Withings device ranged from 126 to 159 mm Hg. Although the average pressure with the Withings device did not differ significantly from the reference pressure, when there were errors, they tended to be large, he reported in an interview.
Diastolic pressure readings similarly were "not acceptable" due to wide variation, Dr. Grim said. With a reference diastolic pressure of 88 mm Hg, readings from either the iHealth arm device or the Withings device ranged from 80 to 100 mm Hg. With a reference diastolic pressure of 92 mm Hg, the iHealth wrist device readings ranged from 92 to 110 mm Hg.
No one should rely on a single blood pressure reading whether using a home device or the auscultatory method, Dr. Grim said. He’d prefer that automated devices be set to take three to five readings at a session. Anyone who chooses to use one of the three devices he tested should have a clinician check that the device is accurate on them, but the best way to test this is not clear, he added.
"I still have not found an automatic blood pressure device that is as accurate as auscultatory readings on me," he said.
Dr. Nilay Kumar, a hospitalist for Cambridge (Mass.) Health Alliance, separately reported at the meeting that he searched the popular video-sharing website YouTube using the terms "hypertension" and "high blood pressure." He and his associates analyzed English-language videos from the first 10 pages of search results for each term, comprising 209 videos of the 361,200 possible search results, and designated each video as useful, misleading, or a video of personal experiences.
While most were deemed useful (63%), 33% were misleading, and 4% represented patients’ personal experiences with hypertension (J. Am. Soc. Hypertens. 2014;8:e14-e15).
Cumulatively, the videos had been viewed more than 5.6 million times. Their usefulness did not correlate with the number of views per day, the number of "likes" or "dislikes" indicated by viewers, or comments left on the sites, he said in an e-mail interview. In fact, misleading videos had the highest numbers of views per day. Misleading videos were more likely to include advertisements for products for sale (52%), and 70% of misleading videos contained coverage of alternative treatments, often for products that are not recommended by American Heart Association guidelines.
The source of the video, however, did predict its usefulness. "Patients should trust videos from authoritative sources such as universities, professional organizations, and health information websites," Dr. Kumar said.
Dr. Grim and Dr. Kumar reported having no financial disclosures.
On Twitter @sherryboschert
Separate studies related to hypertension send cautionary messages about smartphone-connected blood pressure cuffs and the quality of videos that patients see online about hypertension.
In one study, readings from three smartphone-connected blood pressure cuffs produced a wide range of measurements in an individual patient, raising questions about the apps’ accuracy even though those brands of devices previously had been validated. A separate survey of videos about hypertension posted on YouTube found lots of misleading information, often in the most popular videos.
Investigators presented the studies at the annual meeting of the American Society of Hypertension in New York.
Dr. Clarence E. Grim, an endocrinologist and former professor of medicine at the Medical College of Wisconsin, Milwaukee, tested three devices that connect to iPhones to enable patients to measure their blood pressure, store the results, and send the readings to others. Quality validation studies have been published for all three using international hypertension protocols, he said, and each passed muster with the Food and Drug Administration.
In multiple sessions over a 3-month period, Dr. Grim took his own blood pressure five times per session after being seated for 5 minutes, using the iHealth BP3 upper arm cuff, the iHealth BP7 wrist cuff, or the Withings upper arm blood pressure monitor. For reference measurements, he used a Tycos TR-2 Home Aneroid with an attached stethoscope for auscultatory measurements, validated against a mercury manometer.
In comparison with a reference systolic pressure of 138 using the auscultatory method, measurements using the iHealth arm device ranged from 127 to 158 mm Hg, with an average error of 8 mm Hg higher than the reference pressure. Measurements using the iHealth wrist device ranged from 123 to 164 mm Hg, with an average error of 13 mm Hg higher than the reference. Measurements using the Withings device ranged from 126 to 159 mm Hg. Although the average pressure with the Withings device did not differ significantly from the reference pressure, when there were errors, they tended to be large, he reported in an interview.
Diastolic pressure readings similarly were "not acceptable" due to wide variation, Dr. Grim said. With a reference diastolic pressure of 88 mm Hg, readings from either the iHealth arm device or the Withings device ranged from 80 to 100 mm Hg. With a reference diastolic pressure of 92 mm Hg, the iHealth wrist device readings ranged from 92 to 110 mm Hg.
No one should rely on a single blood pressure reading whether using a home device or the auscultatory method, Dr. Grim said. He’d prefer that automated devices be set to take three to five readings at a session. Anyone who chooses to use one of the three devices he tested should have a clinician check that the device is accurate on them, but the best way to test this is not clear, he added.
"I still have not found an automatic blood pressure device that is as accurate as auscultatory readings on me," he said.
Dr. Nilay Kumar, a hospitalist for Cambridge (Mass.) Health Alliance, separately reported at the meeting that he searched the popular video-sharing website YouTube using the terms "hypertension" and "high blood pressure." He and his associates analyzed English-language videos from the first 10 pages of search results for each term, comprising 209 videos of the 361,200 possible search results, and designated each video as useful, misleading, or a video of personal experiences.
While most were deemed useful (63%), 33% were misleading, and 4% represented patients’ personal experiences with hypertension (J. Am. Soc. Hypertens. 2014;8:e14-e15).
Cumulatively, the videos had been viewed more than 5.6 million times. Their usefulness did not correlate with the number of views per day, the number of "likes" or "dislikes" indicated by viewers, or comments left on the sites, he said in an e-mail interview. In fact, misleading videos had the highest numbers of views per day. Misleading videos were more likely to include advertisements for products for sale (52%), and 70% of misleading videos contained coverage of alternative treatments, often for products that are not recommended by American Heart Association guidelines.
The source of the video, however, did predict its usefulness. "Patients should trust videos from authoritative sources such as universities, professional organizations, and health information websites," Dr. Kumar said.
Dr. Grim and Dr. Kumar reported having no financial disclosures.
On Twitter @sherryboschert
Don’t push behavior change in diabetes self-care
SAN FRANCISCO – Getting patients to abandon unhealthful behaviors to better control diabetes can be hard, and sometimes the physician is the problem, according to behavioral psychologist William H. Polonsky, Ph.D.
"I think we’re a little too in love with the idea of behavior change," Dr. Polonsky said in the Richard R. Rubin Award lecture at the annual scientific sessions of the American Diabetes Association. "The major thing I’ve learned from my patients is we need to look in the mirror" to figure out why efforts at behavior change aren’t working.
Certainly, healthy behaviors are incredibly helpful. Patients who reported a high level of disease self-management were nearly 40% less likely to die over a 12-year period in a study of 340 patients with type 2 diabetes (Diabetes Care 2014; 37:1604-12). But when behavior change isn’t happening, think about three common mistakes that clinicians make in the process, said Dr. Polonsky, president of the nonprofit Behavioral Diabetes Institute, San Diego:
1. Not taking enough time. Don’t rush patients to change their unhealthful behavior too soon, Dr. Polonsky advised. Make certain your patient believes that the selected behavior change is worthwhile.
"I push my patients way too hard, and I push them when I shouldn’t be pushing them," he said. "It’s this urge we have because we care and probably because we’re overtrained as problem-solvers."
Many clinicians now employ motivational interviewing, for example, which is supposed to end with formulation of concrete, realistic goals for change. However, in reviewing four fairly large randomized, controlled trials published in 2010-2013 that compared motivational interviewing techniques to usual care in managing patients with diabetes, Dr. Polonsky found that the change in hemoglobin A1c (HbA1c) levels differed between groups by an average of only 0.1%. Two other studies found that using motivational interviewing was significantly less effective than diabetes education in changing HbA1c levels.
Perhaps, the emphasis on formulating a concrete goal does not allow enough time to convince a patient that a specific behavior change would be worthwhile, he said.
2. Not focusing on the mundane. Clinicians in recent decades have tended to focus on dramatic factors that may influence behavior in people with diabetes, such as depression, eating disorders, or fear of hypoglycemia. Certainly these conditions should be treated when clinically significant, but these may not be as common as clinicians believe, he said.
Old data suggested that 23%-45% of people with diabetes have depressive symptoms, but newer data suggest that only 5% of people with type 1 diabetes and 4% of those with type 2 diabetes meet the criteria for major depressive disorder, comparable to percentages in the general population, Dr. Polonsky said. Other data suggest that eating disorders may affect 10% of middle-aged adults with type 2 diabetes and 10% of young women with type 1 diabetes. "My hunch is that it’s not as big an issue as we think it is," he said. As many as 26% of people with type 2 diabetes and an unknown proportion of people with type 1 diabetes may fear hypoglycemia, "but I’m not sure we’re talking about big, dramatic fears," he said.
A bigger obstacle may be what Dr. Polonsky called "diabetes meh" – indifference or apathy, when patients just don’t’ really care. This can manifest in statements like, "I have more important things to worry about than diabetes," or "This disease will eventually get me no matter what I do," or "Changing how I eat is too much of a bother."
A related concept is "diabetes distress" – patients’ feelings that diabetes takes up too much mental and physical energy, that the disease controls their lives, and that they often fail with their diabetes regimen. "Should we rename this ‘diabetes fatigue’?" he asked. As many as 39% of patients with type 1 diabetes and 35% of patients with type 2 diabetes may suffer from diabetes distress and its sense of powerlessness, based on research reports.
Try focusing on conveying the "worthwhileness" of interventions, Dr. Polonsky suggested. One way to do that is by "making the invisible visible" by asking patients to check their blood glucose levels right before and right after taking a 45-minute walk each day for just 1 week. The results may surprise them in a motivating way.
3. Not helping patients choose actions that matter. Help patients understand which actions and strategies are more valuable than others. Think of it as looking for "the biggest bang for your buck," he said.
For most patients, that would be knowing their numbers (for glucose and HbA1c), and taking the right medications. Those are more important than, for example, a deprivation strategy like choosing to eat two fewer tortillas per day, he said. Collaborate with patients to select actions that can make a real difference.
Dr. Polonsky reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Getting patients to abandon unhealthful behaviors to better control diabetes can be hard, and sometimes the physician is the problem, according to behavioral psychologist William H. Polonsky, Ph.D.
"I think we’re a little too in love with the idea of behavior change," Dr. Polonsky said in the Richard R. Rubin Award lecture at the annual scientific sessions of the American Diabetes Association. "The major thing I’ve learned from my patients is we need to look in the mirror" to figure out why efforts at behavior change aren’t working.
Certainly, healthy behaviors are incredibly helpful. Patients who reported a high level of disease self-management were nearly 40% less likely to die over a 12-year period in a study of 340 patients with type 2 diabetes (Diabetes Care 2014; 37:1604-12). But when behavior change isn’t happening, think about three common mistakes that clinicians make in the process, said Dr. Polonsky, president of the nonprofit Behavioral Diabetes Institute, San Diego:
1. Not taking enough time. Don’t rush patients to change their unhealthful behavior too soon, Dr. Polonsky advised. Make certain your patient believes that the selected behavior change is worthwhile.
"I push my patients way too hard, and I push them when I shouldn’t be pushing them," he said. "It’s this urge we have because we care and probably because we’re overtrained as problem-solvers."
Many clinicians now employ motivational interviewing, for example, which is supposed to end with formulation of concrete, realistic goals for change. However, in reviewing four fairly large randomized, controlled trials published in 2010-2013 that compared motivational interviewing techniques to usual care in managing patients with diabetes, Dr. Polonsky found that the change in hemoglobin A1c (HbA1c) levels differed between groups by an average of only 0.1%. Two other studies found that using motivational interviewing was significantly less effective than diabetes education in changing HbA1c levels.
Perhaps, the emphasis on formulating a concrete goal does not allow enough time to convince a patient that a specific behavior change would be worthwhile, he said.
2. Not focusing on the mundane. Clinicians in recent decades have tended to focus on dramatic factors that may influence behavior in people with diabetes, such as depression, eating disorders, or fear of hypoglycemia. Certainly these conditions should be treated when clinically significant, but these may not be as common as clinicians believe, he said.
Old data suggested that 23%-45% of people with diabetes have depressive symptoms, but newer data suggest that only 5% of people with type 1 diabetes and 4% of those with type 2 diabetes meet the criteria for major depressive disorder, comparable to percentages in the general population, Dr. Polonsky said. Other data suggest that eating disorders may affect 10% of middle-aged adults with type 2 diabetes and 10% of young women with type 1 diabetes. "My hunch is that it’s not as big an issue as we think it is," he said. As many as 26% of people with type 2 diabetes and an unknown proportion of people with type 1 diabetes may fear hypoglycemia, "but I’m not sure we’re talking about big, dramatic fears," he said.
A bigger obstacle may be what Dr. Polonsky called "diabetes meh" – indifference or apathy, when patients just don’t’ really care. This can manifest in statements like, "I have more important things to worry about than diabetes," or "This disease will eventually get me no matter what I do," or "Changing how I eat is too much of a bother."
A related concept is "diabetes distress" – patients’ feelings that diabetes takes up too much mental and physical energy, that the disease controls their lives, and that they often fail with their diabetes regimen. "Should we rename this ‘diabetes fatigue’?" he asked. As many as 39% of patients with type 1 diabetes and 35% of patients with type 2 diabetes may suffer from diabetes distress and its sense of powerlessness, based on research reports.
Try focusing on conveying the "worthwhileness" of interventions, Dr. Polonsky suggested. One way to do that is by "making the invisible visible" by asking patients to check their blood glucose levels right before and right after taking a 45-minute walk each day for just 1 week. The results may surprise them in a motivating way.
3. Not helping patients choose actions that matter. Help patients understand which actions and strategies are more valuable than others. Think of it as looking for "the biggest bang for your buck," he said.
For most patients, that would be knowing their numbers (for glucose and HbA1c), and taking the right medications. Those are more important than, for example, a deprivation strategy like choosing to eat two fewer tortillas per day, he said. Collaborate with patients to select actions that can make a real difference.
Dr. Polonsky reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Getting patients to abandon unhealthful behaviors to better control diabetes can be hard, and sometimes the physician is the problem, according to behavioral psychologist William H. Polonsky, Ph.D.
"I think we’re a little too in love with the idea of behavior change," Dr. Polonsky said in the Richard R. Rubin Award lecture at the annual scientific sessions of the American Diabetes Association. "The major thing I’ve learned from my patients is we need to look in the mirror" to figure out why efforts at behavior change aren’t working.
Certainly, healthy behaviors are incredibly helpful. Patients who reported a high level of disease self-management were nearly 40% less likely to die over a 12-year period in a study of 340 patients with type 2 diabetes (Diabetes Care 2014; 37:1604-12). But when behavior change isn’t happening, think about three common mistakes that clinicians make in the process, said Dr. Polonsky, president of the nonprofit Behavioral Diabetes Institute, San Diego:
1. Not taking enough time. Don’t rush patients to change their unhealthful behavior too soon, Dr. Polonsky advised. Make certain your patient believes that the selected behavior change is worthwhile.
"I push my patients way too hard, and I push them when I shouldn’t be pushing them," he said. "It’s this urge we have because we care and probably because we’re overtrained as problem-solvers."
Many clinicians now employ motivational interviewing, for example, which is supposed to end with formulation of concrete, realistic goals for change. However, in reviewing four fairly large randomized, controlled trials published in 2010-2013 that compared motivational interviewing techniques to usual care in managing patients with diabetes, Dr. Polonsky found that the change in hemoglobin A1c (HbA1c) levels differed between groups by an average of only 0.1%. Two other studies found that using motivational interviewing was significantly less effective than diabetes education in changing HbA1c levels.
Perhaps, the emphasis on formulating a concrete goal does not allow enough time to convince a patient that a specific behavior change would be worthwhile, he said.
2. Not focusing on the mundane. Clinicians in recent decades have tended to focus on dramatic factors that may influence behavior in people with diabetes, such as depression, eating disorders, or fear of hypoglycemia. Certainly these conditions should be treated when clinically significant, but these may not be as common as clinicians believe, he said.
Old data suggested that 23%-45% of people with diabetes have depressive symptoms, but newer data suggest that only 5% of people with type 1 diabetes and 4% of those with type 2 diabetes meet the criteria for major depressive disorder, comparable to percentages in the general population, Dr. Polonsky said. Other data suggest that eating disorders may affect 10% of middle-aged adults with type 2 diabetes and 10% of young women with type 1 diabetes. "My hunch is that it’s not as big an issue as we think it is," he said. As many as 26% of people with type 2 diabetes and an unknown proportion of people with type 1 diabetes may fear hypoglycemia, "but I’m not sure we’re talking about big, dramatic fears," he said.
A bigger obstacle may be what Dr. Polonsky called "diabetes meh" – indifference or apathy, when patients just don’t’ really care. This can manifest in statements like, "I have more important things to worry about than diabetes," or "This disease will eventually get me no matter what I do," or "Changing how I eat is too much of a bother."
A related concept is "diabetes distress" – patients’ feelings that diabetes takes up too much mental and physical energy, that the disease controls their lives, and that they often fail with their diabetes regimen. "Should we rename this ‘diabetes fatigue’?" he asked. As many as 39% of patients with type 1 diabetes and 35% of patients with type 2 diabetes may suffer from diabetes distress and its sense of powerlessness, based on research reports.
Try focusing on conveying the "worthwhileness" of interventions, Dr. Polonsky suggested. One way to do that is by "making the invisible visible" by asking patients to check their blood glucose levels right before and right after taking a 45-minute walk each day for just 1 week. The results may surprise them in a motivating way.
3. Not helping patients choose actions that matter. Help patients understand which actions and strategies are more valuable than others. Think of it as looking for "the biggest bang for your buck," he said.
For most patients, that would be knowing their numbers (for glucose and HbA1c), and taking the right medications. Those are more important than, for example, a deprivation strategy like choosing to eat two fewer tortillas per day, he said. Collaborate with patients to select actions that can make a real difference.
Dr. Polonsky reported having no relevant financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM THE ADA ANNUAL SCIENTIFIC SESSIONS
Hypoglycemia common after bariatric surgery
SAN FRANCISCO – Hypoglycemic episodes were common and largely unnoticed after bariatric surgery, a controlled study of 45 patients found.
During a 3-day period of "normal living," symptomatic hypoglycemias occurred in 22% of 15 patients after gastric bypass surgery, 20% of 15 patients after biliopancreatic diversion with duodenal switch, and in none of 15 obese, nondiabetic control patients matched to the surgical patients by body mass index.
Continuous glucose monitoring showed that patients in both postsurgery groups spent significant amounts of time in hypoglycemia, Dr. Niclas Abrahamsson and his associates reported at the annual scientific session of the American Diabetes Association.
After gastric bypass, patients averaged 42 minutes per day with glucose levels lower than 3.3 mmol/L and 21 minutes per day with levels lower than 2.8 mmol/L. After duodenal switch surgery, patients averaged 85 minutes per day with glucose levels lower than 3.3 mmol/L and 39 minutes per day with levels lower than 2.8 mmol/L. No patients in the control group had glucose levels that low, reported Dr. Abrahamsson of the University of Uppsala, Sweden.
"We were very surprised that they had so many hypoglycemic episodes, especially since the controls had none," he said. Patients were unaware of approximately 80% of the hypoglycemic episodes, he added.
"The clinical significance should be that one should be alert to any hypoglycemia symptoms," Dr. Abrahamsson said.
Patients in the post–duodenal switch group had the lowest mean glucose level (4.6 mmol/L) and mean hemoglobin A1c level (29 mmol/mol), compared with the post–gastric bypass group (mean glucose 5.3 mmol/L and HbA1c 36 mmol/mol) and the control group (mean glucose 5.9 mmol/L and HbA1c 38 mmol/mol).
Glucose curves on continuous monitoring were more variable in the post–gastric bypass group, compared with controls, and less variable in the post–duodenal switch group, compared with controls. That difference between the two surgical groups probably relates to the different glucose absorption capabilities after surgery, he suggested.
Dr. Abrahamsson has been a speaker for Eli Lilly and Sanofi and has held stock in AstraZeneca.
On Twitter @sherryboschert
The finding that patients with recent duodenal switch surgery spent 85 minutes per day with hypoglycemia, compared with 42 minutes per 24 hours for patients in the gastric bypass group, is quite alarming. Although these hypoglycemias were largely unnoticed, we know that hypoglycemia can affect brain function, cognition, and motor function.
 |
|
The problem with continuous glucose monitoring is that it’s a research tool, but it’s not very practical to be doing in every single patient who’s had a gastric bypass surgery. The problem with doing blood glucose measurement is that it’s a snapshot and you can potentially miss hypoglycemia. So, this has a lot of clinical implications as to how we investigate such patients.
This study has safety and legal implications for things like driving and operating machinery and raises questions of how we can best manage patients in terms of mitigating the effects of hypoglycemia. I think it opens up a whole area of questions at which we need to look.
I think this study will change my practice. It has opened my eyes. I was quite shocked at the data. At my center, we don’t tend to do many duodenal switches. We do many more sleeve gastrectomies than the bypass procedures. But, certainly, following a bypass procedure, I will be much more cognizant of the potential for hypoglycemia and caution our patients regarding driving and about monitoring their sugars closely following the procedure.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the University of Warwick, England. These comments are excerpted from an interview at the meeting. Dr. Barber reported having no financial disclosures.
The finding that patients with recent duodenal switch surgery spent 85 minutes per day with hypoglycemia, compared with 42 minutes per 24 hours for patients in the gastric bypass group, is quite alarming. Although these hypoglycemias were largely unnoticed, we know that hypoglycemia can affect brain function, cognition, and motor function.
 |
|
The problem with continuous glucose monitoring is that it’s a research tool, but it’s not very practical to be doing in every single patient who’s had a gastric bypass surgery. The problem with doing blood glucose measurement is that it’s a snapshot and you can potentially miss hypoglycemia. So, this has a lot of clinical implications as to how we investigate such patients.
This study has safety and legal implications for things like driving and operating machinery and raises questions of how we can best manage patients in terms of mitigating the effects of hypoglycemia. I think it opens up a whole area of questions at which we need to look.
I think this study will change my practice. It has opened my eyes. I was quite shocked at the data. At my center, we don’t tend to do many duodenal switches. We do many more sleeve gastrectomies than the bypass procedures. But, certainly, following a bypass procedure, I will be much more cognizant of the potential for hypoglycemia and caution our patients regarding driving and about monitoring their sugars closely following the procedure.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the University of Warwick, England. These comments are excerpted from an interview at the meeting. Dr. Barber reported having no financial disclosures.
The finding that patients with recent duodenal switch surgery spent 85 minutes per day with hypoglycemia, compared with 42 minutes per 24 hours for patients in the gastric bypass group, is quite alarming. Although these hypoglycemias were largely unnoticed, we know that hypoglycemia can affect brain function, cognition, and motor function.
 |
|
The problem with continuous glucose monitoring is that it’s a research tool, but it’s not very practical to be doing in every single patient who’s had a gastric bypass surgery. The problem with doing blood glucose measurement is that it’s a snapshot and you can potentially miss hypoglycemia. So, this has a lot of clinical implications as to how we investigate such patients.
This study has safety and legal implications for things like driving and operating machinery and raises questions of how we can best manage patients in terms of mitigating the effects of hypoglycemia. I think it opens up a whole area of questions at which we need to look.
I think this study will change my practice. It has opened my eyes. I was quite shocked at the data. At my center, we don’t tend to do many duodenal switches. We do many more sleeve gastrectomies than the bypass procedures. But, certainly, following a bypass procedure, I will be much more cognizant of the potential for hypoglycemia and caution our patients regarding driving and about monitoring their sugars closely following the procedure.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the University of Warwick, England. These comments are excerpted from an interview at the meeting. Dr. Barber reported having no financial disclosures.
SAN FRANCISCO – Hypoglycemic episodes were common and largely unnoticed after bariatric surgery, a controlled study of 45 patients found.
During a 3-day period of "normal living," symptomatic hypoglycemias occurred in 22% of 15 patients after gastric bypass surgery, 20% of 15 patients after biliopancreatic diversion with duodenal switch, and in none of 15 obese, nondiabetic control patients matched to the surgical patients by body mass index.
Continuous glucose monitoring showed that patients in both postsurgery groups spent significant amounts of time in hypoglycemia, Dr. Niclas Abrahamsson and his associates reported at the annual scientific session of the American Diabetes Association.
After gastric bypass, patients averaged 42 minutes per day with glucose levels lower than 3.3 mmol/L and 21 minutes per day with levels lower than 2.8 mmol/L. After duodenal switch surgery, patients averaged 85 minutes per day with glucose levels lower than 3.3 mmol/L and 39 minutes per day with levels lower than 2.8 mmol/L. No patients in the control group had glucose levels that low, reported Dr. Abrahamsson of the University of Uppsala, Sweden.
"We were very surprised that they had so many hypoglycemic episodes, especially since the controls had none," he said. Patients were unaware of approximately 80% of the hypoglycemic episodes, he added.
"The clinical significance should be that one should be alert to any hypoglycemia symptoms," Dr. Abrahamsson said.
Patients in the post–duodenal switch group had the lowest mean glucose level (4.6 mmol/L) and mean hemoglobin A1c level (29 mmol/mol), compared with the post–gastric bypass group (mean glucose 5.3 mmol/L and HbA1c 36 mmol/mol) and the control group (mean glucose 5.9 mmol/L and HbA1c 38 mmol/mol).
Glucose curves on continuous monitoring were more variable in the post–gastric bypass group, compared with controls, and less variable in the post–duodenal switch group, compared with controls. That difference between the two surgical groups probably relates to the different glucose absorption capabilities after surgery, he suggested.
Dr. Abrahamsson has been a speaker for Eli Lilly and Sanofi and has held stock in AstraZeneca.
On Twitter @sherryboschert
SAN FRANCISCO – Hypoglycemic episodes were common and largely unnoticed after bariatric surgery, a controlled study of 45 patients found.
During a 3-day period of "normal living," symptomatic hypoglycemias occurred in 22% of 15 patients after gastric bypass surgery, 20% of 15 patients after biliopancreatic diversion with duodenal switch, and in none of 15 obese, nondiabetic control patients matched to the surgical patients by body mass index.
Continuous glucose monitoring showed that patients in both postsurgery groups spent significant amounts of time in hypoglycemia, Dr. Niclas Abrahamsson and his associates reported at the annual scientific session of the American Diabetes Association.
After gastric bypass, patients averaged 42 minutes per day with glucose levels lower than 3.3 mmol/L and 21 minutes per day with levels lower than 2.8 mmol/L. After duodenal switch surgery, patients averaged 85 minutes per day with glucose levels lower than 3.3 mmol/L and 39 minutes per day with levels lower than 2.8 mmol/L. No patients in the control group had glucose levels that low, reported Dr. Abrahamsson of the University of Uppsala, Sweden.
"We were very surprised that they had so many hypoglycemic episodes, especially since the controls had none," he said. Patients were unaware of approximately 80% of the hypoglycemic episodes, he added.
"The clinical significance should be that one should be alert to any hypoglycemia symptoms," Dr. Abrahamsson said.
Patients in the post–duodenal switch group had the lowest mean glucose level (4.6 mmol/L) and mean hemoglobin A1c level (29 mmol/mol), compared with the post–gastric bypass group (mean glucose 5.3 mmol/L and HbA1c 36 mmol/mol) and the control group (mean glucose 5.9 mmol/L and HbA1c 38 mmol/mol).
Glucose curves on continuous monitoring were more variable in the post–gastric bypass group, compared with controls, and less variable in the post–duodenal switch group, compared with controls. That difference between the two surgical groups probably relates to the different glucose absorption capabilities after surgery, he suggested.
Dr. Abrahamsson has been a speaker for Eli Lilly and Sanofi and has held stock in AstraZeneca.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSION
Key clinical point: Be alert for frequent hypoglycemia after bariatric surgery.
Major finding: Patients averaged 42 minutes/day in hypoglycemia after gastric bypass surgery or 85 minutes/day after biliopancreatic diversion with duodenal switch, compared with no hypoglycemia in controls.
Data source: A prospective study of continuous glucose monitoring during 3 days of normal living in 15 patients after gastric bypass, 15 patients after duodenal switch surgery, and 15 matched obese control patients.
Disclosures: Dr. Abrahamsson has been a speaker for Eli Lilly and Sanofi and has held stock in AstraZeneca.
Fractures increased with two diabetes drugs
SAN FRANCISCO – Adults who started taking sulfonylurea drugs for diabetes were 9% more likely to develop fractures within 5 years, and patients starting thiazolidinediones were 9% more likely to have fractures, compared with patients on other medications in a retrospective study of 99,892 adults.
Those significantly increased risks emerged after adjusting for the effects of multiple factors including age, gender, region, medical conditions, and concomitant medications, Sandhya Mehta, Ph.D. and her associates reported at the annual scientific sessions of the American Diabetes Association. Patients had no prior history of fracture.
The longitudinal retrospective analysis of a large administrative claims database found a 10% incidence of fracture on sulfonylureas and 11% on thiazolidinediones, compared with 7% on biguanides (metformin), 8% on dipeptidyl peptidase-4 (DPP-4) inhibitors, 11% on meglitinide analogues, and 6% on incretin mimetic agents. After adjusting for the confounders, the hazard ratios for each of the other three types of drugs hovered around 1 and were not statistically significantly different but increased to 1.09 for sulfonylureas and 1.4 for thiazolidinediones, reported Dr. Mehta of Inovalon Inc. in Bowie, Md., a health care data analytics company.
In the cohort as a whole, 7% of patients developed fractures. Roughly 15% of patients started sulfonylureas, 3% took thiazolidinediones, 78% were on metformin, 3% took DPP-4 inhibitors, 1% were on incretin mimetics, and 1% took meglitinides.
Previous reports have shown an increased risk of fracture in patients on thiazolidinediones, compared with those on metformin, and the current results support the hypothesis that thiazolidinediones decrease bone mineral density, stimulate adipocyte and osteoclast differentiation, and inhibit osteoblast differentiation to make fracture more likely, Dr. Mehta said.
The association between sulfonylureas and increased fracture risk appears to be new, however, and deserves further study, she added.
The study did not look at the effects of combination drug therapy.
Data came from the Medical Outcomes Research for Effectiveness and Economics (MORE) Registry, which is owned by Inovalon, drawing from the years 2008-2012.
Dr. Mehta reported having no financial disclosures.
On Twitter @sherryboschert
This study confirms that we observe more fracture risks with thiazolidinediones. To my knowledge, this is the first time that this has been shown for sulfonylureas.
 |
|
One concern about the study is so-called residual confounding. The confounders were not entirely clear in the presentation. One possible confounder is what might have preceded the fracture. If, in fact, patients on sulfonylureas were having more low blood glucose values and consequently fell, then that would be interesting to know. Unfortunately, the investigators couldn’t tell us that.
With thiazolidinediones, I’ve been told that a cell that hasn’t decided yet whether it’s going to be a bone cell or a fat cell might, in the presence of a thiazolidinedione, go on to be a fat cell instead of a bone cell. In which case, you would possibly have a problem with fewer bone cells. This study set out to look at bone metabolism but, to be fair, it could not show anything about that. That was rather ambitious.
I think there is no clinical message from this as yet. The investigators might want to look back at trials that randomized people to sulfonylureas or something else and meta-analyze that to see if there were differences in fractures.
The study suggests that the other second-line agents are okay, but again, we can’t really know what they’re doing to bones without knowing if there’s something else going on. If you took a drug that made you more likely to topple over, your bones could be equally strong as those who didn’t fall over, yet you end up with a fracture.
I’m not going to change my practice on the basis of this study.
Dr. Amanda Adler is consultant physician at Cambridge University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence in England. She gave these comments in an interview at the meeting.
This study confirms that we observe more fracture risks with thiazolidinediones. To my knowledge, this is the first time that this has been shown for sulfonylureas.
 |
|
One concern about the study is so-called residual confounding. The confounders were not entirely clear in the presentation. One possible confounder is what might have preceded the fracture. If, in fact, patients on sulfonylureas were having more low blood glucose values and consequently fell, then that would be interesting to know. Unfortunately, the investigators couldn’t tell us that.
With thiazolidinediones, I’ve been told that a cell that hasn’t decided yet whether it’s going to be a bone cell or a fat cell might, in the presence of a thiazolidinedione, go on to be a fat cell instead of a bone cell. In which case, you would possibly have a problem with fewer bone cells. This study set out to look at bone metabolism but, to be fair, it could not show anything about that. That was rather ambitious.
I think there is no clinical message from this as yet. The investigators might want to look back at trials that randomized people to sulfonylureas or something else and meta-analyze that to see if there were differences in fractures.
The study suggests that the other second-line agents are okay, but again, we can’t really know what they’re doing to bones without knowing if there’s something else going on. If you took a drug that made you more likely to topple over, your bones could be equally strong as those who didn’t fall over, yet you end up with a fracture.
I’m not going to change my practice on the basis of this study.
Dr. Amanda Adler is consultant physician at Cambridge University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence in England. She gave these comments in an interview at the meeting.
This study confirms that we observe more fracture risks with thiazolidinediones. To my knowledge, this is the first time that this has been shown for sulfonylureas.
 |
|
One concern about the study is so-called residual confounding. The confounders were not entirely clear in the presentation. One possible confounder is what might have preceded the fracture. If, in fact, patients on sulfonylureas were having more low blood glucose values and consequently fell, then that would be interesting to know. Unfortunately, the investigators couldn’t tell us that.
With thiazolidinediones, I’ve been told that a cell that hasn’t decided yet whether it’s going to be a bone cell or a fat cell might, in the presence of a thiazolidinedione, go on to be a fat cell instead of a bone cell. In which case, you would possibly have a problem with fewer bone cells. This study set out to look at bone metabolism but, to be fair, it could not show anything about that. That was rather ambitious.
I think there is no clinical message from this as yet. The investigators might want to look back at trials that randomized people to sulfonylureas or something else and meta-analyze that to see if there were differences in fractures.
The study suggests that the other second-line agents are okay, but again, we can’t really know what they’re doing to bones without knowing if there’s something else going on. If you took a drug that made you more likely to topple over, your bones could be equally strong as those who didn’t fall over, yet you end up with a fracture.
I’m not going to change my practice on the basis of this study.
Dr. Amanda Adler is consultant physician at Cambridge University’s Addenbrooke’s Hospital and chair of the technology appraisals committee for the National Institute for Health and Clinical Excellence in England. She gave these comments in an interview at the meeting.
SAN FRANCISCO – Adults who started taking sulfonylurea drugs for diabetes were 9% more likely to develop fractures within 5 years, and patients starting thiazolidinediones were 9% more likely to have fractures, compared with patients on other medications in a retrospective study of 99,892 adults.
Those significantly increased risks emerged after adjusting for the effects of multiple factors including age, gender, region, medical conditions, and concomitant medications, Sandhya Mehta, Ph.D. and her associates reported at the annual scientific sessions of the American Diabetes Association. Patients had no prior history of fracture.
The longitudinal retrospective analysis of a large administrative claims database found a 10% incidence of fracture on sulfonylureas and 11% on thiazolidinediones, compared with 7% on biguanides (metformin), 8% on dipeptidyl peptidase-4 (DPP-4) inhibitors, 11% on meglitinide analogues, and 6% on incretin mimetic agents. After adjusting for the confounders, the hazard ratios for each of the other three types of drugs hovered around 1 and were not statistically significantly different but increased to 1.09 for sulfonylureas and 1.4 for thiazolidinediones, reported Dr. Mehta of Inovalon Inc. in Bowie, Md., a health care data analytics company.
In the cohort as a whole, 7% of patients developed fractures. Roughly 15% of patients started sulfonylureas, 3% took thiazolidinediones, 78% were on metformin, 3% took DPP-4 inhibitors, 1% were on incretin mimetics, and 1% took meglitinides.
Previous reports have shown an increased risk of fracture in patients on thiazolidinediones, compared with those on metformin, and the current results support the hypothesis that thiazolidinediones decrease bone mineral density, stimulate adipocyte and osteoclast differentiation, and inhibit osteoblast differentiation to make fracture more likely, Dr. Mehta said.
The association between sulfonylureas and increased fracture risk appears to be new, however, and deserves further study, she added.
The study did not look at the effects of combination drug therapy.
Data came from the Medical Outcomes Research for Effectiveness and Economics (MORE) Registry, which is owned by Inovalon, drawing from the years 2008-2012.
Dr. Mehta reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Adults who started taking sulfonylurea drugs for diabetes were 9% more likely to develop fractures within 5 years, and patients starting thiazolidinediones were 9% more likely to have fractures, compared with patients on other medications in a retrospective study of 99,892 adults.
Those significantly increased risks emerged after adjusting for the effects of multiple factors including age, gender, region, medical conditions, and concomitant medications, Sandhya Mehta, Ph.D. and her associates reported at the annual scientific sessions of the American Diabetes Association. Patients had no prior history of fracture.
The longitudinal retrospective analysis of a large administrative claims database found a 10% incidence of fracture on sulfonylureas and 11% on thiazolidinediones, compared with 7% on biguanides (metformin), 8% on dipeptidyl peptidase-4 (DPP-4) inhibitors, 11% on meglitinide analogues, and 6% on incretin mimetic agents. After adjusting for the confounders, the hazard ratios for each of the other three types of drugs hovered around 1 and were not statistically significantly different but increased to 1.09 for sulfonylureas and 1.4 for thiazolidinediones, reported Dr. Mehta of Inovalon Inc. in Bowie, Md., a health care data analytics company.
In the cohort as a whole, 7% of patients developed fractures. Roughly 15% of patients started sulfonylureas, 3% took thiazolidinediones, 78% were on metformin, 3% took DPP-4 inhibitors, 1% were on incretin mimetics, and 1% took meglitinides.
Previous reports have shown an increased risk of fracture in patients on thiazolidinediones, compared with those on metformin, and the current results support the hypothesis that thiazolidinediones decrease bone mineral density, stimulate adipocyte and osteoclast differentiation, and inhibit osteoblast differentiation to make fracture more likely, Dr. Mehta said.
The association between sulfonylureas and increased fracture risk appears to be new, however, and deserves further study, she added.
The study did not look at the effects of combination drug therapy.
Data came from the Medical Outcomes Research for Effectiveness and Economics (MORE) Registry, which is owned by Inovalon, drawing from the years 2008-2012.
Dr. Mehta reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Consider possible increased fracture risks with thiazolidinediones and sulfonylureas when choosing diabetes drug therapy.
Major finding: The 5-year fracture risk was 9% higher with sulfonylureas and 40% higher with thiazolidinediones, compared with other diabetes medications.
Data source: Retrospective analysis of data on 98,892 adults with no history of fracture who started a diabetes medication.
Disclosures: Dr. Mehta reported having no financial disclosures.
Monoclonal antibody attacks new asthma target
SAN DIEGO – An investigational human monoclonal antibody suggested a new approach to asthma treatment by showing evidence of anti-inflammatory activity and partial attenuation of early and late asthmatic responses in a proof-of-concept study of 31 patients with mild asthma.
Patients were randomized to intravenous treatment with AMG 157 or placebo for up to 3 months before undergoing allergen-induced challenge and testing. AMG 157 binds human thymic stromal lymphopoietin (TSLP), an epithelial cell–derived cytokine that might be important in initiating allergic inflammation, and prevents receptor interaction.
By day 84, the maximum percentage decrease in the forced expiratory volume at 1 second (FEV1) during late asthmatic response (3-7 hours after allergy challenge) was 46% smaller in the treatment group, vs. placebo, a significant difference, Gail M. Gauvreau, Ph.D., and her associates reported at an international conference of the American Thoracic Society.
Among secondary outcomes, the area under the curve (AUC) of the time-adjusted percent decrease in FEV1 during the early asthmatic response was significantly smaller in the treatment group than the control group on day 84. Patients who got AMG 157 showed significantly lower levels of blood and sputum eosinophils before and after allergy challenge and in the fraction of exhaled nitric oxide.
Adverse events were reported in 15 patients on AMG 157 and 12 patients on placebo. No serious adverse events were seen, reported Dr. Gauvreau of the Firestone Institute of Respiratory Health at McMaster University, Hamilton, Ont.
The study was published online by the New England Journal of Medicine (2014 May 20 [doi: 10.1056/NEJMoa1402895]). "This proof-of-concept study suggests that TSLP is a pivotal cytokine not only in allergen-induced airway responses but also in persistent airway inflammation in patients with allergic asthma," the investigators wrote.
The company that is developing AMG 157 has started a phase II clinical trial, Dr. Gauvreau said in an interview at the meeting.
The population of mild asthmatics in the proof-of-concept study is not the kind of patient who might use this treatment, she said, but this potential treatment pathway offers hope for a new therapy for patients with steroid-resistant asthma.
Amgen, which is developing AMG 157, funded the study and analyzed the data. Many of the researchers reported financial associations with Amgen and other companies.
On Twitter @sherryboschert
 |
|
Dr. Eric Gartman, FCCP, comments: For our most difficult-to-control asthma patients, we are longing for an effective and more directed alternative to systemic corticosteroids. While this agent has yet to be studied in the appropriate population, any advancement in the science of developing therapies against novel targets in asthma is a needed step in the right direction.
 |
|
Dr. Eric Gartman, FCCP, comments: For our most difficult-to-control asthma patients, we are longing for an effective and more directed alternative to systemic corticosteroids. While this agent has yet to be studied in the appropriate population, any advancement in the science of developing therapies against novel targets in asthma is a needed step in the right direction.
 |
|
Dr. Eric Gartman, FCCP, comments: For our most difficult-to-control asthma patients, we are longing for an effective and more directed alternative to systemic corticosteroids. While this agent has yet to be studied in the appropriate population, any advancement in the science of developing therapies against novel targets in asthma is a needed step in the right direction.
SAN DIEGO – An investigational human monoclonal antibody suggested a new approach to asthma treatment by showing evidence of anti-inflammatory activity and partial attenuation of early and late asthmatic responses in a proof-of-concept study of 31 patients with mild asthma.
Patients were randomized to intravenous treatment with AMG 157 or placebo for up to 3 months before undergoing allergen-induced challenge and testing. AMG 157 binds human thymic stromal lymphopoietin (TSLP), an epithelial cell–derived cytokine that might be important in initiating allergic inflammation, and prevents receptor interaction.
By day 84, the maximum percentage decrease in the forced expiratory volume at 1 second (FEV1) during late asthmatic response (3-7 hours after allergy challenge) was 46% smaller in the treatment group, vs. placebo, a significant difference, Gail M. Gauvreau, Ph.D., and her associates reported at an international conference of the American Thoracic Society.
Among secondary outcomes, the area under the curve (AUC) of the time-adjusted percent decrease in FEV1 during the early asthmatic response was significantly smaller in the treatment group than the control group on day 84. Patients who got AMG 157 showed significantly lower levels of blood and sputum eosinophils before and after allergy challenge and in the fraction of exhaled nitric oxide.
Adverse events were reported in 15 patients on AMG 157 and 12 patients on placebo. No serious adverse events were seen, reported Dr. Gauvreau of the Firestone Institute of Respiratory Health at McMaster University, Hamilton, Ont.
The study was published online by the New England Journal of Medicine (2014 May 20 [doi: 10.1056/NEJMoa1402895]). "This proof-of-concept study suggests that TSLP is a pivotal cytokine not only in allergen-induced airway responses but also in persistent airway inflammation in patients with allergic asthma," the investigators wrote.
The company that is developing AMG 157 has started a phase II clinical trial, Dr. Gauvreau said in an interview at the meeting.
The population of mild asthmatics in the proof-of-concept study is not the kind of patient who might use this treatment, she said, but this potential treatment pathway offers hope for a new therapy for patients with steroid-resistant asthma.
Amgen, which is developing AMG 157, funded the study and analyzed the data. Many of the researchers reported financial associations with Amgen and other companies.
On Twitter @sherryboschert
SAN DIEGO – An investigational human monoclonal antibody suggested a new approach to asthma treatment by showing evidence of anti-inflammatory activity and partial attenuation of early and late asthmatic responses in a proof-of-concept study of 31 patients with mild asthma.
Patients were randomized to intravenous treatment with AMG 157 or placebo for up to 3 months before undergoing allergen-induced challenge and testing. AMG 157 binds human thymic stromal lymphopoietin (TSLP), an epithelial cell–derived cytokine that might be important in initiating allergic inflammation, and prevents receptor interaction.
By day 84, the maximum percentage decrease in the forced expiratory volume at 1 second (FEV1) during late asthmatic response (3-7 hours after allergy challenge) was 46% smaller in the treatment group, vs. placebo, a significant difference, Gail M. Gauvreau, Ph.D., and her associates reported at an international conference of the American Thoracic Society.
Among secondary outcomes, the area under the curve (AUC) of the time-adjusted percent decrease in FEV1 during the early asthmatic response was significantly smaller in the treatment group than the control group on day 84. Patients who got AMG 157 showed significantly lower levels of blood and sputum eosinophils before and after allergy challenge and in the fraction of exhaled nitric oxide.
Adverse events were reported in 15 patients on AMG 157 and 12 patients on placebo. No serious adverse events were seen, reported Dr. Gauvreau of the Firestone Institute of Respiratory Health at McMaster University, Hamilton, Ont.
The study was published online by the New England Journal of Medicine (2014 May 20 [doi: 10.1056/NEJMoa1402895]). "This proof-of-concept study suggests that TSLP is a pivotal cytokine not only in allergen-induced airway responses but also in persistent airway inflammation in patients with allergic asthma," the investigators wrote.
The company that is developing AMG 157 has started a phase II clinical trial, Dr. Gauvreau said in an interview at the meeting.
The population of mild asthmatics in the proof-of-concept study is not the kind of patient who might use this treatment, she said, but this potential treatment pathway offers hope for a new therapy for patients with steroid-resistant asthma.
Amgen, which is developing AMG 157, funded the study and analyzed the data. Many of the researchers reported financial associations with Amgen and other companies.
On Twitter @sherryboschert
Key clinical point: A proof-of-concept study suggests that there may be a new asthma treatment pathway, to be tested next in a phase II clinical trial.
Major finding: The maximum percentage decrease in the FEV1 3-7 hours after allergy challenge was 46% smaller in the treatment group, compared with placebo on day 84 (P = .02)
Data source: A double-blind, placebo-controlled study of 31 patients with mild asthma treated with 3 months of intravenous AMG 157 or placebo assessed after allergen challenge.
Disclosures: Amgen, which is developing AMG 157, funded the study and analyzed the data. Dr. Gauvreau reported financial associations with Amgen and three other companies. Fourteen of her coinvestigators reported financial associations with Amgen and multiple other companies.
Diabetes Outcomes Similar With Physicians, Advanced Practice Providers
SAN FRANCISCO – Physicians and advanced practice health care providers saw comparable types of patients with diabetes in the Veterans Affairs health care system and helped patients achieve comparable changes in hemoglobin A1C levels, a study of 19,238 health care providers found.
"At the time of diagnosis of diabetes and during 4 years of follow-up care, nurse practitioners and physician assistants have patient populations that are comparable to those of physicians, and their diabetes management is as good as that provided by physicians," Dr. Lawrence S. Phillips said at the annual scientific sessions of the American Diabetes Association.
Diabetes affects more than 20% of patients in the VA system, which is the largest employer of nurse practitioners and physician assistants in the country, he said. Dr. Phillips and his associates analyzed VA data to identify patients who saw a physician, nurse practitioner, or physician assistant for more than 50% of health care visits since a new diagnosis of diabetes in 2008-2012.
Average A1C levels at the time of diabetes diagnosis, at the initiation of medications, and during follow-up years did not differ significantly between provider groups after patient characteristics were adjusted for, reported Dr. Phillips, professor of medicine at Emory University, Atlanta. Baseline A1C levels were 7.18%, 7.14%, and 7.20% with nurse practitioners, physician assistants, and physicians, respectively, and dropped to 6.75%, 6.75%, and 6.78% by 2012.
Patient demographics were similar between provider groups. Their mean age was roughly 69 years, about 95% were male, and their mean body mass index was about 32.4 kg/m2. The cohort seen by physicians had a smaller percentage of white patients (77%) than did the cohort seen by physician assistants (81%).
Patient comorbidity levels, as measured by the Charlson Comorbidity Index, were the same in each provider group (a score of 1 in each group). The proportion of patients on any diabetes therapy was similar between groups: 81% with physicians, 80% with nurse practitioners, and 79% with physician assistants.
A significantly smaller proportion of patients seeing physician assistants were on insulin (12%), compared with those seeing physicians (15%) or nurse practitioners (14%), Dr. Phillips reported. Physician assistants also referred a significantly smaller proportion of patients to diabetes specialists (5%), compared with physicians (8%) or nurse practitioners (7%).
The findings surprised the investigators and suggested that the VA model of using advanced practice providers might be broadly useful to help the U.S. meet demand for primary care providers, he said.
Dr. Phillips reported having financial associations with multiple pharmaceutical companies but none related to this study.
On Twitter @sherryboschert
This study defined provider type by whether a physician or midlevel practitioner saw the patient in 50% or more of the patient’s visits. But it could be that the VA system has appropriate and selective use of MD specialists, who guide the initiation of insulin and escalation of therapy, and then, appropriately, the midlevel providers deliver more education-related or lifestyle-related care. I think a little bit more understanding of who is doing what, not just where the majority of care is being conducted, is needed to fully understand this.
 |
|
We don’t live in a world where specialists can be delivering all of diabetes care. The numbers don’t add up. Where we need to go is figuring out how we can effectively use each of our provider types.
I would lean more toward this study being a first step in understanding. Are we talking about replacing or complementing physicians? Before we see more data, I would think that we still are in a complementing world, but we need to refine that.
Dr. Sanjeev N. Mehta of the Joslin Diabetes Center, Boston, gave these comments in an interview at the meeting. He reported having no financial disclosures.
This study defined provider type by whether a physician or midlevel practitioner saw the patient in 50% or more of the patient’s visits. But it could be that the VA system has appropriate and selective use of MD specialists, who guide the initiation of insulin and escalation of therapy, and then, appropriately, the midlevel providers deliver more education-related or lifestyle-related care. I think a little bit more understanding of who is doing what, not just where the majority of care is being conducted, is needed to fully understand this.
 |
|
We don’t live in a world where specialists can be delivering all of diabetes care. The numbers don’t add up. Where we need to go is figuring out how we can effectively use each of our provider types.
I would lean more toward this study being a first step in understanding. Are we talking about replacing or complementing physicians? Before we see more data, I would think that we still are in a complementing world, but we need to refine that.
Dr. Sanjeev N. Mehta of the Joslin Diabetes Center, Boston, gave these comments in an interview at the meeting. He reported having no financial disclosures.
This study defined provider type by whether a physician or midlevel practitioner saw the patient in 50% or more of the patient’s visits. But it could be that the VA system has appropriate and selective use of MD specialists, who guide the initiation of insulin and escalation of therapy, and then, appropriately, the midlevel providers deliver more education-related or lifestyle-related care. I think a little bit more understanding of who is doing what, not just where the majority of care is being conducted, is needed to fully understand this.
 |
|
We don’t live in a world where specialists can be delivering all of diabetes care. The numbers don’t add up. Where we need to go is figuring out how we can effectively use each of our provider types.
I would lean more toward this study being a first step in understanding. Are we talking about replacing or complementing physicians? Before we see more data, I would think that we still are in a complementing world, but we need to refine that.
Dr. Sanjeev N. Mehta of the Joslin Diabetes Center, Boston, gave these comments in an interview at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Physicians and advanced practice health care providers saw comparable types of patients with diabetes in the Veterans Affairs health care system and helped patients achieve comparable changes in hemoglobin A1C levels, a study of 19,238 health care providers found.
"At the time of diagnosis of diabetes and during 4 years of follow-up care, nurse practitioners and physician assistants have patient populations that are comparable to those of physicians, and their diabetes management is as good as that provided by physicians," Dr. Lawrence S. Phillips said at the annual scientific sessions of the American Diabetes Association.
Diabetes affects more than 20% of patients in the VA system, which is the largest employer of nurse practitioners and physician assistants in the country, he said. Dr. Phillips and his associates analyzed VA data to identify patients who saw a physician, nurse practitioner, or physician assistant for more than 50% of health care visits since a new diagnosis of diabetes in 2008-2012.
Average A1C levels at the time of diabetes diagnosis, at the initiation of medications, and during follow-up years did not differ significantly between provider groups after patient characteristics were adjusted for, reported Dr. Phillips, professor of medicine at Emory University, Atlanta. Baseline A1C levels were 7.18%, 7.14%, and 7.20% with nurse practitioners, physician assistants, and physicians, respectively, and dropped to 6.75%, 6.75%, and 6.78% by 2012.
Patient demographics were similar between provider groups. Their mean age was roughly 69 years, about 95% were male, and their mean body mass index was about 32.4 kg/m2. The cohort seen by physicians had a smaller percentage of white patients (77%) than did the cohort seen by physician assistants (81%).
Patient comorbidity levels, as measured by the Charlson Comorbidity Index, were the same in each provider group (a score of 1 in each group). The proportion of patients on any diabetes therapy was similar between groups: 81% with physicians, 80% with nurse practitioners, and 79% with physician assistants.
A significantly smaller proportion of patients seeing physician assistants were on insulin (12%), compared with those seeing physicians (15%) or nurse practitioners (14%), Dr. Phillips reported. Physician assistants also referred a significantly smaller proportion of patients to diabetes specialists (5%), compared with physicians (8%) or nurse practitioners (7%).
The findings surprised the investigators and suggested that the VA model of using advanced practice providers might be broadly useful to help the U.S. meet demand for primary care providers, he said.
Dr. Phillips reported having financial associations with multiple pharmaceutical companies but none related to this study.
On Twitter @sherryboschert
SAN FRANCISCO – Physicians and advanced practice health care providers saw comparable types of patients with diabetes in the Veterans Affairs health care system and helped patients achieve comparable changes in hemoglobin A1C levels, a study of 19,238 health care providers found.
"At the time of diagnosis of diabetes and during 4 years of follow-up care, nurse practitioners and physician assistants have patient populations that are comparable to those of physicians, and their diabetes management is as good as that provided by physicians," Dr. Lawrence S. Phillips said at the annual scientific sessions of the American Diabetes Association.
Diabetes affects more than 20% of patients in the VA system, which is the largest employer of nurse practitioners and physician assistants in the country, he said. Dr. Phillips and his associates analyzed VA data to identify patients who saw a physician, nurse practitioner, or physician assistant for more than 50% of health care visits since a new diagnosis of diabetes in 2008-2012.
Average A1C levels at the time of diabetes diagnosis, at the initiation of medications, and during follow-up years did not differ significantly between provider groups after patient characteristics were adjusted for, reported Dr. Phillips, professor of medicine at Emory University, Atlanta. Baseline A1C levels were 7.18%, 7.14%, and 7.20% with nurse practitioners, physician assistants, and physicians, respectively, and dropped to 6.75%, 6.75%, and 6.78% by 2012.
Patient demographics were similar between provider groups. Their mean age was roughly 69 years, about 95% were male, and their mean body mass index was about 32.4 kg/m2. The cohort seen by physicians had a smaller percentage of white patients (77%) than did the cohort seen by physician assistants (81%).
Patient comorbidity levels, as measured by the Charlson Comorbidity Index, were the same in each provider group (a score of 1 in each group). The proportion of patients on any diabetes therapy was similar between groups: 81% with physicians, 80% with nurse practitioners, and 79% with physician assistants.
A significantly smaller proportion of patients seeing physician assistants were on insulin (12%), compared with those seeing physicians (15%) or nurse practitioners (14%), Dr. Phillips reported. Physician assistants also referred a significantly smaller proportion of patients to diabetes specialists (5%), compared with physicians (8%) or nurse practitioners (7%).
The findings surprised the investigators and suggested that the VA model of using advanced practice providers might be broadly useful to help the U.S. meet demand for primary care providers, he said.
Dr. Phillips reported having financial associations with multiple pharmaceutical companies but none related to this study.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Diabetes outcomes similar with physicians, midlevel providers
SAN FRANCISCO – Physicians and midlevel health care providers saw comparable types of patients with diabetes in the Veterans Affairs health care system and helped patients achieve comparable changes in hemoglobin A1c levels, a study of 19,238 health care providers found.
"At the time of diagnosis of diabetes and during 4 years of follow-up care, nurse practitioners and physician assistants have patient populations that are comparable to those of physicians, and their diabetes management is as good as that provided by physicians," Dr. Lawrence S. Phillips said at the annual scientific sessions of the American Diabetes Association.
Diabetes affects more than 20% of patients in the VA system, which is the largest employer of nurse practitioners and physician assistants in the country, he said. Dr. Phillips and his associates analyzed VA data to identify patients who saw a physician, nurse practitioner, or physician assistant for more than 50% of health care visits since a new diagnosis of diabetes in 2008-2012.
Average HbA1c levels at the time of diabetes diagnosis, at the initiation of medications, and during follow-up years did not differ significantly between provider groups after patient characteristics were adjusted for, reported Dr. Phillips, professor of medicine at Emory University, Atlanta. Baseline HbA1c levels were 7.18%, 7.14%, and 7.20% with nurse practitioners, physician assistants, and physicians, respectively, and dropped to 6.75%, 6.75%, and 6.78% by 2012.
Patient demographics were similar between provider groups. Their mean age was roughly 69 years, about 95% were male, and their mean body mass index was about 32.4 kg/m2. The cohort seen by physicians had a smaller percentage of white patients (77%) than did the cohort seen by physician assistants (81%).
Patient comorbidity levels, as measured by the Charlson Comorbidity Index, were the same in each provider group (a score of 1 in each group). The proportion of patients on any diabetes therapy was similar between groups: 81% with physicians, 80% with nurse practitioners, and 79% with physician assistants.
A significantly smaller proportion of patients seeing physician assistants were on insulin (12%), compared with those seeing physicians (15%) or nurse practitioners (14%), Dr. Phillips reported. Physician assistants also referred a significantly smaller proportion of patients to diabetes specialists (5%), compared with physicians (8%) or nurse practitioners (7%).
The findings surprised the investigators and suggested that the VA model of using midlevel providers might be broadly useful to help the U.S. meet demand for primary care providers, he said.
Dr. Phillips reported having financial associations with multiple pharmaceutical companies but none related to this study.
On Twitter @sherryboschert
This study defined provider type by whether a physician or midlevel practitioner saw the patient in 50% or more of the patient’s visits. But it could be that the VA system has appropriate and selective use of MD specialists, who guide the initiation of insulin and escalation of therapy, and then, appropriately, the midlevel providers deliver more education-related or lifestyle-related care. I think a little bit more understanding of who is doing what, not just where the majority of care is being conducted, is needed to fully understand this.
 |
|
We don’t live in a world where specialists can be delivering all of diabetes care. The numbers don’t add up. Where we need to go is figuring out how we can effectively use each of our provider types.
I would lean more toward this study being a first step in understanding. Are we talking about replacing or complementing physicians? Before we see more data, I would think that we still are in a complementing world, but we need to refine that.
Dr. Sanjeev N. Mehta of the Joslin Diabetes Center, Boston, gave these comments in an interview at the meeting. He reported having no financial disclosures.
This study defined provider type by whether a physician or midlevel practitioner saw the patient in 50% or more of the patient’s visits. But it could be that the VA system has appropriate and selective use of MD specialists, who guide the initiation of insulin and escalation of therapy, and then, appropriately, the midlevel providers deliver more education-related or lifestyle-related care. I think a little bit more understanding of who is doing what, not just where the majority of care is being conducted, is needed to fully understand this.
 |
|
We don’t live in a world where specialists can be delivering all of diabetes care. The numbers don’t add up. Where we need to go is figuring out how we can effectively use each of our provider types.
I would lean more toward this study being a first step in understanding. Are we talking about replacing or complementing physicians? Before we see more data, I would think that we still are in a complementing world, but we need to refine that.
Dr. Sanjeev N. Mehta of the Joslin Diabetes Center, Boston, gave these comments in an interview at the meeting. He reported having no financial disclosures.
This study defined provider type by whether a physician or midlevel practitioner saw the patient in 50% or more of the patient’s visits. But it could be that the VA system has appropriate and selective use of MD specialists, who guide the initiation of insulin and escalation of therapy, and then, appropriately, the midlevel providers deliver more education-related or lifestyle-related care. I think a little bit more understanding of who is doing what, not just where the majority of care is being conducted, is needed to fully understand this.
 |
|
We don’t live in a world where specialists can be delivering all of diabetes care. The numbers don’t add up. Where we need to go is figuring out how we can effectively use each of our provider types.
I would lean more toward this study being a first step in understanding. Are we talking about replacing or complementing physicians? Before we see more data, I would think that we still are in a complementing world, but we need to refine that.
Dr. Sanjeev N. Mehta of the Joslin Diabetes Center, Boston, gave these comments in an interview at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Physicians and midlevel health care providers saw comparable types of patients with diabetes in the Veterans Affairs health care system and helped patients achieve comparable changes in hemoglobin A1c levels, a study of 19,238 health care providers found.
"At the time of diagnosis of diabetes and during 4 years of follow-up care, nurse practitioners and physician assistants have patient populations that are comparable to those of physicians, and their diabetes management is as good as that provided by physicians," Dr. Lawrence S. Phillips said at the annual scientific sessions of the American Diabetes Association.
Diabetes affects more than 20% of patients in the VA system, which is the largest employer of nurse practitioners and physician assistants in the country, he said. Dr. Phillips and his associates analyzed VA data to identify patients who saw a physician, nurse practitioner, or physician assistant for more than 50% of health care visits since a new diagnosis of diabetes in 2008-2012.
Average HbA1c levels at the time of diabetes diagnosis, at the initiation of medications, and during follow-up years did not differ significantly between provider groups after patient characteristics were adjusted for, reported Dr. Phillips, professor of medicine at Emory University, Atlanta. Baseline HbA1c levels were 7.18%, 7.14%, and 7.20% with nurse practitioners, physician assistants, and physicians, respectively, and dropped to 6.75%, 6.75%, and 6.78% by 2012.
Patient demographics were similar between provider groups. Their mean age was roughly 69 years, about 95% were male, and their mean body mass index was about 32.4 kg/m2. The cohort seen by physicians had a smaller percentage of white patients (77%) than did the cohort seen by physician assistants (81%).
Patient comorbidity levels, as measured by the Charlson Comorbidity Index, were the same in each provider group (a score of 1 in each group). The proportion of patients on any diabetes therapy was similar between groups: 81% with physicians, 80% with nurse practitioners, and 79% with physician assistants.
A significantly smaller proportion of patients seeing physician assistants were on insulin (12%), compared with those seeing physicians (15%) or nurse practitioners (14%), Dr. Phillips reported. Physician assistants also referred a significantly smaller proportion of patients to diabetes specialists (5%), compared with physicians (8%) or nurse practitioners (7%).
The findings surprised the investigators and suggested that the VA model of using midlevel providers might be broadly useful to help the U.S. meet demand for primary care providers, he said.
Dr. Phillips reported having financial associations with multiple pharmaceutical companies but none related to this study.
On Twitter @sherryboschert
SAN FRANCISCO – Physicians and midlevel health care providers saw comparable types of patients with diabetes in the Veterans Affairs health care system and helped patients achieve comparable changes in hemoglobin A1c levels, a study of 19,238 health care providers found.
"At the time of diagnosis of diabetes and during 4 years of follow-up care, nurse practitioners and physician assistants have patient populations that are comparable to those of physicians, and their diabetes management is as good as that provided by physicians," Dr. Lawrence S. Phillips said at the annual scientific sessions of the American Diabetes Association.
Diabetes affects more than 20% of patients in the VA system, which is the largest employer of nurse practitioners and physician assistants in the country, he said. Dr. Phillips and his associates analyzed VA data to identify patients who saw a physician, nurse practitioner, or physician assistant for more than 50% of health care visits since a new diagnosis of diabetes in 2008-2012.
Average HbA1c levels at the time of diabetes diagnosis, at the initiation of medications, and during follow-up years did not differ significantly between provider groups after patient characteristics were adjusted for, reported Dr. Phillips, professor of medicine at Emory University, Atlanta. Baseline HbA1c levels were 7.18%, 7.14%, and 7.20% with nurse practitioners, physician assistants, and physicians, respectively, and dropped to 6.75%, 6.75%, and 6.78% by 2012.
Patient demographics were similar between provider groups. Their mean age was roughly 69 years, about 95% were male, and their mean body mass index was about 32.4 kg/m2. The cohort seen by physicians had a smaller percentage of white patients (77%) than did the cohort seen by physician assistants (81%).
Patient comorbidity levels, as measured by the Charlson Comorbidity Index, were the same in each provider group (a score of 1 in each group). The proportion of patients on any diabetes therapy was similar between groups: 81% with physicians, 80% with nurse practitioners, and 79% with physician assistants.
A significantly smaller proportion of patients seeing physician assistants were on insulin (12%), compared with those seeing physicians (15%) or nurse practitioners (14%), Dr. Phillips reported. Physician assistants also referred a significantly smaller proportion of patients to diabetes specialists (5%), compared with physicians (8%) or nurse practitioners (7%).
The findings surprised the investigators and suggested that the VA model of using midlevel providers might be broadly useful to help the U.S. meet demand for primary care providers, he said.
Dr. Phillips reported having financial associations with multiple pharmaceutical companies but none related to this study.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Patients who saw midlevel providers for most of their visits achieved HbA1c levels comparable with those of patients who saw primarily physicians.
Major finding: The characteristics and comorbidity levels of patients with diabetes, and their HbA1c levels after treatment, were similar among patients seen predominantly by physicians, nurse practitioners, or physician assistants.
Data source: A retrospective study of patients with diabetes seen by 19,238 physicians or midlevel providers in the VA health care system from 2008 to 2012.
Disclosures: Dr. Phillips reported having financial associations with multiple pharmaceutical companies but none related to this study.