ORLANDO – Women are at lower risk than men for new-onset atrial fibrillation during hospitalization, but when it does occur it’s associated with significantly greater in-hospital mortality, according to a massive retrospective study presented at the American Heart Association scientific sessions.
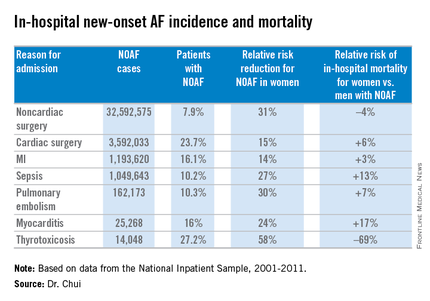
Dr. Philip W. Chui analyzed 38,403,360 cases of new-onset atrial fibrillation during hospitalization (NOAF) in 2001-2011. The source was the National Inpatient Sample database. Fully 85% of all cases occurred in patients admitted for noncardiac surgery, which also was the cause of admission with the lowest incidence of NOAF. Among the patients hospitalized for sepsis, women were 27% less likely than men to develop new-onset atrial fibrillation, but when they did they were 13% more likely to die in-hospital.
In a multivariate logistic regression analysis extensively adjusted for numerous comorbid conditions and demographic factors, female gender was associated with a significantly reduced risk of NOAF across the board for all major admitting conditions known to be triggers for NOAF. The magnitude of this relative risk reduction favoring women ranged from as low as 14% for patients with an admitting diagnosis of acute MI to 58% with admission for thyrotoxicosis, reported Dr. Chui, an internal medicine resident at the University of California, Irvine.
The most provocative study finding was the significantly higher in-hospital mortality for women, compared with men with NOAF for all but two of the seven major reasons for admission studied: noncardiac surgery and thyrotoxicosis. Dr. Chui asserted that this appears to be a quality of care issue.
“The overwhelming majority of new-onset AF in-hospital occurs in postsurgical patients, who may be under the care of providers with less experience in managing AF,” he said. “Our results suggest clinicians need to be aware of the subtleties in presentation and management of female new-onset AF patients compared to their male counterparts.”
Dr. Chui reported having no financial conflicts regarding his study, which was financially supported by the university’s department of internal medicine.