A 72-year-old man has a three-week history of fatigue, lethargy, and shortness of breath. He tires easily with minimal ambulation; it takes him longer than usual to get out of bed in the morning, and he frequently falls asleep on his sofa while watching television. He denies chest pain, palpitations, or syncope but states that on at least two occasions he has felt dizzy and lightheaded while getting out of bed. He’s never had this problem before and says he hasn’t done anything differently in the past month. He is concerned that it “may be my time to die,” as his wife died after having similar symptoms five years ago.
Medical history is remarkable for type 2 diabetes, hypercholesterolemia, coronary artery disease, and a remote inferior myocardial infarction (MI) 14 years ago. Surgical history includes a cholecystectomy and an open reduction and internal fixation of a left high ankle fracture.
His current medication list includes metformin, isosorbide dinitrate, metoprolol, and atorvastatin. He has an anaphylactic allergy to sulfa. He cannot give a family history, as he was adopted and does not know his biological family.
The patient, a retired welder, is a recovering alcoholic; he attends Alcoholics Anonymous meetings regularly and has been sober for more than 12 years. He smoked a half-pack of cigarettes each day as a teenager but quit when he got married 52 years ago. He is a widower. His son died in an automobile accident at age 32; his daughter lives nearby and checks on him every day.
Review of systems is remarkable for neuropathic foot pain due to diabetes, recurrent constipation, corrective lenses, and hearing aids. The remainder of the review is noncontributory.
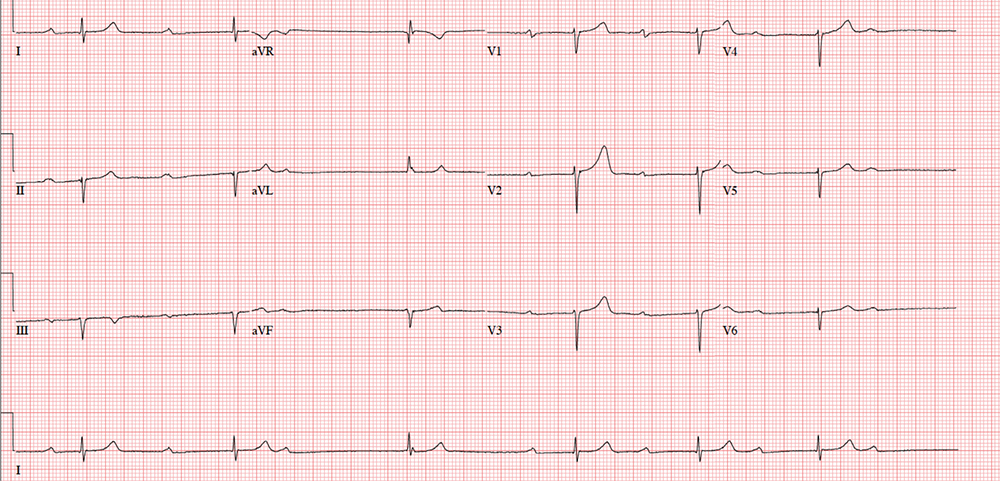
Vital signs include a blood pressure of 112/56 mm Hg; pulse, 40 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 99.2°F. His height is 76 in and his weight, 194 lb. Physical exam reveals an elderly but otherwise healthy-looking male in no distress.
The HEENT exam is remarkable for early cataract formation but is otherwise normal. His dentition is in remarkably excellent health. There is no thyromegaly or jugular venous distention, and the lungs are clear in all fields without wheezes or crackles.
Cardiac exam reveals a roughly normal rate of 40 beats/min. It is difficult to determine whether there is respiratory variation, given the slower rate. There is an early grade II/VI systolic murmur of aortic sclerosis best heard at the left upper sternal border. It does not radiate elsewhere. There are no extra heart sounds or rubs.
The abdomen has well-healed surgical scars with no palpable organomegaly. Bowel sounds are present in all quadrants. A rectal exam reveals impaction of firm stool; the prostate is not palpable given the amount of firm stool present.
The extremities have full range of motion without clubbing, cyanosis, or edema. Peripheral pulses are full bilaterally in both upper and lower extremities. A well-healed surgical scar is present on the left lateral lower extremity, and a plate is palpable beneath the skin. Skin sensitivity testing with 2-point pinprick of the soles and toes of both feet reveals extensive paresthesias. Apart from this, the neurologic exam is grossly normal. There is no evidence of diabetic foot ulcers.
An ECG shows a ventricular rate of 38 beats/min; no discernable PR interval; QRS duration, 78 ms; QT/QTc interval, 434/345 ms; P axis, 25°; R axis, –78°; and T axis, 13°. What is your interpretation?