TREATMENT
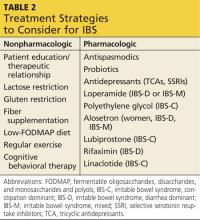
Evidence supports a number of therapeutic options, both lifestyle and pharmacologic (see Table 2). Lifestyle options include comprehensive patient education, dietary manipulation, cognitive behavioral therapy (CBT), and exercise. Pharmacologic options include antispasmodic agents, antidepressants, antidiarrheal agents, osmotic laxatives, alosetron, lubiprostone, rifaximin, and linaclotide.
Lifestyle changes
A therapeutic relationship that includes a nonjudgmental attitude, realistic expectations, and patient-directed care is the cornerstone of successful nonpharmacologic IBS management.4 In addition, patient education should emphasize management instead of cure, and the patient should be informed that IBS may wax and wane over a lifetime but will not shorten his/her lifespan.4
A six-week, single-blind, randomized trial (N = 262) attempted to assess the impact of patient–provider interaction on IBS symptoms and HRQOL. Participants were assigned to one of three groups: waiting list, limited intervention, and augmented intervention, with the last group receiving the greatest amount of education and patient–provider interaction. After three and six weeks, participants in the augmented group reported significant improvements in global IBS symptoms and HRQOL scores.8 Although these findings are limited by a short follow-up period, they underscore the importance of a strong therapeutic relationship in a successful outcome.
Diet. Since food sensitivities—to lactose; gluten; fiber; fermentable oligosaccharides, disaccharides, and monosaccharides, and polyols (FODMAP); and carbohydrates—are thought to be integral to the etiology of IBS, dietary manipulation plays a major role in managing symptoms.4
Due to overlapping symptoms, a lactose-restricted diet may be appropriate in a subset of IBS-D and IBS-M patients. A prospective clinical trial enrolled 70 adult participants with IBS, 24% of whom were lactose intolerant. All participants were given a lactose-restricted diet for six weeks, and a significant improvement of IBS symptoms in the lactose-intolerant subgroup was observed. This subgroup was advised to continue a lactose-restricted diet and was then followed for five years. Of the 14 participants who remained in the study for the five years, none reported IBS complaints.9 While limited by its small sample size, this study supports the ACG recommendation to consider lactose hydrogen breath testing to screen for lactose-intolerance in a select group of patients with IBS symptoms.
Gluten. It has been observed that gluten withdrawal may improve IBS symptoms. A recent four-week randomized controlled trial (RCT; N = 45) evaluated the effect of gluten restriction on subjective markers including stool frequency, form, and ease of passage, and on objective markers related to intestinal function in adults with known IBS-D who did not have gluten sensitivity or celiac disease.10 Participants on the gluten-restricted diet reported a significant reduction in stool frequency, especially among those with HLA DQ2 and DQ8 genotypes. There was no effect on stool form or ease of passage.10
An RCT conducted by Biesiekierski and colleagues enrolled 30 patients with IBS who reported symptom control on a gluten-free diet.11 Study participants were randomly assigned to either a continued gluten-free diet or to a gluten-containing diet. Over the six-week
follow-up period, significantly more participants on a gluten-containing diet reported inadequate control of IBS symptoms.11 The small sample size and short follow-up period led the researchers to conclude that additional studies are needed to confirm whether gluten restriction attenuates IBS symptoms.
Fiber. Data are inconclusive regarding efficacy of fiber in reducing IBS symptoms. A subgroup of patients with IBS report increased abdominal pain and bloating when increasing their fiber intake.1 This was supported by a systematic review that found no clinical improvement in IBS symptoms with bulking agents.12 That said, patients with IBS-C may benefit from a trial of dietary fiber, which should be introduced at a low dose (eg, 1/2 to 1 Tb of wheat bran or psyllium daily) and titrated up as needed and tolerated.1
FODMAP. A number of clinical trials have suggested that there is a benefit to consuming a diet low in FODMAP foods (see chart). Shepherd and colleagues conducted an RCT (N = 25) that compared the effects of high- and low-FODMAP diets on IBS symptoms over a two-week period. Of participants in the high-FODMAP group, 79% reported inadequate IBS symptom control, while only 14% in the low-FODMAP group reported inadequate IBS symptom control.13
In a second trial (N = 30) that had similar objectives, symptoms worsened significantly on a
high-FODMAP diet compared to a low one among the IBS participants. Healthy participants experienced more flatulence on the high-FODMAP diet compared to those on a low one.14
Carbohydrates. In a small clinical trial (N = 17), IBS-D participants consumed a standard diet for two weeks followed by a very low carbohydrate diet (< 20 g/d) for four weeks. They were assessed weekly for adequate relief of IBS symptoms. For purposes of the study, a patient was considered a responder if he/she experienced adequate relief of IBS symptoms during at least two of the four treatment weeks. In addition to symptom relief, secondary measures included abdominal pain, stool frequency, stool consistency, and quality of life.15
Of the 13 participants who completed the study, all were considered responders; 10 of 13 (77%) reported adequate relief of IBS symptoms for four out of four treatment weeks. There were significant improvements in abdominal pain, stool frequency, stool consistency, and quality of life during treatment weeks.15 Additional trials with larger sample sizes and longer follow-up periods are needed to confirm these preliminary findings.
Exercise. Regular exercise not only offers general health benefits but may also simultaneously reduce IBS symptoms. An RCT (N =102) assigned patients with IBS either to their normal daily activity or to 20 to 60 minutes of moderate-to-vigorous exercise three to five days a week. After 12 weeks, the exercise group showed decreased IBS symptom severity. They were also significantly less likely to report worsening IBS symptoms.16
Cognitive behavioral therapy. CBT may be helpful in reducing IBS symptoms. In an RCT (N = 75) that assigned patients with IBS to conventional CBT, self-administered CBT, or a control group, IBS symptoms improved significantly in those assigned to both CBT groups.17 A systematic review and meta-analysis reported a relative risk (RR) of persistent IBS symptoms with CBT of 0.67 and a number needed to treat (NNT) of 4.18
Continued on next page >>