User login
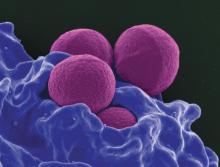
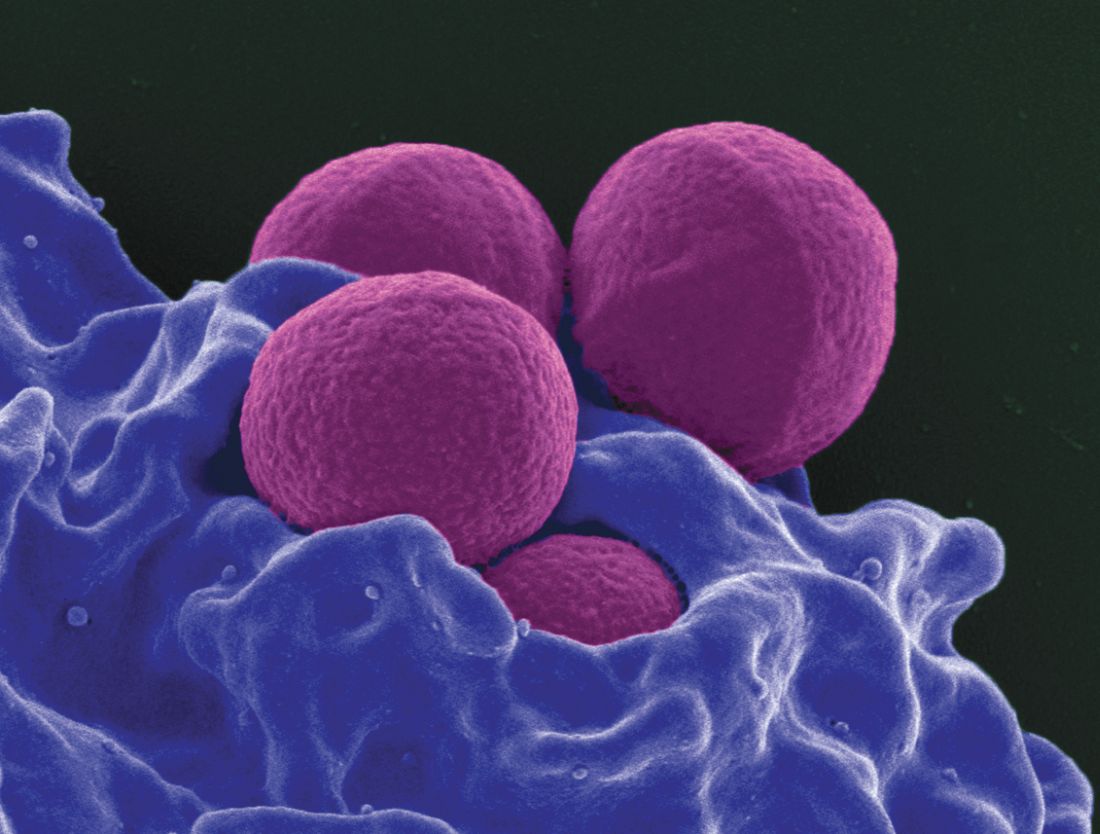
NEW ORLEANS – Compared with vancomycin monotherapy, vancomycin combined with cefepime improved some outcomes for patients with methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections, a retrospective study of 109 patients revealed.
A lower likelihood of microbiological failure and fewer bloodstream infections persisting 7 days or more were the notable differences between treatment groups.
All patients had at least 72 hours of vancomycin therapy to treat MRSA bacteremia confirmed by blood culture. During 2008-2015, 38 adults received vancomycin monotherapy and 71 received vancomycin plus 24 hours or more of cefepime.
Compared with monotherapy, the combination treatment was associated with a nonsignificant reduction in the primary composite treatment failure outcome of 30-day all-cause mortality, in bacteremia duration of 7 days or more, and in 60-day bloodstream-infection recurrence: 55% for monotherapy versus 42% for combination therapy (P = .195). The difference was primarily associated with decreased duration of sepsis and fewer MRSA bloodstream infections persisting 7 days or more in the combination cohort.
Rates of bacteremia duration of 7 days or more were 42% in monotherapy patients and 20% in combination patients (P = .013). Differences in 60-day bloodstream-infection recurrence were nonsignificant, 8% versus 4%, respectively (P = .42).
Thirty-day mortality, however, was lower among monotherapy patients than combination patients – 13% vs. 25% – although the difference was nonsignificant (P = .21).
“From what I see here … it seems like they will have a lower duration of bacteremia, which is always great,” Ms. Atwan said. “You want to decrease length of stay in the hospital,” which will cut down on costs and on patients’ risks of getting more infections.
Although the primary outcome was a composite endpoint, “when we looked at them separately, we found the patients in the combination group had more mortality,” Ms. Atwan said at the annual meeting of the American Society for Microbiology. “That surprised me initially. But those patients are sicker and more likely to get dual coverage.”
The investigators confirmed the association between the severity of MRSA bacteremia and combination therapy by looking at Acute Physiology and Chronic Health Evaluation (APACHE II) scores. The median APACHE score was 23 in the combination group, compared with 13.5 in the monotherapy group (P = 0003). Higher APACHE scores were associated with greater odds of meeting the composite failure endpoint (adjusted odds ratio, 1.08) and of developing endocarditis (aOR, 3.6) in multivariate analyses.
More patients in the combination group had pneumonia as the primary source of infection than did patients in the monotherapy group: 54% vs. 29% (P = .016). Further, more of them had skin or soft tissue infections as the primary infection source: 29% vs. 13% (P = .036).
Although the exact mechanism remains unknown, synergy between the two agents could be caused by an increase in penicillin-binding proteins, Ms. Atwan said.
The study is still ongoing; Ms. Atwan hopes additional patients and data will lead to statistically significant differences between the outcomes of combination therapy and vancomycin monotherapy.
“I want to say that combination therapy is something you will always want to go to when you have a sicker patient, but I can’t really tell you that combination therapy is going to cause better outcomes for your patient,” she cautioned. “Hopefully, I can by the end of the study.”
In the meantime, “it looks like vancomycin and beta-lactams could be beneficial for MRSA bacteremia,” she added.
The researchers noted that although vancomycin monotherapy is a mainstay of treatment for MRSA bloodstream infections, emergence of reduced susceptibility and treatment failures warrants other therapeutic strategies.
Ms. Atwan had no relevant financial disclosures.
NEW ORLEANS – Compared with vancomycin monotherapy, vancomycin combined with cefepime improved some outcomes for patients with methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections, a retrospective study of 109 patients revealed.
A lower likelihood of microbiological failure and fewer bloodstream infections persisting 7 days or more were the notable differences between treatment groups.
All patients had at least 72 hours of vancomycin therapy to treat MRSA bacteremia confirmed by blood culture. During 2008-2015, 38 adults received vancomycin monotherapy and 71 received vancomycin plus 24 hours or more of cefepime.
Compared with monotherapy, the combination treatment was associated with a nonsignificant reduction in the primary composite treatment failure outcome of 30-day all-cause mortality, in bacteremia duration of 7 days or more, and in 60-day bloodstream-infection recurrence: 55% for monotherapy versus 42% for combination therapy (P = .195). The difference was primarily associated with decreased duration of sepsis and fewer MRSA bloodstream infections persisting 7 days or more in the combination cohort.
Rates of bacteremia duration of 7 days or more were 42% in monotherapy patients and 20% in combination patients (P = .013). Differences in 60-day bloodstream-infection recurrence were nonsignificant, 8% versus 4%, respectively (P = .42).
Thirty-day mortality, however, was lower among monotherapy patients than combination patients – 13% vs. 25% – although the difference was nonsignificant (P = .21).
“From what I see here … it seems like they will have a lower duration of bacteremia, which is always great,” Ms. Atwan said. “You want to decrease length of stay in the hospital,” which will cut down on costs and on patients’ risks of getting more infections.
Although the primary outcome was a composite endpoint, “when we looked at them separately, we found the patients in the combination group had more mortality,” Ms. Atwan said at the annual meeting of the American Society for Microbiology. “That surprised me initially. But those patients are sicker and more likely to get dual coverage.”
The investigators confirmed the association between the severity of MRSA bacteremia and combination therapy by looking at Acute Physiology and Chronic Health Evaluation (APACHE II) scores. The median APACHE score was 23 in the combination group, compared with 13.5 in the monotherapy group (P = 0003). Higher APACHE scores were associated with greater odds of meeting the composite failure endpoint (adjusted odds ratio, 1.08) and of developing endocarditis (aOR, 3.6) in multivariate analyses.
More patients in the combination group had pneumonia as the primary source of infection than did patients in the monotherapy group: 54% vs. 29% (P = .016). Further, more of them had skin or soft tissue infections as the primary infection source: 29% vs. 13% (P = .036).
Although the exact mechanism remains unknown, synergy between the two agents could be caused by an increase in penicillin-binding proteins, Ms. Atwan said.
The study is still ongoing; Ms. Atwan hopes additional patients and data will lead to statistically significant differences between the outcomes of combination therapy and vancomycin monotherapy.
“I want to say that combination therapy is something you will always want to go to when you have a sicker patient, but I can’t really tell you that combination therapy is going to cause better outcomes for your patient,” she cautioned. “Hopefully, I can by the end of the study.”
In the meantime, “it looks like vancomycin and beta-lactams could be beneficial for MRSA bacteremia,” she added.
The researchers noted that although vancomycin monotherapy is a mainstay of treatment for MRSA bloodstream infections, emergence of reduced susceptibility and treatment failures warrants other therapeutic strategies.
Ms. Atwan had no relevant financial disclosures.
NEW ORLEANS – Compared with vancomycin monotherapy, vancomycin combined with cefepime improved some outcomes for patients with methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections, a retrospective study of 109 patients revealed.
A lower likelihood of microbiological failure and fewer bloodstream infections persisting 7 days or more were the notable differences between treatment groups.
All patients had at least 72 hours of vancomycin therapy to treat MRSA bacteremia confirmed by blood culture. During 2008-2015, 38 adults received vancomycin monotherapy and 71 received vancomycin plus 24 hours or more of cefepime.
Compared with monotherapy, the combination treatment was associated with a nonsignificant reduction in the primary composite treatment failure outcome of 30-day all-cause mortality, in bacteremia duration of 7 days or more, and in 60-day bloodstream-infection recurrence: 55% for monotherapy versus 42% for combination therapy (P = .195). The difference was primarily associated with decreased duration of sepsis and fewer MRSA bloodstream infections persisting 7 days or more in the combination cohort.
Rates of bacteremia duration of 7 days or more were 42% in monotherapy patients and 20% in combination patients (P = .013). Differences in 60-day bloodstream-infection recurrence were nonsignificant, 8% versus 4%, respectively (P = .42).
Thirty-day mortality, however, was lower among monotherapy patients than combination patients – 13% vs. 25% – although the difference was nonsignificant (P = .21).
“From what I see here … it seems like they will have a lower duration of bacteremia, which is always great,” Ms. Atwan said. “You want to decrease length of stay in the hospital,” which will cut down on costs and on patients’ risks of getting more infections.
Although the primary outcome was a composite endpoint, “when we looked at them separately, we found the patients in the combination group had more mortality,” Ms. Atwan said at the annual meeting of the American Society for Microbiology. “That surprised me initially. But those patients are sicker and more likely to get dual coverage.”
The investigators confirmed the association between the severity of MRSA bacteremia and combination therapy by looking at Acute Physiology and Chronic Health Evaluation (APACHE II) scores. The median APACHE score was 23 in the combination group, compared with 13.5 in the monotherapy group (P = 0003). Higher APACHE scores were associated with greater odds of meeting the composite failure endpoint (adjusted odds ratio, 1.08) and of developing endocarditis (aOR, 3.6) in multivariate analyses.
More patients in the combination group had pneumonia as the primary source of infection than did patients in the monotherapy group: 54% vs. 29% (P = .016). Further, more of them had skin or soft tissue infections as the primary infection source: 29% vs. 13% (P = .036).
Although the exact mechanism remains unknown, synergy between the two agents could be caused by an increase in penicillin-binding proteins, Ms. Atwan said.
The study is still ongoing; Ms. Atwan hopes additional patients and data will lead to statistically significant differences between the outcomes of combination therapy and vancomycin monotherapy.
“I want to say that combination therapy is something you will always want to go to when you have a sicker patient, but I can’t really tell you that combination therapy is going to cause better outcomes for your patient,” she cautioned. “Hopefully, I can by the end of the study.”
In the meantime, “it looks like vancomycin and beta-lactams could be beneficial for MRSA bacteremia,” she added.
The researchers noted that although vancomycin monotherapy is a mainstay of treatment for MRSA bloodstream infections, emergence of reduced susceptibility and treatment failures warrants other therapeutic strategies.
Ms. Atwan had no relevant financial disclosures.
AT ASM MICROBE 2017
Key clinical point:
Major finding: Median duration of MRSA bacteremia was 4 days with combination therapy, versus 6 days with vancomycin alone.
Data source: A retrospective, single-center comparison of 109 patients treated with either vancomycin plus cefepime or vancomycin alone.
Disclosures: Safana M. Atwan had no relevant financial disclosures.