Basal cell carcinoma (BCC) is the most common skin malignancy, but it can still be a tricky and difficult diagnosis even in the most experienced hands. Many BCCs exhibit only some of the defining clinical characteristics, and even when these findings are present, they can be hard to detect without excellent background and oblique lighting and handheld magnification that is 5-power or greater.
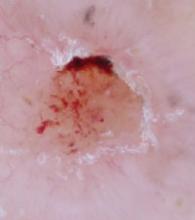
Most clinicians are familiar with classic BCC characteristics of pearliness, rolled edges, telangiectasia, bleeding, and crusting. However, the telangiectasias may be so fine that they are difficult or impossible to see, even with excellent lighting and magnification. FIGURE 1A illustrates a histologically verified nodular BCC with telangiectasias that are not readily visible, even with camera macro magnification.
Some BCC papules or plaques lack the classic rolled edges, even when viewed with oblique lighting and magnification. Some lesions may be more scaly than pearly, and others do not bleed and crust until later in their clinical course. With such variation in clinical presentation, all possible clues to BCC are welcome.
Dark dots: Connecting them to BCC
One underappreciated sign that may help with the diagnosis of BCC is the “dark dot sign.”1,2 Dermoscopists are familiar with patterns of pigmentation associated with BCCs, and introductory dermoscopy texts contain pictures of these patterns (blue/blue-gray blotches, maple leaf structures, and spoke-wheel structures).3,4 What is less well known is that this pigmentation may be visible on routine skin examination as “dark dots”—blue, gray, black, or a combination thereof, such as blue-gray. When visible clinically, these dark dots may bolster one’s confidence in the diagnosis—or, in my experience, occasionally even be the best visible hint for a tentative diagnosis of BCC.
Case in point. During a routine skin examination of a patient’s back, I identified an asymptomatic lesion the patient was unaware of, exhibiting no bleeding or crusting. It drew attention because it was different from surrounding lesions (FIGURE 2A), which has been called the “ugly duckling sign.”5 On closer examination, I noted the lesion had a pearly sheen, telangiectasias, and a plethora of dark dots (FIGURE 2B)—the poster child for the “dark dot sign.” Unlike this profound example, most lesions that have dark dots have just one or a few visible dots.
Now review FIGURE 1A again carefully. Above the lesion’s central crater there is an arcuate hemorrhagic crust, and, between the 12 and 1 o’clock positions, a small dark dot, which helps corroborate the clinical impression of BCC. FIGURE 1B is a dermoscopic image of the same lesion. It shows the dark dot well and illustrates the ease with which telangiectasias are seen on dermoscopy, lending a high degree of certainty to the diagnosis of BCC.
Dermoscopy (FIGURE 2C) for the lesion on the patient’s back in FIGURE 2B, however, adds nothing (beyond magnification) because telangiectasias and dark dots were visible clinically.
CASE #1
FIGURE 1A
Basal cell carcinoma. Even with photography, which is often clearer than magnified clinical inspection, telangiectasias are not well seen in this basal cell carcinoma. A dark dot, however, is visible between the 12 and 1 o’clock positions.
FIGURE 1B
A dermoscopic view of the BCC in FIGURE 1A clearly shows telangiectasias and a dark dot.
CASE #2
FIGURE 2A
Ugly duckling sign. The circled lesion on this patient’s back wasn’t crusty or bleeding, but it drew attention because it was different from surrounding lesions. This has been called the “ugly duckling sign.”
FIGURE 2B
Dark dots. A closer look at the lesion on the patient’s back revealed multiple dark dots and telangiectasias, virtually diagnostic of basal cell carcinoma.
FIGURE 2C
A dermoscopic view of the lesion in FIGURE 2B adds little to what was well visualized clinically.
Caution: Context is critical
Because dots or blotches of pigment may occur in squamous cell carcinoma, pigmented actinic keratoses, seborrheic keratoses, and hypomelanotic or “amelanotic” melanoma, it is not possible clinically to confirm a diagnosis of BCC solely on the basis of dark dots. (In fact, even in the absence of pigment, any “red and white” lesion could be an amelanotic melanoma.) However, when added to other findings, such as a firm, pearly papule, the finding increases the likelihood of BCC.
How to proceed to biopsy
Lesions such as the ones I’ve shown should never be treated without preserving a specimen for pathology examination (eg, directly frozen). That said, there is no one right biopsy technique. The choice will depend on your clinical suspicion and perhaps other factors in your patient’s circumstance.