User login
How I solved my e-prescribing dilemma
Even with government incentives, I physicians have been slow to make the leap to electronic medical records (EMR) and full electronic prescribing (e-prescribing). My transition to e-prescribing evolved over about a decade, and I was a satisfied e-prescriber—for a while.
Around 2000, I began writing electronic prescriptions using iScribe for Palm handhelds.1 The final transition to full e-prescribing required only a WiFi connection in the office for use with my Palm, and hitting Send to submit the prescription to the pharmacy. iScribe was user friendly and fast. It eliminated pharmacy “callbacks, “ provided printed receipts for charting, and maintained a record of each prescription on the Palm, filed under the patient’s name. A full prescription history for each patient archived on the Palm reduced the need to pull charts for medication questions.
A rude surprise
Then iScribe was acquired by another company whose e-prescribing product, in my opinion, lengthened patient encounters because it required several additional steps to complete a prescription. This was unacceptable to me, and returning to handwritten prescriptions was out of the question. I needed a better solution.
I was disinclined to invest in another e-prescribing product whose tenure could end as abruptly as iScribe’s had. To wit: I recently read about another user-friendly, well-supported medical software program that was scooped up by a larger company selling less functional and more expensive products (while charging for a costly conversion of existing records and delivering poorer customer service).2 And e-prescribing in general has received mixed reviews.3
I briefly considered designing my own prescription writer. A full-featured writer using a relational database, such as Microsoft Access, would be ideal. But developing it would be daunting without software-specific training. The same would be true for spreadsheet software. Adobe Acrobat or word processors with directories or hyperlinks or search functions didn’t seem appropriate.
A welcome surprise
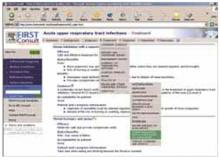
Microsoft Office 2010 software for PC and Mac platforms now includes OneNote, a program new to me. (Price at Costco for Office Home and Student, September 2010, was $119.) OneNote (in which I have no vested interest) is an “electronic notebook” program—a digital version of the multisubject, tabbed binders we all used in school. The user creates tabs, which appear across the top of the notebook interface. Each tab can accommodate as many pages as the user desires, just as in the sections of a paper notebook (FIGURE 1). In OneNote, each page has a title, and the title appears on the page tab on the right side of the screen (left side is an option). Several layers of subpages are also available for each page, similar to subdirectories in a computerized filing system.
FIGURE 1
Tabbed sections
OneNote’s Tabs are visible across the top. Most of the pages on the right side are obscured in this view by the search results window.
First tab: Summary sheet of patient “problems”
Since 2005, my practice has been limited to skin disease and it has been my custom to create paper “problem lists” as a handy method of tracking each patient’s malignancy types, dates, and anatomic locations. I decided to make these lists electronic, using OneNote (FIGURE 2). OneNote allows default templates, whereby clicking on New Page creates a fully formatted page. I used the template to create a derm summary sheet tab. Under that, I created an electronic page for each of the practice’s patients with a malignancy.
These patient pages are rapidly accessible with OneNote’s search box. As each additional letter is entered, the search feature narrows the possible matches. Usually, entering the first couple of letters of the last name presents the desired match in the search window. I then click on the patient’s name and hit Print; the summary is produced faster than the time it would take to find the information in an alphabetized paper notebook.
The advantage of an electronic summary sheet is that it can be updated and printed at each visit. Electronic summary sheets can be designed in any format—eg, a main page with Problems, Medications, Medication Allergies, Social History, Family History, etc, and a second page with a Health Maintenance flow sheet, or whatever makes sense for the clinician’s practice.
With OneNote, tables, graphics, and text with various fonts can be placed anywhere on the page, as can elements created with drawing tools. Pages can be any size: 3x5 card, letter, legal, or endless (like a Web page). OneNote supports “copy and paste” and “drag and drop” from other programs, as well as hyperlinks to documents outside OneNote.
The user can easily design a variety of templates for use in each tab, simply by designing a page and designating a template. One template can be set as the default for that tab. For example, when I click New Page in the Summary tab, a new summary form appears in that section. Pages can be deleted, copied, or moved within and between sections, just as in a word processing program.
FIGURE 2
Summary sheet
Each patient has a page (identifying information at right is covered) that lists his or her chronic/acute problems, as well as malignancies. One can locate the proper page by typing the first few letters of the patient’s last name in the search field.
A second tab for prescriptions
I decided to add a second tab to my notebook: Prescriptions. I designed a prescription template and set that as my default New Page for the prescription section. I created a new page for each of my common prescriptions—eg, doxycycline, minocycline, various topical acne preparations. OneNote’s search function at the top of the pages section is nearly instantaneous and shows all possible matches for a string of characters. Entering “tre” will show all matches with “tretinoin. “ It’s easy, then, to select the preparation of interest, hit Print, and have a printed prescription in seconds. For even greater efficiency, I have created new prescription pages for multiple medications I often use in combination—eg, a morning antimicrobial and an evening retinoid for acne, or compounds such as magic mouthwash (FIGURE 3).
Our office check-in process includes producing printed sticky labels with a patient’s name and address and the current date, which we can affix to things like pictures and pathology slips. So I designed my prescription blank to accommodate such labels. I print prescriptions from my wireless notebook computer to a wireless printer. The nurse affixes a label, I sign the document, and in seconds the patient has a detailed, legible prescription. The only disadvantage with this system is that unlike iScribe, I cannot look up a patient’s prescription history electronically because there is no electronically filed copy saved with the patient’s name. One option would be to enter every patient on a page and put prescriptions as subpages under the patient’s page. But that is more work than I want to do in patient exam rooms during a visit. Instead, I print 2 copies of each prescription, one of which goes into the paper chart.
I populated my Prescriptions tab with my prescription “favorites” before going live. But this can also be done “on the fly. “ You simply enter a new prescription as the need arises. OneNote automatically saves the prescription for future use (unless it’s intentionally deleted).
To produce new prescriptions, I set the Prescription blank as the default template. I click New Page and a blank prescription form appears. So, let’s say that lidocaine gel is not in the prescriber. I search “lido, “ and the ointment and transdermal formulations that have already been entered come up. I click New Page, a blank prescription form appears, and I type the details of the prescription (lidocaine gel 2%, dispense 30 grams, apply 30 to 60 minutes before procedure, refill zero). This prescription is saved automatically and will be available the next time I search “lido. “ Alternatively, an existing prescription can be copied and easily modified, as in copying a “cream” prescription and changing to “ointment” in the copy so both are available for future use.
All sorts of variations are possible: “endocarditis prophylaxis” options could be entered as a list on one prescription form. Before the list is printed, the user could simply check the desired option for that patient. Because OneNote saves all changes automatically, any changes made to the default prescriptions (eg, choosing to give a medication once daily rather than the default of twice daily) are saved automatically. When I make any custom changes, I use the Undo button, which I placed on my Quick Access Toolbar, to easily return to my preferred default status.
FIGURE 3
Prescription page for multiple medications
Medications commonly used together can be combined on a single prescription form. Additional information may be included (and discussed in advance with patients), to reduce formulary callback and preauthorization issues. Alphabetizing the prescriptions is unnecessary, given that the robust search function matches even partial words.
A third tab for patient education
After the success with the Summary sheets and Prescriptions tabs, I added a Patient Ed tab (FIGURE 4). I use handouts liberally to reinforce discussions, to give directions for medication use (eg, retinoids, imiquimod, fluorouracil, permethrin, prednisone), and to educate patients about diseases (eg, dysplastic nevi, melanoma, scabies). Most of this information resides on my computer, and OneNote allows me to rapidly locate and print the documents. I copy the links to patient education files onto corresponding individual OneNote pages, organized by the handouts’ identifying key words.
For example, for the isotretinoin-inflammatory bowel disease information sheet, I created a page called “Isotretinoin - Inflammatory Bowel Disease” in the Patient Education tab. That page contains a hyperlink to the desired document on my computer. The original document can be updated as new information becomes available, and OneNote will always link to the current version. For less commonly used handouts, I can enter key title words in the search box, click on the appropriate page, and print the document.
Because the printer is in the hall 2 steps from each exam room, I can do that faster than the nurse can find these documents in our paper system. This is particularly useful if the information on the possible link between isotretinoin and inflammatory bowel disease is missing from our isotretinoin packet.
FIGURE 4
Patient education tab
OneNote can be used as an indexing aid for patient education materials by simply dragging and dropping into it the links to “original” patient education documents. By clicking on this link, one can go to the information that resides elsewhere, and print out the material for the patient.
Many advantages with this new system
With OneNote, I have elements of a mini-electronic record with summary sheets for patients with malignancies, prescription writing, and patient handouts. In addition, I will not lose this system in a corporate buyout or be charged exorbitant fees to transfer records. Tabs can be password protected for security, and all pages under a tab can be saved in Adobe Acrobat, Microsoft Word, and OneNote formats. Those features help assure security and portability. (This system does not, however, qualify users for government incentives, as it lacks certain functions that are available with a true EMR.)
True e-prescribing—which, for me, included entering patient demographics and offered electronic access to my prescribing history for each patient—is usually an intermediary step for those moving toward full EMR implementation. Using OneNote, I carry a laptop/notebook room to room and print a lot of patient information handouts that otherwise would have to be retrieved from elsewhere.
As a trial, I used the OneNote system along with iScribe’s replacement e-prescribing product for several weeks. My OneNote system was faster. Now, only when patients specifically request e-prescriptions do I use the iScribe replacement product, which, after the corporate merger, has been continued at no charge for 2 to 3 years for existing users. (E-prescribing for Medicare patients at least 25 times in 2011 will qualify users for the Medicare incentive bonus.)
Because the “computer” portion of patient encounters usually occurs at the end of the visit, it does not interfere with the patient-physician relationship. Additionally, my average patient has already been “teched” with a digital scale, digital blood pressure cuff, and digital camera, so a computer is probably one of the more familiar pieces in the technoscape.
OneNote has become a powerful ally in my clinical practice. I thought I had everything I needed with Word, Excel, and Acrobat. But I’m glad I opened OneNote out of curiosity. It’s not only helped me to modernize my patient “problem lists, “ but it’s proven to be the solution to my e-prescribing dilemma.
CORRESPONDENCE
Gary N. Fox, MD, Defiance Clinic, 1400 E. 2nd Street, Defiance, OH 43512; foxgary@yahoo.com
1. Fox GN. Electronic prescribing: drug dealing twenty-first century style. In: Strayer SM, Reynolds PL, Ebell MH, eds. Handhelds in Medicine: A Practical Guide for Clinicians. New York, NY: Springer; 2005.
2. Levine N. Before implementing EMRs, heed words of warning. Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/Before-implementing-EMRs-heedwords-of-warning/ArticleStandard/Article/detail/666763. Accessed May 28, 2010.
3. Nash K. E-prescribing: a boon or a bane to dermatology practices? Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/E-prescribing-a-boon-or-a-bane-to-dermatology-prac/ArticleStandard/Article/detail/666779. Accessed May 28, 2010.
Even with government incentives, I physicians have been slow to make the leap to electronic medical records (EMR) and full electronic prescribing (e-prescribing). My transition to e-prescribing evolved over about a decade, and I was a satisfied e-prescriber—for a while.
Around 2000, I began writing electronic prescriptions using iScribe for Palm handhelds.1 The final transition to full e-prescribing required only a WiFi connection in the office for use with my Palm, and hitting Send to submit the prescription to the pharmacy. iScribe was user friendly and fast. It eliminated pharmacy “callbacks, “ provided printed receipts for charting, and maintained a record of each prescription on the Palm, filed under the patient’s name. A full prescription history for each patient archived on the Palm reduced the need to pull charts for medication questions.
A rude surprise
Then iScribe was acquired by another company whose e-prescribing product, in my opinion, lengthened patient encounters because it required several additional steps to complete a prescription. This was unacceptable to me, and returning to handwritten prescriptions was out of the question. I needed a better solution.
I was disinclined to invest in another e-prescribing product whose tenure could end as abruptly as iScribe’s had. To wit: I recently read about another user-friendly, well-supported medical software program that was scooped up by a larger company selling less functional and more expensive products (while charging for a costly conversion of existing records and delivering poorer customer service).2 And e-prescribing in general has received mixed reviews.3
I briefly considered designing my own prescription writer. A full-featured writer using a relational database, such as Microsoft Access, would be ideal. But developing it would be daunting without software-specific training. The same would be true for spreadsheet software. Adobe Acrobat or word processors with directories or hyperlinks or search functions didn’t seem appropriate.
A welcome surprise
Microsoft Office 2010 software for PC and Mac platforms now includes OneNote, a program new to me. (Price at Costco for Office Home and Student, September 2010, was $119.) OneNote (in which I have no vested interest) is an “electronic notebook” program—a digital version of the multisubject, tabbed binders we all used in school. The user creates tabs, which appear across the top of the notebook interface. Each tab can accommodate as many pages as the user desires, just as in the sections of a paper notebook (FIGURE 1). In OneNote, each page has a title, and the title appears on the page tab on the right side of the screen (left side is an option). Several layers of subpages are also available for each page, similar to subdirectories in a computerized filing system.
FIGURE 1
Tabbed sections
OneNote’s Tabs are visible across the top. Most of the pages on the right side are obscured in this view by the search results window.
First tab: Summary sheet of patient “problems”
Since 2005, my practice has been limited to skin disease and it has been my custom to create paper “problem lists” as a handy method of tracking each patient’s malignancy types, dates, and anatomic locations. I decided to make these lists electronic, using OneNote (FIGURE 2). OneNote allows default templates, whereby clicking on New Page creates a fully formatted page. I used the template to create a derm summary sheet tab. Under that, I created an electronic page for each of the practice’s patients with a malignancy.
These patient pages are rapidly accessible with OneNote’s search box. As each additional letter is entered, the search feature narrows the possible matches. Usually, entering the first couple of letters of the last name presents the desired match in the search window. I then click on the patient’s name and hit Print; the summary is produced faster than the time it would take to find the information in an alphabetized paper notebook.
The advantage of an electronic summary sheet is that it can be updated and printed at each visit. Electronic summary sheets can be designed in any format—eg, a main page with Problems, Medications, Medication Allergies, Social History, Family History, etc, and a second page with a Health Maintenance flow sheet, or whatever makes sense for the clinician’s practice.
With OneNote, tables, graphics, and text with various fonts can be placed anywhere on the page, as can elements created with drawing tools. Pages can be any size: 3x5 card, letter, legal, or endless (like a Web page). OneNote supports “copy and paste” and “drag and drop” from other programs, as well as hyperlinks to documents outside OneNote.
The user can easily design a variety of templates for use in each tab, simply by designing a page and designating a template. One template can be set as the default for that tab. For example, when I click New Page in the Summary tab, a new summary form appears in that section. Pages can be deleted, copied, or moved within and between sections, just as in a word processing program.
FIGURE 2
Summary sheet
Each patient has a page (identifying information at right is covered) that lists his or her chronic/acute problems, as well as malignancies. One can locate the proper page by typing the first few letters of the patient’s last name in the search field.
A second tab for prescriptions
I decided to add a second tab to my notebook: Prescriptions. I designed a prescription template and set that as my default New Page for the prescription section. I created a new page for each of my common prescriptions—eg, doxycycline, minocycline, various topical acne preparations. OneNote’s search function at the top of the pages section is nearly instantaneous and shows all possible matches for a string of characters. Entering “tre” will show all matches with “tretinoin. “ It’s easy, then, to select the preparation of interest, hit Print, and have a printed prescription in seconds. For even greater efficiency, I have created new prescription pages for multiple medications I often use in combination—eg, a morning antimicrobial and an evening retinoid for acne, or compounds such as magic mouthwash (FIGURE 3).
Our office check-in process includes producing printed sticky labels with a patient’s name and address and the current date, which we can affix to things like pictures and pathology slips. So I designed my prescription blank to accommodate such labels. I print prescriptions from my wireless notebook computer to a wireless printer. The nurse affixes a label, I sign the document, and in seconds the patient has a detailed, legible prescription. The only disadvantage with this system is that unlike iScribe, I cannot look up a patient’s prescription history electronically because there is no electronically filed copy saved with the patient’s name. One option would be to enter every patient on a page and put prescriptions as subpages under the patient’s page. But that is more work than I want to do in patient exam rooms during a visit. Instead, I print 2 copies of each prescription, one of which goes into the paper chart.
I populated my Prescriptions tab with my prescription “favorites” before going live. But this can also be done “on the fly. “ You simply enter a new prescription as the need arises. OneNote automatically saves the prescription for future use (unless it’s intentionally deleted).
To produce new prescriptions, I set the Prescription blank as the default template. I click New Page and a blank prescription form appears. So, let’s say that lidocaine gel is not in the prescriber. I search “lido, “ and the ointment and transdermal formulations that have already been entered come up. I click New Page, a blank prescription form appears, and I type the details of the prescription (lidocaine gel 2%, dispense 30 grams, apply 30 to 60 minutes before procedure, refill zero). This prescription is saved automatically and will be available the next time I search “lido. “ Alternatively, an existing prescription can be copied and easily modified, as in copying a “cream” prescription and changing to “ointment” in the copy so both are available for future use.
All sorts of variations are possible: “endocarditis prophylaxis” options could be entered as a list on one prescription form. Before the list is printed, the user could simply check the desired option for that patient. Because OneNote saves all changes automatically, any changes made to the default prescriptions (eg, choosing to give a medication once daily rather than the default of twice daily) are saved automatically. When I make any custom changes, I use the Undo button, which I placed on my Quick Access Toolbar, to easily return to my preferred default status.
FIGURE 3
Prescription page for multiple medications
Medications commonly used together can be combined on a single prescription form. Additional information may be included (and discussed in advance with patients), to reduce formulary callback and preauthorization issues. Alphabetizing the prescriptions is unnecessary, given that the robust search function matches even partial words.
A third tab for patient education
After the success with the Summary sheets and Prescriptions tabs, I added a Patient Ed tab (FIGURE 4). I use handouts liberally to reinforce discussions, to give directions for medication use (eg, retinoids, imiquimod, fluorouracil, permethrin, prednisone), and to educate patients about diseases (eg, dysplastic nevi, melanoma, scabies). Most of this information resides on my computer, and OneNote allows me to rapidly locate and print the documents. I copy the links to patient education files onto corresponding individual OneNote pages, organized by the handouts’ identifying key words.
For example, for the isotretinoin-inflammatory bowel disease information sheet, I created a page called “Isotretinoin - Inflammatory Bowel Disease” in the Patient Education tab. That page contains a hyperlink to the desired document on my computer. The original document can be updated as new information becomes available, and OneNote will always link to the current version. For less commonly used handouts, I can enter key title words in the search box, click on the appropriate page, and print the document.
Because the printer is in the hall 2 steps from each exam room, I can do that faster than the nurse can find these documents in our paper system. This is particularly useful if the information on the possible link between isotretinoin and inflammatory bowel disease is missing from our isotretinoin packet.
FIGURE 4
Patient education tab
OneNote can be used as an indexing aid for patient education materials by simply dragging and dropping into it the links to “original” patient education documents. By clicking on this link, one can go to the information that resides elsewhere, and print out the material for the patient.
Many advantages with this new system
With OneNote, I have elements of a mini-electronic record with summary sheets for patients with malignancies, prescription writing, and patient handouts. In addition, I will not lose this system in a corporate buyout or be charged exorbitant fees to transfer records. Tabs can be password protected for security, and all pages under a tab can be saved in Adobe Acrobat, Microsoft Word, and OneNote formats. Those features help assure security and portability. (This system does not, however, qualify users for government incentives, as it lacks certain functions that are available with a true EMR.)
True e-prescribing—which, for me, included entering patient demographics and offered electronic access to my prescribing history for each patient—is usually an intermediary step for those moving toward full EMR implementation. Using OneNote, I carry a laptop/notebook room to room and print a lot of patient information handouts that otherwise would have to be retrieved from elsewhere.
As a trial, I used the OneNote system along with iScribe’s replacement e-prescribing product for several weeks. My OneNote system was faster. Now, only when patients specifically request e-prescriptions do I use the iScribe replacement product, which, after the corporate merger, has been continued at no charge for 2 to 3 years for existing users. (E-prescribing for Medicare patients at least 25 times in 2011 will qualify users for the Medicare incentive bonus.)
Because the “computer” portion of patient encounters usually occurs at the end of the visit, it does not interfere with the patient-physician relationship. Additionally, my average patient has already been “teched” with a digital scale, digital blood pressure cuff, and digital camera, so a computer is probably one of the more familiar pieces in the technoscape.
OneNote has become a powerful ally in my clinical practice. I thought I had everything I needed with Word, Excel, and Acrobat. But I’m glad I opened OneNote out of curiosity. It’s not only helped me to modernize my patient “problem lists, “ but it’s proven to be the solution to my e-prescribing dilemma.
CORRESPONDENCE
Gary N. Fox, MD, Defiance Clinic, 1400 E. 2nd Street, Defiance, OH 43512; foxgary@yahoo.com
Even with government incentives, I physicians have been slow to make the leap to electronic medical records (EMR) and full electronic prescribing (e-prescribing). My transition to e-prescribing evolved over about a decade, and I was a satisfied e-prescriber—for a while.
Around 2000, I began writing electronic prescriptions using iScribe for Palm handhelds.1 The final transition to full e-prescribing required only a WiFi connection in the office for use with my Palm, and hitting Send to submit the prescription to the pharmacy. iScribe was user friendly and fast. It eliminated pharmacy “callbacks, “ provided printed receipts for charting, and maintained a record of each prescription on the Palm, filed under the patient’s name. A full prescription history for each patient archived on the Palm reduced the need to pull charts for medication questions.
A rude surprise
Then iScribe was acquired by another company whose e-prescribing product, in my opinion, lengthened patient encounters because it required several additional steps to complete a prescription. This was unacceptable to me, and returning to handwritten prescriptions was out of the question. I needed a better solution.
I was disinclined to invest in another e-prescribing product whose tenure could end as abruptly as iScribe’s had. To wit: I recently read about another user-friendly, well-supported medical software program that was scooped up by a larger company selling less functional and more expensive products (while charging for a costly conversion of existing records and delivering poorer customer service).2 And e-prescribing in general has received mixed reviews.3
I briefly considered designing my own prescription writer. A full-featured writer using a relational database, such as Microsoft Access, would be ideal. But developing it would be daunting without software-specific training. The same would be true for spreadsheet software. Adobe Acrobat or word processors with directories or hyperlinks or search functions didn’t seem appropriate.
A welcome surprise
Microsoft Office 2010 software for PC and Mac platforms now includes OneNote, a program new to me. (Price at Costco for Office Home and Student, September 2010, was $119.) OneNote (in which I have no vested interest) is an “electronic notebook” program—a digital version of the multisubject, tabbed binders we all used in school. The user creates tabs, which appear across the top of the notebook interface. Each tab can accommodate as many pages as the user desires, just as in the sections of a paper notebook (FIGURE 1). In OneNote, each page has a title, and the title appears on the page tab on the right side of the screen (left side is an option). Several layers of subpages are also available for each page, similar to subdirectories in a computerized filing system.
FIGURE 1
Tabbed sections
OneNote’s Tabs are visible across the top. Most of the pages on the right side are obscured in this view by the search results window.
First tab: Summary sheet of patient “problems”
Since 2005, my practice has been limited to skin disease and it has been my custom to create paper “problem lists” as a handy method of tracking each patient’s malignancy types, dates, and anatomic locations. I decided to make these lists electronic, using OneNote (FIGURE 2). OneNote allows default templates, whereby clicking on New Page creates a fully formatted page. I used the template to create a derm summary sheet tab. Under that, I created an electronic page for each of the practice’s patients with a malignancy.
These patient pages are rapidly accessible with OneNote’s search box. As each additional letter is entered, the search feature narrows the possible matches. Usually, entering the first couple of letters of the last name presents the desired match in the search window. I then click on the patient’s name and hit Print; the summary is produced faster than the time it would take to find the information in an alphabetized paper notebook.
The advantage of an electronic summary sheet is that it can be updated and printed at each visit. Electronic summary sheets can be designed in any format—eg, a main page with Problems, Medications, Medication Allergies, Social History, Family History, etc, and a second page with a Health Maintenance flow sheet, or whatever makes sense for the clinician’s practice.
With OneNote, tables, graphics, and text with various fonts can be placed anywhere on the page, as can elements created with drawing tools. Pages can be any size: 3x5 card, letter, legal, or endless (like a Web page). OneNote supports “copy and paste” and “drag and drop” from other programs, as well as hyperlinks to documents outside OneNote.
The user can easily design a variety of templates for use in each tab, simply by designing a page and designating a template. One template can be set as the default for that tab. For example, when I click New Page in the Summary tab, a new summary form appears in that section. Pages can be deleted, copied, or moved within and between sections, just as in a word processing program.
FIGURE 2
Summary sheet
Each patient has a page (identifying information at right is covered) that lists his or her chronic/acute problems, as well as malignancies. One can locate the proper page by typing the first few letters of the patient’s last name in the search field.
A second tab for prescriptions
I decided to add a second tab to my notebook: Prescriptions. I designed a prescription template and set that as my default New Page for the prescription section. I created a new page for each of my common prescriptions—eg, doxycycline, minocycline, various topical acne preparations. OneNote’s search function at the top of the pages section is nearly instantaneous and shows all possible matches for a string of characters. Entering “tre” will show all matches with “tretinoin. “ It’s easy, then, to select the preparation of interest, hit Print, and have a printed prescription in seconds. For even greater efficiency, I have created new prescription pages for multiple medications I often use in combination—eg, a morning antimicrobial and an evening retinoid for acne, or compounds such as magic mouthwash (FIGURE 3).
Our office check-in process includes producing printed sticky labels with a patient’s name and address and the current date, which we can affix to things like pictures and pathology slips. So I designed my prescription blank to accommodate such labels. I print prescriptions from my wireless notebook computer to a wireless printer. The nurse affixes a label, I sign the document, and in seconds the patient has a detailed, legible prescription. The only disadvantage with this system is that unlike iScribe, I cannot look up a patient’s prescription history electronically because there is no electronically filed copy saved with the patient’s name. One option would be to enter every patient on a page and put prescriptions as subpages under the patient’s page. But that is more work than I want to do in patient exam rooms during a visit. Instead, I print 2 copies of each prescription, one of which goes into the paper chart.
I populated my Prescriptions tab with my prescription “favorites” before going live. But this can also be done “on the fly. “ You simply enter a new prescription as the need arises. OneNote automatically saves the prescription for future use (unless it’s intentionally deleted).
To produce new prescriptions, I set the Prescription blank as the default template. I click New Page and a blank prescription form appears. So, let’s say that lidocaine gel is not in the prescriber. I search “lido, “ and the ointment and transdermal formulations that have already been entered come up. I click New Page, a blank prescription form appears, and I type the details of the prescription (lidocaine gel 2%, dispense 30 grams, apply 30 to 60 minutes before procedure, refill zero). This prescription is saved automatically and will be available the next time I search “lido. “ Alternatively, an existing prescription can be copied and easily modified, as in copying a “cream” prescription and changing to “ointment” in the copy so both are available for future use.
All sorts of variations are possible: “endocarditis prophylaxis” options could be entered as a list on one prescription form. Before the list is printed, the user could simply check the desired option for that patient. Because OneNote saves all changes automatically, any changes made to the default prescriptions (eg, choosing to give a medication once daily rather than the default of twice daily) are saved automatically. When I make any custom changes, I use the Undo button, which I placed on my Quick Access Toolbar, to easily return to my preferred default status.
FIGURE 3
Prescription page for multiple medications
Medications commonly used together can be combined on a single prescription form. Additional information may be included (and discussed in advance with patients), to reduce formulary callback and preauthorization issues. Alphabetizing the prescriptions is unnecessary, given that the robust search function matches even partial words.
A third tab for patient education
After the success with the Summary sheets and Prescriptions tabs, I added a Patient Ed tab (FIGURE 4). I use handouts liberally to reinforce discussions, to give directions for medication use (eg, retinoids, imiquimod, fluorouracil, permethrin, prednisone), and to educate patients about diseases (eg, dysplastic nevi, melanoma, scabies). Most of this information resides on my computer, and OneNote allows me to rapidly locate and print the documents. I copy the links to patient education files onto corresponding individual OneNote pages, organized by the handouts’ identifying key words.
For example, for the isotretinoin-inflammatory bowel disease information sheet, I created a page called “Isotretinoin - Inflammatory Bowel Disease” in the Patient Education tab. That page contains a hyperlink to the desired document on my computer. The original document can be updated as new information becomes available, and OneNote will always link to the current version. For less commonly used handouts, I can enter key title words in the search box, click on the appropriate page, and print the document.
Because the printer is in the hall 2 steps from each exam room, I can do that faster than the nurse can find these documents in our paper system. This is particularly useful if the information on the possible link between isotretinoin and inflammatory bowel disease is missing from our isotretinoin packet.
FIGURE 4
Patient education tab
OneNote can be used as an indexing aid for patient education materials by simply dragging and dropping into it the links to “original” patient education documents. By clicking on this link, one can go to the information that resides elsewhere, and print out the material for the patient.
Many advantages with this new system
With OneNote, I have elements of a mini-electronic record with summary sheets for patients with malignancies, prescription writing, and patient handouts. In addition, I will not lose this system in a corporate buyout or be charged exorbitant fees to transfer records. Tabs can be password protected for security, and all pages under a tab can be saved in Adobe Acrobat, Microsoft Word, and OneNote formats. Those features help assure security and portability. (This system does not, however, qualify users for government incentives, as it lacks certain functions that are available with a true EMR.)
True e-prescribing—which, for me, included entering patient demographics and offered electronic access to my prescribing history for each patient—is usually an intermediary step for those moving toward full EMR implementation. Using OneNote, I carry a laptop/notebook room to room and print a lot of patient information handouts that otherwise would have to be retrieved from elsewhere.
As a trial, I used the OneNote system along with iScribe’s replacement e-prescribing product for several weeks. My OneNote system was faster. Now, only when patients specifically request e-prescriptions do I use the iScribe replacement product, which, after the corporate merger, has been continued at no charge for 2 to 3 years for existing users. (E-prescribing for Medicare patients at least 25 times in 2011 will qualify users for the Medicare incentive bonus.)
Because the “computer” portion of patient encounters usually occurs at the end of the visit, it does not interfere with the patient-physician relationship. Additionally, my average patient has already been “teched” with a digital scale, digital blood pressure cuff, and digital camera, so a computer is probably one of the more familiar pieces in the technoscape.
OneNote has become a powerful ally in my clinical practice. I thought I had everything I needed with Word, Excel, and Acrobat. But I’m glad I opened OneNote out of curiosity. It’s not only helped me to modernize my patient “problem lists, “ but it’s proven to be the solution to my e-prescribing dilemma.
CORRESPONDENCE
Gary N. Fox, MD, Defiance Clinic, 1400 E. 2nd Street, Defiance, OH 43512; foxgary@yahoo.com
1. Fox GN. Electronic prescribing: drug dealing twenty-first century style. In: Strayer SM, Reynolds PL, Ebell MH, eds. Handhelds in Medicine: A Practical Guide for Clinicians. New York, NY: Springer; 2005.
2. Levine N. Before implementing EMRs, heed words of warning. Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/Before-implementing-EMRs-heedwords-of-warning/ArticleStandard/Article/detail/666763. Accessed May 28, 2010.
3. Nash K. E-prescribing: a boon or a bane to dermatology practices? Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/E-prescribing-a-boon-or-a-bane-to-dermatology-prac/ArticleStandard/Article/detail/666779. Accessed May 28, 2010.
1. Fox GN. Electronic prescribing: drug dealing twenty-first century style. In: Strayer SM, Reynolds PL, Ebell MH, eds. Handhelds in Medicine: A Practical Guide for Clinicians. New York, NY: Springer; 2005.
2. Levine N. Before implementing EMRs, heed words of warning. Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/Before-implementing-EMRs-heedwords-of-warning/ArticleStandard/Article/detail/666763. Accessed May 28, 2010.
3. Nash K. E-prescribing: a boon or a bane to dermatology practices? Dermatology Times. May 2010. Available at: http://www.modernmedicine.com/modernmedicine/Modern+Medicine+Now/E-prescribing-a-boon-or-a-bane-to-dermatology-prac/ArticleStandard/Article/detail/666779. Accessed May 28, 2010.
An aid for spotting basal cell carcinoma
Basal cell carcinoma (BCC) is the most common skin malignancy, but it can still be a tricky and difficult diagnosis even in the most experienced hands. Many BCCs exhibit only some of the defining clinical characteristics, and even when these findings are present, they can be hard to detect without excellent background and oblique lighting and handheld magnification that is 5-power or greater.
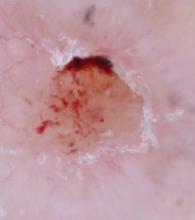
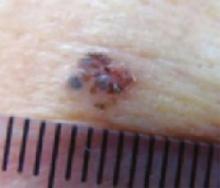
Most clinicians are familiar with classic BCC characteristics of pearliness, rolled edges, telangiectasia, bleeding, and crusting. However, the telangiectasias may be so fine that they are difficult or impossible to see, even with excellent lighting and magnification. FIGURE 1A illustrates a histologically verified nodular BCC with telangiectasias that are not readily visible, even with camera macro magnification.
Some BCC papules or plaques lack the classic rolled edges, even when viewed with oblique lighting and magnification. Some lesions may be more scaly than pearly, and others do not bleed and crust until later in their clinical course. With such variation in clinical presentation, all possible clues to BCC are welcome.
Dark dots: Connecting them to BCC
One underappreciated sign that may help with the diagnosis of BCC is the “dark dot sign.”1,2 Dermoscopists are familiar with patterns of pigmentation associated with BCCs, and introductory dermoscopy texts contain pictures of these patterns (blue/blue-gray blotches, maple leaf structures, and spoke-wheel structures).3,4 What is less well known is that this pigmentation may be visible on routine skin examination as “dark dots”—blue, gray, black, or a combination thereof, such as blue-gray. When visible clinically, these dark dots may bolster one’s confidence in the diagnosis—or, in my experience, occasionally even be the best visible hint for a tentative diagnosis of BCC.
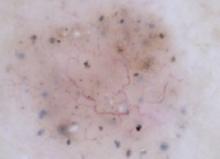
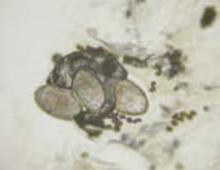
Case in point. During a routine skin examination of a patient’s back, I identified an asymptomatic lesion the patient was unaware of, exhibiting no bleeding or crusting. It drew attention because it was different from surrounding lesions (FIGURE 2A), which has been called the “ugly duckling sign.”5 On closer examination, I noted the lesion had a pearly sheen, telangiectasias, and a plethora of dark dots (FIGURE 2B)—the poster child for the “dark dot sign.” Unlike this profound example, most lesions that have dark dots have just one or a few visible dots.
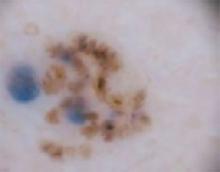
Now review FIGURE 1A again carefully. Above the lesion’s central crater there is an arcuate hemorrhagic crust, and, between the 12 and 1 o’clock positions, a small dark dot, which helps corroborate the clinical impression of BCC. FIGURE 1B is a dermoscopic image of the same lesion. It shows the dark dot well and illustrates the ease with which telangiectasias are seen on dermoscopy, lending a high degree of certainty to the diagnosis of BCC.
Dermoscopy (FIGURE 2C) for the lesion on the patient’s back in FIGURE 2B, however, adds nothing (beyond magnification) because telangiectasias and dark dots were visible clinically.
CASE #1
FIGURE 1A
Basal cell carcinoma. Even with photography, which is often clearer than magnified clinical inspection, telangiectasias are not well seen in this basal cell carcinoma. A dark dot, however, is visible between the 12 and 1 o’clock positions.
FIGURE 1B
A dermoscopic view of the BCC in FIGURE 1A clearly shows telangiectasias and a dark dot.
CASE #2
FIGURE 2A
Ugly duckling sign. The circled lesion on this patient’s back wasn’t crusty or bleeding, but it drew attention because it was different from surrounding lesions. This has been called the “ugly duckling sign.”
FIGURE 2B
Dark dots. A closer look at the lesion on the patient’s back revealed multiple dark dots and telangiectasias, virtually diagnostic of basal cell carcinoma.
FIGURE 2C
A dermoscopic view of the lesion in FIGURE 2B adds little to what was well visualized clinically.
Caution: Context is critical
Because dots or blotches of pigment may occur in squamous cell carcinoma, pigmented actinic keratoses, seborrheic keratoses, and hypomelanotic or “amelanotic” melanoma, it is not possible clinically to confirm a diagnosis of BCC solely on the basis of dark dots. (In fact, even in the absence of pigment, any “red and white” lesion could be an amelanotic melanoma.) However, when added to other findings, such as a firm, pearly papule, the finding increases the likelihood of BCC.
How to proceed to biopsy
Lesions such as the ones I’ve shown should never be treated without preserving a specimen for pathology examination (eg, directly frozen). That said, there is no one right biopsy technique. The choice will depend on your clinical suspicion and perhaps other factors in your patient’s circumstance.
If you believe the lesion could be a cutaneous melanoma, the ideal option is full excision (to reduce sampling error pathologically), with a narrow margin (to preserve lymphatics, should sentinel node biopsy be considered later) and full thickness (to subcutaneous fat for prognostic staging; remember the dermis on the back is very thick). If you are confident the lesion is BCC, an initial shave biopsy preserves the option for treatment via curettage should the histology reveal superficial or nodular BCC. Pathology findings that indicate infiltrative, morpheaform, or micronodular BCC require excision; curettage is not adequate treatment for these lesions.
Treating the 2 patients
The patient in FIGURE 1A had no symptoms and no history of skin cancer. Because he was skeptical of the diagnosis, I performed a shave biopsy for histologic verification. The pathology report confirmed nodular BCC. We discussed options, and the patient elected excision.
In the case of the second lesion (FIGURE 2B), the diagnosis of BCC was fairly certain. Because of the patient’s advanced age, declining health, and difficulty arranging transportation, we decided to perform a primary excision at the outset. Had histology shown BCC with micronodular architecture or infitrative features, a shave biopsy for diagnosis, plus curettage, would not have been ideal treatment. Histology showed a nodular BCC.
Acknowledgements
The author thanks the St. Vincent Mercy Medical Center (Toledo) staff for its expert assistance.
Correspondence
Gary N. Fox, MD, Defiance Clinic, 1400 E 2nd Street, Defiance, OH 43512; foxgary@yahoo.com
1. Goldberg LH, Friedman RH, Silapunt S. Pigmented speckling as a sign of basal cell carcinoma. Dermatol Surg. 2004;30:1553-1555.
2. Bates B. A black dot appears to flag early basal cell carcinoma. Family Practice News. 2006;36(11):38.-Available at: http://www.familypracticenews.com/article/PIIS0300707306733047/fulltext. Accessed December 4, 2008.
3. Johr R, Soyer HP, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy: The Essentials. New York: Mosby; 2004:107-117, 157.
4. Polsky D. Non-melanocytic lesions: pigmented basal cell carcinoma [Chapter 6a]. In: Marghoob AA, Braun RP, Kopf AW, eds. Atlas of Dermoscopy. New York: Taylor & Francis; 2005:55-59.
5. Grob JJ, Bonerandi JJ. The ‘ugly duckling’ sign: identification of the common characteristics of nevi in an individual as a basis for melanoma screening. Arch Dermatol. 1998;134:103-104.
Basal cell carcinoma (BCC) is the most common skin malignancy, but it can still be a tricky and difficult diagnosis even in the most experienced hands. Many BCCs exhibit only some of the defining clinical characteristics, and even when these findings are present, they can be hard to detect without excellent background and oblique lighting and handheld magnification that is 5-power or greater.
Most clinicians are familiar with classic BCC characteristics of pearliness, rolled edges, telangiectasia, bleeding, and crusting. However, the telangiectasias may be so fine that they are difficult or impossible to see, even with excellent lighting and magnification. FIGURE 1A illustrates a histologically verified nodular BCC with telangiectasias that are not readily visible, even with camera macro magnification.
Some BCC papules or plaques lack the classic rolled edges, even when viewed with oblique lighting and magnification. Some lesions may be more scaly than pearly, and others do not bleed and crust until later in their clinical course. With such variation in clinical presentation, all possible clues to BCC are welcome.
Dark dots: Connecting them to BCC
One underappreciated sign that may help with the diagnosis of BCC is the “dark dot sign.”1,2 Dermoscopists are familiar with patterns of pigmentation associated with BCCs, and introductory dermoscopy texts contain pictures of these patterns (blue/blue-gray blotches, maple leaf structures, and spoke-wheel structures).3,4 What is less well known is that this pigmentation may be visible on routine skin examination as “dark dots”—blue, gray, black, or a combination thereof, such as blue-gray. When visible clinically, these dark dots may bolster one’s confidence in the diagnosis—or, in my experience, occasionally even be the best visible hint for a tentative diagnosis of BCC.
Case in point. During a routine skin examination of a patient’s back, I identified an asymptomatic lesion the patient was unaware of, exhibiting no bleeding or crusting. It drew attention because it was different from surrounding lesions (FIGURE 2A), which has been called the “ugly duckling sign.”5 On closer examination, I noted the lesion had a pearly sheen, telangiectasias, and a plethora of dark dots (FIGURE 2B)—the poster child for the “dark dot sign.” Unlike this profound example, most lesions that have dark dots have just one or a few visible dots.
Now review FIGURE 1A again carefully. Above the lesion’s central crater there is an arcuate hemorrhagic crust, and, between the 12 and 1 o’clock positions, a small dark dot, which helps corroborate the clinical impression of BCC. FIGURE 1B is a dermoscopic image of the same lesion. It shows the dark dot well and illustrates the ease with which telangiectasias are seen on dermoscopy, lending a high degree of certainty to the diagnosis of BCC.
Dermoscopy (FIGURE 2C) for the lesion on the patient’s back in FIGURE 2B, however, adds nothing (beyond magnification) because telangiectasias and dark dots were visible clinically.
CASE #1
FIGURE 1A
Basal cell carcinoma. Even with photography, which is often clearer than magnified clinical inspection, telangiectasias are not well seen in this basal cell carcinoma. A dark dot, however, is visible between the 12 and 1 o’clock positions.
FIGURE 1B
A dermoscopic view of the BCC in FIGURE 1A clearly shows telangiectasias and a dark dot.
CASE #2
FIGURE 2A
Ugly duckling sign. The circled lesion on this patient’s back wasn’t crusty or bleeding, but it drew attention because it was different from surrounding lesions. This has been called the “ugly duckling sign.”
FIGURE 2B
Dark dots. A closer look at the lesion on the patient’s back revealed multiple dark dots and telangiectasias, virtually diagnostic of basal cell carcinoma.
FIGURE 2C
A dermoscopic view of the lesion in FIGURE 2B adds little to what was well visualized clinically.
Caution: Context is critical
Because dots or blotches of pigment may occur in squamous cell carcinoma, pigmented actinic keratoses, seborrheic keratoses, and hypomelanotic or “amelanotic” melanoma, it is not possible clinically to confirm a diagnosis of BCC solely on the basis of dark dots. (In fact, even in the absence of pigment, any “red and white” lesion could be an amelanotic melanoma.) However, when added to other findings, such as a firm, pearly papule, the finding increases the likelihood of BCC.
How to proceed to biopsy
Lesions such as the ones I’ve shown should never be treated without preserving a specimen for pathology examination (eg, directly frozen). That said, there is no one right biopsy technique. The choice will depend on your clinical suspicion and perhaps other factors in your patient’s circumstance.
If you believe the lesion could be a cutaneous melanoma, the ideal option is full excision (to reduce sampling error pathologically), with a narrow margin (to preserve lymphatics, should sentinel node biopsy be considered later) and full thickness (to subcutaneous fat for prognostic staging; remember the dermis on the back is very thick). If you are confident the lesion is BCC, an initial shave biopsy preserves the option for treatment via curettage should the histology reveal superficial or nodular BCC. Pathology findings that indicate infiltrative, morpheaform, or micronodular BCC require excision; curettage is not adequate treatment for these lesions.
Treating the 2 patients
The patient in FIGURE 1A had no symptoms and no history of skin cancer. Because he was skeptical of the diagnosis, I performed a shave biopsy for histologic verification. The pathology report confirmed nodular BCC. We discussed options, and the patient elected excision.
In the case of the second lesion (FIGURE 2B), the diagnosis of BCC was fairly certain. Because of the patient’s advanced age, declining health, and difficulty arranging transportation, we decided to perform a primary excision at the outset. Had histology shown BCC with micronodular architecture or infitrative features, a shave biopsy for diagnosis, plus curettage, would not have been ideal treatment. Histology showed a nodular BCC.
Acknowledgements
The author thanks the St. Vincent Mercy Medical Center (Toledo) staff for its expert assistance.
Correspondence
Gary N. Fox, MD, Defiance Clinic, 1400 E 2nd Street, Defiance, OH 43512; foxgary@yahoo.com
Basal cell carcinoma (BCC) is the most common skin malignancy, but it can still be a tricky and difficult diagnosis even in the most experienced hands. Many BCCs exhibit only some of the defining clinical characteristics, and even when these findings are present, they can be hard to detect without excellent background and oblique lighting and handheld magnification that is 5-power or greater.
Most clinicians are familiar with classic BCC characteristics of pearliness, rolled edges, telangiectasia, bleeding, and crusting. However, the telangiectasias may be so fine that they are difficult or impossible to see, even with excellent lighting and magnification. FIGURE 1A illustrates a histologically verified nodular BCC with telangiectasias that are not readily visible, even with camera macro magnification.
Some BCC papules or plaques lack the classic rolled edges, even when viewed with oblique lighting and magnification. Some lesions may be more scaly than pearly, and others do not bleed and crust until later in their clinical course. With such variation in clinical presentation, all possible clues to BCC are welcome.
Dark dots: Connecting them to BCC
One underappreciated sign that may help with the diagnosis of BCC is the “dark dot sign.”1,2 Dermoscopists are familiar with patterns of pigmentation associated with BCCs, and introductory dermoscopy texts contain pictures of these patterns (blue/blue-gray blotches, maple leaf structures, and spoke-wheel structures).3,4 What is less well known is that this pigmentation may be visible on routine skin examination as “dark dots”—blue, gray, black, or a combination thereof, such as blue-gray. When visible clinically, these dark dots may bolster one’s confidence in the diagnosis—or, in my experience, occasionally even be the best visible hint for a tentative diagnosis of BCC.
Case in point. During a routine skin examination of a patient’s back, I identified an asymptomatic lesion the patient was unaware of, exhibiting no bleeding or crusting. It drew attention because it was different from surrounding lesions (FIGURE 2A), which has been called the “ugly duckling sign.”5 On closer examination, I noted the lesion had a pearly sheen, telangiectasias, and a plethora of dark dots (FIGURE 2B)—the poster child for the “dark dot sign.” Unlike this profound example, most lesions that have dark dots have just one or a few visible dots.
Now review FIGURE 1A again carefully. Above the lesion’s central crater there is an arcuate hemorrhagic crust, and, between the 12 and 1 o’clock positions, a small dark dot, which helps corroborate the clinical impression of BCC. FIGURE 1B is a dermoscopic image of the same lesion. It shows the dark dot well and illustrates the ease with which telangiectasias are seen on dermoscopy, lending a high degree of certainty to the diagnosis of BCC.
Dermoscopy (FIGURE 2C) for the lesion on the patient’s back in FIGURE 2B, however, adds nothing (beyond magnification) because telangiectasias and dark dots were visible clinically.
CASE #1
FIGURE 1A
Basal cell carcinoma. Even with photography, which is often clearer than magnified clinical inspection, telangiectasias are not well seen in this basal cell carcinoma. A dark dot, however, is visible between the 12 and 1 o’clock positions.
FIGURE 1B
A dermoscopic view of the BCC in FIGURE 1A clearly shows telangiectasias and a dark dot.
CASE #2
FIGURE 2A
Ugly duckling sign. The circled lesion on this patient’s back wasn’t crusty or bleeding, but it drew attention because it was different from surrounding lesions. This has been called the “ugly duckling sign.”
FIGURE 2B
Dark dots. A closer look at the lesion on the patient’s back revealed multiple dark dots and telangiectasias, virtually diagnostic of basal cell carcinoma.
FIGURE 2C
A dermoscopic view of the lesion in FIGURE 2B adds little to what was well visualized clinically.
Caution: Context is critical
Because dots or blotches of pigment may occur in squamous cell carcinoma, pigmented actinic keratoses, seborrheic keratoses, and hypomelanotic or “amelanotic” melanoma, it is not possible clinically to confirm a diagnosis of BCC solely on the basis of dark dots. (In fact, even in the absence of pigment, any “red and white” lesion could be an amelanotic melanoma.) However, when added to other findings, such as a firm, pearly papule, the finding increases the likelihood of BCC.
How to proceed to biopsy
Lesions such as the ones I’ve shown should never be treated without preserving a specimen for pathology examination (eg, directly frozen). That said, there is no one right biopsy technique. The choice will depend on your clinical suspicion and perhaps other factors in your patient’s circumstance.
If you believe the lesion could be a cutaneous melanoma, the ideal option is full excision (to reduce sampling error pathologically), with a narrow margin (to preserve lymphatics, should sentinel node biopsy be considered later) and full thickness (to subcutaneous fat for prognostic staging; remember the dermis on the back is very thick). If you are confident the lesion is BCC, an initial shave biopsy preserves the option for treatment via curettage should the histology reveal superficial or nodular BCC. Pathology findings that indicate infiltrative, morpheaform, or micronodular BCC require excision; curettage is not adequate treatment for these lesions.
Treating the 2 patients
The patient in FIGURE 1A had no symptoms and no history of skin cancer. Because he was skeptical of the diagnosis, I performed a shave biopsy for histologic verification. The pathology report confirmed nodular BCC. We discussed options, and the patient elected excision.
In the case of the second lesion (FIGURE 2B), the diagnosis of BCC was fairly certain. Because of the patient’s advanced age, declining health, and difficulty arranging transportation, we decided to perform a primary excision at the outset. Had histology shown BCC with micronodular architecture or infitrative features, a shave biopsy for diagnosis, plus curettage, would not have been ideal treatment. Histology showed a nodular BCC.
Acknowledgements
The author thanks the St. Vincent Mercy Medical Center (Toledo) staff for its expert assistance.
Correspondence
Gary N. Fox, MD, Defiance Clinic, 1400 E 2nd Street, Defiance, OH 43512; foxgary@yahoo.com
1. Goldberg LH, Friedman RH, Silapunt S. Pigmented speckling as a sign of basal cell carcinoma. Dermatol Surg. 2004;30:1553-1555.
2. Bates B. A black dot appears to flag early basal cell carcinoma. Family Practice News. 2006;36(11):38.-Available at: http://www.familypracticenews.com/article/PIIS0300707306733047/fulltext. Accessed December 4, 2008.
3. Johr R, Soyer HP, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy: The Essentials. New York: Mosby; 2004:107-117, 157.
4. Polsky D. Non-melanocytic lesions: pigmented basal cell carcinoma [Chapter 6a]. In: Marghoob AA, Braun RP, Kopf AW, eds. Atlas of Dermoscopy. New York: Taylor & Francis; 2005:55-59.
5. Grob JJ, Bonerandi JJ. The ‘ugly duckling’ sign: identification of the common characteristics of nevi in an individual as a basis for melanoma screening. Arch Dermatol. 1998;134:103-104.
1. Goldberg LH, Friedman RH, Silapunt S. Pigmented speckling as a sign of basal cell carcinoma. Dermatol Surg. 2004;30:1553-1555.
2. Bates B. A black dot appears to flag early basal cell carcinoma. Family Practice News. 2006;36(11):38.-Available at: http://www.familypracticenews.com/article/PIIS0300707306733047/fulltext. Accessed December 4, 2008.
3. Johr R, Soyer HP, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy: The Essentials. New York: Mosby; 2004:107-117, 157.
4. Polsky D. Non-melanocytic lesions: pigmented basal cell carcinoma [Chapter 6a]. In: Marghoob AA, Braun RP, Kopf AW, eds. Atlas of Dermoscopy. New York: Taylor & Francis; 2005:55-59.
5. Grob JJ, Bonerandi JJ. The ‘ugly duckling’ sign: identification of the common characteristics of nevi in an individual as a basis for melanoma screening. Arch Dermatol. 1998;134:103-104.
10 derm mistakes you don’t want to make
I’ve seen my share of missed diagnoses over the years while caring for patients who, through physician- or self-referral, have made their way to our multi-specialty group practice where I focus solely on skin.
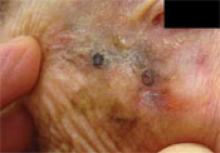
There was the 93-year-old patient whose “sun spot” had been evaluated and treated by 2 different dermatologists in the past and turned out to be a lentigo maligna melanoma (FIGURE 1).
There was the patient who had a lesion on her lip for “at least 10—maybe 20—years” that neither caught the attention of her physician, nor her dentist (FIGURE 2). Histology showed she had an infiltrative basal cell carcinoma.
And then there was the wife of a healthcare professional who decided she wanted a “second opinion” for the asymptomatic lesion on her leg that her husband assured her was benign. Her diagnosis was not so simple: She had a MELanocytic Tumor of Unknown Malignant Potential (MELTUMP) that required careful follow-up (FIGURE 3).
Early detection, as we all know, is the name of the game when it comes to skin malignancies. Yet every day, opportunities to catch small, early lesions are missed.
During the past couple of years, I’ve had thousands of patient visits for skin problems and diagnosed more than 1000 skin malignancies. The majority of patients have had some treatment for their presenting dermatosis prior to arrival. Based on my experiences with these patients, I’ve developed a list of common dermatology “mistakes.” Here they are, with some tips for avoiding them.
FIGURE 1
Melanoma missed by 2 dermatologists
This “sun spot” was of no concern to the 93-year-old patient because she had been evaluated and treated by 2 different dermatologists. The darkest areas are dermoscopically-directed pen markings for incisional biopsy. (The size of the lesion and proximity to the eye precluded primary excisional biopsy.) This “sun spot” turned out to be lentigo maligna melanoma.
FIGURE 2
Lesion on lip for “10—maybe 20—years”
This patient had a lesion that had been on her lip for “at least 10—maybe 20—years.” The patient said it had never bled or crusted. Telangiectasia, pearliness, and some infiltration were present. Histologic diagnosis: infiltrative basal cell carcinoma.
FIGURE 3
A case of MELTUMP
Two dermatopathologists read the biopsy as Spitzoid malignant melanoma, Clark Level III, and Breslow thickness 0.9 mm. Two independent dermatopathologists read the same original slides in consultation as atypical Spitz nevus. The 4 could not reach agreement. Final clinical diagnosis: MEL anocytic Tumor of Unknown Malignant Potential (MELTUMP).
Mistake #1: Not looking (and not biopsying)
I had a woman come into the office to have a lesion assessed. She had seen a dermatologist a couple of weeks earlier and even had a number of lesions removed during that visit. The patient told me that she’d repeatedly tried to show the dermatologist one specific lesion—the one of greatest concern to her—just below her underpants line, but the physician was in and out so fast each time, she never had the chance to point out this one melanocytic, changing lesion.
The lesion turned out to be a dysplastic nevus with severe architectural and cytologic atypia. This type of lesion requires histology to differentiate it from melanoma, and could just as easily have been a melanoma.
Almost daily I treat patients who are being seen by their primary care physicians regularly, and have obvious basal cell carcinomas (BCC) or squamous cell carcinomas. I have even found skin malignancies on physicians, their spouses, and their family members.1 These lesions can be easily missed—if you don’t look carefully.
Consider, the following:
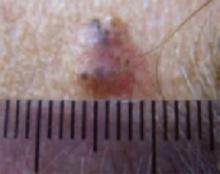
- FIGURE 4 illustrates a superficial BCC on the forearm of a physician who was totally unaware of it. (It was detected on “routine” skin examination.)
- FIGURE 5 illustrates a BCC on a patient’s central forehead that, by her history, had been there for many years, and was not of any concern to her. The patient was referred to our office for evaluation of itchy skin on her legs.
- FIGURE 2 illustrates a lesion that, according to the patient, had been on her lip for at least 10—and perhaps even 20—years and was of no concern to her. (It was not the reason for the visit.) Over the years, this patient certainly had numerous primary care and dental visits, but no one “saw” the lesion. Histology confirmed the clinical impression of BCC.
FIGURE 4
Superficial BCC on physician’s forearm
A physician asked for a skin examination, but was totally unaware of this asymptomatic lesion on his dorsal forearm. Once it was identified, he could provide no history about its duration. The lesion had never bled or crusted. Pathology confirmed that it was a superficial basal cell carcinoma.
FIGURE 5
“Mole” on forehead for many years
This patient was referred for itchy legs. She was unconcerned about a prominent “mole” noted on examination of her forehead, one that she said had been there, unchanged, for many years. Histology confirmed nodular basal cell carcinoma.
- Look, look, and look again, especially at sun-exposed areas (faces, ears, scalps [as hair thins], and dorsal forearms).
- Make sure patients are appropriately gowned no matter what the reason for their visit. Listening to heart and lung sounds and palpating abdomens through overcoats may work for some physicians, but not those interested in finding asymptomatic basal cell carcinomas, actinic keratoses, dysplastic nevi, and melanomas. Melanoma in men is most common on the back; in women, it’s most common on the legs. Seeing these areas requires that they be accessible.
- Biopsy when you’re in doubt. If you see a lesion and it is not recognizable as benign (eg, cherry angioma, seborrheic keratosis, nevus), biopsy it. Let the pathologist determine if it’s benign or malignant. If the lesion is questionable and is in an area that you are uncomfortable biopsying, refer the patient for evaluation and potential biopsy.
Mistake #2: Using insufficient light
As a former family practice academic, I used to preach to residents that they needed to use “light, light, and more light” for evaluation of skin lesions. Despite this, I was often asked to evaluate a patient with a resident who hadn’t even bothered to turn on a goose-neck lamp for illumination.
Even with my current “double bank” daylight fluorescent examination room lighting, it often takes additional (surgical-type) lighting to see the diagnostic features of skin lesions. Without such intense light, it is often impossible to see whether there is pearliness, rolled edges, or fine telangiectasia.
- Use whatever intense source of light you have, whether it’s a goose-neck lamp, a halogen, or a surgical light. If you don’t have at least a portable source of bright light, you are under-equipped for a good skin exam.
Mistake #3: Using insufficient (or no) magnification
I was once examining a patient in a hospital room that had inadequate light, despite my best efforts. So I took out my digital camera with flash and autofocus feature and photographed the lesion. I then looked at the lesion on the camera’s LCD monitor and determined that it was a BCC.
The benefit of the camera was 2-fold: Not only did the flash serve as an instant source of light, but the macro feature also provided magnification. Viewing a magnified digital image on a computer screen also allows unhurried, self “second opinions,” where details can often be ascertained that were not immediately apparent in “real time,” such as rolled edges, telangiectasia, dots, streaks, and subtleties of color.
- Use a hand-held magnifying lens (5X to 10X) routinely during skin exams. They’re not expensive and should be part of every primary care physician’s armamentarium—just like stethoscopes, ophthalmoscopes, and reflex hammers.
- Use a digital camera to provide the magnification needed to see details that can be missed clinically. I’m convinced that using a digital camera has made me a better observer—and clinician. Additionally, digital photographs can be stored and compared with histologic results as “self-education.” When purchasing a camera for this purpose, make sure it has a good close-up (macro) feature.
Mistake #4: Assuming that pathology is a perfect science
Most physicians assume that dermatopathologists have a high rate of interrater concordance with diagnoses such as melanoma. Unfortunately, that is not always the case. Consider the following:
- As part of a National Institutes of Health consensus conference on melanoma, 8 dermatopathologists considered experts in melanoma were asked to provide 5 slides each. The slides were relabeled and sent to the same 8 dermatopathologists. (Three slides were eliminated.) Their findings: At the extremes, 1 pathologist called 21 cases melanoma and 16 benign, whereas another called 10 melanoma, 26 benign, and one indeterminate.2 (Remember: These were all experts in melanoma.)
- In a study of 30 melanocytic lesion specimens (including Spitzoid lesions), 10 Harvard dermatopathologists evaluated each sample independently of each other. Given 5 diagnostic categories to choose from, in only one case did as many as 6 of the 10 agree on a diagnosis. In all of these cases, there was long-term clinical follow-up, so the biologic behavior of these lesions was known. Some lesions that proved fatal were categorized by most observers as benign (eg, Spitz nevi or atypical Spitz tumors). The converse, reporting benign lesions as melanoma, also occurred.3
So consider this: If this degree of discordance occurs among dermatopathologists, what results could we expect from non-dermatopathologists?
I have personally seen instances where reports of melanoma from non-dermatopathologists did not even report Clark and Breslow staging information (although one could determine Clark staging from reading the body of the report), and reports of dysplastic nevi that were accompanied by recommendations for re-excision with 1 cm margins.
When I have a report from a general pathologist suggesting a potentially worrisome lesion (melanoma, severely dysplastic nevus, [atypical] Spitz nevus), I always suggest to my patients that we get a dermatopathologic second opinion. (I send all my dermatopathology specimens to dermatopathologists, so this applies to patients referred in with prior pathology in hand.)
Sometimes, even the dermatopathologists do not agree on the nature of the lesion. In such cases, I have my “MELTUMP discussion” with patients. That is, I tell patients that we don’t know for sure what it is, and that ultimately only the final lab test—time—will tell us the true nature of the lesion (FIGURE 3).4
- Send all “skin” to a dermatopathologist. You owe it to your patients.
- Send pictures (electronic or hard copy) to the dermatopathologist when the pathology report and clinical picture do not appear to match. While pictures of skin lesions and dermoscopic photographs would most likely be meaningless to general pathologists, they are useful to dermatopathologists. Research has shown that pathologists in various areas of medicine may alter their diagnosis or differential diagnosis when presented with additional clinical information.5
Mistake #5: Freezing neoplasms without a definitive Dx
“We’ll freeze it and if it doesn’t go away, then…”
This approach poses a significant risk to you (medicolegally) and your patient.
While most of the time what I see has been inappropriately frozen first by first-line providers, that is not always the case. Dermatologists also fall into this trap. FIGURE 6 shows a lesion just behind the hairline on the frontoparietal scalp that was frozen by a very good, and reputable, dermatologist. The patient came to me for a second opinion with an “obvious” BCC.
Some clinicians are “thrown off” when a lesion (like the one on this patient) has hair. Some sources6 indicate that BCCs never have hair, but this is patently untrue.
FIGURE 6
This shouldn’t have been frozen
A dermatologist froze this lesion on a patient’s scalp, believing that it was seborrheic keratosis, based on the patient’s history. The patient sought a second opinion, and the lesion (which had hair) was histologically identified as basal cell carcinoma.
- Don’t freeze a lesion when you are unsure; biopsy it. This is especially critical when you consider that cryotherapy is not considered a first-line treatment for BCC, the most common human malignancy. It is better to biopsy, assure the diagnosis, and then provide the appropriate therapy.
Mistake #6: Treating psoriasis with systemic corticosteroids
Plaque psoriasis can, albeit uncommonly, be transformed to pustular psoriasis after the administration of oral or injectable systemic corticosteroids.7 Although this rarely occurs, most experts consider this poor practice and not worth the risk. In addition, some experts note that systemic glucocorticoids are a drug trigger for inducing or exacerbating psoriasis.8
- Avoid systemic corticosteroids in psoriasis, since psoriasis is generally a long-term disease and systemic corticosteroids are a short-term fix. if there is widespread psoriasis and you are not familiar with systemic treatments, refer the patient. If there is localized disease, consider topical treatment options—such as various strengths of corticosteroids, calcipotriene, and tazarotene (individually or in combination)—depending on location and plaque thickness.
Mistake #7: Doing shave biopsies on melanocytic lesions
For a melanoma, not only can shaving part way through the vertical dimension of the lesion interfere with staging, it can also hinder the pathologist’s ability to arrive at the correct diagnosis.9
- Do a full-thickness, narrow-margin, fully excisional biopsy when you suspect melanoma. Certainly, there are individuals who are expert at saucerization (deep shave biopsies, often with scalloped, sloping edges that go to the deep reticular dermis) and who can perform biopsies of melanocytic lesions while still obtaining reasonable pathologic staging information.
Mistake #8: Using corticosteroid/antifungal combination products
Corticosteroid/antifungal combination products are generally shunned by dermatologists, although they are used extensively by nondermatologists.9 The difficulty with a preparation like Lotrisone, which contains a class III corticosteroid (betamethasone dipropionate [Diprosone]) and the antifungal clotrimazole, is that it is often used long-term for presumed fungal infection on thin-skinned areas. Unfortunately, though, chronic use in these areas can lead to atrophy and striae (FIGURE 7).
Additionally, corticosteroid is essentially “fungus food.” Majocchi’s granulomas can form because the corticosteroid interferes with clotrimazole’s antifungal effect. Note also that these combination products can suppress fungus sufficiently to render cultures and KOH preparations falsely negative and alter the clinical appearance of psoriasiform dermatitis, interfering with subsequent, accurate diagnosis.
FIGURE 7
Striae after corticosteroid combination therapy
This patient developed striae and atrophy after using a combination high-potency topical corticosteroid/antifungal preparation in a thin-skinned area (proximal medial thigh). It was unclear what the prescriber was treating.
- Consider compounding with miconazole powder and hydrocortisone powder, if a corticosteroid/antifungal combination is necessary (which it rarely is). For example, hydrocortisone 1% or 0.5% ointment can be compounded with miconazole powder for short-term, careful external application, in cases of angular cheilitis.
- Limit your use of a topical corticosteroid for a fungal eruption (if one must be used) to the first few days of treatment. The corticosteroid class should be appropriate to the site of application.9
- Counsel your patients about the risks of using topical corticosteroids on thinskinned areas for more than a few days (few weeks, maximum). On the face, corticosteroids can cause rosacea and perioral dermatitis, as well as “rebound” vasodilation. Thus, topical corticosteroids should be used with great caution—and generally as a last resort—for chronic facial dermatoses.
Mistake #9: Corticosteroid underdosing and undercounseling
It’s not uncommon during the warm weather months for me to see patients who are near finishing a Medrol Dosepak that was prescribed by their primary care physicians for a case of contact dermatitis (eg, poison ivy). They come to me because the eruption has returned and it is “as bad as ever.”
Underdosing. Medrol Dosepaks are generally underpowered (too low a dosage) and too short a course.7,10,11
Undercounseling. Patients don’t always realize that contact dermatitis may actually last for 3 weeks or longer. They may also mistakenly believe that systemic treatment will get them through the whole episode (rather than the worst part).
- Design your own prednisone taper for when such tapers are needed. You might even have the prescription, with taper, prefilled on paper for signature. for significant allergic contact dermatitis, the taper may last 2 weeks.
- Dispel myths. Assure patients that by taking a thorough soap shower (and laundering the clothing they were wearing), they will remove all of the oil responsible for the disease.
- Limit your use of injectable corticosteroids. There is little need for injectable corticosteroids in cases of contact dermatitis. Oral corticosteroids work just as well, can be more easily titered based on response, and pose no injection risk of tissue atrophy or abscess formation.9
Mistake #10: Requiring red flags in both history and exam
Skin diagnosis is an “or” game—not an “and” game. By that I mean: If either the history (eg, rapid change, bleeding, crusting, nonhealing ulcer) or the examination is worrisome, biopsy. Even dermoscopy can be completely reassuring with biopsy yielding a melanoma.12 Note, too, our earlier examples of patients with suspect examinations who gave reassuring histories of lesions that had been present for many years. Either a worrisome history or a suspect examination is sufficient for concern. Remember, in general, the worst-case scenario from a biopsy is a scar; from a missed melanoma, an autopsy report.
- Get back to basics. Look carefully at your patient’s skin—even if it’s not the reason for the visit. Take a moment to ask your patient: Do you have any changing lesions or is there anything on your skin that is scaly, bleeding, or crusting? Doing so will cut down on the number of patients who ultimately learn that the lesion that’s “always been there,” and that “didn’t worry the other doctors” is actually a skin cancer.
Correspondence
Gary N. Fox, MD, 1400 E 2nd St, Defiance, OH 43512; foxgary@yahoo.com
1. Fox GN, Mehregan DR. A new papule and “age spots.” J Fam Pract 2007;56:278-282.
2. Farmer ER, Gonin R, Hanna MP. Discordance in the histopathologic diagnosis of melanoma and melanocytic nevi between expert pathologists. Hum Pathol 1996;27:528-531.
3. Barnhill RL, Argenyi ZB, From L, et al. Atypical Spitz nevi/tumors: lack of consensus for diagnosis, discrimination from melanoma, and prediction of outcome. Hum Pathol 1999;30:513-520.
4. Elder DE, Xu X. The approach to the patient with a difficult melanocytic lesion. Pathology 2004;36:428-434.
5. McBroom HM, Ramsay AD. The clinicopathological meeting. A means of auditing diagnostic performance. Am J Surg Pathol 1993;17:75-80.
6. Johr R, Soyer HP, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy: The Essentials. New York, NY: Mosby; 2004.
7. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. New York, NY: Mosby; 2004.
8. Wolff K, Johnson RA, Suurmond D. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 5th ed. New York, NY: McGraw-Hill; 2005.
9. Edwards L. Dermatology in Emergency Care. New York, NY: Churchill Livingstone; 1997.
10. Brodell RT, Williams L. Taking the itch out of poison ivy. Postgrad Med 1999;106:69-70.
11. Hall JC. Dermatologic allergy. In: Hall JC, ed. Sauer’s Manual of Skin Diseases. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:82.
12. Braun RP, Gaide O, Skaria AM, Kopf AW, Saurat JH, Marghoob AA. Exclusively benign dermoscopic pattern in a patient with acral melanoma. Arch Dermatol 2007;143:1213-1215.
I’ve seen my share of missed diagnoses over the years while caring for patients who, through physician- or self-referral, have made their way to our multi-specialty group practice where I focus solely on skin.
There was the 93-year-old patient whose “sun spot” had been evaluated and treated by 2 different dermatologists in the past and turned out to be a lentigo maligna melanoma (FIGURE 1).
There was the patient who had a lesion on her lip for “at least 10—maybe 20—years” that neither caught the attention of her physician, nor her dentist (FIGURE 2). Histology showed she had an infiltrative basal cell carcinoma.
And then there was the wife of a healthcare professional who decided she wanted a “second opinion” for the asymptomatic lesion on her leg that her husband assured her was benign. Her diagnosis was not so simple: She had a MELanocytic Tumor of Unknown Malignant Potential (MELTUMP) that required careful follow-up (FIGURE 3).
Early detection, as we all know, is the name of the game when it comes to skin malignancies. Yet every day, opportunities to catch small, early lesions are missed.
During the past couple of years, I’ve had thousands of patient visits for skin problems and diagnosed more than 1000 skin malignancies. The majority of patients have had some treatment for their presenting dermatosis prior to arrival. Based on my experiences with these patients, I’ve developed a list of common dermatology “mistakes.” Here they are, with some tips for avoiding them.
FIGURE 1
Melanoma missed by 2 dermatologists
This “sun spot” was of no concern to the 93-year-old patient because she had been evaluated and treated by 2 different dermatologists. The darkest areas are dermoscopically-directed pen markings for incisional biopsy. (The size of the lesion and proximity to the eye precluded primary excisional biopsy.) This “sun spot” turned out to be lentigo maligna melanoma.
FIGURE 2
Lesion on lip for “10—maybe 20—years”
This patient had a lesion that had been on her lip for “at least 10—maybe 20—years.” The patient said it had never bled or crusted. Telangiectasia, pearliness, and some infiltration were present. Histologic diagnosis: infiltrative basal cell carcinoma.
FIGURE 3
A case of MELTUMP
Two dermatopathologists read the biopsy as Spitzoid malignant melanoma, Clark Level III, and Breslow thickness 0.9 mm. Two independent dermatopathologists read the same original slides in consultation as atypical Spitz nevus. The 4 could not reach agreement. Final clinical diagnosis: MEL anocytic Tumor of Unknown Malignant Potential (MELTUMP).
Mistake #1: Not looking (and not biopsying)
I had a woman come into the office to have a lesion assessed. She had seen a dermatologist a couple of weeks earlier and even had a number of lesions removed during that visit. The patient told me that she’d repeatedly tried to show the dermatologist one specific lesion—the one of greatest concern to her—just below her underpants line, but the physician was in and out so fast each time, she never had the chance to point out this one melanocytic, changing lesion.
The lesion turned out to be a dysplastic nevus with severe architectural and cytologic atypia. This type of lesion requires histology to differentiate it from melanoma, and could just as easily have been a melanoma.
Almost daily I treat patients who are being seen by their primary care physicians regularly, and have obvious basal cell carcinomas (BCC) or squamous cell carcinomas. I have even found skin malignancies on physicians, their spouses, and their family members.1 These lesions can be easily missed—if you don’t look carefully.
Consider, the following:
- FIGURE 4 illustrates a superficial BCC on the forearm of a physician who was totally unaware of it. (It was detected on “routine” skin examination.)
- FIGURE 5 illustrates a BCC on a patient’s central forehead that, by her history, had been there for many years, and was not of any concern to her. The patient was referred to our office for evaluation of itchy skin on her legs.
- FIGURE 2 illustrates a lesion that, according to the patient, had been on her lip for at least 10—and perhaps even 20—years and was of no concern to her. (It was not the reason for the visit.) Over the years, this patient certainly had numerous primary care and dental visits, but no one “saw” the lesion. Histology confirmed the clinical impression of BCC.
FIGURE 4
Superficial BCC on physician’s forearm
A physician asked for a skin examination, but was totally unaware of this asymptomatic lesion on his dorsal forearm. Once it was identified, he could provide no history about its duration. The lesion had never bled or crusted. Pathology confirmed that it was a superficial basal cell carcinoma.
FIGURE 5
“Mole” on forehead for many years
This patient was referred for itchy legs. She was unconcerned about a prominent “mole” noted on examination of her forehead, one that she said had been there, unchanged, for many years. Histology confirmed nodular basal cell carcinoma.
- Look, look, and look again, especially at sun-exposed areas (faces, ears, scalps [as hair thins], and dorsal forearms).
- Make sure patients are appropriately gowned no matter what the reason for their visit. Listening to heart and lung sounds and palpating abdomens through overcoats may work for some physicians, but not those interested in finding asymptomatic basal cell carcinomas, actinic keratoses, dysplastic nevi, and melanomas. Melanoma in men is most common on the back; in women, it’s most common on the legs. Seeing these areas requires that they be accessible.
- Biopsy when you’re in doubt. If you see a lesion and it is not recognizable as benign (eg, cherry angioma, seborrheic keratosis, nevus), biopsy it. Let the pathologist determine if it’s benign or malignant. If the lesion is questionable and is in an area that you are uncomfortable biopsying, refer the patient for evaluation and potential biopsy.
Mistake #2: Using insufficient light
As a former family practice academic, I used to preach to residents that they needed to use “light, light, and more light” for evaluation of skin lesions. Despite this, I was often asked to evaluate a patient with a resident who hadn’t even bothered to turn on a goose-neck lamp for illumination.
Even with my current “double bank” daylight fluorescent examination room lighting, it often takes additional (surgical-type) lighting to see the diagnostic features of skin lesions. Without such intense light, it is often impossible to see whether there is pearliness, rolled edges, or fine telangiectasia.
- Use whatever intense source of light you have, whether it’s a goose-neck lamp, a halogen, or a surgical light. If you don’t have at least a portable source of bright light, you are under-equipped for a good skin exam.
Mistake #3: Using insufficient (or no) magnification
I was once examining a patient in a hospital room that had inadequate light, despite my best efforts. So I took out my digital camera with flash and autofocus feature and photographed the lesion. I then looked at the lesion on the camera’s LCD monitor and determined that it was a BCC.
The benefit of the camera was 2-fold: Not only did the flash serve as an instant source of light, but the macro feature also provided magnification. Viewing a magnified digital image on a computer screen also allows unhurried, self “second opinions,” where details can often be ascertained that were not immediately apparent in “real time,” such as rolled edges, telangiectasia, dots, streaks, and subtleties of color.
- Use a hand-held magnifying lens (5X to 10X) routinely during skin exams. They’re not expensive and should be part of every primary care physician’s armamentarium—just like stethoscopes, ophthalmoscopes, and reflex hammers.
- Use a digital camera to provide the magnification needed to see details that can be missed clinically. I’m convinced that using a digital camera has made me a better observer—and clinician. Additionally, digital photographs can be stored and compared with histologic results as “self-education.” When purchasing a camera for this purpose, make sure it has a good close-up (macro) feature.
Mistake #4: Assuming that pathology is a perfect science
Most physicians assume that dermatopathologists have a high rate of interrater concordance with diagnoses such as melanoma. Unfortunately, that is not always the case. Consider the following:
- As part of a National Institutes of Health consensus conference on melanoma, 8 dermatopathologists considered experts in melanoma were asked to provide 5 slides each. The slides were relabeled and sent to the same 8 dermatopathologists. (Three slides were eliminated.) Their findings: At the extremes, 1 pathologist called 21 cases melanoma and 16 benign, whereas another called 10 melanoma, 26 benign, and one indeterminate.2 (Remember: These were all experts in melanoma.)
- In a study of 30 melanocytic lesion specimens (including Spitzoid lesions), 10 Harvard dermatopathologists evaluated each sample independently of each other. Given 5 diagnostic categories to choose from, in only one case did as many as 6 of the 10 agree on a diagnosis. In all of these cases, there was long-term clinical follow-up, so the biologic behavior of these lesions was known. Some lesions that proved fatal were categorized by most observers as benign (eg, Spitz nevi or atypical Spitz tumors). The converse, reporting benign lesions as melanoma, also occurred.3
So consider this: If this degree of discordance occurs among dermatopathologists, what results could we expect from non-dermatopathologists?
I have personally seen instances where reports of melanoma from non-dermatopathologists did not even report Clark and Breslow staging information (although one could determine Clark staging from reading the body of the report), and reports of dysplastic nevi that were accompanied by recommendations for re-excision with 1 cm margins.
When I have a report from a general pathologist suggesting a potentially worrisome lesion (melanoma, severely dysplastic nevus, [atypical] Spitz nevus), I always suggest to my patients that we get a dermatopathologic second opinion. (I send all my dermatopathology specimens to dermatopathologists, so this applies to patients referred in with prior pathology in hand.)
Sometimes, even the dermatopathologists do not agree on the nature of the lesion. In such cases, I have my “MELTUMP discussion” with patients. That is, I tell patients that we don’t know for sure what it is, and that ultimately only the final lab test—time—will tell us the true nature of the lesion (FIGURE 3).4
- Send all “skin” to a dermatopathologist. You owe it to your patients.
- Send pictures (electronic or hard copy) to the dermatopathologist when the pathology report and clinical picture do not appear to match. While pictures of skin lesions and dermoscopic photographs would most likely be meaningless to general pathologists, they are useful to dermatopathologists. Research has shown that pathologists in various areas of medicine may alter their diagnosis or differential diagnosis when presented with additional clinical information.5
Mistake #5: Freezing neoplasms without a definitive Dx
“We’ll freeze it and if it doesn’t go away, then…”
This approach poses a significant risk to you (medicolegally) and your patient.
While most of the time what I see has been inappropriately frozen first by first-line providers, that is not always the case. Dermatologists also fall into this trap. FIGURE 6 shows a lesion just behind the hairline on the frontoparietal scalp that was frozen by a very good, and reputable, dermatologist. The patient came to me for a second opinion with an “obvious” BCC.
Some clinicians are “thrown off” when a lesion (like the one on this patient) has hair. Some sources6 indicate that BCCs never have hair, but this is patently untrue.
FIGURE 6
This shouldn’t have been frozen
A dermatologist froze this lesion on a patient’s scalp, believing that it was seborrheic keratosis, based on the patient’s history. The patient sought a second opinion, and the lesion (which had hair) was histologically identified as basal cell carcinoma.
- Don’t freeze a lesion when you are unsure; biopsy it. This is especially critical when you consider that cryotherapy is not considered a first-line treatment for BCC, the most common human malignancy. It is better to biopsy, assure the diagnosis, and then provide the appropriate therapy.
Mistake #6: Treating psoriasis with systemic corticosteroids
Plaque psoriasis can, albeit uncommonly, be transformed to pustular psoriasis after the administration of oral or injectable systemic corticosteroids.7 Although this rarely occurs, most experts consider this poor practice and not worth the risk. In addition, some experts note that systemic glucocorticoids are a drug trigger for inducing or exacerbating psoriasis.8
- Avoid systemic corticosteroids in psoriasis, since psoriasis is generally a long-term disease and systemic corticosteroids are a short-term fix. if there is widespread psoriasis and you are not familiar with systemic treatments, refer the patient. If there is localized disease, consider topical treatment options—such as various strengths of corticosteroids, calcipotriene, and tazarotene (individually or in combination)—depending on location and plaque thickness.
Mistake #7: Doing shave biopsies on melanocytic lesions
For a melanoma, not only can shaving part way through the vertical dimension of the lesion interfere with staging, it can also hinder the pathologist’s ability to arrive at the correct diagnosis.9
- Do a full-thickness, narrow-margin, fully excisional biopsy when you suspect melanoma. Certainly, there are individuals who are expert at saucerization (deep shave biopsies, often with scalloped, sloping edges that go to the deep reticular dermis) and who can perform biopsies of melanocytic lesions while still obtaining reasonable pathologic staging information.
Mistake #8: Using corticosteroid/antifungal combination products
Corticosteroid/antifungal combination products are generally shunned by dermatologists, although they are used extensively by nondermatologists.9 The difficulty with a preparation like Lotrisone, which contains a class III corticosteroid (betamethasone dipropionate [Diprosone]) and the antifungal clotrimazole, is that it is often used long-term for presumed fungal infection on thin-skinned areas. Unfortunately, though, chronic use in these areas can lead to atrophy and striae (FIGURE 7).
Additionally, corticosteroid is essentially “fungus food.” Majocchi’s granulomas can form because the corticosteroid interferes with clotrimazole’s antifungal effect. Note also that these combination products can suppress fungus sufficiently to render cultures and KOH preparations falsely negative and alter the clinical appearance of psoriasiform dermatitis, interfering with subsequent, accurate diagnosis.
FIGURE 7
Striae after corticosteroid combination therapy
This patient developed striae and atrophy after using a combination high-potency topical corticosteroid/antifungal preparation in a thin-skinned area (proximal medial thigh). It was unclear what the prescriber was treating.
- Consider compounding with miconazole powder and hydrocortisone powder, if a corticosteroid/antifungal combination is necessary (which it rarely is). For example, hydrocortisone 1% or 0.5% ointment can be compounded with miconazole powder for short-term, careful external application, in cases of angular cheilitis.
- Limit your use of a topical corticosteroid for a fungal eruption (if one must be used) to the first few days of treatment. The corticosteroid class should be appropriate to the site of application.9
- Counsel your patients about the risks of using topical corticosteroids on thinskinned areas for more than a few days (few weeks, maximum). On the face, corticosteroids can cause rosacea and perioral dermatitis, as well as “rebound” vasodilation. Thus, topical corticosteroids should be used with great caution—and generally as a last resort—for chronic facial dermatoses.
Mistake #9: Corticosteroid underdosing and undercounseling
It’s not uncommon during the warm weather months for me to see patients who are near finishing a Medrol Dosepak that was prescribed by their primary care physicians for a case of contact dermatitis (eg, poison ivy). They come to me because the eruption has returned and it is “as bad as ever.”
Underdosing. Medrol Dosepaks are generally underpowered (too low a dosage) and too short a course.7,10,11
Undercounseling. Patients don’t always realize that contact dermatitis may actually last for 3 weeks or longer. They may also mistakenly believe that systemic treatment will get them through the whole episode (rather than the worst part).
- Design your own prednisone taper for when such tapers are needed. You might even have the prescription, with taper, prefilled on paper for signature. for significant allergic contact dermatitis, the taper may last 2 weeks.
- Dispel myths. Assure patients that by taking a thorough soap shower (and laundering the clothing they were wearing), they will remove all of the oil responsible for the disease.
- Limit your use of injectable corticosteroids. There is little need for injectable corticosteroids in cases of contact dermatitis. Oral corticosteroids work just as well, can be more easily titered based on response, and pose no injection risk of tissue atrophy or abscess formation.9
Mistake #10: Requiring red flags in both history and exam
Skin diagnosis is an “or” game—not an “and” game. By that I mean: If either the history (eg, rapid change, bleeding, crusting, nonhealing ulcer) or the examination is worrisome, biopsy. Even dermoscopy can be completely reassuring with biopsy yielding a melanoma.12 Note, too, our earlier examples of patients with suspect examinations who gave reassuring histories of lesions that had been present for many years. Either a worrisome history or a suspect examination is sufficient for concern. Remember, in general, the worst-case scenario from a biopsy is a scar; from a missed melanoma, an autopsy report.
- Get back to basics. Look carefully at your patient’s skin—even if it’s not the reason for the visit. Take a moment to ask your patient: Do you have any changing lesions or is there anything on your skin that is scaly, bleeding, or crusting? Doing so will cut down on the number of patients who ultimately learn that the lesion that’s “always been there,” and that “didn’t worry the other doctors” is actually a skin cancer.
Correspondence
Gary N. Fox, MD, 1400 E 2nd St, Defiance, OH 43512; foxgary@yahoo.com
I’ve seen my share of missed diagnoses over the years while caring for patients who, through physician- or self-referral, have made their way to our multi-specialty group practice where I focus solely on skin.
There was the 93-year-old patient whose “sun spot” had been evaluated and treated by 2 different dermatologists in the past and turned out to be a lentigo maligna melanoma (FIGURE 1).
There was the patient who had a lesion on her lip for “at least 10—maybe 20—years” that neither caught the attention of her physician, nor her dentist (FIGURE 2). Histology showed she had an infiltrative basal cell carcinoma.
And then there was the wife of a healthcare professional who decided she wanted a “second opinion” for the asymptomatic lesion on her leg that her husband assured her was benign. Her diagnosis was not so simple: She had a MELanocytic Tumor of Unknown Malignant Potential (MELTUMP) that required careful follow-up (FIGURE 3).
Early detection, as we all know, is the name of the game when it comes to skin malignancies. Yet every day, opportunities to catch small, early lesions are missed.
During the past couple of years, I’ve had thousands of patient visits for skin problems and diagnosed more than 1000 skin malignancies. The majority of patients have had some treatment for their presenting dermatosis prior to arrival. Based on my experiences with these patients, I’ve developed a list of common dermatology “mistakes.” Here they are, with some tips for avoiding them.
FIGURE 1
Melanoma missed by 2 dermatologists
This “sun spot” was of no concern to the 93-year-old patient because she had been evaluated and treated by 2 different dermatologists. The darkest areas are dermoscopically-directed pen markings for incisional biopsy. (The size of the lesion and proximity to the eye precluded primary excisional biopsy.) This “sun spot” turned out to be lentigo maligna melanoma.
FIGURE 2
Lesion on lip for “10—maybe 20—years”
This patient had a lesion that had been on her lip for “at least 10—maybe 20—years.” The patient said it had never bled or crusted. Telangiectasia, pearliness, and some infiltration were present. Histologic diagnosis: infiltrative basal cell carcinoma.
FIGURE 3
A case of MELTUMP
Two dermatopathologists read the biopsy as Spitzoid malignant melanoma, Clark Level III, and Breslow thickness 0.9 mm. Two independent dermatopathologists read the same original slides in consultation as atypical Spitz nevus. The 4 could not reach agreement. Final clinical diagnosis: MEL anocytic Tumor of Unknown Malignant Potential (MELTUMP).
Mistake #1: Not looking (and not biopsying)
I had a woman come into the office to have a lesion assessed. She had seen a dermatologist a couple of weeks earlier and even had a number of lesions removed during that visit. The patient told me that she’d repeatedly tried to show the dermatologist one specific lesion—the one of greatest concern to her—just below her underpants line, but the physician was in and out so fast each time, she never had the chance to point out this one melanocytic, changing lesion.
The lesion turned out to be a dysplastic nevus with severe architectural and cytologic atypia. This type of lesion requires histology to differentiate it from melanoma, and could just as easily have been a melanoma.
Almost daily I treat patients who are being seen by their primary care physicians regularly, and have obvious basal cell carcinomas (BCC) or squamous cell carcinomas. I have even found skin malignancies on physicians, their spouses, and their family members.1 These lesions can be easily missed—if you don’t look carefully.
Consider, the following:
- FIGURE 4 illustrates a superficial BCC on the forearm of a physician who was totally unaware of it. (It was detected on “routine” skin examination.)
- FIGURE 5 illustrates a BCC on a patient’s central forehead that, by her history, had been there for many years, and was not of any concern to her. The patient was referred to our office for evaluation of itchy skin on her legs.
- FIGURE 2 illustrates a lesion that, according to the patient, had been on her lip for at least 10—and perhaps even 20—years and was of no concern to her. (It was not the reason for the visit.) Over the years, this patient certainly had numerous primary care and dental visits, but no one “saw” the lesion. Histology confirmed the clinical impression of BCC.
FIGURE 4
Superficial BCC on physician’s forearm
A physician asked for a skin examination, but was totally unaware of this asymptomatic lesion on his dorsal forearm. Once it was identified, he could provide no history about its duration. The lesion had never bled or crusted. Pathology confirmed that it was a superficial basal cell carcinoma.
FIGURE 5
“Mole” on forehead for many years
This patient was referred for itchy legs. She was unconcerned about a prominent “mole” noted on examination of her forehead, one that she said had been there, unchanged, for many years. Histology confirmed nodular basal cell carcinoma.
- Look, look, and look again, especially at sun-exposed areas (faces, ears, scalps [as hair thins], and dorsal forearms).
- Make sure patients are appropriately gowned no matter what the reason for their visit. Listening to heart and lung sounds and palpating abdomens through overcoats may work for some physicians, but not those interested in finding asymptomatic basal cell carcinomas, actinic keratoses, dysplastic nevi, and melanomas. Melanoma in men is most common on the back; in women, it’s most common on the legs. Seeing these areas requires that they be accessible.
- Biopsy when you’re in doubt. If you see a lesion and it is not recognizable as benign (eg, cherry angioma, seborrheic keratosis, nevus), biopsy it. Let the pathologist determine if it’s benign or malignant. If the lesion is questionable and is in an area that you are uncomfortable biopsying, refer the patient for evaluation and potential biopsy.
Mistake #2: Using insufficient light
As a former family practice academic, I used to preach to residents that they needed to use “light, light, and more light” for evaluation of skin lesions. Despite this, I was often asked to evaluate a patient with a resident who hadn’t even bothered to turn on a goose-neck lamp for illumination.
Even with my current “double bank” daylight fluorescent examination room lighting, it often takes additional (surgical-type) lighting to see the diagnostic features of skin lesions. Without such intense light, it is often impossible to see whether there is pearliness, rolled edges, or fine telangiectasia.
- Use whatever intense source of light you have, whether it’s a goose-neck lamp, a halogen, or a surgical light. If you don’t have at least a portable source of bright light, you are under-equipped for a good skin exam.
Mistake #3: Using insufficient (or no) magnification
I was once examining a patient in a hospital room that had inadequate light, despite my best efforts. So I took out my digital camera with flash and autofocus feature and photographed the lesion. I then looked at the lesion on the camera’s LCD monitor and determined that it was a BCC.
The benefit of the camera was 2-fold: Not only did the flash serve as an instant source of light, but the macro feature also provided magnification. Viewing a magnified digital image on a computer screen also allows unhurried, self “second opinions,” where details can often be ascertained that were not immediately apparent in “real time,” such as rolled edges, telangiectasia, dots, streaks, and subtleties of color.
- Use a hand-held magnifying lens (5X to 10X) routinely during skin exams. They’re not expensive and should be part of every primary care physician’s armamentarium—just like stethoscopes, ophthalmoscopes, and reflex hammers.
- Use a digital camera to provide the magnification needed to see details that can be missed clinically. I’m convinced that using a digital camera has made me a better observer—and clinician. Additionally, digital photographs can be stored and compared with histologic results as “self-education.” When purchasing a camera for this purpose, make sure it has a good close-up (macro) feature.
Mistake #4: Assuming that pathology is a perfect science
Most physicians assume that dermatopathologists have a high rate of interrater concordance with diagnoses such as melanoma. Unfortunately, that is not always the case. Consider the following:
- As part of a National Institutes of Health consensus conference on melanoma, 8 dermatopathologists considered experts in melanoma were asked to provide 5 slides each. The slides were relabeled and sent to the same 8 dermatopathologists. (Three slides were eliminated.) Their findings: At the extremes, 1 pathologist called 21 cases melanoma and 16 benign, whereas another called 10 melanoma, 26 benign, and one indeterminate.2 (Remember: These were all experts in melanoma.)
- In a study of 30 melanocytic lesion specimens (including Spitzoid lesions), 10 Harvard dermatopathologists evaluated each sample independently of each other. Given 5 diagnostic categories to choose from, in only one case did as many as 6 of the 10 agree on a diagnosis. In all of these cases, there was long-term clinical follow-up, so the biologic behavior of these lesions was known. Some lesions that proved fatal were categorized by most observers as benign (eg, Spitz nevi or atypical Spitz tumors). The converse, reporting benign lesions as melanoma, also occurred.3
So consider this: If this degree of discordance occurs among dermatopathologists, what results could we expect from non-dermatopathologists?
I have personally seen instances where reports of melanoma from non-dermatopathologists did not even report Clark and Breslow staging information (although one could determine Clark staging from reading the body of the report), and reports of dysplastic nevi that were accompanied by recommendations for re-excision with 1 cm margins.
When I have a report from a general pathologist suggesting a potentially worrisome lesion (melanoma, severely dysplastic nevus, [atypical] Spitz nevus), I always suggest to my patients that we get a dermatopathologic second opinion. (I send all my dermatopathology specimens to dermatopathologists, so this applies to patients referred in with prior pathology in hand.)
Sometimes, even the dermatopathologists do not agree on the nature of the lesion. In such cases, I have my “MELTUMP discussion” with patients. That is, I tell patients that we don’t know for sure what it is, and that ultimately only the final lab test—time—will tell us the true nature of the lesion (FIGURE 3).4
- Send all “skin” to a dermatopathologist. You owe it to your patients.
- Send pictures (electronic or hard copy) to the dermatopathologist when the pathology report and clinical picture do not appear to match. While pictures of skin lesions and dermoscopic photographs would most likely be meaningless to general pathologists, they are useful to dermatopathologists. Research has shown that pathologists in various areas of medicine may alter their diagnosis or differential diagnosis when presented with additional clinical information.5
Mistake #5: Freezing neoplasms without a definitive Dx
“We’ll freeze it and if it doesn’t go away, then…”
This approach poses a significant risk to you (medicolegally) and your patient.
While most of the time what I see has been inappropriately frozen first by first-line providers, that is not always the case. Dermatologists also fall into this trap. FIGURE 6 shows a lesion just behind the hairline on the frontoparietal scalp that was frozen by a very good, and reputable, dermatologist. The patient came to me for a second opinion with an “obvious” BCC.
Some clinicians are “thrown off” when a lesion (like the one on this patient) has hair. Some sources6 indicate that BCCs never have hair, but this is patently untrue.
FIGURE 6
This shouldn’t have been frozen
A dermatologist froze this lesion on a patient’s scalp, believing that it was seborrheic keratosis, based on the patient’s history. The patient sought a second opinion, and the lesion (which had hair) was histologically identified as basal cell carcinoma.
- Don’t freeze a lesion when you are unsure; biopsy it. This is especially critical when you consider that cryotherapy is not considered a first-line treatment for BCC, the most common human malignancy. It is better to biopsy, assure the diagnosis, and then provide the appropriate therapy.
Mistake #6: Treating psoriasis with systemic corticosteroids
Plaque psoriasis can, albeit uncommonly, be transformed to pustular psoriasis after the administration of oral or injectable systemic corticosteroids.7 Although this rarely occurs, most experts consider this poor practice and not worth the risk. In addition, some experts note that systemic glucocorticoids are a drug trigger for inducing or exacerbating psoriasis.8
- Avoid systemic corticosteroids in psoriasis, since psoriasis is generally a long-term disease and systemic corticosteroids are a short-term fix. if there is widespread psoriasis and you are not familiar with systemic treatments, refer the patient. If there is localized disease, consider topical treatment options—such as various strengths of corticosteroids, calcipotriene, and tazarotene (individually or in combination)—depending on location and plaque thickness.
Mistake #7: Doing shave biopsies on melanocytic lesions
For a melanoma, not only can shaving part way through the vertical dimension of the lesion interfere with staging, it can also hinder the pathologist’s ability to arrive at the correct diagnosis.9
- Do a full-thickness, narrow-margin, fully excisional biopsy when you suspect melanoma. Certainly, there are individuals who are expert at saucerization (deep shave biopsies, often with scalloped, sloping edges that go to the deep reticular dermis) and who can perform biopsies of melanocytic lesions while still obtaining reasonable pathologic staging information.
Mistake #8: Using corticosteroid/antifungal combination products
Corticosteroid/antifungal combination products are generally shunned by dermatologists, although they are used extensively by nondermatologists.9 The difficulty with a preparation like Lotrisone, which contains a class III corticosteroid (betamethasone dipropionate [Diprosone]) and the antifungal clotrimazole, is that it is often used long-term for presumed fungal infection on thin-skinned areas. Unfortunately, though, chronic use in these areas can lead to atrophy and striae (FIGURE 7).
Additionally, corticosteroid is essentially “fungus food.” Majocchi’s granulomas can form because the corticosteroid interferes with clotrimazole’s antifungal effect. Note also that these combination products can suppress fungus sufficiently to render cultures and KOH preparations falsely negative and alter the clinical appearance of psoriasiform dermatitis, interfering with subsequent, accurate diagnosis.
FIGURE 7
Striae after corticosteroid combination therapy
This patient developed striae and atrophy after using a combination high-potency topical corticosteroid/antifungal preparation in a thin-skinned area (proximal medial thigh). It was unclear what the prescriber was treating.
- Consider compounding with miconazole powder and hydrocortisone powder, if a corticosteroid/antifungal combination is necessary (which it rarely is). For example, hydrocortisone 1% or 0.5% ointment can be compounded with miconazole powder for short-term, careful external application, in cases of angular cheilitis.
- Limit your use of a topical corticosteroid for a fungal eruption (if one must be used) to the first few days of treatment. The corticosteroid class should be appropriate to the site of application.9
- Counsel your patients about the risks of using topical corticosteroids on thinskinned areas for more than a few days (few weeks, maximum). On the face, corticosteroids can cause rosacea and perioral dermatitis, as well as “rebound” vasodilation. Thus, topical corticosteroids should be used with great caution—and generally as a last resort—for chronic facial dermatoses.
Mistake #9: Corticosteroid underdosing and undercounseling
It’s not uncommon during the warm weather months for me to see patients who are near finishing a Medrol Dosepak that was prescribed by their primary care physicians for a case of contact dermatitis (eg, poison ivy). They come to me because the eruption has returned and it is “as bad as ever.”
Underdosing. Medrol Dosepaks are generally underpowered (too low a dosage) and too short a course.7,10,11
Undercounseling. Patients don’t always realize that contact dermatitis may actually last for 3 weeks or longer. They may also mistakenly believe that systemic treatment will get them through the whole episode (rather than the worst part).
- Design your own prednisone taper for when such tapers are needed. You might even have the prescription, with taper, prefilled on paper for signature. for significant allergic contact dermatitis, the taper may last 2 weeks.
- Dispel myths. Assure patients that by taking a thorough soap shower (and laundering the clothing they were wearing), they will remove all of the oil responsible for the disease.
- Limit your use of injectable corticosteroids. There is little need for injectable corticosteroids in cases of contact dermatitis. Oral corticosteroids work just as well, can be more easily titered based on response, and pose no injection risk of tissue atrophy or abscess formation.9
Mistake #10: Requiring red flags in both history and exam
Skin diagnosis is an “or” game—not an “and” game. By that I mean: If either the history (eg, rapid change, bleeding, crusting, nonhealing ulcer) or the examination is worrisome, biopsy. Even dermoscopy can be completely reassuring with biopsy yielding a melanoma.12 Note, too, our earlier examples of patients with suspect examinations who gave reassuring histories of lesions that had been present for many years. Either a worrisome history or a suspect examination is sufficient for concern. Remember, in general, the worst-case scenario from a biopsy is a scar; from a missed melanoma, an autopsy report.
- Get back to basics. Look carefully at your patient’s skin—even if it’s not the reason for the visit. Take a moment to ask your patient: Do you have any changing lesions or is there anything on your skin that is scaly, bleeding, or crusting? Doing so will cut down on the number of patients who ultimately learn that the lesion that’s “always been there,” and that “didn’t worry the other doctors” is actually a skin cancer.
Correspondence
Gary N. Fox, MD, 1400 E 2nd St, Defiance, OH 43512; foxgary@yahoo.com
1. Fox GN, Mehregan DR. A new papule and “age spots.” J Fam Pract 2007;56:278-282.
2. Farmer ER, Gonin R, Hanna MP. Discordance in the histopathologic diagnosis of melanoma and melanocytic nevi between expert pathologists. Hum Pathol 1996;27:528-531.
3. Barnhill RL, Argenyi ZB, From L, et al. Atypical Spitz nevi/tumors: lack of consensus for diagnosis, discrimination from melanoma, and prediction of outcome. Hum Pathol 1999;30:513-520.
4. Elder DE, Xu X. The approach to the patient with a difficult melanocytic lesion. Pathology 2004;36:428-434.
5. McBroom HM, Ramsay AD. The clinicopathological meeting. A means of auditing diagnostic performance. Am J Surg Pathol 1993;17:75-80.
6. Johr R, Soyer HP, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy: The Essentials. New York, NY: Mosby; 2004.
7. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. New York, NY: Mosby; 2004.
8. Wolff K, Johnson RA, Suurmond D. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 5th ed. New York, NY: McGraw-Hill; 2005.
9. Edwards L. Dermatology in Emergency Care. New York, NY: Churchill Livingstone; 1997.
10. Brodell RT, Williams L. Taking the itch out of poison ivy. Postgrad Med 1999;106:69-70.
11. Hall JC. Dermatologic allergy. In: Hall JC, ed. Sauer’s Manual of Skin Diseases. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:82.
12. Braun RP, Gaide O, Skaria AM, Kopf AW, Saurat JH, Marghoob AA. Exclusively benign dermoscopic pattern in a patient with acral melanoma. Arch Dermatol 2007;143:1213-1215.
1. Fox GN, Mehregan DR. A new papule and “age spots.” J Fam Pract 2007;56:278-282.
2. Farmer ER, Gonin R, Hanna MP. Discordance in the histopathologic diagnosis of melanoma and melanocytic nevi between expert pathologists. Hum Pathol 1996;27:528-531.
3. Barnhill RL, Argenyi ZB, From L, et al. Atypical Spitz nevi/tumors: lack of consensus for diagnosis, discrimination from melanoma, and prediction of outcome. Hum Pathol 1999;30:513-520.
4. Elder DE, Xu X. The approach to the patient with a difficult melanocytic lesion. Pathology 2004;36:428-434.
5. McBroom HM, Ramsay AD. The clinicopathological meeting. A means of auditing diagnostic performance. Am J Surg Pathol 1993;17:75-80.
6. Johr R, Soyer HP, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy: The Essentials. New York, NY: Mosby; 2004.
7. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. New York, NY: Mosby; 2004.
8. Wolff K, Johnson RA, Suurmond D. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 5th ed. New York, NY: McGraw-Hill; 2005.
9. Edwards L. Dermatology in Emergency Care. New York, NY: Churchill Livingstone; 1997.
10. Brodell RT, Williams L. Taking the itch out of poison ivy. Postgrad Med 1999;106:69-70.
11. Hall JC. Dermatologic allergy. In: Hall JC, ed. Sauer’s Manual of Skin Diseases. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:82.
12. Braun RP, Gaide O, Skaria AM, Kopf AW, Saurat JH, Marghoob AA. Exclusively benign dermoscopic pattern in a patient with acral melanoma. Arch Dermatol 2007;143:1213-1215.
A new papule and “age spots”
An 87-year-old woman came to the office for evaluation of a lesion above her lip (FIGURE 1) that had “been there a while” and had intermittently been bleeding and crusting for the last few months. On examination, there was a distinct, firm (but not hard) papule with some adjacent erythema. No distinct telangiectasias, ulceration, blood, or crusts were visible with handheld magnification or upon dermoscopy. (see “The digital camera: Another stethoscope for the skin,”)
FIGURE 1
Lesion above lip
An evaluation of the remainder of the woman’s face revealed 3 more lesions that the patient termed “age spots.” They had been present for quite some time, had not had any notable rapid change, and had not caused her (or a physician in the family) any concern. These “age spots” are depicted in (FIGURE 2A) (left temple), (FIGURE 2B) (forehead), and (FIGURE 2C) (left cheek). Digital photographs were taken through the dermatoscope of the temple, forehead, and cheek lesions (FIGURE 3A, B, AND C).
FIGURE 2A
Digital photos
FIGURE 2B
Digital photos
FIGURE 2C
Digital photos
The 4 lesions are easily identified as worrisome, given that they were pigmented and asymmetric, with a variety of bizarre colors.
The lip. In particular, the lesion above the upper lip (FIGURE 1) clinically presented a wide range of possibilities, including basal cell carcinoma (BCC), milial cyst, nevus, trichoepithelioma, fibrous papule, or any of a variety of adnexal skin neoplasms. Knowing that the lesion was relatively new and had bled and crusted was sufficient to warrant biopsy.
The temple. Dermoscopically, the temple lesion (FIGURE 3A) had blue and brown ovoid structures (also called “blebs” or “blobs”), white areas within the lesion (whiter than normal surrounding skin), a high degree of asymmetry, and distinct telangiectatic vessels. The pink color on dermoscopy was also a cause for concern. The blue ovoid structures plus telangiectasias were highly suggestive of basal cell carcinoma.
FIGURE 3A
Dermoscopy images
The forehead. Dermoscopy of the forehead lesion (FIGURE 3B) showed leaf-like structures (12 o’clock) and maple-leaf structures (6 o’clock). These alone were highly suggestive of pigmented basal cell carcinoma—but in the absence of distinct telangiectasias, we decided to do a deep incisional biopsy rather than risk potentially “shaving a melanoma.” (If a melanoma is biopsied via a shave technique, the ability to histologically measure its thickness and to stage it according to Clark and Breslow staging is lost.)
FIGURE 3B
Dermoscopy images
The cheek. Dermoscopically, the lesion on the cheek (FIGURE 3C) also had no obvious telangiectasias but had a “spoke-wheel” structure (6 o’clock) highly suggestive of basal cell carcinoma.
FIGURE 3C
Dermoscopy images
All the lesions—except for the temple lesion, which was biopsied via a shave technique—were biopsied via generous incisional ellipses.
What is your diagnosis?
How would you treat?
Diagnosis: Basal cell carcinoma
Histology confirmed that all 4 lesions were basal cell carcinomas, the most common type of skin malignancy. The temple lesion in Figures 2A AND 3A and the forehead lesion in Figures 2B AND 3B were histologically both pigmented nodular basal cell carcinomas, clinically characterized as pearly papules with pigment. (FIGURE 3A) also demonstrates telangiectasia.
Differential diagnosis: Innocent papule or carcinoma?
The lip lesion, the presenting “symptom,” did not have evident bleeding and crusting on visual or dermoscopic examination. In the absence of a complete history, it could have been “passed off” as an innocent papule, such as a molluscum (though not common in the elderly) or a milial or epidermoid cyst.
Remember that basal cell carcinoma can be subtle. These lesions were missed by a patient and her family—which included a physician within the household—and grew slowly enough that the patient felt they were simply “age spots.” We have seen basal cell carcinomas that patients have indicated have not changed in years—have not bled, ulcerated, or crusted, while symptomatic lesions have been the least impressive, clinically, at the time of the exam. Always maintain a high index of suspicion.
The clinical types of basal cell carcinoma and their dermoscopic findings are summarized in the (TABLE).
TABLE
Clinical types of basal cell carcinoma and dermoscopic findings
| CLINICAL TYPE | DERMOSCOPIC FINDINGS | NOTES |
|---|---|---|
Nodular (including noduloulcerative and cystic) “Wart” on a supraclavicular area—note pearly translucency of nodular basal cell carcinoma. | Arborizing (tree-like branching telangiectasias) Dermoscopy of lesion at left, clearly showing arborized telangiectatic vessels. |
|
| Pigmented |
|
|
| Sclerosing, cicatricial, or morpheaform | Arborizing telangiectasias |
|
| Superficial | Arborizing telangiectasias |
|
| *Sensitivity/specificity. Sensitivity is the percentage of basal cell carcinomas that possess the feature. Specificity listed is the percentage of melanomas that lack the feature.1 All discussion of dermoscopic diagnosis of basal cell carcinoma assumes absence of a melanocytic pigment network, the presence of which suggests a melanocytic lesion such as a nevus, lentigo, or melanoma. | ||
| Note: The primary use of dermoscopy is the evaluation of pigmented lesions. Thus, except to aid in visualization of telangiectasias and ulceration, there are no characteristic dermoscopic findings in other types of basal cell carcinoma. Telangiectasias may not be visualized if the dermatoscope is applied with sufficient pressure to blanch them. Basal cell carcinomas may exhibit no definite or suggestive findings by dermoscopy, as was the case with the lip papule on this patient. | ||
Tips for making an accurate diagnosis
Basal cell carcinoma and melanoma can mimic other lesions, so keep these tips in mind:
- The “company” a lesion keeps sometimes can help in diagnosis. A patient may have a group of small “pearly papules,” only one of which may show the typical umbilication that allows a confident diagnosis of molluscum contagiosum, for example. Here, 3 lesions had similar dermoscopic structures, only one of which exhibited telangiectasia. A fourth lesion lacked diagnostic characteristics. The best guess, based on the sum total appearance of all of these lesions, is that all are basal cell carcinomas because of the “company they are keeping”—but note that this is also potentially a trap: missing the single basal cell carcinoma lesion among a field of sebaceous hyperplasia, for instance.
- Don’t focus exclusively on the symptomatic lesion. Do a survey of the general region. For ultraviolet-associated lesions (including basal cell carcinoma), it’s preferable to perform, at minimum, a survey of “high-radiation” areas (face, exposed scalp, neck, ears, and dorsal hands and forearms) for other ultraviolet “damage” (eg, actinic keratoses).
- Be meticulous when examining patients’ backs. Patients may not spot lesions on their backs—especially if they are older and have poor vision.
- Avoid thinking in terms of absolutes like “never” and “always.” The clinical axiom that basal cell carcinomas “never” have hair growing from them is disproved by (FIGURE 3A), which clinically, dermoscopically, and histologically is a basal cell carcinoma lesion. Some of the hair seen here is overlying, loose scalp hair “caught” in the dermoscopic field because of the location of this lesion on the temple adjacent to the hairline. But there are also very distinct hairs seen coming out from areas (at about 6 and 8 o’clock) that are clearly part of the lesion, especially on its periphery.
When in doubt, biopsy
When in doubt about which technique to perform, do an incisional biopsy—preferably excisional, but at least a good sampling of the most worrisome area(s).
Suspected basal cell carcinoma, when the examiner is confident the lesion is not a melanoma, can be further evaluated by superficial shave biopsy. Potential melanoma generally should not be evaluated by the shave technique.
Options for therapy
Therapy options for basal cell carcinoma vary based on location (high-risk vs low-risk locations), histologic type of basal cell carcinoma, patient preference, and local availability of therapy. The primary therapies for basal cell carcinoma are surgical excision (including Mohs surgery) and curettage, often combined with electrodesiccation. 5-flurouracil (5-FU) should not be used because it can treat the surface tumor while deeper tumor proliferates.3 Imiquimod is not approved for facial lesions or nodular basal cell carcinomas.
While dermatoscopes are the true “skin stethoscopes,” most primary care physicians do not have them. Many, however, do have a digital camera. A digital camera with a macro-focus feature can be viewed as another stethoscope for the skin. Pictures allow great magnification on the computer screen, presenting color and detail that may be missed on routine clinical inspection. They allow an unhurried “self–second opinion”; you can evaluate lesions with no motion, breathing, or other distractions, following the office visit.
Digital images may also be important for:
- the patient, who may not be able to see the lesion, because it’s on his back, buttocks, or behind his ears. Consider, too, the older patient who may not be able to see the seborrhea in his eyebrow with his bifocals, but he can see it on the camera’s monitor.
- the medical record (printed or electronically stored).
- the pathologist—when forwarded with the pathology specimen. The images can be helpful in developing a clinical correlation to include in the pathology report.
- the insurance carrier, as indisputable documentation for the clinical rationale for biopsying 4 lesions on 1 visit in the event of a “Dear Bad Doctor” Medicare letter. In fact, if not for the indisputable photographic record, one author (GNF) would have been extremely hesitant to perform 4 biopsies on a Medicare patient in 1 session.
- light and magnification where the 2 may be in short supply, such as a poorly mobile patient in a hospital bed. A camera with flash, auto-focus, and macro mode may allow access to otherwise inaccessible lesions.
ACKNOWLEDGMENTS
Gary N. Fox wishes to acknowledge the assistance of Peggy Elston and Lisa Nichols for their help with portions of this article.
CORRESPONDENCE
Gary N. Fox, MD, 2458 Willesden Green, Toledo, OH. E-mail: foxgary@yahoo.com
1. Marghoob AA, Braun RP, Kopf AW, eds. Atlas of Dermoscopy. New York: Taylor & Francis; 2005.
2. Johr R, Soyer HP, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy: The Essentials. New York: Mosby; 2004.
3. Premalignant and malignant nonmelanoma skin tumors [chapter 21]. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. New York: Mosby; 2004.
An 87-year-old woman came to the office for evaluation of a lesion above her lip (FIGURE 1) that had “been there a while” and had intermittently been bleeding and crusting for the last few months. On examination, there was a distinct, firm (but not hard) papule with some adjacent erythema. No distinct telangiectasias, ulceration, blood, or crusts were visible with handheld magnification or upon dermoscopy. (see “The digital camera: Another stethoscope for the skin,”)
FIGURE 1
Lesion above lip
An evaluation of the remainder of the woman’s face revealed 3 more lesions that the patient termed “age spots.” They had been present for quite some time, had not had any notable rapid change, and had not caused her (or a physician in the family) any concern. These “age spots” are depicted in (FIGURE 2A) (left temple), (FIGURE 2B) (forehead), and (FIGURE 2C) (left cheek). Digital photographs were taken through the dermatoscope of the temple, forehead, and cheek lesions (FIGURE 3A, B, AND C).
FIGURE 2A
Digital photos
FIGURE 2B
Digital photos
FIGURE 2C
Digital photos
The 4 lesions are easily identified as worrisome, given that they were pigmented and asymmetric, with a variety of bizarre colors.
The lip. In particular, the lesion above the upper lip (FIGURE 1) clinically presented a wide range of possibilities, including basal cell carcinoma (BCC), milial cyst, nevus, trichoepithelioma, fibrous papule, or any of a variety of adnexal skin neoplasms. Knowing that the lesion was relatively new and had bled and crusted was sufficient to warrant biopsy.
The temple. Dermoscopically, the temple lesion (FIGURE 3A) had blue and brown ovoid structures (also called “blebs” or “blobs”), white areas within the lesion (whiter than normal surrounding skin), a high degree of asymmetry, and distinct telangiectatic vessels. The pink color on dermoscopy was also a cause for concern. The blue ovoid structures plus telangiectasias were highly suggestive of basal cell carcinoma.
FIGURE 3A
Dermoscopy images
The forehead. Dermoscopy of the forehead lesion (FIGURE 3B) showed leaf-like structures (12 o’clock) and maple-leaf structures (6 o’clock). These alone were highly suggestive of pigmented basal cell carcinoma—but in the absence of distinct telangiectasias, we decided to do a deep incisional biopsy rather than risk potentially “shaving a melanoma.” (If a melanoma is biopsied via a shave technique, the ability to histologically measure its thickness and to stage it according to Clark and Breslow staging is lost.)
FIGURE 3B
Dermoscopy images
The cheek. Dermoscopically, the lesion on the cheek (FIGURE 3C) also had no obvious telangiectasias but had a “spoke-wheel” structure (6 o’clock) highly suggestive of basal cell carcinoma.
FIGURE 3C
Dermoscopy images
All the lesions—except for the temple lesion, which was biopsied via a shave technique—were biopsied via generous incisional ellipses.
What is your diagnosis?
How would you treat?
Diagnosis: Basal cell carcinoma
Histology confirmed that all 4 lesions were basal cell carcinomas, the most common type of skin malignancy. The temple lesion in Figures 2A AND 3A and the forehead lesion in Figures 2B AND 3B were histologically both pigmented nodular basal cell carcinomas, clinically characterized as pearly papules with pigment. (FIGURE 3A) also demonstrates telangiectasia.
Differential diagnosis: Innocent papule or carcinoma?
The lip lesion, the presenting “symptom,” did not have evident bleeding and crusting on visual or dermoscopic examination. In the absence of a complete history, it could have been “passed off” as an innocent papule, such as a molluscum (though not common in the elderly) or a milial or epidermoid cyst.
Remember that basal cell carcinoma can be subtle. These lesions were missed by a patient and her family—which included a physician within the household—and grew slowly enough that the patient felt they were simply “age spots.” We have seen basal cell carcinomas that patients have indicated have not changed in years—have not bled, ulcerated, or crusted, while symptomatic lesions have been the least impressive, clinically, at the time of the exam. Always maintain a high index of suspicion.
The clinical types of basal cell carcinoma and their dermoscopic findings are summarized in the (TABLE).
TABLE
Clinical types of basal cell carcinoma and dermoscopic findings
| CLINICAL TYPE | DERMOSCOPIC FINDINGS | NOTES |
|---|---|---|
Nodular (including noduloulcerative and cystic) “Wart” on a supraclavicular area—note pearly translucency of nodular basal cell carcinoma. | Arborizing (tree-like branching telangiectasias) Dermoscopy of lesion at left, clearly showing arborized telangiectatic vessels. |
|
| Pigmented |
|
|
| Sclerosing, cicatricial, or morpheaform | Arborizing telangiectasias |
|
| Superficial | Arborizing telangiectasias |
|
| *Sensitivity/specificity. Sensitivity is the percentage of basal cell carcinomas that possess the feature. Specificity listed is the percentage of melanomas that lack the feature.1 All discussion of dermoscopic diagnosis of basal cell carcinoma assumes absence of a melanocytic pigment network, the presence of which suggests a melanocytic lesion such as a nevus, lentigo, or melanoma. | ||
| Note: The primary use of dermoscopy is the evaluation of pigmented lesions. Thus, except to aid in visualization of telangiectasias and ulceration, there are no characteristic dermoscopic findings in other types of basal cell carcinoma. Telangiectasias may not be visualized if the dermatoscope is applied with sufficient pressure to blanch them. Basal cell carcinomas may exhibit no definite or suggestive findings by dermoscopy, as was the case with the lip papule on this patient. | ||
Tips for making an accurate diagnosis
Basal cell carcinoma and melanoma can mimic other lesions, so keep these tips in mind:
- The “company” a lesion keeps sometimes can help in diagnosis. A patient may have a group of small “pearly papules,” only one of which may show the typical umbilication that allows a confident diagnosis of molluscum contagiosum, for example. Here, 3 lesions had similar dermoscopic structures, only one of which exhibited telangiectasia. A fourth lesion lacked diagnostic characteristics. The best guess, based on the sum total appearance of all of these lesions, is that all are basal cell carcinomas because of the “company they are keeping”—but note that this is also potentially a trap: missing the single basal cell carcinoma lesion among a field of sebaceous hyperplasia, for instance.
- Don’t focus exclusively on the symptomatic lesion. Do a survey of the general region. For ultraviolet-associated lesions (including basal cell carcinoma), it’s preferable to perform, at minimum, a survey of “high-radiation” areas (face, exposed scalp, neck, ears, and dorsal hands and forearms) for other ultraviolet “damage” (eg, actinic keratoses).
- Be meticulous when examining patients’ backs. Patients may not spot lesions on their backs—especially if they are older and have poor vision.
- Avoid thinking in terms of absolutes like “never” and “always.” The clinical axiom that basal cell carcinomas “never” have hair growing from them is disproved by (FIGURE 3A), which clinically, dermoscopically, and histologically is a basal cell carcinoma lesion. Some of the hair seen here is overlying, loose scalp hair “caught” in the dermoscopic field because of the location of this lesion on the temple adjacent to the hairline. But there are also very distinct hairs seen coming out from areas (at about 6 and 8 o’clock) that are clearly part of the lesion, especially on its periphery.
When in doubt, biopsy
When in doubt about which technique to perform, do an incisional biopsy—preferably excisional, but at least a good sampling of the most worrisome area(s).
Suspected basal cell carcinoma, when the examiner is confident the lesion is not a melanoma, can be further evaluated by superficial shave biopsy. Potential melanoma generally should not be evaluated by the shave technique.
Options for therapy
Therapy options for basal cell carcinoma vary based on location (high-risk vs low-risk locations), histologic type of basal cell carcinoma, patient preference, and local availability of therapy. The primary therapies for basal cell carcinoma are surgical excision (including Mohs surgery) and curettage, often combined with electrodesiccation. 5-flurouracil (5-FU) should not be used because it can treat the surface tumor while deeper tumor proliferates.3 Imiquimod is not approved for facial lesions or nodular basal cell carcinomas.
While dermatoscopes are the true “skin stethoscopes,” most primary care physicians do not have them. Many, however, do have a digital camera. A digital camera with a macro-focus feature can be viewed as another stethoscope for the skin. Pictures allow great magnification on the computer screen, presenting color and detail that may be missed on routine clinical inspection. They allow an unhurried “self–second opinion”; you can evaluate lesions with no motion, breathing, or other distractions, following the office visit.
Digital images may also be important for:
- the patient, who may not be able to see the lesion, because it’s on his back, buttocks, or behind his ears. Consider, too, the older patient who may not be able to see the seborrhea in his eyebrow with his bifocals, but he can see it on the camera’s monitor.
- the medical record (printed or electronically stored).
- the pathologist—when forwarded with the pathology specimen. The images can be helpful in developing a clinical correlation to include in the pathology report.
- the insurance carrier, as indisputable documentation for the clinical rationale for biopsying 4 lesions on 1 visit in the event of a “Dear Bad Doctor” Medicare letter. In fact, if not for the indisputable photographic record, one author (GNF) would have been extremely hesitant to perform 4 biopsies on a Medicare patient in 1 session.
- light and magnification where the 2 may be in short supply, such as a poorly mobile patient in a hospital bed. A camera with flash, auto-focus, and macro mode may allow access to otherwise inaccessible lesions.
ACKNOWLEDGMENTS
Gary N. Fox wishes to acknowledge the assistance of Peggy Elston and Lisa Nichols for their help with portions of this article.
CORRESPONDENCE
Gary N. Fox, MD, 2458 Willesden Green, Toledo, OH. E-mail: foxgary@yahoo.com
An 87-year-old woman came to the office for evaluation of a lesion above her lip (FIGURE 1) that had “been there a while” and had intermittently been bleeding and crusting for the last few months. On examination, there was a distinct, firm (but not hard) papule with some adjacent erythema. No distinct telangiectasias, ulceration, blood, or crusts were visible with handheld magnification or upon dermoscopy. (see “The digital camera: Another stethoscope for the skin,”)
FIGURE 1
Lesion above lip
An evaluation of the remainder of the woman’s face revealed 3 more lesions that the patient termed “age spots.” They had been present for quite some time, had not had any notable rapid change, and had not caused her (or a physician in the family) any concern. These “age spots” are depicted in (FIGURE 2A) (left temple), (FIGURE 2B) (forehead), and (FIGURE 2C) (left cheek). Digital photographs were taken through the dermatoscope of the temple, forehead, and cheek lesions (FIGURE 3A, B, AND C).
FIGURE 2A
Digital photos
FIGURE 2B
Digital photos
FIGURE 2C
Digital photos
The 4 lesions are easily identified as worrisome, given that they were pigmented and asymmetric, with a variety of bizarre colors.
The lip. In particular, the lesion above the upper lip (FIGURE 1) clinically presented a wide range of possibilities, including basal cell carcinoma (BCC), milial cyst, nevus, trichoepithelioma, fibrous papule, or any of a variety of adnexal skin neoplasms. Knowing that the lesion was relatively new and had bled and crusted was sufficient to warrant biopsy.
The temple. Dermoscopically, the temple lesion (FIGURE 3A) had blue and brown ovoid structures (also called “blebs” or “blobs”), white areas within the lesion (whiter than normal surrounding skin), a high degree of asymmetry, and distinct telangiectatic vessels. The pink color on dermoscopy was also a cause for concern. The blue ovoid structures plus telangiectasias were highly suggestive of basal cell carcinoma.
FIGURE 3A
Dermoscopy images
The forehead. Dermoscopy of the forehead lesion (FIGURE 3B) showed leaf-like structures (12 o’clock) and maple-leaf structures (6 o’clock). These alone were highly suggestive of pigmented basal cell carcinoma—but in the absence of distinct telangiectasias, we decided to do a deep incisional biopsy rather than risk potentially “shaving a melanoma.” (If a melanoma is biopsied via a shave technique, the ability to histologically measure its thickness and to stage it according to Clark and Breslow staging is lost.)
FIGURE 3B
Dermoscopy images
The cheek. Dermoscopically, the lesion on the cheek (FIGURE 3C) also had no obvious telangiectasias but had a “spoke-wheel” structure (6 o’clock) highly suggestive of basal cell carcinoma.
FIGURE 3C
Dermoscopy images
All the lesions—except for the temple lesion, which was biopsied via a shave technique—were biopsied via generous incisional ellipses.
What is your diagnosis?
How would you treat?
Diagnosis: Basal cell carcinoma
Histology confirmed that all 4 lesions were basal cell carcinomas, the most common type of skin malignancy. The temple lesion in Figures 2A AND 3A and the forehead lesion in Figures 2B AND 3B were histologically both pigmented nodular basal cell carcinomas, clinically characterized as pearly papules with pigment. (FIGURE 3A) also demonstrates telangiectasia.
Differential diagnosis: Innocent papule or carcinoma?
The lip lesion, the presenting “symptom,” did not have evident bleeding and crusting on visual or dermoscopic examination. In the absence of a complete history, it could have been “passed off” as an innocent papule, such as a molluscum (though not common in the elderly) or a milial or epidermoid cyst.
Remember that basal cell carcinoma can be subtle. These lesions were missed by a patient and her family—which included a physician within the household—and grew slowly enough that the patient felt they were simply “age spots.” We have seen basal cell carcinomas that patients have indicated have not changed in years—have not bled, ulcerated, or crusted, while symptomatic lesions have been the least impressive, clinically, at the time of the exam. Always maintain a high index of suspicion.
The clinical types of basal cell carcinoma and their dermoscopic findings are summarized in the (TABLE).
TABLE
Clinical types of basal cell carcinoma and dermoscopic findings
| CLINICAL TYPE | DERMOSCOPIC FINDINGS | NOTES |
|---|---|---|
Nodular (including noduloulcerative and cystic) “Wart” on a supraclavicular area—note pearly translucency of nodular basal cell carcinoma. | Arborizing (tree-like branching telangiectasias) Dermoscopy of lesion at left, clearly showing arborized telangiectatic vessels. |
|
| Pigmented |
|
|
| Sclerosing, cicatricial, or morpheaform | Arborizing telangiectasias |
|
| Superficial | Arborizing telangiectasias |
|
| *Sensitivity/specificity. Sensitivity is the percentage of basal cell carcinomas that possess the feature. Specificity listed is the percentage of melanomas that lack the feature.1 All discussion of dermoscopic diagnosis of basal cell carcinoma assumes absence of a melanocytic pigment network, the presence of which suggests a melanocytic lesion such as a nevus, lentigo, or melanoma. | ||
| Note: The primary use of dermoscopy is the evaluation of pigmented lesions. Thus, except to aid in visualization of telangiectasias and ulceration, there are no characteristic dermoscopic findings in other types of basal cell carcinoma. Telangiectasias may not be visualized if the dermatoscope is applied with sufficient pressure to blanch them. Basal cell carcinomas may exhibit no definite or suggestive findings by dermoscopy, as was the case with the lip papule on this patient. | ||
Tips for making an accurate diagnosis
Basal cell carcinoma and melanoma can mimic other lesions, so keep these tips in mind:
- The “company” a lesion keeps sometimes can help in diagnosis. A patient may have a group of small “pearly papules,” only one of which may show the typical umbilication that allows a confident diagnosis of molluscum contagiosum, for example. Here, 3 lesions had similar dermoscopic structures, only one of which exhibited telangiectasia. A fourth lesion lacked diagnostic characteristics. The best guess, based on the sum total appearance of all of these lesions, is that all are basal cell carcinomas because of the “company they are keeping”—but note that this is also potentially a trap: missing the single basal cell carcinoma lesion among a field of sebaceous hyperplasia, for instance.
- Don’t focus exclusively on the symptomatic lesion. Do a survey of the general region. For ultraviolet-associated lesions (including basal cell carcinoma), it’s preferable to perform, at minimum, a survey of “high-radiation” areas (face, exposed scalp, neck, ears, and dorsal hands and forearms) for other ultraviolet “damage” (eg, actinic keratoses).
- Be meticulous when examining patients’ backs. Patients may not spot lesions on their backs—especially if they are older and have poor vision.
- Avoid thinking in terms of absolutes like “never” and “always.” The clinical axiom that basal cell carcinomas “never” have hair growing from them is disproved by (FIGURE 3A), which clinically, dermoscopically, and histologically is a basal cell carcinoma lesion. Some of the hair seen here is overlying, loose scalp hair “caught” in the dermoscopic field because of the location of this lesion on the temple adjacent to the hairline. But there are also very distinct hairs seen coming out from areas (at about 6 and 8 o’clock) that are clearly part of the lesion, especially on its periphery.
When in doubt, biopsy
When in doubt about which technique to perform, do an incisional biopsy—preferably excisional, but at least a good sampling of the most worrisome area(s).
Suspected basal cell carcinoma, when the examiner is confident the lesion is not a melanoma, can be further evaluated by superficial shave biopsy. Potential melanoma generally should not be evaluated by the shave technique.
Options for therapy
Therapy options for basal cell carcinoma vary based on location (high-risk vs low-risk locations), histologic type of basal cell carcinoma, patient preference, and local availability of therapy. The primary therapies for basal cell carcinoma are surgical excision (including Mohs surgery) and curettage, often combined with electrodesiccation. 5-flurouracil (5-FU) should not be used because it can treat the surface tumor while deeper tumor proliferates.3 Imiquimod is not approved for facial lesions or nodular basal cell carcinomas.
While dermatoscopes are the true “skin stethoscopes,” most primary care physicians do not have them. Many, however, do have a digital camera. A digital camera with a macro-focus feature can be viewed as another stethoscope for the skin. Pictures allow great magnification on the computer screen, presenting color and detail that may be missed on routine clinical inspection. They allow an unhurried “self–second opinion”; you can evaluate lesions with no motion, breathing, or other distractions, following the office visit.
Digital images may also be important for:
- the patient, who may not be able to see the lesion, because it’s on his back, buttocks, or behind his ears. Consider, too, the older patient who may not be able to see the seborrhea in his eyebrow with his bifocals, but he can see it on the camera’s monitor.
- the medical record (printed or electronically stored).
- the pathologist—when forwarded with the pathology specimen. The images can be helpful in developing a clinical correlation to include in the pathology report.
- the insurance carrier, as indisputable documentation for the clinical rationale for biopsying 4 lesions on 1 visit in the event of a “Dear Bad Doctor” Medicare letter. In fact, if not for the indisputable photographic record, one author (GNF) would have been extremely hesitant to perform 4 biopsies on a Medicare patient in 1 session.
- light and magnification where the 2 may be in short supply, such as a poorly mobile patient in a hospital bed. A camera with flash, auto-focus, and macro mode may allow access to otherwise inaccessible lesions.
ACKNOWLEDGMENTS
Gary N. Fox wishes to acknowledge the assistance of Peggy Elston and Lisa Nichols for their help with portions of this article.
CORRESPONDENCE
Gary N. Fox, MD, 2458 Willesden Green, Toledo, OH. E-mail: foxgary@yahoo.com
1. Marghoob AA, Braun RP, Kopf AW, eds. Atlas of Dermoscopy. New York: Taylor & Francis; 2005.
2. Johr R, Soyer HP, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy: The Essentials. New York: Mosby; 2004.
3. Premalignant and malignant nonmelanoma skin tumors [chapter 21]. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. New York: Mosby; 2004.
1. Marghoob AA, Braun RP, Kopf AW, eds. Atlas of Dermoscopy. New York: Taylor & Francis; 2005.
2. Johr R, Soyer HP, Argenziano G, Hofmann-Wellenhof R, Scalvenzi M. Dermoscopy: The Essentials. New York: Mosby; 2004.
3. Premalignant and malignant nonmelanoma skin tumors [chapter 21]. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. New York: Mosby; 2004.
Itching and rash in a boy and his grandmother
A boy came to the office with a rash and progressively severe itching for approximately 2 months (FIGURE 1). Examination showed an excoriated generalized papular eruption, including some urticarial-type papules and chronic eczematoid changes near the waist, axillae, hands, and wrists.
His grandmother, with whom he spends most weekends and a lot of time after school, also has had a rash and progressive itch for approximately 3 weeks. One feature of the dermopathy observed clinically, first located by hand lens examination and then confirmed by dermoscopy, is depicted in FIGURE 2.
FIGURE 1
Excoriated eruptions
FIGURE 2
Dermoscopic photograph of the dermatosis
What is your diagnosis?
Diagnosis: Scabies
The boy and his grandmother both have scabies, an infectious disease—in fact, the first human disease proven to be caused by a specific agent.1Sarcoptes scabiei var hominis, or scabies, is a mite in the arachnid class.2 In some states and localities, scabies cases or scabies outbreaks are reportable to the public health department.
The cardinal symptom of scabies is pruritus. The itch, especially with initial scabietic infestation, may be gradual in onset.3 Physical examination findings can vary from subtle and nonspecific to overwhelming and distinctive. Scabies can also mimic other dermopathies, complicating diagnosis. Undiagnosed and untreated, scabies can last a protracted period.
The dermopathy may be characterized by urticarial-type papules, vesicles, eczematoid change, excoriation, and bacterial superinfection, especially in children. Nodules may be present, particularly on the penis and scrotum. These may last for months after the infestation has cleared.3 The most commonly involved areas include fingers and finger webs, wrist folds, elbows, knees, the lower abdomen, armpits, thighs, male genitals, nipples, breasts, buttocks, and shoulder blades.3,4 In young children, scabies may be found anywhere, including palms, soles, face and scalp.
Affliction of multiple family members and finding dermatitis in these distinctive locations is helpful in diagnosis. Finding the mites’ burrows is considered pathognomonic because other burrowing diseases (eg, cutaneous larva migrans) are easily distinguished clinically.4 Extensive excoriation is a clinical clue to look for burrows.3
Transmission usually skin-to-skin
Scabies is generally transmitted by prolonged skin-to-skin contact, such as occurs in families or during sexual contact. It is possible to acquire scabies infestation via contaminated items of clothing or bed linens, but this is not regarded as a significant route of transmission.3 Transmission by casual contact, such as a handshake or hug, is unlikely.
Infestation with the S scabiei mite, referred to as scabies in man, is termed “mange” in other mammals known to host the mite (dogs, cats, rabbits, cattle, pigs, and horses). Mites from one host species generally do not establish themselves on another species, and thus are referred to as varieties, variants, or forms. Humans develop a transient dermopathy from infestation by animal scabies, but such infestations are mild and disappear spontaneously unless the person is in frequent contact with the infested animal.3,4
Differential diagnosis
The differential diagnosis of scabies—a great masquerader—is extensive, and includes atopic dermatitis, contact dermatitis, impetigo, insect bites, vasculitis, neurodermatitis, folliculitis, prurigo nodularis, psoriasis (crusted scabies), and a host of other dermopathies.3,4
Confirming the diagnosis
Finding the causative mite, its ova (eggs), or scybala (feces), confirms the diagnosis, although failure to find these does not rule out scabies. Papules or burrows that have not been excoriated are best for obtaining preparations for microscopic examination.3 Burrows may be found with nakedeye inspection, although use of a hand-held magnifier and good illumination make finding burrows easier.
Dermoscopy
Dermoscopy, performed with an otoscope-like, illuminated magnifier designed for skin assessment, provides reliable confirmation of S- or Z-shaped burrows. During dermoscopy, carefully examining the distal end of the burrows in the skin may reveal the “triangular black dot” of the scabies mite (FIGURE 2, top right)—the head of the mite.5 The body of the mite—light in color and oval—is not visible even with the most careful dermoscopic examination. The “black dot” of the mite may be visible with careful inspection with a hand lens. In the appropriate clinical setting, dermoscopic identification of an unequivocal burrow with the dark “triangle sign” at one end is diagnostic for scabies. When a digital photograph obtained through the dermatoscope is magnified, the distal end of the burrow (FIGURE 3) reveals the triangular head parts of the mite and the body within the burrow. This body is not evident with dermoscopy alone; the additional magnification via photography allows its visualization.
FIGURE 3
Magnification
Scabies mount
In instances where the physician is going to make an institution-wide recommendation with major ramifications, it is wise to positively identify the mite. A scabies mount performed at the location of the triangular dot will readily provide a mite for identification. Scabies mounts are prepared via a very superficial shave technique without anesthesia. The skin flakes are transferred to a slide and a drop of mineral oil is added. Alternatively, a drop of mineral oil can be placed on the skin and a superficial sample obtained.
Note that this technique differs from that of potassium hydroxide (KOH) preparation for fungal identification. The scabies mount technique is more like a superficial shave biopsy (with the knife blade parallel to the skin) than a KOH preparation (blade dragged along the skin surface more perpendicular to the skin).Microscopic examination of each slide reveals a mite (FIGURES 4 AND 5).
In our patient, 3 burrows were identified with a hand lens and confirmed by dermoscopy. In 2 burrows, the triangular dots were transferred to slides by doing a very superficial shave (without anesthesia) of the stratum corneum with a number 15 blade and handle. The material was placed on a slide, a drop of mineral oil added, and the slide examined microscopically (FIGURES 4 AND 5). These dermoscopically guided preparations each yielded a mite and little other debris.
FIGURE 4
Scabies mite
FIGURE 5
Mite, ova, and feces
Ink test
The “ink test” is another adjunct to help identify burrows. A nontoxic, watersoluble felt-tip marker is rubbed over an area suspected of having burrows. After waiting a few moments for the ink to sink into the disrupted stratum corneum overlying burrows, the ink is washed off, leaving an ink-demarcated burrow to examine.4 This can be performed as an adjunct to dermoscopy.5
The course of scabies
The mite’s life cycle
There are 4 stages in the mite’s life cycle: egg, larva, nymph, and adult. Female mites deposit 2 to 3 eggs per day as they create their burrows. The eggs are oval, 0.1 to 0.15 mm in length, and hatch in 3 to 8 days. The resultant larvae migrate to the skin surface and burrow into the intact stratum corneum to construct almost invisible, short burrows called molting pouches.
The larvae progress through 2 nymphal stages before a final molt to the adult stage. Larvae and nymphs live in molting pouches or in hair follicles. They appear similar to adults except for smaller size and, during the larval stage, 3 pair of legs. Adult female mites are 0.3 to 0.4 mm long and about 0.25 to 0.35 mm wide, about twice the size of males. Mating occurs when a male penetrates the molting pouch of the adult female. Impregnated females then extend their molting pouches to form the characteristic serpentine burrows, laying eggs in the process. The total period to progress from egg to the gravid female stage takes 10 to 14 days. The impregnated females spend the remaining 2 months of their lives in burrows.3,4
The mites live in and on the stratum corneum, burrowing into but never below the stratum corneum. The burrows appear as raised, serpentine lines varying from a few millimeters up to several centimeters long. Transmission occurs by the transfer of ova-bearing females.3,4
Cause of the rash and itch
The mites do not “bite.” Instead, the hallmark of scabies, when found, are the burrows created by the mites. However, it is common to see a papular urticarial type response as an allergic reaction to antigens associated with the mite itself, its scybala, and eggs. In fact, after acquiring scabies for the first time, itch does not appear for 2 to 6 weeks (average, 3 to 4 weeks) because the host needs to be sensitized to these antigens.4
It is not until the immunologic reactivity or sensitization develops that the host becomes symptomatic and aware of a problem. This requirement for sensitization explains the often gradual onset of itch. The incubation period is important in transmission to other individuals during the asymptomatic phase.3 However, a previously sensitized host may experience itch within hours to days after reinfestation.4
Epidemiology of scabies
Scabies infestations occur in all geographic areas and climates, and affects people of all ages and socioeconomic strata.7 For unexplained reasons, those with African ancestry rarely acquire scabies.7
It is most common in those who have close physical contact with others and, therefore, disproportionately affects children, mothers of young children, sexually active young adults, nursing home populations, and those in crowded living situations. Scabies is commonplace in developing countries. It is possible to acquire scabies after sleeping in unsanitary bedding. The scabies mite does not carry other diseases.7
Crusted scabies
Crusted scabies, a rare form of scabies also known as Norwegian scabies, is an aggressive infestation that usually occurs in immunodeficient, debilitated, or malnourished persons. Crusted scabies, because of the huge mite burden, is associated with greater transmissibility than scabies.7 Interestingly, because of impaired allergic response or indifference to itch, some of these patients may exhibit little pruritus.7
Treatment of scabies
Perhaps the most difficult job in treatment of scabies is treating asymptomatic contacts. Physicians may be reluctant to prescribe, and contacts themselves may be reluctant to take, appropriate treatment. These individuals often spread the infection for 4 to 6 weeks before they develop sensitization and clinical symptoms. Thus, it is essential that these asymptomatic contacts be treated or a cycle of reinfestation will be created.3 All sexual contacts, close personal contacts, and household contacts from within the preceding month should be examined and treated.8
Permethrin cream. The recommended treatment by the Centers for Disease Control and Prevention (CDC) is permethrin cream (5%) applied to all areas of the body from the neck down and thoroughly washed off after 8 to 14 hours. This recommendation includes careful application under fingernails, between toes, and on palms and soles. Infants may need the face and scalp treated in addition. Treatment of the face beyond infancy frequently results in a contact irritant dermatitis. Permethrin is effective and safe but costs more than lindane.8
Lindane. The CDC guidelines offer 2 alternatives to permethrin. One alternative, lindane 1% cream or lotion, can be applied in a thin layer to all areas of the body from the neck down and thoroughly washed off after 8 hours.
Lindane should not be used immediately after a bath or shower, and should not be used by persons who have extensive dermatitis, pregnant or lactating women, or children aged less than 2 years. Lindane resistance has been reported, including in the United States. Seizures have occurred when lindane was applied after a bath or used by patients who had extensive dermatitis. Aplastic anemia following lindane use also has been reported. Infants, young children, and pregnant or lactating women should not be treated with lindane; they can be treated with permethrin.8
Applying topical treatments. Topical scabicides should be applied to all skin from neck down, including intertriginous areas and the gluteal fold. The medication needs to be reapplied to hands if the hands are washed after application. It is advisable to cut fingernails short before applying scabicides and to ensure that scabicide is applied under fingernails. A toothpick can be used if necessary to assist in application under nails. In infants and small children, medication should be applied to face and scalp, avoiding the periorbital area.6
Other treatments. Ivermectin, the third treatment recommended by the CDC, can be administered as a single dose of 200 mcg/kg orally, and repeated in 2 weeks. Ivermectin is not recommended for pregnant or lactating patients. The safety of ivermectin in children who weigh less than 15 kg has not been determined.8
Some specialists recommend retreatment after 1 to 2 weeks for patients who are still symptomatic. Patients who do not respond to the recommended treatment should be retreated with an alternative regimen.8
Patients who have uncomplicated scabies and also are infected with HIV should receive the same treatment regimens as those who are HIV-negative.8 For patients with crusted scabies, the optimal regimen is unknown because no controlled therapeutic trials have been conducted. Expert opinion suggests augmented and combined regimens should be used for this aggressive infestation. Lindane should be avoided because of risks of neurotoxicity with heavy applications.8 Control of scabies epidemics (eg, in nursing homes, hospitals, residential facilities) require treatment of the entire population at risk.
Ancillary measures
Scabies mites may survive for a few days after leaving human skin. Thus, frequent bed linen changes minimize transmission via bedding. Hot-water laundry in temperatures of 120°F (49°s mites in 10 minutes and is sufficient to disinfect all bedding, clothing, and washable items.3
Other methods of disinfection include placing items in a dryer on the hot cycle for 10 to 30 minutes, pressing them with a warm iron, dry-cleaning, or placing in a sealed plastic bag for 7 to 14 days. Carpets or upholstery should be vacuumed through the heavy traffic areas. Fumigation of living areas and furniture with insecticide is unnecessary.6-8 Pets do not need to be treated.6 Children may return to school and childcare immediately following initial treatment.6
Follow-up of scabies patient
The boy’s mother is allowed to view the mites through the microscope, fostering her accepting the diagnosis and enhancing the chance for compliance with treatment, which involves treating the entire family.
Patients should be informed that the rash and pruritus of scabies may persist for 4 weeks after treatment because scabietic antigenic material remains until natural epidermal sloughing and turnover occurs.3 When symptoms or signs persist, evaluation should ensue for faulty application of topical scabicides and for treatment failure.7
Acknowledgments
The author (GNF) wishes to acknowledge the assistance of Peggy Elston and Heather Martinez, without whose assistance photographs like these would never happen; and Lisa Nichols, without whose acquisitive skills it never would have occurred to me to mite-hunt with a dermatoscope.
CORRESPONDENCE
Gary N. Fox, MD, Defiance Clinic, 1400 East Second Street, Defiance, OH 43512. E-mail: foxgary@yahoo.com
1. Binder WD. Scabies. eMedicine [online database]. Available at: www.emedicine.com/emerg/topic517.htm. Accessed on July 6, 2006.
2. Arachnid. Wikipedia [online encyclopedia]. Available at: en.wikipedia.org/wiki/Arachnid. Accessed on July 6, 2006.
3. Scabies. DPDx—CDC Parasitology Diagnostic Website. Available at: www.dpd.cdc.gov/dpdx/HTML/Scabies.htm. Accessed on July 6, 2006.
4. Arya V, Molinaro MJ, Majewski SS, Schwartz RA. Pediatric scabies. Cutis 2003;71:193-196.
5. Vazquez-Lopez F, Kreusch JF, Marghoob AA. Other uses of dermoscopy. In: Marghoob AA, Braun RP, Kopf AW, eds. Atlas of Dermoscopy. New York: Taylor & Francis; 2005:301,305-306.
6. FAQs—scabies. Texas Department of Health Services, Infectious Disease Control Unit website. Available at: www.dshs.state.tx.us/idcu/disease/scabies/faqs/. Accessed on July 6, 2006.
7. Infestations and bites [chapter 15]. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. New York: Mosby; 2004:497-503.
8. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep 2002;51(RR-6):68-69.
A boy came to the office with a rash and progressively severe itching for approximately 2 months (FIGURE 1). Examination showed an excoriated generalized papular eruption, including some urticarial-type papules and chronic eczematoid changes near the waist, axillae, hands, and wrists.
His grandmother, with whom he spends most weekends and a lot of time after school, also has had a rash and progressive itch for approximately 3 weeks. One feature of the dermopathy observed clinically, first located by hand lens examination and then confirmed by dermoscopy, is depicted in FIGURE 2.
FIGURE 1
Excoriated eruptions
FIGURE 2
Dermoscopic photograph of the dermatosis
What is your diagnosis?
Diagnosis: Scabies
The boy and his grandmother both have scabies, an infectious disease—in fact, the first human disease proven to be caused by a specific agent.1Sarcoptes scabiei var hominis, or scabies, is a mite in the arachnid class.2 In some states and localities, scabies cases or scabies outbreaks are reportable to the public health department.
The cardinal symptom of scabies is pruritus. The itch, especially with initial scabietic infestation, may be gradual in onset.3 Physical examination findings can vary from subtle and nonspecific to overwhelming and distinctive. Scabies can also mimic other dermopathies, complicating diagnosis. Undiagnosed and untreated, scabies can last a protracted period.
The dermopathy may be characterized by urticarial-type papules, vesicles, eczematoid change, excoriation, and bacterial superinfection, especially in children. Nodules may be present, particularly on the penis and scrotum. These may last for months after the infestation has cleared.3 The most commonly involved areas include fingers and finger webs, wrist folds, elbows, knees, the lower abdomen, armpits, thighs, male genitals, nipples, breasts, buttocks, and shoulder blades.3,4 In young children, scabies may be found anywhere, including palms, soles, face and scalp.
Affliction of multiple family members and finding dermatitis in these distinctive locations is helpful in diagnosis. Finding the mites’ burrows is considered pathognomonic because other burrowing diseases (eg, cutaneous larva migrans) are easily distinguished clinically.4 Extensive excoriation is a clinical clue to look for burrows.3
Transmission usually skin-to-skin
Scabies is generally transmitted by prolonged skin-to-skin contact, such as occurs in families or during sexual contact. It is possible to acquire scabies infestation via contaminated items of clothing or bed linens, but this is not regarded as a significant route of transmission.3 Transmission by casual contact, such as a handshake or hug, is unlikely.
Infestation with the S scabiei mite, referred to as scabies in man, is termed “mange” in other mammals known to host the mite (dogs, cats, rabbits, cattle, pigs, and horses). Mites from one host species generally do not establish themselves on another species, and thus are referred to as varieties, variants, or forms. Humans develop a transient dermopathy from infestation by animal scabies, but such infestations are mild and disappear spontaneously unless the person is in frequent contact with the infested animal.3,4
Differential diagnosis
The differential diagnosis of scabies—a great masquerader—is extensive, and includes atopic dermatitis, contact dermatitis, impetigo, insect bites, vasculitis, neurodermatitis, folliculitis, prurigo nodularis, psoriasis (crusted scabies), and a host of other dermopathies.3,4
Confirming the diagnosis
Finding the causative mite, its ova (eggs), or scybala (feces), confirms the diagnosis, although failure to find these does not rule out scabies. Papules or burrows that have not been excoriated are best for obtaining preparations for microscopic examination.3 Burrows may be found with nakedeye inspection, although use of a hand-held magnifier and good illumination make finding burrows easier.
Dermoscopy
Dermoscopy, performed with an otoscope-like, illuminated magnifier designed for skin assessment, provides reliable confirmation of S- or Z-shaped burrows. During dermoscopy, carefully examining the distal end of the burrows in the skin may reveal the “triangular black dot” of the scabies mite (FIGURE 2, top right)—the head of the mite.5 The body of the mite—light in color and oval—is not visible even with the most careful dermoscopic examination. The “black dot” of the mite may be visible with careful inspection with a hand lens. In the appropriate clinical setting, dermoscopic identification of an unequivocal burrow with the dark “triangle sign” at one end is diagnostic for scabies. When a digital photograph obtained through the dermatoscope is magnified, the distal end of the burrow (FIGURE 3) reveals the triangular head parts of the mite and the body within the burrow. This body is not evident with dermoscopy alone; the additional magnification via photography allows its visualization.
FIGURE 3
Magnification
Scabies mount
In instances where the physician is going to make an institution-wide recommendation with major ramifications, it is wise to positively identify the mite. A scabies mount performed at the location of the triangular dot will readily provide a mite for identification. Scabies mounts are prepared via a very superficial shave technique without anesthesia. The skin flakes are transferred to a slide and a drop of mineral oil is added. Alternatively, a drop of mineral oil can be placed on the skin and a superficial sample obtained.
Note that this technique differs from that of potassium hydroxide (KOH) preparation for fungal identification. The scabies mount technique is more like a superficial shave biopsy (with the knife blade parallel to the skin) than a KOH preparation (blade dragged along the skin surface more perpendicular to the skin).Microscopic examination of each slide reveals a mite (FIGURES 4 AND 5).
In our patient, 3 burrows were identified with a hand lens and confirmed by dermoscopy. In 2 burrows, the triangular dots were transferred to slides by doing a very superficial shave (without anesthesia) of the stratum corneum with a number 15 blade and handle. The material was placed on a slide, a drop of mineral oil added, and the slide examined microscopically (FIGURES 4 AND 5). These dermoscopically guided preparations each yielded a mite and little other debris.
FIGURE 4
Scabies mite
FIGURE 5
Mite, ova, and feces
Ink test
The “ink test” is another adjunct to help identify burrows. A nontoxic, watersoluble felt-tip marker is rubbed over an area suspected of having burrows. After waiting a few moments for the ink to sink into the disrupted stratum corneum overlying burrows, the ink is washed off, leaving an ink-demarcated burrow to examine.4 This can be performed as an adjunct to dermoscopy.5
The course of scabies
The mite’s life cycle
There are 4 stages in the mite’s life cycle: egg, larva, nymph, and adult. Female mites deposit 2 to 3 eggs per day as they create their burrows. The eggs are oval, 0.1 to 0.15 mm in length, and hatch in 3 to 8 days. The resultant larvae migrate to the skin surface and burrow into the intact stratum corneum to construct almost invisible, short burrows called molting pouches.
The larvae progress through 2 nymphal stages before a final molt to the adult stage. Larvae and nymphs live in molting pouches or in hair follicles. They appear similar to adults except for smaller size and, during the larval stage, 3 pair of legs. Adult female mites are 0.3 to 0.4 mm long and about 0.25 to 0.35 mm wide, about twice the size of males. Mating occurs when a male penetrates the molting pouch of the adult female. Impregnated females then extend their molting pouches to form the characteristic serpentine burrows, laying eggs in the process. The total period to progress from egg to the gravid female stage takes 10 to 14 days. The impregnated females spend the remaining 2 months of their lives in burrows.3,4
The mites live in and on the stratum corneum, burrowing into but never below the stratum corneum. The burrows appear as raised, serpentine lines varying from a few millimeters up to several centimeters long. Transmission occurs by the transfer of ova-bearing females.3,4
Cause of the rash and itch
The mites do not “bite.” Instead, the hallmark of scabies, when found, are the burrows created by the mites. However, it is common to see a papular urticarial type response as an allergic reaction to antigens associated with the mite itself, its scybala, and eggs. In fact, after acquiring scabies for the first time, itch does not appear for 2 to 6 weeks (average, 3 to 4 weeks) because the host needs to be sensitized to these antigens.4
It is not until the immunologic reactivity or sensitization develops that the host becomes symptomatic and aware of a problem. This requirement for sensitization explains the often gradual onset of itch. The incubation period is important in transmission to other individuals during the asymptomatic phase.3 However, a previously sensitized host may experience itch within hours to days after reinfestation.4
Epidemiology of scabies
Scabies infestations occur in all geographic areas and climates, and affects people of all ages and socioeconomic strata.7 For unexplained reasons, those with African ancestry rarely acquire scabies.7
It is most common in those who have close physical contact with others and, therefore, disproportionately affects children, mothers of young children, sexually active young adults, nursing home populations, and those in crowded living situations. Scabies is commonplace in developing countries. It is possible to acquire scabies after sleeping in unsanitary bedding. The scabies mite does not carry other diseases.7
Crusted scabies
Crusted scabies, a rare form of scabies also known as Norwegian scabies, is an aggressive infestation that usually occurs in immunodeficient, debilitated, or malnourished persons. Crusted scabies, because of the huge mite burden, is associated with greater transmissibility than scabies.7 Interestingly, because of impaired allergic response or indifference to itch, some of these patients may exhibit little pruritus.7
Treatment of scabies
Perhaps the most difficult job in treatment of scabies is treating asymptomatic contacts. Physicians may be reluctant to prescribe, and contacts themselves may be reluctant to take, appropriate treatment. These individuals often spread the infection for 4 to 6 weeks before they develop sensitization and clinical symptoms. Thus, it is essential that these asymptomatic contacts be treated or a cycle of reinfestation will be created.3 All sexual contacts, close personal contacts, and household contacts from within the preceding month should be examined and treated.8
Permethrin cream. The recommended treatment by the Centers for Disease Control and Prevention (CDC) is permethrin cream (5%) applied to all areas of the body from the neck down and thoroughly washed off after 8 to 14 hours. This recommendation includes careful application under fingernails, between toes, and on palms and soles. Infants may need the face and scalp treated in addition. Treatment of the face beyond infancy frequently results in a contact irritant dermatitis. Permethrin is effective and safe but costs more than lindane.8
Lindane. The CDC guidelines offer 2 alternatives to permethrin. One alternative, lindane 1% cream or lotion, can be applied in a thin layer to all areas of the body from the neck down and thoroughly washed off after 8 hours.
Lindane should not be used immediately after a bath or shower, and should not be used by persons who have extensive dermatitis, pregnant or lactating women, or children aged less than 2 years. Lindane resistance has been reported, including in the United States. Seizures have occurred when lindane was applied after a bath or used by patients who had extensive dermatitis. Aplastic anemia following lindane use also has been reported. Infants, young children, and pregnant or lactating women should not be treated with lindane; they can be treated with permethrin.8
Applying topical treatments. Topical scabicides should be applied to all skin from neck down, including intertriginous areas and the gluteal fold. The medication needs to be reapplied to hands if the hands are washed after application. It is advisable to cut fingernails short before applying scabicides and to ensure that scabicide is applied under fingernails. A toothpick can be used if necessary to assist in application under nails. In infants and small children, medication should be applied to face and scalp, avoiding the periorbital area.6
Other treatments. Ivermectin, the third treatment recommended by the CDC, can be administered as a single dose of 200 mcg/kg orally, and repeated in 2 weeks. Ivermectin is not recommended for pregnant or lactating patients. The safety of ivermectin in children who weigh less than 15 kg has not been determined.8
Some specialists recommend retreatment after 1 to 2 weeks for patients who are still symptomatic. Patients who do not respond to the recommended treatment should be retreated with an alternative regimen.8
Patients who have uncomplicated scabies and also are infected with HIV should receive the same treatment regimens as those who are HIV-negative.8 For patients with crusted scabies, the optimal regimen is unknown because no controlled therapeutic trials have been conducted. Expert opinion suggests augmented and combined regimens should be used for this aggressive infestation. Lindane should be avoided because of risks of neurotoxicity with heavy applications.8 Control of scabies epidemics (eg, in nursing homes, hospitals, residential facilities) require treatment of the entire population at risk.
Ancillary measures
Scabies mites may survive for a few days after leaving human skin. Thus, frequent bed linen changes minimize transmission via bedding. Hot-water laundry in temperatures of 120°F (49°s mites in 10 minutes and is sufficient to disinfect all bedding, clothing, and washable items.3
Other methods of disinfection include placing items in a dryer on the hot cycle for 10 to 30 minutes, pressing them with a warm iron, dry-cleaning, or placing in a sealed plastic bag for 7 to 14 days. Carpets or upholstery should be vacuumed through the heavy traffic areas. Fumigation of living areas and furniture with insecticide is unnecessary.6-8 Pets do not need to be treated.6 Children may return to school and childcare immediately following initial treatment.6
Follow-up of scabies patient
The boy’s mother is allowed to view the mites through the microscope, fostering her accepting the diagnosis and enhancing the chance for compliance with treatment, which involves treating the entire family.
Patients should be informed that the rash and pruritus of scabies may persist for 4 weeks after treatment because scabietic antigenic material remains until natural epidermal sloughing and turnover occurs.3 When symptoms or signs persist, evaluation should ensue for faulty application of topical scabicides and for treatment failure.7
Acknowledgments
The author (GNF) wishes to acknowledge the assistance of Peggy Elston and Heather Martinez, without whose assistance photographs like these would never happen; and Lisa Nichols, without whose acquisitive skills it never would have occurred to me to mite-hunt with a dermatoscope.
CORRESPONDENCE
Gary N. Fox, MD, Defiance Clinic, 1400 East Second Street, Defiance, OH 43512. E-mail: foxgary@yahoo.com
A boy came to the office with a rash and progressively severe itching for approximately 2 months (FIGURE 1). Examination showed an excoriated generalized papular eruption, including some urticarial-type papules and chronic eczematoid changes near the waist, axillae, hands, and wrists.
His grandmother, with whom he spends most weekends and a lot of time after school, also has had a rash and progressive itch for approximately 3 weeks. One feature of the dermopathy observed clinically, first located by hand lens examination and then confirmed by dermoscopy, is depicted in FIGURE 2.
FIGURE 1
Excoriated eruptions
FIGURE 2
Dermoscopic photograph of the dermatosis
What is your diagnosis?
Diagnosis: Scabies
The boy and his grandmother both have scabies, an infectious disease—in fact, the first human disease proven to be caused by a specific agent.1Sarcoptes scabiei var hominis, or scabies, is a mite in the arachnid class.2 In some states and localities, scabies cases or scabies outbreaks are reportable to the public health department.
The cardinal symptom of scabies is pruritus. The itch, especially with initial scabietic infestation, may be gradual in onset.3 Physical examination findings can vary from subtle and nonspecific to overwhelming and distinctive. Scabies can also mimic other dermopathies, complicating diagnosis. Undiagnosed and untreated, scabies can last a protracted period.
The dermopathy may be characterized by urticarial-type papules, vesicles, eczematoid change, excoriation, and bacterial superinfection, especially in children. Nodules may be present, particularly on the penis and scrotum. These may last for months after the infestation has cleared.3 The most commonly involved areas include fingers and finger webs, wrist folds, elbows, knees, the lower abdomen, armpits, thighs, male genitals, nipples, breasts, buttocks, and shoulder blades.3,4 In young children, scabies may be found anywhere, including palms, soles, face and scalp.
Affliction of multiple family members and finding dermatitis in these distinctive locations is helpful in diagnosis. Finding the mites’ burrows is considered pathognomonic because other burrowing diseases (eg, cutaneous larva migrans) are easily distinguished clinically.4 Extensive excoriation is a clinical clue to look for burrows.3
Transmission usually skin-to-skin
Scabies is generally transmitted by prolonged skin-to-skin contact, such as occurs in families or during sexual contact. It is possible to acquire scabies infestation via contaminated items of clothing or bed linens, but this is not regarded as a significant route of transmission.3 Transmission by casual contact, such as a handshake or hug, is unlikely.
Infestation with the S scabiei mite, referred to as scabies in man, is termed “mange” in other mammals known to host the mite (dogs, cats, rabbits, cattle, pigs, and horses). Mites from one host species generally do not establish themselves on another species, and thus are referred to as varieties, variants, or forms. Humans develop a transient dermopathy from infestation by animal scabies, but such infestations are mild and disappear spontaneously unless the person is in frequent contact with the infested animal.3,4
Differential diagnosis
The differential diagnosis of scabies—a great masquerader—is extensive, and includes atopic dermatitis, contact dermatitis, impetigo, insect bites, vasculitis, neurodermatitis, folliculitis, prurigo nodularis, psoriasis (crusted scabies), and a host of other dermopathies.3,4
Confirming the diagnosis
Finding the causative mite, its ova (eggs), or scybala (feces), confirms the diagnosis, although failure to find these does not rule out scabies. Papules or burrows that have not been excoriated are best for obtaining preparations for microscopic examination.3 Burrows may be found with nakedeye inspection, although use of a hand-held magnifier and good illumination make finding burrows easier.
Dermoscopy
Dermoscopy, performed with an otoscope-like, illuminated magnifier designed for skin assessment, provides reliable confirmation of S- or Z-shaped burrows. During dermoscopy, carefully examining the distal end of the burrows in the skin may reveal the “triangular black dot” of the scabies mite (FIGURE 2, top right)—the head of the mite.5 The body of the mite—light in color and oval—is not visible even with the most careful dermoscopic examination. The “black dot” of the mite may be visible with careful inspection with a hand lens. In the appropriate clinical setting, dermoscopic identification of an unequivocal burrow with the dark “triangle sign” at one end is diagnostic for scabies. When a digital photograph obtained through the dermatoscope is magnified, the distal end of the burrow (FIGURE 3) reveals the triangular head parts of the mite and the body within the burrow. This body is not evident with dermoscopy alone; the additional magnification via photography allows its visualization.
FIGURE 3
Magnification
Scabies mount
In instances where the physician is going to make an institution-wide recommendation with major ramifications, it is wise to positively identify the mite. A scabies mount performed at the location of the triangular dot will readily provide a mite for identification. Scabies mounts are prepared via a very superficial shave technique without anesthesia. The skin flakes are transferred to a slide and a drop of mineral oil is added. Alternatively, a drop of mineral oil can be placed on the skin and a superficial sample obtained.
Note that this technique differs from that of potassium hydroxide (KOH) preparation for fungal identification. The scabies mount technique is more like a superficial shave biopsy (with the knife blade parallel to the skin) than a KOH preparation (blade dragged along the skin surface more perpendicular to the skin).Microscopic examination of each slide reveals a mite (FIGURES 4 AND 5).
In our patient, 3 burrows were identified with a hand lens and confirmed by dermoscopy. In 2 burrows, the triangular dots were transferred to slides by doing a very superficial shave (without anesthesia) of the stratum corneum with a number 15 blade and handle. The material was placed on a slide, a drop of mineral oil added, and the slide examined microscopically (FIGURES 4 AND 5). These dermoscopically guided preparations each yielded a mite and little other debris.
FIGURE 4
Scabies mite
FIGURE 5
Mite, ova, and feces
Ink test
The “ink test” is another adjunct to help identify burrows. A nontoxic, watersoluble felt-tip marker is rubbed over an area suspected of having burrows. After waiting a few moments for the ink to sink into the disrupted stratum corneum overlying burrows, the ink is washed off, leaving an ink-demarcated burrow to examine.4 This can be performed as an adjunct to dermoscopy.5
The course of scabies
The mite’s life cycle
There are 4 stages in the mite’s life cycle: egg, larva, nymph, and adult. Female mites deposit 2 to 3 eggs per day as they create their burrows. The eggs are oval, 0.1 to 0.15 mm in length, and hatch in 3 to 8 days. The resultant larvae migrate to the skin surface and burrow into the intact stratum corneum to construct almost invisible, short burrows called molting pouches.
The larvae progress through 2 nymphal stages before a final molt to the adult stage. Larvae and nymphs live in molting pouches or in hair follicles. They appear similar to adults except for smaller size and, during the larval stage, 3 pair of legs. Adult female mites are 0.3 to 0.4 mm long and about 0.25 to 0.35 mm wide, about twice the size of males. Mating occurs when a male penetrates the molting pouch of the adult female. Impregnated females then extend their molting pouches to form the characteristic serpentine burrows, laying eggs in the process. The total period to progress from egg to the gravid female stage takes 10 to 14 days. The impregnated females spend the remaining 2 months of their lives in burrows.3,4
The mites live in and on the stratum corneum, burrowing into but never below the stratum corneum. The burrows appear as raised, serpentine lines varying from a few millimeters up to several centimeters long. Transmission occurs by the transfer of ova-bearing females.3,4
Cause of the rash and itch
The mites do not “bite.” Instead, the hallmark of scabies, when found, are the burrows created by the mites. However, it is common to see a papular urticarial type response as an allergic reaction to antigens associated with the mite itself, its scybala, and eggs. In fact, after acquiring scabies for the first time, itch does not appear for 2 to 6 weeks (average, 3 to 4 weeks) because the host needs to be sensitized to these antigens.4
It is not until the immunologic reactivity or sensitization develops that the host becomes symptomatic and aware of a problem. This requirement for sensitization explains the often gradual onset of itch. The incubation period is important in transmission to other individuals during the asymptomatic phase.3 However, a previously sensitized host may experience itch within hours to days after reinfestation.4
Epidemiology of scabies
Scabies infestations occur in all geographic areas and climates, and affects people of all ages and socioeconomic strata.7 For unexplained reasons, those with African ancestry rarely acquire scabies.7
It is most common in those who have close physical contact with others and, therefore, disproportionately affects children, mothers of young children, sexually active young adults, nursing home populations, and those in crowded living situations. Scabies is commonplace in developing countries. It is possible to acquire scabies after sleeping in unsanitary bedding. The scabies mite does not carry other diseases.7
Crusted scabies
Crusted scabies, a rare form of scabies also known as Norwegian scabies, is an aggressive infestation that usually occurs in immunodeficient, debilitated, or malnourished persons. Crusted scabies, because of the huge mite burden, is associated with greater transmissibility than scabies.7 Interestingly, because of impaired allergic response or indifference to itch, some of these patients may exhibit little pruritus.7
Treatment of scabies
Perhaps the most difficult job in treatment of scabies is treating asymptomatic contacts. Physicians may be reluctant to prescribe, and contacts themselves may be reluctant to take, appropriate treatment. These individuals often spread the infection for 4 to 6 weeks before they develop sensitization and clinical symptoms. Thus, it is essential that these asymptomatic contacts be treated or a cycle of reinfestation will be created.3 All sexual contacts, close personal contacts, and household contacts from within the preceding month should be examined and treated.8
Permethrin cream. The recommended treatment by the Centers for Disease Control and Prevention (CDC) is permethrin cream (5%) applied to all areas of the body from the neck down and thoroughly washed off after 8 to 14 hours. This recommendation includes careful application under fingernails, between toes, and on palms and soles. Infants may need the face and scalp treated in addition. Treatment of the face beyond infancy frequently results in a contact irritant dermatitis. Permethrin is effective and safe but costs more than lindane.8
Lindane. The CDC guidelines offer 2 alternatives to permethrin. One alternative, lindane 1% cream or lotion, can be applied in a thin layer to all areas of the body from the neck down and thoroughly washed off after 8 hours.
Lindane should not be used immediately after a bath or shower, and should not be used by persons who have extensive dermatitis, pregnant or lactating women, or children aged less than 2 years. Lindane resistance has been reported, including in the United States. Seizures have occurred when lindane was applied after a bath or used by patients who had extensive dermatitis. Aplastic anemia following lindane use also has been reported. Infants, young children, and pregnant or lactating women should not be treated with lindane; they can be treated with permethrin.8
Applying topical treatments. Topical scabicides should be applied to all skin from neck down, including intertriginous areas and the gluteal fold. The medication needs to be reapplied to hands if the hands are washed after application. It is advisable to cut fingernails short before applying scabicides and to ensure that scabicide is applied under fingernails. A toothpick can be used if necessary to assist in application under nails. In infants and small children, medication should be applied to face and scalp, avoiding the periorbital area.6
Other treatments. Ivermectin, the third treatment recommended by the CDC, can be administered as a single dose of 200 mcg/kg orally, and repeated in 2 weeks. Ivermectin is not recommended for pregnant or lactating patients. The safety of ivermectin in children who weigh less than 15 kg has not been determined.8
Some specialists recommend retreatment after 1 to 2 weeks for patients who are still symptomatic. Patients who do not respond to the recommended treatment should be retreated with an alternative regimen.8
Patients who have uncomplicated scabies and also are infected with HIV should receive the same treatment regimens as those who are HIV-negative.8 For patients with crusted scabies, the optimal regimen is unknown because no controlled therapeutic trials have been conducted. Expert opinion suggests augmented and combined regimens should be used for this aggressive infestation. Lindane should be avoided because of risks of neurotoxicity with heavy applications.8 Control of scabies epidemics (eg, in nursing homes, hospitals, residential facilities) require treatment of the entire population at risk.
Ancillary measures
Scabies mites may survive for a few days after leaving human skin. Thus, frequent bed linen changes minimize transmission via bedding. Hot-water laundry in temperatures of 120°F (49°s mites in 10 minutes and is sufficient to disinfect all bedding, clothing, and washable items.3
Other methods of disinfection include placing items in a dryer on the hot cycle for 10 to 30 minutes, pressing them with a warm iron, dry-cleaning, or placing in a sealed plastic bag for 7 to 14 days. Carpets or upholstery should be vacuumed through the heavy traffic areas. Fumigation of living areas and furniture with insecticide is unnecessary.6-8 Pets do not need to be treated.6 Children may return to school and childcare immediately following initial treatment.6
Follow-up of scabies patient
The boy’s mother is allowed to view the mites through the microscope, fostering her accepting the diagnosis and enhancing the chance for compliance with treatment, which involves treating the entire family.
Patients should be informed that the rash and pruritus of scabies may persist for 4 weeks after treatment because scabietic antigenic material remains until natural epidermal sloughing and turnover occurs.3 When symptoms or signs persist, evaluation should ensue for faulty application of topical scabicides and for treatment failure.7
Acknowledgments
The author (GNF) wishes to acknowledge the assistance of Peggy Elston and Heather Martinez, without whose assistance photographs like these would never happen; and Lisa Nichols, without whose acquisitive skills it never would have occurred to me to mite-hunt with a dermatoscope.
CORRESPONDENCE
Gary N. Fox, MD, Defiance Clinic, 1400 East Second Street, Defiance, OH 43512. E-mail: foxgary@yahoo.com
1. Binder WD. Scabies. eMedicine [online database]. Available at: www.emedicine.com/emerg/topic517.htm. Accessed on July 6, 2006.
2. Arachnid. Wikipedia [online encyclopedia]. Available at: en.wikipedia.org/wiki/Arachnid. Accessed on July 6, 2006.
3. Scabies. DPDx—CDC Parasitology Diagnostic Website. Available at: www.dpd.cdc.gov/dpdx/HTML/Scabies.htm. Accessed on July 6, 2006.
4. Arya V, Molinaro MJ, Majewski SS, Schwartz RA. Pediatric scabies. Cutis 2003;71:193-196.
5. Vazquez-Lopez F, Kreusch JF, Marghoob AA. Other uses of dermoscopy. In: Marghoob AA, Braun RP, Kopf AW, eds. Atlas of Dermoscopy. New York: Taylor & Francis; 2005:301,305-306.
6. FAQs—scabies. Texas Department of Health Services, Infectious Disease Control Unit website. Available at: www.dshs.state.tx.us/idcu/disease/scabies/faqs/. Accessed on July 6, 2006.
7. Infestations and bites [chapter 15]. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. New York: Mosby; 2004:497-503.
8. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep 2002;51(RR-6):68-69.
1. Binder WD. Scabies. eMedicine [online database]. Available at: www.emedicine.com/emerg/topic517.htm. Accessed on July 6, 2006.
2. Arachnid. Wikipedia [online encyclopedia]. Available at: en.wikipedia.org/wiki/Arachnid. Accessed on July 6, 2006.
3. Scabies. DPDx—CDC Parasitology Diagnostic Website. Available at: www.dpd.cdc.gov/dpdx/HTML/Scabies.htm. Accessed on July 6, 2006.
4. Arya V, Molinaro MJ, Majewski SS, Schwartz RA. Pediatric scabies. Cutis 2003;71:193-196.
5. Vazquez-Lopez F, Kreusch JF, Marghoob AA. Other uses of dermoscopy. In: Marghoob AA, Braun RP, Kopf AW, eds. Atlas of Dermoscopy. New York: Taylor & Francis; 2005:301,305-306.
6. FAQs—scabies. Texas Department of Health Services, Infectious Disease Control Unit website. Available at: www.dshs.state.tx.us/idcu/disease/scabies/faqs/. Accessed on July 6, 2006.
7. Infestations and bites [chapter 15]. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. New York: Mosby; 2004:497-503.
8. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep 2002;51(RR-6):68-69.
Puzzling palmar papules and pits
A 54-year-old African American woman came to the office with a problem on her hands that began about 10 years before: small, hard plugs that formed on her palms (Figures 1 and 2). These areas remain tender for 1 to 2 days after the plugs first form and while they “stick up.” After a few days, the plugs fall out, leaving small pits. The patient experienced no other symptoms once the plugs fall out; just the appearance of her palms.
Many years ago, a physician tried freezing the lesions, believing them to be warts. That therapy provided no benefit. The patient found that filing down the plugs and lubricating them with white petrolatum helped during the symptomatic phase.
The patient was married, with no history of sexually transmitted diseases or significant occupational exposures. She did take medication to control her hypertension, hyperlipidemia, and hypothyroidism. However, the problem with her hands predated taking these medications. There was no personal or family history of skin malignancy. The remainder of the skin examination was unremarkable.
FIGURE 1
Lesions on left palm
FIGURE 2
Lateral view
What is your diagnosis?
Diagnosis: keratosis punctata of the palmar creases
Keratosis punctata of the palmar creases (KPPC) is a benign, largely asymptomatic condition of the hands, seen almost exclusively those with African ancestry. KPPC presents as small keratotic papules (Figure 3) that evolve into discreet conical pits (Figure 4).1,2 Although KPPC is not a novel or rare condition among African Americans, it is not found in standard dermatology texts used by primary care physicians. However, reference to KPPC may be found in ethnic dermatology texts, including reference to it as “a common normal finding in the black palm.”1
The lesions of KPPC characteristically are 1 to 5 mm in diameter, sharply defined hyperkeratotic pits that occur in the flexural creases of the hands, both on the palms and volar surfaces of the fingers. KPPC has also referred to as keratotic pits of the palmar creases, punctate keratoses of the palmar creases, keratoderma punctata, hyperkeratosis penetrans, lenticular atrophia of the palmar creases, and hyperkeratosis punctata of the palmar creases.
FIGURE 3
Close-up of a “plug”
FIGURE 4
Close-up of a “pit”
Distinguishing KPPC from KPPP
KPPC has also been regarded as a variant of keratosis punctata palmaris et plantaris (KPPP).3,4 KPPP and KPPC share some similarities with respect to the size and number of lesions per palm, probable exacerbation by trauma, and predilection for occurring in those of Afro-Caribbean descent.1,3,4
Historically, there has been some confusion in distinguishing KPPC from KPPP—in fact, it is possible for the 2 conditions to occur simultaneously. The papular lesions of KPPP tend to occur over the entire palm, volar wrist, and medial aspects of the feet. These entities differ in age at onset, prevalence, symptoms, and prognosis.
Sources differ regarding the average age of onset for KPPP; some report onset from infancy to 70 years.5-7 For KPPC, the age of onset generally is between 15 and 40 years.3 Among African Americans, the prevalence of KPPC is between 1.9% and 3.1%,3,6,8 whereas the prevalence of KPPP may be up to 11%.3,4 While KPPP is largely asymptomatic, the lesions of KPPC tend to be noticed more often. Once present, KPPP lesions usually remain stable over time, whereas, KPPC lesions usually increase in number and size.3
Demographics and causes
KPPC is rarely seen in Caucasians. Of 1001 white patients examined for palmar lesions, none fulfilled the diagnostic criteria for KPPC.9 In a study of 534 patients, Weiss et al discovered 7 cases— all in African American patients and representing 3.1% of this racial group.8
The cause of KPPC is unknown. No medications have been implicated, and it has been difficult to link it to a virus.3 Although some authors have suggested that KPPC represents flexural calluses related to manual labor, lesions also occur in patients without this history.1,5 There is no association between KPPC and arsenical agents or syphilis.8
It is generally believed that KPPC does not have a recognizable heritable pattern, though there may be exceptions.8 There may be a familial association with ichthyosis vulgaris and other disorders of keratinization. One report included 5 patients in 1 family with keratotic plugs of the palmar creases consistent with an autosomal dominant pattern of inheritance. The syndrome was associated with ichthyosis vulgaris in several family members.10 KPPP and KPPC might be the result of abnormal callus formation in predisposed individuals, as both conditions seem to be due to an abnormal hyperproliferative response to local trauma.3
Differential diagnosis
Punctate keratoses of the palms are fairly common frequently overlooked lesions. The differential diagnosis is extensive (Table), but there are several clinical features of KPPC that distinguish it from other hyperkeratotic conditions. The lesions of KPPC can be painful, have a predilection for jointcreases, and evolve into pits.3 KPPP is similar except not localized to the creases.4
Aquagenic keratoderma is a transitory condition afflicting young women and defined clinically by the appearance of palmar lesions accentuated after immersion in water. These lesions have a characteristic histological appearance (hyperkeratosis, dilated eccrine ducts).13
Palmoplantar pustulosis is characterized by chronically recurring sterile pustules on the palms and soles, usually found on an erythematous base, and a strong association with tobacco use.14Palmoplantar lichen planus may exhibit a variety of morphologic patterns including papules or plaques with pruritus, erythema, and compact hyperkeratosis.15
Cole disease is an uncommon disorder typified by distinctive cutaneous hyperpigmentation and punctate keratoses on the palms and soles. It is a congenital disease with an autosomal dominant inheritance pattern and phenotypic variability.16
Palmoplantar psoriasis is associated with manual labor in 50% of cases. Lesions are restricted to areas exposed to pressure. All patients with unilateral palmar lesions had them on their dominant hand. Biopsy may be necessary to differentiate hyperkeratotic eczema from psoriasis when just localized to the palms and soles.17
TABLE
Differential diagnosis of punctate keratoses of the hands and feet
| Acquired keratoses | Classic clinical description | Associations |
|---|---|---|
| Arsenical | Round, verrucous, or acuminate keratotic papules most common on palms and soles. Typically occur decades after chronic arsenic ingestion | Angiosarcoma of the liver, nonmelanoma skin cancer, bronchial adenocarcinoma |
| Idiopathic filiform porokeratoses | Multiple thin spiny keratotic projections on palms and soles | Breast, renal, colon, and lung cancer |
| Keratosis punctata of the palmar creases | Discrete, sharply marginated, hyperkeratotic, conical, 1–5 mm depressions confined to flexural creases | Dupuytren’s contracture, striate keratoderma, knuckle pads |
| Hereditary keratoses | Classic clinical description | Associations |
| Keratosis punctata palmoplantaris (type I), Buschke-Fischer-Brauer disease | Multiple 1–2 mm punctate keratoses of the palms and soles | Longitudinal nail dystrophy, lichen nitidus, ichthyosis, atopy, recalcitrant warts. Increased risk of malignancy |
| Spiny keratoderma (type II) | Small keratotic spines over entire palmoplantar surfaces. Resembles the spines of an old-fashioned music box | No predisposition to malignancy |
| Acrokeratoelastoidosis lichenoids (type III) | 2–4 mm round to oval papules on the borders of hands, feet and wrists. May be umbilicated and become confluent | Darier’s disease, Cowden’s disease |
| Adapted from Rustad et al 1990,5 Kong et al 2004,7 Asadi 2003,9 Habif 2004,11 and Osman et al 1992.12 | ||
Treatment options: keratolytic agents may help temporarily
The mainstay of therapy is informing the patient of the benign nature of the diagnosis and avoiding unnecessary and unhelpful therapies and diagnostic modalities. Therapy with keratolytic agents or systemic retinoids may temporarily improve symptoms of KPPC.
However, lesions tend to recur when the medications are stopped or decreased.5,7 Temporizing treatment of symptomatic keratoses, such as applying emollients and paring them, is all that is usually necessary. Systemic retinoids have far too many side effects to consider using in this completely benign condition.
Patient outcome
The patient was reassured by the explanation of the condition and chose to try a keratolytic/emollient agent, Lac-Hydrin, for symptomatic recurrences. At her last visit for another health issue, she has reported this to be helpful.
Acknowledgments
The authors would like to acknowledge the unfailingly cheerful cooperation and expert assistance of the St. Vincent Mercy Medical Center library staff.
Corresponding author
Gary N. Fox, MD, 2200 Jefferson Avenue, Toledo, OH 43624. E-mail: foxgary@yahoo.com.
1. Rosen T, Martin S. Variants of normal skin in blacks. In: Atlas of Black Dermatology. 1st ed. Boston, Mass: Little, Brown; 1981;12-13.
2. Dilaimy MS, Owen WR, Sina B. Keratosis punctata of the palmar creases. Cutis 1984;33:394-396.
3. Rustad OJ, Vance JC. Punctate keratoses of the palms and soles and keratotic pits of the palmar creases. J Am Acad Dermatol 1990;22:468-476.
4. Kinsley-Scott TR, Young RJ, 3rd, Meffert JJ. Keratosis punctata of the instep. Cutis 2003;72:451-452.
5. Kong MS, Harford R, O’Neill JT. Keratosis punctata palmoplantaris controlled with topical retinoids: a case report and review of the literature. Cutis 2004;74:173-179.
6. Anderson WA, Elam MD, Lambert WC. Keratosis punctata and atopy. Report of 31 cases with a prospective study of prevalence. Arch Dermatol 1984;120:884-890.
7. Asadi AK. Type I hereditary punctate keratoderma. Dermatol Online J 2003;9:38.-
8. Weiss RM, Rasmussen JE. Keratosis punctata of the palmar creases. Arch Dermatol 1980;116:669-671.
9. Penas PF, Rios-Buceta L, Sanchez-Perez J, Dorado-Bris JM, Aragues M. Keratosis punctata of the palmar creases: case report and prevalence study in Caucasians. Dermatology 1994;188:200-202.
10. Del-Rio E, Vazquez-Veiga H, Aguilar A, Velez A, Sanchez Yus E. Keratosis punctata of the palmar creases. A report on three generations, demonstrating an association with ichthyosis vulgaris and evidence of involvement of the acrosyringium. Clin Exp Dermatol 1994;19:165-167.
11. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. St. Louis, Mo: Mosby; 2004.
12. Osman Y, Daly TJ, Don PC. Spiny keratoderma of the palms and soles. J Am Acad Dermatol 1992;26:879-881.
13. Betlloch I, Vergara G, Albares MP, Pascual JC, Silvestre JF, Botella R. Aquagenic keratoderma. J Eur Acad Dermatol Venereol 2003;17:306-307.
14. Gimenez-Garcia R, Sanchez-Ramon S, Cuellar-Olmedo LA. Palmoplantar pustulosis: a clinicoepidemiological study. The relationship between tobacco use and thyroid function. J Eur Acad Dermatol Venereol 2003;17:276-279.
15. Gunduz K, Inanir I, Turkdogan P, Sacar H. Palmoplantar lichen planus presenting with vesicle-like papules. J Dermatol 2003;30:337-340. 0
16. Vignale R, Yusin A, Panuncio A, Abulafia J, Reyno Z, Vaglio A. Cole disease: hypopigmentation with punctate keratosis of the palms and soles. Pediatr Dermatol 2002;19:302-306.
17. Kumar B, Saraswat A, Kaur I. Palmoplantar lesions in psoriasis. Acta Derm Venereol 2002;82:192-195.
A 54-year-old African American woman came to the office with a problem on her hands that began about 10 years before: small, hard plugs that formed on her palms (Figures 1 and 2). These areas remain tender for 1 to 2 days after the plugs first form and while they “stick up.” After a few days, the plugs fall out, leaving small pits. The patient experienced no other symptoms once the plugs fall out; just the appearance of her palms.
Many years ago, a physician tried freezing the lesions, believing them to be warts. That therapy provided no benefit. The patient found that filing down the plugs and lubricating them with white petrolatum helped during the symptomatic phase.
The patient was married, with no history of sexually transmitted diseases or significant occupational exposures. She did take medication to control her hypertension, hyperlipidemia, and hypothyroidism. However, the problem with her hands predated taking these medications. There was no personal or family history of skin malignancy. The remainder of the skin examination was unremarkable.
FIGURE 1
Lesions on left palm
FIGURE 2
Lateral view
What is your diagnosis?
Diagnosis: keratosis punctata of the palmar creases
Keratosis punctata of the palmar creases (KPPC) is a benign, largely asymptomatic condition of the hands, seen almost exclusively those with African ancestry. KPPC presents as small keratotic papules (Figure 3) that evolve into discreet conical pits (Figure 4).1,2 Although KPPC is not a novel or rare condition among African Americans, it is not found in standard dermatology texts used by primary care physicians. However, reference to KPPC may be found in ethnic dermatology texts, including reference to it as “a common normal finding in the black palm.”1
The lesions of KPPC characteristically are 1 to 5 mm in diameter, sharply defined hyperkeratotic pits that occur in the flexural creases of the hands, both on the palms and volar surfaces of the fingers. KPPC has also referred to as keratotic pits of the palmar creases, punctate keratoses of the palmar creases, keratoderma punctata, hyperkeratosis penetrans, lenticular atrophia of the palmar creases, and hyperkeratosis punctata of the palmar creases.
FIGURE 3
Close-up of a “plug”
FIGURE 4
Close-up of a “pit”
Distinguishing KPPC from KPPP
KPPC has also been regarded as a variant of keratosis punctata palmaris et plantaris (KPPP).3,4 KPPP and KPPC share some similarities with respect to the size and number of lesions per palm, probable exacerbation by trauma, and predilection for occurring in those of Afro-Caribbean descent.1,3,4
Historically, there has been some confusion in distinguishing KPPC from KPPP—in fact, it is possible for the 2 conditions to occur simultaneously. The papular lesions of KPPP tend to occur over the entire palm, volar wrist, and medial aspects of the feet. These entities differ in age at onset, prevalence, symptoms, and prognosis.
Sources differ regarding the average age of onset for KPPP; some report onset from infancy to 70 years.5-7 For KPPC, the age of onset generally is between 15 and 40 years.3 Among African Americans, the prevalence of KPPC is between 1.9% and 3.1%,3,6,8 whereas the prevalence of KPPP may be up to 11%.3,4 While KPPP is largely asymptomatic, the lesions of KPPC tend to be noticed more often. Once present, KPPP lesions usually remain stable over time, whereas, KPPC lesions usually increase in number and size.3
Demographics and causes
KPPC is rarely seen in Caucasians. Of 1001 white patients examined for palmar lesions, none fulfilled the diagnostic criteria for KPPC.9 In a study of 534 patients, Weiss et al discovered 7 cases— all in African American patients and representing 3.1% of this racial group.8
The cause of KPPC is unknown. No medications have been implicated, and it has been difficult to link it to a virus.3 Although some authors have suggested that KPPC represents flexural calluses related to manual labor, lesions also occur in patients without this history.1,5 There is no association between KPPC and arsenical agents or syphilis.8
It is generally believed that KPPC does not have a recognizable heritable pattern, though there may be exceptions.8 There may be a familial association with ichthyosis vulgaris and other disorders of keratinization. One report included 5 patients in 1 family with keratotic plugs of the palmar creases consistent with an autosomal dominant pattern of inheritance. The syndrome was associated with ichthyosis vulgaris in several family members.10 KPPP and KPPC might be the result of abnormal callus formation in predisposed individuals, as both conditions seem to be due to an abnormal hyperproliferative response to local trauma.3
Differential diagnosis
Punctate keratoses of the palms are fairly common frequently overlooked lesions. The differential diagnosis is extensive (Table), but there are several clinical features of KPPC that distinguish it from other hyperkeratotic conditions. The lesions of KPPC can be painful, have a predilection for jointcreases, and evolve into pits.3 KPPP is similar except not localized to the creases.4
Aquagenic keratoderma is a transitory condition afflicting young women and defined clinically by the appearance of palmar lesions accentuated after immersion in water. These lesions have a characteristic histological appearance (hyperkeratosis, dilated eccrine ducts).13
Palmoplantar pustulosis is characterized by chronically recurring sterile pustules on the palms and soles, usually found on an erythematous base, and a strong association with tobacco use.14Palmoplantar lichen planus may exhibit a variety of morphologic patterns including papules or plaques with pruritus, erythema, and compact hyperkeratosis.15
Cole disease is an uncommon disorder typified by distinctive cutaneous hyperpigmentation and punctate keratoses on the palms and soles. It is a congenital disease with an autosomal dominant inheritance pattern and phenotypic variability.16
Palmoplantar psoriasis is associated with manual labor in 50% of cases. Lesions are restricted to areas exposed to pressure. All patients with unilateral palmar lesions had them on their dominant hand. Biopsy may be necessary to differentiate hyperkeratotic eczema from psoriasis when just localized to the palms and soles.17
TABLE
Differential diagnosis of punctate keratoses of the hands and feet
| Acquired keratoses | Classic clinical description | Associations |
|---|---|---|
| Arsenical | Round, verrucous, or acuminate keratotic papules most common on palms and soles. Typically occur decades after chronic arsenic ingestion | Angiosarcoma of the liver, nonmelanoma skin cancer, bronchial adenocarcinoma |
| Idiopathic filiform porokeratoses | Multiple thin spiny keratotic projections on palms and soles | Breast, renal, colon, and lung cancer |
| Keratosis punctata of the palmar creases | Discrete, sharply marginated, hyperkeratotic, conical, 1–5 mm depressions confined to flexural creases | Dupuytren’s contracture, striate keratoderma, knuckle pads |
| Hereditary keratoses | Classic clinical description | Associations |
| Keratosis punctata palmoplantaris (type I), Buschke-Fischer-Brauer disease | Multiple 1–2 mm punctate keratoses of the palms and soles | Longitudinal nail dystrophy, lichen nitidus, ichthyosis, atopy, recalcitrant warts. Increased risk of malignancy |
| Spiny keratoderma (type II) | Small keratotic spines over entire palmoplantar surfaces. Resembles the spines of an old-fashioned music box | No predisposition to malignancy |
| Acrokeratoelastoidosis lichenoids (type III) | 2–4 mm round to oval papules on the borders of hands, feet and wrists. May be umbilicated and become confluent | Darier’s disease, Cowden’s disease |
| Adapted from Rustad et al 1990,5 Kong et al 2004,7 Asadi 2003,9 Habif 2004,11 and Osman et al 1992.12 | ||
Treatment options: keratolytic agents may help temporarily
The mainstay of therapy is informing the patient of the benign nature of the diagnosis and avoiding unnecessary and unhelpful therapies and diagnostic modalities. Therapy with keratolytic agents or systemic retinoids may temporarily improve symptoms of KPPC.
However, lesions tend to recur when the medications are stopped or decreased.5,7 Temporizing treatment of symptomatic keratoses, such as applying emollients and paring them, is all that is usually necessary. Systemic retinoids have far too many side effects to consider using in this completely benign condition.
Patient outcome
The patient was reassured by the explanation of the condition and chose to try a keratolytic/emollient agent, Lac-Hydrin, for symptomatic recurrences. At her last visit for another health issue, she has reported this to be helpful.
Acknowledgments
The authors would like to acknowledge the unfailingly cheerful cooperation and expert assistance of the St. Vincent Mercy Medical Center library staff.
Corresponding author
Gary N. Fox, MD, 2200 Jefferson Avenue, Toledo, OH 43624. E-mail: foxgary@yahoo.com.
A 54-year-old African American woman came to the office with a problem on her hands that began about 10 years before: small, hard plugs that formed on her palms (Figures 1 and 2). These areas remain tender for 1 to 2 days after the plugs first form and while they “stick up.” After a few days, the plugs fall out, leaving small pits. The patient experienced no other symptoms once the plugs fall out; just the appearance of her palms.
Many years ago, a physician tried freezing the lesions, believing them to be warts. That therapy provided no benefit. The patient found that filing down the plugs and lubricating them with white petrolatum helped during the symptomatic phase.
The patient was married, with no history of sexually transmitted diseases or significant occupational exposures. She did take medication to control her hypertension, hyperlipidemia, and hypothyroidism. However, the problem with her hands predated taking these medications. There was no personal or family history of skin malignancy. The remainder of the skin examination was unremarkable.
FIGURE 1
Lesions on left palm
FIGURE 2
Lateral view
What is your diagnosis?
Diagnosis: keratosis punctata of the palmar creases
Keratosis punctata of the palmar creases (KPPC) is a benign, largely asymptomatic condition of the hands, seen almost exclusively those with African ancestry. KPPC presents as small keratotic papules (Figure 3) that evolve into discreet conical pits (Figure 4).1,2 Although KPPC is not a novel or rare condition among African Americans, it is not found in standard dermatology texts used by primary care physicians. However, reference to KPPC may be found in ethnic dermatology texts, including reference to it as “a common normal finding in the black palm.”1
The lesions of KPPC characteristically are 1 to 5 mm in diameter, sharply defined hyperkeratotic pits that occur in the flexural creases of the hands, both on the palms and volar surfaces of the fingers. KPPC has also referred to as keratotic pits of the palmar creases, punctate keratoses of the palmar creases, keratoderma punctata, hyperkeratosis penetrans, lenticular atrophia of the palmar creases, and hyperkeratosis punctata of the palmar creases.
FIGURE 3
Close-up of a “plug”
FIGURE 4
Close-up of a “pit”
Distinguishing KPPC from KPPP
KPPC has also been regarded as a variant of keratosis punctata palmaris et plantaris (KPPP).3,4 KPPP and KPPC share some similarities with respect to the size and number of lesions per palm, probable exacerbation by trauma, and predilection for occurring in those of Afro-Caribbean descent.1,3,4
Historically, there has been some confusion in distinguishing KPPC from KPPP—in fact, it is possible for the 2 conditions to occur simultaneously. The papular lesions of KPPP tend to occur over the entire palm, volar wrist, and medial aspects of the feet. These entities differ in age at onset, prevalence, symptoms, and prognosis.
Sources differ regarding the average age of onset for KPPP; some report onset from infancy to 70 years.5-7 For KPPC, the age of onset generally is between 15 and 40 years.3 Among African Americans, the prevalence of KPPC is between 1.9% and 3.1%,3,6,8 whereas the prevalence of KPPP may be up to 11%.3,4 While KPPP is largely asymptomatic, the lesions of KPPC tend to be noticed more often. Once present, KPPP lesions usually remain stable over time, whereas, KPPC lesions usually increase in number and size.3
Demographics and causes
KPPC is rarely seen in Caucasians. Of 1001 white patients examined for palmar lesions, none fulfilled the diagnostic criteria for KPPC.9 In a study of 534 patients, Weiss et al discovered 7 cases— all in African American patients and representing 3.1% of this racial group.8
The cause of KPPC is unknown. No medications have been implicated, and it has been difficult to link it to a virus.3 Although some authors have suggested that KPPC represents flexural calluses related to manual labor, lesions also occur in patients without this history.1,5 There is no association between KPPC and arsenical agents or syphilis.8
It is generally believed that KPPC does not have a recognizable heritable pattern, though there may be exceptions.8 There may be a familial association with ichthyosis vulgaris and other disorders of keratinization. One report included 5 patients in 1 family with keratotic plugs of the palmar creases consistent with an autosomal dominant pattern of inheritance. The syndrome was associated with ichthyosis vulgaris in several family members.10 KPPP and KPPC might be the result of abnormal callus formation in predisposed individuals, as both conditions seem to be due to an abnormal hyperproliferative response to local trauma.3
Differential diagnosis
Punctate keratoses of the palms are fairly common frequently overlooked lesions. The differential diagnosis is extensive (Table), but there are several clinical features of KPPC that distinguish it from other hyperkeratotic conditions. The lesions of KPPC can be painful, have a predilection for jointcreases, and evolve into pits.3 KPPP is similar except not localized to the creases.4
Aquagenic keratoderma is a transitory condition afflicting young women and defined clinically by the appearance of palmar lesions accentuated after immersion in water. These lesions have a characteristic histological appearance (hyperkeratosis, dilated eccrine ducts).13
Palmoplantar pustulosis is characterized by chronically recurring sterile pustules on the palms and soles, usually found on an erythematous base, and a strong association with tobacco use.14Palmoplantar lichen planus may exhibit a variety of morphologic patterns including papules or plaques with pruritus, erythema, and compact hyperkeratosis.15
Cole disease is an uncommon disorder typified by distinctive cutaneous hyperpigmentation and punctate keratoses on the palms and soles. It is a congenital disease with an autosomal dominant inheritance pattern and phenotypic variability.16
Palmoplantar psoriasis is associated with manual labor in 50% of cases. Lesions are restricted to areas exposed to pressure. All patients with unilateral palmar lesions had them on their dominant hand. Biopsy may be necessary to differentiate hyperkeratotic eczema from psoriasis when just localized to the palms and soles.17
TABLE
Differential diagnosis of punctate keratoses of the hands and feet
| Acquired keratoses | Classic clinical description | Associations |
|---|---|---|
| Arsenical | Round, verrucous, or acuminate keratotic papules most common on palms and soles. Typically occur decades after chronic arsenic ingestion | Angiosarcoma of the liver, nonmelanoma skin cancer, bronchial adenocarcinoma |
| Idiopathic filiform porokeratoses | Multiple thin spiny keratotic projections on palms and soles | Breast, renal, colon, and lung cancer |
| Keratosis punctata of the palmar creases | Discrete, sharply marginated, hyperkeratotic, conical, 1–5 mm depressions confined to flexural creases | Dupuytren’s contracture, striate keratoderma, knuckle pads |
| Hereditary keratoses | Classic clinical description | Associations |
| Keratosis punctata palmoplantaris (type I), Buschke-Fischer-Brauer disease | Multiple 1–2 mm punctate keratoses of the palms and soles | Longitudinal nail dystrophy, lichen nitidus, ichthyosis, atopy, recalcitrant warts. Increased risk of malignancy |
| Spiny keratoderma (type II) | Small keratotic spines over entire palmoplantar surfaces. Resembles the spines of an old-fashioned music box | No predisposition to malignancy |
| Acrokeratoelastoidosis lichenoids (type III) | 2–4 mm round to oval papules on the borders of hands, feet and wrists. May be umbilicated and become confluent | Darier’s disease, Cowden’s disease |
| Adapted from Rustad et al 1990,5 Kong et al 2004,7 Asadi 2003,9 Habif 2004,11 and Osman et al 1992.12 | ||
Treatment options: keratolytic agents may help temporarily
The mainstay of therapy is informing the patient of the benign nature of the diagnosis and avoiding unnecessary and unhelpful therapies and diagnostic modalities. Therapy with keratolytic agents or systemic retinoids may temporarily improve symptoms of KPPC.
However, lesions tend to recur when the medications are stopped or decreased.5,7 Temporizing treatment of symptomatic keratoses, such as applying emollients and paring them, is all that is usually necessary. Systemic retinoids have far too many side effects to consider using in this completely benign condition.
Patient outcome
The patient was reassured by the explanation of the condition and chose to try a keratolytic/emollient agent, Lac-Hydrin, for symptomatic recurrences. At her last visit for another health issue, she has reported this to be helpful.
Acknowledgments
The authors would like to acknowledge the unfailingly cheerful cooperation and expert assistance of the St. Vincent Mercy Medical Center library staff.
Corresponding author
Gary N. Fox, MD, 2200 Jefferson Avenue, Toledo, OH 43624. E-mail: foxgary@yahoo.com.
1. Rosen T, Martin S. Variants of normal skin in blacks. In: Atlas of Black Dermatology. 1st ed. Boston, Mass: Little, Brown; 1981;12-13.
2. Dilaimy MS, Owen WR, Sina B. Keratosis punctata of the palmar creases. Cutis 1984;33:394-396.
3. Rustad OJ, Vance JC. Punctate keratoses of the palms and soles and keratotic pits of the palmar creases. J Am Acad Dermatol 1990;22:468-476.
4. Kinsley-Scott TR, Young RJ, 3rd, Meffert JJ. Keratosis punctata of the instep. Cutis 2003;72:451-452.
5. Kong MS, Harford R, O’Neill JT. Keratosis punctata palmoplantaris controlled with topical retinoids: a case report and review of the literature. Cutis 2004;74:173-179.
6. Anderson WA, Elam MD, Lambert WC. Keratosis punctata and atopy. Report of 31 cases with a prospective study of prevalence. Arch Dermatol 1984;120:884-890.
7. Asadi AK. Type I hereditary punctate keratoderma. Dermatol Online J 2003;9:38.-
8. Weiss RM, Rasmussen JE. Keratosis punctata of the palmar creases. Arch Dermatol 1980;116:669-671.
9. Penas PF, Rios-Buceta L, Sanchez-Perez J, Dorado-Bris JM, Aragues M. Keratosis punctata of the palmar creases: case report and prevalence study in Caucasians. Dermatology 1994;188:200-202.
10. Del-Rio E, Vazquez-Veiga H, Aguilar A, Velez A, Sanchez Yus E. Keratosis punctata of the palmar creases. A report on three generations, demonstrating an association with ichthyosis vulgaris and evidence of involvement of the acrosyringium. Clin Exp Dermatol 1994;19:165-167.
11. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. St. Louis, Mo: Mosby; 2004.
12. Osman Y, Daly TJ, Don PC. Spiny keratoderma of the palms and soles. J Am Acad Dermatol 1992;26:879-881.
13. Betlloch I, Vergara G, Albares MP, Pascual JC, Silvestre JF, Botella R. Aquagenic keratoderma. J Eur Acad Dermatol Venereol 2003;17:306-307.
14. Gimenez-Garcia R, Sanchez-Ramon S, Cuellar-Olmedo LA. Palmoplantar pustulosis: a clinicoepidemiological study. The relationship between tobacco use and thyroid function. J Eur Acad Dermatol Venereol 2003;17:276-279.
15. Gunduz K, Inanir I, Turkdogan P, Sacar H. Palmoplantar lichen planus presenting with vesicle-like papules. J Dermatol 2003;30:337-340. 0
16. Vignale R, Yusin A, Panuncio A, Abulafia J, Reyno Z, Vaglio A. Cole disease: hypopigmentation with punctate keratosis of the palms and soles. Pediatr Dermatol 2002;19:302-306.
17. Kumar B, Saraswat A, Kaur I. Palmoplantar lesions in psoriasis. Acta Derm Venereol 2002;82:192-195.
1. Rosen T, Martin S. Variants of normal skin in blacks. In: Atlas of Black Dermatology. 1st ed. Boston, Mass: Little, Brown; 1981;12-13.
2. Dilaimy MS, Owen WR, Sina B. Keratosis punctata of the palmar creases. Cutis 1984;33:394-396.
3. Rustad OJ, Vance JC. Punctate keratoses of the palms and soles and keratotic pits of the palmar creases. J Am Acad Dermatol 1990;22:468-476.
4. Kinsley-Scott TR, Young RJ, 3rd, Meffert JJ. Keratosis punctata of the instep. Cutis 2003;72:451-452.
5. Kong MS, Harford R, O’Neill JT. Keratosis punctata palmoplantaris controlled with topical retinoids: a case report and review of the literature. Cutis 2004;74:173-179.
6. Anderson WA, Elam MD, Lambert WC. Keratosis punctata and atopy. Report of 31 cases with a prospective study of prevalence. Arch Dermatol 1984;120:884-890.
7. Asadi AK. Type I hereditary punctate keratoderma. Dermatol Online J 2003;9:38.-
8. Weiss RM, Rasmussen JE. Keratosis punctata of the palmar creases. Arch Dermatol 1980;116:669-671.
9. Penas PF, Rios-Buceta L, Sanchez-Perez J, Dorado-Bris JM, Aragues M. Keratosis punctata of the palmar creases: case report and prevalence study in Caucasians. Dermatology 1994;188:200-202.
10. Del-Rio E, Vazquez-Veiga H, Aguilar A, Velez A, Sanchez Yus E. Keratosis punctata of the palmar creases. A report on three generations, demonstrating an association with ichthyosis vulgaris and evidence of involvement of the acrosyringium. Clin Exp Dermatol 1994;19:165-167.
11. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. St. Louis, Mo: Mosby; 2004.
12. Osman Y, Daly TJ, Don PC. Spiny keratoderma of the palms and soles. J Am Acad Dermatol 1992;26:879-881.
13. Betlloch I, Vergara G, Albares MP, Pascual JC, Silvestre JF, Botella R. Aquagenic keratoderma. J Eur Acad Dermatol Venereol 2003;17:306-307.
14. Gimenez-Garcia R, Sanchez-Ramon S, Cuellar-Olmedo LA. Palmoplantar pustulosis: a clinicoepidemiological study. The relationship between tobacco use and thyroid function. J Eur Acad Dermatol Venereol 2003;17:276-279.
15. Gunduz K, Inanir I, Turkdogan P, Sacar H. Palmoplantar lichen planus presenting with vesicle-like papules. J Dermatol 2003;30:337-340. 0
16. Vignale R, Yusin A, Panuncio A, Abulafia J, Reyno Z, Vaglio A. Cole disease: hypopigmentation with punctate keratosis of the palms and soles. Pediatr Dermatol 2002;19:302-306.
17. Kumar B, Saraswat A, Kaur I. Palmoplantar lesions in psoriasis. Acta Derm Venereol 2002;82:192-195.
Facial lesion that came “out of nowhere”
A 33-year-old woman had a facial lesion (Figures 1 and 2) that seemed to “come out of nowhere,” but it was months before she sought medical attention. She was certain that the duration was months, not years, but could not date the exact onset.
The lesion was asymptomatic except for its prominence and aesthetics. The patient had tried cutting the lesion off several times, but it regrew each time. She was married, mono-gamous by history, not pregnant, had no major underlying medical conditions, and had no personal or family history of skin malignancy. The remainder of the skin examination was normal.
FIGURE 1
Facial lesion with sudden onset
FIGURE 2
Detail of the lesion
What is your diagnosis?
What would be your management plan?
Diagnosis: Cutaneous horn
Cutaneous horn,also referred to as cornu cutaneum, is a clinical (morphologic) diagnosis, not a precise pathologic diagnosis. It describes an asymptomatic, projectile, conical, dense, hyperkeratotic lesion that resembles the horn of an animal.
Cutaneous horns can arise from a variety of primary underlying pathologic processes, including benign, premalignant, and malignant lesions. Thus, the important issue when confronted with a cutaneous horn is determining the causative pathologic process. Therefore, for treatment, most authors stress surgical excision with attention to removing the base of the specimen for histopathologic examination.1-4
Cutaneous horns may vary considerably in size and shape. Most are a few millimeters in length, but there are reports of some measuring up to 6 cm in length. They may be perpendicular or inclined in relation to the underlying skin. They usually occur singly and may grow slowly over decades.2,4
Cutaneous horns are more common in older and white individuals, although they have been reported in children and African Americans.5The higher prevalence in older and light-skinned individuals is secondary to the fact that many cutaneous horns are caused by cumulative sun damage over many years, leading to actinic keratoses and nonmelanoma skin cancer.
Differential diagnosis
The differential diagnosis of the underlying causes of cutaneous horns is extensive. Some causes are listed in the Table ; common ones include actinic keratoses (25%–35% of patients with cutaneous horns), verruca vulgaris (15%–25%), and cutaneous malignancies (15%–40%).1
Features that have been reported to increase the chance of an underlying malignancy include older age, male sex, lesion geometry (either alarge base or a large height-to-base ratio), and presence on a sun-exposed location (face, pinnae, dorsal hands and forearms, scalp). More than 70% of cutaneous horns with underlying premalignant or malignant lesions are found on these sun-exposed areas.3,6 Additionally, cutaneous horns on these locations are twice as likely to harbor underlying premalignant or malignant lesions.6 Of patients with malignancies underlying their cutaneous horns, up to one third have a history of skin malignancy.7
TABLE
Some causes of cutaneous horn
| Benign–noninfectious |
| Angiokeratoma |
| Angioma |
| Dermatofibroma |
| Epidermal inclusion cyst (“sebaceous cyst”) |
| Linear verrucous epidermal nevus |
| Fibroma |
| Lichen simplex chronicus (“neurodermatitis”) |
| Lichenoid keratosis |
| Prurigo nodularis |
| Pyogenic granuloma |
| Sebaceous adenoma |
| Seborrheic keratosis |
| Trichilemma |
| Benign–infectious |
| Condyloma acuminata (genital warts) |
| Molluscum contagiosum |
| Verruca vulgaris (common wart) |
| Premalignant/malignant |
| Actinic keratosis |
| Basal cell carcinoma |
| Bowen’s disease |
| Epidermoid carcinoma |
| Kaposi’s sarcoma |
| Keratoacanthoma |
| Malignant melanoma |
| Squamous cell carcinoma |
| Sources: Gould and Brodell 1999,1Akan et al 2001,6 Khaitan 1999.9 |
Treatment options
Cryosurgery
Some textbooks list cryosurgical therapy as an option.8 If there were a clearly benign pre-existing underlying dermopathy, such as verruca vulgaris or molluscum contagiosum, cryosurgery might be considered. However, cryosurgery is destructive; it does not preserve a specimen for pathologic examination. Because cutaneous horns have a 15% to 40% chance of underlying malignancy,1,4 it is difficult to recommend cryosurgical destruction without an initial biopsy-proven diagnosis.
Punch biopsy
In this patient, a 3-mm excisional punch biopsy was performed using a punch-to-ellipse technique. The skin is stretched parallel to the skin lines as the punch biopsy is performed. As the skin relaxes after removal of the punch instrument, an elliptical defect remains, enhancing cosmesis of the repair. Especially for a convex facial surface (which heals less well cosmetically than concave facial surfaces), this technique was believed to offer the potential for a better long-term cosmetic result.
In this case, a shave biopsy would have been a good option for both diagnosis and treatment. If the pathology from a punch biopsy or shave biopsy turned out to demonstrate an underlying skin cancer, then a fusiform excision would be needed to provide adequate surgical margins for the definitive treatment.
Results of histologic exam
With this patient, histologic examination revealed that the underlying condition was verruca vulgaris, or the common wart. Several months after removal of the cutaneous horn, the patient could not locate the surgical site, a cosmetically acceptable result to her and her physician ( Figure 3).
FIGURE 3
After successful treatment
Acknowledgments
The author would like to acknowledge the unfailing cooperation and expert assistance of the St. Vincent Mercy Medical Center library staff.
Correspondence
Gary N. Fox, MD, 2200 Jefferson Avenue, Toledo, OH 43624. E- mail: foxgary@yahoo.com.
1. Gould JW, Brodell RT. Giant cutaneous horn associated with verruca vulgaris. Cutis. 1999;64:111-112.
2. Kastanioudakis I, Skevas A, Assimakopoulos D, Daneilidis B. Cutaneous horn of the auricle. Otolaryngol Head Neck Surg. 1998;118:735.-
3. Korkut T, Tan NB, Oztan Y. Giant cutaneous horn: a patient report. Ann Plast Surg. 1997;39:654-655.
4. Stavroulaki P, Mal RK. Squamous cell carcinoma presenting as a cutaneous horn. Auris Nasus Larynx. 2000;27:277-279.
5. Souza LN, Martins CR, de Paula AM. Cutaneous horn occurring on the lip of a child. Int J Paediatr Dent. 2003;13:365-367.
6. Akan M, Yildirim S, Avci G, Akoz T. Xeroderma pigmento sum with a giant cutaneous horn. Ann Plast Surg. 2001;46:665-666.
7. Spira J, Rabinovitz H. Cutaneous horn present for two months. Dermatol Online J. 2000;6:11.-
8. Benignkin tumors (Chapter 20)Cutaneous horn. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. St. Louis, Mo: Mosby; 2004;706.:
9. Khaitan BK, Sood A, Singh MK. Lichen simplex chronicus with a cutaneous horn. Acta Derm Venereol. 1999;79:243.-
10. Agarwalla A, Agrawal CS, Thakur A, et al. Cutaneous horn on condyloma acuminatum. Acta Derm Venereol. 2000;80:159.
A 33-year-old woman had a facial lesion (Figures 1 and 2) that seemed to “come out of nowhere,” but it was months before she sought medical attention. She was certain that the duration was months, not years, but could not date the exact onset.
The lesion was asymptomatic except for its prominence and aesthetics. The patient had tried cutting the lesion off several times, but it regrew each time. She was married, mono-gamous by history, not pregnant, had no major underlying medical conditions, and had no personal or family history of skin malignancy. The remainder of the skin examination was normal.
FIGURE 1
Facial lesion with sudden onset
FIGURE 2
Detail of the lesion
What is your diagnosis?
What would be your management plan?
Diagnosis: Cutaneous horn
Cutaneous horn,also referred to as cornu cutaneum, is a clinical (morphologic) diagnosis, not a precise pathologic diagnosis. It describes an asymptomatic, projectile, conical, dense, hyperkeratotic lesion that resembles the horn of an animal.
Cutaneous horns can arise from a variety of primary underlying pathologic processes, including benign, premalignant, and malignant lesions. Thus, the important issue when confronted with a cutaneous horn is determining the causative pathologic process. Therefore, for treatment, most authors stress surgical excision with attention to removing the base of the specimen for histopathologic examination.1-4
Cutaneous horns may vary considerably in size and shape. Most are a few millimeters in length, but there are reports of some measuring up to 6 cm in length. They may be perpendicular or inclined in relation to the underlying skin. They usually occur singly and may grow slowly over decades.2,4
Cutaneous horns are more common in older and white individuals, although they have been reported in children and African Americans.5The higher prevalence in older and light-skinned individuals is secondary to the fact that many cutaneous horns are caused by cumulative sun damage over many years, leading to actinic keratoses and nonmelanoma skin cancer.
Differential diagnosis
The differential diagnosis of the underlying causes of cutaneous horns is extensive. Some causes are listed in the Table ; common ones include actinic keratoses (25%–35% of patients with cutaneous horns), verruca vulgaris (15%–25%), and cutaneous malignancies (15%–40%).1
Features that have been reported to increase the chance of an underlying malignancy include older age, male sex, lesion geometry (either alarge base or a large height-to-base ratio), and presence on a sun-exposed location (face, pinnae, dorsal hands and forearms, scalp). More than 70% of cutaneous horns with underlying premalignant or malignant lesions are found on these sun-exposed areas.3,6 Additionally, cutaneous horns on these locations are twice as likely to harbor underlying premalignant or malignant lesions.6 Of patients with malignancies underlying their cutaneous horns, up to one third have a history of skin malignancy.7
TABLE
Some causes of cutaneous horn
| Benign–noninfectious |
| Angiokeratoma |
| Angioma |
| Dermatofibroma |
| Epidermal inclusion cyst (“sebaceous cyst”) |
| Linear verrucous epidermal nevus |
| Fibroma |
| Lichen simplex chronicus (“neurodermatitis”) |
| Lichenoid keratosis |
| Prurigo nodularis |
| Pyogenic granuloma |
| Sebaceous adenoma |
| Seborrheic keratosis |
| Trichilemma |
| Benign–infectious |
| Condyloma acuminata (genital warts) |
| Molluscum contagiosum |
| Verruca vulgaris (common wart) |
| Premalignant/malignant |
| Actinic keratosis |
| Basal cell carcinoma |
| Bowen’s disease |
| Epidermoid carcinoma |
| Kaposi’s sarcoma |
| Keratoacanthoma |
| Malignant melanoma |
| Squamous cell carcinoma |
| Sources: Gould and Brodell 1999,1Akan et al 2001,6 Khaitan 1999.9 |
Treatment options
Cryosurgery
Some textbooks list cryosurgical therapy as an option.8 If there were a clearly benign pre-existing underlying dermopathy, such as verruca vulgaris or molluscum contagiosum, cryosurgery might be considered. However, cryosurgery is destructive; it does not preserve a specimen for pathologic examination. Because cutaneous horns have a 15% to 40% chance of underlying malignancy,1,4 it is difficult to recommend cryosurgical destruction without an initial biopsy-proven diagnosis.
Punch biopsy
In this patient, a 3-mm excisional punch biopsy was performed using a punch-to-ellipse technique. The skin is stretched parallel to the skin lines as the punch biopsy is performed. As the skin relaxes after removal of the punch instrument, an elliptical defect remains, enhancing cosmesis of the repair. Especially for a convex facial surface (which heals less well cosmetically than concave facial surfaces), this technique was believed to offer the potential for a better long-term cosmetic result.
In this case, a shave biopsy would have been a good option for both diagnosis and treatment. If the pathology from a punch biopsy or shave biopsy turned out to demonstrate an underlying skin cancer, then a fusiform excision would be needed to provide adequate surgical margins for the definitive treatment.
Results of histologic exam
With this patient, histologic examination revealed that the underlying condition was verruca vulgaris, or the common wart. Several months after removal of the cutaneous horn, the patient could not locate the surgical site, a cosmetically acceptable result to her and her physician ( Figure 3).
FIGURE 3
After successful treatment
Acknowledgments
The author would like to acknowledge the unfailing cooperation and expert assistance of the St. Vincent Mercy Medical Center library staff.
Correspondence
Gary N. Fox, MD, 2200 Jefferson Avenue, Toledo, OH 43624. E- mail: foxgary@yahoo.com.
A 33-year-old woman had a facial lesion (Figures 1 and 2) that seemed to “come out of nowhere,” but it was months before she sought medical attention. She was certain that the duration was months, not years, but could not date the exact onset.
The lesion was asymptomatic except for its prominence and aesthetics. The patient had tried cutting the lesion off several times, but it regrew each time. She was married, mono-gamous by history, not pregnant, had no major underlying medical conditions, and had no personal or family history of skin malignancy. The remainder of the skin examination was normal.
FIGURE 1
Facial lesion with sudden onset
FIGURE 2
Detail of the lesion
What is your diagnosis?
What would be your management plan?
Diagnosis: Cutaneous horn
Cutaneous horn,also referred to as cornu cutaneum, is a clinical (morphologic) diagnosis, not a precise pathologic diagnosis. It describes an asymptomatic, projectile, conical, dense, hyperkeratotic lesion that resembles the horn of an animal.
Cutaneous horns can arise from a variety of primary underlying pathologic processes, including benign, premalignant, and malignant lesions. Thus, the important issue when confronted with a cutaneous horn is determining the causative pathologic process. Therefore, for treatment, most authors stress surgical excision with attention to removing the base of the specimen for histopathologic examination.1-4
Cutaneous horns may vary considerably in size and shape. Most are a few millimeters in length, but there are reports of some measuring up to 6 cm in length. They may be perpendicular or inclined in relation to the underlying skin. They usually occur singly and may grow slowly over decades.2,4
Cutaneous horns are more common in older and white individuals, although they have been reported in children and African Americans.5The higher prevalence in older and light-skinned individuals is secondary to the fact that many cutaneous horns are caused by cumulative sun damage over many years, leading to actinic keratoses and nonmelanoma skin cancer.
Differential diagnosis
The differential diagnosis of the underlying causes of cutaneous horns is extensive. Some causes are listed in the Table ; common ones include actinic keratoses (25%–35% of patients with cutaneous horns), verruca vulgaris (15%–25%), and cutaneous malignancies (15%–40%).1
Features that have been reported to increase the chance of an underlying malignancy include older age, male sex, lesion geometry (either alarge base or a large height-to-base ratio), and presence on a sun-exposed location (face, pinnae, dorsal hands and forearms, scalp). More than 70% of cutaneous horns with underlying premalignant or malignant lesions are found on these sun-exposed areas.3,6 Additionally, cutaneous horns on these locations are twice as likely to harbor underlying premalignant or malignant lesions.6 Of patients with malignancies underlying their cutaneous horns, up to one third have a history of skin malignancy.7
TABLE
Some causes of cutaneous horn
| Benign–noninfectious |
| Angiokeratoma |
| Angioma |
| Dermatofibroma |
| Epidermal inclusion cyst (“sebaceous cyst”) |
| Linear verrucous epidermal nevus |
| Fibroma |
| Lichen simplex chronicus (“neurodermatitis”) |
| Lichenoid keratosis |
| Prurigo nodularis |
| Pyogenic granuloma |
| Sebaceous adenoma |
| Seborrheic keratosis |
| Trichilemma |
| Benign–infectious |
| Condyloma acuminata (genital warts) |
| Molluscum contagiosum |
| Verruca vulgaris (common wart) |
| Premalignant/malignant |
| Actinic keratosis |
| Basal cell carcinoma |
| Bowen’s disease |
| Epidermoid carcinoma |
| Kaposi’s sarcoma |
| Keratoacanthoma |
| Malignant melanoma |
| Squamous cell carcinoma |
| Sources: Gould and Brodell 1999,1Akan et al 2001,6 Khaitan 1999.9 |
Treatment options
Cryosurgery
Some textbooks list cryosurgical therapy as an option.8 If there were a clearly benign pre-existing underlying dermopathy, such as verruca vulgaris or molluscum contagiosum, cryosurgery might be considered. However, cryosurgery is destructive; it does not preserve a specimen for pathologic examination. Because cutaneous horns have a 15% to 40% chance of underlying malignancy,1,4 it is difficult to recommend cryosurgical destruction without an initial biopsy-proven diagnosis.
Punch biopsy
In this patient, a 3-mm excisional punch biopsy was performed using a punch-to-ellipse technique. The skin is stretched parallel to the skin lines as the punch biopsy is performed. As the skin relaxes after removal of the punch instrument, an elliptical defect remains, enhancing cosmesis of the repair. Especially for a convex facial surface (which heals less well cosmetically than concave facial surfaces), this technique was believed to offer the potential for a better long-term cosmetic result.
In this case, a shave biopsy would have been a good option for both diagnosis and treatment. If the pathology from a punch biopsy or shave biopsy turned out to demonstrate an underlying skin cancer, then a fusiform excision would be needed to provide adequate surgical margins for the definitive treatment.
Results of histologic exam
With this patient, histologic examination revealed that the underlying condition was verruca vulgaris, or the common wart. Several months after removal of the cutaneous horn, the patient could not locate the surgical site, a cosmetically acceptable result to her and her physician ( Figure 3).
FIGURE 3
After successful treatment
Acknowledgments
The author would like to acknowledge the unfailing cooperation and expert assistance of the St. Vincent Mercy Medical Center library staff.
Correspondence
Gary N. Fox, MD, 2200 Jefferson Avenue, Toledo, OH 43624. E- mail: foxgary@yahoo.com.
1. Gould JW, Brodell RT. Giant cutaneous horn associated with verruca vulgaris. Cutis. 1999;64:111-112.
2. Kastanioudakis I, Skevas A, Assimakopoulos D, Daneilidis B. Cutaneous horn of the auricle. Otolaryngol Head Neck Surg. 1998;118:735.-
3. Korkut T, Tan NB, Oztan Y. Giant cutaneous horn: a patient report. Ann Plast Surg. 1997;39:654-655.
4. Stavroulaki P, Mal RK. Squamous cell carcinoma presenting as a cutaneous horn. Auris Nasus Larynx. 2000;27:277-279.
5. Souza LN, Martins CR, de Paula AM. Cutaneous horn occurring on the lip of a child. Int J Paediatr Dent. 2003;13:365-367.
6. Akan M, Yildirim S, Avci G, Akoz T. Xeroderma pigmento sum with a giant cutaneous horn. Ann Plast Surg. 2001;46:665-666.
7. Spira J, Rabinovitz H. Cutaneous horn present for two months. Dermatol Online J. 2000;6:11.-
8. Benignkin tumors (Chapter 20)Cutaneous horn. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. St. Louis, Mo: Mosby; 2004;706.:
9. Khaitan BK, Sood A, Singh MK. Lichen simplex chronicus with a cutaneous horn. Acta Derm Venereol. 1999;79:243.-
10. Agarwalla A, Agrawal CS, Thakur A, et al. Cutaneous horn on condyloma acuminatum. Acta Derm Venereol. 2000;80:159.
1. Gould JW, Brodell RT. Giant cutaneous horn associated with verruca vulgaris. Cutis. 1999;64:111-112.
2. Kastanioudakis I, Skevas A, Assimakopoulos D, Daneilidis B. Cutaneous horn of the auricle. Otolaryngol Head Neck Surg. 1998;118:735.-
3. Korkut T, Tan NB, Oztan Y. Giant cutaneous horn: a patient report. Ann Plast Surg. 1997;39:654-655.
4. Stavroulaki P, Mal RK. Squamous cell carcinoma presenting as a cutaneous horn. Auris Nasus Larynx. 2000;27:277-279.
5. Souza LN, Martins CR, de Paula AM. Cutaneous horn occurring on the lip of a child. Int J Paediatr Dent. 2003;13:365-367.
6. Akan M, Yildirim S, Avci G, Akoz T. Xeroderma pigmento sum with a giant cutaneous horn. Ann Plast Surg. 2001;46:665-666.
7. Spira J, Rabinovitz H. Cutaneous horn present for two months. Dermatol Online J. 2000;6:11.-
8. Benignkin tumors (Chapter 20)Cutaneous horn. In: Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th ed. St. Louis, Mo: Mosby; 2004;706.:
9. Khaitan BK, Sood A, Singh MK. Lichen simplex chronicus with a cutaneous horn. Acta Derm Venereol. 1999;79:243.-
10. Agarwalla A, Agrawal CS, Thakur A, et al. Cutaneous horn on condyloma acuminatum. Acta Derm Venereol. 2000;80:159.
FIRSTConsult: A useful point-of-care clinical reference
Unquestionably, using electronic information sources at the bedside has the potential to improve the quality of clinical care. That potential is moving closer to realization with FIRSTConsult (formerly PDxMD)—a multifunction physician resource designed for point-of-care use. Its name reflects its connection with MDConsult, the well-known electronic collection of textbooks. Both are produced by Elsevier, whose imprints include Saunders, Mosby, and Churchill Livingstone, and whose publications include Dorland’s Medical Dictionary, Gray’s Anatomy, Harriet Lane Handbook, and The Lancet.
FIRSTConsult comes in 2 incarnations: a Web-based version and a handheld version. The latter is available both for the Palm and Pocket PC operating systems, with variants of about 2, 6, and 10 MB. We evaluated the Web version (hereafter “FC-Web”) and the 10-MB Palm OS version (“FC-Palm”). Descriptions of the smaller versions are available on the FIRSTConsult web site.
As long as a user has access to a high-speed Internet connection, we give FC-Web a “thumbs up” as a rapid, real-time, point-of-care resource. FC-Palm is a portable mini-version of the Medical Conditions and Differential Diagnosis sections of FC-Web. In this article, we detail the advantages and disadvantages of both products.
FC-Web
FC-Web’s opening screen (Figure 1) lists its 5 major components, along with a search box that scans all components simultaneously. Searching “tinea,” for example, produces 529 retrievals (Figure 2). Users may modify search parameters with check boxes and drop-down lists.
FIGURE 1
FIRSTConsult’s opening screen
FIGURE 2
Typical FIRSTConsult search screen
Information retrieval with FC-Web
Clicking one of FC-Web’s components opens a search function or an alphabetic list to locate the desired monograph (Figure 3).
Improved search function. The search function for FC-Web is profoundly improved from that of its predecessor, PDxMD. The search retrievals include section titles (eg, Summary, Background, Diagnosis; see Figure 2), allowing users to link directly to the subject of interest. There is extensive mapping by synonyms, such that “AAA” finds “abdominal aortic aneurysm” and “TIA” finds “transient ischemic attack.” The search feature does not take wild cards or partial words and is intolerant to misspelling (eg, “vonWillebrand” vs “von Willebrand”).
Useful hyperlinks. FC-Web has extensive hyperlinks within its monographs and sections and to other components of the program, and they are among the most useful and logical links these reviewers have seen. Additionally, the program contains hyperlinks to MDConsult (for MDConsult subscribers only) and to excellent external resources, such as consensus statements. Where applicable, levels of evidence and references are cited.
Drawbacks. Regarding speed, we believe FC-Web requires high-speed access for true point-of-care use. FC-Web limits users to 1 open window—even hyperlinks to external sources cannot be opened in new windows.
FIGURE 3
Medical Conditions
Differential diagnosis section
This section provides differential diagnoses—broken into categories by patient age—for about 350 symptoms and signs. The search feature maps to close entries. For example, clicking on Differential Diagnosis and entering the search term “burping,” FC-Web maps to flatulence, eructation, and gas pain. Interestingly, some of the more common causes we see for burping in practice—anxiety/aerophagia, ingestion of dissolved gas (carbonated beverages), and ingestion of bicarbonate—do not appear.
For any condition found on the Differential Diagnosis monograph summary screens, a click pulls up a mini-summary of the illness, nicely leveraging the electronic environment (Figure 4). Users can click through to corresponding FC-Web disease monographs (if available) or to the topic in MDConsult (separate subscription required).
Limitations. Unlike differential diagnosis engines such as DXplain (available at www.lcs.mgh.harvard.edu/dxplain.htm), the Differential Diagnosis section of FC-Web does not allow users to enter sets of data (eg, age; sex; findings) to produce a list of possible diagnoses. Surprisingly, FC-web’s Differential section does not include “hyponatremia” (or “SIADH”), although it contains such things as “hypernasality” and “hypogeusia.”
FIGURE 4
Summary of a Differential Diagnosis
Patient handouts
FC-Web contains more than 450 patient education monographs.
The monographs have 3 main tabs. The first 2—View English and View Spanish—have drop-down menus offering handout choices of “Diagnosed Patient” and “General Information.” The third tab, Actions, allows users to customize handouts (add physician’s name, patient’s name, personalized instructions, etc). Defaults can be saved. Printouts are about 3 “airy” pages with liberal use of white space, large type, and bullet points. They are very basic and easy to read.
Handout deficiencies. Inexplicably, hepatitis A and B are included, but not hepatitis C, which would be the most useful information for our practices.
Occasional minor discrepancies exist between handouts and disease monographs. For example, the Acute Upper Respiratory Tract Infection handout says nothing about echinacea or zinc. However, the related monograph states “Echinacea and zinc supplements may be effective in reducing the duration and severity of common cold symptoms.”
Procedure files
Procedure Files contains 30 to 40 procedure monographs, including video clip illustrations of key portions; users have a choice of viewing these with Windows Media Player, RealPlayer, or QuickTime. Reference Centers contains 3 monographs: “Bioterrorism,” “Contraception,” and “Pregnancy” (as of May 2004). Although few in number, these Reference Centers are valuable point-of-care tools.
Medical conditions
We would expect Medical Conditions to be the workhorse section for most physicians. FC-Web advertises that it contains more than 450 conditions.
Rapid access to information. The best feature of this core section is its organization of information—eminently logical, extremely easy to navigate, bulleted, and extensively hyperlinked, taking full advantage of the e-medium.
To illustrate the outstanding layout and hyperlinking, if a user floats the cursor over a tab (eg, Diagnosis or Treatment) in a disease monograph, a menu of subsections drops down (Figure 5). Floating the cursor over some subsections produces a menu of additional options within that subsection. Furthermore, once selected, the resulting information is often extensively hyperlinked to related or more detailed information.
Generic drug names only. Throughout, FIRSTConsult sticks to generic drug names; if the user is uncertain what cefdinir or tamsulosin is, FIRSTConsult will offer no help.
Generous detail. In terms of content, Medical Conditions distills information into bullet points. FC-Web has more depth than, for example, Griffith’s 5-Minute Consult. Also, as a Web-based tool, FC-Web categorizes information multi-dimensionally with the horizontal main tabs plus drop-down, floating subcategories, allowing expeditious jumps to desired information. This organization facilitates rapid access to information.
Superb summary for point-of-care use. The Summary of Therapeutic Options subcategory of the Treatment section is particular noteworthy—an outstanding feature for busy clinicians—and concrete evidence that FC-Web was truly designed with point-of-care in mind. In this subsection, options are listed by bullet points and very briefly described (1 or 2 lines), which allows easy visual scanning. Each option (eg, medication) is then hyperlinked to its more detailed description (eg, dosage, route, etc) in the section, Drugs and Other Therapies: Details.
Sometimes, FC-Web fails to provide “drug of choice” recommendations, listing interventions randomly, which hinders rapid, point-of-care decision-making.
FIGURE 5
Typical FIRSTConsult monograph
Putting FC-Web to the test
FC-Web answered all general questions for which a monograph existed:
- What is the preferred therapy for head lice? (“Permethrin: … Treatment of choice for uncomplicated pediculosis.”)
- At what aneurysm diameter should a patient with an abdominal aortic aneurysm be referred? (“In general, patients with aneurysms larger than 5 cm in diameter, symptomatic aneurysms, or rapidly enlarging aneurysms should be considered for repair. Treatment for aneurysms between 4 and 5 cm is controversial.”)
- What is the basic workup for kidney stones?
- What are the indications for and monitoring of hydroxyurea for adults with sickle cell anemia?
- What are the therapeutic options for mycobacterium avium complex in an HIV-positive patient?
- How should one follow pulmonary sarcoid when tapering steroids? (A link to an external guideline was especially informative.)
Surprising shortcomings. FC-Web’s Medical Conditions section includes some less common entities—restless legs syndrome, Osgood-Schlatter’s disease, for example—but no monographs are devoted to conditions such as SIADH, paroxysmal supraventricular tachycardia, or portal or pulmonary hypertension.
Contact Information
FIRSTConsult, Customer Services, open Monday to Friday, 7:30 am to 7:00 pm Central Time; 1-800-401-9962. Web site: www.FIRSTConsult.com; e-mail contact available through web site, including subscription information.
Pricing
Physicians: $149; $109 if MDConsult subscription also purchased separately.
Residents/Students: $89
Price includes 1 year of Web access and hand-held updates; components are not available separately. After 1 year, hand-held content continues to function (not “time-bombed”) but renewal necessary for updates. Discount pricing available for groups of as few as 2 individuals.
30-day free trial of Web content with registration at www.FIRSTConsult.com. Free trial of partially functional handheld content through handheld link.
Minimum Requirements
Desktop: Windows PC with Windows 95; Macintosh PC with OS 9; Internet connection; Internet Explorer version 5.0 or Netscape version 6.2.
Palm-OS handheld devices: PalmOS version 3.5.3 with 4 MB of RAM, Palm Desktop 4.0. Additional memory or memory expansion card necessary to run larger products.
Pocket PC handheld devices: Pocket PC with ActiveSync (installed on the desktop computer); 32MB RAM; StrongARM processor.
Despite the evidence and reference citations, there were times we took issue with FC-Web. For example, FC-Web indicates the dosage of amoxicillin for otitis media in children older than 3 months is “25–45 mg/kg/day orally in divided doses (maximum dose 80 mg/kg/day).” In response to the rapid dissemination of drugresistant Streptococcus pneumoniae, the Centers for Disease Control has recommended, in general, that “the initial dose of amoxicillin should be increased from 40 to 45 mg/kg/day to 80 to 90 mg/kg/day.” Also, there are occasional disconnects within monographs. Under “Tinea Infections” in both the Summary and Diagnosis sections is a “Key! Don’t Miss Points” that says: “Patients with HIV infection may have severe onychomycosis and Malassezia folliculitis (pustular hair follicle infection).” However, no mention is made of how to treat Malassezia folliculitis.
Head-to-head with UpToDate. Compared with UpToDate [see “UpToDate: A comprehensive clinical database,” J Fam Pract 2003; 52(9):706–710], FC-Web obviously has been designed from a point-of-care focus. With UpToDate it is often laborious to cull key clinical information at the point-of-care. FC-Web is much less encyclopedic, has a superb layout, and whiz-click access to such amenities as the “Summary of therapeutic options”—with hyperlinking to details if needed.
Although FC-Web has no “history” or “favorites” functions, it is seldom a problem relocating information because of the simplicity of its design (unlike the complex paths one often follows in UpToDate to locate information).
FC-Web’s patient education monographs are more accessible, shorter, and at the opposite literacy extreme from UpToDate’s.
FC-Palm
FIRSTConsult versions for handhelds are available for download with purchase. On the Palm, users must first download and install FC’s EReader, a 90K application. Both EReader and FC-Palm easily load to memory cards and function briskly on recommended versions of Palm OS devices. However, “crashes” are common (and, in some instances, fully reproducible), requiring soft resets of the handheld device.
Shortcomings of the FC-Palm
FC-Palm’s opening screen lists its 2 components, Differential Diagnosis and Medical Conditions. (The other sections are not included in the handheld versions).
One noteworthy peculiarity with EReader is that, if the user presses the Palm’s off button, it exits the application but does not turn off the Palm. The user must press the button a second time to turn off the Palm. Similarly, at the user’s set “time out” (eg, after 2 minutes of inactivity), first FC-Palm/EReader times out, and only then does the countdown begin for the Palm to time out and turn off. Once users are forewarned, this is unlikely to be a problem, but we are not familiar with any other Palm application that exhibits this behavior.
Another curiosity: when FC-Palm times out, it does not resume where it exited. Users must retrace their steps to continue.
Levels of evidence are not included in FC-Palm. Elsevier indicates FC-Palm is updated approximately weekly. Unfortunately, there is no auto-update feature. Updating the 10MB version is time-consuming, particularly hot-syncing to a Palm card (and, if using dial-up connection, downloading), making it unlikely users would update frequently.
FC-Palm has no search function, and, interestingly, Palm’s search feature appears nonfunctional with this program.
Many medical handheld applications, ePocrates for example, employ lists that scroll alphabetically as users enter successive letters, such that entering “c,” “o,” and “l” would automatically scroll to the first listing under “c,” then under “co,” then under “col,” and so on. FC-Palm does not have this feature. Instead, it must be navigated by selecting a letter of the alphabet from the top of the screen (eg, R for Restless Legs), and then scrolling to the entry (via slide bar or Palm buttons) (Figure 6).
There are no icons or shortcuts to frequently used features (eg, “T” to jump to Therapy). Once in an entry, FC-Palm users navigate with a drop-down list to the section of interest. Each section is separate and can be entered only with the drop-down list (Figure 7).
No user-defined preferences are available to select FC-Palm’s monographs’ opening section (eg, Therapeutics).
Conveniently, FC-Palm has forward and back browser-type navigation controls.
Generic drug names are used throughout.
Comparing handheld versions, FIRSTConsult weighs in at 10 MB as opposed to UpToDate’s 800 MB—which may reflect upon the ease and speed of finding information at the point-of-care.
FIGURE 6
Navigating the Palm version
FIGURE 7
Selecting a topic in FC-Palm
Differential diagnosis
In content, FC-Palm’s Differential Diagnosis section is similar to that of FC-Web, except index listings appear only once (eg, “increased tearing, abnormal”) as opposed to appearing under all permutations in FC-Web’s index (eg, under “abnormal,” “increased,” and “tearing”). FC-Palm also employs extensive hyperlinking. Selecting “Incontinence, urinary” produces its differential; tapping “benign prostatic hypertrophy” in the resultant list produces a disease summary, with a link to the corresponding monograph in the Medical Conditions section.
The Differential Diagnosis section does not contain “hyponatremia,” but the Medical Conditions section does. Under the subheading Drugs and Other Therapies, only 2 therapies are listed—demeclocycline and fludrocortisone. There is no mention of water restriction (SIADH) or volume replacement (hypovolemia) per se—just drugs. In contrast, FC-Web’s comparable monograph incorporates volume replacement and free water restriction but only includes the issue of “urgent” volume replacement in the Immediate Action section, not in the important Summary of Therapeutic Options section.
Similarly, FC-Web’s monograph nicely summarizes drug options for pelvic inflammatory disease, but FC-Palm simply provides a listing of individual drugs without any hints about the appropriate combinations—significantly compromising users’ ability to quickly select therapy at point of care.
FC-Palm falls short of the mark for gonorrhea in the same way. The therapeutics screen simply lists 10 drugs (all hyperlinked to further information) without any hints as to recommended or preferred choices. In fact, hyperlinking to further information on ceftriaxone, the Centers for Disease Control’s recommended therapy in pregnancy, one finds the oxymoronic “Use caution in pregnancy (category B),” which might lead a neophyte on a search for the Holy Grail (ie, the nonexistent “better” drug for use in pregnancy).
Final word on firstconsult
FC-Web is well laid out and, using a high-speed connection, functional for point-of-care use, offering sufficiently detailed and extensively hyperlinked disease monographs. For the most common diseases, key questions are generally answered efficiently and in a manner consistent with current evidence or thought. As a bonus, FC-Web provides basic patient education handouts in English and Spanish.
FC-Palm lacks state-of-the-art navigation and search capabilities. FC-Web’s outstanding Summary of Therapeutic Options sections have been gutted in FC-Palm to be substantially less helpful—and potentially misleading—lists of non-prioritized therapies (primarily drugs).
Before we can recommend it as a prime-time handheld application, FC-Palm needs to upgrade its Therapeutics section to be equivalent to FC-Web’s Summary of Therapeutic Options; it should also remedy the nonstandard behaviors, improve navigation, add search options and some user preferences, and incorporate an auto-update feature.
Unquestionably, using electronic information sources at the bedside has the potential to improve the quality of clinical care. That potential is moving closer to realization with FIRSTConsult (formerly PDxMD)—a multifunction physician resource designed for point-of-care use. Its name reflects its connection with MDConsult, the well-known electronic collection of textbooks. Both are produced by Elsevier, whose imprints include Saunders, Mosby, and Churchill Livingstone, and whose publications include Dorland’s Medical Dictionary, Gray’s Anatomy, Harriet Lane Handbook, and The Lancet.
FIRSTConsult comes in 2 incarnations: a Web-based version and a handheld version. The latter is available both for the Palm and Pocket PC operating systems, with variants of about 2, 6, and 10 MB. We evaluated the Web version (hereafter “FC-Web”) and the 10-MB Palm OS version (“FC-Palm”). Descriptions of the smaller versions are available on the FIRSTConsult web site.
As long as a user has access to a high-speed Internet connection, we give FC-Web a “thumbs up” as a rapid, real-time, point-of-care resource. FC-Palm is a portable mini-version of the Medical Conditions and Differential Diagnosis sections of FC-Web. In this article, we detail the advantages and disadvantages of both products.
FC-Web
FC-Web’s opening screen (Figure 1) lists its 5 major components, along with a search box that scans all components simultaneously. Searching “tinea,” for example, produces 529 retrievals (Figure 2). Users may modify search parameters with check boxes and drop-down lists.
FIGURE 1
FIRSTConsult’s opening screen
FIGURE 2
Typical FIRSTConsult search screen
Information retrieval with FC-Web
Clicking one of FC-Web’s components opens a search function or an alphabetic list to locate the desired monograph (Figure 3).
Improved search function. The search function for FC-Web is profoundly improved from that of its predecessor, PDxMD. The search retrievals include section titles (eg, Summary, Background, Diagnosis; see Figure 2), allowing users to link directly to the subject of interest. There is extensive mapping by synonyms, such that “AAA” finds “abdominal aortic aneurysm” and “TIA” finds “transient ischemic attack.” The search feature does not take wild cards or partial words and is intolerant to misspelling (eg, “vonWillebrand” vs “von Willebrand”).
Useful hyperlinks. FC-Web has extensive hyperlinks within its monographs and sections and to other components of the program, and they are among the most useful and logical links these reviewers have seen. Additionally, the program contains hyperlinks to MDConsult (for MDConsult subscribers only) and to excellent external resources, such as consensus statements. Where applicable, levels of evidence and references are cited.
Drawbacks. Regarding speed, we believe FC-Web requires high-speed access for true point-of-care use. FC-Web limits users to 1 open window—even hyperlinks to external sources cannot be opened in new windows.
FIGURE 3
Medical Conditions
Differential diagnosis section
This section provides differential diagnoses—broken into categories by patient age—for about 350 symptoms and signs. The search feature maps to close entries. For example, clicking on Differential Diagnosis and entering the search term “burping,” FC-Web maps to flatulence, eructation, and gas pain. Interestingly, some of the more common causes we see for burping in practice—anxiety/aerophagia, ingestion of dissolved gas (carbonated beverages), and ingestion of bicarbonate—do not appear.
For any condition found on the Differential Diagnosis monograph summary screens, a click pulls up a mini-summary of the illness, nicely leveraging the electronic environment (Figure 4). Users can click through to corresponding FC-Web disease monographs (if available) or to the topic in MDConsult (separate subscription required).
Limitations. Unlike differential diagnosis engines such as DXplain (available at www.lcs.mgh.harvard.edu/dxplain.htm), the Differential Diagnosis section of FC-Web does not allow users to enter sets of data (eg, age; sex; findings) to produce a list of possible diagnoses. Surprisingly, FC-web’s Differential section does not include “hyponatremia” (or “SIADH”), although it contains such things as “hypernasality” and “hypogeusia.”
FIGURE 4
Summary of a Differential Diagnosis
Patient handouts
FC-Web contains more than 450 patient education monographs.
The monographs have 3 main tabs. The first 2—View English and View Spanish—have drop-down menus offering handout choices of “Diagnosed Patient” and “General Information.” The third tab, Actions, allows users to customize handouts (add physician’s name, patient’s name, personalized instructions, etc). Defaults can be saved. Printouts are about 3 “airy” pages with liberal use of white space, large type, and bullet points. They are very basic and easy to read.
Handout deficiencies. Inexplicably, hepatitis A and B are included, but not hepatitis C, which would be the most useful information for our practices.
Occasional minor discrepancies exist between handouts and disease monographs. For example, the Acute Upper Respiratory Tract Infection handout says nothing about echinacea or zinc. However, the related monograph states “Echinacea and zinc supplements may be effective in reducing the duration and severity of common cold symptoms.”
Procedure files
Procedure Files contains 30 to 40 procedure monographs, including video clip illustrations of key portions; users have a choice of viewing these with Windows Media Player, RealPlayer, or QuickTime. Reference Centers contains 3 monographs: “Bioterrorism,” “Contraception,” and “Pregnancy” (as of May 2004). Although few in number, these Reference Centers are valuable point-of-care tools.
Medical conditions
We would expect Medical Conditions to be the workhorse section for most physicians. FC-Web advertises that it contains more than 450 conditions.
Rapid access to information. The best feature of this core section is its organization of information—eminently logical, extremely easy to navigate, bulleted, and extensively hyperlinked, taking full advantage of the e-medium.
To illustrate the outstanding layout and hyperlinking, if a user floats the cursor over a tab (eg, Diagnosis or Treatment) in a disease monograph, a menu of subsections drops down (Figure 5). Floating the cursor over some subsections produces a menu of additional options within that subsection. Furthermore, once selected, the resulting information is often extensively hyperlinked to related or more detailed information.
Generic drug names only. Throughout, FIRSTConsult sticks to generic drug names; if the user is uncertain what cefdinir or tamsulosin is, FIRSTConsult will offer no help.
Generous detail. In terms of content, Medical Conditions distills information into bullet points. FC-Web has more depth than, for example, Griffith’s 5-Minute Consult. Also, as a Web-based tool, FC-Web categorizes information multi-dimensionally with the horizontal main tabs plus drop-down, floating subcategories, allowing expeditious jumps to desired information. This organization facilitates rapid access to information.
Superb summary for point-of-care use. The Summary of Therapeutic Options subcategory of the Treatment section is particular noteworthy—an outstanding feature for busy clinicians—and concrete evidence that FC-Web was truly designed with point-of-care in mind. In this subsection, options are listed by bullet points and very briefly described (1 or 2 lines), which allows easy visual scanning. Each option (eg, medication) is then hyperlinked to its more detailed description (eg, dosage, route, etc) in the section, Drugs and Other Therapies: Details.
Sometimes, FC-Web fails to provide “drug of choice” recommendations, listing interventions randomly, which hinders rapid, point-of-care decision-making.
FIGURE 5
Typical FIRSTConsult monograph
Putting FC-Web to the test
FC-Web answered all general questions for which a monograph existed:
- What is the preferred therapy for head lice? (“Permethrin: … Treatment of choice for uncomplicated pediculosis.”)
- At what aneurysm diameter should a patient with an abdominal aortic aneurysm be referred? (“In general, patients with aneurysms larger than 5 cm in diameter, symptomatic aneurysms, or rapidly enlarging aneurysms should be considered for repair. Treatment for aneurysms between 4 and 5 cm is controversial.”)
- What is the basic workup for kidney stones?
- What are the indications for and monitoring of hydroxyurea for adults with sickle cell anemia?
- What are the therapeutic options for mycobacterium avium complex in an HIV-positive patient?
- How should one follow pulmonary sarcoid when tapering steroids? (A link to an external guideline was especially informative.)
Surprising shortcomings. FC-Web’s Medical Conditions section includes some less common entities—restless legs syndrome, Osgood-Schlatter’s disease, for example—but no monographs are devoted to conditions such as SIADH, paroxysmal supraventricular tachycardia, or portal or pulmonary hypertension.
Contact Information
FIRSTConsult, Customer Services, open Monday to Friday, 7:30 am to 7:00 pm Central Time; 1-800-401-9962. Web site: www.FIRSTConsult.com; e-mail contact available through web site, including subscription information.
Pricing
Physicians: $149; $109 if MDConsult subscription also purchased separately.
Residents/Students: $89
Price includes 1 year of Web access and hand-held updates; components are not available separately. After 1 year, hand-held content continues to function (not “time-bombed”) but renewal necessary for updates. Discount pricing available for groups of as few as 2 individuals.
30-day free trial of Web content with registration at www.FIRSTConsult.com. Free trial of partially functional handheld content through handheld link.
Minimum Requirements
Desktop: Windows PC with Windows 95; Macintosh PC with OS 9; Internet connection; Internet Explorer version 5.0 or Netscape version 6.2.
Palm-OS handheld devices: PalmOS version 3.5.3 with 4 MB of RAM, Palm Desktop 4.0. Additional memory or memory expansion card necessary to run larger products.
Pocket PC handheld devices: Pocket PC with ActiveSync (installed on the desktop computer); 32MB RAM; StrongARM processor.
Despite the evidence and reference citations, there were times we took issue with FC-Web. For example, FC-Web indicates the dosage of amoxicillin for otitis media in children older than 3 months is “25–45 mg/kg/day orally in divided doses (maximum dose 80 mg/kg/day).” In response to the rapid dissemination of drugresistant Streptococcus pneumoniae, the Centers for Disease Control has recommended, in general, that “the initial dose of amoxicillin should be increased from 40 to 45 mg/kg/day to 80 to 90 mg/kg/day.” Also, there are occasional disconnects within monographs. Under “Tinea Infections” in both the Summary and Diagnosis sections is a “Key! Don’t Miss Points” that says: “Patients with HIV infection may have severe onychomycosis and Malassezia folliculitis (pustular hair follicle infection).” However, no mention is made of how to treat Malassezia folliculitis.
Head-to-head with UpToDate. Compared with UpToDate [see “UpToDate: A comprehensive clinical database,” J Fam Pract 2003; 52(9):706–710], FC-Web obviously has been designed from a point-of-care focus. With UpToDate it is often laborious to cull key clinical information at the point-of-care. FC-Web is much less encyclopedic, has a superb layout, and whiz-click access to such amenities as the “Summary of therapeutic options”—with hyperlinking to details if needed.
Although FC-Web has no “history” or “favorites” functions, it is seldom a problem relocating information because of the simplicity of its design (unlike the complex paths one often follows in UpToDate to locate information).
FC-Web’s patient education monographs are more accessible, shorter, and at the opposite literacy extreme from UpToDate’s.
FC-Palm
FIRSTConsult versions for handhelds are available for download with purchase. On the Palm, users must first download and install FC’s EReader, a 90K application. Both EReader and FC-Palm easily load to memory cards and function briskly on recommended versions of Palm OS devices. However, “crashes” are common (and, in some instances, fully reproducible), requiring soft resets of the handheld device.
Shortcomings of the FC-Palm
FC-Palm’s opening screen lists its 2 components, Differential Diagnosis and Medical Conditions. (The other sections are not included in the handheld versions).
One noteworthy peculiarity with EReader is that, if the user presses the Palm’s off button, it exits the application but does not turn off the Palm. The user must press the button a second time to turn off the Palm. Similarly, at the user’s set “time out” (eg, after 2 minutes of inactivity), first FC-Palm/EReader times out, and only then does the countdown begin for the Palm to time out and turn off. Once users are forewarned, this is unlikely to be a problem, but we are not familiar with any other Palm application that exhibits this behavior.
Another curiosity: when FC-Palm times out, it does not resume where it exited. Users must retrace their steps to continue.
Levels of evidence are not included in FC-Palm. Elsevier indicates FC-Palm is updated approximately weekly. Unfortunately, there is no auto-update feature. Updating the 10MB version is time-consuming, particularly hot-syncing to a Palm card (and, if using dial-up connection, downloading), making it unlikely users would update frequently.
FC-Palm has no search function, and, interestingly, Palm’s search feature appears nonfunctional with this program.
Many medical handheld applications, ePocrates for example, employ lists that scroll alphabetically as users enter successive letters, such that entering “c,” “o,” and “l” would automatically scroll to the first listing under “c,” then under “co,” then under “col,” and so on. FC-Palm does not have this feature. Instead, it must be navigated by selecting a letter of the alphabet from the top of the screen (eg, R for Restless Legs), and then scrolling to the entry (via slide bar or Palm buttons) (Figure 6).
There are no icons or shortcuts to frequently used features (eg, “T” to jump to Therapy). Once in an entry, FC-Palm users navigate with a drop-down list to the section of interest. Each section is separate and can be entered only with the drop-down list (Figure 7).
No user-defined preferences are available to select FC-Palm’s monographs’ opening section (eg, Therapeutics).
Conveniently, FC-Palm has forward and back browser-type navigation controls.
Generic drug names are used throughout.
Comparing handheld versions, FIRSTConsult weighs in at 10 MB as opposed to UpToDate’s 800 MB—which may reflect upon the ease and speed of finding information at the point-of-care.
FIGURE 6
Navigating the Palm version
FIGURE 7
Selecting a topic in FC-Palm
Differential diagnosis
In content, FC-Palm’s Differential Diagnosis section is similar to that of FC-Web, except index listings appear only once (eg, “increased tearing, abnormal”) as opposed to appearing under all permutations in FC-Web’s index (eg, under “abnormal,” “increased,” and “tearing”). FC-Palm also employs extensive hyperlinking. Selecting “Incontinence, urinary” produces its differential; tapping “benign prostatic hypertrophy” in the resultant list produces a disease summary, with a link to the corresponding monograph in the Medical Conditions section.
The Differential Diagnosis section does not contain “hyponatremia,” but the Medical Conditions section does. Under the subheading Drugs and Other Therapies, only 2 therapies are listed—demeclocycline and fludrocortisone. There is no mention of water restriction (SIADH) or volume replacement (hypovolemia) per se—just drugs. In contrast, FC-Web’s comparable monograph incorporates volume replacement and free water restriction but only includes the issue of “urgent” volume replacement in the Immediate Action section, not in the important Summary of Therapeutic Options section.
Similarly, FC-Web’s monograph nicely summarizes drug options for pelvic inflammatory disease, but FC-Palm simply provides a listing of individual drugs without any hints about the appropriate combinations—significantly compromising users’ ability to quickly select therapy at point of care.
FC-Palm falls short of the mark for gonorrhea in the same way. The therapeutics screen simply lists 10 drugs (all hyperlinked to further information) without any hints as to recommended or preferred choices. In fact, hyperlinking to further information on ceftriaxone, the Centers for Disease Control’s recommended therapy in pregnancy, one finds the oxymoronic “Use caution in pregnancy (category B),” which might lead a neophyte on a search for the Holy Grail (ie, the nonexistent “better” drug for use in pregnancy).
Final word on firstconsult
FC-Web is well laid out and, using a high-speed connection, functional for point-of-care use, offering sufficiently detailed and extensively hyperlinked disease monographs. For the most common diseases, key questions are generally answered efficiently and in a manner consistent with current evidence or thought. As a bonus, FC-Web provides basic patient education handouts in English and Spanish.
FC-Palm lacks state-of-the-art navigation and search capabilities. FC-Web’s outstanding Summary of Therapeutic Options sections have been gutted in FC-Palm to be substantially less helpful—and potentially misleading—lists of non-prioritized therapies (primarily drugs).
Before we can recommend it as a prime-time handheld application, FC-Palm needs to upgrade its Therapeutics section to be equivalent to FC-Web’s Summary of Therapeutic Options; it should also remedy the nonstandard behaviors, improve navigation, add search options and some user preferences, and incorporate an auto-update feature.
Unquestionably, using electronic information sources at the bedside has the potential to improve the quality of clinical care. That potential is moving closer to realization with FIRSTConsult (formerly PDxMD)—a multifunction physician resource designed for point-of-care use. Its name reflects its connection with MDConsult, the well-known electronic collection of textbooks. Both are produced by Elsevier, whose imprints include Saunders, Mosby, and Churchill Livingstone, and whose publications include Dorland’s Medical Dictionary, Gray’s Anatomy, Harriet Lane Handbook, and The Lancet.
FIRSTConsult comes in 2 incarnations: a Web-based version and a handheld version. The latter is available both for the Palm and Pocket PC operating systems, with variants of about 2, 6, and 10 MB. We evaluated the Web version (hereafter “FC-Web”) and the 10-MB Palm OS version (“FC-Palm”). Descriptions of the smaller versions are available on the FIRSTConsult web site.
As long as a user has access to a high-speed Internet connection, we give FC-Web a “thumbs up” as a rapid, real-time, point-of-care resource. FC-Palm is a portable mini-version of the Medical Conditions and Differential Diagnosis sections of FC-Web. In this article, we detail the advantages and disadvantages of both products.
FC-Web
FC-Web’s opening screen (Figure 1) lists its 5 major components, along with a search box that scans all components simultaneously. Searching “tinea,” for example, produces 529 retrievals (Figure 2). Users may modify search parameters with check boxes and drop-down lists.
FIGURE 1
FIRSTConsult’s opening screen
FIGURE 2
Typical FIRSTConsult search screen
Information retrieval with FC-Web
Clicking one of FC-Web’s components opens a search function or an alphabetic list to locate the desired monograph (Figure 3).
Improved search function. The search function for FC-Web is profoundly improved from that of its predecessor, PDxMD. The search retrievals include section titles (eg, Summary, Background, Diagnosis; see Figure 2), allowing users to link directly to the subject of interest. There is extensive mapping by synonyms, such that “AAA” finds “abdominal aortic aneurysm” and “TIA” finds “transient ischemic attack.” The search feature does not take wild cards or partial words and is intolerant to misspelling (eg, “vonWillebrand” vs “von Willebrand”).
Useful hyperlinks. FC-Web has extensive hyperlinks within its monographs and sections and to other components of the program, and they are among the most useful and logical links these reviewers have seen. Additionally, the program contains hyperlinks to MDConsult (for MDConsult subscribers only) and to excellent external resources, such as consensus statements. Where applicable, levels of evidence and references are cited.
Drawbacks. Regarding speed, we believe FC-Web requires high-speed access for true point-of-care use. FC-Web limits users to 1 open window—even hyperlinks to external sources cannot be opened in new windows.
FIGURE 3
Medical Conditions
Differential diagnosis section
This section provides differential diagnoses—broken into categories by patient age—for about 350 symptoms and signs. The search feature maps to close entries. For example, clicking on Differential Diagnosis and entering the search term “burping,” FC-Web maps to flatulence, eructation, and gas pain. Interestingly, some of the more common causes we see for burping in practice—anxiety/aerophagia, ingestion of dissolved gas (carbonated beverages), and ingestion of bicarbonate—do not appear.
For any condition found on the Differential Diagnosis monograph summary screens, a click pulls up a mini-summary of the illness, nicely leveraging the electronic environment (Figure 4). Users can click through to corresponding FC-Web disease monographs (if available) or to the topic in MDConsult (separate subscription required).
Limitations. Unlike differential diagnosis engines such as DXplain (available at www.lcs.mgh.harvard.edu/dxplain.htm), the Differential Diagnosis section of FC-Web does not allow users to enter sets of data (eg, age; sex; findings) to produce a list of possible diagnoses. Surprisingly, FC-web’s Differential section does not include “hyponatremia” (or “SIADH”), although it contains such things as “hypernasality” and “hypogeusia.”
FIGURE 4
Summary of a Differential Diagnosis
Patient handouts
FC-Web contains more than 450 patient education monographs.
The monographs have 3 main tabs. The first 2—View English and View Spanish—have drop-down menus offering handout choices of “Diagnosed Patient” and “General Information.” The third tab, Actions, allows users to customize handouts (add physician’s name, patient’s name, personalized instructions, etc). Defaults can be saved. Printouts are about 3 “airy” pages with liberal use of white space, large type, and bullet points. They are very basic and easy to read.
Handout deficiencies. Inexplicably, hepatitis A and B are included, but not hepatitis C, which would be the most useful information for our practices.
Occasional minor discrepancies exist between handouts and disease monographs. For example, the Acute Upper Respiratory Tract Infection handout says nothing about echinacea or zinc. However, the related monograph states “Echinacea and zinc supplements may be effective in reducing the duration and severity of common cold symptoms.”
Procedure files
Procedure Files contains 30 to 40 procedure monographs, including video clip illustrations of key portions; users have a choice of viewing these with Windows Media Player, RealPlayer, or QuickTime. Reference Centers contains 3 monographs: “Bioterrorism,” “Contraception,” and “Pregnancy” (as of May 2004). Although few in number, these Reference Centers are valuable point-of-care tools.
Medical conditions
We would expect Medical Conditions to be the workhorse section for most physicians. FC-Web advertises that it contains more than 450 conditions.
Rapid access to information. The best feature of this core section is its organization of information—eminently logical, extremely easy to navigate, bulleted, and extensively hyperlinked, taking full advantage of the e-medium.
To illustrate the outstanding layout and hyperlinking, if a user floats the cursor over a tab (eg, Diagnosis or Treatment) in a disease monograph, a menu of subsections drops down (Figure 5). Floating the cursor over some subsections produces a menu of additional options within that subsection. Furthermore, once selected, the resulting information is often extensively hyperlinked to related or more detailed information.
Generic drug names only. Throughout, FIRSTConsult sticks to generic drug names; if the user is uncertain what cefdinir or tamsulosin is, FIRSTConsult will offer no help.
Generous detail. In terms of content, Medical Conditions distills information into bullet points. FC-Web has more depth than, for example, Griffith’s 5-Minute Consult. Also, as a Web-based tool, FC-Web categorizes information multi-dimensionally with the horizontal main tabs plus drop-down, floating subcategories, allowing expeditious jumps to desired information. This organization facilitates rapid access to information.
Superb summary for point-of-care use. The Summary of Therapeutic Options subcategory of the Treatment section is particular noteworthy—an outstanding feature for busy clinicians—and concrete evidence that FC-Web was truly designed with point-of-care in mind. In this subsection, options are listed by bullet points and very briefly described (1 or 2 lines), which allows easy visual scanning. Each option (eg, medication) is then hyperlinked to its more detailed description (eg, dosage, route, etc) in the section, Drugs and Other Therapies: Details.
Sometimes, FC-Web fails to provide “drug of choice” recommendations, listing interventions randomly, which hinders rapid, point-of-care decision-making.
FIGURE 5
Typical FIRSTConsult monograph
Putting FC-Web to the test
FC-Web answered all general questions for which a monograph existed:
- What is the preferred therapy for head lice? (“Permethrin: … Treatment of choice for uncomplicated pediculosis.”)
- At what aneurysm diameter should a patient with an abdominal aortic aneurysm be referred? (“In general, patients with aneurysms larger than 5 cm in diameter, symptomatic aneurysms, or rapidly enlarging aneurysms should be considered for repair. Treatment for aneurysms between 4 and 5 cm is controversial.”)
- What is the basic workup for kidney stones?
- What are the indications for and monitoring of hydroxyurea for adults with sickle cell anemia?
- What are the therapeutic options for mycobacterium avium complex in an HIV-positive patient?
- How should one follow pulmonary sarcoid when tapering steroids? (A link to an external guideline was especially informative.)
Surprising shortcomings. FC-Web’s Medical Conditions section includes some less common entities—restless legs syndrome, Osgood-Schlatter’s disease, for example—but no monographs are devoted to conditions such as SIADH, paroxysmal supraventricular tachycardia, or portal or pulmonary hypertension.
Contact Information
FIRSTConsult, Customer Services, open Monday to Friday, 7:30 am to 7:00 pm Central Time; 1-800-401-9962. Web site: www.FIRSTConsult.com; e-mail contact available through web site, including subscription information.
Pricing
Physicians: $149; $109 if MDConsult subscription also purchased separately.
Residents/Students: $89
Price includes 1 year of Web access and hand-held updates; components are not available separately. After 1 year, hand-held content continues to function (not “time-bombed”) but renewal necessary for updates. Discount pricing available for groups of as few as 2 individuals.
30-day free trial of Web content with registration at www.FIRSTConsult.com. Free trial of partially functional handheld content through handheld link.
Minimum Requirements
Desktop: Windows PC with Windows 95; Macintosh PC with OS 9; Internet connection; Internet Explorer version 5.0 or Netscape version 6.2.
Palm-OS handheld devices: PalmOS version 3.5.3 with 4 MB of RAM, Palm Desktop 4.0. Additional memory or memory expansion card necessary to run larger products.
Pocket PC handheld devices: Pocket PC with ActiveSync (installed on the desktop computer); 32MB RAM; StrongARM processor.
Despite the evidence and reference citations, there were times we took issue with FC-Web. For example, FC-Web indicates the dosage of amoxicillin for otitis media in children older than 3 months is “25–45 mg/kg/day orally in divided doses (maximum dose 80 mg/kg/day).” In response to the rapid dissemination of drugresistant Streptococcus pneumoniae, the Centers for Disease Control has recommended, in general, that “the initial dose of amoxicillin should be increased from 40 to 45 mg/kg/day to 80 to 90 mg/kg/day.” Also, there are occasional disconnects within monographs. Under “Tinea Infections” in both the Summary and Diagnosis sections is a “Key! Don’t Miss Points” that says: “Patients with HIV infection may have severe onychomycosis and Malassezia folliculitis (pustular hair follicle infection).” However, no mention is made of how to treat Malassezia folliculitis.
Head-to-head with UpToDate. Compared with UpToDate [see “UpToDate: A comprehensive clinical database,” J Fam Pract 2003; 52(9):706–710], FC-Web obviously has been designed from a point-of-care focus. With UpToDate it is often laborious to cull key clinical information at the point-of-care. FC-Web is much less encyclopedic, has a superb layout, and whiz-click access to such amenities as the “Summary of therapeutic options”—with hyperlinking to details if needed.
Although FC-Web has no “history” or “favorites” functions, it is seldom a problem relocating information because of the simplicity of its design (unlike the complex paths one often follows in UpToDate to locate information).
FC-Web’s patient education monographs are more accessible, shorter, and at the opposite literacy extreme from UpToDate’s.
FC-Palm
FIRSTConsult versions for handhelds are available for download with purchase. On the Palm, users must first download and install FC’s EReader, a 90K application. Both EReader and FC-Palm easily load to memory cards and function briskly on recommended versions of Palm OS devices. However, “crashes” are common (and, in some instances, fully reproducible), requiring soft resets of the handheld device.
Shortcomings of the FC-Palm
FC-Palm’s opening screen lists its 2 components, Differential Diagnosis and Medical Conditions. (The other sections are not included in the handheld versions).
One noteworthy peculiarity with EReader is that, if the user presses the Palm’s off button, it exits the application but does not turn off the Palm. The user must press the button a second time to turn off the Palm. Similarly, at the user’s set “time out” (eg, after 2 minutes of inactivity), first FC-Palm/EReader times out, and only then does the countdown begin for the Palm to time out and turn off. Once users are forewarned, this is unlikely to be a problem, but we are not familiar with any other Palm application that exhibits this behavior.
Another curiosity: when FC-Palm times out, it does not resume where it exited. Users must retrace their steps to continue.
Levels of evidence are not included in FC-Palm. Elsevier indicates FC-Palm is updated approximately weekly. Unfortunately, there is no auto-update feature. Updating the 10MB version is time-consuming, particularly hot-syncing to a Palm card (and, if using dial-up connection, downloading), making it unlikely users would update frequently.
FC-Palm has no search function, and, interestingly, Palm’s search feature appears nonfunctional with this program.
Many medical handheld applications, ePocrates for example, employ lists that scroll alphabetically as users enter successive letters, such that entering “c,” “o,” and “l” would automatically scroll to the first listing under “c,” then under “co,” then under “col,” and so on. FC-Palm does not have this feature. Instead, it must be navigated by selecting a letter of the alphabet from the top of the screen (eg, R for Restless Legs), and then scrolling to the entry (via slide bar or Palm buttons) (Figure 6).
There are no icons or shortcuts to frequently used features (eg, “T” to jump to Therapy). Once in an entry, FC-Palm users navigate with a drop-down list to the section of interest. Each section is separate and can be entered only with the drop-down list (Figure 7).
No user-defined preferences are available to select FC-Palm’s monographs’ opening section (eg, Therapeutics).
Conveniently, FC-Palm has forward and back browser-type navigation controls.
Generic drug names are used throughout.
Comparing handheld versions, FIRSTConsult weighs in at 10 MB as opposed to UpToDate’s 800 MB—which may reflect upon the ease and speed of finding information at the point-of-care.
FIGURE 6
Navigating the Palm version
FIGURE 7
Selecting a topic in FC-Palm
Differential diagnosis
In content, FC-Palm’s Differential Diagnosis section is similar to that of FC-Web, except index listings appear only once (eg, “increased tearing, abnormal”) as opposed to appearing under all permutations in FC-Web’s index (eg, under “abnormal,” “increased,” and “tearing”). FC-Palm also employs extensive hyperlinking. Selecting “Incontinence, urinary” produces its differential; tapping “benign prostatic hypertrophy” in the resultant list produces a disease summary, with a link to the corresponding monograph in the Medical Conditions section.
The Differential Diagnosis section does not contain “hyponatremia,” but the Medical Conditions section does. Under the subheading Drugs and Other Therapies, only 2 therapies are listed—demeclocycline and fludrocortisone. There is no mention of water restriction (SIADH) or volume replacement (hypovolemia) per se—just drugs. In contrast, FC-Web’s comparable monograph incorporates volume replacement and free water restriction but only includes the issue of “urgent” volume replacement in the Immediate Action section, not in the important Summary of Therapeutic Options section.
Similarly, FC-Web’s monograph nicely summarizes drug options for pelvic inflammatory disease, but FC-Palm simply provides a listing of individual drugs without any hints about the appropriate combinations—significantly compromising users’ ability to quickly select therapy at point of care.
FC-Palm falls short of the mark for gonorrhea in the same way. The therapeutics screen simply lists 10 drugs (all hyperlinked to further information) without any hints as to recommended or preferred choices. In fact, hyperlinking to further information on ceftriaxone, the Centers for Disease Control’s recommended therapy in pregnancy, one finds the oxymoronic “Use caution in pregnancy (category B),” which might lead a neophyte on a search for the Holy Grail (ie, the nonexistent “better” drug for use in pregnancy).
Final word on firstconsult
FC-Web is well laid out and, using a high-speed connection, functional for point-of-care use, offering sufficiently detailed and extensively hyperlinked disease monographs. For the most common diseases, key questions are generally answered efficiently and in a manner consistent with current evidence or thought. As a bonus, FC-Web provides basic patient education handouts in English and Spanish.
FC-Palm lacks state-of-the-art navigation and search capabilities. FC-Web’s outstanding Summary of Therapeutic Options sections have been gutted in FC-Palm to be substantially less helpful—and potentially misleading—lists of non-prioritized therapies (primarily drugs).
Before we can recommend it as a prime-time handheld application, FC-Palm needs to upgrade its Therapeutics section to be equivalent to FC-Web’s Summary of Therapeutic Options; it should also remedy the nonstandard behaviors, improve navigation, add search options and some user preferences, and incorporate an auto-update feature.
UpToDate: A comprehensive clinical database
How many clinical questions arise during an average day at the office? How many more questions might one entertain if clear-cut, expert advice were seconds away? Enter UpToDate, an electronic clinical database for, well, acquiring up-to-date clinical information—plus continuing medical education (CME) credits and patient handouts.
Unlike a textbook, UpToDate is not set up for paging through content from beginning to end. Rather, it is designed for searches that yield lists of relevant monographs. UpToDate’s initial screen displays simple menu bars and a prominent search box (Figure 1). The next step allows one to narrow the search (Figure 2).
Per its educational objectives, UpToDate provides “instant access to the most current clinical information and recommendations on patient care and treatment,” yet is “comprehensive” from “physiological concepts through results of the most recent clinical trials and protocols.” Each monograph indicates when the literature was last reviewed and the document updated. The service is available in 3 formats: personal computer-based, online, and Pocket PC. We reviewed these formats using Windows PCs.
FIGURE 1
UpToDate’s main screen
Main search screen after entry of search term “pulmonary hypertension” and performing the initial search.
FIGURE 2
Typical UpToDate search screen
List of monographs retrieved after clicking “Pulmonary hypertension” from the list in Figure 1 Note that “Find in Text” is not active, but an option to “Narrow search results” results in a secondary search screen. Users selecting this option may then either enter a term in the secondary search box or choose among a list of “modifiers” that vary by topic.
Testing uptodate in a clinical context
Following are a few questions that needed answering during a half-day of practice:
- How effective is topical terbinafine (Lamisil) in treating Candida skin infections?
- What is a reasonable algorithm to determine the cause of chronic renal failure?
- How does one compound nitroglycerin ointment to treat an anal fissure?
- What is the latest thinking on interstitial cystitis?
- What is the preferred empiric antibiotic therapy for presumed bacterial conjunctivitis in adults?
- Does efficacy differ between injectable and intranasal forms of calcitonin for relief of pain from osteoporotic vertebral compression fractures in postmenopausal women?
UpToDate answered 4 of the 6 questions quickly, requiring no more than a few minutes for each search. We found that 2% nitroglycerin must be diluted to 0.2% for use on anal fissures. We also obtained summarized information on interstitial cystitis, a treatment recommendation for conjunctivitis, and data regarding the efficacy of calcitonin administered by either of 2 routes. The information generally was excellent.
More difficult searches
Testing UpToDate further, we searched for less common maladies. We found 4 sentences on proctalgia fugax that, remarkably, seemed to cover the topic adequately. Transient global amnesia was covered tersely (3 sentences) but, again, adequately. Restless legs syndrome was covered well, in several paragraphs, although drug therapies were discussed in random order rather than by drug of choice. Piriformis syndrome was covered inadequately, and presbyesophagus was not listed at all.
Controversial topics
Subsequent searches yielded excellent discussions on controversial topics. Many monographs lend themselves best to leisurely reading, but they could also be used at the point of care. For example, the controversial diastolic “J-curve phenomenon” in treating hypertension is covered in about fourteen 2- to 6-sentence paragraphs. A summary appears first, typical of UpToDate’s style (Figure 3).
This section on diastolic blood pressure is subdivided into “Positive studies,” “Negative studies,” and the “HOT trial.” Users may jump directly to the “HOT trial” summary by clicking on that title on the left window. References appear in a text box at the bottom of the screen. The relative sizes of these 3 windows may be changed by grabbing and dragging the lines dividing them.
FIGURE 3
Typical UpToDate monograph
Users can minimize the left-hand and bottom panes to have a larger main text pane. Although not marked like typical hyperlinks, clicking any reference in the text window pops up that reference and, if available, its abstract. Clicking any subheading in the left-side outline pane transports the user to that section (eg, “HOT trial”). Clicking “Recent Topics” on the upper menu bar produces a list of the last 20 sections visited. Revisiting a topic is then possible with one additional click.
Drug mentions
Drugs mentioned in UpToDate are hot-linked to the corresponding Lexi-Comp drug information monograph, which is “intended to serve as a rapidly accessible, concise initial [drug] reference resource.” UpToDate/Lexi-Comp does not provide guidance regarding cost of drug therapies.
Notable Features
Graphics
When the user clicks on a graphic’s link in the text, a figure, table, or picture is superimposed on the text. The image disappears when the user returns to the text.
Patient education handouts
UpToDate offers patient education handouts; however, these could be made much more accessible. Veteran users know exactly where to look for these handouts, but novices may apply the “3 clicks and you’re out” rule when the process proves too frustrating.
Both “Prostate Cancer Screening” (including PSA testing) and “Screening for Breast Cancer” (including mammography) are about 5 single-spaced pages long when printed using Times New Roman 12-point. Although controversies are covered well, our guesstimate of the reading comprehension level is 1 or 2 years post–high school— maybe too difficult for patient education.
Search engine
UpToDate’s search engine is rudimentary. Multiword medical term searches are supported (eg, “chronic renal failure” and “vertebral compression fracture”), as are initial word fragments (eg, “spondyl”). However, searches incorporating Boolean operators (AND, OR, NOT) and unrelated words are not directly supported, although an obtuse “secondary search” does provide for one AND operation. On this secondary search screen, users may choose to focus on a specific category of information, such as diagnosis, treatment, pathogenesis, or patient information.
The search function can be quirky. Although the words “gluteus medius bursitis” appear in the text, cutting and pasting those words into the search function yields no retrievals; this makes it more difficult to locate information. Searching “restless legs syndrome” produces the suggestion that the user search “restless legs”—which, when searched, produces a most relevant topic: “restless legs syndrome.”
Additional digital tools
Other features of UpToDate take excellent advantage of the electronic environment.
Hyperlinking. Extensive hyperlinking within and between monographs facilitates access to information.
Retracing steps. “Back” and “forward” buttons allow users to navigate linearly.
Text-string searches.The “Find in Text” feature, or its keyboard shortcut, Ctrl-F, allows users to find text string matches within the current monograph.
Search history. A “Recent Topics” button in the menu bar makes it possible to revisit the prior 20 topics viewed by a user.
Accessing citations. Clicking on any reference links users to that article’s citation and, if available, MEDLINE abstract. Citations may be exported to a text file, but may not be directly cut-and-pasted.
Exporting monographs. Users may print a monograph, export a monograph as text or in rich text format (*.rtf), export a monograph’s abstracts into WordPad, or (from the Web version) e-mail a monograph to a colleague with an optional, complimentary 7-day guest pass to UpToDate Online. Graphics can be exported into Windows Paint.
CME tracking. UpToDate keeps track of a user’s “CME time,” crediting up to 10 minutes (in hundredths of an hour increments) per topic per use of UpToDate. CME from the CD is unlimited; up to 50 hours may be accumulated online. Credits may be totalled for submission for a fee of $25 per transmittal.
Room for improvement
Some of UpToDate’s advice is open to question. Although information is generally well-referenced, a few statements should have been referenced but were not.
For example (in reference to bacterial conjunctivitis): “Aminoglycoside drops and ointments (Genoptic®, Tobrex®) are poor choices since they are toxic to the corneal epithelium and can cause a reactive keratoconjunctivitis after several days of use.”
UpToDate prominently advises that the Pediatric module is a work in progress. In searching for “delayed menarche,” the closest match we found was “Pubertal changes (Tanner stages).” Information was sufficient to answer most clinical questions. However, UpToDate did not provide a clinically useful graphic listing sentinel events (Tanner stages, peak height velocity, menarche) in typical chronological order with anticipated normal age ranges.
Digital design problems
UpToDate fails to take full advantage of the electronic environment. Inexplicably, in the Contents menu screens, Find in Text is not active, and users cannot navigate using the Page-Up/Page-Down or (Ctrl+)Home/End buttons on their keypads. For example, following Contents through “Patient Education” to “Women’s Health Issues,” users find 48 topics in 19 sections as they try to locate the one of interest.
“Mammography” is integrated into “Screening for breast cancer,” and is not a separate keyword for users who are visually scanning for that word (the only option).
Right-clicking is not supported.
An Editmenu is absent. Windows’ Cut and Paste keyboard conventions (Ctrl-c/Ctrl-v) are supported in the main UpToDate window—but not in other windows.
Bookmarking—the electronic equivalent of the folded page corner—is unavailable, as is a favoriteslist.
Highlighting—electronic yellow, blue, and pink markers—is not supported.
No facility for user-added annotation is available.
Opening multiple windows of information simultaneously is not possible.
Standard resizing of the main UpToDate window (by “grabbing” edges of the window) is not supported.
Finally, an ability to limit searches from the main screen to patient handouts or Lexi-Comp would be desirable.
Pocket version
UpToDate also provides a Pocket PC version. The Pocket PC version searches the same database with a search engine similar to the other versions. It lacks the search history offered in the CD version. Although faster than searching through a textbook, an average UpToDate search on Dell Axim X5 400 mHz (Intel PXA250) with 64 MB RAM and a SanDisk 1G CompactFlash card took about 10 to 27 seconds, plus more time to navigate through the long and sometimes cumbersome submenus.
The primary intent for palmtop medical software is point-of-care use. The extensiveness of UpToDate’s text—occupying 800 MB of the 1G card—and limited speed of palmtop computers often makes this impractical. However, it should be emphasized that this rich, inclusive database is a valuable reference when time is not at a premium. Certainly, the Pocket PC version provides ultimate portability. Users contemplating use of UpToDate/Pocket PC should budget for a highend Pocket PC and a 1G card.
Conclusions
UpToDate is a clinically useful, searchable database of medical information updated every 4 months and available on CD, online, and for souped-up Pocket PC palmtop devices. It is almost as if UpToDate purposely incorporated an unsophisticated search engine and did not optimize the electronic environment to flaunt its forte—the clinical database.
For family physicians, the database is of sufficiently high quality, and it will be even more useful as the pediatric module expands. We hope that future enhancements to UpToDate will include clinical bullets for point-of-care use and optimization of the electronic environment. The latter should include implementation of Boolean searches; bookmarks; highlighters; a user-added note facility; copying and pasting of references; links to drug cost information; and—the whole point of Windows! — multi-window capability and conventional window resizing.
Patient information needs to be more accessible to be clinically useful. Also, versions of the patient information handouts with less complex language to appeal to the average patient would be helpful. As is, UpToDate’s importance will only increase. Highly recommended.
CONTACT INFORMATION
UpToDate, 34 Washington Street, Wellesley, MA 02481. Phone: 800-998-6374 (US and Canada) or 781-237-4788; Fax: 781-239-0391.
Free customer support line, Monday–Friday, 8:00 AM–6:30 PM (EST). Subscription or order information: customerservice@uptodate.com. General inquiries: info@uptodate.com. Technical support: support@upto-date.com. Web site: www.uptodate.com.
PRICING
New annual subscription: $495; renewal: $395; trainees: $195; group and institutional pricing: contact enterprise@uptodate.com.
Shipping to US and Canada: $15/year; elsewhere: $35/year. 60-day trial period during which purchaser may return all materials for a full refund.
Virtual tour available at www.uptodate.com. American Academy of Family Physicians members: free 14-day trial via www.aafp.org. Upon expiration (4 months), message alerts user that content is out of date. CDs cease to function 1 year from issue date.
SPECIFICATIONS
Initial: Windows or Macintosh and Pocket PC CD-ROMs, online user name and password. Two updates shipped at 4-month intervals (12-month subscription). Installation and activation directions, search tips, CD-based (or online) tutorial.
MINIMUM REQUIREMENTS
Computer requirements: CD-ROM drive (8X recommended), 16 MB RAM, 15 MB free hard disk space. Windows PC: 486/66 or Pentium processor running Microsoft Windows 95 or later. Macintosh: Power PC or G3/G4 processor running OS 8.1 or later. Online:Standard Web browser with cookies enabled. Recommended connection speed of at least 56K. Pocket PC requirements: Windows PC with CD-ROM drive. Pocket PC device running Windows Pocket PC 2000 or 2002 with Type II CompactFlash slot, expanded storage card/drive (1 GB; uses 800 MB), Pocket PC cradle, and media reader (connects storage device directly to the PC). Additional details: www.uptodate.com
Correspondence
Gary N. Fox, MD, Mercy Health Partners Family Practice Residency Program, 2200 Jefferson Ave, Toledo OH 43624-1117. E-mail: foxgary@yahoo.com.
How many clinical questions arise during an average day at the office? How many more questions might one entertain if clear-cut, expert advice were seconds away? Enter UpToDate, an electronic clinical database for, well, acquiring up-to-date clinical information—plus continuing medical education (CME) credits and patient handouts.
Unlike a textbook, UpToDate is not set up for paging through content from beginning to end. Rather, it is designed for searches that yield lists of relevant monographs. UpToDate’s initial screen displays simple menu bars and a prominent search box (Figure 1). The next step allows one to narrow the search (Figure 2).
Per its educational objectives, UpToDate provides “instant access to the most current clinical information and recommendations on patient care and treatment,” yet is “comprehensive” from “physiological concepts through results of the most recent clinical trials and protocols.” Each monograph indicates when the literature was last reviewed and the document updated. The service is available in 3 formats: personal computer-based, online, and Pocket PC. We reviewed these formats using Windows PCs.
FIGURE 1
UpToDate’s main screen
Main search screen after entry of search term “pulmonary hypertension” and performing the initial search.
FIGURE 2
Typical UpToDate search screen
List of monographs retrieved after clicking “Pulmonary hypertension” from the list in Figure 1 Note that “Find in Text” is not active, but an option to “Narrow search results” results in a secondary search screen. Users selecting this option may then either enter a term in the secondary search box or choose among a list of “modifiers” that vary by topic.
Testing uptodate in a clinical context
Following are a few questions that needed answering during a half-day of practice:
- How effective is topical terbinafine (Lamisil) in treating Candida skin infections?
- What is a reasonable algorithm to determine the cause of chronic renal failure?
- How does one compound nitroglycerin ointment to treat an anal fissure?
- What is the latest thinking on interstitial cystitis?
- What is the preferred empiric antibiotic therapy for presumed bacterial conjunctivitis in adults?
- Does efficacy differ between injectable and intranasal forms of calcitonin for relief of pain from osteoporotic vertebral compression fractures in postmenopausal women?
UpToDate answered 4 of the 6 questions quickly, requiring no more than a few minutes for each search. We found that 2% nitroglycerin must be diluted to 0.2% for use on anal fissures. We also obtained summarized information on interstitial cystitis, a treatment recommendation for conjunctivitis, and data regarding the efficacy of calcitonin administered by either of 2 routes. The information generally was excellent.
More difficult searches
Testing UpToDate further, we searched for less common maladies. We found 4 sentences on proctalgia fugax that, remarkably, seemed to cover the topic adequately. Transient global amnesia was covered tersely (3 sentences) but, again, adequately. Restless legs syndrome was covered well, in several paragraphs, although drug therapies were discussed in random order rather than by drug of choice. Piriformis syndrome was covered inadequately, and presbyesophagus was not listed at all.
Controversial topics
Subsequent searches yielded excellent discussions on controversial topics. Many monographs lend themselves best to leisurely reading, but they could also be used at the point of care. For example, the controversial diastolic “J-curve phenomenon” in treating hypertension is covered in about fourteen 2- to 6-sentence paragraphs. A summary appears first, typical of UpToDate’s style (Figure 3).
This section on diastolic blood pressure is subdivided into “Positive studies,” “Negative studies,” and the “HOT trial.” Users may jump directly to the “HOT trial” summary by clicking on that title on the left window. References appear in a text box at the bottom of the screen. The relative sizes of these 3 windows may be changed by grabbing and dragging the lines dividing them.
FIGURE 3
Typical UpToDate monograph
Users can minimize the left-hand and bottom panes to have a larger main text pane. Although not marked like typical hyperlinks, clicking any reference in the text window pops up that reference and, if available, its abstract. Clicking any subheading in the left-side outline pane transports the user to that section (eg, “HOT trial”). Clicking “Recent Topics” on the upper menu bar produces a list of the last 20 sections visited. Revisiting a topic is then possible with one additional click.
Drug mentions
Drugs mentioned in UpToDate are hot-linked to the corresponding Lexi-Comp drug information monograph, which is “intended to serve as a rapidly accessible, concise initial [drug] reference resource.” UpToDate/Lexi-Comp does not provide guidance regarding cost of drug therapies.
Notable Features
Graphics
When the user clicks on a graphic’s link in the text, a figure, table, or picture is superimposed on the text. The image disappears when the user returns to the text.
Patient education handouts
UpToDate offers patient education handouts; however, these could be made much more accessible. Veteran users know exactly where to look for these handouts, but novices may apply the “3 clicks and you’re out” rule when the process proves too frustrating.
Both “Prostate Cancer Screening” (including PSA testing) and “Screening for Breast Cancer” (including mammography) are about 5 single-spaced pages long when printed using Times New Roman 12-point. Although controversies are covered well, our guesstimate of the reading comprehension level is 1 or 2 years post–high school— maybe too difficult for patient education.
Search engine
UpToDate’s search engine is rudimentary. Multiword medical term searches are supported (eg, “chronic renal failure” and “vertebral compression fracture”), as are initial word fragments (eg, “spondyl”). However, searches incorporating Boolean operators (AND, OR, NOT) and unrelated words are not directly supported, although an obtuse “secondary search” does provide for one AND operation. On this secondary search screen, users may choose to focus on a specific category of information, such as diagnosis, treatment, pathogenesis, or patient information.
The search function can be quirky. Although the words “gluteus medius bursitis” appear in the text, cutting and pasting those words into the search function yields no retrievals; this makes it more difficult to locate information. Searching “restless legs syndrome” produces the suggestion that the user search “restless legs”—which, when searched, produces a most relevant topic: “restless legs syndrome.”
Additional digital tools
Other features of UpToDate take excellent advantage of the electronic environment.
Hyperlinking. Extensive hyperlinking within and between monographs facilitates access to information.
Retracing steps. “Back” and “forward” buttons allow users to navigate linearly.
Text-string searches.The “Find in Text” feature, or its keyboard shortcut, Ctrl-F, allows users to find text string matches within the current monograph.
Search history. A “Recent Topics” button in the menu bar makes it possible to revisit the prior 20 topics viewed by a user.
Accessing citations. Clicking on any reference links users to that article’s citation and, if available, MEDLINE abstract. Citations may be exported to a text file, but may not be directly cut-and-pasted.
Exporting monographs. Users may print a monograph, export a monograph as text or in rich text format (*.rtf), export a monograph’s abstracts into WordPad, or (from the Web version) e-mail a monograph to a colleague with an optional, complimentary 7-day guest pass to UpToDate Online. Graphics can be exported into Windows Paint.
CME tracking. UpToDate keeps track of a user’s “CME time,” crediting up to 10 minutes (in hundredths of an hour increments) per topic per use of UpToDate. CME from the CD is unlimited; up to 50 hours may be accumulated online. Credits may be totalled for submission for a fee of $25 per transmittal.
Room for improvement
Some of UpToDate’s advice is open to question. Although information is generally well-referenced, a few statements should have been referenced but were not.
For example (in reference to bacterial conjunctivitis): “Aminoglycoside drops and ointments (Genoptic®, Tobrex®) are poor choices since they are toxic to the corneal epithelium and can cause a reactive keratoconjunctivitis after several days of use.”
UpToDate prominently advises that the Pediatric module is a work in progress. In searching for “delayed menarche,” the closest match we found was “Pubertal changes (Tanner stages).” Information was sufficient to answer most clinical questions. However, UpToDate did not provide a clinically useful graphic listing sentinel events (Tanner stages, peak height velocity, menarche) in typical chronological order with anticipated normal age ranges.
Digital design problems
UpToDate fails to take full advantage of the electronic environment. Inexplicably, in the Contents menu screens, Find in Text is not active, and users cannot navigate using the Page-Up/Page-Down or (Ctrl+)Home/End buttons on their keypads. For example, following Contents through “Patient Education” to “Women’s Health Issues,” users find 48 topics in 19 sections as they try to locate the one of interest.
“Mammography” is integrated into “Screening for breast cancer,” and is not a separate keyword for users who are visually scanning for that word (the only option).
Right-clicking is not supported.
An Editmenu is absent. Windows’ Cut and Paste keyboard conventions (Ctrl-c/Ctrl-v) are supported in the main UpToDate window—but not in other windows.
Bookmarking—the electronic equivalent of the folded page corner—is unavailable, as is a favoriteslist.
Highlighting—electronic yellow, blue, and pink markers—is not supported.
No facility for user-added annotation is available.
Opening multiple windows of information simultaneously is not possible.
Standard resizing of the main UpToDate window (by “grabbing” edges of the window) is not supported.
Finally, an ability to limit searches from the main screen to patient handouts or Lexi-Comp would be desirable.
Pocket version
UpToDate also provides a Pocket PC version. The Pocket PC version searches the same database with a search engine similar to the other versions. It lacks the search history offered in the CD version. Although faster than searching through a textbook, an average UpToDate search on Dell Axim X5 400 mHz (Intel PXA250) with 64 MB RAM and a SanDisk 1G CompactFlash card took about 10 to 27 seconds, plus more time to navigate through the long and sometimes cumbersome submenus.
The primary intent for palmtop medical software is point-of-care use. The extensiveness of UpToDate’s text—occupying 800 MB of the 1G card—and limited speed of palmtop computers often makes this impractical. However, it should be emphasized that this rich, inclusive database is a valuable reference when time is not at a premium. Certainly, the Pocket PC version provides ultimate portability. Users contemplating use of UpToDate/Pocket PC should budget for a highend Pocket PC and a 1G card.
Conclusions
UpToDate is a clinically useful, searchable database of medical information updated every 4 months and available on CD, online, and for souped-up Pocket PC palmtop devices. It is almost as if UpToDate purposely incorporated an unsophisticated search engine and did not optimize the electronic environment to flaunt its forte—the clinical database.
For family physicians, the database is of sufficiently high quality, and it will be even more useful as the pediatric module expands. We hope that future enhancements to UpToDate will include clinical bullets for point-of-care use and optimization of the electronic environment. The latter should include implementation of Boolean searches; bookmarks; highlighters; a user-added note facility; copying and pasting of references; links to drug cost information; and—the whole point of Windows! — multi-window capability and conventional window resizing.
Patient information needs to be more accessible to be clinically useful. Also, versions of the patient information handouts with less complex language to appeal to the average patient would be helpful. As is, UpToDate’s importance will only increase. Highly recommended.
CONTACT INFORMATION
UpToDate, 34 Washington Street, Wellesley, MA 02481. Phone: 800-998-6374 (US and Canada) or 781-237-4788; Fax: 781-239-0391.
Free customer support line, Monday–Friday, 8:00 AM–6:30 PM (EST). Subscription or order information: customerservice@uptodate.com. General inquiries: info@uptodate.com. Technical support: support@upto-date.com. Web site: www.uptodate.com.
PRICING
New annual subscription: $495; renewal: $395; trainees: $195; group and institutional pricing: contact enterprise@uptodate.com.
Shipping to US and Canada: $15/year; elsewhere: $35/year. 60-day trial period during which purchaser may return all materials for a full refund.
Virtual tour available at www.uptodate.com. American Academy of Family Physicians members: free 14-day trial via www.aafp.org. Upon expiration (4 months), message alerts user that content is out of date. CDs cease to function 1 year from issue date.
SPECIFICATIONS
Initial: Windows or Macintosh and Pocket PC CD-ROMs, online user name and password. Two updates shipped at 4-month intervals (12-month subscription). Installation and activation directions, search tips, CD-based (or online) tutorial.
MINIMUM REQUIREMENTS
Computer requirements: CD-ROM drive (8X recommended), 16 MB RAM, 15 MB free hard disk space. Windows PC: 486/66 or Pentium processor running Microsoft Windows 95 or later. Macintosh: Power PC or G3/G4 processor running OS 8.1 or later. Online:Standard Web browser with cookies enabled. Recommended connection speed of at least 56K. Pocket PC requirements: Windows PC with CD-ROM drive. Pocket PC device running Windows Pocket PC 2000 or 2002 with Type II CompactFlash slot, expanded storage card/drive (1 GB; uses 800 MB), Pocket PC cradle, and media reader (connects storage device directly to the PC). Additional details: www.uptodate.com
Correspondence
Gary N. Fox, MD, Mercy Health Partners Family Practice Residency Program, 2200 Jefferson Ave, Toledo OH 43624-1117. E-mail: foxgary@yahoo.com.
How many clinical questions arise during an average day at the office? How many more questions might one entertain if clear-cut, expert advice were seconds away? Enter UpToDate, an electronic clinical database for, well, acquiring up-to-date clinical information—plus continuing medical education (CME) credits and patient handouts.
Unlike a textbook, UpToDate is not set up for paging through content from beginning to end. Rather, it is designed for searches that yield lists of relevant monographs. UpToDate’s initial screen displays simple menu bars and a prominent search box (Figure 1). The next step allows one to narrow the search (Figure 2).
Per its educational objectives, UpToDate provides “instant access to the most current clinical information and recommendations on patient care and treatment,” yet is “comprehensive” from “physiological concepts through results of the most recent clinical trials and protocols.” Each monograph indicates when the literature was last reviewed and the document updated. The service is available in 3 formats: personal computer-based, online, and Pocket PC. We reviewed these formats using Windows PCs.
FIGURE 1
UpToDate’s main screen
Main search screen after entry of search term “pulmonary hypertension” and performing the initial search.
FIGURE 2
Typical UpToDate search screen
List of monographs retrieved after clicking “Pulmonary hypertension” from the list in Figure 1 Note that “Find in Text” is not active, but an option to “Narrow search results” results in a secondary search screen. Users selecting this option may then either enter a term in the secondary search box or choose among a list of “modifiers” that vary by topic.
Testing uptodate in a clinical context
Following are a few questions that needed answering during a half-day of practice:
- How effective is topical terbinafine (Lamisil) in treating Candida skin infections?
- What is a reasonable algorithm to determine the cause of chronic renal failure?
- How does one compound nitroglycerin ointment to treat an anal fissure?
- What is the latest thinking on interstitial cystitis?
- What is the preferred empiric antibiotic therapy for presumed bacterial conjunctivitis in adults?
- Does efficacy differ between injectable and intranasal forms of calcitonin for relief of pain from osteoporotic vertebral compression fractures in postmenopausal women?
UpToDate answered 4 of the 6 questions quickly, requiring no more than a few minutes for each search. We found that 2% nitroglycerin must be diluted to 0.2% for use on anal fissures. We also obtained summarized information on interstitial cystitis, a treatment recommendation for conjunctivitis, and data regarding the efficacy of calcitonin administered by either of 2 routes. The information generally was excellent.
More difficult searches
Testing UpToDate further, we searched for less common maladies. We found 4 sentences on proctalgia fugax that, remarkably, seemed to cover the topic adequately. Transient global amnesia was covered tersely (3 sentences) but, again, adequately. Restless legs syndrome was covered well, in several paragraphs, although drug therapies were discussed in random order rather than by drug of choice. Piriformis syndrome was covered inadequately, and presbyesophagus was not listed at all.
Controversial topics
Subsequent searches yielded excellent discussions on controversial topics. Many monographs lend themselves best to leisurely reading, but they could also be used at the point of care. For example, the controversial diastolic “J-curve phenomenon” in treating hypertension is covered in about fourteen 2- to 6-sentence paragraphs. A summary appears first, typical of UpToDate’s style (Figure 3).
This section on diastolic blood pressure is subdivided into “Positive studies,” “Negative studies,” and the “HOT trial.” Users may jump directly to the “HOT trial” summary by clicking on that title on the left window. References appear in a text box at the bottom of the screen. The relative sizes of these 3 windows may be changed by grabbing and dragging the lines dividing them.
FIGURE 3
Typical UpToDate monograph
Users can minimize the left-hand and bottom panes to have a larger main text pane. Although not marked like typical hyperlinks, clicking any reference in the text window pops up that reference and, if available, its abstract. Clicking any subheading in the left-side outline pane transports the user to that section (eg, “HOT trial”). Clicking “Recent Topics” on the upper menu bar produces a list of the last 20 sections visited. Revisiting a topic is then possible with one additional click.
Drug mentions
Drugs mentioned in UpToDate are hot-linked to the corresponding Lexi-Comp drug information monograph, which is “intended to serve as a rapidly accessible, concise initial [drug] reference resource.” UpToDate/Lexi-Comp does not provide guidance regarding cost of drug therapies.
Notable Features
Graphics
When the user clicks on a graphic’s link in the text, a figure, table, or picture is superimposed on the text. The image disappears when the user returns to the text.
Patient education handouts
UpToDate offers patient education handouts; however, these could be made much more accessible. Veteran users know exactly where to look for these handouts, but novices may apply the “3 clicks and you’re out” rule when the process proves too frustrating.
Both “Prostate Cancer Screening” (including PSA testing) and “Screening for Breast Cancer” (including mammography) are about 5 single-spaced pages long when printed using Times New Roman 12-point. Although controversies are covered well, our guesstimate of the reading comprehension level is 1 or 2 years post–high school— maybe too difficult for patient education.
Search engine
UpToDate’s search engine is rudimentary. Multiword medical term searches are supported (eg, “chronic renal failure” and “vertebral compression fracture”), as are initial word fragments (eg, “spondyl”). However, searches incorporating Boolean operators (AND, OR, NOT) and unrelated words are not directly supported, although an obtuse “secondary search” does provide for one AND operation. On this secondary search screen, users may choose to focus on a specific category of information, such as diagnosis, treatment, pathogenesis, or patient information.
The search function can be quirky. Although the words “gluteus medius bursitis” appear in the text, cutting and pasting those words into the search function yields no retrievals; this makes it more difficult to locate information. Searching “restless legs syndrome” produces the suggestion that the user search “restless legs”—which, when searched, produces a most relevant topic: “restless legs syndrome.”
Additional digital tools
Other features of UpToDate take excellent advantage of the electronic environment.
Hyperlinking. Extensive hyperlinking within and between monographs facilitates access to information.
Retracing steps. “Back” and “forward” buttons allow users to navigate linearly.
Text-string searches.The “Find in Text” feature, or its keyboard shortcut, Ctrl-F, allows users to find text string matches within the current monograph.
Search history. A “Recent Topics” button in the menu bar makes it possible to revisit the prior 20 topics viewed by a user.
Accessing citations. Clicking on any reference links users to that article’s citation and, if available, MEDLINE abstract. Citations may be exported to a text file, but may not be directly cut-and-pasted.
Exporting monographs. Users may print a monograph, export a monograph as text or in rich text format (*.rtf), export a monograph’s abstracts into WordPad, or (from the Web version) e-mail a monograph to a colleague with an optional, complimentary 7-day guest pass to UpToDate Online. Graphics can be exported into Windows Paint.
CME tracking. UpToDate keeps track of a user’s “CME time,” crediting up to 10 minutes (in hundredths of an hour increments) per topic per use of UpToDate. CME from the CD is unlimited; up to 50 hours may be accumulated online. Credits may be totalled for submission for a fee of $25 per transmittal.
Room for improvement
Some of UpToDate’s advice is open to question. Although information is generally well-referenced, a few statements should have been referenced but were not.
For example (in reference to bacterial conjunctivitis): “Aminoglycoside drops and ointments (Genoptic®, Tobrex®) are poor choices since they are toxic to the corneal epithelium and can cause a reactive keratoconjunctivitis after several days of use.”
UpToDate prominently advises that the Pediatric module is a work in progress. In searching for “delayed menarche,” the closest match we found was “Pubertal changes (Tanner stages).” Information was sufficient to answer most clinical questions. However, UpToDate did not provide a clinically useful graphic listing sentinel events (Tanner stages, peak height velocity, menarche) in typical chronological order with anticipated normal age ranges.
Digital design problems
UpToDate fails to take full advantage of the electronic environment. Inexplicably, in the Contents menu screens, Find in Text is not active, and users cannot navigate using the Page-Up/Page-Down or (Ctrl+)Home/End buttons on their keypads. For example, following Contents through “Patient Education” to “Women’s Health Issues,” users find 48 topics in 19 sections as they try to locate the one of interest.
“Mammography” is integrated into “Screening for breast cancer,” and is not a separate keyword for users who are visually scanning for that word (the only option).
Right-clicking is not supported.
An Editmenu is absent. Windows’ Cut and Paste keyboard conventions (Ctrl-c/Ctrl-v) are supported in the main UpToDate window—but not in other windows.
Bookmarking—the electronic equivalent of the folded page corner—is unavailable, as is a favoriteslist.
Highlighting—electronic yellow, blue, and pink markers—is not supported.
No facility for user-added annotation is available.
Opening multiple windows of information simultaneously is not possible.
Standard resizing of the main UpToDate window (by “grabbing” edges of the window) is not supported.
Finally, an ability to limit searches from the main screen to patient handouts or Lexi-Comp would be desirable.
Pocket version
UpToDate also provides a Pocket PC version. The Pocket PC version searches the same database with a search engine similar to the other versions. It lacks the search history offered in the CD version. Although faster than searching through a textbook, an average UpToDate search on Dell Axim X5 400 mHz (Intel PXA250) with 64 MB RAM and a SanDisk 1G CompactFlash card took about 10 to 27 seconds, plus more time to navigate through the long and sometimes cumbersome submenus.
The primary intent for palmtop medical software is point-of-care use. The extensiveness of UpToDate’s text—occupying 800 MB of the 1G card—and limited speed of palmtop computers often makes this impractical. However, it should be emphasized that this rich, inclusive database is a valuable reference when time is not at a premium. Certainly, the Pocket PC version provides ultimate portability. Users contemplating use of UpToDate/Pocket PC should budget for a highend Pocket PC and a 1G card.
Conclusions
UpToDate is a clinically useful, searchable database of medical information updated every 4 months and available on CD, online, and for souped-up Pocket PC palmtop devices. It is almost as if UpToDate purposely incorporated an unsophisticated search engine and did not optimize the electronic environment to flaunt its forte—the clinical database.
For family physicians, the database is of sufficiently high quality, and it will be even more useful as the pediatric module expands. We hope that future enhancements to UpToDate will include clinical bullets for point-of-care use and optimization of the electronic environment. The latter should include implementation of Boolean searches; bookmarks; highlighters; a user-added note facility; copying and pasting of references; links to drug cost information; and—the whole point of Windows! — multi-window capability and conventional window resizing.
Patient information needs to be more accessible to be clinically useful. Also, versions of the patient information handouts with less complex language to appeal to the average patient would be helpful. As is, UpToDate’s importance will only increase. Highly recommended.
CONTACT INFORMATION
UpToDate, 34 Washington Street, Wellesley, MA 02481. Phone: 800-998-6374 (US and Canada) or 781-237-4788; Fax: 781-239-0391.
Free customer support line, Monday–Friday, 8:00 AM–6:30 PM (EST). Subscription or order information: customerservice@uptodate.com. General inquiries: info@uptodate.com. Technical support: support@upto-date.com. Web site: www.uptodate.com.
PRICING
New annual subscription: $495; renewal: $395; trainees: $195; group and institutional pricing: contact enterprise@uptodate.com.
Shipping to US and Canada: $15/year; elsewhere: $35/year. 60-day trial period during which purchaser may return all materials for a full refund.
Virtual tour available at www.uptodate.com. American Academy of Family Physicians members: free 14-day trial via www.aafp.org. Upon expiration (4 months), message alerts user that content is out of date. CDs cease to function 1 year from issue date.
SPECIFICATIONS
Initial: Windows or Macintosh and Pocket PC CD-ROMs, online user name and password. Two updates shipped at 4-month intervals (12-month subscription). Installation and activation directions, search tips, CD-based (or online) tutorial.
MINIMUM REQUIREMENTS
Computer requirements: CD-ROM drive (8X recommended), 16 MB RAM, 15 MB free hard disk space. Windows PC: 486/66 or Pentium processor running Microsoft Windows 95 or later. Macintosh: Power PC or G3/G4 processor running OS 8.1 or later. Online:Standard Web browser with cookies enabled. Recommended connection speed of at least 56K. Pocket PC requirements: Windows PC with CD-ROM drive. Pocket PC device running Windows Pocket PC 2000 or 2002 with Type II CompactFlash slot, expanded storage card/drive (1 GB; uses 800 MB), Pocket PC cradle, and media reader (connects storage device directly to the PC). Additional details: www.uptodate.com
Correspondence
Gary N. Fox, MD, Mercy Health Partners Family Practice Residency Program, 2200 Jefferson Ave, Toledo OH 43624-1117. E-mail: foxgary@yahoo.com.
Tools for rapid preoperative cardiovascular risk assessment
Stating that a patient is “cleared for surgery” is no longer considered adequate; rather, the patient should be assessed for surgical risk, a major component of which is cardiovascular risk. The risk level helps the surgical team determine which preoperative, intraoperative, and postoperative assessments and therapies are indicated.1
Clinical decision tools to assist physicians perform preoperative cardiovascular assessment have been developed and validated, and some have been adapted to handheld computers (Table 1).1-8 Yet few prospective or randomized studies have been conducted to establish the value of various preoperative assessment strategies on outcome.1 In this report, we review the studies underlying these rules and the corresponding software programs for handheld computers (also known as personal digital assistants, or PDAs). Our goal is to find readily applicable software that assists physicians in performing rapid preoperative cardiovascular assessment of patients in the office or hospital.
Cardiovascular Decision Tools
Some cardiovascular decision tools, such as those developed by the American College of Physicians (ACP) and American College of Cardiology/American Heart Association (ACC/AHA), are algorithmic approaches that make direct recommendations about whether to pursue cardiac testing. These tools are designed to be widely applicable to potential candidates for noncardiac surgery.
Other decision tools provide a risk score or index, which the user must interpret and translate into perioperative recommendations. The physician must also assure that the index is appropriate to the patient being evaluated by considering the original study’s patient selection criteria, the setting in which the rule was validated (eg, referral center), and which outcomes the rule predicts. Table 2provides more detailed information about each rule, as well as an assessment of each rule’s methodologic rigor (adapted from methodologic standards for clinical prediction rules developed by Wasson et al10).
Limitations
Even when applied correctly, these indices have substantial limits. The positive predictive values (percentage of patients predicted to have complications who actually suffer a complication) are generally low and, especially in the case of higher-risk surgery, a low risk score does not eliminate the risk of complications.2
It is therefore important to consider the overall risk of adverse outcomes for patients undergoing a particular kind of surgery (the “pretest probability”): the same patient planning cataract surgery and vascular surgery has 2 distinctly different risks, despite having the same score on the biomedical components of the index. Also, these decision support tools were developed using information from patients enrolled during past decades, and their results may not be directly applicable to current surgical risks.4 Finally, these indices cannot be used on all patients. For example, a patient with a rare or unusual problem such as left atrial myxoma may be at a higher risk than would otherwise be indicated by one of the decision support tools.3
TABLE 1
Program information
| Algorithm | Program | Version | Size | Cost | Source |
|---|---|---|---|---|---|
| ACC/AHA1 2002 | STAT Cardiac Clearance | 1.1 | 97 KB | Free | http://www.statcoder.com |
| Detsky3 | MedRules | 2.5 | 324 KB | Free | http://pbrain.hypermart.net/ |
| Detsky6 | InfoRetriever | 4.2 (beta) | 2.1 MB | Beta is free;cost of final version unknown | http://www.infopoems.com |
TABLE 2
Selected characteristics of studies of perioperative risk assessment
| Decision rule | Study population characteristics | Derivation and validation set sample size; years of enrollment | Prospective data collection and reviewer blinding | Major outcomes measured and number of outcomes | Pretest probabilities† | |
|---|---|---|---|---|---|---|
| ACC/AHA1 | All noncardiac surgery, major & minor | N/A / N/A Evidencebased guideline | N/A | N/A | N/A | |
| ACP2 | All noncardiac surgery, major & minor | N/A / N/A Evidence based consensus guideline | N/A | N/A | N/A | |
| Detsky3,6 | All noncardiac surgery, major & minor, at a large teaching hospital. Patients were 40 years and older, referred by the surgical services for consultation because of a question of cardiac risk or chronic disease.a | Not specified/ 455; Enrollment years not specified | Blinded,* prospective collection of validation data | Cardiac death, nonfatal myocardial infarction, ventricular tachycardia or fibrillation requiring counter shock, and nonfatal alveolar pulmonary edema;30 outcomes occurred3 | Major surgery‡
| |
| Minor surgery 1.6%/2.1% (eg, TURP, cataracts) | ||||||
| Mangano/Goldman4,9 | Consecutive unselected patients at a large teaching hospital. Patients were 40 years and older; patients with angina or those undergoing minor surgery were excludedb | 1001/None; 1975–1976 | Derivation set data not uniformly prospective; blinding not mentioned | Myocardial infarction,pulmonary edema, ventricular tachycardia; 58 outcomes occurred | 5.8% | |
| Lee5 | All patients at a large teaching hospital, 50 years and older, with an anticipated surgical length of stay ≥ 2 daysc | 2893/1422; 1989–1994 | Blinded, prospective collection of derivation and validation set data | Myocardial infarction,pulmonary edema, ventricular fibrillation or cardiac arrest, complete heart block; 36 outcomes occurred | 2.5% | |
| Steyerberg7 | Consecutive patients for primary elective abdominal aortic aneurysm surgery at a university hospital in the Netherlandsd | 238/None; 1977–1988 | Unclear whether data collection was prospective and whether reviewer was blinded | Surgical mortality; 18 deaths | 7.6% | |
| L’Italien8 | Consecutive vascular surgery patients at 5 teaching hospitals referred to their respective institutions’ nuclear cardiology laboratory for preoperative ipyridamole-thallium testing.e | 567/514; 1988–1991 | Derivation data collection was retrospective; validation data collection was prospective. Unclear whether reviewer was blinded | Cardiac death, fatal/nonfatal myocardial infarction, not pulmonary edema or congestive heart failure; 39 outcomes occurred | Surgical type | Training/Validation sets |
| Aortic | 6% / 6% | |||||
| Infrainguinal | 13% / 10% | |||||
| Carotid | 6% / 6% | |||||
| Total | 8% / 8% | |||||
| All studies described the mathematical model used in constructing the decision rule. None of the studies reported measuring the clinical effect of applying the decision rule. It is evident most rules are based on studies with methodologic concerns and relatively small numbers of target outcomes. The small numbers of outcome events in any 1 subgroup, group, or study means that a difference of 1 or 2 more or fewer outcomes could substantially change the reported results, especially the pretest probability. | ||||||
| *Blinding of postoperative evaluators to preoperative information and classification. | ||||||
| †Overall rate in study of target outcomes when more specific data are not available. | ||||||
| ‡First percentage: Rate of cardiac death, myocardial infarction, pulmonary edema; second percentage additionally includes worsened coronary insufficiency and congestive heart failure without pulmonary edema. | ||||||
| a. "Not a sample of consecutive patients undergoing surgery, and, therefore, our pretest probabilities will be higher than those that would be found in [a consecutive series]." | ||||||
| b. Because 1977 data excluded minor surgery, unclear how 1995 revision was constructed to include patients undergoing minor procedures. Subject to ascertainment bias because all patients were not studied postoperatively for silent myocardial infarction and other complications. | ||||||
| c. Validation set performed poorly for abdominal aortic aneurysm surgery; authors speculated low number of patients (~100) in derivation set responsible. | ||||||
| d. Patient sample from Netherlands. 238 patients represents "core" because authors used "unique" methods ("We used a new statistical method to quantify the combined effect...") that may be subject to question to "expand" their sample size beyond the actual number of patients studied. | ||||||
| e. Applicable to vascular surgery candidates who require preoperative nuclear stress tests. | ||||||
| N/A, not applicable, none or not specified, not available; TURP, transurethral prostatectomy. | ||||||
Assessing risk factors
Regardless of the risk assessment strategy, physicians should avoid overly aggressive preoperative investigation. The ACC/AHA state in their guideline on perioperative risk assessment that “intervention is rarely necessary simply to lower the risk of surgery unless such intervention is indicated irrespective of the preoperative context.”1
Coronary arteriography has a 0.3% mortality risk. Coronary artery bypass grafting (CABG) is associated with an overall operative mortality risk of 3%.11 In patients undergoing noncardiac surgery who have significant coronary artery disease without antecedent CABG, overall cardiac mortality is 2.4%, compared with 0.5% for those with antecedent CABG.12 Therefore, performing otherwise unnecessary bypass grafting simply to lower the risk of a subsequent surgical procedure incurs an antecedent mortality of greater than 3% from the CABG, whereas proceeding directly to the indicated procedure, on average, produces a 2.4% cardiac mortality.
However, patients who are otherwise candidates for CABG may be first identified when being evaluated for another surgical procedure. In such cases, when the intended surgery can be safely delayed, performing the CABG first is then most logical because the combined mortality of the procedures will be lowest when the CABG is performed first.
All of these tools focus exclusively on cardiovascular risk stratification or preoperative cardiac management (except the decision tool of Steyerburg et al 7; see below). Interestingly, few or none incorporate such risk factors as smoking, hypertension, or serum albumin, which are not independent predictors of major perioperative cardiac events. Two risk factors common to all algorithms are heart failure and prior myocardial infarction (MI). Seven of the 8 algorithms incorporate renal insufficiency, signs or symptoms of current coronary ischemia, and age. In branching algorithms, factors that may be included in an algorithm may not always be considered for a particular patient.
Electronic Decision Tools
STAT Cardiac Clearance
STAT Cardiac Clearance (STAT CC) version 1.1 (March 2002) is single-function software that exclusively performs cardiac preoperative assessment. After starting the program, the user chooses between the ACC/AHA 2002 algorithm and the ACP 1997 algorithm. Both of these algorithms provide management recommendations based on patient characteristics and surgical type. Both algorithms present users a series of yes/no questions (Figure 1), check boxes, and multiple choice questions, all completed by a tap with the stylus on the handheld computer’s touch-sensitive screen.
For the ACP algorithm, users eventually arrive at a management recommendation, such as “Sequence coronary revascularization and noncardiac management according to relative urgency of each and patient preference” or “Proceed directly to surgery.” Similarly, following the ACC/AHA algorithm, users receive recommendations such as “Operating room. Postoperative risk stratification and risk factor management.” The only problem in following either protocol’s implementation for the handheld is STAT CC-ACP algorithm’s use of “creatinine >260 mmol/L” (this value should be 260 μmol/L) and failure to note that this value is equivalent to 3 mg/dL. Both algorithms include patients with known coronary heart disease and patients undergoing major noncardiac and minor surgical procedures. The full text of the executive summary of the ACC/AHA article is available on STAT CC’s pull-down menu.
An addendum in the print version of the ACP protocol recommends “the perioperative use of atenolol in patients with coronary artery disease or risk factors for coronary artery disease… unless the patient has significant contraindications” based on information that became available after the guidelines were approved.2 This recommendation is not mentioned in the electronic implementation.
FIGURE 1
Stat Cardiac Clearance’s implementation of ACC/AHA guidelines
MedRules
MedRules (version 2.5, 2002) is a compilation of about 40 clinical prediction rules. Among these are 3 preoperative risk indices. Other than providing the literature citation for each rule, no assistance is provided in applying the rules. For example, users are not provided information to determine to which specific patient populations each rule applies.
MedRules’ Detsky calculator is a series of 3 screens of check boxes, all straightforward except the undefined “CCS Class” (Figure 2). Users can easily navigate among these screens to change entries if desired. The final result is a point total, risk class, and prediction of risk of major cardiac complications, eg, “15/100 points = class III: 20% risk of major cardiac complications.” Similarly, MedRules’ Goldman calculator is 3 screens of check boxes, also easily navigable in both directions.
In MedRules’ incarnation, an obvious major difference between the Detsky and Goldman implementations is Goldman’s categorization of surgical type into low-risk (minor) and high-risk (major) surgery. With other factors equal, risk of major cardiac complications may range from 3% (minor surgery) to 30% (high-risk procedure). An example result from MedRules’ Goldman index is “14/53 points = class III: 12% risk of major cardiac complications.” The original reference 4 and the software yield the same point totals and risk class.
However, at break points in the classification system, marked changes in risk occur with a 1-point differential in score. For example, for major noncardiac surgery, no difference in risk is reported between 6 and 12 points (4%) and no difference between 13 and 25 points (12%), but risk triples from 4% to 12% by adding 1 point from 12 to 13 points.
MedRules’ third algorithm, Lee’s Simple Cardiac Risk Score,5 fits on 2 screens. The maximum Lee score is 6 points. However, 1 point yields a risk of about 1%, whereas “class IV” is 3 or more points, for which the risk according to Lee et al5 is 9.1% in the derivation set and 11.0% in the validation set. For 3 or more points, MedRules’ calculator indicates “at high risk, >10% risk of major cardiac complications.” At 2 points, the risk is estimated at 7%, regardless of which factors are selected. With either 0 or 1 point, the Lee calculator returns a “<1% risk of major cardiac complications,” even if that risk is abdominal aortic aneurysm repair or a positive exercise stress test.
Obviously, with a 6-point scale and essentially 3 risk categories (in MedRules’ implementation, <1%, 7%, >10%), the Lee algorithm is extremely insensitive to small changes in risk.
FIGURE 2
MedRules’ Detsky calculator
InfoRetriever
The 3 preoperative risk assessment tools on InfoRetriever (version 4.2 for Palm OS, 2002) comprise a tiny piece of this large (by palmtop standards) 2088K (2.1MB) collection of 90 clinical decision rules and other clinical tools. InfoRetriever’s opening screen offers a choice among “Clinical decision rules,” “Diagnostic tests,” and “History and physical.” After choosing “Clinical decision rules,” the user taps to invoke a drop-down menu, and then selects “CV–pre-op eval.” At this point, choices for 3 decision rules appear: “AAA surgery” (Steyerberg), “Non-vascular surgery” (Detsky), and “Vascular surgery” (L’Italien).
The major difference between InfoRetriever’s and MedRules’ Detsky calculators is that InfoRetriever divides surgery into major or minor procedures. The 2 algorithms also differ in asking whether unstable angina has been present in the past 3 months (MedRules) or past 6 months (InfoRetriever). Interestingly, Detsky’s 2 publications about his 1 study also differ in this regard.3,6 InfoRetriever defines angina class, eg, “class III: symptoms w/ level walking of 1 to 2 blocks or climbing ≥1 flight stairs,” whereas MedRules does not. Both of Detsky’s publications allow users to choose any desired pretest probability (overall operation-specific surgical risk) and, from a nomogram that includes the Detsky score, find the corresponding posttest probability (patient’s specific calculated risk).
Neither InfoRetriever’s nor MedRules’ Detsky calculators allow user input of pretest probability. InfoRetriever uses 2 stated, predetermined pretest probabilities (eg, 5% and 10%) and generates 2 corresponding, patient-specific posttest probabilities. MedRules uses a single, unstated pretest probability. Therefore, although both programs accurately calculate Detsky point totals, we conclude that neither completely reproduces the originally published material.
Comparing results between InfoRetriever’s and MedRules’ Detsky calculators, entering the same data for a patient whose MedRules’ Detsky result is 25/100 points, or a 20% risk of major cardiac complications, into InfoRetriever’s Detsky calculator results in “Moderate risk (II): Peri-operative risk of MI, CHF, or death is 15.9% given a pretest risk of 5%; 28.5% given a pretest risk of 10%.” Entering a higher-risk patient, MedRules’ Detsky calculates 40/100 points, and a “100% risk of major cardiac complications,” whereas InfoRetriever’s Detsky calculation produces “44% given a pretest risk of 5%, 62.3% given a pretest risk of 10%.” In contrast to MedRules, for this (and its other indices), InfoRetriever’s information screens discuss the patient population, provide a “quality score” (but no explanation of it) for the index’s referenced study, and specify the number of patients in the study. However, we believe this information is inadequate to guide clinicians in using the indices.
InfoRetriever’s vascular surgery risk index includes risk stratification based on whether a dipyridamole-thallium stress test was performed and, if so, whether a fixed defect, reversible defect, ≥1 mm ST segment depression, or any combination of these findings, was identified.8 The calculator requires the “complication rate at your institution (%),” without providing additional assistance. From the article by L’Italien et al,8 the reader can infer that the “average risk of a major perioperative cardiac event among vascular surgery candidates” would be acceptable as the input for the complication rate. However, the pretest probability for the specific type of vascular surgery (eg, carotid, infrainguinal) would be preferable (Table 2). Study end points were cardiac death, fatal and nonfatal MI, but not pulmonary edema caused by cardiac ischemia.
InfoRetriever’s final calculator, the algorithm by Steyerberg et al7 for elective repair of abdominal aortic aneurysms (AAA), is 2 screens comprising mostly check boxes. Drop-down menus are provided for age group (3 choices) and “Your center’s mean surgical mortality” (which should specify mortality for elective AAA repair), with choices from 3% to 12% (Figure 3). Steyerberg’s algorithm differs from the others in this review in that the intent is to predict total surgical mortality, not solely major cardiac risk. The focus is to help physicians assess and compare the operative risk of elective AAA repair with the reported natural history of nonoperative management of AAA, which may be particularly important in patients at advanced ages or with a limited life expectancy. No validation set is available for this index; the derivation set was 238 consecutive AAA patients enrolled from 1977 to 1988 from 1 institution in the Netherlands. It is unclear from the report7 whether the patients were enrolled prospectively. Until validated, we believe this decision aid needs to be cautiously applied.
FIGURE 3
InfoRetriever’s abdominal aortic aneurysm decision rule
Discussion And Conclusion
Based on our evaluation, we believe that few physicians will have detailed knowledge of the pertinent literature and the expertise to apply these risk indices accurately. However, the electronic implementation of the indices simplifies carrying them to the bedside. In our opinion, their main use is as checklists that serve as reminders of independent risk factors for adverse perioperative cardiac outcomes.
A major enhancement to each of these programs would be the addition of an opening screen that explained to which patients the program should be applied. However, the algorithmic preoperative management tools are well suited to the electronic and clinical environment.
Because the ACC/AHA decision support tool is newer (2002), we prefer it to the ACP tool (1997). STAT CC’s implementation is straightforward, occupies only 97K, and is free. For physicians who wish a low-, intermediate-, and high-risk classification, we recommend using Eagle’s 5-point, 3-class (0, 1–2, 3 points or more), easy-to-memorize scale (age >70, angina, prior MI [by history or ECG Q-waves], diabetes mellitus, congestive heart failure)—and forget the electronics.#
We believe an index such as the Detsky could (and should) be adapted for handheld computers, but the implementation of the versions we reviewed lack the features necessary for general utility. Such a version requires not only an explanation of angina classes, but also entry of pretest probability, specifically surgical risk for the surgical type. Many potential users probably will not know their institutions’ risk numbers for specific surgical types. Therefore, users should be assisted with estimating this entry based on literature values and suggestions about altering those values for the specific situation. While we like Steyerberg’s concept of estimating operative versus nonoperative mortality in AAA clinical decision-making, we await validation of this index.
1. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary: a report of the American College of Cardiology/American Heart Association Task Force onPractice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol 2002;39:542-53.
2. Guidelines for assessing and managing the perioperative risk from coronary artery disease associated with major noncardiac surgery-American College of Physicians. Ann Intern Med 1997;127:309-12.Also available at: http://www.acponline.org/journals/annals/15aug97/ppcad1.htm.
3. Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery. A multifactorial clinical risk index. Arch Intern Med 1986;146:2131-4.
4. Mangano DT, Goldman L. Preoperative assessment of patients with known or suspected coronary disease. N Engl J Med 1995;333:1750-6.
5. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043-9.
6. Detsky AS, Abrams HB, McLaughlin JR, et al. Predicting cardiac complications in patients undergoing non-cardiac surgery. J Gen Intern Med 1986;1:211-9.
7. Steyerberg EW, Kievit J, de Mol Van Otterloo JC, van Bockel JH, Eijkemans MJ, Habbema JD. Perioperative mortality of elective abdominal aortic aneurysm surgery. A clinical prediction rule based on literature and individual patient data. Arch Intern Med 1995;155:1998-2004.
8. L’Italien GJ, Paul SD, Hendel RC, et al. Development and validation of a Bayesian model for perioperative cardiac risk assessment in a cohort of 1,081 vascular surgical candidates. J Am Coll Cardiol 1996;27:779-86.
9. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297:845-50.
10. Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med 1985;313:793-9.
11. Romero L, de Virgilio C. Preoperative cardiac risk assessment: an updated approach. Arch Surg 2001;136:1370-6.
12. Hollenberg SM. Preoperative cardiac risk assessment. Chest 1999;115(suppl):51S-57S.
13. Paul SD, Eagle KA. A stepwise strategy for coronary risk assessment for noncardiac surgery. Med Clin North Am 1995;79:1241-62.
Stating that a patient is “cleared for surgery” is no longer considered adequate; rather, the patient should be assessed for surgical risk, a major component of which is cardiovascular risk. The risk level helps the surgical team determine which preoperative, intraoperative, and postoperative assessments and therapies are indicated.1
Clinical decision tools to assist physicians perform preoperative cardiovascular assessment have been developed and validated, and some have been adapted to handheld computers (Table 1).1-8 Yet few prospective or randomized studies have been conducted to establish the value of various preoperative assessment strategies on outcome.1 In this report, we review the studies underlying these rules and the corresponding software programs for handheld computers (also known as personal digital assistants, or PDAs). Our goal is to find readily applicable software that assists physicians in performing rapid preoperative cardiovascular assessment of patients in the office or hospital.
Cardiovascular Decision Tools
Some cardiovascular decision tools, such as those developed by the American College of Physicians (ACP) and American College of Cardiology/American Heart Association (ACC/AHA), are algorithmic approaches that make direct recommendations about whether to pursue cardiac testing. These tools are designed to be widely applicable to potential candidates for noncardiac surgery.
Other decision tools provide a risk score or index, which the user must interpret and translate into perioperative recommendations. The physician must also assure that the index is appropriate to the patient being evaluated by considering the original study’s patient selection criteria, the setting in which the rule was validated (eg, referral center), and which outcomes the rule predicts. Table 2provides more detailed information about each rule, as well as an assessment of each rule’s methodologic rigor (adapted from methodologic standards for clinical prediction rules developed by Wasson et al10).
Limitations
Even when applied correctly, these indices have substantial limits. The positive predictive values (percentage of patients predicted to have complications who actually suffer a complication) are generally low and, especially in the case of higher-risk surgery, a low risk score does not eliminate the risk of complications.2
It is therefore important to consider the overall risk of adverse outcomes for patients undergoing a particular kind of surgery (the “pretest probability”): the same patient planning cataract surgery and vascular surgery has 2 distinctly different risks, despite having the same score on the biomedical components of the index. Also, these decision support tools were developed using information from patients enrolled during past decades, and their results may not be directly applicable to current surgical risks.4 Finally, these indices cannot be used on all patients. For example, a patient with a rare or unusual problem such as left atrial myxoma may be at a higher risk than would otherwise be indicated by one of the decision support tools.3
TABLE 1
Program information
| Algorithm | Program | Version | Size | Cost | Source |
|---|---|---|---|---|---|
| ACC/AHA1 2002 | STAT Cardiac Clearance | 1.1 | 97 KB | Free | http://www.statcoder.com |
| Detsky3 | MedRules | 2.5 | 324 KB | Free | http://pbrain.hypermart.net/ |
| Detsky6 | InfoRetriever | 4.2 (beta) | 2.1 MB | Beta is free;cost of final version unknown | http://www.infopoems.com |
TABLE 2
Selected characteristics of studies of perioperative risk assessment
| Decision rule | Study population characteristics | Derivation and validation set sample size; years of enrollment | Prospective data collection and reviewer blinding | Major outcomes measured and number of outcomes | Pretest probabilities† | |
|---|---|---|---|---|---|---|
| ACC/AHA1 | All noncardiac surgery, major & minor | N/A / N/A Evidencebased guideline | N/A | N/A | N/A | |
| ACP2 | All noncardiac surgery, major & minor | N/A / N/A Evidence based consensus guideline | N/A | N/A | N/A | |
| Detsky3,6 | All noncardiac surgery, major & minor, at a large teaching hospital. Patients were 40 years and older, referred by the surgical services for consultation because of a question of cardiac risk or chronic disease.a | Not specified/ 455; Enrollment years not specified | Blinded,* prospective collection of validation data | Cardiac death, nonfatal myocardial infarction, ventricular tachycardia or fibrillation requiring counter shock, and nonfatal alveolar pulmonary edema;30 outcomes occurred3 | Major surgery‡
| |
| Minor surgery 1.6%/2.1% (eg, TURP, cataracts) | ||||||
| Mangano/Goldman4,9 | Consecutive unselected patients at a large teaching hospital. Patients were 40 years and older; patients with angina or those undergoing minor surgery were excludedb | 1001/None; 1975–1976 | Derivation set data not uniformly prospective; blinding not mentioned | Myocardial infarction,pulmonary edema, ventricular tachycardia; 58 outcomes occurred | 5.8% | |
| Lee5 | All patients at a large teaching hospital, 50 years and older, with an anticipated surgical length of stay ≥ 2 daysc | 2893/1422; 1989–1994 | Blinded, prospective collection of derivation and validation set data | Myocardial infarction,pulmonary edema, ventricular fibrillation or cardiac arrest, complete heart block; 36 outcomes occurred | 2.5% | |
| Steyerberg7 | Consecutive patients for primary elective abdominal aortic aneurysm surgery at a university hospital in the Netherlandsd | 238/None; 1977–1988 | Unclear whether data collection was prospective and whether reviewer was blinded | Surgical mortality; 18 deaths | 7.6% | |
| L’Italien8 | Consecutive vascular surgery patients at 5 teaching hospitals referred to their respective institutions’ nuclear cardiology laboratory for preoperative ipyridamole-thallium testing.e | 567/514; 1988–1991 | Derivation data collection was retrospective; validation data collection was prospective. Unclear whether reviewer was blinded | Cardiac death, fatal/nonfatal myocardial infarction, not pulmonary edema or congestive heart failure; 39 outcomes occurred | Surgical type | Training/Validation sets |
| Aortic | 6% / 6% | |||||
| Infrainguinal | 13% / 10% | |||||
| Carotid | 6% / 6% | |||||
| Total | 8% / 8% | |||||
| All studies described the mathematical model used in constructing the decision rule. None of the studies reported measuring the clinical effect of applying the decision rule. It is evident most rules are based on studies with methodologic concerns and relatively small numbers of target outcomes. The small numbers of outcome events in any 1 subgroup, group, or study means that a difference of 1 or 2 more or fewer outcomes could substantially change the reported results, especially the pretest probability. | ||||||
| *Blinding of postoperative evaluators to preoperative information and classification. | ||||||
| †Overall rate in study of target outcomes when more specific data are not available. | ||||||
| ‡First percentage: Rate of cardiac death, myocardial infarction, pulmonary edema; second percentage additionally includes worsened coronary insufficiency and congestive heart failure without pulmonary edema. | ||||||
| a. "Not a sample of consecutive patients undergoing surgery, and, therefore, our pretest probabilities will be higher than those that would be found in [a consecutive series]." | ||||||
| b. Because 1977 data excluded minor surgery, unclear how 1995 revision was constructed to include patients undergoing minor procedures. Subject to ascertainment bias because all patients were not studied postoperatively for silent myocardial infarction and other complications. | ||||||
| c. Validation set performed poorly for abdominal aortic aneurysm surgery; authors speculated low number of patients (~100) in derivation set responsible. | ||||||
| d. Patient sample from Netherlands. 238 patients represents "core" because authors used "unique" methods ("We used a new statistical method to quantify the combined effect...") that may be subject to question to "expand" their sample size beyond the actual number of patients studied. | ||||||
| e. Applicable to vascular surgery candidates who require preoperative nuclear stress tests. | ||||||
| N/A, not applicable, none or not specified, not available; TURP, transurethral prostatectomy. | ||||||
Assessing risk factors
Regardless of the risk assessment strategy, physicians should avoid overly aggressive preoperative investigation. The ACC/AHA state in their guideline on perioperative risk assessment that “intervention is rarely necessary simply to lower the risk of surgery unless such intervention is indicated irrespective of the preoperative context.”1
Coronary arteriography has a 0.3% mortality risk. Coronary artery bypass grafting (CABG) is associated with an overall operative mortality risk of 3%.11 In patients undergoing noncardiac surgery who have significant coronary artery disease without antecedent CABG, overall cardiac mortality is 2.4%, compared with 0.5% for those with antecedent CABG.12 Therefore, performing otherwise unnecessary bypass grafting simply to lower the risk of a subsequent surgical procedure incurs an antecedent mortality of greater than 3% from the CABG, whereas proceeding directly to the indicated procedure, on average, produces a 2.4% cardiac mortality.
However, patients who are otherwise candidates for CABG may be first identified when being evaluated for another surgical procedure. In such cases, when the intended surgery can be safely delayed, performing the CABG first is then most logical because the combined mortality of the procedures will be lowest when the CABG is performed first.
All of these tools focus exclusively on cardiovascular risk stratification or preoperative cardiac management (except the decision tool of Steyerburg et al 7; see below). Interestingly, few or none incorporate such risk factors as smoking, hypertension, or serum albumin, which are not independent predictors of major perioperative cardiac events. Two risk factors common to all algorithms are heart failure and prior myocardial infarction (MI). Seven of the 8 algorithms incorporate renal insufficiency, signs or symptoms of current coronary ischemia, and age. In branching algorithms, factors that may be included in an algorithm may not always be considered for a particular patient.
Electronic Decision Tools
STAT Cardiac Clearance
STAT Cardiac Clearance (STAT CC) version 1.1 (March 2002) is single-function software that exclusively performs cardiac preoperative assessment. After starting the program, the user chooses between the ACC/AHA 2002 algorithm and the ACP 1997 algorithm. Both of these algorithms provide management recommendations based on patient characteristics and surgical type. Both algorithms present users a series of yes/no questions (Figure 1), check boxes, and multiple choice questions, all completed by a tap with the stylus on the handheld computer’s touch-sensitive screen.
For the ACP algorithm, users eventually arrive at a management recommendation, such as “Sequence coronary revascularization and noncardiac management according to relative urgency of each and patient preference” or “Proceed directly to surgery.” Similarly, following the ACC/AHA algorithm, users receive recommendations such as “Operating room. Postoperative risk stratification and risk factor management.” The only problem in following either protocol’s implementation for the handheld is STAT CC-ACP algorithm’s use of “creatinine >260 mmol/L” (this value should be 260 μmol/L) and failure to note that this value is equivalent to 3 mg/dL. Both algorithms include patients with known coronary heart disease and patients undergoing major noncardiac and minor surgical procedures. The full text of the executive summary of the ACC/AHA article is available on STAT CC’s pull-down menu.
An addendum in the print version of the ACP protocol recommends “the perioperative use of atenolol in patients with coronary artery disease or risk factors for coronary artery disease… unless the patient has significant contraindications” based on information that became available after the guidelines were approved.2 This recommendation is not mentioned in the electronic implementation.
FIGURE 1
Stat Cardiac Clearance’s implementation of ACC/AHA guidelines
MedRules
MedRules (version 2.5, 2002) is a compilation of about 40 clinical prediction rules. Among these are 3 preoperative risk indices. Other than providing the literature citation for each rule, no assistance is provided in applying the rules. For example, users are not provided information to determine to which specific patient populations each rule applies.
MedRules’ Detsky calculator is a series of 3 screens of check boxes, all straightforward except the undefined “CCS Class” (Figure 2). Users can easily navigate among these screens to change entries if desired. The final result is a point total, risk class, and prediction of risk of major cardiac complications, eg, “15/100 points = class III: 20% risk of major cardiac complications.” Similarly, MedRules’ Goldman calculator is 3 screens of check boxes, also easily navigable in both directions.
In MedRules’ incarnation, an obvious major difference between the Detsky and Goldman implementations is Goldman’s categorization of surgical type into low-risk (minor) and high-risk (major) surgery. With other factors equal, risk of major cardiac complications may range from 3% (minor surgery) to 30% (high-risk procedure). An example result from MedRules’ Goldman index is “14/53 points = class III: 12% risk of major cardiac complications.” The original reference 4 and the software yield the same point totals and risk class.
However, at break points in the classification system, marked changes in risk occur with a 1-point differential in score. For example, for major noncardiac surgery, no difference in risk is reported between 6 and 12 points (4%) and no difference between 13 and 25 points (12%), but risk triples from 4% to 12% by adding 1 point from 12 to 13 points.
MedRules’ third algorithm, Lee’s Simple Cardiac Risk Score,5 fits on 2 screens. The maximum Lee score is 6 points. However, 1 point yields a risk of about 1%, whereas “class IV” is 3 or more points, for which the risk according to Lee et al5 is 9.1% in the derivation set and 11.0% in the validation set. For 3 or more points, MedRules’ calculator indicates “at high risk, >10% risk of major cardiac complications.” At 2 points, the risk is estimated at 7%, regardless of which factors are selected. With either 0 or 1 point, the Lee calculator returns a “<1% risk of major cardiac complications,” even if that risk is abdominal aortic aneurysm repair or a positive exercise stress test.
Obviously, with a 6-point scale and essentially 3 risk categories (in MedRules’ implementation, <1%, 7%, >10%), the Lee algorithm is extremely insensitive to small changes in risk.
FIGURE 2
MedRules’ Detsky calculator
InfoRetriever
The 3 preoperative risk assessment tools on InfoRetriever (version 4.2 for Palm OS, 2002) comprise a tiny piece of this large (by palmtop standards) 2088K (2.1MB) collection of 90 clinical decision rules and other clinical tools. InfoRetriever’s opening screen offers a choice among “Clinical decision rules,” “Diagnostic tests,” and “History and physical.” After choosing “Clinical decision rules,” the user taps to invoke a drop-down menu, and then selects “CV–pre-op eval.” At this point, choices for 3 decision rules appear: “AAA surgery” (Steyerberg), “Non-vascular surgery” (Detsky), and “Vascular surgery” (L’Italien).
The major difference between InfoRetriever’s and MedRules’ Detsky calculators is that InfoRetriever divides surgery into major or minor procedures. The 2 algorithms also differ in asking whether unstable angina has been present in the past 3 months (MedRules) or past 6 months (InfoRetriever). Interestingly, Detsky’s 2 publications about his 1 study also differ in this regard.3,6 InfoRetriever defines angina class, eg, “class III: symptoms w/ level walking of 1 to 2 blocks or climbing ≥1 flight stairs,” whereas MedRules does not. Both of Detsky’s publications allow users to choose any desired pretest probability (overall operation-specific surgical risk) and, from a nomogram that includes the Detsky score, find the corresponding posttest probability (patient’s specific calculated risk).
Neither InfoRetriever’s nor MedRules’ Detsky calculators allow user input of pretest probability. InfoRetriever uses 2 stated, predetermined pretest probabilities (eg, 5% and 10%) and generates 2 corresponding, patient-specific posttest probabilities. MedRules uses a single, unstated pretest probability. Therefore, although both programs accurately calculate Detsky point totals, we conclude that neither completely reproduces the originally published material.
Comparing results between InfoRetriever’s and MedRules’ Detsky calculators, entering the same data for a patient whose MedRules’ Detsky result is 25/100 points, or a 20% risk of major cardiac complications, into InfoRetriever’s Detsky calculator results in “Moderate risk (II): Peri-operative risk of MI, CHF, or death is 15.9% given a pretest risk of 5%; 28.5% given a pretest risk of 10%.” Entering a higher-risk patient, MedRules’ Detsky calculates 40/100 points, and a “100% risk of major cardiac complications,” whereas InfoRetriever’s Detsky calculation produces “44% given a pretest risk of 5%, 62.3% given a pretest risk of 10%.” In contrast to MedRules, for this (and its other indices), InfoRetriever’s information screens discuss the patient population, provide a “quality score” (but no explanation of it) for the index’s referenced study, and specify the number of patients in the study. However, we believe this information is inadequate to guide clinicians in using the indices.
InfoRetriever’s vascular surgery risk index includes risk stratification based on whether a dipyridamole-thallium stress test was performed and, if so, whether a fixed defect, reversible defect, ≥1 mm ST segment depression, or any combination of these findings, was identified.8 The calculator requires the “complication rate at your institution (%),” without providing additional assistance. From the article by L’Italien et al,8 the reader can infer that the “average risk of a major perioperative cardiac event among vascular surgery candidates” would be acceptable as the input for the complication rate. However, the pretest probability for the specific type of vascular surgery (eg, carotid, infrainguinal) would be preferable (Table 2). Study end points were cardiac death, fatal and nonfatal MI, but not pulmonary edema caused by cardiac ischemia.
InfoRetriever’s final calculator, the algorithm by Steyerberg et al7 for elective repair of abdominal aortic aneurysms (AAA), is 2 screens comprising mostly check boxes. Drop-down menus are provided for age group (3 choices) and “Your center’s mean surgical mortality” (which should specify mortality for elective AAA repair), with choices from 3% to 12% (Figure 3). Steyerberg’s algorithm differs from the others in this review in that the intent is to predict total surgical mortality, not solely major cardiac risk. The focus is to help physicians assess and compare the operative risk of elective AAA repair with the reported natural history of nonoperative management of AAA, which may be particularly important in patients at advanced ages or with a limited life expectancy. No validation set is available for this index; the derivation set was 238 consecutive AAA patients enrolled from 1977 to 1988 from 1 institution in the Netherlands. It is unclear from the report7 whether the patients were enrolled prospectively. Until validated, we believe this decision aid needs to be cautiously applied.
FIGURE 3
InfoRetriever’s abdominal aortic aneurysm decision rule
Discussion And Conclusion
Based on our evaluation, we believe that few physicians will have detailed knowledge of the pertinent literature and the expertise to apply these risk indices accurately. However, the electronic implementation of the indices simplifies carrying them to the bedside. In our opinion, their main use is as checklists that serve as reminders of independent risk factors for adverse perioperative cardiac outcomes.
A major enhancement to each of these programs would be the addition of an opening screen that explained to which patients the program should be applied. However, the algorithmic preoperative management tools are well suited to the electronic and clinical environment.
Because the ACC/AHA decision support tool is newer (2002), we prefer it to the ACP tool (1997). STAT CC’s implementation is straightforward, occupies only 97K, and is free. For physicians who wish a low-, intermediate-, and high-risk classification, we recommend using Eagle’s 5-point, 3-class (0, 1–2, 3 points or more), easy-to-memorize scale (age >70, angina, prior MI [by history or ECG Q-waves], diabetes mellitus, congestive heart failure)—and forget the electronics.#
We believe an index such as the Detsky could (and should) be adapted for handheld computers, but the implementation of the versions we reviewed lack the features necessary for general utility. Such a version requires not only an explanation of angina classes, but also entry of pretest probability, specifically surgical risk for the surgical type. Many potential users probably will not know their institutions’ risk numbers for specific surgical types. Therefore, users should be assisted with estimating this entry based on literature values and suggestions about altering those values for the specific situation. While we like Steyerberg’s concept of estimating operative versus nonoperative mortality in AAA clinical decision-making, we await validation of this index.
Stating that a patient is “cleared for surgery” is no longer considered adequate; rather, the patient should be assessed for surgical risk, a major component of which is cardiovascular risk. The risk level helps the surgical team determine which preoperative, intraoperative, and postoperative assessments and therapies are indicated.1
Clinical decision tools to assist physicians perform preoperative cardiovascular assessment have been developed and validated, and some have been adapted to handheld computers (Table 1).1-8 Yet few prospective or randomized studies have been conducted to establish the value of various preoperative assessment strategies on outcome.1 In this report, we review the studies underlying these rules and the corresponding software programs for handheld computers (also known as personal digital assistants, or PDAs). Our goal is to find readily applicable software that assists physicians in performing rapid preoperative cardiovascular assessment of patients in the office or hospital.
Cardiovascular Decision Tools
Some cardiovascular decision tools, such as those developed by the American College of Physicians (ACP) and American College of Cardiology/American Heart Association (ACC/AHA), are algorithmic approaches that make direct recommendations about whether to pursue cardiac testing. These tools are designed to be widely applicable to potential candidates for noncardiac surgery.
Other decision tools provide a risk score or index, which the user must interpret and translate into perioperative recommendations. The physician must also assure that the index is appropriate to the patient being evaluated by considering the original study’s patient selection criteria, the setting in which the rule was validated (eg, referral center), and which outcomes the rule predicts. Table 2provides more detailed information about each rule, as well as an assessment of each rule’s methodologic rigor (adapted from methodologic standards for clinical prediction rules developed by Wasson et al10).
Limitations
Even when applied correctly, these indices have substantial limits. The positive predictive values (percentage of patients predicted to have complications who actually suffer a complication) are generally low and, especially in the case of higher-risk surgery, a low risk score does not eliminate the risk of complications.2
It is therefore important to consider the overall risk of adverse outcomes for patients undergoing a particular kind of surgery (the “pretest probability”): the same patient planning cataract surgery and vascular surgery has 2 distinctly different risks, despite having the same score on the biomedical components of the index. Also, these decision support tools were developed using information from patients enrolled during past decades, and their results may not be directly applicable to current surgical risks.4 Finally, these indices cannot be used on all patients. For example, a patient with a rare or unusual problem such as left atrial myxoma may be at a higher risk than would otherwise be indicated by one of the decision support tools.3
TABLE 1
Program information
| Algorithm | Program | Version | Size | Cost | Source |
|---|---|---|---|---|---|
| ACC/AHA1 2002 | STAT Cardiac Clearance | 1.1 | 97 KB | Free | http://www.statcoder.com |
| Detsky3 | MedRules | 2.5 | 324 KB | Free | http://pbrain.hypermart.net/ |
| Detsky6 | InfoRetriever | 4.2 (beta) | 2.1 MB | Beta is free;cost of final version unknown | http://www.infopoems.com |
TABLE 2
Selected characteristics of studies of perioperative risk assessment
| Decision rule | Study population characteristics | Derivation and validation set sample size; years of enrollment | Prospective data collection and reviewer blinding | Major outcomes measured and number of outcomes | Pretest probabilities† | |
|---|---|---|---|---|---|---|
| ACC/AHA1 | All noncardiac surgery, major & minor | N/A / N/A Evidencebased guideline | N/A | N/A | N/A | |
| ACP2 | All noncardiac surgery, major & minor | N/A / N/A Evidence based consensus guideline | N/A | N/A | N/A | |
| Detsky3,6 | All noncardiac surgery, major & minor, at a large teaching hospital. Patients were 40 years and older, referred by the surgical services for consultation because of a question of cardiac risk or chronic disease.a | Not specified/ 455; Enrollment years not specified | Blinded,* prospective collection of validation data | Cardiac death, nonfatal myocardial infarction, ventricular tachycardia or fibrillation requiring counter shock, and nonfatal alveolar pulmonary edema;30 outcomes occurred3 | Major surgery‡
| |
| Minor surgery 1.6%/2.1% (eg, TURP, cataracts) | ||||||
| Mangano/Goldman4,9 | Consecutive unselected patients at a large teaching hospital. Patients were 40 years and older; patients with angina or those undergoing minor surgery were excludedb | 1001/None; 1975–1976 | Derivation set data not uniformly prospective; blinding not mentioned | Myocardial infarction,pulmonary edema, ventricular tachycardia; 58 outcomes occurred | 5.8% | |
| Lee5 | All patients at a large teaching hospital, 50 years and older, with an anticipated surgical length of stay ≥ 2 daysc | 2893/1422; 1989–1994 | Blinded, prospective collection of derivation and validation set data | Myocardial infarction,pulmonary edema, ventricular fibrillation or cardiac arrest, complete heart block; 36 outcomes occurred | 2.5% | |
| Steyerberg7 | Consecutive patients for primary elective abdominal aortic aneurysm surgery at a university hospital in the Netherlandsd | 238/None; 1977–1988 | Unclear whether data collection was prospective and whether reviewer was blinded | Surgical mortality; 18 deaths | 7.6% | |
| L’Italien8 | Consecutive vascular surgery patients at 5 teaching hospitals referred to their respective institutions’ nuclear cardiology laboratory for preoperative ipyridamole-thallium testing.e | 567/514; 1988–1991 | Derivation data collection was retrospective; validation data collection was prospective. Unclear whether reviewer was blinded | Cardiac death, fatal/nonfatal myocardial infarction, not pulmonary edema or congestive heart failure; 39 outcomes occurred | Surgical type | Training/Validation sets |
| Aortic | 6% / 6% | |||||
| Infrainguinal | 13% / 10% | |||||
| Carotid | 6% / 6% | |||||
| Total | 8% / 8% | |||||
| All studies described the mathematical model used in constructing the decision rule. None of the studies reported measuring the clinical effect of applying the decision rule. It is evident most rules are based on studies with methodologic concerns and relatively small numbers of target outcomes. The small numbers of outcome events in any 1 subgroup, group, or study means that a difference of 1 or 2 more or fewer outcomes could substantially change the reported results, especially the pretest probability. | ||||||
| *Blinding of postoperative evaluators to preoperative information and classification. | ||||||
| †Overall rate in study of target outcomes when more specific data are not available. | ||||||
| ‡First percentage: Rate of cardiac death, myocardial infarction, pulmonary edema; second percentage additionally includes worsened coronary insufficiency and congestive heart failure without pulmonary edema. | ||||||
| a. "Not a sample of consecutive patients undergoing surgery, and, therefore, our pretest probabilities will be higher than those that would be found in [a consecutive series]." | ||||||
| b. Because 1977 data excluded minor surgery, unclear how 1995 revision was constructed to include patients undergoing minor procedures. Subject to ascertainment bias because all patients were not studied postoperatively for silent myocardial infarction and other complications. | ||||||
| c. Validation set performed poorly for abdominal aortic aneurysm surgery; authors speculated low number of patients (~100) in derivation set responsible. | ||||||
| d. Patient sample from Netherlands. 238 patients represents "core" because authors used "unique" methods ("We used a new statistical method to quantify the combined effect...") that may be subject to question to "expand" their sample size beyond the actual number of patients studied. | ||||||
| e. Applicable to vascular surgery candidates who require preoperative nuclear stress tests. | ||||||
| N/A, not applicable, none or not specified, not available; TURP, transurethral prostatectomy. | ||||||
Assessing risk factors
Regardless of the risk assessment strategy, physicians should avoid overly aggressive preoperative investigation. The ACC/AHA state in their guideline on perioperative risk assessment that “intervention is rarely necessary simply to lower the risk of surgery unless such intervention is indicated irrespective of the preoperative context.”1
Coronary arteriography has a 0.3% mortality risk. Coronary artery bypass grafting (CABG) is associated with an overall operative mortality risk of 3%.11 In patients undergoing noncardiac surgery who have significant coronary artery disease without antecedent CABG, overall cardiac mortality is 2.4%, compared with 0.5% for those with antecedent CABG.12 Therefore, performing otherwise unnecessary bypass grafting simply to lower the risk of a subsequent surgical procedure incurs an antecedent mortality of greater than 3% from the CABG, whereas proceeding directly to the indicated procedure, on average, produces a 2.4% cardiac mortality.
However, patients who are otherwise candidates for CABG may be first identified when being evaluated for another surgical procedure. In such cases, when the intended surgery can be safely delayed, performing the CABG first is then most logical because the combined mortality of the procedures will be lowest when the CABG is performed first.
All of these tools focus exclusively on cardiovascular risk stratification or preoperative cardiac management (except the decision tool of Steyerburg et al 7; see below). Interestingly, few or none incorporate such risk factors as smoking, hypertension, or serum albumin, which are not independent predictors of major perioperative cardiac events. Two risk factors common to all algorithms are heart failure and prior myocardial infarction (MI). Seven of the 8 algorithms incorporate renal insufficiency, signs or symptoms of current coronary ischemia, and age. In branching algorithms, factors that may be included in an algorithm may not always be considered for a particular patient.
Electronic Decision Tools
STAT Cardiac Clearance
STAT Cardiac Clearance (STAT CC) version 1.1 (March 2002) is single-function software that exclusively performs cardiac preoperative assessment. After starting the program, the user chooses between the ACC/AHA 2002 algorithm and the ACP 1997 algorithm. Both of these algorithms provide management recommendations based on patient characteristics and surgical type. Both algorithms present users a series of yes/no questions (Figure 1), check boxes, and multiple choice questions, all completed by a tap with the stylus on the handheld computer’s touch-sensitive screen.
For the ACP algorithm, users eventually arrive at a management recommendation, such as “Sequence coronary revascularization and noncardiac management according to relative urgency of each and patient preference” or “Proceed directly to surgery.” Similarly, following the ACC/AHA algorithm, users receive recommendations such as “Operating room. Postoperative risk stratification and risk factor management.” The only problem in following either protocol’s implementation for the handheld is STAT CC-ACP algorithm’s use of “creatinine >260 mmol/L” (this value should be 260 μmol/L) and failure to note that this value is equivalent to 3 mg/dL. Both algorithms include patients with known coronary heart disease and patients undergoing major noncardiac and minor surgical procedures. The full text of the executive summary of the ACC/AHA article is available on STAT CC’s pull-down menu.
An addendum in the print version of the ACP protocol recommends “the perioperative use of atenolol in patients with coronary artery disease or risk factors for coronary artery disease… unless the patient has significant contraindications” based on information that became available after the guidelines were approved.2 This recommendation is not mentioned in the electronic implementation.
FIGURE 1
Stat Cardiac Clearance’s implementation of ACC/AHA guidelines
MedRules
MedRules (version 2.5, 2002) is a compilation of about 40 clinical prediction rules. Among these are 3 preoperative risk indices. Other than providing the literature citation for each rule, no assistance is provided in applying the rules. For example, users are not provided information to determine to which specific patient populations each rule applies.
MedRules’ Detsky calculator is a series of 3 screens of check boxes, all straightforward except the undefined “CCS Class” (Figure 2). Users can easily navigate among these screens to change entries if desired. The final result is a point total, risk class, and prediction of risk of major cardiac complications, eg, “15/100 points = class III: 20% risk of major cardiac complications.” Similarly, MedRules’ Goldman calculator is 3 screens of check boxes, also easily navigable in both directions.
In MedRules’ incarnation, an obvious major difference between the Detsky and Goldman implementations is Goldman’s categorization of surgical type into low-risk (minor) and high-risk (major) surgery. With other factors equal, risk of major cardiac complications may range from 3% (minor surgery) to 30% (high-risk procedure). An example result from MedRules’ Goldman index is “14/53 points = class III: 12% risk of major cardiac complications.” The original reference 4 and the software yield the same point totals and risk class.
However, at break points in the classification system, marked changes in risk occur with a 1-point differential in score. For example, for major noncardiac surgery, no difference in risk is reported between 6 and 12 points (4%) and no difference between 13 and 25 points (12%), but risk triples from 4% to 12% by adding 1 point from 12 to 13 points.
MedRules’ third algorithm, Lee’s Simple Cardiac Risk Score,5 fits on 2 screens. The maximum Lee score is 6 points. However, 1 point yields a risk of about 1%, whereas “class IV” is 3 or more points, for which the risk according to Lee et al5 is 9.1% in the derivation set and 11.0% in the validation set. For 3 or more points, MedRules’ calculator indicates “at high risk, >10% risk of major cardiac complications.” At 2 points, the risk is estimated at 7%, regardless of which factors are selected. With either 0 or 1 point, the Lee calculator returns a “<1% risk of major cardiac complications,” even if that risk is abdominal aortic aneurysm repair or a positive exercise stress test.
Obviously, with a 6-point scale and essentially 3 risk categories (in MedRules’ implementation, <1%, 7%, >10%), the Lee algorithm is extremely insensitive to small changes in risk.
FIGURE 2
MedRules’ Detsky calculator
InfoRetriever
The 3 preoperative risk assessment tools on InfoRetriever (version 4.2 for Palm OS, 2002) comprise a tiny piece of this large (by palmtop standards) 2088K (2.1MB) collection of 90 clinical decision rules and other clinical tools. InfoRetriever’s opening screen offers a choice among “Clinical decision rules,” “Diagnostic tests,” and “History and physical.” After choosing “Clinical decision rules,” the user taps to invoke a drop-down menu, and then selects “CV–pre-op eval.” At this point, choices for 3 decision rules appear: “AAA surgery” (Steyerberg), “Non-vascular surgery” (Detsky), and “Vascular surgery” (L’Italien).
The major difference between InfoRetriever’s and MedRules’ Detsky calculators is that InfoRetriever divides surgery into major or minor procedures. The 2 algorithms also differ in asking whether unstable angina has been present in the past 3 months (MedRules) or past 6 months (InfoRetriever). Interestingly, Detsky’s 2 publications about his 1 study also differ in this regard.3,6 InfoRetriever defines angina class, eg, “class III: symptoms w/ level walking of 1 to 2 blocks or climbing ≥1 flight stairs,” whereas MedRules does not. Both of Detsky’s publications allow users to choose any desired pretest probability (overall operation-specific surgical risk) and, from a nomogram that includes the Detsky score, find the corresponding posttest probability (patient’s specific calculated risk).
Neither InfoRetriever’s nor MedRules’ Detsky calculators allow user input of pretest probability. InfoRetriever uses 2 stated, predetermined pretest probabilities (eg, 5% and 10%) and generates 2 corresponding, patient-specific posttest probabilities. MedRules uses a single, unstated pretest probability. Therefore, although both programs accurately calculate Detsky point totals, we conclude that neither completely reproduces the originally published material.
Comparing results between InfoRetriever’s and MedRules’ Detsky calculators, entering the same data for a patient whose MedRules’ Detsky result is 25/100 points, or a 20% risk of major cardiac complications, into InfoRetriever’s Detsky calculator results in “Moderate risk (II): Peri-operative risk of MI, CHF, or death is 15.9% given a pretest risk of 5%; 28.5% given a pretest risk of 10%.” Entering a higher-risk patient, MedRules’ Detsky calculates 40/100 points, and a “100% risk of major cardiac complications,” whereas InfoRetriever’s Detsky calculation produces “44% given a pretest risk of 5%, 62.3% given a pretest risk of 10%.” In contrast to MedRules, for this (and its other indices), InfoRetriever’s information screens discuss the patient population, provide a “quality score” (but no explanation of it) for the index’s referenced study, and specify the number of patients in the study. However, we believe this information is inadequate to guide clinicians in using the indices.
InfoRetriever’s vascular surgery risk index includes risk stratification based on whether a dipyridamole-thallium stress test was performed and, if so, whether a fixed defect, reversible defect, ≥1 mm ST segment depression, or any combination of these findings, was identified.8 The calculator requires the “complication rate at your institution (%),” without providing additional assistance. From the article by L’Italien et al,8 the reader can infer that the “average risk of a major perioperative cardiac event among vascular surgery candidates” would be acceptable as the input for the complication rate. However, the pretest probability for the specific type of vascular surgery (eg, carotid, infrainguinal) would be preferable (Table 2). Study end points were cardiac death, fatal and nonfatal MI, but not pulmonary edema caused by cardiac ischemia.
InfoRetriever’s final calculator, the algorithm by Steyerberg et al7 for elective repair of abdominal aortic aneurysms (AAA), is 2 screens comprising mostly check boxes. Drop-down menus are provided for age group (3 choices) and “Your center’s mean surgical mortality” (which should specify mortality for elective AAA repair), with choices from 3% to 12% (Figure 3). Steyerberg’s algorithm differs from the others in this review in that the intent is to predict total surgical mortality, not solely major cardiac risk. The focus is to help physicians assess and compare the operative risk of elective AAA repair with the reported natural history of nonoperative management of AAA, which may be particularly important in patients at advanced ages or with a limited life expectancy. No validation set is available for this index; the derivation set was 238 consecutive AAA patients enrolled from 1977 to 1988 from 1 institution in the Netherlands. It is unclear from the report7 whether the patients were enrolled prospectively. Until validated, we believe this decision aid needs to be cautiously applied.
FIGURE 3
InfoRetriever’s abdominal aortic aneurysm decision rule
Discussion And Conclusion
Based on our evaluation, we believe that few physicians will have detailed knowledge of the pertinent literature and the expertise to apply these risk indices accurately. However, the electronic implementation of the indices simplifies carrying them to the bedside. In our opinion, their main use is as checklists that serve as reminders of independent risk factors for adverse perioperative cardiac outcomes.
A major enhancement to each of these programs would be the addition of an opening screen that explained to which patients the program should be applied. However, the algorithmic preoperative management tools are well suited to the electronic and clinical environment.
Because the ACC/AHA decision support tool is newer (2002), we prefer it to the ACP tool (1997). STAT CC’s implementation is straightforward, occupies only 97K, and is free. For physicians who wish a low-, intermediate-, and high-risk classification, we recommend using Eagle’s 5-point, 3-class (0, 1–2, 3 points or more), easy-to-memorize scale (age >70, angina, prior MI [by history or ECG Q-waves], diabetes mellitus, congestive heart failure)—and forget the electronics.#
We believe an index such as the Detsky could (and should) be adapted for handheld computers, but the implementation of the versions we reviewed lack the features necessary for general utility. Such a version requires not only an explanation of angina classes, but also entry of pretest probability, specifically surgical risk for the surgical type. Many potential users probably will not know their institutions’ risk numbers for specific surgical types. Therefore, users should be assisted with estimating this entry based on literature values and suggestions about altering those values for the specific situation. While we like Steyerberg’s concept of estimating operative versus nonoperative mortality in AAA clinical decision-making, we await validation of this index.
1. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary: a report of the American College of Cardiology/American Heart Association Task Force onPractice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol 2002;39:542-53.
2. Guidelines for assessing and managing the perioperative risk from coronary artery disease associated with major noncardiac surgery-American College of Physicians. Ann Intern Med 1997;127:309-12.Also available at: http://www.acponline.org/journals/annals/15aug97/ppcad1.htm.
3. Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery. A multifactorial clinical risk index. Arch Intern Med 1986;146:2131-4.
4. Mangano DT, Goldman L. Preoperative assessment of patients with known or suspected coronary disease. N Engl J Med 1995;333:1750-6.
5. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043-9.
6. Detsky AS, Abrams HB, McLaughlin JR, et al. Predicting cardiac complications in patients undergoing non-cardiac surgery. J Gen Intern Med 1986;1:211-9.
7. Steyerberg EW, Kievit J, de Mol Van Otterloo JC, van Bockel JH, Eijkemans MJ, Habbema JD. Perioperative mortality of elective abdominal aortic aneurysm surgery. A clinical prediction rule based on literature and individual patient data. Arch Intern Med 1995;155:1998-2004.
8. L’Italien GJ, Paul SD, Hendel RC, et al. Development and validation of a Bayesian model for perioperative cardiac risk assessment in a cohort of 1,081 vascular surgical candidates. J Am Coll Cardiol 1996;27:779-86.
9. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297:845-50.
10. Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med 1985;313:793-9.
11. Romero L, de Virgilio C. Preoperative cardiac risk assessment: an updated approach. Arch Surg 2001;136:1370-6.
12. Hollenberg SM. Preoperative cardiac risk assessment. Chest 1999;115(suppl):51S-57S.
13. Paul SD, Eagle KA. A stepwise strategy for coronary risk assessment for noncardiac surgery. Med Clin North Am 1995;79:1241-62.
1. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary: a report of the American College of Cardiology/American Heart Association Task Force onPractice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol 2002;39:542-53.
2. Guidelines for assessing and managing the perioperative risk from coronary artery disease associated with major noncardiac surgery-American College of Physicians. Ann Intern Med 1997;127:309-12.Also available at: http://www.acponline.org/journals/annals/15aug97/ppcad1.htm.
3. Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery. A multifactorial clinical risk index. Arch Intern Med 1986;146:2131-4.
4. Mangano DT, Goldman L. Preoperative assessment of patients with known or suspected coronary disease. N Engl J Med 1995;333:1750-6.
5. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043-9.
6. Detsky AS, Abrams HB, McLaughlin JR, et al. Predicting cardiac complications in patients undergoing non-cardiac surgery. J Gen Intern Med 1986;1:211-9.
7. Steyerberg EW, Kievit J, de Mol Van Otterloo JC, van Bockel JH, Eijkemans MJ, Habbema JD. Perioperative mortality of elective abdominal aortic aneurysm surgery. A clinical prediction rule based on literature and individual patient data. Arch Intern Med 1995;155:1998-2004.
8. L’Italien GJ, Paul SD, Hendel RC, et al. Development and validation of a Bayesian model for perioperative cardiac risk assessment in a cohort of 1,081 vascular surgical candidates. J Am Coll Cardiol 1996;27:779-86.
9. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297:845-50.
10. Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med 1985;313:793-9.
11. Romero L, de Virgilio C. Preoperative cardiac risk assessment: an updated approach. Arch Surg 2001;136:1370-6.
12. Hollenberg SM. Preoperative cardiac risk assessment. Chest 1999;115(suppl):51S-57S.
13. Paul SD, Eagle KA. A stepwise strategy for coronary risk assessment for noncardiac surgery. Med Clin North Am 1995;79:1241-62.