User login
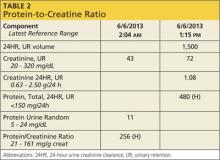
Q: Even though you suggested a random urine ACR (albumin-to-creatinine ratio), the internal medicine group ordered a 24-hour urine test for protein. As you can see from the results (see Table 2), the PCR (protein-to-creatinine ratio) is high. What does this mean? Does my patient have more severe kidney disease than I thought for her age?
Advanced age is a risk factor for CKD, and the patient has also had weight loss that can affect her serum creatinine. Because of her femur fracture, she has likely been in pain and probably has been taking nephrotoxic analgesics, such as NSAIDs or a ketorolac injection, commonly given postoperatively.
The patient’s weight does not appear to be stable, and she may have a degree of malnutrition. Both malnutrition and reduced muscle mass are known to decrease serum creatinine, which can mask worsening kidney disease. Thus she may have a lower true GFR than predicted by CG, which tends to overestimate renal function in the case of lower levels of creatinine production.6
Looking at all of these factors, it is likely that she has some degree of renal disease; however, it is important to determine if this is an acute change or a chronic issue. Looking closely at the higher-than-normal urinary protein result requires some out-of-the-box thinking.
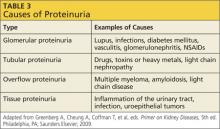
Proteinuria has four types; each indicates a particular disorder.5 Table 3 provides examples of causative factors for each type.
Based on the data provided (Table 2), you have a high urinary protein result and are unsure if it is albumin. It is important to determine if this is albumin—and therefore pathognomonic for progressive kidney disease—or if the protein is of a nonalbumin type that will require further evaluation. What started as just an elderly female with a femur fracture and decreased GFR can turn into a diagnosis of multiple myeloma (which is more common in this age-group), kidney damage from postoperative medications, or another form of kidney disease. Only by looking at urinary protein type can one “tease out” what this might be.
In conclusion, there are many different ways to determine renal function, either by creatinine clearance or by using an estimation formula. Each one, used correctly, can offer advantages in certain populations. It is extremely important to determine whether an individual has diminished kidney function in order to be able to delay the progression of CKD.
Catherine B. York, MSN, APRN-BC
Springfield Nephrology
Associates, Springfield, MO
References
1. CDC. National chronic kidney disease fact sheet: general information and national estimates on chronic kidney disease in the United States, 2010. Atlanta, GA: US Department of Health and Human Services, CDC; 2010.
2. US Renal Data System. USRDS 2012 annual data report: atlas of end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2012.
3. US Renal Data System. USRDS 2012 annual data report: atlas of end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2011.
4. Clarkson MR, Brenner BM. Clinical assessment of the patient with kidney disease. In: Clarkson MR, Brenner BM. Pocket Companion to Brenner & Rector’s The Kidney. 7th ed. Philadelphia, PA: Elsevier Saunders; 2005: 3-19.5.
5. Hsu C. Clinical evaluation of kidney function. In: Greenberg A, Cheung A, Coffman T, et al, eds. Primer on Kidney Diseases, 5th ed. Philadelphia, PA; Saunders Elsevier; 2009:19-237.
6. Kidney Disease Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1-150.
7. National Kidney Foundation. Guideline 5: assessment of proteinuria. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification; 2000.
8. Stevens LA, Coresh J, Greene T, et al. Assessing kidney function-measured and estimated glomerular filtration rate. N Engl J Med. 2006;354:2473-2483.
Q: Even though you suggested a random urine ACR (albumin-to-creatinine ratio), the internal medicine group ordered a 24-hour urine test for protein. As you can see from the results (see Table 2), the PCR (protein-to-creatinine ratio) is high. What does this mean? Does my patient have more severe kidney disease than I thought for her age?
Advanced age is a risk factor for CKD, and the patient has also had weight loss that can affect her serum creatinine. Because of her femur fracture, she has likely been in pain and probably has been taking nephrotoxic analgesics, such as NSAIDs or a ketorolac injection, commonly given postoperatively.
The patient’s weight does not appear to be stable, and she may have a degree of malnutrition. Both malnutrition and reduced muscle mass are known to decrease serum creatinine, which can mask worsening kidney disease. Thus she may have a lower true GFR than predicted by CG, which tends to overestimate renal function in the case of lower levels of creatinine production.6
Looking at all of these factors, it is likely that she has some degree of renal disease; however, it is important to determine if this is an acute change or a chronic issue. Looking closely at the higher-than-normal urinary protein result requires some out-of-the-box thinking.
Proteinuria has four types; each indicates a particular disorder.5 Table 3 provides examples of causative factors for each type.
Based on the data provided (Table 2), you have a high urinary protein result and are unsure if it is albumin. It is important to determine if this is albumin—and therefore pathognomonic for progressive kidney disease—or if the protein is of a nonalbumin type that will require further evaluation. What started as just an elderly female with a femur fracture and decreased GFR can turn into a diagnosis of multiple myeloma (which is more common in this age-group), kidney damage from postoperative medications, or another form of kidney disease. Only by looking at urinary protein type can one “tease out” what this might be.
In conclusion, there are many different ways to determine renal function, either by creatinine clearance or by using an estimation formula. Each one, used correctly, can offer advantages in certain populations. It is extremely important to determine whether an individual has diminished kidney function in order to be able to delay the progression of CKD.
Catherine B. York, MSN, APRN-BC
Springfield Nephrology
Associates, Springfield, MO
References
1. CDC. National chronic kidney disease fact sheet: general information and national estimates on chronic kidney disease in the United States, 2010. Atlanta, GA: US Department of Health and Human Services, CDC; 2010.
2. US Renal Data System. USRDS 2012 annual data report: atlas of end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2012.
3. US Renal Data System. USRDS 2012 annual data report: atlas of end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2011.
4. Clarkson MR, Brenner BM. Clinical assessment of the patient with kidney disease. In: Clarkson MR, Brenner BM. Pocket Companion to Brenner & Rector’s The Kidney. 7th ed. Philadelphia, PA: Elsevier Saunders; 2005: 3-19.5.
5. Hsu C. Clinical evaluation of kidney function. In: Greenberg A, Cheung A, Coffman T, et al, eds. Primer on Kidney Diseases, 5th ed. Philadelphia, PA; Saunders Elsevier; 2009:19-237.
6. Kidney Disease Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1-150.
7. National Kidney Foundation. Guideline 5: assessment of proteinuria. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification; 2000.
8. Stevens LA, Coresh J, Greene T, et al. Assessing kidney function-measured and estimated glomerular filtration rate. N Engl J Med. 2006;354:2473-2483.
Q: Even though you suggested a random urine ACR (albumin-to-creatinine ratio), the internal medicine group ordered a 24-hour urine test for protein. As you can see from the results (see Table 2), the PCR (protein-to-creatinine ratio) is high. What does this mean? Does my patient have more severe kidney disease than I thought for her age?
Advanced age is a risk factor for CKD, and the patient has also had weight loss that can affect her serum creatinine. Because of her femur fracture, she has likely been in pain and probably has been taking nephrotoxic analgesics, such as NSAIDs or a ketorolac injection, commonly given postoperatively.
The patient’s weight does not appear to be stable, and she may have a degree of malnutrition. Both malnutrition and reduced muscle mass are known to decrease serum creatinine, which can mask worsening kidney disease. Thus she may have a lower true GFR than predicted by CG, which tends to overestimate renal function in the case of lower levels of creatinine production.6
Looking at all of these factors, it is likely that she has some degree of renal disease; however, it is important to determine if this is an acute change or a chronic issue. Looking closely at the higher-than-normal urinary protein result requires some out-of-the-box thinking.
Proteinuria has four types; each indicates a particular disorder.5 Table 3 provides examples of causative factors for each type.
Based on the data provided (Table 2), you have a high urinary protein result and are unsure if it is albumin. It is important to determine if this is albumin—and therefore pathognomonic for progressive kidney disease—or if the protein is of a nonalbumin type that will require further evaluation. What started as just an elderly female with a femur fracture and decreased GFR can turn into a diagnosis of multiple myeloma (which is more common in this age-group), kidney damage from postoperative medications, or another form of kidney disease. Only by looking at urinary protein type can one “tease out” what this might be.
In conclusion, there are many different ways to determine renal function, either by creatinine clearance or by using an estimation formula. Each one, used correctly, can offer advantages in certain populations. It is extremely important to determine whether an individual has diminished kidney function in order to be able to delay the progression of CKD.
Catherine B. York, MSN, APRN-BC
Springfield Nephrology
Associates, Springfield, MO
References
1. CDC. National chronic kidney disease fact sheet: general information and national estimates on chronic kidney disease in the United States, 2010. Atlanta, GA: US Department of Health and Human Services, CDC; 2010.
2. US Renal Data System. USRDS 2012 annual data report: atlas of end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2012.
3. US Renal Data System. USRDS 2012 annual data report: atlas of end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2011.
4. Clarkson MR, Brenner BM. Clinical assessment of the patient with kidney disease. In: Clarkson MR, Brenner BM. Pocket Companion to Brenner & Rector’s The Kidney. 7th ed. Philadelphia, PA: Elsevier Saunders; 2005: 3-19.5.
5. Hsu C. Clinical evaluation of kidney function. In: Greenberg A, Cheung A, Coffman T, et al, eds. Primer on Kidney Diseases, 5th ed. Philadelphia, PA; Saunders Elsevier; 2009:19-237.
6. Kidney Disease Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1-150.
7. National Kidney Foundation. Guideline 5: assessment of proteinuria. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification; 2000.
8. Stevens LA, Coresh J, Greene T, et al. Assessing kidney function-measured and estimated glomerular filtration rate. N Engl J Med. 2006;354:2473-2483.