ECG Challenge
His Head Is In the Game–His Heart, Not So Much
A company racquetball tournament takes a turn for the worse when this 47-year-old man suddenly collapses. Despite complaining of chest discomfort...
Lyle W. Larson, PhD, PA-C, is clinical faculty in the Department of Medicine, Division of Cardiology, Cardiac Electrophysiology, at the University of Washington, Seattle.
A 70-year-old man recently diagnosed with prostate cancer is undergoing preoperative assessment for prostate surgery. His cardiac history is remarkable for longstanding hypertension, which has been well-managed with diuretics and a ß-blocker. Three years ago, he developed exertional angina. He underwent stress testing, was started on isosorbide dinitrate, and has had no further episodes.
He also has chronic obstructive pulmonary disease (COPD) due to chronic smoking, and sleep apnea for which he uses a continuous positive airway pressure (CPAP) device at night.
At age 24, he had an appendectomy for a ruptured appendix. The patient’s surgical history also includes bilateral total knee replacements (seven and eight years ago) and a laparoscopic cholecystectomy (converted to an open procedure due to adhesions) three years ago.
The patient is a retired mail carrier, a widower, and one of the most active members in his retirement community. Each night, he drinks one to two glasses of Scotch, and he has smoked one pack of cigarettes every day since he was 16. He has no interest in breaking either habit.
Family history reveals a father and mother who succumbed to myocardial infarction. His older brother died of complications following surgery, and his sister died of breast cancer.
The patient’s current medication list includes hydrochlorothiazide, metoprolol, and isosorbide dinitrate. He is allergic to sulfa, with a documented anaphylactic reaction in early adulthood. During the review of systems, he mentions that his heart has been “thumping” irregularly off and on for the past couple of months, corresponding with the expiration of his metoprolol prescription. He decided to wait for his preoperative assessment to have it refilled.
Vital signs include a blood pressure of 130/84 mm Hg; pulse, 110 beats/min and irregular; and temperature, 97.8°F.
On physical exam, his weight is 234 lb and his height, 69 in. He is a pleasant, euphoric male in no distress. He wears corrective lenses and hearing aids. Pertinent physical findings include crackles in both lower lung fields that clear with coughing; an irregularly irregular heart rhythm with an occasional early systolic murmur heard at the left upper sternal border; multiple old abdominal surgical scars; and surgical scars consistent with bilateral knee replacements. He is neurologically intact.
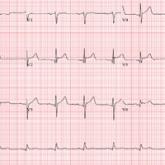
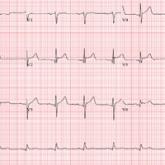
An ECG reveals a ventricular rate of 110 beats/min; QRS duration, 144 ms; QT/QTc interval, 298/403 ms; P axis, unmeasurable; R axis, –36°; T axis, 169°. What is your interpretation?
This ECG shows atrial fibrillation with aberrancy and a rapid ventricular response, left-axis deviation, and a left bundle branch block (LBBB).
While the physical exam can identify atrial fibrillation with a rapid ventricular response, an ECG is necessary to determine left-axis deviation and LBBB.
Left-axis deviation is evidenced by an R axis of –36°.
Aberrancy is identified by a QRS duration > 120 ms with poor R wave progression in precordial leads V 1 to V 3 and a wide positive R wave in V 5 and V 6.
Of note, the 10th beat on the rhythm strip is narrow and complex and is not aberrantly conducted.
A company racquetball tournament takes a turn for the worse when this 47-year-old man suddenly collapses. Despite complaining of chest discomfort...

While shoveling gravel several days ago, a 62-year-old man developed exertional angina. Though he stopped to rest, the pain persisted and radiated...

One week ago, a 67-year-old African-American woman with a history of diabetes, hypertension, and smoking developed a nonproductive cough and chest...
