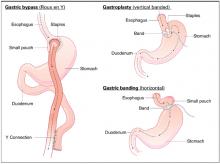
Gastric bypass results in weight loss of approximately 33% at 2 years and 25% at 8 years (strength of recommendation [SOR]: B, based on a cohort study). Gastric bypass is one type of bariatric surgery, which also includes gastroplasty and gastric banding procedures ( Figure 1 ). These procedures all can produce enough weight loss to measurably improve health, but they differ in the amount of long-term weight loss, as well as side effects, which can be serious.
Gastric bypass is more effective than gastroplasty for weight loss and is associated with fewer revisions, but it has more side effects (SOR: A, based on a systematic review). Limited evidence suggests that gastric bypass produces more weight loss than gastric banding (SOR: B, based on a cohort study).
Bariatric surgery, including gastric bypass, improves conditions comorbid with obesity, including diabetes, abnormal lipid profiles, and low quality-of-life scores. It decreases the incidence of hypertension at 2 years after surgery, but whether this effect is sustained is unclear (SOR: B, based on a cohort study and multiple case series). Bariatric surgery also improves obstructive sleep apnea, obesity hypoventilation syndrome, menstrual irregularity, and female urinary stress incontinence (SOR: C, based on multiple case series). Bariatric surgery has a complication rate of 13% and a mortality rate of 0.2% (SOR: B, based on 1 cohort study).
FIGURE 1
Bariatric surgical techniques for weight loss
Evidence summary
A systematic review comparing bariatric surgery with conventional medical therapy for obesity included 1 randomized controlled trial and the Swedish Obesity Study, a large cohort study with matched controls. Surgery produced 23 to 28 kg more weight loss at 2 years.1 The study demonstrated 33% ± 10% weight loss for gastric bypass and 0% for medical therapy (not described) at 2 years,2 and 25% ± 6% loss vs 0.9% gain at 8 years.3 Among bariatric surgical techniques, patients undergoing gastric bypass lost more weight than those with gastroplasty (using staples to partition the stomach, either horizontally or vertically ( Figure 1 ) (P=.057, not significant) or gastric banding (placing a constricting ring around the stomach) (P<.05) at 8 years.3
The same systematic review assessed multiple randomized controlled trials comparing gastric bypass with gastroplasty and found greater weight loss, fewer revisions, and more side effects from gastric bypass ( Figure 2 ).1 Five trials comparing gastric bypass with horizontal gastroplasty demonstrated significantly greater weight loss from gastric bypass. Five other trials comparing weight loss from gastric bypass with vertical gastroplasty produced mixed results, with 3 trials favoring gastric bypass and 2 showing no difference.1 Fewer patients required revision after gastric bypass (0%–4%) compared with vertical gastroplasty (9%) or horizontal gastroplasty (19%–40%). One included trial found that postoperative dumping syndrome (28% vs 0%, P<0.05) and heartburn (59% vs 32%, P<.05) were more common with gastric bypass than with gastroplasty.1
Bariatric surgery, including gastric bypass, improves a variety of obesity-related comorbid conditions. Diabetes prevalence decreased among gastric bypass patients at 2 years (0.0% vs 4.7%, P<0.005) and 8 years (3.6% vs 18.5%, P<.0005) compared with those receiving medical therapy.2,3 In a case series involving 154 diabetic gastric bypass patients, diabetes resolved for 83% by 1 year, and for 86% at 5 to 7 years.4 In several case series, most patients became euglycemic and discontinued insulin or oral agents.
In the Swedish Obesity Study, hypertriglyceridemia decreased postoperatively but hypercholesterolemia did not.5 In a case series, bariatric surgery reduced triglycerides (50%) as well as total cholesterol (15%) (P<.05 for both) at 6 months and significantly increased high-density lipoprotein cholesterol levels at 1 and 5 years.6
Bariatric surgery significantly lowered the incidence of hypertension at 2 years (3.2%) compared with conventional treatment (9.9%), but after 8 years this difference disappeared.2,3,5 However, in multiple large case series with morbidly obese patients, hypertension resolved or improved. The largest study showed resolution of hypertension for 69% at 1 to 2 years (91% follow-up), 66% at 5 to 7 years (50% follow-up), and 51% at 10 to 12 years (37% follow-up).4
Bariatric surgery improved obstructive sleep apnea and obesity hypoventilation syndrome in 2 case series. In one, Epworth Sleepiness Scale scores, minimum O2 saturation, and other measures improved significantly (P<.001) by 3 to 21 months after surgery.7